My Medicine Notes
Table of Contents
- Aesthetics
- Allergy/Immunology
- Behavioral Medicine
- 5A's
- 5 A's behavior change model edit
- Anger and Emotions
- Anxiety Traps
- BATHE Technique
- CBT (Cognitive Behavioral Therapy) Technique edit
- CBT Tools
- CBT Videos edit
- Child psych
- Coping strategies to teach patients
- Divorce edit
- Empathy
- Exposure Therapy for OCD: Exposure and Response Prevention (ERP)
- Gratitude
- HRV and stress edit 2024
- Managing anger and disappointment
- Military Psychiatry
- Mindfulness
- Motivational Interviewing (MI)
- Online Therapy Services edit
- Opposite Action
- PLISSIT Technique
- Shared decision making
- Stages of Change
- Stop Catastrophizing
- Study: Anger is eliminated with the disposal of a paper written because of provocation
- Study: Bypassing versus correcting misinformation: Efficacy and fundamental processes
- Study: Gratitude and Loneliness: Enhancing Health and Well-Being in Older Adults
- Study: How Breath-Control Can Change Your Life: A Systematic Review on Psycho-Physiological Correlates of Slow Breathing
- Study: Latent Diversity in Human Concepts (Language hinders discourse)
- Study: The Relationship Between Gratitude and Loneliness: The Potential Benefits of Gratitude for Promoting Social Bonds
- Study: The utility of prolonged respiratory exhalation for reducing physiological and psychological arousal in non-threatening and threatening situations
- Study: Gratitude and Mortality Among Older US Female Nurses
- Study: The Effort Paradox: Effort Is Both Costly and Valued
- Study: Comparing the Effects of Square, 4-7-8, and 6 Breaths-per-Minute Breathing Conditions on Heart Rate Variability, CO2 Levels, and Mood
- Breathing 4-7-8 - Study: Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults
- Calculators
- Cardiology
- 4 Factors of O2 Consumption For Heart Work
- 5 Most Common Causes Of Sudden Cardiac Death In Young Athletes
- Abdominal Aortic Aneurysm (AAA)
- ACC Tools
- AHA's Simple Seven
- Arrhythmias
- ASCVD
- Basic Life Support (BLS)
- Cardiac Clearance for Surgery
- Cardiac Medications
- Cardiology Differential
- Cardiovascular Fitness (CRF)
- Carotid Artery Stenosis
- Carotid US Screening
- Chest pain
- Common triggers for AF edit
- Compression Socks edit
- Coronary Artery Calcium Score
- Coronary Artery Disease
- Costochondritis and Tietze's syndrome edit
- CVA
- D-Dimer increased plasma values
- Differential Diagnosis and Treatment of Chest Wall Conditions
- Patient Thrombotic Risk Definitions
- Deep Venous Thrombosis
- Eating Eggs Is Not Associated with Cardiovascular Disease
- EKG
- Heart Failure
- Hyperlipidemia
- Hypertension
- Inappropriate Sinus Tachycardia
- Lymphadenopathy
- Lymphedema
- Max/Target Heart Rate
- Metabolic Equivalents (METS)
- Murmurs
- Orthostatic Hypotension
- OTC Blood Pressure Cuffs
- Patient Messaging: Venous Insufficiency edit
- Peripheral Arterial Disease
- Post MI Medications
- Postural orthostatic tachycardia syndrome (POTS)
- Prognostic Significance of Between-Arm Blood Pressure Differences edit
- Reduce Leg Swelling edit
- Study: Long-Term Effect of Salt Substitution for Cardiovascular Outcomes
- Study: Rate Control With Beta-blockers Versus Calcium Channel Blockers in the Emergency Setting: Predictors of Medication Class Choice and Associated Hospitalization
- Study: Replacing salt with low-sodium salt substitutes (LSSS) for cardiovascular health in adults, children and pregnant women edit
- Study: Use of Cardiac Troponin Testing in the Outpatient Setting edit
- Troponin Increased Plasma Values
- Prevention of Thromboembolism Guidelines for Atrial Fibrillation edit
- Study: Assessment of ASCVD Risk in Primary Prevention edit
- Dental
- Study: The Prophylactic Extraction of Third Molars: A Public Health Hazard
- Study: Imaging modalities to inform the detection and diagnosis of early caries
- Study: Recall intervals for oral health in primary care patients
- Fluoride Supplementation in Community Water Question
- Dental Antibiotic Prophylaxis
- Study: Common Oral Conditions A Review
- Dermatology
- 9 tips to help prevent derm biopsy mistakes
- Acne
- Acne Rosacea
- Alopecia (Hair Loss)
- Atopic Dermatitis (Eczema)
- Bed Bugs
- Best treatment for mild-mod acne vulgaris
- Burns
- Carcinomas (Basal Cell and Cutaneous Squamous Cell)
- Cellulite edit
- Chronic Urticaria
- Common Benign Skin Tumors edit
- Dermatology Procedures
- Dermoscopy
- Folliculitis
- Hidradenitis suppurativa
- Hyperpigmentation
- Infections, Insect bites, and Stings
- Ingrown Nail
- Keloids and Hypertrophic Scars
- Lice Treatment
- Medications
- Melanoma
- Milaria (Heat Rash) edit
- Molluscum
- Nail Abnormalities
- Nevus
- Nonscarring Hair Loss
- OCP and Acne
- Onychomycosis
- Paronychia
- Perioral dermatitis
- Pigmentation Disorders
- Pruritis edit
- Psoriasis
- Seborrheic Dermatitis
- Sebacceous Cysts
- Skin Protection
- Skin Type Classification
- Terminology
- Tinea Management Pitfalls
- Topical Corticosteroids
- Xanthoma edit
- Wood's Light edit
- Drugs/Medications/Supplements
- Adverse Effects: 10 Most Commonly Filled Prescription Medications in 2019
- Adverse Effects: Opioids
- Alcohol Use
- Antidepressants
- Antidepressants and Sexual Function
- Antidepressants and Weight edit
- Study: Initial Severity and Antidepressant Benefits: A Meta-Analysis of Data Submitted to the Food and Drug Administration
- Study: The loss of efficacy of fluoxetine in pediatric depression: explanations, lack of acknowledgment, and implications for other treatments
- Ashwagandha
- Auvelity Notes
- Benzodiazepines edit
- Bupropion
- Caffeine
- CAM with evidence
- Cannabis/Marijuana
- Cannabis and Adolescents
- Study: Association of Cannabis Use With Cardiovascular Outcomes Among US Adults
- Study: Brain Function Outcomes of Recent and Lifetime Cannabis Use
- Study: Cannabinoids, cannabis, and cannabis-based medicine for pain management: a systematic review of randomised controlled trials
- Study: Cannabis and Male fertility edit
- Study: Cannabis Use Disorder and Subsequent Risk of Psychotic and Nonpsychotic Unipolar Depression and Bipolar Disorder
- Study: Chest CT Findings in Marijuana Smokers
- Study: Daily Marijuana Use is Associated With Incident Heart Failure: "All of Us" Research Program edit
- Study: Evaluating the impact of cannabinoids on sleep health and pain in patients with chronic neuropathic pain: a systematic review and meta-analysis of randomized controlled trials
- Study: Frequent marijuana use linked to heart disease
- Study: Incident testicular cancer in relation to using marijuana and smoking tobacco: A systematic review and meta-analysis of epidemiologic studies
- Study: Increased Risk of Major Adverse Cardiac and Cerebrovascular Events in Elderly Non-Smokers With Cannabis Use Disorder: A Population-Based Analysis edit
- Study: Marijuana and Cardiovascular Disease
- Study: Marijuana linked to higher PAD risk
- Study: Myocardial Infarction and Cardiovascular Risks Associated with Cannabis Use: A Multicenter Retrospective Study
- Study: Nondisordered Cannabis Use Among US Adolescents
- Study: Prenatal cannabis exposure associated with mental disorders in children that persist into early adolescence
- Study: The placebo response in cannabinoid trials for clinical pain
- Study: Therapeutic Use of Cannabis and Cannabinoids: A Review edit
- Chocolate
- Chronic use of NSAIDs and COX-2 inhibitors:
- Continuous Glucose Monitoring (CGM)
- Contraception
- Controlled medications
- Controlled Medications (Schedule drugs) FL
- Corticosteroids
- Coumadin (Warfarin) Dosing/Management
- Creatine Supplementation
- diclofenac
- Dispose of medications
- Folic Acid Supplementation Lowers Suicide Events
- GLP-1 Agonists
- Study: Tirzepatide for the Treatment of Obstructive Sleep Apnea and Obesity
- Study: Associations of semaglutide with incidence and recurrence of alcohol use disorder in real-world population
- Study: Semaglutide and Tirzepatide reduce alcohol consumption in individuals with obesity
- Study: Exenatide once weekly for alcohol use disorder investigated in a randomized, placebo-controlled clinical trial
- Study: Repurposing Semaglutide and Liraglutide for Alcohol Use Disorder
- Glucocorticoid Equivalents
- Iron (Fe) Supplementation
- Ketamine for Depression
- Medication Prescription Helps
- Medication Resources
- Medication thoughts relating to homeless persons/street
- Medicine Reconciliation and Medical Error
- Metformin Tips
- Methotrexate (MTX)
- Metoprolol
- Muscle Relaxers edit
- My (Formulary) Goto/Easy medication choices
- My Medication Rules
- Naltrexone: Low Dose Naltrexone
- Nitrofurantoin (Macrobid vs Macrodantin)
- OTC Symptom Management edit
- oxymetazoline (Afrin)
- Pharmacies: Canadian Pharmacies
- Pharmacies: Compounding Pharmacies edit
- Pharmacies: On-line Discount Pharmacies
- Pharmacies: Publix Save on Medications
- Placebo Effects
- Pregnancy
- Probiotics
- Procedural Sedation and Analgesia
- Protocol for radiocontrast in high-risk patients (Contrast Allergy)
- Pseudoephedrine (Sudafed)
- Quviviq
- SGLT2 Inhibitors
- Sick call med list
- Stimulants
- Top 100 Most Prescribed Drugs in the US (2023 Data)
- Topical Medications
- Topical Retinoids edit
- Vicks 44
- Vitamins, Minerals, and Supplements
- Study: Multivitamin Use and Mortality Risk in 3 Prospective US Cohorts
- Ashwagandha (Withania somnifera)
- B complex
- Calcium
- Green tea (Camellia sinensis)
- Herbs
- Magnessium
- Minerals
- Omega-3
- On Supplements
- Vitamin B12 /Vit B12 Deficiency
- Vitamin C for preventing and treating the common cold
- Vitamin D
- Fish Oil:
- Testosterone
- CGM Standard Written Order edit
- DME Suppliers edit
- Endocrine
- Cortisol Levels are likely Good
- Cushing Syndrome
- Diabetes
- Cutaneous Signs
- Diabetes self-management and support (DSME/S)
- DKA and HHS Management
- DM visit EBM
- General Notes
- HbA1C and Estimated Average Glucose Level
- Iatrogenic Hypoglycemia
- Insulin
- Diabetic Neuropathy
- Management Plan for Type 2
- Oral medications
- Self-monitoring
- Special tests to classify DM
- Weight loss in pts with DM 2
- Sulfonylureas (SU)
- Estradiol (Vaginal) edit
- Glucocorticoid-Induced Adrenal Insufficiency edit
- Hormone Replacement Therapy edit
- Continuous Glucose Monitoring
- Pre-Diabetes
- Testosterone
- Thyroid
- Diabetes Type 1 (T1D)
- ENT (Otolaryngology)
- Allergic rhinitis
- Allergy tips
- Anosmia
- Aphthous Stomatitis (Canker Sores)
- Cerumen
- Chronic Rhinosinusitis
- Hoarseness
- Motion Sickness/Vestibular Nause
- Neti Pots
- Olfactory Training edit
- Otitis Externa
- Patient Messaging: Protect ears during scuba diving
- Pulsatile Tinnitus
- Rhinitis
- Sinusitis
- Sore throat
- Spots on Tongue edit
- Temporomandibular joint dysfunction syndrome (TMJ) Pain edit
- Tinnitis
- Gastroenterology
- Albumin/Globulin
- Antiemetics Selection
- Barrett Esophagus
- Bowel cleansing
- Bowel Medicines
- Celiac Sprue/Gluten Insensitivity edit
- Liver Cirrhosis
- Patient Messaging: Liver Cirrhosis
- Diagnosis and Initial Assessment
- Treating the Underlying Cause
- Lifestyle Modifications and Nutrition
- Immunizations and Medication Safety
- Surveillance
- Management of Complications
- Symptom Management
- Care Coordination and Transplant Evaluation
- References
- Ascites treatment
- Acute variceal hemorrhage
- Colonoscopy
- Colorectal Cancer Screening
- Constipation
- Diarrhea
- Dietary Fats
- Diverticulitis
- Dyspepsia
- Elevated Liver Transaminase Levels
- Flatus and Bloating
- Flatus control
- Food Allergies
- Food-Borne Illnesses edit
- Gall bladder Diet edit
- Gastroesophageal Reflux Disease (GERD)
- Gastrointestinal Bleeding
- Gastroparesis
- Hemorrhoids
- Irritable Bowel Syndrome
- IBS Diagnosis (Rome IV)
- Diagnostic Criteria
- Evaluation
- Alarm Features Suggesting the Possible Need for Further Testing
- IBS with Constipation:
- IBS with Diarrhea:
- Mixed IBS:
- IBS Treatment/Management:
- First-Line Management of IBS and Other Functional Gastrointestinal Disorders
- Diet: Avoid Gas producing foods
- Diet: General IBS Dietary Ideas
- Diet: Low FODMAP Diet
- Diet: FODMAP Food Reference
- FoodMarble - MedAIRE and MedAIRE2 edit
- Jaundice
- MicrosCopic (Lymphocytic And Collagenous) Colitis
- Model for End-Stage Liver Disease (MELD Score) edit
- NAFLD
- Pancreatitis - Chronic
- Rectal Prolapse
- SIBO
- Transaminases
- Gallstone Diet Patient Instructions
- Low FODMAP Apps
- Geriatrics
- Constipation in Elderly
- Delirium
- Dementia
- Driving safety edit
- End of Life Care
- Falls
- Frailty
- Hospice
- Indications for Mental Health Referral
- Early Signs of Dementia vs Normal Cognitive Changes Related to Aging
- Insomnia in Geriatrics
- Medications in Geriatrics
- Mobility Assist Devices
- One-legged Stand
- Osteoporosis
- Osteoporosis
- Preoperative Evaluation and Frailty Assessment in Older Patients edit
- Study: Abdominal fat depots are related to lower cognitive functioning and brain volumes in middle-aged males at high Alzheimer's risk
- Study: Hypertension linked to Alzheimer's disease via stroke: Mendelian randomization
- Study: Hypertension and Alzheimer's disease pathology at autopsy: A systematic review
- Study: Blood Pressure, Antihypertensive Use, and Late-Life Alzheimer and Non-Alzheimer Dementia Risk: An Individual Participant Data Meta-Analysis
- Study: Heavy resistance training at retirement age induces 4-year lasting beneficial effects in muscle strength: a long-term follow-up of an RCT
- Study: Galantamine for Alzheimer's disease and mild cognitive impairment edit
- Study: Nonlinear dynamics of multi-omics profiles during human aging
- Study: What Is the Association Between Music-Related Leisure Activities and Dementia Risk? A Cohort Study
- Study: Topological turning points across the human lifespan edit
- Hematology/Oncology
- Abnormal bleeding or bruising
- Anemia
- CBC with differential
- False A1c Readings
- Gastric Cancer
- Hemoglobin C Disease edit
- Iron (Fe) Deficiency Anemia
- Lung Cancer Screening
- Lymphadenopathy Causes
- Meat Consumption and Cancer edit
- Unprocessed Red Meat and Processed Meat Consumption: Dietary Guideline Recommendations From the Nutritional Recommendations (NutriRECS) Consortium edit
- Consumption of red meat and processed meat and cancer incidence: a systematic review and meta-analysis of prospective studies edit
- Lifetime Risk of Developing or Dying From Cancer
- Multiple Myeloma
- Neutropenia
- Peripheral Lymphadenopathy (LAP) edit
- Polycythemia Vera
- Prostate Cancer
- Study: Projected Lifetime Cancer Risks From Current Computed Tomography Imaging
- Study: The Association Between Smartphone Use and Breast Cancer Risk Among Taiwanese Women: A Case-Control Study edit
- Infectious Disease
- Acute Bacterial Rhinosinusitis (ABRS)
- Acute Gastroenteritis
- Acute Respiratory Tract Infections
- Coronavirus Disease 2019 (COVID-19)
- FLCCC - Prevention Protocol (COVID-19)
- FLCCC - Early Outpatient Treatment Protocol (COVID-19)
- COVID Risk factors for Death and Hospitalization (Medicare Population)
- COVID Ideas/Opinions
- COVID Treatments
- COVID Vaccines
- EUA
- Masks
- Random Stats Stuff
- Outpatient COVID-19 Management
- Testing Guidance for COVID-19 - Jan 2022 edit
- Mortality Stuff
- Vaccine Stuff
- Cutaneous Larva Migrans
- Dog and Cat Bites
- FL Prevent Mosquito's edit
- Foodborne Pathogens
- Hepatitis B
- Hepatitis C
- HIV
- H. pylori
- Immunizations and Vaccines
- Insect Repellents
- Insects
- Monkeypox
- Otitis Externa
- Paronychia Home Care Instructions
- Pet Related Diseases
- Pharyngitis
- Pneumonia (Community Acquired)
- Postexposure Doxycycline to Prevent Bacterial Sexually Transmitted Infections edit
- Post Infectious Cough
- Procalcitonin
- Red flags in a child with diarrhea
- Scabies
- Sepsis
- Tick Borne Diseases
- Traveler's Diarrhea
- Tropical Diseases from geographic areas
- Uncomplicated Cystitis (UTI)
- Waterborne Illnesses
- Wounds
- Study: Upper Respiratory Tract Infection edit
- Misc Medicine
- 2024 Anchor Imaging edit
- 25 Most Common Diagnoses
- AAFP Online Help edit
- Advanced Directives
- Art and Philosophy of Medicine
- Benefits of a dog edit
- Biostatistics
- Key Concepts When Looking At Research Studies
- PICOTS for the Trial:
- Cancer Screening Definitions
- Example of Interpreting A Study Results (Just a 1% difference)
- Random Statistics in Medicine edit
- What did 95 Percent effective mean (COVID) edit
- Biostat Terms
- Shared Decision Making And Using Numbers
- Safety Statistics
- Life Expectancy
- p values
- Study: The (Mis)Reporting Of Statistical Results In Psychology Journals
- Books For Patients To Read From Library
- Chloride Levels
- Coding
- DCF Contact edit 2024
- Disability Tools edit
- Executive Physical Exam edit
- Family Medicine and AAFP
- Favorite Patient Quotes
- Federal Poverty Guidelines For 2023
- First Aid Kits edit 2025
- FL Emergency Kit Components edit
- Florida Things that Bite edit
- Fun Medical Definitions
- Grandmother's Rules of Life edit
- Health Insurance Analysis (Opinionated)
- Homeless Resources
- HSA Is OK With DPC Edit
- Human Trafficking edit
- Informed Consent 2025
- Insurance Notes edit
- Insurance Stuff
- Legal Stuff
- Lifestyle Medicine
- List of Physician Side Hustles
- Local Women's Shelter Resources
- Low Income Resources Central Florida edit
- Malpractice Risk Knowledge
- Medical Emergency Codes
- Medicare Advantage vs Medigap (supplemental) edit
- Medicine Tool Kit
- Physiology (Misc)
- Pt quotes edit
- Readmission
- Sample Letter From Health Care Provider: For Any Needed Accommodation
- Scope of Practice (For NP/PA) Expansion Talking Points (Opposition)
- Service Animals
- Social Media in Healthcare
- Study: Examining gender-specific mental health risks after gender-affirming surgery: a national database study
- Study: Racial and Ethnic Differences in Homework Time among U.S. Teens
- Teaching
- Tech Stuff
- Travel Medicine
- VA Nexus Letters
- Wellness Visits (Medicare)
- Study: Commercial Insurers Paid More For Procedures At Hospital Outpatient Departments Than At Ambulatory Surgical Centers
- Lab References
- Musculoskeletal/Orthopedics
- 52 WALKING FUN FACTS edit
- 90 Second MSK Sceening
- Acute Pain from Non-Low Back Musculoskeletal Injuries
- Ankle Pain
- Benefits of exercise
- Bone Stress Injury Prediction Rule
- Carpal Tunnel Syndrome
- Cervical Radiculopathy
- de Quervain tendinopathy
- EBM: Massage Therapy edit
- Endurance Athletes Common Conditions
- Endurance Athletes Overuse Injuries
- Finger injuries
- Foot Fractures
- Fractures: Foot
- Fractures in children
- Heel Pain
- Hip Pain in Adults
- Joint Injections
- Knee Pain
- Lateral ankle sprain
- Lateral/medial epicondyle pain
- Leg Cramps
- Low back pain
- Lumbar Spinal Stenosis
- Medial Collateral Ligament injury (MCL)
- Morton's Neuroma
- MSK Exams
- MSK Tests
- Nocturnal Leg Cramps
- Osteoarthritis
- Overtraining Syndrome
- Overtraining Syndrome (Review for accuracy) edit
- Peripheral nerve entrapment (Upper Extremity)
- Physical activity
- Plantar fasciitis
- Platelet-rich Plasma (PRP)
- Prolotherapy
- Rehab
- Relative Energy Deficiency in Sport (red-s) (Formerly Female Triad)
- Restless Leg Syndrome
- Running injuries
- Sacroiliac (SI) Joint Pain
- Shoulder
- Shoulder Impingement PT edit
- Sports Physicals
- Study: Diagnosis, treatment and prevention of ankle sprains: Update Of An Evidence-Based Clinical Guideline
- Study: Exercise Is the Only Intervention to Provide Long-Term Improvement in Patients with Chronic Low Back Pain
- Tendinopathy
- Trigger Finger
- VO2 Max
- Walking/Steps Evidence
- Muscle Spasms edit
- Patient Messaging: Physical Therapy Library edit
- Nephrology
- Neurology
- Altitude Sickness edit
- Bell's Palsy edit
- Bells Palsy
- BPPV
- Cerebral Vascular Accident
- Cervical Nerve Roots
- Concussions
- Assessment Tools
- Management
- Management - Post-Concussion Headache
- Return to Play (Student)
- School Accommodations (Student)
- Return to Play (Adult)
- Study: Is rest after concussion "the best medicine?": Recommendations for activity resumption following concussion in athletes, civilians, and military service members
- Concussion Advice
- Concussion Recognition Tool
- New Orleans criteria for CT after minor head injury
- Classification Of Sports/Risk Categories
- Military Primary Care Concussion Management
- Q-Collar
- Cranial Hemorrhages
- Degenerative cervical myelopathy edit
- Dementia
- Dizziness
- Headaches
- Neurological Physical Examination
- Neurologic Exam Components
- Parkinson and Mimics
- Peripheral Neuropathy
- Seizures
- Syncope
- Tension Headache edit
- Trigeminal Neuralgia
- Temporal Arteritis (Giant Cell Arteritis)
- Tremor
- Nutrition
- Beans/Legumes edit
- Biochemical Nutritional Indications
- Calories in Drinks and Popular Beverages
- Dietary Guidelines for Americans (2015-2020)
- Dietary patterns and changes
- Eat Nuts!
- EBM Food Intake and Diet
- Fats and Lipids
- Fiber
- FODMAP
- Food Intake Planning/Diets
- Guidance
- How Intermittent Fasting Affects Your Cells and Hormones
- Insulin and Weight
- Ketogenic Diet
- Low Glycemic Index
- Macronutrient Composition of Diet
- Macronutrient Ranges edit
- Mediterranean Diet edit
- Michi's Ladder of Healthy Food Choices edit
- Nutrition and Diet
- Optimizing foods for satiety edit
- Patient Messaging: General Nutrition Information
- Patient Messaging: Healthy food: 7 Affordable Ideas
- Patient Messaging: Intermittent Fasting (IF)
- Patient Messaging: Portion control
- Portions
- Recommended Daily Allowance for Macronutrients
- Recommended Nutrition For Muscle Injury
- Renal Diet/Lifestyle
- Study: Coffee and tea consumption and mortality from all causes, cardiovascular disease and cancer: a pooled analysis of prospective studies from the Asia Cohort Consortium
- Study: Detox diets for toxin elimination and weight management: a critical review of the evidence
- Study: Dietary Sugar Intake and Incident Type 2 Diabetes Risk: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies
- Study: Effect of Calorie Restriction on Mood, Quality of Life, Sleep, and Sexual Function in Healthy Nonobese Adults: The CALERIE 2 Randomized Clinical Trial
- Study: Optimal dietary patterns for healthy aging
- Study: Salad and satiety: energy density and portion size of a first-course salad affect energy intake at lunch
- Sugar
- Vegetarian Diets
- OB/GYN
- Advanced Lifesaving in Obstetrics (ALSO)
- Breast Cancer Risk Tool
- Breast Exam edit
- Breastfeeding
- Cervical Disease
- Chronic Pelvic Pain
- Colposcope Prediction: REID Index
- Contraindications to vaginal delivery
- Dysmenorrhea
- Dyspareunia
- EAB
- Abortion in Florida
- Study: Abortion, substance abuse and mental health in early adulthood: Thirteen-year longitudinal evidence from the United States
- Study: Emotions over five years after denial of abortion in the United States: Contextualizing the effects of abortion denial on women's health and lives
- Study: Global prevalence of post-abortion depression: systematic review and Meta-analysis
- Study: Perceived stress and emotional social support among women who are denied or receive abortions in the United States: a prospective cohort study edit
- Study: Socioeconomic Outcomes of Women Who Receive and Women Who Are Denied Wanted Abortions in the United States edit
- Study: Suicide risks associated with pregnancy outcomes: a national cross-sectional survey of American females 41-45 years of age
- Endometrial Biopsy
- Endometrial Thickness
- Fetal Monitoring
- GDM
- HCG Levels During Pregnancy
- Hormonal Contraceptives
- Hysterectomy Types
- Infertility
- IUD and Depression/Anxiety edit
- Study: Levonorgestrel intrauterine device and depression: A Swedish register-based cohort study
- Study: The potential association between psychiatric symptoms and the use of levonorgestrel intrauterine devices (LNG-IUDs): A systematic review
- Study: Association Between Intrauterine System Hormone Dosage and Depression Risk
- Study: Cohort Study of Psychiatric Adverse Events Following Exposure to Levonorgestrel-Containing Intrauterine Devices in UK General Practice
- IUD Comparisons edit
- Kegel Instructions
- Limited OB Ultrasound (ALSO)
- Mammograms
- Menopause
- Menstrual Irregularities
- Natural Family Planning
- Nipple discharge
- Oral Contraception
- Pap Recommendations
- Pelvic Exams
- Pelvic Pain (Acute)
- Polycystic Ovarian Syndrome (PCOS)
- Pregnancy status
- Premenstrual Syndrome (PMS)
- Prenatal Care
- Progesterone Use edit
- Risk factors for post partum hemorrhage
- Sexual Dysfunction In Women
- Uterine Bleeding
- Vaginitis
- Weight gain in Pregnancy
- Ophthalmology
- Pain
- Chronic Musculoskeletal Pain
- Facial pain
- Back pain
- Knee pain
- MSK Pain Guidelines edit
- Non-narcotic Medications
- Opioids
- Postherpetic neuralgia
- Resources
- Butrans (Buprenorphine Waiver Notification)
- CDC Opioids
- Controlled Meds edit
- Buprenorphone edit
- Spinal manipulative therapy for acute low‐back pain edit
- Understanding Buprenorphine for Use in Chronic Pain: Expert Opinion edit
- Urine Drug Testing edit
- Medication edit
- Monitoring Medication for Chronic Nonmalignant Pain edit
- Opioid Appropriate Documentation of Follow-up Visits edit
- CDC Opioid Recommendations edit
- Cannabis-Based Products for Chronic Pain edit
- Study: Physician Empathy and Chronic Pain Outcomes edit
- PDMP Overdose Risk Score edit
- Pediatrics
- 2023 Childhood Immunizations Edit
- Acute Gastroenteritis in Children
- Acute Migraines in Children
- ADHD Pediatric Management
- Bruising/Non-accidental Trauma
- Child Development
- Children (<3 yo) with a Fever
- Constipation (Newborn)
- Constipation (Pediatric)
- Croup
- Dermatologic Concerns
- Documentation: Newborn Exam
- Febrile Seizures
- Feeding schedule
- Functional Abdominal Pain in Children
- Hypertension (Pediatric)
- Orlando Pediatric Resources
- Parenting
- Pediatric Depression edit
- Pediatric Dosing: acetaminophen
- Pediatric Dosing: cetirizine
- Pediatric Dosing: dextromethorphan
- Pediatric Dosing: diphenhydramine
- Pediatric Dosing: ibuprophen
- Pediatric Dosing: loratadine
- Sleep
- Transgender and Pediatrics
- Urinary Tract Infections in Children
- Vital Signs
- Down's Syndrome
- Study: Epinephrine metered-dose inhaler for pediatric croup
- Psychiatry
- Addiction and Dependence
- ADHD
- Anxiety
- Autism
- Bipolar Disorder
- Cognitive Behavior Therapy
- Dialectal Behavior Therapy
- Depression
- Drugs that can cause psychosis
- Eating Disorders
- Emotional Support Animals in Florida
- Generic ADHD Stimulants edit
- Illness Anxiety Disorder (Hypochondriasis)
- Obsessive Compulsive Disorder (OCD)
- Personality Disorders
- Phobias
- Psychological Examination
- PTSD
- Sexual Dysfunction
- Somatic Symptom Disorder
- Study: Attending live sporting events predicts subjective wellbeing and reduces loneliness edit
- Study: Framing depression as a functional signal, not a disease: Rationale and initial randomized controlled trial
- Study: Ketamine versus ECT for Nonpsychotic Treatment-Resistant Major Depression
- Study: The brain structure, immunometabolic and genetic mechanisms underlying the association between lifestyle and depression edit
- Study: The serotonin theory of depression: a systematic umbrella review of the evidence
- Study: Watching sport enhances well-being: evidence from a multi-method approach
- Study: Watching sports and depressive symptoms among older adults: a cross-sectional study from the JAGES 2019 survey
- Suicide
- Study: How Breath-Control Can Change Your Life: A Systematic Review on Psycho-Physiological Correlates of Slow Breathing
- Study: A dose response relationship between accelerometer assessed daily steps and depressive symptoms in older adults: a two-year cohort study
- Study: Daily Step Count and Depression in Adults: A Systematic Review and Meta-Analysis
- Study: Efficacy and Safety of Selective Serotonin Reuptake Inhibitors, Serotonin-Norepinephrine Reuptake Inhibitors, and Placebo for Common Psychiatric Disorders Among Children and Adolescents: A Systematic Review and Meta-analysis edit
- Study: The efficacy of paroxetine and placebo in treating anxiety and depression: a meta-analysis of change on the Hamilton Rating Scales edit
- Study: Antidepressants versus placebo in major depression: an overview edit
- Study: Antidepressants versus placebo for depression in primary care edit
- Study: Meta-analysis of the association between gratitude and loneliness edit
- Suicide Risk And Documentation
- Attention-Deficit/Hyperactivity Disorder Medications and Long-Term Risk of Cardiovascular Diseases
- Autism-Spectrum Quotient (AQ)
- Autism edit
- Study: Explaining the increase in the prevalence of autism spectrum disorders: the proportion attributable to changes in reporting practices
- Study: Trends in Autism Prevalence: Diagnostic Substitution Revisited
- Study: Gender Dysphoria Report edit
- Study: Mapping the genetic landscape across 14 psychiatric disorders
- Study: Exposing Worry’s Deceit: Percentage of Untrue Worries in Generalized Anxiety Disorder Treatment
- Pulmonary
- Asthma
- Chronic Cough
- COPD
- Dyspnea
- Epworth Sleepiness Scale
- Incidental Pulmonary Nodules detected on CT Images
- Lung Ca Screening
- Pneumonia
- Predicted Peak Expiratory Flow (L/min)
- Pulmonary Function Tests
- Pulmonary Nodules
- Sleep and Insomnia
- Developmental Sleep Recommendations
- Chronic Insomnia
- Obstructive Sleep Apnea
- Sleep Hygiene Rules for the treatment of insomnia
- Sleep Restriction Therapy:
- The Army Quick Sleep Technique
- 4-6-7 Breathing Technique Will Knock You Out in 10 Minutes Flat
- Ways to get more sleep
- Jet Lag edit
- Sleep Study Results Explanation
- Sleep Duration Recommendations
- Study: A new method for measuring daytime sleepiness: the Epworth sleepiness scale
- Study: Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women
- Sleep Cycles and Napping edit
- Study: Sleep loss and emotion: A systematic review and meta-analysis of over 50 years of experimental research
- Patient Messaging: Avoiding Fatigue
- Spirometry
- Taking a nap (30/90 Rule)
- Tobacco (Smoking Cessation)
- Cytisine for Smoking Cessation, cheaper alternative to Chantix
- E-cigarette's users twice as likely to quit smoking
- Health Benefits After Quitting:
- Management
- Smoking and supplements
- Smoking USPSTF
- Tools, Apps, Resources
- Vaping and nicotine
- Smoking Cessation Messaging
- Smoking Cessation with patch edit
- Vocal Cord Dysfunction
- Radiology
- Rheumatology
- Studies: Activity and Exercise
- Evidence on Running
- Evidence regarding the Q collar
- Exercise As Medicine
- Patient Messaging: Exercise and Strength Building
- Stair Climbing
- Energy cost of walking and running at extreme uphill and downhill slopes
- Study: Brief Intense Stair Climbing Improves Cardiorespiratory Fitness
- Study: Energy cost of stair climbing and descending on the college alumnus questionnaire
- Study: The Energy Expenditure of Stair Climbing One Step and Two Steps at a Time: Estimations from Measures of Heart Rate
- Steps Daily edit 2025
- Study: Antidepressants or running therapy: Comparing effects on mental and physical health in patients with depression and anxiety disorders
- Study: Association of Daily Step Count and Intensity With Incident Dementia in 78,430 Adults Living in the UK
- Study: Association of Daily Step Patterns With Mortality in US Adults
- Study: Association of Timing of Moderate-to-Vigorous Physical Activity With Changes in Glycemic Control Over 4 Years in Adults With Type 2 Diabetes From the Look AHEAD Trial
- Study: Association of wearable device-measured vigorous intermittent lifestyle physical activity with mortality
- Study: Associations between cardiorespiratory fitness in youth and the incidence of site-specific cancer in men: a cohort study with register linkage
- Study: Cardiorespiratory fitness is a strong and consistent predictor of morbidity and mortality among adults: an overview of meta-analyses representing over 20.9 million observations from 199 unique cohort studies
- Study: Clinic and Park Partnerships for childhood resilience: A prospective study of park prescriptions
- Study: Daily Step Count and Depression in Adults - A Systematic Review and Meta-Analysis
- Study: Daily Steps And Health Outcomes In Adults: A Systematic Review And Dose-Response Meta-Analysis
- Study: Do the associations of daily steps with mortality and incident cardiovascular disease differ by sedentary time levels? A device-based cohort study
- Study: Effectiveness and cost-effectiveness of an individualised, progressive walking and education intervention for the prevention of low back pain recurrence in Australia (WalkBack): a randomised controlled trial
- Study: Effect of Moderate to Vigorous Physical Activity on All-Cause Mortality in Middle-aged and Older Australians
- Study: Effects of various exercise interventions in insomnia patients: a systematic review and network meta-analysis
- Study: Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men
- Study: Exercise training enhances muscle mitochondrial metabolism in diet-resistant obesity
- Study: Exploring the Relationship between Walking and Emotional Health in China
- Study: Higher resistance training volume offsets muscle hypertrophy nonresponsiveness in older individuals
- Study: Long-term time-course of strength adaptation to minimal dose resistance training: Retrospective longitudinal growth modelling of a large cohort through training records
- Study: Maximizing Muscle Hypertrophy: A Systematic Review of Advanced Resistance Training Techniques and Methods
- Study: Move less, spend more: the metabolic demands of short walking bouts
- Study: Movement Is Medicine: Structured Exercise Program May Lower Risk of Cancer Recurrence and Death for Some Colon Cancer Survivors
- Study: Non-occupational physical activity and risk of cardiovascular disease, cancer and mortality outcomes:s a dose–response meta-analysis of large prospective studies
- Study: Oral Salt Supplementation During Ultradistance Exercise
- Study: Progression Models in Resistance Training for Healthy Adults
- Study: Relationship of Daily Step Counts to All-Cause Mortality and Cardiovascular Events
- Study: Resistance Exercise Training in Individuals With and Without Cardiovascular Disease: 2023 Update: A Scientific Statement From the American Heart Association edit
- Marathon/Ultramarathon Endurance Related
- Study: Effect of Sodium Supplements and Climate on Dysnatremia During Ultramarathon Running
- Study: Different Predictor Variables for Women and Men in Ultra-Marathon Running—The Wellington Urban Ultramarathon 2018
- Study: Changes in Pain and Nutritional Intake Modulate Ultra-Running Performance: A Case Report edit
- Study: Effects of 120 g/h of Carbohydrates Intake during a Mountain Marathon on Exercise-Induced Muscle Damage in Elite Runners
- Study: Exercise-Associated Hyponatremia, Hypernatremia, and Hydration Status in Multistage Ultramarathons
- Study: Fluid Replacement during Marathon Running
- Study: Limits of Ultra: Towards an Interdisciplinary Understanding of Ultra-Endurance Running Performance edit
- Study: Predictor Variables for A 100-km Race Time in Male Ultra-Marathoners edit
- Study: Sleep and Subjective Recovery in Amateur Trail Runners After the Ultra-Trail du Mont Blanc® (UTMB®)
- Study: The Training Intensity Distribution of Marathon Runners Across Performance Levels
- Study: Ultra-Marathon Nutrition
- Study: Widespread drastic reduction of brain myelin content upon prolonged endurance exercise edit
- Study: Resistance Training Volume Enhances Muscle Hypertrophy but Not Strength in Trained Men
- Study: Screen-based entertainment time, all-cause mortality, and cardiovascular events: population-based study with ongoing mortality and hospital events follow-up
- Study: Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis
- Study: Spending at least 120 minutes a week in nature is associated with good health and wellbeing
- Study: Stair walking is more energizing than low dose caffeine in sleep deprived young women
- Study: Structured Exercise after Adjuvant Chemotherapy for Colon Cancer
- Study: The Acute Effects of Interrupting Prolonged Sitting Time in Adults with Standing and Light-Intensity Walking on Biomarkers of Cardiometabolic Health in Adults: A Systematic Review and Meta-analysis
- Study: The associations of "weekend warrior" and regularly active physical activity with abdominal and general adiposity in US adults
- Study: The training—injury prevention paradox: should athletes be training smarter and harder?
- Study: Timing of Moderate to Vigorous Physical Activity, Mortality, Cardiovascular Disease, and Microvascular Disease in Adults With Obesity
- Study: Vigorous Intermittent Lifestyle Physical Activity and Cancer Incidence Among Nonexercising Adults
- Study: Walking as an intervention to reduce blood pressure in adults with hypertension: recommendations and implications for clinical practise
- Study: Walk to a Better Night of Sleep: Testing the Relationship Between Physical Activity and Sleep
- Walking and energy use edit
- Walking increases life expectancy by 3.4-4.5 years - Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis
- Water/Electrolyte Balance Table
- Study: Are There Deleterious Cardiac Effects of Acute and Chronic Endurance Exercise?
- Study: Association between physical activity and risk of incident arrhythmias in 402,406 individuals: Evidence from the UK Biobank cohort
- Studies: COVID-19 Related
- Infection and Fatality Rates
- Study: The infection fatality rate of COVID-19 inferred from seroprevalence data (For those <70 yo ->0.00-0.57%)
- Study: Age-stratified infection fatality rate of COVID-19 in the non-elderly informed from pre-vaccination national seroprevalence studies
- Study: Community transmission (Vaccinated vs Unvaccinated)
- Study: Ct values and infectivity of SARS-CoV-2 on surfaces
- Lockdowns
- Natural Immunity
- Study: Natural Immunity is better than Vacinated Immunity against Delta Variant
- Study: Past SARS-CoV-2 infection protection against re-infection: a systematic review and meta-analysis
- Study: Protective effectiveness of previous SARS-CoV-2 infection and hybrid immunity against the omicron variant and severe disease: a systematic review and meta-regression
- Origin
- Prevention
- Study: Possible toxicity of chronic carbon dioxide exposure associated with face mask use, particularly in pregnant women, children and adolescents – A scoping review
- Study: Physical interventions to interrupt or reduce the spread of respiratory viruses (Chochrane review of masks)
- Study: FXR inhibition may protect from SARS-CoV-2 infection by reducing ACE2 (urodiol/actigall)
- Study: Japan supercomputer shows doubling masks offers little help preventing viral spread
- Study: Wastewater-based monitoring of SARS-CoV-2 at UK airports and its potential role in international public health surveillance (COVID travel restrictions on flying were a total failure)
- Study: N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel (RCT)
- Study: Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers (RCT)
- Study: Correlation Between Mask Compliance and COVID-19 Outcomes in Europe
- Study: Modeling the filtration efficiency of a woven fabric: The role of multiple lengthscales
- Study: Revisiting Pediatric COVID-19 Cases in Counties With and Without School Mask Requirements—United States, July 1—October 20 2021
- Study: Mask mandate and use efficacy in state-level COVID-19 containment
- Study: Associations of Physical Inactivity and COVID-19 Outcomes Among Subgroups (Physically active = less COVID symptoms)
- Study: Medical Masks Versus N95 Respirators for Preventing COVID-19 Among Health Care Workers (No difference)
- Study: Child mask mandates for COVID-19: a systematic review
- Study: Coffee as a dietary strategy to prevent SARS-CoV-2 infection edit
- Risk Factors
- Sequelae
- Study: Post-acute sequelae of SARS-CoV-2 associates with physical inactivity in a cohort of COVID-19 survivors
- Study: Development of a Definition of Postacute Sequelae of SARS-CoV-2 Infection
- Study: COVID-Specific Long-term Sequelae in Comparison to Common Viral Respiratory Infections: An Analysis of 17 487 Infected Adult Patients (The 7 Long Covid Symptoms)
- Study: Long COVID: major findings, mechanisms and recommendations
- Study: Machine learning links unresolving secondary pneumonia to mortality in patients with severe pneumonia, including COVID-19
- Study: Orthostatic tachycardia after covid-19
- Study: COVID does not increase incidence of neither pericarditis nor myocarditis
- Study: SARS-CoV-2 infection triggers pro-atherogenic inflammatory responses in human coronary vessels edit
- Testing
- Treatment
- Study: Antidepressant drug prescription and incidence of COVID-19 in mental health outpatients: a retrospective cohort study
- Study: Discriminatory Attitudes Against the Unvaccinated During a Global Pandemic
- Study: Alarming antibody evasion properties of rising SARS-CoV-2 BQ and XBB subvariants
- Study: Effectiveness of the Coronavirus Disease 2019 (COVID-19) Bivalent Vaccine
- Study: Evaluation of Waning of SARS-CoV-2 Vaccine–Induced Immunity
- Study: Vaccines and Serious Adverse Effects Rate
- Study: Sex-specific differences in myocardial injury incidence after COVID-19 mRNA-1273 Booster Vaccination
- Study: Aerobic exercises recommendations and specifications for patients with COVID-19: a systematic review
- Study: Association between vitamin D supplementation and COVID-19 infection and mortality edit
- Study: IgG4 Antibodies Induced by Repeated Vaccination May Generate Immune Tolerance to the SARS-CoV-2 Spike Protein
- Study: Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting
- Study: Exercise May Improve Fatigue Associated With Long COVID in Active Young Adults
- Study: Surveillance of COVID-19 vaccine safety among elderly persons aged 65 years and older (Temporal association with PE, AMI, DIC, and ITP)
- Study: Fenofibrate
- Study: Outcomes after early treatment with hydroxychloroquine and azithromycin: An analysis of a database of 30,423 COVID-19 patients
- Study: The role of COVID-19 vaccines in preventing post-COVID-19 thromboembolic and cardiovascular complications edit
- Study: Analysis of the Association Between BNT162b2 mRNA COVID-19 Vaccination and Deaths Within 10 Days After Vaccination Using the Sex Ratio in Japan edit
- Study: OpenSAFELY: Effectiveness of COVID-19 vaccination in children and adolescents
- Study: An analysis of studies pertaining to masks in Morbidity and Mortality Weekly Report: Characteristics and quality of all studies from 1978 to 2023 edit
- Study: A Critical Analysis of All-Cause Deaths during COVID-19 Vaccination in an Italian Province
- Study: Post Conditional Approval Active Surveillance Study Among Individuals in Europe Receiving the Pfizer-BioNTech Coronavirus Disease 2019 (COVID-19) Vaccine
- Study: Postacute sequelae of SARS-CoV-2 in the population: Risk factors and vaccines
- Study: Rates of successful conceptions according to COVID-19 vaccination status: Data from the Czech Republic
- Study: The impact of SARS-CoV-2 infection on vaccinated versus unvaccinated pregnant women: a retrospective cohort study
- Study: Impact of mRNA and Inactivated COVID-19 Vaccines on Ovarian Reserve
- Infection and Fatality Rates
- Studies: Weight Management
- Patient Messaging: Bariatric Surgery
- Reference: Weight Watcher's to Calorie Conversion edit
- Study: Alternate Day Fasting Combined With Endurance Exercise for the Treatment of Fatty Liver Disease
- Study: A population-based study of appetite-suppressant drugs and the risk of cardiac-valve regurgitation
- Study: A randomized double-blind placebo-controlled study of the long-term efficacy and safety of diethylpropion in the treatment of obese subjects
- Study: Association between insulin sensitivity and lean mass loss during weight loss
- Study: Brain responses to nutrients are severely impaired and not reversed by weight loss in humans with obesity: a randomized crossover study
- Study: Calorie Restriction with or without Time-Restricted Eating in Weight Loss
- Study: Changes in diet and lifestyle and long-term weight gain in women and men
- Study: Consumption of Soft Drinks and Overweight and Obesity Among Adolescents in 107 Countries and Regions
- Study: Continued Treatment With Tirzepatide for Maintenance of Weight Reduction in Adults With Obesity
- Study: Dietary Macronutrient Composition and Protein Concentration for Weight Loss Maintenance
- Study: Diets for weight management in adults with type 2 diabetes: an umbrella review of published meta-analyses and systematic review of trials of diets for diabetes remission
- Study: Does time-restricted eating add benefits to calorie restriction? A systematic review edit
- Study: Effectiveness of Intermittent Fasting and Time-Restricted Feeding Compared to Continuous Energy Restriction for Weight Loss
- Study: Efficacy and safety of tirzepatide, GLP-1 receptor agonists, and other weight loss drugs in overweight and obesity: a network meta-analysis
- Study: Energy expenditure and obesity across the economic spectrum
- Study: Healthy weight loss maintenance with exercise, GLP-1 receptor agonist, or both combined followed by one year without treatment: a post-treatment analysis of a randomised placebo-controlled trial edit
- Study: Host-diet-gut microbiome interactions influence human energy balance: a randomized clinical trial
- Study: Impact of weight loss achieved through a multidisciplinary intervention on appetite in patients with severe obesity edit
- Study: Incident type 2 diabetes attributable to suboptimal diet in 184 countries
- Study: Increased Physical Activity Associated with Less Weight Regain Six Years After "The Biggest Loser" Competition
- Study: Less frequent dosing of GLP-1 receptor agonists as a viable weight maintenance strategy
- Study: Lifestyle Strategies after Intentional Weight Loss: Results from the MAINTAIN-pc Randomized Trial
- Study: Liraglutide versus semaglutide for weight reduction—A cost needed to treat analysis
- Study: Low-calorie diet-induced weight loss is associated with altered brain connectivity and food desire in obesity
- Study: Modeling potential cost-effectiveness of tirzepatide versus lifestyle modification for patients with overweight and obesity
- Study: Nut consumption, gut microbiota, and body fat distribution: results of a large, community-based population study
- Study: Persistent metabolic adaptation 6 years after "The Biggest Loser" competition
- Study: Pharmacotherapy for adults with overweight and obesity: a systematic review and network meta-analysis of randomised controlled trials
- Study: Polycystic ovary syndrome is associated with weight-loss attempts and perception of overweight independent of BMI: a population-based cohort study
- Study: Reducing Social Media Use Improves Appearance and Weight Esteem in Youth With Emotional Distress
- Study: RE: Pulmonary Hypertension Associated with Use of Phentermine?
- Study: Semaglutide 2.4 mg/wk for weight loss in patients with severe obesity and with or without a history of bariatric surgery
- Study: Sugar-sweetened beverage consumption and weight gain in children and adults: a systematic review and meta-analysis of prospective cohort studies and randomized controlled trials
- Study: The association between weight loss medications and cardiovascular complications
- Study: The spread of obesity in a large social network over 32 years
- Study: Three- and six-month efficacy and safety of phentermine in a Mexican obese population
- Study: Time-Restricted Eating Without Calorie Counting for Weight Loss in a Racially Diverse Population
- Study: Tirzepatide Once Weekly for the Treatment of Obesity
- Study: Triple–Hormone-Receptor Agonist Retatrutide for Obesity — A Phase 2 Trial
- Study: Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension edit
- Weight and Psychiatric Medications edit
- Study: People With Lowest Physical Functioning Scores Showed Greatest Improvement After Tirzepatide Treatment
- Study: Obesity as a Risk Factor for Autoimmune Diseases: A Systematic Review and Meta-Analysis
- Wegovy Studies
- Study: Addition of Phentermine-Topiramate to a Digitally Enhanced Lifestyle Intervention: A Double-Blind Randomized Clinical Trial
- Study: Weight regain after cessation of medication for weight management: systematic review and meta-analysis
- Study: Energy expenditure and obesity across the economic spectrum
- Trauma/Emergency
- Urology
- Acute simple cystitis in women (Simple UTI)
- Bladder Cancer
- BPH
- Common Causes of Abnormal Urine Coloration
- Erectile Dysfunction
- Hematuria
- Incontinence edit
- Infertility (Male)
- Interstitial Cystitis and Bladder Pain Syndrome
- Male Hormones 2025
- Men's Health
- Nephrolithiasis
- Nocturia
- Prostate Specific Antigen (PSA)
- Semen
- Study: Efficacy of Clomiphene Citrate Versus Enclomiphene Citrate for Male Infertility Treatment: A Retrospective Study
- Uncomplicated cystitis
- Urinary Tract Infections
- Weight Management/ABCD
- 5 A's of discussing Obesity/ABCD
- Weight Loss Success Strategies
- - (1) - Identify appropriate patients who need to lose weight
- - (2) - Physical Assessment
- - (3) - Screening
- - (4) - Treat Comorbidities
- Medical and psychosocial consequences of obesity
- Obesity and Atrial Fibrilation
- Obesity and Cancer
- Obesity and Gall bladder disease
- Obesity and Heart Disease
- Obesity and Hypertension
- Obesity and Non-alcoholic Fatty Liver Disease (NAFLD)
- Obesity and Psychosocial impact
- Obesity and Sleep
- Obesity and Sleep Apnea
- Obesity and Stroke
- Obesity Paradox - Things made worse with weight loss
- - (5) - Lifestyle modification
- - (6a) - Pharmacotherapy
- - (6b) - Bariatric surgery
- - (7) - Maintenance of Weight Loss and Prevention of Weight Regain
- Basics of all practice guidelines:
- Coding for Weight Loss
- Epidemiology and physiology
- Medicine Quotes
- Pediatric Obesity
- Pregnancy and Weight
- Resources
- Patient Messaging
- Org
- CBD Autism
- Anxiety Stuff and Messaging edit
- Anxiety Messaging
- General Anxiety Strategies:
- CBT edit
- Progressive Muscle Relaxation
- Face your fears (Graded Exposure)
- Challenge your thoughts
- Calming imagery
- Time Management Strategies
- Do Stretches
- Mindful Breathing
- Name that emotion
- Relaxation Strategies
- Challenge your Negative Thoughts edit
- Decatastrophizing edit
- Cognitive Distortions
- 9 Essential CBT Techniques and Tools
- Diabetes Care Standards (2024) edit
- ADHD Stuff to Edit
- Core CBT Techniques
- DM with Hemoglobinopathies
- Male Infertility
- AF
- Asymptomatic Hypertension
- Chronic Urticaria
- Osteoporosis
- Minimal Exercise Necessary edit
- Overcome Social Anxiety edit
- Study: Objective assessment of health or pre-chronic disease state based on a health test index derived from routinely measured clinical laboratory parameters
- To Capture edit 2025
- Study: Role of Inactivity in Chronic Diseases: Evolutionary Insight and Pathophysiological Mechanisms
- Study: Optimism is associated with exceptional longevity in 2 epidemiologic cohorts of men and women
- homocysteine
- Follow up: HRT testosterone edit 2025
- Helping healthy people? edit 2025
- Study: Why more social interactions lead to more polarization in societies
- Counselors edit 2025
- Pompe Disease edit
- Study: Open-label placebos—a systematic review and meta-analysis of experimental studies with non-clinical samples edit
- Study: Listening to Prozac but hearing placebo: A meta-analysis of antidepressant medication edit
- Study: Efficacy of antidepressants: a re-analysis and re-interpretation of the Kirsch data edit
- Study: The effect of vitamin D supplementation on depression: a systematic review and dose–response meta-analysis of randomized controlled trials edit
- Study: Risk of suicide, suicide attempt, and suicidal ideation among people with vitamin D deficiency: a systematic review and metaanalysis edit
- Effect sizes on Depression edit
- Study: Cholesterol-lowering effects of oats induced by microbially produced phenolic metabolites in metabolic syndrome: a randomized controlled trial edit
- Study: Safety and Efficacy of Glucagon-Like Peptide-1 Receptor Agonists Use in Elderly People With Obesity—A Meta-Analysis
- Study: Heritability of intrinsic human life span is about 50% when confounding factors are addressed edit
- Study: Effect of exercise on depression and anxiety symptoms: systematic umbrella review with meta-meta-analysis edit
- Evidence Based Ways To Increase Testosterone Using Lifestyle Changes
Aesthetics
Botox/Xeomin Injections (botulinum toxin type A)
Good article: Botulinum toxin in facial plastic surgery
General Techniques:
- Inject while retracting
- Patient in a 60 degree recline
- Touch up 2 weeks later if needed
- Use white eyeliner to mark safety zones
- Compress injection sites firmly away into safety zone
- Wipe area with EtOH swab
- Inject with muscles contracted (Frown and Forehead)
| Botox | Xeomin | Disport | |
|---|---|---|---|
| Equiv Units | 1 | 1 | 3 |
| Diffusion Rate | + | ++ | |
| Results show | 4-5 | 3-5 | 2-3 |
| Price/unit | $$ | $$ | $ |
| Price Overall | $$ | $$ | $$ |
| Allergens to avoid | egg/latex |
Reconstitution
| 50 unit vial | 100 unit vial | 200 unit vial | |
|---|---|---|---|
| 0.9% NaCl* | 2.5 mL | 5 mL | 10 mL |
*Preservative Free
Reconstitution and Dilution - Flip It. Don't Shake It.
- Prior to injection, reconstitute each vial of XEOMIN with sterile, preservative-free 0.9% Sodium Chloride Injection
- A 20 to 27-gauge short-bevel needle is recommended for reconstitution
- Draw up an appropriate amount of preservative-free 0.9% Sodium Chloride Injection, USP into a syringe
Steps:
- Step 1: Vial preparation
- Clean the exposed portion of the rubber stopper of the vial with alcohol (70%) prior to insertion of the needle.1
- Step 2: Saline injection
- After vertical insertion of the needle through the rubber stopper, the vacuum will draw the saline into the vial. Gently inject any remaining saline into the vial to avoid foam formation. If the vacuum does not pull the saline into the vial, then XEOMIN must be discarded.1
- Step 3: Mixing
- Remove the syringe from the vial and mix XEOMIN with the saline by carefully swirling and inverting/flipping the vial—do not shake vigorously.1
Frown Lines
Injection sites:
- 1 cm above eyebrow (orbital rim) at the medial edge of eye line (medial Canthus) (Corrugator muscle)
- 2 - 4 u each side
- 1 cm above eyebrow (orbital rim) on the medial edge of the iris line (Limbus) (Corrugator muscle)
- 2 u each side
- Standing in front of patient, inject into Procerus muscle
- Imagine an X from medial canthus to Corrugator injection (#1)
- 4 u (2.5 - 5 u)
Total dose:
- Women: 20 units
- Men: 25 units
Reference:
Forehead Lines
General Injection Strategy:
- Superior half to third of forehead inject 2 units symmetrically in ridges (not valleys) (Frontalis muscle)
- Consider 4 sites in horizontal line
- 2 units each (8 total)
- If needed add another line in a ridge consisting of 2- 3 sites in spaces between previous injections
- Might look best if in a V shape
- 2 units each (4 to 6 units)
- Approach with 30 degree angle
Total dose:
- Women: 15 - 20 units
- Men: 20 - 25 units
Botox Aftercare Instructions
Aftercare instructions:
- No physical exercise (24 hours)
- Avoid heat exposure (24 hours)
- Avoid alcohol and painkillers
- Don't wear anything on the treatment area
- No laying down after your Botox treatment (4 hours); Also, avoid sleeping on your face for at least 1 night
- No touching your face or massaging the treatment area
Injection Plan:
- Use 8 units Glabellar
- 4 u Precerus
- 2 u Bilat Corrugator
- Use 12 units Forehead
- 1 line of 4 sites
- 1 line of 2 sites (if needed) . . . . . .
Botox FAQ
How long is BOTOX good for after reconstitution?
Ideally you will want to use the reconstituted vial of botulinum toxin within 3 weeks, however it can last up to eight weeks when stored properly in the fridge (Hexcel et al 2003). What is the standard dilution for BOTOX?
The recommended dose is 100 Units of BOTOX, and is the maximum recommended dose. The recommended dilution is 100 Units/10 mL with preservative-free 0.9% Sodium Chloride Injection, USP (see Table 1).
Does BOTOX require reconstitution?
BOTOX® Cosmetic dilution and reconstitution processes are the same for moderate to severe forehead lines, lateral canthal lines, and glabellar lines. Note: once open and reconstituted, use within 24 hours, because product and diluent do not contain a preservative. How do you store BOTOX after reconstitution?
BOTOX should be administered within 24 hours after reconstitution. During this time period, reconstituted BOTOX should be stored in a refrigerator (2° to 8°C).
What is Botox reconstitution?
Allergan advocates 100 U of BOTOX® diluted in 2 cc of preservative-free normal saline, which results in a concentration of 5 U/per 0.1 mL. Reconstitution is performed using a vial of BOTOX®, which must remain upright. A 21-gauge, 2-inch needle is attached to a 5 mm syringe.
Reference:
Allergy/Immunology
Allergic Rhinitis
Allergic rhinitis
- An immunoglobulin E–mediated process
Preventions that don't work
- High-efficiency particulate air (HEPA) filters are not effective at decreasing allergy symptoms.
- Dust mite–proof mattress covers do not prevent allergic rhinitis in children two years and younger.
History
- Whether the symptoms are seasonal or perennial
- Symptom triggers
- Severity
Common examination findings
- Clear rhinorrhea
- Pale nasal mucosa
- Swollen nasal turbinates
- Watery eye discharge
- Conjunctival swelling
- Allergic shiners
Testing:
- Serum or skin testing for specific allergens should be performed when there is inadequate response to empiric treatment, if diagnosis is uncertain, or to guide initiation or titration of therapy.
- If allergy testing is performed, trigger-directed immunotherapy can be effectively delivered subcutaneously or sublingually
Treatment
- Intranasal corticosteroids are first-line treatment for allergic rhinitis.
- Second-line therapies include antihistamines and leukotriene receptor antagonists and neither shows superiority.
Approximately 1 in 10 patients with allergic rhinitis will develop asthma.
Reference:
- Am Fam Physician. 2023;107(5):466-473
Anaphylaxis
USE epinephrine!
- Corticosteroids and diphenhydramine help stave off rebound anaphylaxis
Eosinophilic Esophagitis
- Empiric 6 food elimination diet (SFED) resolves inflammation in 66% of patients
- Milk, Wheat, Soy, Eggs, Treenuts/peanuts, and fish/shellfish
- Food elimination based on allergy testing resolves esophageal inflammatiton in 50% of patients
- Often (69%), patients are able to identify a single food trigger
- Medication options for eosinophilic esophagitis include
- Topical steroids delivered via an asthma inhaler and then swallowed
- PPI
- Dysphagia with eosinophilic esophagitis is often secondary to esophageal strictures, which can be treated with endoscopic dilation
Causes:
- Dairy: 50%
- Wheat: 31%
- Soy
- Egg: 36%
- Nuts
- Fish/Shellfish
References:
- AFP Vol 103 No 9 May 2021
- Zalewski A, Doerfler B, Krause A, Hirano I, Gonsalves N. Long Term Outcomes of the Six Food Elimination Diet and Food Reintroduction in a Large Cohort of Adults with Eosinophilic Esophagitis. Am J Gastroenterol. 2022 Aug 12. doi: 10.14309/ajg.0000000000001949. Epub ahead of print. PMID: 35971213.
There are quite a few studies on a 4-6 food elimination diet to help with food allergies and sensitivities.
This is the process:
- Take the top 6 most common food allergens out of your diet for 6 weeks (milk products, eggs, wheat, soy, peanut/tree nuts, and fish/shellfish).
- At 6 weeks into the diet, review your symptoms.
- Bring the foods back into your diet, one at a time, for a 2 week trial each. See if you have any symptoms from them - if so, avoid their use.
Food Allergies
9 foods are responsible for the majority (90%) of allergic reactions:
- Cow's milk: cheese, yogurt, baked goods
- Eggs: mayonnaise, pasta, baked goods
- Fish: salmon, tuna, sauces
- Peanuts: peanut butter, sauces, candies
- Sesame: Seeds, tahini, bread
- Shellfish: shrimp, crab, lobster
- Soy: tofu, soy milk, soy sauce
- Tree nuts: almonds, cashews, hazelnuts, pistachios
- Wheat: Bread, pasta, processed foods
Risk factors (OR):
- Latex allergy (7.9)
- Asthma (3.2)
- Urticaria (2.9)
- Insect venom allergy (2.50
- Allergic rhinitis (2.3)
- Atopic dermatitis (1.9)
- Medication allergy (1.9)
Reduce risk:
- Early introduction of peanuts, cow's milk, wheat, and cooked eggs between 4-6 mo decreases risk of developing food allergies
- Early introduction of peanuts and cooked eggs at 4-6 mo is safe and effective for reducing risk of food allergy
| Airborne allergen | Food |
|---|---|
| Birch pollen | carrots, celery, fresh fruit, hazelnuts, parsnips, potatoes |
| Grass pollen | kiwi, tomatoes |
| Ragweed pollen | bananas, melons |
Reference:
- AFP Vol 108 No 2 Aug 2023
- https://www.aaaai.org/conditions-treatments/allergies/food-allergy
Seasonal Allergies
Allergy Medications
- Antihistamines: These medications are commonly used to treat allergies such as allergic rhinitis or sometimes urticaria (hives).
- Immunomodulator Medications: These medications act by directly changing the behavior of the immune system. These are also known as biological medications.
- Leukotriene Modifiers: These medications are used for relief of allergic rhinitis symptoms.
- Nasal Sprays and Sinus Medications: This table includes the various nasal sprays approved to treat allergic rhinitis and/or non-allergic rhinitis.
- Devices: This includes information on devices that have been approved for use to treat or manage allergic rhinitis.
- Eye Drops: This table lists the medications available to treat allergic conjunctivitis (allergic eye).
- Allergic Emergency Medications: These are the medications used to treat anaphylaxis.
- Topical Ointments & Creams: Here are the topical medications used to treat conditions such as atopic dermatitis and eczema.
- Treatment of Hereditary Angioedema: Replacement therapy or immune modulating medicines pertaining to hereditary angioedema.
- Oral Corticosteroids: These medications are sometimes used to treat severe allergies and can also be used as a rescue medication for asthma.
- Sublingual Immunotherapy (SLIT) Allergy Tablets: Allergy tablets are another form of allergy immunotherapy therapy and involves administering the allergens under the tongue generally on a daily basis.
To manage allergy symptoms, these are the medications with the strongest evidence:
- Flonase (fluticasone) spray (or similar like Nasocort) 2 sprays in each nostril daily. This takes at least a week of use before you will notice it working. To use, look down touching chin to chest, Spray into nose use other side arm (for example: left arm on right side)
- There is one antihistamine nasal spray which will help symptoms very quickly: Astepro allergy (azelastine)
- Also helpful are medications like: Allegra, Claritin, or Zyrtec. I find Allegra to be stronger than Claritin and Zyrtec. Use this every day when allergies are worse.
- To manage excessive congestion, you can use Sudafed 30-60 mg every 4 hours as needed. This medication might keep you awake, so be cautious with use at night.
My recommended maximal allergy management would be:
- Flonase daily
- Allegra-D (generic is fine)
- Astepro allergy (OTC antihistamine nasal spray)
IgG vs IgM
IgM
- IgM antibodies are produced by the body immediately after the exposure to a specific antigen
- Mainly found in blood and lymph fluid
- Quantity produced upon exposure to the antigen is nearly 6 times as much of IgG
- IgM antibodies usually also have 10 binding sites (compared to only 2 in IgG)
- Only about half of the binding sites can actually be used to bind IgM to an antigen
- IgM is multivalent: Multiple monomers are bonded together
- Temporary - disappear within 2 to 3 weeks following infection
IgG
- IgG refers to an immunity for a particular disease
- A late stage response as compared to IgM
- Abundant in the body
- Protects against various disease causing foreign agents
- IgM antibodies are replaced by IgG antibodies that last for life time
Systemic reaction to insect sting
- Evaluate patients with skin testing
- If positive: treat with venom immunotherapy
Reference:
- AFP Vol 106 No 6 Dec 2022
Mast Cell Activation Syndrome (MCAS)
Symptoms - The symptoms most consistent with anaphylaxis are:
- Heart related symptoms: rapid pulse (tachycardia), low blood pressure (hypotension) and passing out (syncope).
- Skin related symptoms: itching (pruritus), hives (urticaria), swelling (angioedema) and skin turning red (flushing).
- Lung related symptoms: wheezing, shortness of breath and harsh noise when breathing (stridor) that occurs with throat swelling.
- Gastrointestinal tract symptoms: diarrhea, nausea with vomiting and crampy abdominal pain.
Reference:
Diagnosis
Diagnostic criteria for mast cell activation syndrome
According to the algorithm proposed by Valent et al, MCAS should be considered when the following 3 criteria are met:
- Presence of typical and recurrent severe symptoms of excess MC activation (often diagnosed as anaphylaxis affecting at least 2 organs).
- The typical symptoms include
- Urticaria
- Flushing
- Pruritus
- Wheezing
- Angioedema
- Nasal congestion
- Tachycardia
- Hypotension
- Diarrhea
- Headaches, memory loss, and impaired concentration may also be observed, although these symptoms are less specific.
- The typical symptoms include
- Confirmed excess of MC activation in biochemical tests. The preferred marker is tryptase (elevated serum levels by 20% above the upper limit of the normal range or by at least 20% above baseline plus 2 ng/ml within 4 hours after a symptomatic period). Other metabolites include serum and urinary histamine and urine prostaglandin D2, leukotrienes C4 and E4, and 11β-prostaglandin F2α. Prostaglandin D2 in 24-hour urine collection is considered the most specific marker of excess MC activation, but its availability is highly limited.
- Positive response to symptom treatment as in mastocytosis. By consensus, this criterion should be fulfilled by antihistamine agents; however, response to other drugs, such as leukotriene receptor blockers, systemic glucocorticoids, and sodium cromoglycate, may also be useful, although they are considered less specific and thus more efficient in other diseases than MCAS. The withdrawal of symptoms should be complete or at least major, as self-reported by patients.
In the case of nonsevere, transient symptoms (criterion 1 not fulfilled) and positive criteria 2 and 3, systemic or local (if the range of skin symptoms is limited) mast cell activation (MCA) is diagnosed with a similar clinical approach to that in MCAS. In other cases, if the patient does not respond to standard MCAS treatment and requires repeated epinephrine administration, MCA might be diagnosed provided that typical symptoms (criterion 1) and elevated levels of MC-derived mediator (criterion 2) are present and the criteria for primary MCAS are met (see below).
Once the diagnosis is confirmed, MCAS is classified according to an underlying cause. Primary MCAS involves monoclonal MC proliferation, similar to SM but not fulfilling its criteria. In this type of MCAS, CD25+ mastocytes, the KIT D816V mutation, or both are observed in bone marrow biopsy. The diagnosis of mastocytosis is superior to that of MCAS, which means that if at any point the criteria for mastocytosis are fulfilled, MCAS is no longer considered. Secondary MCAS is defined as MC activation due to comorbidities.8 The most typical cause is type 1 hypersensitivity according to the Gell and Coombs classification, which leads to persistent MC activation through allergen-specific IgE.9 Hymenoptera venom, food, and drug intolerance or allergies are currently discussed as the most important causes of secondary MCAS. Although receptors for IgE (FcεRI) are considered the strongest MC activator, many different receptors are present on cell surface.10 Bacterial components might activate MC directly with toll-like receptors 2, 3, 4, and 6 as well as fMLP receptor or through complement activation.11 Excess of hormones may also induce secondary MCAS through estrogen, progesterone, corticotropin-releasing hormone, and α-melanocyte–stimulating hormone receptors. The chronic use of certain drugs such as opioids, muscle relaxants, intravenous contrast media, or adenosine may also activate MCs. If the primary and secondary causes are excluded, idiopathic MCAS may be diagnosed.
Importantly, some patients may be diagnosed with primary and secondary MCAS, as is the case in patients with mastocytosis and insect venom allergy (IVA) who require specific lifelong immunotherapy.12,13 It is recommended that these patients are provided with lifelong immunotherapy, in addition to antimediator treatment and an emergency kit including at least 2 epinephrine autoinjectors.
Labs
The most important first-line examination in patients with suspected mastocytosis or primary MCAS is the measurement of tryptase levels in peripheral blood.19 In the absence of urticaria pigmentosa, the patient with the tryptase level below 15 ng/ml and no increase during the suspected reaction should be followed. The tryptase level above 25 ng/ml is an indication for bone marrow studies including histopathology, cytology, flow cytometry, and detection of the KIT mutation.19 Patients with the level between 15 and 25 ng/ml and a REMA score of 2 or higher or with the KIT D816V mutation detected in peripheral blood should also undergo bone marrow studies.18
The elevated tryptase level may be related to other comorbidities, including hematologic, nonhematologic reactive, and other disorders.2 Hematologic diseases include chronic leukemia (myeloid, eosinophilic, basophilic), acute basophilic or myeloid leukemia, myelodysplastic syndrome, myeloproliferative neoplasm especially with mutated PDGFR or FGFR genes, and myelomastocytic leukemia.2,29 Nonhematologic reactive conditions with elevated tryptase levels are allergic disorders, mainly exacerbated chronic urticaria, chronic inflammatory diseases, and chronic helminth infection. Other conditions include end-stage kidney disease and hereditary alpha tryptasemia. Elevated tryptase level can be rarely found in healthy individuals or as a false positive result due to heterophilic antibodies.2 Additional mediators, such as histamine in plasma or urine, histamine metabolites in urine, or prostaglandin metabolites in 24-hour urine collection, may also be used as indicators of MCA.30 The positive result should be based on an event-related increase in at least 2 of these mediators or, preferably, at least 50% higher values after the reaction in comparison with the baseline value.2
Mast cells are known to produce many molecules that cause inflammation, but only a few mediators or their stable breakdown products (metabolites) have been found reliably elevated in episodes of MCAS and measurable in commercial laboratory tests. Increases in serum mast cell tryptase and in urine levels of N-methylhistamine, 11B -Prostaglandin F2α (11B-PGF2α) and/or Leukotriene E4 (LTE4) are the only useful tests in diagnosis of MCAS.
Total serum mast cell tryptase should be drawn between 30 minutes and two hours after the start of an episode, with baseline level obtained many days later. The urine tests are performed on a 24 hour collection of urine that is started immediately.
Since these are not standard laboratory tests, patients should work with their local allergist who can communicate with emergency and lab personnel to assure they are ordered and completed in a timely fashion.
Management
The aim of chronic treatment is to prevent symptoms by prophylactic use of antimediator drugs.5 The first-line choice is histamine receptor blockers 1 and 2. Patients with gastrointestinal symptoms may benefit from additional treatment with proton pump inhibitors. Some patients also benefit from administration of cromones, low-dose glucocorticoids, and, in the case of psychological disorders, antidepressants.5,48-50
The goals of treatment are both diagnosis and patient relief. The immediate goal is to provide relief for the patient. Lack of response to these treatments suggests that MCAS is not present.
The treatment of acute episodes should follow the recommendations for treatment of anaphylaxis, starting with epinephrine, if indicated by the severity of symptoms.
Antihistamines, such as the first generation histamine type 1 receptor blockers diphenhydramine and hydroxyzine, can be effective for itching, abdominal discomfort and flushing, but their use may be limited by side effects (sleepiness). Second generation antihistamines, including loratadine, cetirizine and fexofenadine, are preferable due to fewer side effects.
Treatment with histamine type 2 receptor blockers, such as ranitidine or famotidine, can be helpful for abdominal pain and nausea.
Aspirin blocks production of prostaglandin D2 and can reduce flushing.
Montelukast and zafirlukast block the effects of leukotriene C4 (LTC4) and zileuton blocks LTC4 production, so these reduce wheezing and abdominal cramping.
Corticosteroids are helpful for edema, hives and wheezing but should only be used as a last resort.
Omalizumab (which blocks binding of IgE to its receptors) has been reported to reduce mast cell reactivity and sensitivity to activation which can reduce anaphylactic episodes.
Safer short-term action steps that you can take to provide some relief include:
- Adopting a low-histamine diet: For some people with MCAD, a low-histamine diet provides significant relief. Supplemental diamine oxidase can also help by increasing histamine breakdown. But, it's important to keep in mind that this is only reducing exogenous (outside) histamine, and not altering the amount produced by your mast cells endogenously (within the body). Histamine is also only one of many mediators produced during mast cell degranulation.
- Focus on nutrients and foods known to stabilize mast cells: Many nutrients, including selenium (21) and vitamin C (22), have been shown to stabilize mast cells. A number of herbs and spices, like holy basil (23), peppermint (24), ginger (25), thyme (26), and turmeric (27) also have this effect. I have also seen good results with supplemental forms of quercetin (28), bromelain, nigella sativa (29), nettle (30), and butterbur. (31)
- Reducing stress: Corticotropin hormone, released in response to physical or psychological stress, destabilizes mast cells and causes them to release their mediators. (32)
- Entraining circadian rhythms: Mast cell activity closely mirrors circadian rhythms (33), so getting enough sleep and avoiding blue light at night is crucial.
Ultimately though, we need to address the root cause:
- Treat infections: A comprehensive stool test can help identify parasites and other infections that could be contributing to mast cell activation.
- Heal your gut: Remove inflammatory foods and focus on nutrient density. Include plenty of probiotic, prebiotic, and healing foods in your diet.
Behavioral Medicine
5A's
5As for Adults
The 5A's provide health practitioners with five steps to better manage their patients' health issues (such as smoking cessation or weight loss):
- ASK for permission to discuss weight and explore readiness
- ASSESS obesity related risks and 'root causes' of obesity
- ADVISE on health risks and treatment options
- AGREE on health outcomes and behavioral goals and followup
- ASSIST in accessing appropriate resources and providers
References:
5 A's behavior change model edit
5 A's behavior change model
The 5 A's Behavior Change Model2 has been adapted for self-management support improvement.
The 5 A's Behavior Change Model includes the following steps:
- Assess: Ask about or assess behavioral health risk(s) and factors affecting choice of behavior change goals or methods
- Advise: Give clear, specific, and personalized behavior change advice, including information about personal health harms and benefits
- Agree: Collaboratively select appropriate treatment goals and methods based on the beneficiary's interest in and willingness to change the behavior
- Assist: Using behavior change strategies (self-help and/or counseling), aid the beneficiary in achieving agreed-upon goals by acquiring the skills, confidence, and social or environmental supports for behavior change, supplemented with adjunctive medical treatments when appropriate
- Arrange: Schedule follow-up contacts (in person or by telephone) to provide ongoing assistance or support and to adjust the treatment plan as needed, including referral to more intensive or specialized treatment
More info: 5 A's Behavior Change Model: Adapted for Self-Management Support Improvement
Reference:
- Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med. 2002;22(4):267–84
- https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-management/diabetes/game-plan-preventing-type-2-diabetes/how-talk-patients-about-prediabetes-diagnosis/support-your-patients-with-behavior-change-strategies#fiveas
Anger and Emotions
Managing Anger/Stocism
- Recognize Anger as a Choice:
- Stoics believe we choose how we react to situations, not the situations themselves. Anger is a feeling we allow ourselves to experience; it's not an inevitable consequence of events. Recognizing this empowers us to make a different choice.
- Identify Your Triggers:
- Become aware of what consistently provokes anger. Is it specific people, situations, or types of behavior? Once you know your triggers, you can start to develop strategies for managing them.
- Practice Negative Visualization:
- This involves mentally rehearsing potential negative outcomes. While it may seem counterintuitive, imagining the worst-case scenario can help you appreciate what you have and reduce your attachment to things that might cause anger.
- Focus on What You Can Control:
- Stoicism emphasizes focusing on our own thoughts and actions rather than external factors. We can't control other people's behavior, but we can control how we respond to it. Direct your energy towards what you can influence.
- Reframe Your Thoughts:
- Challenge negative or irrational thoughts that fuel anger. Ask yourself if your thoughts are based on facts or assumptions. Look for alternative, more rational perspectives.
- Practice Emotional Regulation Techniques:
- Deep breathing exercises, mindfulness meditation, and physical activity can help calm your mind and body when you feel anger rising.
- Seek Wisdom from Stoic Texts:
- Read the works of prominent Stoics like Seneca, Epictetus, and Marcus Aurelius. Their writings offer timeless wisdom on managing emotions and living a virtuous life.
Remember: Anger is a natural emotion, but it's how we manage it that matters. By applying Stoic principles, you can learn to control your anger and respond to challenges with greater resilience and clarity.
Here are some practical techniques to handle anger and disappointment, blending elements of mindfulness, cognitive reframing, and emotional regulation:
- Pause & Breathe:
- When you feel anger or disappointment rising, take a few deep breaths. Count your inhalations and exhalations. This creates a space between the feeling and your reaction.
- Physical Release:
- Find a healthy outlet for pent-up energy such as going for a walk. Physical movement can help dissipate tension.
- Find activities that help you manage stress and emotions: Exercise, hobbies, spending time with loved ones, journaling, meditation, or therapy
- Name the Feeling:
- Acknowledge the emotion without judgment. Saying to yourself, "I'm feeling angry right now" or "This is disappointing," helps create distance from the overwhelming feeling.
- Remove Yourself (If Possible):
- If the situation allows, step away briefly. Go for a walk, find a quiet space, or simply change your surroundings. This can give you time to cool down and process your emotions.
You can also use Cognitive Reframing:
- Challenge Your Thoughts:
- Ask yourself: Is my reaction proportional to the situation? Are there other ways to look at this? Often, our initial thoughts are influenced by strong emotions and may not be entirely rational.
- Focus on What You Can Control:
- Remind yourself that you can't control everything. Focus on what you can influence – your own actions, reactions, and choices.
- Practice Gratitude:
- Shift your attention to things you are grateful for. This can help reframe your perspective and reduce feelings of negativity.
Remember, managing emotions is an ongoing process. Be patient with yourself, practice these techniques consistently, and celebrate your progress along the way.
Anxiety Traps
- Catastrophizing: Imagining the worst possible outcome. "I will get fired if the presentation has any glitches."
- Mind reading: Imagining what others are thinking. "I know he doesn't like working with me because he thinks I'm dumb."
- Fortune telling: Imagining what the future holds, but without data. "They will all hate me in the new group because I'm the only one who isn't a physicist."
- Black-and-white thinking: Considering only two possible outcomes. "I'll either hit a home run or get fired."
- Overgeneralizing: Painting all situations with a generalized outcome. "I presented to the CEO last year, and it didn't go well. I never get things right or always fail when it comes to executive audiences."
How to get out of the traps:
- Pause the pattern.
- Name the trap.
- Separate FUD from fact. Create a two-column list. On one side list all your fears, uncertainties, and doubts, or FUD. The second column is for verified facts.
- Tell more stories. When we're anxious, we tend not only to believe our own stories, we believe the most extreme and negative forms of them. Instead of curbing this reflexive habit, indulge it. Compose three separate stories and ensure they're very different from each other.
- Walk your talk. Ask yourself what you'd advise others to do.
BATHE Technique
BATHE for Primary Care Counselling
- Background
- Affect
- Trouble
- Handling
- Empathy
CBT (Cognitive Behavioral Therapy) Technique edit
It's a framework for thinking about psychological problems that incorporates many different methods. Exposure, mindfulness, hypothesis testing, self-acceptance, problem-solving, goal-setting and other ideas all fall into the CBT umbrella.
CBT encourages people to notice and question their automatic thoughts. Then, they use reasoning and experimentation to test their beliefs and adopt more realistic ones.
Beliefs –> Situations –> Automatic Thoughts –> Feelings and Behaviors
Example: I'm incompetent –> Mixed feedback on work project –> "I'm a failure. I can't do anything" –> Depressed and Stay in bed all day
- Focuses on the identification and modification of dysfunctional thoughts to improve affect
- Cognitive restructuring
- Help patients change the way they think about themselves
- Address catostrophic thinking
- Treach patients to view a setback as a temporary lapse
- Teach positive thinking (like replace thoughts that undermine weight management efforts)
Behavior Therapy:
- Change behavior and the feelings will follow
- Reinforce or extinguish a behavior (rewards, aversive stimuli, restructured environment)
- Relaxation training (music, progressive body relaxation, yoga, deep breathing, walks, etc)
Components of Behavioral Therapy:
- Self-monitoring
- Daily records of food intake, physical activity, weight
- Stimulus control
- Avoidance, narrowing, use of inhibitory stimuli to reduce triggers
- Problem solving
- Define the problem; brainstorm solutions; implement strategy
- Goal setting
- Establish dietary and weight goals
- Contingency management
- Develop recovery methods from overeating or weight gain
- Enlist social support
- Recruit family/friends to help modify lifestyle behaviors
- Relapse prevention training
- Expect setbacks; be prepared; view as temporary
- Stress management
- Decrease negative impact of stress on positive behavior patterns
- Rewards
- Congratulate self on successes, not mistakes; plan rewards for achieving goals
- Ongoing contact
- To maintain progress, most programs require short interval appointments
Reference:
- In brief: Cognitive behavioral therapy (CBT) - InformedHealth.org - NCBI Bookshelf
- OMA Review Course 2016
Recognizing Disordered Thinking edit
Disordered thinking patterns people who suffer from psychological distress frequently engage in:
- All-or-nothing thinking, e.g., “I'm either a winner or a loser.”
- Catastrophizing, e.g., “If my partner leaves me, I won't be able to live.”
- Ignoring evidence for positive interpretations, e.g., “I only passed the test because I got lucky.”
- Emotional reasoning, e.g., “I feel like a failure, so I must be one.”
- Labeling, e.g., “I'm a loser.”
- Magnification/minimization, e.g., “A mixed review means I'm incompetent. Positive reviews don't mean anything.”
- Mental filter, e.g., “Because one person at the party didn't like me, I must be a loser.” (Even if other people did like you.)
- Mind-reading, e.g., “She thinks I'm an idiot.”
- Overgeneralization, e.g., “I messed up the recipe. I can't do anything right.”
- Personalization, e.g., “Susan canceled our plans because she hates me.” (Ignoring that she might have had another reason.)
- Imperative thinking, e.g., “I should never make mistakes.”
- Tunnel vision, e.g., “He's such an idiot. He can't do anything right.”
flatly deny these statements. Indeed, they're often partially true, and it's that grain of truth that allows them to take deep root in our minds.
Instead, the therapist encourages patients to begin to notice these automatic thoughts. Then, through a process of Socratic questioning, the patient assesses their validity. Patients are asked to give reasons why a belief might be true, and also offer reasons it might not be.
A friend not replying to a text message might trigger the thought, “She doesn't like me. Nobody likes me.” But considering other possibilities, “Maybe she is busy?” or remembering that she helped you move last year and invited you to a party recently, can help you to question the validity of that belief.
Reference:
Action Plans: The “B” in CBT edit
dysfunctional actions people take.
Consider anxiety. A socially anxious person starts to feel anxious when asked to present at work. All month, he sweats over the proposed presentation, finally asking his boss to find someone else to do it.
Avoiding his anxiety, however, has two major consequences:
- The relief he feels in not having to do the presentation reinforces his behavior. Like a rat rewarded for pressing a lever, the motivational part of his brain is encouraged to find ways to avoid presenting in the future.
- By not presenting, he never gets to see if his feelings about presenting were accurate. He may have believed he would have been humiliated, but he'll never get disconfirming evidence that such an outcome was unlikely.
Action plans and behavioral experiments designed to test the validity of beliefs are central to CBT. These are especially important for depressed patients, whose illness makes even doing simple chores or self-care incredibly difficult. By taking small actions, you pry open a gap between the self-sustaining feedback loop depressive thoughts and inaction generate.
CBT Tools
CBT (Cognitive Behavioral Therapy) tools like STOPP and 3-2-1 Grounding are practical techniques designed to help individuals manage overwhelming emotions, reduce anxiety, or interrupt unhelpful thought patterns. They're rooted in CBT principles, which focus on changing negative thoughts and behaviors to improve emotional well-being.
Here's a breakdown of each:
STOPP
STOPP is an acronym that stands for a structured, step-by-step process to pause and regain control when you're caught in a spiral of negative thinking or emotional distress. It's commonly used to manage automatic reactions and encourage more rational responses. The steps are:
- S – Stop: Pause what you're doing or thinking. Don't react immediately.
- T – Take a Breath: Slow down with a few deep breaths to calm your mind and body.
- O – Observe: Notice what's happening. What are you thinking? Feeling? What's triggering this?
- P – Pull Back: Get some perspective. Ask yourself: Is this thought a fact or an opinion? What would I tell a friend in this situation?
- P – Practice What Works: Decide on a constructive next step. What's the best thing to do right now for yourself or the situation?
It's like hitting the brakes on a runaway train of thoughts—giving you space to respond rather than react. Therapists often teach this to help people with anxiety, anger, or impulsive behaviors.
STOPP is more cognitive — tackling thought patterns
Purpose of STOPP:
- To interrupt automatic negative thought patterns.
- To create space for a more considered response.
- To reduce impulsivity in emotional situations.
- To increase self-awareness of thoughts, feelings, and physical sensations.
- To promote a sense of control in challenging moments.
STOPP is CBT in a nutshell.
- Learn this ONE KEY SKILL and you can start to take control of your emotions and your life.
- "Between stimulus and response there is a space. In that space lies our freedom to choose our response. In our response lies our growth and our freedom". Viktor Frankl.
HOW TO USE STOPP:
- Practise the first two steps often for a few days - many times every day at any time.
- Read through the steps often.
- Carry written reminders with you (use the printable resources below).
- Practise STOPP by running through all the steps several times a day, every day…when you don't need it.
- Start to use it for little upsets.
Gradually, you will find that you can use it for more distressing situations. Like any new habit or skill, it will become automatic over time.
References:
Apps:
3-2-1 Grounding
The 3-2-1 Grounding technique is a sensory-based exercise to bring you back to the present moment, often used for anxiety, panic attacks, or dissociation. It anchors you by focusing on your immediate surroundings through your senses. Here's how it works:
- 3 – Name 3 things you can see: Look around and identify three specific things (e.g., a blue mug, a tree outside, your shoe).
- 2 – Name 2 things you can hear: Tune in to sounds (e.g., a car passing, your own breathing).
- 1 – Name 1 thing you can feel: Focus on a physical sensation (e.g., the chair beneath you, the texture of your clothes).
You can repeat or adjust it as needed. The idea is to shift your attention away from racing thoughts or flashbacks and into the here-and-now, using your senses as an anchor.
3-2-1 is sensory, pulling you out of your head and into your environment.
Purpose of 3-2-1 Grounding:
- To shift focus away from distressing thoughts and feelings.
- To engage your senses and connect you with your immediate environment.
- To provide a sense of being present and grounded.
- To help calm the nervous system during moments of anxiety or stress.
- To be a quick and accessible tool that can be used anywhere.
- 5-4-3-2-1 Grounding (Expanded Version)
- What it is: A more detailed version of 3-2-1 Grounding, engaging all five senses.
- How it works:
- 5 things you see
- 4 things you can touch
- 3 things you hear
- 2 things you smell
- 1 thing you taste (or imagine tasting)
- Why it's useful: Great for intense anxiety or dissociation, as it fully immerses you in the present.
Thought Record (or ABC Model)
- What it is: A way to break down and analyze thoughts to see how they affect your feelings and actions.
- How it works:
- A – Activating Event: What happened? (e.g., "I got a critical email from my boss.")
- B – Belief: What did you think about it? (e.g., "I'm terrible at my job.")
- C – Consequence: How did you feel or act? (e.g., "I felt anxious and avoided work.")
- Then, challenge the belief: Is there evidence for this? What's an alternative thought? (e.g., "One email doesn't define my skills.")
- Why it's useful: Helps you spot distorted thinking (like catastrophizing) and replace it with balanced perspectives.
Worry Postponement
- What it is: A technique to delay worrying instead of getting stuck in it.
- How it works: When a worry pops up, tell yourself, “I'll think about this later.” Set a specific “worry time” (e.g., 15 minutes at 6 PM). Until then, redirect your focus to something else.
- Why it's useful: Breaks the cycle of endless rumination and often, by “worry time,” the issue feels less urgent.
Behavioral Activation
- What it is: A simple action-oriented tool to combat low mood or procrastination.
- How it works: Pick a small, manageable task (e.g., washing dishes, taking a walk) and do it, even if you don't feel like it. Notice how it affects your mood afterward.
- Why it's useful: Gets you moving when depression or inertia sets in, proving action can shift feelings.
Positive Data Log (Win List)
- What it is: A way to counter negative self-beliefs by collecting evidence of your strengths.
- How it works: Keep a daily note of anything positive about yourself (e.g., “I helped a friend,” “I finished a task”). Review it regularly.
- Why it's useful: Builds self-esteem and challenges beliefs like “I'm worthless” with real examples.
Square Breathing (or Box Breathing)
- What it is: A breathing exercise to calm the nervous system.
- How it works:
- Inhale for 4 seconds
- Hold for 4 seconds
- Exhale for 4 seconds
- Hold for 4 seconds
- Repeat a few times.
- Why it's useful: Quick way to reduce stress or panic by regulating your breath.
The 3 Cs (Catch, Check, Change)
- What it is: A shorthand for reframing negative thoughts.
- How it works:
- Catch: Notice the negative thought (e.g., “I'll fail this test”).
- Check: Question it — Is it 100% true? What's the evidence?
- Change: Replace it with a more balanced thought (e.g., “I might struggle, but I've prepared as best I can”).
- Why it's useful: Fast and memorable for on-the-spot thought management.
CBT Videos edit
Child psych
Children's Medication Clinic - Serious behavioral and emotional problems not requiring inpatient
- Up to 17yo
- Princeton Plaze
- 1800 Mercy dr
- Orlando, FL 32808
- 507-875-3700
Coping strategies to teach patients
- Regularly practice relaxation techniques
- Deep breathing
- Muscle relaxation
- Make a list of worries in the evening before bedtime and give yourself permission to address them tomorrow
- Enlist or accept emotional support from others
- Reduce caffeine consumption gradually (FDA recommends <400 mg for adults)
- Adopt effective sleep hygiene practices
- Use a digital application to promote self-help
- Search in app store for: wellness, sleep, stress, etc
References:
- JFP Vol 69, No 7 Sep 2020
Divorce edit
Nearly a third of American children experience parental divorce before adulthood. To understand its consequences, we use linked tax and Census records for over 5 million children to examine how divorce affects family arrangements and children's long-term outcomes. Following divorce, parents move apart, household income falls, parents work longer hours, families move more frequently, and households relocate to poorer neighborhoods with less economic opportunity. This bundle of changes in family circumstances suggests multiple channels through which divorce may affect children's development and outcomes. In the years following divorce, we observe sharp increases in teen births and child mortality. To examine long-run effects on children, we compare siblings with different lengths of exposure to the same divorce. We find that parental divorce reduces children's adult earnings and college residence while increasing incarceration, mortality, and teen births. Changes in household income, neighborhood quality, and parent proximity account for 25 to 60 percent of these divorce effects.
Reference:
- Johnston, Andrew C and Jones, Maggie R and Pope, Nolan G. Divorce, Family Arrangements, and Children's Adult Outcomes. National Bureau of Economic Research Working Paper. Working Paper Series. No 33776, 2025, May, https://doi.org/10.3386/w33776. http://www.nber.org/papers/w33776
Empathy
How to have EMPATHY
- Eye contact - establish
- Muscles of facial expression
- Posture (open/closed)
- Affect - recognize
- Tone of voice - recognize
- Hear the whole person (understand the context)
- Your response
References:
- TED. (2013, December 12). Dr. Helen Riess: The power of empathy [Video file]. Retrieved from https://www.youtube.com/watch?v=baHrcC8B4WM
Exposure Therapy for OCD: Exposure and Response Prevention (ERP)
Learning to gradually face your fears is one of the most effective ways to break the OCD cycle. For OCD, the technique for facing fears is called exposure and response prevention (ERP).
ERP is done by:
- Exposing (E) yourself to situations that bring on obsessions (triggers)
- Not engaging in the unhelpful coping strategies that include compulsions or rituals, and avoidance (Ritual Prevention- RP)
Steps:
- Step 1: Get to know your OCD better
- To face your fears, it is helpful to know what you are thinking (your obsessions) and identify the triggers that bring on your obsessions and compulsions.
- You can do this by keeping track of the triggers on a daily basis for 1 week by using the Obsessive Fear Monitoring Form. (see end)
- Because obsessions can happen frequently, writing down 3 triggers per day (e.g. 1 in the morning, 1 in the afternoon, and 1 in the evening) will be enough to give you a good overview of your obsessions and compulsions.
- In the column labeled ¡§Fear¡¨, rate how intense the fear was in the specific situation. Use a 0-10 rating scale, where 0 = no fear and 10 = extreme fear.
- Finally, record all the compulsions/coping strategies you used in response to the obsession. Be sure to include both behavioural and/or mental strategies you used to manage the obsession and fear.
- Step 2: Build a fear ladder
- After about 1 week of tracking your obsessions and compulsions, you will be ready to make a list of all the different situations that you fear.
- Build a fear ladder by rank, ordering your triggers from least scary to most scary. For example, if you have contamination fears, being at a friend¡¦s apartment may be a situation that is low on the fear ladder because it only evokes a fear of 1/10. But using the bathroom in a shopping mall may be a situation that is very high on the ladder because it evokes a 9/10 fear. See Examples of Fear Ladders for some ideas about building your fear ladder.
- TIP: Build a separate ladder for each of your obsessive fears. For example, you may need a separate hierarchy for all situations related to your fear of contamination. You may also need a separate ladder for all situations related to your fear of causing something terrible to happen.
- Step 3: Climb the fear ladder ¡V ERP
- Once you have built a fear ladder, you are ready to face your fears by putting yourself in situations that bring on your obsessions (exposure), while resisting doing anything to control the obsessions and the anxiety associated with them (response prevention).
KEY POINTS TO MANAGING YOUR OCD (see Facing your Fears: Exposure for more tips):
- Bottom up. Start with the easiest item on the fear ladder first (i.e. fear=2/10) and work your way up.
- Track progress. Track your anxiety level throughout the exposure exercise in order to see the gradual decline in your fear of a particular situation. Use the Facing Fears Form to help you do this.
- Feeling anxious when you try these exercises is a sign that you are on the right track. If you¡¦re not anxious you might be too low on your ladder, and if you are feeling flooded with excessive anxiety, chances are you started too high up on the ladder. Remember that regardless of how intense your fear is, it will peak and then level off. What goes up must come down! Even if you do nothing about it the fear will eventually go away on its own.
- Don¡¦t avoid. During exposure, try not to engage in subtle avoidance (e.g. thinking about other things, talking to someone, touching the doorknob only with one finger instead of the whole hand, making mental promises to de-contaminate later on, etc.). Avoidance actually makes it harder to get over your fears in the long term.
- Don¡¦t rush. It is important to try to stay in the situation until your fear drops by at least half (e.g. from 6/10 to 3/10), or until you notice a significant reduction from your fear at the start (e.g. from 7/10 to 4/10). Also, focus on overcoming 1 fear at a time. It is a good idea to do the exposure repeatedly until the first item on the hierarchy no longer causes much of a problem for you.
Engaging in Response Prevention
- Resist the urge. In order for exposure to work, it is important that you try to resist, as much as possible, carrying out your compulsions during or after the exposure. The whole point of ERP is to learn to face your fear without having compulsions.
- Modeling. If you have been performing compulsions for some time, it may be difficult to know how to face a feared situation without doing them. In this case, it can be helpful to ask a family member or a close friend who does not have OCD to show you how to, for example, wash hands quickly or leave home without rechecking appliances, and then model, or copy, their behaviour.
- Delaying and reducing ritualizing as an alternative. You might find it very difficult to completely resist a compulsion, especially the first time you are facing your fears. In that case, you can try to delay acting on the compulsion rather than not doing it at all. For example, after touching the floor (exposure), wait for 5 minutes before washing your hands, and wash for 1 minute instead of 3 minutes. Try to gradually prolong the delay, so that you can eventually resist the compulsion altogether.
- Re-exposure. If you do end up performing a compulsion, try to re-expose yourself to the same feared situation immediately, and repeat the practice until your fear drops by half. For example, Practice 1: touch the floor and wait for 5 minutes before washing hands for 1 minute. Practice 2: touch the floor again immediately after washing, and wait for another 5 minutes before washing for 1 minute. Repeat this process until your anxiety drops from, say, 6/10 to 3/10.
How to move on.
- Once you experience only a little anxiety when completing an exercise, you can move on to the next one.
- For example, after several practices, you might feel very little anxiety when you wait 5 minutes to wash your hands after touching the floor. You can then challenge yourself to wait for 8 minutes before washing your hands after touching the floor. Again, repeat this practice until your anxiety drops by half or is significantly reduced from where it was at the start.
References:
| Date | Triggers for Obsessions (specific situations, objects, people, or thoughts that provoke obsessive fears) | Obsession | Fear (0-10) | Compulsions/Coping Strategies |
|---|---|---|---|---|
| Step | Situation | Fear Rating |
|---|---|---|
| 3. | Ask a coworker what they did on the weekend | 4 |
| 2. | Ask coworkers questions about how to complete tasks at work | 3 |
| 1. | Say stuff to coworkers | 2 |
Daily Exposure Practice Form Task:_________________________ Ritual prevention (or delay)_____________________________ Expected Initial Distress rating % (before starting Exposure)________________________ Goal: Distress level % (after Exposure) _ Frequency of Exposures _ times per __ (day/week)
| Day/Date | Start time | Stop time | Distress% start | Distress % end | Comments |
|---|---|---|---|---|---|
Distress Rating 0-100 (No or minimal/Moderate/Severe/Worst ever distress) Use this form when undertaking Exposure & Response Prevention (ERP), when NOT responding to the urge to perform a ritual or compulsion. It is normal to feel very anxious and distressed at the thought of either delaying or not doing the ritual
Gratitude
Here are four popular gratitude interventions to try:
- Gratitude Journal: Reflect on and write down 3-5 things for which you are grateful 2-4 times a week.
- Three Good Things: Similar to the gratitude journal, reflect on and write down 3 things you are grateful for and/or 3 things that went well. You should also include the reasons behind those three good things. Do this 2-4 times a week.
- Mental Subtraction (Writing Optional): Imagine what your life would be like if a positive event had not happened.
- Gratitude Letter: Write a letter to someone to whom you are grateful but have never explicitly told. Reading the letter out loud to the person or having them read it will help strengthen your relationship with them.
Gratitude can be described in three ways:
- As a trait - how naturally grateful is a person?
- Trait gratitude is also linked to a more positive outlook on life, increased optimism and hope, and having a more positive interpretation of social situations.
- As a mood – how does gratitude fluctuate throughout the day?
- Grateful people tend to view adversity as an opportunity for growth, which can increase resilience.
- This positive perspective may prevent one from hyper-focusing on thoughts or experiences, which can lead to decreased depression and anxiety over time.
- as an emotion – how fleeting is the feeling of gratitude after a positive interaction with someone?
- Experiencing gratitude can also keep a person grounded in the present, leading to increased mindfulness.
There are many individual benefits one may experience by being grateful, including
- Improved physical and psychological health
- Increased happiness
- Life satisfaction
- Positive mood
- Meaning in life
- Quality of sleep
Reference:
- Mary Katherine A. Lee. Gratitude as an Antidote to Anxiety and Depression: All the Benefits, None of the Side Effects. Issue Number 5. May 2019
HRV and stress edit 2024
Based on the provided search results, here's a comprehensive overview of how Heart Rate Variability (HRV) relates to stress:
- Changes in HRV under stress: Studies consistently show that stress induces changes in HRV, including:
- Decreased HRV (reduced variability) in response to acute stress (e.g., [1], [2], [3])
- Increased sympathetic nervous system (SNS) activity, leading to reduced parasympathetic nervous system (PNS) activity and decreased HRV (e.g., [4], [5])
- HRV as a stress indicator: HRV can serve as a biomarker for stress levels, as it reflects the balance between SNS and PNS activity. Low HRV values are often associated with high stress levels, while high HRV values indicate a more relaxed state (e.g., [6], [7])
- Impact of chronic stress on HRV: Prolonged exposure to stress can lead to decreased HRV, potentially indicating a state of chronic stress (e.g., [8], [9])
- HRV and stress management: Monitoring HRV can help individuals identify and manage stress levels. For example, high HRV values may indicate a need for relaxation techniques, while low values may suggest the need for stress-reducing strategies (e.g., [10], [11])
- Autonomic nervous system imbalance: HRV can reveal imbalances in the autonomic nervous system, which are often linked to stress. A dominance of SNS over PNS activity, reflected in low HRV, may indicate chronic stress and increased risk of cardiovascular disease (e.g., [12], [13])
- Individual differences: HRV responses to stress can vary significantly between individuals, highlighting the importance of considering individual differences when interpreting HRV data (e.g., [14], [15])
- In summary, HRV is sensitive to stress and can serve as a valuable indicator of stress levels, autonomic nervous system balance, and overall physiological state. By monitoring HRV, individuals can gain insights into their stress levels and develop strategies to manage and reduce stress.
Normal HRV:
- HRV varies from person to person, and there is no single “normal” range that applies to everyone.
- Age and gender can influence HRV, with younger adults (20-29 years) typically exhibiting higher HRV (24-62 milliseconds) and older adults (60-69 years) having lower HRV (16-28 milliseconds).
- A common range for HRV in healthy adults is between 20-200 milliseconds, with some sources suggesting a narrower range of 19-107 milliseconds.
- Elite athletes may have higher HRV (35-107 ms) compared to healthy adults.
References:
- Kageyama et al. (2018) - Stress-induced changes in HRV in healthy adults
- Vrijkotte et al. (2018) - HRV and job stress in white-collar workers
- Mefford et al. (2019) - HRV and stress reactivity in medical residents
- Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996) - HRV and stress
- Dimitriev et al. (2019) - HRV and mental stress in healthy adults
- Firstbeat Science (2023) - HRV and stress management
- Heart Rate Variability (HRV) - Influencing Factors & How to Monitor (2024) - HRV and stress levels
- Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature (2018) - Chronic stress and HRV
- A Systematic Review of Heart Rate Variability as a Measure of Stress in Medical Professionals (2020) - Chronic stress and HRV in medical professionals
- Make Heart Rate Variability Your Secret Anti-Stress Weapon (2024) - HRV and stress management
- Heart Rate Variability (HRV): What It Is and How You Can Track It (2024) - HRV and stress levels
- Autonomic Nervous System Imbalance and Cardiovascular Disease (2020) - HRV and autonomic nervous system imbalance
- Heart Rate Variability and Stress-Related Cardiovascular Disease (2020) - HRV and cardiovascular disease
- Individual Differences in HRV Responses to Stress (2020) - HRV and individual differences
- Heart Rate Variability and Stress Management: A Review (2020) - HRV and stress management
Managing anger and disappointment
Managing Anger/Stocism
- Recognize Anger as a Choice:
- Stoics believe we choose how we react to situations, not the situations themselves. Anger is a feeling we allow ourselves to experience; it's not an inevitable consequence of events. Recognizing this empowers us to make a different choice.
- Identify Your Triggers:
- Become aware of what consistently provokes anger. Is it specific people, situations, or types of behavior? Once you know your triggers, you can start to develop strategies for managing them.
- Practice Negative Visualization:
- This involves mentally rehearsing potential negative outcomes. While it may seem counterintuitive, imagining the worst-case scenario can help you appreciate what you have and reduce your attachment to things that might cause anger.
- Focus on What You Can Control:
- Stoicism emphasizes focusing on our own thoughts and actions rather than external factors. We can't control other people's behavior, but we can control how we respond to it. Direct your energy towards what you can influence.
- Reframe Your Thoughts:
- Challenge negative or irrational thoughts that fuel anger. Ask yourself if your thoughts are based on facts or assumptions. Look for alternative, more rational perspectives.
- Practice Emotional Regulation Techniques:
- Deep breathing exercises, mindfulness meditation, and physical activity can help calm your mind and body when you feel anger rising.
- Seek Wisdom from Stoic Texts:
- Read the works of prominent Stoics like Seneca, Epictetus, and Marcus Aurelius. Their writings offer timeless wisdom on managing emotions and living a virtuous life.
Remember: Anger is a natural emotion, but it's how we manage it that matters. By applying Stoic principles, you can learn to control your anger and respond to challenges with greater resilience and clarity.
Military Psychiatry
Extreme in theater:
- Separate / Hold / Monitor until able to address
- Judiciously restrain
- Neurolepticize if needed with caution
Not as extreme in theater: (PIE)
- P - Proximity - Start treatment as far forward as possible
- I - Immediacy - Treatment begins ASAP
- E - Expectancy - Instill expectancy in SM that they will return to duty
4 Steps:
- H&P
- BATHE
- Background: What happened?
- Affect: How does it make you feel?
- Troubles: What troubles you about _ ?
- Handle: How are you handling _ ?
- Empathy: Demonstrate empathy
- Mental Status Exam / SIG E CAPS
- Eval though content/process, ego mechanisms (impulses, coping skills, etc)
- Disposition
Mindfulness
- Acknowldege
- Notice triggers
- Remember why
Example:
- Acknoledge pain when it occurs
- Notice whether something is making it worse in the moment
- Remember the top 3 reasons that you want to stay off opioids:
- My kids
- I do not want to be dependent on something
- My health
NAME it to Tame it:
- Notice
- Notice the strong emotions that are occurring and name them (anger, fear, unease, etc)
- Choose a word to describe the emotional reaction
- Acknowledge
- Acknowledge this emotion and calmly hover over it to allow your executive brain to filter and organize it
- Make room
- Make room for the emotion. Be with the anger, fear, and unease without explaining it.
- Expand awareness
- Expand awareness and monitor strong emotions so that the emotions do not take over when they return
Reference:
- AFP Nov 2023 Vol 108, No 5
Motivational Interviewing (MI)
- Spirit of MI: Emphasizes personal choice and control
- Collaborative: Partnership between patient and clinician
- Evocative: Reasons to change come from the patient rather than the doctor
- Autonomy supporting: Ultimately the patient decides what to do
- Four Guiding Principles: (RULE)
- R - Resist the righting reflex
- U - Understand your patient's motivation
- L - Listen (actively) to your patient
- E - Empower your patient
- Guiding Principles: (GRACE)
- G - Generate a gap (develop discrepancy)
- R - Roll with resistance
- A - Avoid arguments
- C - Can do (support self efficacy)
- E - Express empathy
- Key Processes:
- Engagement
- Set the agenda collaboratively
- Non-judgemental
- Patient-centered
- Focusing
- Develop the conversation around a single issue
- Evoking (DARN)
- Move the conversation toward a prepatory change talk
- D - Desire to change (want, like, wish..)
- A - Ability to change (can, could..)
- R - Reasons to change (if..then)
- N - Need to change (need, have to, got to..)
- Importance ruler (scale 1-10)
- Planning
- Explore barriers to change
- Fascilitate change
- Explore commitment
- Engagement
- Practitioner Approach: (OARS)
- O - Open questions
- A - Affirmations
- R - Reflections
- S - Summaries
- Motivational Interviewing:
- Agenda setting - Would you mind if I talked with you about your weight?
- Exploration
- Patient's desire - Are you interested in being more active?
- Patient's ability - Would you be able to walk for 30min each day?
- Patient's reasons - You mentioned you are now more open to exercising. What makes you open to it now?
- Patient's need - How important is it that you get more fit?
- Providing information - Obesity has been linked to a greater risk of DM. Losing even a modest amount of weight can lower your risk. There are several options available to help you.
- Listening and summarizing - It sounds like you are interested in seeing a dietition for nutrition advice but are worried about finding the right one.
- Generating options and contracting - It sounds like you have several good ideas about how to reduce your calorie intake. Which one do you think would work best? I look forward to hearing about it at our next appointment.
References:
- CME Bulletin - Diagnosis and Management of Obesity
- FPM Sep/Oct 2016
- OMA Review Course 2016
Online Therapy Services edit
2023's Best Online Therapy Services Compared
- Best Overall Provider:
- Talkspace
- Most Affordable Provider:
- Best for Couples Therapy:
- Hey Ritual
- Bi-weekly solo therapy sessions:
- $100/month ($100 total)
- $85/month with 3-month commitment ($255 total)
- $75/month with 6-month commitment ($225 total)
- Weekly solo therapy sessions:
- $160/month ($160 total)
- $136/month with 3-month commitment ($408 total)
- $120/month with 6-month commitment ($360 total)
- Couples sessions (three solo and one couple session/month):
- $260/month ($260 total)
- $221/month with 3-month commitment ($663 total)
- $195/month with 6-month commitment ($1170 total)
- Most User-Friendly:
- Brightside
- Best for CBT:
- Online-Therapy.com (also couples)
- Basic Plan: The cost is $50 per week, billed monthly as $200. This plan includes all their interactive features and therapy resources, as well as therapy via chat. However, no live sessions are included in this package. This might be perfectly sufficient for users that just need some guided support, or those that want to test out the platform before upgrading to a plan with live sessions.
- Standard Plan: The cost is $80 per week, billed monthly as $320, and includes one live 45-minute therapy session via video, voice or text per week in addition to all the other features.
- Premium Plan: The cost is $110 per week, billed monthly as $440, and includes two live 45-minute therapy sessions via video, voice or text per week in addition to all the other features.
- Couples Therapy Plan: The cost $110 per week, billed monthly. This includes unlimited messaging with a therapist for the couple, one weekly 45-minute couples therapy session via video, voice or text, as well as access to all the other features.
- Large Pool of Therapists:
- BetterHelp (Adults, couples, and teens)
- Best for Teens:
- Best for LGBTQIA+:
- Great Video Therapy Platform:
- Amwell
Reference:
Opposite Action
Act opposite to the emotional urge in the service of pursuing values or goals.
- Many often become obsessively focused on pain or anxiety that they allow it to limit their participation in activities
- They can instead engage in counteractivities, within reason, despite pain or anxiety being present.
- They can engage in activities (physical and mental) as tolerated despite feeling pain or anxiety
PLISSIT Technique
PLISSIT
- Permission
- Limited Information
- Specific Suggestions
- Intensive Therapy
Shared decision making
- Identify percieved risks and benefits
- Address percieved risks and benefits
- Establish ease of use
- Make a plan
References:
- JFP 2013;62(12 suppl CME):S20-S26
Stages of Change
- Pre-contemplation (Start MI here)
- Contemplation (MI)
- Preparation (use CBT here)
- Action (CBT)
- Maintenance (CBT)
Reference:
- OMA Review Course 2016
Stop Catastrophizing
Catastrophize:
- On hearing uncertain news, you imagine the worst possible outcome
Catastophizers learn to choose the worst possible outcome because it allows for the greatest sense of relief when they are reassured.
Catastrophizers rush to external sources to calm themselves down:
- checking whether anyone else has "come through" the same problem;
- matching symptoms online to obtain a diagnosis and treatment options;
- asking a professional to tell them that they will survive.
Once they are reassured, they feel better, they have "rewarded" this seeking behavior. The next time they feel uncertain or threatened, they will ratchet up their anxiety with a catastrophic thought, then look outwards for reassurance even faster than before.
In this way, catastrophizing soon becomes a well-entrenched habit. The greatest problem with seeking others to alleviate anxiety is that it offers only temporary relief.
Plan for tackling anxiety:
- Accept yourself.
- Anxiety is energy. Look for enjoyable ways to challenge yourself and use your energy more positively:
- Taking regular aerobic exercise.
- Learning something new.
- Taking up a creative passion.
- Anxiety is energy. Look for enjoyable ways to challenge yourself and use your energy more positively:
- Take control.
- Establish a regular "worry time".
- Start by setting aside half an hour every day. Write down all your concerns in specific terms
- Assign a score on a scale of 0 to 100% to estimate how distressed this possibility makes you feel
- List all the possible explanations for your concern, then rank each one according to how likely it is to be correct
- Score your worry for the level of distress it is causing you now. Gradually, you will be able to reduce the amount and frequency of worry time.
- Establish a regular "worry time".
- Use the "best friend test".
- Ask yourself what you would advise your best friend to do about each concern, and take that action
- Learn to self-soothe.
- Whenever you are overwhelmed by anxiety and feel you must seek reassurance, give yourself permission to do so – but not straight away.
- Start with 2 min.
- Breathing slowly in through your nose and out through your mouth, or taking some gentle exercise, will help.
- Gradually, you will find you can wait longer.
- When you get to the point where you can wait more than 20 minutes, most people find they no longer need to be reassured by others.
- Start with 2 min.
- Whenever you are overwhelmed by anxiety and feel you must seek reassurance, give yourself permission to do so – but not straight away.
Study: Anger is eliminated with the disposal of a paper written because of provocation
Anger suppression is important in our daily life, as its failure can sometimes lead to the breaking down of relationships in families. Thus, effective strategies to suppress or neutralise anger have been examined.
This study shows that physical disposal of a piece of paper containing one's written thoughts on the cause of a provocative event neutralises anger, while holding the paper did not.
In this study, participants wrote brief opinions about social problems and received a handwritten, insulting comment consisting of low evaluations about their composition from a confederate. Then, the participants wrote the cause and their thoughts about the provocative event.
Half of the participants (disposal group) disposed of the paper in the trash can (Experiment 1) or in the shredder (Experiment 2), while the other half (retention group) kept it in a file on the desk.
All the participants showed an increased subjective rating of anger after receiving the insulting feedback. However, the subjective anger for the disposal group decreased as low as the baseline period, while that of the retention group was still higher than that in the baseline period in both experiments.
We propose this method as a powerful and simple way to eliminate anger.
Reference:
- Kanaya Y, Kawai N. Anger is eliminated with the disposal of a paper written because of provocation. Sci Rep. 2024 Apr 9;14(1):7490. doi: 10.1038/s41598-024-57916-z. PMID: 38594343; PMCID: PMC11003969.
Study: Bypassing versus correcting misinformation: Efficacy and fundamental processes
The standard method for addressing the consequences of misinformation is the provision of a correction in which the misinformation is directly refuted. However, the impact of misinformation may also be successfully addressed by introducing or bolstering alternative beliefs with opposite evaluative implications.
Six preregistered experiments clarified important processes influencing the impact of bypassing versus correcting misinformation via negation.
- First, we find that, following exposure to misinformation, bypassing generally changes people's attitudes and intentions more than correction in the form of a simple negation.
- Second, this relative advantage is not a function of the depth at which information is processed but rather the degree to which people form attitudes or beliefs when they receive the misinformation. When people form attitudes when they first receive the misinformation, bypassing has no advantage over corrections, likely owing to anchoring.
In contrast, when individuals focus on the accuracy of the statements and form beliefs, bypassing is significantly more successful at changing their attitudes because these attitudes are constructed based on expectancy-value principles, while misinformation continues to influence attitudes after correction.
Broader implications of this work are discussed. (PsycInfo Database Record (c) 2024 APA, all rights reserved).
Reference:
- Granados Samayoa JA, Albarracín D. Bypassing versus correcting misinformation: Efficacy and fundamental processes. J Exp Psychol Gen. 2024 Nov 18. doi: 10.1037/xge0001687. Epub ahead of print. PMID: 39556359.
Don't waste time correcting misinformation. Instead, try the "bypassing technique"
Bypassing Technique: A strategy we can all use to push back against pseudoscience, conspiracy, and falsehoods.
"The gold standard for tackling misinformation is [usually] a correction that factually contradicts the misinformation."
- Suppose, for example, that your dad passes back the roast potatoes over a family dinner saying, "Are these GMOs? Nah, don't want any more allergies." You might then say, "Actually, the health bodies of all the G7 agree that GMOs do not cause allergies or rashes."
Bypassing is where, instead of providing some negative rebuttal to a claim, you instead provide positive counterclaims about the topic.
- For example, if someone says aluminum causes bone problems, you should reply, "Aluminium is one of the key elements in boosting our immune system and making the vaccine effective."
- Or, if someone tells you that 5G kills birds, tell them that 5G adds trillions to the world economy.
Make no mention of the false claim. Do not attack the misinformation but override it with positive, true information.
Bypassing is largely about attitudes to policies, not about belief change or belief correction.
- So, for example, your dad might still believe that GMOs cause allergies, but, thanks to your bypassing, be okay with their widespread use worldwide.
When it comes to policy decisions and willingness to accept a certain technology or medicine, bypassing seems like a valuable tool to add to your kit.
- Don't correct people.
- Don't fact-check.
- Don't fight the misinformed on their own ground.
- Make the case for the other side seem better.
Reference:
Study: Gratitude and Loneliness: Enhancing Health and Well-Being in Older Adults
We experimentally investigated gratitude's impact on loneliness and health in older adults.
Participants were assigned to a daily gratitude writing exercise (treatment group) or a control group.
Self-reported loneliness and health (i.e., subjective well-being, subjective health, health symptoms) were measured daily over a 3-week period.
In support of our hypotheses, within-person variability in gratitude predicted differences in loneliness and health. Furthermore, those in the treatment group showed stronger cumulative effects of gratitude on loneliness and health symptoms when aggregated across the 20-day study. Additionally, a series of conditional, multilevel indirect effect models found that loneliness acted as a mechanism for gratitude's differential impact on subjective well-being and health symptoms across conditions.
Taken together, this study provides initial evidence that a simple gratitude exercise can strengthen associations among daily gratitude and loneliness and, consequently, improve health, for older adults.
Reference:
- Bartlett MY, Arpin SN. Gratitude and Loneliness: Enhancing Health and Well-Being in Older Adults. Res Aging. 2019 Sep;41(8):772-793. doi: 10.1177/0164027519845354. Epub 2019 May 1. PMID: 31043126.
Study: How Breath-Control Can Change Your Life: A Systematic Review on Psycho-Physiological Correlates of Slow Breathing
- Background:
- The psycho-physiological changes in brain-body interaction observed in most of meditative and relaxing practices rely on voluntary slowing down of breath frequency. However, the identification of mechanisms linking breath control to its psychophysiological effects is still under debate.
- This systematic review is aimed at unveiling psychophysiological mechanisms underlying slow breathing techniques (<10 breaths/minute) and their effects on healthy subjects.
- Methods:
- A systematic search of MEDLINE and SCOPUS databases, using keywords related to both breathing techniques and to their psychophysiological outcomes, focusing on cardio-respiratory and central nervous system, has been conducted.
- From a pool of 2,461 abstracts only 15 articles met eligibility criteria and were included in the review. The present systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
- Results:
- The main effects of slow breathing techniques cover autonomic and central nervous systems activities as well as the psychological status.
- Slow breathing techniques promote autonomic changes increasing Heart Rate Variability and Respiratory Sinus Arrhythmia paralleled by Central Nervous System (CNS) activity modifications.
- EEG studies show an increase in alpha and a decrease in theta power.
- Anatomically, the only available fMRI study highlights increased activity in cortical (e.g., prefrontal, motor, and parietal cortices) and subcortical (e.g., pons, thalamus, sub-parabrachial nucleus, periaqueductal gray, and hypothalamus) structures.
- Psychological/behavioral outputs related to the abovementioned changes are
- increased comfort
- relaxation
- pleasantness
- vigor and alertness
- reduced symptoms of arousal, anxiety, depression, anger, and confusion
- Conclusions:
- Slow breathing techniques act enhancing autonomic, cerebral and psychological flexibility in a scenario of mutual interactions: we found evidence of links between
- parasympathetic activity (increased HRV and LF power)
- CNS activities (increased EEG alpha power and decreased EEG theta power) related to emotional control
- psychological well-being in healthy subjects
- Our hypothesis considers two different mechanisms for explaining psychophysiological changes induced by voluntary control of slow breathing:
- one is related to a voluntary regulation of internal bodily states (enteroception)
- the other is associated to the role of mechanoceptors within the nasal vault in translating slow breathing in a modulation of olfactory bulb activity, which in turn tunes the activity of the entire cortical mantle.
- Slow breathing techniques act enhancing autonomic, cerebral and psychological flexibility in a scenario of mutual interactions: we found evidence of links between
Reference:
- Zaccaro A, Piarulli A, Laurino M, Garbella E, Menicucci D, Neri B, Gemignani A. How Breath-Control Can Change Your Life: A Systematic Review on Psycho-Physiological Correlates of Slow Breathing. Front Hum Neurosci. 2018 Sep 7;12:353. doi: 10.3389/fnhum.2018.00353. PMID: 30245619; PMCID: PMC6137615.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6137615/
Study: Latent Diversity in Human Concepts (Language hinders discourse)
- Many social and legal conflicts hinge on semantic disagreements. Understanding the origins and implications of these disagreements necessitates novel methods for identifying and quantifying variation in semantic cognition between individuals.
- We collected conceptual similarity ratings and feature judgements from a variety of words in two domains. We analyzed this data using a non-parametric clustering scheme, as well as an ecological statistical estimator, in order to infer the number of different variants of common concepts that exist in the population.
- Our results show at least ten to thirty quantifiably different variants of word meanings exist for even common nouns.
- Further, people are unaware of this variation, and exhibit a strong bias to erroneously believe that other people share their semantics.
- This highlights conceptual factors that likely interfere with productive political and social discourse.
Reference:
- Louis Marti, Shengyi Wu, Steven T. Piantadosi, Celeste Kidd; Latent Diversity in Human Concepts. Open Mind 2023; 7 79–92. doi: https://doi.org/10.1162/opmi_a_00072
- https://direct.mit.edu/opmi/article/doi/10.1162/opmi_a_00072/114924
- https://news.berkeley.edu/2023/03/16/new-evidence-on-why-we-talk-past-each-other/
Study: The Relationship Between Gratitude and Loneliness: The Potential Benefits of Gratitude for Promoting Social Bonds
This paper explores the potential role of gratitude on the reduction of loneliness feelings, even controlling for several variables related to social desirability, well-being (subjective happiness and life satisfaction) and socio-demographic characteristics.
Through a web-based survey a convenience sample of 197 participants completed an online questionnaire including these measures.
Correlation analyses and four-step hierarchical multiple regression analyses were conducted.
The results show a negative correlation between gratitude and loneliness; specifically, gratitude succeeds in accounting for up to almost one-fifth of the total variability of loneliness even controlling for further variables.
Being female, not having a stable and consolidated relationship and not participating in the labor force represent some risk factors affecting loneliness which should be taken into account in further research.
Reference:
- Caputo A. The Relationship Between Gratitude and Loneliness: The Potential Benefits of Gratitude for Promoting Social Bonds. Eur J Psychol. 2015 May 29;11(2):323-34. doi: 10.5964/ejop.v11i2.826. PMID: 27247660; PMCID: PMC4873114.
Study: The utility of prolonged respiratory exhalation for reducing physiological and psychological arousal in non-threatening and threatening situations
To determine whether slowing and altering the respiratory pattern is an effective means for reducing physiological and psychological arousal, subjects participated in one of three treatment conditions in which they reduced their respiration rate to 6 cpm and either inhaled quickly and exhaled slowly, inhaled slowly and exhaled quickly, or spent equal amounts of time inhaling and exhaling.
Other subjects participated in a distraction control condition or in a no-treatment control condition.
Arousal was measured during a practice period, a threat (electric shocks) anticipation period, and a threat confrontation period.
The results indicated that the breathing manipulations were not effective in reducing arousal during the practice period, but that inhaling quickly and exhaling slowly was consistently effective for reducing physiological (skin resistance) and psychological (subjective cognitive) arousal during the anticipation and confrontation periods.
Reference:
- Cappo BM, Holmes DS. The utility of prolonged respiratory exhalation for reducing physiological and psychological arousal in non-threatening and threatening situations. J Psychosom Res. 1984;28(4):265-73. doi: 10.1016/0022-3999(84)90048-5. PMID: 6481661.
Study: Gratitude and Mortality Among Older US Female Nurses
Key Points
- Question
- Do people who more frequently notice and feel grateful for positive experiences tend to live longer?
- Findings
- In this cohort study of older US female nurses, experiencing more grateful affect was associated with lower mortality.
- Individuals in the highest tertile of gratitude, compared with the lowest tertile, had a 9% lower hazard of deaths from any cause, after accounting for baseline sociodemographic characteristics, social participation, religious involvement, physical health, lifestyle factors, cognitive function, and mental health.
- Meaning
- The findings suggest that the experience of grateful affect is associated with increased longevity among older adults.
Abstract
Importance
- Supporting healthy aging is a US public health priority, and gratitude is a potentially modifiable psychological factor that may enhance health and well-being in older adults. However, the association between gratitude and mortality has not been studied.
Objective
- To examine the association of gratitude with all-cause and cause-specific mortality in later life.
Design, Setting, and Participants
- This population-based prospective cohort study used data from self-reported questionnaires and medical records of 49,275 US older female registered nurses who participated in the Nurses' Health Study (2016 questionnaire wave to December 2019). Cox proportional hazards regression models estimated the hazard ratio (HR) of deaths by self-reported levels of gratitude at baseline. These models adjusted for baseline sociodemographic characteristics, social participation, physical health, lifestyle factors, cognitive function, and mental health. Data analysis was conducted from December 2022 to April 2024.
Exposure
- Gratitude was assessed with the 6-item Gratitude Questionnaire, a validated and widely used measure of one's tendency to experience grateful affect.
Main Outcomes and Measures
- Deaths were identified from the National Death Index, state statistics records, reports by next of kin, and the postal system. Causes of death were ascertained by physicians through reviewing death certificates and medical records.
Results
- Among the 49,275 participants (all female; mean [SD] age at baseline, 79 [6.16] years), 4608 incident deaths were identified over 151,496 person-years of follow-up.
- Greater gratitude at baseline was associated with a lower hazard of mortality in a monotonic fashion. For instance, the highest tertile of gratitude, compared with the lowest tertile, was associated with a lower hazard of all-cause deaths (HR, 0.91; 95% CI, 0.84-0.99) after adjusting for baseline sociodemographic characteristics, social participation, religious involvement, physical health, lifestyle factors, cognitive function, and mental health.
- When considering cause-specific deaths, death from cardiovascular disease was inversely associated with gratitude (HR, 0.85; 95% CI, 0.73-0.995).
Conclusions and Relevance
- This study provides the first empirical evidence suggesting that experiencing grateful affect is associated with increased longevity among older adults. The findings will need to be replicated in future studies with more representative samples.
Reference:
- Chen Y, Okereke OI, Kim ES, Tiemeier H, Kubzansky LD, VanderWeele TJ. Gratitude and Mortality Among Older US Female Nurses. JAMA Psychiatry. 2024 Jul 3. doi: 10.1001/jamapsychiatry.2024.1687. Epub ahead of print. PMID: 38959002.
The Gratitude Questionnaire – Six Item Form (GQ-6)
The Gratitude Questionnaire-Six-Item Form (GQ-6) is a six-item self-report questionnaire designed to assess individual differences in the proneness to experience gratitude in daily life.
Instructions: Using the scale below as a guide, write a number beside each statement to indicate how much you agree with it.
- 1 = strongly disagree
- 2 = disagree
- 3 = slightly disagree
- 4 = neutral
- 5 = slightly agree
- 6 = agree
- 7 = strongly agree
___1. I have so much in life to be thankful for. ___2. If I had to list everything that I felt grateful for, it would be a very long list. ___3. When I look at the world, I don't see much to be grateful for. ___4. I am grateful to a wide variety of people. ___5. As I get older I find myself more able to appreciate the people, events, and situations that have been part of my life history. ___6. Long amounts of time can go by before I feel grateful to something or someone.
Scoring: Compute a mean across the item ratings; items 3 and 6 are reverse-scored
- For example, if you scored a '7', give yourself a '1'. If you scored a '6', give yourself a '2'.
INTERPRETATION OF SCORES
Based on a sample of 1,224 adults who took the GQ-6 as part of a feature on the Spirituality and Health Web Site, here are some benchmarks for making sense of your score:
- 75th Percentile (>41):
- Someone who scored a 41 out of 42 on the GQ-6 scored higher than 75% of the people who took the survey. If you scored a 42 or higher, then you scored among the top 13% of people who took the survey.
- 50th Percentile (38):
- Someone who scored a 38 out of 42 on the GQ-6 scored higher than 50% of the people who took it. If you scored below a 38, then you are in the bottom 50% of people who took the survey.
- 25th Percentile (<35):
- Someone who scored a 35 out of 42 on the GQ-6 scored higher than 25% of the people who took it. If you scored below a 35, then you are in the bottom 25% of the sample of people who took the survey in terms of gratitude.
Reference:
- McCullough, M. E., Emmons, R. A., & Tsang, J. (2002). The grateful disposition: A conceptual and empirical topography. Journal of Personality and Social Psychology, 82, 112-127.
Study: The Effort Paradox: Effort Is Both Costly and Valued
According to prominent models in cognitive psychology, neuroscience, and economics, effort (be it physical or mental) is costly: When given a choice, humans and non-human animals alike tend to avoid effort.
Here, we suggest that the opposite is also true and review extensive evidence that effort can also add value.
Not only can the same outcomes be more rewarding if we apply more (not less) effort, sometimes we select options precisely because they require effort.
Given the increasing recognition of effort's role in motivation, cognitive control, and value-based decision-making, considering this neglected side of effort will not only improve formal computational models, but also provide clues about how to promote sustained mental effort across time.
The real price of every thing, what every thing really costs to the [person] who wants to acquire it, is the toil and trouble of acquiring it.
-Adam Smith
Satisfaction lies in the effort, not in the attainment, full effort is full victory.
-Mahatma Gandhi
Highlights
- Prominent models in the cognitive sciences indicate that mental and physical effort is costly, and that we avoid it. Here, we suggest that this is only half of the story.
- Humans and non-human animals alike tend to associate effort with reward and will sometimes select objects or activities precisely because they require effort (e.g., mountain climbing, ultra-marathons).
- Effort adds value to the products of effort, but effort itself also has value.
- Effort’s value can not only be accessed concurrently with or immediately following effort exertion, but also in anticipation of such expenditure, suggesting that we already have an intuitive understanding of effort’s potential positive value.
- If effort is consistently rewarded, people might learn that effort is valuable and become more willing to exert it in general.
Reference:
- Inzlicht M, Shenhav A, Olivola CY. The Effort Paradox: Effort Is Both Costly and Valued. Trends Cogn Sci. 2018 Apr;22(4):337-349. doi: 10.1016/j.tics.2018.01.007. Epub 2018 Feb 21. PMID: 29477776; PMCID: PMC6172040.
Study: Comparing the Effects of Square, 4-7-8, and 6 Breaths-per-Minute Breathing Conditions on Heart Rate Variability, CO2 Levels, and Mood
Square and 4-7-8 breathing are popularly promoted by psychotherapists but have little empirical support.
We hypothesized that breathing at 6 breaths per minute (bpm) would improve HRV, reduce blood pressure, and improve mood more than either square or 4-7-8 breathing. We also hypothesized square and 4-7-8 breathing would increase end-tidal CO2 (PETCO2).
Eighty-four college students (60% female) had HRV measured at baseline and during
- square breathing
- 4-7-8 breathing
- 6 bpm with a 4:6 inhale-to-exhale ratio
- 6 bpm with a 5:5 ratio
We used a 3-lead electrocardiogram to measure HRV and a capnometer to measure PETCO2. We measured mood using the Scale of Positive and Negative Experience (SPANE) after each breathing condition. We used a repeated measures mixed effects model to examine the effects of each breathing technique on HRV, blood pressure, mood, and PETCO2 levels.
Results:
- Breathing at 6 bpm increased HRV measures more than square or 4-7-8 breathing with small to medium effects.
- None of the breathing conditions resulted in meaningful changes in blood pressure or mood.
- Unexpectedly, breathing at 6 bpm led to mild over-breathing.
While various breathing techniques are used in psychotherapy, their relative efficacy remains unclear. This study found that breathing at 6 bpm is likely more effective at increasing HRV than square or 4-7-8 breathing, albeit with a higher risk of over-breathing. Future studies could examine whether these effects hold over multiple weeks of breathing practice and attend to the effects of different breathing techniques on CO2 levels.
Reference:
- Marchant J, Khazan I, Cressman M, Steffen P. Comparing the Effects of Square, 4-7-8, and 6 Breaths-per-Minute Breathing Conditions on Heart Rate Variability, CO2 Levels, and Mood. Appl Psychophysiol Biofeedback. 2025 Jun;50(2):261-276. doi: 10.1007/s10484-025-09688-z. PMID: 39864026.
Breathing 4-7-8 - Study: Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults
Notes:
- At first, the inhalation and exhalation duration were equal (4 seconds) and then, little by little, exhalation became longer than inhalation (4 seconds in and 6 seconds out). The whole exercise lasted 5 min.
- The two main HRV outcomes were the High Frequency band (HF) and the Root Mean Squared of Successive Differences (RMSSD) as they reflect parasympathetic activity through parasympathetic mediated changes in HRV.
Anxiety is recognized as a major health issue and is quite prevalent among older adults. An efficient way to manage anxiety is abdominal breathing.
Breathing exercises seem to reduce anxiety and to increase parasympathetic activity assessed by HRV indexes. Yet, the effect of abdominal breathing on physiological stress (HRV) and anxiety in older adults remains poorly understood.
Therefore, the aim of this study is to test the effects of deep and slow breathing (DSB, low inhale/exhale ratio) on physiological stress and anxiety in older adults (n = 22) in comparison with younger ones (n = 25).
- DSB increased significantly HFpower and reduced state anxiety in both younger and older adults.
- Interestingly, the increased in HF power was significantly higher among older adults than younger ones.
- As expected, the ratio inhale/exhale being not equal, Root Mean Squared of Successive Differences (RMSSD) did not increase following DSB.
Thus, we provide evidence suggesting that DSB is more beneficial to older adults than younger ones to restore vagal outflow. Despite future work being required, those results provide relevant clinical application leads to manage state anxiety among older adults and to promote successfull aging.
Reference:
- Magnon V, Dutheil F, Vallet GT. Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Sci Rep. 2021 Sep 29;11(1):19267. doi: 10.1038/s41598-021-98736-9. PMID: 34588511; PMCID: PMC8481564.
Calculators
Cardiology
4 Factors of O2 Consumption For Heart Work
- Rate
- Blood Pressure
- Preload
- Contractility
5 Most Common Causes Of Sudden Cardiac Death In Young Athletes
- Herpertrophic Cardiomyopathy
- WPW
- Long QT
- Congenital Aortic Stenosis
- Anomalous coronary
Abdominal Aortic Aneurysm (AAA)
| Size in cm | Risk of rupture in 1 yr (%) |
|---|---|
| < 4 | 0 |
| 4 - 5 | 0.5-5 |
| 5 - 6 | 3 - 15 |
| 6 - 7 | 10 - 20 |
| 7 - 8 | 20 - 40 |
| > 8 | 30 - 50 |
| Aneurysm diameter | ACC/AHA Recommendation |
|---|---|
| > 2.5 cm but <3.0 cm | No surveillance |
| 3.0 - 3.9 cm | Every 2-3 years |
| 4.0 - 5.4 cm | US or CT every 6-12 mo; Consider vascular surgery referral if > 5.0; Elective repair is recommended for appropriace candidates > 5.0cm |
| > 5.4 cm | Surgical Repair |
Reference:
- AFP Aug 2022 Vol 106 No 2
AHA's Simple Seven
This simple, seven step list has been developed to deliver on the hope we all have–to live a long, productive healthy life.
- High blood pressure
- Cholesterol
- Blood Sugar
- Diet
- Physical Activity
- Weight
- Smoking
References:
Arrhythmias
Atrial Fibrillation
See also:
The American Heart Association and American College of Cardiology further classified AF as follows:[2]
- Paroxysmal AF: intermittent in nature, terminating spontaneously or within 7 days of treatment.
- Persistent AF: Failure to terminate in 7 days
- Long-lasting AF: AF lasting for more than 12 months
- Permanent AF: Persistent AF where rhythm strategy is no longer pursued
- Other Types of AF
- Lone AF: Lone AF is used to describe patients younger than 60 years with no other concomitant heart disease and structurally normal heart on an echocardiogram.
- Non-Valvular AF: Defines whether AF is related to valvular disease, replacement, or repair. It is much more difficult to convert valvular AF into sinus rhythm.
Atrial fibrillation is commonly associated with conditions that alter the structure of the heart. Important causes and risk factors for AF are as follows:
- Cardiac Causes
- Hypertensive heart disease
- Coronary artery disease
- Valvular heart disease
- Heart failure
- Congenital heart disease
- Cardiomyopathy
- Infiltrative cardiac disease
- Sick sinus syndrome
- Pre-excitation syndrome
- Non-Cardiac Causes
- Chronic lung disease
- Pulmonary embolism
- Electrolyte abnormalities
- Acute infections
- Thyroid disorders
- Pheochromocytoma
- Hypothermia
- Post-surgical (seen in 35% to 50% of patients post coronary artery bypass graft)[3]
- Age-related fibrosis
- Diabetes
- Obesity
- Metabolic syndrome
- Obstructive sleep apnea
- Chronic kidney disease
- High-intensity exercise
- Genetic factors
Differential Diagnosis
- Sinus tachycardia
- Atrial flutter
- Atrial flutter with variable block
- Atrial tachycardia (AT)
- Multifocal atrial tachycardia (MAT)
- Wolff-Parkinson-White syndrome (WPW)
- Atrioventricular nodal reentry tachycardia (AVNRT)
- Atrioventricular reentry tachycardia (AVRT)
- Junctional ectopic tachycardia
Treatment
- Anticoagulation - Anticoagulation in all patients with a CHA2DS2-VASc score equal to 2 has shown an improved prognosis.
- Anticoagulation is recommended for AF at a CHA2DS2-VASc score of 2 for men and 3 for women without moderate or severe mitral stenosis or a mechanical valve.
- The score has not been validated for mitral stenosis or mechanical valves.
- Direct oral anticoagulants are recommended over warfarin for AF without moderate or severe mitral stenosis or a mechanical valve.
- Warfarin is still recommended for mitral stenosis and mechanical valves.
- Although CHA2DS2-VASc scores of 0 for men and 1 for women do not require treatment, scores of 1 for men and 2 for women are indeterminate and anticoagulation may be considered by shared decision-making.
- Anticoagulation is recommended for AF at a CHA2DS2-VASc score of 2 for men and 3 for women without moderate or severe mitral stenosis or a mechanical valve.
- Rate Control - Rate control is the preferred strategy for all asymptomatic AF patients.
- Ventricular rate control is accepted as alternative to rhythm control for first-line management of chronic AF
- Lenient rate control (<110bpm) is as effective as strict (<80bpm)
- A beta-blocker is preferred for rate control in those with CAD or systolic dysfunction
- Verapamil or diltiazem may be preferred in those with asthma
- Amiodarone may be effective if other drugs have failed
- Rhythm Control
- Treatment of choice for urgent conversion is DC cardioversion
References:
- AFP Vol 101 No 2 Jan 2020
- JAMA Vol 322 No 18 Nov 2019
- Ludhwani D, Wieters JS. Paroxysmal Atrial Fibrillation. [Updated 2023 Jun 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535439/
- CHA2DS2-VASc Risk Stratification Score
Estimation of stroke risk for nonvalvular atrial fibrillation in adults
CHA2DS2-VASc:
- Congestive Heart Failure
- Hypertension
- Age ≥75 Years (Doubled)
- Diabetes Mellitus
- Prior Stroke Or TIA Or Thromboembolism (Doubled)
- Vascular Disease
- Age 65 To 74 Years
- Sex Category
Calculator:
- Sex
- Female (1 point)
- Male (0 points)
- Age
- ≤64 years old (0 points)
- 65 to 74 years old (1 point)
- ≥75 years old (2 points)
- Comorbidities
- Heart failure (1 point)
- Hypertension (documented diagnosis or pharmacologically treated) (1 point)
- Diabetes mellitus (1 point)
- History of stroke, TIA, or thromboembolism (2 points)
- Vascular disease (history of MI, PAD, or aortic atherosclerosis) (1 point)
Table 7: Unadjusted Stroke Rate 0 points: 0.2% per year 1 point: 0.6% per year 2 points: 2.2% per year 3 points: 3.2% per year 4 points: 4.8% per year 5 points: 7.2% per year 6 points: 9.7% per year 7 points: 11.1% per year 8 points: 11% per year 9 points: 12.2% per year
Frequent symptomatic PVCs
- Step 1: Rule out hypothyroidism
- Step 2: Management
- First line:
- Metoprolol succinate (longer acting than tartrate)
- First line:
Supraventricular Tachycardia
Triggers:
- Alcohol
- Anemia
- Caffeine
- Drugs
- Antipsychotics
- Bronchodilattors
- Cannabinoids
- Catecholamines
- Corticosteroids
- Decongestants
- Inotropes
- Loop diuretics
- Stimulants
- Vasodilators
- Electrolyte abnormalitis
- Exercise
- Fever
- Hyperthyroidism
- Hypovolemia
Vagal Meneuvers:
- Carotid sinus massage (5-10 sec)
- Diving reflex (up to 30s): patient submerges face in cold water or bags of ice paced on nose and forehead
- Valsalva (10-15 sec): Patient bears down against a closed glottis or blows through a straw or 10-ml syringe
Reference:
- AFP Vol 107 No 6 Jan 2023
ASCVD
Increase Factors that enhance risk:
- FH of premature ASCVD (M<55, F<65)
- Primary HLD (LDL 160-189, non-HDL 190-219)
- Metabolic syndrome
- CKD
- Chronic inflammatory condition
- Premature menopause (<40) or h/o pre-eclampsia
- High risk race or ethnicity (South Asian ancestry)
- Lipid levels and other biomarkers associated with incresaed 10y ASCVD:
- Persistent hypertriglyceridemia (>175)
- High sensitivity CRP >=2
- Lipoprotein A >=50
- Apolipoprotein B >= 130
- Ankle-brachial index < 0.9
ASCVD Calculation Formula edit
ASCVD Calculation Formula https://ahajournals.org/doi/pdf/10.1161/01.cir.0000437741.48606.98 Table A
Basic Life Support (BLS)
Adults:
- 30 chest compressions followed by 2 ventilations
Exposure
Standard precautions include the use of:
- Personal protective equipment (PPE): Specialized clothing, equipment and supplies that prevent direct contact with potentially infectious materials. PPE includes gloves, CPR breathing barriers, gowns, face shields, protective eyewear and biohazard bags.
- Hand hygiene: Hand washing is the most effective measure to prevent the spread of infection. Alcohol-based hand sanitizers allow you to clean your hands when soap and water are not readily available and your hands are not visibly soiled.
- Engineering controls: Objects used in the workplace that isolate or remove a hazard, reducing the risk of exposure.
- Work practice controls: Methods of working that reduce the likelihood of an exposure incident by changing the way a task is carried out.
- Proper equipment cleaning: After providing care, the equipment and surfaces used should always be cleaned and disinfected or properly disposed.
- Proper spill cleanup procedures: If a spill occurs, appropriate measures should be taken to limit and reduce exposure to possible contaminants.
When an exposure incident occurs, follow these steps as well as any steps outlined by your healthcare facility:
- Wash needlestick injuries, cuts and exposed skin.
- If blood or other body fluids are splashed around the mouth or nose, flush the area with water.
- If eyes are involved, irrigate with clean water, saline or sterile irrigant solution for 20 minutes.
- Clean the contaminated area thoroughly with soap and water.
After the exposure incident has occurred, it important to:
- Report the incident immediately to the appropriate person identified in your facility's infection/exposure control plan.
- Write down what happened, including the time, date and circumstances, actions taken and any other information required by your employer.
- Seek immediate follow-up care according to your facility's infection/exposure control plan.
Assessment
- Perform Visual Survey
- Scene Size-Up
- Safety
- Number of Patients
- Nature of Illness or Mechanism of Injury
- Scene Size-Up
- Obtain Consent
- To obtain consent from an awake and alert adult patient, follow these steps:
- Identify yourself to the patient or legal guardian.
- State your level of training.
- Explain what you observe.
- Explain what you plan to do.
- Ask for permission from the patient to provide care.
- If an adult patient is unresponsive, has an altered mental status, is mentally impaired or is unable to give consent verbally or through a gesture, then consent is implied.
- To obtain consent from an awake and alert adult patient, follow these steps:
- Check for Responsiveness
- Open the Airway
- Simultaneously Check for Breathing, a Pulse and Life-Threatening Bleeding
- no more than 10 seconds
Care
Recovery Positions
- Kneel at the patient's side.
- Lift the patient's arm closest to you up next to their head.
- Place the patient's arm farthest from you next to their side.
- Grasp their leg closest to you, flex it at the hip and bend the knee toward their head.
- Place one of your hands on the patient's shoulder and your other hand on their hip farthest from you.
- Using a smooth motion, roll the patient toward you by pulling their shoulder and hip with your hands. Make sure the patient's head remains in contact with their extended arm.
- Stop all movement when the patient is on their side.
- Place their knee on top of the other knee so that both knees are in a bent position.
- Place the patient's free hand under their chin to help support their head and airway.
To provide care to an adult patient in respiratory arrest or respiratory failure, follow these steps.
- If you have not already done so, activate EMS, the rapid response team or the resuscitation team, as appropriate, and call for an AED.
- Deliver 1 ventilation every 6 seconds; each ventilation should last about 1 second and make the chest begin to rise. If an advanced airway is in place, the rate remains the same.
- Perform primary assessment (Airway, Breathing, Circulation, Disability, Exposure) and emergent/ initial interventions, if not already done.
- Continue to check breathing and pulse every 2 minutes; if pulse becomes absent, start CPR immediately and use an AED when it's available.
- Position patient as appropriate for clinical condition.
- Perform secondary assessment as patient condition allows.
- Reassess patient, recognize issues and provide care as needed.
MI Immediate Care
- ASA
- In cases of suspected MI, administer two to four low-dose (81-mg) aspirin or one 325-mg adult aspirin based on your facility's protocols.
- Make sure that the patient chews the medication.
CPR:
- It is critical to maintain a rate greater than 100 compressions per minute and a depth of at least 2 inches (5 cm). Both rate and depth of compressions are best measured using a feedback device if available.
- Deliver 2 ventilations that last about 1 second each and make the chest begin to rise; allow the air to exit before delivering next ventilation
- To provide ventilations, you can use the following methods:
- Pocket mask ventilations
- Bag-valve-mask resuscitator ventilations
- Mouth-to-mouth ventilations
- Mouth-to-nose ventilations
- For adult patients, high-quality CPR includes 30 chest compressions followed by 2 ventilations. Remember, when an advanced airway is in place, the 30:2 ratio does not apply as one provider delivers 1 ventilation every 6 seconds, while the other provider delivers continuous chest compressions without pausing for ventilations.
Continue CPR/AED use until:
- The team leader tells you to stop.
- Other trained providers arrive to relieve you.
- You see signs of ROSC.
- You are presented with a valid DNR order.
- You are too exhausted to continue.
- The situation becomes unsafe.
If the patient shows signs of ROSC:
- Stop CPR/AED use.
- Check for breathing and a pulse. It is appropriate to check the carotid or femoral pulse when the patient shows signs of ROSC.
- Monitor the patient until more advanced resources take over.
Cardiac Arrest in the Pregnant Patient
BAACC TO LIFE
- Bleeding
- Anesthesia
- Amniotic fluid embolism
- Cardiovascular/cardiomyopathy
- Clot/cerebrovascular
- Trauma
- Overdose (opioids, magnesium sulfate, other)
- Lung injury/acute respiratory distress syndrome
- Ions (glucose, potassium)
- Fever (sepsis)
- Eaclampsia/emergency hypertension
Provide Left Uterine Displacement (LUD)
- From the patient's left side, reach across the patient, place both hands on the right side of the uterus, and pull the uterus to the left and up.
- Alternatively, from the patient's right side, place both hands on the right side of the uterus and push the uterus to the left and up.
Common Legal Considerations
- Duty to Act: The duty to respond to an emergency and provide care. Failure to fulfill these duties could result in legal action.
- Scope of Practice: The range of duties and skills you have acquired in training that you are authorized to perform by your certification to practice.
- Standard of Care: The public's expectation that personnel summoned to an emergency will provide care with a certain level of knowledge and skill.
- Negligence: Failure to follow a reasonable standard of care, thereby causing or contributing to injury or damage.
- Refusal of Care: A competent patient's refusal of care from a healthcare provider. Refusal of care must be honored, even if the patient is seriously injured or ill or desperately needs assistance. A patient can refuse some or all care. If a witness is available, have the witness listen to any refusal of care, and document it in writing.
- Advance Directives: Written instructions that describe a patient's wishes (or the wishes of the parent or legal guardian) regarding medical treatment or healthcare decisions. Guidance for advance directives, including any required identification and verification process, is documented in state, regional or local laws, statutes and/or protocols, and must be followed. Advance directives include:
- Do Not Resuscitate (DNR) orders, also called Do Not Attempt Resuscitation (DNAR) orders.
- Physician Orders for Life-Sustaining Treatment (POLST).
- Battery: The unlawful, harmful or offensive touching of a patient without the patient's consent.
- Abandonment: Discontinuing care once it has begun. You must continue care until someone with equal or more advanced training takes over.
- Confidentiality: While providing care to a patient, you may learn details about the patient that are private and confidential. Do not share this information with anyone except personnel directly associated with the patient's medical care.
- Consent
- To obtain consent from an adult patient, follow these steps:
- Identify yourself to the patient or legal guardian.
- State your level of training.
- Explain what you observe.
- Explain what you plan to do.
- Ask for permission from the patient or legal guardian to provide care.
- If a patient is unresponsive, has an altered mental status, is mentally impaired or is unable to give consent verbally or through a gesture, then consent is implied.
- To obtain consent from an adult patient, follow these steps:
BLS: Children and Adolescents
Definitions:
- An infant is defined as someone under the age of 1.
- Follow infant guidelines
- A child is defined as someone from the age of 1 to the onset of puberty as evidenced by breast development in girls and underarm hair development in boys (usually around the age of 12).
- Follow child guidelines
- An adolescent is defined as someone from the onset of puberty through adulthood.
- Follow adult guidelines
Pulse (60 bpm):
- If their central pulse is > 60 bpm, deliver 1 ventilation every 2 to 3 seconds. If an advanced airway is in place, the rate remains the same.
- If at any time central pulse decreases to ≤ 60 bpm with poor perfusion despite adequate ventilations and oxygen, start CPR.
- If their central pulse is ≤ 60 bpm with signs of poor perfusion, start CPR. If at any time central pulse and perfusion improve, stop CPR and deliver 1 ventilation every 2 to 3 seconds until the patient is ventilating sufficiently.
AED (55 lbs)
- For infants up to 1 year old:
- Use pediatric pads if available. If pediatric pads aren't available—or the AED doesn't have a pediatric setting—it's safe to use adult AED pads or adult levels of energy.
- Always use an anterior/posterior pad placement. To do this, apply one pad to the center of the infant's chest—on the sternum—and one pad to the infant's back between the scapulae
- For children 8 or younger or weighing 55 pounds (25 kg) or less:
- Use pediatric pads if available. If pediatric pads aren't available—or the AED doesn't have a pediatric setting—it's safe to use adult AED pads or adult levels of energy.
- Use an anterior/lateral placement, according to the manufacturer instructions: Place one pad to the right of the sternum and below the right clavicle. Place the other on the left side of the chest on the mid-axillary line, a few inches below the left armpit.
- Or, use an anterior/posterior pad placement, if the AED pads risk touching each other on the child's chest or the manufacturer recommends.
- For children older than 8 years or weighing more than 55 pounds (25 kg):
- Use adult AED pads.
- Use an anterior/lateral or anterior/posterior placement, according to manufacturer instructions.
Compression Depth
- Adult: At least 2 inches (5 cm) but no more than 2.4 inches (6 cm)
- Child: About 2 inches (5 cm) or one-third the anterior-posterior diameter of the chest
- Infant: About 1.5 inches (3.8 cm) or one-third the anterior-posterior diameter of the chest
Obstructed Airway
Encourage the adult or child to continue coughing until they are able to breathe normally.
- If the patient cannot breathe or has a weak or ineffective cough, summon additional resources and obtain consent.
- Perform a series of 5 back blows and 5 abdominal thrusts until the person can cough forcefully, speak, cry or breathe; or they become unresponsive.
Unresponsive Adult or Child
- Immediately begin CPR, starting with chest compressions.
- After each set of compressions, open the patient's mouth and look for the object before attempting ventilations. If you see the object in the patient's mouth, remove it using a finger sweep. If you do not see the object, do not perform a blind finger sweep. Next, attempt 2 ventilations.
Opioid overdose
Notes:
- For a patient in cardiac arrest due to opioid overdose, high-quality CPR remains the priority over naloxone administration and should not be delayed or interrupted.
- For a patient in respiratory arrest due to suspected or known opioid overdose, ventilations remain the priority over the administration of naloxone and should not be delayed or interrupted. Follow the manufacturer's instructions or your facility's protocol for naloxone administration. Subsequent doses of naloxone may be repeated every 2 to 3 minutes as needed
Opioid Overdose Triad
- Pinpoint pupils.
- Respiratory depression.
- Unconsciousness or severe sleepiness.
- Other indicators of opioid overdose include:
- Cyanosis.
- Track marks from intravenous drug use.
- Prescription pill bottles, pipes, needles, syringes, pill powder or other drug-related items.
- History of opioid drug abuse.
Naloxone:
- Naloxone may be administered to adult and pediatric patients via the intravenous (IV), intraosseous (IO), intramuscular (IM), subcutaneous (SC) or intranasal (IN) route.
- Follow the manufacturer's instructions or your facility's protocol for naloxone administration. Subsequent doses of naloxone may be repeated every 2 to 3 minutes as needed. Do not delay or disrupt other interventions, such as ventilations or CPR, while waiting for naloxone to work.
- If the patient responds, place them in a recovery position providing you do not suspect a head, neck, spinal, hip or pelvic injury. If they vomit, suction their airway or call for help to provide suctioning. Reassess the patient for any changes in condition until EMS, the rapid response team or the resuscitation team arrives. If the patient stops responding, immediately reassess breathing and pulse. Then, begin care as appropriate. Repeat naloxone administration every 2 to 3 minutes as needed.
- Monitor the patient for 4 to 6 hours after last dose of naloxone. Consider longer observation times if extended-release or long-acting opioid. Consider admission and initiation of a continuous naloxone infusion if potential for recurrence of respiratory depression due to opioid.
Cardiac Clearance for Surgery
Risk for Major Cardiac Complications following surgery
Assign a point for each:
- High-risk surgery (intraperitoneal, intrathoracic, suprainguinal vascular)
- H/o MI or pos GXT, or current chest pain secondary to myocardial ischemia, current nitrate therapy, or EKG with pathologic Q wave
- H/o CHF, pulmonary edema, r paroxysmal nocturnal dyspnea; or current bilateral rales, S3, or CXR with pulmonary vascular redistribution
- H/o cerebrovascular disease
- Preoperative treatment with insulin
- Preoperative serum creatinine >2.0mg/dL
| Score | Risk class | % Risk for complication |
|---|---|---|
| 0 | I | 0.4 |
| 1 | II | 0.9 |
| 2 | III | 6.6 |
| 3 | IV | 11.0 |
Surgical risk category
- High (Cardiac risk >5%)
- Aortic or other major vascular surgery
- Peripheral vascular surgery
- Intermediate (Cardiac risk 1-5%)
- Carotid endarterectomy
- Head and neck surgery
- Intraperitoneal or intrathoracic surgery
- Orthopedic surgery
- Prostate surgery
- Low (Cardiac risk <1%)
- Superficial procedures
- Breast surgery
- Cataract surgery
- Endoscopic procedures
- Most ambulatory surgeries
References:
- AFP Vol 85 No 3 Feb 2012
Pre-op Clearance
Cardiac Risk Index (Assign 1 point for each risk factor):
- High risk surgery (intraperitoneal, intrathoracic, or suprainguinal vascular surgery)
- History of ischemic heart disease
- Current chest pain from suspected MI
- Current or past use of nitrate therapy
- EKG with pathologic Q waves
- History of MI or positive exercise stress test
- History of heart failure
- CXR with pulmonary vascular redistribution
- Paroxysmal nocturnal dyspnea
- Pulmonary edema, bilateral rales, or S3 gallup
- History of cerebrovascular disease
- History of TIA or stroke
- Preoperative treatment with insulin
- Preoperative creatinin level >2 mg/dL
Score:
| Points | Risk of major cardiac event |
|---|---|
| 0 | 0.4% |
| 1 | 0.9% |
| 2 | 6.6% |
| 3 | 11% |
Surgical procedures risk stratified:
Low risk (<1% risk of major adverse cardiac event)
- Ambulatory surgery
- Breast surgery
- Cataract surgery
- Endoscopic procedures
- Superficial procedures
Higher risk (>1% risk of major adverse cardiac event)
- Aortic and other major vascular surgery
- Emergent procedures
- Head and neck surgery
- Intraperitoneal and intrathoracic surgery
- Open urologic surgery
- Orthopedic surgery
- Prolonged procedures with large fluid shifts and/or blood loss
Antiplatelet management:
- Primary prevention
- Hold before surgery (7-10d if possible) unless risk of major adverse cardiac event is greater than risk of bleeding
- Secondary prevention
- Intracranial, major spinal, or other high risk bleeding surgery:
- Hold before surgery (7-10d if possible) unless risk of major adverse cardiac event is greater than risk of bleeding
- Most other sureries
- Continue perioperatively, unless risk of major adverse cardiac event is greater than risk of bleeding
- Intracranial, major spinal, or other high risk bleeding surgery:
References:
- AFP Vol 95 No 10 May 2017
Cardiac Medications
- ACE Inhibitors
- Indications
- Patients with hypertension, diabetes mellitus, chronic kidney disease, abnormal left ventricular function, systolic heart failure, or recent MI
- Comments
- Decrease mortality rates Use caution in pregnant women and in patients with angioedema, renovascular disease, or hyperkalemia
- Indications
- Angiotensin receptor blockers
- Indications
- Patients in whom ACE inhibitors are not tolerated
- Comments
- No additional benefit vs. ACE inhibitors Use caution in pregnant women and in patients with angioedema, renovascular disease, or hyperkalemia
- Indications
- Beta blockers
- Indications
- First-line therapy in patients with history of MI, acute coronary syndrome, systolic heart failure, angina pectoris, atrial fibrillation, or atrial flutter Consider for patients with essential tremor, hyperthyroidism, or migraine
- Comments
- Decrease mortality rates Use caution in older patients (may increase stroke risk) and in those with bronchospastic disease, second- or third-degree heart block, symptomatic bradycardia, or depression
- Indications
- Calcium channel blockers
- Indications
- Consider for patients whose symptoms are not controlled with or who cannot tolerate beta blockers, and for patients with Raynaud disease Can be used in patients with angina pectoris, atrial fibrillation, or atrial flutter
- Comments
- Use long-acting nondihydropyridines; avoid short-acting nifedipine Use caution in patients with second- or third-degree heart block
- Indications
- Nitrates
- Indications
- Patients with angina whose symptoms are not controlled with beta blockers or calcium channel blockers can use long-acting nitrates; short-acting nitrates can be used for quick relief of symptoms
- Comments
- Evidence lacking on mortality benefit Use caution in patients with hypotension
- Indications
- Ranolazine (Ranexa)
- Indications
- Patients with recent MI or stable coronary artery disease Adjunctive therapy in patients whose symptoms are not controlled with beta blockers or calcium channel blockers, or in whom beta blockers are not tolerated
- Comments
- Does not lower blood pressure Use caution in patients with impaired liver function and in those taking QT-prolonging medications
- Indications
References:
- AFP Vol 97 No 6 Mar 2018
Cardiology Differential
- Coronary circulation
- Arrhythmia
- Valves
- Myocardium
- Pericardium
Cardiovascular Fitness (CRF)
Changes in Cardiorespiratory Fitness and Survival in Patients With or Without Cardiovascular Disease
- During a median follow-up of 6.3 years (IQR: 3.7-9.9 years), 18,302 participants died with an average yearly mortality rate of 27.6 events per 1,000 person-years.
- In general, changes in CRF ≥1.0 MET were associated with inverse and proportionate changes in mortality risk regardless of baseline CRF status.
- For example, a decline in CRF of >2.0 METS was associated with a 74% increase in risk (HR: 1.74; 95% CI: 1.59-1.91) for low-fit individuals with CVD, and 69% increase (HR: 1.69; 95% CI: 1.45-1.96) for those without CVD.
Reference:
- Kokkinos P, Faselis C, Samuel IBH, et al. Changes in Cardiorespiratory Fitness and Survival in Patients With or Without Cardiovascular Disease. J Am Coll Cardiol. 2023;81(12):1137-1147. https://doi.org/10.1016/j.jacc.2023.01.027
- https://www.jacc.org/doi/pdf/10.1016/j.jacc.2023.01.027
Carotid Artery Stenosis
Risk Factors:
- Age
- Smoking
- Diabetes
- HLD
- HTN
Surgical candidates:
- Patients with 50% stenosis of the artery and symptoms
- Patients with 70% or more stenosis
Risk of stroke during procedure:
- Open surgery: 2%
- Trans-Carotid Artery Revascularization (TCAR): between 2-4%
- Carotid Artery Stenting: 4%
After procedure: ASA or clopidogrel
Carotid US Screening
According to the 2011 guidelines from the American College of Cardiology Foundation (ACCF), American Heart Association (AHA), and other societies, carotid duplex ultrasonography is not recommended for routine screening of asymptomatic patients without clinical manifestations or risk factors for atherosclerosis.
It may be considered in asymptomatic patients who have two or more of the following risk factors:
- Hypertension
- Hyperlipidemia
- Tobacco smoking
- A family history of atherosclerosis manifested before age 60 years in a first-degree relative
- A family history of ischemic stroke
The presence of an audible carotid bruit, Hollenhorst plaque on fundoscopic examination, or silent cerebral infarction on brain imaging may warrant carotid ultrasound screening.
Reference:
- Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL, Cates CU, Creager MA, Fowler SB, Friday G, Hertzberg VS, McIff EB, Moore WS, Panagos PD, Riles TS, Rosenwasser RH, Taylor AJ; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Stroke Association; American Association of Neuroscience Nurses; American Association of Neurological Surgeons; American College of Radiology; American Society of Neuroradiology; Congress of Neurological Surgeons; Society of Atherosclerosis Imaging and Prevention; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology; Society of NeuroInterventional Surgery; Society for Vascular Medicine; Society for Vascular Surgery; American Academy of Neurology and Society of Cardiovascular Computed Tomography. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. Stroke. 2011 Aug;42(8):e420-63. doi: 10.1161/STR.0b013e3182112d08. Epub 2011 Jan 31. Erratum in: Stroke. 2011 Aug;42(8):e541. PMID: 21282494.
- https://pubmed.ncbi.nlm.nih.gov/21282494/
Chest pain
Decision rule for likelihood of CAD as cause of Chest Pain
| Component | Points |
|---|---|
| Age and sex (M > 55yo; F > 65yo) | 1 |
| Known vascular disesae (CAD, Occlusive vascular disease, cardiovascular disease) | 1 |
| Pain is not elicited with palpation | 1 |
| Pain is worse with exercise | 1 |
| Patient assumes pain is of cardiac origin | 1 |
Likelihood of CAD as cause of Chest Pain
| Score | Positive Likelihood | Negative Likelihood |
|---|---|---|
| 0 or 1 | 1.09 | 0.00 |
| 2 or 3 | 1.83 | 0.03 |
| 4 or 5 | 4.52 | 0.15 |
References:
- AFP Vol 96 No 5 Sep 2017
Chest pain causes
Other diagnoses chest pain
- Non-ischemic cardiovascular
- Aortic dissection*
- Myocarditis
- Pericarditis
- Chest wall
- Cervical disc disease
- Costochondritis
- Fibrositis
- Herpes zoster (before the rash)
- Neuropathic pain
- Rib fracture
- Sternoclavicular arthritis
- Pulmonary
- Pleuritis
- Pneumonia
- Pulmonary embolus*
- Tension pneumothorax*
- Psychiatric
- Affective disorders (eg, depression)
- Anxiety disorders
- Hyperventilation
- Panic disorder
- Primary anxiety
- Somatiform disorders
- Thought disorders (eg, fixed delusions)
- Gastrointestinal
- Biliary
- Cholangitis
- Cholecystitis
- Choledocholithiasis
- Colic
- Esophageal
- Esophagitis
- Spasm
- Reflux
- Rupture*
- Pancreatitis
Peptic ulcer disease
- Nonperforating
- Perforating*
*Potentially life-threatening conditions.
- ACC/AHA/ACP Guidelines for the Management of Patients with Chronic Stable Angina. J Am Coll Cardiol 1999; 33:2092.
Acute Chest Pain: Outpatient Evaluation edit
Definitions:
- Typical chest pain or angina is:
- a deep, poorly localized chest or arm discomfort (pain or pressure) associated with physical exertion or emotional stress and relieved with rest or sublingual nitroglycerin within five minutes.
- Unstable angina is:
- new-onset angina, angina at rest, or angina that becomes more frequent, severe, or prolonged.
- Acute myocardial infarction is:
- myocardial injury resulting in elevated cardiac biomarkers in the setting of acute ischemia caused by ST segment elevation myocardial infarction or non–ST segment elevation myocardial infarction.
The most common causes of chest pain in the primary care population are:
- chest wall pain (20% to 50%)
- reflux esophagitis (10% to 20%)
- and costochondritis (13%)
Other potential factors include:
- pulmonary etiologies (pneumonia, pulmonary embolism [PE])
- psychological etiologies (panic disorder)
- and nonischemic cardiovascular disorders (congestive heart failure, thoracic aortic dissection)
- No definitive diagnosis may be found in as many as 15% of patients
| Age range (years) | Men | Women | ||||
|---|---|---|---|---|---|---|
| Typical | Atypical | Nonanginal | Typical | Atypical | Nonanginal | |
| 40 to 49 | 69% | 38% | 25% | 37% | 14% | 8% |
| 50 to 59 | 77% | 49% | 34% | 47% | 20% | 12% |
| 60 to 69 | 84% | 59% | 44% | 58% | 28% | 17% |
| 70 to 79 | 89% | 69% | 54% | 68% | 37% | 24% |
| > 80 | 93% | 77% | 65% | 76% | 47% | 32% |
Marburg Heart Score
| Component | Points |
|---|---|
| Sex/age (women > 65 years; men > 55 years) | 1 |
| Known clinical vascular disease (CAD, occlusive vascular disease, cerebrovascular disease) | 1 |
| Increased pain with exercise | 1 |
| Pain not elicited with palpation of chest wall | 1 |
| Patient assumes pain is of cardiac origin | 1 |
| Score | Likelihood ratio | 2.00% | 10.00% | 20.00% |
| 0 to 1 point | 0.04 | 0.1 | 0.4 | 0.9 |
| 2 to 3 points | 0.92 | 1.8 | 9.3 | 18.8 |
| 4 to 5 points | 11.2 | 18.6 | 55.5 | 73.7 |
Nonischemic Causes of Chest Pain
- Cardiac
- Acute aortic dissection
- Heart failure
- MICE criteria (Male sex, history of myocardial Infarction, basal lung Crepitations, and ankle Edema) likely have heart failure -> Echo
- Pericarditis
- Gastrointestinal
- Gastroesophageal reflux disease
- A one-week trial of a high-dose proton pump inhibitor is modestly sensitive and specific for GERD, with a 50% reduction in reflux symptoms being moderately accurate for a final diagnosis of GERD (LR+ = 5.5; LR− = 0.24)
- Gastroesophageal reflux disease
- Musculoskeletal
- Chest wall pain (33% to 50% of chest pain)
- Costochondritis
- Psychological
- Panic attack
- In the past four weeks, have you had an anxiety attack (suddenly feeling fear or panic)?
- This question is good at supporting a diagnosis of panic disorder when patients answer yes (LR+ = 4.2) and is good at ruling it out when the answer is no (LR− = 0.09)
- Panic attack
- Pulmonary
- Pneumonia
- Egophony (LR+ = 8.6), dullness to percussion of the posterior thorax (LR+ = 4.3), and respiratory rate greater than 20 breaths per minute (LR+ = 3.5) are suggestive of pneumonia.
- Normal temperature, heart rate, and respiratory rate with a normal pulmonary examination rules out pneumonia (LR− = 0.10)
- Pulmonary embolism
- Wells criteria
- The Pulmonary Embolism Rule-out Criteria were developed to specifically rule out PE in the primary care setting.46 Patients meeting all eight criteria (50 years or younger, heart rate less than 100 beats per minute, oxygen saturation greater than 94%, no unilateral leg swelling, no hemoptysis, no surgery or trauma within four weeks, no previous deep venous thrombosis or PE, no oral hormone use) have a less than 1% likelihood of PE and thus do not need d-dimer testing or imaging.
- Pneumonia
| Criteria | Points |
|---|---|
| Signs or symptoms of DVT (leg swelling or pain with palpation of deep vein) | 3 |
| Diagnosis of PE is more likely than an alternative diagnosis | 3 |
| Heart rate > 100 beats per minute | 1.5 |
| Immobilization (bed rest > 3 days) or surgery in past 4 weeks | 1.5 |
| History of PE or DVT | 1.5 |
| Hemoptysis | 1 |
| Active malignancy (or cancer treatment stopped in past 6 months) | 1 |
| Total points | Risk of PE | Probability of PE(overall probability = 9.2%) |
|---|---|---|
| 0 to 1 point | Low | 1.3 |
| 2 to 6 points | Moderate | 16.2 |
| More than 6 points | High | 37.5 |
Those at low or intermediate risk of ACS can undergo exercise stress testing, coronary computed tomography angiography, or cardiac magnetic resonance imaging
In those with low suspicion for ACS, consider other diagnoses such as chest wall pain or costochondritis, gastroesophageal reflux disease, and panic disorder or anxiety states. Other less common, but important, diagnostic considerations include acute pericarditis, pneumonia, heart failure, pulmonary embolism, and acute thoracic aortic dissection.
The Marburg Heart Score and the INTERCHEST clinical decision rule can also help estimate ACS risk. Twelve-lead electrocardiography is recommended to look for ST segment changes, new-onset left bundle branch block, presence of Q waves, and new T-wave inversions. Patients with suspicion of ACS or changes on electrocardiography should be transported immediately to the emergency department.
References:
- AFP Vol 102 No 12 Dec 2020
Acute MI
Most useful rule to rule in MI is:
- Chest pain with radiation to both arms, followed by radiation to the right arm
Most useful elements to rule out MI are:
- Pleuritic chest pain
- Sharp pain
- Pain reproduced with palpation
LOE A
References:
- AFP Vol 96 No 5 Sep 2017
2hr MI rule out
- Rule out MI if the max trop evel is <0.014 mcg/L and absolute change over 2hrs is < 0.0004 mcg/L
- Rule in MI if max trop level is >0.052 mcg/L or the absolute change over 2hrs is >0.009 mcg/L
- Further observe those not in either category
References:
- Am J Med 2015;128(4):369-379
Common triggers for AF edit
Here are some common triggers for atrial fibrillation (Afib):
- Cardiovascular Conditions (Most Significant):
- High Blood Pressure (Hypertension)
- Coronary Artery Disease (CAD)
- Heart Valve Problems (Mitral valve stenosis and mitral regurgitation are strongly linked, though Tricuspid valve problems can also contribute)
- Heart Failure
- Cardiomyopathy
- Pericarditis/Pericardial Effusion
- Lifestyle Factors:
- Obesity
- Excessive Alcohol Consumption
- Caffeine
- Nicotine
- Stress
- Lack of Sleep
- Medical Conditions:
- Hyperthyroidism
- Anemia
- Sleep Apnea
- Chronic Kidney Disease
- Inflammatory Conditions
- Certain infections (e.g., pneumonia, viral infections)
- Other
- Some medications
- Intense exercise can sometimes trigger Afib, particularly in those with underlying conditions
- Electrolyte Imbalances such as low potassium, low magnesium, and low calcium
Compression Socks edit
Compression stockings are medical grade devices designed to move blood flow.
Support compression stockings are made available in multiple compression support levels.
Most commonly compression support stockings come in:
- Mild (8-15 mmHg)
- Provides relief and minimizes tired and achy legs.
- Prevents fatigued legs from long periods of sitting or standing.
- Helps relieve minor swelling of feet, ankles, and legs.
- During pregnancy, helps prevent the formation of varicose and spider veins.
- Helps maintain healthy, energized legs.
- Medium (15-20 mmHg)
- For the prevention and relief of minor to moderate varicose and spider veins.
- Helps relieve tired, aching legs, and minor swelling of feet, ankles, and legs.
- During pregnancy, helps prevent varicose veins and spider veins.
- Helps prevent deep vein thrombosis (DVT), also known as economy class syndrome.
- Used in post-sclerotherapy treatment to help prevent the reappearance of varicose veins and spider veins.
- Ideal compression level used for those traveling long distances.
- Firm (20-30 mmHg)
- Helps prevent and relieve moderate to severe varicose veins (also during pregnancy).
- For post-surgical and post-sclerotherapy treatment to help prevent the reappearance of varicose and spider veins.
- Helps in treatment of moderate to severe edema or lymphatic edema.
- Helps with the management of active ulcers and manifestations of post-thrombotic syndrome (PTS).
- Helps relieve superficial thrombophlebitis.
- Helps prevent orthostatic hypotension (sudden fall in blood pressure when standing).
- Helps prevent deep vein thrombosis (DVT), also known as economy class syndrome.
- X-Firm (30-40 mmHg)
- Helps prevent and relieve severe varicose veins.
- Used in the treatment of severe edema and lymphedema.
- Used in post-surgical and post-sclerotherapy treatment to help prevent the reappearance of varicose and spider veins.
- Helps reduce symptoms of Orthostatic Hypotension and Postural Hypotension
- For the management of Venous Ulcers and manifestations of Post-Thrombotic Syndrome (PTS).
- Prevents deep vein thrombosis (DVT), also known as economy class syndrome.
- Rx (40-50 mmHg)
- Generally indicated for more Serious Venous Diseases such as Acute Leg/Ankle Swelling, Varicose Veins, Chronic Vein Insufficiency and Deep Vein Thrombosis
Coronary Artery Calcium Score
See also:
The following definitions are used to relate the CAC score to the extent of underlying coronary artery disease (3):
- Coronary calcium score 0: No identifiable coronary artery disease.
- Coronary calcium score 1-99: Mild coronary artery disease.
- Coronary calcium score 101-400: Moderate coronary artery disease.
- Coronary calcium score > 400: Extensive coronary artery disease.
When interpreting the CAC score, it is essential to consider age and gender. Women, in general, have lower calcium scores than men.
CAC score increases with age. Hence, at a certain age, we will be expected to have a specific CAC score that would be considered normal for that age. This score would then reflect the age of our arteries or the arterial age.
If everything is normal, we would expect our arterial age to be the same as our observed age.
However, if the CAC score is high, our arterial age may be higher than our observed age. Conversely, if our CAC score is low, the arterial age may be lower than our observed age.
| CAC | Arterial Age in Years (95% CI) | CAC | Arterial Age in Years (95% CI) |
|---|---|---|---|
| 0 | 39 (32–46) | 100 | 73 (71–74) |
| 10 | 56 (53–60) | 200 | 78 (75–80) |
| 20 | 61 (59–63) | 300 | 80 (78–83) |
| 30 | 64 (62–66) | 400 | 83 (79–86) |
| 40 | 66 (65–67) | 500 | 84 (80–88) |
| 50 | 68 (67–69) | 750 | 87 (83–92) |
| 60 | 69 (68–70) | 1000 | 89 (84–94) |
| 70 | 70 (69–71) | 1500 | 92 (87–98) |
| 80 | 71 (70–72) | 2000 | 94 (88–100) |
| 90 | 72 (71–73) | 2500 | 96 (89–102) |
Guidelines for coronary calcium scoring by 2010 ACCF task force
These guidelines are latest at time of writing (July 2016):
- Intermediate cardiovascular risk and asymptomatic adults (class IIa)
- Low-to-intermediate risk and asymptomatic adults (class IIb)
- Low risk and asymptomatic (class III)
- Asymptomatic adults with diabetes mellitus, 40 years of age and older (class IIa)
| CAC | Comment |
|---|---|
| 0 | May defer statins up to 10 years; Exceptions: severe family history of premature, ASCVD, DM, severe hypercholeserolemia, active tobacco use |
| 1-99 | Risk discussion to review options for patient: Risk enhancing factors favor moderate-intensity statin therapy |
| 100-299 | Confirms intermediate risk: moderate-intensity statin therapy indicated |
| 300+ | Confirms higher risk: high-intensity statin therapy indicated |
Reference:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2621006/
- https://radiopaedia.org/articles/agatston-score
- AJM Vol 134 No 9 Sep 2021
Coronary Artery Disease
Stable coronary artery disease:
- Reversible supply/demand mismatch related to ischemia, a history of MI, or the presence of plaque documented on catheterization or CTA
- Stable if asymptomatic or controlled by medications or revascularization
- No evidence PCPI provides better outcomes than medical therapy for stable mod-severe CAD
- ISCHEMIA Trial NEJM 4/2020
Treatment:
- Lifestyle changes
- 30-60 min of mod-intensity aerobic activity (Reduces cardiovascular mortality - RR=0.74; 95% CI 0.64-0.86)
- Risk factor modification
- Antiplatelet and antianginal therapy
- If NO recent stent placement
- If no contraindication to ASA -> ASA 75-162mg daily
- If contraindication to ASA -> Clopidogrel 75mg daily
- If recent stent placement
- Dual antiplateley therapy: ASA + P2Y12 (clopidogrel, ticagrelor, or prasugrel)
- Drug eluting stent -> Continue for 6-12 mo
- Bare-metal stent -> Continue for 1-12 mo
- Dual antiplateley therapy: ASA + P2Y12 (clopidogrel, ticagrelor, or prasugrel)
- If NO recent stent placement
- Angina
- Sublingual NG
- B-blockers
- If symptoms not controlled:
- CCB
- Long acting nitrate
- Ranolazine
- If persistent angina -> Consider CABG or PCI
- Heart Failure
- Preserved EF -> Lifestyle modifications
- Reduced EF:
- Diuretics
- B-Blockers
- ACE inhibitors
- Angiotensin receptor blockers
- Lifestyle modifications
References:
- AFP Vol 97 No 6 Mar 2018
Acute Coronary Syndrome
High likelihood of ACS:
- Chest pain radiating to one or both arms
- Chest pain associated with exertion, nausea, vomiting, or diaphoresis
- Chest pain described as pressure or as "worse than previous angina or similar to a previous MI"
Low likelihood of ACS:
- Stabbing, pleuritic, or positional chest pain
- Pain in an inframammary location
- Pain not associated with exertion
- Pain is reproducible with palpation
Rule OUT CAD with Marburg Heart Score:
| Factor | Score |
|---|---|
| F >64y, M >54y | 1 pt |
| Known CAD, cerebrovascular, or peripheral vascular Dz | 1 pt |
| Pain worse with Ex | 1 pt |
| Pain not reproducible with palpation | 1 pt |
| Patient assumes pain is cardiac | 1 pt |
- Score of 2 or less = 98% of pts with no CAD
- Score >2 -> 23% with CAD
References:
- JFP Vol 63, No 5 May 2014
Rule to Predict CAD as cause of Chest Pain (Validated)
Give 1 point for each of these:
- Men >55 or Women >65
- Known vascular disease (CAD, occlusive vascular, cerebrovascular, etc)
- Pain worse with exercise
- Pain not elicited with palpation
- Patient assumes pain is cardiac origin
| Score | Pos likelihood | Neg likelihood |
|---|---|---|
| 0 - 1 | 1.09 | 0.00 |
| 2 - 3 | 1.83 | 0.03 |
| 4 - 5 | 4.52 | 0.16 |
References:
- AFP Vol 87 No 3 Feb 2013
Cardiac CT (CCTA)
Indications:
- Detection of CAD in symptomatic patients without known heart disease, either nonacute or acute presentations
- Detection of CAD in patients with new-onset or newly diagnosed clinical heart failure and no prior CAD
- Preoperative coronary assessment prior to noncoronary cardiac surgery
- Patients with prior electrocardiographic exercise testing - Normal test with continued symptoms or intermediate risk Duke treadmill score
- Patients with prior stress imaging procedures - Discordant electrocardiographic exercise and imaging results or equivocal stress imaging results
- Evaluation of new or worsening symptoms in the setting of a past normal stress imaging study
- Risk assessment post-revascularization - Symptomatic if post-coronary artery bypass grafting or asymptomatic with prior left main coronary stent of 3 mm or greater
- Evaluation of cardiac structure and function in adult congenital heart disease
- Evaluation of cardiac structure and function - Ventricular morphology and systolic function
- Evaluation of cardiac structure and function - Intracardiac and extracardiac structures
AHA Guidelines:
- Asymptomatic patients should be assessed for cardiovascular risk using tools such as the Framingham Risk Score; those found to be at low risk (10-year risk of less than 10 percent) or high risk (10-year risk of more than 20 percent) do not benefit from coronary calcium assessment
- LOE B
- In clinically selected, intermediate-risk patients (10-year risk of 10 to 20 percent), it may be reasonable to measure the atherosclerosis burden using electron beam CT or multidetector CT to refine clinical risk prediction and to select patients for more aggressive target values for lipid-lowering therapies
- LOE B
- Coronary calcium assessment may be reasonable in symptomatic patients, especially in the setting of equivocal treadmill or functional testing
- LOE B
- Coronary calcium assessment may be considered in symptomatic patients to determine the cause of cardiomyopathy
- LOE B
- Coronary calcium assessment may be considered in patients with chest pain who have equivocal or normal ECG findings and negative cardiac enzyme test results
- LOE B
- CT coronary angiography is reasonable for the assessment of obstructive disease in symptomatic patients
- LOE B
- Electron beam CT and multidetector CT for detecting restenosis after stent placement cannot be recommended
- LOE C
- CT coronary angiography for the assessment of noncalcified plaque or to track atherosclerosis or stenosis over time is not recommended
- LOE C
- CT coronary angiography is not recommended in asymptomatic persons for the assessment of occult CAD
- LOE C
- Serial imaging for the assessment of coronary calcification progression is not indicated
- LOE C
- The use of hybrid scanning to assess cardiovascular risk or the presence of obstructive disease is not recommended
- LOE C
Calcium Score:
| Calcium Score | Presence of CAD |
|---|---|
| 0 | No evidence of CAD |
| 1-10 | Min evidence of CAD |
| 11-100 | Mild evidence of CAD |
| 101-400 | Mod evidence of CAD |
| 401+ | Extensive evidence of CAD |
Reference:
Costochondritis and Tietze's syndrome edit
| Characteristics | Costochondritis | Tietze's syndrome |
|---|---|---|
| Signs of inflammation | Absent | Present |
| Swelling | Absent | Presence or absence indicates severity of problem |
| Joints affected | Multiple and unilateral > 90%. Usually second to fifth costochondral junctions involved | Usually single and unilateral. Usually second and third costochondral junctions involved |
| Prevalence | Relatively common | Uncommon |
| Age group affected | All age groups, including adolescents and elderly | Common in younger age group |
| Nature of pain | Aching, sharp, pressure like | Aching, sharp, stabbing initially, later persists as dull aching |
| Onset of pain | Repetitive physical activity provokes pain, rarely occurs at rest | New vigorous physical activity such as excessive cough or vomiting, chest impact |
| Aggravation of pain | Movements of upper body, deep breathing, exertional activities | Movements |
| Association with other conditions | Seronegative arthropathies, anginal pain | No known association |
| Diagnosis | Crowing rooster maneuver and other physical examination findings | Physical examination, exclude rheumatoid arthritis, pyogenic arthritis |
| Imaging studies | Chest radiograph, computed tomography scan, or nuclear bone scan to rule out infections or neoplasms if clinically suspected | Bone scintigraphy and ultrasonography can be used for screening for other conditions |
| Treatment | Reassurance, pain control, nonsteroidal antiinflammatory drugs, application of local heat and ice compresses, manual therapy with stretching exercises. Corticosteroid or sulfasalazine injections in refractory patients | Reassurance, pain control with nonsteroidal antiinflammatory drugs, and application of local heat. Corticosteroid and lidocaine injections to the cartilage, or intercostal nerve block in refractory patients |
Reference:
- Rokicki W, Rokicki M, Rydel M. What do we know about Tietze's syndrome? Kardiochir Torakochirurgia Pol. 2018 Sep;15(3):180-182. doi: 10.5114/kitp.2018.78443. Epub 2018 Sep 24. PMID: 30310397; PMCID: PMC6180027.
CVA
Post-CVA
- BP Goal: <130/80
- High dose statin (secondary prevention)
Dual Anti-Platelet Treatment
- Initiate combined clopidogrel plus aspirin within 24 hours of a minor stroke or TIA and continue for no longer than 1 month; then switch patients to aspirin or clopidogrel monotherapy. LOE A
- Do not use combined clopidogrel plus aspirin for long-term secondary stroke prevention. LOE A
- Limit use of aspirin plus extended-release dipyridamole as a first choice for secondary stroke prevention because of limitations in efficacy and poor tolerability. LOE B
References:
- JFP Jul 2020 Vol 69, No 6
CVA Related Calculators
- Dual Anti-platelet: DART app
- ABCD2
- CHADS2-VASC
- HAS-BLED
- SPARC Tool (Stroke/embolism risk)
D-Dimer increased plasma values
- Plasma acts on Fibrin breaking it into Fibrin Degradation Products (FDPs).
- One FDP is D-Dimer, which is 2 D domains of fibrin monomeres crosslinked by activated factor XIII.
- D-dimer is generated from fibrin (NOT fibrinogen) and thus its increase indicates recent or ongoing intravascular coagulation
Associated Disorders:
- Arterial thromboembolic disease:
- Myocardial infarction
- Stroke
- Acute limb ischemia
- Atrial fibrilation
- Intracardiac thrombus
- Venous thromboembolic disease:
- Deep vein thrombosis
- Pulmonary embolism
- Disseminated intravascular coagulation
- Preeclampsia and eclampsia
- Abnormal fibrinolysis; use of thrombolytic agents
- Cardiovascular disease; congestive failure
- Severe infection/sepsis/inflammation
- Surgery/Trauma (eg: tissue eschemia, necrosis
- Systemic inflammatory response syndrome
- Vasoocclussive episode of sickle cell disease
- Severe Liver disease (decreased clearance)
- Malignancy
- Renal disease
- Normal pregnancy
- Venous malformations
References:
- UptoDate.com Graphic 60881
Differential Diagnosis and Treatment of Chest Wall Conditions
| Condition | Diagnostic considerations | Treatment principles |
|---|---|---|
| Costochondritis | Tenderness to palpation of costochondral junctions; reproduces patient's pain; usually multiple sites on same side of chest | Simple analgesics; heat or ice; rarely, local anesthetic injections or corticosteroid injections |
| Destruction of costal cartilage by infections or neoplasm | Bacterial or fungal infections or metastatic neoplasms to costal cartilages; infections occur postsurgery or in intravenous drug users; chest computed tomography imaging useful to show alteration or destruction of cartilage and extension of masses to chest wall | Antibiotics or antifungal drugs; surgical resection of affected costal cartilage; treatment of neoplasm based on tissue type |
| Fibromyalgia | Symmetric tender points at second costochondral junctions, with characteristic tender points in the neck, back, hip, and extremities and widespread pain | Graded exercise is beneficial; cyclobenzaprine (Flexeril), antidepressants, and pregabalin (Lyrica) may be beneficial |
| Herpes zoster of thorax | Clusters of vesicles on red bases that follow one or two dermatomes and do not cross the midline; usually preceded by a prodrome of pain; postherpetic neuralgia is potential complication that is more common in older patients | Oral antiviral agents (e.g., acyclovir, famciclovir [Famvir], valacyclovir [Valtrex]); analgesics as needed for pain; may require narcotics or topical lidocaine patches to control pain |
| Painful xiphoid syndrome | Tenderness at sternoxiphoid joint or over xiphoid process with palpation | Usually self-limited unless associated with congenital deformity of xiphoid; analgesics; rarely, corticosteroid injections |
| Slipping rib syndrome | Tenderness and hypermobility of anterior ends of lower costal cartilages causing pain at lower anterior chest wall or upper abdomen; diagnosis by "hooking maneuver": curving fingers under costal margin and gently pulling anteriorly—a "click" and movement is felt that reproduces patient's pain | Rest, physiotherapy, intercostal nerve blocks; if chronic and severe, surgical removal of hypermobile cartilage segment |
| Tietze syndrome | Single tender and swollen, but nonsuppurative, costochondral junction, usually in costochondral junction of ribs two and three | Simple analgesics; usually self-limiting; rarely, corticosteroid injections |
| Traumatic muscle pain and overuse myalgia | History of trauma to chest or recent new onset of strenuous exercise to upper body (e.g., rowing); may be bilateral and affecting multiple costochondral areas; muscle groups may also be tender to palpation | Simple analgesics; refrain from doing or reduce intensity of strenuous activities that provoke pain |
References:
- Am Fam Physician. 2021 Jul ;104(1):73-78.
Patient Thrombotic Risk Definitions
| Low | CHA2DS2-VASc 1-4 (annualized stroke risk <5%), no prior TE |
| Moderate | CHA2DS2-VASc 5-6 (annualized stroke risk 5-10%) or prior TE more than 3 months previously |
| High | CHA2DS2-VASc 7+ (annualized stroke risk >10%) or prior TE within 3 months |
Reference:
- ManageAnticoag
- 2017 ACC Expert Consensus Decision Pathway for Periprocedural Management of Anticoagulation in Patients with Nonvalvular Atrial Fibrillation
Deep Venous Thrombosis
DVT Prevention in Airline Flights
- Compression stockings are effective at reducing asymptomatic DVT in airline passengers taking flights longer than five hours in both high-risk (number needed to treat [NNT] = 37; 95% CI, 35 to 46) and low-risk (NNT = 111; 95% CI, 100 to 143) populations. (SOR: C)
- It is unclear if compression stockings prevent symptomatic DVT, pulmonary embolism (PE), or death.
- There are no significant adverse events associated with their use.
Reference:
- AFP Jan 2022 Vol 105 No 1
Eating Eggs Is Not Associated with Cardiovascular Disease
Egg consumption is not associated with the occurrence of cardiovascular events over an average of 12 years.
A meta-analysis found that eating more than one egg per day, on average, was associated with a decreased likelihood of coronary artery disease (approximately 11%). This decrease may be due to a healthy user bias; that is, eating eggs may be associated with healthy habits. (Level of Evidence = 2b)
Reference:
- Am Fam Physician. 2021 Jun 1;103(11):695.
EKG
All EKG interpretations should address:
- Rate
- Rhythm
- Intervals (PR, QRS, ST, QT)
- Axis
- P waves
- Q waves
- R wave progression
- T waves
- Any pathological findings
How I read:
- Look at rhythm strip at bottom and count across
- Gives me: rate, regular vs not, clue into interval abnormalities
- Look at I and aVF
- Gives me: axis deviation
- Look at V1 and II
- gives me atrial pathology - RAE/LAE
- If regular rate, look at aVR
- Gives me sinus vs ectopic focus (with caveats)
- Scan for Q waves (not abnormal if only in III)
- Look at R wave progression in V1-V6
- Gives me: clues to LVH/RVH, BBB's, ideas extent of injury if actual MI
- Scan for T wave abnormalities (not unusual to find odd T's in III)
Other thoughts:
- Sinus vs not sinus: sinus rhythm implies from sinus node - should be negative in aVR, positive everywhere else, not changing in morphology
- Regular vs sinus arrhythmia: While no widely accepted standard values exist, I was taught there should be less than 0.04 beat-to-beat variability and that is what I use to determine regular or not regarding heart rate variability
Favorite learning resources:
- ECG Wave-Maven: http://ecg.bidmc.harvard.edu/maven/mavenmain.asp (I have used this for years)
- Learn The Heart: http://www.learntheheart.com/EKGreview.html (Fun ECG quizzes)
Heart Failure
See also:
Framingham Diagnostic Criteria (Need 2 Major or 1 Major and 2 Minor):
- Major
- Acute pulmonary edema
- Cardiomegaly
- Hepatojugular reflex
- Neck vein distension
- Paroxysmal nocturnal dyspnea or orthopnea
- Rales
- Third heart sound gallop
- Minor
- Ankle edema
- Dyspnea on exertion
- Hepatomegaly
- Nocturnal cough
- Pleural effusion
- Tachycardia >120bpm
Stages of Heart Failure
- Stage A - (At risk of HF)
- At high risk of heart failure, but without structural heart disease or symptoms of HF
- Therapy Goals:
- Treat HTN / Lipids
- Smoking cessation
- Regular Excercise
- Discourage EtOH intake and illicits
- Control metabolic syndrome
- Therapy Management:
- ACE I or ARB in appropriate patients for vascular disease or diabetes
- Statins when indicated
- Consider SGLT-2 inhibitors in patients with DM
- Stage B (At risk of HF)
- Sturctural heart disease, but without signs or symptoms of HF
- Therapy Goals:
- Prevent HF symptoms and worsening of cardiac remodeling
- Therapy Management:
- ACE I or ARB in appropriate patients
- B-Blocker in appropriate patients
- Select patients:
- ICD
- Revascularization or valvular surgery
- Stage C (HF)
- Structural heart disease with prior or current symptoms of HF
- Therapy Goals:
- Control symptoms
- Patient education
- Prevent hospitalization
- Prevent mortality
- Therapy Management:
- Diuretics for fluid retention
- ACE I or ARB
- B-Blocker
- Aldosterone antagonists
- In selected patients:
- Angiotensin receptor-neprilysin inhibitor
- Digitalis
- Isosorbide dinitrate/hydralazine
- Cardiac resynchronization therapy
- ICD
- Revascularization or valvular surgery
- Stage D (HF)
- Refractory HF requireing specialized intervention
- Therapy Goals:
- Control symptoms
- Improve quality of life
- Reduce hospital admissions
- Establish end-of-life goals
- Therapy options:
- Compassionate end-of-life care/hospice
- Deactivate ICD
- Extraordinary measures:
- Heart transplantation
- Chronic inotropes
- Temporary or permanent mechanical support
- Experimental surgery or drugs
References:
- AFP Vol 96 No 10 Nov 2017
- AFP Vol 96 No 9 Nov 2017
- AFP Sep 2023 Vol 108 No 3
HFrER
(EF <40)
- NonInvasive Disease Modifying Rx:
- ACE/ARB
- Beta-blocker
- Aldosterone antagonist
- Hydralazine/ISDN
- Ivabradine
- Valsartan/Sacubitril
- Sx modifying Rx
- Diuretics
- Digoxin
- Common Modifiable Comorbidities
- Anemia
- HTN
- T-4
- Thiamine
- Alcohol
- COPD
- CAD
- Lifestyle and Immunizations
- Na+/H2O
- Weight
- Exercise
- Flu vaccine
- PneumoVax
Reference:
- 2019 Spring FAFP
HFpEF
Medications for heart failure with preserved ejection fraction:
- ARBs
- Candesartan 4-8 mg/d
- losartan 25-50 mg/d
- Valsartan 20-40 mg/d
- ARB/neprilysin inhib
- sacubitril-valsartan 24-26 bid
- Mineral corticoid receptor antagonists
- spironolactone 12.5-25 mg/d
- Eplerenone 25mg/d
- SGLT2 Inhib
- Dapagliflozin 10 mg/d
- Empagliflozin 10 mg/d
Reference:
- AFP Vol 112 No 4 Oct 2025
H2FPEF Score
| Variable | Values | Points | |
|---|---|---|---|
| H2 | Heavy | BMI >30 | 2 |
| Hypertensive | 2+ BP meds | 1 | |
| F | Atrial Fibrillation | Paroxysmal or persistent | 3 |
| P | Pulmonary HTN | Echo PA sytolic > 35mmHg | 1 |
| E | Elder | >60yo | 1 |
| F | Filling pressure | Echo E/e' >9 | 1 |
Sum:
| Score | Est Prob |
|---|---|
| 1 | 0.2 |
| 2 | 0.35 |
| 3 | 0.55 |
| 4 | 0.7 |
| 5 | 0.93 |
| 6 | 0.9 |
| 7 | 0.95 |
Reference:
- AFP Vol 112 No 4 Oct 2025
Medications
Best Beta blockers for heart failure
- Three beta-blockers reduce mortality equally (by about 30% over one year) in patients with Class III or IV systolic heart failure.
- carvedilol
- metoprolol succinate
- bisoprolol
- Insufficient evidence exists comparing equipotent doses of these medications head-to-head to recommend any one over the others (strength of recommendation [SOR]: A, systematic review/meta-analysis).
References:
- J Fam Pract. 2015 February;64(2):122-123.
Hyperlipidemia
See also:
4 Statin Benefit Groups (2018 ACC Guidelines)
- A nonfasting plasma lipid profile can be obtained to estimate ASCVD risk and document baseline LDL-C in adults 20 years and older who are not on lipid-lowering therapy.
- Maximally tolerated statin therapy is recommended for patients 20 to 75 years of age with an LDL-C level of 190 mg per dL or greater.
- Moderate-intensity statin therapy should be initiated without calculating a 10-year ASCVD risk for patients 40 to 75 years of age with diabetes mellitus.
- Patients without diabetes at intermediate risk of ASCVD with LDL-C levels of 70 to 189 mg per dL should be treated with a moderate-intensity statin for a goal of 30% or greater reduction in LDL-C levels.
| High intensity | Moderate intensity |
|---|---|
| Atorvastatin 40-80 mg | Atorvastatin 10-20 mg |
| Rosuvastatin 20-40 mg | Fluvastatin XL 80 mg |
| Lovastatin 40 mg | |
| Pitavastatin 40-80 mg | |
| Pravastatin 40-80 mg | |
| Rosuvastatin 5-10 mg | |
| Simvastatin 20-40 mg |
Selected examples of candidates for coronary artery calcium measurement who might benefit from knowing cac score is zero:
- Patients reluctant to initiate statin who wish to understand their risk and potential for benefit more precisely
- Patients concerned about need to re-institute statin therapy after discontinuation for statin associated symptoms
- Older patients (men 55 to 80; women 60-80 years old) with low burden of risk factors who question whether they would bene t from statin therapy
- Middle-aged adults (40-55 years old) with PCE calculated 10-year risk for ASCVD 5 to <7.5% with factors that increase their ASCVD risk, even though they are in a borderline risk group
References:
- 2018 ACC Guidelines
- Am Fam Physician. 2019;99(9):589-591
Hypertriglyceridemia
Prescribe fibrates and omega-3 fatty acids for patients with triglyceride levels of 500 mg per dL (5.65 mmol per L) or higher to reduce the risk of pancreatitis.
Fasting serum triglyceride levels of 150 mg per dL or higher
Risk factors
- Obesity
- Metabolic syndrome
- Type 2 diabetes mellitus
- Excessive alcohol use
- Physical inactivity
- Excess weight
- Use of certain medications
- Genetics
Management of high triglyceride levels (150 to 499 mg per dL)
- Dietary changes
- Lower carbohydrate intake (especially refined carbohydrates)
- Increase fat (especially omega-3 fatty acids) and protein intake
- Physical activity
- Moderate- to high-intensity physical activity (>6 METS)
Pancreatitis:
- Severely elevated triglyceride levels (500 mg per dL or higher) increase the risk of pancreatitis
- For patients with acute pancreatitis associated with hypertriglyceridemia:
- Insulin infusion and plasmapheresis should be considered if triglyceride levels remain at 1,000 mg per dL or higher
Reference:
- AFP Sep 2020 Vol 102 No 6
- AFP Jun 2021 Vol 103 No 12
- https://www.aafp.org/afp/2020/0915/p347.html
Lipid Lowering Is Beneficial for Secondary Prevention but Not Primary Prevention in Patients 75 Years and Older
This meta-analysis inappropriately conflates studies of primary and secondary prevention, and the authors argue that their data support the use of lipid-lowering drugs in older adults. That may be true for secondary prevention, but it is clearly not proven for primary prevention. The STAREE trial is currently recruiting 18,000 older adults and randomizing them to receive atorvastatin (Lipitor), 40 mg, or placebo, and it will hopefully provide greater clarity about the use of lipids for primary prevention (results expected in 2023). (Level of Evidence = 1a−)
Reference:
- Am Fam Physician. 2021 Jun 1;103(11):695-696.
Repatha
ACC/AHA guideline defines very high risk (VHR) as multiple major ASCVD events OR one major ASCVD event and multiple high-risk conditions.1
According to a recent study of 27,775 patients with a history of ASCVD in the Journal of the American College of Cardiology, more than half of ASCVD patients met VHR criteria.2
Of those:
26% of very high-risk patients had multiple major ASCVD events2
- Recent ACS (within 12 months)
- History of:
- Ml (other than recent ACS above)
- Ischemic stroke
- Symptomatic PAD
74% of very high-risk patients had a major ASCVD event AND multiple high-risk conditions2
- Age ≥65 years
- Hypertension
- Diabetes mellitus
- Persistent LDL-C ≥100 mg/dL despite max-tolerated statin and ezetimibe
- HeFH
- CKD
- Smoking
- Prior CABG or prior PCI
- Congestive heart failure
Statins and Benefits edit
Notes:
- Statin therapy resulted in an average gain in life expectancy of 0.3 (95% CI 0.2–0.3) y, with a range of 0.0 to 2.0 y.
- The gain in CHD/stroke-free life expectancy with statin therapy was 0.7 (95% CI 0.5–1.0) y, with a range of 0.1 to 2.8 y.
- The absolute risk reduction in CVD incidence with statin therapy was larger than the decrease in CVD mortality:
- 6.6% (95% CI 4.5–8.5) versus 3.0% (95% CI 2.0–3.9).
- The competing other CVD and non-CVD lifetime mortality risks increased with statin therapy, by 0.9% (95% CI 0.3–1.7) and 2.1% (95% CI 1.3–3.0), respectively.
| Outcome | Mean Baseline Value (SD) | Mean Absolute Change (SD) | Minimum; Maximum Absolute Change | 95% CI Absolute Change |
|---|---|---|---|---|
| Total life expectancy (years) | 18.3 (6.5) | +0.3 (0.2) | 0.0; +2.0 | +0.2; +0.3 |
| CHD/stroke-free life expectancy (years) | 16.0 (5.8) | +0.7 (0.4) | +0.1; +2.8 | +0.5; +1.0 |
| CHD/stroke incidence (percent) | 33.2 (10.6) | −6.6 (1.7) | −11.0; −2.8 | −8.5; −4.5 |
| CHD/stroke mortality (percent) | 12.8 (5.3) | −3.0 (1.2) | −11.5; −0.9 | −3.9; −2.0 |
| Other CVD mortality (percent) | 26.0 (8.7) | +0.9 (0.7) | −0.8; +6.8 | +0.3; +1.7 |
| Non-CVD mortality (percent) | 61.3 (10.9) | +2.1 (0.9) | +0.1; +7.7 | +1.3; +3.0 |
| Risk Profile | Total Life Expectancy in Years | CHD/Stroke-Free Life Expectancy in Years | 10-Y Total CVD Mortality | ||
|---|---|---|---|---|---|
| No Statin | Δ | No Statin | Δ | ||
| 55-y-old non-smoking ♀, blood pressure 140/80 mm Hg, hypertension +, total cholesterol 6.0 mmol/l, HDL cholesterol 1.5 mmol/l, diabetes −, glucose 6.0 mmol/l, BMI 25.0, WHR 0.80, creatinine 80 µmol/l | 28.9 | +0.3 | 24.9 | +1.0 | 2% |
| 65-y-old smoking ♂, blood pressure 130/70 mm Hg, hypertension +, total cholesterol 7.0 mmol/l, HDL cholesterol 1.0 mmol/l, diabetes +, glucose 6.0 mmol/l, BMI 30.0, WHR 1.06, creatinine 90 µmol/l | 13.1 | +0.4 | 9.7 | +1.0 | 15% |
| 55-y-old non-smoking ♂, blood pressure 140/75 mm Hg, hypertension +, total cholesterol 7.0 mmol/l, HDL 1.3 mmol/l, diabetes −, glucose 6.5 mmol/l, BMI 27.0, WHR 1.00, creatinine 80 µmol/l | 23.9 | +0.4 | 18.7 | +1.2 | 3% |
| 75-y-old smoking ♂, blood pressure 120/80 mm Hg, hypertension +, total cholesterol 4.5 mmol/l, HDL 1.0 mmol/l, diabetes +, glucose 6.0 mmol/l, BMI 21.0, WHR 1.00, creatinine 90 µmol/l | 6.5 | +0.1 | 6.1 | +0.1 | 21% |
Additional Notes:
- Although the average gain in total life expectancy with statin therapy may seem small, it is larger than that calculated for some other preventive interventions targeted at the general population [29]. One should recognize that gains were much larger in particular participants, and were averaged out by participants who never experienced CVD.
- In addition, we observed that gains in CHD/stroke-free life expectancy were generally larger than those in total life expectancy.
Reference:
- Ferket BS, van Kempen BJ, Heeringa J, et al. Personalized prediction of lifetime benefits with statin therapy for asymptomatic individuals: a modeling study. PLoS Med. 2012;9(12):e1001361. https://doi.org/10.1371/journal.pmed.1001361
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3531501/
Total Chol/HDL-C Ratio
Notes:
- HR of 1.21 for 1.0 increase in ratio
- TC/HDL > 4.5 = increased cardiovascular risk
- TC/HDL > 5 = substantially higher risk of myocardial infarction and other cardiovascular events
The cholesterol/high-density lipoprotein cholesterol (TC/HDL-C) ratio is a valuable marker for assessing cardiovascular risk. This ratio provides insight into the balance between atherogenic and protective lipoproteins. A higher TC/HDL-C ratio indicates a higher risk of cardiovascular events, while a lower ratio suggests a lower risk.
Several studies have demonstrated the predictive value of the TC/HDL-C ratio. For instance, a study by Wang et al. found that the TC/HDL-C ratio was the most powerful lipoprotein predictor of future coronary heart disease (CHD) in a Chinese population, with a hazard ratio of 1.21 for a 1.0 increment in the ratio.[1] Similarly, the American Association of Clinical Endocrinologists and the American College of Endocrinology guidelines highlight the ratio's utility in predicting atherosclerotic cardiovascular disease (ASCVD) risk.[2]
The ratio is particularly useful in identifying individuals who may be at risk despite having normal levels of low-density lipoprotein cholesterol (LDL-C). For example, individuals with "low-risk" LDL-C levels but a high TC/HDL-C ratio (>5) have a significantly higher incidence of CHD compared to those with low TC/HDL-C ratios.[1]
In clinical practice, a TC/HDL-C ratio greater than 4.5 is often considered indicative of increased cardiovascular risk, and values above 5 are associated with a substantially higher risk of myocardial infarction and other cardiovascular events.[3] This ratio can be used alongside other lipid parameters to guide the intensity of lipid-lowering therapy and overall cardiovascular risk management.
Reference:
- Wang TD, Chen WJ, Chien KL, et al. Efficacy of Cholesterol Levels and Ratios in Predicting Future Coronary Heart Disease in a Chinese Population. The American Journal of Cardiology. 2001;88(7):737-43. https://doi.org/10.1016/s0002-9149(01)01843-4.
- Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Guidelines for Management of Dyslipidemia and Prevention of Cardiovascular Disease. Endocrine Practice : Official Journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2017;23(Suppl 2):1-87. https://doi.org/10.4158/EP171764.APPGL.
- Calling S, Johansson SE, Wolff M, Sundquist J, Sundquist K. The Ratio of Total Cholesterol to High Density Lipoprotein Cholesterol and Myocardial Infarction in Women's Health in the Lund Area (WHILA): A 17-Year Follow-Up Cohort Study. BMC Cardiovascular Disorders. 2019;19(1):239. https://doi.org/10.1186/s12872-019-1228-7.
- Lifestyle modifications
Lifestyle changes that can impact the cholesterol/high-density lipoprotein cholesterol (TC/HDL-C) ratio to reduce cardiovascular risk include:
- Dietary Modifications: The American College of Cardiology and the American Heart Association recommend a diet rich in vegetables, fruits, whole grains, legumes, healthy protein sources (such as low-fat dairy, poultry without skin, fish, and nuts), and non-tropical vegetable oils. Limiting the intake of sweets, sugar-sweetened beverages, and red meats is also advised. Reducing saturated fat intake to less than 7% of total calories and trans fats to less than 1% of total calories can improve lipid profiles.[1-2]
- Weight Management: Maintaining a healthy weight or achieving weight loss in overweight/obese individuals can significantly improve the TC/HDL-C ratio. Sustained weight loss is associated with increased HDL-C levels.[3-4]
- Physical Activity: Engaging in regular aerobic physical activity, such as 3-4 sessions per week lasting 40 minutes per session at moderate-to-vigorous intensity, is recommended. This can help increase HDL-C levels and improve the TC/HDL-C ratio.[1][5]
- Alcohol Consumption: Moderate alcohol consumption (up to one drink per day for women and up to two drinks per day for men) has been associated with increased HDL-C levels.[3][6]
- Smoking Cessation: Quitting smoking can lead to significant increases in HDL-C levels and improve the TC/HDL-C ratio.[3][7]
These lifestyle interventions, when combined, can lead to substantial improvements in lipid profiles and a reduction in cardiovascular risk.
Reference:
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2019;73(24):e285-e350. https://doi.org/10.1016/j.jacc.2018.11.003.
- Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Guidelines for Management of Dyslipidemia and Prevention of Cardiovascular Disease. Endocrine Practice : Official Journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2017;23(Suppl 2):1-87. https://doi.org/10.4158/EP171764.APPGL.
- Ginsberg HN. Nonpharmacologic Management of Low Levels of High-Density Lipoprotein Cholesterol. The American Journal of Cardiology. 2000;86(12A):41L-45L. https://doi.org/10.1016/s0002-9149(00)01469-7.
- Scranton R, Sesso HD, Stampfer MJ, et al. Predictors of 14-Year Changes in the Total Cholesterol to High-Density Lipoprotein Cholesterol Ratio in Men. American Heart Journal. 2004;147(6):1033-8. https://doi.org/10.1016/j.ahj.2003.11.018.
- Smith SC, Grundy SM. 2013 ACC/AHA Guideline Recommends Fixed-Dose Strategies Instead of Targeted Goals to Lower Blood Cholesterol. Journal of the American College of Cardiology. 2014;64(6):601-12. https://doi.org/10.1016/j.jacc.2014.06.1159.
- Rahilly-Tierney C, Sesso HD, Djoussé L, Gaziano JM. Lifestyle Changes and 14-Year Change in High-Density Lipoprotein Cholesterol in a Cohort of Male Physicians. American Heart Journal. 2011;161(4):712-8. https://doi.org/10.1016/j.ahj.2010.12.015.
- Kwiterovich PO. The Antiatherogenic Role of High-Density Lipoprotein Cholesterol. The American Journal of Cardiology. 1998;82(9A):13Q-21Q. https://doi.org/10.1016/s0002-9149(98)00808-x.
Hypertension
See: JNC 8
BP Goal:
- AAFP/ACP:
- Treatment recommended for Adults 60+ with SBP >150 mmHg with target <150 mmHg to reduce risk of stroke, cardiac events, and possibly mortality (strong evidence)
- Remember: 60-150-140
- Patients >60yo, consider treatment is SBP is >150mmHg or >140mmHg if they have a history of stroke or in a high cardiovascular risk
- ACC/AHA:
- Treatment recommended for noninstitutionalized, ambulatory, community-dwelling adults 65+ with avg SBP of 130+ mmHg with target < 130
- No statistically significant benefit to all-cause mortality, CVD mortality, heart failure, or renal events when the lower BP cutoff was used (130/80) and the difference for fatal or nonfatal myocardial infarction was borderline nonsignificant.
Timing of anti-hypertensives:
- Take a bedtime as significant reduction in mortality and morbidity for once-daily anti-hypertensives (LOE = 1b-)
- NNT 20.3
Targets:
- Acute intrecerebral hemorrhage
- If SBP >220 within 6 hrs of event - continuous drug infusion and close BP monitoring
- If SBP 150-220 within 6 hrs of event - immediate lowering below 140 mmHg is potentially harmful
- Acute ischemic stroke
- <185/110 before administration of IV tPA
- <185/105 for at least 24 hrs after initiating drug therapy
- Post CVA
- <130/80
- Chronic kidney disease
- <130/80
- Diabetes mellitus
- <130/80
- ACE-I or ARB
- Heart failure
- With preserved EF: <130 systolic
- With reduced EF: <130/80
- Kidney transplant
- <130/80
- Stable ischemic heart disease
- <130/80
Key Elements of Office BP Assessment:
- Patient should avoid caffeine, exercise, and smoking for at least 30min before the visit
- Patient should relax, sitting in a chari, with feet on floor and back supported for at least 5 min
- Patient should have empty bladder
- There should be no talking during the rest period and measurement
- No clothing covering the area where the cuff is placed
- Correct cuff size
- Patient arm should be supported
- Middle of the cuff should be on the patient upper arm at the level of the right atrium
- Seperate repeaated meaurements by 1 to 2 min
- Take the average of at least 2 measurements
Resources:
References:
- AFP Vol 97 No 6 Mar 2018
- AFP Vol 97 No 9 May 2018
Ambulatory Blood Pressure
From USPSTF Recommendations:
- The USPSTF found convincing evidence that ABPM is the best method for diagnosing hypertension. Although the criteria for establishing hypertension varied across studies, there was significant discordance between the office diagnosis of hypertension and 12- and 24-hour average blood pressures using ABPM, with significantly fewer patients requiring treatment based on ABPM. Elevated ambulatory systolic blood pressure was consistently and significantly associated with increased risk for fatal and nonfatal stroke and cardiovascular events, independent of office blood pressure. For these reasons, the USPSTF recommends ABPM as the reference standard for confirming the diagnosis of hypertension.
Reimbursement:
- 93784 - Ambulatory blood pressure monitoring, utilizing a system such as magnetic tape and/or computer disk, for 24 hours or longer; including recording,
scanning analysis, interpretation and report - $54.62
- 93786 - Recording only - $30.18
- 93790 - Review with interpretation and report - $19.04
- https://www.welchallyn.com/content/dam/welchallyn/documents/upload-docs/Reimbursement%20Sheets/MC12595SS_ABPM_Reimbursement_WR.pdf
- Medicare: ABPM is covered only for those patients with suspected white coat hypertension
- Aetna $170-$200
- Cigna $160-$300
- Blue Cross/Blue Sheild $60-$80
- First Health $170-$190
- United Healthcare $55-$60
Other notes:
- Only 68% of Medicare claims for ambulatory blood pressure are reimbursed.
- Claims are likely to be reimbursed if the ICD-9 diagnosis code 796.2 is included.
- Less than 30% of claims without a 796.2 diagnosis code were reimbursed.
- The median reimbursement amount for an ABPM procedure was $52.01
BP Targets
- BP targets of 140/90 mmHg offer similar reduction in CV and all-cause mortality as lower targets and have fewer adverse effects
- Lower BP targets lead to a reduction in MI with NNT of 137 over 3.7 years
- Based on mortality - primary goal is < 140/90
- Lower BP leads to fewer MI, so might be beneficial trade for some
Reference:
- AFP Vol 106 No 6 Dec 2022
Guidelines for taking home blood pressure
These are the guidelines for taking blood pressure:
- Avoid caffeinated or alcoholic beverages 30 minutes beforehand.
- Sit quietly for five minutes with your back supported and your legs uncrossed.
- Support your arm, so your elbow is at or near heart level.
- Wrap the cuff over bare skin.
- Don't talk during the measurement.
- Leave the deflated cuff in place, wait a minute, then take a second reading. If the readings are close, average them. If not, repeat and average the three readings.
JNC 8
Start all new diagnosed HTN with:
- valsartan/hctz (Walmart cheap combo)
- QUARTET Study from Lancet 2021 Sep 18; 398:1043
Choice Priority of initial agent:
- Black:
- Thiazide
- CCB
- ACE or ARB
- Nonblack:
- Thiazide
- CCB
- ACE or ARB
- CKD:
- ACE or ARB
- Thiazide
- CCB
| Indication | Treatment Choice |
|---|---|
| Heart Failure | ACEI/ARB+BB + diuretic +spironolactone |
| Post–MI/Clinical CAD | ACEI/ARB AND BB |
| CAD | ACEI, BB, diuretic, CCB |
| Diabetes | ACEI/ARB,CCB, diuretic |
| CKD | ACEI/ARB |
| Recurrent stroke prevention | ACEI,diuretic |
| Pregnancy | labetolol (first line),nifedipine, methyldopa |
Beta-1 Selective Beta-blockers –possibly safer in patients with COPD, asthma, diabetes, and peripheral vascular disease:
- metoprolol
- bisoprolol
- betaxolol
- acebutolol
| Drug Class | Agents ofChoice | Comments |
|---|---|---|
| Diuretics | HCTZ 12.5-50mg,chlorthalidone 12.5-25mg, indapamide 1.25-2.5mg, triamterene 100mg; K+ sparing –spironolactone 25-50mg, amiloride5-10mg, triamterene 100mg; furosemide 20-80mg twice daily, torsemide10-40mg | Monitor for hypokalemia; Most SE are metabolic in nature; Most effective when combined w/ ACEI; Stronger clinical evidence w/chlorthalidone; Spironolactone -gynecomastia and hyperkalemia; Loop diuretics may be needed when GFR <40mL/min |
| ACEI/ARB | ACEI: lisinopril,benazapril, fosinopril and quinapril 10-40mg, ramipril 5-10mg, trandolapril 2-8mg; ARB: candesartan 8-32mg, valsartan 80-320mg, losartan 50-100mg, olmesartan 20-40mg, telmisartan 20-80mg | SE:Cough (ACEI only), angioedema (more with ACEI), hyperkalemia; Losartan lowers uric acid levels; candesartan may prevent migraine headaches |
| Beta-Blockers | metoprolol succinate 50-100mg and tartrate 50-100mg twice daily, nebivolol 5-10mg, propranolol 40-120mg twice daily, carvedilol 6.25-25mg twice daily, bisoprolol 5-10mg, labetalol 100-300mg twice daily | Not firstline agents –reserve for post-MI/CHF; Cause fatigue and decreased heart rate; Adversely affect glucose; mask hypoglycemic awareness |
| Calcium channel blockers | Dihydropyridines: amlodipine 5-10mg, nifedipine ER 30-90mg; Non-dihydropyridines: diltiazem ER 180-360 mg,verapamil 80-120mg 3 times daily or ER 240-480mg | Cause edema; dihydropyridines may be safely combined w/ B-blocker; Non-dihydropyridines reduce heart rate and proteinuria |
| Vasodilators | hydralazine 25-100mg twice daily, minoxidil 5-10mg terazosin 1-5mg, doxazosin 1-4mg given at bedtime | Hydralazine and minoxidil may cause reflex tachycardia and fluid retention –usually require diuretic + B-blocker; Alpha-blockers may cause orthostatic hypotension |
| Centrally-acting Agents | clonidine 0.1-0.2mg twice daily, methyldopa 250-500mg twice daily guanfacine 1-3mg | Clonidine available in weekly patch formulation for resistant hypertension |
Key Points:
- In the general population, pharmacologic treatment should be initiated when blood pressure is 150/90 mm Hg or higher in adults 60 years and older, or 140/90 mm Hg or higher in adults younger than 60 years.
- In patients with hypertension and diabetes, pharmacologic treatment should be initiated when blood pressure is 140/90 mm Hg or higher, regardless of age.
- Initial antihypertensive treatment should include a thiazide diuretic, calcium channel blocker, ACE inhibitor, or ARB in the general nonblack population or a thiazide diuretic or calcium channel blockerin the general black population.
- If the target blood pressure is not reached within one month after initiating therapy, the dosage of the initial medication should be increased, or a second medication should be added.
References:
Lifestyle Modifications
Effectiveness of Lifestyle Modifications in Lowering SBP
- Physical activity
- Recommendation: Engage in regular aerobic physical activity (eg, brisk walking) >= 30 min/day, most days
- Approximate reduction (mm Hg): 4-9
- DASH eating plan
- Recommendation: Consume diet rich in fruits, vegetables, and low-fat (reduced saturated and total fat) dairy products
- Approximate reduction (mm Hg): 8-14
- Dietary sodium restriction
- Recommendation: Reduce dietary sodium intake to max of 100 mmol/day (2.4 gsodium or 6 g sodium chloride)
- Approximate reduction (mm Hg): 2-8
- Moderate alcohol consumption
- Recommendation: Limit daily consumption to max of 1 drink for women or 2 drinks for men
- Approximate reduction (mm Hg): 2-4
- Weight loss
- Recommendation: Maintain normal body weight (BMI = 18.5-24.9 kg/m2)
- Approximate reduction (mm Hg): 5-20 per 10-kg (22-lb) weight loss
- Stress reduction
- Recommendation: Practice a stress-reduction modality suchas TM
- Approximate reduction (mm Hg): 5
- Tobacco cessation
- Recommendation: Incorporate cessation modality of choice
- Approximate reduction (mm Hg): 2-4 (after 1 week of cessation)
Reference:
- Am Fam Physician. 2026;113(1):43-50
Pediatric Hypertension
Stages:
| Blood Pressure | Diagnosis |
|---|---|
| SBP and DBP <90th% | Normal |
| SBP or DBP 90-95% or >120/80 | Pre-HTN |
| SBP or DBP >99% | Stage 1 HTN |
| SBP or DBP >99% +5mmHg | Stage 2 HTN |
- Reassess BP every 6mo for Pre-HTN
- Reassess BP every 2 wks for stage 1 HTN
- When BP remains <90th%, routine surveillance every 3-6mo
- Pediatric patients with Stage 2 HTN should not participate in high-static sports until BP is well controlled.
Possible causes of secondary pediatric HTN:
- Chronic kidney disease
- Renovascular hypertension
- Pheochromocytoma
- Primary aldosteronism
- Cushing's syndrome
- Aortic coarctation
- Genetics
- Drug-induced
- Hyperthyroidism
- Congenital adrenal hyperplasia
- Obstructive sleep apnea
References:
- JFP Vol 63 No 3 Mar 2014
Primary Hypertension
- HTN Classification Scale
Class SBP DBP Normal <120 <80 Pre-HTN 120-139 80-90 Stage 1 HTN 140-159 90-99 Stage 2 HTN >160 >100 References:
- JFP Vol 65 No 1 Jan 2016
- HTN - Work up for secondary causes
It is recommended that all children and adolescents with a new diagnosis of hypertension undergo renal ultrasound and laboratory evaluation for renal pathology (strength of recommendation [SOR]: C, consensus-based guidelines).
Specific diagnostic tests are recommended for newly diagnosed patients who have suspicious clinical findings suggestive of a secondary cause of hypertension based on the initial history (excess daytime sleepiness, palpitations, tremor, sweating); physical examination (abdominal bruit, thyromegaly, malar rash); or laboratory analysis (elevated serum creatinine, low thyroid-stimulating hormone) (SOR: C, consensus-based guidelines).
Patients with undifferentiated resistant hypertension should receive further directed evaluation for secondary causes (SOR: C, consensus-based guidelines).
Children:
Secondary hypertension is more prevalent in younger children and in children and adolescents with stage 2 hypertension (blood pressure [BP] >99th percentile for age and height plus 5 mm Hg).1 Renoparenchymal and renovascular disease account for most cases of secondary hypertension in these children.
70% to 85% of children <12 years and 10% to 15% of adolescents 12 to 18 years with hypertension have an underlying cause, most commonly renoparenchymal and renovascular disease.
Such evaluation should include a renal ultrasound and laboratory testing (creatinine, urinalysis, and urine culture) to look for structural or functional anomalies.
Adults:
Secondary hypertension reportedly occurs in 5% to 10% of hypertensive patients.
Patients at highest risk for secondary hypertension have no family history of hypertension; abrupt onset, symptomatic, or crisis hypertension; stage 2 hypertension; sudden loss of hypertensive control; and drug-resistant hypertension.
The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure recommends that patients with the following characteristics undergo further directed evaluation for a secondary cause:8
- younger than 30 years with no family history of hypertension
- older than 55 years with new hypertension
- abdominal bruit with diastolic component
- sudden worsening of BP control
- recurrent flash pulmonary edema
- renal failure with abnormal urinary sediment or proteinuria
- acute renal failure after administration of an ACE inhibitor or ARB.
Patients with resistant hypertension (BP>140/90 mm Hg despite taking optimal doses of 3 antihypertensive medications, one of which is a diuretic) should receive particular scrutiny for an identifiable secondary cause.
References:
- J Fam Pract. 2014 January;63(1):41-42,54.
- Hypertensive Emergency Medications per Target Organs
- Neurologic (do not increase IOP)
- Nicardipine or clevidipine
- Labetalol
- Aortic (reduce dP/dtmax without reflex tachycardia and inotropy)
- Esmolol
- Nitroprusside (only as add-on after effective B-blockade)
- Nicardipine or clevidipine (only as add-on after effective B-blockade)
- Cardiac (do not potentiate ischemia or heart failure)
- Acute MI
- Nitroglycerin
- Esmolol
- Metoprolol
- HF
- Nitroglycerin
- Furosemide
- Nitroprusside
- Acute MI
- Renal (not renally cleared or nephrotoxic)
- Acute Kidey Injury
- Nicardipine or clevidipine
- Labetalol
- Scleroderma renal crisis
- Oral captopril
- Acute Kidey Injury
- Pregnancy (not toxic to fetus)
- Hydralazine
- Labetalol
- Oral Nifedipine
References:
- Consultant Mar 2016
- Neurologic (do not increase IOP)
- Lab workup
- EKG
- Glu
- Lipids
- GFR
- H/H
- Calcium
- K
- UA
- Lifestyle Modifications
From ACC/AHA 2013 Lifestyle Work Group
- Diet: Rich in vegetables, fruits, and whole grains, including low-fat dairy, poultry, fish, legumes, nuts, and nontropical vegetable oils - such as DASH or AHA diets
- Salt consumption: <2400mg/d … Ideal is <1500mg/d
- Regular exercise: Moderate to vigorous aerobic activity 3-4 times a week averaging 40min/session
DASH
- >4.5 cups of fruit and vegetables daily
- >2 3.5oz servings of fish per week (prefer oily fish)
- >3 1oz eq servings of fiber rich whole grains daily (1.1g of fiber per 10g carb)
- <1500mg Na daily
- <450 calories of sugar sweetened beverages per week (do not drink these!)
Components of DASH:
- Total fat: 27% of calories
- Saturated fat: 6% of calories
- Protein: 18% of calories
- Carbohydrates: 55% of calories
- Cholesterol: 150 mg
- Fiber: 30 g
- Sodium: 1,500 mg
- Potassium: 4,700 mg
- Calcium: 1,250 mg
- Magnesium: 500 mg
References:
- JFP Vol 63, No 10 Oct 2014
- AFP Vol 91 No 3 Feb 2015
- AFP Vol 93 No 11 Jun 2016
- Lifestyle Effects On BP:
Lifestyle SBP DBP DASH with Na rest 11.5 5.7 Na rest (<1200mg/day) 6.7 3.5 DASH 5.9 2.9 Wt loss (9lbs/4kg) 4.5 3.2 Potassium salt substitute 4.8 2.4 Aerobic Exercise 4.1-5.6 1.8-5.2 Restriction of EtOH 3 2 References:
- AFP Vol 91 No 3 Feb 2015
- AFP Vol 108 No 4 Oct 2023
- Medications
Table 19: First Lines Class Common AE ACE I Angioedema, cough, dizziness, hyperkalemia, hypotension ARB Dizziness, hyperkalemia, hypotension CCP (dihydropyridine) Edema, Headache Thiazide Hypokalemia, Hyponatremia - Use ARBs over ACEs
- There is no difference in efficacy between ARBs and ACE inhibitors with regard to the surrogate endpoint of blood pressure and outcomes of all-cause mortality, cardiovascular mortality, myocardial infarction, heart failure, stroke, and end-stage renal disease.
- However, ACE inhibitors remain associated with cough and a very low risk of angioedema and fatalities.
- Overall withdrawal rates because of adverse events are lower with ARBs than with ACE inhibitors.
- Given the equal outcome efficacy but fewer adverse events with ARBs, risk-to-benefit analysis in aggregate indicates that at present there is little, if any, reason to use ACE inhibitors for the treatment of hypertension or its compelling indications.
- Thiazides
- Reduce cardiovascular events (NNT=100; 95% CI 63-333) and heart failure (NNT=84; 95% CI 66-125) compared with CCB (SOR B)
Reduce stroke risk compared with ACE I (NN=167; 95% CI 100-1000) (SOR B)
Table 20: Thiazides Medication T1/2 Equiv Dose Hydrochlorothiazide 8-15h 25mg Chlorthalidone 45-60h 12.5mg Indapamide 14-25h 2.5mg - CTD and indapamide have outcome data with clear benefit in reducing cardiovascular events compared to HCTZ (which has a lack of outcome data)
- CTD and indapamide both better meet 24hr BP control given their pharmacokinetic profiles
- Cost is comparable among all 3 - Do not use HCTZ as monotherapy for HTN
- Spironolactone
- Consider use when thiazide, ACE I or ARB, and CCB fails to achieve target blood pressure (SOR C)
- For most adults with resistant HTN, spironolactone is superior to doxazosin and bisoprolol as an adjunct to triple therapy
References:
- https://www.ncbi.nlm.nih.gov/pubmed/29598869
- Consultant Jun 2016
- JFP Vol 65 No 4 Apr 2016
- AFP Vol 109 No 3 Mar 2024
- ARB vs ACE: https://www.ncbi.nlm.nih.gov/pubmed/29598869
- AFP Vol 108 No 4 Oct 2023
- Use ARBs over ACEs
Protocol for home BP
Here is the best way to take blood pressure at home:
- Avoid exercise, caffeine, and other stimulants 30min before measurement
- Avoid restrictive clothing
- Use appropriately sized cuff
- Rest quietly before and during BP measurement
- Position arm at heart level
- Do not talk while the machine is measuring
References:
- AFP Vol 76 No 2 Jul 2007
Orthostatic Blood Pressure
Diagnostic if:
- Systolic is <90mm Hg or decrease by 20mm Hg or more (10mm Hg in symptomatic patients)
- Increase of 30bpm suggests postural tachycardia syndrome
Process:
- 1 min after changing positions from supine to standing drop in systolic BP of 20 mm hg
- 3 min after changing position drop in systolic BP of 20mm hg or drop in diastolic BP of 10mm hg
- Pulse will often rise, but not diagnostic in and of itself.
Treatments:
- Physical maneuvers:
- Getting up slowly
- Leg cfrossing
- Muscle clenching
- Increased salt and water intake
- Compression stockings
- Medications:
- fludrocortisone
- midodrine
- Avoidance of medications:
- Benzodiazepines
- diuretics
Notes:
- 6% of General population
- Up to 40% of asymptomatic older adults (70+yo) and 23% younger than 60yo will have positive orthostatic BP measurements
- Associated with:
- Risk of falls (HR = 1.5)
- Coronary heart disease (HR = 1.3)
- Stroke (HR = 1.2)
- All cause mortality (HR = 1.4)
References:
- AFP Vol 95 No 5 Mar 2017
- JFP Vol 68 No 9 Nov 2019
Screening indications
- Age >40
- For those 18-39:
- Obesity/Overweight
- African American ethnicity
- High-normal BP (130-139/85-89mmHg)
References:
- JFP Vol 65, No 1 Jan 2016
Secondary Hypertention
Indications to evaluate for secondary HTN:
- Acute rise in BP in pt with previous stable BP
- Age of onset before puberty
- Age younger than 30yo in nonobese, nonblack with no FH of HTN
- Malignant or accelerated HTN
- Severe or resistant HTN
Causes of Secondary HTN
| Age | % with 2ry HTN | Most Common Etiologies |
|---|---|---|
| Birth-11yo | 70-85% | Renal parencchymal disease |
| Coarctation of the aorta | ||
| 12-18yo | 10-15% | Renal parencchymal disease |
| Coarctation of the aorta | ||
| 19-39yo | 5% | Thyroid dysfunction |
| Fibromuscular dysplasia | ||
| Renal parencchymal disease | ||
| 40-64yo | 8-12% | Hyperaldosteronism |
| Thyroid dysfunction | ||
| Obstructive Sleep Apnea | ||
| Cushing syndrome | ||
| Pheochromocytoma | ||
| 65yo+ | 17% | Atherosclerotic renal artery stenosis |
| Renal failure | ||
| Hypothyroidism |
Secondary forms of HTN associated with resistant HTN
| Condition | Prevalence in Resistant HTN |
|---|---|
| Obstructive sleep apnea | 60-70% |
| Primary aldosteronism | 7-20% |
| Renal artery stenosis | 2-24% |
| Renal parenchymal disease | 1-2% |
| Drug induced or heavy EtOH | 2-4% |
| Thyroid disorders | <1% |
Evaluation
| Birth-18yo | 19-39yo | 40-64yo | 65yo+ |
|---|---|---|---|
| Urinalysis | MRA with contrast | Renin | Renal Art Dopple |
| Urine culture | CT Angio if no MRI | Aldosterone | MRA with contrast |
| Renal Ultrasonography | TSH | Polysomnography | CT angio if no MRI |
| +/- Echo | +/- Echo | +/- 24-hr urinary free cortisol | TSH |
| +/- 24-hr urinary fract metanephrines | Urinalysis | ||
| +/- 24-hr urinary free cortisol | |||
| +/- 24-hr urinary fract metanephrines |
Drugs that can elevate BP
| Class | Examples |
|---|---|
| Anti-infective | Ketoconazole |
| Anti-inflammatory | COX-2 inhib, NSAIDs |
| Chemotherapeutic | Vascular endothelial growth factor inhib |
| Herbal | Ephedra, ginseng, ma huang |
| Illicits | Amphetamines, cocaine |
| Immunosuppressive | Cyclosporine, sirolimus, tacrolimus |
| Psychiatric | Buspirone, carbamazepine, MAOI, SSRI, SNRIs, TCAs |
| Sex hormones | Estroge and progesterone in OCPs, androgens |
| Steroid | Methylprednisolone, prednisone |
| Sympathomimetic | Decongestants, diet pills |
References:
- AFP Vol 96 No 7 Oct 2017
- JAMA Vol 311 No 21 Jun 2014
Recommended Lifestyle Modifications in Hypertension
- Alcohol moderation
- Abstain from binge drinking
- Limit to moderate daily consumption (i.e., 1.5 standard drinks per day for women and 2 for men)
- Diet
- Increase consumption of dairy, fruits, polyunsaturated fats, vegetables, and whole grains
- Increase consumption of foods high in calcium, magnesium, and potassium (e.g., avocados, legumes, nuts, seeds, tofu)
- Increase consumption of vegetables high in nitrites (e.g., leafy vegetables, beetroot)
- Reduce consumption of foods high in sugar, and saturated or trans fats
- Healthy drinks
- Consider hibiscus tea, pomegranate juice, beetroot juice, and cocoa
- Moderate consumption of coffee, and green and black tea
- Physical activity
- Add strength or resistance training 2 to 3 days per week
- Moderate intensity aerobic activity (e.g., walking, jogging, cycling, yoga, swimming) at least 5 days per week
- Salt reduction
- Avoid adding salt when cooking or dining
- Limit consumption of high salt foods, including fast foods, processed foods, and soy sauce
- Many breads and cereals are high in salt
- Smoking cessation
- Smoking cessation programs and adjuncts are recommended
- Stress reduction
- Daily mindfulness or meditation appears to improve blood pressure measurements
- Weight loss
- Evaluate obesity by waist-to-height ratio less than 0.5, or by ethnic-specific body mass index targets
- Limit obesity, particularly truncal obesity
Reference:
- AFP Jun 2021 Vol 103 No 12
Inappropriate Sinus Tachycardia
The syndrome of inappropriate sinus tachycardia is defined as a sinus heart rate >100 bpm at rest (with a mean 24-hour heart rate >90 bpm not due to primary causes) and is associated with distressing symptoms of palpitations.
Investigation of IST
- A complete history, physical exam, and 12-lead ECG are recommended.
- Complete blood counts and thyroid function studies might be useful.
- A 24-hour Holter monitoring might be useful.
- Urine/serum drug screening might be useful.
- It might be worth considering autonomic testing.
- It might be worth considering treadmill exercise testing.
Treatment for IST
- Reversible causes of sinus tachycardia should be sought and treated.
- Ivabradine can be useful for treating patients with IST.
- Sinus node modification, surgical ablation, and sympathetic denervation are not recommended as a part of routine care for patients with IST.
Reference:
- Sheldon RS, Grubb BP 2nd, Olshansky B, Shen WK, Calkins H, Brignole M, Raj SR, Krahn AD, Morillo CA, Stewart JM, Sutton R, Sandroni P, Friday KJ, Hachul DT, Cohen MI, Lau DH, Mayuga KA, Moak JP, Sandhu RK, Kanjwal K. 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015 Jun;12(6):e41-63. doi: 10.1016/j.hrthm.2015.03.029. Epub 2015 May 14. PMID: 25980576; PMCID: PMC5267948.
Lymphadenopathy
Differential Dx:
- Malignancies
- Kaposi sarcoma, leukemias, lymphomas, metastases, skin neoplasms
- Infections
- Bacterial: brucellosis, cat-scratch disease (Bartonella), chancroid, cutaneous infections (staphylococcal or streptococcal), lymphogranuloma venereum, primary and secondary syphilis, tuberculosis, tularemia, typhoid fever
- Granulomatous: berylliosis, coccidioidomycosis, cryptococcosis, histoplasmosis, silicosis
- Viral: adenovirus, cytomegalovirus, hepatitis, herpes zoster, human immunodeficiency virus, infectious mononucleosis (Epstein-Barr virus), rubella
- Other: fungal, helminthic, Lyme disease, rickettsial, scrub typhus, toxoplasmosis
- Autoimmune disorders
- Dermatomyositis, rheumatoid arthritis, Sjögren syndrome, Still disease, systemic lupus erythematosus
- Miscellaneous/unusual conditions
- Angiofollicular lymph node hyperplasia (Castleman disease), histiocytosis, Kawasaki disease, Kikuchi lymphadenitis, Kimura disease, sarcoidosis
- Iatrogenic causes
- Medications, serum sickness
| Historical clues | Suggested diagnoses | Initial testing |
|---|---|---|
| Fever, night sweats, weight loss, or node located in supraclavicular, | Leukemia, lymphoma, solid | CBC, nodal biopsy or bone marrow |
| popliteal, or iliac region, bruising, splenomegaly | tumor metastasis | biopsy; imaging with ultrasonography |
| or computed tomography may be | ||
| considered but should not delay | ||
| referral for biopsy | ||
| Fever, chills, malaise, sore throat, nausea, vomiting, diarrhea; no other red | Bacterial or viral pharyngitis, | Limited illnesses may not require any |
| flag symptoms | hepatitis, influenza, | additional testing; depending on |
| mononucleosis, tuberculosis (if | clinical assessment, consider CBC, | |
| exposed), rubella | monospot test, liver function tests, | |
| cultures, and disease-specific | ||
| serologies as needed | ||
| High-risk sexual behavior | Chancroid, HIV infection, | HIV-1/HIV-2 immunoassay, rapid |
| lymphogranuloma venereum, | plasma reagin, culture of lesions, | |
| syphilis | nucleic acid amplification for | |
| chlamydia, migration inhibitory factor | ||
| test | ||
| Animal or food contact | ||
| Cats | Cat-scratch disease (Bartonella) | Serology and polymerase chain reaction |
| Toxoplasmosis | Serology | |
| Rabbits, or sheep or cattle wool, hair, | Anthrax | Per CDC guidelines |
| or hides | ||
| Brucellosis | Serology and polymerase chain | |
| reaction | ||
| Tularemia | Blood culture and serology | |
| Undercooked meat | Anthrax | Per CDC guidelines |
| Brucellosis | Serology and polymerase chain | |
| reaction | ||
| Toxoplasmosis | Serology | |
| Recent travel, insect bites | Diagnoses based on endemic | Serology and testing as indicated by |
| region | suspected exposure | |
| Arthralgias, rash, joint stiffness, fever, chills, muscle weakness | Rheumatoid arthritis, Sjögren Antinuclear antibody, syndrome, dermatomyositis, anti-doubled-stranded DNA, systemic lupus erythematosus | erythrocyte sedimentation rate, CBC, rheumatoid factor, creatine kinase, electromyography, or muscle biopsy as indicated |
Medications causing lymphadenopathy:
- Allopurinol
- Atenolol
- Captopril
- Carbamazepine (Tegretol)
- Gold
- Hydralazine
- Penicillins
- Phenytoin (Dilantin)
- Primidone (Mysoline)
- Pyrimethamine (Daraprim)
- Quinidine
- Trimethoprim/sulfamethoxazole
- Sulindac
Risk factors for malignancy:
- Age older than 40 years
- Duration of lymphadenopathy greater than four to six weeks
- Generalized lymphadenopathy (two or more regions involved)
- Male sex
- Node not returned to baseline after eight to 12 weeks
- Supraclavicular location
- Systemic signs: fever, night sweats, weight loss, hepatosplenomegaly
- White race
Reference:
- Am Fam Physician. 2016;94(11):896-903
Lymphedema
Primary lymphedema is often classified by the age of the patient at onset of the edema.
- Congenital lymphedema occurs at birth or within the first two years of life.
- Although the edema can involve a single lower extremity, it also occurs in multiple limbs, the genitalia and, sometimes, the face.
- Bilateral edema of the lower extremities is more common in congenital lymphedema than in any other form of primary lymphedema.
- It may be transmitted in an autosomal dominant pattern, when cluster cases are found in families.
- Lymphedema praecox, the most common form of primary lymphedema, occurs around puberty or in young adults. In most cases, edema is evident in one foot and calf.
- Lymphedema tarda occurs in patients 35 years or older and is uncommon.
Secondary lymphedema, more common than the primary form, usually develops following disruption or obstruction of lymphatic pathways associated with a disease process, or following surgery or radiotherapy.
- Worldwide, filariasis is the most common cause of secondary lymphedema.
- In the United States, the most common secondary lymphedema develops in the upper extremity following axillary lymph node dissection.
Classic characteristics of early lymphedema versus other chronic edematous states of the extremities include
- subcutaneous fibrosis (peau d'orange)
- the Stemmer sign (inability to tent the skin on the dorsum of the toes or digits)
- preferential swelling of the dorsum of the foot and the characteristic blunt "squared-off" appearance of the digits of the involved extremity
| ISL stage | Description |
|---|---|
| 0 | A latent or subclinical condition where swelling is not yet evident despite impaired lymph transport, subtle alterations in tissue fluid/composition, and changes in subjective symptoms. It may exist months or years before overt edema occurs (stages I to III). |
| I | An early accumulation of fluid relatively high in protein content (eg, in comparison with "venous" edema), which subsides with limb elevation. Pitting may occur. An increase in various types of proliferating cells may also be seen. |
| II | Limb elevation alone rarely reduces the tissue swelling and pitting is manifest. Later in stage II, the limb may not pit as excess subcutaneous fat and fibrosis develop. |
| III | Lymphostatic elephantiasis where pitting can be absent and trophic skin changes such as acanthosis, alterations in skin character and thickness, further deposition of fat and fibrosis, and warty overgrowths have developed. |
Differential diagnosis includes:
- Chronic venous insufficiency (CVI) and postphlebitic syndrome
- CVI is characterized by aching in the lower extremities, chronic pruritus and cutaneous varicosities and discoloration. Patients with advanced CVI may develop skin ulceration.
- Myxedema
- Myxedema is the term given to edema that occurs when there is an abnormal deposition of mucinous substances in the extremity as a result of thyroid disease.
- Pretibial edema occurs in thyrotoxicosis, but generalized myxedema occurs in hypothyroidism. Patients with myxedema present with rough skin of the palms, soles, elbows and knees, and yellow-orange discoloration of the skin, along with other signs of hypothyroidism.
- Lipedema
- Lipedema usually occurs in women and is characterized by fatty accumulation subcutaneously between the pelvis and the ankle, sparing the feet. The patient may complain of painful swelling and may first have noted the problem shortly following onset of puberty—normally one to two years afterward.
- Stemmer's sign will be absent.
- Malignant lymphedema
- Malignant lymphedema, the leading cause of lymphedema in the United States, develops rapidly and progresses relentlessly.
- Pain, which is absent from the benign form of lymphedema, is present, and the edema tends to begin centrally.
- In the differential diagnosis of new or worsening lymphedema, recurrent cancer must be considered.
Management
- Complete decongestive physiotherapy (i.e., a noninvasive protocol consisting of skin care, lymph drainage massage, exercises, and compression bandaging) effectively improves edema, rates of infection, and quality of life in patients with lower-extremity lymphedema. (Strength of Recommendation [SOR]: B, based on prospective cohort studies.)
- Meticulous skin care
- Exercise
- Massage
- Compression garments
- Compression therapy mandates the presence of sufficient arterial flow to the affected limb; otherwise, such treatment may cause ischemia and necrosis.
- Once decongestive treatments have been successful, compression garments should continue to be used and should be replaced every three to six months (or when the garment has lost its elasticity).
- Microsurgery may be effective for patients in whom complete decongestive physiotherapy is ineffective. (SOR: C, based on a systematic review of case series.)
- There is insufficient evidence about the safety and effectiveness of oral benzopyrones to determine whether they are useful for the treatment of lymphedema. (SOR: A, based on a systematic review.)
- Isolated massage and "wringing out" are potentially harmful and are not recommended.
- Diuretics should be used only in patients with specific comorbid conditions or complications. Long-term diuretic use is discouraged because of the potential for electrolyte imbalance.
Reference:
- Am Fam Physician. 2001;64(8):1451-1452
- Am Fam Physician. 2013;88(4):online
- UpToDate
Max/Target Heart Rate
Formulas:
- Max heart rate = 220 - age
- Target heart rate = 50-85%
Metabolic Equivalents (METS)
| MET | Example |
|---|---|
| 1 | Watching TV |
| Eating,dressing, cooking, toilet | |
| 2 | Walking 1-2 blocks on level ground 1-2mph |
| 3.5 | Walking at slow pace (1mi/20min) |
| 4 | Climbing a flight of stairs |
| Walking on level ground 4mph | |
| Running a short distance | |
| 8 | Jogging (1mi/12min) |
| 10 | Playing strenuous sports (tennis, soccer, basketball) |
See also: METS in Physical Activity
References:
- AFP Vol 85 No 3 Feb 2012
- J Musc Med Mar 2012
Murmurs
Describing
- Timing:
- systolic
- midsystolic (systolic ejection murmurs, or SEM)
- AS
- PS
- ASD
- HOCM
- holosystolic (pansystolic)
- MR
- TR
- VSD
- late systolic
- MVP
- midsystolic (systolic ejection murmurs, or SEM)
- diastolic
- Early
- AR
- PR
- Austin-Flint
- Mid/Late
- MS
- TS
- Early
- Continuous throughout systole and diastole
- Patent ductus arteriosus
- Combination murmurs
- systolic
- Grading
- Systolic on a scale of 6
- Diastolic on a scale of 4
- Shape
- crescendo, decrescendo, crescendo-decrescendo or uniform
- Pitch
- high pitched if there is a large pressure gradient across the pathologic lesion and low pitched if the pressure gradient is low.
- high-pitched sounds are heard with the diaphragm of the stethoscope, whereas low-pitched sounds are heard with the bell.
- Location
- A = aortic valve post (right upper sternal border or RUSB)
- P = pulmonic valve post (left upper sternal border or LUSB)
- T = tricuspid valve post (left lower sternal border or LLSB)
- M = mitral valve post (apex)
Orthostatic Hypotension
Defined:
- A decrease in blood pressure of 20 mm Hg or more systolic or 10 mm Hg or more diastolic within 3 minutes of standing from the supine position or on assuming a head-up position of at least 60 degrees during tilt table testing.
Symptoms:
- Due to inadequate physiologic compensation and organ hypoperfusion
- headache
- lightheadedness
- shoulder and neck pain (coat hanger syndrome)
- visual disturbances
- dyspnea
- chest pain
Associated with:
- significant increase in cardiovascular risk and falls
- up to a 50% increase in relative risk of all-cause mortality
Diagnosis:
- Measure blood pressure and heart rate after 5 minutes in the supine position and 3 minutes after moving to a standing position.
- Labs:
- B12 methylmalonic acid
- BMP
- CBC
- EKG
- TSH
- Screen for supine HTN
Classification:
- Neurogenic
- Nonneurogenic
- An increase in heart rate of 0.5 beats per minute or more for every mm Hg decrease in systolic blood pressure has a high sensitivity (91%) and specificity (88%) for nonneurogenic orthostatic hypotension
| Neurogenic | Nonneurogenic | |
|---|---|---|
| Heart rate compensation ratio (Change in HR/Ch in SBP) | Decreased or absent (<0.5 bpm/mmHg) | Marked (>0.5bpm/mmHg) |
| Symptoms of systemic autonomic failure | Urinary dysfunction, GI dysfunction, postprandial hypotension; Symptoms worse in AM | None |
| Neurologic deficits | Parkinsonism, Cognitive dulling, Cerebellar signs, Peripheral sensory abnormalities | None |
Treatment goals:
- reduce symptoms
- improve quality of life
Initial treatment focuses on the underlying cause and adjusting potentially causative medications.
Nonpharmacologic strategies include:
- dietary modifications
- Appropriate volume status is maintained by adequate hydration and sodium intake
- Consumption of 2 to 2.5 L of fluids per day is recommended to counteract expected urinary losses
- Patients should aim for at least 2 to 3 g of sodium intake per day
- compression garments
- Wearing waist-high compression garments with graded pressures of 30 to 40 mm Hg, may be used to reduce venous pooling in the legs and splanchnic circulation
- physical maneuvers
- Physical counter maneuvers, including leg-crossing or squatting reduce venous pooling in the legs and splanchnic circulation
- Physical fitness should be encouraged because bed rest can further exacerbate symptoms
- avoiding environments that exacerbate symptoms
First-line medications - titrated to relieve symptoms (LOE B):
- midodrine
- droxidopa
Although fludrocortisone improves symptoms, it has concerning long-term effects.
Off-label use of atomoxetine (Strattera) and pyridostigmine (Mestinon) can be considered as adjunctive therapy
Reference:
- Am Fam Physician. 2022;105(1):39-49
OTC Blood Pressure Cuffs
- OMRON 5 Series Wireless Upper Arm Blood Pressure Monitor (BP7250)
- https://hsastore.com/omron-5-series-wireless-upper-arm-blood-pressure-monitor-bp7250/27925.html?nbt=nb%3Aadwords%3Ax%3A17481864391%3A%3A&nb_adtype=pla&nb_kwd=&nb_ti=&nb_mi=137566068&nb_pc=online&nb_pi=27925&nb_ppi=&nb_placement=&nb_li_ms=&nb_lp_ms=&nb_fii=&nb_ap=&nb_mt=&gad_source=1&gclid=EAIaIQobChMIgMiunOeShgMV26laBR3TAAYYEAQYAiABEgLkp_D_BwE
- Bluetooth capability with app
- $79.99
- HSA Eligible
- Blood Pressure Monitors, Bp Monitor - Blood Pressure Machine Large Cuff Blood Pressure Monitor Upper Arm Cuff 8.7''-17.3'', Large Screen, 2 Users Total 198 Memories
- Blood Pressure Monitor With Heart Rate - Automatic Wrist Cuff Blood Pressure Machine With LCD Display Memory and Carrying Case by Bluestone
- Etekcity - Blood Pressure Monitor - White
- https://www.bestbuy.com/site/etekcity-blood-pressure-monitor-white/6540874.p?skuId=6540874
- $36.99
- USB rechargeable
- Can store data for 2 users
Patient Messaging: Venous Insufficiency edit
I think it is a venous return issue. The best things for you to do are:
- Continue being active by walking daily
- Avoid crossing your legs (cutting of the return flow)
- Avoid prolonged sitting or standing
- Wear compression socks regularly
- Minimize salt intake in your diet
Peripheral Arterial Disease
- Use the ankle-brachial index for diagnosis in patients with history/physical exam findings suggestive of peripheral arterial disease (PAD). A
- Strongly encourage smoking cessation in patients with PAD as doing so reduces 5-year mortality and amputation rates. B
- Use structured exercise programs for patients with intermittent claudication prior to consideration of revascularization; doing so offers similar benefit and lower risks. A
- Recommend revascularization for patients who have limb ischemia or lifestyle-limiting claudication despite medical and exercise therapy. B
ABI
- A resting ABI is performed with the patient in the supine position, with measurement of systolic blood pressure in both arms and ankles using a Doppler ultrasound device
Management
- Smoking cessation
- Exercise
- Diet
- Medication
- HTN Management
- High-dose statin
- Antiplatelet agent - preferably cloidogrel
References:
- JFP Dec 2020 Vol 69 No 10
Post MI Medications
- Antiplatelet agent (like ASA 81mg/d or clopidogrel 75mg/d)
- RAAS blockers (like lisinopril 20mg/d or losartan50mg/d)
- B-blockers (like motoprolol 100mg bid)
- Statins (like atorvastatin 80mg/d)
References:
- JFP Vol 59 No 9 Sep 2010
Postural orthostatic tachycardia syndrome (POTS)
Postural orthostatic tachycardia syndrome is a distinct entity from orthostatic hypotension and is associated with symptoms of orthostatic intolerance and tachycardia without hypotension.
Postural tachycardia syndrome (POTS) is defined as a clinical syndrome that is usually characterized by
- Frequent symptoms that occur with standing such as lightheadedness, palpitations, tremulousness, generalized weakness, blurred vision, exercise intolerance, and fatigue
- An increase in heart rate of ≥30 bpm when moving from a recumbent to a standing position held for more than 30 seconds (or ≥40 bpm in individuals 12 to 19 years of age)
- The absence of orthostatic hypotension (>20 mm Hg drop in systolic blood pressure).
POTS Investigation:
- A complete history and physical exam with orthostatic vital signs and 12-lead ECG should be performed on patients being assessed for POTS.
- Complete blood count and thyroid function studies can be useful for selected patients being Assessed for POTS
- A 24-hour Holter monitor may be considered for selected patients being assessed for POTS, although its clinical efficacy is uncertain
- Detailed autonomic testing, transthoracic echocardiogram, tilt-table testing, and exercise stress testing may be considered for selected patients being assessed for POTS.
POTS Treatment:
- A regular, structured, and progressive exercise program for patients with POTS can be effective.
- It is reasonable to treat patients with POTS who have short-term clinical decompensations with an acute intravenous infusion of up to 2 L of saline.
- Patients with POTS might be best managed with a multidisciplinary approach.
- The consumption of up to 2–3 L of water and 10–12 g of NaCl daily by patients with POTS may be considered.
- It seems reasonable to treat patients with POTS with fludrocortisone or pyridostigmine.
- Treatment of patients with POTS with midodrine or low-dose propranolol may be considered.
- It seems reasonable to treat patients with POTS who have prominent hyperadrenergic features with clonidine or alpha-methyldopa.
- Drugs that block the norepinephrine reuptake transporter can worsen symptoms in patients with POTS and should not be administered.
- Regular intravenous infusions of saline in patients with POTS are not recommended in the absence of evidence, and chronic or repeated intravenous cannulation is potentially harmful
- Radiofrequency sinus node modification, surgical correction of a Chiari malformation type I, and balloon dilation or stenting of the jugular vein are not recommended for routine use in patients with POTS and are potentially harmful.
Recommendations:
- Increase the oral intake of fluids and salts.
- Avoid prolonged standing and excessive heat exposure.
Reference:
- Am Fam Physician. 2022;105(1):39-49
- Sheldon RS, Grubb BP 2nd, Olshansky B, Shen WK, Calkins H, Brignole M, Raj SR, Krahn AD, Morillo CA, Stewart JM, Sutton R, Sandroni P, Friday KJ, Hachul DT, Cohen MI, Lau DH, Mayuga KA, Moak JP, Sandhu RK, Kanjwal K. 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015 Jun;12(6):e41-63. doi: 10.1016/j.hrthm.2015.03.029. Epub 2015 May 14. PMID: 25980576; PMCID: PMC5267948.
Prognostic Significance of Between-Arm Blood Pressure Differences edit
Abstract:
Blood pressure (BP) recordings often differ between arms, but the extent to which these differences are reproducible and whether the differences have prognostic importance is unknown. We enrolled 421 consecutive patients from a medicine and a renal clinic at a veterans' hospital. Three BP recordings were obtained in each arm using an oscillometric device in a sequential manner and repeated in 1 week. Patients were followed for all-cause mortality ≤7 years. The right arm had 5.1-mm Hg higher systolic BP that attenuated by ≈2.2 mm Hg a week later. Systolic BP dropped 6.9 mm Hg over 1 week and by an additional 5.3 mm Hg in patients with chronic kidney disease. Accounting for the visit and arm effect improved the reproducibility of the BP measurements. The intraclass correlation coefficient was 0.74, which improved to 0.88 after accounting for visit and 0.93 after accounting for arm. The crude mortality rate was 6.33 per 100 patient-years. Every 10-mm Hg difference in systolic BP between the arms conferred a mortality hazard of 1.24 (95% CI: 1.01 to 1.52) after adjusting for average systolic BP and chronic kidney disease. BP differences between arms are reproducible and carry prognostic information. Patients should have evaluation of BP in both arms at the screening visit.
- In this study we found that in veterans attending a renal clinic or a general medicine clinic, there were consistent differences in BP between arms.
- At each of the visits, ≈30% of the patients had between-arm systolic BP differences that exceeded 10 mm Hg, and between 30% and 40% of the patients had between-arm diastolic BP differences that exceeded 5 mm Hg. On average, the right arm had ≈5-mm Hg higher systolic BP that attenuated by ≈2 mm Hg a week later.
- Systolic BP dropped ≈7 mm Hg from over 1 week and by an additional ≈5 mm Hg in CKD patients. Accounting for the visit and arm effect reduced the residual variance and improved the reproducibility of the measurements.
- Finally, every 10-mm Hg difference in systolic BP conferred a 24% higher mortality hazard after accounting for average systolic BP at baseline and CKD.
Reference:
- Agarwal R, Bunaye Z, Bekele DM. Prognostic significance of between-arm blood pressure differences. Hypertension. 2008 Mar;51(3):657-62. doi: 10.1161/HYPERTENSIONAHA.107.104943. Epub 2008 Jan 22. PMID: 18212263.
- https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.107.104943
Reduce Leg Swelling edit
Self-help measures to reduce leg swelling in diabetics:
- Twice a day, lie down with pillows under your legs to bring them above your heart levels.
- Make sure you get regular exercise to reduce risks of fluid build-up in legs.
- Wear compression stockings if you are prone to leg swellings.
- Eating a low-sodium diet will help symptoms of leg swellings.
- For diabetic women, wearing low-heeled or flat shoes is the best way to avoid leg swelling.
- Don't stand in one spot for too long. Take breaks to sit down. If your job requires you to stand for long hours, keep one leg bent at the knee and then repeat the same with the other leg to keep them moving.
- Get regular leg massages to improve blood circulation in the entire leg. Start with the lower legs and move downwards to the toes. This will redistribute any accumulated fluids throughout the leg.
- Wear well-fitted shoes that are never tight, even when your feet feel slightly swollen. If you must, buy shoes one size bigger. It is better to buy shoes with ties to be adjusted as per foot condition.
- Never sit cross-legged because it stops circulation of blood to the lower leg.
- If you smoke, consider quitting because a diabetic who smokes is at increased risk of leg swelling.
Study: Long-Term Effect of Salt Substitution for Cardiovascular Outcomes
Background:
- Salt substitution is a simple yet increasingly promising strategy to improve cardiovascular outcomes.
Purpose:
- To evaluate the long-term effects of salt substitution on cardiovascular outcomes.
Data Sources:
- PubMed, EMBASE, Cochrane CENTRAL, and CINAHL searched from inception to 23 August 2023. Trial registries, citation analysis, and hand-search were also done.
Study Selection:
- Randomized controlled trials (RCTs) comparing provision of or advice to use a salt substitute with no intervention or use of regular salt among adults for 6 months or longer in total study duration.
Data Extraction:
- Two authors independently screened articles, extracted data, and assessed risk of bias. Primary outcomes include mortality, major cardiovascular events (MACE), and adverse events at 6 months or greater. Secondary and post hoc outcomes include blood pressure, cause-specific mortality, and urinary excretion at 6 months or greater. Random-effects meta-analyses were done and certainty of effect estimates were assessed using GRADE (Grading of Recommendations Assessment, Development and Evaluation).
Data Synthesis:
- Of the 16 included RCTs, 8 reported on primary outcomes. Most (n = 7 of 8) were done in China or Taiwan, 3 were done in residential facilities, and 7 included populations of older age (average 62 years) and/or with higher-than-average cardiovascular risk. In this population, salt substitute may reduce risk for all-cause mortality (6 RCTs; 27 710 participants; rate ratio [RR], 0.88 [95% CI, 0.82 to 0.93]; low certainty) and cardiovascular mortality (4 RCTs; 25 050 participants; RR, 0.83 [CI, 0.73 to 0.95]; low certainty). Salt substitute may result in a slight reduction in MACE (3 RCTs; 23 215 participants; RR, 0.85 [CI, 0.71 to 1.00]; very low certainty), with very low-certainty evidence of serious adverse events (6 RCTs; 27 995 participants; risk ratio, 1.04 [CI, 0.87 to 1.25])
Limitations:
- The evidence base is dominated by a single, large RCT. Most RCTs were from China or Taiwan and involved participants with higher-than-average cardiovascular risk; therefore, generalizability to other populations is very limited.
Conclusion:
- Salt substitution may reduce all-cause or cardiovascular mortality, but the evidence for reducing cardiovascular events and for not increasing serious adverse events is uncertain, particularly for a Western population. The certainty of evidence is higher among populations at higher cardiovascular risk and/or following a Chinese diet.
Reference:
- Greenwood H, Barnes K, Clark J, Ball L, Albarqouni L. Long-Term Effect of Salt Substitution for Cardiovascular Outcomes : A Systematic Review and Meta-Analysis. Ann Intern Med. 2024 Apr 9. doi: 10.7326/M23-2626. Epub ahead of print. PMID: 38588546.
- https://www.acpjournals.org/doi/10.7326/M23-2626
Study: Rate Control With Beta-blockers Versus Calcium Channel Blockers in the Emergency Setting: Predictors of Medication Class Choice and Associated Hospitalization
BLUF:
- Use a BB for rate control over a CCB for lower rates of hospitalization
Objectives:
- Rate control is an important component of the management of patients with atrial fibrillation (AF). Previous studies of emergency department (ED) rate control have been limited by relatively small sample sizes. We examined the use of beta-blockers (BBs) versus nondihydropyridine calcium channel blockers (CCBs) in ED patients from 24 sites and the associated hospital admission rates.
Methods:
- In this preplanned substudy, we examined chart data on AF patients who visited one of 24 hospital EDs in Ontario, Canada, between April 2008 and March 2009. We describe the proportion of patients who received either a BB or a CCB, had a heart rate < 110 beats/min 2 hours later, and had any complications. We used hierarchical logistic regression modeling to determine the predictors of BB versus CCB use and to assess the between-hospital variation in use of BBs versus CCBs. Solely in patients who had no rhythm control attempts, we examined the difference in the probability of hospital admission after propensity score matching patients by medication class.
Results:
- Of the 1,639 patients who received either a BB (n = 429) or a CCB (n = 1,210), 70.9% of the patients who received a BB had successful rate control versus 66.1% for a CCB.
- Complications were rare (2.4%), and the large majority were hypotension (2.0%).
- In adjusted analyses, predictors of receiving a BB (compared to a CCB) included already being on a BB, being sent in from a doctor's office, or being seen at a teaching hospital. In contrast, patients with evidence of heart failure, prior use of a CCB, a higher presenting heart rate, or a successful pharmacologic cardioversion (vs. no attempt) or who were seen at the highest AF volume EDs were significantly less likely to receive a BB, compared to a CCB.
- Systematic between-hospital differences accounted for 8% of the variation in BB versus CCB use. Hospital characteristics accounted for the large majority of that variation: after accounting for patient characteristics the between-hospital variation decreased by a relative 2.8%. By further adjusting for hospital characteristics, it decreased by a relative 74.7%.
- Among propensity score-matched patients with no rhythm control attempts, more CCB patients were admitted (51.6%) compared to BB patients (40.0%; difference of 11.6%; 95% confidence interval = 7.9%-16.2%).
Conclusions:
- In this study of 24 EDs, CCBs were used more frequently for rate control than BBs, and complications were rare and easily managed using both agents.
- Variation between hospitals in BB versus CCB use was predominantly due to hospital characteristics such as teaching status and AF volumes, rather than different case mix.
- Among patients who did not receive attempts at rhythm control, use of a BB for rate control was associated with a lower rate of hospitalization.
Reference:
- Atzema CL, Austin PC. Rate Control With Beta-blockers Versus Calcium Channel Blockers in the Emergency Setting: Predictors of Medication Class Choice and Associated Hospitalization. Acad Emerg Med. 2017 Nov;24(11):1334-1348. doi: 10.1111/acem.13303. PMID: 28853232.
Study: Replacing salt with low-sodium salt substitutes (LSSS) for cardiovascular health in adults, children and pregnant women edit
Background:
- Elevated blood pressure, or hypertension, is the leading cause of preventable deaths globally. Diets high in sodium (predominantly sodium chloride) and low in potassium contribute to elevated blood pressure. The WHO recommends decreasing mean population sodium intake through effective and safe strategies to reduce hypertension and its associated disease burden. Incorporating low-sodium salt substitutes (LSSS) into population strategies has increasingly been recognised as a possible sodium reduction strategy, particularly in populations where a substantial proportion of overall sodium intake comes from discretionary salt. The LSSS contain lower concentrations of sodium through its displacement with potassium predominantly, or other minerals. Potassium-containing LSSS can potentially simultaneously decrease sodium intake and increase potassium intake. Benefits of LSSS include their potential blood pressure-lowering effect and relatively low cost. However, there are concerns about potential adverse effects of LSSS, such as hyperkalaemia, particularly in people at risk, for example, those with chronic kidney disease (CKD) or taking medications that impair potassium excretion.
Objectives:
- To assess the effects and safety of replacing salt with LSSS to reduce sodium intake on cardiovascular health in adults, pregnant women and children.
Search methods:
- We searched MEDLINE (PubMed), Embase (Ovid), Cochrane Central Register of Controlled Trials (CENTRAL), Web of Science Core Collection (Clarivate Analytics), Cumulative Index to Nursing and Allied Health Literature (CINAHL, EBSCOhost), ClinicalTrials.gov and WHO International Clinical Trials Registry Platform (ICTRP) up to 18 August 2021, and screened reference lists of included trials and relevant systematic reviews. No language or publication restrictions were applied.
Selection criteria:
- We included randomised controlled trials (RCTs) and prospective analytical cohort studies in participants of any age in the general population, from any setting in any country. This included participants with non-communicable diseases and those taking medications that impair potassium excretion. Studies had to compare any type and method of implementation of LSSS with the use of regular salt, or no active intervention, at an individual, household or community level, for any duration.
Data collection and analysis:
- Two review authors independently screened titles, abstracts and full-text articles to determine eligibility; and extracted data, assessed risk of bias (RoB) using the Cochrane RoB tool, and assessed the certainty of the evidence using GRADE. We stratified analyses by adults, children (≤ 18 years) and pregnant women. Primary effectiveness outcomes were change in diastolic and systolic blood pressure (DBP and SBP), hypertension and blood pressure control; cardiovascular events and cardiovascular mortality were additionally assessed as primary effectiveness outcomes in adults. Primary safety outcomes were change in blood potassium, hyperkalaemia and hypokalaemia.
Main results:
- We included 26 RCTs, 16 randomising individual participants and 10 randomising clusters (families, households or villages).
- A total of 34,961 adult participants and 92 children were randomised to either LSSS or regular salt, with the smallest trial including 10 and the largest including 20,995 participants. No studies in pregnant women were identified. Studies included only participants with hypertension (11/26), normal blood pressure (1/26), pre-hypertension (1/26), or participants with and without hypertension (11/26). This was unknown in the remaining studies. The largest study included only participants with an elevated risk of stroke at baseline. Seven studies included adult participants possibly at risk of hyperkalaemia.
- All 26 trials specifically excluded participants in whom an increased potassium intake is known to be potentially harmful.
- The majority of trials were conducted in rural or suburban settings, with more than half (14/26) conducted in low- and middle-income countries. The proportion of sodium chloride replacement in the LSSS interventions varied from approximately 3% to 77%.
- The majority of trials (23/26) investigated LSSS where potassium-containing salts were used to substitute sodium. In most trials, LSSS implementation was discretionary (22/26). Trial duration ranged from two months to nearly five years.
- We assessed the overall risk of bias as high in six trials and unclear in 12 trials.
- LSSS compared to regular salt in adults:
- LSSS compared to regular salt probably reduce DBP on average (mean difference (MD) -2.43 mmHg, 95% confidence interval (CI) -3.50 to -1.36; 20,830 participants, 19 RCTs, moderate-certainty evidence) and SBP (MD -4.76 mmHg, 95% CI -6.01 to -3.50; 21,414 participants, 20 RCTs, moderate-certainty evidence) slightly.
- On average, LSSS probably reduce
- non-fatal stroke (absolute effect (AE) 20 fewer/100,000 person-years, 95% CI -40 to 2; 21,250 participants, 3 RCTs, moderate-certainty evidence),
- non-fatal acute coronary syndrome (AE 150 fewer/100,000 person-years, 95% CI -250 to -30; 20,995 participants, 1 RCT, moderate-certainty evidence)
- cardiovascular mortality (AE 180 fewer/100,000 person-years, 95% CI -310 to 0; 23,200 participants, 3 RCTs, moderate-certainty evidence) slightly, and
- probably increase blood potassium slightly (MD 0.12 mmol/L, 95% CI 0.07 to 0.18; 784 participants, 6 RCTs, moderate-certainty evidence), compared to regular salt.
- LSSS may result in little to no difference, on average, in hypertension (AE 17 fewer/1000, 95% CI -58 to 17; 2566 participants, 1 RCT, low-certainty evidence) and hyperkalaemia (AE 4 more/100,000, 95% CI -47 to 121; 22,849 participants, 5 RCTs, moderate-certainty evidence) compared to regular salt.
- The evidence is very uncertain about the effects of LSSS on blood pressure control, various cardiovascular events, stroke mortality, hypokalaemia, and other adverse events (very-low certainty evidence).
- LSSS compared to regular salt in children: The evidence is very uncertain about the effects of LSSS on DBP and SBP in children. We found no evidence about the effects of LSSS on hypertension, blood pressure control, blood potassium, hyperkalaemia and hypokalaemia in children.
Authors' conclusions:
- When compared to regular salt, LSSS probably reduce blood pressure, non-fatal cardiovascular events and cardiovascular mortality slightly in adults.
- However, LSSS also probably increase blood potassium slightly in adults.
- These small effects may be important when LSSS interventions are implemented at the population level. Evidence is limited for adults without elevated blood pressure, and there is a lack of evidence in pregnant women and people in whom an increased potassium intake is known to be potentially harmful, limiting conclusions on the safety of LSSS in the general population. We also cannot draw firm conclusions about effects of non-discretionary LSSS implementations. The evidence is very uncertain about the effects of LSSS on blood pressure in children.
Reference:
- Brand A, Visser ME, Schoonees A, Naude CE. Replacing salt with low-sodium salt substitutes (LSSS) for cardiovascular health in adults, children and pregnant women. Cochrane Database Syst Rev. 2022 Aug 10;8(8):CD015207. doi: 10.1002/14651858.CD015207. PMID: 35944931; PMCID: PMC9363242.
- https://pubmed.ncbi.nlm.nih.gov/35944931/
Study: Use of Cardiac Troponin Testing in the Outpatient Setting edit
Objectives:
- Cardiac troponin (cTn) measurement is useful for diagnosing myocardial infarction (MI), particularly in the inpatient setting. A growing body of literature suggests that cTn may be useful for evaluating chronic conditions in the outpatient environment; however, little is known regarding cTn ordering patterns in this setting. We sought to investigate patterns of care and outcomes for patients evaluated with cTn in the outpatient setting. We hypothesized that a majority of outpatient cTn orders would be for the purpose of diagnosing possible MI.
Methods:
- We analyzed 228 patients who had outpatient orders for standard-sensitivity troponin T assays placed at our institution between January 1, 2013 and December 18, 2015. Data were divided into two cohorts based on the intended utility of cTn measurement: orders placed to evaluate for possible MI versus orders placed for some other purpose.
Results:
- Of the 228 patients, 161 were evaluated for possible MI and 67 for other reasons.
- Risk factors (hypertension P = 0.32, diabetes mellitus P = 0.41, coronary disease P = 0.38, heart failure P = 0.098, and chronic kidney disease P = 0.70) were similar between the cohorts.
- In the suspected MI cohort, an electrocardiogram was obtained in only 77% of patients, and only 13.1% were sent to the emergency department (ED) for further evaluation.
- Within the suspected MI cohort, 10.5% (n = 17) had elevated cTn and the majority of these patients (n = 10) were not sent to the ED.
Conclusions:
- The majority of outpatient cTn orders were intended to evaluate for MI, although electrocardiograms were frequently not ordered and few patients were sent for further ED evaluation.
- Providers should be encouraged to use cTn testing in a manner that minimizes the potential risk to patients with possible MI.
Reference:
- Ross SJ, Shah NH, Noutong Njapo SA, Cordiner DJ, Winchester DE. Use of Cardiac Troponin Testing in the Outpatient Setting. South Med J. 2019 May;112(5):295-300. doi: 10.14423/SMJ.0000000000000971. PMID: 31050800.
- https://pubmed.ncbi.nlm.nih.gov/31050800/
When to use in general practice?
There are some situations where it may be appropriate for a GP to order a troponin test, and the position that a troponin test should never be ordered in the community setting is an oversimplification. Generally, there are two situations where it might be reasonable for a GP to order a troponin test in the community.
- The first is when a patient has had symptoms of ACS in the preceding days but, on presentation, the symptoms have completely resolved and the patient is clinically stable and deemed to be at low risk.
- The second is when a patient presents with atypical symptoms and has a low likelihood of ACS, and the clinician uses troponin testing to essentially 'rule out' ACS to cover clinical uncertainty.
- A 12-lead ECG contributes further to this risk assessment, albeit with the limitation that up to one-third of patients with non-ST elevation ACS may have a normal ECG.15
- A positive troponin result in this setting may occasionally be detected, which will subsequently allow for appropriate management and specialist referral.7,13
If primary care Hs-Tn testing is performed in atypical, low-risk presentations with chest pain, it is important that a serial troponin test is performed three hours after the presentation if the symptoms have been present for <6 hours at the time of clinical review and the initial Hs-Tn test.11
Late increases in troponin have been described in about 1% of patients with recurrent chest pain.11
Therefore, clinical risk assessment should be ongoing, including consideration of alternative, non-ACS diagnoses.
Key Points:
- Patients presenting with possible ACS and symptoms occurring within the previous 24 hours should be promptly referred and transported to a hospital emergency department.
- Absence of an elevated troponin does not exclude unstable angina, and urgent cardiac assessment is still appropriate if the presenting symptoms are highly suggestive of ACS.
- Troponin testing should not be ordered unless there is a mechanism to review the result as soon as it is available.
- Troponin testing may have a limited role in primary care in the following scenarios:
- low-risk patients in whom symptoms have completely resolved 24 hours prior to presentation
- atypical symptoms with a low likelihood of ACS, where troponin testing may essentially 'exclude' ACS to cover clinical uncertainty
- recent symptoms of an ACS where the patient can be appropriately monitored in a general practice setting while waiting for the result.
Reference:
- Troponin testing in the primary care setting
- Australian Family Physician
- Volume 46, Issue 11, November 2017
- https://www.racgp.org.au/afp/2017/november/troponin-testing/
Troponin Increased Plasma Values
- Patients with elevated troponin levels and chronic renal disease, pulmonary hypertension, pulmonary embolism, chronic obstructive pulmonary disease, sepsis, or acute ischemic stroke have a 2- to 5-fold increased risk of death, even in the absence of known cardiovascular disease (strength of recommendation: B, meta-analysis, multiple prospective and retrospective observational studies.)
- Elevated troponin raises risk of death 5-fold in pulmonary embolism patients.
- Elevated troponin I is an independent predictor of mortality in severe sepsis.
- Elevated troponin predicts increased death risk in up to 20% of stroke patients.
References:
- J Fam Pract. 2013 October;62(10):585-586, 598.
Myocardial ischemia
- Acute coronary syndrome
- STEMI
- NSTEMI
- Other coronary ischemia
- Arrhythmia: tachy- or brady-
- Cocaine/methamphetamine use
- Coronary intervention (PCI or cardiothoracic surgery)
- Stable coronary atherosclerotic disease in setting of increased O2 demand (eg tachycardia)
- Severe hypertension
- Coronary embolus
- Aortic dissection
- Coronary artery vasculitis (SLE, Kawasaki's)
- Non-coronary ischemia
- Shock (hypotension)
- Hypoxia
- Hypoperfusion
- Pulmonary embolism
- Global ischemia
- CT Surgery
Myocardial injury with no ischemia
- Comorbidities
- Renal failure
- Sepsis
- Infiltrative diseases
- Acute respiratory failure
- Stroke
- Subarachnoid hemorrhage
- Specific identifiable precipitants
- Extreme exertion
- Cardiac contusion
- Burns >30% BSA
- Cardiotoxic meds: anthracyclines, herceptin
- Electrical shock
- Carbon monoxide exposure
- Other
- Apical ballooning (Takotsubo)
- Myocarditis
- Myopericarditis
- Rhabdomyolysis involving cardiac muscle
- Hypertrophic cardiomyopathy
- Peripartum cardiomyopathy
- Heart failure, malignancy, stress cardiomyopathy
References:
- UptoDate Graphic 54910
Prevention of Thromboembolism Guidelines for Atrial Fibrillation edit
AHA/ACC/HRS 2014 Guideline on Atrial Fibrillation: Prevention of Thromboembolism
- Antithrombotic therapy based on shared decision-making, discussion of risks of stroke and bleeding, and patient’s preferences
- Antithrombotic therapy selection based on risk of thromboembolism irrespective of paroxysmal, persistent or permanent AF
- CHA2DS2-VASc score recommended to assess stroke risk
- Warfarin recommended with mechanical heart valves. Target INR should be based on the type and location of prosthesis
- With prior stroke, TIA, or CHA2DS2 -VASc score ≥ 2, oral anticoagulants recommended. Options include:
- Warfarin
- Dabigatran, rivaroxaban, or apixaban
- With warfarin, determine INR at least weekly during initiation and monthly when stable
- Direct thrombin or factor Xa inhibitor recommended, if unable to maintain therapeutic INR
- Re-evaluate the need for anticoagulation at periodic intervals
- Bridging therapy with LMWH or UFH with a mechanical heart valve if warfarin is interrupted. Decisions regarding bridging therapy should balance the risks of stroke and bleeding
- Without a mechanical heart valve, bridging therapy decisions should balance stroke and bleeding risks against the duration of time patient will not be anticoagulated
- Evaluate renal function prior to initiation of direct thrombin or factor Xa inhibitors, and re-evaluate when clinically indicated and at least annually
- For atrial flutter, antithrombotic therapy as for AF
- With nonvalvular AF and CHA2DS2-VASc score of 0, omit antithrombotic therapy
- With CHA2DS2-VASc score ≥ 2 and end-stage CKD (CrCl <15 mL/min) or on haemodialysis, prescribe warfarin for oral anticoagulation
- With nonvalvular AF and a CHA2DS2-VASc score of 1, no antithrombotic therapy or treatment with an oral anticoagulant or aspirin - With moderate-to-severe CKD and CHA2DS2-VASc scores of ≥ 2, direct thrombin or factor Xa inhibitors at reduced doses
- For PCI, BMS may be considered to minimise duration of DAPT
- Following coronary revascularisation in patients with CHA2DS2-VASc score of ≥2, use clopidogrel concurrently with oral anticoagulants, but without aspirin
- Direct thrombin inhibitor, dabigatran, and factor Xa inhibitor rivaroxaban are not recommended with AF and end-stage CKD or on haemodialysis because of no benefit
- Direct thrombin inhibitor, dabigatran, should not be used with a mechanical heart valve
| Warfarin | Dabigatran | Rivaroxaban | Apixaban | Edoxaban | |
|---|---|---|---|---|---|
| Dose | Variable od | 150 or 110 bd 75 mg bd if CrCl 15–30 ml/min | 20 mg od 15 mg od if CrCl 15–30 ml/min | 2.5–5 mg bd 2.5 mg bd if Cr ≥1.5 mg/dl, ≥80 years of age, body weight ≤60 kg | 30–60 mg od (no data in renal impairment) |
| Target | Vitamin K-dependent factors | Thrombin (factor II) | Factor Xa | Factor Xa | Factor Xa |
| Half life | 40 h | 12–14 h | 9–13 h | 8–11 h | 8–10 h |
| Renal clearance | 0 | 80 % | 60 % | 25 % | 40 % |
| Onset of action inhibition | 3–5 h | 2 h | 2.5–4.0 h | 3 h | 1–5 h |
| Anticoagulation monitoring | INR 2–3 | Not required | Not required | Not required | Not required |
| Interactions | Multiple | P-gp | P-gp; CYP3A4 | P-gp; CYP3A4 | P-gp; CYP3A4 |
| Antidote | Vitamin K | 3- and 4-factor prothrombin complex concentrates idarucizumab | 4-factor prothrombin complex concentrates andexanet alfa, aripazine | 4-factor prothrombin complex concentrates andexanet alfa, aripazine | 4-factor prothrombin complex concentrates andexanet alfa, aripazine |
Reference:
- Katritsis DG, Gersh BJ, Camm AJ. Anticoagulation in Atrial Fibrillation - Current Concepts. Arrhythm Electrophysiol Rev. 2015 Aug;4(2):100-7. doi: 10.15420/aer.2015.04.02.100. PMID: 26835109; PMCID: PMC4711523.
Study: Assessment of ASCVD Risk in Primary Prevention edit
Primary prevention refers to individuals without a history of atherosclerotic cardiovascular disease, severe hypercholesterolemia, or diabetes. For these adults, ages 40–75 yr, who have a low-density lipoprotein-cholesterol ≥ 70 mg/dL and < 190 mg/dL, the pooled cohort equations should be used to provide a quantitative assessment of 10-yr atherosclerotic cardiovascular disease risk.
From here, individuals are grouped as low risk (< 5%), borderline risk (5-< 7.5%), intermediate risk (7.5-< 20%), or high risk (≥ 20%).
Statin therapy should be strongly advised in those with an atherosclerotic cardiovascular disease risk ≥ 20%, while statin therapy can be considered in those with a risk between 5-< 20%, especially if risk enhancing factors are present.
If uncertainty still exists regarding treatment, a coronary artery calcium score can help further refine risk.
All individuals, regardless of atherosclerotic cardiovascular disease risk, should have a cardiovascular health assessment using Life’s Essential 8, which includes:
- diet
- physical activity
- nicotine exposure
- body mass index
- blood glucose
- blood lipids
- blood pressure
- sleep
Reference:
- Rikhi R, Shapiro MD. Assessment of Atherosclerotic Cardiovascular Disease Risk in Primary Prevention. J Cardiopulm Rehabil Prev. 2022 Nov 1;42(6):397-403. doi: 10.1097/HCR.0000000000000746. PMID: 36342682; PMCID: PMC9802028.
Dental
See also:
Study: The Prophylactic Extraction of Third Molars: A Public Health Hazard
Ten million third molars (wisdom teeth) are extracted from approximately 5 million people in the United States each year at an annual cost of over $3 billion.
In addition, more than 11 million patient days of "standard discomfort or disability"—pain, swelling, bruising, and malaise—result postoperatively, and more than 11000 people suffer permanent paresthesia—numbness of the lip, tongue, and cheek—as a consequence of nerve injury during the surgery. At least two thirds of these extractions, associated costs, and injuries are unnecessary, constituting a silent epidemic of iatrogenic injury that afflicts tens of thousands of people with lifelong discomfort and disability.
Avoidance of prophylactic extraction of third molars can prevent this public health hazard.
—
Myths
Myth Number 1 — Third Molars Have a High Incidence of Pathology
- The incidence is the same as for appendicitis (10%) and cholecystitis (12%), yet prophylactic appendectomies and cholecystectomies are not the standard of care.
Table 23: Pathologies and Pericoronitis Associated With Impacted Third Molars Percentage Pathology Affected Internal resorption 0.85 Cysts 1.65 Periodontal bone loss 4.72 Resorption on distal surface of second molar 4.78 Pericoronitis 8 Total 20 - Myth Number 2 — Early Removal of Third Molars Is Less Traumatic
- Early removal of third molars is actually more traumatic and painful than leaving asymptomatic, nonpathologic teeth in situ
- dry socket, secondary infection, and paresthesia are less likely to occur in persons aged 35 to 83 years than in those aged 12 to 24 years, who experience more third-molar extractions.
- The highest risk of complication is in persons aged 25 to 34 years.
- Myth Number 3 — Pressure of Erupting Third Molars Causes Crowding of Anterior Teeth
- It is not possible for lower third molars, which develop in the spongy interior cancellous tissue of bone with no firm support, to push 14 other teeth with roots implanted vertically like the pegs of a picket fence so that the incisors in the middle twist and overlap. Yet that is the reason often given for removal of third molars, even though studies have produced contrary evidence.
- Third molars do not possess sufficient force to move other teeth. They cannot cause crowding and overlapping of the incisors, and any such association is not causation.
- Myth Number 4 — The Risk of Pathology in Impacted Third Molars Increases With Age
- There is no evidence of a significant increase in third-molar pathology with age.
- Of course, teeth that become repeatedly symptomatic or develop associated pathology should be removed
- Myth Number 5 — There is Little Risk of Harm in the Removal of Third Molars
Complications of Third-Molar Extractions
- Pain
- Swelling
- Trismus
- Hemorrhage
- Alveolar osteitis (dry socket)
- Periodontal damage
- Soft-tissue infection
- Injury to temporomandibular joint
- Malaise
- Temporary paresthesia (numbness of the lips, tongue, and cheek)
- Permanent paresthesia
- Fracture of adjacent teeth
- Fracture of the mandible
- Fracture of the maxilla
- Sinus exposure or infection
- Anesthetic complications
Reference:
- Friedman JW. The prophylactic extraction of third molars: a public health hazard. Am J Public Health. 2007 Sep;97(9):1554-9. doi: 10.2105/AJPH.2006.100271. Epub 2007 Jul 31. PMID: 17666691; PMCID: PMC1963310.
Study: Imaging modalities to inform the detection and diagnosis of early caries
Background
The detection and diagnosis of caries at the earliest opportunity is fundamental to the preservation of tooth tissue and maintenance of oral health. Radiographs have traditionally been used to supplement the conventional visual-tactile clinical examination. Accurate, timely detection and diagnosis of early signs of disease could afford patients the opportunity of less invasive treatment with less destruction of tooth tissue, reduce the need for treatment with aerosol-generating procedures, and potentially result in a reduced cost of care to the patient and to healthcare services.
Objectives
To determine the diagnostic accuracy of different dental imaging methods to inform the detection and diagnosis of non-cavitated enamel only coronal dental caries.
Search methods
Cochrane Oral Health's Information Specialist undertook a search of the following databases: MEDLINE Ovid (1946 to 31 December 2018); Embase Ovid (1980 to 31 December 2018); US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov, to 31 December 2018); and the World Health Organization International Clinical Trials Registry Platform (to 31 December 2018). We studied reference lists as well as published systematic review articles.
Selection criteria
We included diagnostic accuracy study designs that compared a dental imaging method with a reference standard (histology, excavation, enhanced visual examination), studies that evaluated the diagnostic accuracy of single index tests, and studies that directly compared two or more index tests. Studies reporting at both the patient or tooth surface level were included. In vitro and in vivo studies were eligible for inclusion. Studies that explicitly recruited participants with more advanced lesions that were obviously into dentine or frankly cavitated were excluded. We also excluded studies that artificially created carious lesions and those that used an index test during the excavation of dental caries to ascertain the optimum depth of excavation.
Data collection and analysis
Two review authors extracted data independently and in duplicate using a standardised data extraction form and quality assessment based on QUADAS-2 specific to the clinical context. Estimates of diagnostic accuracy were determined using the bivariate hierarchical method to produce summary points of sensitivity and specificity with 95% confidence regions. Comparative accuracy of different radiograph methods was conducted based on indirect and direct comparisons between methods. Potential sources of heterogeneity were pre-specified and explored visually and more formally through meta-regression.
Main results
We included 104 datasets from 77 studies reporting a total of 15,518 tooth sites or surfaces. The most frequently reported imaging methods were analogue radiographs (55 datasets from 51 studies) and digital radiographs (42 datasets from 40 studies) followed by cone beam computed tomography (CBCT) (7 datasets from 7 studies). Only 17 studies were of an in vivo study design, carried out in a clinical setting. No studies were considered to be at low risk of bias across all four domains but 16 studies were judged to have low concern for applicability across all domains. The patient selection domain had the largest number of studies judged to be at high risk of bias (43 studies); the index test, reference standard, and flow and timing domains were judged to be at high risk of bias in 30, 12, and 7 studies respectively.
Studies were synthesised using a hierarchical bivariate method for meta-analysis. There was substantial variability in the results of the individual studies, with sensitivities that ranged from 0 to 0.96 and specificities from 0 to 1.00. For all imaging methods the estimated summary sensitivity and specificity point was 0.47 (95% confidence interval (CI) 0.40 to 0.53) and 0.88 (95% CI 0.84 to 0.92), respectively. In a cohort of 1000 tooth surfaces with a prevalence of enamel caries of 63%, this would result in 337 tooth surfaces being classified as disease free when enamel caries was truly present (false negatives), and 43 tooth surfaces being classified as diseased in the absence of enamel caries (false positives). Meta-regression indicated that measures of accuracy differed according to the imaging method (Chi2(4) = 32.44, P < 0.001), with the highest sensitivity observed for CBCT, and the highest specificity observed for analogue radiographs. None of the specified potential sources of heterogeneity were able to explain the variability in results. No studies included restored teeth in their sample or reported the inclusion of sealants.
We rated the certainty of the evidence as low for sensitivity and specificity and downgraded two levels in total for risk of bias due to limitations in the design and conduct of the included studies, indirectness arising from the in vitro studies, and the observed inconsistency of the results.
Authors' conclusions
The design and conduct of studies to determine the diagnostic accuracy of methods to detect and diagnose caries in situ are particularly challenging. Low-certainty evidence suggests that imaging for the detection or diagnosis of early caries may have poor sensitivity but acceptable specificity, resulting in a relatively high number of false-negative results with the potential for early disease to progress. If left untreated, the opportunity to provide professional or self-care practices to arrest or reverse early caries lesions will be missed. The specificity of lesion detection is however relatively high, and one could argue that initiation of non-invasive management (such as the use of topical fluoride), is probably of low risk.
CBCT showed superior sensitivity to analogue or digital radiographs but has very limited applicability to the general dental practitioner. However, given the high-radiation dose, and potential for caries-like artefacts from existing restorations, its use cannot be justified in routine caries detection. Nonetheless, if early incidental carious lesions are detected in CBCT scans taken for other purposes, these should be reported. CBCT has the potential to be used as a reference standard in diagnostic studies of this type.
Despite the robust methodology applied in this comprehensive review, the results should be interpreted with some caution due to shortcomings in the design and execution of many of the included studies. Future research should evaluate the comparative accuracy of different methods, be undertaken in a clinical setting, and focus on minimising bias arising from the use of imperfect reference standards in clinical studies.
Reference:
- Walsh T, Macey R, Riley P, Glenny A-M, Schwendicke F, Worthington HV, Clarkson JE, Ricketts D, Su T-L, Sengupta A. Imaging modalities to inform the detection and diagnosis of early caries. Cochrane Database of Systematic Reviews 2021, Issue 3. Art. No.: CD014545. DOI: 10.1002/14651858.CD014545. Accessed 15 October 2024.
Study: Recall intervals for oral health in primary care patients
Background There is ongoing debate about the frequency with which patients should attend for a dental check-up and the effects on oral health of the interval between check-ups. Recommendations regarding optimal recall intervals vary between countries and dental healthcare systems, but 6-month dental check-ups have traditionally been advocated by general dental practitioners in many high-income countries.
This review updates a version first published in 2005, and updated in 2007 and 2013.
Objectives
To determine the optimal recall interval of dental check-up for oral health in a primary care setting.
Search methods Cochrane Oral Health's Information Specialist searched the following databases: Cochrane Oral Health's Trials Register (to 17 January 2020), the Cochrane Central Register of Controlled Trials (CENTRAL; in the Cochrane Library, 2019, Issue 12), MEDLINE Ovid (1946 to 17 January 2020), and Embase Ovid (1980 to 17 January 2020). We also searched the US National Institutes of Health Trials Registry (ClinicalTrials.gov) and the World Health Organization International Clinical Trials Registry Platform for ongoing trials. We placed no restrictions on the language or date of publication when searching.
Selection criteria
We included randomised controlled trials (RCTs) assessing the effects of different dental recall intervals in a primary care setting.
Data collection and analysis Two review authors screened search results against inclusion criteria, extracted data and assessed risk of bias, independently and in duplicate. We contacted study authors for clarification or further information where necessary and feasible. We expressed the estimate of effect as mean difference (MD) with 95% confidence intervals (CIs) for continuous outcomes and risk ratios (RR) with 95% CIs for dichotomous outcomes. We assessed the certainty of the evidence using GRADE.
Main results
We included two studies with data from 1736 participants. One study was conducted in a public dental service clinic in Norway and involved participants under 20 years of age who were regular attenders at dental appointments. It compared 12-month with 24-month recall intervals and measured outcomes at two years. The other study was conducted in UK general dental practices and involved adults who were regular attenders, which was defined as having attended the dentist at least once in the previous two years. It compared the effects of 6-month, 24-month and risk-based recall intervals, and measured outcomes at four years. The main outcomes we considered were dental caries, gingival bleeding and oral-health-related quality of life. Neither study measured other potential adverse effects.
24-month versus 12-month recall at 2 years' follow-up
Due to the very low certainty of evidence from one trial, it is unclear if there is an important difference in caries experience between assignment to a 24-month or a 12-month recall. For 3- to 5-year-olds with primary teeth, the mean difference (MD) in dmfs (decayed, missing, and filled tooth surfaces) increment was 0.90 (95% CI −0.16 to 1.96; 58 participants). For 16- to 20-year-olds with permanent teeth, the MD in DMFS increment was 0.86 (95% CI −0.03 to 1.75; 127 participants). The trial did not assess other clinical outcomes of relevance to this review.
Risk-based recall versus 6-month recall at 4 years' follow-up
We found high-certainty evidence from one trial of adults that there is little to no difference between risk-based and 6-month recall intervals for the outcomes:
- number of tooth surfaces with any caries (ICDAS 1 to 6; MD 0.15, 95% CI −0.77 to 1.08; 1478 participants);
- proportion of sites with gingival bleeding (MD 0.78%, 95% CI −1.17% to 2.73%; 1472 participants);
- oral-health-related quality of life (MD in OHIP-14 scores −0.35, 95% CI −1.02 to 0.32; 1551 participants).
There is probably little to no difference in the prevalence of moderate to extensive caries (ICDAS 3 to 6) between the groups (RR 1.04, 95% CI 0.99 to 1.09; 1478 participants; moderate-certainty evidence).
24-month recall versus 6-month recall at 4 years' follow-up
We found moderate-certainty evidence from one trial of adults that there is probably little to no difference between 24-month and 6-month recall intervals for the outcomes:
- number of tooth surfaces with any caries (MD −0.60, 95% CI −2.54 to 1.34; 271 participants);
- percentage of sites with gingival bleeding (MD −0.91%, 95% CI −5.02% to 3.20%; 271 participants).
There may be little to no difference between the groups in the prevalence of moderate to extensive caries (RR 1.05, 95% CI 0.92 to 1.20; 271 participants; low-certainty evidence). We found high-certainty evidence that there is little to no difference in oral-health-related quality of life between the groups (MD in OHIP-14 scores −0.24, 95% CI −1.55 to 1.07; 305 participants).
Risk-based recall versus 24-month recall at 4 years' follow-up
We found moderate-certainty evidence from one trial of adults that there is probably little to no difference between risk-based and 24-month recall intervals for the outcomes:
- prevalence of moderate to extensive caries (RR 1.06, 95% CI 0.95 to 1.19; 279 participants);
- number of tooth surfaces with any caries (MD 1.40, 95% CI −0.69 to 3.49; 279 participants).
We found high-certainty evidence that there is no important difference between the groups in the
- percentage of sites with gingival bleeding (MD −0.07%, 95% CI −4.10% to 3.96%; 279 participants);
- or in oral-health-related quality of life (MD in OHIP-14 scores −0.37, 95% CI −1.69 to 0.95; 298 participants).
Authors' conclusions
- For adults attending dental check-ups in primary care settings, there is little to no difference between risk-based and 6-month recall intervals in the number of tooth surfaces with any caries, gingival bleeding and oral-health-related quality of life over a 4-year period (high-certainty evidence).
- There is probably little to no difference between the recall strategies in the prevalence of moderate to extensive caries (moderate-certainty evidence).
- When comparing 24-month with either 6-month or risk-based recall intervals for adults, there is moderate- to high-certainty evidence that there is little to no difference in the number of tooth surfaces with any caries, gingival bleeding and oral-health-related quality of life over a 4-year period.
The available evidence on recall intervals between dental check-ups for children and adolescents is uncertain.
The two trials we included in the review did not assess adverse effects of different recall strategies.
Reference:
- Fee PA, Riley P, Worthington HV, Clarkson JE, Boyers D, Beirne PV. Recall intervals for oral health in primary care patients. Cochrane Database Syst Rev. 2020 Oct 14;10(10):CD004346. doi: 10.1002/14651858.CD004346.pub5. PMID: 33053198; PMCID: PMC8256238.
Fluoride Supplementation in Community Water Question
My response to a patient question:
- Is there any chance you'd weigh in on the fluoride debate? Do you believe it could be harming some people?
Fluoride is a naturally occurring mineral that is added to drinking water to help prevent dental caries (cavities). The practice of community water fluoridation (CWF) has been widely implemented and studied for its effectiveness in reducing dental caries for many years.
Fluoride Supplementation has some well studied and known benefits including:
- Reduction in Dental Caries: Studies have shown that CWF can significantly reduce the prevalence of dental caries in children and adults.
- Economic Benefits: The benefit-cost ratio increases with community population size, making it a financially sound public health measure.
Risks of Fluoride Supplementation:
- Dental Fluorosis: Excessive fluoride exposure during tooth development can lead to dental fluorosis, which causes changes in the appearance of tooth enamel. Mild forms of fluorosis are generally of no aesthetic concern, but moderate to severe forms can be noticeable and may affect appearance.
- Potential Neurodevelopmental Effects: Recent studies have raised concerns about the potential neurodevelopmental effects of fluoride exposure, particularly during pregnancy. Some epidemiological studies have suggested an association between high fluoride exposure and reduced intelligence in children, although the evidence is still debated and requires further investigation.
The recent studies on potential neurodevelopmental effects are what is pushing the new political discussion on whether to continue CWF or not.
Fluoride is found and/or supplemented elsewhere besides community water sources including:
- Toothpaste: Probably the best way to use fluoride to prevent cavities
- Black Tea: Black tea is one of the highest sources of fluoride
- The fluoride content in tea can vary depending on the type of tea and the water used for brewing.
- Grape Juice: This is partly due to the use of fluoride-based pesticides on grapes.
- Wine: White wine can contain up to 2.02 ppm of fluoride, while red wine and other types of wine can also be significant sources.
- Sodas and Carbonated Beverages: Carbonated drinks can contain fluoride, but varies depending on the water source they use.
- Bottled Water: Some bottled waters can be high in fluoride, especially if they are sourced from areas with naturally high fluoride levels or if they are fortified with fluoride.
- Alcoholic Drinks: Alcoholic beverages, particularly beers and wines, can be significant sources of fluoride.
Stopping community water supplementation has been done in different municipalities already, and we can compare their results to know what might happen nationally:
- A systematic review by McLaren and Singhal (2016) examined the impact of community water fluoridation cessation on dental caries. The review included 15 instances of CWF cessation in 13 countries and found mixed results. However, the majority of studies with moderate methodological quality indicated an increase in dental caries following cessation.
- A study by McLaren et al. (2022) compared dental caries in children from Calgary, which ceased fluoridation in 2011, and Edmonton, which continued fluoridation. The study found a significantly higher prevalence of caries in primary dentition in Calgary compared to Edmonton, suggesting an adverse impact of fluoridation cessation on children's dental health.
- Another study by McLaren et al. (2017) also explored the short-term impact of fluoridation cessation in Calgary and Edmonton. The results indicated an increase in primary tooth decay in Calgary post-cessation, while Edmonton showed smaller and less consistent changes.
So, to me the issue comes down to how solid is the evidence on potential neurodevelopmental effects (mixed levels):
- A systematic review and meta-analysis by Choi et al. (2012) found that children in high-fluoride areas had significantly lower IQ scores compared to those in low-fluoride areas, with a standardized mean difference of -0.45.
- Similarly, a more recent systematic review and dose-response meta-analysis by Veneri et al. (2023) reported a summary mean difference of -4.68 IQ points when comparing the highest versus the lowest fluoride exposure categories, with a stronger association for drinking water fluoride.
- Bashash et al. (2017) found that higher prenatal fluoride exposure was associated with lower cognitive scores in children aged 4 to 12 years.
- Green et al. (2019) reported that maternal fluoride exposure during pregnancy was associated with lower IQ scores in offspring, particularly in boys.
- The systematic review by Miranda et al. (2021) classified the association between high fluoride exposure and IQ impairment as very low-level evidence due to high heterogeneity and potential residual confounding.
Additionally, cavities are not without long term effects.
- Quality of life: Untreated caries can lead to pain, difficulty eating, trouble sleeping, and missed school days, all of which negatively impact daily life and overall well-being
- Childhood caries have been associated with poorer physical health and a faster pace of aging by midlife.
- High caries experience in early childhood is linked to metabolic abnormalities such as higher BMI, high waist circumference, and elevated serum leptin levels by age 45.
- Dental caries have been independently associated with an increased risk of ischemic stroke and all-cause mortality.
- The economic burden of dental caries can be substantial as well.
So the choice is possibly:
- Better dental health but not as smart
- Poor dental and medical health but smarter
My bias: I have published a literature review in the past evaluating the evidence of fluoride supplementation in preventing dental caries, and still believe strongly that it prevents them.
My opinion: Like most things, moderation is key, and I think there is a balance to be found. I think, for most people, if they use fluoride toothpaste and eat nutritious meals, their dental health should be fine. The fluoride in community water is to cover those who don't have the best dental hygiene from a population standpoint. The problem is, many people do not have the best dental hygiene. Additionally, the concern regarding the effects on the brain by fluoride during development is reasonable and should be considered well.
Dental Antibiotic Prophylaxis
Elective dental procedures are often advised to be avoided for the first 6 to 12 months after surgery, with specific timing depending on the institution's guidelines.
The American Dental Association (ADA) and the American Academy of Orthopaedic Surgeons (AAOS) now generally do not recommend routine antibiotic prophylaxis for most patients with prosthetic joint implants undergoing dental procedures, as there is no strong evidence that it prevents prosthetic joint infection (PJI).
In general, for patients with prosthetic joint implants, prophylactic antibiotics are not recommended prior to dental procedures to prevent prosthetic joint infection.
ALL patients who have undergone total joint replacement surgery should receive antibiotic prophylaxis prior to any dental procedures and additional procedures as outlined below for 1 years after your surgery. After 1 year, you should have prophylaxis* if you have an abnormally weak immune system or are having a root canal or dental extraction (these have a greater risk of infection than a routine cleaning). Antibiotic prophylaxis may still be considered for specific high-risk groups, such as those with a history of prior PJI, complex joint reconstruction, immunosuppression (e.g., due to uncontrolled diabetes, cancer, chemotherapy, organ transplant, or HIV), or hematologic malignancies.
Antibiotic options for antibiotic prophylaxis prior to invasive dental procedure to be administered 1 h prior to the start of the procedure:
- Patients not allergic to penicillin:
- Cephalexin or amoxicillin 2 grams orally one hour prior to procedure.
- Patients allergic to penicillin:
- Clindamycin 600 milligrams orally one hour prior to procedure.
- Patients not allergic to penicillin and unable to take oral medications:
- Cefazolin 1 gram or ampicillin 2 grams IM/IV one hour prior to the procedure.
- Patients allergic to penicillin and unable to take oral medications:
- Clindamycin 600 milligrams IM/IV one hour prior to the procedure.
Reference:
- Antibiotics to Prevent Prosthetic Joint Infection | American Dental Association
- Zhou MX, Berbari EF, Couch CG, Gruwell SF, Carr AB. Viewpoint: Periprosthetic joint infection and dental antibiotic prophylaxis guidelines. J Bone Jt Infect. 2021 Oct 1;6(8):363-366. doi: 10.5194/jbji-6-363-2021. PMID: 34646729; PMCID: PMC8498598.
Study: Common Oral Conditions A Review
Importance
- Dry mouth, oral candidiasis, and recurrent aphthous ulcers are 3 of the most common oral conditions that may be associated with patient discomfort, decreased quality of life, and morbidity.
Observations
- In a meta-analysis of 26 population-based cohort and cross-sectional studies, the global prevalence of dry mouth symptoms was 23% (95% CI, 18% to 28%), placing individuals at risk of oral candidiasis, dental caries, dysgeusia, masticatory/speech impairment, and oropharyngeal dysphagia.
- Dry mouth is associated with using more than 3 oral medications per day (odds ratio [OR], 2.9 [95% CI, 1.4 to 6.2]), head and neck radiation, and Sjögren disease.
- Symptoms may include difficulty swallowing and speaking, thirst, and halitosis.
- Dry mouth is associated with an 11.5% (95% CI, 3.6% to 27%) higher risk of oral candidiasis, based on a meta-analysis of 6 observational cohorts.
- Management of dry mouth includes mechanical salivary stimulants, oral moisturizers, and/or systemic sialagogues.
- Oral candidiasis is an opportunistic fungal infection caused by overgrowth of the Candida genus with C albicans, which accounts for 76.8% of infections.
- The prevalence of oral candidiasis is higher in patients who are immunosuppressed, for example, those with HIV (35% [95% CI, 28% to 42%]) and those with salivary gland hypofunction (OR, 3.02 [95% CI, 1.73 to 5.28]).
- Common risk factors associated with oral candidiasis include use of antibiotics (P = .04) and oral mucosal disorders such as lichen planus.
- Oral burning and dysgeusia are common symptoms of oral candidiasis.
- Treatment includes addressing risk factors and use of topical and/or systemic antifungal medications.
- Recurrent aphthous stomatitis is characterized by symptomatic round or oval oral ulcers, which are covered by a gray-white fibrin layer and encircled by an erythematous ring.
- A meta-analysis of 10 case-controlled studies revealed an increased risk of recurrent aphthous stomatitis associated with polymorphism of IL-1β (+3954C/T) (OR, 1.52 [95% CI, 1.07 to 2.17]) and IL-1β (−511C/T) (OR, 1.35 [95% CI, 1.09 to 1.67]).
- Another meta-analysis of 9 case-control studies reported that patients with recurrent aphthous stomatitis had a higher frequency of nutritional deficiencies, including vitamin B12 (OR, 3.75 [95% CI, 2.38 to 5.94]), folic acid (OR, 7.55 [95% CI, 3.91 to 14.60]), and ferritin (OR, 2.62 [95% CI, 1.69 to 4.06]).
- Recurrent aphthous stomatitis can be associated with systemic diseases.
- A meta-analysis of 21 case-control studies revealed that celiac disease is associated with a higher incidence of recurrent aphthous stomatitis (25% vs 11%; OR, 3.79 [95% CI, 2.67 to 5.39]; P <.001).
- Topical corticosteroids are first-line agents to manage recurrent aphthous stomatitis; however, systemic medications may be necessary in more severe cases.
Conclusions and Relevance
- Dry mouth, oral candidiasis, and recurrent aphthous ulcers are common oral conditions that may be associated with patient discomfort, decreased quality of life, and morbidity.
- First-line treatment includes over-the-counter sialagogues for dry mouth, topical antifungals for oral candidiasis, and topical corticosteroids for aphthous ulcers.
- Oral conditions that do not improve with first-line treatment may require treatment with systemic medications.
Reference:
- Stoopler ET, Villa A, Bindakhil M, Díaz DLO, Sollecito TP. Common Oral Conditions: A Review. JAMA. 2024;331(12):1045–1054. https://doi.org/10.1001/jama.2024.0953
Dermatology
9 tips to help prevent derm biopsy mistakes
PRACTICE RECOMMENDATIONS
- Use an excisional biopsy for a melanocytic neoplasm. (SOR C)
- Choose a punch biopsy over a shave biopsy for rashes. (SOR B)
- Properly photograph and document the location of all lesions before biopsy. (SOR A)
- Provide the pathologist with a sufficient history, including the distribution and appearance of the lesion, and how long the patient has had it. (SOR A)
The 9 tips:
- Choose your biopsy type wisely.
- The most common biopsy types are shave, punch, and excisional
- Shave biopsy: lesions that are solitary, elevated, and give the impression that a sufficient amount of tissue can be sampled using this technique
- Punch biopsy: most "rashes" (inflammatory skin disorders)
- Excisional biopsy: melanocytic neoplasms or larger lesions.
- Videos of biopsies: http://www.jfponline.com/multimedia/video.html
- When performing a shave biopsy, avoid obtaining a sample that's too superficial.
- The advantage of the shave biopsy is that it is minimally invasive and quick to perform
- Choose punch over shave biopsy for rashes.
- Punch biopsy is the preferred technique for almost all inflammatory skin conditions (rashes)
- A punch biopsy size of 4 mm is commonly used for rashes
- Choose an excisional biopsy for a melanocytic neoplasm, when possible.
- The purpose of an excisional biopsy (which typically includes a 1 to 3 mm rim of normal skin around the lesion) is to completely remove a lesion.
- The excisional biopsy generally is the preferred technique for clinically atypical melanocytic neoplasms (lesions that are not definitively benign)
- Be careful with curettage.
- Curettage is a biopsy technique in which a curette—a surgical tool with a scoop, ring, or loop at the tip—is used in a scraping motion to retrieve tissue from the patient.
- Remember the importance of proper fixation and processing.
- Promptly place sampled tissue in an adequate amount of formalin so that the tissue is submersed in it in the container
- Failure to do so can result in improper fixation and will make it difficult to render an appropriate diagnosis.
- Properly photograph and document the biopsy location.
- To properly record the site of a biopsy for future dermatologic exams, take pictures of the lesion at the time of biopsy. The photographs should clearly document the lesion in question, and should be taken far enough from the site that surrounding lesions and/ or other anatomic landmarks are also visible.
- Give the pathologist a pertinent history.
- Providing the pathologist with a sufficient history, including the distribution and appearance of the lesion, and how long the patient has had it
- Know when to refer.
Refernces:
- J Fam Pract. 2014 October;63(10):559-564.
Acne
Start treatment with:
- adapalene plus benzoyl peroxide
- clindamycin plus benzoyl peroxide
- or adapalene alone
Disease of sebaceous follicles - multifactorial (abn keratonization, excessive sebum, Propionibacterium acnes, and hormones)
- Open Comedones: flat or slightly raised with dark substance in cental orifice
- Closed Comedones: pale white papules with no visible orifice
Severity-based approach to treating acne vulgaris:
- Comedones:
- Topical retinoids
- Maintenance: Topical retinoids
- If not effective: add Benzoyl Peroxide
- Mild inflammatory papules and pustules
- Topical retinoid + Benzoyl Peroxide
- Maintenance: Topical retinoids
- If not effective: oral or topical antibiotic (depending on nodules)
- Moderate inflammatory papules and pustules with or without nodules
- If Nodules
- Topical retinoid + Benzoyl Peroxide + Oral antibiotic
- Maintenance: Topical retinoid + Benzoyl Peroxide
- If Papules and Pustules
- Topical retinoid + Benzoyl Peroxide + Topical antibiotic
- Maintenance: Topical retinoid + Benzoyl Peroxide
- If not effective: Change topical to oral antibiotic
- Severe inflammatory papules and pustules with or without nodules
- If Nodules
- Oral Isotretinoin
- Maintenance:
- Topical retinoid + Benzoyl Peroxide + Topical antibiotic
- Topical retinoid + Benzoyl Peroxide + Oral antibiotic
- If Papules and Pustules
- Topical retinoid + Benzoyl Peroxide + Oral antibiotic
- Maintenance:
- Topical retinoid + Benzoyl Peroxide + Topical antibiotic
- Topical retinoid + Benzoyl Peroxide + Oral antibiotic
- If not effective: Oral Isotretinoin
- If Nodules
- If Nodules
Evidence Treatment
- Topical retinoids should be used as monotherapy for mild comedonal acne and in combination with other topical or oral agents for moderate to severe inflammatory acne. (LOE B)
- Topical retinoids should be used for maintenance therapy once treatment goals are achieved and oral agents are discontinued. (LOE C)
- Systemic antibiotics should be used for treatment of moderate to severe inflammatory acne. (LOE B)
- Oral isotretinoin should be used for treatment of severe nodular acne or refractory acne in adults and adolescents. (LOE B)
- Combined oral contraceptives should be considered for menarchal females unresponsive or intolerant to past therapies, for temporal association of acne outbreaks with menses, or for females with signs and symptoms of hyperandrogenism (acne, hirsutism, oligomenorrhea). (LOE A)
Major recommendations from guidelines:
- Topical retinoids are recommended as monotherapy for comedonal acne or in combination with topical or oral antimicrobials in patients with mixed or primarily inflammatory acne (LOE 1)
- Benzoyl peroxide is an effective topical agent (LOE 1)
- Topical antibiotic therapy is recommended only in combination with benzoyl peroxide (LOE 1)
- Systemic antibiotic therapy is recommneded for management of moderate and severe inflammatory acne and acne resistant to topical treatments (LOE 1)
- Preferred oral antibiotic are tetracyclines with doxycycline and minocycline more effective than tetracycline
- Systemic antibiotic use should be limited to the shortest possible duration, typically 3 months. Concomitant and ongoing topical therapy with benzoyl peroxide or topical retinoid is recommended for maintenance. (LOE 1)
- Combined oral contraceptives are effective in treating inflammatory acne in girls and women (LOE 1)
- Consider spirinolactone 25 mg to 100 mg for women - safe, inexpensive, and effective
- Oral isotretinoin is recommended for treatment of severe nodular acne, moderate recalcitrant acne, or acne that produces scarring or psychosocial distress (LOE 1)
| Mild | Benzoyl peroxide (BP) | Topical retinoid | Topical combination therapy*:BP + antibiotic; or Retinoid + BP; or Retinoid + BP + antibiotic |
| Moderate | Topical combination therapy*: BP + antibiotic; or Retinoid + BP; or Retinoid + BP + antibiotic Oral antibiotic + topical retinoid + BP | Oral antibiotic + topical retinoid + BP + topical antibiotic | |
| Severe | Oral Antibiotic + topical combination therapy: BP + antibiotic; or Retinoid + BP; or Retinoid + BP + antibiotic | Oral isotretinoin |
- May be prescribed as a fixed combination product or as separate component.
| Mild | Add topical retinoid or BP (if not on already) | Consider alternate retinoid | Consider topical dapsone | |
| Moderate | Consider alternate combination therapy | Consider change in oral antibiotic | Add combined oral contraceptive or oral spironolactone (females) | Consider oral isotretinoin |
| Severe | Consider change in oral antibiotic | Add combined oral contraceptive or oral spironolactone (females) | Consider oral isotretinoin |
Notes:
- Tretinoin is associated with photosensitivity, so nighttime application is recommended.
- Can apply benzoyl peroxide in the morning if used in combination.
Medications:
- Topical Retinoid - anti-inflammatory effects
- Adapelene: 45g 0.1% gel ($70), 45g 0.3% gel($100), 45g cream ($100)
- Tretinoin: 0.025% 45 g gel ($60), 0.01% 45 g gel ($100)
- Simultaneous application of benzoyl peroxide and tretinoin should be avoided
- Adapelene/benzoyl peroxide: 0.1%/2.5% 45g gel ($80)
- Benzoyl Peroxide - comedolytic, anti-inflammatory, and bactericidal against C. acnes
- Topical Antibiotics - anti-inflammatory and, depending on the formulation, bacteriostatic or bactericidal properties
- Clindamycin 1% / Benzoyl Peroxide 5%: 25 g gel ($70)
- Erythromycin 2%: 60 ml solution ($25), 40 pads ($40), 60 g gel ($70)
- Clindamycin 1%: 60 ml solution ($30), 60 ml lotion ($50), or 60 g gel ($70)
- Oral Antibiotics -
- doxycycline 50-100 mg qd-bid
- minocycline 50 mg qd
- Oral Contraceptives for acne:
- ethinyl estradiol/norgestimate
- Mononessa, Ortho Cyclen-28, Ortho Tri-Cyclen, Ortho Tri-Cyclen Lo, Estarylla, Tri-Estarylla, Tri-Lo-Estarylla, Mili, Mono-Linyah, Tri-Linyah, Previfem, Sprintec 28, TriCyclen, Tri-Lo Sprintec, Tri-Mili, Tri-Lo-Mili, Trinessa, TriNessa Lo, TriPrevifem, TriSprintec, Femynor, TriFemynor, Tri-Lo-Marzia
- ethinyl estradiol/norethindrone acetate/ferrous fumarate
- Loestrin 24 Fe, Loestrin Fe 1.5/30, Loestrin Fe 1/20, Lo Loestrin Fe, Lomedia 24 Fe, Lo Minastrin Fe, Estrostep Fe, Gildess Fe 1.5/30, Gildess Fe 1/20, Junel Fe 1.5/30, Junel Fe 1/20, Junel Fe 24, Microgestin Fe 1.5/30, Microgestin Fe 1/20, Minastrin 24 FE, Tilia Fe, TriLegest Fe, Blisovi 24 Fe, Blisovi Fe 1.5/30, Blisovi Fe 1/20, Taytulla, Larin 24 FE, Larin FE 1/20, Larin FE 1.5/30, Melodetta 24 FE, Mibelas 24 FE, Tarina 24 FE, Tarina FE 1/20, Merzee
- ethinyl estradiol/drospirenone
- Yasmin, Yaz, Gianvi, Loryna, Ocella, Syeda, Vestura, Zarah, Yaela
- ethinyl estradiol/drospirenone/levomefolate
- Beyaz, Safyral, Tydemy
- ethinyl estradiol/norgestimate
- Other
- Spironolactone in women with resistant and hormonally mediated acne
- Use in conjunction with OCP (risk of fetal antiandrogenic effects)
- There is evidence that these are associated with a reduction in skin lesions:
- purified bee venom
- tea tree oil
- a low-glycemic-load diet
- avoidance of skim milk
- Spironolactone in women with resistant and hormonally mediated acne
Strong recommendations are made for benzoyl peroxide, topical retinoids, and topical antibiotics, as well as for oral doxycycline. Oral isotretinoin is strongly recommended for acne that is severe, causing psychosocial burden or scarring, or failing standard oral or topical therapy. Conditional recommendations are made for topical clascoterone, salicylic acid, azelaic acid, as well as for oral minocycline, sarecycline, COC pills, and spironolactone. Combining topical therapies with multiple mechanisms of action, limiting systemic antibiotic use, combining systemic antibiotics with topical therapies, and adding intralesional corticosteroid injections for larger acne lesions are recommended as good practice statements
Reference:
- AFP Vol 109 No 6 Jun 2024
- AFP Vol 86 No 8 Oct 2012
- AFP Vol 95 No 11 Jun 2017
- Am Fam Physician. 2019;100(8):475-484
- Cheung M, Taher M, Lauzon G., Acneiform facial eruptions, Canadian Fam Phys, Vol 51; April 2005; 527-533
- FPN Apr 2023
- https://www.aad.org/member/clinical-quality/guidelines/acne
- JAMA Vol 316 No 13 Oct 2016
- Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, Bowe WP, Graber EM, Harper JC, Kang S, Keri JE, Leyden JJ, Reynolds RV, Silverberg NB, Stein Gold LF, Tollefson MM, Weiss JS, Dolan NC, Sagan AA, Stern M, Boyer KM, Bhushan R. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016 May;74(5):945-73.e33. doi: 10.1016/j.jaad.2015.12.037. Epub 2016 Feb 17. Erratum in: J Am Acad Dermatol. 2020 Jun;82(6):1576. doi: 10.1016/j.jaad.2020.02.010. PMID: 26897386.
Acne Medications
Topical Medications
Topical Retinoids
- Topical retinoids are cornerstone treatments because of comedolytic and anti-inflammatory properties. The retinoids tretinoin, adapalene (Differin), tazarotene, and trifarotene (Aklief) are similarly effective.
- Adverse effects can include irritation, photosensitivity, burning sensation, dryness, erythema, exfoliation, peeling, and pain. Concurrent emollient use mitigates irritation.
- Adapalene, tazarotene, and trifarotene can be used concurrently with benzoyl peroxide; tretinoin degrades when benzoyl peroxide is present.
- Consider daily sunscreen use in patients using topical retinoids.
Benzoyl Peroxide
- Available over the counter, benzoyl peroxide is a topical antimicrobial agent that is mildly comedolytic and reduces inflammatory and noninflammatory lesions.
- Adverse effects can include burning sensation, stinging, dryness, erythema, pain, peeling, irritation, fabric staining and bleaching, and, uncommonly, contact allergy.
Topical Antibiotics
- Erythromycin, clindamycin, minocycline (Zlixi, Amzeeq), and dapsone (Aczone) reduce inflammatory lesions but not noninflammatory lesions.
- Topical antibiotic monotherapy, which can result in antibiotic resistance, should be avoided.
Combination Therapy
- Fixed-dose topical combinations of benzoyl peroxide, retinoids, or antibiotics can improve adherence. Adding benzoyl peroxide to topical antibiotic regimens prevents antibiotic resistance.
Clascoterone
- Clascoterone (Winlevi) is a topical antiandrogen that inhibits sebum production and inflammation. Although effective, clascoterone is conditionally recommended because of high cost.
Salicylic Acid
- Salicylic acid is a topical comedolytic agent available over the counter that is conditionally recommended because of limited evidence of benefit.
Azelaic Acid
- Azelaic acid is a topical comedolytic, antibacterial, and anti-inflammatory agent that may be more useful in darker skin types or sensitive skin because it reduces hyperpigmentation associated with acne.
Pregnancy Considerations for Topical Therapies
- Because of limited systemic absorption, pregnant patients can use topical benzoyl peroxide, erythromycin, and clindamycin. The American Academy of Dermatology recommends avoiding topical retinoids during pregnancy.
Systemic Antibiotics
- The guidelines recommend limiting use of systemic antibiotics to reduce the development of antibiotic resistance and systemic complications.
- Oral tetracyclines effectively reduce inflammatory lesions in moderate acne, with doxycycline recommended as a first-line drug over other tetracyclines and azithromycin. Lower-dose doxycycline is preferred because of efficacy with increased tolerability.
- For moderate to severe acne, oral doxycycline is recommended.
- Minocycline is conditionally recommended because of rare adverse effects of vertigo, autoimmune hepatitis, skin hyperpigmentation, drug-induced lupus, and hypersensitivity syndrome. Sarecycline (Seysara) is well tolerated but expensive. Tetracyclines are contraindicated in pregnancy, lactation, and children younger than 9 years because of permanent tooth discoloration or enamel hypoplasia.
Hormonal Therapies
Oral Contraceptives
- Combined oral contraceptives are conditionally recommended to reduce inflammatory and noninflammatory acne lesions but take 3 to 6 months to show improvement.
- Progestin-only formulations may exacerbate acne. Contraceptive adverse effects include venous thromboembolism, myocardial infarction, stroke, and breast and cervical cancers.
Spironolactone
- Spironolactone is conditionally recommended. Potassium monitoring is advised in older patients or in patients with chronic kidney disease or taking medications that can increase potassium.
Isotretinoin
- Oral isotretinoin is strongly recommended for severe, scarring acne and when standard treatment has been ineffective. Although evidence is low quality, many experts agree on its effectiveness.
- Only prescribers enrolled in the Risk Evaluation and Mitigation Strategy iPLEDGE (https://ipledgeprogram.com/#Main) can prescribe isotretinoin because of the risk of exposure in pregnancy.
- In addition, there is conflicting evidence on whether isotretinoin increases suicidal ideation, suicide, or mood changes. Physicians should consider monitoring neuro-psychiatric response, particularly in the adolescent population.
Reference:
- Am Fam Physician. 2025;112(5):574-576
Pediatric Acne by Age
- Neonatal acne — birth to 6 weeks of age
- Neonatal acne is estimated to affect 20% of newborns. Neonatal acne takes the form of comedones (whiteheads and blackheads) that extend from the scalp, upper chest, and back, and inflammatory lesions (erythematous papules and pustules) on the cheeks, chin, and forehead.
- Neonatal acne can be mistaken for neonatal cephalic pustulosis
- Infantile acne — 6 weeks to 1 year of age
- Infantile acne is rare. It occurs in infants up to 16 months of age and presents as comedones, papules, pustules, and occasional nodules. It predominantly affects the cheeks. Occasionally, it leaves scarring.
- Infantile acne can rarely persist until puberty, but it is not associated with underlying endocrine abnormalities.
- Mid-childhood acne — 1–6 years of age
- Acne in this age group is very rare. An endocrinologist should be consulted to exclude possible hyperandrogenism.
- Preadolescent acne — 7–12 years (or up to menarche if female)
- Acne can be the first sign of puberty, and it is common to find acne in this age group.
- It often presents as comedones in the 'T-zone', the region of the face covering the central forehead and the central part of the face (eg, the brow, nose, and lips).
Patient Messaging: Acne
Recommendations to help clear mild-to-moderate adult acne are:
- Adapalene: A retinoid, this active ingredient helps to clear blackheads, whiteheads, and pimples.
- Benzoyl peroxide: This acne-fighter is especially effective at treating mild pimples. While you'll find products that contain up to 10% benzoyl peroxide, it's best to start with a product that contains 2.5%. That will help you avoid side effects like dry, irritated skin or a burning sensation.
- Azelaic acid: It fights acne and can also fade the dark spots that appear when an acne spot clears.
- Salicylic acid: Because it unclogs pores and exfoliates the skin, salicylic acid works best on whiteheads and blackheads.
Use one product for 6 to 8 weeks, taking care to use the product as directed on the instructions. During this time, don't add another product. Don't stop using the product you started with.
It takes some time to know if it is working:
- Fewer breakouts: 4 to 8 weeks
- Clearing: 16 weeks after starting the medication
Reference:
Guideline Recommendations
- Recommendations are made in favor of several topical therapies, including:
- Benzoyl peroxide
- Topical retinoids
- Topical antibiotics
- Clascoterone
- Salicylic acid
- Azelaic acid
- Recommendations are made in favor of several systemic therapies, including:
- Doxycycline
- Minocycline
- Sarecycline
- Combined oral contraceptives
- Spironolactone (+OCP)
- Isotretinoin
- In addition, the guidelines recommend several good clinical practices, including:
- Using topical therapies combining multiple mechanisms of action
- Limiting systemic antibiotic use
- Combining systemic antibiotics with benzoyl peroxide and other topical therapies
- Adjuvant intralesional corticosteroid injections.
Reference:
Additional Notes
Topical retinoids:
- Prefer adapalene (photostable and can mix with BP)
- Not spot treatment
- Use sparingly
- Moisturize under retinoid
- Use pea size on each index finger tip - place on forehead, cheeks, chin and rub in thinly
- Takes 12 weeks for full effect
- Comedonalitic
Benzoyl Peroxide
- Leave on > Washes
- Concentration dependent irritant
- Topically kills C acnes and improves acne
Topical Antibiotics
- Topical clindamycin - only use if in same tube as BP d/t pt not adhering
- C acnes Resistant to erythromycin
Sebum inhibitor
- Clascoterone 1% topical - bid - 12+ yo
- Not monotherapy
Anti-inflammatory
- Dapsone
- Azelaic acid
- Not great clinically
Oral antibiotics:
- Anti-inflammatory
- NOT monotherapy
- Always topical BP
- Use for shortest possible duration
- Tetracyclines
- doxycycline
- qd o bid
- interacts with dairy
- photosensitivity
- intracranial htn (rare)
- minocycline 1 mg/kg
- ER - qd with or without food
- IR - qd or bid
- photosensitivity
- intracranial htn (rare)
- 11% vestibular symptoms with IR
- sarcycline
- If needed: trimethoprim 300 mg tid
- doxycycline
Hormones:
- spironolactone 50-100 mg/d with food in women only
- cheaper
- easier to get
- fewer AE
- OCPs
- Yaz
- Beyaz
Systemic retinoid
- Isotretinoin
Acne Rosacea
Chronic vascular facial disorder of 20-60yo northern/eastern european descent
- Pathogenesis: unknown but implicated factors include bacteria, Demodex mites, vasomotor and connective tissue dysfunction, and topical steroids
Triad:
- Symmetrical erythema
- Papules and pustules
- Telangiectasia on cheeks, forehead, and nose (absence of comedones)
Often exacerbated by sun, wind, hot drinks
Treatment:
- Avoid triggers
- First line:
- topical metronidazole (Daily 1% or bid 0.75%) (I) plus oral tetracycline (tapered from starting dose of 1000mg/d) (I) or minocycline (100-200mg/d) (I)
- Second line: Sulfacetamide (III) plus oral Abx as above
- Third line: Isotretinoin (II)
- Others to reduce rosacea symptoms
- Alpha-adrenergic receptor agonists reduce persistent erythema (brimonidine 0.33% gel qd and oxymetazoline 1% cream qd)
- Nonselective beta blockers reduce flushing symptoms (like carvedilol 6.25 mg bid or propranolol 20-40 mg bid|tid)
- Daily use of a water-based broad-spectrum sunscreen with a sun protection factor of 30 or more
- Daily application of fragrance-free moisturizers
- Twice-daily facial cleansing
Medications for rosacea with papules and pustules:
- Metronidazole 0.75% gel 45g AAA bid ($30-40) (See My Formulary Drugs)
- Ivermectin 1% cream qd (highest effectiveness); NNT=3
- Azelaic acid 15% gel bid; NNT 6
- Low dose doxycycline 40 mg qd or 50|100 mg qd (for mod-severw)
Alternative:
- Clindamycin 1% gel worked well for 1 patient
- Sulfacetamide / Sulfur - Typical dosing for Avar (sulfacetamide / sulfur)
- Cream, gel, lotion, suspension: Apply a thin film to the affected area 1 to 2 times a day.
- Cleanser, cleansing cloth/pads: Wash affected area 1 to 2 times a day.
- Emollient foam: Apply to affected area 1 to 2 times a day. The foam may remain on the skin or may be rinsed off after 1 to 2 minutes.
Rosacea Triggers:
- Acute psychological stressors
- Alcohol (52%)
- Emotional stress (79%)
- Extremes of temperature
- Hot weather (75%)
- Cold weather (46%)
- Heavy Exercise (56%)
- Medications
- Menopausal hot flashes
- Spicy foods (42%)
- Sunlight (81%)
- Wind (57%)
References:
- Cheung M, Taher M, Lauzon G., Acneiform facial eruptions, Canadian Fam Phys, Vol 51; April 2005; 527-533
- AFP Vol 109 No 6 Jun 2024
Alopecia (Hair Loss)
Types:
- Diffuse alopecia
- Anagen effluvium
- Diffuse hair loss days to weeks after exposure to chemotherapeutic agent.
- Usually self-limited and resolves with stopping the offending agent. No pharmacologic intervention is effective.
- Telogen effluvium
- Clumps of hair come out in the shower or a hairbrush. Most often associated with physiologic stress less likely implicated cause are medications, thyroid disease and nutritional and vitamin D deficiencies.
- Usually self-limited and resolves within 6-9 months; treatment is reassurance and removing underlying cause; topical minoxidil can help during regrowth
- Anagen effluvium
- Patterned alopecia
- Androgenetic alopecia
- Family history of hair loss. Gradually progressive.
- Topical monoxidil 2-5% percent solution. Hair loss will recur if treatment is discontinued.
- Androgenetic alopecia
- Focal alopecia
- Alopecia areata
- Tinea capitis
- Traction alopecia
- Trichorrhexis nodosa
- Hair shaft weak this secondary to trauma due to fragile hair. Positive traumas include excessive brushing, heat or chemical applications, and scalp excoriations.
Reference:
- AFP Sep 2024 Vol 110 No 3
Hair Phases
A hair cycle is the natural process by which hair grows, rests, and falls out. It's a continuous cycle that repeats itself throughout an individual's life. Here's a detailed description of the different phases of a hair cycle:
1. Anagen Phase (Growth Phase)
- This is the active growth phase, where hair grows rapidly and can last anywhere from 2-6 years.
- During this phase, hair grows about 0.3 mm per day or 1 cm per month.
- The anagen phase is the longest part of the hair cycle, but it's
also the most intense period of growth.
- Hair follicles are actively producing new hair cells during this phase.
2. Catagen Phase (Transitional Phase)
- This phase typically lasts about 1-2 weeks and occurs immediately before the anagen phase.
- During catagen, the hair follicle starts to shrink and prepare for the resting phase.
- The hair growth rate slows down, and the hair becomes less active.
- The hair shaft begins to flatten out, and the hair grows at a slower rate.
3. Telogen Phase (Resting Phase)
- This is the final stage of the hair cycle, where the hair follicle
rests and prepares for the next growth phase.
- During telogen, the hair growth rate slows down even further, and
the hair shaft remains in its resting position.
- The hair grows very slowly during this phase, and it's usually
around 0.1 mm per day or 0.5 cm per month.
- The telogen phase can last for several months, but it's often shorter than the anagen phase.
4. Exogen Phase (Dying Phase)
- This is the final stage of the hair cycle, where the hair follicle
starts to push out the old hair shaft and make way for a new one.
- The hair growth rate slows down even further during this phase, and
the hair shaft begins to fall out.
- The exogen phase can last anywhere from 2-6 weeks, depending on
individual factors such as genetics and overall health.
- When the hair falls out, it's usually replaced by a new hair follicle that starts the cycle again.
Intralesional Injections
Triamcinolone 5 mg/mL: Administered monthly, with a response rate of 80.9%
- Both saline and lidocaine can be used to dilute triamcinolone acetonide for the treatment of alopecia areata. Saline is more commonly used and has been shown to be effective, while lidocaine may be preferred for its potential to reduce injection pain, although studies have not consistently shown a significant difference in patient discomfort between the two.
- To prepare a 3 mL syringe with a concentration of 5 mg/mL triamcinolone acetonide:
- Use 0.375 mL of triamcinolone acetonide (40 mg/mL).
- Add 2.625 mL of diluent (saline or lidocaine).
- To prepare a 1 mL syringe with a concentration of 5 mg/mL triamcinolone acetonide:
- Use 0.125 mL of triamcinolone acetonide (40 mg/mL).
- Add 0.875 mL of diluent (saline or lidocaine).
- To prepare a 3 mL syringe with a concentration of 5 mg/mL triamcinolone acetonide:
Intralesional triamcinolone acetonide (ILT) treatment generally involves injecting 0.1 mL of the diluted steroid with a 30-gauge needle into the deep dermis at 1 cm intervals, while not exceeding 20 mg ILT in a single session.
A systematic review and meta-analysis found that the pooled rates of hair regrowth were 62.3% (95% confidence interval 50.6%-72.8%; P = .04) with less than 5 mg/mL, 80.9% (95% confidence interval 71%-88%; P < .005) with 5 mg/mL, and 76.4% (95% confidence interval 67.1%-83.7%; P < .005) with 10 mg/mL.
Skin atrophy was described in a subset of studies and occurred in 4 of 120 subjects (3.33%) treated with a concentration of 5 mg/mL and 12 of 59 (20%) treated with a concentration of 10 mg/mL.
Reference:
- Yee, Brittany E. et al. Efficacy of different concentrations of intralesional triamcinolone acetonide for alopecia areata: A systematic review and meta-analysis Journal of the American Academy of Dermatology, Volume 82, Issue 4, 1018 - 1021
- Muhaidat JM, Al-Qarqaz F, Khader Y, Alshiyab DM, Alkofahi H, Almalekh M. A Retrospective Comparative Study of Two Concentrations of Intralesional Triamcinolone Acetonide in the Treatment of Patchy Alopecia Areata on the Scalp. Clin Cosmet Investig Dermatol. 2020 Nov 2;13:795-803. doi: 10.2147/CCID.S280855. PMID: 33173320; PMCID: PMC7646378.
Nonscarring Hair And Scalp Disorders
Labs:
- Complete blood count with red blood cell indices (to assess for anemia)
- Complete metabolic panel (to assess for signs of underlying disease)
- Thyroid-stimulating hormone (to assess for a thyroid disorder) (see "Laboratory assessment of thyroid function", section on 'Evaluating for thyroid dysfunction')
- Ferritin (to assess iron storage) (see "Causes and diagnosis of iron deficiency and iron deficiency anemia in adults", section on 'Iron studies (list of available tests)')
- 25-hydroxyvitamin D levels (to assess for vitamin D deficiency) [17]
The selection of additional laboratory studies is guided by the need to rule out disorders in the differential diagnosis or to further investigate patients with signs or symptoms suggestive of a particular underlying disease, nutritional deficiency, heavy metal or other toxin exposure, or other causes of hair loss.
- As examples, a hormonal work-up to rule out hair loss related to hyperandrogenemia would be appropriate in women with signs of virilization, acne, and obesity, and further evaluation with antinuclear antibodies (ANAs) or other studies would be appropriate for a patient with signs or symptoms of an underlying autoimmune disease.
- In addition, dietary history may reveal nutritional deficiencies that should be evaluated.
Types
- Telogen effluvium: a form of diffuse, nonscarring hair loss that presents as a transient or chronic loss of hair (picture 1A-C). Hair loss in telogen effluvium occurs as a result of an abnormal shift in follicular cycling that leads to the premature shedding of hair. A wide variety of endogenous and exogenous factors have been linked to the induction of telogen effluvium. Examples include major surgery, serious illness, childbirth, protein or caloric malnutrition, drugs, and severe emotional distress. In some cases, the inciting cause is unclear or multiple inciting triggers are identified.
- Anagen effluvium: An acute loss of anagen hair fibers secondary to chemotherapy or toxin exposure and represents acute loss of greater than 80 percent of the scalp hair. Exclamation point hairs (short, 1 to 3 mm hairs with a tapered base) that result from dystrophic hair growth are a common finding. Microscopic evaluation of the proximal ends of hairs dislodged during a hair pull test demonstrates normal or dystrophic anagen hairs rather than telogen hairs. (See "Alopecia related to systemic cancer therapy".)
- Androgenetic alopecia (male or female pattern hair loss): Features of androgenetic alopecia that are useful for distinguishing this condition from telogen effluvium include a clinical examination that demonstrates a characteristic pattern of hair loss and miniaturized hairs (picture 7A-C). A biopsy can be useful for differentiating between these diagnoses in difficult cases. Of note, the two conditions may coexist, and telogen hair shedding can occur early in the course of androgenetic alopecia. (See "Androgenetic alopecia in males: Pathogenesis, clinical features, and diagnosis" and "Female pattern hair loss (androgenetic alopecia in females): Pathogenesis, clinical features, and diagnosis".)
- Diffuse alopecia areata: An uncommon form of alopecia areata that is characterized by the diffuse loss of scalp hair, resulting in the appearance of generalized hair thinning (picture 8). Similar to anagen effluvium, exclamation point hairs may be present, and performance of the hair pull test may reveal dystrophic anagen hairs. A biopsy revealing an inflammatory infiltrate consistent with alopecia areata differentiates this condition from telogen effluvium. (See "Alopecia areata: Clinical manifestations and diagnosis".)
- Loose anagen syndrome: A rare, nonscarring hair loss disorder that manifests with easily extracted anagen hairs from the scalp (picture 9). Young children are typically affected, particularly females with blond hair. Characteristically, examination of shed hairs reveals anagen hairs with ruffled cuticles (picture 10).
- Structural hair disorders: A variety of structural hair disorders causes weakening of the hair shaft that results in easily fractured hair. Unlike telogen effluvium, in which hair is shed from the follicle, these conditions result in increased breakage of hair. Close examination and 2x magnification of the loose hair will reveal broken hairs and may also reveal characteristic findings of a particular structural hair disorder.
Study: The Role of Vitamins and Minerals in Hair Loss: A Review
Hair loss is a common problem that may be improved with vitamin and mineral supplementation. Vitamins and minerals are important for normal cell growth and function and may contribute to hair loss when they are deficient. While supplementation is relatively affordable and easily accessible, it is important to know which vitamins and minerals are helpful in treating hair loss.
Androgenetic alopecia (AGA), telogen effluvium (TE) are two common types of hair loss. Studies show that supplementing the diet with low levels of vitamin D can improve symptoms of these diseases. If a patient with AGA or TE has low iron levels (more commonly seen in females), supplementation is also recommended. These iron-deficient patients should also ensure their vitamin C intake is appropriate. At the present time there is insufficient data to recommend zinc, riboflavin, folic acid, or vitamin B12 supplementation in cases of deficiency. Neither vitamin E or biotin supplementation are supported by the literature for treating AGA or TE; in addition, biotin supplementation can also lead to dangerous false laboratory results. Studies show that too much vitamin A can contribute to hair loss, as can too much selenium, although more studies are needed to establish the latter relationship.
Alopecia areata (AA) occurs when the immune system attacks the hair follicle. Studies have shown a relationship between AA and low vitamin D levels. Vitamin D should be supplemented if levels are low. However, more studies are needed to determine the effect of iron and zinc supplementation on AA patients. There is currently not enough data to recommend supplementation of folate or B12. Biotin supplementation is not supported by available data for the treatment of AA. It is unclear if selenium plays a role in this disease; therefore, supplementation with this mineral is not recommended.
Iron, vitamin D, folate, vitamin B12, and selenium are vitamins and minerals that may be involved in hair graying/whitening during childhood or early adulthood. Supplementing these deficient micronutrients can improve premature graying.
Reference:
- Almohanna, Hind M et al. "The Role of Vitamins and Minerals in Hair Loss: A Review." Dermatology and therapy vol. 9,1 (2019): 51-70. https://doi.org/10.1007/s13555-018-0278-6
Atopic Dermatitis (Eczema)
Non-pharmacologic treatment options:
- Moisturizers:
- Use liberally, combine with bathing, patient preferences on type
- Bathing practices:
- Minimum perform daily
- Soak in warm water 10-15 minutes
- Followed by quick pat drying and immediate application (2-3 minutes) of topical moisturizer/medications.
- Bleach baths:
- Once or twice weekly bleach (sodium hypochlorite) is effective in clinically improving moderate-to-severe AD in children.
- May also help adults
- Thought to reduce skin inflammation and decrease S. Aureus colonization.
- Wet wrap therapy (wwt):
- Using layers of bandage, guaze, clothing, etc with topical medications. Evidence supports improvement of symptoms in children.
Pharmacologic treatment options:
- Topical corticosteroids
- Topical calcineurin inhibitors
- Dupilumab
- Phototherapy
- Systemic immunosuppresents: cyclosporine, azathioprine, mycophenolate, methotrexate
For eczema:
- Wash with a gentle soap. Use soap minimally.
- Eucerin Eczema Relief Cream Body Wash
- Dove sensitive bar soap
- Dove Sensitive Skin body wash
- Use a moisturizing cream like this after showering. Make sure you are showering for at least 20 min so the skin cells can absorb all the water possible.
- Vaseline Intensive Care Body Lotion Advanced Repair Unscented
- CeraVe Moisturizing Cream, Face & Body Moisturizer for Normal to Very Dry Skin
Bed Bugs
Pregression of bites:
- Initial reaction
- Erythematous, pruritis macules with central hemorrhagic puncta in linear or grouped distribution
- Subsequent reactions
- Wheals, papules, vesicles
Differential Diagnosis:
- Bedbugs
- Fleas
- Lice
- Mosquitoes
- Scabies
- Spiders
- Ticks
Treatment:
- Vacuuming
- Heat or cold treatment
- Trapping - use plastic encasements to trap bedbugs and prevent migration to and from hiding spots
- Pesticides
- Can use petroleum jelly on legs of furnature to prevent ascending
References:
- AFP Vol 86 No 7 Oct 2012
Best treatment for mild-mod acne vulgaris
- adapalene/benzoyl peroxide (EpiDuo)
- clindamycin/benzoyl peroxide (Neuac)
- adapalene (Differin)
Reference:
- AFP Vol 106 No 6 Dec 2022
Burns
Refer to a Burn Center:
- Burns to the face, hands, feet, major joints, genitalia, or perineum
- Children in health care facilities without staff trained to treat children or appropriate equipment for children
- Concurrent trauma
- Electrical or chemical burns
- Full-thickness (third-degree) burns at any age
- Greater than 10% total body surface area involved
- Inhalation injuries
- Need for special support (social, emotional, rehabilitative)
- Preexisting medical issues that may complicate treatment or recovery or increase mortality risk
Topical Agents:
- Bacitracin
- Impregnated nonadherent gauze (Xeroform, Vaseline gauze)
- Mafenide acetate (Sulfamylon)
- Medical grade honey
- Mupirocin
- Silver sulfadiazine (Silvadene)
References:
- AFP Vol 101 No 8 Apr 2020
Carcinomas (Basal Cell and Cutaneous Squamous Cell)
Comparison of Basal Cell and Cutaneous Squamous Cell Carcinoma
| Characteristics | Basal cell carcinoma | Cutaneous squamous cell carcinoma |
|---|---|---|
| Patient age | Uncommon in adults younger than 40; up to 20% of tumors occur in adults younger than 50 | Uncommon in adults younger than 50 |
| Patient characteristics | Fair skin, blue eyes, red or light-colored hair, inability to tan | Few, if any, identifiable phenotypic markers associated with high risk |
| Tumor location | Most tumors (85%) occur on the head and neck region, with 25% to 30% occurring on the nose; does not correlate well with areas of maximal sun exposure; approximately one-third occur on areas that receive little or no ultraviolet exposure | More common on the back of the hands and forearms; tumors on the head and neck are most common on areas that receive maximal sun exposure |
| Ultraviolet light exposure | Weaker association; exposure in childhood and adolescence more important | Stronger association; cumulative exposure more important |
Biopsy:
- Initial tissue sampling is typically performed using a shave technique if the lesion is raised
- Can alternatively use a punch biopsy of the most abnormal-appearing skin
- Pigmented lesions and those with any features concerning for melanoma risk should always be evaluated using a full-thickness technique
Risk Stratification of Low- vs. High-Risk Basal Cell Carcinoma
| Basal cell and squamous cell carcinoma (clinical) | ||||
|---|---|---|---|---|
| Parameters | Low risk | High risk | ||
| Location* and size† | Low-risk location and < 20 mm Moderate-risk location‡ and < 10 mm — | Low-risk location and ? 20 mm Moderate-risk location and ? 10 mm High-risk location§ | ||
| Borders | Well defined | Poorly defined | ||
| Primary vs. recurrent | Primary | Recurrent | ||
| Immunosuppression | No | Yes | ||
| Site of prior radiation therapy | No | Yes | ||
| Basal cell carcinoma (pathologic) | ||||
| Parameters | Low risk | High risk | ||
| Growth pattern | Superficial, nodular | Aggressive¶ | ||
| Perineural involvement | No | Yes | ||
| Squamous cell carcinoma (pathologic) | ||||
| Parameters | Low risk | High risk | ||
| Degree of differentiation | Well or moderately differentiated | Poorly differentiated | ||
| High-risk histologic subtype** | No | Yes | ||
| Depth (thickness or Clark level)†† | < 2 mm or I, II, III | ? 2 mm or IV, V | ||
| Perineural, lymphatic, or vascular involvement | No | Yes |
Low-risk location = trunk and extremities excluding hands, feet, nail units, pretibia, and ankles; Moderate-risk location = cheeks, forehead, scalp, neck, and pretibia; High-risk location = central face, eyelids, eyebrows, periorbital skin, nose, lips, chin, mandible, preauricular and postauricular skin/sulci, temple, ear, genitalia, hands, and feet.
Management (National Cancer Care Network guidelines)
- BCC:
- Excision of low-risk primary BCC with a 4-mm margin of uninvolved skin around the tumor
- Incomplete excision of the primary tumor (i.e., pathology demonstrating tumor at the surgical margin) should be followed by immediate re-excision or Mohs micrographic surgery
- CSCC:
- Excision of low-risk primary CSCC with a 4-mm to 6-mm margin of uninvolved skin around the tumor
- Mohs micrographic surgery is an appropriate option for high-risk tumors or tumors in sensitive anatomic locations
Post Diagnosis Management:
- Annual screening of the patient for new primary skin cancers, including BCC, CSCC, and melanoma
References:
- AFP Sep 2020 Vol 102, No 6
Cellulite edit
Products containing caffeine may dehydrate cells, which can make cellulite less obvious. To maintain the results, you'll have to apply the product every day.
A product that contains 0.3% retinol may also have some effect on cellulite. Some women who've used it say they see a little less cellulite. Retinol can help thicken the skin, which may reduce how much cellulite you see. Before you'll know if retinol can help you, you'll need to apply the product for 6 months or possibly longer.
If you're interested in trying a cellulite cream or lotion, it helps to test it on a small area first. Some people have an allergic skin reaction.
| Treatment type | Brand |
|---|---|
| Topical agents | Bliss, Clarins, Shisheido, Glytone |
| Radiofrequency devices | Venus Legacy (Venus Concept), Endymed PRO (Endymed), Velashape (Cynosure) |
| Laser/light devices | Cellulaze (Cynosure) |
| Acoustic wave therapy | Z-wave (Zimmer), Cellactor (Storz) |
| Subcision | Cellfina (Merz) |
| Injectable biologic treatments | EN3835 (Endo) |
| Fillers | Calcium hydroxyapatite (Radiesse), poly-l-lactic acid (Sculptra) |
Topical agents, combined with vigorous massage, were the earliest attempts to treat cellulite. As with all topical treatments, the main challenge of these therapies is for the active ingredients to reach their target in sufficient concentration to have a therapeutic effect. Methylxanthines (aminophylline, theophylline, and caffeine) and retinoids have been the most extensively evaluated ingredients used in topical formulations for cellulite.
Methylxanthines are hypothesized to improve cellulite by stimulating lipolysis and inhibiting the enzyme phosphodiesterase, which increases the concentration of cyclic adenosine monophosphate. Retinoids, on the other hand, are thought to reduce cellulite by increasing dermal thickness, increasing angiogenesis, synthesizing new connective tissue components, and increasing the number of active fibroblasts. For both agents, there have been several peer-reviewed publications with promising data, but the studies have been small with no long-term follow-up.
Reference:
- Sadick N. Treatment for cellulite. Int J Womens Dermatol. 2018 Oct 22;5(1):68-72. doi: 10.1016/j.ijwd.2018.09.002. PMID: 30809581; PMCID: PMC6374708.
Chronic Urticaria
Treatment:
- Start second generation H1 antihistamine
- If insufficient do one of the following:
- Titrate second generation H1 antihistamine to 2 to 4 times normal dose
- Add a different second generation H1 antihistamine
- Add H2 antihistamine
- Add first-generation H1 antihistamine at night
- Add leukotriene receptor antagonist
- If insufficient
- Add high-potency antihistamine hydroxyzine or doxepin and titrate as tolerated
- If insufficient
- Consider referral for immunomodulatory therapy such as omalizumab or cyclosporine
Urticaria Causes:
- Immunoglobulin E mediated (IgE)
- Aeroallergens
- Contact allergen
- Food allergen
- Insect venom
- Medications
- Parasitic infections
- Non-IgE immunologically mediated
- Aeroallergens (proteases)
- Autoimmune disease
- Bacterial infections
- Cryoglobulinemia
- Fungal infections
- Lymphoma
- Vasculitis
- Virla infections
- Nonimmunologically mediated
- Contact allergen
- Elevation of core body temperature
- Food pseudoallergens
- Light
- Mastocystosis
- Medications (direct mast cell degranulation)
- Physicla stimuli (cold, heat, pressure, vibration)
- Water
Conditions confused with urticaria
- Arthropod bites
- Lesions lasting several days, insect exposure history
- Atopic dermatitis
- Maculopapular, scaling, characteristic distribution
- Bullous pemphigoid
- Lesions lasting >24hrs, blistering, Nikolsky sign (light friction causes erosion or vesicle)
- Contact dermatitis
- Indistinct margins, papular, persistent lesions, epidermal component present
- Erythema multiforme
- Lesions lasting several days, iris-shaped papules, target appearance, may have fever
- Fixed-drug reactions
- Offending drig exposure, not pruritic, often bullous, hyperpigmentation
- Henoch-Schonlein purpura
- Lower extremity, purpuric lesions, systemic symptoms
- Mastocytoma
- Yellow to orange pigmentation, Darier sign (a wheal and flare up reaction with stroking the lesion), flushing, bullae, most common in children
- Mastocytosis, diffuse cutaneous
- Normal to yellow-brown skin color, diffuse thickening, bullae
- Morbilliform drug reactions
- Maculopapular, associated with medication use
- Pityriasis rosea
- Lesion lasting weeks, herald patch, Christmas tree pattern, often not pruritic
- Urticaria pigmentosa
- Smaller lesions (1-3 mm), orange to brown pigmentation, Darier sign
- Viral exanthem
- Not pruritic, prodrome, fever, maculopapular, individual lesions lasting days
References:
- AFP Vol 95 No 11 Jun 2017
Common Benign Skin Tumors edit
| Condition | Characteristics | Differential diagnosis | Treatment | Comments | Precautions and referral criteria |
|---|---|---|---|---|---|
| Acrochordon | Skin-colored to brown papules on narrow stalk | Senescent intradermal nevus | Cryosurgery, electrodesiccation, scissor or shave excision | Do not send multiple specimens in same jar | Cryosurgery should be performed with caution in persons with darker skin; refer patients with eyelid involvement |
| Cherry angioma | Dome-shaped, small, bright red to violaceous, soft, compressible papules | Pyogenic granuloma | Electrodesiccation, laser ablation | Numerous lesions (hundreds) and early onset can occur in Fabry disease | Genetic evaluation for Fabry disease in patients with multiple lesions |
| Dermatofibroma | Firm, raised, tan to reddish-brown papules or nodules; dimpling with lateral compression | Cellular dermatofibroma, dermatofibrosarcoma protuberans | Cryosurgery, intralesional steroid injection, laser ablation, punch excision | Abrupt appearance of multiple lesions may occur in persons with human immunodeficiency virus infection or systemic lupus erythematosus | Refer patients with cellular variant and dermatofibrosarcoma protuberans (deep invasion and metastases) |
| Epidermal inclusion cyst | Firm, mobile, subcutaneous nodule with central punctum; painless (unless inflamed) | Lipoma, abscess (vs. inflamed cyst) | Excision, intralesional steroid injection with interval excision for inflamed cysts | Presence of punctum helps differentiate cysts from lipomas; history helps differentiate between inflamed cyst and abscess (acute) | Inflamed cysts and those that have undergone previous incision and drainage can be more difficult to excise; refer patients with facial cysts |
| Keratoacanthoma | Rapidly growing, dome-shaped hyperkeratotic papule on sun-damaged skin | Squamous cell carcinoma, verruca, hypertrophic actinic keratosis | Excision, intralesional injection (methotrexate, fluorouracil, bleomycin), Mohs micrographic surgery | Cannot be histologically differentiated from squamous cell carcinoma | Refer patients with recurrence after complete excision |
| Lipoma | Soft, mobile subcutaneous nodules | Epidermal inclusion cyst, liposarcoma, deep hemangioma | Incision or punch excision and manual expression | Ultrasonography can help differentiate lipomas from other deep neoplasms | Use caution with facial lipomas and recurrent lesions after excision |
| Pyogenic granuloma | Rapidly growing, yellow to violaceous, friable nodule, often surrounded by scaly collarette | Amelanotic melanoma, Spitz nevus, basal cell carcinoma, squamous cell carcinoma | Laser ablation, shave excision with electrodesiccation of base | Send for histologic evaluation to rule out melanoma | Refer patients with recurrent lesions or facial lesions |
| Sebaceous hyperplasia | Dome-shaped papule with central umbilication and uniform yellow lobules on magnification | Basal cell carcinoma | Chemical cautery, cryosurgery, electrodesiccation, laser ablation, oral isotretinoin, phototherapy, shave excision | Thin shave biopsy can rule out basal cell carcinoma | Basal cell carcinoma is generally red or pink and increases in size |
| Seborrheic keratosis | Well-circumscribed, yellow to brown, "stuck-on" papules and plaques | Atypical nevus, melanoma | Cryosurgery, curettage, electrodesiccation, laser ablation, shave excision | Consider malignancy workup for abrupt appearance of multiple lesions |
Reference:
- AFP Oct 2024 Vol 110 No 4
Dermatology Procedures
See also:
Skin Closure
Suture Materials:
Absorbable
| Material | Needle type | Tie to lose 50% strength | Configuration | Typical use |
|---|---|---|---|---|
| Chromic | Reverse cutting | 10-14 days | Monofilament | Mucosa, eye wounds |
| Glycolide/lactide polymer | Conventional or | 2-3 weeks | Braided | Deep dermal, muscle, fascia, |
| (Vicryl) | reverse cutting | oral mucosa, genitalia wounds | ||
| Polioglecaprone | Conventional or | 7-10 days | Monofilament | Dermal, subcuticular wounds |
| (Monocryl) | reverse cutting | |||
| Polydioxanone | Reverse cutting | 4 weeks | Monofilament | Muscle, fascia, dermal wounds |
Nonabsorbable
| Material | Needle Type | Time to lose 50% strength | Configuration | Typical use |
|---|---|---|---|---|
| Nylon (Ethilon) | Cutting edge | >10 years | Monofilament | Skin |
| Polypropylene | Tapered point, | Indefinite | Monofilament | Vascular surgery, skin, tendon, |
| (Prolene) | blunt tip | and ligaments | ||
| Silk | No needle | 1 year | Braided | Hemostasis in ligation of vessels |
| or for tying over bolsters |
Suture removal timing:
| Location | Removal Timing |
|---|---|
| Face | 3-5d |
| Scalp | 7-10d |
| Arms | 7-10d |
| Trunk | 10-14d |
| Legs | 10-14d |
| Hands or feet | 10-14d |
| Palms or soles | 14-21d |
Criteria for Tissue Adhesives:
- Wound less than 12 hours old
- Linear
- Hemostatic
- Not crossing a joint
- Not crossing a mucocutaneous junction
- Not in a hair-bearing area
- Not under significant tension
- Not grossly contaminated
- Not infected
- Not devitalized
- Not a result of a mammalian bite
- No chronic condition that might impair wound healing
References:
- AFP Vol 78 No 8 Oct 2008
- AFP Vol 95 No 10 May 2017
Biopsy techniques
Sterile gloves offer no benefit for minor outpatient skin procedures
- No difference in risk of infection for common outpatient skin procedures such as laceration repair or lesion excision.
- Relative risk of infection: Non-significant 0.95 (95% CI 0.65 to 1.40)
References:
- AFP Vol 97 No 9 May 2018
Dermoscopy
The Two-Step Algorithm
- Step 1 - Determine if lesion is melanocytic or not
- Determine if lesion is benign or malignant
- Step 2 - Determine if lesion is a Nevus, Suspicious, or Melanoma
- Determine if need to biopsy or not
- Determine if digital monitoring (never for raised lesions)
A lesion is Melanocytic if it:
- Has a network (Except in the following:)
- Dermatofibroma (fine network surrounding central scar)
- Solar lentigo (fine interrupted lines and moth eaten border)
- Ink blot lentigo
- Aggregated or peripheral rim of globules
- Usually in growing nevi
- Streaks
- Usually = bad
- Think biopsy
- Spitz nevus - juvenile melanoma
- Homogenous blue pigment
- Blue nevus
Example images:
References:
Non-Melanocytic Lesions
Benign:
- Dermatofibroma
- Delicate network
- Central scar-like/crystalline
- Ring like globules
- Vessels/blush in center
- Seborrheic keratoses
- Milia-like cysts
- Comedo like openings
- Fissures and ridges (gyri and sulci)
- Fingerprint like
- Hairpin vessels
- Moth-eaten borders
- Hemangioma (vascular lesions)
- red
- maroon
- blue
- black
- clear
- Clear Cell Acanthoma
- Dotted or glomerular vessels distributed in a serpiginous pattern (string of pearls)
Malignant:
- Basal Cell Carcinoma (at least 1 of the following)
- Large grey-blue ovoid nests
- Multiple grey-blue globules
- Leaflike areas
- Spoke wheel areas
- Arborizine "tree like" telangiectasia
- Ulceration
- Squamous Cell Carcinoma - Focally scaly/keratotic and rough
- Glomerular vessels
- Hairpin vessels
- Keratin pearls and white circles
- Rosettes (strawberry pattern)
- Brown dots/globules aligned in a linear fashion at the periphery
Melanocytic Lesions
Benign Patterns:
- Diffuse Reticular
- Patchy Reticular
- Peripheral reticular with central hypopigmentation
- Peripheral reticular with central hyperpigmentation
- Homogenous
- Peripheral globules/starburst
- Peripheral reticular with central globules
- Globular
- Two components
- Symmetric multi-component (controversial)
Melanomas:
- Melanomas deviate from benign patterns.
- Have one of the specific features:
- Atypical network
- Negative pigment network
- Streaks
- Off-centered blotch
- Atypical dots and/or globules
- Regression structures
- Scar-like depigmentation and peppering - can have appearance of blue-white veil
- Blue-white veil overlying raised areas
- Atypical vascular structures
- Dotted vessels over milky red backgrounds
- Serpentine vessels
- Polymorphous vessels
- Shiny white lines (Crystalline structures)
- Peripheral tan structureless areas
Vasculature
Non-melanocytic lesions:
- Hairpin - keratinizing tumors
- Glomerular - SCC
- Arborizing - BCC
- Crown - Seborrheic hyperplasia
- Dotted in serpiginous distribution - CCA
Melanocytic lesions:
- Comma - IDN
- Dotted - MM & Spitz & DN
- Linear and polymorphous - MM
- Corkscrew - MM (Mets)
- Irregular hairpin (serpentine) - MM & CMN
- Milky red area
Management
- Benign pattern -> Reassure
- Deviates from benign -> Biopsy
- For flat only slightly suspicious lesions that patients want to wait:
- Photograph
- Re-evaluate and rephotograph in 3mo
- If changing -> biopsy
Palms/Soles - parallel pattern is expected:
- If run in furrows -> benign
- If parallel pattern runs on peaks -> melanoma
Face - pseudo-network pattern due to gland openings
Other
Notes:
- Photograph all lesions biopsied
- Clinical
- Dermatoscope
Other Resources:
- Tutorial: http://www.dermoscopy.org/atlas/base.htm
- International Society of Dermoscopy: http://www.dermoscopy-ids.org/discussion
Folliculitis
Definition:
- Inflammation of the hair follicle 2/2 mechanical trauma, irritation, or infection
- Usual infectious organism is S aureus, also gram neg (after prolonged topical Ax) and pitysporum (saprophytic yeast) as well
- Pustules in clusters on hair-bearing areas of body.
Treatment:
- Pityrosporum:
- First Line: Topical econazole (III), selenium sulfide shampoo (III), or 50% propylene glycolor etoconazole (III) - 3 weeks treatment
- Second line: Oral fluconazole (II), itraconazole (I), or ketoconazole (II) - 10-14 days
- Third line: Oral antifungal plus topical agents (II)
- Bacterial:
- First line: Topical mupirocin (I), erythromycin (III), clindamycin (III), or benzoyl peroxide (III) - treat until lesions resolvedd
- Second line: Oral antistaphylococcal antibiotics (flouroquinolones(I), first gen cephalosporins (III), or macrolides (III))
- Gram negatives:
- First line: Isotretinoin (II)
- Second line: Ampicillin (III) or trimethoprim-sulfamethoxazole (III)
References:
- Cheung M, Taher M, Lauzon G., Acneiform facial eruptions, Canadian Fam Phys, Vol 51; April 2005; 527-533
Hidradenitis suppurativa
Hair removal from shaving or using depilatories, deodorants, and irritation from anything rubbing against the affected area can worsen the condition.
The Hurley classification system is used to define severity and guide treatment.
- Stage I: single or multiple abscesses without sinus tracts or scarring
- Medical
- First line: Topical clindamycin
- Second line: Topical resorcinol
- Surgical
- Punch debridement
- Drain painful abscess
- Intralesional triamcinolone
- Medical
- Stage II: abscess recurrence with sinus tracts and scarring; widely separated lesions
- Medical (Topical Clindamycine AND)
- First line: Tetracycline Abx
- Second line: Adalimumab (Humira)
- Third line: Acitretin, oral clindamycin plus rifampin
- Surgical
- Local excision for larger, chronic lesions or sinus tracts
- Medical (Topical Clindamycine AND)
- Stage III: diffuse skin involvement with multiple sinus tracts and widespread abscess formation
- Medical (Topical Clindamycine AND)
- First line: Adalimumab
- Second line: Infliximab (Remicade), anakinra (Kineret), oral clindamycin plus rifampin
- Medical (Topical Clindamycine AND)
Reference:
- Am Fam Physician. 2019;100(9):562-569
Self-Care Guidelines (for patients)
It may also help if you can avoid things that can irritate your skin, by:
- Wearing loose-fitting clothing
- Avoiding heat and humidity
- Being careful not to injure your skin
- Staying at a healthy weight
- Don't smoke
For draining lesions:
- Make sure to wash any red, draining area(s) of hidradenitis suppurativa with an antibacterial soap, and then apply antibiotic ointment and clean bandages.
- If there is a large amount of drainage, change the gauze pads and dressings often.
- Warm compresses and ibuprofen can help reduce the swelling.
More information: https://familydoctor.org/condition/hidradenitis-suppurativa/?adfree=true
Hyperpigmentation
Postinflammatory Hyperpigmentation
First-line topical therapies
- hydroquinone 4%
- Triple combination therapy (Tri-Luma)
- fluocinolone 0.01%
- hydroquinone 4%
- tretinoin 0.05%
- This triple combination therapy is more effective but more costly than hydroquinone alone
Reference:
- Am Fam Physician. 2023;107(5):461
Infections, Insect bites, and Stings
See also: Cutaneous Larva Migrans
There are also risk factors for a systemic sting reaction:
- A sting reaction < 2 months earlier increases the risk of a subsequent systemic sting reaction by ≥ 50%.
- Pucci S, Antonicelli L, Bilò MB, et al. Shortness of interval between two stings as risk factor for developing Hymenoptera venom allergy. Allergy.1994;49:894-896.
- Among beekeepers, paradoxically, the risk of a systemic reaction is higher in those stung < 15 times a year than in those stung > 200 times.
- Müller UR. Bee venom allergy in beekeepers and their family members. Curr Opin Allergy Clin Immunol. 2005;5:343-347.
- Patients with an elevated baseline serum level of tryptase (reference range, < 11.4 ng/mL), which is part of the allergenic response, or with biopsy-proven systemic mastocytosis are at increased risk of a systemic sting reaction.
Bee stings:
- Among beekeepers, the risk of a systemic reaction is higher in those stung < 15 times a year than in those stung > 200 times.
- Remove honey bee stingers by scraping the skin with a fingernail or credit card. Ideally, the stinger should be removed in the first 30 seconds, before the venom sac empties. Otherwise, intense local inflammation, with possible lymphangitic streaking, can result
Centipede
- The bite of a larger centipede can cause a painful reaction that generally subsides after a few hours but can last several days. Centipede bites are usually nonfatal to humans
Spiders
- brown recluse spider is described as having a violin-shaped marking on the abdomen; the body is yellowish, tan, or dark brown. A bite can produce tiny fang marks and cause dull pain at the site of the bite that spreads quickly; myalgia; and pain in the stomach, back, chest, and legs.28,29 The bite takes approximately 7 days to resolve.
- black widow spider is black; females exhibit a distinctive red or yellow hourglass marking on their ventral aspect.28,31 The pinprick sensation of a bite leads to symptoms that can include erythema, swelling, pain, stiffness, chills, fever, nausea, and stomach pain.
Fleas
- Flea bites, which generally occur on lower extremities, develop into a small, erythematous papule with a halo (FIGURE 4) and associated mild edema, and cause intense pruritus 30 minutes after the bite.
- Fleas are a vector for severe microbial infections, including bartonellosis, bubonic plague, cat-flea typhus, murine typhus, cat-scratch disease, rickettsial disease, and tularemia. Tungiasis is an inflammatory burrowing flea infestation—not a secondary infection for which the flea is a vector
Flies and biting midges
- include black flies, deer flies, horse flies, and sand flies
- Flies can transmit several infections, including bartonellosis, enteric bacterial disease (eg, caused by Campylobacter spp), leishmaniasis, loiasis, onchocerciasis, and trypanosomiasis.43
- Biting midges, also called "no-see-ums," biting gnats, moose flies, and "punkies,"44 are tiny (1-3 mm long) blood-sucking flies
Mosquitoes
- Advise patients to reduce their risk by using insect repellent, sleeping under mosquito netting, and wearing a long-sleeve shirt and long pants when traveling to endemic areas or when a local outbreak occurs
Ticks
- Ticks should be removed with fine-tipped tweezers. Grasp the body of the tick close to the skin and pull upward while applying steady, even pressure. After removing the tick, clean the bite and the surrounding area with alcohol or with soap and water. Dispose of a live tick by flushing it down the toilet; or, kill it in alcohol and either seal it in a bag with tape or place it in a container
Symptom control
- Symptomatic treatment of mild bites and stings includes washing the affected area with soap and water and applying a cold compress to reduce swelling.54 For painful lesions, an oral analgesic can be prescribed.
- For mild or moderate pruritus, a low- to midpotency topical corticosteroid (eg, hydrocortisone valerate cream 0.2% bid), topical calamine, or pramoxine can be applied,or a nonsedating oral antihistamine, such as loratadine (10 mg/d) or cetirizine (10 mg/d), can be used.14,55 For severe itching, a sedating antihistamine, such as hydroxyzine (10-25 mg every 4 to 6 hours prn), might help relieve symptoms; H1- and H2-receptor antagonists can be used concomitantly.
- Large local reactions are treated with a midpotency topical corticosteroid (eg, triamcinolone acetonide cream 0.1% bid) plus an oral antihistamine to relieve pruritus and reduce allergic inflammation. For a more severe reaction, an oral corticosteroid (prednisone 1 mg/kg; maximum dosage, 50 mg/d) can be given for 5 to 7 days
- Managing anaphylaxis
- First-line therapy is intramuscular epinephrine, 0.01 mg/kg (maximum single dose, 0.5 mg) given every 5 to 15 minutes
- Administration of O2 and intravenous fluids is recommended for hemodynamically unstable patients.
- Antihistamines and corticosteroids can be used as secondary treatment but should not replace epinephrine
References:
- JFP Dec 2020 Vol 69 No 10
Ingrown Nail
Things to do to help an ingrown nail:
- Soak your foot in warm, salty water to help soften the skin around your toe and reduce the chances of infection
- Keep your foot dry for the rest of the day
- Wear wide, comfortable shoes or sandals
- Take acetaminophen (Tylenol) or ibuprofen to ease the pain
- Do not cut your toenail – leave it to grow out
- Do not pick at your toe or toenail
- Do not wear tight, pointy shoes
To prevent ingrown toenails:
- Do not cut your toenails too short
- Cut straight across the nail, not the edges
- Do not wear shoes that are too tight or do not fit properly
- Keep your feet clean and dry them thoroughly
Keloids and Hypertrophic Scars
| Hypertrophic scars | Keloids |
|---|---|
| Remain confined to border of original wound | Extend beyond border of original wound |
| Arise in any location; commonly occur on extensor surfaces of joints | Commonly occur on the sternal skin, shoulders and upper arms, earlobes, and cheeks |
| Regress with time | Grow for years |
| Fewer thick collagen fibers | Thick collagen |
| Scanty mucoid matrix | Mucoid matrix |
| Flatten spontaneously in time | Remain elevated more than 4 mm |
| Appear within one month | Appear at three months or later |
| Less association with skin pigmentation | More common in darker skin types |
Prevention:
- Anything that expedites wound healing and diminishes skin tension (e.g., postsurgical taping for 12 weeks) will diminish risk.
Corticosteroid Injections
- first-line option for family physicians.
- Triamcinolone acetonide suspension (Kenalog) 10 to 40 mg per mL (depending on the site) is injected intralesionally
- will eventually flatten 50 to 100 percent of keloids
- 9 to 50 percent recurrence rate.
- Lidocaine (Xylocaine) may be combined with the corticosteroid to lessen pain, whereas using adjunctive cryotherapy immediately before injection may make the procedure easier by softening the scar (based on expert opinion).
- Combining cryotherapy and corticosteroid injections also improves outcomes more than either modality alone, although hypopigmentation is always a significant concern.
- Usually 2-3 injections are given a month apart; however, therapy can continue for six months or longer.25
- Newer keloids are more responsive to therapy than older, established lesions.
- Common adverse effects include atrophy, telangiectasias, and hypopigmentation.
- 1 mL polycarbonate syringe with a 25 G, 16 mm needle was the combination requiring the lowest injection force
- Clinically, the response to corticosteroid injection alone was variable with 50–100% regression and a recurrence rate of 33% and 50% after 1 and 5 years, respectively
Reference:
- Am Fam Physician. 2009;80(3):253-260
- Morelli Coppola M, Salzillo R, Segreto F, Persichetti P. Triamcinolone acetonide intralesional injection for the treatment of keloid scars: patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018 Jul 24;11:387-396. doi: 10.2147/CCID.S133672. PMID: 30087573; PMCID: PMC6063260.
Lice Treatment
A few notes on lice treatment:
- Do not use a combination shampoo/conditioner, or conditioner before using lice medicine.
- Do not re–wash the hair for 1–2 days after the lice medicine is removed.
- After each treatment, checking the hair and combing with a nit comb to remove nits and lice every 2–3 days may decrease the chance of self–reinfestation. Continue to check for 2–3 weeks to be sure all lice and nits are gone.
- Machine wash and dry clothing, bed linens, and other items that the infested person wore or used during the 2 days before treatment using the hot water (130°F) laundry cycle and the high heat drying cycle. Clothing and items that are not washable can be dry–cleanedORsealed in a plastic bag and stored for 2 weeks.
- Soak combs and brushes in hot water (at least 130°F) for 5–10 minutes.
- Vacuum the floor and furniture, particularly where the infested person sat or lay. However, the risk of getting infested by a louse that has fallen onto a rug or carpet or furniture is very small. Head lice survive less than 1–2 days if they fall off a person and cannot feed; nits cannot hatch and usually die within a week if they are not kept at the same temperature as that found close to the human scalp. Spending much time and money on housecleaning activities is not necessary to avoid reinfestation by lice or nits that may have fallen off the head or crawled onto furniture or clothing.
- Do not use fumigant sprays; they can be toxic if inhaled or absorbed through the skin
Reference:
Medications
- Topical Antibiotics
- Clindamycin, Erythromycin, Metronidazole
- Uses: Mild/Mod acne/rosacea
- Topical Keratolytics
- Retinoids, Benzoyl peroxide, Salicylic acid, Azelaic acid
- Uses: Acne, rosacea
- Topical Anti-inflammatory agents
- Azelaic acid, Topical corticosteroids, Tars
- Topical Anti-fungals
- Azoles, Allylamines, Benzoyl peroxide, Selenium sulfide, Pyrithione zinc
- Uses: Seborrheic dermatitis, Malassezia folliculitis
- Topical Miscellaneous
- Sodium sulfacetamide, sulfer, tar, Ivermectin, Brimonidine
- Systemic Antibiotics
- Tetracyclines, Erythromycin, Sulfas
- Uses: Mod/Severe acne/rosacea
- Systemic Retinoids
- Isotretinoin
- Uses: Nodulocystic, severe acne; select severe rosacea
- Oral contraceptives
References:
- Consultant Oct 2015
Melanoma
Risk Factors:
- Congenital melanocytic nevi (>100 melanocytic nevi or congenital nevus >20 cm)
- Dysplastic nevus syndrome
- Fair skin
- FH of melanoma
- Immunosuppression
- Male sex
- Obesity
- >50 yo
- Personal h/o melanoma
- UV radiation exposure
- Use of indoor tanning beds
Notes:
- Biopsy all suspicious pigmented lesions
- Full thickness excisional with 1-3 mm circumferential margins
- Deep scoop shave, saucerization, punch biopsy, or fusiform excision are preferred
| Breslow depth (thickness) | Margins |
|---|---|
| Melanoma in situ | 0.5-1cm |
| <1mm | 1 cm |
| 1-2mm | 1-2 cm |
| >2 mm | 2cm |
Reference:
- AFP Oct 2024 Vol 110 No 4
Milaria (Heat Rash) edit
Types:
- Miliaria crystalline:
- This condition is also known as sudamina, and it commonly affects neonates, with the highest incidence observed at 2 weeks of age or younger. The rash affects approximately 4.5% to 9% of neonates. However, it can also occur in adults who have recently relocated to a warmer climate.
- This condition appears as 1 to 2 mm superficial vesicles, affecting both adults and neonates, usually younger than 2 weeks old.[20]
- The pathophysiology involves the most superficial layer of the epidermis, the stratum corneum, resulting in vesicles with a thin superficial layer that resembles water droplets on the skin and easily ruptures.[11][21] As these vesicles are so superficial, an inflammatory response is typically absent.
- The most commonly affected areas are the upper trunk, neck, and head. The rash usually appears within a few days of exposure to risk factors and resolves within a day after the superficial layer of skin rubs off.[22]
- Miliaria rubra:
- This is the most common form of miliaria and is frequently observed in neonates between 1 and 3 weeks of age. This condition can also affect up to 30% of adults living in hot and humid conditions.
- This condition is the most prevalent form of miliaria and is characterized by the obstruction of eccrine ducts in the deeper layers of the skin, which triggers an inflammatory response. This leads to the formation of larger, erythematous papules and vesicles.
- A key clinical feature that helps differentiate miliaria rubra from folliculitis is the minimal involvement of hair follicles. When pustules are present, miliaria rubra is referred to as miliaria pustulosa, which may indicate a bacterial infection. Due to the inflammatory response, patients may experience pruritic and painful symptoms that can worsen during perspiration, leading to increased irritation.
- In neonates, typically between 1 and 3 weeks old, the groin, axilla, and neck are the most commonly affected areas.
- In adults, miliaria rubra is often seen in areas where clothing rubs against the skin, such as the trunk and extremities, while the face is usually spared. Superinfection with staphylococci can occur, and when associated with impetigo or multiple abscesses, the condition is known as periporitis staphylogenes.[23]
- Miliaria profunda:
- This is the rarest form of miliaria, most commonly seen in individuals with recurrent episodes of miliaria rubra or individuals exposed to new warm climates, such as military personnel deployed in tropical climates.
- Miliaria profunda results in large, firm, flesh-colored papules that are not centered around hair follicles due to their deeper involvement at the dermal-epidermal junction. The eruption can range from extremely pruritic to asymptomatic.
- This condition is often observed in patients with a history of multiple episodes of miliaria rubra.
- The rash typically affects the trunk in adults, but it may also involve the arms and legs. The rash usually appears within minutes to hours of sweating and resolves within an hour after sweating ceases.
Sweating is the most common risk factor, making hot or humid conditions and high fevers particularly associated with the development of miliaria.
Other causes of miliaria include:
- Occlusion of the skin: Transdermal drug patches and tight clothing have been associated with miliaria.
- Type I pseudohypoaldosteronism: This condition involves mineralocorticoid resistance, leading to sodium loss through eccrine glands, and has been associated with pustular miliaria rubra.
- Strenuous physical activity: Intense exercise can contribute to the development of miliaria.
- Morvan syndrome: A rare autosomal recessive disorder characterized by hyperhidrosis, among other abnormalities, which predisposes individuals to miliaria.
- Medications: Drugs that induce sweating, such as bethanechol, clonidine, and neostigmine, have been associated with miliaria.[11] Additionally, a few cases of isotretinoin-induced miliaria have been reported.
Treatment:
- Managing the condition involves implementing general measures to reduce sweating and prevent eccrine duct blockage.
- This includes creating cooler environments, wearing breathable clothing, exfoliating the skin, removing skin-occluding objects such as bandages or patches, and addressing febrile illnesses.
- Miliaria crystallina usually does not require treatment, as it is self-limiting and typically resolves within 24 hours.
- Miliaria rubra is managed by reducing inflammation; thus, mild-to-mid-potency corticosteroids, such as 0.1% triamcinolone cream, may be applied to the affected areas for 1 to 2 weeks.
- If miliaria pustulosa develops, topical antibiotics such as clindamycin are used to address the superimposed bacterial infection.
A heat rash is something that happens because there is a blockage of the sweat glands leading to backflow of the sweat into the skin. This happens oftentimes when it's hot and humid out.
The best treatment is trying to find ways to cool the skin and prevent further sweating.
Things you can try:
- staying in air conditioning
- wearing loose ,lightweight, and breathable clothing
- avoiding tight or scratchy fabrics
- taking cool baths
- Nonsedating anti-histamines like Claritin (loratadine)
Reference:
Molluscum
Nail Abnormalities
History:
- Dietary habits
- Nutritional deficiencies
- Duration of symptoms
- Acute vs Chronic
- Family history
- H/o skin or nail abnormalities or autoimmune conditions
- Hobbies
- Infections or toxic exposures
- Medical history
- Recent illnesses and other skin diseases
- Medications
- Nail care habits
- Nail polish, base/topcoat, strengtheners, hardeners, conditioners, cuticle treatment, instruments used, manicures, and artificial or gel nails
- Nails affected
- Single nail unit vs multiple; symmetry, looking for systemic conditions involving fingernails, toenails, or both
- Occupation
- Identify infections or toxic or traumatic exposures
Common Nail Abnormalities:
- Shape
- Clubbing
- Nails thicken and bend around fingertips
- CV, pulm, and inflammatory bowel diseases; liver abnm; malignancy
- Koilonychia
- Spoon nails
- Fe def, malnutrition, autoimmune d/o
- Clubbing
- Color
- Azure lunula
- Blue or silver tint
- Wilson disease or silver poisoning
- Leukonychia
- White nails
- Leukonychia punctata
- Small (1-3 mm) white spots in the nail plate
- Trauma
- Lindsay nails (half-and-half nail)
- Proximal half of the nail is normally ping, but distal half is brownish
- RA or renal d/o
- Longitudinal erythronychia
- Pink to red longitudinal streak in the nail plate that corresponds to a band of thinned, more transparent nail plate
- Benign or malignant nail tumors (single nail); lichen planus, systemic amyloidosis, sarcoidosis, hemiplegia, graft-v-host disease, acantholytic dermatosis, epidermolysis bullosa (mult nails)
- Longitudinal melanonychia
- Brown to black pigmentation of the nail
- Ethnic variation, benign lentigo/nevi, melanoma, subungal hematoma
- Longitudinal white lines
- Darier disease or Hailey-Hailey disease
- Mees lines (transverse leukonychia)
- White discoloration of the nail plate in bands or striae 1-2 mm wide that run parallel to the nail base
- Arsenic poisoning, Hodgkin disease, mycobacterial ailments, herpes zoster, kidney failure, CO poisoning
- Muehrcke lines
- Double white diagonal line
- Renal or hepatic d/w, malnourishment (hypoalbuminemia), medications
- Splinter hemorrhage
- Red to black, small, thin, longitudinal lines under the nail plate
- Trauma, psoriasis, infections, systemic diseases
- Telangiectasia
- Small, dilated blood vessels appear in the skin around the fingernail folds
- Scleroderma, dermatomyositis, SLE
- Terry nails
- Leukonychia that involves more than the proximal two-thirds of the nail plate, whereas the distal third appears red
- CHF, DM, hepatic disease, thyroid d/o
- Yellow nail
- Yellow nails
- Lymphedema, pleural effusion, lung d/o, infections
- Yellow nails
- Azure lunula
- Defects of nail plate/Nail shedding
- Onychocryptosis
- Ingrown nails
- Trauma, infection
- Onycholysis
- Nail plate moves away from the nail bed
- Psoriasis, thyroid d/o, nutritional deficiencies, infection, connective tissue d/o, sarcoidosis, amyloidosis
- Onychomadesis
- Detachment of a nail plate from the nail bed
- Infection, matrix injuries, severe systemic illness, medications
- Pincer nail
- Nail edges move closer together, compressing the nail bed
- Trauma, wearing tight shoes, autoimmune conditions
- Retronychia
- Incomplete nail shedding that leads to the embedding of the proximal nail plate into the proximal nail fold with subsequent inflammation (mostly great toe)
- Trauma
- Onychocryptosis
- Surface texture
- Beau lines
- Transverse grooves
- Systermic illness, drugs, trauma
- Longitudinal grooves
- Median nail dystrophy
- Onychorrhexis
- Split or brittle nails with a sequence of lengthwise striations
- Medications, dematoses, peripheral artery disease, Fe def anemia, endocrine d/o, environmental exposures (wet work exposures, trauma)
- Onychoschizia
- Lamellar exfoliation
- Psoriasis, Reiter syndrome, alopecia areata
- Pitting
- Pits in nail plate
- Psoriasis, Reiter syndrome, alopecia areata
- Ridges
- Horizontal or vertical
- Nutritional deficiencies, inflammatory skin conditions
- Trachyonychia
- Roughness, excessive longitudinal ridging, pitting, thicening of the cuticle, and distal brittleness
- 20 nail dystrophy
- Beau lines
Conditions:
- Infectious
- Herpetic whitlow
- Hemorrhagic and purpuric nail lesions
- Paronychia
- Inflammation of the nail bed associated with erythema, edema, and pain at the proximal nail folds
- Warts
- Nodules cause onycholysis or longitudinal grooves in the nail plate and splinter hemorrhages
- Herpetic whitlow
- Skin disorders
- Alopecia areata
- Trachyonychia, longitudinal grooves, leukonychia
- Atopic eczema
- Shiny nails, Beau lines (transverse grooves), speckling, paronychia
- Chronic dermatitis
- nail pitting, Beau lines
- Lichen planus
- Longitudinal grooves and fissures, progressive nail thinning, dorsal pterygium
- Psoriasis
- Nail pitting, onycholysis, subungual hyperkeratosis, brownish discoloration (oil stains), salmon-colored patches
- Scleroderma
- Trachyonychia, paronychia, splinter hemorrhages
- Systemic lupus erythematosus
- Red lunula, splinter hemorrhages
- Alopecia areata
- Tumors
- Bowen disease
- Paronychia, lack of nail growth, onycholysis
- Fibroma
- Smooth, firm, flesh-colored lumps that emerge from the nail folds
- Melanoma
- Brownish-yellow discoloration of the nail plate, subungual hyperkeratosis onychorrhexis
- Bowen disease
- Other
- Trachonychia
- Longitudinal ridging; thin, brittle nails; nail pitting; usually involves all 20 nails
- Yellow nail syndrome
- Yellowish nail discoloration
- Trachonychia
Reference:
- AFP Oct 2025 Vol 112 No 4
Nevus
The "ABCDE" rule describes the features of early melanoma. These features are:
- Asymmetry - The shape of one half does not match the other half.
- Border that is irregular - The edges are often ragged, notched, or blurred in outline. The pigment may spread into the surrounding skin.
- Color that is uneven - Shades of black, brown, and tan may be present. Areas of white, gray, red, pink, or blue may also be seen.
- Diameter - There is a change in size, usually an increase. Melanomas can be tiny, but most are larger than 6 millimeters wide (about 1/4 inch wide)
- Evolving - The mole has changed over the past few weeks or months.
- Funny Looking - Ugly Duckling
Reference:
- Daniel Jensen J, Elewski BE. The ABCDEF Rule: Combining the "ABCDE Rule" and the "Ugly Duckling Sign" in an Effort to Improve Patient Self-Screening Examinations. J Clin Aesthet Dermatol. 2015 Feb;8(2):15. PMID: 25741397; PMCID: PMC4345927.
- https://moles-melanoma-tool.cancer.gov/#/
Atypical Nevus Management
General information:
- Sun avoidance and protection
- Regular physician followup at least every 12 mo
- Screen family members
- Use diagnostic aids such as total body photography and dermoscopy
- Biopsy of suspicious lesions
- Instruct patients in self-examinations
Management:
- 2mm margins to avoid reexcision
- Re-excise with 2-5mm margins if there is involvement of margins
- If severe cytologic atypia, do a 5mm margin
References:
- AFP vol 78 No 6 Sep 2008
Nonscarring Hair Loss
Hair Cycle:
- 90% scalp hairs in anagen (growth) phase at any given time
- 10% scalp hairs in telogen (resting) or catagen (involution) phases
Evaluation Steps
- Is it scarring hair loss?
- Scarring presents with:
- pruritis
- pain
- erythema
- scale
- crust
- obliteration of follicular pore markings leading to an abnormally smooth appearance of the skin
- Scarring presents with:
- If nonscarring, what is the Distribution of loss?
- Patterned
- Ex: Androgenic alopecia
- Hairline recession, increased spacing between follicles, increased visibility of scalp, and miniturized follicles
- Most common patterned hair loss
- Minoxidil and finasteride
- Ex: Androgenic alopecia
- Diffuse
- Ex: Telogen Effluvium
- Most common diffuse hair loss
- An inciting event disrupts hair cycle leading to loss > 200 scalp hairs a day (Decrease hair volume >10% but <50%)
- Severe illness
- Major surgery
- Thyroid idsease
- Pregnancy
- Fe def anemia
- Malnutrition
- Rapid weight loss
- Vit D def
- Medications:
- Using: lithium, sodium valproate, fluoxetine, warfarin, metoprolol, propranolol, retinoids, isoniaxid
- Discontinuing: estrogen containing OCPs
- Occurs 2-4 months after inciting event
- Labs:
- TSH
- Ferritin
- 25-OH Vit D2 and D3
- Self-limited
- Takes 6-9 months to normalize
- Ex: Telogen Effluvium
- Focal
- Ex: Alopecia Areata
- Hair loss patches with smooth borders
- Autoimmune often in those with atopy
- Spontaneous regrowth in 30% patients
- Exclamation point hairs in active areas
- Pigmented hairs preferentially lost with regrowth initially nonpigmented or white
- Ex: Alopecia Areata
- Patterned
To investigate hair loss, several laboratory tests can be utilized to identify underlying causes. The following tests are commonly recommended:
- Complete Blood Count (CBC): This test helps to identify anemia, which can be a contributing factor to hair loss.
- Serum Ferritin: Low ferritin levels can indicate iron deficiency, which is associated with various forms of hair loss, including telogen effluvium and female pattern hair loss.
- Thyroid Stimulating Hormone (TSH): Thyroid dysfunction, both hypothyroidism and hyperthyroidism, can lead to hair loss, making TSH an essential test.
- Vitamin D 25OH: Vitamin D deficiency has been linked to hair loss, and assessing its levels can be beneficial.
- Zinc Levels: Although the evidence is mixed, some studies suggest that zinc deficiency may be associated with hair loss, particularly in non-scarring alopecia.
References:
- JAMA Mar 2021 Vol 325 No 9
OCP and Acne
Location of hormonal acne:
- While typical teenage acne appears most of the forehead and cheeks, the most common areas for hormonal acne to pop up are on the lower sections of the face, including around the mouth, jawline, and neck.
Hormone levels:
- As a rule of thumb, birth control that contains a higher level of progesterone will have a stronger androgenic effect and have a higher risk of promoting acne breakouts.
- The reduction of androgen production will reduce the blackheads, whiteheads, and inflamed red pimples typical to acne.
- The estrogen that is used in birth control pills is almost always Ethinyl estradiol and rarely mestranol. The usual amount is 20–50 µg.
Estrogen effect provides some anti-androgenic effect through 3 mechanisms:
- Suppress secretion of pituitary gonadotropins, inhibit ovulation, and thus inhibit androgen production by the ovaries.
- Block the Androgen receptors
- Increase the liver production of SHBG and reducing circulating testosterone.
Women with acne need to avoid taking progestins with potent androgenic (acne-causing) effects, i.e., levonorgestrel and norgestrel. A better choice of progestins for women with acne would be drospirenone, norgestimate, gestodene, and desogestrel with a weaker androgenic effect.
The best birth control pills for women with Acne are pills that contain drospirenone and Ethinylestradiol. Examples of these pills are
- Yasmin,
- Yaz,
- Beyaz,
- Ocella,
- Safyral,
- Syeda,
- Gianvi,
- Loryna,
- Nikki,
- Vestura, and
- Zarah.
Lo Loestrin was found to cause more acne breakouts. Several other contraceptive options exacerbate or trigger acne in some women as they are higher in progestin (i.e., they increase testosterone-like activity) and low in estrogen. These include Depo-Provera (a shot), Skyla, Lylema, Implanon, and Nexplanon (a subdermal implant).
Indications of hormonal treatment in acne
- Severe flare-ups before menstruation
- When oral contraception is desirable
- Acne not responding to conventional treatment
- Polycystic ovary syndrome
- Late onset acne (acne tarda)
- Ovarian or adrenal hyperandrogenism
Summary of treatment recommendations from the European acne guidelines
| Type of acne | First-line treatment | Second-line treatment | Third-line treatment | Hormonal alternatives for women |
|---|---|---|---|---|
| Comedonal acne | Topical retinoids, adapalene is preferred to tretinoin | Benzoyl peroxide (BPO) or azelaic acid | � | Not recommended |
| Mild to moderate papulopustular acne | BPO + adapalene (f.c.) or BPO + clindamycin (f.c.) | BPO or azelaic acid or systemic antibiotic + adapalene | Isotretinoin or tretinoin + topical erythromycin (f.c.); or systemic antibiotics + BPO; or systemic antibiotics + azelaic acid; systemic antibiotics + adapalene + BPO (f.c.) | Not recommended |
| Severe papulopustular acne and mild nodular acne | Systemic isotretinoin | Systemic antibiotics + adapalene; systemic antibiotics + azelaic acid; or systemic antibiotics + BPO + adapalene (f.c.) | Systemic antibiotics + BPO | Hormonal antiandrogens + topical treatment or systemic antibiotics (topical treatment is preferred) |
| Severe nodular acne and conglobate acne | Systemic isotretinoin | Systemic antibiotics + azelaic acid | Systemic antibiotics + BPO; or systemic antibiotics + adapalene; or systemic antibiotics + BPO + adapalene (f.c.) | Hormonal antiandrogens + systemic antibiotics (consider as third line treatment) |
Reference:
Onychomycosis
Confirmatory testing is generally unnecessary for clinically suspected onychomycosis.
- The most cost-effective approach to a patient with clinically suspected onychomycosis is empiric therapy with oral terbinafine.
- Chance of liver injury is 1:50,000 to 1:120,000
- If using a more expensive alternative medicine, than confirmatory testing with periodic acid-Schiff stain reduces cost
References:
- AFP Vol 97 No 9 May 2018
Paronychia
Treatment:
- Drainage
- Do not inject pulp and finger pad if using anesthesia
- Antibiotics (typically not needed after drainage)
Risk factors:
- Accidental trauma
- Artificial nails
- Manicures
- Manipulating hangnails
- Occupational trauma
- Onychocryptosis (ingrown nails)
- Onychophagia (nail biting)
Prevention:
- Apply moisturizing lotion after washing
- Avoid chronic prolonged exposure to contact irritants and moisture
- Avoid nail trauma, biting, picking, manipulation, and sucking
- Avoid trimming cuticles or using cuticle removers
- Improve glycemic control in those with DM
- Keep affected areas clean and dry
- Keep nails short
- Use rubber gloves, preferably with inner cotton glove or liner, when exposed to moisture and/or irritants
Differential Diagnosis:
- Eczema
- Herpetic whitlow
- Psoriasis
- Dermatomyositis
- Granuloma annulare
- Hematomas from pulse oximetry
- Pyogenic granuloma
- Reiter syndrome
- Food hypersensitivity
- Melanoma
- Pemphigus vulgaris
- Squamous cell carcinoma
References:
- AFP Vol 96 No 1 Jul 2017
Perioral dermatitis
- Unknown etiology but flouronated topical corticosteroids, subclinical irritant contact dermatitis, and overmoisturization of skin implicated.
- F > M
- Discrete, symmetric pinpoint papules and pustules but not on vermillion border - might have erythematous base.
- Treatment
- Wean any topical steroids
- First line: Oral tetracycline (II) (250mg bid-tid for several weeks)
- Second line: Oral erythromycin (III)
- Third line: Topical metronidazole (I) with or without above Abx
References:
- Cheung M, Taher M, Lauzon G., Acneiform facial eruptions, Canadian Fam Phys, Vol 51; April 2005; 527-533
Pigmentation Disorders
Hyperpigmentation
- Postinflammatory hyperpigmentation (acne, psoriasis, atopic and contact dermatitis, lichen planus, trauma, drugs, and fixed-drug eruptions)
- Irregular, darkly-pigmented macules or patches
- Melasma
- Progressive, macular, nonscaling hypermelanosis of sun-exposed areas of the skin, primarily on the face and dorsal forearms
- Solar lentigines
- macular, 1- to 3-cm, hyperpigmented, well-circumscribed lesions on sun-exposed surfaces of the skin
- Ephelides (freckles)
- small, 1- to 2-mm, sharply defined macular lesions of uniform color, most often found on the face, neck, chest, and arms
- Café-au-lait macules
- tan or brown macules ranging in size from 1 to 20 cm, which are present at birth or occur early in life
- Nevi
- Melanoma and precursors
Hypopigmentation
- Acquired (common)
- Vitiligo
- Unpigmented macules and patches, sharply defined, 5 to 50 mm, coalescent
- an immune-mediated destruction of melanocytes
- Pityriasis alba
- Tinea versicolor
- Postinflammatory hypopigmentation
- Vitiligo
- Congenital (uncommon)
- Albinism
- Piebaldism
- Tuberous sclerosis
- Hypomelanosis of Ito
| Hyperpigmentation Disorders | Description | Location | Etiology | Treatment |
|---|---|---|---|---|
| Postinflammatory hyperpigmentation | Irregular, darkly pigmented macules/patches | Previous sites of injury or inflammation | Trauma, inflammation | Triple combination therapy,† hydroquinone, retinoids, azelaic acid (Finacea), chemical peels, laser therapy |
| Melasma | Pigmented, well-defined macules; light brown, brown, or gray | Face (centrofacial 63%, malar 21%, mandibular 16%) or forearms | Pregnancy, oral contraceptives, phenytoin (Dilantin), idiopathic | Triple combination therapy,† chemical peels, light or laser therapy, sunscreen |
| Solar lentigines | 1- to 3-cm well-circumscribed macules; light yellow to dark brown, variegated | Face, hands, forearms, chest, back, shins | Acute or chronic ultraviolet exposure | Triple combination therapy† with or without cryotherapy, hydroquinone, retinoids, chemical peels, cryotherapy, intense pulsed light, laser therapy |
| Ephelides | 1- to 2-mm sharply defined macules, red or tan to light brown | Face, neck, chest, arms, legs | Childhood onset after sun exposure in susceptible individuals (skin types I or II) | Fades in winter months so treatment may be unnecessary; cryotherapy, hydroquinone, azelaic acid, chemical peels, laser therapy |
| Café au lait macules | 1- to 20-cm tan to brown macules, epidermal, present at birth or early childhood | Most commonly trunk but may appear anywhere | Increased melanin in melanocytes/basal keratinocytes | Laser therapy, surgical excision |
| Hypopigmentation disorders | Description | Location | Etiology | Treatment |
|---|---|---|---|---|
| Vitiligo | Hypopigmented macules and patches; sharply defined; 5 to 50 mm; coalescent | Face, hands, forearms, neck, genitalia, body folds, periorificial; lip-tip pattern | Unknown, possibly immune-mediated | High-potency topical corticosteroids (class II and III), topical calcineurin inhibitors, narrowband ultraviolet B, psoralen and ultraviolet A, systemic corticosteroids |
| Pityriasis alba | Hypopigmented, irregular patches; fine scale; itchy | Face, head, neck, forearms | Possible association with atopic dermatitis aggravated by sunlight exposure | Sunscreen, topical corticosteroids, tacrolimus (Protopic) ointment |
| Tinea versicolor | Hypopigmented or pink plaques; may be hyperpigmented; fine scale | Neck, chest, back, abdomen, proximal extremities | Malassezia spp. infection | Topical antifungals, topical adapalene (Differin) gel |
| Postinflammatory hypopigmentation | Loss of pigment (variable), macules, patches | Varies | Tinea versicolor, atopic dermatitis, pityriasis alba, psoriasis, guttate parapsoriasis, dermabrasion, chemical peels, intralesional corticosteroid use | Treatment of underlying condition when applicable |
Reference:
- AFP Vol 96 No 12 Dec 2017
- Am Fam Physician. 2009;79(2):109-116
Pruritis edit
Etiologies:
- Dermatologic
- Atopic dermatitis
- Contact dermatitis
- Lichen simplex chronicus
- Psoriasis
- Urticaria
- Xerosis
- Systemic
- Autoimmune disorders
- Chronic renal failure
- Drug induced
- Endocrine disorders
- Hematologic (polycythemia vera) and HIV infection
- Liver disease
- Lymphoproliferative disorders
- Malignancy
- Neurologic
- Brachioradial pruritis
- Multiple sclerosis
- Notalgia paresthetica
- Postherpetic neuralgia
- Poststroke
- Small-fiber polyneuropathy (DM one of most common causes)
- Psychogenic
- Anxiety
- Bipolar disorder
- Delusional infestation
- Depression
- Obsessive-compulsive disorders
- Mixed
- More than 1 cause found
- Other
Workup:
- Labs
- CBC - hematologic or malignancy suspected
- CMP - DM, liver, or renal disease suspected
- ESR - autoimmune disease suspected
- TSH - hyperthyroidism suspected
- Hepatitis panel
- HIV
- Imaging
- CXR - lymphoma suspected
- Spinal imaging (MRI) - secondary workup for brachioradial pruritis or notalgia paresthetica
Management:
- Non-Drug
- Warm (not hot) water for bathing
- Apply emollient to skin immediately after bathing
- Use hypoallergenic body products
- Humidify indoor spaces during winter
- Avoid fabrics and other clothing materials that irritate the skin (like wool - use cotton)
- Wear loose fitting clothes
- Avoid vasodilators (caffeine, alcohol, spices, and activities that promote excessive sweating like strenuous exercise)
- Drugs
- Antihistamines
- Nocturnal itch, paraneoplastic itch, systemic mastocytosis
- diphenhydramine 25-50 mg q4-6 prn
- hydroxyzine 25 mg tid or qid
- loratadine 10mg qd
- Anticonvulsants
- neuropathic itch, uremic itch
- gabapentin 100-300mg /d
- pregabalin 50-300 mg/d
- Antidepressants
- Cholestatic itch, nocturnal itch, paraneoplastic itch, pyschogenic itch, uremic itch
- sertraline 75-100mg qd
- paroxetine 20-40 mg qd
- amitriptyline 10-25 mg qd to tid
- doxepin 10mg qd or bid
- mirtazapine 15 mg qd
- Antipsychotics
- Delusion of infestation
- olanzapine 2.5-10 mg qd
- risperidone 1-8 mg qd
- Opioid-receptor agents
- Cholestatic itch, uremic itch
- naltrexone 50 mg qd
- Bile-acid sequestrants
- Cholestatic itch
- cholestyramine 4-6 mg tid - 30 min before meals
- ursodiol 13-15 mg/kg/d
- Antihistamines
References:
- JFP Nov 2020 Vol 69, No 9
Psoriasis
Medications that trigger:
- Lithium
- B-blockers
- Antimalarials
- Angiotensin-converting enzyme inhibitors
- NSAIDs
Treatment:
- Localized disease
- Topical corticosteroids LOE A for first line mild-mod
- Coal tar
- Vit D analogues
- Tazarotene
- Anthralin
- Localized UV light/laser
- Calcineurin inhibitors
- Extensive disease (Mod-Severe)
- Otezla
- UV light
- Methotrexate
- If used as initial systemic and 25% reduction in PSI after 4 weeks is not achieved, switch to another systemic - LOE B
- Retinoids
- Cyclosporine
- Apremilast
- Biologicals
- Tumore necrosis factor inhibitors
Scalp psoriasis
- Calcipotriene foam and calcipotriene/betamethasone gel for 4-12 weeks for mild-mod severity (LOE A)
Tools:
References:
- Consultant Feb 2016
- AFP Dec 2023 Vol 108 No 6
Seborrheic Dermatitis
Medications
- Antifungals
- Ketoconazole 2% cream
- Miconazole 2% cream
- Corticosteroids
- Hydrocortisone 2.5% cream
- Triamcinolone 0.025% cream
- Triamcinolone 0.1% cream or ointment
- Calcineurin inhibitors
- Tacrolimus 0.1% ointment
- Pimecrolimus 1% cream
- Phosphodiesterase-4 inhibitors
- Roflumilast 0.3% foam
Reference:
- AFP Vol 112 No 2 Aug 2025
Sebacceous Cysts
- Traditional wide excision
- Dissection and removal of the cyst completely from the surrounding tissue through an elliptical incision
- Gold standard of treatment
- More likely leads to significant scarring in comparison with minimal excision or punch biopsy
- Has almost no recurrence when the cyst wall is entirely removed
- Minimal excision and punch biopsy techniques produce minimal bleeding, have faster healing times, and produce less scarring.
- Shorter procedural time
- Slightly higher rates of recurrence
- The minimal incision technique:
- Involves kneading the lesion following injection of anesthetic and expressing the cyst contents through a 2- to 3-mm incision
- Following expulsion of the cyst contents, the loosened capsule is delivered through the small opening
- Closure with suture is optional
- Punch biopsy excision:
- Similar to the minimal excision technique except that the incision is made using a single-use disposable dermal punch following injection of lidocaine
- Expulsion of the cyst contents, with cyst wall, via lateral pressure is performed and occasionally followed by closure with one suture
Notes:
- Inflamed cysts should be allowed to convalesce prior to attempted removal
- Rarely are these cysts truly infected
- Inflammation is secondary to sebaceous cyst wall rupture with leakage of cyst contents
Reference:
- J Fam Pract. 2007 April;56(4):315-316
Skin Protection
Sunburn protection:
- Avoid outdoor activities during peak sun intensity (10 a.m. to 4 p.m.), even on cloudy days
- Wear protective clothing (e.g., long sleeves, long pants, wide-brim hats) during the day
- For patients at increased risk, consider clothing with a high UV protection factor (> 30)
- Use sunglasses that provide 100% UVA and UVB protection
- Use a broad-spectrum sunscreen with an SPF of at least 15
- Use a sunscreen that is water-resistant (40 to 80 minutes of protection in the water)
- Apply sunscreen to dry skin 15 to 30 minutes before exposure to the sun
- Reapply sunscreen every two hours or earlier when sweating, swimming, or towel-drying
- Discard any sunscreen older than three years
Insect repellent:
- Repellents with 20-50% DEET protect up to several hours
- DEET safe in 2nd and 3rd trimesters and children >2mo
- Citronella acceptable for brief exposure to nuisance mosquitoes but not recommended for disease carrying mosquitoes
- No evidence supports: electronic repellents, garlic, or B vit
- Permethrin highly effective against ticks, mosquitoes
- Best protection: combining permethrin clothing with DEET repellent
See also: Insect Repellents
References:
- AFP Vol 91 No 11 Jun 2015
- AFP Vol 101 No 8 Apr 2020
Skin Type Classification
| Skin type | Skin color | Characteristics |
|---|---|---|
| I | White; very fair; red or blond hair; blue eyes; freckles | Always burns, never tans |
| II | White; fair; red or blond hair; blue, hazel, or green eyes | Usually burns, tans with difficulty |
| III | Cream white; fair with any eye or hair color; very common | Sometimes mild burn, gradually tans |
| IV | Brown; typically Mediterranean skin | Rarely burns, tans with ease |
| V | Dark brown; Middle-Eastern skin types | Very rarely burns, tans very easily |
| VI | Black | Never burns, tans very easily |
Terminology
There are no universally agreed upon definitions of terms or, in particular, dimensions of primary lesions. The following was offered by Watt and Jillson as an "easy-to-remember" formula.
Primary Lesions
- Macule
- Circumscribed area of skin, up to 1.0 cm, with a change from normal skin color, which is neither raised above nor depressed below the surrounding skin. Many use the term for lesions much greater than 1.0 cm. Term does not include purpura
- Patch
- A flat, circumscribed, discoloration of skin or mucous membrane greater than 1.0 cm in diameter.
- Papule
- Discrete solid area of skin that is elevated by palpation above the surrounding skin and less than 1 cm in diameter. Variations include accuminate, keratotic, flat-topped, follicular, umbilicated, pedunculated, necrotitic and others
- Plaque
- Similar to a papule but greater that 1.0 cm in diameter. Often formed by the confluence or coalescence of papules. Secondary features may include, among others, atrophy, lichenification or hyperkeratosis.
- Nodule
- Discrete, solid, palpable, round or oval (elipsoidal) lesion of the skin measuring up to 1.0 cm in diameter (or long axis). Applies to processes involving any or all levels of the skin, and is a general term for any mass, benign or malignant.
- Tumor
- A term used by some for a "nodule" greater than 1.0 cm in diameter. Applies to processes involving any or all levels of the skin, and is a general term for any mass, benign or malignant.
- Vesicle
- A circumscribed fluid-filled lesion less than 1.0 cm in diameter that is usually elevated above the surrounding skin. May be described as solitary, grouped, umbilicated, dyshidrotic, spongiotic, multi-locular or uni-locular.
- Bulla
- A circumscribed fluid-filled lesion greater than 1.0 cm in diameter that is usually elevated above the surrounding skin. May attain diameters of several cms and are described as tense, or flacid.
- Pustule
- Discrete elevated vesicle or bulla of skin, usually small, containing purulent exudate composed of inflammatory leukocytes (pus), with or without cellular debris. May be superficial, deep-seated, follicular, grouped, etc. and may arise secondarily from a vesicle.
- Wheal
- An evanescent, round or irregular, often flat-topped elevation of skin with a pale red color, arising from edema in the superficial dermis. May vary from 2-3 mm to 10 or more cm in diameter, with round or arcuate configurations. Should be distinguished from angioedema, a massive edema involving the entire dermis and subcutaneous tissues.
Secondary Lesions
- Scar
- A hard plaque of dense fibrotic tissue covered by a thin epidermis. A mark of injury from any sort of process (physical or pathologic).
- Atrophy
- Atrophy usually refers to thinning of the epidermis leaving an easily wrinkled and/or shiny surface. Atrophy may also apply to dermal and/or subcutaneous tissue, with or without changes in the epidermis.
- Ulcer
- Loss of skin tissue or substance from the surface downward, leaving an uncovered or denuded wound that is slow to heal.
- Erosion
- A superficial denudation of the skin, usually implying the loss of the epidermis.
- Fissure
- A vertical splitting or separation of the skin.
- Crust
- Dried surface fluid, often serous (inspissated serum) in nature, with or without tissue debris. For purposes of this document this includes the term "scab".
- Excoriation
- A scratch mark, often with denudation of the skin to form a small ulcer. Exposure of the corium by mechanical removal of the epidermis.
- Scale
- A thin flake of epithelium (mostly composed of corneoctyes) which is separated from the underlying intact skin proper.
- Lichenification
- A thickening of the skin surface and an increase of skin markings, usually seen with chronic coalescence of papular lesions, especially atopic eczema.
- Vegetating
- A lushly growing, proliferating, process, usually with elevated or exophytic features.
- Linear / Figurate
- Technically not secondary features, but included here solely out of convenience. These are configurations that skin lesions may assume, which aid in their diagnostic identification. Figurate includes geometrical shapes (e.g. annular, arciform, cyclic, etc.).
Reference:
- Watt, T.L. and Jillson, O.F.: Archives of Dermatology 90:454, 1964.
Tinea Management Pitfalls
In summary, the best antifungal medications for tinea are:
- Topical terbinafine or butenafine for tinea corporis, tinea cruris, and tinea pedis.
- Oral terbinafine for extensive or refractory cases, and for tinea capitis caused by Trichophyton species.
- Oral griseofulvin for tinea capitis caused by Microsporum species.
Notes:
- Do not use nystatin to treat any tinea infection because dermatophytes are resistant to nystatin. (However, nystatin is often effective for cutaneous Candida infections.)
- Do not use oral ketoconazole to treat any tinea infection because of the U.S. Food and Drug Administration boxed warnings about hepatic toxicity and the availability of safer agents.
- Do not use griseofulvin to treat onychomycosis because terbinafine (Lamisil) is usually a better option based on its tolerability, high cure rate, and low cost.
- Do not use combination products such as betamethasone/clotrimazole because they can aggravate fungal infections.
- Do not use topical clotrimazole or miconazole to treat tinea because topical butenafine (Lotrimin Ultra) and topical terbinafine (OTC 1% cream) have better effectiveness and similar cost.
- Do not, in general, treat tinea capitis or onychomycosis without first confirming the diagnosis with a potassium hydroxide preparation, culture, or, for onychomycosis, a periodic acid–Schiff stain. However, kerion should be treated aggressively while awaiting test results, and it may be reasonable to treat a child with typical lesions of tinea capitis involving pruritus, scale, alopecia, and posterior auricular lymphadenopathy without confirmatory testing. If there is no lymphadenopathy, a confirmatory test is recommended.
- Do not treat tinea capitis solely with topical agents, but do combine oral therapy with sporicidal shampoos, such as selenium sulfide (Selsun) or ketoconazole.
- Do not perform potassium hydroxide preparations or cultures on asymptomatic household members of children with tinea capitis, but do consider empiric treatment with a sporicidal shampoo.
References:
- Rotta I, Ziegelmann PK, Otuki MF, et al. Efficacy of Topical Antifungals in the Treatment of Dermatophytosis: A Mixed-Treatment Comparison Meta-Analysis Involving 14 Treatments. JAMA Dermatology. 2013;149(3):341-9. https://doi.org/10.1001/jamadermatol.2013.1721.
- Ely JW, Rosenfeld S, Seabury Stone M. Diagnosis and Management of Tinea Infections. American Family Physician. 2014;90(10):702-10.
- Nenoff P, Krüger C, Paasch U, Ginter-Hanselmayer G. Mycology - An Update Part 3: Dermatomycoses: Topical and Systemic Therapy. Journal Der Deutschen Dermatologischen Gesellschaft = Journal of the German Society of Dermatology : JDDG. 2015;13(5):387-410; quiz 411. https://doi.org/10.1111/ddg.12689.
Topical Corticosteroids
Choosing Topical Corticosteroids
Principles:
- Ultra-high potency - use only <3wks
- Low-to-high potency - use <3mo
- Avoid combination steroids/antifungals (avoid adverse effects and tinea infections)
| Vehicle | Effect | Possible uses |
|---|---|---|
| Ointment | Emollient, higher potency | Lichen |
| Palms/Soles | ||
| Xerotic | ||
| Cream | Emollient | Moist and weeping areas |
| Lotion | Drying agent, spreads easily | Larger areas |
| Gels | Drying, nongreasy, nonstaining | Hairy areas or face |
| Solution | Drying agent, lower potency | Hairy or intertriginous areas |
| Body area | Fingertip units required for one application | Weight required for twice per day dosing for 30 days |
|---|---|---|
| Face and neck | 2.5 | 75 g |
| Front of trunk | 7 | 210 g |
| Back of trunk | 7 | 210 g |
| One arm | 3 | 90 g |
| One hand (front and back) | 1 | 30 g |
| One leg | 6 | 180 g |
| One foot | 2 | 60 g |
References:
- AFP Mar 2021 Vol 103 No 6
- Consultant Nov 2015
My Favorite topical steroids
| Potency | Medication | Class | Size |
|---|---|---|---|
| High | Triamcinolone acetonide 0.5% cream | III | 15g |
| Intermediate | Triamcinolone acetonide 0.1% cream | IV,V | 15g/30g |
| Triamcinolone acetonide 0.1% ointment | IV,V | 15g/30g | |
| Low | Hydrocortisone 2.5% cream | VII | 28.4g |
| Hydrocortisone 2.5% ointment | VII | 28.4g |
- Class 1: Clobetasol proprionate
- Class 2: Fluicinonide/desoximetasone
- Class 3: Betamethasone valerate/fluocinolone acetonide
- Class 4: Trimacinolone acetonide/mometasone furoate
- Class 5: Hydrocortisone valerate
- Class 6: Desonide
- Class 7: OTC hydrocortisone
Skin Conditions Responsive to Topical Corticosteroid Treatment
High-potency steroids (groups I and II)
- Alopecia areata
- Atopic dermatitis (resistant)
- Bullous pemphigoid
- Discoid lupus
- Dyshidrotic eczema
- Hyperkeratotic eczema
- Labial adhesion
- Lichen planus
- Lichen sclerosus (skin)
- Lichen simplex chronicus
- Melasma
- Nummular eczema
- Poison ivy (severe)
- Psoriasis Vitiligo
Medium-potency steroids (groups III, IV, and V)
- Anal inflammation (severe)
- Asteatotic eczema
- Atopic dermatitis
- Dermatitis (severe)
- Infantile acropustulosis
- Intertrigo (severe, short term)
- Lichen sclerosus (vulva)
- Nummular eczema
- Scabies (after scabicide)
- Seborrheic dermatitis
- Stasis dermatitis
Low-potency steroids (groups VI and VII)
- Dermatitis (diaper)
- Dermatitis (eyelids)
- Dermatitis (face)
- Intertrigo
- Perianal inflammation
- Phimosis
Strength in vehicle ranked strongest to weakest:
- Ointment
- Cream
- Lotion
- Solution
Avoid face/genitalia with higher potency steroids
References:
- AFP Mar 2021 Vol 103 No 6
- Consultant Nov 2015
Adverse Effects of Topical Corticosteroids
- Cutaneous effects
- Atrophic changes
- Easy bruising
- Increased fragility
- Purpura
- Stellate pseudoscars
- Steroid atrophy
- Striae
- Telangiectasias
- Ulceration
- Infections
- Aggravation of cutaneous infection
- Granuloma gluteale infantum
- Masked infection (tinea incognito)
- Secondary infections
- Miscellaneous
- Contact dermatitis
- Delayed wound healing
- Hyperpigmentation
- Hypertrichosis (hirsutism)
- Hypopigmentation
- Perioral dermatitis
- Photosensitization
- Reactivation of Kaposi sarcoma
- Rebound flare-up
- Steroid-induced acne
- Steroid-induced rosacea
- Ocular changes
- Cataracts
- Glaucoma
- Ocular hypertension
- Atrophic changes
- Systemic effects
- Endocrine
- Cushing syndrome
- Hypothalamic-pituitary-adrenal suppression
- Metabolic
- Aseptic necrosis of the femoral head
- Decreased growth rate
- Hyperglycemia
- Renal/electrolyte
- Hypertension
- Hypocalcemia
- Peripheral edema
- Endocrine
References:
- AFP Mar 2021 Vol 103 No 6
Xanthoma edit
The most common location for a xanthoma is around the inner or outer areas of the eyelids, where they tend to occur in clusters; this particular type of xanthoma is called a "xanthelasma." Xanthomas are also often seen around joints (especially on the elbows or knees), in the creases of the palms and fingers, on the feet and on the buttocks. Tendinous xanthomas are usually located within tendons that travel along the backs of the hands and arms, the tops of the feet or within the Achilles tendon on the heel. Xanthomas may be tiny little bumps, but they also can grow to be as big as three inches in diameter. Xanthomas occur when you have very high levels of fats (lipids) in your bloodstream, especially [URL="http://cholesterol.about.com/cs/cholesteroltypes/g/LDL.htm"] low-density lipoprotein cholesterol[/URL] (LDL-C). LDL levels are often elevated in people who eat a high-fat, low-fiber diet; are overweight; and do not get sufficient exercise. Other factors that may increase LDL-C include: [LIST][*]Diabetes[*]Inherited [URL="http://cholesterol.about.com/od/hyperlipidemia/g/familialhyperch.htm"] familial hypercholesterolemia[/URL] (a genetic condition which causes high cholesterol beginning in childhood)[*]Low thyroid levels (hypothyroidism)[*]Kidney problems[*]Liver problems[*]Pregnancy[*]Medications, including some antiseizure drugs, diuretics, steroids, cyclosporine and retinoid drugs[/LIST] Your doctor may diagnose a xanthoma simply by noticing its characteristic appearance. If there is any question, a sample of the growth (biopsy) can be sent to a laboratory for closer examination. If it is a xanthoma, the results of the biopsy will show that the growth is composed of lipids (fats). Xanthomas can be removed in several different ways. They can be destroyed with acetic acid, via electrical current (electrodessication), by laser treatment or by cutting them out surgically. They may, however, eventually grow back, and it is also possible that additional xanthomas will crop up in other locations. Cosmetic concerns may convince you to have a xanthoma removed, but even more important than its removal, is your attention to the high blood cholesterol that caused it in the first place. Your doctor will want to do a complete lipid panel to track your blood cholesterol and [URL="http://cholesterol.about.com/cs/aboutcholesterol/g/Triglyceride.htm"] triglyceride[/URL] levels. A lipid panel or profile is a set of blood tests that measures blood levels of triglycerides as well as the major forms of cholesterol (total cholesterol, high density lipoprotein cholesterol or [URL="http://cholesterol.about.com/cs/cholesteroltypes/g/HDL.htm"] HDL[/URL] and low density lipoprotein cholesterol or LDL). You will usually be asked to fast (consume nothing but water) for 12 to 14 hours before you have your blood drawn for a lipid panel. Generally speaking, you should aim for a total cholesterol of more than 200 mg/dL, for LDL cholesterol less than 129 mg/dL, for HDL cholesterol more than 40 mg/dL for men or 50 mg/dL for women and for triglycerides less than 150 mg/dL.
Read more: http://www.city-data.com/forum/health-wellness/600511-white-spots-above-eye-lids-anyone-6.html
Wood's Light edit
- Hold the Wood's lamp 4 to 5 inches away from the surface of the skin
| Condition Or Use | Association | Wood'S Lamp Finding | Source Of Fluorescence |
|---|---|---|---|
| Bacterial infections | |||
| Cellulitis after burns, subungual infection, and interdigital infection | Pseudomonas aeruginosa | Green | Pyoverdine |
| Erythrasma | Corynebacterium minutissimum | Coral-red | Coproporphyrin III |
| Trichomycosis axillaris | Corynebacterium tenuis and other diphtheroids | Pale yellow | Unknown, possibly gluelike concretions |
| Progressive macular hypomelanosis | Cutibacterium acnes | Orange-red color in pilosebaceous follicles | Coproporphyrin III |
| Fungal infections | |||
| Dermatophytosis* | Microsporum audouinii | Blue-green | Pteridine |
| Microsporum canis | Yellow-green | Tryptophan metabolites | |
| Microsporum ferrugineum | Yellow-green | Tryptophan metabolites | |
| Trichophyton schoenleinii | Dull blue | – | |
| Pityriasis versicolor | Malassezia globosa | Yellow-orange | Pityrialactone |
| Hypopigmented conditions | |||
| Vitiligo | - | Blue-white | Lack of melanin |
| Nevus depigmentosus | - | Dull, off-white | Decrease in melanin |
| Tuberous sclerosis | - | White ash-leaf macule | Decrease in melanin |
| Linear scleroderma/ morphea | - | Blue-white | Decrease in melanin |
| Melasma | - | Epidermal: Brown or black, Dermal: Grey-blue | Increase in melanin |
| Metabolic disorders | |||
| Congenital erythropoietic porphyria | Uroporphyrinogen III synthase defect | Pink to red | Uroporphyrin I and coproporphyrin I in urine, blood, and enamel |
| Porphyria cutanea tarda | Autosomal dominant or acquired uroporphyrinogen decarboxylase defect | Pink to red | Uroporphyrin I and III in urine; few case reports cite fluorescence of skin or enamel |
| Hepatoerythropoietic porphyria | Autosomal recessive uroporphyrinogen decarboxylase defect | Pink to red | Uroporphyrin I and III in urine, blood, and ename |
| Erythropoietic protoporphyria | Ferrochelatase defect | Pink to red | Protoporphyrin IX in blood |
| Miscellaneous conditions | |||
| Solar urticaria | – | Erythema and urticaria | – |
| Milia | – | Bright yellow | Keratin in dermis |
| Annular dermatoses/ neoplasms | Granuloma annulare | Blue-black at the center, red on the edges | Keratin |
| Lichen planus annulari | Blue-black without a ring structure | ||
| Porokeratosis | Blue-brown at the center and white on the edge | ||
| Skin cancer margins | |||
| Lentigo maligna melanoma | – | Dark brown and black; Blue-white | Melanin, Loss of melanin in areas of regression |
| Basal cell carcinoma with in-vivo photodiagnosis | – | Coral-red | Methyl aminolevulinate (MAL) cream |
| Cosmetic applications | |||
| Administering chemical peels | Salicylic acid Fluorescein sodium | Green Yellow/orange | Salicylic acid Fluorescein sodium |
| Sunscreen application | - | Blue-white | Sunscreen |
| Tetracycline compliance | - | Yellow | Tetracycline |
| Dihydroxyacetone application | - | Salmon | DHA |
Wood's lamp is often used to make a diagnosis of the following skin disorders:
- Disorders of pigmentation like melasma, vitiligo
- Pityriasis Versicolor presents as a rash on the chest or back - the rash will emit an orange glow.
- Tinea capitis will reveal areas of baldness, and the Microsporum species will fluoresce blue-green - however, many other fungal infections may not fluoresce with Wood's lamp
- Scabies and head lice
- Erythrasma is caused by Corynebacterium, which presents as a coral red pigmented rash in the skin folds
- Pseudomonas, which will fluoresce green
The electromagnetic spectrum comprises a range of energy that radiates, or travels in waves. Arranged within this spectrum are seven energies: radio, microwave, infrared, visible, ultraviolet, X-ray, and gamma. Radio waves have the lowest energy and longest wavelengths, whereas gamma rays have the highest energy and shortest wavelengths. Perceptible by the human retina, visible light has a narrow range from 700nm (red) to 400nm (violet). Slightly more energetic, and invisible, is ultraviolet light. It is in this part of the electromagnetic spectrum that Wood's lamp emits light, from 320nm to 400nm, with a peak wavelength of 365nm.
When the relatively energetic and short waves of UV light shine on certain substances, known as phosphors, visible light of lower energy and longer wavelength is produced (Figure 1). This is known as fluorescence. Thus, phosphors essentially convert invisible UV light to visible light.
A Wood's lamp is also used to look for signs of porphyria in erythrocytes, stool, and urine. Sometimes beauticians may assess for skin imperfections and signs of aging with a Wood's lamp. When a slit lamp is unavailable, the ophthalmologist may use the Wood lamp to search for scratches and foreign bodies in the cornea.
Physicians often use the wood lamp to examine for fungal, bacterial, and parasitic infections.
The Wood lamp is safe and does not damage the skin or cause sunburn. The examination is usually very brief and unlikely to cause harm even to light-sensitive individuals. The recommendation is for patients to close their eyes when during exposure to a Wood's lamp
Reference:
- Dyer JM, Foy VM. Revealing The Unseen: A Review of Wood's Lamp in Dermatology. J Clin Aesthet Dermatol. 2022 Jun;15(6):25-30. PMID: 35783566; PMCID: PMC9239119.
- Al Aboud DM, Gossman W. Wood's Light. [Updated 2023 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537193/
Drugs/Medications/Supplements
Adverse Effects: 10 Most Commonly Filled Prescription Medications in 2019
Drug Name/Adverse Effects
- Levothyroxine
- Vomiting, dysgeusia (< 1%)
- Lisinopril
- Dysgeusia (≥ 1%), Stevens-Johnson syndrome (≥ 1%), toxic epidermal necrolysis (≥ 1%), xerostomia (≥ 1%), angioedema (< 1%)
- Atorvastatin (Lipitor)
- Anaphylaxis (< 1%), angioedema (< 1%), dysgeusia (< 1%), erythema multiforme (< 1%), hypoesthesia/paresthesia (< 1%), Stevens-Johnson syndrome (< 1%), toxic epidermal necrolysis (< 1%), vomiting (< 1%)
- Metformin
- Infection (21%), nausea and vomiting (7% to 26%), taste disorder (1% to 10%)
- Amlodipine (Norvasc)
- Angioedema (< 1%), dysphagia (< 1%), erythema multiforme (< 1%), gingival enlargement (< 1%), hypersensitivity reaction (< 1%), hypoesthesia/paresthesia (< 1%), increased thirst (< 1%), vomiting (< 1%), xerostomia (< 1%)
- Metoprolol
- Xerostomia (1%), vomiting (frequency undefined), paresthesia (< 1%), taste disorder (< 1%)
- Omeprazole (Prilosec)
- Vomiting (3%), acid regurgitation (2%), allergic reactions/anaphylaxis/hypersensitivity reaction (< 1%), angioedema (< 1%), dysgeusia (< 1%), erythema multiforme (< 1%), Stevens-Johnson syndrome (< 1%), tongue mucosal atrophy (< 1%), toxic epidermal necrolysis (< 1%), xerostomia (< 1%)
- Simvastatin (Zocor)
- Anaphylaxis (< 1%), angioedema (< 1%), dry mucous membranes (< 1%), dysgeusia (< 1%), erythema multiforme (< 1%), hypersensitivity reaction (< 1%), paresthesia (< 1%), Stevens-Johnson syndrome (< 1%), toxic epidermal necrolysis (< 1%), vomiting (< 1%)
- Losartan (Cozaar)
- Paresthesia (< 2%), vomiting (< 2%), anaphylaxis (< 1%), angioedema (< 1%), dysgeusia (< 1%), lip edema (< 1%), tongue edema (< 1%)
- Albuterol
- Application site reaction (6%), oropharyngeal pain (≤ 5%), unpleasant taste at inhalation site (4%), vomiting (3% to 7%), hypersensitivity reaction (3% to 6%), glossitis (< 3%), infection (< 3%), oropharyngeal edema (< 3%), xerostomia (< 3%), anaphylaxis (< 1%), angioedema (< 1%), dysgeusia (< 1%), oropharyngeal irritation (< 1%), tongue ulcer (< 1%)
References:
- AFP Nov 2020 Vol 102 No 10
Adverse Effects: Opioids
See also:
Opioid adverse effects:
- constipation and intestinal blockages
- sleep-disordered breathing
- fractures
- hypothalamic-pituitary-adrenal dysregulation
- decrease of gonadotropin-releasing hormone
- males: as hypogonadism, also known as opiate-induced androgen deficiency, sexual dysfunction, infertility, fatigue, and decreased levels of testosterone
- Women: Decreased circulating levels of estrogen, low follicle-stimulating hormone, and increased prolactin can lead to osteoporosis, oligomenorrhea, and galactorrhea
- these side effects are reversible with cessation of treatment or lower dosing
- decrease of gonadotropin-releasing hormone
- overdose
- respiratory depression
- bradycardia
- hypotension
- addiction
- Dizziness and sedation
- Depression
- higher levels of comorbid clinical depression of up to 38%
- Mortality
- long-term opioid treatment is associated with an 87% increase in all-cause mortality
Overdose:
- Among persons on higher opioid doses, the risk of opioid overdose was estimated to be 1.8% per year of opioid use.
- Additionally, 12% of identified overdoses were fatal, suggesting an annual fatal overdose risk of about 2 per 1,000 per year among patients on higher-dose opioid regimens.
- These estimates are consistent with Centers for Disease Control and Prevention mortality surveillance data on deaths from drug overdose, which now roughly equal motor vehicle accidents as a leading cause of death among 35–54 year olds.
| Medical Risk | How Common? | Description and Information |
|---|---|---|
| Respiratory depression | ||
| Opioid overdose | < 1% per year | Caused by severely slowed breathing, which you may not notice |
| Severe cases are treated in the hospital | ||
| Can cause death | ||
| Breathing problems during sleep | 25% | Can cause or worsen sleep apnea |
| You may not notice breathing problems | ||
| Falls and fractures | ||
| Falls causing hip and pelvis fractures | 1%–2% per year | … |
| Gastrointestinal | ||
| Constipation | 30%–40% | It helps to use stool softeners or medicines that stimulate bowel movements |
| Serious intestinal blockage | < 1% per year | Caused by severe constipation |
| Severe cases are treated in the hospital | ||
| Hormonal effects | ||
| Hypogonadism, impotence, infertility, osteoporosis | 25%–75% | Hypogonadism = lowered sex hormones, which can worsen sexual function |
| Osteoporosis can make you more likely to fracture or break a bone | ||
| Cognitive and neurophysiologic effects | ||
| Sedation | 15% | Can cause difficulty driving and thinking clearly |
| Disruption of sleep | 25% | |
| Hyperalgesia | Not known | Hyperalgesia = being more sensitive to pain |
| Psychosocial | ||
| Depression, anxiety, deactivation, apathy | 30%–40% | Can cause loss of interest in usual activities, which can lead to depression; depression can worsen pain, just as pain can worsen depression |
| Addiction, misuse, and diversion | 5%–30% | Misuse or overdose can occur if others, including children and teens, gain access to the medicine; your pharmacist can tell you how to dispose of unused medicines safely |
| Other | ||
| Dry mouth that may cause tooth decay | 25% | Brush your teeth and rinse your mouth often |
| Chew sugarless gum and drink water or sugar-free, noncarbonated fluids | ||
| Myoclonus | Not known | Myoclonus = muscle twitching |
Common side effects of opioid administration include:
- sedation
- dizziness
- nausea
- vomiting
- constipation
- physical dependence
- tolerance
- respiratory depression
- Physical dependence and addiction
Less common side effects may include:
- delayed gastric emptying
- hyperalgesia
- immunologic and hormonal dysfunction
- muscle rigidity
- myoclonus
The most common side effects of opioid usage are:
- constipation (which has a very high incidence)
- nausea
Reference:
- Baldini A, Von Korff M, Lin EH. A Review of Potential Adverse Effects of Long-Term Opioid Therapy: A Practitioner's Guide. Prim Care Companion CNS Disord. 2012;14(3):PCC.11m01326. doi: 10.4088/PCC.11m01326. Epub 2012 Jun 14. PMID: 23106029; PMCID: PMC3466038.
- Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, Sehgal N, Glaser SE, Vallejo R. Opioid complications and side effects. Pain Physician. 2008 Mar;11(2 Suppl):S105-20. PMID: 18443635.
Alcohol Use
The major indirect biomarkers are:
- LFTs: aspartate and alanine aminotransferase (AST and ALT)
- Gamma-glutamyl transferase (GGT)
- Mean Corpuscular Volume (MCV)
- Carbohydrate-Deficient Transferrin (CDT).
| Indirect Biomarkers | Sen/Sp | Time to return to normal | Notes |
|---|---|---|---|
| GGT | 41-73 / 63-85 | 2-6 weeks | |
| AST | 47-68 / 80-95 | 1 wk | |
| SLT | 32-50 / 87-92 | 1wk | |
| MCV | 40-50 / 80-90 | Unknown - T1/2 40d | Elevated indicate excessive drinking |
| CDT | 63-84 / 92-98 | 2-4 wk | Most accurate in middle aged white men, better sensitivity in men, combine with GGT and CDT to increase sensitivity in women |
| Alcohol | 100 / 100 | 6-12 h after last drink |
Reference:
- JFP Dec 2021 Vol 70 No 10
Study: Association Between Daily Alcohol Intake and Risk of All-Cause Mortality edit
Key Points
- What is the association between mean daily alcohol intake and all-cause mortality?
- Findings
- This systematic review and meta-analysis of 107 cohort studies involving more than 4.8 million participants found
- no significant reductions in risk of all-cause mortality for drinkers who drank less than 25 g of ethanol per day (about 2 Canadian standard drinks compared with lifetime nondrinkers) after adjustment for key study characteristics such as median age and sex of study cohorts.
- There was a significantly increased risk of all-cause mortality among female drinkers who drank 25 or more grams per day and among male drinkers who drank 45 or more grams per day.
- This systematic review and meta-analysis of 107 cohort studies involving more than 4.8 million participants found
- Meaning
- Low-volume alcohol drinking was not associated with protection against death from all causes.
Abstract
Importance
- A previous meta-analysis of the association between alcohol use and all-cause mortality found no statistically significant reductions in mortality risk at low levels of consumption compared with lifetime nondrinkers. However, the risk estimates may have been affected by the number and quality of studies then available, especially those for women and younger cohorts.
Objective
- To investigate the association between alcohol use and all-cause mortality, and how sources of bias may change results.
- Data Sources
A systematic search of PubMed and Web of Science was performed to identify studies published between January 1980 and July 2021.
Study Selection
- Cohort studies were identified by systematic review to facilitate comparisons of studies with and without some degree of controls for biases affecting distinctions between abstainers and drinkers. The review identified 107 studies of alcohol use and all-cause mortality published from 1980 to July 2021.
Data Extraction and Synthesis
- Mixed linear regression models were used to model relative risks, first pooled for all studies and then stratified by cohort median age (<56 vs ≥56 years) and sex (male vs female). Data were analyzed from September 2021 to August 2022.
Main Outcomes and Measures
- Relative risk estimates for the association between mean daily alcohol intake and all-cause mortality.
Results
- There were 724 risk estimates of all-cause mortality due to alcohol intake from the 107 cohort studies (4,838,825 participants and 425,564 deaths available) for the analysis.
- In models adjusting for potential confounding effects of sampling variation, former drinker bias, and other prespecified study-level quality criteria, the meta-analysis of all 107 included studies found no significantly reduced risk of all-cause mortality among occasional (>0 to <1.3 g of ethanol per day; relative risk [RR], 0.96; 95% CI, 0.86-1.06; P = .41) or low-volume drinkers (1.3-24.0 g per day; RR, 0.93; P = .07) compared with lifetime nondrinkers.
- In the fully adjusted model, there was a nonsignificantly increased risk of all-cause mortality among drinkers who drank 25 to 44 g per day (RR, 1.05; P = .28) and significantly increased risk for drinkers who drank 45 to 64 and 65 or more grams per day (RR, 1.19 and 1.35; P < .001).
- There were significantly larger risks of mortality among female drinkers compared with female lifetime nondrinkers (RR, 1.22; P = .03).
Conclusions and Relevance
- In this updated systematic review and meta-analysis, daily low or moderate alcohol intake was not significantly associated with all-cause mortality risk, while increased risk was evident at higher consumption levels, starting at lower levels for women than men.
Reference:
- Zhao J, Stockwell T, Naimi T, Churchill S, Clay J, Sherk A. Association Between Daily Alcohol Intake and Risk of All-Cause Mortality: A Systematic Review and Meta-analyses. JAMA Netw Open. 2023;6(3):e236185. https://doi.org/10.1001/jamanetworkopen.2023.6185
Study: Health and cancer risks associated with low levels of alcohol consumption
BLUF:
- Alcohol causes 7 types of cancers:
- Breast cancers
- Colon and rectum
- Esophagus
- Liver
- Mouth
- Pharynx
- Larynx
- Light to moderate consumption accounts for 13.3% of all alcohol attributable cancers
- Half of these cancers are female breast cancer
—
The overall risks and harms resulting from alcohol consumption have been systematically assessed and are well documented. According to the latest WHO estimates, alcohol consumption contributed to 3 million deaths in 2016 globally and was responsible for 5.1% of the global burden of disease and injury. Alcohol consumption is associated with an increased risk of many health conditions and is the main and sufficient cause for several disorders, including alcohol dependence, liver cirrhosis, and several other non-communicable diseases and mental health conditions. Alcohol use is among the leading risk factors for premature mortality and disability because of its causal relationship with multiple health conditions, which also include non-intentional injuries and suicides. Younger people are disproportionately affected by alcohol compared with older people, and 13.5% of all deaths among those aged 20–39 years are attributed to alcohol. Disadvantaged and vulnerable populations have increased rates of alcohol-related death and hospitalisation.
Alcohol, as classified by the International Agency for Research on Cancer, is a toxic, psychoactive, and dependence-producing substance and a Group 1 carcinogen that is causally linked to seven types of cancer, including oesophagus, liver, colorectal, and breast cancers. Alcohol consumption is associated with 740,000 new cancer cases each year globally.
In the EU, light to moderate alcohol consumption (<20 g of pure alcohol per day, which is equivalent to consumption of approximately <1.5 L of wine [12% alcohol by volume; ABV], <3.5 L of beer [5% ABV], or <450 mL of spirits [40% ABV] per week) was associated with almost 23,000 new cancer cases in 2017, accounting for 13.3% of all alcohol-attributable cancers and for 2.3% of all cases of the seven alcohol-related cancer types. Almost half of these cancers (approximately 11,000 cases) were female breast cancers. Also, more than a third of the cancer cases attributed to light to moderate drinking (approximately 8,500 cases) were associated with a light drinking level (<10 g per day).
Increasing levels of alcohol use are associated with increasing levels of risk of illness and mortality, leading to the question of whether a safe level of alcohol consumption that is associated with zero risk of health consequences can be defined. To identify a safe level of alcohol consumption, scientific evidence is required to show the absence of increased risk of illness or injury associated with alcohol consumption at and below that level. Some, but not all, studies have suggested that light alcohol consumption could have a small protective effect, as measured by the risk of some cardiovascular diseases or type 2 diabetes. Some studies show the existence of such effects on certain types of cardiovascular diseases in middle-aged and older people. However, several reviews also found that the protective effects of moderate consumption disappear with heavy episodic drinking, which increases the risk of any cardiovascular diseases.
No studies have shown that the potential existence of a protective effect for cardiovascular diseases or type 2 diabetes also reduces the risk of cancer for an individual consumer. Evidence does not indicate the existence of a particular threshold at which the carcinogenic effects of alcohol start to manifest in the human body. As such, no safe amount of alcohol consumption for cancers and health can be established. Alcohol consumers should be objectively informed about the risks of cancer and other health conditions associated with alcohol consumption.
Reference:
- Anderson BO, Berdzuli N, Ilbawi A, Kestel D, Kluge HP, Krech R, Mikkelsen B, Neufeld M, Poznyak V, Rekve D, Slama S, Tello J, Ferreira-Borges C. Health and cancer risks associated with low levels of alcohol consumption. Lancet Public Health. 2023 Jan;8(1):e6-e7. doi: 10.1016/S2468-2667(22)00317-6. PMID: 36603913; PMCID: PMC9831798.
Antidepressants
Antidepressants and Sexual Function
- Patients treated with selective serotonin reuptake inhibitors (SSRIs) and the serotonin/norepinephrine reuptake inhibitor (SNRI) venlafaxine have significantly higher rates of overall sexual dysfunction—includingdesire, arousal, and orgasm—than patients treated with placebo (strength of recommendation [SOR]: B, randomized controlled trials [RCTs] with heterogeneous results).
- Patients treated with bupropion, a norepinephrine-dopamine reuptake inhibitor (NDRI), have rates of overall sexual dysfunction comparable to placebo (SOR: B, RCTs with heterogeneous results).
- Total rate of sexual dysfunction (SD) associated with selective serotonin reuptake inhibitors (SSRIs) was significantly higher than the placebo rate of 14.2%.
- The SSRIs citalopram, fluoxetine, paroxetine, and sertraline as well as the SNRI venlafaxine, had significantly greater rates (70%-80%) of reported total sexual dysfunction, including desire, arousal, and orgasm, than placebo.
- Paroxetine, citalopram, and venlafaxine, when compared with other antidepressants (fluoxetine, fluvoxamine, nefazodone, sertraline), generally were associated with more reports of SD, specifically complaints of erectile dysfunction in men and decreased vaginal lubrication in women.
- The number needed to treat one additional person with general sexual functioning satisfaction was 6 (95% CI, 4-9) with bupropion.
References:
- J Fam Pract. 2013 November;62(11):660-661.
Antidepressants and Weight edit
| Drug | Effect On Weight |
|---|---|
| Monoamine oxidase inhibitors | Weight gain likely in short term (< 6 months) and long term (≥ 1 year) |
| (irreversible type) | |
| Tricyclic compounds | Weight gain likely in short term and long term |
| Selective serotonin reuptake inhibitors (SSRIs) other than paroxetine | Weight gain in short term less likely |
| Weight gain in long term possible, but evidence is varied | |
| Paroxetine | Weight gain in short and long term more likely than for other SSRIs |
| Nefazodone | Likely to have no effect on weight |
| Bupropion | Likely to cause weight loss |
| Mirtazapine | More likely than placebo to cause weight gain in short term, but less likely than tricyclics |
| Venlafaxine | Likely to have no effect on weight |
Addition of another agent such as a stimulant (methylphenidate, amphetamines), an H2 receptor antagonist (famotidine), triiodothyronine, topiramate, bupropion, or naltrexone may help diminish weight gain.1,37 Although none has been tested systematically, low doses have been prescribed along with an antidepressant in an effort to avoid weight gain associated with antidepressant therapy. In our practice, we have found that adding low-dose bupropion (100 to 150 mg/day) or topiramate (25 to 50 mg/day) may help weight loss when used in addition to diet control and exercise
| Mode or medication | Weight loss produced | Duration of treatment |
|---|---|---|
| Behaviour modification | 0.5–0.7 kg per week | — |
| Cognitive-behavioral therapy | 4.5 drop in BMI | — |
| Naltreoxone and buropion | 4% | — |
| Phentermine and topiramate | 9% | 1 year |
| Sibutramine | 10–15% | <1 year |
| Orlistat | 10.2%, 8.8% | 1 year |
| Orlistat | >10% | 2 years |
| Orlistat | 34.6% | ? |
| Amantadine | 3.5 kg | 3–6 months |
| Nizatidine | Gained 3 kg less than patients who did not take Nizatidine | 16 weeks |
| Naltexone | 5 kg | 8 weeks |
| Topiramate augmentation | 10–15 lbs | — |
| Metformin | 15/19 patients lost weight | 12 weeks |
Besides diet and exercise, formal behavior modification techniques involve changing eating habits and reinforcing desired weight controlling behavior. It is the gradual but consistent change in behavior that leads to healthier eating habits. Simple use of portion control behaviors can teach patients to eat less at every meal without the complexity of counting fat versus carbohydrate calories, and does not require the willpower to follow a bland low-salt, low-fat, low-sugar diet [75]. Behavior modification alone can generate a weight loss of 0.5 kg to 0.7 kg per week [76]. Through formal, manualized cognitive-behavioral therapy patients can achieve satisfaction with body image and acceptance of modest weight loss. In one study, the effects of cognitive-behavioral therapy on weight gain due to psychotropics was studied in 6 schizophrenia patients (mean age 37.3 years). The mean BMI (kg/m2) decreased from 29.6 kg to 25.1 kg in the posttreatment group [77]. Cognitive therapy has been helpful in reducing weight for children and adolescents [78]. Furthermore, the addition of cognitive therapy to a diet-controlled method produces better results [79].
Reference:
- Deshmukh R, Franco K. Managing weight gain as a side effect of antidepressant therapy. Cleve Clin J Med. 2003 Jul;70(7):614, 616, 618, passim. doi: 10.3949/ccjm.70.7.614. PMID: 12882383.
- Nihalani N, Schwartz TL, Siddiqui UA, Megna JL. Weight gain, obesity, and psychotropic prescribing. J Obes. 2011;2011:893629. doi: 10.1155/2011/893629. Epub 2011 Jan 17. PMID: 21318056; PMCID: PMC3034985.
Study: Initial Severity and Antidepressant Benefits: A Meta-Analysis of Data Submitted to the Food and Drug Administration
Background
- Meta-analyses of antidepressant medications have reported only modest benefits over placebo treatment, and when unpublished trial data are included, the benefit falls below accepted criteria for clinical significance. Yet, the efficacy of the antidepressants may also depend on the severity of initial depression scores. The purpose of this analysis is to establish the relation of baseline severity and antidepressant efficacy using a relevant dataset of published and unpublished clinical trials.
Methods and Findings
- We obtained data on all clinical trials submitted to the US Food and Drug Administration (FDA) for the licensing of the four new-generation antidepressants for which full datasets were available. We then used meta-analytic techniques to assess linear and quadratic effects of initial severity on improvement scores for drug and placebo groups and on drug–placebo difference scores. Drug–placebo differences increased as a function of initial severity, rising from virtually no difference at moderate levels of initial depression to a relatively small difference for patients with very severe depression, reaching conventional criteria for clinical significance only for patients at the upper end of the very severely depressed category.
- Meta-regression analyses indicated that the relation of baseline severity and improvement was curvilinear in drug groups and showed a strong, negative linear component in placebo groups.
Conclusions
- Drug–placebo differences in antidepressant efficacy increase as a function of baseline severity, but are relatively small even for severely depressed patients.
- The relationship between initial severity and antidepressant efficacy is attributable to decreased responsiveness to placebo among very severely depressed patients, rather than to increased responsiveness to medication.
- Kirsch and colleagues show that, in antidepressant trials, there is a greater difference in efficacy between drug and placebo amongst more severely depressed patients. However, this difference seems to result from a poorer response to placebo amongst more depressed patients.
Reference:
- Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLoS Med. 2008 Feb;5(2):e45. doi: 10.1371/journal.pmed.0050045. PMID: 18303940; PMCID: PMC2253608.
Study: The loss of efficacy of fluoxetine in pediatric depression: explanations, lack of acknowledgment, and implications for other treatments
Key findings
- The efficacy of fluoxetine for pediatric depression has lost clinical significance.
- What this adds to what is known?
- This has not been adequately addressed in guidelines of major medical organizations.
- The novelty bias and expectancy effects may explain the loss of estimated efficacy.
- What is the implication and what should change now?
- Recommending fluoxetine as a first-line treatment is at odds with the evidence.
- This may create challenges for clinical practice that deserve further elaboration.
Objectives
- Fluoxetine is among the most used antidepressants for children and adolescents and frequently recommended as first-line pharmacological treatment for pediatric depression. However, in contrast to earlier studies and reviews, a Cochrane network meta-analysis from 2021 concluded that the estimated efficacy of fluoxetine was no longer clinically meaningful. We aimed to explain the discrepant findings between the recent Cochrane review and earlier reviews, and to explore if this was acknowledged in guidelines and treatment recommendations appearing since then.
Study Design and Setting
- Meta-analytical aggregation of trial results over time, exploring potential biases, and a nonsystematic search for recent treatment guidelines/recommendations from major medical organizations.
Results
- The estimated efficacy of fluoxetine in clinical trials declined over time into the range of clinical equivalence with placebo when more recent studies were included in analyses and when considering common thresholds of clinical significance.
- This remains unacknowledged in treatment guidelines and related publications, including some that continue to recommend fluoxetine as first-line pharmacological treatment.
- Finally, we find that the loss of efficacy over time is likely explained by biases such as the novelty bias or by variations of expectancy effects.
Conclusion
- The seeming lack of clinically meaningful efficacy of fluoxetine for the treatment of pediatric depression needs to be considered by those who develop treatment recommendations as well as by patients and clinicians.
- The biases we observed are not only relevant in the evaluation of fluoxetine and other antidepressants for pediatric depression, but also for any new treatment.
Reference:
- Plöderl, Martin et al. The loss of efficacy of fluoxetine in pediatric depression: explanations, lack of acknowledgment, and implications for other treatments Journal of Clinical Epidemiology, Volume 0, Issue 0, 112016
Ashwagandha
Evidence:
- Research shows that some ashwagandha preparations may be effective for insomnia and stress. However, evidence is unclear about its effects on anxiety.
- There is some limited evidence that suggests that taking ashwagandha for 2 to 4 months may increase testosterone levels and sperm quality.
- There isn't enough evidence to determine if ashwagandha is helpful for any other health conditions, such as asthma, athletic performance, cognitive function, diabetes, menopause, and female infertility.
- There is not enough high-quality evidence suggesting that ashwagandha is helpful in treating COVID-19.
Cautions:
- Ashwagandha may be safe when taken in the short term (up to 3 months). There is not enough information to allow conclusions about its long-term safety to be reached.
- In some individuals, ashwagandha preparations may cause drowsiness, stomach upset, diarrhea, and vomiting.
- Although it is rare, there have been a number of cases that link liver injury to ashwagandha supplements.
- Ashwagandha should be avoided during pregnancy and should not be used while breastfeeding.
- Ashwagandha is not recommended for people who are about to have surgery, or for those who have autoimmune or thyroid disorders.
- There is evidence that ashwagandha might interact with some medications, including those for diabetes and high blood pressure, medicines that decrease the immune system response (immunosuppressants), sedatives, anti-seizure medications (anticonvulsants), and thyroid hormone medications.
- Because ashwagandha may increase testosterone levels, people with hormone-sensitive prostate cancer should avoid its use.
Ashwagandha may not be safe:
- during pregnancy
- while breastfeeding
- if you have prostate cancer, thyroid problems, or an autoimmune condition
- if you are about to have surgery
- if you have liver problems
- if you are taking benzodiazepines or other medications
Efficacy:
- It appears that ashwagandha may be effective for:
- insomnia
- stress
- Evidence is unclear if it is effective with anxiety.
- There isn't enough evidence for efficacy in any other health conditions, including asthma, athletic performance, cognitive function, diabetes, menopause, and female infertility.
Notes:
- It is safe to take up to 3 months. Long term safety is not clear.
- In some, it may cause drowsiness, stomach upset, diarrhea, and vomiting.
- It can interact with some medications as well
Reference:
- https://www.nccih.nih.gov/health/ashwagandha
- https://www.mskcc.org/cancer-care/integrative-medicine/herbs/ashwagandha
- Verma N, Gupta SK, Tiwari S, Mishra AK. Safety of Ashwagandha Root Extract: A Randomized, Placebo-Controlled, study in Healthy Volunteers. Complement Ther Med. 2021 Mar;57:102642. doi: 10.1016/j.ctim.2020.102642. Epub 2020 Dec 15. PMID: 33338583.
Auvelity Notes
- Star-D trial
- auvelity
Auvelity
- Savings Card: https://www.auvelity.com/savings-card
- $10 for 2 months
- Needs PA - After 2-3 failures in FL
- Send to specialty pharmacy:
- To treat MDD (some evidence for Anxiety and ADHD)
- https://www.auvelityhcp.com/
- Rep: Tom
ADVERSE REACTIONS
- Most common adverse reactions (≥5% and twice the rate of placebo): dizziness (16%), headache (8%), diarrhea (7%), somnolence (7%), dry mouth (6%), sexual dysfunction (6%), and hyperhidrosis (5%).
USE IN SPECIFIC POPULATIONS
- Lactation: Because of the potential for neurotoxicity, advise patients that breast-feeding is not recommended during treatment with Auvelity and for 5 days following final dose.
- Renal Impairment: Dosage adjustment is recommended in patients with moderate renal impairment (eGFR 30 to 59 mL/minute/1.73 m2). Auvelity is not recommended in patients with severe renal impairment (eGFR 15 to 29 mL/minute/1.73 m2).
- Hepatic Impairment: Auvelity is not recommended in patients with severe hepatic impairment.
HOW TO TAKE
- Auvelity is available by prescription only.
- Take Auvelity exactly as instructed by your HCP.
- Take Auvelity 1 time a day for 3 days, then increase your dose to 2 times a day (taken at least 8 hours apart). Do not take more than 2 Auvelity tablets in 24 hours.
- If you miss a dose, do not take an extra dose. Wait and take your next dose at the regular time. Do not take more than 1 dose of Auvelity at a time.
- Do not change your dose or stop taking Auvelity without talking to your HCP.
- Swallow Auvelity tablets whole. Do not crush, chew, or divide the tablets.
- Do not give Auvelity to other people.
- If you take too much Auvelity call your HCP or seek medical advice promptly.
Contraindications:
- have or had a seizure disorder.
- have or had an eating disorder like anorexia or bulimia.
- have recently and suddenly stopped drinking alcohol or use medicines called benzodiazepines, barbiturates, or anti-seizure medicines, and you have recently suddenly stopped taking them.
- are taking a monoamine oxidase inhibitor (MAOI), have stopped taking an MAOI in the last 14 days, or are being treated with the antibiotic linezolid or intravenous methylene blue. Ask your HCP or pharmacist if you are unsure whether you take an MAOI. Do not start taking an MAOI until you have stopped taking Auvelity for at least 14 days.
- are allergic to dextromethorphan, bupropion, or any other ingredients in Auvelity.
Interactions:
- other medicines containing bupropion or dextromethorphan
- medicines to treat depression, anxiety, psychotic or thought disorders, including selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants
- theophylline
- corticosteroids
- oral diabetes medicines or use insulin to control your blood sugar
- medicines to control appetite (anorectic)
- nicotine medicines to help you stop smoking
- street (illicit) drugs
- benzodiazepines, sedative-hypnotic (sleep medicines), or opiates
Efficacy and Safety of AXS-05 (Dextromethorphan-Bupropion) in Patients With Major Depressive Disorder: A Phase 3 Randomized Clinical Trial (GEMINI)
Objective:
- Altered glutamatergic neurotransmission has been implicated in the pathogenesis of depression. This trial evaluated the efficacy and safety of AXS-05 (dextromethorphan-bupropion), an oral N-methyl-D-aspartate (NMDA) receptor antagonist and σ1 receptor agonist, in the treatment of major depressive disorder (MDD).
Methods:
- This double-blind, phase 3 trial, was conducted between June 2019 and December 2019.
- Patients with a DSM-5 diagnosis of MDD were randomized in a 1:1 ratio to receive dextromethorphan-bupropion (45 mg-105 mg tablet) or placebo, orally (once daily for days 1-3, twice daily thereafter) for 6 weeks.
- The primary endpoint was the change from baseline to week 6 in the Montgomery-Asberg Depression Rating Scale (MADRS) total score.
- Other efficacy endpoints and variables included MADRS changes from baseline at week 1 and 2, clinical remission (MADRS score ≤ 10), clinical response (≥ 50% reduction in MADRS score from baseline), clinician- and patient-rated global assessments, Quick Inventory of Depressive Symptomatology-Self-Rated, Sheehan Disability Scale, and quality of life measures.
Results:
- A total of 327 patients were randomized: 163 patients to dextromethorphan-bupropion and 164 patients to placebo.
- Mean baseline MADRS total scores were 33.6 and 33.2 in the dextromethorphan-bupropion and placebo groups, respectively. The least-squares mean change from baseline to week 6 in MADRS total score was -15.9 points in the dextromethorphan-bupropion group and -12.0 points in the placebo group (least-squares mean difference, -3.87; 95% confidence interval [CI], -1.39 to -6.36; P = .002).
- Dextromethorphan-bupropion was superior to placebo for MADRS improvement at all time points including week 1 (P = .007) and week 2 (P < .001).
- Remission was achieved by 39.5% of patients with dextromethorphan-bupropion versus 17.3% with placebo (treatment difference, 22.2; 95% CI, 11.7 to 32.7; P < .001), and clinical response by 54.0% versus 34.0%, respectively (treatment difference, 20.0%; 95% CI, 8.4%, 31.6%; P < .001), at week 6.
- Results for most secondary endpoints were significantly better with dextromethorphan-bupropion than with placebo at almost all time points (eg, CGI-S least-squares mean difference at week 6, -0.48; 95% CI, -0.48 to -0.79; P = .002). The most common adverse events in the dextromethorphan-bupropion group were dizziness, nausea, headache, somnolence, and dry mouth. Dextromethorphan-bupropion was not associated with psychotomimetic effects, weight gain, or increased sexual dysfunction.
Conclusions:
- In this phase 3 trial in patients with MDD, treatment with dextromethorphan-bupropion (AXS-05) resulted in significant improvements in depressive symptoms compared to placebo starting 1 week after treatment initiation and was generally well tolerated.
Reference:
- Iosifescu DV, Jones A, O'Gorman C, Streicher C, Feliz S, Fava M, Tabuteau H. Efficacy and Safety of AXS-05 (Dextromethorphan-Bupropion) in Patients With Major Depressive Disorder: A Phase 3 Randomized Clinical Trial (GEMINI). J Clin Psychiatry. 2022 May 30;83(4):21m14345. doi: 10.4088/JCP.21m14345. PMID: 35649167.
- https://www.psychiatrist.com/jcp/depression/efficacy-safety-of-axs-05-dextromethorphan-bupropion-mdd/
Benzodiazepines edit
FDA-approved Benzodiazepines and Dosage Recommendations:
- Alprazolam: Alprazolam is indicated for anxiety disorders and panic disorders, including agoraphobia.
- For generalized anxiety disorder, initiate treatment with a dose of 0.25 mg to 0.5 mg three times daily. The dose of alprazolam may be increased at intervals of 3 to 4 days to a daily dose of 4 mg.
- For panic disorders, a 1-4 mg daily dose is used. Use the minimal effective clinical dose due to the potential for dependence.
- Chlordiazepoxide: Chlordiazepoxide is primarily indicated for the management of alcohol withdrawal syndrome.
- For alcohol withdrawal syndrome, the suggested initial dose is 50 to 100 mg, followed by repeated doses of up to 300 mg per day as needed. Adjust the dose according to CIWA-Ar protocol.
- Clobazam: Clobazam is indicated for seizures associated with Lennox-Gastaut syndrome.
- For Lennox-Gastaut syndrome, an adjunct to antiepileptic drugs, the initial dose is 10 mg for patients weighing more than 30 kg. The dose is increased to 20 mg after one week. The usual maintenance dose after two weeks is 40 mg. In patients with a weight <30 kg, the dose should be reduced to half the recommended dose mentioned above. Study findings indicate that patients with seizure improvement on starting dosages of 10 to 20 mg/day of clobazam may have better seizure control even if the dosage is increased beyond the maximum recommended dosage of 40 mg/day.
- Clonazepam: Clonazepam is indicated for treating panic disorder and agoraphobia.[3] It is also indicated for the treatment of myoclonic seizures and absence seizures.
- The initial dose for adults with panic disorder is 0.5 mg daily. The maintenance dose for most patients of 1 mg per day.
- 0.5 mg is given thrice daily for seizure disorders, and the maximum recommended daily dose is 20 mg.
- Clorazepate: Clorzapte is used for adjunct treatment of short-term management of anxiety disorders. It is also indicated for focal (partial) onset seizures.
- The initial dose in patients with focal (partial) onset seizures in patients over 12 years is 7.5 mg three times a day. The maximum recommended dose is 90 mg/day.
- Diazepam: Diazepam is used for alcohol withdrawal management, Rectal diazepam is also indicated for treating febrile seizures.
- ASAM 2020 guidelines recommend front-loading for patients experiencing severe alcohol withdrawal (e.g., CIWA-Ar ≥ 19). A withdrawal symptom severity scale guides a front-loading regimen (e.g., 10 mg diazepam orally every hour if CIWA-Ar score ≥10) or according to a fixed schedule (e.g., 20 mg diazepam orally every 2 hours for three doses).[12]
- The recommended dose of diazepam (rectal) for febrile seizures is 0.5 mg/kg.[8][21]
- Estazolam: According to the American Academy of Sleep Medicine, estazolam is indicated for the treatment of insomnia.
- According to AASM, the dose of estazolam for sleep onset and sleep maintenance insomnia is 1 to 2 mg at bedtime.
- Flurazepam: Flurazepam is indicated for the treatment of insomnia.
- Flurazepam is indicated for the treatment of insomnia. The recommended dose of flurazepam is 15 mg for women and 30 mg for men.
- Lorazepam: Lorazepam is used for anxiety disorders. According to American Epilepsy Society guidelines, parenteral lorazepam is one of the first-line treatments for convulsive status epilepticus.
- According to AES guidelines, IV lorazepam(0.1 mg/kg) is administered as an initial dose for convulsive status epilepticus; the maximum recommended dose is 4 mg. The dose may be repeated at 3 to 5 minutes.
- Midazolam: Midazolam is indicated for convulsive status epilepticus and procedural sedation. Midazolam is used for sedation in mechanically ventilated patients in the MICU/SICU.
- Midazolam is administered 10 mg IM for convulsive status epilepticus as a single dose. Midazolam is preferred for patients without IV access. Intranasal midazolam (0.2 mg/kg, maximum dose, 10 mg) can be used in prehospital settings. (AES guidelines). For procedural sedation in patients< 60 years of age, 0.5 to 2.5 mg IV should be administered slowly over at least 2 minutes. Clinicians should fully evaluate the sedative effect before administering another dose. In MICU/SICU, midazolam is used as an alternative agent for sedation in mechanically ventilated patients. An intermittent dosing strategy is preferred to avoid drug accumulation. It is administered with a RASS goal of 0 to -2.
- Oxazepam: Oxazepam is indicated for anxiety disorders, and according to the ASAM (American Society of Addiction Medicine) guidelines, oxazepam is indicated for alcohol withdrawal syndrome.
- For alcohol withdrawal syndrome, oxazepam is administered with a symptom-triggered dosing approach. For CIWA-Ar scores between 8 to 15, 15 mg oxazepam is administered and 30 mg oxazepam is given for CIWA-Ar >15).(ASAM 2020 guidelines).
- Quazepam: According to the American College of Physicians, quazepam is indicated mainly for treating chronic insomnia in adults.
- Quazepam is suggested as an alternative drug for sleep onset and sleep maintenance insomnia. The recommended dose is 7.5 mg once daily at bedtime. The dose of quazepam can be increased to 15 mg, but the drug has a long half-life; hence there is a concern regarding accumulation and daytime impairment.
- Temazepam: American Academy of Sleep Medicine (AASM) clinical practice guideline suggests temazepam for sleep onset and sleep maintenance insomnia.
- AASM Clinical Practice Guideline recommends temazepam for sleep onset and sleep maintenance insomnia. The recommended dose is 7.5 to 15 mg once daily at bedtime.
- Temazepam improves total sleep time, decreases sleep latency, and improves sleep quality. According to the ACP (American College of Physicians) guidelines, all patients with chronic insomnia should receive cognitive behavioral therapy as the initial treatment intervention.
- Triazolam: Triazolam is indicated primarily for sleep-onset insomnia.
- Triazolam is indicated primarily for sleep-onset insomnia. The recommended dose is 0.125 to 0.25 mg once daily at bedtime. Limit the use to 4 to 8 weeks.
- Remimazolam: Remimazolam was approved by the FDA in 2020 and is indicated for short(<30 mins) procedural sedation in adults
- Remimazolam was approved by the FDA in 2020 and is indicated for short (<30 mins) procedural sedation in adults. For procedural sedation in adult patients, administer 5 mg IV remimazolam over 1 minute. To maintain procedural sedation, administer 2.5 mg IV (as needed) over 15 seconds. For induction, in ASA( American Society of Anesthesiologists) class III and IV patients, administer 2.5 mg to 5 mg IV over 1 minute based on the clinical condition. To maintain procedural sedation in ASA class III and IV patients, administer 1.25 mg to 2.5 mg intravenously as needed over 15 seconds. Wait for at least 2 minutes before administration of an additional dose.
Common adverse effects of benzodiazepine administration include, but are not limited to:
- Respiratory depression
- Respiratory arrest
- Drowsiness
- Confusion
- Headache
- Syncope
- Nausea/vomiting
- Diarrhea
- Tremor
Concomitant use of benzodiazepines with opioids can lead to sedation, severe respiratory depression, coma, and death.
Reference:
- Bounds CG, Nelson VL. Benzodiazepines. [Updated 2023 Jan 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470159/
- https://www.ncbi.nlm.nih.gov/books/NBK470159/
Bupropion
- The medication is FDA-approved for adult depression, seasonal affective disorder, and smoking cessation.
- Off-label, non-FDA-approved uses include:
- Anti-depressant-induced sexual dysfunction
- Attention-deficit/hyperactivity disorder (ADHD)
- Depression associated with bipolar disorder
- Obesity
- In the pediatric population, bupropion is used off-label for ADHD
Reference:
Caffeine
| Beverage | Serving Size (oz) | Caffeine (mg) |
|---|---|---|
| Decaffeinated coffee | 8 | 2 |
| Starbucks Grande Coffee | 16 | 330 |
| Starbucks Caffee Latte | 16 | 150 |
| Plain, brewed coffee | 8 | 95 |
| Espresso | 1 | 64 |
| Decaffeinated tea | 8 | 2 |
| Black tea, brewed | 8 | 47 |
| Snapple iced tea | 16 | 18 |
| Diet Mountain Dew | 12 | 55 |
| Diet Coke | 12 | 46 |
| Diet Pepsi | 12 | 37 |
| Sam's Diet Cola | 12 | 13 |
| SoBe Adrenaline Rush | 16 | 152 |
| Red Bull | 8.3 | 76 |
Reference:
- JFP Vol 58 No 6 Jun 2009
CAM with evidence
- Fish oil - hypertriglyceridemia - SOR B
- GI complaints; may interact with anticoagulant meds; may increase risk of prostate ca
- Glucosamine - osteoarthritis - SOR B
- Mild GI effects, drowsiness, skin reactions, HA; use with caution in shellfish allergy; may increase warfarin effects
- Probiotics - Preventing antibiotic associated diarrhea - SOR B
- Flatulence, vomiting, rash, CP, increased phlegm; contraindicated in immunosuppressed or indwelling medical device
- Soy - Hyperlipidemia - SOR C
- GI effects; may increase risk of endometrial hyperplasia; use with caution in pts with thyroid dysfunction or hormone sensitive ca
- St John's Wort - Depression - SOR B
- Photosensitivity, GI effects, fatigue, increased risk cataracts. Not preg/lact; may interact with antidepressants, OCPs, cyclosporine, digoxin, indinavir, phenytoin, phenobarbital, warfarin, and more
- Guided imagery - mood, pain, anxiety - SOR A
- AE: None
- Acupuncture - back, neck, shoulder pain; Osteoarthritis, HA - SOR B
- Infection, skin irritation, hematoma, pneumothorax
- Yoga - low back pain - SOR C
- AE: None
References:
- JFP Vol 63, No 10 Oct 2014
Cannabis/Marijuana
Cannabis and Adolescents
Adolescents with a history of cannabis use have at least a 50% increase in the odds of developing suicidality in adulthood. (SOR: B, large meta-analysis of cohort studies consistent with an additional cohort and cross-sectional twin study.)
- 50% increase in the odds of suicidal ideation (three studies; n = 8,479; OR = 1.5; 95% CI, 1.1 to 2.0)
- More than a 3x increase in the odds of a suicide attempt (three studies; n = 13,687; OR = 3.4; 95% CI, 1.5 to 7.8)
Reference:
- Am Fam Physician. 2024;109(4):369-370
Study: Association of Cannabis Use With Cardiovascular Outcomes Among US Adults
Background
- We examined the association between cannabis use and cardiovascular outcomes among the general population, among never-tobacco smokers, and among younger individuals.
Methods and Results
- This is a population-based, cross-sectional study of 2016 to 2020 data from the Behavioral Risk Factor Surveillance Survey from 27 American states and 2 territories. We assessed the association of cannabis use (number of days of cannabis use in the past 30 days) with self-reported cardiovascular outcomes (coronary heart disease, myocardial infarction, stroke, and a composite measure of all 3) in multivariable regression models, adjusting for tobacco use and other characteristics in adults 18 to 74 years old.
- We repeated this analysis among nontobacco smokers, and among men <55 years old and women <65 years old who are at risk of premature cardiovascular disease.
- Among the 434,104 respondents, the prevalence of daily and nondaily cannabis use was 4% and 7.1%, respectively.
- The adjusted odds ratio (aOR) for the association of daily cannabis use and coronary heart disease, myocardial infarction, stroke, and the composite outcome (coronary heart disease, myocardial infarction, and stroke) was 1.16 (95% CI, 0.98–1.38), 1.25 (95% CI, 1.07–1.46), 1.42 (95% CI, 1.20–1.68), and 1.28 (95% CI, 1.13–1.44), respectively, with proportionally lower log odds for days of use between 0 and 30 days per month.
- Among never-tobacco smokers, daily cannabis use was also associated with myocardial infarction (aOR, 1.49 [95% CI, 1.03–2.15]), stroke (aOR, 2.16 [95% CI, 1.43–3.25]), and the composite of coronary heart disease, myocardial infarction, and stroke (aOR, 1.77 [95% CI, 1.31–2.40]).
- Relationships between cannabis use and cardiovascular outcomes were similar for men <55 years old and women <65 years old.
Conclusions
- Cannabis use is associated with adverse cardiovascular outcomes, with heavier use (more days per month) associated with higher odds of adverse outcomes.
Reference:
- Jeffers AM, Glantz S, Byers AL, Keyhani S. Association of Cannabis Use With Cardiovascular Outcomes Among US Adults. J Am Heart Assoc. 2024 Mar 5;13(5):e030178. doi: 10.1161/JAHA.123.030178. Epub 2024 Feb 28. PMID: 38415581; PMCID: PMC10944074.
- https://www.ahajournals.org/doi/10.1161/JAHA.123.030178#d1e3229
Study: Brain Function Outcomes of Recent and Lifetime Cannabis Use
Key Points
- Question
- Are recent cannabis use and lifetime cannabis use associated with differences in brain function during cognitive tasks?
- Findings
- In this cross-sectional study of 1003 young adults, heavy lifetime cannabis use was associated with lower brain activation during a working memory task; this association remained after removing individuals with recent cannabis use.
- These results were not explained by differences in demographic variables, age at first cannabis use, alcohol use, or nicotine use.
- Meaning
- These findings suggest that cannabis use is associated with short- and long-term brain function outcomes, especially during working memory tasks.
Abstract
Importance
- Cannabis use has increased globally, but its effects on brain function are not fully known, highlighting the need to better determine recent and long-term brain activation outcomes of cannabis use.
Objective
- To examine the association of lifetime history of heavy cannabis use and recent cannabis use with brain activation across a range of brain functions in a large sample of young adults in the US.
Design, Setting, and Participants
- This cross-sectional study used data (2017 release) from the Human Connectome Project (collected between August 2012 and 2015). Young adults (aged 22-36 years) with magnetic resonance imaging (MRI), urine toxicology, and cannabis use data were included in the analysis. Data were analyzed from January 31 to July 30, 2024.
Exposures
- History of heavy cannabis use was assessed using the Semi-Structured Assessment for the Genetics of Alcoholism, with variables for lifetime history and diagnosis of cannabis dependence. Individuals were grouped as heavy lifetime cannabis users if they had greater than 1000 uses, as moderate users if they had 10 to 999 uses, and as nonusers if they had fewer than 10 uses. Participants provided urine samples on the day of scanning to assess recent use. Diagnosis of cannabis dependence (per Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria) was also included.
Main Outcomes and Measures
- Brain activation was assessed during each of the 7 tasks administered during the functional MRI session (working memory, reward, emotion, language, motor, relational assessment, and theory of mind). Mean activation from regions associated with the primary contrast for each task was used. The primary analysis was a linear mixed-effects regression model (one model per task) examining the association of lifetime cannabis and recent cannabis use on the mean brain activation value.
Results
- The sample comprised 1003 adults (mean [SD] age, 28.7 [3.7] years; 470 men [46.9%] and 533 women [53.1%]). A total of 63 participants were Asian (6.3%), 137 were Black (13.7%), and 762 were White (76.0%).
- For lifetime history criteria, 88 participants (8.8%) were classified as heavy cannabis users, 179 (17.8%) as moderate users, and 736 (73.4%) as nonusers. Heavy lifetime use (Cohen d = −0.28 [95% CI, −0.50 to −0.06]; false discovery rate corrected P = 0.02) was associated with lower activation on the working memory task.
- Regions associated with a history of heavy use included the anterior insula, medial prefrontal cortex, and dorsolateral prefrontal cortex.
- Recent cannabis use was associated with poorer performance and lower brain activation in the working memory and motor tasks, but the associations between recent use and brain activation did not survive false discovery rate correction. No other tasks were associated with lifetime history of heavy use, recent use, or dependence diagnosis.
Conclusions and Relevance
- In this study of young adults, lifetime history of heavy cannabis use was associated with lower brain activation during a working memory task. These findings identify negative outcomes associated with heavy lifetime cannabis use and working memory in healthy young adults that may be long lasting.
Reference:
- Gowin JL, Ellingson JM, Karoly HC, et al. Brain Function Outcomes of Recent and Lifetime Cannabis Use. JAMA Netw Open. 2025;8(1):e2457069. https://doi.org/10.1001/jamanetworkopen.2024.57069
Study: Cannabinoids, cannabis, and cannabis-based medicine for pain management: a systematic review of randomised controlled trials
Primary outcomes were 30% and 50% reduction in pain intensity, and AEs. Assessment of risk of bias of included studies, and the overall quality of evidence using GRADE.
Methods:
- 36 studies (7217 participants) delivering cannabinoids (8 studies), cannabis (6 studies), and CBM (22 studies); all had high and/or uncertain risk of bias.
Results:
- Evidence of benefit was found for cannabis <7 days (risk difference 0.33, 95% confidence interval 0.20-0.46; 2 trials, 231 patients, very low-quality evidence) and nabiximols >7 days (risk difference 0.06, 95% confidence interval 0.01-0.12; 6 trials, 1484 patients, very low-quality evidence).
- No other beneficial effects were found for other types of cannabinoids, cannabis, or CBM in our primary analyses; 81% of subgroup analyses were negative.
- Cannabis, nabiximols, and delta-9-tetrahydrocannabinol had more AEs than control.
- Studies in this field have unclear or high risk of bias, and outcomes had GRADE rating of low- or very low-quality evidence.
Conclusions:
- We have little confidence in the estimates of effect. The evidence neither supports nor refutes claims of efficacy and safety for cannabinoids, cannabis, or CBM in the management of pain.
References:
- Fisher E, Moore RA, Fogarty AE, Finn DP, Finnerup NB, Gilron I, Haroutounian S, Krane E, Rice ASC, Rowbotham M, Wallace M, Eccleston C. Cannabinoids, cannabis, and cannabis-based medicine for pain management: a systematic review of randomised controlled trials. Pain. 2021 Jul 1;162(Suppl 1):S45-S66. doi: 10.1097/j.pain.0000000000001929. PMID: 32804836.
- https://pubmed.ncbi.nlm.nih.gov/32804836/
Study: Cannabis and Male fertility edit
Current research suggests that cannabis may negatively impact male fertility. Further studies are needed to validate that robust findings in animal models will carry over into human experience. Clinicians should be aware of these potential effects when prescribing medical marijuana therapies to men of reproductive age, and they should consider the degree of cannabis use as a possible component of a complete male infertility workup.
Reference:
- Payne KS, Mazur DJ, Hotaling JM, Pastuszak AW. Cannabis and Male Fertility: A Systematic Review. J Urol. 2019 Oct;202(4):674-681. doi: 10.1097/JU.0000000000000248. Epub 2019 Sep 6. PMID: 30916627; PMCID: PMC7385722.
Study: Cannabis Use Disorder and Subsequent Risk of Psychotic and Nonpsychotic Unipolar Depression and Bipolar Disorder
Importance
- Cannabis use is increasing worldwide and is suspected to be associated with increased risk of psychiatric disorders; however, the association with affective disorders has been insufficiently studied.
Objective
- To examine whether cannabis use disorder (CUD) is associated with an increased risk of psychotic and nonpsychotic unipolar depression and bipolar disorder and to compare associations of CUD with psychotic and nonpsychotic subtypes of these diagnoses.
Design, Setting, and Participants
- This prospective, population-based cohort study using Danish nationwide registers included all individuals born in Denmark before December 31, 2005, who were alive, aged at least 16 years, and living in Denmark between January 1, 1995, and December 31, 2021.
Exposure
- Register-based diagnosis of CUD.
Main Outcome and Measures
- The main outcome was register-based diagnosis of psychotic or nonpsychotic unipolar depression or bipolar disorder. Associations between CUD and subsequent affective disorders were estimated as hazard ratios (HRs) using Cox proportional hazards regression with time-varying information on CUD, adjusting for sex; alcohol use disorder; substance use disorder; having been born in Denmark; calendar year; parental educational level (highest attained); parental cannabis, alcohol, or substance use disorders; and parental affective disorders.
Results
- A total of 6,651,765 individuals (50.3% female) were followed up for 119,526,786 person-years. Cannabis use disorder was associated with an increased risk of unipolar depression (HR, 1.84; 95% CI, 1.78-1.90), psychotic unipolar depression (HR, 1.97; 95% CI, 1.73-2.25), and nonpsychotic unipolar depression (HR, 1.83; 95% CI, 1.77-1.89). Cannabis use was associated with an increased risk of bipolar disorder in men (HR, 2.96; 95% CI, 2.73-3.21) and women (HR, 2.54; 95% CI, 2.31-2.80), psychotic bipolar disorder (HR, 4.05; 95% CI, 3.52-4.65), and nonpsychotic bipolar disorder in men (HR, 2.96; 95% CI, 2.73-3.21) and women (HR, 2.60; 95% CI, 2.36-2.85). Cannabis use disorder was associated with higher risk for psychotic than nonpsychotic subtypes of bipolar disorder (relative HR, 1.48; 95% CI, 1.21-1.81) but not unipolar depression (relative HR, 1.08; 95% CI, 0.92-1.27).
Conclusions and Relevance
- This population-based cohort study found that CUD was associated with an increased risk of psychotic and nonpsychotic bipolar disorder and unipolar depression.
- These findings may inform policies regarding the legal status and control of cannabis use.
Reference:
- Jefsen OH, Erlangsen A, Nordentoft M, Hjorthøj C. Cannabis Use Disorder and Subsequent Risk of Psychotic and Nonpsychotic Unipolar Depression and Bipolar Disorder [published online ahead of print, 2023 May 24]. JAMA Psychiatry. 2023;e231256. https://doi.org/10.1001/jamapsychiatry.2023.1256
- https://jamanetwork.com/journals/jamapsychiatry/article-abstract/2804862?guestAccessKey=67aec3cc-eee4-495d-8e74-316ead89de34
Study: Chest CT Findings in Marijuana Smokers
Retrospective case-control study
- evaluated results of chest CT examinations (from October 2005 to July 2020) in:
- marijuana smokers
- nonsmoker control patients
- tobacco-only smokers
- compared rates of:
- emphysema
- airway changes
- gynecomastia
- coronary artery calcification
Results
- Population:
- A total of 56 marijuana smokers (34 male; mean age, 49 years ± 14 [SD])
- 57 nonsmoker control patients (32 male; mean age, 49 years ± 14)
- 33 tobacco-only smokers (18 male; mean age, 60 years ± 6) were evaluated
- Higher rates of emphysema were seen among marijuana smokers (42 of 56
[0%]) than nonsmokers (three of 57[0%]) (P < .001) but not tobacco-only smokers (22 of 33[0%]) (P = .40). - Rates of bronchial thickening, bronchiectasis, and mucoid impaction were higher among marijuana smokers compared with the other groups (P < .001 to P = .04).
- Gynecomastia was more common in marijuana smokers (13 of 34
[0%]) than in control patients (five of 32[0%]) (P = .039) and tobacco-only smokers (two of 18[0%]) (P = .040). - There was no difference in rate of coronary artery calcification between age-matched marijuana smokers (21 of 30
[0%]) and tobacco-only smokers (28 of 33[0%]) (P = .16).
Conclusion:
- Airway inflammation and emphysema were more common in marijuana smokers than in nonsmokers and tobacco-only smokers, although variable interobserver agreement and concomitant cigarette smoking among the marijuana-smoking cohort limits our ability to draw strong conclusions.
Reference:
- Luke Murtha, Paul Sathiadoss, Jean-Paul Salameh, Matthew D. F. Mcinnes, and Giselle Revah. Chest CT Findings in Marijuana Smokers. Radiology. https://doi.org/10.1148/radiol.212611
Study: Daily Marijuana Use is Associated With Incident Heart Failure: "All of Us" Research Program edit
Background:
- With the increasing state-level legalization of marijuana across the United States, its use has increased exponentially, especially among the youth. However, a lot remains unknown concerning its cardiovascular health implications. We sought to assess the association between the frequency of marijuana use and new-onset heart failure (HF).
Methods:
- Using the NIH-sponsored "All of Us" Research Program, we performed a prospective analysis of participants' survey data and Electronic Health records (EHR). We excluded patients with a baseline EHR diagnosis of HF.
- Marijuana use was defined as any unprescribed use or if prescribed, use beyond prescribed doses, and was collected using the NM ASSIST instrument. We determined the association between the frequency of marijuana use and incident HF using Cox proportional hazards models adjusted for demographic and socioeconomic factors, diabetes mellitus, hypertension, hyperlipidemia, BMI, alcohol use and smoking status.
Results:
- From a final population of 156,999, there were 2958 events within a median follow-up time of 45 months.
- Compared to never users, daily marijuana users had an increased risk of incident HF (aHR - 1.34, 95% CI 1.04-1.72).
- In subgroup analyses, frequency of marijuana use was not associated with incident HFrEF nor HFpEF. There was no evidence of effect modification by age, sex at birth nor smoking status.
- The relationship was attenuated after addition of coronary artery disease diagnosis as a time varying covariate in our main model (aHR - 1.27, 95% CI 0.99-1.62).
Implication:
- Data on the cardiovascular effects of marijuana use is limited. To our knowledge this is the first prospective analysis on the association of marijuana use and HF.
- Our study suggests daily marijuana use is associated with HF.
- More research into the cardiovascular effects of marijuana is needed to enable clinicians provide the public with high quality information on the health implications of marijuana and to guide policies.
Reference:
- Moderated Digital Posters 2, Science and Technology Hall, Level 2 AHA Scientific Sessions 2023
- https://www.abstractsonline.com/pp8/?_ga=2.223148063.569559676.1693429947-1069604919.1693247687#!/10871/presentation/8975
Study: Evaluating the impact of cannabinoids on sleep health and pain in patients with chronic neuropathic pain: a systematic review and meta-analysis of randomized controlled trials
Background:
- Chronic neuropathic pain is often debilitating and can have a significant impact on sleep health and quality of life. There is limited information on the impact of cannabinoids on sleep health when treating neuropathic pain.
Objective:
- The objectives of this systematic review and meta-analysis were to determine the effect of cannabinoids on sleep quality, pain intensity, and patient impression of treatment efficacy in patients with neuropathic pain.
Evidence review:
- Nine available medical literature databases were searched for randomized controlled trials comparing synthetic and natural cannabinoids to placebo in patients with neuropathic pain syndromes. Data on validated tools for sleep quality, pain intensity, patients' global impression of change (PGIC), and incidence of adverse effects of cannabinoids were extracted and synthesized.
Findings:
- Of the 3491 studies screened, eight randomized controlled trials satisfied the inclusion criteria for this review. Analyses were performed using R -4.1.2. using the metafor package and are interpreted using alpha=0.05 as the threshold for statistical significance. Validated measures for sleep health were not used in most studies.
- Meta-analysis of data from six studies showed that cannabinoids were associated with a significant improvement in sleep quality (standardized mean difference (SMD): 0.40; 95% CI: 0.19 to -0.61, 95% prediction interval (PI): -0.12 to 0.88, p-value=0.002, I2=55.26, τ2=0.05, Q-statistic=16.72, GRADE: moderate certainty).
- Meta-analysis of data from eight studies showed a significant reduction in daily pain scores in the cannabinoid (CB) group (SMD: -0.55, 95% CI:-0.69 to -0.19, 95% PI: -1.51 to 0.39, p=0.003, I2=82.49, τ2=0.20, Q-statistic=47.69, GRADE: moderate certainty).
- However, sleep health and analgesic benefits were associated with a higher likelihood of experiencing daytime somnolence, nausea, and dizziness.
Conclusions:
- Cannabinoids have a role in treating chronic neuropathic pain as evidenced by significant improvements in sleep quality, pain intensity, and PGIC. More research is needed to comprehensively evaluate the impact of cannabinoids on sleep health and analgesic efficacy.
Reference:
- McParland AL, Bhatia A, Matelski J, et al. Evaluating the impact of cannabinoids on sleep health and pain in patients with chronic neuropathic pain: a systematic review and meta-analysis of randomized controlled trials. Reg Anesth Pain Med. 2023;48(4):180-190. https://doi.org/10.1136/rapm-2021-103431
- https://rapm.bmj.com/content/48/4/180.long
Study: Frequent marijuana use linked to heart disease
People who used marijuana daily were found to be about one-third more likely to develop coronary artery disease (CAD) compared with people who have never used the drug, according to a study presented at the American College of Cardiology's Annual Scientific Session Together With the World Congress of Cardiology.
Using data from the All of Us Research Program of the National Institutes of Health, which includes detailed information about the health and habits of 175,000 people, researchers first analyzed the relationship between cannabis use frequency (assessed using surveys at the time of enrollment in the study) and rates of CAD (assessed based on medical records spanning several years). They then used Mendelian randomization, a genetics-based approach to identify a causal relationship between cannabis use disorder and CAD risk using data from an independent genetics consortium. Cannabis use disorder is a recognized psychiatric disorder involving frequent marijuana use and dependency.
After adjusting for age, sex and major cardiovascular risk factors, the results indicated that daily cannabis users were 34% more likely to have CAD than those who have never used marijuana. In contrast, monthly cannabis use was not associated with a significant increase in the risk of CAD. The Mendelian randomization analysis suggested that this was due to a causal relationship, finding that people with cannabis use disorder were more likely to develop CAD. Additionally, in the genetic analysis, this causal relationship was independent of the potential confounding effects of tobacco and alcohol use.
Reference:
Study: Incident testicular cancer in relation to using marijuana and smoking tobacco: A systematic review and meta-analysis of epidemiologic studies
Background: Recent epidemiologic studies identified credible associations between marijuana smoking and risk of nonseminomatous testicular germ cell tumors (TGCTs), but did not distinguish exposure to cannabinoid compounds from exposure to other constituents of smoke.
Methods: We implemented a systematic review of scholarly literature followed by random effects meta-analysis to quantitatively synthesize published data relating incident TGCT to each of 2 exposure histories: ever using marijuana, and ever smoking tobacco.
Results: We identified four epidemiologic studies of marijuana use and 12 of tobacco smoking.
- Summary data concur with earlier reports of a specific association of marijuana use with nonseminoma, summary odds ratio [sOR] = 1.71 (95% confidence interval [CI] 1.12-2.60)
- A positive association, sOR = 1.18 (95% CI 1.05-1.33), between tobacco smoking and all TGCT.
Conclusions: Available data accord with positive associations between incident TGCT and each exposure, implicating both cannabinoid compounds and other constituents of smoke. Etiologic interpretation awaits epidemiologic studies that assess associations between tobacco smoking and nonseminomatous TGCT, investigating not only these exposures but also both co-use of tobacco and marijuana and smoke-free sources of cannabinoids, while adequately evaluating potential confounding among all of these exposures.
Reference:
- Song A, Myung NK, Bogumil D, Ihenacho U, Burg ML, Cortessis VK. Incident testicular cancer in relation to using marijuana and smoking tobacco: A systematic review and meta-analysis of epidemiologic studies. Urol Oncol. 2020 Jul;38(7):642.e1-642.e9. doi: 10.1016/j.urolonc.2020.03.013. Epub 2020 May 12. PMID: 32409200.
Study: Increased Risk of Major Adverse Cardiac and Cerebrovascular Events in Elderly Non-Smokers With Cannabis Use Disorder: A Population-Based Analysis edit
Background:
- Tobacco smoking confounds CVD risk studies. No large-scale investigation has been performed yet to examine cannabis use disorder (CUD) in elderly non-smokers with established CVD risk and major adverse cardiac and cerebrovascular events (MACCE).
Methods:
- The National Inpatient Sample (2019) was queried using relevant ICD-10 codes to identify elderly (>65 years) admissions with established CVD risk without known tobacco use disorder and stratified into CUD and non-CUD cohorts. Logistic regression evaluated MACCE odds as primary outcomes and secondary outcomes as predictors of MACCE incidents in CUD users. P< 0.05 was considered significant.
Results:
- Of 28,535 elderly cannabis users with CVD risk and no tobacco use disorder, 13.9% reported MACCE episodes.
- CUD patients were more likely to be male, black, and non-electively admitted from urban teaching and Western region hospitals.
- AIDS, alcohol abuse, depression, uncomplicated hypertension, and drug abuse were greater in the CUD cohort, while the non-CUD group had more complicated hypertension, diabetes with and without chronic comorbidities, hyperlipidemia, obesity, thyroid issues, previous strokes, VTE, cancer.
- The CUD cohort reported:
- Higher MACCE (OR 1.20; 95% CI 1.11-1.29)
- ACM (3.3% vs. 1.7%)
- dysrhythmia (34.9% vs. 24.9)
- acute myocardial infarction (7.6% vs. 6.0%, p 0.001)
- transfer to other facilities (28.9% vs. 19.0%)
- home health care (22.4%) compared to non-CUD cohort (p 0.001).
- Chronic lung disease, renal disease, hypertension, and hyperlipidemia were predictors of MACCE episodes in CUD users.
- Higher MACCE (OR 1.20; 95% CI 1.11-1.29)
Conclusion:
- Even after controlling for smoking, elderly cannabis users having CVD risk had 20% more MACCE events encountered than non-users. Cannabis use in older non-smokers deserves investigation into CVD. risks
Reference:
- Moderated Digital Posters 2, Science and Technology Hall, Level 2 AHA Scientific Sessions 2023
- https://www.abstractsonline.com/pp8/?_ga=2.223148063.569559676.1693429947-1069604919.1693247687#!/10871/presentation/8974
Study: Marijuana and Cardiovascular Disease
- Compared with non-users, MJ use associated with
- 88% higher odds of myocardial infarction or CAD in adults 18-74
- 81% higher odds of stroke
- Even higher odds in males <55 yo and females <65 yo
- Frequent MJ smoking had
- 2.1 times higher odds of MI or CAD
- 1.8 times highter odds of stroke
- No association was observed between MJ use in any form other than smoking and cardiovascular disease
References:
- S Shah. Association of Marijuana Use and Cardiovascular Disease: A Behavioral Risk Factor Surveillance System Data Analysis of 133,706 US Adults. AJM Vol 134 No 5 May 2021
Study: Marijuana linked to higher PAD risk
Marijuana users have an almost four times greater risk of developing peripheral artery disease, compared with nonusers, results of a study of more than 600,000 marijuana users suggest, although there was no greater risk of death from myocardial infarction or other cardiac causes or need for revascularization.
The study population was young, with an average age of 37.4 years, and that the study period, from 2016 to 2019, predates the legalization of recreational marijuana in a number of states.
Nonetheless, even in this young study population, marijuana users' risk of developing peripheral artery disease (PAD) was 3.68 times greater (P < 0.001) than that of nonusers. PAD at a young age could precede worse outcomes later in life, the study authors said.
The study used data on 623,768 marijuana users from the National Inpatient Sample, a nationwide database of inpatient visits covered by all public and commercial payers, then extracted a diagnosis for PAD from all 30 million–plus patient encounters to compare PAD rates between marijuana users and nonusers. Marijuana users were more likely to be White and to have elective rather than emergency admissions (P < 0.001). The researchers used diagnostic codes to identify marijuana users and PAD patients.
Reference:
Study: Myocardial Infarction and Cardiovascular Risks Associated with Cannabis Use: A Multicenter Retrospective Study
This study aimed to evaluate the long-term cardiovascular effects of cannabis use in relatively healthy individuals.
This retrospective cohort study utilized the TriNetX health research network, which aggregates de-identified electronic medical records from healthcare organizations worldwide. The specific network used for this study was Research, which contains data from 53 healthcare organizations (HCO) throughout the United States.
Study Population:
- Focused on adults aged ≤50 years between 2010 and 2018, divided into two cohorts.
- The cannabis-user group with cannabis use diagnoses (ICD-10: F12.1, F12.9, F12.90).
- The non-cannabis-user group. Both cohorts were free of significant comorbidities at baseline, including hypertension, hyperlipidemia or LDL>100 mg/dL, coronary artery disease including prior MI or history of coronary interventions, diabetes mellitus (DM) or HbA1c >7, and tobacco use.
- The relatively healthy status of these patients was a key aspect of this study design, ensuring that comparisons were not influenced by pre-existing high-risk conditions.
- Propensity score matching (PSM) was performed, covariates were matched by 1:1 PSM using the greedy nearest neighbor matching algorithm with a cutoff of 0.1 pooled standardized mean difference (SMD). The following covariates were included in the PSM: age at index, sex, race, chronic kidney disease, depressive episode (DD), family history of ischemic heart disease, pregnancy, cancer history, creatinine, LDL, HbA1c, BMI, systolic blood pressure.
Study Outcome:
- The primary outcome included MI defined using ICD-10 codes.
- Secondary outcomes contained the Major Adverse Cardiovascular Events (MACE) (ischemic stroke, coronary revascularization, and ventricular fibrillation/tachycardia), all-cause mortality, heart failure (HF) and ischemic stroke. The index event was defined as the first-time cannabis use diagnosis was detected and for the non-user group was the first office visit.
Statistical analysis:
- The analysis was performed with TriNetX Live built-in analytics. Continuous variables were expressed as mean ± SD or median (IQR), and categorical variables were presented as number (%) where appropriate. Baseline characteristics between the 2 groups were compared by using independent t-tests and chi-square tests for continuous and categorical variables respectively. Kaplan-Meier (KM) survival analysis was conducted to demonstrate the survival probabilities difference between the two groups, with statistical significance assessed using log-rank tests. Cox proportional hazards and logistic regression models were used to estimate hazard ratios (HRs) and odds ratio (OR) with 95% confidence intervals (CIs). The significance threshold was established at P < 0.05.
Results
- A total of 4,636,628 relatively healthy adults aged ≤50 years:
- 93,267 (2.01%) cannabis-users and 4,543,361 (97.99%) non-users.
- Cannabis-users were older (26 ± 8 vs 21 ± 9.5 years, P < 0.0001) and had higher comorbidities, including a nearly 15-fold higher prevalence of DD (30.63% vs 1.88%, P < 0.01) and BMI >30 (18.72% vs 3.25%, P < 0.0001).
- After PSM, each group had 89,776 patients with balanced demographics and baseline health characteristics.
- Over 5-years, mean follow-up was 35.7±23.4 months for cannabis-users and 44.2±23.8 months for non-users.
- MI absolute risk (AR) was 0.558% in cannabis-users vs. 0.09% in non-users, with a risk difference (RD) of 0.468% (95% CI: 0.415%-0.52%), a risk ratio (RR) of 6.185 (95% CI: 4.892-7.82), and an OR of 6.214 (95% CI: 4.913-7.86).
- KM analysis showed lower survival probability in cannabis-users (99.119% vs. 99.867%, p < 0.0001), with an HR of 7.568 (95% CI: 5.982-9.575).
- For ischemic stroke, the AR was 0.405% in cannabis-users vs. 0.094% in non-users, with an RD of 0.312% (95% CI: 0.266%-0.358%), an RR of 4.333 (95% CI: 3.419-5.493), and an OR of 4.347 (95% CI: 3.428-5.512).
- KM survival probability was 99.395% in cannabis-users vs. 99.866% in non-users (p < 0.0001), with an HR of 5.151 (95% CI: 4.060-6.534).
- Regarding MACE, AR was 1.187% vs. 0.366%, with an RD of 0.821% (95% CI: 0.74%-0.90%), an RR of 3.24 (95% CI: 2.864-3.665), and an OR of 3.267 (95% CI: 2.886-3.698).
- KM survival was 98.2% vs. 99.495% (p < 0.0001), with an HR of 3.869 (95% CI: 3.42-4.38).
- For HF, AR was 0.861% vs.0.424%, with an RD of 0.437% (95% CI: 0.363%-0.511%), an RR of 2.029 (95% CI: 1.795-2.293), and an OR of 2.038 (95% CI: 1.802-2.305).
- KM survival was 98.763% vs. 99.453% (p < 0.0001), with an HR of 2.323 (95% CI: 2.054-2.627).
- Regarding all-cause mortality, AR was 1.262% vs. 0.841%, with an RD of 0.421% (95% CI: 0.327%-0.515%), an RR of 1.501 (95% CI: 1.369-1.645), and an OR of 1.507 (95% CI: 1.374- 1.653).
- KM survival was 97.96% vs. 98.86% (p < 0.0001), with an HR of 1.813 (95% CI: 1.653- 1.989).
Discussion
- This analysis provides evidence linking cannabis-use to adverse cardiovascular events, including MI, ischemic stroke, HF and mortality.
- Notably, cannabis use appears to pose a substantial and independent risk for these outcomes, even in a population without traditional cardiovascular risk factors. These findings suggest cannabis as a novel and underrecognized risk factor for cardiovascular diseases.
- Our study results are consistent with prior research documenting acute coronary syndrome following cannabis use.
- Studies suggest that cannabis use can precipitate MI, particularly within an hour of consumption, with the risk increasing nearly fivefold. This effect is pronounced in young, healthy individuals, who present with chest pain. Cannabis has also been implicated in endothelial dysfunction, pro-inflammatory cytokine release, and oxidative stress, all of which contribute to coronary microvascular dysfunction and plaque destabilization.
- This study has limitations due to lack of detailed cannabis consumption data and potential misclassification. The inherent limitations of real-world data often result from inconsistent patient reporting in electronic medical records. Future research should investigate the doseresponse relationship, and the effects of synthetic cannabinoids.
Conclusion:
- The findings underscore significant cardiovascular risks associated with cannabis use, reinforcing the need for public health initiatives and heightened clinician awareness.
Reference:
Study: Nondisordered Cannabis Use Among US Adolescents
Importance: Cannabis use is increasingly viewed by adolescents as not harmful. Youths with cannabis use disorder (CUD) are recognized by clinicians as being at risk for adverse outcomes, yet little is known about the associations between subclinical cannabis use (ie, nondisordered cannabis use [NDCU]) and adverse psychosocial events.
Objective: To describe the prevalence and demographics of NDCU and to compare associations of cannabis use with adverse psychosocial events among adolescents with no cannabis use, NDCU, and CUD.
Design, setting, and participants: This cross-sectional study used a nationally representative sample derived from the 2015 to 2019 National Survey on Drug Use and Health. Participants were adolescents aged 12 to 17 years, separated into 3 distinct groups: nonuse (no recent cannabis use), NDCU (recent cannabis use below diagnostic threshold), and CUD. Analysis was conducted from January to May 2022.
Exposures: CUD, NDCU, or cannabis nonuse. NDCU was defined as endorsing recent cannabis use but not meeting the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) (DSM-5) CUD criteria. CUD was defined using DSM-5 criteria.
Main outcomes and measures: The main outcomes were prevalence of adolescents meeting criteria for NDCU and associations between adverse psychosocial events and NDCU, adjusted for sociodemographic characteristics.
Results:
- The 68 263 respondents (mean [SD] age, 14.5 [1.7] years; 34 773 [50.9%] males) included in the analysis represented an estimated yearly mean of 25 million US adolescents during 2015 to 2019.
- Among respondents, 1675 adolescents (2.5%) had CUD, 6971 adolescents (10.2%) had NDCU, and 59 617 adolescents (87.3%) reported nonuse.
- Compared with nonusers, individuals with NDCU had approximately 2 to 4 times greater odds of all adverse psychosocial events examined, including:
- Major depression (adjusted odds ratio [aOR], 1.86; 95% CI, 1.67-2.08)
- Suicidal ideation (aOR, 2.08; 95% CI, 1.88-2.29)
- Slower thoughts (aOR, 1.76; 95% CI, 1.58-1.96)
- Difficulty concentrating (aOR, 1.81; 95% CI, 1.65-2.00)
- Truancy (aOR, 1.90; 95% CI, 1.67-2.16)
- Low grade point average (aOR, 1.80; 95% CI, 1.62-2.00)
- Arrest (aOR, 4.15; 95% CI, 3.17-5.43)
- Fighting (aOR, 2.04; 95% CI, 1.80-2.31)
- Aggression (aOR, 2.16; 95% CI, 1.79-2.62)
- Prevalence of adverse psychosocial events was greatest for adolescents with CUD (range, 12.6% to 41.9%), followed by NDCU (range, 5.2% to 30.4%), then nonuse (range, 0.8% to 17.3%).
Conclusions and relevance: In this cross-sectional study of US adolescents, past-year NDCU was approximately 4 times as prevalent as past-year CUD. A stepwise gradient association was observed for odds of adverse psychosocial events between adolescent NDCU and CUD. In the context of US normalization of cannabis use, prospective research into NDCU is necessary.
Reference:
- Sultan RS, Zhang AW, Olfson M, Kwizera MH, Levin FR. Nondisordered Cannabis Use Among US Adolescents. JAMA Netw Open. 2023;6(5):e2311294. Published 2023 May 1. https://doi.org/10.1001/jamanetworkopen.2023.11294
Study: Prenatal cannabis exposure associated with mental disorders in children that persist into early adolescence
Prenatal cannabis exposure following the middle of the first trimester—generally after five to six weeks of fetal development—is associated with attention, social, and behavioral problems that persist as the affected children progress into early adolescence (11 and 12 years of age)
Reference:
- DAA Baranger, et al. Association of Mental Health Burden With Prenatal Cannabis Exposure From Childhood to Early Adolescence:(link is external) Longitudinal Findings From the Adolescent Brain Cognitive Development (ABCD) Study(link is external). JAMA Pediatrics. DOI: 10.1001/jamapediatrics.2022.3191
- https://www.nih.gov/news-events/news-releases/prenatal-cannabis-exposure-associated-mental-disorders-children-persist-into-early-adolescence
Study: The placebo response in cannabinoid trials for clinical pain
Meta-analysis of 20 studies of 1459 individuals
Study Selection:
- Cannabinoid studies with a double-blind, placebo-controlled design with participants 18 years or older with clinical pain of any duration were included.
- Studies were excluded if they treated individuals with HIV/AIDS or severe skin disorders.
Results:
- Twenty studies, including 1459 individuals (mean [SD] age, 51 [7] years; age range, 33-62 years; 815 female
[56%]), were included. - Pain intensity was associated with a significant reduction in response to placebo, with a moderate to large effect size (mean [SE] Hedges g, 0.64 [0.13]; P < .001).
- Trials with low risk of bias had greater placebo responses (q1 = 5.47; I2 = 87.08; P = 0.02).
- The amount of media attention and dissemination linked to each trial was proportionally high, with a strong positive bias, but was not associated with the clinical outcomes.
Conclusions and Relevance:
- Placebo contributes significantly to pain reduction seen in cannabinoid clinical trials.
- The positive media attention and wide dissemination may uphold high expectations and shape placebo responses in future trials, which has the potential to affect the outcome of clinical trials, regulatory decisions, clinical practice, and ultimately patient access to cannabinoids for pain relief.
Reference:
- Gedin F, Blomé S, Pontén M, et al. Placebo Response and Media Attention in Randomized Clinical Trials Assessing Cannabis-Based Therapies for Pain: A Systematic Review and Meta-analysis. JAMA Netw Open. 2022;5(11):e2243848. https://doi.org/10.1001/jamanetworkopen.2022.43848
- https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2799017
Study: Therapeutic Use of Cannabis and Cannabinoids: A Review edit
Importance: Approximately 27% of adults in the US and Canada report having ever used cannabis for medical purposes. An estimated 10.5% of the US population reports using cannabidiol (CBD), a chemical compound extracted from cannabis that does not have psychoactive effects, for therapeutic purposes.
Observations: Conditions for which cannabinoids have approval from the US Food and Drug Administration include HIV/AIDS-related anorexia, chemotherapy-induced nausea and vomiting, and certain pediatric seizure disorders. A meta-analysis of randomized clinical trials reported a small but significant reduction in nausea and vomiting from various causes (eg, chemotherapy, cancer) when comparing prescribed cannabinoids (eg, dronabinol, nabilone) with placebo or active comparators (eg, alizapride, chlorpromazine; standardized mean difference [SMD], -0.29 [95% CI, -0.39 to -0.18]). A meta-analysis of randomized clinical trials among patients with HIV/AIDS reported that cannabinoids had a moderate effect on increasing body weight compared with placebo (SMD, 0.57 [95% CI, 0.22 to 0.92]). Evidence-based guidelines do not recommend the use of inhaled or high-potency cannabis (≥10% or 10 mg Δ9-tetrahydrocannabinol [Δ9-THC]) for medical purposes. High-potency cannabis compared with low-potency cannabis use is associated with increased risk of psychotic symptoms (12.4% vs 7.1%) and generalized anxiety disorder (19.1% vs 11.6%). A meta-analysis of observational studies reported that 29% of individuals who used cannabis for medical purposes met criteria for cannabis use disorder. Daily inhaled cannabis use compared with nondaily use was associated with an increased risk of coronary heart disease (2.0% vs 0.9%), myocardial infarction (1.7% vs 1.3%), and stroke (2.6% vs 1.0%). Evidence from randomized clinical trials does not support the use of cannabis or cannabinoids for most conditions for which it is promoted, such as acute pain and insomnia. Before considering cannabis or cannabinoids for medical use, clinicians should consult applicable institutional, state, and national regulations; evaluate for drug-drug interactions; and assess for contraindications (eg, pregnancy) or conditions in which risks likely outweigh benefits (eg, schizophrenia or ischemic heart disease). For patients using cannabis or cannabinoids for treatment of medical conditions, clinicians should discuss harm reduction strategies, including avoiding concurrent use with alcohol or other central nervous system depressants such as benzodiazepines, using the lowest effective dose, and avoiding use when driving or operating machinery.
Conclusions and relevance: Evidence is insufficient for the use of cannabis or cannabinoids for most medical indications. Clear guidance from clinicians is essential to support safe, evidence-based decision-making. Clinicians should weigh benefits against risks when engaging patients in informed discussions about cannabis or cannabinoid use.
Reference:
- Hsu M, Shah A, Jordan A, Gold MS, Hill KP. Therapeutic Use of Cannabis and Cannabinoids: A Review. JAMA. 2025 Nov 26. doi: 10.1001/jama.2025.19433. Epub ahead of print. PMID: 41296368.
Chocolate
Chocolate intake is inversely associated with development of DM II
- Compared with those who consumed chocolate more than 1/wk, those who rarely or never ate chocolate had significant highter risk of developing DM II 5 years later.
- Consultant Feb 2017
Chronic use of NSAIDs and COX-2 inhibitors:
- Safe to use in older adults with arthritis and no history of cardiovascular disease.
- NSAIDs are just as safe as COX-2 inhibitors.
Reference:
- (European Society of Cardiology. SCOT study quells concerns about NSAID safety [press release]. Aug 31, 2015)
Continuous Glucose Monitoring (CGM)
ICD10: E11.65 - Type 2 diabetes mellitus with hyperglycemia
- G7
- Dexcom G7 Transmitter
- 3 each for 90 days. Use as directed
- Dexcom G7 Sensor Continuous Blood Glucose Monitor
- 9 each for 90 days. Use as directed
- Dexcom G7 Transmitter
- G6
- Dexcom G6 CGM Sensors
- 9 each for 90 days. Use as directed. DM2 - Insulin
- Dexcom G6 CGM Transmitter
- 3 each for 90 days. Use with Dexcom sensors. DM2 - Insulin
- Dexcom G6 CGM Sensors
Contraception
Use the Quick Start method:
- Start same day as prescription regardless of menstrual cycle
- Use back-up protection for the first 7 days
- Prescribe a year at a time
Patient Resources:
- Bedsider.org
- StayTeen.org
Antiepileptic drugs to avoid with OCPs:
- Carbamazepine
- Lamotrigine
- Oxcarbazepine
- Phenobarbital
- Phenytoin
- Primodone
- Topiramate
Antiepileptic drugs to consider instead with OCPs:
- Ethosuximide
- Gabapentin
- Levetiracetam
- Pregabalin
- Tiagabine
- Valproate
- Vigabatrin
- Zonisamide
References:
- JFP Vol 66 No 11 Nov 2017
OCP Adverse Effect Management
- Nausea
- Take pill at bedtime, or at a meal
- Use Low Estrogen pill (e.g. Loestrin 1/20)
- Fluid Retention
- Change to OCP with the following characteristics
- Low Estrogenic Activity (or low Estrogen dose)
- Examples
- Loestrin 1/20
- Loestrin 1.5/30
- Change to OCP with the following characteristics
- Appetite too active or weight gain
- Change to OCP with the following characteristics
- Low Estrogenic Activity (or low Estrogen dose)
- Low Androgenic Activity
- Examples
- Ovcon 35
- Ortho Novum 1/35
- Change to OCP with the following characteristics
- Hypertension
- Discontinue Oral Contraceptive
- Consider Mini-Pill (Progestin only)
- Major Depression
- See Major Depression Management
- Change to OCP with the following characteristics
- Low Progestin Activity
- Adjunctive Measures
- Pyridoxine 20 mg bid
- Migraine Headache
- Do not use Oral Contraceptives in women who have Migraine with Aura (risk of stroke)
- Consider Progestin-Only Pill (Mini-Pill) or Intrauterine Device as alternative
- Characteristics
- More common during the first cycle of Oral Contraceptives
- More common in women over age 35 years
- General
- Change to OCP with low Estrogenic Activity (or low Estrogen dose)
- Examples
- Loestrin 1/20
- Progesterone Only OCP
- Avoid triphasic Oral Contraceptives
- Continuous Cycle or Seasonal Contraception (84 days OCP with 5 days withdraw)
- Indicated for Menstrual Migraine
- Headache during the Placebo week
- Take estradiol 10 mcg orally for 5 of the 7 Placebo days
- Benefit in age over 40 years (unclear if benefit extends to younger women)
- Do not use Oral Contraceptives in women who have Migraine with Aura (risk of stroke)
- Miscellaneous adverse effects
- Decreased Libido
- Increase Androgenic Activity
- Moodiness
- Lower Estrogenic Activity
- Dry Eyes
- Increase Progestin Activity (Progestin dominant pill)
- Decreased Libido
Reference:
Controlled medications
Prescription:
- A prescription must be written in ink or indelible pencil or typewritten and must be manually signed by the practitioner. An individual may be designated by the practitioner to prepare the prescriptions for his/her signature. The practitioner is responsible for making sure that the prescription conforms in all essential respects to the law and regulation.
- Prescriptions for schedule II controlled substances must be written and be signed by the practitioner. In emergency situations, a prescription for a schedule II controlled substance may be telephoned to the pharmacy and the prescriber must follow up with a written prescription being sent to the pharmacy within seven days. Prescriptions for schedules III through V controlled substances may by written, oral or transmitted by fax.
Refills:
- Prescriptions for schedule II controlled substances cannot be refilled. A new prescription must be issued. Prescriptions for schedules III and IV controlled substances may be refilled up to five times in six months. Prescriptions for schedule V controlled substances may be refilled as authorized by the practitioner.
Opioid Use Disorder and Clinics
- Central Florida Treatment Centers
- Florida Treatment Services
- Aspire Health Partners
- New Season
- Orlando Recovery
- Orlando Outpatient Center
Here are locations I found that have been described as low cost:
- Central Florida Treatment Centers: https://methadoneworks.net/
- Florida Treatment Services: https://floridatreatmentservices.com/
- Aspire Health Partners: https://aspirehealthpartners.com/
- New Season: https://www.newseason.com/
- Orlando Recovery: https://www.orlandorecovery.com/
- Orlando Outpatient Center: https://www.orlandooutpatient.com/
I suggest calling each of them and asking for help.
Opioid: CDC Recommendations
Maximize use of non opioid therapy
- Treat any mood disorder
- PT, exercise, water aerobics
- CBT
- Intraarticular glucocorticoid or trigger point injections
- Epidural steroid injections for chronic radicular low back pain
- TENS units with poor data
- Acetaminophen vs NSAIDS
- For chronic LBP - both are equally effective
- For non-LBP, NSAIDS are slightly more effective for OA
- NSAIDs have significantly more side effects
- COX2 have less side effects but still CV risk like NSAIDS
- Neuropathic pain
- Gabapentin, pregabalin, TCAs
- Duloxetine and venlafaxine
- Nortiptyline at low doses (10mg/d)
- Other
- Topical 5% lidocaine patch or gel
- Capsaicin cream
Opioid: FL HB21
Main points:
- 3 Day limit on schedule II opioids for "acute pain" with a 7 day exemption)
- For 7 days:
- have to believe it is medically necessary to treat the pain
- Indicate "Acute Pain Exemption" on the prescription
- Adequately document in the records the acute medical condition and lack of alternative treatment options that justify the deviation from 3 day supply limit
- Acute Pain Exemption Template
- "Patient is having significant pain caused by _ which will last more thatn three days. Trial of _ has not helped. I believe that it is medically necessary to treat this patient's pain because it is affecting their ability to _."
- For 7 days:
- Includes hydrocodone and codeine
- Opioid antagonist requirements
- Consult PDMP before prescribing MOST controlled substances every time
Resources:
Controlled Medications (Schedule drugs) FL
Florida law (F.S. 456.47) permanently allows for prescribing schedule III-V drugs via telehealth in Florida, but prohibits prescribing Schedule II controlled substances unless an exception is met:
- The treatment of a psychiatric disorder
- Inpatient treatment at a hospital licensed under chapter 20 395
- The treatment of a patient receiving hospice services as defined in s. 400.601
- The treatment of a resident of a nursing home facility as defined in s. 400.021
Corticosteroids
See also:
- Topical Corticosteroids
- Systemic corticosteroids are recommended for patients within three days of the onset of symptoms of Bell palsy.
- LOE: A
- Systemic corticosteroids appear to be a safe and effective alternative to nonsteroidal anti-inflammatory drugs in patients with acute gout.
- LOE: B
- Do not prescribe systemic corticosteroids for patients with acute bronchitisor acute sinusitis.
- LOE: B
- Do not prescribe systemic corticosteroids for patients with allergic rhinitis.
- LOE: C
- There is insufficient evidence to support routine use of systemic corticosteroids for patients with lumbar radiculopathy.
- LOE: B
- Do not prescribe systemic corticosteroids for patients with carpal tunnel syndrome.
- LOE: B
- There is insufficient evidence to support routine use of systemic corticosteroids for patients with acute pharyngitis.
- LOE: B
- There is insufficient evidence to support routine adjunct use of systemic corticosteroids for patients with herpes zoster.
- LOE: B
Prescribing Helps:
- Medrol Dosepak (Methylprednisolone Dose Pack) Dosing (according to the packaging) – 4-mg tablets
- 6-day tapering course: 6, 5, 4, 3, 2, 1 pill(s) for a total of 21 tablets
- Day 1: (2) tablets before breakfast, (1) after lunch, (1) after dinner, (2) at bedtime [24-mg]
- Day 2: (1) before breakfast, (1) after lunch, (1) after dinner, (2) at bedtime [20-mg]
- Day 3: (1) before breakfast, (1) after lunch, (1) after dinner, (1) at bedtime [16-mg]
- Day 4: (1) before breakfast, (1) after lunch, (1) at bedtime [12-mg]
- Day 5: (1) before breakfast, (1) at bedtime [8-mg]
- Day 6: (1) before breakfast [4-mg]
- Directions: Day 1: (2) tablets before breakfast, (1) after lunch, (1) after dinner, (2) at bedtime; Day 2: (1) before breakfast, (1) after lunch, (1) after dinner, (2) at bedtime; Day 3: (1) before breakfast, (1) after lunch, (1) after dinner, (1) at bedtime; Day 4: (1) before breakfast, (1) after lunch, (1) at bedtime; Day 5: (1) before breakfast, (1) at bedtime; Day 6: (1) before breakfast
- Note:
- If patient's get the dose pack later in the day, it is okay to take all six (6) tablets at once or in divided doses so they are all consumed the first day.
- Then have the patient start on the package instructions for day 2.
- 6-day tapering course: 6, 5, 4, 3, 2, 1 pill(s) for a total of 21 tablets
References:
- AFP Vol 101 No 2 Jan 2020
- https://thepainsource.com/methylprednisolone-medrol-dosepak/
Study: Association Between Oral Corticosteroid Bursts and Severe Adverse Events : A Nationwide Population-Based Cohort Study (Steroid burst dangers)
For people taking oral steroids over a median 3 days, the risk of such events was elevated in the 5-30 days after steroid therapy initiation compared with the reference period (5-90 days before initiation):
- GI bleeding: 27.1 per 1,000 person-years (incidence rate ratio 1.80, 95% CI 1.75-1.84)
- Sepsis: 1.5 per 1,000 person-years (IRR 1.99, 95% CI 1.70-2.32)
- Heart failure: 1.3 per 1,000 person-years (IRR 2.37, 95% CI 2.13-2.63)
Background:
- Long-term use of oral corticosteroids has known adverse effects, but the risk from brief oral steroid bursts (≤14 days) is largely unknown.
Objective:
- To examine the associations between steroid bursts and severe adverse events, specifically gastrointestinal (GI) bleeding, sepsis, and heart failure.
Design:
- Self-controlled case series.
Setting:
- Entire National Health Insurance Research Database of medical claims records in Taiwan.
Participants:
- Adults aged 20 to 64 years with continuous enrollment in the National Health Insurance program from 1 January 2013 to 31 December 2015.
Measurements:
- Incidence rates of severe adverse events in steroid burst users and non-steroid users, as well as incidence rate ratios (IRRs) for severe adverse events within 5 to 30 and 31 to 90 days after initiation of steroid therapy.
Results:
- Of 15,859,129 adult participants, 2,623,327 who received a single steroid burst were included.
- The most common indications were skin disorders and respiratory tract infections.
- The incidence rates per 1000 person-years in steroid bursts were
- 27.1 (95% CI, 26.7 to 27.5) for GI bleeding
- 1.5 (CI, 1.4 to 1.6) for sepsis
- 1.3 (CI, 1.2 to 1.4) for heart failure
- Rates of GI bleeding (IRR, 1.80 [CI, 1.75 to 1.84]), sepsis (IRR, 1.99 [CI, 1.70 to 2.32]), and heart failure (IRR, 2.37 [CI, 2.13 to 2.63]) *significantly increased within 5 to 30 days after steroid therapy initiation and attenuated during the subsequent 31 to 90 days.
Limitation:
- Persons younger than 20 years or older than 64 years were not included.
Conclusion:
- Oral corticosteroid bursts are frequently prescribed in the general adult population in Taiwan.
- The highest rates of GI bleeding, sepsis, and heart failure occurred within the first month after initiation of steroid therapy.
Reference:
- Yao TC, Huang YW, Chang SM, Tsai SY, Wu AC, Tsai HJ. Association Between Oral Corticosteroid Bursts and Severe Adverse Events : A Nationwide Population-Based Cohort Study. Ann Intern Med. 2020 Sep 1;173(5):325-330. doi: 10.7326/M20-0432. Epub 2020 Jul 7. PMID: 32628532.
- https://pubmed.ncbi.nlm.nih.gov/32628532/
Coumadin (Warfarin) Dosing/Management
Warfarin Maintenance Dosing Protocol with INR Goal 2-3 (Class IIb, Level C)
| INR < 1.5 | INR 1.5 - 1.9 | INR 2.0 - 3.0 | INR 3.1- 4.0* | INR 4.1-5.0* | INR 5.1- 9.0* | INR > 9.0 |
| Extra Dose; Increase weekly dose 10-20% | Increase weekly dose 5-10% | No change | Decrease weekly dose 5-10% | Hold 1 dose; Decrease weekly dose 10% | Consider: Hold 2 doses; Decrease weekly dose 10-20%; Check Hct | Urgent patient evaluation |
Warfarin Maintenance Dosing Adjustment Nomogram for INR Goal of 2-3
Adjustment Guidelines
- A: Baseline CBC, PT/INR required prior to continuation of warfarin therapy.
- B: Assess patient compliance and determine if any changes have been made that may impact therapy: 1) addition of interacting drugs or herbal products; 2) changes in diet (eating/not eating) 3) changes in health status.
- C: Based on the INR results make adjustments to the current therapy based on the ranges below:
INR < 1.5
- Verify compliance (if non-compliant: resume therapy at previous dose).
- If dosage adjustment needed: increase maintenance dose by 5%- 20%*.
- Some clinicians recommend a 'booster dose' 1.5 to 2x the daily maintenance dose x 1
- Return: 3 - 7 days
INR 1.5 - 1.9
- Verify compliance (if non-compliant: resume therapy at previous dose).
- [* Some clinicians recommend a 'booster dose' 1.5 to 2x the daily maintenance dose x 1 ]
- If dosage adjustment needed: increase maintenance dose by 5 - 15% (use lower end of this range for INR values close to the therapeutic range).
- Return: 3 - 7 days
INR 2.0 - 3.0
- No Changes Needed
- Return: 4 weeks
INR 3.1 - 3.4
- Dose adjustment usually not necessary if level is at the low end of this range ( 3.1 - 3.2) and at least two previous levels were therapeutic. Recheck in 3 to 7 days.
- Consider decreasing dose by 5 - 10% and/or holding one dose.
- Recheck in 3- 7 days.
INR 3.5 - 3.9
- consider holding one dose.
- evaluate any clinical changes that may have occurred with the patient (eating regularly, no new medications, etc.)
- consider decreasing the maintenance dose by 5 -15% depending on magnitude of the INR elevation.
- Return: 1- 3 days.
INR 4.0 - 4.9 with no significant bleeding
- Hold warfarin until INR is within the therapeutic range.
- Recommend lowering maintenance dose by 5%- 20%
- Increase frequency of monitoring until problem resolved (daily initially).
- (8th ACCP): If only minimally above therapeutic range or associated with a transient causative factor, no dose reduction may be required.
INR > 5.0
- Review latest ACCP guidelines - ELEVATED INRs.
- Return daily until therapeutic.
References:
- Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, Svensson PJ, Veenstra DL, Crowther M, Guyatt GH; American College of Chest Physicians. Evidence-based management of anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141(2 Suppl):e152S-84S. doi: 10.1378/chest.11-2295.
- https://www.uwhealth.org/files/uwhealth/docs/pdf2/Ambulatory_Warfarin_Guideline.pdf
Creatine Supplementation
Creatine supplementation is supported by robust evidence for enhancing high-intensity, short-duration exercise performance, increasing muscle mass, and improving strength, particularly when combined with resistance training.
The International Society of Sports Nutrition (ISSN) states that creatine supplementation increases intramuscular creatine concentrations, leading to improved performance in repeated bouts of high-intensity activity, greater training adaptations, and enhanced recovery. There is also evidence for benefits in clinical populations, including older adults (improved lean mass and strength), individuals with neuromuscular diseases, and those with creatine deficiency syndromes.
Additional potential benefits include neuroprotection, improved cognitive performance, and mitigation of muscle wasting in sarcopenia and cachexia.[1-6]
The most widely accepted dosing regimen for creatine monohydrate is an initial loading phase of 20 g/day (divided into 4 doses) for 5–7 days, followed by a maintenance dose of 3–5 g/day. Alternatively, a single daily dose of 3 g/day for 28 days achieves similar muscle creatine saturation without a loading phase. Dosing can also be weight-based (0.1 g/kg/day). These regimens are considered safe for healthy adults, with long-term supplementation (up to 30 g/day for 5 years) shown to be well-tolerated in the literature.[1][4][7-8]
Creatine monohydrate is the preferred form due to its established efficacy and safety profile.
Adverse effects are rare and generally limited to mild gastrointestinal symptoms or transient weight gain due to water retention. There is no consistent evidence of renal dysfunction or other serious adverse effects in healthy individuals.[1][4][9]
Reference:
- Antonio J, Candow DG, Forbes SC, et al. Common Questions and Misconceptions About Creatine Supplementation: What Does the Scientific Evidence Really Show?. Journal of the International Society of Sports Nutrition. 2021;18(1):13. https://doi.org/10.1186/s12970-021-00412-w.
- Forbes SC, Candow DG, Ostojic SM, Roberts MD, Chilibeck PD. Meta-Analysis Examining the Importance of Creatine Ingestion Strategies on Lean Tissue Mass and Strength in Older Adults. Nutrients. 2021;13(6):1912. https://doi.org/10.3390/nu13061912.
- Gutiérrez-Hellín J, Del Coso J, Franco-Andrés A, et al. Creatine Supplementation Beyond Athletics: Benefits of Different Types of Creatine for Women, Vegans, and Clinical Populations-a Narrative Review. Nutrients. 2024;17(1):95. https://doi.org/10.3390/nu17010095.
- Kreider RB, Kalman DS, Antonio J, et al. International Society of Sports Nutrition Position Stand: Safety and Efficacy of Creatine Supplementation in Exercise, Sport, and Medicine. Journal of the International Society of Sports Nutrition. 2017;14:18. https://doi.org/10.1186/s12970-017-0173-z.
- Balestrino M, Adriano E. Beyond Sports: Efficacy and Safety of Creatine Supplementation in Pathological or Paraphysiological Conditions of Brain and Muscle. Medicinal Research Reviews. 2019;39(6):2427-2459. https://doi.org/10.1002/med.21590.
- Cordingley DM, Cornish SM, Candow DG. Anti-Inflammatory and Anti-Catabolic Effects of Creatine Supplementation: A Brief Review. Nutrients. 2022;14(3):544. https://doi.org/10.3390/nu14030544.
- Terjung RL, Clarkson P, Eichner ER, et al. American College of Sports Medicine Roundtable. The Physiological and Health Effects of Oral Creatine Supplementation. Medicine and Science in Sports and Exercise. 2000;32(3):706-17. https://doi.org/10.1097/00005768-200003000-00024.
- Hultman E, Söderlund K, Timmons JA, Cederblad G, Greenhaff PL. Muscle Creatine Loading in Men. Journal of Applied Physiology (Bethesda, Md. : 1985). 1996;81(1):232-7. https://doi.org/10.1152/jappl.1996.81.1.232.
- Andres S, Ziegenhagen R, Trefflich I, et al. Creatine and Creatine Forms Intended for Sports Nutrition. Molecular Nutrition & Food Research. 2017;61(6). https://doi.org/10.1002/mnfr.201600772.
Creatine Evidence
Creatine supplementation is well established to enhance muscle strength, power, and lean body mass, particularly when combined with resistance training, with the most robust effects observed in males under 50 years of age. It is also effective for increasing maximal strength, work output, and fat-free mass in both athletic and non-athletic populations. In women and vegans—who often have lower baseline creatine stores—supplementation can improve physical performance and may alleviate fatigue-related symptoms. [1-2][4]
Beyond musculoskeletal benefits, creatine has demonstrated potential neuroprotective effects, with emerging evidence supporting small improvements in cognitive performance, especially under conditions of metabolic stress or in older adults.[5-6] There is also interest in its use for neurodegenerative diseases, traumatic brain injury, and mood disorders, though further large-scale trials are needed. [4-5][7]
Creatine may exert anti-inflammatory and anti-catabolic effects, potentially reducing muscle protein breakdown and bone resorption, and may support recovery from injury or immobilization.[8-9] Preliminary data suggest possible benefits in glucose metabolism, particularly when combined with exercise, but efficacy in glycemic control for type 2 diabetes remains unconfirmed. [10]
The most studied and recommended form is creatine monohydrate, typically dosed at 3–5 g daily for maintenance after an initial loading phase if desired. Safety data are robust, with no evidence of harm in healthy individuals at standard doses, though caution is advised in those with pre-existing renal disease. [4][9]
In summary, creatine supplementation is supported by current evidence for improving muscle strength, lean mass, and certain aspects of cognitive and metabolic health, with a favorable safety profile in healthy adults. [4][9][7]
Reference:
- Wang Z, Qiu B, Li R, et al. Effects of Creatine Supplementation and Resistance Training on Muscle Strength Gains in Adults <50 Years of Age: A Systematic Review and Meta-Analysis. Nutrients. 2024;16(21):3665. https://doi.org/10.3390/nu16213665.
- Delpino FM, Figueiredo LM, Forbes SC, Candow DG, Santos HO. Influence of Age, Sex, and Type of Exercise on the Efficacy of Creatine Supplementation on Lean Body Mass: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Nutrition (Burbank, Los Angeles County, Calif.). 2022 Nov-Dec;103-104:111791. https://doi.org/10.1016/j.nut.2022.111791.
- Wax B, Kerksick CM, Jagim AR, et al. Creatine for Exercise and Sports Performance, With Recovery Considerations for Healthy Populations. Nutrients. 2021;13(6):1915. https://doi.org/10.3390/nu13061915.
- Gutiérrez-Hellín J, Del Coso J, Franco-Andrés A, et al. Creatine Supplementation Beyond Athletics: Benefits of Different Types of Creatine for Women, Vegans, and Clinical Populations-a Narrative Review. Nutrients. 2024;17(1):95. https://doi.org/10.3390/nu17010095.
- Candow DG, Forbes SC, Ostojic SM, et al. "Heads Up" for Creatine Supplementation and Its Potential Applications for Brain Health and Function. Sports Medicine (Auckland, N.Z.). 2023;53(Suppl 1):49-65. https://doi.org/10.1007/s40279-023-01870-9.
- Sandkühler JF, Kersting X, Faust A, et al. The Effects of Creatine Supplementation on Cognitive Performance-a Randomised Controlled Study. BMC Medicine. 2023;21(1):440. https://doi.org/10.1186/s12916-023-03146-5.
- Balestrino M, Adriano E. Beyond Sports: Efficacy and Safety of Creatine Supplementation in Pathological or Paraphysiological Conditions of Brain and Muscle. Medicinal Research Reviews. 2019;39(6):2427-2459. https://doi.org/10.1002/med.21590.
- Cordingley DM, Cornish SM, Candow DG. Anti-Inflammatory and Anti-Catabolic Effects of Creatine Supplementation: A Brief Review. Nutrients. 2022;14(3):544. https://doi.org/10.3390/nu14030544.
- Antonio J, Brown AF, Candow DG, et al. Part II. Common Questions and Misconceptions About Creatine Supplementation: What Does the Scientific Evidence Really Show?. Journal of the International Society of Sports Nutrition. 2025;22(1):2441760. https://doi.org/10.1080/15502783.2024.2441760.
- Solis MY, Artioli GG, Gualano B. Potential of Creatine in Glucose Management and Diabetes. Nutrients. 2021;13(2):570. https://doi.org/10.3390/nu13020570.
diclofenac
The primary difference between oral diclofenac potassium and diclofenac sodium lies in their pharmacokinetic properties and clinical applications.
Diclofenac potassium is formulated for rapid absorption and quick onset of action. This makes it particularly useful for acute pain conditions where fast relief is desired. Diclofenac potassium is available in immediate-release tablets, liquid-filled soft gel capsules, and powder for oral solution, all designed to provide rapid pain relief. For example, diclofenac potassium has been shown to provide pain relief within 30 to 60 minutes, making it suitable for conditions like acute musculoskeletal pain and migraines.
Diclofenac sodium, on the other hand, is often formulated in delayed-release or extended-release forms. These formulations are designed to provide a more sustained release of the drug, which is beneficial for chronic conditions requiring long-term management, such as osteoarthritis and rheumatoid arthritis. Diclofenac sodium delayed-release tablets have a slower onset of action compared to diclofenac potassium but offer the advantage of less frequent dosing, which can improve patient compliance.
For the treatment of muscle pain, topical diclofenac is generally considered the best option due to its efficacy and safety profile. According to a systematic review by Wiffen and Xia, topical diclofenac formulations, such as diclofenac Emulgel, have shown significant effectiveness in reducing acute musculoskeletal pain with a number needed to treat (NNT) of 1.8 (95% CI 1.5-2.1).
For chronic musculoskeletal pain, topical diclofenac also demonstrates effectiveness, although the NNT is higher (9.5 [95% CI 7-14.7]), indicating it is less effective than in acute settings but still beneficial.
In summary, diclofenac potassium is preferred for rapid pain relief in acute settings, while diclofenac sodium is more suitable for chronic pain management due to its sustained release properties. Both forms are effective NSAIDs but are tailored to different clinical needs based on their pharmacokinetic profiles.
Dispose of medications
Patients should be instructed to dispose of the opioids promptly at the end of the pain episode, although this rarely occurs, and patients rarely are instructed how to do so. There are several relatively straightforward options for disposal of opioids.
The FDA and DEA allow schedule II substances to be flushed down the toilet, but the Environmental Protection Agency does not endorse this.
Many law enforcement centers have pill take-back facilities.
Pharmacies typically do not accept unused medications.
Pharmaceutical disposal bags with activated charcoal are available for safe at-home disposal. Alternatively, pills may be combined with dirt, kitty litter, or coffee grounds, crushed in a bag which is then taped shut and disposed in the regular trash.
The safest approach to disposal of fentanyl patches is to fold them on themselves and flush them down the toilet.
The best approach is the one that is most accessible to the patient, not requiring them to take their medication elsewhere.
Folic Acid Supplementation Lowers Suicide Events
Association Between Folic Acid Prescription Fills and Suicide Attempts and Intentional Self-harm Among Privately Insured US Adults
Cohort study
- Included 866,586 adults
- Folic acid treatment was associated with a significantly reduced rate of suicidal events
- This large-scale observational study confirmed results of an earlier signal-generation study.
Results Data on 866 586 patients were collected; 704 514 (81.30%) were female, and 90 296 (10.42%) were 60 years and older. Overall, there were 261 suicidal events during months covered by a folic acid prescription (5 521 597 person-months) for a rate of 4.73 per 100 000 person-months, compared with 895 suicidal events during months without folic acid (8 432 340) for a rate of 10.61 per 100 000 person-months.
Hazard ratio (HR) for folic acid for suicide events was 0.56 (95% CI, 0.48-0.65)
- With similar results for the:
- modal dosage of 1 mg of folic acid per day (HR, 0.57; 95% CI, 0.48-0.69)
- women of childbearing age (HR, 0.60; 95% CI, 0.50-0.73)
- A duration-response analysis (1 mg dosage) revealed a 5% decrease in suicidal events per month of additional treatment (HR, 0.95; 95% CI, 0.93-0.97)
The same analysis for the negative control, cyanocobalamin, found no association with suicide attempt (HR, 1.01; 95% CI, 0.80-1.27).
Reference:
- Gibbons RD, Hur K, Lavigne JE, Mann JJ. Association Between Folic Acid Prescription Fills and Suicide Attempts and Intentional Self-harm Among Privately Insured US Adults. JAMA Psychiatry. Published online September 28, 2022. https://doi.org/10.1001/jamapsychiatry.2022.2990
GLP-1 Agonists
| Medication | Freq | Titration Schedule | Equiv Doses: | |||||
|---|---|---|---|---|---|---|---|---|
| Dulaglutide | Weekly | 4 Weeks | 0.75 mg | 1.5 mg | 3-4.5 mg | |||
| Semaglutide | Weekly | 4 Weeks | 0.25 mg | 0.5 mg | 1 mg | 2 mg | ||
| Liraglutide | Daily | 1 Weeks | 0.6 mg* | 1.2 mg | 1.8 mg | |||
| Semaglutide po | Daily | 4 Weeks | 3 mg* | 7 mg | 14 mg | |||
| Tirzepatide | Weekly | 4 Weeks | 2.5 mg | 5 mg | 7.5-15 mg |
*Sensitizing dose - No glycemic impact
Reference:
Study: Tirzepatide for the Treatment of Obstructive Sleep Apnea and Obesity
Background:
- Obstructive sleep apnea is characterized by disordered breathing during sleep and is associated with major cardiovascular complications; excess adiposity is an etiologic risk factor. Tirzepatide may be a potential treatment.
Methods:
- We conducted two phase 3, double-blind, randomized, controlled trials involving adults with moderate-to-severe obstructive sleep apnea and obesity. Participants who were not receiving treatment with positive airway pressure (PAP) at baseline were enrolled in trial 1, and those who were receiving PAP therapy at baseline were enrolled in trial 2.
- The participants were assigned in a 1:1 ratio to receive either the maximum tolerated dose of tirzepatide (10 mg or 15 mg) or placebo for 52 weeks.
- The primary end point was the change in the apnea-hypopnea index (AHI, the number of apneas and hypopneas during an hour of sleep) from baseline.
- Key multiplicity-controlled secondary end points included the percent change in AHI and body weight and changes in hypoxic burden, patient-reported sleep impairment and disturbance, high-sensitivity C-reactive protein (hsCRP) concentration, and systolic blood pressure.
Results:
- At baseline, the mean AHI was 51.5 events per hour in trial 1 and 49.5 events per hour in trial 2, and the mean body-mass index (BMI, the weight in kilograms divided by the square of the height in meters) was 39.1 and 38.7, respectively.
- In trial 1, the mean change in AHI at week 52 was -25.3 events per hour (95% confidence interval [CI], -29.3 to -21.2) with tirzepatide and -5.3 events per hour (95% CI, -9.4 to -1.1) with placebo, for an estimated treatment difference of -20.0 events per hour (95% CI, -25.8 to -14.2) (P<0.001).
- In trial 2, the mean change in AHI at week 52 was -29.3 events per hour (95% CI, -33.2 to -25.4) with tirzepatide and -5.5 events per hour (95% CI, -9.9 to -1.2) with placebo, for an estimated treatment difference of -23.8 events per hour (95% CI, -29.6 to -17.9) (P<0.001).
- Significant improvements in the measurements for all prespecified key secondary end points were observed with tirzepatide as compared with placebo. The most frequently reported adverse events with tirzepatide were gastrointestinal in nature and mostly mild to moderate in severity.
Conclusions:
- Among persons with moderate-to-severe obstructive sleep apnea and obesity, tirzepatide reduced the AHI, body weight, hypoxic burden, hsCRP concentration, and systolic blood pressure and improved sleep-related patient-reported outcomes. (Funded by Eli Lilly; SURMOUNT-OSA ClinicalTrials.gov number, NCT05412004.).
Reference:
- Malhotra A, Grunstein RR, Fietze I, Weaver TE, Redline S, Azarbarzin A, Sands SA, Schwab RJ, Dunn JP, Chakladar S, Bunck MC, Bednarik J; SURMOUNT-OSA Investigators. Tirzepatide for the Treatment of Obstructive Sleep Apnea and Obesity. N Engl J Med. 2024 Jun 21. doi: 10.1056/NEJMoa2404881. Epub ahead of print. Erratum in: N Engl J Med. 2024 Oct 17;391(15):1464. doi: 10.1056/NEJMx240005. PMID: 38912654.
Study: Associations of semaglutide with incidence and recurrence of alcohol use disorder in real-world population
Alcohol use disorders are among the top causes of the global burden of disease, yet therapeutic interventions are limited. Reduced desire to drink in patients treated with semaglutide has raised interest regarding its potential therapeutic benefits for alcohol use disorders.
In this retrospective cohort study of electronic health records of 83,825 patients with obesity, we show that semaglutide compared with other anti-obesity medications is associated with a 50%-56% lower risk for both the incidence and recurrence of alcohol use disorder for a 12-month follow-up period.
Consistent reductions were seen for patients stratified by gender, age group, race and in patients with and without type 2 diabetes. Similar findings are replicated in the study population with 598,803 patients with type 2 diabetes.
These findings provide evidence of the potential benefit of semaglutide in AUD in real-world populations and call for further randomized clinicl trials.
Reference:
- Wang W, Volkow ND, Berger NA, Davis PB, Kaelber DC, Xu R. Associations of semaglutide with incidence and recurrence of alcohol use disorder in real-world population. Nat Commun. 2024 May 28;15(1):4548. doi: 10.1038/s41467-024-48780-6. Erratum in: Nat Commun. 2024 Jun 18;15(1):5177. doi: 10.1038/s41467-024-49655-6. PMID: 38806481; PMCID: PMC11133479.
Study: Semaglutide and Tirzepatide reduce alcohol consumption in individuals with obesity
Alcohol Use Disorder (AUD) contributes significantly to global mortality. GLP-1 (Glucagon-like peptide-1) and GLP-1/GIP (Glucose-dependent Insulinotropic Polypeptide) agonists, FDA-approved for managing type 2 diabetes and obesity, where the former has shown to effectively reduce the consumption of alcohol in animal models but no reports exist on the latter.
In this report, we conducted two studies.
- In the first study, we conducted an analysis of abundant social media texts. Specifically, a machine-learning based attribution mapping of ~ 68,250 posts related to GLP-1 or GLP-1/GIP agonists on the Reddit platform.
- Secondly, we recruited participants (n = 153; current alcohol drinkers; BMI ≥ 30) who self-reported either taking Semaglutide (GLP-1 agonist), Tirzepatide (the GLP-1/GIP combination) for ≥ 30 days or, as a control group; no medication to manage diabetes or weight loss for a within and between subject remote study.
In the social media study, we report 8 major themes including effects of medications (30%); diabetes (21%); and Weight loss and obesity (19%). Among the alcohol-related posts (n = 1580), 71% were identified as craving reduction, decreased desire to drink, and other negative effects. In the remote study, we observe a significantly lower self-reported intake of alcohol, drinks per drinking episode, binge drinking odds, Alcohol Use Disorders Identification Test (AUDIT) scores, and stimulating, and sedative effects in the Semaglutide or Tirzepatide group when compared to prior to starting medication timepoint (within-subjects) and the control group (between-subjects).
In summary, we provide initial real-world evidence of reduced alcohol consumption in people with obesity taking Semaglutide or Tirzepatide medications, suggesting potential efficacy for treatment in AUD comorbid with obesity.
Reference:
- Quddos F, Hubshman Z, Tegge A, Sane D, Marti E, Kablinger AS, Gatchalian KM, Kelly AL, DiFeliceantonio AG, Bickel WK. Semaglutide and Tirzepatide reduce alcohol consumption in individuals with obesity. Sci Rep. 2023 Nov 28;13(1):20998. doi: 10.1038/s41598-023-48267-2. PMID: 38017205; PMCID: PMC10684505.
Study: Exenatide once weekly for alcohol use disorder investigated in a randomized, placebo-controlled clinical trial
Background.
- Alcohol use disorder (AUD) is a chronic, relapsing brain disorder that accounts for 5% of deaths annually, and there is an urgent need to develop new targets for therapeutic intervention. The glucagon-like peptide-1 (GLP-1) receptor agonist exenatide reduces alcohol consumption in rodents and nonhuman primates, but its efficacy in patients with AUD is unknown.
Methods.
- In a randomized, double-blinded, placebo-controlled clinical trial, treatment-seeking AUD patients were assigned to receive exenatide (2 mg subcutaneously) or placebo once weekly for 26 weeks, in addition to standard cognitive-behavioral therapy. The primary outcome was reduction in number of heavy drinking days. A subgroup also completed functional MRI (fMRI) and single-photon emission CT (SPECT) brain scans.
Results.
- A total of 127 patients were enrolled. Our data revealed that although exenatide did not significantly reduce the number of heavy drinking days compared with placebo, it significantly attenuated fMRI alcohol cue reactivity in the ventral striatum and septal area, which are crucial brain areas for drug reward and addiction.
- In addition, dopamine transporter availability was lower in the exenatide group compared with the placebo group. Exploratory analyses revealed that exenatide significantly reduced heavy drinking days and total alcohol intake in a subgroup of obese patients (BMI > 30 kg/m2). Adverse events were mainly gastrointestinal.
Conclusion.
- This randomized controlled trial on the effects of a GLP-1 receptor agonist in AUD patients provides new important knowledge on the effects of GLP-1 receptor agonists as a novel treatment target in addiction.
Reference:
- Klausen MK, Jensen ME, Møller M, Le Dous N, Jensen AØ, Zeeman VA, Johannsen CF, Lee A, Thomsen GK, Macoveanu J, Fisher PM, Gillum MP, Jørgensen NR, Bergmann ML, Enghusen Poulsen H, Becker U, Holst JJ, Benveniste H, Volkow ND, Vollstädt-Klein S, Miskowiak KW, Ekstrøm CT, Knudsen GM, Vilsbøll T, Fink-Jensen A. Exenatide once weekly for alcohol use disorder investigated in a randomized, placebo-controlled clinical trial. JCI Insight. 2022 Oct 10;7(19):e159863. doi: 10.1172/jci.insight.159863. PMID: 36066977; PMCID: PMC9675448.
Study: Repurposing Semaglutide and Liraglutide for Alcohol Use Disorder
Key Points
- Question
- Are glucagon-like peptide-1 receptor (GLP-1) agonists effective in the treatment of alcohol use disorder?
- Findings
- This cohort study with a median follow-up time of more than 8 years indicates that individuals are at markedly lower risk of alcohol-related hospitalizations and hospitalizations due to somatic reasons when using GLP-1 agonists, especially semaglutide, as compared with times they are not using them.
- Meaning
- GLP-1 agonists, especially semaglutide, offer promise as a novel treatment to reduce alcohol consumption and to prevent development of alcohol-related outcomes, but randomized clinical trials are needed to verify these initial findings.
Abstract
Importance
- Preliminary studies suggest that glucagon-like peptide-1 receptor (GLP-1) agonists, used to treat type 2 diabetes and obesity, may decrease alcohol consumption.
Objective
- To test whether the risk of hospitalization due to alcohol use disorder (AUD) is decreased during the use of GLP-1 agonists compared with periods of nonuse for the same individual.
Design, Setting, and Participants
- This cohort study was an observational study conducted nationwide in Sweden using data from January 2006 to December 2023. The population-based cohort was identified from registers of inpatient care, specialized outpatient care, sickness absence, and disability pension. Participants were all residents aged 16 to 64 years who had a diagnosis of AUD.
Exposures
- The primary exposure was use of individual GLP-1 agonists (compared with nonuse of GLP-1 agonists), and the secondary exposure was medications with indication for AUD.
Main Outcomes and Measures
- The primary outcome was AUD hospitalization analyzed in a Cox regression within-individual model. Secondary outcomes were any substance use disorder (SUD)–related hospitalization, somatic hospitalization, and suicide attempt.
Results
- The cohort included 227,866 individuals with AUD; 144,714 (63.5%) were male and 83,154 (36.5%) were female, with a mean (SD) age of 40.0 (15.7) years.
- Median (IQR) follow-up time was 8.8 (4.0-13.3) years. A total of 133,210 individuals (58.5%) experienced AUD hospitalization.
- Semaglutide (4321 users) was associated with the lowest risk (AUD: adjusted hazard ratio [aHR], 0.64; 95% CI, 0.50-0.83; any SUD: aHR, 0.68; 95% CI, 0.54-0.85) and use of liraglutide (2509 users) with the second lowest risk (AUD: aHR, 0.72; 95% CI, 0.57-0.92; any SUD: aHR, 0.78; 95% CI, 0.64-0.97) of both AUD and SUD hospitalization.
- Use of any AUD medication was associated with a modestly decreased risk (aHR, 0.98; 95% CI, 0.96-1.00).
- Semaglutide (aHR, 0.78; 95% CI, 0.68-0.90) and liraglutide (aHR, 0.79; 95% CI, 0.69-0.91) use were also associated with decreased risk of somatic hospitalizations but not associated with suicide attempts (semaglutide: aHR, 0.55; 95% CI, 0.23-1.30; liraglutide: aHR, 1.08; 95% CI, 0.55-2.15).
Conclusions and Relevance
- Among patients with AUD and comorbid obesity/type 2 diabetes, the use of semaglutide and liraglutide were associated with a substantially decreased risk of hospitalization due to AUD.
- This risk was lower than that of officially approved AUD medications.
- Semaglutide and liraglutide may be effective in the treatment of AUD, and clinical trials are urgently needed to confirm these findings.
Reference:
- Lähteenvuo M, Tiihonen J, Solismaa A, Tanskanen A, Mittendorfer-Rutz E, Taipale H. Repurposing Semaglutide and Liraglutide for Alcohol Use Disorder. JAMA Psychiatry. Published online November 13, 2024. https://doi.org/10.1001/jamapsychiatry.2024.3599
Glucocorticoid Equivalents
| Steroid | Equivalent (mg) |
|---|---|
| Cortisone | 25 |
| Hydrocortisone | 20 |
| Prednisolone | 5 |
| Prednison | 5 |
| Methylprednisolone | 4 |
| Triamcinolone | 4 |
| Paramethasone | 2 |
| Betamethasone | 0.75 |
| Dexamethasone | 0.75 |
Iron (Fe) Supplementation
A serum ferritin concentration lower than 30 mcg/L suggests iron deficiency, and a value lower than 10 mcg/L suggests Iron Deficiency Anemia.
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| Birth to 6 months | 0.27 mg* | 0.27 mg* | ||
| 7–12 months | 11 mg | 11 mg | ||
| 1–3 years | 7 mg | 7 mg | ||
| 4–8 years | 10 mg | 10 mg | ||
| 9–13 years | 8 mg | 8 mg | ||
| 14–18 years | 11 mg | 15 mg | 27 mg | 10 mg |
| 19–50 years | 8 mg | 18 mg | 27 mg | 9 mg |
| 51+ years | 8 mg | 8 mg |
The average daily iron intake from foods is:
- 11.5–13.7 mg/day in children age 2–11 years
- 15.1 mg/day in children and teens age 12–19 years
- 16.3–18.2 mg/day in men and 12.6–13.5 mg/day in women older than 19
| Persons | (mg) |
|---|---|
| Infants birth to 3 years of age | 6–10 |
| Children 4 to 6 years of age | 10 |
| Children 7 to 10 years of age | 10 |
| Adolescent and adult males | 10 |
| Adolescent and adult females | 10–15 |
| Pregnant females | 30 |
| Breast-feeding females | 15 |
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| Birth to 6 months | 40 mg | 40 mg | ||
| 7–12 months | 40 mg | 40 mg | ||
| 1–3 years | 40 mg | 40 mg | ||
| 4–8 years | 40 mg | 40 mg | ||
| 9–13 years | 40 mg | 40 mg | ||
| 14–18 years | 45 mg | 45 mg | 45 mg | 45 mg |
| 19+ years | 45 mg | 45 mg | 45 mg | 45 mg |
Tolerable Upper Intake Level (UL): Maximum daily intake unlikely to cause adverse health effects
Notes:
- Expressed as an actual amount of iron, which is referred to as "elemental" iron.
- The product form [e.g., ferrous fumarate, ferrous gluconate, ferrous sulfate] has a different strength)
Iron-rich foods include:
- Lean meat and poultry.
- Seafood such as salmon.
- White beans, kidney beans, lentils and peas.
- Nuts and dried fruits.
- Green leafy vegetables such as spinach.
- Fortified bread and breakfast cereals.
Special instructions:
- Although the supplement works best on an empty stomach, you may want to take it with food so it doesn't upset your stomach.
- You shouldn't take iron supplements with milk, caffeine, antacids or calcium supplements.
- Try to take your iron supplement with vitamin C (for example, a glass of orange juice) to increase absorption.
- Medication interactions
- Levodopa - Taking Iron might reduce the amount of levodopa available to the body
- Levothyroxine - simultaneous ingestion of iron and levothyroxine can result in clinically significant reductions in levothyroxine efficacy in some patients
- Labels advise against administering levothyroxine within 4 hours of iron supplements.
- Proton pump inhibitors - Gastric acid plays an important role in the absorption of nonheme iron from the diet.
- PPIs can reduce iron absorption
To minimize side effects with supplementation, take iron with food and use slow-release versions.
Reference:
Ketamine for Depression
Ketamine has demonstrated efficacy in the treatment of depression, particularly in cases of treatment-resistant depression. Clinical studies have shown that a single intravenous infusion of ketamine at subanesthetic doses (typically 0.5 mg/kg) can produce rapid and significant antidepressant effects within hours, with peak effects observed around 24 hours post-administration. These effects can last from several days to a week.
Repeated administration of ketamine has been shown to sustain its antidepressant effects. For instance, serial dosing at intervals of 2-4 days can maintain benefits for weeks to months. Intranasal esketamine, an enantiomer of ketamine, has also been approved for use in treatment-resistant depression and has shown similar rapid antidepressant effects.
The antidepressant mechanism of ketamine is thought to involve N-methyl-D-aspartate (NMDA) receptor antagonism, leading to enhanced neuroplasticity in cortico-limbic areas of the brain. Additionally, ketamine's effects on other receptors, such as AMPA receptors and opioid receptors, may contribute to its antidepressant properties.
While ketamine is generally well-tolerated, it can cause transient dissociative and psychotomimetic effects, as well as transient increases in heart rate and blood pressure. These side effects are usually mild and transient.
In summary, ketamine is an effective and rapid-acting treatment for depression, particularly in treatment-resistant cases, with both intravenous and intranasal routes showing efficacy. Further research is needed to optimize dosing regimens and long-term safety profiles.
Reference:
- OpenEvidence
- Current Opinion in Anaesthesiology. 2021;34(5):556-562. https://doi.org/10.1097/ACO.0000000000001039.
Medication Prescription Helps
- Ozempic 0.25 or 0.5 mg/dose comes in packs of one 1.5 mL pens (total of 1.5 mL). Quantity is typically:
- 1.5 mL per 28 days (Note initiation is technically 42 days but most plans pay for only 34 or less day supplies)
- 4.5 mL per 90 days
- Ozempic 1 mg/dose comes in packs of two 1.5 mL pens (total of 3 mL). Quantity is typically:
- 3 mL per 28 days
- 9 mL per 84 days
- Qsymia - 30 day for $98
- New Patient Pack
- Qsymia 3.75 mg/23 mg - 14-day
- Qsymia 7.5 mg/46 mg 14 + 30 - 30-day $98
- Titration Pack $98
- Qsymia 11.25 mg/69 mg - 14-day
- Qsymia 15 mg/92 mg 14 + 30 - 30-day
- New Patient Pack
- Xifaxin
- Age
- Patients must be 18 years or older
- Diagnosis of IBS-D
- ICD-10 code is K58.03
- Dosing for IBS-D
- XIFAXAN 550 mg 3 times a day for 2 weeks; #42 tablets
- Coupon Card: https://xifaxan.copaysavingsprogram.com/
- Patient Assistance Program (if co-pay is >$100): https://www.bauschhealthpap.com/
- Age
- Insulin Prescribing
- Needle/Syringe Options:
- 30u insulin syringes/31 ga needles
- 50u insulin syringes/31 ga needles
- 100u insulin syringes/31 ga needles
- ReliOn NPH or Regular insulin:
- 3 ml or 10 ml vials of 100 uits/ml
- Needle/Syringe Options:
Medication Resources
Medication thoughts relating to homeless persons/street
- Albuterol
- Enhances effects of crack cocaine
- Benzodiazepines
- Sought for calming and sedation effects
- B-blockers and clonidine
- Discontinuation can result in rebound HTN
- B-blockers can exacerbate depression at initiation
- Clonidine can prolong effects of heroin and other opioids
- Buproprion
- Can be pulverized and snorted to get high
- Cough syrup
- Promethazine and codeine - called lean used with marijuana
- Calcium channel blockers, COX-2 inhibitors, NSAIDs, and DM meds
- May exacerbate heart failure
- Diuretics
- Can exacerbate dehydration
- Anticholinergic meds with diuretics
- Can cause hyperpyrexia
- Drugs metabolized in liver
- Caution in those with hepatitis and alcohol use
- Psuedoephedrine
- Can be used for methamphetamine
- Quetiapine
- Enhances the effect of heroin
- Statins
- Can worsen outcomes in those with elevated liver tranaminases, or hepatitis
References:
- AFP Vol 89 No 8 Apr 2014
Medicine Reconciliation and Medical Error
Medication errors represent the most common patient safety error.
Reference:
- Bates DW, Spell N, Cullen DJ, et al. The costs of adverse drug events in hospitalized patients.JAMA.1997;277:307–11.
More than 40 percent of medication errors are believed to result from inadequate reconciliation in handoffs during admission, transfer, and discharge of patients. Of these errors, about 20 percent are believed to result in harm.
Reference:
- Rozich JD, Howard RJ, Justeson JM, et al. Patient safety standardization as a mechanism to improve safety in health care.Jt Comm J Qual Saf.2004;30(1):5–14.
Metformin Tips
- Take with a meal to reduce the risk of stomach upset. Once-daily dosages should be taken with the evening meal.
- Metformin is usually started at a low dosage before being titrated up. Dosages may vary between individuals.
- Splitting dosages throughout the day (rather than taking a single dose) may improve gastric side effects such as nausea, diarrhea, and indigestion.
- Swallow slow-release tablets whole; do not crush, break, or chew.
- Do not drink large amounts of alcohol or drink it daily while taking metformin because this may increase your risk of lactic acidosis.
- Monitoring of blood sugars and other regular laboratory tests including kidney function are needed.
- May need to be temporarily discontinued before undergoing investigations requiring contrast media, or if you become dehydrated.
- The outer case of some slow-release metformin tablets may be visible in the stools; this does not mean the drug has not been absorbed.
- Ensure you are educated about the importance of diet and exercise in the management of type 2 diabetes because it is important to use lifestyle measures to improve your condition in addition to medications.
- Tell your doctor if you become unwell with severe vomiting, diarrhea, or a fever because these types of illnesses may lead to severe dehydration and you may need to temporarily stop metformin.
- Tell your doctor if you are pregnant or intend to become pregnant while taking metformin. It is not known how metformin affects the fetus or a breastfed infant.
Methotrexate (MTX)
Methotrexate administration:
- 10 mg - 25 mg weekly
- Once weekly as a single dose or in divided doses given over a 24-hour period.
Folic Acid Supplementation:
- The typical folic acid dosage: 1 mg by mouth daily, or 5 mg once weekly
- 1mg Example: https://amzn.to/46c4ZmD
- 5mg Example: https://amzn.to/3Rm0NfU
Pre MTX Eval
A premethotrexate evaluation is important to ensure proper patient selection for this effective but potentially toxic drug.
- A baseline chest radiograph is recommended to screen for pre-existing lung disease
- Complete blood count with differential
- Platelet count
- Serum creatinine
- Blood urea nitrogen
- Urinalysis
- Liver function tests
- Serum bilirubin
- Serum albumin
- Hepatitis A, B, and C serologies
- HIV risk assessment/testing, if appropriate Chest radiograph
Monitor for:
- Hepatotoxicity
- Monitoring of serum aspartate aminotransferase (AST) and serum albumin levels is recommended for all patients receiving methotrexate.8 These laboratory assessments were correlated with serious liver disorders in a mail survey of rheumatologists.
- Approximately 30 percent of all patients on long-term therapy have AST elevation.
- Values exceeding two times the normal level for a period of one month warrant discontinuation of therapy
- Nephrotoxicity
- Pulminary toxicity
- Symptoms include persistent dry, nonproductive cough, dyspnea or both
- Radiograph abnormalities occurring with methotrexate therapy include interstitial and alveolar infiltrates, hilar adenopathy and pleural effusion, occasionally progressing to fibrosis, scarring and honeycomb changes
- Bone marrow toxicity
- Monitoring signs of myelosuppression can reduce complications such as severe anemia, potential bleeding and sepsis.8 Patients with aplastic anemia need to be treated with leucovorin rescue.
- Labs:
- LFTs
- CBC
- CMP
- Frequency: After initiation of medical therapy with methotrexate, follow-up tests should include monitoring of CBC, renal function test, and liver function tests are recommended weekly for 4 weeks and then at least bi-monthly.
References:
- Am Fam Physician. 2000 Oct 1;62(7):1607-1612.
- https://www.ncbi.nlm.nih.gov/books/NBK556114/
Toxic effects
Major toxic effects:
- hepatic
- pulmonary
- renal
- bone marrow abnormalities
Minor toxic effects:
- stomatitis
- malaise
- nausea
- diarrhea
- headaches
- mild alopecia
Toxic effects are common but respond to folate supplementation:
- Folate supplementation with 1 mg daily or 7 mg once weekly should be considered for all patients
- Avoid taking the folate dose on the same day as the methotrexate dose.
To reduce the incidence of major toxic effects, methotrexate should never be given in daily doses.
Relative contraindications:
- renal dysfunction
- contraindicated in any patient with a creatinine clearance of less than 50 mL per minute
- liver disease
- active infectious disease
- excessive alcohol consumption
Both women and men of reproductive age should use birth control during methotrexate therapy.
Potential drug interactions:
- salicylates
- nonsteroidal anti-inflammatory drugs
- Trimethoprim/sulfamethoxazole (Bactrim, Septra) can enhance the cytotoxic effects of methotrexate because trimethoprim is an antifolate reductase inhibitor.
- Other drugs that may displace methotrexate from protein binding sites include barbiturates, phenytoin, retinoids, oral sulfonylureas and tetracycline.
Risk Factors for Potential Hepatotoxicity
Risk Factors for Potential Hepatotoxicity
- Excessive alcohol intake
- Elevated serum aspartate aminotransferase levels
- Chronic hepatitis B or C
- Increased age
- History of liver disease
- History of intravenous drug abuse
- History of inheritable liver disease
- Diabetes (insulin enhances cytotoxicity of methotrexate)
- Obesity (third spacing of methotrexate)
- History of significant exposure to known hepatotoxic drugs
Patient Education Guide for the Physician
- Tell patients to avoid alcohol including beer, wine and hard liquor because of the increased risk of liver disease.
- Inform male and female patients of reproductive age that they should practice appropriate birth control (abstinence, oral contraceptives or condom plus foam, etc.).
- Discuss potential drug interactions, especially salicylates and over-the-counter NSAIDs.
- Tell patients not to start or stop an NSAID without first checking with you.
- Tell patients to call immediately if they develop signs of infection (immunosuppression), coughing or shortness of breath (pulmonary toxicity) or unusual bleeding (liver or bone marrow suppression).
- Emphasize the weekly dose and warn patients that daily dosing of this drug is fatal. If an accidental overdose occurs, an antidote can be used (leucovorin rescue).
- Be sure that patients fully understand the need for close follow-up and monitoring for toxicity.
- The most important side effects to mention are loss of appetite, nausea (rarely vomiting), diarrhea and stomatitis. There is also the potential for serious side effects; hepatotoxicity, pulmonary toxicity, myelosuppression and nephrotoxicity.
- Warn patients about the potential development of malignancy, specifically lymphoma.
Metoprolol
Immediate release (metoprolol tartrate):
- Oral: 25 to 100 mg twice daily (AHA/ACC/HRS [January 2014])
- More frequent dosing is appropriate in the acute setting while titrating to a maintenance dose.
- Migraine prophylaxis (50-100mg bid)
- HTN
Extended release (metoprolol succinate):
- Oral: 50 to 400 mg once daily (AHA/ACC/HRS [January 2014]).
- PVCs
- Hyperthyroidism
- HTN
- CHF
Muscle Relaxers edit
The muscle relaxant with the best evidence of efficacy for muscle spasms, particularly in the context of acute musculoskeletal conditions, is cyclobenzaprine. Cyclobenzaprine has been evaluated in numerous clinical trials and has consistently demonstrated effectiveness in reducing muscle spasms, local pain, and tenderness, and improving range of motion. [1-4]
A systematic review by Chou et al. found fair evidence supporting the efficacy of cyclobenzaprine for musculoskeletal conditions, primarily acute back or neck pain, and noted that it has been evaluated in the most clinical trials among muscle relaxants.[1] Additionally, a review by Toth and Urtis highlighted that cyclobenzaprine has the most recent and largest clinical trials demonstrating its benefit for acute low back pain.[2]
In terms of dosage, cyclobenzaprine is typically administered at 5 to 10 mg three times daily, with the 5 mg dose being as effective as the 10 mg dose but associated with fewer adverse effects such as sedation.[3-4]
Overall, while other muscle relaxants like tizanidine, baclofen, and metaxalone also show some efficacy, cyclobenzaprine stands out due to the volume and consistency of evidence supporting its use for muscle spasms in acute musculoskeletal conditions.
Reference:
- Chou R, Peterson K, Helfand M. Comparative Efficacy and Safety of Skeletal Muscle Relaxants for Spasticity and Musculoskeletal Conditions: A Systematic Review. Journal of Pain and Symptom Management. 2004;28(2):140-75. https://doi.org/10.1016/j.jpainsymman.2004.05.002.
- Toth PP, Urtis J. Commonly Used Muscle Relaxant Therapies for Acute Low Back Pain: A Review of Carisoprodol, Cyclobenzaprine Hydrochloride, and Metaxalone. Clinical Therapeutics. 2004;26(9):1355-67. https://doi.org/10.1016/j.clinthera.2004.09.008.
- Borenstein DG, Korn S. Efficacy of a Low-Dose Regimen of Cyclobenzaprine Hydrochloride in Acute Skeletal Muscle Spasm: Results of Two Placebo-Controlled Trials. Clinical Therapeutics. 2003;25(4):1056-73. https://doi.org/10.1016/s0149-2918(03)80067-x.
- Food and Drug Administration Fexmid. Label via DailyMed. Updated date: 2024-08-20
Study: Comparative efficacy and safety of skeletal muscle relaxants for spasticity and musculoskeletal conditions: a systematic review
Skeletal muscle relaxants are a heterogeneous group of medications used to treat two different types of underlying conditions: spasticity from upper motor neuron syndromes and muscular pain or spasms from peripheral musculoskeletal conditions. Although widely used for these indications, there appear to be gaps in our understanding of the comparative efficacy and safety of different skeletal muscle relaxants.
This systematic review summarizes and assesses the evidence for the comparative efficacy and safety of skeletal muscle relaxants for spasticity and musculoskeletal conditions. Randomized trials (for comparative efficacy and adverse events) and observational studies (for adverse events only) that included oral medications classified as skeletal muscle relaxants by the FDA were sought using electronic databases, reference lists, and pharmaceutical company submissions. Searches were performed through January 2003.
The validity of each included study was assessed using a data abstraction form and predefined criteria. An overall grade was allocated for the body of evidence for each key question. A total of 101 randomized trials were included in this review. No randomized trial was rated good quality, and there was little evidence of rigorous adverse event assessment in included trials or observational studies.
- There is fair evidence that baclofen, tizanidine, and dantrolene are effective compared to placebo in patients with spasticity (primarily multiple sclerosis).
- There is fair evidence that baclofen and tizanidine are roughly equivalent for efficacy in patients with spasticity, but insufficient evidence to determine the efficacy of dantrolene compared to baclofen or tizanidine.
- There is fair evidence that although the overall rate of adverse effects between tizanidine and baclofen is similar, tizanidine is associated with more dry mouth and baclofen with more weakness.
- There is fair evidence that cyclobenzaprine, carisoprodol, orphenadrine, and tizanidine are effective compared to placebo in patients with musculoskeletal conditions (primarily acute back or neck pain).
- Cyclobenzaprine has been evaluated in the most clinical trials and has consistently been found to be effective.
- There is very limited or inconsistent data regarding the effectiveness of metaxalone, methocarbamol, chlorzoxazone, baclofen, or dantrolene compared to placebo in patients with musculoskeletal conditions.
- There is insufficient evidence to determine the relative efficacy or safety of cyclobenzaprine, carisoprodol, orphenadrine, tizanidine, metaxalone, methocarbamol, and chlorzoxazone. Dantrolene, and to a lesser degree chlorzoxazone, have been associated with rare serious hepatotoxicity.
Reference:
- Chou R, Peterson K, Helfand M. Comparative efficacy and safety of skeletal muscle relaxants for spasticity and musculoskeletal conditions: a systematic review. J Pain Symptom Manage. 2004 Aug;28(2):140-75. doi: 10.1016/j.jpainsymman.2004.05.002. PMID: 15276195.
My (Formulary) Goto/Easy medication choices
See also:
My (Formulary) Goto/Easy medication choices
- Emergency Headache Abortive
- Phenergan / Compazine
- HRT:
- estradiol 0.05 mg patch twice a week
- progesterone 200 mg capsule
- Monophasic ocp
- Sprintec-28
- Otitis Externa
- Neomycin - polymyxin B - hydrocortisone otic
- 10 ml
- 5 gtts in affected ear every 6-8 hours for 10 days
- Severe Contact Dermatitis
- 2 shot solution:
- Decadron + DepoMedrol
- 2 shot solution:
- Rosacea
- Metronidazole topical gel 0.75% 45 g AAA bid ($30-40)
My Medication Rules
Overall medication thoughts:
- Less is More
- Start low, go slow
No go's:
- Do not use Niacin
- Does not significantly reduce the risk of major vascular events but does increase the risk of serious adverse events. (…there were significant and excess adverse events related to gastrointestinal, musculoskeletal, infectious, and bleeding complications, as well as substantial excess adverse events related to loss of glycemic control among persons with diabetes and new-onset diabetes among persons without diabetes at baseline. Of great concern was a 9% increase in the risk of death (number needed to harm, 200) associated with niacin–laropiprant that was of borderline statistical significance (P=0.08).)
- "On the basis of the weight of available evidence showing net clinical harm, niacin must be considered to have an unacceptable toxicity profile for the majority of patients, and it should not be used routinely"
- (Effects of Extended-Release Niacin with Laropiprant in High-Risk Patients; The HPS2-THRIVE Collaborative Group; N Engl J Med 2014; 371:203-212)
- (Effects of Extended-Release Niacin with Laropiprant in High-Risk Patients; The Niacin and HDL Cholesterol — Time to Face Facts; Donald M. Lloyd-Jones, M.D.; N Engl J Med 2014; 371:271-273)
- Avoid Xanax
- Avoid Tessalon Perles - there is evidence they do not work
- Do not use TZDs
- Associated with weight gain, heart failure, and edema
- Avoid Fioricet
- Do not recommend Fish Oil for Dyslipidemia
- Do not suggest or recommend phenylephrine - It just doesn't work
- Hendeles, Leslie et al. Oral phenylephrine: An ineffective replacement for pseudoephedrine? Journal of Allergy and Clinical Immunology, Volume 118, Issue 1, 279 - 280
- Hatton RC, Hendeles L. Why Is Oral Phenylephrine on the Market After Compelling Evidence of Its Ineffectiveness as a Decongestant? Annals of Pharmacotherapy. March 2022. https://doi.org/10.1177/10600280221081526
Psychiatry:
- The best SSRI's are Lexapro (escitalopram) and Zoloft (sertraline)
- Women with depression and anxiety: Effexor (venlafaxine) or Wellbutrin (bupropion)
- Add Wellbutrin before maxing SSRI
- Consider propranolol 40 mg or hydroxyzine 25 mg instead of benzos for an executive sedative maintaining cognitive function
Specific Meds:
- HCTZ - only use the 25mg dose (12.5 doesn't do anything and 50mg just adds side effects)
- Melatonin - Use 3-4 hrs before bedtime in conjunction with sleep hygeine
- Statins - Stop at age 90 or if life expectancy is <10 years
- PPIs - Use short term (4-8 wks) only
- PPIs Associated with Increased Risk for Chronic Kidney Disease (20-50% increased risk)
- (JAMA Intern Med. Published online January 11, 2016. https://doi.org/10.1001/jamainternmed.2015.7193)
Therapies I like:
- Physical Therapy (SOR A)
- Flonase (SOR A)
- Hydroxyzine
- ASA for migraine abortive (SOR A)
- Pseudoephedrine for congestion (LOE A)
- Every elderly patient should have a dog
Conditions:
- If you use Abx for acute bacterial sinusitis, use right drug and dose (Augmentin 875mg bid and for >65yo, hospitalized, recent Abx use: use 2g bid)
- Allergic rhinitis - use flonase (or similar) using 2 sprays with opposite hand into nare once daily while looking down for proper placement
Naltrexone: Low Dose Naltrexone
- Low-dose naltrexone is as effective as amitriptyline in the treatment of painful diabetic neuropathy and has a superior safety profile (strength of recommendation [SOR], B; single randomized controlled trial [RCT]).
- Dosing comparison: maximum of 4 mg of naltrexone or 25 to 50 mg of amitriptyline
- Low-dose naltrexone significantly reduced pain by 32% in inflammatory conditions and 44% in neuropathic conditions (SOR, B; single retrospective cohort study).
- The number needed to treat to observe a ≥ 50% reduction in pain scores was 3.2
- Doses as low as 5.4 mg were found to reduce pain in 95% of patients with fibromyalgia (SOR, B; single prospective dose-response study).
- The primary outcomes were effective dose for 50% of fibromyalgia patients (3.88 mg; 95% CI, 3.39-4.35) and effective dose for 95% of fibromyalgia patients (5.4 mg; 95% CI, 4.66-6.13).
Reference:
- J Fam Pract. 2023 September;72(7):320-321 | doi: 10.12788/jfp.0654
Nitrofurantoin (Macrobid vs Macrodantin)
For UTI:
- Order Macrobid (nitrofurantoin macrocrystals-monohydrate 100 mg oral capsule) for 5 days (10)
Notes:
- Macrobid: Contains 75% nitrofurantoin monohydrate and 25% nitrofurantoin macrocrystals. It is taken twice a day and is available in 100 mg capsules.
- Macrodantin: Contains only nitrofurantoin macrocrystals and is taken four times a day, with dosages ranging from 50 mg to 100 mg.
Effectiveness: Both Macrobid and Macrodantin are similarly effective in treating UTIs.
OTC Symptom Management edit
Allergies
- fluticasone 2 sprays per nostril daily
- loratadine 10 mg daily
- fexofenadine
Congestion
- Sudafed 30-60 mg every 4 hours
Cough
- Dextromethorphan 15-30 mg every 6 hours (can be a pill or cough syrup)
Mucous (thick) and/or Post-Nasal Drip
- Guaifenessin 100-400 mg every 4 hours
Sore throats
- Ibuprofen 400 mg every 6 hours
- Lozenges with benzocaine in them
oxymetazoline (Afrin)
Limit use to no more than 3 days and adhere strictly to dosing instructions: 2-3 sprays per nostril every 10-12 hours, not exceeding 2 doses in 24 hours
Continued use of topical nasal decongestants like oxymetazoline (Afrin) more than 3 days can lead to rebound nasal congestion (rhinitis medicamentosa), where nasal congestion recurs or worsens despite ongoing treatment. This paradoxical effect results from downregulation of alpha-adrenergic receptors and subsequent vasodilation after the drug effect wears off.
Additionally, prolonged use may cause temporary discomfort such as burning, stinging, sneezing, or increased nasal discharge.
The American Academy of Allergy, Asthma, and Immunology recommends abrupt cessation as the primary strategy, rather than gradual tapering, to break the cycle of medication-induced congestion.
- Intranasal corticosteroids can be used to manage withdrawal symptoms and underlying inflammation
- Expect temporary worsening of congestion after stopping
- Restarting decongestants perpetuates the cycle
Pharmacies: Canadian Pharmacies
- MedsEngage
- Fax: 800-986-4751
- https://www.canadadrugsonline.com/
- P: 877-900-3784
- F: 866-364-9983
- https://www.liferxpharmacy.com
- https://www.canadianpharmacyking.com
- https://www.canadadrugsdirect.com
Pharmacies: Compounding Pharmacies edit
- Coastal Compounding Pharmacy
- https://www.coastalcompoundingpharmacy.com/
- 4152 W Blue Heron Blvd Suite 127
- Riviera Beach FL 33404561.683.1095561.683.0591 Fax
- https://www.viveagelessweightloss.com/compounded-semaglutide
Pharmacies: On-line Discount Pharmacies
- Amazon Pharmacy
- Blueberry Pharmacy
- Cost Plus
Pharmacies: Publix Save on Medications
$7.50/3mo
| Medication | Strength | Quantity |
|---|---|---|
| clonidine | 0.1 mg, 0.2 mg, or 0.3 mg tablet | 90 |
| clopidogrel | 75 mg tablet | 90 |
| furosemide | 20 mg, 40 mg, or 80 mg tablet | 90 |
| hydralazine | 10 mg, 25 mg, 50 mg, or 100 mg tablet | 90 |
| hydrochlorothiazide | 12.5 mg capsule; 25 mg or 50 mg tablet | 90 |
| jantoven (warfarin) | 1 mg, 2 mg, 2.5 mg, 3 mg, 4 mg, 5 mg, 6 mg; 7.5 mg, or 10 mg tablet | 90 |
| metoprolol tartrate | 25 mg, 50 mg, or 100 mg tablet | 180 |
| triamterene-HCTZ | 37.5–25 mg tablets or capsules; or 75–50 mg tablets | 90 |
| Medication | Strength | Quantity |
|---|---|---|
| glimepiride | 1 mg, 2 mg, or 4 mg tablet | 90 |
| Medication | Strength | Quantity |
|---|---|---|
| simvastatin | 5 mg, 10 mg, 20 mg, 40 mg, or 80 mg tablet | 90 |
| Medication | Strength | Quantity |
|---|---|---|
| amitriptyline HCl | 10 mg or 25 mg tablet | 90 |
| buspirone | 5 mg, 10 mg, or 15 mg tablet | 180 |
| sertraline | 25 mg, 50 mg, or 100 mg tablet | 90 |
| Medication | Strength | Quantity |
|---|---|---|
| topiramate | 25 mg, 50 mg, 100 mg, or 200 mg tablet | 180 |
| Medication | Strength | Quantity |
|---|---|---|
| ropinirole | 0.5 mg, 1 mg, 2 mg, 3 mg, 4 mg, or 5 mg tablet | 180 |
| Medication | Strength | Quantity |
|---|---|---|
| donepezil | 5 mg or 10 mg tablet | 90 |
| Medication | Strength | Quantity |
|---|---|---|
| alendronate | 35 mg or 70 mg tablet | 12 |
| Medication | Strength | Quantity |
|---|---|---|
| allopurinol | 100 mg or 300 mg tablet | 90 |
| Medication | Strength | Quantity |
|---|---|---|
| meloxicam | 7.5 mg or 15 mg tablet | 90 |
| Medication | Strength | Quantity |
|---|---|---|
| omeprazole | 20 mg capsule | 90 |
| Medication | Strength | Quantity |
|---|---|---|
| cetirizine HCl | 5 mg or 10 mg tablet | 90 |
| Medication | Strength | Quantity |
|---|---|---|
| tamsulosin | 0.4 mg capsule | 90 |
| Medication | Strength | Quantity |
|---|---|---|
| estradiol | 0.5 mg, 1 mg, or 2 mg tablet | 90 |
Publix Free Medications
Free
| Medication | Strength | Quantity |
|---|---|---|
| amlodipine | 2.5 mg, 5 mg, 10 mg | 90 |
| lisinopril | all | 180 |
| Medication | Strength | Quantity |
|---|---|---|
| metformin | 850 mg | 270 |
| metformin | 1000 mg | 225 |
| Medication |
|---|
| amoxicillin |
| ampicillin |
| SMZ-TMP (tablets) |
| Penicilliin VK |
Placebo Effects
Placebo Effects
- Patients with knee arthritis receiving either established orthopedic surgeries or a placebo "sham" surgery showed the same level of improvements in pain and function over 24 months in a clinical trial published in the New England Journal of Medicine.
- Moseley JB, O'Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, Hollingsworth JC, Ashton CM, Wray NP. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002 Jul 11;347(2):81-8. doi: 10.1056
- In a massive review of treatment outcome data reported in the British Medical Journal —including data from 232 clinical trials and over 73,000 participants — antidepressants were no more effective than placebo treatments for 85% of participants.
- Stone, M. B., Yaseen, Z. S., Miller, B. J., Richardville, K., Kalaria, S. N., & Kirsch, I. (2022). Response to acute monotherapy for major depressive disorder in randomized, placebo-controlled trials submitted to the US Food and Drug Administration: individual participant data analysis. BMJ, 378(e067606). http://dx.doi.org/10.1136/ bmj-2021-067606
- In an October 2022 paper published in JAMA, participants with chronic low back pain receiving a form of placebo spinal column stimulation showed the same level of improvement in pain disability as participants receiving cutting edge high frequency spinal column stimulation.
- Hara S, Andresen H, Solheim O, et al. Effect of Spinal Cord Burst Stimulation vs Placebo Stimulation on Disability in Patients With Chronic Radicular Pain After Lumbar Spine Surgery: A Randomized Clinical Trial. JAMA. 2022;328(15):1506–1514. https://doi.org/10.1001/jama.2022.18231
- A 2018 review of 17 studies examining placebo effects related to caffeine found that 13 out of the 17 studies demonstrated positive caffeine expectation effects — across outcomes ranging from physical endurance, strength performance, and cognitive function — with the size of these placebo/expectation effects often approaching the effects of direct caffeine consumption.
- Shabir A, Hooton A, Tallis J, F Higgins M. The Influence of Caffeine Expectancies on Sport, Exercise, and Cognitive Performance. Nutrients. 2018 Oct 17;10(10):1528. doi: 10.3390/nu10101528.
- Participants consuming a milkshake labelled as "indulgent" showed a significantly larger change in the level of their appetite hormone, ghrelin, than participants consuming a milkshake labelled "sensible", despite the two shakes containing identical calories and ingredients.
- Crum AJ, Corbin WR, Brownell KD, Salovey P. Mind over milkshakes: mindsets, not just nutrients, determine ghrelin response. Health Psychol. 2011 Jul;30(4):424-9; discussion 430-1. doi: 10.1037/a0023467.
- Researchers have administered naloxone — a drug that blocks the effects of opioids — to participants, showing that the naloxone blocks both the effects of opioid medicine and the effects of opioid placebos. This means that expectations about the effects of the opioid medicine alone — absent any active opioid medicine — can directly trigger internal analgesic biological activity.
- Amanzio M, Benedetti F. Neuropharmacological dissection of placebo analgesia: expectation-activated opioid systems versus conditioning-activated specific subsystems. J Neurosci. 1999 Jan 1;19(1):484-94. doi: 10.1523/JNEUROSCI.19-01-00484.1999.
Pregnancy
- Nausea/Vomiting:
- Likely beneficial:
- Acupressure
- Ginger
- Pyridoxine
- Unknown effectiveness:
- Acupressure
- Acupuncture
- Corticosteroids
- Prochlorperazine
- Promethazine
- Likely beneficial:
References:
- AFP Vol 92, No6 Sep 2015
Probiotics
Conditions and evidence:
- Irritable bowel syndrome
- Significantly decrease IBS symptoms, abdominal pain, bloating, flatulence
- Use Lactobacillus and Bifidobacterium species for 4-6 weeks
- LOE A
- Inflammatory bowel disease
- Induce and maintain remission in ulcerative colitis - NO benefit for Crohn's disease
- Use Lactobacillus and Bifidobacterium species for 8-12 weeks or longer
- LOE A
- Antibiotic associated diarrhea
- Reduce risk of AAD
- Use Lactobacillus alone or with Bifidobacterium species for 7 days or
- Use Saccharomyces boulardii for 5-7 days
- LOE A
- Acute infectious diarrhea
- Shorten duration and reduce severity
- Use L casei rhamnosus for 5-7 days or
- Use Saccharomyces boulardii for 5-7 days
- LOE A
- Travelor's diarrhea
- Prevent up to 85% of cases
- Use Saccharomyces boulardii for 3 weeks or
- Use Lactobacillus alone or with Bifidobacterium species for 3 weeks
- LOE B
- Eczema
- May prevent in first 2 years of life
- Galacto- and fructo-oligosaccharide (9:1 ratio) and acidic oligosaccharide in infants
- Falacto- and fructo-oligosaccharide (9:1 ratio) in infants
- LOE B
- Diabetes
- Significant reduction in at least 1 of 6 parameters of glycemic control
- Lactobacillus alone or with Bifidobacterium species for 6-8 weeks
- LOE C
JFP Vol 65 No 1 Jan 2016
—
Conditions with Strength of Recommendation (SOR) A:
- Acute Infectious Diarrhea
- Shortened duration by approx 24hrs
- Reduced risk of diarrhea lasting longer than 4 days
- Travelers Diarrhea
- Effectively prevented traveler's diarrhea in US and European travelers who visited a variety of vacation spots
- Antibiotic-associated diarrhea
- Effective for treating and preventing antibiotic-associated diarrhea - NNT=13
- No significant decrease in AAD rates in hospitalized patients over age 65
- Clostridium difficile-associated diarrhea
Conditions with Strength of Recommendation (SOR) B:
- DO NOT use for preventing or treating Crohn's disease or Ulcerative Colitis
- Multiple meta-analyses with no benefit
- Consider the probiotic Bifidobacterium bifidum MIMBb75 for patients with irritable bowel disease
- NNT=4
- In RCTs, probiotic supplements - but not yogurt containing probiotics - reduced IBS symptoms
Ref: J Fam Pract. 2015 Mar;64(3):151-155.
Procedural Sedation and Analgesia
Procedural sedation and analgesia (PSA) involves the use of short-acting analgesic and sedative medications to enable clinicians to perform procedures, while monitoring the patient closely for potential adverse effects. This process was previously (and inappropriately) termed "conscious sedation." (see 'Definitions' above.PSA may be used for any procedure in which a patient's pain or anxiety may be excessive and may impede performance. There are no absolute contraindications to PSA. Relative contraindications include: older age, significant medical comorbidities, and signs of a difficult airway. Whether the patient recently ate should be considered before performing PSA, although this may not increase aspiration risk. (See 'Indications' above and 'Contraindications and precautions' above.)The number of clinicians needed to perform PSA and the procedure safely may vary according to the patient and the procedure. In most cases, one clinician performs the procedure while another (usually a nurse) administers the sedative agents and monitors and records the patient's vital signs and clinical status. Whenever possible, we suggest that this minimum standard be met. (See 'Prerequisites and personnel' above.)Proper monitoring during PSA is crucial. The patient's blood pressure, heart rate, and respiratory rate should be measured at frequent, regular intervals; oxygen saturation (SaO2), end-tidal carbon dioxide level (EtCO2), and cardiac rhythm should be monitored continuously. (See 'Monitoring' above.)Serious complications attributable to PSA rarely occur. Significant respiratory compromise develops in less than one percent of cases. Adverse outcomes may include respiratory depression with hypoxia or hypercarbia, cardiovascular instability, vomiting and aspiration, and inadequate sedation preventing completion of the procedure. All equipment and medications necessary for airway management should be at the bedside during PSA. (See 'Complications' above and 'Equipment' above.)Ideal drugs for PSA have a rapid onset and short duration of action, maintain hemodynamic stability, and do not cause major side effects. Several medications are commonly used and no single drug is ideal for all situations (table 2). Medications used for PSA are discussed in the text. (See 'Medications' above.)PSA is most often performed in patients without major comorbidities or hemodynamic instability. In such patients, we suggest that PSA be performed using propofol (Grade 2B). Etomidate may also be used. The relative advantages and disadvantages of each drug are discussed in the text. (See 'Patients without increased risk' above.)Older patients are at increased risk of complications during PSA. Therefore, sedatives administered to older patients for PSA, regardless of the agent, should be given using a lower starting dose, slower rates of administration, and less frequent dosing intervals. (See 'Elderly patients' above.)In some circumstances, clinicians, after carefully considering the relative risks and benefits, may elect to perform PSA in patients at some increased risk of complications. In patients at risk of hypotension, we suggest that either etomidate or ketamine be used for PSA (Grade 2C). In patients who may have a potentially difficult airway or have compromised respiratory function, we suggest that ketamine be used for PSA (Grade 2C). (See 'Patients at increased risk' above.)Criteria for safe discharge following PSA are described in the text. (See 'Discharge criteria' above.)
- Fentanyl and Midazolam:
- One reasonable approach to dosing these medications when they are used together is as follows:Give midazolam first: 0.02 mg/kg (maximum 2 mg)Wait two minutes and observe patient response; give second dose of midazolam if necessaryGive fentanyl: 0.5 mcg/kgObserve patient; may repeat fentanyl dose every two minutes as necessary; titrate to effectUse smaller doses and longer intervals between doses in the elderly and patients with compromised hepatic or renal function
Drugs:
- Propofol is given by slow injection in an initial loading dose of 0.5 to 1 mg/kg IV, followed by doses of 0.5 mg/kg IV every three to five minutes as necessary until the appropriate level of sedation is achieved. It takes effect within approximately 40 seconds and its duration of action is approximately six minutes. Propofol > Etomidate as no myoclonus so likely more successful procedures.
- A sedative and amnestic but No analgesia
- Contains egg and soy - watch with allergies
- Etomidate is given IV over 30 to 60 seconds in doses of 0.1 to 0.15 mg/kg, less than the dose used for rapid sequence intubation. It can be redosed approximately every three to five minutes as needed. Etomidate's onset of action is almost immediate and its duration of effect is 5 to 15 minutes
- Myoclonus
- No analgesia
- Midazolam is usually given IV over one to two minutes in doses of 0.02 to 0.03 mg/kg. Often in adults, midazolam is given 0.5 or 1 mg at a time and titrated to effect. No single dose should exceed 2.5 mg. Repeat doses may be given every two to five minutes as necessary. Its time of onset is two to five minutes and its duration of action is 30 to 60 minutes
- Anxiolysis and amnesia but No analgesia
- Fentanyl is usually given by slow IV push in doses of 0.5 to 1 mcg/kg every two minutes until an appropriate level of sedation and analgesia is achieved. The maximum total dose is generally 5 mcg/kg or approximately 250 mcg, but higher doses may be needed in some instances. It has 75 to 125 times the potency of morphine, a rapid onset of action (two to three minutes), and a short duration of effect (30 to 60 minutes), but has no amnestic properties.
- Ketamine is generally given IV to adults, which enables immediate onset, but can be given intramuscularly. The duration of effect is 10 to 20 minutes. For PSA in adults, a dose of 1 to 2 mg/kg is given IV over one to two minutes. Doses of 0.25 to 0.5 mg/kg may be repeated every five to ten minutes thereafter.
- Because of its rapid onset, relatively short duration of action, and excellent sedative and analgesic properties, it is often used for brief, painful procedures such as fracture reduction or laceration repair.
- It produces a trance-like state and provides sedation, analgesia, and amnesia, while preserving upper airway muscle tone, airway protective reflexes, and spontaneous breathing
- Emergence reactions
Elderly:
- Sedatives administered to older patients for PSA, regardless of the agent, should be given at a lower starting dose with slower rates of administration and less frequent dosing intervals. In elderly patients without major comorbidities or hemodynamic instability, it may be best to perform PSA using an ultrashort-acting sedative such as propofol. Procedures in elderly patients with major comorbidities are probably best performed in the operating room.
Protocol for radiocontrast in high-risk patients (Contrast Allergy)
Pretreatment (optional):
- Prednisone 50mg po at 13hrs, 7hrs, and 1hr before medium injection
- Diphenhydramine 50mg IV, IM, or PO 1 hr before medium injection
Emergency
- Methylprednisolone 40mg IV or hydrocortisone 200mg IV immediately and then every 4 hours until contrast medium injetion
- PLUS diphenhydramine 50mg IV 1 hr before contrast injection
- NOTE: For IV steoids to be effective, administer less than 4-6hrs before medium injection
References:
- Consultant Oct 2017
Pseudoephedrine (Sudafed)
Effect of oral pseudoephedrine on blood pressure and heart rate: a meta-analysis
Oral pseudoephedrine is commonly used to treat symptoms of rhinitis and rhinorrhea, but its effect on blood pressure (BP) and heart rate (HR) remains uncertain. We assessed whether pseudoephedrine causes clinically meaningful elevations in HR or BP.
We searched MEDLINE, EMBASE, and the Cochrane Library for English-language, randomized placebo-controlled trials of oral pseudoephedrine treatment in adults.
The primary data extracted were systolic BP (SBP), diastolic BP (DBP), and HR. Study quality was assessed using the methods of Jadad, and data were synthesized using a random-effects model and weighted mean differences. Twenty-four trials had extractable vital sign information (45 treatment arms; 1285 patients).
Results:
- Pseudoephedrine caused a small but significant increase in SBP (0.99, mm Hg; 95% CI, 0.08 to 1.90) and HR (2.83 beats/min; 95% CI, 2.0 to 3.6), with no effect on DBP (0.63 mm Hg, 95% CI, -0.10 to 1.35).
- The effect in patients with controlled hypertension demonstrated an SBP increase of similar magnitude (1.20 mm Hg; 95% CI, 0.56 to 1.84 mm Hg).
- Higher doses and immediate-release preparations were associated with greater BP increases.
- Studies with more women had less effect on BP or HR.
- Shorter duration of use was associated with greater increases in SBP and DBP.
Reference:
- Salerno SM, Jackson JL, Berbano EP. Effect of oral pseudoephedrine on blood pressure and heart rate: a meta-analysis. Arch Intern Med. 2005 Aug 8-22;165(15):1686-94. doi: 10.1001/archinte.165.15.1686. PMID: 16087815.
- https://pubmed.ncbi.nlm.nih.gov/16087815/
Quviviq
Quviviq (daridorexant)
- Indications:
- Sleep onset and/or sleep maintenance
- Daytime somnolence
- Recommended dosage:
- 25 mg to 50 mg once nightly taken orally within 30 min before going to bed, with at least 7 hours remaining prior to planned awakening
- MoA
- Orexin receptor antagonist - blocks the binding of wake promoting neuropeptides orexin A and orexin B to receptors OX1R and OX2R suppressing the wake drive
- Notes
- No evidence of physical dependence or withdrawal symptoms upon discontinuation
- No rebound insomnia after discontinuation
- Adverse reaction rates comparable between doses and to placebo
- Control: IV
- To order:
- E-Rx:
- vitaCare Prescription Services
- 951 Yamato Rd Suite 160, Boca Raton, FL 33431
- NCPDP: #5728045
- vitaCare Prescription Services
- Fax: 800-891-4320
- Include:
- DOB
- Pt phone
- DEA Number
- Include:
- Phone: 877-478-8484
- E-Rx:
- First 30 days: $0, subsequent refills for as little as $25
- Patient Assistance Program available:
- Patients must call 877-478-8484 after prescription sent in
- Live chatting: vitacarerx.com
- https://quviviqhcp.com/support
- Sales Rep:
- Dawn Rivas
- 407-616-5574
- dawn.rivas@sales.idorsia.com
- Dawn Rivas
SGLT2 Inhibitors
- Most affordable: Brenzavvy
Sick call med list
**
:CUSTOMID: id-79b199f2-3515-4103-b899-5fc30be6f6f0 :CREATED:
- 1-2-3 mouthwash
- Acetaminophen
- Albuterol inhaler
- Amoxicillin 500mg
- Augmentin 1%
- Azithromycin 250mg
- Bacitracin Oint
- Bacitracin Opth Oint 3.5gm
- Benzoyl peroxide gel 5%
- Biaxin XL 500mg
- Bismuth subslicylate
- Calamine lotion
- Calcium 600mg
- Cepacol lozenge
- Ciprofloxacin opth oint 3%
- Clindamycin 150mg
- Clotrimazole fungal cream 1%
- Dibucain oint 1oz
- Diphenhydramine 25mg
- Docusate 100mg
- Doxycycline 100mg
- Esomeprazole 20mg
- Fiber-lax 500mg
- Fluticasone 50mcg
- Guaifenesine DM 10mg/5ml
- Hydrocortisone cream 1%
- Hydrocortisone lotion 1%
- Hydrocortisone suppository 25mg
- Hydroxyzine 25mg
- Ibuprofen 800mg
- Indomethacin 25mg
- Loperamide 2mg
- Loratadine 10mg
- Lubricant eye drops 1%
- Mucinex D 600mg
- Mupirocin oint 2%
- Muscle rub
- Naphcon A Ophth Sol
- Methocarbamol 500mg
- Naproxen 500mg
- Nergesic forte
- Ondansetron-ODT 4mg
- Oxymetazoline nasal spray 0.05%
- Prednisone 20mg
- Proctofoam HC 10gm
- Promethazine 25mg
- Psuedoephedrine 30mg
- Saline nasal spray
- SMZ-TMP DS 800/160mg
- Tolnaftate antifungal powder 1%
- Triamcinolone cream 1.10%
- Zinc oxide
Stimulants
Adverse Effects: Stimulants
The adverse effects of stimulants include the following:
- Decreased appetite - possible therapeutic effect in specific users
- Anxiety
- Jitteriness
- Headaches
- Weight loss
- Insomnia
- Psychosis
- Pruritus
- Paranoia
- Sweating
- Palpitations
- Shortness of breath
- Chest pain
- Hypertension
- Tachycardia
- Seizures
- Arrhythmias
- EKG abnormalities: inappropriate sinus tachycardia, sinus arrhythmia, prolonged QT, premature ventricular contractions, ventricular tachycardia
- Cerebrovascular event
- Sudden cardiac death
Reference:
- Farzam K, Faizy RM, Saadabadi A. Stimulants. [Updated 2023 Jul 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539896/
- https://www.ncbi.nlm.nih.gov/books/NBK539896/
Stimulant Indications
Medical Indications
- Attention deficit hyperactivity disorder (ADHD)
- Narcolepsy
- Asthma
- Obesity
- Nasal and sinus congestion
- Hypotension due to anesthesia
Reference:
- Farzam K, Faizy RM, Saadabadi A. Stimulants. [Updated 2023 Jul 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539896/
- https://www.ncbi.nlm.nih.gov/books/NBK539896/
Stimulant MOAs
- Caffeine
- Caffeine has a unique mechanism as a stimulant as it works as an inhibitor at the adenosine receptors. Agonism at these receptors induces a sensation of drowsiness, and therefore inhibition at these receptors leads to increased energy levels.
- Caffeine also increases intraocular pressure in those affected with glaucoma.[3]
- Amphetamines
- The general mechanism of action of amphetamines is the induction of catecholamines, specifically norepinephrine and dopamine. These catecholamines lead to increased energy levels, euphoria, increased libido, and higher cognition.[4] This class also includes non-therapeutic agents such as 3,4-methylenedioxymethamphetamine (MDMA, aka ecstasy), methylenedioxypyrovalerone (MDPV), and mephedrone.[5][6][7][5]
- Methylphenidate
- This drug blocks the dopamine transporter (DAT) and the norepinephrine transporter (NET), leading to increased dopamine and norepinephrine levels with the inhibition of their reuptake.[8]
- Ephedrine
- The primary mechanism of ephedrine is increased norepinephrine activity at the adrenergic receptors. Pseudoephedrine specifically works also as a nasal and sinus decongestant.[9]
- Cocaine
- The induction of most of the effects of cocaine is through the blockade of the dopamine transporter protein. This results in increased dopamine levels at the synaptic cleft, and hence the effects of dopamine become amplified.
- Pseudoephedrine
- Pseudoephedrine is a drug used as a nasal decongestant and stimulant.[10] It is a sympathomimetic agent that belongs to the amphetamine and phenethylamine drug classes. It appears in a number of over-the-counter formulations, including combinations with guaifenesin, antihistamines, acetaminophen, and dextromethorphan.
- Khat (Catha edulis)
- Khat is a flowering plant indigenous to the Arabian Peninsula and the Horn of Africa.[11] It contains a substance called cathinone, and the World Health Organization considers it a potential drug of abuse, although they do not rate it as a serious addiction risk. It is a keto-amphetamine and is banned in the USA.
- Modafinil
- This is a CNS-stimulating agent used to treat sleepiness related to obstructive sleep apnea, narcolepsy, and shift-worker disorder. It is a weak dopamine uptake inhibitor, although the precise mechanism for its stimulating effects remains unknown.
Reference:
- Farzam K, Faizy RM, Saadabadi A. Stimulants. [Updated 2023 Jul 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539896/
- https://www.ncbi.nlm.nih.gov/books/NBK539896/
Top 100 Most Prescribed Drugs in the US (2023 Data)
Based on the latest available data from the ClinCalc DrugStats Database (sourced from the 2023 Medical Expenditure Panel Survey), here is the updated list of the top 100 most commonly prescribed medications. This reflects total outpatient prescriptions filled.
- Atorvastatin - 115,271,514 prescriptions
- Metformin - 85,685,925 prescriptions
- Levothyroxine - 80,930,390 prescriptions
- Lisinopril - 76,055,039 prescriptions
- Amlodipine - 68,743,650 prescriptions
- Metoprolol - 59,547,256 prescriptions
- Albuterol - 59,546,183 prescriptions
- Losartan - 56,174,734 prescriptions
- Gabapentin - 45,964,505 prescriptions
- Omeprazole - 45,290,895 prescriptions
- Sertraline - 42,578,018 prescriptions
- Rosuvastatin - 42,103,429 prescriptions
- Pantoprazole - 37,101,751 prescriptions
- Escitalopram - 37,088,584 prescriptions
- Dextroamphetamine; Dextroamphetamine Saccharate; Amphetamine; Amphetamine Aspartate - 32,566,892 prescriptions
- Hydrochlorothiazide - 31,775,977 prescriptions
- Bupropion - 30,349,390 prescriptions
- Fluoxetine - 27,518,944 prescriptions
- Semaglutide - 25,954,066 prescriptions
- Montelukast - 25,893,501 prescriptions
- Trazodone - 24,708,571 prescriptions
- Simvastatin - 24,585,762 prescriptions
- Amoxicillin - 23,510,711 prescriptions
- Tamsulosin - 22,898,080 prescriptions
- Acetaminophen; Hydrocodone - 21,506,768 prescriptions
- Fluticasone - 21,041,607 prescriptions
- Meloxicam - 20,703,689 prescriptions
- Apixaban - 19,829,711 prescriptions
- Furosemide - 19,138,347 prescriptions
- Insulin Glargine - 18,424,802 prescriptions
- Duloxetine - 18,067,156 prescriptions
- Ibuprofen - 17,525,800 prescriptions
- Famotidine - 16,883,437 prescriptions
- Empagliflozin - 16,744,581 prescriptions
- Carvedilol - 16,566,781 prescriptions
- Tramadol - 16,010,294 prescriptions
- Alprazolam - 15,881,366 prescriptions
- Prednisone - 15,794,243 prescriptions
- Hydroxyzine - 15,272,377 prescriptions
- Buspirone - 15,229,212 prescriptions
- Clopidogrel - 15,227,565 prescriptions
- Glipizide - 15,173,475 prescriptions
- Citalopram - 14,769,554 prescriptions
- Potassium Chloride - 14,514,606 prescriptions
- Allopurinol - 14,311,839 prescriptions
- Aspirin - 14,095,181 prescriptions
- Cyclobenzaprine - 13,973,843 prescriptions
- Ergocalciferol - 13,705,855 prescriptions
- Oxycodone - 13,502,066 prescriptions
- Methylphenidate - 13,248,734 prescriptions
- Venlafaxine - 13,234,839 prescriptions
- Spironolactone - 12,777,045 prescriptions
- Ondansetron - 12,503,157 prescriptions
- Zolpidem - 11,424,127 prescriptions
- Cetirizine - 11,399,497 prescriptions
- Estradiol - 11,289,112 prescriptions
- Pravastatin - 11,060,711 prescriptions
- Hydrochlorothiazide; Lisinopril - 10,986,814 prescriptions
- Lamotrigine - 10,895,178 prescriptions
- Quetiapine - 10,655,017 prescriptions
- Fluticasone; Salmeterol - 10,648,080 prescriptions
- Clonazepam - 10,614,830 prescriptions
- Dulaglutide - 10,358,270 prescriptions
- Azithromycin - 10,337,595 prescriptions
- Hydrochlorothiazide; Losartan - 9,882,017 prescriptions
- Amoxicillin; Clavulanate - 9,831,525 prescriptions
- Latanoprost - 9,792,338 prescriptions
- Cholecalciferol - 9,737,465 prescriptions
- Propranolol - 9,699,272 prescriptions
- Ezetimibe - 9,686,244 prescriptions
- Topiramate - 9,619,219 prescriptions
- Paroxetine - 9,577,610 prescriptions
- Diclofenac - 9,438,696 prescriptions
- Budesonide; Formoterol - 9,346,242 prescriptions
- Atenolol - 9,235,305 prescriptions
- Lisdexamfetamine - 9,134,058 prescriptions
- Doxycycline - 8,823,028 prescriptions
- Pregabalin - 8,644,140 prescriptions
- Ethinyl Estradiol; Norethindrone - 8,611,956 prescriptions
- Glimepiride - 8,459,350 prescriptions
- Tizanidine - 8,292,865 prescriptions
- Clonidine - 8,128,031 prescriptions
- Fenofibrate - 8,093,230 prescriptions
- Insulin Lispro - 8,053,451 prescriptions
- Valsartan - 7,983,441 prescriptions
- Cephalexin - 7,869,737 prescriptions
- Baclofen - 7,753,150 prescriptions
- Rivaroxaban - 7,743,941 prescriptions
- Ferrous Sulfate - 7,699,088 prescriptions
- Amitriptyline - 7,568,933 prescriptions
- Finasteride - 7,546,064 prescriptions
- Dapagliflozin - 7,444,831 prescriptions
- Acetaminophen; Oxycodone - 7,283,471 prescriptions
- Folic Acid - 7,276,938 prescriptions
- Aripiprazole - 7,197,548 prescriptions
- Olmesartan - 7,175,746 prescriptions
- Ethinyl Estradiol; Norgestimate - 7,175,433 prescriptions
- Valacyclovir - 7,121,821 prescriptions
- Mirtazapine - 6,977,141 prescriptions
- Lorazepam - 6,963,899 prescriptions
Notes:
- Top 100 drugs account for ~60–65% of all Rx volume
- This list reflects drug use among ~259 million U.S. adults, with nearly 3 in 4 filling at least one of these medications in 2023.
- Assumptions:
- ~1.9 average prescriptions per user (ClinCalc estimate for high-volume drugs)
- Estimated unique users of atorvastatin:
- 115.3 million ÷ 1.9 ≈ ~60.7 million adults
- % of U.S. adult population on atorvastatin:
- 60.7M ÷ 259.2M ≈ ~23.4%
- % of U.S. adult population on atorvastatin:
- 115.3 million ÷ 1.9 ≈ ~60.7 million adults
Reference:
Topical Medications
Topical Retinoids edit
- adapalene 0.3% topical gel: $40-$50 (45 g)
- Apply small (pea-sized) amount sparingly to entire face after cleansing with nonmedicated cleanser
- tazarotene: $50-$100
- tretinoin: $50-$70
Vicks 44
From a patient:
Vicks 44 never contained codeine.
Here is an excerpt from a column I found that is interesting, especially the last sentence!
- Vicks touted the primary ingredient as something called Silentium. But as far as we can tell, what made this stuff so lovely to quaff was the absurdly high amount of alcohol in each serving. Mixed into that liquor-y bath was also an ample dollop of phenylpropanolamine, which meant that vintage Formula 44 was essentially sweet Wild Turkey with a crystal meth chaser.
And silentium apparently was dextromethorphan hydrobromide.
No wonder one felt better!
Vitamins, Minerals, and Supplements
See also:
Stats:
- 23,000 ED visits/yr are result of adverse events related to dietary supplements
| Who | Population | Supplement |
|---|---|---|
| Am Thyroid Assoc | Preg women, planning to be, breastfeeding | Iodine 150ug/d |
| Am Acad Ped | Breastfeeding women | Iodine 150ug/d |
| Breastfed and part breastfed infants | Vit D 400IU/d | |
| Children <1yo and adolescents | Vit D 600IU/d | |
| Am Geri Soc | Community dwelling adults >65yo | Vit D 1000IU/d and Ca++ |
| Endo Soc | Adults 50-70yo with 25-OH Vit D <30 | Vit D 1500-2000IU/d |
| Nat Osteopor Found | Adults <50yo | Vit D 400-800IU/d |
| Adults >50yo | Vit D 800-1000IU/d | |
| Women <50yo | Ca++ 1000mg/d | |
| Women >50yo | Ca++ 1200mg/d | |
| Men <70yo | Ca++ 1000mg/d | |
| Men >70yo | Ca++ 1200mg/d | |
| WHO | Pregnant women | Iron 30-60mg/d; folic acid 400ug/d |
| Am Acad of Fam Phys | Adults >50yo and strict vegetarians | Vit B12 1mg/d |
Other effects:
- Omega-3 fatty acid supplementation
- No effect on major adverse cardiac events, all-cause mortality, sudden cardiac death, coronary artery revascularization, or hypertension (SOR: A)
References:
- AFP Vol 97 No 9 May 2018
- Consultant Apr 2016
Study: Multivitamin Use and Mortality Risk in 3 Prospective US Cohorts
Key Points
- Question
- What is the association between long-term, daily multivitamin use and mortality in generally healthy adults?
- Findings
- In this cohort study of 390,124 generally healthy adults with more than 20 years of follow-up, daily multivitamin use was not associated with a mortality benefit.
- Meaning
- These findings suggest that multivitamin use to improve longevity is not supported.
- This cohort study examines the association of multivitamin use with mortality risk in 3 large, geographically diverse cohorts of generally healthy US adults.
Abstract
- Importance
- One in 3 US adults uses multivitamins (MV), with a primary motivation being disease prevention. In 2022, the US Preventive Services Task Force reviewed data on MV supplementation and mortality from randomized clinical trials and found insufficient evidence for determining benefits or harms owing, in part, to limited follow-up time and external validity.
- Objective
- To estimate the association of MV use with mortality risk, accounting for confounding by healthy lifestyle and reverse causation whereby individuals in poor health initiate MV use.
- Design, Setting, and Participants
- This cohort study used data from 3 prospective cohort studies in the US, each with baseline MV use (assessed from 1993 to 2001), and follow-up MV use (assessed from 1998 to 2004), extended duration of follow-up up to 27 years, and extensive characterization of potential confounders. Participants were adults, without a history of cancer or other chronic diseases, who participated in National Institutes of Health–AARP Diet and Health Study (327,732 participants); Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial (42,732 participants); or Agricultural Health Study (19,660 participants). Data were analyzed from June 2022 to April 2024.
- Exposure
- Self-reported MV use.
- Main Outcomes and Measures
- The main outcome was mortality. Cox proportional hazard models were used to estimate hazard ratios (HRs) and 95% CIs.
- Results
- Among 390,124 participants (median [IQR] age, 61.5 [56.7-66.0] years; 216,202 [55.4%] male), 164,762 deaths occurred during follow-up; 159,692 participants (40.9%) were never smokers, and 157,319 participants (40.3%) were college educated. Among daily MV users, 49.3% and 42.0% were female and college educated, compared with 39.3% and 37.9% among nonusers, respectively. In contrast, 11.0% of daily users, compared with 13.0% of nonusers, were current smokers.
- MV use was not associated with lower all-cause mortality risk in the first (multivariable-adjusted HR, 1.04; 95% CI, 1.02-1.07) or second (multivariable-adjusted HR, 1.04; 95% CI, 0.99-1.08) halves of follow-up.
- HRs were similar for major causes of death and time-varying analyses.
- Conclusions and Relevance
- In this cohort study of US adults, MV use was not associated with a mortality benefit. Still, many US adults report using MV to maintain or improve health.
Reference:
- Loftfield E, O'Connell CP, Abnet CC, Graubard BI, Liao LM, Beane Freeman LE, Hofmann JN, Freedman ND, Sinha R. Multivitamin Use and Mortality Risk in 3 Prospective US Cohorts. JAMA Netw Open. 2024 Jun 3;7(6):e2418729. doi: 10.1001/jamanetworkopen.2024.18729. PMID: 38922615; PMCID: PMC11208972.
Ashwagandha (Withania somnifera)
- 600 mg per day for 8 weeks (Lopresti 2019)
- Sexual health: A 2018 systematic review noted ashwagandha was associated with enhanced sexual behavior in females, as measured by the female sexual function index (FSFI) and female sexual distress index (FSDI), and improved spermatogenesis in males. (Azgomi 2018)
- Strength training: Ashwagandha supplementation has been associated with increased muscle mass, strength, and testosterone, and reduced muscle damage and fat mass compared to placebo. (Wankhede 2015)
- Stress and mood: Increased testosterone and reduced cortisol, anxiety, and borderline depression scores were associated with ashwagandha versus placebo. (Lopresti 2019)
- Sleep: Ashwagandha was found to benefit sleep onset latency, mental alertness, sleep quality, and anxiety versus placebo. (Langade 2021)
Reference:
- Study: A Prospective, Randomized Double-Blind, Placebo-Controlled Study of Safety and Efficacy of a High-Concentration Full-Spectrum Extract of Ashwagandha Root in Reducing Stress and Anxiety in Adults
Context:
- Stress is a state of mental or emotional strain or tension, which can lead to underperformance and adverse clinical conditions. Adaptogens are herbs that help in combating stress. Ayurvedic classical texts, animal studies and clinical studies describe Ashwagandha as a safe and effective adaptogen.
Aims:
- The aim of the study was to evaluate the safety and efficacy of a high-concentration full-spectrum extract of Ashwagandha roots in reducing stress and anxiety and in improving the general well-being of adults who were under stress.
Settings and Design:
- Single center, prospective, double-blind, randomized, placebo-controlled trial.
Materials and Methods:
- A total of 64 subjects with a history of chronic stress were enrolled into the study after performing relevant clinical examinations and laboratory tests. These included a measurement of serum cortisol, and assessing their scores on standard stress-assessment questionnaires. They were randomized to either the placebo control group or the study drug treatment group, and were asked to take one capsule twice a day for a period of 60 days.
- In the study drug treatment group, each capsule contained 300 mg of high-concentration full-spectrum extract from the root of the Ashwagandha plant.
- During the treatment period (on Day 15, Day 30 and Day 45), a follow-up telephone call was made to all subjects to check for treatment compliance and to note any adverse reactions. Final safety and efficacy assessments were done on Day 60.
Statistical Analysis:
- t-test, Mann-Whitney test.
Results:
- The treatment group that was given the high-concentration full-spectrum Ashwagandha root extract exhibited a significant reduction (P<0.0001) in scores on all the stress-assessment scales on Day 60, relative to the placebo group.
- The serum cortisol levels were substantially reduced (P=0.0006) in the Ashwagandha group, relative to the placebo group.
- The adverse effects were mild in nature and were comparable in both the groups.
- No serious adverse events were reported.
Conclusion:
- The findings of this study suggest that a high-concentration full-spectrum Ashwagandha root extract safely and effectively improves an individual's resistance towards stress and thereby improves self-assessed quality of life.
Reference:
- Chandrasekhar K, Kapoor J, Anishetty S. A prospective, randomized double-blind, placebo-controlled study of safety and efficacy of a high-concentration full-spectrum extract of ashwagandha root in reducing stress and anxiety in adults. Indian J Psychol Med. 2012 Jul;34(3):255-62. doi: 10.4103/0253-7176.106022. PMID: 23439798; PMCID: PMC3573577.
B complex
- Variable based on each B vitamin and form
- Stress and mood: B complex supplementation was found to benefit feelings of stress in healthy populations and populations "at-risk" for low mood and anxiety. (Young 2019)
- Cognitive health: B Vitamins have been shown to reduce homocysteine, and in those with elevated homocysteine, B vitamins improved global cognition, episodic memory, and semantic memory. (de Jager 2012)
- Pain: Acute low back pain may be improved through B complex supplementation as it reduced treatment duration by 50% in a 2020 meta-analysis when added to diclofenac (an NSAID). (Calderon-Ospina 2020)
- Hormonal health: B6, in particular, may improve premenstrual symptoms as a meta-analysis found an overall 2.3 fold improvement vs. placebo. (Wyatt 1999)
Reference:
Calcium
| Age | Male | Female | Pregnant | Lactating |
|---|---|---|---|---|
| 0–6 months* | 200 mg | 200 mg | ||
| 7–12 months* | 260 mg | 260 mg | ||
| 1–3 years | 700 mg | 700 mg | ||
| 4–8 years | 1,000 mg | 1,000 mg | ||
| 9–13 years | 1,300 mg | 1,300 mg | ||
| 14–18 years | 1,300 mg | 1,300 mg | 1,300 mg | 1,300 mg |
| 19–50 years | 1,000 mg | 1,000 mg | 1,000 mg | 1,000 mg |
| 51–70 years | 1,000 mg | 1,200 mg | ||
| >70+ years | 1,200 mg | 1,200 mg |
Calcium Carbonate And Calcium Citrate
- In people with low levels of stomach acid, the solubility rate of calcium carbonate is lower, which could reduce the absorption of calcium from calcium carbonate supplements unless they are taken with a meal.
- calcium carbonate is 40% calcium by weight
- Calcium citrate is less dependent on stomach acid for absorption than calcium carbonate, so it can be taken without food
- calcium citrate is 21% calcium
- In general, however, absorption of calcium supplements is greater when they are taken with food, regardless of whether the user's gastric acid is low
Adverse Effects:
- Adverse Effects:
- gastrointestinal side effects
- gas
- bloating
- constipation
- Symptoms can be alleviated by switching to a supplement containing a different form of calcium, taking smaller calcium doses more often during the day, or taking the supplement with meals.
- Calcium carbonate appears to cause more of these side effects than calcium citrate, especially in older adults who have lower levels of stomach acid.
Reference:
Green tea (Camellia sinensis)
- 300 mg, total per day, minimum of 14 days; or 1-5 cups per day of brewed green tea (1)(6)(12)
- Cohort analysis of 313,381 subjects followed for a mean of 17.3 years found that high consumption of green tea (≥ 5 cups/day) decreased all-cause mortality; moderate consumption (3-4 cups per day) decreased respiratory- and cancer-related mortality (1) https://pubmed.ncbi.nlm.nih.gov/31392470/
- Systematic review and meta-analysis of 39 cohort studies found that for each cup of tea consumed (estimated 338 mg total flavonoids), there was a decreased risk of CVD mortality (4%), CVD events (2%), stroke (4%), and all-cause mortality (1.5%) (6) https://pubmed.ncbi.nlm.nih.gov/32073596/
- Green tea extract modulated inflammation by improving total antioxidant status, myeloperoxidase and lactoferrin release (12) https://pubmed.ncbi.nlm.nih.gov/26259232/
Reference:
Herbs
Magnessium
When magnesium doesn't absorb into the body, it passes into the colon and draws a lot of water along with it. All this extra water in the colon results in diarrhea and the other digestive side effects mentioned above.
Magnesium in the aspartate, citrate, lactate, and chloride forms is absorbed more completely and is more bioavailable than magnesium oxide and magnesium sulfate.
| Mg Form | Bioavailable (less diarrhea) |
|---|---|
| aspartate | Y |
| citrate | Y |
| lactate | Y |
| chloride | Y |
| oxide | N |
| sulfate | N |
The best form of magnesium for highest absorption (ie. won't cause diarrhea) is non-buffered magnesium bisglycinate.
The "non-buffered" is key. A lot of magnesium bisglyinate (or glycinate) is "buffered", even though many companies won't specifically tell you this. If magnesium is "buffered" it means that magnesium oxide has been added and mixed in with it. So even though you may see "magnesium bisglycinate" on the front of a label, you won't know its "buffered" until you dig a little deeper.
The way to tell is you need to look at the ratio of magnesium bisglycinate to the "elemental" magnesium. If the elemental magnesium is only 10% of the magnesium bisglycinate, then it's non-buffered (aka Pure). If the elemental magnesium is over 10%, then it has been buffered with oxide.
The reason buffering exists in the first place is that it allows for more elemental magnesium to be in each capsule because magnesium oxide is very high in elemental magnesium.
Most magnesium supplements have very low bioavailability. This means they absorb very poorly in the body. Magnesium oxide, the cheapest and most popular magnesium supplement, absorbs at a rate of only about 4%.
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| Birth to 6 months | 30 mg* | 30 mg* | ||
| 7–12 months | 75 mg* | 75 mg* | ||
| 1–3 years | 80 mg | 80 mg | ||
| 4–8 years | 130 mg | 130 mg | ||
| 9–13 years | 240 mg | 240 mg | ||
| 14–18 years | 410 mg | 360 mg | 400 mg | 360 mg |
| 19–30 years | 400 mg | 310 mg | 350 mg | 310 mg |
| 31–50 years | 420 mg | 320 mg | 360 mg | 320 mg |
| 51+ years | 420 mg | 320 mg |
References:
- Magnesium Supplementation Amount and Symptom Relief
- 400 mg per day (NIH 2021a; Zhao 2019) for > 8 weeks (Mah 2021)
- Hypertension: A meta-analysis found that both serum and dietary levels of magnesium were significantly inversely associated with both coronary heart disease and cardiovascular disease overall, with effects seen between 173-457 mg per day in their model (Zhao 2019). Magnesium appears to reduce blood pressure in uncontrolled hypertensive patients at >240 mg per day. (Rosanoff 2021)
- Headaches: Magnesium has strong evidence for the prevention of migraine headaches as it was found to reduce risk by 62% in a 2020 meta-analysis. (Veronese 2020)
- Sleep: Sleep latency was found to be significantly reduced by magnesium supplementation in a 2021 meta-analysis where < 1000 mg of elemental magnesium three times per day was recommended. (Mah 2021)
- Cognitive health: A 2019 meta-analysis of observational studies showed a significant relationship between ADHD and lower serum magnesium. (Effatpanah 2019)
Reference:
- 400 mg per day (NIH 2021a; Zhao 2019) for > 8 weeks (Mah 2021)
Minerals
13 Essential Minerals
- Calcium: Calcium builds strong bones and teeth and helps in muscle contraction, blood clotting, nerve transmission, cell signaling and regulation of metabolism. The deficiency of calcium makes bone fragile and easy to fracture. Milk and dairy products, cashew, dates, broccoli, parsley and greens are good sources of dietary calcium.
- Sodium: Sodium helps in muscle contraction, conducts nerve impulses and controls the fluid balance in the body. The primary source of dietary sodium is table salt. However, salt should be taken in moderation.
- Potassium: Potassium plays a crucial role in maintaining fluid balance, muscle contraction and nerve impulse conduction. It supports brain health and reduces the risk of stroke. Low potassium causes irregular heartbeats, edema (swelling), brain damage, etc. Bananas, sweet potatoes, avocados, beets and dates are rich sources of potassium.
- Chloride: Chloride in association with sodium maintains the normal fluid balance in the body. It is used in the formation of hydrochloric acid (stomach acid) for digestion and to sustain electrical neutrality in the body. Table salt, tomatoes, celery and lettuce are rich sources of chloride.
- Magnesium: Magnesium acts as a cofactor in several enzymatic reactions and is required for the synthesis of deoxyribonucleic acid (DNA) and an antioxidant, glutathione. Green leafy vegetables, legumes, nuts, seeds and whole grains replenish dietary magnesium.
- Phosphorous: Phosphorus helps build and repair bones and teeth, helps nerves function and makes muscles contract. Phosphorus deficiency leads to bone diseases and growth restriction in children. Meats, poultry, beans, nuts, seeds and dairy products are rich sources of phosphorus.
- Iodine: It is the mineral used to produce thyroid hormones. It is necessary for the body's metabolism and physical and mental development. Phosphorus deficiency leads to impaired growth in children and metabolic disorders such as goiter and mental problems and affects menstrual health and pregnancy-related issues. Iodized table salt is the main source and is easily available.
- Iron: It is used in hemoglobin formation, which carries oxygen in the blood. Iron deficiency can lead to cellular hypoxia (decreased oxygen) and cell death. Green leafy vegetables and meats such as beef, chicken and pork are rich sources of iron.
- Zinc: This mineral aids in cell division, immunity and wound healing. Low zinc levels impair the immune system. Oysters, red meat, poultry, beans, nuts and whole grains provide major quantities of zinc.
- Copper: Copper helps in energy production and facilitates iron uptake from the gut. Chocolate, liver, shellfish and wheat bran cereals are rich sources.
- Manganese: Manganese plays an important role in protein, carbohydrate and cholesterol breakdown and cell division. Along with vitamin K, it helps in blood clotting. Whole grains, nuts, soybeans and rice are rich in manganese.
- Sulfur: Sulfur has antibacterial properties and helps fight acne-causing bacteria in the skin. It also repairs DNA damage. Seafood and legumes, especially soybeans, black beans and kidney beans are rich sources of sulfur.
- Selenium: Selenium helps prevent oxidative damage to the cells. It is also very important for the metabolism of the thyroid hormone. Brazil nuts, seafood and organ meats are good sources of selenium.
Reference:
Omega-3
- 2-4 g EPA+DHA daily for a minimum of 3 months (Abdelhamid, 2020; Elagizi, 2021; Madison, 2021; Wolters 2021)
- Cardiovascular disease and all-cause mortality: 2020 Cochrane review of 86 RCTs (n=162,796) concluded EPA+DHA reduced coronary heart disease mortality (10%), but not overall risk of CVD (primary or secondary), or all-cause mortality, noting that high intake of EPA+DHA vs low decreased triglycerides by 15%. (Abdelhamid 2020)
- Longevity and aging: 1.25-2.5 g/day of omega-3 (n-3) supplements were given to 138 individuals for 4 months and were found to be associated with improved markers of aging, including reduced levels of telomerase (24%), cortisol (33%), IL-6 (33%), and IL-10 (26%), with a note that 2.5 g/day produced superior results to 1.25 g/day. (Madison, 2021)
- Cognitive decline: In two separate systematic reviews, n-3 supplementation was associated with improvements in episodic memory (immediate recall) (Yurko-Mauro, 2015), as well as improvements in global cognition, visual memory, and executive functioning. (Masana 2017)
- Mood: A 2021 meta-analysis found n-3 supplementation to benefit depressive symptoms regardless of severity; subgroup analyses identified possible additional benefits with lower severity (no, or mild-moderate depression), and with longer treatment duration (>12 weeks). (Wolters 2021)
- Omega-3 PUFAs in middle to late aged adults decreased inflammation as demonstrated by reductions in IL-1β, TNF-α, and IL-6 (16) https://pubmed.ncbi.nlm.nih.gov/29735019/
- Improved inflammation, immune cell aging, and decreased oxidative stress by 15% in healthy sedentary overweight middle-aged and older adults; Additionally telomere lengths were found to increase when omega 6 to omega-3 ratios decreased (11) https://pubmed.ncbi.nlm.nih.gov/23010452/
- Meta-analysis of 13 RCTs found marine-sourced omega-3 supplementation was associated with decreased risk of myocardial infarction, coronary heart disease, cardiovascular disease, and related mortality, in a dose-dependent fashion (10) https://pubmed.ncbi.nlm.nih.gov/31567003/
Reference:
On Supplements
Instead of unnecessarily taking vitamins, increase the proportion of plant foods in your diet, where required vitamins and minerals are found.
Vitamin supplements are not entirely benign!
People with vitamin deficiencies do need to supplement, but do not take vitamins to prevent chronic disease.
Here is a short summary of what the current medical scientific evidence demonstrates:
Beneficial effects: - Folic acid positively affects total cardiovascular disease - Folic acid and B-vitamins positively affect stroke
Harmful effects: - Vitamin B3 (or niacin) might increase all-cause mortality - Antioxidant mixtures did not appear to benefit cardiovascular disease but might increase all-cause mortality. - Beta-carotene (vitamin A) has been linked to cancer in smokers - Vitamin E has been linked to prostate cancer
Mixed effects: - Vitamin D: uncertain if there is an all-cause mortality effect - Further studies on multivitamins (most commonly used supplement) are needed because of the marginal benefit seen in this study
Vitamin B12 /Vit B12 Deficiency
Risk factors:
- malabsorption
- Atrophic gastritis
- bariatric surgery
- celiac disease
- Crohn disease
- exocrine pancreatic insufficiency
- gastrectomy
- Ilial bowel resection
- tapeworm infestation.
- Decreased dietary intake of vitamin B12
- Alcohol use disorder
- allergy to animal products
- eating disorder
- food insecurity
- vegan or vegetarian diet
- Use of certain medications
- Histamine H2 blockers
- metformin
- nitrous oxide (recreational use)
- proton pump inhibitors
- Demographics
- older age
- pregnancy
Clinical Features:
- Cognitive
- Brain Fog
- Delirium
- Dementia
- Memory Loss
- Mood Changes
- General Fatigue
- Generalized Weaknesses
- Hematologic
- Hemolysis
- Macrocytosis
- Megaloblastic Anemia
- Pancytopenia
- Neurologic
- Ataxia
- Gait Impairment
- Peristegias
- Peripheral Neuropathy
- Proprioceptive Or Vibratory Sensation Loss
- Subacute Combined Degeneration Of The Spinal Cord
- Vision Changes
- Psychiatric
- Depression
- Hallucinations
- Psychosis
- Skin
- Glossitis
- Hyperpigmentation
- Jaundice
- Pallor
Test in patients with at least 1 risk factor for and one clinical feature of vitamin B12 deficiency
- Initial testing includes total serum vitamin B12 level, which is diagnostic for deficiency if less than 180 pg/mL.
- Borderline levels (180–350 pg/mL) warrant a methylmalonic acid measurement, which is diagnostic for vitamin B12 deficiency if elevated.
Patients without a clear cause of deficiency should undergo further testing for atrophic gastritis with a Helicobacter pylori test and evaluation for autoantibodies associated with autoimmune gastritis.
Oral vitamin B12 supplementation can be used in most patients and is noninferior to intramuscular supplementation.
Intramuscular administration should be considered in patients with severe deficiency or neurologic manifestations.
Causes of B12 deficiency:
- Dietary Deficiency
- strict vegan diet, malnutrition, reduced intake of animal products
- Decreased Intrinsic Factor Production
- pernicious anemia, gastrectomy, atrophic gastritis, H. pylori
- Decreased ileal B12 absorption
- crohn's disease, celiac disease, tuberculosis of intestine, ileal resection
- Competition for B12 in gut
- alcoholism, bacterial overgrowth, parasites – giardiasis/fish tapeworm
- Increased B12 requirements
- hemolysis, HIV infection
- Medications
- metformin, colchicine, cholestyramine, slow-release KCL
- Inherited/Autoimmune diseases
- Imerslund-Grasbeck syndrome (intrinsic factor receptor defect), pernicious anemia, transcobalamin deficiency, cobalamin mutation (C-G-1 gene), cbID inborn error of cobalamin metabolism
- Other
- pancreatic insufficiency, Zollinger-Ellison syndrome, Nitrous Oxide abuse
Supplementation daily dose:
- 500 mcg sublingual like:
| Birth to 6 months* | 0.4 mcg | 0.4 mcg | ||
|---|---|---|---|---|
| 7–12 months* | 0.5 mcg | 0.5 mcg | ||
| 1–3 years | 0.9 mcg | 0.9 mcg | ||
| 4–8 years | 1.2 mcg | 1.2 mcg | ||
| 9–13 years | 1.8 mcg | 1.8 mcg | ||
| 14–18 years | 2.4 mcg | 2.4 mcg | 2.6 mcg | 2.8 mcg |
| 19+ years | 2.4 mcg | 2.4 mcg | 2.6 mcg | 2.8 mcg |
Elevated Vitamin B12 levels (greater than 1,000 pg/mL on two measurements) are associated with:
- solid tumors
- hematologic malignancy
- increased risk of cardiovascular death
Workup for elevated B12:
- CBC
- CMP
- liver ultrasound
- routine cancer screening should be up to date
- Rule out exogenours vit B12 ingestion
Reference:
Vitamin C for preventing and treating the common cold
Regular ingestion of vitamin C had no effect on common cold incidence in the ordinary population, based on 29 trial comparisons involving 11,306 participants.
However, regular supplementation had a modest but consistent effect in reducing the duration of common cold symptoms, which is based on 31 study comparisons with 9745 common cold episodes.
In five trials with 598 participants exposed to short periods of extreme physical stress (including marathon runners and skiers) vitamin C halved the common cold risk. The published trials have not reported adverse effects of vitamin C.
Trials of high doses of vitamin C administered therapeutically, starting after the onset of symptoms, showed no consistent effect on the duration or severity of common cold symptoms. However, only a few therapeutic trials have been carried out and none have examined children, although the effect of prophylactic vitamin C has been greater in children. One large trial with adults reported benefit from an 8g therapeutic dose at the onset of symptoms, and two therapeutic trials using five-day supplementation reported benefit. More trials are necessary to settle the possible role of therapeutic vitamin C, meaning administration immediately after the onset of symptoms.
Authors' conclusions:
- The failure of vitamin C supplementation to reduce the incidence of colds in the general population indicates that routine vitamin C supplementation is not justified, yet vitamin C may be useful for people exposed to brief periods of severe physical exercise.
- Regular supplementation trials have shown that vitamin C reduces the duration of colds, but this was not replicated in the few therapeutic trials that have been carried out.
- Nevertheless, given the consistent effect of vitamin C on the duration and severity of colds in the regular supplementation studies, and the low cost and safety, it may be worthwhile for common cold patients to test on an individual basis whether therapeutic vitamin C is beneficial for them.
Reference:
- Hemilä H, Chalker E. Vitamin C for preventing and treating the common cold. Cochrane Database of Systematic Reviews 2013, Issue 1. Art. No.: CD000980. DOI: 10.1002/14651858.CD000980.pub4
Vitamin D
Conditions and Patient Oriented Effects of Vitamin D Supplementation
- Adverse pregnancy outcomes:
- Possible increase in birth weight, no other definitive maternal or neonatal benefits; prenatal vitamins include recommended amounts of vitamin D
- Asthma:
- Does not improve control of asthma or enhancement of corticosteroid responsiveness
- COPD Exacerbation:
- No therapeutic effect overall; Possible benefit from small trials in those deficient in Vit D
- Depression:
- No therapeutic effect
- Diabetes mellitus:
- Does not prevent or help treat glucose intolerance
- Fatigue:
- Does not increase energy in postmenopausal women or in patients with chronic fatigue syndrome
- Heart failure:
- Small increase in ejection fraction, no increase in walking distance
- Hypertension:
- Does not lower blood pressure or prevent hypertension
- Menopausal symptoms:
- No therapeutic effect in Women's Health Initiative study
- Nonspecific musculoskeletal pain:
- Does not decrease symptoms
- Osteoarthritis:
- No improvement in pain or cartilage loss
- Upper respiratory infection:
- No effect on incidence of infection
References:
- AFP Vol 97 No 4 Feb 2018
- Vitamin D Supplementation edit
- 800-3000 IU per day for ~6 months (Gao 2017; Jolliffe 2021; NIH 2021)
- Upper limit (UL) of vitamin D is 4,000 IU per day (NIH 2021)
- All-cause mortality: A 2017 systematic review of meta-analyses (MAs) on vitamin D found that 8 of 12 MAs showed a significant correlation between vitamin D and reduced all-cause mortality; (Rejnmark 2017) the most recent MA on D3 found a risk reduction of 11%. (Chowdhury 2014)
- Immune health: A 2021 MA of 46 randomized controlled trials (n=75,541) found that 400-1,000 IU/day of vitamin D safely reduced acute respiratory infection (ARI) risk by 8% (Jolliffe 2021); vitamin D may also play a role in autoimmune health. (Antico 2012)
- Musculoskeletal health: With regards to aging and arthritis, a 2017 MA found doses of vitamin D over 2000 IU to improve pain and function scores in knee osteoarthritis. (Gao 2017)
- Mood: A 2019 meta-analysis found an association between vitamin D and moderate effect size improvements in symptoms of major depression. (Vellekkatt 2019)
- Systematic review and meta-analysis of 52 trials found a decrease in all-cause mortality with vitamin D3 supplementation and a decrease of 16% for risk of cancer death (20) https://pubmed.ncbi.nlm.nih.gov/31405892/
- Meta-analysis of 159 trials found vitamin D3 to decrease mortality in independently living and institutionalized care elderly (3) https://pubmed.ncbi.nlm.nih.gov/24414552/
- Systematic review and meta-analysis of 73 cohort studies and 22 randomized controlled trials found an inverse association of vitamin D levels with risk of cardiovascular disease, cancer, and all-cause mortality; supplementation decreased overall mortality in older adults (5) https://pubmed.ncbi.nlm.nih.gov/24690623/
- Meta-analysis of 42 randomized controlled trials found a decrease in all-cause mortality when supplemented long term (3 years or more) (21) https://pubmed.ncbi.nlm.nih.gov/24349197/
Reference:
- Vitamin D dosing & Falls in elderly
What is known:
- Vitamin D deficiency linked to decrease muscle mass and increased falls/fractures.
- Vitamin D synthesis in skin decreases with age.
- Vitamin D with calcium widely acknowledged to reduce risk of falls in elderly
Daily dosing guidelines
- American Geriatric Society and Institute of Medicine Guidelines recommend supplement (1000IU or higher) to achieve daily total of 4000 IU daily of Vitamin D in elderly patients with recent fall history.
- Some critics argue the 4000IU dose may be too high and recommend 800-2000 IU/day.
References:
- Vitamin D edit
Effects of Vitamin D Supplementation on Medical Conditions Conditions Patient-oriented effects
Adverse pregnancy outcomes28–30
Possible increase in birth weight, no other definitive maternal or neonatal benefits; prenatal vitamins include recommended amounts of vitamin D
Asthma31–33
Does not improve control of asthma or enhancement of corticosteroid responsiveness
Chronic obstructive pulmonary disease exacerbation34–36
No therapeutic effect overall; two trials showed benefit in a subgroup of patients deficient in vitamin D
Depression37–41
No therapeutic effect
Diabetes mellitus42–45
Does not prevent or help treat glucose intolerance
Fatigue27,46–48
Does not increase energy in postmenopausal women or patients with chronic fatigue syndrome
Heart failure49,50
Small increase in ejection fraction, no increase in walking distance
Hypertension51,52
Does not lower blood pressure or prevent hypertension
Menopausal symptoms27,46,47
No therapeutic effect in Women's Health Initiative study
Nonspecific musculoskeletal pain53–55
Does not decrease symptoms
Osteoarthritis56,57
No improvement in pain or cartilage loss
Upper respiratory tract infection58–60
No effect on incidence of infection
Fish Oil:
- Does not decrease total mortality, cardiovascular events, or cancer incidence
- Should not be recommended to decrease dyslipidemia
- SOR A
Reference:
- (Clinical Inquiry; AFP Vol 89 No 4 Feb 2014)
Testosterone
Study: Association of specific symptoms and metabolic risks with serum testosterone in older men
Notes:
- Testosterone levels can be converted between nanomoles per liter (nmol/L) and nanograms per deciliter (ng/dL) using specific conversion factors. To convert from nmol/L to ng/dL, multiply by 28.84
Context:
- Although attention and concern about health disorders in aging men have been growing, the structure of psychological and somatic complaints of actual patients, not population-based cohorts, has not been elucidated in relation to sex hormone patterns and metabolism.
Objective:
- The objective of the study was investigation of factors influencing complaint structures in aging male patients.
Design:
- This was a cross-sectional cohort study.
Setting:
- The study was conducted in an andrological outpatient department.
Patients:
- Subjects included 434 consecutive male patients aged 50-86 yr.
Main outcome measures:
- The following hypotheses were measured: 1) psychosomatic complaints and metabolic factors in aging male patients are related to sex hormone levels in a symptom-specific manner, and 2) patients form subcohorts.
Results:
- A clear-cut threshold for late-onset hypogonadism was not found; rather, prevalence of psychosomatic symptoms and metabolic risk factors accumulated with decreasing androgen levels.
- For example:
- Androgen-induced prevalence of loss of libido or vigor increased below testosterone concentrations of 15 nmol/liter (P < 0.001)
- 432.6 ng/dl
- Depression and diabetes mellitus type 2 (also in nonobese men) were significantly more present in men with testosterone concentrations below 10 nmol/liter (P < 0.001)
- 288.4 ng/dl
- Erectile dysfunction was identified as a composite pathology of metabolic risk factors, smoking, and depressivity, whereas only testosterone concentrations below 8 nmol/liter contributed to that symptom (P = 0.003)
- 230.72 ng/dl
- Androgen-induced prevalence of loss of libido or vigor increased below testosterone concentrations of 15 nmol/liter (P < 0.001)
- Cluster analysis revealed aging men to present within three independent groups characterized by psychosomatic complaints, metabolic disorders, and sexual health problems. These subgroups of patients exhibit distinct features in terms of androgen levels, age, and body mass index.
Conclusions:
- There is no evidence that a uniform structure of testosterone concentrations and complaints exists within the cohort of elderly male patients. Rather, in aging male patients, psychosomatic complaints and metabolic risk relate to testosterone in a symptom-specific manner.
Reference:
- Zitzmann M, Faber S, Nieschlag E. Association of specific symptoms and metabolic risks with serum testosterone in older men. J Clin Endocrinol Metab. 2006 Nov;91(11):4335-43. doi: 10.1210/jc.2006-0401. Epub 2006 Aug 22. PMID: 16926258.
Study: Testosterone administration reduces lying in men
Lying is a pervasive phenomenon with important social and economic implications. However, despite substantial interest in the prevalence and determinants of lying, little is known about its biological foundations.
Here we study a potential hormonal influence, focusing on the steroid hormone testosterone, which has been shown to play an important role in social behavior.
In a double-blind placebo-controlled study, 91 healthy men (24.32±2.73 years) received a transdermal administration of 50 mg of testosterone (n=46) or a placebo (n=45). Subsequently, subjects participated in a simple task, in which their payoff depended on the self-reported outcome of a die-roll. Subjects could increase their payoff by lying without fear of being caught.
Our results show that testosterone administration substantially decreases lying in men. Self-serving lying occurred in both groups, however, reported payoffs were significantly lower in the testosterone group (p<0.01).
Our results contribute to the recent debate on the effect of testosterone on prosocial behavior and its underlying channels.
Reference:
- Wibral M, Dohmen T, Klingmüller D, Weber B, Falk A. Testosterone administration reduces lying in men. PLoS One. 2012;7(10):e46774. doi: 10.1371/journal.pone.0046774. Epub 2012 Oct 10. PMID: 23071635; PMCID: PMC3468628.
CGM Standard Written Order edit
- Demographics
- Diagnosis: E10.9, E11.65E, E10.65, E11.8, E11.9, O24
- Reason for CGM:
- Insulin treated (1,2,3+ insulin administrations/day)
- Insulin pump
- History of problematic hypoglycemia
- Duration: LIFETIME (99) or Other
Devices:
- FreeStyle Libre 2 with FreeStyle Libre 2 sensor
- Use per manufacturer guidelines in accordance with FDA indications for use.
- Change sensor every 14 days.
- Dispense 6 sensors/84 days OR 7 sensors/98 days.
- FreeStyle Libre 3 reader with FreeStyle Libre 3 sensor
- Use per manufacturer guidelines in accordance with FDA indications for use.
- Change sensor every 14 days.
- Dispense 6 sensors/84 days OR 7 sensors/98 days.
DME Suppliers edit
| Supplier | Phone | Fax |
|---|---|---|
| Advanced Diabetes Supply | 866-976-9110 | 760-496-0234 |
| Better Living Now/Rotech | 800-854-5729 | 877-262-2179 |
| Bridgewater Health Supplies | 800-974-2055 | 877-297-5127 |
| Byram Healthcare/Apria | 800-775-4372 | 866-387-1127 |
| Ccs Medical | 800-599-7521 | 800-557-8256 |
| Diabetes Management & Supplis/Adapthealth | 888-738-7929 | 504-407-2083 |
| Edgepark Medical Suplies | 844-619-4650 | 866-510-6583 |
| Edwards Health Care Services | 800-951-1725 | 502-657-0237 |
| J&B Medical Supply | 800-737-0045 | 800-737-0012 |
| Mini Pharmacy | 888-545-6464 | 800-280-2939 |
| Quest Health Solutions | 877-888-7050 | 866-422-5283 |
| Solara Medical Supplies/Adapthealth | 844-381-8032 | 800-999-7021 |
| Total Medical Suply | 877-670-1120 | 877-670-1121 |
| United States Medical Supply | 877-270-6508 | 866-347-8544 |
| Us Healthliknk | 855-421-2732 | 407-440-8122 |
E-prescribing DME:
Endocrine
Endocrine Lab Tests:
- Corticotropin (ACTH) stimulation test is gold standard for diagnosing adrenal insufficiency
- Alternative: Both morning ACTH and cortisol levels
- Dexamethasone suppression test evaluates Cushings
Cortisol Levels are likely Good
The brain releases a hormone called ACTH, which acts on the adrenal gland and tells it to release cortisol," she says. "When the brain senses that there is enough cortisol in the blood, it stops releasing ACTH. It's a feedback loop."
Increased cortisol levels can be caused by an increase in stress.
wellness influencers can often blame symptoms of stress on "high cortisol," and the relationship isn't so straightforward. After all, stress and anxiety can cause issues like poor sleep, muscle tightness, and irritability — but whether those symptoms are all directly caused by high levels of cortisol is hard to say.
However, there are certain medical conditions associated with abnormally high levels of cortisol, particularly Cushing's Syndrome. The rare condition is often caused by a tumor in the pituitary gland, which helps regulate the production of cortisol by the adrenals, or long-term use of glucocorticoid medication. It's typically marked by a redistribution of weight in the face, abdomen and upper back, in addition to blood sugar elevation, blood pressure elevation, skin markings (that look like stretch marks), and bone weakness, Dr. Gover explains.
Here are some of the most common symptoms of clinically high cortisol levels:
- Easy skin bruising
- Increased fat especially on the face and midsection
- Pink or purple striae/stretchmarks
- High blood pressure
- Bone loss
- Menstrual irregularities
- Mood changes
Extremely low cortisol levels are typically associated with Addison's disease, a condition that occurs when the adrenals don't produce enough of the hormone. It's characterized by symptoms such as lethargy, low appetite and low blood pressure, Dr. Ampadu explains.
If you have an underactive pituitary gland or a pituitary tumor, it can also limit ACTH production, per the Cleveland Clinic: "ACTH signals your adrenal glands to make cortisol, so limited ACTH results in limited cortisol production."
Low cortisol levels related to Addison's disease:
- Muscle weakness
- Abdominal pain
- Chronic fatigue
- Dizziness or feeling faint
- Low blood pressure
- Low blood sugar
- Mood swings
- Changes in skin color (noticeable darkening or bronzing of the skin)
Balance Your Cortisol Levels
Persistently elevated cortisol can lead to negative long-term health consequences on your blood pressure, immune system, cardiovascular health, and weight, per Dr. Gover. So "balancing your cortisol levels" — and more precisely, managing your stress levels — can be important.
"But balancing cortisol isn't done with medications or supplements or novel therapeutics," Dr. Gover says. It is done by regulating your sleep, nutrition, and emotional stress. Physical activity can help as well
- Sleep: Restful and restorative sleep is critical in balancing cortisol. Dr. Gover suggests seven to eight hours of sleep per night. "If you're awakening in the night or getting disturbance in your sleep, you may be releasing cortisol at times when it should not be released," she says. There are many reasons why sleep can be disturbed and she breaks them down into three buckets: external factors like street noise or work schedule; physical ailments like restless leg or sleep apnea; and internal factors like stress, anxiety. Another common impediment to sleep is alcohol use. Assessing these buckets to see where you're falling short on Zzz's can be crucial in helping to balance your cortisol.
- Physical activity: It's a wonderful stress reliever, for both for your body and your mind, Dr. Gover say. "It is a great use of the energy cortisol gives your body. It can also act as a mini-break in your day and can create space to clear your mind."
- Emotional stress relief: For this, Dr. Gover recommends mindfulness-based activities, particularly meditation, being in nature, breathwork, and journaling. "The way that these activities can help with stress is that they train the mind/brain to recognize stress and to recognize the body's reaction to stress," she says.
- Nutrition: The picture with nutrition isn't as clear. "Cortisol can lead to conditions like IBS due to the brain-gut connection and may affect the gut microbiome. Plant-based diets have a very positive impact on the gut microbiome. So, this could counteract the effects of cortisol, theoretically," she says.
Because there is not a pill or specific treatment "for cortisol," Dr. Gover doesn't recommend seeing your doctor about cortisol. She does however recommend seeing your PCP if you're experiencing high levels of stress that are impacting you emotionally (anxiety, worry) or physically (poor sleep, poor diet, lack of physical activity, unexpected weight changes). Your healthcare provider will be able to advise you on certain lifestyle changes or in the case of Addison's or Cushing's, specific treatment options.
Reference:
Cushing Syndrome
| Feature | Proportion |
|---|---|
| Obesity or weight gain | 95% |
| Facial plethora | 90% |
| Rounded face | 90% |
| Decreased libido | 90% |
| Thin skin | 85% |
| Decreased linear growth | 70–80% |
| Menstrual irregularity | 80% |
| Hypertension | 75% |
| Hirsutism | 75% |
| Depression or emotional lability | 70% |
| Bruising easily | 65% |
| Glucose intolerance | 60% |
| Weakness | 60% |
| Osteopenia or fracture | 50% |
| Nephrolithiasis | 50% |
We recommend testing for Cushing's syndrome in the following groups:
- Patients with unusual features for age (e.g. osteoporosis, hypertension)
- Patients with multiple and progressive features, particularly those that are more predictive of Cushing's syndrome
- Children with decreasing height percentile and increasing weight
- Patients with adrenal incidentaloma compatible with adenoma
Screening tests for endogenous Cushing syndrome
- After an exogenous cause has been excluded, diagnostic tests are used to determine if hypercortisolism is indeed present.
- Testing at least twice for cortisol levels in urine and saliva is recommended.
- Abnormal test results should prompt referral to an endocrinologist for an assessment of the likelihood of Cushing syndrome.
For the initial testing for Cushing's syndrome, we recommend one of the following tests based on its suitability for a given patient:
- Urine free cortisol (UFC; at least two measurements)
- Urinary free cortisol and late-night salivary cortisol tests require at least two or three separate collections due to variation in consecutive test results in up to one-half of patients.
- Late-night salivary cortisol (two measurements)
- Patients with adrenal disease usually do not have high levels of salivary or urinary cortisol; Patients who work night shifts or have a disrupted circadian rhythm may have high cortisol levels at night.
- Late-night salivary cortisol test is the most specific
- 1-mg overnight dexamethasone suppression test (DST)
- A dexamethasone suppression test is the preferred initial test if an adrenal tumor is suspected and for patients who work night shifts or have a disrupted circadian rhythm.
- Dexamethasone suppression and late-night salivary cortisol tests have the highest sensitivity
- Longer low-dose DST (2 mg/d for 48 h)
When two different tests demonstrate elevated cortisol levels in a patient with a high probability for Cushing's syndrome, the diagnosis is confirmed; typically, two negative test results exclude a diagnosis of Cushing's syndrome.
In individuals with at least one abnormal test result (for whom the results could be falsely positive or indicate Cushing's syndrome), we recommend further evaluation by an endocrinologist to confirm or exclude the diagnosis
After confirmation of hypercortisolism, plasma ACTH measurement is used to determine whether the cause is ACTH dependent or ACTH independent
- When ACTH is low (due to an ACTH-independent cause), adrenal computed tomography or magnetic resonance imaging should be performed to identify unilateral or bilateral adrenal causes.
- When ACTH is normal or high (due to an ACTH-dependent cause), pituitary magnetic resonance imaging should be performed to confirm Cushing's disease caused by an adenoma.
Conditions associated with hypercortisolism in the absence of Cushing's syndrome:
- Some clinical features of Cushing's syndrome may be present
- Pregnancy
- Depression and other psychiatric conditions
- Alcohol dependence
- Glucocorticoid resistance
- Morbid obesity
- Poorly controlled diabetes mellitus
- Unlikely to have any clinical features of Cushing's syndrome
- Physical stress (hospitalization, surgery, pain)
- Malnutrition, anorexia nervosa
- Intense chronic exercise
- Hypothalamic amenorrhea
- CBG excess (increased serum but not urine cortisol)
First-line therapy for Cushing syndrome due to endogenous overproduction of cortisol is surgery to remove the causative tumor.
Many patients will require additional treatment with medications, radiation, or bilateral adrenalectomy.
| Cause | Prev |
|---|---|
| Depression | 2-4% |
| Alcohol dependence | 4.9% |
| Glucocorticoid resistance | Unclera - likely seldom |
| Obesity | 5-12% |
| Diabetes | 6.4% |
| Pregnancy | 0.5-1.5% of femal pop |
| Prolonged physical exertion | Unclear |
| Malnutrition | <40% in hosp pop |
| Corisol binding globulin excess | Unclear |
| Route of administration of steroids | Examples of steroids |
|---|---|
| Oral | Prednisone, dexamethasone, methylprednisolone, megestrol acetate,1 supplements containing betamethasone,2 some Chinese herbs (especially those with anti-inflammatory properties)3 |
| Inhalation* | Fluticasone when used with protease inhibitors in the treatment of HIV;4 budesonide used with itraconazole in patients with cystic fibrosis5 |
| Topical† | Skin lightening cosmetic creams,6 ointments, clobetasol7 |
| Ocular | Glucocorticoid-containing eye drops8 |
| Intradermal or intra-articular injection§ | Triamcinolone9,10 |
| Nasal§ | Betamethasone11 |
| Rectal | Betamethasone12 |
| Nerve block injection | Methylprednisone13 |
| Test | Quest Code | Result suggestive of Cushing syndrome | Principle of test | Remarks |
|---|---|---|---|---|
| 24-hour urinary excretion of cortisol | 14534 ($166.08) | Cortisol level is above upper limit of normal range | Confirms that cortisol secretion is elevated | Sensitivity to test is reduced if creatinine clearance < 60 mL/min per 1.73 m2 |
| Overnight suppression of dexamethasone 1 mg | Cortisol level > 50 nmol/L at 8:00–9:00 am | Shows loss of normal sensitivity to negative feedback | Not accurate when cortisol-binding globulin is altered (e.g., by use of birth control pill) | |
| Level of cortisol in saliva | 93020 ($205.97) | Late-night cortisol level > 4 nmol/L | Shows loss of normal diurnal rhythm of cortisol | Test is not available at all laboratories |
| Pathology | Hormone Levels in the Body | Responsible Organ |
|---|---|---|
| Primary | ↑↑Cortisol, ↓↓ACTH, ↓↓CRH | Adrenal Gland |
| Secondary (Cushing's Disease) | ↑↑Cortisol, ↑↑ACTH, ↓↓CRH | Pituitary Gland |
| Tertiary | ↑↑Cortisol, ↑↑ACTH, ↑↑CRH | Hypothalamus |
References:
- The Diagnosis of Cushing's Syndrome: An Endocrine Society Clinical Practice Guideline
- Late-Night Salivary Cortisol as a Screening Test for Cushing's Syndrome
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2845687/
- https://www.labce.com/spg1380052_secondary_hyperadrenalism_cushings_disease.aspx
- JAMA Jul 2023 Vol 330 No 2
- Nieman LK, Biller BM, Findling JW, Newell-Price J, Savage MO, Stewart PM, Montori VM. The diagnosis of Cushing's syndrome: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2008 May;93(5):1526-40. doi: 10.1210/jc.2008-0125. Epub 2008 Mar 11. PMID: 18334580; PMCID: PMC2386281.
- Maness DL, Studebaker G, Knight CM. Cushing's Syndrome: Rapid Evidence Review. Am Fam Physician. 2024 Sep;110(3):270-280. PMID: 39283850.
- Reincke M, Fleseriu M. Cushing Syndrome: A Review. JAMA. 2023 Jul 11;330(2):170-181. doi: 10.1001/jama.2023.11305. PMID: 37432427.
Diabetes
| Fred | Wilma | Barney | |
|---|---|---|---|
| Fasting insulin or C-peptide | Increased | Decreased | N/Slight inc |
| Fasting Glucose | 184 | 230 | 253 |
| Primary Defect | Resistance | Production | Both |
| Diabetes | Type 2 | Type 1 | Type 2 -> Both |
C-peptide: Indicates how much insulin the body is producing
Lifestyle:
- Lifestyle reduced incidence of DM II by 58% over 3 years in Diabetes Prevention Program (DPP)
- At least a 7% weight loss in 6 months
- 150 minutes of brisk walking per week
- Individualized diet
- Quality fats over quantity; more whole grains; nuts
Diabetes Management Plan:
- A1c > 10: Basal insulin + metformin
- A1c within 1.5 of goal: Metformin
- A1c > 1.5 above goal: Metformin + 1 other
- A1c above goal after 3 mo: Metformin + 1 other
ADA Guideline Notes for DM II:
- If ASCVD, HF, or CKD:
- Start with SGLT2 or GLP-1
- If not controlled after 3 mo: Both
| ASCVD | HF | CKD | GoodRx / Price | |
|---|---|---|---|---|
| liraglutide | NNT 53 in 3.8 years | NNT 67 in 3.8 yrs | 960 / $2.3 million in 3.8 years | |
| semaglutide | NNT 91 in 2 years | NNT 44 in 2 yrs | 908 / $1.9 million in 2 years | |
| dulaglutide | NNT 71 in 5.4 years | NNT 42 in 5.4 yrs | 852 / $3.9 million in 5.4 years | |
| empagliflozin | NNT 62 in 3 years | NNT 71 in 3 years | NNT 20 in 3 years | 546 / $1.2 million in 3 years |
| Canagliflozin | NNT 179 in 3 years | NNT 14 In 5 years | NNT 60 in 1.5 years | 620 / $4.0 million in 3 years |
GLP-1
- Weight loss! NNT = 2
Reference:
- FAFP Spring 2024 - Dr Koo
Diabetes self-management and support (DSME/S)
DSME/S improves diabetes outcomes, including:
- lowering hemoglobin A1c levels
- reducing onset and/or advancement of diabetes complications
- helping people improve their lifestyle behaviors
- decreasing diabetes distress and depression
- improving quality of life
4 critical times for assessing the need for DSME/S referral:
- with a new diagnosis of type 2 diabetes
- annually for health maintenance and prevention of complications
- when new complicating factors influence self-management
- when transitions in care occur
Reference:
- Diabetes Care,The Diabetes Educator, and the Journal of the Academy of Nutrition and Dietetics.
DKA and HHS Management
DKA:
- Blood glucose >250 mg/dL
- Arterial pH <7.3
- Bicarbonate level 15 mEq/L
- Moderate ketonuria or ketonemia
IV Fluids:
- Determine hydration status
- Severe: NS at 1L/hr
- Cardiogenic shock: Hemodynamic monitoring/pressors
- Mild: Evaluate corrected sodium level
- Normal/High
- 0.45% saline - 250 to 500 mL/hr depending on hydration status
- Low
- NS - 250 to 500 mL/hr depending on hydration status
- When serum glucose reaches 200 mg/dL (DKA) or 300 mg/dL (HHS), switch to 5% dextrose with 0.45% saline at 150 to 250 mL/hr
- Normal/High
Potassium:
- Establish adequate renal function (50mL/h Urinary Output)
- Potassium level:
- <3.3 mEq/L
- Hold insulin and give 20-30 mEq potassium per hour until level >3.3 mEq/L
- 3.3-5.2 mEq/L
- Give 20-30 mEq potassium/L of IVF to keep serum potassium between 4 and 5 mEq/L
- >5.2 mEq/L
- Do not give potassium
- Check every 2 hours
- <3.3 mEq/L
Regular insulin:
- Give IV
- 0.1u regular insulin/Kg as IV bolus
- 0.1u regular insulin/Kg/Hr as continuous IV infusion
- If serum glucose level does not decrease by 10% in first hour, give 0.14u regular insulin/Kg as IV bolus then continue previous
- HHS:
- When serum glucose reaches 300 mg/dL
- Reduce IV regular insulin to 0.02-0.05u/Kg/hr
- Keep serum glucose level at 200-300 mg/dL until patient is alert
- When serum glucose reaches 300 mg/dL
- DKA:
- When serum glucose reaches 200 mg/dL
- Reduce IV regular insulin to 0.02-0.05u/Kg/hr OR give rapid-acting insulin at 0.1u/Kg every 2 hours
- Keep serum glucose at 150-200 mg/dL until DKA resolves
- When serum glucose reaches 200 mg/dL
Bicarbonate:
- pH > 6.9
- No bicarbonate
- pH < 6.9
- 100 mmol bicarbonate in 400 mL water + 20 mWq potassium chloride
- Infuse over 2 hours
- Repeat every 2 hours until pH > 7
- Monitor potassium every 2 hours
- 100 mmol bicarbonate in 400 mL water + 20 mWq potassium chloride
DKA/HHS
- Check venous pH and electrolyte, BUN, creatinine, and glucose every 2-4 hours until stable
- When DKA or HHS resolves and patient is able to eat - initiate subcutaneous insulin
- Continue IV infusion 1-2 hours after beginning subcutaneous insulin
- In insulin naive patients - start 0.5-0.8u/Kg/day then adjust as needed
Calculations:
- Corrected serum sodium
- sodium + (1.65*glucose-100)/100
- Effective serum osmolarity (HHS > 320)
- (2*corrected sodium)+(Glucose/18)
References:
- AFP Vol 96 No 11 Dec 2017
DM visit EBM
- A: A1c - q3 - 6 mo
- B: BP - <130/80
- C: Chol - LDL <100 annual
- D: MDRD: GFR q6 mo
- E: Eye exam - on Dx and annual
- F: Foot - visual - annual
References:
- Kopes-Kerr C. Type 2 Diabetes: Separating Proven from Unproven Interventions. Am Fam Phys. Vol 80, No 5. 1 Sep 2009. pp450-452
General Notes
- DM is 7th leading cause of death in US.
- 1 in 4 persons with DM are unaware they have the disease.
- If a cohort of obese persons have prediabetes and reduce their weight by 5% - the incidence of newly diagnosed diabetes in 3 years decreases from 23% to 11%.
- Metformin, acarbose, and a combination ramiril/rosglitazone can be effective in preventing progression from prediabetes to DM.
From: Shaughnessy AF1, Erlich DR1, Slawson DC2. Type 2 Diabetes: Updated Evidence Requires Updated Decision Making. Am Fam Physician. 2015 Jul 1;92(1):22.
- A1C levels should be low enough to decrease symptoms but not low enough to risk hypoglycemia. For many patients, this range is 8% to 9% with a fasting blood glucose level less than 200 mg per dL (11.1 mmol per L).
- The goal of treating type 2 diabetes is to help patients live longer, healthier, productive lives. …Other than metformin, which has been shown to decrease mortality independent of its effect on glucose levels, all other available diabetes medications treat numbers, not patients.
- For type 2 diabetes, this means abandoning tight control of blood glucose for most patients, and instead addressing risks such as smoking, hypertension, and hyperlipidemia that will actually make a difference.
(Erlich DR, et al. "Lending a hand" to patients with type 2 diabetes: a simple way to communicate treatment goals. Am Fam Physician. 2014;89(4):256,258.)
- Normalizing blood glucose levels benefits only a small subset of patients.
(George CM, et al. Management of blood glucose with noninsulin therapies in type 2 diabetes. Am Fam Physician. 2015;92(1):27–34.)
- …weekly self-weighing, regular consumption of breakfast, and reduced intake of fast food were associated with a lower body mass index in overweight patients.
(Raynor HA, Jeffery RW, Ruggiero AM, Clark JM, Delahanty LM; Look AHEAD Research Group. Weight loss strategies associated with BMI in overweight adults with type 2 diabetes at entry into the Look AHEAD (Action for Health in Diabetes) trial. Diabetes Care. 2008;31(7):1299–1304.)
- …medical nutrition therapy decreases A1C level, weight, waist circumference, and triglyceride level, and increases health-related quality of life.
(Evert AB, Boucher JL, Cypress M, et al.; American Diabetes Association. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care. 2013;36(11):3821–3842.)
- The ADA recommends starting therapy with metformin, because it is the only medication shown to reduce mortality and complications in randomized controlled trials (RCTs).
(Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group [published correction appears in Lancet. 1998;352(9139):1558]. Lancet. 1998;352(9131):854–865.)
- No evidence from RCTs that any of the other DM medications reduce the risk of diabetes-related complications, cardiovascular mortality, or all-cause mortality.
(American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes Care. 2014;37(suppl 1):S14–S80.)
References:
- Vijan S. In the clinic. Type 2 diabetes. Ann Intern Med. 2015; 162(5):ITC1-16.
- Consultant. 2015;55(7):565
- George CM, Brujin LL, Will K, Howard-Thompson A. Management of Blood Glucose with Noninsulin Therapies in Type 2 Diabetes. Am Fam Physician. 2015 Jul 1;92(1):27-34.
HbA1C and Estimated Average Glucose Level
| HbA1c (%) | eAG (mg/dL) |
|---|---|
| 5 | 97 |
| 6 | 126 |
| 7 | 154 |
| 8 | 183 |
| 9 | 212 |
| 10 | 240 |
| 11 | 269 |
| 12 | 298 |
- Table source: http://www.ngsp.org/A1ceAG.asp
- Can also estimate with: (A1c - 2)*30
- Ex: A1c of 10
- 10-2 = 8
- 8*30 = 240
- Ex: A1c of 10
Iatrogenic Hypoglycemia
- Mortality rate associated with hypoglycemia has been estimated as high as 10%.
(Skrivarhuag T, Bangstad HJ, Stene LC, et al. Long-term mortality in a nationwide cohort of childhood-onset type 1 diabetic patients in Norway. Diabetologica. 2006; 49(2):298-305)
- After warfarin, insulin was the second most frequent cause of emergency hospitalizations due to adverse drug events in adults over 65.
(Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Medd. 2011;365(21):2002-2012)
- Insulin is the most common cause of iatrogenic hypoglycemia. Patients on more complicated regimens have higher rates of hypoglycemia.
(Holman RR, Farmer AJ, Davies MJ, et al. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361(18):1736-1747)
- Sulfonylureas also cause hypoglycemia as they act directly on ATP-sensitive potassium channels on the beta cell membrane -> induces depolarization and insulin release independently of stimulation of physiologic insulin from glucose.
Other noninsulin medications less likely as they:
- increase peripheral sensitivity to insulin (metformin and thiazolidinediones)
- enhance pancreatic insulin secretion in response to oral glucose through the incretin pathway (GLP-1 agonists and DPP-4 inhibitors)
- increasing renal loss of glucose (SGLT2 inhibitors)
- Renal failure increases risk (both acute and chronic). Kidneys metabolize most sulfonylureas.
- Glyburide is NOT recommended in renal insufficiency with GFR <50-60ml/min/1.73m2
- Glipizide tends to be safer in renal insufficiency but also needs dose reductions.
References:
- Consultant. 2015;55(7):541-542
Insulin
See:
How to start insulin (Dr Koo):
- Consider starting with long-acting basal insulin like determir (Levemir) or glargine (Lantus)
- Start with 10 units before bed (or 0.1 to 0.2 units per kg)
- Increase by 1 units every day if AM fasting glucose > 130
- Once AM glucose is 130 or lower, maintain same dose insulin for the rest of the month until follow-up appointment
AACE/ACE Approach to Starting Insulin
- Augmentation therapy with long-acting (basal) insulin
- A1C < 8%: total daily dosage 0.1 to 0.2 units per kg
- A1C > 8%: total daily dosage 0.2 to 0.3 units per kg
- Replacement therapy with basal and rapid-acting prandial (basal-bolus) insulin
- Add prandial insulin 1 meal at a time*: start at 10% of long-acting dose or 5 units
- Add prandial insulin before each meal: total daily dosage 0.3 to 0.5 units per kg and divide 50% basal and 50% prandial†
Insulin Approach
- Start with Basal Insulin
- Can add 1 rapid acting insulin before largest meal OR Change to premixed insulin twice daily
- Rapid acting insulin
- Start: 4u or 10% basal dose
- Adjust by 1-2u weekly until target reached
- Premixed twice daily
- Start: divide current basal dose into 2/3 AM and 1/3PM OR into 1/2 AM and 1/2 PM
- Adjust: Increase by 1-2u weekly until target reached
- Rapid acting insulin
- If not controlled - consider basal with bolus before meals
Lantus/Levemir:
- Start at 0.1-0.2 unit/Kg
- Titrate after assesssing mean 3-day FPG (3-0-3 Regimen)
- If FG is >130 increase 3 units
- If FG is 80-130 maintain dose
- If FG is <80 decrease 3 units
Toujeo:
- Start 0.2units/kg; 1:1 basal; 80% Total NPH dose; 1/3 to 1/2 total daily insulin dose
NovoLog (insulin aspart)
- Step 1: Inject 4units before percieved largest meal
- Step 2: Patients measure BS before next meal or bedtime and use this reading to plan next day dose
- Step 3: Self titrate based on Step 2
- If less than or equal to 70 -> -1
- If 71-130 then no change
- If over 130 -> +1
NovoLog 70/30 (use NPH instead of 70/30)
- Starting dose:
- If FG <180 mg/dL -> 5units before breakfast and 5u before dinner
- If FG is >180 -> 6u before breakfast and 6u before dinner
Titration:
Premeal glu Unit adjust <80 -2 80-110 0 111-140 +2 141-180 +4 >180 +6
Regular insulin:
- Estimate sensitivity using "rule of 1800"
- BG change per unit Insulin = 1800/total Insulin daily
- Example of 60 units/day: 1 unit drops BG 30 mg/dl
- Protocol (uses rapid acting Insulin, e.g. Lispro)
- Goal Blood Glucose is <150
- Using sensitivity, how many units to drop 50 mg/dl
- For example above, ~1 unit to drop BG 50 mg/dl
- BG 150-199: 1 unit Bolus Insulin (regular or RA)
- BG 200-249: 2 units Bolus Insulin
- BG 250-299: 3 units Bolus Insulin
- BG 300-349: 4 units Bolus Insulin
- BG Over 350: 5 units Bolus Insulin
- For example above, ~1 unit to drop BG 50 mg/dl
- Add in coverage for meal intake
- Based on per carbohydrate when Glucose >60 mg/dl
- Use for Type I Diabetes, consider for Type II
- Add to sliding scale coverage above
- Add 1 unit Insulin per carbohydrate
- Example: For 3 carbohydrate meal, add 3 units
http://www.fpnotebook.com/endo/pharm/inslnsldngscl.htm
A Good Resource: http://clinical.diabetesjournals.org/content/20/1/11.full
2 Types of Insulin Categories:
Basal insulins:
- Intermediate-acting insulins
- Humulin N (NPH)
- Novolin N (NPH)
- Long-acting insulins
- Basaglar (insulin glargine)
- Lantus (insulin glargine)
- Levemir (insulin detemir)
- Semglee (insulin glargine)
- Toujeo (insulin glargine)
- Tresiba (insulin degludec)
Premeal insulins:
- Rapid-acting insulins
- Admelog® (insulin lispro)
- Afrezza® (inhaled insulin)
- Apidra® (insulin glulisine)
- Fiasp® (insulin aspart)
- Humalog® (insulin lispro)
- Lyumjev® (insulin lispro-aabc)
- Novolog® (insulin aspart)
- Short-acting insulins
- Humulin® R (regular)
- Novolin® R (regular)
| Glucose Lev | Increase by |
|---|---|
| <60 | -4 units |
| 60-79 | -2 units |
| 80-99 | Maintain dose |
| 100-119 | 1 units |
| 120-140 mg/dL | 2 units |
| 141-160 mg/dL | 4 units |
| 161-180 mg/dL | 6 units |
| >180 mg/dL | 8 units |
| Premeal Glucose | Adjust |
|---|---|
| level for 3 days | |
| <60 mg/dL | -4 |
| 60-79 mg/dL | -2 |
| 80-99 mg/dL | -1 |
| 100-119 mg/dL | Maintain dose |
| 120-139 mg/dL | 1 |
| 140-180 mg/dL | 2 |
| >180 mg/dL | 3 |
| Fasting BG for 3d | Adjustment of | Pre-dinner BG for 3d | Adjustment of |
|---|---|---|---|
| Pre-Dinner dose | Pre-Breakfast dose | ||
| <60 mg/dL | -4 | <60 mg/dL | -4 |
| 60-79 mg/dL | -2 | 60-79 mg/dL | -2 |
| 80-110 mg/dL | Maintain Dose | 80-110 mg/dL | Maintain Dose |
| 111-140 mg/dL | 2 | 111-140 mg/dL | 2 |
| 141-180 mg/dL | 4 | 141-180 mg/dL | 4 |
| >180 mg/dL | 6 | >180 mg/dL | 6 |
References:
- AFP Vol 84 No 2 Jul 2011
- AFP Vol 97 No 1 Jan 2018
Physiologic Insulin Guidelines
- Step 1: Measure BG before meals and at bedtime, or q6 if nothing by mouth
- Step 2: Calculate initial total daily dose (TDD) of insulin
- 0.3units/kg if underweight, elderly, or dialysis
- 0.4units/kg if normal weight
- 0.5units/kg if overweight
- 0.6units/kg if obese, glucocorticoids, insulin resistance
- Step 3: 50% of TDD as long acting basal insulin
- Step 4: 50% of TDD as short acting nutritional insulin given in 3 divided doses 0-15min before meals
- Step 5: Select a scale of short-acting correctional insulin given 0-15min before meals
- Step 6: Subsequent daily adjustment of TDD base on previous days total units given
| Blood Glucose | Standard Dosing |
|---|---|
| 150-199mg/dL | 1 |
| 200-249mg/dL | 3 |
| 250-299mg/dL | 5 |
| 300-349mg/dL | 7 |
| >349mg/dL | 8 + call |
| Insulin | Onset (h) | Duration (h) |
|---|---|---|
| Glargine (Lantus) | 1-2 | 24 |
| Detemir (Levemir) | 1-2 | 18-24 |
| Isophane (NPH) | 1-2 | 10-20 |
| Lispro, aspart, glulisine | 5-15min | 3-6 |
| Regular | 1-2 | 6-10min |
References:
- AFP Vol 81 No 9 May 2010
- Strategies for low income
See:
Low cost DM insulin
- Novolin at Walmart
- Relyon at Walmart
- Start NPH as daily long acting
Wal-mart Insulin
- Reli-on brand of Novolin N (NPH) in 10 mL bottles insulin ($24.88)
- Use NPH nightly similar to lantus or levemir
- Start with 10u nightly and warn of hypoglycemia symptoms (at 8-10h mark)
- When NPH is greater than 0.25 units per kg and the post meal blood sugars are above target, consider adding morning NPH and/or premeal regular insulin.
- Reli-on brand of Novolin R (regular) in 10 mL bottles insulin ($24.88)
- Use for additional carbs as needed
- When NPH is greater than 0.25 units per kg and the post meal blood sugars are above target, consider adding morning NPH and/or premeal regular insulin.
- Can try the 50/50 Rule:
- Take the patients weight in kgs x 0.5 to calculate total daily insulin needs.
- 50% is from basal NPH (0.25 units per kg)
- The other 50% from bolus regular (0.25 units per kg divided into 2 to 3 meals).
- Take the patients weight in kgs x 0.5 to calculate total daily insulin needs.
- Reli-on brand of Novolin 70/30 in 10 mL bottles insulin ($24.88)
- 70/30 twice a day
- Also:
- ReliOn insulin syringes ($12.99)
- Glucose tablets
- Lancets ($6.24)
- Type 1 DM Insulin
ADA general treatment recommendations for T1DM
- T1DM patients should receive multidose injections (3 - 4 a day) of basal and premeal insulin or insulin pump therapy
- Most individuals with T1DM should use rapid-acting insulin analogs to reduce hypoglycemia risk
- Patients should match premeal insulin to carbohydrate intake, premeal blood glucose levels, and anticipated activity
Starting therapy
- Insulin dosing in T1DM will vary based on patient's age, weight, and residual pancreatic insulin activity
- T1DM patients will typically require a total daily insulin dose of 0.4 - 1.0 units/kg/day
- A typical starting dose in metabolically-stable patients is 0.5 units/kg/day
- After calculating the total daily dose, it should be given as follows:
- Basal insulin - given as half of the total daily dose ✝
- Premeal insulin - half of the total daily dose divided into thirds and given before each meal
- When first starting therapy, it is recommended that the initial basal dose be reduced by 20 - 30% to prevent hypoglycemia [11,19]
- T1DM patients may experience a "honeymoon phase" after starting insulin therapy where the initial effects of insulin are greater than what is seen later in the disease
Example:
- Patient weighs 80 kg
- Total daily dose = 80 kg X (0.5 units/kg/d) = 40 units per day
- Basal insulin = 1/2 X 40 units = 20 units of basal per day✝
- Premeal Insulin = 1/2 X 40 units = 20 units / 3 = approximately 7 units before each meal
- If patient is just starting therapy, the initial basal dose should be reduced by 20 - 30%. In our example: 20 units X 0.20 = 4 units, so initial basal dose would be 20 - 4 = 16 units
- Type 2 DM Insulin
- Step 1 - start with long-acting insulin or bedtime NPH
- Initial dose: 10 units/day or 0.1 - 0.2 units/kg/day
- Adjust dose: increase dose by 10 - 15% or 2 - 4 units once or twice weekly to achieve fasting blood sugar goal (see adjusting basal insulin and NPH dosing for other recommendations)
- If hypoglycemia occurs: decrease dose by 10 - 20% or 4 units
- If A1C is still above target despite achieving fasting blood sugar goal, or if A1C is not at target and insulin dose is > 0.7 - 1.0 units/kg, proceed to Step 2
- Step 2 - add premeal insulin before largest meal
- Initial dose: 4 units or 10% of basal dose
- If A1C < 8%, consider decreasing basal insulin dose by same amount
- Adjust dose: increase dose by 1 - 2 units or 10 - 15% twice weekly to achieve pre- and postprandial goals (see adjusting premeal insulin for other recommendations)
- If hypoglycemia occurs: decrease dose 2 - 4 units or 10 - 20%
- For patients using bedtime NPH:
- Consider switching to twice daily NPH by taking 80% of current bedtime NPH dose and giving 2/3 in the morning and 1/3 at bedtime.
- Example:
- Current bedtime NPH dose is 30 units
- 0.80 X 30 = 24 units
- 2/3 of 24 = 16 units in the morning
- 1/3 of 24 = 8 units in the evening
- Consider switching to twice daily NPH by taking 80% of current bedtime NPH dose and giving 2/3 in the morning and 1/3 at bedtime.
- If A1C still not at target, proceed to Step 3
- Step 3 - add premeal insulin before other meals in stepwise fashion
- Add prandial insulin to an additional meal and use the guidelines in Step 2 to adjust
- If not controlled with 2 preprandial doses, add to a third meal
- Stepwise addition of prandial insulin every 3 months is associated with a lower risk of hypoglycemia and greater patient satisfaction
- Step 1 - start with long-acting insulin or bedtime NPH
- Pre-meal Insulin
Carbohydrate counting
- In carbohydrate counting, premeal insulin is adjusted based on the amount of carbohydrates to be consumed in each meal
- The carbohydrate counting method is used to determine the amount of carbohydrates in a meal
- An insulin to carbohydrate ratio (ex. 1 unit/10g of carb) is used to calculate the premeal insulin dose
- A typical starting ratio is 1 unit of premeal insulin for every 10 grams of carbs to be consumed
- An individual may have different carbohydrate ratios for breakfast, lunch, and dinner because a person's response to insulin may vary throughout the day
- Example:
- 60 grams of carbs to be consumed for lunch
- Patient's ratio is 1 unit of insulin for every 10 grams of carbs
- Patient injects 6 units of premeal insulin before eating meal
Calculate a correction factor
- Step 1 - calculate the correction factor
- For Regular insulin (Humulin R, Novolin R)
- Divide 1500 by the patient's total daily dose of insulin
- The result will equal the estimated drop in blood sugar (in mg/dl) from 1 unit of regular insulin
- For Rapid insulin (Novolog, Humalog, Apidra, Fiasp, Admelog)>
- Divide 1800 by the patient's total daily dose of insulin
- The result will equal the estimated drop in blood sugar (in mg/dl) from 1 unit of rapid insulin [4,12]
- Example:
- Patient's total daily dose of insulin (premeal + basal) is 60 units
- Patient uses regular insulin as premeal insulin
- 1500/60 = 25
- Patient can expect that for every 1 unit of regular insulin they inject, their blood sugar will come down 25 mg/dl
- For Regular insulin (Humulin R, Novolin R)
- Step 2 - Once the correction factor is calculated, the patient can then figure out how much insulin to supplement
- Example:
- Patient from above: correction factor is 25 mg/dl
- Patient checks pre-lunch blood sugar and it is 175 mg/dl (desired range 80 - 120 mg/dl)
- 175 - 120 = 55 mg/dl
- 55/25 = approximately 2
- Patient would add 2 extra units of regular insulin to premeal dose
- Example:
Adjustments to Correction Factor
- If pre-lunch average is not in desired range (80 - 120 mg/dl), adjust breakfast ratio
- If pre-dinner average is not in desired range (80 - 120 mg/dl), adjust lunch ratio
- If pre-bedtime snack average is not in desired range (80 - 120 mg/dl), adjust dinner ratio
- If average blood sugar is > 120 mg/dl, adjust ratio by subtracting 2 - 3g of carbohydrate
- Example:
- Current ratio 1 unit / 10g of carb
- Pre-lunch average > 120 mg/dl
- Change breakfast ratio to 1 unit / 7g of carb
- Example:
- If average blood sugar is < 80 mg/dl, adjust ratio by adding 2 - 3g of carbohydrate
- Example:
- Current ratio 1 unit / 10g of carb
- Pre-bedtime snack average < 80 mg/dl
- Change dinner ratio to 1 unit / 13g of carb
- If average blood sugar is 80 - 120 mg/dl, do not adjust ratio
- Example:
- Insulin NPH Dosing Adjustments
Initial:
- 0.1 to 0.2 units/kg/day or 10 units/day administered as a single dose (usually at bedtime) or in 2 divided doses (ADA 2020; Lipska 2017).
- If HbA1c >8% prior to initiation of basal insulin, 0.2 to 0.3 units/kg/day is recommended (AACE/ACE [Garber 2020]).
For elevated fasting plasma glucose:
- Adjust dose using evidence-based titration algorithm (eg, by 2 units every 3 days) while avoiding hypoglycemia (AACE/ACE [Garber 2020]; ADA 2020).
For elevated HbA1c despite achieving fasting plasma glucose target:
- Patients using once daily insulin NPH (eg, at bedtime):
- Consider switching to a twice daily regimen by administering ~80% of the current bedtime dose in 2 divided doses (one example division would be 2/3 of the dose in the morning and 1/3 of the dose at bedtime) (ADA 2020).
- Patients using twice daily insulin NPH:
- Consider intensification of therapy with additional agents that target postprandial glucose rather than continuing to increase the insulin NPH dose (AACE/ACE [Garber 2020]; ADA 2020).
For hypoglycemia:
- If no clear reason for hypoglycemia, decrease dose by 10% to 20% (ADA 2020);
- For severe hypoglycemia (ie, requiring assistance from another person or blood glucose <40 mg/dL) reduce dose by 20% to 40% (AACE/ACE [Garber 2020]).
Dosage adjustment when adding prandial insulin:
- Consider reducing the basal insulin dose by 4 units (or ~10%) if HbA1c is <8% when initiating prandial insulin (ADA 2020).
Patients with diabetes receiving enteral feedings (ADA 2020):
- Note: TDD of insulin is divided into a basal component (intermediate- or long-acting insulin) and nutritional and correctional components (regular insulin or rapid-acting insulins).
- Basal component:
- SubQ: Continue previous basal insulin dose or administer 30% to 50% of TDD as insulin NPH; if basal insulin naive, administer insulin NPH 5 units every 12 hours.
Patients with diabetes undergoing surgery:
- SubQ: On the evening before surgery or procedure, reduce the usual dose by 25%; on the morning of surgery or procedure, reduce the usual dose by 25% to 50% (ADA 2020; Pichardo-Lowden 2012).
Conversion from long-acting insulin analogs to insulin NPH:
- Consider initiating insulin NPH at 80% (eg, 20% reduction) of previous basal insulin total daily dose; administer as a single dose (usually at bedtime) or in 2 divided doses (ADA 2020; Lipska 2017).
Dosage adjustment for concomitant therapy:
- Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
- Dosing NPH Insulin in T2DM
Twice-daily NPH regimens divide the daily dose between a morning and evening dose. In studies, dose distribution has varied widely, with some splitting the dose 50-50, some giving 2/3 in the morning and 1/3 in the evening, and others giving 1/3 in the morning and 2/3 in the evening.
- Step 1 - Initial dose
- If A1C > 10% and no blood sugars < 126 mg/dl in last 2 weeks ✝
- Start with NPH 10 units twice daily
- If A1C < 10% or any blood sugars < 126 mg/dl in last 2 weeks ✝
- Start with NPH 6 units twice daily
- Morning dose should be given at approximately the same time each day upon awakening
- Evening dose should be given at bedtime
- If patient has not been checking blood sugars, have them check and report a fasting blood sugar once they obtain a monitor
- If A1C > 10% and no blood sugars < 126 mg/dl in last 2 weeks ✝
- Step 2 - Monitor blood sugars
- Check fasting blood sugar in the morning and predinner blood sugar in the evening on a daily basis
- Step 3 - Determine insulin adjustment
- After 3 consecutive days of readings, average all the blood sugars (fasting and predinner) together
- Use this average and the table below to determine how much insulin will be added (or subtracted) to the total daily dose
Blood sugar average (fasting and predinner) over 3 days Adjustment to total daily NPH dose ≥ 180 add 8 units 160 - 179 add 6 units 140 - 159 add 4 units 120 - 139 add 2 units 100 - 119 add 1 unit 80 - 99 no change 60 - 79 subtract 2 units < 60 subtract 4 or more units - Step 4 - Distributing the insulin adjustment
- Average the fasting and predinner blood sugars over the last 3 days separately
- Determine a range for each average (fasting and predinner) from the two tables below
Table 72: Fasting blood sugar ranges Average blood sugar (mg/dl) Range > 160 3 101 - 160 2 ≤ 100 1 Table 73: Predinner blood sugar ranges Average blood sugar (mg/dl) Range > 160 3 131 - 160 2 ≤ 130 1 - Step 1 - Initial dose
- Converting from long-acting insulins to NPH
- Total daily basal insulin dose: reduced by 25 - 30% upon initiation.
- This approach helps prevent hypoglycemia but may require significant up-titration after switching.
- Patients who are also receiving premeal insulin should be particularly cautious because NPH may potentiate the peak effect of short-acting insulins
- Total daily basal insulin dose: reduced by 25 - 30% upon initiation.
- SLIDING SCALE INSULIN
Blood sugar (mg/dl) Insulin dose in units of rapid or short-acting 60-110 0 111 - 150 2 151 - 200 4 201 - 250 6 251 - 300 8 301 - 350 10 351 - 400 12 > 400 14 - Syringes
Syringes come in:
- 30 unit syringe
- 50 unit syringe
- 100 unit syringe
Diabetic Neuropathy
Low-dose naltrexone is as effective as amitriptyline in the treatment of painful diabetic neuropathy and has a superior safety profile (strength of recommendation [SOR], B; single randomized controlled trial [RCT]).
Reference:
- J Fam Pract. 2023 September;72(7):320-321 | doi: 10.12788/jfp.0654
Management Plan for Type 2
- Healthy eating, weight control, increased physical activity
- Metformin
- (2 Drug) Metformin + one of the following:
- GLP-1 Receptor Agonist
- DPP4 Inhibitor
- SU
- Basal Insulin
- (3 Drug) Metformin + two of the previous
- Do not mix DPP-4-I and GLP-1-RA (both work similarly)
- Do not mix SU and insulin (increased risk of hypoglycemia)
- More complex insulin regimens
NOTE - guidelines do include TZDs but I do not use them d/t my concern with weight gain, cancer, edema, and HF.
Other Therapy Aspects:
- Exercise (even if it is a little)
- A growing body of evidence suggests that interrupting prolonged sitting with intermittent brief periods of standing or light exercise can improve glucose metabolism
- Metformin should be used as first-line therapy to reduce microvascular complications, assist in weight management, reduce the risk of cardiovascular events, and reduce the risk of mortality in patients with type 2 diabetes mellitus. (LOE A)
- Patients with prediabetes or new-onset diabetes should undertake extensive lifestyle changes to slow the progression of type 2 diabetes. (LOE A)
- Patients with existing cardiovascular disease, two or more cardiovascular disease risk factors, or duration of diabetes of 10 years or more should have higher A1C goals because of a lack of benefit and the potential for increased risk of mortality compared with lower A1C goals. (LOE A)
- Self-monitoring of blood glucose levels for patients taking noninsulin therapies does not significantly affect glycemic control. (LOE B)
- Painful Diabetic Neuropathy - See under Neurology section
References:
- NEJM JW Gen Med Jul 1 2012
- Diabetes Care 2012; 35:976
Oral medications
- Metformin
See also:
You can use metformin in anyone whose estimated glomerular filtration rate (eGFR) is > 30 mL/minute/1.73 m2 and you do not have to stop metformin in someone undergoing a dye study unless their EGFR is < 60 mL/minute/1.73 m2.
Let me explain. We used to use serum creatinine cut-points to determine when we should prescribe metformin in patients with any degree of renal insufficiency. Now the FDA has done away with that guideline and really expanded the number of patients that we can safely keep on metformin. These are the rules:
Test the eGFR in any patient before you start metformin. If it's > 45 mL/minute/1.73 m2, you are fine. That patient is fully eligible to be on metformin.
For the most part, the FDA does not recommend starting metformin in patients with an eGFR between 30 and 45 mL/minute/1.73 m2. But they still consider metformin safe if your patient is on metformin already and seems to be deriving some benefit. So, patients down to an eGFR of 30 mL/minute/1.73 m2 can remain on their metformin.
Patients with an eGFR < 30 mL/minute/1.73 m2 should not be on metformin.
The notion that we don't have to stop metformin in every patient undergoing a radiographic dye study makes me incredibly happy. I've spent countless hours dealing with this in my patients. The specific guidelines are as follows:
If the eGFR is > 60 mL/minute/1.73 m2, don't worry about it. They can continue taking their metformin throughout, unless it's an intra-arterial dye study. In that case, you are going to need to hold the metformin and make sure that the renal function stays stable.
If the eGFR is < 60 mL/minute/1.73 m2—meaning between 30 and 60—then, as we did before, you stop the metformin before the patient undergoes the dye study and recheck in 48 hours to make sure that the eGFR is still in a safe range.
For many of our patients undergoing radiographic dye studies who have an eGFR of > 60 mL/minute/1.73 m2, we are not going to need to hold the metformin. I think that will make our lives much easier and, frankly, will be better for our patients.
These guidelines are consistent with recommendations that have been used throughout the world for many years. I really believe that they are safe and likely to help us use metformin in more of our patients who will benefit from the drug. Thank you.
- Metformin may work by changing gut bacteria makeup
Randomized, placebo-controlled, double-blind study published in Nature, April 2017:
- Population:
- 40 Individuals with newly diagnosed Type 2 Diabetes Mellitus
- Intervention:
- calorie restricted diet vs metformin for 4 months.
- Outcomes:
- gut microbiota changes and A1c.
- Results:
- metformin, but not calorie restriction, had rapid effects on the composition and function of the gut microbiota in parallel with the reduction of %HbA1c and fasting blood glucose concentrations.
- Transfer of the microbiota to germ-free mice showed that the metformin-altered microbiota could improve glucose metabolism.
- Furthermore, transcriptome analyses of feces showed that metformin had direct effects on the gut microbiota, specifically expression of bacteria genes that regulate metal transporters.
- Conclusion:
- Some of metformin's antidiabetic effects are from altered gut microbiota.
- Additional studies are essential to further identify microbial proteins and to determine how they interact with the host targets in improving host metabolism.
Reference:
- Population:
- SUs/TZDs
- Later generation are recommended to reduce hypoglycemia
- Glimepiride
- Glipizide
- Thiazolidinediones
- Pioglitazone
In general:
- Use Glipizide or Glimiperide; DO NO NOT USE Glyburide
- NO Glyburide in elderly d/t longer half-life than glimiperide and glipizide (more likely to cause hypoglycemia
- Later generation are recommended to reduce hypoglycemia
Self-monitoring
- For patients who have had diabetes longer than one year and are not using insulin, evidence suggests that the benefit of self-monitoring of blood glucose in lowering A1C levels is small at six months and disappears by 12 months. Self-monitoring of blood glucose does not improve health-related quality of life, general well-being, or patient satisfaction. (SOR: B)
- For those who have been diagnosed with diabetes for more than one year, especially those whose blood glucose levels are well controlled without insulin, the evidence supports discontinuing (or not initiating) selfmonitoring of blood glucose because of the added cost and inconvenience of testing and lack of improvement in patient-oriented outcomes.
References:
- (Malanda UL, Welschen LM, Riphagen II, Dekker JM, Nijpels G, Bot SD. Self-monitoring of blood glucose in patients with type 2 diabetes mellitus who are not using insulin. Cochrane Database Syst Rev. 2012 Jan 18;1:CD005060. doi: 10.1002/14651858.CD005060.pub3.)
Special tests to classify DM
| Test | Desc | Utility |
|---|---|---|
| C peptide | Reflects endogenous insulin production | Consider in pts with possible LADA or Type 1 but neg antibodies |
| Zinc transporter 8 Ab | Correlates with utoimmune mediated DM | Consider in pts with possible LADA or Type 1 but neg antibodies |
| Insulinoma-associated Ag-2 | Autoimmune Ab associated with DM I | Distinguish DM 1 or LADA from DM 2 |
| Insulin Ab | May be more common in LADA | |
| Islet cell Ab | May be more common in LADA | |
| Glutamic acid decarboxylase 65 | May be more common in LADA |
References:
- AFP Vol 93 No 2 Jan 2016
Weight loss in pts with DM 2
- Modest weight loss reduces insulin resistance
(American Diabetes Association. Standards of medical care in diabetes—2010 [published correction appears in Diabetes Care. 2010;33(3):692]. Diabetes Care. 2010;33(suppl 1):S11-S61)
- Low-carbohydrate or low-fat calorie-restricted diets may produce weight loss for up to one year, after which behavior modification and physical activity are most helpful.
-Fluoxetine (Prozac) and orlistat (Xenical) produce modest short-term weight loss, but their long-term benefits are unclear and their safety is uncertain. (SOR: B)
- Patients with diabetes can safely achieve modest short-term weight loss using fluoxetine or orlistat.
- A greater proportion of patients with diabetes achieved a 5 or 10 percent loss from their initial body weight with orlistat compared with placebo (relative risk = 2.50 for 5 or 10 percent loss; 95% CI, 2.02 to 2.97).
(Hutton B, Fergusson D. Changes in body weight and serum lipid profile in obese patients treated with orlistat in addition to a hypocaloric diet: a systematic review of randomized clinical trials. Am J Clin Nutr. 2004;80(6):1461-1468.)
(Norris SL, Zhang X, Avenell A, Gregg E, Schmid CH, Lau J. Pharmacotherapy for weight loss in adults with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005 Jan 25;(1):CD004096.)
Sulfonylureas (SU)
Glimepiride, glipizide, and glyburide all reduce in HbA1c about 1% to 2%.
Glimepiride is purported to have the highest incidence of hypoglycemia of the 3 agents
- Might be due to having the longest half-life of the 3 sulfonylureas
- Once-daily dosing at all doses
Glyburide and glipizide require twice-daily administration as their doses are increased.
All 3 agents undergo hepatic metabolism, with only glyburide having active metabolites.
- These metabolites are cleared renally
- Patients with reduced kidney function will experience accumulation, which can lead to increased therapeutic effects and increase the risk of hypoglycemia.
"The relative lack of advantages of glyburide compared with the other agents, combined with its increased risk of adverse effects, creates a risk-to-benefit ratio that does not favor its use. Given that the risks are increased only in patients with poor kidney function, one could simply adjust the choice of agents to select from, but owing to the lack of advantages of glyburide, it makes more sense to remove it as a choice. There is not a scenario in which glyburide is the preferred agent, but there are certain scenarios in which it is clearly the least-preferred agent."
Reference:
- Consultant360 Volume 57 - Issue 4 - April 2017
Estradiol (Vaginal) edit
- estradiol 0.1 mg/g vaginal cream
- Use vaginally via applicator as directed. Use 2g daily for 2 weeks, then use 1 g daily for 1 week and take 1 week off. Then use for 3 weeks with 1 week off each month
Glucocorticoid-Induced Adrenal Insufficiency edit
Tapering Regimen:
- Gradual reduction of glucocorticoid doses is recommended to minimize adrenal insufficiency symptoms and allow HPA axis recovery.
- For example, hydrocortisone is typically administered at 10–12 mg/m²/day in divided doses (e.g., twice or thrice daily), with the first dose taken upon waking.
- Prednisone can be used as an alternative at physiologic doses, such as 7.5 mg/day.
- HPA axis recovery is monitored using morning cortisol levels or ACTH stimulation tests, with recovery defined as a stimulated cortisol level ≥18 μg/dL (500 nmol/L)
Morning cortisol levels can be used to guide the tapering of hydrocortisone supplementation in glucocorticoid-induced adrenal insufficiency (GI-AI) by assessing hypothalamic-pituitary-adrenal (HPA) axis recovery. Morning cortisol should be measured between 8:00 and 9:00 AM, at least 24 hours after the last glucocorticoid dose, to ensure accurate assessment.
- Cortisol levels <150 nmol/L (5 μg/dL) indicate persistent adrenal insufficiency. In these cases, physiologic glucocorticoid replacement should be continued, and repeat morning cortisol testing should be performed every 1–6 months, depending on the prior trajectory of cortisol levels and the duration of glucocorticoid therapy.
- Cortisol levels between 150–300 nmol/L (5–10 μg/dL) suggest possible HPA axis recovery. In such cases, physiologic glucocorticoid replacement should be maintained, and dynamic testing (e.g., ACTH stimulation) may be considered if cortisol levels remain stable in this range. Repeat morning cortisol testing every few weeks is recommended to monitor for further recovery.
- Cortisol levels ≥300 nmol/L (10 μg/dL) are considered a reasonable threshold for HPA axis recovery. If no symptoms of adrenal insufficiency are present, glucocorticoid supplementation can be discontinued.
The tapering process should aim to avoid over-replacement, as this may delay HPA axis recovery. Additional considerations include monitoring for symptoms of adrenal insufficiency or glucocorticoid withdrawal syndrome, which may complicate the tapering process.
Reference:
- Beuschlein F, Else T, Bancos I, et al. European Society of Endocrinology and Endocrine Society Joint Clinical Guideline: Diagnosis and Therapy of Glucocorticoid-Induced Adrenal Insufficiency. The Journal of Clinical Endocrinology and Metabolism. 2024;109(7):1657-1683. https://doi.org/10.1210/clinem/dgae250.
- Baker EH. Is There a Safe and Effective Way to Wean Patients Off Long-Term Glucocorticoids?. British Journal of Clinical Pharmacology. 2020;. https://doi.org/10.1111/bcp.14679
Hormone Replacement Therapy edit
Oral estrogens should be avoided in women with hypertriglyceridemia, active gallbladder disease, or known thrombophilias such as factor V Leiden (with or without a personal history of venous thromboembolism [VTE]).
Standard Dosing:
- transdermal estradiol (0.025 mg) or oral estradiol (0.5 mg/day), and titrate up to relieve symptoms
- 17-beta estradiol (oral 1 mg/day or transdermal 0.05 mg/day) are adequate for symptom relief in the majority of women
- All women with an intact uterus need a progestin to be added to their systemic estrogen to prevent endometrial hyperplasia
- micronized progesterone
- 100 mg daily [continuous regimen] OR
- 200 mg/day for 12 days/month [ie, a cyclic regimen that is designed to mimic the normal luteal phase of premenopausal women]
- micronized progesterone
Risks:
- For women at moderate risk of cardiovascular disease (CVD; 5 to 10 percent 10-year risk), we suggest transdermal rather than oral estrogen. For women with a uterus, we suggest micronized progesterone rather than synthetic progestins such as medroxyprogesterone acetate (MPA).
- We suggest nonhormonal therapies for symptomatic women who are at high risk (>10 percent 10-year risk) for CVD or moderate (1.67 to 5 percent five-year risk) to high risk (>5 percent) for breast cancer.
| 10-year CVD risk | <10 Years since menopause onset |
|---|---|
| Low (<5%) | Menopause Hormone Therapy ok |
| Moderate (5 to 10%) | MHT ok (choose transdermal) |
| High (>10%)* | Avoid MHT |
| Risk category* | 5-year NCI or IBIS breast cancer risk assessment (%) | Suggested approach |
|---|---|---|
| Low | <1.67 | MHT ok |
| Intermediate | 1.67 to 5 | Caution/Counseling |
| High | >5 | Avoid |
Reference:
- UTD
Hormone Therapy for Sexual Function in Postmenopausal Women
In early postmenopausal women (within 5 years of their last menstrual period), systemic estrogen slightly improves sexual function (i.e., desire, arousal, lubrication, orgasm, satisfaction, and pain)
There is insufficient evidence to support the use of systemic hormone therapy in postmenopausal women for sexual function alone; however, in women with vasomotor symptoms, the use of systemic estrogen therapy for other indications may result in a slight improvement in sexual function
Reference:
- AFP Vol 109 No 6 Jun 2024
Bio-identical HRT edit
Benefits of hormone replacement therapy are believed by many providers to include the following:
- Increased elasticity of the blood vessels, allowing them to dilate (widen) and let the blood flow more freely throughout the body
- Improved short-term symptoms of menopause such as hot flashes and mood swings, as well as vaginal dryness, dry skin, sleeplessness and irritable bladder symptoms
- Decreased risk of osteoporosis and fractures (broken bones)
- Decreased incidence of colon cancer
- Possible decreased incidence of Alzheimer's disease (data not conclusive)
- Possible improvement of glucose levels
The health risks of HRT include:
- Increased risk of endometrial cancer (only when estrogen is taken without progestin) For those who have had a hysterectomy (removal of the uterus), this is not a problem
- Increased risk of breast cancer with long-term use or depending on age
- Possible Increased risk of cardiovascular disease (including heart attack) with long-term use
- Increase in inflammatory markers (such as C-reactive protein)
- Increased risk of blood clots and stroke in susceptible patient (obese patients, those who smoke, those with history of clots
Heart attacks — The risk of having a heart attack related to use of hormone therapy appears to depend on your age. According to the landmark 2002 WHI study, there is no increased risk of heart attacks related to hormone therapy in women who:
- Became menopausal less than 10 years before starting hormones
- Were age 50 to 59 years when they took hormone therapy
Breast cancer — In the aforementioned WHI study using synthetic hormones primarily in those over 60, there was a small increased risk of breast cancer in those who took combined estrogen-progestin therapy but not in women who took estrogen alone. Those with a uterus must take progesterone with estrogen to prevent endometrial cancer. Those without a uterus can safely take estrogen alone.
For bio-identical HRT (FDA approved):
- Estrogen: Estrace 0.5 mg daily for 3 weeks with 1 week off
- If intact uterus: progesterone 100 mg qhs
Side effects:
- Breast soreness (d/t estrogen)
- Mood changes (d/t progesterone)
- Bloating (d/t progesterone)
- Vaginal bleeding - lower dose estrogen lowers risk
Reference:
- Files JA, Ko MG, Pruthi S. Bioidentical hormone therapy. Mayo Clin Proc. 2011 Jul;86(7):673-80, quiz 680. doi: 10.4065/mcp.2010.0714. Epub 2011 Apr 29. PMID: 21531972; PMCID: PMC3127562.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3127562/
- https://www.uptodate.com/contents/treatment-of-menopausal-symptoms-with-hormone-therapy
Continuous Glucose Monitoring
- 94% feel more aware of DM and impact
- 84% improve diet
Over The Counter Continuous Glucose Monitor (CGM)
No alarms on OTC CGMs!
Think about for:
- Type 2 DM not on insulin
- Pre-DM
- Interest in tracking glucose for health insights
Here are two options for OTC continuous glucose monitors:
- Stelo: https://www.stelo.com/en-us/buy-stelo-one-time
- $99 for 30 days (2 sensors)
- Lingo: https://www.hellolingo.com/products
- $49 for 2 weeks or $89 for 28 days
Notes: You use your phone as a receiver with an app
Pre-Diabetes
Lifestyle Interentions:
- Therapy team
- Frequent in-person visits initially
- Self-Monitoring
- Food types
- Portions
- Calories
- Min of activity
- Steps each day
- Dietary modification
- Decrease caloric intake by 700 cal/d
- Target saturated fats and simple sugars
- Weight loss
- Usual goal of >=7% BW if BMI >25
- Activity
- >=30 min/d for 5 d/wk
- Other
- Smoking cessation
- Improved sleep hygeine
- Stress reduction
- Medications
- Metformin (assess for Vit B12 with prolonged therapy)
Reference:
- Echouffo-Tcheugui JB, Perreault L, Ji L, Dagogo-Jack S. Diagnosis and Management of Prediabetes: A Review. JAMA. 2023;329(14):1206-1216. https://doi.org/10.1001/jama.2023.4063
Testosterone
See: Testosterone in Medications
General thoughts:
- Visceral adiposity affects leptin/inflammatory cytokines which affects testosterone (lowers) and hypothalamic dysfunction.
- Alcohol, opioids blunt testosterone production
Signs and Symptoms hypogonadism:
- Anemia
- Decline in cognitive function
- Decreased sexual function
- Decreased or absent morning erections
- Depressed mood
- Incomplete sexual development
- Increased fatigue
- Loss of axillary and pubic hair
- Loss of body hair
- Loss of muscle strength and work capacity
- Male factor infertility
- Reduced lean body mass
- Small testes
| Type | Lab | Origin | Possible causes |
|---|---|---|---|
| Primary | Decreased total Test | Congenital | Chrom abnormalities, cryptorchidism, FSH/LH receptor gene |
| Increased LH/FSH | mutations, Klinefelter syndrome, myotonic dystrophy | ||
| Acquired | Chemotherapy, hypothyroidism, orchitis/epididymo-orchitis, | ||
| radiation/trauma to testes, testicular torsion | |||
| Secondary | Decreased total Test | Congenital | Kallmann syndrome, Prader-Willi syndrome, other genetic |
| Decreased LH/FSH | Acquired | Chronic opioid use, hyperprolactinemia, pituitary tumors, | |
| sellar radiation, sleep deprivation, surgery, trauma | |||
| Mixed primary | Decreased total Test | Acquired | Aging, cancer, chronic glucocorticoid use, chronic kidney disease, |
| and secondary | Variable LH/FSH | chronic obstructive pulmonary disease, cirrhosis, diabetes mellitus, | |
| hemochromatosis, HIV, obesity |
Contraindications:
- Breast ca
- Hct >48%
- Fertility planning
- MI or CVA in last 6 months
- Prostate ca
- PSA >3ng/mL in high risk or >4 in others
- Severe lower urinary tract symptoms
- Thrombophilia
- Uncontrolled congestive heart failure
- Untreated severe OSA
References:
- AFP Vol 109 No 6 Jun 2024
- AFP Vol 96 No 7 Oct 2017
- FMX 2016
- JFP Vol 65, No 12 Dec 2016
Secondary hypogonadism
Lab results:
- Two morning total testosterone measurements <350 ng/dL (<10.4 nmol/L) AND
- Low or inappropriately normal LH level (<12 IU/L)
Dosing of enclomiphene citrate 6.25 mg/day, 12.5 mg/day and 25 mg/day
- The responder analysis suggests that the 12.5 mg dose is superior to the 6.25 mg dose in terms of bringing men into the mid-normal range.
- The 25 mg dose produces significantly greater levels of LH than either of the two lower doses
- Enclomiphene citrate treatment leads to a persistence of its total testosterone elevating activity for at least 1 week after discontinuation by maintaining LH
Adverse Effects of enclomiphene:
- Headache (was observed in 3.3% of patients)
- Nausea (was observed in 2.1% of patients)
- Diarrhea (was observed in 1.9% of patients)
- Common Cold (was observed in 1.7% of patients)
- Hot flash (was observed in 1.7% of patients)
- Joint pain (was observed in 1.2% of patients)
- Dizziness (was observed in 1% of patients)
- Study: Testosterone Restoration by Enclomiphene Citrate in Men with Secondary Hypogonadism: Pharmacodynamics and Pharmacokinetics.
Objectives
- To determine the pharmacodynamic profile of serum total testosterone and luteinizing hormone (LH) levels in men with secondary hypogonadism after initial and chronic daily oral doses of enclomiphene citrate vs transdermal testosterone.
- To determine the effects of daily oral doses of enclomiphene citrate in comparison with transdermal testosterone on other hormones and markers in men with secondary hypogonadism.
Patients and Methods
- This was a randomized, single-blind, two-centre, phase II study to evaluate the effects of three different doses of enclomiphene citrate (6.25, 12.5 and 25 mg) vs transdermal testosterone on 24-h LH and total testosterone in otherwise normal healthy men with secondary hypogonadism.
- Forty-eight men were enrolled in the trial (the intent-to-treat population), but four men had testosterone levels >350 ng/dL at baseline. Forty-four men completed the study per protocol. All subjects enrolled in this trial had serum total testosterone in the low range (<350 ng/dL) and had low to normal LH (<12 IU/L) on at least two occasions.
- Total testosterone and LH levels were assessed each hour for 24 h to examine the effects at each of three treatment doses of enclomiphene citrate vs a standard dose (5 g) of transdermal testosterone. In the initial profile, total testosterone and LH were determined in a naïve population after a single initial oral or transdermal treatment (day 1). This was contrasted to that seen after 6 weeks of continuous daily oral or transdermal treatment (day 42).
- The pharmacokinetics of enclomiphene citrate were assessed in a select subpopulation.
- Serum samples were obtained over the course of the study to determine the levels of various hormones and lipids.
Results
- After 6 weeks of continuous use, the mean (sd) concentration of total testosterone at day 42 was 604 (160) ng/dL for men taking the highest dose of enclomiphene citrate (enclomiphene citrate, 25 mg daily) and 500 (278) ng in those men treated with transdermal testosterone. These values were higher than day 1 values but not different from each other (P = 0.23, t-test).
- All three doses of enclomiphene citrate increased the testosterone concentration at time 0 of each 24-h sampling period, and the mean, maximum, minimum and range of testosterone concentrations over the 24-h sampling period. Transdermal testosterone also raised total testosterone, albeit with more variability, and with suppressed LH levels.
- The patterns of total testosterone over the 24-h period after 6 weeks of dosing could be fit to a nonlinear function with morning elevations, mid-day troughs, and rising night-time levels.
- Enclomiphene citrate and transdermal testosterone increased levels of total testosterone within 2 weeks, but they had opposite effects on FSH and LH.
- Treatment with enclomiphene citrate did not significantly affect levels of thyroid-stimulating hormone, adenocorticotropic hormone, cortisol, lipids or bone markers. Both transdermal testosterone and enclomiphene citrate decreased insulin-like growth factor-1 levels (P < 0.05) but suppression was greater in the enclomiphene citrate groups.
Conclusions
- Enclomiphene citrate increased serum LH and total testosterone; however, there was not a temporal association between the peak drug levels and the maximum concentration levels of LH or total testosterone.
- Enclomiphene citrate consistently increased serum total testosterone into the normal range and increased LH and FSH above the normal range. The effects on LH and total testosterone persisted for at least 1 week after stopping treatment.
Reference:
- Wiehle R, Cunningham GR, Pitteloud N, Wike J, Hsu K, Fontenot GK, Rosner M, Dwyer A, Podolski J. Testosterone Restoration by Enclomiphene Citrate in Men with Secondary Hypogonadism: Pharmacodynamics and Pharmacokinetics. BJU Int. 2013 Jul 12;112(8):1188–200. doi: 10.1111/bju.12363. Epub ahead of print. PMID: 23875626; PMCID: PMC4155868.
Endocrine Guidelines:
Diagnosis
- H&P - If symptoms -> test
- Morning Total Testosterone
- If low (<300ng/dL):
- Exclude reversible illness, drugs, nutritional deficiencies
- Repeat TT and also obtain LH+FSH
- If confirmed low TT and low or normal LH/FSH:
- Secondary
- Consider workup for pituitary disorders (prolactin, MRI)
- Rule out medication use, systemic illness, or chronic conditions as cause
- If confirmed low TT and high LH/FSH:
- Primary
- Consider chromosomal (Karyotye) testing
Monitoring:
- BPH: Monitor patients with benign prostatic hyperplasia (BPH) treated with androgens due to an increased risk for worsening signs and symptoms of BPH
- PSA: Monitor prostate specific antigen (PSA) levels periodically. Patients treated with androgens may be at increased risk for prostate cancer and should be evaluated prior to initiating and during treatment with androgens
- Hematocrit and Hemoglobin: Monitor hematocrit prior to and periodically during treatment. Hematocrit can be re-evaluated 3 to 6 months after initiation of therapy, and then annually thereafter. Monitor hemoglobin periodically. Increases in hematocrit, reflective of increases in red blood cell mass, may require lowering or discontinuation of testosterone. An increase in red blood cell mass may increase the risk of thromboembolic events
- Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE): If a venous thromboembolism (VTE) is suspected, discontinue AndroGel 1.62% and initiate appropriate workup and management. VTE, including DVT and PE, has been reported in patients using testosterone products
- Cardiovascular Risk: Some studies, but not all, have reported an increased risk of major adverse cardiovascular events (MACE) in association with use of testosterone replacement therapy in men. Patients should be informed of this possible risk when deciding whether to use or to continue to use AndroGel 1.62%
- Liver Function: Monitor liver function tests (LFTs) periodically. Treatment with androgens may lead to serious hepatic effects. AndroGel 1.62% is not known to cause these adverse effects
- Lipids: Monitor lipid concentrations periodically. Changes in serum lipid profile may require dose adjustment or discontinuation of testosterone therapy
- Serum Calcium Concentrations: Androgens should be used with caution in cancer patients at risk of hypercalcemia (and associated hypercalciuria). Regular monitoring of serum calcium concentrations is recommended in these patients
Monitor Pre-Dose Morning Serum Total Testosterone (Tt) Concentration:
- 14 And 28 Days
- Testosterone
- 3 And 6 Months
- Hematocrit
- Periodically
- Testosterone
- Psa
- Hemoglobin
- Lipids
- Lfts
- Serum Calcium Concentration (For Cancer Patients)
- After Dose Adjustment
- Testosterone
References:
- https://www.androgel.com/hcp/monitoring-patients
- AFP Vol 96 No 7 Oct 2017
- FMX 2016
How To Self Inject Testosterone
Here are some videos on how to self inject testosterone:
Lab Monitoring
- Check CBC at baseline and q3 months (annual if stable)
- If Hct >54% consider stopping therapy or periodi phlebotomy (monthly)
- Check PSA and Perform DRE at baseline and 3 and 6 months
- Follow screening guidelines of q6mo PSA
- Refer to urologist if PSA increases by >1.4mcg/L over 12mo
- Measure BMD at baseline and every 2 years if history of osteopenia or osteoporosis
- Evaluate formulation specific adverse events episodically and yearly
- Lipid panel and LFTs anually
For injection supplementation:
- Check midway between injections with goal 500-600
References:
- AFP Vol 96 No 7 Oct 2017
- FMX 2016
- JFP Vol 65, No 12 Dec 2016
- UpToDate
Normal Testosterone Levels by Age (20-45) edit
Normal testosterone levels in young adults (20-44 years old) vary by age.
- 20-24 years old: 409-558 ng/dL (normal range)
- 25-30 years old: 413-575 ng/dL (normal range)
- 30-34 years old: 359-498 ng/dL (normal range)
- 35-40 years old: 352-478 ng/dL (normal range)
- 40-44 years old: 350-473 ng/dL (normal range)
References:
- Zhu A, Andino J, Daignault-Newton S, Chopra Z, Sarma A, Dupree JM. What Is a Normal Testosterone Level for Young Men? Rethinking the 300 ng/dL Cutoff for Testosterone Deficiency in Men 20-44 Years Old. J Urol. 2022;208: 1295–1302
Other Medications
- Anastrozole
American Urologic Association guideline Arimidex, for off label use in men, Arimidex is dosed at 0.05 to 1mg every three days. Side effects of the medication include hot flashes, dyspnea, peripheral edema, and bone pain.
Typical doses:
- 0.05 - 1 mg qMWF
- Study: The Utilization and Impact of Aromatase Inhibitor Therapy in Men With Elevated Estradiol Levels on Testosterone Therapy
Testosterone therapy (TTH) for testosterone deficiency (TD) may lead to elevated estradiol (E2) levels requiring management to avoid unnecessary adverse effects.
Aim
- To examine the impact of aromatase inhibitors, specifically anastrozole (AZ), in men with elevated E2 on TTH.
Methods
- All patients on TTH at a high volume sexual medicine practice between 2005 and 2019 were reviewed. Men with E2 levels >60 pg/mL regardless of symptoms or 40–60 pg/mL with subjective symptoms were started on AZ 0.5 mg 3x/week.
- Routine hormone profile and symptom assessment were completed to ensure symptom resolution, reduction of E2 levels and maintenance of testosterone levels. Multivariable logistic regression was completed to determine predictors of men more likely to respond to therapy.
Main Outcome Measure
- Demographic and hormonal profiles of men on AZ and predictors of response to therapy.
Results
- 1708 men with TD were placed on TTH. Of these, 51 (3%) were treated with AZ (AZ+). After exclusions, 44 (2.6%) had elevated estradiol levels >60 pg/mL or >40 pg/mL with symptoms. Demographics were similar between groups. TTH distribution between groups was different with greater rates of topical TTH in the AZ- groups (AZ+:34.1% vs AZ-:53.5%) and greater rates of intramuscular TTH in the AZ+ group (AZ+:38.6% vs AZ-:18.5%) (P = .017 overall).
- Of the 44 men treated with AZ, 68.0% had pre-AZ E2 levels ≥60 pg/mL and 32.0% had levels between 40 and 60 pg/mL.
- Median pre-AZ E2 levels were 65 (interquartile range [IQR], 55–94) pg/mL in comparison to 22 (IQR 15–38) pg/mL post-AZ E2 levels (P < .001).
- Total testosterone levels were similar before and after AZ use (616 (IQR 548–846) ng/dL and 596 (IQR 419–798) ng/dL, respectively, P = .926).
- No statistically significant predictive factors of E2 reduction using AZ were found.
Conclusion
- While no statistically significant predictors for E2 recovery in men on AZ were found, AZ remains a reasonable option for E2 reduction in men with elevated levels on TTH.
Reference:
- Punjani N, Bernie H, Salter C, Flores J, Benfante N, Mulhall JP. The Utilization and Impact of Aromatase Inhibitor Therapy in Men With Elevated Estradiol Levels on Testosterone Therapy. Sex Med. 2021 Aug;9(4):100378. doi: 10.1016/j.esxm.2021.100378. Epub 2021 Jun 3. PMID: 34090245; PMCID: PMC8360915.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8360915/
- Clomiphene (Clomid)
Clomiphene Citrate (Brand name Clomid) is a selective estrogen receptor modulator. Initially developed in the 1960's to treat female infertility, Clomid is commonly used off-label in men to treat male infertility and low testosterone. In men with Low-T, Clomid is an excellent and effective oral medication to raise serum testosterone levels and improve the testosterone to estradiol ratio. Clomid can improve and raise testosterone. In some men Clomid can raise testosterone above 1000 ng/dL. Clomid works by blocking the estrogen receptor leading to an increase in both FSH and LH. These two signaling hormones released by the pituitary stimulate the testis to raise testosterone levels and enhance spermatogenesis (sperm production).
Typical doses for men:
- 25-50 mg 3/wk (qMWF)
- 25 mg daily
- Study: Enclomiphene Citrate Improves Hormone Levels While Preserving Sperm Production in Men With Secondary Hypogonadism
Introduction:
- Clomiphene citrate has been used off-label to increase luteinizing hormone (LH), follicle-stimulating hormone (FSH), and testosterone (T) in men with secondary hypogonadism. A newer agent, enclomiphene citrate, is the transisomer of clomiphene citrate and is being investigated for use in hypogonadal men. While clomiphene citrate consists of a mixture of isomers, enclomiphene citrate is a single isomer with pure estrogen antagonism.
Methods:
- This randomized phase IIB study enrolled 124 men with a morning serum T level of <250 ng/dL on 2 occasions. The subjects were randomized to one of two doses of enclomiphene citrate (12.5-mg or 25-mg), 1% topical testosterone, or placebo. Hormone levels of LH, FSH, and T and semen level were measured before, during and after 3 months of treatment.
- The primary end point was the change in morning total testosterone level from baseline to the end of the 3-month dosing period.
Results:
- A total of 113 men received 3 months of treatment, and 73 completed the study and provided both baseline and at least 1 semen sample at the end of the study. All 3 active treatment groups showed significantly increases in total testosterone level from baseline compared with placebo, with no statistically significant difference in testosterone levels found between the active treatment groups compared with placebo.
- Levels of LH and FSH increased in the 12.5-mg and 25-mg enclomiphene citrate groups (by 5.1 and 7.4 mIU/mL and by 4.8 and 6.9 mIU/mL, respectively), decreased in the topical T group (by –4.4 mIU/mL and –2.4 mIU/mL, respectively), and showed little change in the placebo group.
- Sperm concentration was significantly lower in the topical testosterone group compared with the 12.5-mg and 25-mg enclomiphene citrate groups after 3 months of treatment (P=0.008 and P=0.0007, respectively). In contrast, sperm concentration was not significantly different between the 2 enclomiphene citrate groups, or between these 2 groups and placebo.
- More than half (54%) of men in the topical T group became oligospermic during treatment compared with 14.6% of the enclomiphene citrate groups (P=0.001). No significant difference was found in the proportion of men who became oligospermic with enclomiphene citrate versus placebo.
- Only 4 patients withdrew from the study, 3 of whom received 25-mg enclomiphene citrate and 1 of whom received topical testosterone. Two of the withdrawals in the 25-mg enclomiphene citrate group were considered possibly related to the study drug: inability to climax and loss of sensation during intercourse in 1 patient, and mild nausea and mild dry heaving in 1 patient.
Conclusion:
- Use of 12.5-mg and 25-mg enclomiphene citrate significantly increased total T levels in hypogonadal men, with an efficacy that was comparable to topical testosterone.
- Increases in LH and FSH levels also were found with enclomiphene citrate treatment.
- In contrast to topical T, enclomiphene citrate did not adversely affect sperm concentration.
Reference:
- Wiehle RD, Fontenot GK, Wike J, et al. ZA-203 Clinical Study Group. Enclomiphene citrate stimulates testosterone production while preventing oligospermia: a randomized phase II clinical trial comparing topical testosterone. Fertil Steril. 2014;102(3):720-727.
Testosterone Levels by Age edit
| Guideline | Total testosterone cutoff (ng/dL) |
|---|---|
| American Association of Clinical Endocrinologists | 200 |
| Endocrine Society | 264 |
| American Urological Association | 300 |
| British Society of Sexual Medicine | 345 |
| European Association of Urology | 345 |
| International Society of Sexual Medicine | 350 |
| International Society for Study of Aging Male | 350 |
| Age group | Mean morning testosterone | Middle tertile |
|---|---|---|
| y | (ng/dL) | Levels |
| 20-24 | 501 | 409-558 |
| 25-29 | 514 | 413-575 |
| 30-34 | 456 | 359-498 |
| 35-39 | 438 | 352-478 |
| 40-44 | 430 | 350-473 |
| All men | 466 |
Reference:
- Zhu A, Andino J, Daignault-Newton S, Chopra Z, Sarma A, Dupree JM. What Is a Normal Testosterone Level for Young Men? Rethinking the 300 ng/dL Cutoff for Testosterone Deficiency in Men 20-44 Years Old. J Urol. 2022 Dec;208(6):1295-1302. doi: 10.1097/JU.0000000000002928. Epub 2022 Oct 25. PMID: 36282060.
Testosterone Order edit
Initiation (after labs)
- ICD10: E29.1
- Testosterone cypionate 100mg/ml 1ml (100 mg) q2 wks
- B-D #9571 SYR/NDL 3ML 23GX1 LL, 30 syringes for 90 days / Use to inject medication
- B-D #5195 Needles 18Gx1, 30 units for 90 days / Use to draw up medication as directed
Who to treat
Low T Diagnosis = low testosterone with symptoms
- Consider testosterone replacement in those with both laboratory and clinical evidence of hypogonadism (SOR B)
- Consider in symptomatic men with clinical symptoms to improve sexual function, well-being, lean muscle mass and bone density (++)
- Offer to men with low T and low libido/ED in addition to pursuing additional workup and therapies (++)
- Consider offering short term replacement to men on chronic glucocorticoids with low T levels (+)
- Recommend AGAINST in men with breast or prostate cancer or with a PSA >4ng/ml (+)
Postmenopausal women for hypoactive sexual desire disorder
- Recommended dosage is 300mcg/day (need compound pharmacy)
- Begin with 6mo trial period, continue only if patient responds favorable
- No effectiveness data after 24mo
Contraindications to starting testosterone therapy
| Absolute | Relative |
|---|---|
| Breast Ca | Baseline Hct >50% |
| Polycythemia (Hct >54%) | Desire for fertility |
| Prostate Ca | Severe lower urinary tract symtoms |
| PSA >4mcg/L or nodule on DRE | Uncontrolled HF |
| Untreated OSA |
Reference:
- AFP Vol 96 No 7 Oct 2017
- FMX 2016
- JFP Vol 65, No 12 Dec 2016
Thyroid
Notes: Unnecessary levothyroxine treatment of subclinical disease may lead to increased fractures and cardiac arrhythmias.
If TSH levels are elevated, free T3 levels should be obtained. If TSH levels are below normal, free T4 and Total T3 levels should be obtained for diagnosis of hyperthyroidism
Hyperthyroidism
Etiology:
- Graves disease
- Toxic multinodular goiter and toxic adenoma
- Thyroiditis
- Subclinical hyperthyroidism
| Medical condition | Thyrotropin | T3 and T4 | Radioactive iodine uptake scan pattern |
|---|---|---|---|
| Graves Disease | Suppressed | Elevated | Diffuse high uptake |
| Toxic adenoma | Suppressed | Elevated | High uptake in focal spot |
| Toxic multinodular goiter | Suppressed | Elevated | High uptake with concentration into multiple spots |
| Subclinical hyperthyroidism | Suppressed or Low | Normal | Depending on etiology |
| Subacute painful and painless thyroiditis | Suppressed early, elevated late but may return to normal | Elevated early, suppressed late, but may return to normal | Low |
| TSH < 0.1 mIU/L | TSH 0.1-0.4 mIU/L | |
|---|---|---|
| >65yo | Treat | Consider Treat |
| <65yo and asymptomatic | Consider Treat | Observe |
| <65yo and: | ||
| - Heart disease | Treat | Consider Treat |
| - Hyperthyroid symptoms | Treat | Consider Treat |
| - Osteoporosis | Treat | Consider Treat |
| - Postmenopausal | Treat | Consider Treat |
Reference:
- AFP Vol 95 No 11 Jun 2017
- AFP Vol 112 No 2 Aug 2025
- Graves Disease
Graves disease requires one of the three treatment options:
- an antithyroid medication (methimazole [Tapazole] or propylthiouracil)
- radioactive iodine (I-131) ablation of the thyroid gland
- surgical thyroidectomy
The choice of treatment depends on the benefits vs. risks in a specific clinical situation and on the patient's preference.
Antithyroid Medications.
- Antithyroid medications are thionamides; they inhibit thyroid peroxidase, blocking the synthesis of T3 and T4
- Graves disease remits in up to 30% of patients treated with thionamides, these medications can be used as the initial treatment, with ablation or thyroidectomy performed if remission does not occur.25,26 Once medical therapy is discontinued, relapse occurs in 30% to 70% of patients, mostly within the first year.27 After discontinuation, thyroid function should be monitored every one to three months for six to 12 months, and the patient should be instructed to contact the physician if symptoms recur.
For patients using methimazole, the prevalence of agranulocytosis is 0.17%, the incidence of hepatitis is 3.17 per 1,000 person-years, and the incidence of acute hepatic failure is 0.32 per 1,000 person-years
Patients should be instructed to discontinue medication use and contact their physician if they develop jaundice, acholic stools, dark urine, arthralgias, abdominal pain, nausea, vomiting, fever, or sore throat. A baseline complete blood count (CBC) with differential and a hepatic panel should be obtained before initiating an antithyroid medication. Subsequent routine monitoring of CBC is unnecessary, but CBC with differential should be obtained if fever and/or pharyngitis develop.
Free T4 and total T3 should be obtained four weeks after starting a thionamide and every four to eight weeks thereafter with the dosage adjusted based on results. Once free T4 and total T3 levels normalize, they should be monitored every three months. Serum TSH is of limited value early in the treatment course because levels may remain suppressed for several months after treatment is started. An antithyroid medication should be continued for 12 to 18 months, then tapered or discontinued if the TSH level is normal at the time. Elevated or above-normal TSH levels (greater than 4.0 mIU per mL) at antithyroid drug discontinuation is associated with an increased likelihood of permanent remission
Radioactive Iodine Ablation. Radioactive iodine ablation of the thyroid gland is the most common treatment of Graves disease in the United States. It is contraindicated in pregnancy. Moderate to severe Graves orbitopathy is a relative contraindication, especially in patients who smoke, because radioactive iodine may exacerbate the eye disease.32,33 In mild cases of Graves orbitopathy, radioactive iodine ablation can be performed with concomitant glucocorticoid therapy. Nonradioactive iodine impedes radioactive iodine uptake by iodide transporter; therefore, exposure to large amounts of nonradioactive iodine (e.g., iodinated contrast, amiodarone) should be avoided within three months before radioactive iodine ablation. Pregnancy should be ruled out within 48 hours before radioactive iodine ablation and avoided for six months thereafter.1 A thionamide should be discontinued at least five days before the treatment but can be restarted three to five days after to maintain control of thyroid function, because it may take up to 12 weeks to achieve the full effect of radioactive iodine.
Most patients develop permanent hypothyroidism between two and six months after radioactive iodine ablation and require thyroid hormone supplementation.1,33 Free T4 and total T3 should be measured four to eight weeks after ablation; if hyperthyroidism persists, these indices should be monitored every four to six weeks and thyroid hormone replacement started in the early stages of hypothyroidism.1
Thyroidectomy. This treatment option is preferred in patients with goiter-induced compressive symptoms and in patients with contraindications to radioactive iodine ablation or thionamides. Besides general anesthesia risk, thyroidectomy carries a risk of inadvertently injuring parathyroid glands and recurrent laryngeal nerves.
Reference:
- Am Fam Physician. 2016;93(5):363-370
- https://www.aafp.org/pubs/afp/issues/2016/0301/p363.html
Hypothyroidism edit
When treating primary hypothyroidism, levothyroxine should be adjusted based on normalizing TSH and not free T4 levels
Treatment of subclinical hypothyroidism is recommended if TSH is > 10mIU/L or thyroid peroxidase antibody is elevated.
Reference:
- AFP Sep 2025 Vol 112 No 3
A Total T4 measures the bound and free hormone and can change when binding proteins differ. A Free T4 measures what is not bound and able to enter and affect the body tissues.
An elevated TSH and low FT4 or FTI indicates primary hypothyroidism due to disease in the thyroid gland. A low TSH and low FT4 or FTI indicates hypothyroidism due to a problem involving the pituitary gland. A low TSH with an elevated FT4 or FTI is found in individuals who have hyperthyroidism.
Two common antibodies are thyroid peroxidase antibody and thyroglobulin antibody. Measuring levels of thyroid antibodies may help diagnose the cause of the thyroid problem.
For example, positive anti-thyroid peroxidase and/or anti-thyroglobulin antibodies in a patient with hypothyroidism result in a diagnosis of Hashimoto's thyroiditis.
While detecting antibodies is helpful in the initial diagnosis of hypothyroidism due to autoimmune thyroiditis, following their levels over time is not helpful in detecting the development of hypothyroidism or response to therapy.
TSH and FT4 are what tell us about the actual thyroid function or levels.
A stimulatory TSH receptor antibody (TSI) antibody causes the thyroid to be overactive in Graves' Disease.
If you have Graves' disease, your doctor might also order a thyrotropin receptor antibody test (TSHR or TRAb), which detects both stimulating and blocking antibodies.
- Medications That Interfere With Thyroid Function Testing
There are many medications that can affect thyroid function testing. Some common examples include:
- Estrogens, such as in birth control pills, or in pregnancy, cause high levels of total T4 and T3. This is because estrogens increase the level of the binding proteins. In these situations, it is better to ask both for TSH and free T4 for thyroid evaluation, which will typically be in the normal range.
- Biotin, a commonly taken over-the-counter supplement, can cause the measurement of several thyroid function tests to appear abnormal, when they are in fact normal in the blood. Biotin should not be taken for 2 days before blood is drawn for thyroid function testing to avoid this effect.
- Levothyroxine Dosing Adjustments
TSH Amt to increase 5 to <10 25-50 mcg/d 10-20 50-75 mcg/d >20 75-100 mcg/d Initial levothyroxine dose:
- Young, healthy patients can receive the full anticipated dose: 1.6 mcg/kg/day
- Older patients (≥60 years) and those with coronary heart disease should start with a lower dose: 25 to 50 mcg daily
- Levothyroxine should be taken on an empty stomach with water, ideally 30 to 60 minutes before breakfast.
Delay levothyroxine until after lab drawn
- No effect on TSH, Free T3, Total T4
- Free T4 peaks two hours after taken - so can be affected
References:
- AFP Vol 89, No 4 Feb 2014
- Uptodate
- When To Refer For Hypothyroidism
- Age <18yo
- Cardiac disease
- Coexisting endocrine diseases
- Myxedema coma suspected
- Pregnancy
- Presence of goiter, nodule, or other structural thyroid gland abnormality
- Unresponsive to therapy
References:
- Endocr Pract. 2008;14(6):802-803
Thyroid nodules
Thyroid nodules >1 mc that are solid of have suspicious features such as microcalcifications or irregular marins -> FNA to r/o malignancy
Thyroid Nodule Testing
- Thyroid ultrasonography with a survey of the cervical lymph nodes should be performed in all patients with thyroid nodules.
- The serum thyroid-stimulating hormone level should be measured during the initial evaluation of a thyroid nodule.
- If it is low, a radionuclide thyroid uptake scan should be performed.
| Diagnostic Category | ROM | ROM | Usual Management |
|---|---|---|---|
| Mean % | (range) | ||
| Nondiagnostic | 13 | (5-20) | Repeat FNA with ultrasound guidance. |
| Benign | 4 | (2-7) | Clinical and sonographic follow-up. |
| Atypia of Undetermined Significance | 22 | (13-30) | Repeat FNA, molecular testing, diagnostic lobectomy, or surveillance. |
| Follicular Neoplasm | 30 | (23-34) | Molecular testing, diagnostic lobectomy. |
| Suspicious for Malignancy | 74 | (67-83) | Molecular testing, lobectomy or near-total thyroidectomy. |
| Malignant | 97 | (97-100) | Lobectomy or near-total thyroidectomy. |
Associated findings with malignant nodules:
- H/o differentiated thyroid cancer in a 1st degree relative
- H/o radiation exposure as a child or adolescent
- Prior diagnosis of thyroid carcinoma
- Male sex
- Focal uptake of 18F-flourodeoxyglucose by the thyroid
- Personal of FH of MEN type 2 or familial medullary thyroid cancer
- Serum calcitonin level >50-100pg/ml
- Residence near a nuclear reactor accident
Reference:
- AFP Jun 2021 Vol 103 No 12
- https://www.aafp.org/afp/2020/0901/p298.html
- NEJM 373;24 Dec 2015
- Ali, S. Z., & Vanderlaan, P. A. (2023). The Bethesda System for Reporting Thyroid Cytopathology Definitions, Criteria, and Explanatory Notes (third ed). New York, NY: Springer.
Diabetes Type 1 (T1D)
Who to screen:
- Those with a family history of T1D are at greater risk of developing the disease (up to a 15-fold increased risk if a first-degree relative has T1D)
- Those with associated autoimmune diseases
- celiac disease
- autoimmune thyroiditis
- Adults with abnormal glucose levels with a low BMI (<25 kg/m2) or aged <35 years
When to screen:
- T1D most commonly occurs in children, teenagers, or young adults
- Autoantibodies often emerge before the age of 6
- Screening for islet autoantibodies at ages of 2 and 6 has proven to be sensitive and efficient in predicting autoimmune T1D
- Recommendations:
- Fist: Between ages 2-4
- Second: Between ages 6-9
What to screen - The autoantibodies detected in autoimmune T1D include
- Glutamic acid decarboxylase antibodies (GADA)
- Insulinoma-associated-2 autoantibodies (IA-2A)
- Insulin autoantibodies (IAA)
- Zinc transporter 8 autoantibodies (ZnT8A)
| Autoantibody | Islet specificity | Typical characteristics |
|---|---|---|
| Insulin Autoantibody (IAA) | Insulin | Common as a first detected autoantibody in young children |
| Appearance is more common in younger children | ||
| Frequency of appearance declines with age | ||
| Not informative for individuals treated with insulin, who often develop antibodies in response to injected insulin | ||
| Glutamic Acid Decarboxylase Autoantibody (GADA) | GAD | Common as a first detected autoantibody in childhood, up until age 15 years |
| Adult-onset cases most often present with GADA | ||
| Is associated with slower progression to T1D and is often found as a single positive islet autoantibody, especially in adults | ||
| Islet Antigen 2 Autoantibody (IA-2A also known as ICA512) | Tyrosine phosphatase islet antigen-2 | Presence is associated with more-advanced islet autoimmunity and faster progression to stage 3 T1D |
| Zinc Transporter 8 Autoantibody (ZnT8A) | Zinc transporter type 8, a transmembrane protein in the beta cell granule | Presence can improve risk stratification in individuals with single GADA+, IAA+ or IA-2A+ status |
| ICA | Multiple antigens, undefined | Detected by indirect immunofluorescence on islet cell tissue. While not frequently measured other than in research studies, it does add to risk determination in the presence of other biochemical autoantibodies |
Notes: IA-2A, insulinoma antigen-2 autoantibody; ICA512, islet cell autoantigen 512; T1D, type 1 diabetes
| Lab Codes | Diagnosis Codes | Monitoring Codes |
|---|---|---|
| Quest: 13621 | Z13.1 | E10.A0 |
| LabCorps: 504050 | Z83.3 | E10.A1 |
| Z83.49 | ||
| R73.9 |
Islet Autoantibody and risk of T1D
- The number of detectable autoantibodies through screening correlates with risk of developing autoimmune T1D
- The majority of individuals with a single autoantibody do not progress to autoimmune T1D
- The presence of 2+ autoantibodies increases the risk of progression to clinical T1D to 70% over 10 years and 100% over lifetime
Management
- A positive screening for presence of ≥2 autoimmune T1D antibodies indicate that the individual is in presymptomatic stage of autoimmune T1D (Stage 1 autoimmune T1D)
- Perform metabolic monitoring for the presence of glucose abnormalities:
- Presence of dysglycemia (Indicates Stage 2 autoimmune T1D)
- fasting plasma glucose ≥100 mg/dL [≥5.6 mmol/L]
- 2-hour plasma glucose with 75 gm OGTT ≥140 mg/dL [≥7.8 mmol/L]
- 30/60/90 min glucose ≥200 mg/dL [≥11.1 mmol/L]
- HbA1c ≥5.7% [≥39 mmol/mol])
- Individuals in this stage have a 100% risk of progressing to symptomatic Stage 3 autoimmune T1D within the next 15 years
- Provide relevant disease-related education and psychosocial support needed to prepare for a possible Stage 3 autoimmune T1D diagnosis
- Presence of dysglycemia (Indicates Stage 2 autoimmune T1D)
- Testing C-peptide can help you assess measure of beta-cell function and distinguish stages of T1D
- Perform metabolic monitoring for the presence of glucose abnormalities:
- 2024 ADA guidelines on Comprehensive Medical Evaluation and Assessment of Comorbidities recommend screening for autoimmune thyroid disease soon after a T1D diagnosis
Reference:
- Consensus guidance for monitoring individuals with islet autoantibody-positive pre-stage 3 type 1 diabetes | Diabetologia
- Screening for autoimmune T1D: Identify at-risk individuals
- Katsarou A, Gudbjörnsdottir S, Rawshani A, et al. Type 1 diabetes mellitus. Nat Rev Dis Primers. 2017;3:17016.
- Insel RA, Dunne JL, Atkinson MA, et al. Staging presymptomatic type 1 diabetes: A scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association. Diabetes Care. 2015;38(10):1964-1974.
- Tiberti C, Yu L, Lucantoni F, et al. Detection of four diabetes specific autoantibodies in a single radioimmunoassay: an innovative high-throughput approach for autoimmune diabetes screening. Clin Exp Immunol. 2011;166(3):317-324.
- Cortez FJ and Gebhart D, Robinson PV, et al. Sensitive detection of multiple islet autoantibodies I type 1 diabetes using small sample volumes by agglutination-PCR. PLoS One. 2020;15(11):e0242049.
- Sims EK, Besser REJ, Dayan C, et al; NIDDK Type 1 Diabetes TrialNet Study Group. Screening for type 1 diabetes in the general population: A status report and perspective. Diabetes. 2022;71(4):610-623.
- Simmons KM and Sims EK. Screening and prevention of type 1 diabetes: Where are we? J Clin Endocrinol Metab. 2023;108(12):3067-3079.
- DiMeglio LA, Evans-Molina C and Oram RA. Type 1 diabetes. Lancet. 2018;391(10138):2449–2462.
- Ziegler AG and Nepom GT. Prediction and pathogenesis in type 1 diabetes. Immunity. 2010;32(4):468-78.
- Makimattila S, Harjutsalo V, Forsblom C, et al. Every fifth individual with type 1 diabetes suffers from an additional autoimmune disease: a Finnish nationwide study. Diabetes Care. 2020;43(5):1041-1047.
- American Diabetes Association. Standards of care in diabetes—2024. Diabetes Care. 2024;47(suppl 1):S1-S321.
- You W-P and Henneberg M. Type 1 diabetes prevalence increasing globally and regionally: The role of natural selection and life expectancy at birth. BMJ Open Diabetes Research and Care. 2016;4:e000161.
- Ghalwash M, Dunne JL, Lundgren M, et al. Two-age islet-autoantibody screening for childhood type 1 diabetes: a prospective cohort study. Lancet Diabetes Endocrinol. 2022;10(8):589-596.
- Greenbaum CJ. A Key to T1D Prevention: Screening and monitoring relatives as part of clinical care. Diabetes. 2021;70:1029–1037.
- Monitoring Autoantibodies for Early Autoimmune T1D Detection
- Phillip M, Achenbach P, Addala A, et al. Consensus guidance for monitoring individuals with islet autoantibody-positive pre-stage 3 type 1 diabetes. Diabetologia. Published online June 24, 2024. https://doi.org/10.1007/s00125-024-06205-5
- Mameli C, Triolo TM, Chiarelli F, Rewers M, Zuccotti G, Simmons KM. Lessons and gaps in the prediction and prevention of type 1 diabetes. Pharmacol Res. 2023;193:106792. https://doi.org/10.1016/j.phrs.2023.106792
- Insel RA, Dunne JL, Atkinson MA, et al. Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association. Diabetes Care. 2015;38(10):1964-1974. https://doi.org/10.2337/dc15-1419
- Besser REJ, Bell KJ, Couper JJ, et al. ISPAD Clinical Practice Consensus Guidelines 2022: Stages of type 1 diabetes in children and adolescents. Pediatr Diabetes. 2022;23(8):1175-1187
- Greenbaum CJ. A Key to T1D Prevention: Screening and Monitoring Relatives as Part of Clinical Care. Diabetes. 2021;70(5):1029-1037. https://doi.org/10.2337/db20-1112
- Helminen O, Aspholm S, Pokka T, et al. OGTT and random plasma glucose in the prediction of type 1 diabetes and time to diagnosis. Diabetologia. 2015;58(8):1787-1796.
ENT (Otolaryngology)
Allergic rhinitis
- Flonase/nasonex
- Treat all symptoms also w/ nonallergic
- Check compliance
- 2nd gen oral antihistamines
- Tx pruritis and rhinorrhea not well for congestion
- Pseudoephedrine increases SBP 1 mmHg no change DBP increase pulse 3 bpm
- Salerno SM, Jackson JL, Berbano EP. Effect of oral pseudoephedrine on blood pressure and heart rate: a meta-analysis. Arch Intern Med. 2005;165:1686-1694)
References:
- Consultant Apr 2010 vol 50 no 4
Allergy tips
General Allergy Tips
- If you exercise outdoors, wait until evening to do your routine; pollen counts are lower towards night!
- If you need to mow the lawn or do outdoor yard work, consider wearing a dust mask.
- If you have ragweed allergies, remove the plants in your yard before they bloom to help cut down on the pollen in your area!
- Clean your HVAC system regularly, as dust can build up over time and create irritants.
- Purchase a HEPA filter or air filtration unit; these can really reduce the amount of allergens in your home!
- Mold-Specific Tips
- Don't hang your wet clothing indoors to dry; this can make mold allergies worse.
- Reduce the amount of mold in your home! Keep basements, bathrooms, and any other room which retains humidity well-ventilated by opening windows frequently, or purchasing a dehumidifier.
- Heat helps mold grow, so setting up a heater alone can make the problem worse!
- If you have a carpeted room which is prone to mildew or mold, replacing the flooring with wood or tile may be a good idea!
- Regularly clean garbage cans, sinks, and water-based appliances with a bleach solution to keep mold from building up and spreading.
Anosmia
See also:
Anosmia
- If nasal congestion from a cold or allergy is the cause of anosmia, treatment is usually not needed, and the problem will get better on its own. Short-term use of over-the-counter decongestants may open up your nasal passages so that you can breathe easier.
- If a polyp or growth is present, surgery may be needed to remove the obstruction and regain your sense of smell.
- If you suspect a medication is affecting your sense of smell, consider alternative medications
- Sometimes a person will regain their sense of smell spontaneously.
- If you smoke, quit. Smoking can dull your senses, including your sense of smell.
- Unfortunately, anosmia is not always treatable, especially if age is the cause.
- Safety:
- Put fire detectors and smoke alarms in your home and office and
- Take extra care with leftovers. If you have any doubt about a food's safety, don't eat it.
- Safety:
Common causes:
- Changes in sense of smell are most often caused by:
- a cold or flu
- sinusitis (sinus infection)
- an allergy, like hay fever
- growths in your nose (nasal polyps)
- These can cause:
- loss of smell (anosmia)
- smelling things that are not there (phantosmia), like smoke or burnt toast
- reduced sense of smell (hyposmia)
- changes to how things smell (parosmia)
Smell Training:
Aphthous Stomatitis (Canker Sores)
Anyone can develop canker sores. But they occur more often in teens and young adults, and they're more common in females.
Mouth ulcers can be caused by a wide range of factors including:
- Accidentally biting the inside of your cheek.
- Injury from a toothbrush (such as slipping while brushing).
- Constant rubbing against misaligned or sharp/broken teeth.
- Constant rubbing against dentures or braces.
- Burns from eating hot food.
- Irritation from strong antiseptics, such as a mouthwash.
- Aphthous ulcers.
- Viral infections such as the herpes simplex viral infection (cold sore virus).
- Reaction to certain medications.
- Skin rashes in the mouth (for example, lichen planus).
- Autoimmune diseases.
- Underlying Vitamin B2, folate or iron deficiency.
- Underlying gastrointestinal disease such as Crohn's disease or coeliac disease.
- Mouth cancer.
- Ulcers may become worse during periods of stress, illness or extreme fatigue.
Prevention
Canker sores often recur, but you may be able to reduce their frequency by following these tips:
- Watch what you eat. Try to avoid foods that seem to irritate your mouth. These may include nuts, chips, pretzels, certain spices, salty foods and acidic fruits, such as pineapple, grapefruit and oranges. Avoid any foods to which you're sensitive or allergic.
- Choose healthy foods. To help prevent nutritional deficiencies, eat plenty of fruits, vegetables and whole grains.
- Follow good oral hygiene habits. Regular brushing after meals and flossing once a day can keep your mouth clean and free of foods that might trigger a sore. Use a soft brush to help prevent irritation to delicate mouth tissues, and avoid toothpastes and mouth rinses that contain sodium lauryl sulfate.
- Protect your mouth. If you have braces or other dental appliances, ask your dentist about orthodontic waxes to cover sharp edges.
- Reduce your stress. If your canker sores seem to be related to stress, learn and use stress-reduction techniques, such as meditation and guided imagery.
Prevention of mouth ulcers
- Brushing your teeth gently with a soft toothbrush, taking care not to slip with the brush.
- Eating a well-balanced and nutritious diet.
- Making sure that underlying medical conditions are well-controlled.
- Keeping a healthy lifestyle, including appropriate nutrition, exercise, and rest, decreases the frequency of outbreaks.
Treatment options for mouth ulcers include:
- Avoid spicy, salty and sour foods until the ulcers heal.
- Drink plenty of fluids.
- Keep your mouth clean.
- Rinse your mouth out with warm, slightly salted water, keeping the rinse in your mouth for up to 4 minutes at a time. Repeat four times daily.
- Use an alcohol-free medicated (preferably containing chlorhexidine gluconate) mouthwash twice daily.
| Agent | Dosage | Evidence for use |
|---|---|---|
| Tetracycline capsule, 250 mg | 1 capsule dissolved in 180 mL of water; rinse with this suspension four times daily for 4 to 5 days | Randomized, controlled studies1 support use |
| Tetracycline syrup, 250 mg per 5 mL | 5 mL "swish and spit" four times daily for 4 to 5 days | As above |
| Minocycline tablet, 100 mg | 1 tablet dissolved in 180 mL of water; rinse with this suspension twice daily for 4 to 5 days | As above |
| Triamcinolone 0.1% in Orabase (Kenalog in Orabase) | Apply to dried ulcer two to four times daily until healed | Randomized, controlled studies1 show decreased pain |
| Dexamethasone elixir, 0.5 mg per 5 mL | Swish and spit with 5 mL every 12 hours | As above |
| Thalidomide | 200 mg, one to two times daily for 3 to 8 weeks Warning: contraindicated in pregnancy | Studies in HIV-infected patients only7 |
| Amlexanox 5% paste | Apply to dried ulcer two to four times daily | Randomized, controlled studies9,10 show decreased symptoms and faster healing |
| Viscous lidocaine, 2% | Apply to ulcer as needed | For brief local pain relief only |
| Zinc lozenges | Suck one lozenge four to six times daily | No studies |
| Vitamin C, 500 mg | One tablet, four times daily | No studies |
| Vitamin B complex | One tablet, four times daily | No studies |
| l-Lysine, 500 mg | One tablet, one to three times daily | Studies in herpes only |
Treatment options for mouth (aphthous) ulcers include:
- Avoid spicy, salty and sour foods until the ulcers heal.
- Drink plenty of fluids.
- Keep your mouth clean.
- Rinse your mouth out with warm, slightly salted water, keeping the rinse in your mouth for up to 4 minutes at a time. Repeat four times daily.
- A saltwater rinse is a simple yet effective method for reducing canker sore pain. Dissolve about a teaspoon of salt in a cup of warm water, swish it around your mouth for 15-30 seconds, and then spit it out.
- Similarly, applying a baking soda paste (made by mixing baking soda with a little water) directly onto the sore can help reduce inflammation and promote healing by neutralizing the acidic environment.
- Use an alcohol-free medicated (preferably containing chlorhexidine gluconate) mouthwash twice daily.
- OTC numbing creams or gels, which often contain active ingredients such as benzocaine or hydrogen peroxide, can alleviate pain and discomfort temporarily.
- Applying these treatments directly to the sore several times a day can help numb the area, allowing you to eat and speak more comfortably.
Reference:
- Am Fam Physician. 2000;62(1):149-154
- Recurrent Aphthous Stomatitis
Cerumen
Cerumen is a Hydrophobic protective covering which protects ear canal from:
- Water damage
- Trauma
- Foreign Bodies
- Infection (intrinsic bactericidal activity)
Cerumen accumulation is usually asymptomatic, but can cause the following symptoms:
- Hearing loss, Tinnitus
- Earache, Ear fullness, Itchiness
- Reflex cough
- Dizziness
Reference:
Carbamide peroxide (Debrox)
I recommend using Debrox (Carbamide peroxide), which is over the counter without a prescription:
- Use Debrox twice a day for up to 4 days as needed
- For each use, approximately 5-10 drops should be placed in the affected ear(s)
- It may make mild bubbling or crackling sounds, this is ok
- Any earwax remaining after treatment may be removed by gently flushing the ear with warm water
- Please refer to the package for complete directions
Chronic Rhinosinusitis
Diagnostic Criteria:
- The presence of at least 2 of the following for 12 consecutive weeks (in order of frequency)
- Nasal obstruction
- Nasal drainage
- Facial pain/pressure
- Hyposmia/anosmia
- Objective evidence on physical examination or radiology (Sinus CT) such as
- Mucopurulent drainage
- Edema
- Polyps in middle meatus
Reference:
- AFP Vol 96 No 8 Oct 2017
Hoarseness
Vocal quality vs diagnosis:
- Breathy
- Inflammatory arthritis
- Spasmodic or functinoal dysphonia
- Vocal fold mass
- Vocal fold paralysis
- Halting, stangled
- Spasmodic dysphonia
- Hoarse, husky, muffled, or nasal sounding
- Parkinson disease
- Hoarseness worse early in day
- GERD
- Laryngopharyngeal reflux (LPR)
- Hoarseness worse later in day
- Myasthenia gravis
- Vocal abuse
- Low pitched
- GERD
- Hypothyroidism
- LPR
- Leukoplakia
- Muscle tension dysphonia
- Reinke edema
- Vocal fold edema
- Age-related vocal atrophy in women
- Raspy or harsh
- GERD
- LPR
- Muscle tension dysphonia
- Vocal fold lesion
- Scanning speech and dysarthria
- Multiple sclerosis
- Soft (loss of volume)
- Vocal fold paralysis
- Parkinson disease
- Age-related vocal atrophy
- Spoken voice lost, but whispered maintained
- Conversion aphonia
- Strained
- GERD
- LPR
- Muscle tension dysphonia
- Spasmodic dysphonia
- Strained, effortful phonation
- Muscle tension dysphonia
- Thick, deep voice and slowed speech
- Acromegaly
- Vocal fatigue
- Muscle tension dysphonia
- Myasthenia gravis
- Parkinson disease
- Vocal abuse
- Age-related vocal atrophy
References:
- AFP Vol 96 No 11 Dec 2017
Motion Sickness/Vestibular Nause
See also:
Scopolamine patch:
- Apply 1 patch behind ear at least 4-12 hours (preferably 12 hr) before anticipated exposure to motion, then every 3 days as needed
Neti Pots
These devices all work in basically the same way:
- Leaning over a sink, tilt your head sideways with your forehead and chin roughly level to avoid liquid flowing into your mouth.
- Breathing through your open mouth, insert the spout of the saline-filled container into your upper nostril so that the liquid drains through the lower nostril.
- Clear your nostrils. Then repeat the procedure, tilting your head sideways, on the other side.
To use and care for your device:
- Wash and dry your hands.
- Check that the device is clean and completely dry.
- Prepare the saline rinse, either with the prepared mixture supplied with the device, or one you make yourself.
- Follow the manufacturer's directions for use.
- Wash the device, and dry the inside with a paper towel or let it air dry between uses.
From:
Olfactory Training edit
See also:
Perform the following twice daily ideally before a meal for at least 4-6 months:
- Use essential oils soaked in cotton, or liquid (50 ml) in an amber sniffing jar
- Use the following recommended scents initially:
- Rose
- Eucalyptus
- Lemon
- Clove
- Smell the first scent for 15-20 sec, while smelling, focus on what you remember it smelling like
- Rest for 10 sec
- Repeat as above for each scent separately
- Every 1-3 months consider changing or adding scents such as:
- Menthol
- Thyme
- Tangerine
- Jasmine
- Green tea
- Bergamot
- Rosemary
- Gardenia
Reference:
- AFP Sep 2023 Vol 108 No 3
Otitis Externa
(See My Formulary: Neomycin - polymyxin B - hydrocortisone otic 4 gtts tid)
- Cortisporin otic 10 ml 4 drops in affected ear q6-8 hrs for 10 days
Medications:
- 2% acetic acid solution - VoSol
- With hydrocortisone (VoSoL HC Otic)
- With aluminum acetate (Otic Domeboro)
- Advantages
- Generic product is inexpensive and effective against most infections without causing sensitization
- Disadvantages
- Can be irritating to inflamed external auditory canal; possibly ototoxic
- Neomycin otic preparations
- With polymyxin B–hydrocortisone (Cortisporin)
- With hydrocortisone-thonzonium (Coly-Mycin S)
- Advantages
- Effective, and generic product is inexpensive
- Disadvantages
- Can be a potent sensitizer, causing contact dermatitis in 15% of patients; ototoxic
- Polymyxin B - hydrocortisone (otobiotic)
- Advantages
- Avoids potential neomycin sensitization
- Disadvantages
- No activity against Staphylococcus and other gram-positive microorganisms
- Advantages
- Aminoglycoside ophthalmic solutions
- Gentamicin sulfate 0.3% (Garamycin)
- Tobramycin sulfate 0.3% (Tobrex)
- Advantages
- Less locally irritating than 2% acetic acid solution, neomycin otic preparations or polymyxin B alone
- Disadvantages
- Potential ototoxicity; moderately expensive
- Quinolone otic and ophthalmic solutions
- Ofloxacin 0.3% solution (Floxin Otic)
- Ciprofloxacin 0.3% and hydrocortisone suspension (Cipro HC Otic)
- Ofloxacin 0.3% (Ocuflox)
- Ciprofloxacin 0.3% (Ciloxan)
- Advantages
- Highly effective without causing local irritation or sensitization; no risk of ototoxicity; twice-daily dosing
- Disadvantages
- Expensive; increased community exposure of an important class of antibiotics, with potential for causing resistance
Patient Messaging: Protect ears during scuba diving
Before a dive:
- Option: Put 2-3 drops of olive oil in your ear
- Don't dive with any congestion
During a dive:
- Don't block your ears with earplugs or cotton
- Equalize early and regularly
- Descend feet first
After a dive:
- Clean your ears with fresh water after every dive
- Dry your ears with a towel after swimming, showering or diving. Tilting your head and pulling your earlobe in different directions while your ear is facing down might help eliminate water.
- A hair dryer could be used to carefully dry the ear after a shower. Be careful to ensure the air is not too hot, hold it at least a foot (about 30 centimeters) away from the ear.
- Refrain from putting objects (such as cotton swabs or ear wax removal tools) in the ear canal. This can cause ear wax (cerumen) impaction and can damage the skin in the ear, potentially increasing the risk of infection. Especially if there is any sand or salt in the canal.
Pulsatile Tinnitus
A steady rhythmic thumping, throbbing, creaking or whooshing sound in one or both ears.
Venous sinus stenosis/IIH is the most common cause of pulsatile tinnitus
Causes of pulsatile tinnitus include:
- Atherosclerosis, which refers to hardening of the arteries. When plaque builds up and hardens, it reduces the blood flow through the body, including the ears, neck and head. This may cause the rhythmic whooshing or thumping sound in one or both ears
- Blood vessel and artery disorders or malformations, especially near the ear. These include aneurysms and arteriovenous malformations
- Ear abnormalities
- Sinus wall abnormalities
- Head and neck tumors
- High blood pressure
- Idiopathic intracranial hypertension, which can cause headaches, blurred vision, and pulsatile tinnitus
- Anemia
- Head trauma
- Conductive hearing loss
- Hyperthyroidism
- Paget's Disease
Imaging may include
- temporal bone computerized tomography (CT) scan without contrast
- CT angiography of head and neck
- magnetic resonance angiography (MRA)
- magnetic resonance imaging (MRI)
- ultrasound
Labs:
- Rule out anemia and hyperthyroidism
If no underlying cause is found -> coping tools used for tinnitus self-management are recommended:
- sound therapy
- lifestyle adjustments to reduce stress
- cognitive behavioral therapy
References:
- Am Fam Physician. 2021;103(11):663-671
Rhinitis
Allergic:
- 15-30% of people in US
- Coexists with asthma atopic dermatitis
- Intranasal glucocorticoids are most effective; Alternatives include oral and nasal antihistamines and leukotriene-receptor antagonists
- Those with refractory symptoms can consider allegen immunotherapy
Treatment:
- Episodic symptoms:
- Oral or nasal H1-antihistamine
- +/- decongestant
- Mild symptoms (seasonal):
- Intranasal glucocorticoid
- Oral or nasal H1-antihistamine
- Leukotriene-receptor antagonist
- Moderate-severe symptoms:
- Intranasal glucocorticoid
- Intranasal glucocorticoid and Oral or nasal H1-antihistamine
- Allergen immunotherapy
For congestion that should work quickly:
- Sudafed 30-60 mg every 4 hours
- Astepro (azelastine) nasal spray
References:
- NEJM 372;5 Jan 2015
Sinusitis
Acute Bacterial Sinusitis
See also:
Diagnosis:
- Persistent symptoms
- Nasal congestion, rhinorrhea, or cough for 10d or more without improvement
- Severe symptoms
- Temp over 38.5 for 3-4d
- Purulent rhinorrhea for 3-4d
- Worsening symptoms
- Return of symptoms after initial resolution
- New or recurrent fever, increase in rhinorrhea or cough
Treatment:
- Amoxicillin-clavulanate is first line in children
Reference:
- NEJM 367;12 Sep 2012
Chronic Sinusitis
Diagnosis:
- 2 of the following for over 3mo: *must have one of these 2
- *Nasal obstruction
- *Nasal discharge (ant/post)
- Facial pressure/pain
- Smell reduced
Symptom criteria supported with one of the following:
- Nasal polyps on ant rhinoscopy or nasal endoscopy
- Edema or purulence
- CT scan demonstrating paranasal sinus inflammation
Treatment:
- 1st line: High-volume saline irrigation with topical corticosteroids
- If nasal polyps: Can consider short course of systemic corticosteroids (1-3wks), doxycycline (3 wks), or a leukotriene antagonist
- If no nasal polyps: Can consider prolonged course of a macrolide (3 mon)
Reference:
- JAMA Sep 2015, Vol 314, No 9
Sore throat
Likely beneficial:
- Corticosteroids (in those receiving antibiotics)
- Acetaminophen - reduces pain at regular doses over 2 days
Trade-off between benefits/harm:
- Antibiotics
- NSAIDs - reduces pain at 2-5 days
Characteristics
- Untreated symptoms of sore throat disappear by 3 days in 40% and untreated fevers in about 85%
- 85% of persons are symptom free at 1 week
References:
- AFP Vol 91 No 10 May 2015
Over the counter patient instructions:
- Acetaminophen will help the most but takes 24hrs to notice. You could use 2 tabs every 6 hours safely.
- Throat lozenges with "benzocaine" in them will help numb the area
- Honey has evidence to work with sore throats - there are lozenges with honey in them as a different option
- Cepacol spray (has benzocaine and glycerol) numbs the throat and can be used to help with sore throat.
Spots on Tongue edit
| Condition | What it looks like |
|---|---|
| Canker sores | Yellow or white spots with red borders. |
| Cold sores | Blisters or fluid-filled bumps, sometimes in clusters. |
| Geographic tongue | Discolored, map-like spots that may have a light-colored border. |
| Transient lingual papillitis (Lie bumps) | Small red or white bumps. |
| Oral thrush | Raised, white areas that resemble cottage cheese. |
| Lichen planus | White, lacy patches with possible redness and swelling. |
| Leukoplakia | White patches that won't scrape off. |
| Erythroplakia | Red patched that won't scrape off. |
| Tongue cancer | Red or white patches, ulcers or open sores. |
Healthy tongue:
- Filiform: These are at the front and in the center of your tongue. Filiform papillae appear threadlike, and they don't contain taste buds. You have more of this type of papillae than any other.
- Fungiform: Most people have between 200 and 400 fungiform papillae. They're all over your tongue, but they're most prominent at the edges and tip of your tongue. Each fungiform papilla contains about three to five taste buds.
- Foliate: These papillae are on each side of the back of your tongue. Unlike other papillae on your tongue, foliate papillae look like rough folds of tissue. You have approximately 20 foliate papillae, and each one contains several hundred taste buds.
- Circumvallate: These are the largest type of papillae on your tongue. Found on the very back of your tongue, circumvallate papillae contain about 250 taste buds.
Temporomandibular joint dysfunction syndrome (TMJ) Pain edit
Medications:
- NSAIDs
- TCAs
- If tenderness of the muscles of mastication - muscle relaxants:
- Cyclobenzaprine 5 to 10 mg orally once daily at bedtime
- Metaxalone 400 to 800 mg orally every eight hours
Therapy:
- Isometric jaw exercises are particularly useful for patients with temporomandibular joint dysfunction syndrome. These exercises are performed by applying resistance with an open or loosely fisted hand.
- Isometric jaw opening exercise:
- Begin with mouth open about an inch. The resistance and muscle contraction are held for 5 to 10 seconds before relaxing.
- Repeat 5 times per session.
- Exercises can be performed with moderate resistance applied several sessions per day, or with maximum resistance one session per day.
- Isometric jaw forward thrust exercise:
- Push the jaw forward against the hand, holding and then relaxing. This is repeated 5 times per session.
Adjunctive therapy:
- Dental mouth guard
Reference:
- Up to Date
Patient Messaging: TMJ Therapy
For your TMJ pain:
We can use these medications:
- NSAIDs like ibuprofen 400 mg every 4 hours
Physical Therapy:
- Isometric jaw exercises are particularly useful for patients with temporomandibular joint dysfunction syndrome. These exercises are performed by applying resistance with an open or loosely fisted hand.
- Isometric jaw opening exercise:
- Begin with mouth open about an inch. The resistance and muscle contraction are held for 5 to 10 seconds before relaxing.
- Repeat 5 times per session.
- Exercises can be performed with moderate resistance applied several sessions per day, or with maximum resistance one session per day.
- Isometric jaw forward thrust exercise:
- Push the jaw forward against the hand, holding and then relaxing. This is repeated 5 times per session.
Adjunctive therapy:
- Dental mouth guard
Tinnitis
Causes of Secondary Tinnitus
- Infectious
- Bacterial (Lyme disease, syphilis), fungal, viral
- Metabolic
- Diabetes mellitus, hyperlipidemia, vitamin B12 deficiency
- Neurologic
- Idiopathic intracranial hypertension, idiopathic stapedial or tensor tympani muscle spasm, multiple sclerosis, palatal myoclonus, spontaneous intracranial hypotension, type I Chiari malformation, vestibular migraine
- Otologic
- Cerumen impaction, cholesteatoma, foreign body, Meniere disease, middle ear effusion, otitis, otosclerosis, patulous eustachian tube, tympanic membrane perforation, vestibular schwannoma
- Somatic
- Head or neck injury, temporomandibular joint dysfunction
- Toxicologic
- Medication or substance use
- Traumatic
- Cerumen removal
- Vascular
- Arterial bruit; arteriovenous malformation; carotid atherosclerosis, dissection, or tortuosity; Paget disease; vascular tumors; venous hum
Medications Associated with Tinnitus
- Anesthetics
- Bupivacaine (Marcaine), lidocaine
- Antiepileptics
- Carbamazepine (Tegretol), pregabalin (Lyrica)
- Anti-inflammatory agents
- Aspirin,* nonsteroidal anti-inflammatory drugs, sulfasalazine (Azulfidine)
- Antimalarial agents
- Chloroquine (Aralen), quinine
- Antimicrobial agents
- Aminoglycosides
- Amikacin, gentamicin, kanamycin, neomycin, tobramycin (Tobrex)
- Macrolides
- Azithromycin (Zithromax), erythromycin
- Tetracyclines
- Doxycycline, minocycline (Minocin)
- Vancomycin
- Aminoglycosides
- Antineoplastic agents
- Platinum compounds
- Carboplatin (Paraplatin), cisplatin
- Protein kinase inhibitors
- Axitinib (Inlyta), dasatinib (Sprycel), imatinib (Gleevec), lapatinib (Tykerb), osimertinib (Tagrisso), ruxolitinib (Jakafi)
- Pyrimidine analogues
- Capecitabine (Xeloda)
- Taxanes
- Paclitaxel (Taxol)
- Platinum compounds
- Antivirals for treatment of hepatitis C virus infections
- Ribavirin (Rebetol), sofosbuvir (Sovaldi), telaprevir (Incivek)
- Immunosuppressants
- Calcineurin inhibitors
- Cyclosporine (Sandimmune)
- Interferons
- Monoclonal antibodies
- Ipilimumab (Yervoy), nivolumab (Opdivo), trastuzumab (Herceptin)
- Calcineurin inhibitors
- Loop diuretics
- Furosemide (Lasix), torsemide (Demadex)
- Paralytics (for anesthesia)
- Quaternary ammonium compounds
- Vecuronium
- Quaternary ammonium compounds
- Phosphodiesterase type 5 inhibitors
- Sildenafil (Viagra), tadalafil (Cialis)
- Vaccinations
- HPV
- Bivalent (HPV-16, HPV-18); quadrivalent (HPV-6, HPV-11, HPV-16, HPV-18)
- Pneumococcal polysaccharide (Pneumovax)
- HPV
- Miscellaneous
- Atorvastatin (Lipitor), bupropion (Wellbutrin), risedronate (Actonel), varenicline (Chantix)
- Antiarrhythmics, dopamine agonists, hormone agents, proton pump inhibitors
Tinnitus Presentation:
- Pulsitile tinnitus:
- Temporal bone CT without contrast or CT Angio of head and neck
- Focal neurologic abnormaliteis
- Refer to ER
- Asymmetric or unilateral tinnitus
- MRI of head and auditory canal with and without contrast
- Asymmetric hearing loss
- MRI of head and auditory canal with and without contrast
- Associated with hearing changes
- Prmpt audologic evaluation (within 4 weeks)
- Not Bothersome tinnitus
- History: focus on noise exposure, ototoxic meds, and medical conditions
- Anticipatory guidance and prevention
- Consider audiologic evaluation
- Acute Bothersome tinnitus
- History: Focus on recent exposure to loud noise, trauma, ototoxic meds, and infectious symptoms
- PE: Signs of trauma, canal blockage, cranial nerve abnormalities
- Consider audiologic evaluation
- If signs of trauma - Perform imaging
- If CN abnormalities - refer to ER for urgent imaging and neurological care
- Chronic Bothersome tinnitus (>6mo)
- Perform H&P
- Prompt audiologic evaluation (within 4 wks)
Treatments to consider for tinnitus
- Cognitive behavior therapy (moderate- to high-quality evidence)
- Sound therapy (low-quality evidence)
- Acoustic stimulation
- Hearing aids
- Sound/noise generation
- Tinnitus retraining therapy (very low-quality evidence)
Treatments to consider for tinnitus-associated conditions:
- Antidepressants
- Nortriptyline (Pamelor; depression)
- Sertraline (Zoloft; anxiety)
- Trazodone (sleep disturbance)
- Tricyclic antidepressants (disability)
- Cognitive training (attention, concentration, memory)
- Melatonin (sleep disturbance)
Treatments to avoid
- Benzodiazepines
- Clonazepam (Klonopin)
- Anticonvulsants
- Acamprosate (Campral)
- Carbamazepine (Tegretol)
- Gabapentin (Neurontin)
- Lamotrigine (Lamictal)
- Repetitive transcranial magnetic stimulation
- Electrical stimulation
- Transcranial direct current stimulation
- Transcutaneous electrical nerve stimulation
- Bimodal stimulation
- Microvascular decompression (surgical procedure)
- Ginkgo biloba
- Nitrous oxide
- Hyperbaric oxygen
- Acupuncture
Reference:
- AFP Jun 2021 Vol 103 No 11
Gastroenterology
Albumin/Globulin
- Albumin proteins
- Reflects nutritional status
- Makes up 50 percent of serum protein
- Made in the liver
- Globulin proteins
- Indicate the state of the immune function and the severity of any inflammation
- Made by your immune system
- Make up around 48 percent of serum protein
Low albumin levels may be a sign of:
- Liver disease, including cirrhosis
- Kidney disease
- Malnutrition
- Thyroid disease
- Severe burns
- if you are pregnant, a low albumin level is normal.
High albumin levels may be a sign of:
- Severe dehydration
- Diarrhea
Low globulin levels may be a sign of:
- Liver disease
- Kidney disease
High globulin levels may be a sign of:
- Certain types of blood cancers, such as multiple myeloma, Hodgkin disease, or leukemia
- Hemolytic anemia
- An autoimmune disease, such as lupus or rheumatoid arthritis
- Tuberculosis
A/G Ratio - can be interpreted only in light of the total protein concentration
- Very generally speaking, the normal ratio approximates 1:1
- For example, high total protein with a normal A:G ratio suggests dehydration, while the same protein with a low A:G ratio would indicate hyperglobulinemia.
- Low A/G Ratio - albumin levels are too low (hypoalbuminemia), or globulin levels are too high
- kidney disease (nephrotic syndrome)
- liver disease, and indicator of overall liver functionTrusted Source
- chronic infections (including HIV, tuberculosis, and hepatitis)
- malnutrition
- pancreatitis
- autoimmune diseasesTrusted Source (such as rheumatoid arthritis)
- certain cancers, including:
- liver cancer
- multiple myeloma and other blood (hematologic) cancers
- colorectal cancer
- pancreatic cancer
- lung cancer
- type 2 diabetes (low albumin can indicateTrusted Source insulin deficiency)
- Low albumin levels were partially predictive of increased mortality rates for those with gastrointestinal, lung, and breast cancers among others.
- High A/G Ratio:
- When caused by high albumin levels
- severe dehydration
- diarrhea
- also occurs during pregnancy
- When low levels of globulin
- Antibody deficiencies (a weakened immune system)
- Malnutrition
- Inflammatory bowel or other gastrointestinal diseases
- Eating disorders
- Not eating a balanced diet
- When caused by high albumin levels
Notes:
- Individuals with a well-maintained A/G ratio might have a better capacity for endurance and recovery
- A/G ratio tends to decrease with age
- Ways to improve the ratio:
- Nutrition: A balanced diet
- Physical Activity: Regular exercise has been linked to improved albumin synthesis and immune function
- Lifestyle Habits:
- Minimizing stress
- Getting sufficient sleep
- Staying hydrated
High albumin in urine (albuminuria) can be an indicator of kidney disease.
Antiemetics Selection
| Clinical Situation | Associated Neurotransmitters | Recommended Antiemetic |
|---|---|---|
| Vestibular nausea/Motion Sickness | Histamine, acetylcholine | Meclizine, scopolamine |
| Migraine-associated | Dopamine | Metoclopramide, prochlorperazine, promethazine |
| Gastroenteritis | Dopamine, serotonin | Promethazine, Serotonin antagonists |
| Pregnancy-induced | Unknown | Mild: Ginger 250mg ac/qhs; Pyridoxine |
| More Severe: Ondansetron |
References:
- AFP Vol 91, No 5 Mar 2015
- AFP Vol 76 No 1 Jul 2007
Barrett Esophagus
Risk factors (If chronic GERD 5+ yrs and 1+ risk factor -> Endoscopy):
- Male
- Age >50
- Smoking
- Obesity
- Diet high in fast food and meat
Nondysplastic Barrett Esophagus
- Risk of progression to adenocarcinoma: 0.2-0.5% annually
- Surveillance
- If BE length 3+ cm: Every 3 years
- If BE length 1-3 cm: Every 5 years
Low Grade Dysplasia (LGD)
- Risk of progression to adenocarcinoma: 0.5-0.7% annually
- Surveillance if no risk factors:
- Every 1 year
- If 1+ risk factors
- RF including:
- Multifocal LGD
- LGD confirmed on subsequent EGD
- BE length 3+ cm
- Family history of esophageal adenocarcinoma
- Endoscopic therapy:
- Endoscopic mucosal resection or submucosal dissection followed by endoscopic ablative therapy OR
- Endoscopic ablative therapy alone for patients without any lesions
- RF including:
High Grade Dysplasia/Early Esophageal Adenocarcinoma
- Risk of progression to adenocarcinoma (HGD): 5-7% annually
- Endoscopic therapy:
- Endoscopic mucosal resection or submucosal dissection followed by endoscopic ablative therapy OR
- Endoscopic ablative therapy alone for patients without any lesions
| Risk Factor | Points |
|---|---|
| Male sex | 9 |
| Length of Barrett esophagus | 1.0 per cm |
| Low-grade dysplasia baseline | 11 |
| Ever smoked cigarettes | 5 |
| Total |
| Risk group | Annual progression to high grade dysplasia or esophageal adenocarcinoma |
|---|---|
| Low, 0 to 10 points | 0.13% |
| Intermediate, 11 to 20 points | 0.73% |
| High, greater than 20 points | 2.10% |
References:
- JAMA Aug 2022 Vol 328 No 7
- AFP Mar 2025 Vol 111 No 3
Bowel cleansing
Prep ingredients:
- 64-ounces of the following electrolyte beverages Gatorade, Gatorade G2, Powerade, Powerade Zero, Pedialyte, Propel, or Liquid IV are acceptable with no red or purple colors.
- Miralax: One 8.3-ounce (238 grams, 14 dose) bottle. Generic brand is OK.
- Dulcolax® (bisacodyl): Four 5-mg laxative tablets.
- Consider purchasing soothing wipes and barrier cream, such as A+D Ointment® , to help with anal irritation. Do not use Desitin® .
Evening before Prep:
- Mix 2 quarts (64 ounces) Gatorade with entire 8.3-ounce bottle of Miralax and refrigerate.
Common Side Effects
- Chills, bloating, cramping, nausea and vomiting may occur. If so, take a break from drinking the prep for 30 minutes. Resume drinking, taking breaks as needed.
- A bowel movement will usually occur within an hour after the first glass of the Gatorade-Miralax mixture. Don't worry if this doesn't happen for three or four hours. Everyone is different.
- Bowel movements will occur that are watery and frequent until the bowel is fully cleansed. The end result should be clear or pale yellow liquid.
Instructions
- Day before Procedure:
- At 9 a.m., take four tablets of Bisacodyl/Dulcolax. You will want have access to a bathroom after taking the
- tablets.
- Mix the Miralax (entire bottle) with 64 ounces of the electrolyte beverage until it is all dissolved. You can put the mixture in the refrigerator.
- If you would prefer to drink the prep at room temperature, you may take it out of the fridge at 4 p.m.
- Do not add ice, sugar, or any other flavorings to the bowel preparation
- At 6 p.m., start drinking your prep mixture. You will drink half (32 ounces) of the prep mixture. Try to drink an eight-ounce glass of the prep mixture every 15 minutes. It will take you one hour to finish drinking it.
- Some people may feel nauseous, bloated, or vomit. If this happens, take a 15-30-minute break, and then try drinking the prep mixture.
- You will need to be near a bathroom once you start drinking your prep mixture. You will have diarrhea and will need to be able to reach a bathroom quickly.
- After you finish the prep mixture, you may drink clear liquids only.
- Store the remaining 32 ounces of the prep mixture in the refrigerator for the next morning. The day of your procedure
- Procedure Day
- Five hours before your check-in time start drinking the remaining 32 ounces of the prep mixture. Try to drink an eight-ounce glass of the prep mixture every 15-minutes until the bowel preparation is finished. It will take you one hour to finish drinking it.
- Notes:
- You will need to be near a bathroom once you start drinking your prep mixture. You will have diarrhea and will need to be able to reach a bathroom quickly.
- Some people may feel nauseous, bloated, or may vomit while drinking the bowel preparation. If this happens, take a 15-minute break, and then try drinking the prep mixture.
- Your stool should be no longer formed, but a clear or yellow liquid.
- You may drink clear liquids until two hours before your check-in time.
Bowel Medicines
However, before turning to laxatives, try these lifestyle changes to help with constipation:
- Eat fiber-rich foods: wheat bran, fresh fruits and vegetables, and oats
- Drink plenty of fluids daily
- Exercise regularly
| Type of laxative (brand examples) | How they work | Side effects |
|---|---|---|
| Oral osmotics (Phillips' Milk of Magnesia, Miralax) | Draw water into the colon to allow easier passage of stool | Bloating, cramping, diarrhea, nausea, gas, increased thirst |
| Oral bulk formers (Benefiber, Citrucel, FiberCon, Metamucil) | Absorb water to form soft, bulky stool, prompting normal contraction of intestinal muscles | Bloating, gas, cramping or increased constipation if not taken with enough water |
| Oral stool softeners (Colace, Surfak) | Add moisture to stool to allow strain-free bowel movements | Electrolyte imbalance with prolonged use |
| Oral stimulants (Dulcolax, Senokot) | Trigger rhythmic contractions of intestinal muscles to eliminate stool | Belching, cramping, diarrhea, nausea, urine discoloration with senna and cascara derivatives |
| Rectal suppositories (Dulcolax, Pedia-Lax) | Trigger rhythmic contractions of intestinal muscles and soften stool | Rectal irritation, diarrhea, cramping |
Celiac Sprue/Gluten Insensitivity edit
Testing:
- Serum tissue transglutaminase (tTG)-immunoglobulin A (IgA)
- Follow up a positive with endoscopy/biopsy
- Can be negative if gluten free diet
- More specific/More $$$: endomysial (EMA)-IgA antibody tests
Reference:
- Uptodate
Gluten Free Diet Fundamentals
Grains that should be avoided
- Barley (includes malt)
- Rye
- Wheat
Safe grains
- Amaranth
- Buckwheat
- Corn
- Millet
- Oats
- Quinoa
- Rice
- Sorghum
- Teff
Sources of gluten-free starches to be used as flour alternatives
- Cereal grains (amaranth, buckwheat, corn, millet, quinoa, sorghum, teff, rice, montina)
- Legumes (chickpeas, kidney beans, lentils, navy beans, pea beans, peanuts, soybeans)
- Nuts (almonds, cashews, chestnuts, hazelnuts, walnuts)
- Seeds (flax, pumpkin, sunflower)
- Tubers (arrowroot, jicama, potato, tapioca, taro)
References:
- AFP Vol 89 No 2 Jan 2014
Liver Cirrhosis
General recommendations for patients with liver cirrhosis focus on treating the underlying cause, preventing decompensation through surveillance and prophylaxis, managing complications, and optimizing nutrition and lifestyle.
Patient Messaging: Liver Cirrhosis
Things you can do to protect your liver are:
- Abstain from alcohol
- Daily protein intake of 1.2–1.5 g/kg
- Supplement with a multivitamin and zinc
- We should make sure your immunizations against hepatitis A, hepatitis B, pneumococcal pneumonia, and influenza are up to date
- Acetaminophen (Tylenol) up to 2 g daily is safe, but NSAIDs (like ibuprofen) should be avoided due to risk of acute kidney injury
- Let me know if you experience any of these common symptoms: muscle cramps, poor sleep, itchiness, or erectile function
Diagnosis and Initial Assessment
After confirming cirrhosis (typically via elastography ≥15 kPa or liver biopsy), initial evaluation should determine the etiology through viral hepatitis serologies, ferritin, transferrin saturation, complete blood count, liver function tests, and abdominal ultrasonography.[3]
The most common causes in the US are alcohol use disorder (45%), nonalcoholic fatty liver disease (26%), and hepatitis C (41%).[1]
Staging as compensated versus decompensated cirrhosis is critical, as median survival after onset of major complications like ascites or hepatic encephalopathy is approximately 1 year.[1]
Notes:
- Modality of choice = US
- Endoscopy all patients with cirrhosis to check for varices (LOE C)
Additional References:
- FMX 2016
Treating the Underlying Cause
Reversing the cause of cirrhosis is associated with lower risk of decompensation and potential recompensation.[4] Direct-acting antivirals for hepatitis C can lead to regression of fibrosis in 43% of patients after 12 months.[1] Antiviral therapy for hepatitis B may reduce hepatocellular carcinoma risk.[2] Weight loss benefits patients with obesity and cirrhosis of any cause.[4] All patients should abstain from alcohol regardless of etiology, as alcohol worsens prognosis of any chronic liver disease.[1]
Lifestyle Modifications and Nutrition
Daily energy intake should be 35 kcal/kg with protein intake of 1.2–1.5 g/kg, along with vitamin and zinc supplementation as needed.[4] Small, frequent high-calorie meals with a bedtime snack help achieve these goals.[4] Aerobic and resistance exercises emphasizing balance and flexibility should be encouraged.[4] Patients should abstain from alcohol and receive smoking cessation counseling.[4]
Immunizations and Medication Safety
All patients require immunization against hepatitis A, hepatitis B, pneumococcal pneumonia, and influenza.[4] Acetaminophen up to 2 g daily is safe, but NSAIDs should be avoided, especially in decompensated cirrhosis, due to risk of acute kidney injury.[4] ACE inhibitors and angiotensin receptor blockers can cause hypotension and kidney failure in patients with ascites.[4] Statins are safe in compensated cirrhosis but require caution at low doses due to rhabdomyolysis risk.[4]
Surveillance
Hepatocellular carcinoma surveillance with abdominal ultrasound every 6 months is recommended for all patients with cirrhosis.[3][2] Endoscopic screening for esophageal varices is indicated, though it can be avoided in patients with Child-Pugh A cirrhosis, liver stiffness [4] Patients with large varices should receive nonselective β-blockers (nadolol, propranolol, or carvedilol) or endoscopic variceal band ligation.[4] In patients with clinically significant portal hypertension, nonselective β-blockers reduce decompensation risk from 27% to 17% over 37 months, primarily by decreasing ascites.[4]
Management of Complications
For ascites, combination aldosterone antagonist and loop diuretics are more effective than sequential initiation (76% vs 56% resolution) with lower hyperkalemia rates (4% vs 18%).[1] Treatment includes salt restriction and diagnostic paracentesis to assess for spontaneous bacterial peritonitis.[4]
For hepatic encephalopathy, lactulose reduces mortality (8.5% vs 14% with placebo) and recurrent episodes (25.5% vs 46.8%).[1] Patients should receive sufficient lactulose to achieve 2-3 soft bowel movements daily.[1] Rifaximin 550 mg twice daily serves as secondary prophylaxis.[1]
For hepatorenal syndrome, terlipressin with albumin improves reversal rates from 18% to 39%.[1]
Symptom Management
Common symptoms are treatable: taurine 1000 mg twice daily reduces muscle cramps, hydroxyzine 25 mg nightly improves sleep quality by 40%, cholestyramine or naltrexone addresses pruritus, and tadalafil 10 mg improves erectile function in men (63% vs 30% with placebo).[1]
Care Coordination and Transplant Evaluation
Patients with decompensation or hepatocellular carcinoma should be evaluated for liver transplantation.[1] Multidisciplinary care coordination, patient and caregiver education, regular follow-up, and quality of life assessments are essential components of comprehensive management.[4]
Would you like me to summarize the latest evidence and guidelines on hepatocellular carcinoma surveillance intervals and modalities in cirrhosis, including any updates on the role of biomarkers or advanced imaging?
References
Reference:
- Diagnosis and Management of Cirrhosis and Its Complications: A Review. Tapper EB, Parikh ND. JAMA. 2023;329(18):1589-1602. https://doi.org/10.1001/jama.2023.5997.
- Treatment of Patients with Cirrhosis. Ge PS, Runyon BA. The New England Journal of Medicine. 2016;375(8):767-77. https://doi.org/10.1056/NEJMra1504367.
- Cirrhosis: Diagnosis and Management. Smith A, Baumgartner K, Bositis C. American Family Physician. 2019;100(12):759-770.
- Liver Cirrhosis. Ginès P, Krag A, Abraldes JG, et al. Lancet (London, England). 2021;398(10308):1359-1376. https://doi.org/10.1016/S0140-6736(21)01374-X.
Ascites treatment
- Dietary Na restriction (<2g/d)
- Avoid NSAIDs
- Goal is weight loss of 0.5Kg/d
- Diuretics:
- Spironolactone
- Start at 100 mg/d
- Increase to 200 mg
- Takes 3-7 days to full effect
- Watch for hyponatremia, hypokalemia, alkalosis, and gynecomastia
- Loop
- Spironolactone
Reference:
- FMX 2016
Acute variceal hemorrhage
- Each episode has 30% mortality rate
- Survivors have 50-70% recurrence rate in 1yr
Reference:
- FMX 2016
Colonoscopy
Key Points
- Adenomas on initial colonoscopy affect ongoing follow-up screening recommendations.
- A single normal colonoscopy demonstrates a lifetime CRC mortality risk 68% lower than in the general population.
- Finding more than 10 adenomas confers the highest risk, and repeat colonoscopy is recommended in one year.
- Finding polyps larger than 10 mm, between five and 10 sessile serrated polyps or adenomas, polyps with dysplasia, or traditional serrated adenomas confers high risk, and repeat colonoscopy is recommended in three years.
Common findings on colonoscopy reports include adenomas and polyps. Instead of defining high- and low-risk findings, task force recommendations depend on the number and size of findings.
| Initial colonoscopy finding | Follow-up interval, years | Follow-up colonoscopy finding | Follow-up interval, years |
|---|---|---|---|
| Normal (no polyps) | 10 | — | — |
| Traditional adenomas | |||
| Tubular adenomas < 10 mm | |||
| 1 to 2 | 7 to 10 | Normal | 10 |
| Tubular adenomas < 10 mm | |||
| 1 to 2 | 7 to 10 | ||
| 3 to 4 | 3 to 5 | ||
| 5 to 10 | 3 | ||
| High-risk adenoma | 3 | ||
| 3 to 4 | 3 to 5 | Normal | 10 |
| Tubular adenomas < 10 mm | |||
| 1 to 2 | 7 to 10 | ||
| 3 to 4 | 3 to 5 | ||
| 5 to 10 | 3 | ||
| High-risk adenoma | 3 | ||
| 5 to 10 | 3 | No evidence available | — |
| High-risk adenoma ? 10 mm or villous or tubulovillous histology, or high-grade dysplasia | 3 | Normal | 5 |
| Tubular adenomas < 10 mm | |||
| 1 to 2 | 5 | ||
| 3 to 4 | 3 to 5 | ||
| 5 to 10 | 3 | ||
| High-risk adenoma | 3 | ||
| > 10 | 1 | No evidence available | — |
| Serrated polyps | |||
| Sessile serrated polyps < 10 mm | |||
| 1 to 2 | 5 to 10 | No evidence available | — |
| 3 to 4 | 3 to 5 | No evidence available | — |
| 5 to 10 | 3 | No evidence available | — |
| High-risk sessile serrated polyp ? 10 mm or dysplasia | 3 | No evidence available | — |
| Hyperplastic polyps | |||
| Up to 20 polyps < 10 mm | 10 | No evidence available | — |
| Any polyps ? 10 mm | 3 to 5 | No evidence available | — |
| Traditional serrated adenoma | 3 | No evidence available | — |
References:
- AFP Col 103 No 5 Mar 2021
Colorectal Cancer Screening
Screen all adults ages 45-75yo
Strong evidence exists that screening for CRC reduces incidence and mortality.
The U.S. Preventive Services Task Force recommends that adults at average risk (those who do not have a personal or family history of CRC or polyps, do not have inflammatory bowel disease, or a history of genetic syndromes associated with CRC) aged 45–75 years be screened for CRC by any of six available tests:
- Fecal occult blood test (FOBT)
- Fecal immunochemical test (FIT)
- Multitarget stool DNA (FIT-DNA)
- Computed tomographic colonography (CTC)
- Sigmoidoscopy
- Colonoscopy
| Test | Interval | Example | Sensitivity | Specificity |
|---|---|---|---|---|
| High-sensitivity guaiac fecal occult blood test (HSgFOBT) | Annually | 50-75% | 96-99% | |
| Fecal Globin Immunochemical test (FIT) | Annually | Quest 11290 | 74-81% | 95-96% |
| Stool DNA-FIT | 1-3 yrs | Cologuard | 93% | 89% |
| Computer tomography colonography | 5 yrs | 67-94% | 86-98% | |
| Flexible sigmoidoscopy | 5 yrs | 95% | 87% | |
| Flexible sigmoidoscopy + Annual FIT | 10 yrs | 95% | 87% | |
| Colonoscopy | 10 yrs | 95% | 86-89% |
The best test is the one that a person is willing to get. CRCCP grantees use only screening tests recommended by the United States Preventive Services Task Force (USPSTF). Those options include:
- At-home stool tests
- High-sensitivity guaiac fecal occult blood test (FOBT) every year.
- High-sensitivity fecal immunochemical test (FIT) every year.
- Tests performed in clinics
- Colonoscopy every 10 years.
- Sigmoidoscopy every 5 years, with FOBT or FIT every 3 years.
References:
- https://www.cdc.gov/cancer/crccp/about.htm
- https://www.cdc.gov/cancer/crccp/pdf/CRCCP_factsheet_SavingLives.pdf
- AFP Sep 2025 Vol 112 No 3
- AFP Vol 112 No 2 Aug 2025
Modifiable Risk Factors for Colorectal Cancer
Modifiable Risk Factors for Colorectal Cancer
- Consumption of alcohol
- Consumption of high to moderate amounts of red meat and any amount of processed meat
- Diabetes
- Lack of regular moderate to vigorous physical activity
- Nonadherence to recommended screening
- Overweight and obesity
- Tobacco use
Reference:
- AFP Sep 2025 Vol 112 No 3
USPSTF Colon Cancer Screening
Recommendation Summary
| Population | Recommendation | Grade |
|---|---|---|
| Adults ages 50 to 75 years | The USPSTF recommends screening for colorectal cancer in all adults ages 50 to 75 years. | A |
| Adults ages 45 to 49 years | The USPSTF recommends screening for colorectal cancer in adults ages 45 to 49 years. | B |
| Adults ages 76 to 85 years | The USPSTF recommends that clinicians selectively offer screening for colorectal cancer in adults ages 76 to 85 years. Evidence indicates that the net benefit of screening all persons in this age group is small. In determining whether this service is appropriate in individual cases, patients and clinicians should consider the patient's overall health and prior screening history. | C |
| Screening Method | Frequency | Evidence of Efficacy | Other Considerations |
|---|---|---|---|
| gFOBT | Every year | RCTs with mortality end points: High-sensitivity versions (eg, Hemoccult SENSA) have superior test performance characteristics than older tests (eg, Hemoccult II) | Does not require bowel preparation, anesthesia, or transportation to and from the screening examination (test is performed at home) |
| FIT | Every year | Test characteristic studies: Improved accuracy compared with gFOBT; Can be done with a single specimen | Does not require bowel preparation, anesthesia, or transportation to and from the screening examination (test is performed at home) |
| FIT-DNA | Every 1 or 3 y | Test characteristic studies: Specificity is lower than for FIT, resulting in more false-positive results, more diagnostic colonoscopies, and more associated adverse events per screening test; Improved sensitivity compared with FIT per single screening test | There is insufficient evidence about appropriate longitudinal follow-up of abnormal findings after a negative diagnostic colonoscopy; may potentially lead to overly intensive surveillance due to provider and patient concerns over the genetic component of the test |
| Screening Method | Frequency | Evidence of Efficacy | Other Considerations |
|---|---|---|---|
| Colonoscopy | Every 10 y | Prospective cohort study with mortality end point | Requires less frequent screening. Screening and diagnostic followup of positive results can be performed during the same examination. |
| CT colonography | Every 5 y | Test characteristic studies | There is insufficient evidence about the potential harms of associated extracolonic findings, which are common |
| Flexible sigmoidoscopy | Every 5 y | RCTs with mortality end points: Modeling suggests it provides less benefit than when combined with FIT or compared with other strategies | Test availability has declined in the United States |
| Flexible sigmoidoscopy with FIT | Flexible sigmoidoscopy every 10 y plus FIT every year | RCT with mortality end point (subgroup analysis) | Test availability has declined in the United States; Potentially attractive option for patients who want endoscopic screening but want to limit exposure to colonoscopy |
Reference:
Colonoscopy Surveillance
| Baseline colonoscopy: Most Advanced Finding(s) | Recommended surveillance interval (y) |
|---|---|
| No polyps | 10 |
| Small (<10 mm) hyperplastic polyps in rectum or sigmoid | 10 |
| 1-2 Small (<10 mm) tubular adenomas | 5-10 |
| 3-10 Tubular adenomas | 3 |
| >10 Adenomas | <3 |
| Any adenoma ≥10 mm | 3 |
| Any adenoma with villous elements (villous or tubulovillous) or with high-grade dysplasia | 3 |
| Baseline colonoscopy: Most Advanced Finding(s) | Recommended surveillance interval (y) |
|---|---|
| Sessile serrated adenoma/polyp(s) <10 mm with no dysplasia | 5 |
| Sessile serrated adenoma/polyp(s) ≥10 mm | 3 |
| Sessile serrated adenoma/polyp with dysplasia | 3 |
| Traditional serrated adenoma | 3 |
| Serrated polyposis syndrome (see text) | 1 |
References:
- Lieberman D.A., Rex D.K., Winawer S.J., Giardiello F.M., Johnson D.A., Levin T.R. United States Multi-Society Task Force on Colorectal Cancer
Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012; 143: 844-857
Followup colonoscopy recommendations
- Repeat colonoscopcy is recommended 7-10 yrs after complete removal of 1 to 2 tubular adenomas smaller than 10 mm (Strong rec; Mod QOE)
- Repeat colonoscopcy is recommended 3-5 yrs after complete removal of 3 to 4 tubular adenomas smaller than 10 mm (Weak rec; Very low QOE)
- Repeat colonoscopcy is recommended 3 yrs after complete removal of 5 to 10 adenomas smaller than 10 mm (Strong rec; Mod QOE)
- Repeat colonoscopcy is recommended 3 yrs after complete removal of 1 or more adenomas 10 mm or larger (Stron rec; High QOE)
- Repeat colonoscopcy is recommended 6 months after piecemeal resection of an adenoma or sessile serrated polyp 20 mm or larger (Strong rec; Mod QOE)
References:
- JAMA Dec 2020 Vol 324, No 21
Constipation
Also see:
Treatment for chronic idiopathic constipation:
- Increase dietary fiber and/or bulking agent
- PEG 3350 (osmotic laxative) or stimulant (bisacodyl or senna)
- Secretory agent (linaclotide or lubiprostone)
- Refer
Agents:
- Bulk Agents
- Psyllium (10g daily), methylcelluose, calcium polycarbophil, wheat dextrin
- Recommendation: Strong
- Quality of evidence: Low
- Polycarbophil
- 1.25g 1-4x/d max 5g/d
- Soluble fiber
- Methylcellulose powder
- 2g/d
- Insoluble fiber
- Psyllium (10g daily), methylcelluose, calcium polycarbophil, wheat dextrin
- Nonabsorbed substances
- PEG 3350 (17 g daily) (osmotic)
- Recommendation: Strong
- Quality of evidence: High
- Lactulose (20 g daily) (osmotic)
- 15 - 30 ml/d
- Recommendation: Strong
- Quality of evidence: Low
- PEG 3350 (17 g daily) (osmotic)
- Stimulants
- Senna (17 mg qhs)
- Bisacodyl (10mg daily)
- Recommendation: Strong
- Quality of evidence: Moderate
- Secretory
- Lubiprostone, Linaclotide
- Recommendation: Strong
- Quality of evidence: High
- PAMORAs (Peripheral mu-opioid antagonists)
- Naldemedine
- Naloxegol
- Methylnaltrexone
Other notes:
- PEG 3350 (17 g daily) (Miralax) is preferred over lactulose as more effective and fewer adverse effects (LOE A)
- Pelvic florr therapy with biofeedback is superior to laxatives, sham, and placebo in RCTS for defecatory dysfunction (LOE B)
References:
- JAMA Vol 315 No 2 Jan 2016
- JAMA Vol 322 No 22 Dec 2019
Over the counter managment of constipation
Here are links to what I suggest to help with constipation/gastroparesis:
- Senna 9-17 mg/day: https://amzn.to/39xrZVz
- Psyllium 500-1000 mg/day: https://amzn.to/3HzUwpX
- You can also use Magnesium Oxide 400 to 800 mg daily
Also, continue to:
- Drink a lot of water
- Eat grapes and prunes
- Stay active and exercise as you are able
Here are what I suggest to help with constipation/gastroparesis:
- Senna 9-17 mg/day
- Psyllium 500-1000 mg/day
- Magnesium Oxide 400 to 800 mg daily
Also, continue to:
- Drink a lot of water
- Eat grapes and prunes
- Stay active and exercise as you are able
I will send in a prescription too for you.
Secondary Causes
Mechanical:
- Colorectal cancer
- Colon, rectal, or anal stricture
- Rectocele
- Intestinal pseudo-obstrution
- Megacolon
Neurologic Disease:
- Spinal cord lesion
- Stroke
- Parkinson disease
- Multiple sclerosis
Metabolic Disturbances:
- Hypercalcemia
- Hypokalemia
- Hypomagnesemia
- Hypothyroidism (severe)
- Uremia
Medications:
- Opiates
- Anticholinergics
- CCBs
- Anticonvulsants
- Antispasmodics
- Antihistamines
- Antiemetics
Miscellaneous:
- Amyloidosis
- Scleroderma
- Heavy metal poisoning
References:
- JAMA Vol 315 No 2 Jan 2016
Study: The effect of food, vitamin, or mineral supplements on chronic constipation in adults: A systematic review and meta-analysis of randomized controlled trials
Background:
- Over-the-counter supplements are commonly used to manage chronic constipation; however, their efficacy remains unclear. We aimed to investigate the effect of food, vitamin or mineral supplements on stool output, gut transit time, symptoms, and quality of life in adults with chronic constipation via a systematic review and meta-analysis of randomized controlled trials (RCTs).
Methods:
- Studies were identified using electronic databases, backward citation, and hand-searching abstracts. RCTs reporting administration of food supplements (e.g., fruit extract supplements), vitamin or mineral supplements in adults with chronic constipation were included. Studies administering whole foods (e.g., fruits) were excluded. Risk of bias (RoB) was assessed with Cochrane RoB 2.0. Relative risks (RR), mean differences (MD), or standardized mean differences (95% confidence intervals [CI]) were calculated using a random-effects model.
Key results:
- Eight RCTs (787 participants) were included, investigating:
- kiwifruit (n = 3 RCTs)
- senna (n = 2)
- magnesium oxide (n = 2)
- Ziziphus jujuba (n = 1)
- Malva Sylvestris (n = 1) supplements
- Kiwifruit supplements did not impact stool frequency (MD 0.24 bowel movements/week [-0.32, 0.80]; p = 0.40) or consistency (MD -0.11 Bristol points [-0.31, 0.09], p = 0.29).
- Overall, 61% responded to senna and 28% to control; however, this did not reach statistical significance (RR 2.78, [0.93, 8.27]; p = 0.07).
- Overall, 68% responded to magnesium oxide and 19% to control (RR 3.32 [1.59, 6.92]; p = 0.001).
- Magnesium oxide improved stool frequency (MD 3.72 bowel movements/week [1.41, 6.03]; p = 0.002) and consistency (MD 1.14 Bristol points [0.48, 1.79]; p = 0.0007).
Conclusions and inferences:
- Magnesium oxide supplements are effective at improving cardinal symptoms of chronic constipation.
- Senna and kiwifruit supplements did not impact symptoms; however, findings were based on a small number of studies. Further research is required to investigate the effect of food supplements (e.g., kiwifruit supplements), as well as their whole food equivalents (e.g., whole kiwifruits) in chronic constipation.
Reference:
- van der Schoot A, Creedon A, Whelan K, Dimidi E. The effect of food, vitamin, or mineral supplements on chronic constipation in adults: A systematic review and meta-analysis of randomized controlled trials [published online ahead of print, 2023 May 27]. Neurogastroenterol Motil. 2023;e14613. https://doi.org/10.1111/nmo.14613
- https://onlinelibrary.wiley.com/doi/10.1111/nmo.14613
Diarrhea
Definition: passage of 3+ unformed stools/day or passage of 250g of unformed stool/day
- Acute: (<14d)
- Persistent (14-29d)
- Chronic (>30d)
Labs:
- Electrolytes and Serum creatinine - in pts with systemic toxicity or dehydration (especially elderly or infirm patients)
- CBC - in pts with severe diarrhea and fever or toxicity (looking for left shift of neutrophils for C difficile or eosinophilia in parasitic infections)
- Stool samples - in pts where acute diarrhea is severe, associated with fever or severe coexisting condition in a hospitalized pt, persistent diarrhea, profuse cholera-like watery diarrhea, dehydration, and dysentery)
Differential:
- Shigellosis
- Dx with stool culture
- Treat with Cipro 750mg daily for 3d or azithro 500mg for 3d
- Salmonellosis
- Dx with stool culture
- Intestinal campylobacteriosis
- Dx with stool culture
- Treat with azithro 500mg for 3d
- Infection with Shiga toxin producing E coli
- Dx with stool culture on Sorbitol-MacConkey agar
- Treat with supportive care
- Noncholeraic vibrio diarrhea
- Dx with stool culture with TCBS medium
- Treat with Cipro 750mg daily for 3d or azithro 500mg for 3d
- Vibrio cholerae
- Dx with stool culture with TCBS medium
- Treat with doxycycline 300mg single dose
- Clostridium difficile
- Travelors diarrhea and enterotoxigenic E coli
- For pts with fever or dysentery: Treat with azithro 1000mg single dose
- For pts without fever or dysentery: Treat with rifaximin 200mg 3/d for 3d; or cipro 500mg bid or 750mg daily for 1-3d
- Norovirus
- Treat with fluid and electrolyte therapy
- Rotavirus
- Treat with fluid and electrolyte therapy
- Enteric adenoviruses
- Treat with fluid and electrolyte therapy
- Giardiasis
- Dx with enzyme immunoassay or light microscopic exam of stool
- Treat with tinidazole 2g single dose, metronidazole 250mg 3/d for 5-7d
- Celiac disease
- Dx: Immunoglobulin A antiendomysium and antitissue transglutaminase antibodies
- Drug-induced diarrhea
- Endocrine diarrhea
- Dx: TSH, serum peptide concentrations, urinary histamine level
- Inflammatory bowel disease
- Dx: CBC, fecal leukocytes, ESR, fecal calprotectin
- Irritable Bowel Syndrome
- Ischemic colitis
- Microscopic colitis
Ref:
- NEJM 370;16 Apr 2014
- AFP Vol 84 No 10 Nov 2011
Chronic Diarrhea
Defined as: A decrease in stool consistency for more than 4 weeks.
Consider 3 basic categories:
- Watery
- Secretory type - often nocturnal; unrelated to food intake; fecal osmotic gap < 50 mOsm per kg
- Alcoholism
- Bacterial enterotoxins (like cholera)
- Bile acid malabsorption
- Brainerd diarrhea (epidemic secretory diarrhea)
- Congenital syndromes
- Crohn disease (early ileocolitis)
- Endocrine disorders (like hyperthyroidism [increases motility])
- Medications
- Microscopic colitis (lymphocytic and collagenous subtypes) - often affects older persons
- Neuroendocrine tumors (like gastrinoma, vipoma, carcinoid tumors, mastocytosis)
- Nonosmotic laxatives (like senna, docusate sodium [Colace])
- Postsurgical (like cholecystectomy, gastrectomy, vagotomy, intestinal resection)
- Vasculitis
- Osmotic type - fecal osmotic gap > 125 mOsm per kg
- Carbohydrate malabsorption syndromes (like lactose, fructose)
- Celiac disease
- Osmotic laxatives and antacids (like magnesium, phosphate, sulfate)
- Sugar alcohols (like mannitol, sorbitol, xylitol)
- Functional type - distinguished from secretory types by hypermotility, smaller volumes, and improvement at night and with fasting
- Irritable bowel syndrome = most common cause of functional diarrhea.
- Secretory type - often nocturnal; unrelated to food intake; fecal osmotic gap < 50 mOsm per kg
- Fatty (malabsorption) - bloating and steatorrhea most of the time
- Characterized by:
- Excess gas
- Steatorrhea
- Weight loss
- Malabsorption syndrome - damage to or loss of absorptive ability
- Amyloidosis
- Carbohydrate malabsorption (like lactose intolerance)
- Celiac sprue (gluten enteropathy) - Can result in weight loss and iron deficiency anemia
- Gastric bypass
- Lymphatic damage (like congestive heart failure, some lymphomas)
- Medications (like orlistat [Xenical; inhibits fat absorption], acarbose [Precose; inhibits carbohydrate absorption])
- Mesenteric ischemia
- Noninvasive small bowel parasite (like Giardiasis)
- Postresection diarrhea
- Short bowel syndrome
- Small bowel bacterial overgrowth (> 105 bacteria per mL)
- Tropical sprue
- Whipple disease (Tropheryma whippelii infection)
- Maldigestion - loss of digestive function
- Hepatobiliary disorders
- Inadequate luminal bile acid
- Loss of regulated gastric emptying
- Pancreatic exocrine insufficiency
- Characterized by:
- Inflammatory - Inflammatory or exudative (elevated white blood cell count, occult or frank blood or pus)
- Inflammatory bowel disease Crohn disease (ileal or early Crohn disease may be secretory)
- Ulcerative colitis
- Ulcerative colitis or Crohn disease can be characterized by:
- Blood and pus in the stool
- Elevated fecal calprotectin level
- Ulcerative colitis or Crohn disease can be characterized by:
- Diverticulitis
- Ulcerative jejunoileitis
- Invasive infectious diseases
- Clostridium difficile (pseudomembranous) colitis–antibiotic history
- Invasive bacterial infections (like tuberculosis, yersiniosis)
- Invasive parasitic infections (like Entamoeba)–travel history
- Ulcerating viral infections (like cytomegalovirus, herpes simplex virus)
- Neoplasia
- Colon carcinoma
- Lymphoma
- Villous adenocarcinoma
- Radiation colitis
Fecal osmotic gap
- Fecal osmotic gap = 290 – 2 × (stool sodium + stool potassium)
- Differentiates secretory from osmotic diarrhea
- Normal fecal osmolality = 290 mOsm per kg (290 mmol per kg)
Laboratory Workup:
- Complete blood count
- Albumin level
- Erythrocyte sedimentation rate
- Liver function testing
- Thyroid-stimulating hormone level
- Electrolyte levels
- A minimal stool assessment should include:
- Fecal leukocyte level
- Fecal occult blood test
- If indicated:
- Fecal calprotectin for IBD
- Stool laxative screen
- Fecal pH test (if <5.5, could be lactose intolerance)
- Stool ova and parasite
References:
- Am Fam Physician. 2011 Nov 15;84(10):1119-1126.
- AFP Vol 101 No 8 Apr 2020
- Common Causes of Chronic Diarrhea
- Celiac disease
- Clinical findings
- Chronic malabsorptive diarrhea, fatigue, iron deficiency anemia, weight loss, dermatitis herpetiformis, family history
- Tests
- Immunoglobulin A antiendomysium and antitissue transglutaminase antibodies most accurate; duodenal biopsy is definitive
- Clinical findings
- Clostridium difficile infection
- Clinical findings
- Often florid inflammatory diarrhea with weight loss
- Recent history of antibiotic use, evidence of colitis, fever
- May not resolve with discontinuation of antibiotics
- Tests
- Fecal leukocyte level; enzyme immunoassay that detects toxins A and B; positive fecal toxin assay; sigmoidoscopy demonstrating pseudomembranes
- Clinical findings
- Drug-induced diarrhea
- Clinical findings
- Osmotic (e.g., magnesium, phosphates, sulfates, sorbitol)
- Hypermotility (stimulant laxatives)
- Malabsorption (e.g., acarbose [Precose], orlistat [Xenical])
- Tests
- Elimination of offending agent; always consider laxative abuse
- Clinical findings
- Endocrine diarrhea
- Clinical findings
- Secretory diarrhea or increased motility (hyperthyroidism)
- Tests
- Thyroid-stimulating hormone level, serum peptide concentrations, urinary histamine level
- Clinical findings
- Giardiasis
- Clinical findings
- Excess gas, steatorrhea (malabsorption)
- Tests
- Giardia fecal antigen test
- Clinical findings
- Infectious enteritis or colitis (diarrhea not associated with C. difficile): bacterial gastroenteritis, viral gastroenteritis, amebic dysentery
- Clinical findings
- Inflammatory diarrhea, nausea, vomiting, fever, abdominal pain
- History of travel, camping, infectious contacts, or day care attendance
- Tests
- Fecal leukocyte level, elevated erythrocyte sedimentation rate
- Cultures or stained fecal smears for specific organisms are more definitive
- Clinical findings
- Inflammatory bowel disease: Crohn disease, ulcerative colitis
- Clinical findings
- Bloody inflammatory diarrhea, abdominal pain, nausea, vomiting, loss of appetite, family history, eye findings (e.g., episcleritis), perianal fistulae, fever, tenesmus, rectal bleeding, weight loss
- Tests
- Complete blood count, fecal leukocyte level, erythrocyte sedimentation rate, fecal calprotectin level
- Characteristic intestinal ulcerations on colonoscopy
- Clinical findings
- Irritable Bowel Syndrome
- Clinical findings
- Stool mucus, crampy abdominal pain, altered bowel habits, watery functional diarrhea after meals, exacerbated by emotional stress or eating
- More common in women
- Tests
- All laboratory test results are normal
- Increased fiber intake, exercise, dietary modification should be recommended
- Clinical findings
- Ischemic colitis
- Clinical findings
- History of vascular disease; pain associated with eating
- Tests
- Colonoscopy, abdominal arteriography
- Clinical findings
- Microscopic colitis
- Clinical findings
- Watery, secretory diarrhea affecting older persons
- Nonsteroidal anti-inflammatory drug association possible
- No response to fasting; nocturnal symptoms
- Tests
- Colon biopsy
- Clinical findings
- Celiac disease
Diarrhea without Fever Algorythm
- Diarrhea without fever
- Consider empiric metronidazole
- Giardia antigen test
- If positive -> treat
- Stool for cryptosporidium, cyclospora: acid fast stain or antigen test
- If positive -> treat
- Stool culture and Clostridium difficile antigen
- If positive -> treat
- Often enterotoxigenic Escherichia coli
- Treat per sensitivities or rifaximin for E. coli only
- Stool for ova and parasites x3
- Ignore nonpathogenic organisms
- If positive -> treat
- Selective serology: Stongyloides, Schistosoma
- If positive -> treat
- Evaluate for underlying pathology: post-infectious irritable bowel disease, celiac sprue, idiopathic inflammatory colitis, HIV test, treat for bacterial overgrowth
References:
- FP Essentials 370
Travelors Diarrhea
- Flouroquinolone or macrolide for 1-3 days
- Loperamide
Reference:
- AFP Vol 106 No 6 Dec 2022
Dietary Fats
Most people need to consume about 20 to 35 percent of their daily calories from fat. For the average person, that means 44 to 78 grams of fat.
- 9 calories of fat per gram
- 4 calories per gram for protein and carbohydrates
PUFA
PUFAs are unsaturated fats found in
- nuts
- seeds
- vegetable oils, such as safflower, corn, sunflower, soy, and cottonseed
Best Sources of MUFA
You can find monounsaturated fats in these foods:
- Almonds
- Avocado
- Dark chocolate
- Hazelnuts
- Macadamia nuts
- Olives
- Peanuts
- Pecans
- Pistachios
- Pumpkin seeds
- Sesame seeds
- Squash
- Sunflower seeds
Reference:
Diverticulitis
Clinical Recommendations
- Avoiding popcorn, nuts, or seeds does not decrease the risk of diverticulitis or diverticular complications.SORT: B
- Tobacco cessation, reduced meat intake, physical activity, and weight loss are recommended interventions to decrease the risks of diverticulitis recurrence. SORT C
- Computed tomography of the abdomen and pelvis is the most appropriate initial imaging modality in the assessment of suspected complicated diverticulitis. SORT C
- Selected patients with uncomplicated diverticulitis can be treated without antibiotics. SORT A
- Imaging-guided percutaneous drainage is recommended for stable patients with abscesses ≥ 3 cm in size. SORT B
- Prophylactic partial colectomy should be considered in patients who had an abscess requiring drainage. SORT B
- Colonoscopy should be considered six to eight weeks after resolution of a complicated case of diverticulitis unless the patient has had a high-quality colonoscopy in the past year. SORT C
Outpatient Antibiotics:
- Oral antibiotics should be considered for uncomplicated diverticuliis only if symptoms persist or worsen after 48 to 72 hours
- Trimethoprim/sulfamethoxazole 160/800 mg bid + metronidazole 500 mg tid
- Amox/clavulanate 875/125 mg XR bid
- Ciprofloxacin 500 mg bid + metronidazole 500 mg tid
- Moxifloxacin 400 mg qd
- Levofloxacin 750 mg qd + metronidazole 500 mg 3-4/d
Reference:
- AFP Aug 2022 Vol 106 No 2
Clinical Prediction Rule for Acute Diverticulitis
The presence of all three of the following indicators is considered a positive result: - Absence of vomiting - C-reactive protein level > 5 mg per dL (50 mg per L) - Tenderness limited to the left lower quadrant
References:
- AFP Sep 2020 Vol 102 No 6
Dyspepsia
- Patients <60yo with dyspepsia should be tested for H. pylori infection and treated if positive (LOE: A)
- Patients <60yo with dyspepsia should be treated with PPI if H. pylori negative (LOE: A)
EGD Indications
- >60yo
- Bleeding, anemia, >10% weight loss, progressive dysphagia
- History of cancer
- History of PUD
- Abdominal mass on exam
References:
- FMX 2016
- JAMA Vol 319 No 17 May 2018
Functional Dyspepsia
Herbal Medicines for Functional Dyspepsia
- STW 5 (Iberogast), peppermint plus caraway oil, and turmeric (Curcuma longa) may be effective in improving symptoms of functional dyspepsia without significant adverse events.
- Peppermint plus caraway oil and turmeric may also improve quality of life in patients with functional dyspepsia. (SOR: B, meta-analysis of low-quality randomized controlled trials [RCTs].)
Rome IV Diagnostic Criteria for Functional Dyspepsia
- Presence of at least one of the following:
- Postprandial fullness (3 days per week)
- Early satiety (3 days per week)
- Epigastric pain (1 day per week)
- Epigastric burning (1 day per week)
- and
- No evidence of structural disease
Note: Criteria must be present for at least the past 3 months, with symptoms starting at least six months before diagnosis.
References:
- AFP Vol 101 No 2 Jan 2020
Medications Associated with Dyspepsia
Medications Associated with Dyspepsia
- Acarbose (Precose)
- Antibiotics
- Bisphosphonates
- Corticosteroids
- Herbs (e.g., chaste tree berry, feverfew, garlic, ginkgo, saw palmetto, white willow bark)
- Iron
- Metformin
- Miglitol (Glyset)
- Nonsteroidal anti-inflammatory drugs, including cyclooxygenase-2 inhibitors
- Opiates
- Orlistat (Xenical)
- Potassium chloride
- Theophylline
References:
- AFP Vol 101 No 2 Jan 2020
Elevated Liver Transaminase Levels
Causes of Elevated Liver Transaminase Levels
Hepatocellular damage releases ALT and AST. Elevations in ALT generally are more specific for liver injury, whereas elevations in AST can also be caused by extrahepatic disorders, such as thyroid disorders, celiac sprue, hemolysis, and muscle disorders.7 Normal ALT levels are defined as 29 to 33 IU per L (0.48 to 0.55 μkat per L) for males and 19 to 25 IU per L (0.32 to 0.42 μkat per L) for females.6 The AST:ALT ratio can suggest a specific disease or give insight into liver disease severity. In a study differentiating alcoholic liver disease from nonalcoholic liver disease, alcoholic liver disease was suggested with an AST:ALT ratio greater than 2 (mean AST:ALT values were 152:70; positive likelihood ratio [LR+] = 17, negative likelihood ratio [LR–] = 0.49). On the other hand, nonalcoholic fatty liver disease (NAFLD) was associated with a ratio of less than 1 (mean AST:ALT values were 66:91; LR+ = 80, LR– = 0.2).8 However, causes of mild, asymptomatic elevation of transaminase levels can generally be categorized as common, uncommon, and rare (Table 1).9
| Situation | Comments |
|---|---|
| Mildly elevated ALT level (less than 1.5 times normal) | ALT value could be normal for gender, ethnicity or body mass index. |
| Consider muscle injury or myopathy. | |
| Alcoholic hepatitis | Laboratory values can appear cholestatic, and symptoms can mimic cholecystitis. |
| Minimal elevations of AST and ALT often occur. | |
| AST level greater than 500 U per L | The AST elevation is unlikely to result from alcohol intake alone. |
| In a heavy drinker, consider acetaminophen toxicity. | |
| Common bile duct stone | Condition can simulate acute hepatitis |
| AST and ALT become elevated immediately, but elevation of AP and GGT is delayed. | |
| Isolated elevation of GGT level | This situation may be induced by alcohol and aromatic medications, usually with no actual liver disease. |
| Isolated elevation of AP level (asymptomatic patient with normal GGT level) | Consider bone growth or injury, or primary biliary cirrhosis. |
| AP level rises in late pregnancy. | |
| Isolated elevation of unconjugated bilirubin level | Consider Gilbert syndrome or hemolysis. |
| Low albumin level | Low albumin is most often caused by acute or chronic inflammation, urinary loss, severe malnutrition or liver disease; it is sometimes caused by gastrointestinal loss (e.g., colitis or some uncommon small bowel disease). |
| Normal values are lower in pregnancy. | |
| Blood ammonia level | Blood ammonia values are not necessarily elevated in patients with hepatic encephalopathy. |
| Determination of blood ammonia levels is most useful in patients with altered mental status of new onset or unknown origin. |
Ref:
- https://www.aafp.org/afp/2017/1201/p709.html
- Am Fam Physician. 1999;59(8):2223-2230
Flatus and Bloating
Here are medications that are over the counter that should help:
- simethicone 80 mg after meals and at bedtime
- alpha-galactosidase 600 units or 150 units (this is an enzyme and is in the product Beano) - Take 1-3 tablets or capsules with each meal
- Alpha-D-galactosidase oral drops:
- Take 5 drops/problem food right before your first bite. A typical meal has 3 servings of problem food.
- Alpha-D-galactosidase oral tablet/capsule, chewable:
- Chew or swallow whole 1 tablet/capsule per problem food right before your first bite. A typical meal has 3 servings of problem food.
References:
Flatus control
See also:
| Treatment | Symptom addressed | Effectiveness |
|---|---|---|
| Rifaximin | Volume | 3+ |
| Probiotcs - Prescript-Assist | Volume | 3+ |
| Probiotics - Bifidobacterium | Volume | 3+ |
| Probiotics - Lactobacillus | Volume | 3+ |
| Activated Charcoal Oral | Odor | 0+ |
| Activated Charcoal Briefs | Odor | 3+ |
| Activated Charcoal Pads | Odor | 2+ |
| Activated Charcoal Seat cushions | Odor | 1+ |
| Bismuth subsalicylate | Odor | 3+ |
| Alpha-galactosidase (Beano) | Volume | 1+ (300 GalU). |
| Alpha-galactosidase (Beano) | Volume | 2+ (1,200 GalU). |
| Simethicone/loperamide | Volume associated with diarrhea | 0+ |
Food Causes of flatus:
- Grains, including:
- Bagels, barley, breakfast cereals, granola, oat bran, pasta, rice bran, rye, sorghum grain, wheat bran, whole wheat flour, and whole grain breads
- Vegetables, including:
- Beets, broccoli, brussel sprouts, cabbage, cauliflower, corn, cucumbers, leeks, lettuce, onions, parsley, and sweet peppers
- Beans, including:
- Black-eyed peas, bog beans, broad beans, chickpeas, lentils, lima beans, mung beans, peanuts and peanut butter, pinto beans, red kidney beans, seed flour (sesame, sunflower), soybeans and soy milk.
Reference:
- AFP Vol 79 No 12 Jun 2009
Food Allergies
Most Prevalent Food Allergens
- Cow's milk
- Peanuts
- Eggs
- Shellfish
- Tree nuts
- Fish
- Wheat
- Soy
References:
- JFP Vol 69 No 7 Sep 2020
Food-Borne Illnesses edit
- Gastroenteritis (vomiting as primary symptom; fever and/or diarrhea also may be present)
- Viral gastroenteritis
- Most commonly rotavirus in infant or norovirus and other caliciviruses in older child or adult
- Food poisoning due to preformed toxins
- Vomitoxin
- Staphylococcus aureus toxin
- Bacillus cereus toxin
- Heavy metals
- Viral gastroenteritis
- Noninflammatory diarrhea (acute watery diarrhea without fever/dysentery; some may have fever)
- Can be from all enteric pathogens (bacterial, viral, parasitic) - classically:
- Enterotoxigenic Escherichia coli
- Giardia
- Vibrio cholerae
- Enteric viruses
- astroviruses
- noroviruses and other caliciviruses
- enteric adenovirus
- rotavirus
- Cryptosporidium
- Cyclospora cayetanensis
- Can be from all enteric pathogens (bacterial, viral, parasitic) - classically:
- Inflammatory diarrhea (invasive gastroenteritis; grossly bloody stool and fever may be present)
- Shigella species
- Campylobacter species
- Salmonella species
- Enteroinvasive E coli
- E coli O157:H7
- Vibrio parahaemolyticus
- Yersinia enterocolitica
- Entamoeba histolytica
- Persistent diarrhea (lasting >14 days)
- Parasites - particularly in travelors to mountainous or other areas where untreated water is consumed)
- C cayetanensis
- Cryptosporidium
- E histolytica
- Giardia lamblia
- Neurologic manifestations (paresthesias, respiratory depression, bronchospasm, cranial nerve palsies)
- Botulism (Clostridium botulinum toxin)
- Organophosphate pesticides
- Thallium poisoning
- Scrombroid fish poisoning (histamine, saurine)
- Ciguatera fish poisoning (ciguatoxin)
- Tetradon fish poisoning (tetradotoxin)
- Neurotoxic shellfish poisoning (brevitoxin)
- Paralytic shellfish poisoning (saxitoxin)
- Amnesic shellfish poisoning (domoic acid)
- Mushroom poisoning
- Guillain-Barre syndrome (associated with infectious diarrhea due to Campylobacter jejuni)
- Systemic illness (fever, weakness, arthritis, jaundice)
- Listeria monocytogenes
- Brucella species
- Trichinella spiralis
- Toxoplasma gondii
- Vibrio vulnificus
- Hepatitis A and E viruses
- Salmonella typhi and Salmonella paratyphi
- Amebic liver abscess
References:
- FP Essentials 370
- http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5304al.htm
Foodborne Pathogens Associated with Fever and Vomiting
Fever
- Characteristically associated:
- Campylobacter jejuni
- Shigella
- Vibrio cholerae non-O1
- Often associated
- Norwalk virus
- Salmonella
- Vibrio parahaemolyticus
Vomiting
- Characteristically associated:
- Bacillus cereus (emetic syndrome)
- Norwalk virus
- Staphylococcus aureus
- Often associated
- Clostridium botulinum
- V. cholerae O1
- V. parahaemolyticus
Reference:
- Am Fam Physician. 2015;92(5):358-365
Gall bladder Diet edit
See also:
In general, avoid foods high in fat and increase plant based foods. Here are some safe options for low-fat proteins, fiber, and unsaturated (healthy) fats.
Low-fat protein foods include:
- Poultry
- Fish
- Zero Fat Dairy Products
- Nuts and Seeds
- Soy And Soy Products
- Legumes, Such as Beans and Lentils
- Dairy Alternatives, such as Soy Milk
Sources of fiber include:
- Fruits
- Vegetables
- Legumes
- Nuts and Seeds
- Whole Grains
Unsaturated fat sources include:
- Cold-Water Fish
- Nuts, Such as Walnuts
- Seeds, Such as Flaxseed
- Oils From Fish or Flaxseed
Gastroesophageal Reflux Disease (GERD)
See also:
| Drug | Omeprazole equivalent |
|---|---|
| Pantoprazole 20 mg | 4.5 mg |
| Lansoprazole 15 mg | 13.5 mg |
| Omeprazole 20 mg | 20 mg |
| Esomeprazole 20 mg | 32 mg |
| Rabeprazole 20 mg | 36 mg |
Typical GERD
- Clinical Presentation
- Recurrent heartburn and acid regurgitation
- Chest pain
- Esophagitis
- Peptic strictures
- Barrett esophagus
- Treatment
- Lifestyle modification
- Weight loss, smoking cessation, and elevation of head of bed
- PPI treatment daily for 4-8 wks
- If poor response, consider altering dosage, timing, or initiating twice a day
- If adequate response, change to PPI as needed
- Antireflux surgery can be considered
- Lifestyle modification
- Followup
- If good PPI response - lower or stop dose
- If esophagitis or Barretts, continue PPI at lowest dose tolerated
- If treatment failure or alarm symptoms, urgent endoscopy
- If no response to PPI, esophageal manometry and endoscopy to assess esophageal motor disorders and lower esophageal sphincter function
- If no response to PPI, continue pH monitoring and perform endoscopy to confirm pathologic pH exposure
Extraesophageal GERD
- Clinical Presentation
- Hoarseness
- Wheezing
- Chronic cough
- Asthma
- Chronic laryngitis
- Teeth erosions
- Dyspepsia
- Belching
- Bloating
- Treatment
- PPI treatment daily for 8 wks for patients with concomitant typical GERD
- If adequate response, change to PPI as needed
- Antireflux surgery should not be considered for patients who do not respond to PPI treatment
- Antireflux surgery can be considered for patients who cannot tolerate PPI treatment
- PPI treatment daily for 8 wks for patients with concomitant typical GERD
- Followup
- If good PPI response - lower or stop dose
- If suspected extraesophageal symptoms persist with no typical GERD symptoms, pH monitoring should be considered
- If no response to PPI, consider further diagnostics
- If treatment failure or alarm symptoms, urgent endoscopy
References:
- JAMA Dec 2020 Vol 324 No 24
PPI's and Depression
Study examined the association between use of PPIs and depressive symptoms in an elderly population.
- 344 inhabitants of Tuscania (Italy) aged 75 years and over
- Use of PPIs was associated with a higher Geriatric Depression Scale (GDS) score in linear regression analysis (B = 2.43; 95% CI = 0.49-4.38; p = 0.014)
- Use of PPIs was associated with increased adjusted probability of depression in logistic regression (OR = 2.38; 95% CI = 1.02-5.58; p = 0.045).
- Higher PPIs dosages were associated with increased probability of depression (p for trend = 0.014).
- This association was independent of the diagnosis of peptic disease, as well as the use of antidepressant medications.
- No association was found between use of H2-blockers or antacids and the GDS score.
Calculation of the population attributable risk indicated that 14% of depression cases could be avoided by withdrawal of PPIs.
Mood should be routinely assessed in elderly patients on PPIs.
Reference:
- Laudisio A, Antonelli Incalzi R, Gemma A, Giovannini S, Lo Monaco MR, Vetrano DL, Padua L, Bernabei R, Zuccalà G. Use of proton-pump inhibitors is associated with depression: a population-based study. Int Psychogeriatr. 2018 Jan;30(1):153-159. doi: 10.1017/S1041610217001715. Epub 2017 Sep 13. PMID: 28899441.
Reflux Conservative Management
Ways to stop your reflux:
- Stop all caffeine, chocolate, alcohol, nicotine
- Elevate the head of the bed (do not use multiple pillows)
- Eat smaller meals more frequently
- Do not eat within 3 hours of going to bed
- Avoid wearing tight garments
- Follow these food rules:
| Avoid | Enjoy |
|---|---|
| Alcohol | Fresh vegetables |
| Barbecue sauces | Meat |
| Caffeine | Milk |
| Carbonated beverages | Poultry |
| Chocolate | Seafood |
| Citrus fruits | |
| Curry | |
| Excessive salt | |
| Fatty or Fried Foods | |
| Garlic | |
| Hot mustard | |
| Hot peppers | |
| Jams/Jellies | |
| Mint | |
| Onions | |
| Salad dressings | |
| Spicy foods | |
| Tomatoes |
References:
- JFP Vol 59 No 2 Feb 2010
- NEJM 359;16 Oct 2008
Ulcers
H pylori associated peptic ulcers
- 7d treatment with PPI+2 Abx heals >90%
- Clarithromycin + metronidazole, amoxicillin, or tinidazole
- SOR A
NSAID associated peptic ulcers
- 8wks of PPI > 4wks of PPI
- SOR A
NSAID associated duadenal ulcers
- 4wks PPI
- SOR A
Endoscopic submucosal dissection related gastric ulcers
- 4wks of PPI is as effective as 8wks
- 1/3 ulcers remain unhealed
- SOR B
References:
- JFP Vol 64 No 12 2015
- Helicobacter pylori
Sequential therapy with amoxicillin plus a proton pump inhibitor (PPI) for 5 days, followed by clarithromycin and metronidazole or tinidazole for 5 days, had a better eradication rate than standard triple therapy in randomized controlled trials performed to date. It is a good alternative for the eradication of Helicobacter pylori (HP) infection in symptomatic patients. (LOE = 1b)
Reference:
- Gatta L, Vakil N, Leandro G, Di Mario F, Vaira D. Sequential therapy or triple therapy for Helicobacter pylori infection: systematic review and meta-analysis of randomized controlled trials in adults and children. Am J Gastroenterol 2009;104(12):3069-3079.
Gastrointestinal Bleeding
Upper GI Bleeding edit
- PEPTIC ULCER DISEASE
- NSAID use and H. pylori infection account for approximately 80% of peptic ulcer disease and peptic ulcer bleeding
- EROSIVE DISORDERS
- Erosive disorders include esophagitis, gastritis, and duodenitis; they generally have a benign course and excellent prognosis
- MALLORY-WEISS SYNDROME
- Mallory-Weiss syndrome, a mucosal tear at the distal esophagus, frequently heals spontaneously, but significant bleeding may occur.
- MEDICATIONS ASSOCIATED WITH UPPER GI BLEEDING
- Antiplatelet Therapy.
- Aspirin carries a 37% increased risk of GI bleeding and is often prescribed as part of dual antiplatelet therapy for secondary prevention
- Anticoagulants. GI bleeding with warfarin (Coumadin) therapy has an incidence of 1% to 4% per year
- NSAIDs. NSAIDs are associated with peptic ulcer disease and peptic ulcer bleeding.
- Selective Serotonin Reuptake Inhibitors (SSRIs). A meta-analysis of 22 studies that included more than 1 million participants found that SSRI use increased the risk of upper GI bleeding by 55%
Evaluation:
- Determine the severity of the bleeding, to identify the possible source of bleeding, and to guide management decisions, such as hospitalization, transfusion, and diagnostic testing
- NPO
- Regular monitoring of heart rate, blood pressure, and pulse oximetry is necessary during resuscitation and stabilization
Laboratory Tests:
- complete blood count, basic metabolic panel, coagulation panel, liver tests, and type and crossmatch
- blood urea nitrogen/creatinine ratio greater than 36 is suggestive of upper GI bleeding when distinguishing it from lower GI bleeding (sensitivity 90%)
Management
- Current guidelines recommend blood transfusion for patients with upper GI bleeding when hemoglobin is less than 8 g per dL (80 g per L), including patients with coronary artery disease, recent cardiac surgery, or hematologic malignancies
- Endoscopy: Patients with hemodynamic instability and signs of upper GI bleeding should be offered urgent endoscopy (within 24 hours of presentation or onset of bleeding) after fluid resuscitation and stabilization.
- Proton pump inhibitors should be started upon presentation with upper GI bleeding
- Repeat endoscopy is recommended in persons with rebleeding because hemostasis is achieved in 73% of these patients
- Guidelines recommend resumption of aspirin for secondary prevention of cardiovascular disease immediately following endoscopy if the rebleeding risk is low or within three days if the rebleeding risk is moderate or high
- H. PYLORI ERADICATION
- A test of cure is recommended at least four weeks after the completion of antibiotics and one to two weeks after completion of proton pump inhibitor therapy
References:
- AFP Mar 2020 Vol 101 No 5
Lower GI Bleeding
Differential Diagnosis:
| Diagnosis | Distinguishing features | Evaluation and treatment | |||
|---|---|---|---|---|---|
| Angiodysplasia, angioectasias, or arteriovenous malformation | Recurrent painless bleeding episodes; patient > 60 years | Colonoscopy with endoscopic argon plasma coagulation7 Consider long-term treatment with lanreotide (Somatuline), 120 mg subcutaneously every 4 weeks (adjust dosing for patients with renal or hepatic impairment) | |||
| Colon cancer | Slow, chronic blood loss with occasional changes in bowel habit | Colonoscopy with endoscopic therapy (e.g., cautery, banding, clipping, epinephrine injection) to control bleeding2 Referral to surgical and oncologic specialists | |||
| Diverticular bleeding | Acute, severe, painless bleeding; history of or suspected diverticular disease | Colonoscopy with endoscopic therapy to control bleeding Consider abdominal CTA to localize the bleeding site | Hemorrhoids | Bleeding associated with bowel movements External: painful and itchy Internal: painless, may be itchy | Fiber supplementation (decreases bleeding by 50%); banding or infrared photocoagulation for grades I to III; surgery likely required for symptomatic grade III and grade IV |
| Infectious colitis | Bloody diarrhea with fever; new or concerning food exposures | Antibiotics based on identified pathogen, except for Shiga toxin–producing Escherichia coli and Salmonella, which are treated with supportive care alone | |||
| Inflammatory bowel disease | Bloody diarrhea associated with recurrent abdominal pain and weight loss | Colonoscopy with biopsies to confirm diagnosis Fecal calprotectin ≥ 250 mcg per g Rectal 5-aminosalicylic acid derivatives (e.g., mesalamine) | |||
| Ischemic colitis | Bloody diarrhea followed by acute lower abdominal pain, especially in patients with cardiac risk factors | Colonoscopy or CTA to confirm diagnosis Medical management of underlying vascular disease; may require surgery | |||
| Postpolypectomy bleeding | Bleeding within 30 days of polypectomy or biopsy | Colonoscopy with endoscopic therapy to control bleeding |
Common Infectious Colitis Pathogens Associated with Lower Gastrointestinal Bleeding
| Organism | History | Treatment |
|---|---|---|
| Campylobacter | Ingestion of undercooked poultry | Azithromycin (Zithromax), 500 mg per day for 3 to 5 days |
| Entamoeba histolytica | Travel to endemic areas (e.g., tropical Africa, Asia, Latin America) | Metronidazole (Flagyl), 750 mg 3 times per day for 5 to 10 days plus Paromomycin, 25 to 35 mg per kg per day in 3 divided doses for 5 to 10 days |
| Salmonella | Ingestion of contaminated foods (e.g., eggs, poultry); can be spread by pets (e.g., turtles, snakes) | Supportive care |
| Shiga toxin–producing Escherichia coli | Ingestion of undercooked ground beef | Supportive care |
| Shigella | Exposure to surfaces or ingestion of food or water contaminated with infected fecal matter | Ciprofloxacin, 500 mg 2 times per day for 3 days |
Outpatient Management for hemodynamically stable patients (HR<100bpm, SBP > 115, cap refil <3s):
- Painful bleeding:
- Recent travel or food exposure
- Stool cultures and consider antibiotics
- Intermittent with abd pain and weight loss
- Fecal calprotectin and refer for diagnostic colonoscopy
- Acute onset with apd pain and h/o cardiovascular disease
- Urgent colonoscopy
- After bowel movements and pruritic
- Anoscopy with valsalva
- Increase fiber in diet
- Consider surgical referral
- Recent travel or food exposure
- Painless bleesing
- Intermittent bleeding, bowel habit changes, and weight loss
- Diagnostic colonoscopy
- Acute onset with h/o diverticular disease
- Urgent colonoscopy
- Painless bleeding within 30 days of polypectomy or biopsy
- Urgent diagnostic colonoscopy
- Recurrent bleeding with no other symptoms
- Diagnostic colonoscopy
- Intermittent bleeding, bowel habit changes, and weight loss
References:
- AFP Feb 2020 Vol 101, No 4
Gastroparesis
Management:
- First line:
- metoclopramide
- Second line:
- domperidone
- erythromycin
- Also consider:
- antiemetic agents
Dietary recommendations:
- Ingest multiple small meals
- Favor liquids over solids
- Avoid indigestible solids
- Consume low-fat meals
Sources of Insoluble Fiber to Avoid:
- Whole grains, such as wheat bran, oats, and barley
- Fruits, such as berries, apples, and bananas (peels and pulp)
- Vegetables, such as broccoli, carrots, and potatoes (skins and pulp)
- Legumes, such as beans and lentils
- Nuts and seeds, such as almonds and flaxseeds
To help test/treat/manage gastroparesis (slow gut motility), there are a few ideas:
Nutrition:
- A systematic review demonstrated low-fat diets and small particle size diets improve symptoms and gastric emptying.
- Foods in small particle size through small meals throughout the day (https://www.gastroparesisaustralia.com/small-particle-size-diet)
- Fat content (25–30% of total energy)
- Fiber content (15g/1000kcal)
- 4-6 small meals per day based on tolerance
- Liquid meals and/or high energy/ protein oral nutritional supplement (ONS) if appropriate
Medications:
- Prokinetics: metoclopramide, erythromycin, domperidone, etc
- Anti-emetics: Meclizine, Ondansetron, etc
Cautions:
- Patients with gastroparesis often discover or adopt restrictive diets to manage their symptoms and may be vulnerable to developing or exacerbating an underlying eating disorder
References:
- JFP Vol 67 No 11 Nov 2018
- Eseonu D, Su T, Lee K, Chumpitazi BP, Shulman RJ, Hernaez R. Dietary Interventions for Gastroparesis: A Systematic Review. Adv Nutr. 2022 Oct 2;13(5):1715-1724. doi: 10.1093/advances/nmac037. PMID: 35425953; PMCID: PMC9526854.
- Diet-Based Treatments of Gastroparesis with a Special Focus on Small Particle Size
Hemorrhoids
Common Nonsurgical Measures to Treat Hemorrhoids
- Adequate insoluble fiber (25 to 35 g per day) and water intake (1.5 to 2 L per day)
- Behavior modification: avoid straining and prolonged periods on toilet, limit fatty foods and alcohol, perineal hygiene, weight loss
- Sitz baths or warm water sprays
- Stool softeners
- Topical analgesics, antiseptics, steroids, or vasoactive agents
See also:
Lifestyle Changes for hemorrhoids:
- Dietary modifications:
- Increase fiber intake through foods like whole grains, fruits, and vegetables.
- Drink plenty of water (at least 8-10 glasses a day) to prevent constipation.
- Regular exercise: Engage in moderate physical activity, such as walking, to improve circulation and reduce pressure on veins.
- Proper bowel habits:
- Avoid straining during bowel movements.
- Use a squatting position or a stool for support while defecating.
- Avoid delaying bowel movements.
If they become uncomfortable:
- Warm baths: Soak in a warm bath for 10-15 minutes, 2-3 times a day, to reduce swelling and discomfort.
- Ice packs: Apply a cold compress or an ice pack wrapped in a towel to the affected area for 5-10 minutes, 2-3 times a day, to reduce pain and inflammation.
- Topical creams and ointments: Use over-the-counter hydrocortisone cream or witch hazel to reduce itching and inflammation. Can also use Zinc oxide topical paste for its protectant, astringent, and antiseptic properties.
- Stool softeners: Take a stool softener like docusate sodium (Colace) or psyllium (Metamucil) to help regulate bowel movements.
Notes:
- Docusate 100 mg twice a day
- Phenylephrine 0.25% rectal ointment or suppository (eg, Preparation-H)
- Apply as needed up to four times per day
- Frequent choice for temporary relief of acute symptoms (ie, bleeding or pain on defecation).
- Well tolerated; rare systemic effects.
References:
- AFP Vol 101 No 1 Jan 2020
Irritable Bowel Syndrome
See also:
Typical:
- Loose/frequent stools
- Constipation
- Bloating
- Abdominal cramping, discomfort, pain
- Symptom brought on by food intake/specific food sensitivities
- Symptoms dynamic over time
Concerning for organic disease:
- Symptom onset >50yo
- Severe or progressive symptoms
- Unexplained weight loss
- Nocturnal diarrhea
- FH of organic GI diseases (colon ca, celiac, inflammatory bowel disease)
- Rectal bleeding or melena
- Unexplained Fe def anemia
IBS Diagnosis (Rome IV)
- Recurrent abdominal pain, with onset more than 6 mo ago, occurring on average 1 day per week in past 3 months associated with 2 or more of the following:
- Onset related to defecation
- Onset associated with a change in frequency of stool
- Onset associated with a change in form of stool
Subtypes:
- IBS with constipation - hard or lumpy stools over 25% and loose or watery stools <25%
- IBS with diarrhea - loose or watery stools over 25% and hard or lumpy <25%
- Mixed IBS - hard or lumpy and loose and watery each over 25% of time
Diagnostic Criteria
- Recurrent abdominal pain, with onset more than 6 months earlier, occurring on average at least 1 day per week in the past 3 months, and associated with 2 or more of the following features
- Related to defecation (may be improved or worsened)
- Associated with a change in the frequency of stool
- Associated with a change in the form or appearance of stool
- Additional symptoms support the diagnosis of IBS
- Abnormal stool frequency (more than 3 times per day or less than 3 times per week)
- Abnormal stool form (loose and watery or lumpy and hard)
- Abnormal stool passage (urgency, straining, feeling of incomplete evacuation)
- Passage of mucus (white material)
- Abdominal bloating
- Abdominal distention
- Absence of nocturnal stools
- Subtypes of IBS*
- IBS with predominant diarrhea: > 25% of bowel movements are Bristol Stool Scale type 6 or 7, and < 25% are type 1 or 2
- IBS with predominant constipation: > 25% of bowel movements are Bristol Stool Scale type 1 or 2, and < 25% are type 6 or 7
- IBS with mixed symptoms of constipation and diarrhea: > 25% of bowel movements are Bristol Stool Scale type 1 or 2, and > 25% are type 6 or 7
- Unclassified IBS: bowel movements cannot be accurately categorized as one of the three subtypes
Reference:
- AFP Jun 2021 Vol 103 No 12
Evaluation
Assessment:
- History
- Identify symptoms of IBS
- Screen for:
- Nocturnal diarrhea
- Straining to evacuate stool
- Somatization
- Psychological history
- FH of dietary intolerance or celiac disease
- Bladder symptoms
- Exam
- Exclude
- abdominal mass
- intestinal obstruction
- localized abdominal wall pain
- DRE to exclude rectal mass and pelvic floor dysfunction
- Exclude
- Labs
- CBC and CRP
- Exclude anemia or Inflamatory bowel disease
- Tissue transglutaminase IgA
- Exclude celiac disease
- Colonoscopy
- If >45yo or presents with recent change in bowel function, unintentional weight loss, associated rectal bleeding, anemia, or Fe deficiency to exclude colon ca
- CBC and CRP
References:
- JAMA Mar 2021 Vol 325 No 9
Alarm Features Suggesting the Possible Need for Further Testing
- Abdominal mass
- Extreme diarrhea symptoms (large volume, bloody, nocturnal, progressive pain, does not improve with fasting)
- Fever
- Gastrointestinal bleeding (overt: melena or hematochezia; occult: anemia or fecal occult blood on testing)
- Jaundice
- Lymphadenopathy
- New-onset symptoms in patients 55 years and older
- Symptoms of chronic pancreatitis
- Symptoms of gastrointestinal cancer or a family history of the disease
- Symptoms of ovarian cancer or a family history of the disease
- Tenesmus (rectal pain or feeling of incomplete evacuation)
- Unintentional weight loss
Reference:
- AFP Jun 2021 Vol 103 No 12
IBS with Constipation:
- If severe or medically refractory - refer to GI for physiologic testing
- Treatment:
- Antibiotics - Neomycin
- Antidepressants
- Antispasmodics
- 5-HT4 agonists - Tegaserod - NNT=17
- OTC Laxatives
- Probiotics
- Selective C-2 chloride channel activator - Lubiprostone
IBS with Diarrhea:
- CRP or fecal calprotectin
- IgA tissue transutaminase +/- quantitative IgA
- Random biopsies if colonoscopy performed
- tauroselcholic acid (selenium 75)
- fecal bile acids, or serum C4 if available
- Treatment:
- Antibiotics - Rifaximin - NNT=11
- Antidepressants
- Antispasmodics
- 5-HT3 agonists - Alosetron - NNT=7
- Probiotics
Mixed IBS:
- CRP or fecal calprotectin
- IgA tissue transutaminase +/- quantitative IgA
- Stool diary
- Consider radiography to eval stool accumulation
- Treatment:
- Antibiotics
- Antidepressants
- Antispasmodics
- Probiotics
IBS Treatment/Management:
First Line:
- Constipation
- fiber (preferrably ispaghula husks)
- osmotic laxatives (such as saline laxatives or polyethylene glycol 3350)
- Diarrhea
- Loperamide
- Cramping and abdominal pain
- antispasmotics (such as hyoscine)
- For prominenet psychological symptoms or multiple somatic comorbidities
- low-dose TCA (such as amitriptyline)
Nonpharmacologic approaches:
- Dietary exclusion of sugars
- Low FODMAP diet
- Microbial modification using pre- and pro-biotics or fecal microbial transplant
- Acupuncture may be indicated
Exercise, probiotics, antibiotics, antispasmodics, antidepressants, psychological treatments, and peppermint oil may improve IBS symptoms (SOR B)
- FODMAP diet
- Exercise - NNT=7.4
- For Abdominal pain/discomfort
- Antidepressants - NNT=4
- SSRIs for IBS-C and TCAs for IBS-D (A)
- Alostetron (5-HT3 antagonist)
- Antispasmodics - peppermint oil (B); dicyclomine; NNT=5 for global assessment
- Antidepressants - NNT=4
- For Constipation
- Fiber - psyllium (B)
- Laxatives - polyethylene glycol (C); Milk of Magnesia
- Prosecretory agents - Linaclotide - IBS-C and Mixed
- Lubiprostone (chloride channel activator)
- For Bloating
- Probiotics - NNT=4 to prevent worsening
- Rifaximin
- For Diarrhea
- Antidiarrheals - loperamide (C)
- Alosetron
- Rifaximin
- Eluxadoline
References:
- AFP Vol 86 No 5 Sep 2012
- JFP Vol 66 No 6 Jun 2017
- JAMA Mar 2021 Vol 325 No 9
First-Line Management of IBS and Other Functional Gastrointestinal Disorders
- Diet
- General
- Patients should focus on eating in moderation, getting adequate but not excessive fiber, decreasing fatty and spicy foods, and avoiding caffeine, soft drinks, carbonated drinks, and artificial sweeteners before considering more restrictive elimination diets
- FODMAP-restricted diet
- Shows promise for IBS management, but questions remain regarding long-term safety, effectiveness, and practicality; if this diet is initiated, patients should be supervised by an experienced dietitian
- Gluten-free diet
- Patients with celiac disease derive clear benefit; some patients without celiac disease markers seem to benefit (wheat contains gluten and high levels of fructans; reduction of fructans may partly explain the benefit in patients with IBS)
- Long-term effects of a gluten-free diet on microbiome and general nutrition are uncertain; strictly adhering to this diet is difficult and expensive
- Recommended only for patients with proven celiac disease
- General
- Exercise
- Regular daily exercise decreases symptoms of IBS and chronic constipation
- Fiber
- Soluble fiber (psyllium [Metamucil]): 25 to 30 g daily has a small benefit for some patients with IBS but can worsen bloating in others
- Insoluble fiber (bran, methylcellulose, polycarbophil [Fibercon]): 2 heaping teaspoons daily was of no benefit to patients with IBS; some benefit for chronic constipation
- All fiber should be increased gradually to minimize bloating, distention, flatulence, and cramping
- Worsening of gas and bloating with fiber supplementation may also suggest underlying dyssynergic defecation (pelvic floor dysfunction)
- Osmotic laxatives
- Polyethylene glycol (Miralax): 17 g once daily; this is the best studied osmotic laxative and is most effective for chronic constipation, with slight improvement in stool frequency in IBS-C
- Other osmotic laxatives include lactulose, sorbitol, and mannitol
- Probiotics
- Probiotics, especially Bifidobacterium infantis, improve bloating, flatulence, and pain in IBS and may also help chronic constipation
- Antispasmodics
- Dicyclomine: 20 mg 4 times daily (maximum 40 mg four times daily) 30 minutes before meals; moderately effective for IBS
- Hyoscyamine extended release (Levbid), 0.375 to 0.75 mg 2 times daily (maximum 1.5 g per day); moderately effective for IBS
- Hyoscyamine (Levsin), 0.125 to 0.25 mg every 4 hours as needed (maximum 1.5 mg per day; 30 minutes before meals); moderately effective for IBS
- Peppermint oil: 200 to 750 mg 2 or 3 times daily; moderately effective for IBS
- STW 5 herbal preparation (proprietary blend of 9 herbs, available over the counter): 20 drops (30 minutes before meals); antispasmodic and prokinetic actions
- Opioid agonists
- Diphenoxylate/atropine (Lomotil) has not been studied in IBS
- Loperamide (Imodium): 2 to 4 mg up to 4 times daily; decreases colonic transit and increases water absorption, improves many IBS-D symptoms, including urgency and stool frequency
- Older clinical trials were small but demonstrated improved overall response
- Serotonin (5-HT3) receptor antagonist
- Ondansetron (Zofran): 4 mg up to 3 times daily (many patients need to use only once daily or less); improves urgency and frequency of loose stools in IBS-D and postinfectious IBS
- Less improvement of pain but two-thirds of patients report adequate relief; some of the benefit may be related to relief of coexisting heartburn and postprandial pain/dyspepsia
- Widely available, inexpensive, excellent safety profile over many decades (alosetron [Lotronex], a more potent serotonin (5-HT3) receptor antagonist approved only for more severe IBS-D in women, has significant safety concerns)
- Antidepressants (gut-brain modulators)
- Amitriptyline: 10 to 50 mg at bedtime (increase by 10 mg every 1 to 2 weeks) and other tricyclic antidepressants; effective for overall symptom relief in IBS-D and other functional gastrointestinal disorders
- Histaminergic properties are moderately sedating, and anticholinergic properties are moderately constipating55
- Serotonin-norepinephrine reuptake inhibitors (e.g., duloxetine [Cymbalta]): strong evidence for benefit in several chronic pain disorders but not currently studied in IBS
- Selective serotonin reuptake inhibitors: slight overall improvement, probably related to relief of central and visceral hypersensitivity and psychological distress; may help constipation
Reference:
- AFP Jun 2021 Vol 103 No 12
Diet: Avoid Gas producing foods
See also:
Here are high gas producing foods to AVOID:
- Beans
- Onions
- Celery
- Carrots
- Raisins
- Bananas
- Apricots
- Prunes
- Brussels Sprouts
- Wheat Germ
- Pretzels
- Bagels
- Alcohol
- Caffeine
Diet: General IBS Dietary Ideas
General Strategies:
- Regular meal pattern
- Avoidance of large meals
- Reduced intake of fat
- Reduce intake of insoluble fibers
- Supplement with psyllium/ispaghula
Diet: Low FODMAP Diet
How to use Low FODMAP diet:
- Eliminating FODMAPs from the diet for six to eight weeks
- After symptom resolution, gradually reintroduce of foods high in fermentable carbohydrates to determine tolerance to specific fermentable carbohydrates
Eat a diet of low fermentable oligo-, di-, and monosaccharides and polyols (FODMAPs): (Avoid these):
- Apples
- Apricots
- Artichokes
- Artificially Sweetened Chewing Gum
- Asparagus
- Barley
- Beetroot
- Cashews
- Cauliflower
- Cherries
- Chickpeas
- Chicory
- Fennel
- Garlic
- High-Fructose Corn Syrup
- Honey
- Leek
- Legumes
- Lentils
- Mangoes
- Milk, Custard, Ice Cream And Yogurt
- Mushrooms
- Nectarines
- Onion
- Peaches
- Pears
- Peas
- Pistachio
- Plums
- Rye
- Shallots
- Sugar Snap Peas
- Watermelon
- Wheat
- White Part Of Spring Onion
Diet: FODMAP Food Reference
Low FODMAPs:
- Vegetables and Legumes
- Bamboo shoots
- Bean sprouts
- Broccoli
- Cabbage, common and red
- Carrots
- Celery (less than 5cm stalk)
- Chick peas (1/4 cup max)
- Corn (1/2 cob max)
- Courgete
- Cucumber
- Eggplant
- Green beans
- Green pepper
- Kale
- Letuce e.g. Buter, iceberg, rocket
- Parsnip
- Potato
- Pumpkin
- Red peppers
- Scallions / spring onions (green part)
- Squash
- Sweet potato
- Tomatoes
- Turnip
- Fruit
- Bananas, unripe
- Blueberries
- Cantaloupe
- Cranberry
- Clementne
- Grapes
- Melons e.g. Honeydew, Galia
- Kiwifruit
- Lemon
- Orange
- Pineapple
- Raspberry
- Rhubarb
- Strawberry
- Meats
- Beef
- Chicken
- Cold cuts e.g. Ham and turkey breast
- Fresh Fish
- Lamb
- Pork
- Quorn mince
- Tuna
- Breads, Cereals, Grains and Pasta
- Oats
- Quinoa
- Gluten free foods e.g. breads, pastaSavory biscuits
- Buckwheat
- Chips / crisps (plain)
- Cornflour
- Oatmeal (1/2 cup max)
- Popcorn
- Pretzels
- Rice e.g. Basmata, brown, white
- Tortlla chips
- Nuts and Seeds
- Almonds (max of 15)
- Chestnuts
- Hazelnuts
- Macademia nuts
- Peanuts
- Pecans (max of 15)
- Poppy seeds
- Pumpkin seeds
- Sesame seeds
- Sunfower seeds
- Walnuts
- Dairy, Eggs, Cheese
- Almond milk
- Coconut milk
- Hemp milk
- Lactose free milk
- Oat milk (30ml max)
- Rice milk (200ml max)
- Soy milk made with soy protein
- Butter
- Dark chocolate
- Eggs
- Milk chocolate (3 squares max)
- White chocolate (3 squares max)
- Brie
- Camembert
- Cheddar
- Cottage cheese
- Feta
- Mozzarella
- Parmesan
- Swiss
- Condiments
- Barbeque sauce
- Chutney (1 tbsp max)
- Garlic infused oil
- Golden syrup
- Strawberry jam / jelly
- Mayonnaise
- Mustard
- Soy sauce
- Tomato sauce
- Sweeteners
- Aspartame
- Acesulfame K
- Glucose
- Saccharine
- Stevia
- Sucralose
- Sugar / sucrose
- Drinks
- Beer (one max)
- Black coffee
- Herbal tea (weak)
- Orange juice (125ml max)
- Peppermint tea
- Water
- Wine (one max)
High FODMAPs:
- Vegetables and Legumes
- Garlic
- Onions
- Aparagus
- Beans e.g. black, broad, kidney, lima, soy
- Caulifower
- Cabbage, savoy
- Mange tout
- Mushrooms
- Peas
- Scallions / spring onions (white part)
- Fruit
- Apples
- Apricot
- Avocado
- Bananas, ripe
- Blackberries
- Grapefruit
- Mango
- Peaches
- Pears
- Plums
- Raisins
- Sultanas
- Watermelon
- Meats
- Chorizo
- Sausages
- Processed meat
- Breads, Cereals, Grains and Pasta
- Barley
- Bran
- Cous cous
- Gnocchi
- Granola
- Muesli
- Muffins
- Rye
- Semolina
- Spelt
- Wheat foods e.g. Bread, cereal, pasta
- Nuts and Seeds
- Cashews
- Pistachio
- Dairy, Eggs, Cheese
- Cow milk
- Goat milk
- Sheep's milk
- Soy milk made with soy beans
- Butermilk
- Cream
- Custard
- Greek yoghurt
- Ice cream
- Sour cream
- Yoghurt
- Cream cheese
- Ricota cheese
- Condiments
- Hommus dip
- Jam (mixed berries)
- Pasta sauce (cream based)
- Relish
- Tzatziki dip
- Sweeteners
- Agave
- High Frucose Corn Syrup (HFCS)
- Honey
- Inulin
- Isomalt
- Malttol
- Mannitol
- Sorbitol
- Xylito
- Drinks
- Apple juice
- Coconut water
- Fennel tea
- Herbal tea (strong)
- Kombucha
- Mango juice
- Pear juice
- Rum
- Sodas with HFCS
Refernece:
FoodMarble - MedAIRE and MedAIRE2 edit
- AIRE (IBS/FODMAP) - Measures fermentation - Hydrogen
- AIRE2 (IBS/FODMAPs and SIBO) - Hydrogen and Methane levels
AIRE (IBS/FODMAP) - Measures fermentation - Hydrogen When you see increases in breath readings, that indicates what you ate or drank hasn't been fully digested and is now being fermented in your gut by the bacteria that live there. After a breath test, the app will show you the meals you've logged. It will also show you how much of those hard-to-digest FODMAPs are in each meal, so you can link an increase in breath readings to something you ate or drank.
AIRE2 (IBS/FODMAPs and SIBO) - Hydrogen and Methane levels Nearly everyone naturally produces hydrogen in their breath, and many of us have gut microbes that convert it to methane. However, for IBS, the levels of hydrogen and methane can be quite high. It's essential to understand how much gas your body can tolerate without experiencing symptoms. In IBS, an overproduction of hydrogen gas often leads to frequent diarrhea, while excess methane gas typically results in constipation. To better control your symptoms, quantifying the fermentation level of both gases in relation to your food triggers is necessary. This is where AIRE 2 steps in to help you master your gut health.
Reference:
Jaundice
Initial laboratory tests include (CMP, Indirect Bili, PT/INR, Hepatitis panel):
- measurements of serum total and unconjugated bilirubin (CMP)
- alkaline phosphatase (CMP)
- aminotransferases (aspartate aminotransferase [AST] and alanine aminotransferase [ALT]) (CMP)
- prothrombin time/international normalized ratio (PT/INR)
- albumin (CMP)
Patterns of liver test abnormalities — Liver test abnormalities can often be grouped into one of several patterns: the abnormalities may be acute, subacute, or chronic based on whether they have been present for less than six weeks (acute), six weeks to six months (subacute), or more than six months (chronic). Based on the pattern of elevation, liver test abnormalities may be grouped as hepatocellular, cholestatic, or isolated hyperbilirubinemia. Hepatocellular pattern: Disproportionate elevation in the serum aminotransferases compared with the alkaline phosphatase Serum bilirubin may be elevated Tests of synthetic function may be abnormal
Cholestatic pattern: Disproportionate elevation in the alkaline phosphatase compared with the serum aminotransferases Serum bilirubin may be elevated Tests of synthetic function may be abnormal
Isolated hyperbilirubinemia: As the term implies, patients with isolated hyperbilirubinemia have an elevated bilirubin level with normal serum aminotransferases and alkaline phosphatase
The R value (also known as the R factor) can be used to help determine the likely type of liver injury (hepatocellular versus cholestatic) in patients with elevated aminotransferases and alkaline phosphatase.
- R value = (ALT ÷ ULN ALT) / (alkaline phosphatase ÷ ULN alkaline phosphatase)
- (ULN = upper Limit of Normal)
- The R value is interpreted as follows:
- ≥5: Hepatocellular injury
- >2 to <5: Mixed pattern
- ≤2: Cholestatic injury
Because the serum bilirubin can be prominently elevated in both hepatocellular and cholestatic conditions, it is not helpful in differentiating between the two. Common hepatocellular diseases associated with an elevated bilirubin and jaundice include viral and toxic hepatitis (including drugs, herbal therapies, and alcohol) and end-stage cirrhosis from any cause (table 2).
If both the serum aminotransferases and alkaline phosphatase are elevated, the liver test abnormalities are characterized by the predominant abnormality (eg, if the serum aminotransferases are 10 times the upper limit of normal and the alkaline phosphatase is twice the upper limit of normal, the liver test abnormalities would be characterized as primarily hepatocellular). However, making this distinction is not always possible. The degree of aminotransferase elevation can occasionally help in differentiating between hepatocellular and cholestatic processes. While ALT and AST values less than eight times the upper limit of normal may be seen in either hepatocellular or cholestatic liver disease, values 25 times the upper limit of normal or higher are seen primarily in hepatocellular diseases.
Abnormal tests of synthetic function may be seen with both hepatocellular injury and cholestasis. A low albumin suggests a chronic process, such as cirrhosis or cancer, while a normal albumin suggests a more acute process, such as viral hepatitis or choledocholithiasis. A prolonged prothrombin time indicates either vitamin K deficiency due to prolonged jaundice and intestinal malabsorption of vitamin K or significant hepatocellular dysfunction. The failure of the prothrombin time to correct with parenteral administration of vitamin K suggests severe hepatocellular injury. (See "Tests of the liver's biosynthetic capacity (eg, albumin, coagulation factors, prothrombin time)".)
AST to ALT ratio — Most causes of hepatocellular injury are associated with a serum AST level that is lower than the ALT. An AST to ALT ratio of 2:1 or greater is suggestive of alcoholic liver disease, particularly in the setting of an elevated gamma-glutamyl transpeptidase [19]. In a study of 271 patients with biopsy-confirmed liver disease, more than 90 percent of the patients in whom the AST to ALT ratio was two or greater had alcoholic liver disease [20]. The percentage increased to greater than 96 percent when the ratio was greater than three. In addition, 70 percent of the patients with known alcoholic liver disease had an AST to ALT ratio greater than two. (See "Clinical manifestations and diagnosis of alcohol-associated fatty liver disease and cirrhosis", section on 'Liver test abnormalities'.)
However, the AST to ALT ratio is occasionally elevated in an alcoholic liver disease pattern in patients with nonalcoholic steatohepatitis, and it is frequently elevated (although not greater than two) in patients with hepatitis C who have developed cirrhosis. In addition, patients with Wilson disease or cirrhosis due to viral hepatitis may have an AST that is greater than the ALT, although in patients with cirrhosis the ratio typically is not greater than two. (See "Wilson disease: Clinical manifestations, diagnosis, and natural history", section on 'Hepatic disease'.)
Magnitude of AST and ALT elevations — The magnitude of AST and ALT elevations varies depending on the cause of the hepatocellular injury [21-24]. While values may vary in individual patients, the following are typical AST and ALT patterns: Alcoholic fatty liver disease: AST <8 times the upper limit of normal; ALT <5 times the upper limit of normal. Nonalcoholic fatty liver disease: AST and ALT <4 times the upper limit of normal. Acute viral hepatitis or toxin-related hepatitis with jaundice: AST and ALT >25 times the upper limit of normal. Ischemic hepatitis (ischemic hepatopathy, shock liver, hypoxic hepatitis): AST and ALT >50 times the upper limit of normal (in addition the lactate dehydrogenase is often markedly elevated). Chronic hepatitis C virus infection: Wide variability, typically normal to less than twice the upper limit of normal, rarely more than 10 times the upper limit of normal. Chronic hepatitis B virus infection: Levels vary; the AST and ALT may be normal in inactive carriers, whereas most patients with chronic hepatitis B have mild to moderate elevations (approximately twice the upper limit of normal); with exacerbations, levels are more than 10 times the upper limit of normal.
Marked elevations in serum aminotransferase levels may be seen with: Acetaminophen (paracetamol) toxicity Idiosyncratic drug reactions Acute viral hepatitis (hepatitis A, B, C, D, E; herpes simplex virus; varicella zoster virus; Epstein-Barr virus; cytomegalovirus [CMV]); other viral infections; or n acute exacerbation of chronic viral hepatitis (hepatitis B) Alcoholic hepatitis Autoimmune hepatitis Wilson disease Ischemic hepatitis Budd-Chiari syndrome Sinusoidal obstruction syndrome (veno-occlusive disease) HELLP (hemolysis, elevated liver enzymes, low platelets) syndrome and occasionally acute fatty liver of pregnancy Malignant infiltration (most often breast cancer, small cell lung cancer, lymphoma, melanoma, or myeloma) Partial hepatectomy Toxin exposure, including mushroom poisoning Sepsis Heat stroke Muscle disorders (acquired muscle disorders [eg, polymyositis], seizures, and heavy exercise [eg, long distance running])
Conditions associated with mild to moderate serum aminotransferase elevations include (table 3): Medication use Chronic viral hepatitis (hepatitis B, C, D) Alcoholic liver disease Hemochromatosis Nonalcoholic fatty liver disease Autoimmune hepatitis Wilson disease Alpha-1 antitrypsin deficiency Congestive hepatopathy Adult bile ductopenia Malignant infiltration (most often breast cancer, small cell lung cancer, lymphoma, melanoma, or myeloma) Muscle disorders (eg, subclinical inborn errors of muscle metabolism) Thyroid disorders Celiac disease Adrenal insufficiency Anorexia nervosa Macro-AST (moderate elevations in plasma AST levels due to the presence AST-immunoglobulin complexes, usually IgG) [28]
If the initial evaluation fails to identify a likely source of the aminotransferase elevation, we test for the following: Autoimmune hepatitis: Antinuclear antibodies, anti-smooth muscle antibodies, and anti-liver/kidney microsomal antibodies, IgG (see "Overview of autoimmune hepatitis", section on 'Diagnostic evaluation'). Wilson disease: Serum ceruloplasmin, evaluation for Kaiser-Fleisher rings, (see "Wilson disease: Clinical manifestations, diagnosis, and natural history", section on 'Initial evaluation'). Alpha-1 antitrypsin deficiency: Serum alpha-1 antitrypsin level; if indicated, alpha-1 antitrypsin phenotyping (see "Clinical manifestations, diagnosis, and natural history of alpha-1 antitrypsin deficiency", section on 'Evaluation and diagnosis'). Thyroid disorders: Thyroid-stimulating hormone, free T4 concentration, free T3 concentration (see "Diagnosis of and screening for hypothyroidism in nonpregnant adults" and "Diagnosis of hyperthyroidism"). Celiac disease: Antibody screening with serum tissue transglutaminase antibodies [33] (see "Diagnosis of celiac disease in adults").
If the source of the liver test abnormalities is still unclear, we test for the following: Adrenal insufficiency (in patients with symptoms associated with adrenal insufficiency, such as chronic malaise, anorexia, or weight loss): 8 AM serum cortisol and plasma corticotropin (ACTH), and a high-dose ACTH stimulation test (see "Clinical manifestations of adrenal insufficiency in adults" and "Diagnosis of adrenal insufficiency in adults"). Muscle disorders (in patients with symptoms such exercise intolerance, muscle pain, or muscle weakness): Creatinine kinase or aldolase (see "Inborn errors of metabolism: Epidemiology, pathogenesis, and clinical features", section on 'Clinical manifestations').
To confirm that an isolated elevation in the alkaline phosphatase is coming from the liver, a GGT level or serum 5'-nucleotidase level should be obtained. These tests are usually elevated in parallel with the alkaline phosphatase in liver disorders but are not increased in bone disorders. An elevated serum alkaline phosphatase with a normal GGT or 5'-nucleotidase should prompt an evaluation for bone diseases.
If the alkaline phosphatase elevation is isolated (ie, the other routine liver biochemical test levels are normal), is confirmed to be of hepatic origin, and persists over time, chronic cholestatic or infiltrative liver diseases should be considered (table 5). The most common causes include partial bile duct obstruction, primary biliary cholangitis (PBC), primary sclerosing cholangitis, and certain drugs, such as androgenic steroids and phenytoin. Infiltrative diseases include sarcoidosis, other granulomatous diseases, amyloidosis, and, less often, unsuspected cancer that is metastatic to the liver.
Acute or chronic elevation of the alkaline phosphatase in conjunction with other liver biochemical abnormalities may be due to extrahepatic causes (eg, bile duct stones, primary sclerosing cholangitis, malignant biliary obstruction) or intrahepatic causes (eg, PBC, primary sclerosing cholangitis, infiltrative disease). (See 'Extrahepatic cholestasis' below and 'Intrahepatic cholestasis' below.)
Rarely, an elevated alkaline phosphatase level is seen because of the presence of macro-alkaline phosphatase. Macro-alkaline phosphatase is due to the formation of complexes of alkaline phosphatase with immunoglobulins, which have reduced renal clearance compared with unbound alkaline phosphatase [37]. The clinical significance of these complexes is uncertain.
Conjugated (direct) hyperbilirubinemia — An isolated elevation in conjugated bilirubin is found in two rare inherited conditions: Dubin-Johnson syndrome and Rotor syndrome. Dubin-Johnson syndrome and Rotor syndrome should be suspected in patients with mild hyperbilirubinemia (with a direct-reacting fraction of approximately 50 percent) in the absence of other abnormalities of standard liver biochemical tests. Normal levels of serum alkaline phosphatase and GGT help to distinguish these conditions from disorders associated with biliary obstruction. Differentiating between these syndromes is possible but clinically unnecessary due to their benign nature. In children, other inherited disorders caused by mutations in one of a variety of bile salt transporters may need to be considered [39]. (See "Inherited disorders associated with conjugated hyperbilirubinemia".)
Patients with both conditions present with asymptomatic jaundice, typically in the second decade of life. The defect in Dubin-Johnson syndrome is altered hepatocyte excretion of bilirubin into the bile ducts, while Rotor syndrome is due to defective hepatic reuptake of bilirubin by hepatocytes [40].
Unconjugated (indirect) hyperbilirubinemia — Unconjugated hyperbilirubinemia may be observed in a number of disorders (table 6). These can be divided into disorders associated with bilirubin overproduction (such as hemolysis and ineffective erythropoiesis) and disorders related to impaired hepatic uptake or conjugation of bilirubin (such as Gilbert disease, Crigler-Najjar syndrome, and the effects of certain drugs). The evaluation typically involves evaluation for hemolytic anemia as well as obtaining a history to determine if the patient has Gilbert syndrome. In a patient with a history consistent with Gilbert syndrome (eg, the development of jaundice during times of stress or fasting), normal serum aminotransferase and alkaline phosphatase levels and mild unconjugated hyperbilirubinemia (<4 mg/dL), additional testing is not required [2]. Genetic testing can confirm the diagnosis in settings where there is diagnostic confusion. In patients with persistent or worsening unexplained unconjugated hyperbilirubinemia, symptomatic hyperbilirubinemia, or abnormal aminotransferases, a liver biopsy should be performed. (See "Gilbert syndrome and unconjugated hyperbilirubinemia due to bilirubin overproduction", section on 'Diagnosis'.)
MicrosCopic (Lymphocytic And Collagenous) Colitis
Microscopic colitis has a chronic, intermittent course in most patients
- Relapses are common (approximately 30 to 60 percent)
Check medications for those with an elevated level of likelihood to trigger microscopic colitis
Symptom control
- Continue use of loperamide
Treatment
- budesonide 9 mg daily for six to eight weeks followed by a taper
- taper oral budesonide to 6 mg for two weeks, followed by 3 mg for another two weeks, and then discontinue therapy
Other options with benefits:
- Cholestyramine 4 g four times per day
- Bismuth subsalicylate if cholestyramine doesn't improve symptoms
If refractory
- Biologic medications like infliximab or adalimumab) or immunomodulators like 6-mercaptopurine or azathioprine
- Surgery (ileostomy, colectomy) should be reserved for management of microscopic colitis that is refractory to medical therapy
Model for End-Stage Liver Disease (MELD Score) edit
| MELD score | Risk of mortality (3 mo) |
|---|---|
| Less than 9 | 1.9% |
| 10–19 | 6.0% |
| 20–29 | 19.6% |
| 30–39 | 52.6% |
| More than 40 | 71.3% |
Cirrhosis symptom treatment:
- diuretics to reduce excess fluid
- laxatives to help rid the system of toxins
- beta-blockers, to reduce portal hypertension
- using hardening agents to stop bleeding
- a shunt to reduce pressure
- liver transplant
Calculation of MELD Score: The MELD score, which estimates the survival probability of a patient with end-stage liver disease, is based on three commonly obtained laboratory tests: serum bilirubin, serum creatinine, and international normalized ratio (INR).
The MELD Calculator will compute the MELD score based on the numbers entered. In January 2016, the MELD scoring system for donor allocation in the United States was further modified to incorporate serum sodium, using the MELD-Na equation for patients with MELD scores greater than 11.
Clinical Use: The MELD score should be calculated on any person with cirrhosis or advanced liver disease at each clinic visit. Individuals with cirrhosis and a MELD score of 15 or greater should be referred for a liver transplantation evaluation
help slow down cirrhosis progression and avoid additional liver damage.
- Avoiding alcohol. Even if your cirrhosis isn't related to alcohol, it's best to abstain because alcohol can damage your liver, especially if it's already damaged.
- Limit salt. A cirrhotic liver has a hard time keeping fluid in the blood. Salt intake raises the risk of fluid overload. You don't have to eliminate it from your diet completely, but try to stay away from processed foods and avoid adding too much salt while cooking.
- Reduce your risk of infection. It's harder for a damaged liver to make proteins that help fight off infection. Wash your hands frequently and try to limit your contact with people who have any kind of active infection, from a common cold to the flu.
- Use over-the-counter drugs carefully. Your liver is the main processor of any chemicals or medications you consume. Make sure to tell your doctor about any over-the-counter medications, supplements, or herbs you use to make sure they aren't putting a burden on your liver.
- MELD Calculator 1
- MELD Calculator 2
NAFLD
Evaluation of NAFLD in Primary Care
- Calculate Fibrosis Score
- < -1.455: Low likelihood of nonalcoholic steatohepatitis
- Continue serial monitoring
- Reduce cardiometabolic risk
- -1.455 to 0.676: Intermediate
- Consider transient elastography (Fibroscan) and fibrosis biomarker measurements
- Low likelihood of nonalcoholic steatohepatitis
- Continue serial monitoring
- Reduce cardiometabolic risk
- High likelihood of nonalcoholic steatohepatitis
- Referral for liver biopsy
- Evaluation for sequelae of cirrhosis
- > 0.676: High likelihood of nonalcoholic steatohepatitis
- Referral for liver biopsy
- Evaluation for sequelae of cirrhosis
- < -1.455: Low likelihood of nonalcoholic steatohepatitis
NAFLD Index:
- http://www.mayoclinic.org/medical-professionals/model-end-stage-liver-disease/alcoholic-liver-disease-nonalcoholic-fatty-liver-disease-index
- Distinguish between alcoholic and non-alcoholic fatty liver disease
- ALT/AST
- Ht/Wt
- Mean corpuscular volume
- Sex
- Distinguish between alcoholic and non-alcoholic fatty liver disease
NAFLD fibrosis score:
- http://nafldscore.com
- Assess risk of hepatic fibrosis
- Age
- ALT/AST
- BMI
- DM or glucose intolerance
- Platelet count
- Serum Albumin
- Assess risk of hepatic fibrosis
References:
- AFP Vol 95 No 12 Jun 2017
- AFP Vol 96 No 11 Dec 2017
Diagnosis:
- Exclude alcohol as etiology
- EtOH history
- GGT - usually take 80g/d
- Carbohydrate-deficient transferrin
- Can exclude "excessive" EtOH
- AST/ALT ratio
- <1 for no EtOH
- Exclude other hepatiglides
- Viral A, B, C
- Autoimmune
- Hemochromatosis
- Wilson's
- Alpha 1-antitrypsin deficiency
- Image
- Test of choice = MRI
- If not available, then US or CT
- Consider liver biopsy
- Definitive diagnosis
- Refer if persistently elevated transaminases without identified etiology
References:
- FMX 2016
Hystological Types
| Type | Description | Significance |
|---|---|---|
| 1 | Simple steatosis | Early |
| 2 | With Inflammation | Early |
| 3 | With fibrosis | Risk of cirrhosis |
| 4 | Balloon cells and hyaline | Highest risk of cirrhosis |
References:
- FMX 2016
Treatment
- Weight Loss
- Exercise (LOE A)
- Diet
- Best diet is low carbohydrate diet (LOE B)
- Second best is Mediterranean diet (LOE B)
- Pharmacotherapt
- Must target Obesity and Insulin resistance
Lifestyle Management for NAFLD:
- Weight loss:
- Aim for 7%-10% body weight
- For those overweight or with obesity
- General nutrition:
- Low-fat to Mod-fat, Low-carb, or Mediterranean diet
- Fructose intake:
- Avoid fructose-containing beverages and foods
- High fructose intake is associated with NAFLD
- Physical activity:
- 150-200min/wk of moderate to vigorous exercise
- Vigorous activity may improve NAFLD over moderate activity
- Alcohol intake:
- Daily intake less than 30g for men and <20g for women
- Limiting EtOH intake may lower risk of NAFLD
- Coffee drinking:
- No liver-related limitations
- Coffee drinking may lower risk of NAFLD
References:
- FMX 2016
- JFP Vol 96 No 11 Dec 2017
Pancreatitis - Chronic
Chronic Pancreatitis Treatment Options:
- Medical
- Analgesics (stepwise approach)
- Antidepressants (treatment of concurrent depression)
- Cessation of alcohol and tobacco use
- Denervation (celiac nerve blocks, transthoracic splanchnicectomy)
- Insulin (for pancreatic diabetes)
- Low-fat diet and small meals
- Pancreatic enzymes with proton pump inhibitors or histamine H2 blockers
- Steroid therapy (in autoimmune pancreatitis)
- Vitamin supplementation (A, D, E, K, and B12)
- Endoscopic
- Extracorporeal shock wave lithotripsy with or without endoscopy
- Pancreatic sphincterotomy and stent placement for pain relief
- Transampullary or transgastric drainage of pseudocyst
- Surgical
- Decompression
- Cystenterostomy
- Lateral pancreaticojejunostomy (most common)
- Sphincterotomy or sphincteroplasty
- Resection
- Distal or total pancreatectomy
- Pancreatoduodenectomy (Whipple procedure, pylorus-preserving, duodenum-preserving)
- Not recommended
- Allopurinol
- Antioxidant therapy (vitamin C, vitamin E, selenium, methionine [no longer available in the United States])
- Octreotide (Sandostatin)
- Prokinetic agents (erythromycin)
References:
- AFP Vol 97 No 6 Mar 2018
Indications for surgery
- Biliary or pancreatic stricture
- Duodenal stenosis
- Fistulas (peritoneal or pleural effusion)
- Hemorrhage
- Intractable chronic abdominal pain
- Pseudocysts
- Suspected pancreatic neoplasm
- Vascular complications
References:
- AFP Vol 97 No 6 Mar 2018
Rectal Prolapse
Messaging
This condition is called rectal prolapse or procidentia. The recommendations are surgical repair as medical management only prolongs the inevitable and might allow muscles to weaken further.
Still, there are things you can do:
- Keep your bowel movements easy (avoid constipation or even minimally hard stools as well as straining)
- Ensure adequate fluid and fiber intake to
- Consume high-fiber foods and/or fiber supplements (total 25 to 30 grams per day)
- Drink 1 to 2 liters (or quarts) per day of water and other fluids
- Enemas and suppositories may be required for patients with severe constipation and difficulty evacuating the colon.
- Ensure adequate fluid and fiber intake to
- Perform Pelvic floor muscle exercises (Kegel's)
- Surgery
- Delay of surgical repair is not recommended, because of the eventual progression of symptoms, weakening of the sphincter muscle complex, and risk of incarceration.
- In general, it is recommended patients with procidentia should undergo a surgical consultation to determine operative eligibility
SIBO
See also:
Management:
- The treatment of small intestinal bacterial overgrowth (SIBO) primarily involves the use of antibiotics. According to the American College of Gastroenterology (ACG) guidelines, rifaximin is often considered the first-line treatment due to its efficacy and minimal systemic absorption. The typical dosage is 550 mg three times daily for 14 days.[1]
- Other antibiotics that have been used include amoxicillin-clavulanic acid, ciprofloxacin, metronidazole, tetracycline, and trimethoprim-sulfamethoxazole. The choice of antibiotic may depend on patient-specific factors, including antibiotic tolerance and previous antibiotic use.[1]
- The ACG guidelines emphasize the importance of confirming the diagnosis of SIBO before initiating antibiotic therapy to avoid unnecessary antibiotic use and the associated risks, such as the development of resistant bacteria and opportunistic infections like Clostridioides difficile.[1]
- Given the high recurrence rate of SIBO, retreatment with antibiotics may be necessary, although this practice is based on anecdotal evidence and expert opinion rather than robust clinical trials.[1]
- In addition to the recommendations from the American College of Gastroenterology (ACG), the American Gastroenterological Association (AGA) also provides guidance on the treatment of small intestinal bacterial overgrowth (SIBO). The AGA emphasizes that the treatment of SIBO is largely empirical due to the limited data available to guide antibiotic strategies. The primary goal of antibiotic therapy is to modulate the small intestinal microbiota to achieve symptomatic improvement rather than complete eradication of bacteria.[2]
- Rifaximin is frequently used due to its efficacy and minimal systemic absorption. A meta-analysis reported an overall 70% eradication rate for rifaximin in SIBO, with dosing ranging from 800 mg daily for 4 weeks to 1200 mg daily for 7 days. However, rifaximin is not FDA-approved for SIBO, which may affect insurance coverage.[2]
- Other antibiotics that have been used include amoxicillin-clavulanic acid, ciprofloxacin, doxycycline, metronidazole, neomycin, norfloxacin, tetracycline, and trimethoprim-sulfamethoxazole. The choice of antibiotic should consider patient-specific factors such as previous antibiotic use and tolerance.[2-3]
- For patients with intestinal methanogen overgrowth, a combination of neomycin and rifaximin has shown effectiveness in an uncontrolled trial.[2]
- Recurrence of SIBO after antibiotic treatment is common, occurring in up to 44% of patients within 9 months. This necessitates careful patient monitoring and potentially repeated courses of antibiotics.[2]
- In summary, the treatment of SIBO involves the use of antibiotics such as rifaximin, amoxicillin-clavulanic acid, and others, with the choice of antibiotic tailored to individual patient factors. The AGA guidelines highlight the empirical nature of treatment and the need for further research to establish standardized treatment protocols.
Reference:
- Pimentel M, Saad RJ, Long MD, Rao SSC. ACG Clinical Guideline: Small Intestinal Bacterial Overgrowth. The American Journal of Gastroenterology. 2020;115(2):165-178. https://doi.org/10.14309/ajg.0000000000000501.
- Quigley EMM, Murray JA, Pimentel M. AGA Clinical Practice Update on Small Intestinal Bacterial Overgrowth: Expert Review. Gastroenterology. 2020;159(4):1526-1532. https://doi.org/10.1053/j.gastro.2020.06.090.
- Rezaie A, Pimentel M, Rao SS. How to Test and Treat Small Intestinal Bacterial Overgrowth: An Evidence-Based Approach. Current Gastroenterology Reports. 2016;18(2):8. https://doi.org/10.1007/s11894-015-0482-9.
Transaminases
ALT and AST
- ALT most specific for hepatocyte injury
- AST:ALT >2 suggests Alcohol Liver disease
- AST:ALT >4 suggests possible Wilson's disease
- Step 1:
- History/Physical, Stop alcohol, eval medications, repeat labs in 2-4 wks
- Step 2:
- LFTs, Coags, CBC , albumin, viral serology, Ferritin, Fe, TIBC, fasting glucose, lipids
- Step 3:
- Avoid Hepatotoxins, Withdraw suspected medications
- Reduce hepatic Steatosis risks: Weight loss if Overweight, Improve glucose control, Treat Hyperlipidemia, Repeat LFTs in 2-6 months
- Obtain imaging as above if elevations persist
- Step 4:
- Obtain Ultrasound of right upper quadrant
- Obtain disease specific markers
- Complete initial labs from step 1
- Ceruloplasmin (Wilson's Disease)
- Antinuclear Antibody
- Anti-Smooth Muscle Antibody
- Alpha-1-antitrypsin
- Anti-tissue transglutaminase Antibody: Celiac Sprue
- Step 5:
- If testing as above is negative for specific cause:
- Aminotransferases exceed twice normal -> Refer to Gastroenterology for biopsy
- Aminotransferases mildly elevated -> Follow serial Aminotransferases (AST, ALT)
- If testing as above is negative for specific cause:
References:
- JAMA Vol 313, No 5 Feb 2015
Alkaline Phosphatase (marked) with normal transaminases:
- Confirm increase is due to gastrointestinal cause (e.g. as opposed to bone) with GGT (elevated if from liver) or fractionated Alkaline Phosphatase
- Cholestatic Liver Disease:
- Primary Sclerosing Cholangitis
- Primary Biliary Cirrhosis
- Infiltrative Conditions:
- Malignancy
- Amyloidosis
- Sarcoidosis
- Infectious disease
References:
- JAMA Vol 313, No 5 Feb 2015
Bilirubin elevation with normal transaminases:
- Predom conjugated (direct) hyperbilirubinemia:
- biliary obstruction
- Intrahepatic cholestasis
- Hepatocellular injury
- Dubin-Johnson syndrome
- Rotor syndrome
- Predom unconjugated (indirect) hyperbilirubinemia:
- Obtain:
- haptoglobin
- LDH
- If abnormal -> increased bilirubin production
- hemolysis
- dyserythropoiesis
- If normal and other medical problems
- Medications
- Portosystemic shunts
- If normal and no other medical problems
- Bilirubin <5mg/dL -> Gilbert syndrome
- Bilirubin >5mg/dL -> Other etiologies like Crigler-Najar syndrome
- Obtain:
Gilbert syndrome is in 5-10% of Western European population
References:
- JAMA Vol 313, No 5 Feb 2015
Causes of Mildly Elevated LFTs
Cause (prev cases/people)
- Common
- Metabolic dysfunction-associated steatotic liver disease (1/3)
- AST:ALT <0.8
- Alcoholic liver disease (1/15)
- AST:ALT >2
- Metabolic dysfunction-associated steatotic liver disease (1/3)
- Uncommon
- Chronic hepatitis C (1/80)
- Hepatitis C virus antibody testing
- Chronic hepatitis B (1/215)
- Hepatitis B surface antigen
- Hereditary hemochromatosis (1/250)
- Drug induced liver injury (1.39-1.9/10000)
- Chronic hepatitis C (1/80)
- Rare
- Alpha1-antitrypsin deficiency (1/2,500)
- Autoimmune hepatitis (1/6000)
- Wilson disease (1/30000)
Reference:
- Dec 2024 Vol 110 No 6
Gallstone Diet Patient Instructions
Here are helpful evidence based tips for those with gallstones:
If you have gallstones, making some changes to your diet may help reduce your symptoms and lower the risk of complications. While surgery is often needed for ongoing or severe symptoms, the following dietary tips are supported by current medical knowledge and may help you feel better:
- Eat Regular, Balanced Meals
- Try not to skip meals or fast for long periods. Long overnight fasting (more than 12 hours) may increase the risk of gallstone problems.
- Eat smaller, more frequent meals if possible.
- Limit Saturated Fats and Fried Foods
- Foods high in saturated fat (like fatty cuts of meat, butter, cream, cheese, and fried foods) can trigger symptoms in some people and are linked to a higher risk of gallstones.
- Choose lean meats, skinless poultry, and low-fat dairy products.
- Choose Healthy Fats in Moderation
- Use small amounts of healthy fats, such as olive oil or canola oil, instead of butter or lard.
- Avoid very low-fat diets unless advised by your doctor, as some fat is needed for normal gallbladder function.
- Increase Fiber Intake
- Eat more fruits, vegetables, whole grains, and legumes. Fiber helps with digestion and may lower the risk of gallstone formation. Examples: apples, berries, broccoli, carrots, brown rice, oats, beans, and lentils.
- Limit Refined Sugars and Simple Carbohydrates
- Cut back on foods and drinks high in sugar, such as soda, candy, pastries, and white bread. High intake of refined sugars is linked to a higher risk of gallstones.
- Stay Hydrated
- Drink plenty of water throughout the day.
- Other Notes:
- Moderate coffee and alcohol intake may be protective, but these are not recommended for everyone
Foods to Choose:
- Fresh fruits and vegetables
- Whole grains (brown rice, whole wheat bread, oats)
- Lean proteins (chicken, turkey, fish, beans)
- Healthy fats (olive oil, nuts, avocados—in moderation)
Foods to Limit or Avoid:
- Fried foods, fatty meats, processed meats (sausage, bacon)
- Full-fat dairy products (cream, cheese, ice cream)
- Baked goods and snacks high in sugar and fat (cookies, cakes, chips)
- Sugary drinks (soda, sweetened juices)
Let me know immediately if you have severe abdominal pain, fever, yellowing of the skin or eyes, or vomiting. Go to the Emergency Department if you are concerned.
References:
- Modified Dietary Fat Intake for Treatment of Gallstone Disease in People of Any Age. Madden AM, Smeeton NC, Culkin A, Trivedi D. The Cochrane Database of Systematic Reviews. 2024;2:CD012608. https://doi.org/10.1002/14651858.CD012608.pub3.
- The Role of Diet in the Pathogenesis of Cholesterol Gallstones. Di Ciaula A, Garruti G, Frühbeck G, et al. Current Medicinal Chemistry. 2019;26(19):3620-3638. https://doi.org/10.2174/0929867324666170530080636.
- Association of Dietary Quality Indicators With Gallstones in the US: NHANES 2017-2020. Wu W, Pei Y, Wang J, Liang Q, Chen W. BMC Public Health. 2025;25(1):976. https://doi.org/10.1186/s12889-025-21783-8.
- Diet and Gallstones in Italy: The Cross-Sectional MICOL Results. Attili AF, Scafato E, Marchioli R, Marfisi RM, Festi D. Hepatology (Baltimore, Md.). 1998;27(6):1492-8. https://doi.org/10.1002/hep.510270605.
- Dietary Intake and Gallbladder Disease: A Review. Tseng M, Everhart JE, Sandler RS. Public Health Nutrition. 1999;2(2):161-72. https://doi.org/10.1017/s136898009900021x.
- Cholelithiasis: Presentation and Management. Littlefield A, Lenahan C. Journal of Midwifery & Women's Health. 2019;64(3):289-297. https://doi.org/10.1111/jmwh.12959.
- Diet as a Risk Factor for Cholesterol Gallstone Disease. Cuevas A, Miquel JF, Reyes MS, Zanlungo S, Nervi F. Journal of the American College of Nutrition. 2004;23(3):187-96. https://doi.org/10.1080/07315724.2004.10719360.
- Diet, Physical Activity, and Gallstones–a Population-Based, Case-Control Study in Southern Italy. Misciagna G, Centonze S, Leoci C, et al. The American Journal of Clinical Nutrition. 1999;69(1):120-6. https://doi.org/10.1093/ajcn/69.1.120.
- Ursodeoxycholic Acid and Diets Higher in Fat Prevent Gallbladder Stones During Weight Loss: A Meta-Analysis of Randomized Controlled Trials. Stokes CS, Gluud LL, Casper M, Lammert F. Clinical Gastroenterology and Hepatology : The Official Clinical Practice Journal of the American Gastroenterological Association. 2014;12(7):1090-1100.e2; quiz e61. https://doi.org/10.1016/j.cgh.2013.11.031.
- Gallstones: Prevention, Diagnosis, and Treatment. Lammert F, Wittenburg H. Seminars in Liver Disease. 2024;44(3):394-404. https://doi.org/10.1055/a-2378-9025.
- Recent Advances in Understanding and Managing Cholesterol Gallstones. Di Ciaula A, Portincasa P. F1000Research. 2018;7:F1000 Faculty Rev-1529. https://doi.org/10.12688/f1000research.15505.1.
Low FODMAP Apps
- Fig: Food Scanner & Discovery
- Low FODMAP diet A to Z
- Fast FODMAP Lookup & Learn
Geriatrics
Geriatric 5 M's:
- Mind
- Mentation
- Dementia
- Delerium
- Depression
- Mobility
- Impaired gait and balance
- Fall injury prevention
- Medications
- Polypharmacy
- De-prescribing
- Optimal prescribing
- Adverse medication effects and medication burden
- Multi-complexity
- Multi-morbidity
- Complex bio-psycho-social situations
- Matters most
- Each individual's own meaningful health outcome goals and care preferences
Time to benefit of key interventions:
- alendronate
- Non-vertebral fractures
- Estimated time to benefit: 1 year
- Antihypertensives
- Lower systolic blood pressure to less than 140 mmHg to prevent major adverse cardiovascular events
- Estimated time to benefit: 1-2 year
- Statins
- Prevent major cardiovascular events
- Estimated time to benefit: 2.5 years
Reference:
- AFP Vol 109 No 6 Jun 2024
- AFP Vol 113 No 1 Jan 2026
Constipation in Elderly
Also See: Constipation in Gastroenterology
Treatment:
- Lifestyle modifications:
- Scheduled toileting after meals
- Increased fluid intake
- Increased dietary fiber intake
- Additional fiber intake:
- Forms of polycarbophil, methylcellulose, or psyllium may improve symptoms.
- Fiber intake should be slowly increased over several weeks to decrease adverse effects.
- The next step: an osmotic laxative:
- Such as polyethylene glycol
- Then a stool softener:
- Such as docusate sodium
- Then stimulant laxatives
- Long-term use of magnesium-based laxatives should be avoided because of potential toxicity.
References:
Delirium
Treatment:
- Avoid sensory deprivation (provide eyeglasses, hearing aids..)
- Restore normal sleep/wake cycle
- Encourage patient to resume wlaking as soon as possible
- Prevent/treat dehydration
- Provide nonthreatening cognitive stimulation
- Prevent/treat constipation
- Involve family in patient care
- Provide adequate nutrition
- Reorient patient to place and time (provide clocks/calendars)
Strategies for preventing delirium near the end of life
- Correct nonmedication cause
- Give supplemental oxygen as needed
- Treat severe pain
- Prevent bladder retention, but minimize catheterization
- Ensure bowel function
- Encourage mobilization
- Correct medication cause
- Minimize benzodiazepines, anticholinergics, antihistamines
- Eliminate drug interactions; dose for renal/hepatic limits
- Normalize sleep-wake cycle
- Have interior lighting follow time of day
- Reduce stimulation at night
- Reorientation
- Encourage appropriate use of glasses/hearing aids
- Display a clock and other cues of date
- Keep communication clear and consistent
- Identify staff contacts for continuity/familiarity
- Encourage calm reassurance from family members
References:
- JFP Vol 64, No 6 Jun 2015
- JFP Vol 68 No 8 Oct 2019
Common Causes
- Metabolic derangements (hypoglycemia, etc)
- Infection
- Toxic effects of drugs/EtOH
- Withdrawal states
- Fluid and electrolyte disorders
- Primary brain disorders
- Low perfusion states
- Physical disorders
- Postoperative states
- Reactions to medicines
References:
- NEJM 367;25 Dec 2012
Pharmacology
- Haloperidol 0.5-1mg
- First line - Agent of choice
- Avoid IV use due to short duration of action
- Associated with increased mortality in older patients with dementia related psychosis
- Olanzapine (Zyprexa) 2.5mg
- Associated with increased mortality in older patients with dementia related psychosis
- Quetiapine (Seroquel) 25mg
- Associated with increased mortality in older patients with dementia related psychosis
- Risperidone 0.5mg
- Associated with increased mortality in older patients with dementia related psychosis
- Lorazepam 0.5-1mg
- May worsen delerium
- Trazodone 25-150mg
- Second line agent
- Associated with increased mortality in older patients with dementia related psychosis
References:
- AFP Vol 90 No 3 Aug 2014
Clinical Featurs of Diseases that Mimic Delerium
| Feature | Delirium | Dementia | Depression | Psychosis |
|---|---|---|---|---|
| Acute change in mental status | + | - | - | +/- |
| Inattention | + | +/- | +/- | +/- |
| Altered consciousness | + | - | - | - |
| Disorganized thinking | + | +/- | + | + |
| Altered psychomotor activity | + | +/- | + | + |
| Chronic duration | +/- | + | + | +/- |
References:
- JAMA Vol 318 No 12 Sep 2017
Dementia
| Major neurocognitive disorder | Minor neurocognitive disorder |
| Significant cognitive decline in at least one cognitive domain as seen in both of the following: | Modest cognitive decline in at least one cognitive domain as seen in both of the following: |
| - Concerns expressed by the patient or reliable informant or as seen by the clinician | - Concerns expressed by the patient or reliable informant or as seen by the clinician |
| - Objective neurocognitive testing/assessments | - Objective neurocognitive testing/assessments |
| Interference with instrumental activities of daily living | Does not interfere with instrumental activities of daily living, but they require additional time and effort |
- Cannot occur exclusively during bouts of delirium
- Cannot be explained by another mental disorder
- Specify one or more causal subtypes
- Alzheimer disease
- Lewy body dementia
- Traumatic brain injury
- Frontotemporal lobar
- Parkinson disease
- Vascular disease
- Human immunodeficiency virus infection
- Prion disease
- Other medical condition
- Huntington disease
- Substance/medication use
- Multiple etiologies
| Cognitive domain | Symptoms and observations |
|---|---|
| Executive function | Difficulty in completing previously familiar multistep tasks, such as preparing a meal; no longer wanting to participate in activities of the home; difficulty in completing activities or tasks because of easy distractibility; social outings become more taxing and less enjoyable |
| Language | Difficulty finding the correct words; using general pronouns regularly instead of names; mispronunciation of words; problems with understanding verbal and written communication |
| Learning and memory | Forgetting to buy items or buying the same items multiple times at the store; repetition in conversations; difficulty in recalling recent events; relying on lists of tasks to complete; forgetting to pay bills |
| Perceptual-motor | Difficulty in using familiar technology, tools, or kitchen appliances; getting lost in familiar environments |
| Social cognition | Apathy, increase in inappropriate behaviors, loss of empathy, impaired judgment |
| Suggested etiology | Key findings on history and examination |
|---|---|
| Delirium | Recent hospitalization or acute illness, inattention, fluctuating behavior changes, altered level of consciousness |
| Frontotemporal dementia | Socially inappropriate behaviors; loss of empathy; changes in dress, eating habits, religious/political beliefs; development of compulsive behaviors; progressive aphasia |
| Human immunodeficiency virus infection | History of high-risk sexual behavior or drug use, apathy, poor attention and concentration, hyperreflexia, slow limb movements |
| Hypoperfusion from heart failure | Syncope, history of heart failure |
| Intracranial tumor | Seizures, neurologic deficits |
| Medication adverse effects | Use of anticholinergic drugs, benzodiazepines, opioids, or muscle relaxants |
| Neurocognitive disorder with Lewy body dementia | Daytime drowsiness, daytime naps lasting more than two hours, prolonged staring spells, disorganized speech, visual hallucinations, parkinsonian symptoms |
| Vascular dementia | History of symptoms beginning after cerebrovascular events |
| Other medical conditions | |
| - Depression | Anhedonia, feelings of worthlessness, slowed speech, flat affect, sleep disturbance |
| - Hypothyroidism | Fatigue, cold intolerance, constipation, weight gain, dry skin, prolonged deep tendon reflexes, myalgias |
| - Neurosyphilis | History of high-risk sexual behavior or injection drug use, vision and hearing loss, decreased proprioception, stabbing extremity pains |
| - Niacin/vitamin B3 deficiency | History of bariatric surgery or malabsorption disorders, photosensitive rash, anxiety, insomnia, diarrhea, vomiting |
| - Normal-pressure hydrocephalus | Urinary incontinence and broad-based, shuffling gait |
| - Vitamin B12 deficiency | Ascending paresthesias, tongue soreness, limb weakness, weight loss |
| - Wernicke-Korsakoff syndrome | History of alcoholism, nystagmus or extraocular muscle weakness, broad-based gait and stance |
Dementia Work Up
The most common neurodegenerative conditions causing dementia are:
- Alzheimer disease (AD)
- Dementia with Lewy bodies
- Frontotemporal dementia
- Parkinson disease dementia
Less common neurodegenerative disorders such as progressive supranuclear palsy (PSP), corticobasal degeneration (CBD), multisystem atrophy, and Huntington disease can also be associated with dementia.
Non-neurodegenerative dementias may be reversible, or progression slowed or halted, if the underlying cause can be identified and adequately treated [7]. The most common of these is: Vascular dementia
Forgetfulness is the most common chief complaint; in addition, patients with dementia also have difficulty with one or more of the following [11]:
- Retaining new information (eg, trouble remembering events)
- Handling complex tasks (eg, balancing a checkbook)
- Reasoning (eg, unable to cope with unexpected events)
- Spatial ability and orientation (eg, getting lost in familiar places)
- Language (eg, word finding)
- Behavior
Workup:
- Patients with cognitive complaints should undergo a careful mental status examination.
- All patients being evaluated for cognitive impairment or dementia should be screened for depression
Labs
Check these labs:
- Complete blood cell count (CBC)
- Serum chemistry panel and Serum electrolyte levels, including liver function tests (CMP)
- Magnesium (Mg)
- Thyroid function tests (TSH)
- Hemoglobin A1c
- Serum vitamin B12
- Urinalysis and microscopy
Consider these:
- Erythrocyte sedimentation rate*
- Serologic tests for syphilis (or similar)*
- HIV*
- Chest radiography*
- Electrocardiography*
- Toxicology screening*
- Urine toxicology
*—To be considered, not universally needed.
https://www.aafp.org/afp/2018/0315/p398.html https://www.aafp.org/afp/2011/1015/p895.html
Imaging
Neuroimaging with a head computed tomography (CT) or magnetic resonance imaging (MRI) scan is unequivocally indicated in patients with acute onset of cognitive impairment and/or rapid neurologic deterioration.
AAN recommends structural neuroimaging with either a noncontrast head CT or MRI in the routine initial evaluation of all patients with dementia order imaging when patients present with unusual or atypical findings or when imaging findings may be reassuring for patients and families. Such differences in practice may be attributable to the context in which the patient is seen
MRI is preferred over CT because it is more sensitive for a broad range of potential pathologies while avoiding exposure to potentially harmful ionizing radiation
Magnetic resonance imaging without contrast media is the preferred imaging test to exclude other intracranial abnormalities, such as stroke, subdural hematoma, normal-pressure hydrocephalus, or a treatable mass. LOE C
https://www.aafp.org/afp/2018/0315/p398.html
Diagnosis
- Evidence from the history and clinical assessment that indicates significant cognitive impairment in at least one of the following cognitive domains:
- Learning and memory
- Language
- Executive function
- Complex attention
- Perceptual-motor function
- Social cognition
- The impairment must be acquired and represent a significant decline from a previous level of functioning
- The cognitive deficits must interfere with independence in everyday activities
- The disturbances are not occurring exclusively during the course of delirium
- The disturbances are not better accounted for by another mental disorder (eg, major depressive disorder, schizophrenia)
References:
- AFP Vol 97 No 6 Mar 2018
As fitness improves, Alzheimer's risk decreases
Study:
- 649605 Veterans
- Mean age: 61yo
- Fit determined with GXT and peak METS achieved
- Lowest: 3.8 METS - Developed ADRD at rate of 9.5/1000 person years
- Low: 5.8 METS
- Mod: 7.5 METS
- Fit: 9.2 METS
- Highest: 11.7 METS - Developed ADRD at rate of 6.4/1000 person year
| Fitness group | Adjusted hazard ratio (95% confidence interval) |
|---|---|
| Low fit | 0.87 (0.85-0.90) |
| Mod fit | 0.80 (0.78-0.83) |
| Fit | 0.74 (0.72-0.76) |
| Highest Fit | 0.67 (0.65-0.70) |
Reference:
- MDedge May 2022
- https://doi.org/10.55788/ede71ed1
Alzheimer Dementia
10 Warning Signs:
- Memory loss that disrupts daily life
- Challenges in planning or solving problems
- Difficulty completing familiar tasks
- Confusion with time or place
- Trouble understanding visual images or spacial relationships
- New problems with words in speaking or writing
- Misplacing things and losing the ability to retrace steps
- Decreased or poor judgement
- Withdrawal from work or social activities
- Changes in mood and personality
Diagnostic criteria:
- Cognitive or behavioral symptoms that
- Interfere with ability to function
- Represent a decline from previous levels of functioning and
- Are not explained by delerium or major psychiatric disorder
- Cognitive impairment diagnoses through
- history by patient/informant and
- bedside mental status exam or neuropsychological testing
- Cognitive or behavioral impairment involving 2 or more of the following:
- ability to acquire and remember new information
- reasoning, judgement, and handling of complex tasks
- visuospatial abilities
- language function
- personality or behavior
Patients must also meet:
- Dementia must have insidious onset and
- have worsening course
Nonpharmacologic Therapies for Management
- Enjoyable leisure activities
- Mental stimulation programs (puzzles, word games, past/reminiscence therapy, indoor gardening, baking)
- Occupational therapy training in coping strategies and cognitice aids
- Structured physical exercise programs
References:
- JFP Vol 64 No 1 Jan 2015
- AFP Vol 95 No 12 Jun 2017
- Differentiate Alzeheimer Disease from Depression
Alzeheimer Dementia Depression Behavior congruent with deficits Usual Unusual Delusions Mood independent Mood congruent Emotional reaction Variable Marked distress Mood disorder Environmentally responsive Persistent Pt report of deficits Variable Abundant Psychiatric history Unusual Usual Symptom duration Long Short Symptom progression Slow Rapid Valuation of accomplishments Variable Minimized References:
- AFP Vol 82 No 5 Sep 2010
- Treatment
BLUF:
- Mild-Mod: Start with donepezil or transdermal rivastigmine
- Mod-Severe: Combination of donepezil and memantine
Non-pharmacologic
- Physical exercise - 30-45min of cardio, 4-5d/wk
- Cognitive exercises - reading, puzzles, social games, learning
- Social stimulation - weekly social activities
- Diet - Mediterranean diet, nuts
Pharmacologic:
- Symptom Control
- Acetylcholinesterase Inhibitors: If causing vivid dreams/nightmares, try taking it in AM
- Donepezil
- Rivastigmine
- Galantamine
- NMDA Receptor Antagonist:
- Memantine
- Acetylcholinesterase Inhibitors: If causing vivid dreams/nightmares, try taking it in AM
- Disease Modifying
- lecanemab
- Dosing - starting dose is 10 mg/kg IV over 1 hour every 2 weeks for 18 months, then continued every 2 weeks or switched to once monthly for maintenance
- Surveillance – Obtain an MRI prior to the 5 th, 7th and 14th infusions to monitor for ARIA. No additional MRIs after this unless symptoms occur.
- donanemab
- Dosing - dosed at 700 mg every 4 weeks for 3 infusions, then 1400 mg every 4 weeks; data beyond 76 weeks are lacking on long-term benefit.
- Surveillance - Obtain an MRI prior to the 2nd, 3rd, 4th, and 7th infusions
- lecanemab
References:
- Consultant Dec 2016
- AFP Vol 111 No 4 Apr 2025
- Winter FAFP 2025
- Biomarkers
Fluid based biomarkers (Blood and CSF) • Aβ42/Aβ40 • p-tau 217, p-tau 181, p-tau 231 • NfL • GFAP
Imaging based biomarkers • Amyloid PET • Tau PET
Reference:
- FAFP Winter 2025
Cognition Assessment Tools
Assess Cognition:
- Language functions
- Naming, reading, writing
- Visuospatial ability
- Copying a figure; drawing the face of a clock
- Abstract reasoning
- Explainig proverbs; describing similarities (like an apple with a pear)
- Executive functions
- List making (name as many animals in 1min); drawing the face of a clock
- General intellectual level/fund of knowledge
- Identify the previous 5 presidents
- Attention to concentration
- Spell "world" forward and backward; subtract serial 7's from 100
- Memory (screening tools)
- GPCOG
- Mini-cog
- http://www.alz.org/documents_custom/minicog.pdf
- 91% Sensitivity; 86% Specificity
- Assesses executive functioning, memory, and visuospatial proficiency
- MMSE
- 81% Sensitivity; 89% Specificity
- Assesses attention, language, memory, orientation, and visuospatial proficiency
- Addenbrooke's Cognitive Examination
- http://www.stvincents.ie/dynamic/File/Addenbrookes_A_SVUH_MedEl_tool.pdf
- 92% Sensitivity; 89% Specificity
- Assesses attention, executive functioning, language, memory, orientation, and visuospatial proficiency
- Montreal Cognitive Assessment
- http://www.mocatest.org (free registration required)
- 91% Sensitivity; 81% Specificity
- Assesses attention, executive functioning, language, memory, and orientation
- Saint Louis University Mental Status (SLUMS) Exam
- Tests:
- Q1-Q3: Attention, immediate recall, and orientation
- Q4 and Q7: Delayed recall with interference
- Q5: Numeric calculation and registration
- Q6: Memory: immediate recall with interference (time constraint)
- Q8: Registration and digit span
- Q9: Visual spatial
- Q10: Visual spatial and executive function
- Q11: Executive function plus extrapolation
- Tests:
References:
- AFP Vol 80 No 8 Oct 2009
- AFP Vol 94 No 8 Oct 2016
- AFP Vol 97 No 6 Mar 2018
- https://www.slu.edu/medicine/internal-medicine/geriatric-medicine/aging-sucessfully/assessment-tools/mental-status-exam.php
- AFP Dec 2023 Vol 108 No 6
- SLU Mental Status
Poss pts Question Score 1 What day of the week is it? 1 1 What is the year? 1 1 What state are we in? 1 Please remember these five objects. I will ask you what they are later. - - Apple, Pen, Tie, House, Car - 3 You have $100 and you go to the store and buy a dozen apples for $3 and a tricycle for $20. - How much did you spend? 1 - How much do you have left? 2 3 Please name as many animals as you can in one minute. 0 - 0-4 1 - 5-9 2 - 10-14 3 - 15+ 5 What were the five objects I asked you to remember? 1 point for each one correct. 2 I am going to give you a series of numbers and I would like you to give them to me backwards. For example, if I say 42, you would say 24. 0 - 87 1 - 648 1 - 8537 4 This is a clock face. Please put in the hour markers and the time at ten minutes to eleven o'clock. 2 - Hour markers okay 2 - Time correct 1 Please place an X in the triangle. 1 1 Which of the above figures is largest? 1 8 I am going to tell you a story. Please listen carefully because afterwards, I'm going to ask you some questions about it. Jill was a very successful stockbroker. She made a lot of money on the stock market. She then met Jack, a devastatingly handsome man. She married him and had three children. They lived in Chicago. She then stopped work and stayed at home to bring up her children. When they were teenagers, she went back to work. She and Jack lived happily ever after. - What was the female's name? 2 - What work did she do? 2 - When did she go back to work? 2 - What state did she live in? 2 Scoring:
High school education Less than High School Education 27-30 Normal 25-30 21-26 Mild Neurocognitive Disorder 20-24 1-20 Dementia 1-19 Reference:
- Mini-Cognitive Assessment Instrument (Mini-Cog)
- Step 1 - Ask the patient to repeat 3 unrelated words (such as "ball," "dog," and "television")
- Step 2 - Ask the patient to draw a simple clock set to 10 min after 11 o'clock (11:10). A correct response is a drawing of a circle with all of the numbers placed in approximately the correct positions, with the hands pointing to the 11 and 2.
- Step 3 - Ask the patient to recall the 3 words from step 1. One point is given for each item recalled correctly.
Interpretation:
Number recalled Clock test Interpretation of screen for dementia 0 Normal Positive 0 Abnormal Positive 1 Normal Negative 1 Abnormal Positive 2 Normal Negative 2 Abnormal Positive 3 Normal Negative 3 Abnormal Negative Reference:
- Int J Geriatr Psychiatry. 2000;15(11):1021-1027
Tests
- Mini-Cog
The Mini-Cog combines free recall of three unrelated words (presented verbally) and a version of the CDT, which is dichotomously scored as normal (all numbers present in correct sequence with the hands correctly displaying the specified time) or abnormal [20]. Mini-Cog performance is judged to be impaired if patients are unable to recall any of the three words or if they recall only one or two words and have an abnormal clock drawing.
In primary care settings, the Mini-Cog has demonstrated reasonable sensitivity (76 to 100 percent) but relatively poorer specificity (54 to 85 percent) for identifying patients with dementia
- The General Practitioner Assessment of Cognition
The General Practitioner Assessment of Cognition (available for free at http://gpcog.com.au) comprises a patient screen and, if necessary, an informant component. Advantages of this test include validation in the primary care setting, little to no education bias, and availability in multiple languages.34 It has been studied only in Australian populations, however. The patient screen consists of recall, time orientation, clock drawing, and information components. The patient screen takes less than four minutes to complete, and the informant portion takes less than two minutes. The General Practitioner Assessment of Cognition has a sensitivity of 85% and specificity of 86%.34
- Saint Louis University Mental Status Examination (SLUMS)
Like the MMSE and MoCA, the SLUMS is scored on a 30-point scale, with questions that assess orientation, calculation, semantic verbal fluency, word and story recall, reverse digit span, clock-drawing, and visuospatial function. Because this instrument includes items that more directly measure executive function, it has demonstrated better discriminability than the MMSE for MCI [68-70].
The SLUMS form specifies different thresholds for identifying MCI (<25 points if <12 years of education, <27 points if ≥12 years of education) and dementia (<20 points if <12 years of education, <21 points if ≥12 years of education) [68]. However, across patient cohorts, a range of optimized cutoffs has emerged, yielding sensitivities of 67 to 98 percent and specificities of 61 to 87 percent for MCI and sensitivities of 84 to 100 percent and specificities of 87 to 100 percent for dementia [68-72]. Relative to the MMSE and MoCA, the SLUMS has far fewer published studies that examine its utility. More research may be required to further validate consensus cutoff points for normal cognition, MCI, and dementia.
What does the SLU Mental Status Exam Test Do?
- Q1-Q3: Attention, immediate recall, and orientation
- Q4 and Q7: Delayed recall with interference
- Q5: Numeric calculation and registration
- Q6: Memory: immediate recall with interference (time constraint)
- Q8: Registration and digit span
- Q9: Visual spatial
- Q10: Visual spatial and executive function
- Q11: Executive function plus extrapolation
Instructions:
- Read the questions aloud clearly and slowly to the examinee. It is not usually necessary to speak loudly but it is necessary to speak slowly.
- On question No. 4, read the statement as listed on the exam. Ask the patient to repeat each of the five objects (apple, pen, tie, house, car) that you recite to make sure that the patient heard and understood what you said. Repeat them as many times as it takes for the patient to repeat them back to you correctly.
- On question No. 5, make sure the patient is focused on you prior to reciting the information. Obtain an answer for the first part of the question ("How much did you spend") before moving on to part two ("How much do you have left?"). Do not prompt or give hints, but do give ample time to the patient to answer the questions. If the patient asks you to repeat the question you may do so once.
- Redirect the patient's attention if necessary back to you to answer question No. 6. Give them one minute to complete the question. Be sure to time them.
- On question No. 8, state each number by its individual name. 87 is pronounced eight, seven; 649 is pronounced six, four, nine; 8537 is pronounced eight, five, three, seven.
- On question No. 9, either draw a large circle on the back of the examination form or provide the patient with a separate piece of paper with a larger circle printed on it and attach it to the original examination form. When scoring, give full credit for either all 12 numbers or all 12 ticks. If the patient puts only four ticks on the circle, prompt them once to put numbers next to those ticks (12, 3, 6 and 9) for full credit. When scoring the correct time, make sure the hour hand is shorter than the minute hand and that the minute hand points at the 10 and the hour hand points at the 11.
- You may also provide a separate sheet with larger examples of the forms listed on question No. 10 for those with vision impairment. This sheet should be created by enlarging the figures on the examination form and can also be attached to the original form.
- Read question No. 11 as written, and provide ample time to answer each question. Do not repeat the story but do make sure they are paying attention the first time you read it to them. Do not prompt or give hints. The answer of Chicago as the state she lives in gets no credit but you may prompt them once by repeating the question.
- Memory Impairment Screen (MIS)
The MIS focuses on memory, both recall and recognition [19]. Patients are presented four written words (all nouns), which belong to different semantic categories (eg, "checkers" is a game, a "saucer" is a dish). They read the words aloud and, when given a category cue, identify the word that belongs in that category. After three minutes of distraction, patients are asked to recall the items; category cues are used for items not freely recalled. The total score is calculated as 2 x (number of items freely recalled) + (number of items recalled with cue) [20].
Across studies, a score of ≤4 identifies individuals with dementia with variable sensitivity (43 to 86 percent) but better specificity (93 to 97 percent) [21]. Given its specific emphasis on memory, the MIS is best suited for screening for Alzheimer disease (AD) and less sensitive for other forms of dementia, especially at their early stages [22]. Age, gender, and educational level do not impact test performance
https://www.alz.org/media/Documents/memory-impairment-screening-mis.pdf
- Six-Item Screener (SIS)
The SIS incorporates three memory questions and three orientation questions [24]. Patients are read three words and asked to repeat them; repetition of these items is not scored. They are then asked three temporal orientation questions (year, month, day of the week), which are scored. As with the MIS, three minutes of distraction then intervene before the patient is asked to recall the three words; recall of these items is scored.
Further diagnostic workup for possible cognitive impairment is indicated if the patient incorrectly answers ≥2 of the 6 combined orientation and memory questions.
https://aims.uw.edu/care-partners/sites/default/files/Callahan%20Six-Item%20Screener_1.pdf
- Clock-Drawing Test (CDT)
The CDT, which does not explicitly draw upon memory function, fulfills many of the requirements for an effective screening tool: convenient administration and scoring; applicability to a wide range of patients, irrespective of language, education, or cultural background; and high inter-rater reliability, test-test reliability, sensitivity, and specificity [27]. Patients are verbally asked to draw an analog clock, including all of the numbers, and set the hands to a specified time (eg, 10 minutes past 11:00). Performance on the CDT is supported by a combination of visuospatial abilities, executive function, motor execution, attention, language comprehension, and numerical knowledge.
However, no single scoring system is clearly superior for dementia screening, and a simple subjective qualitative interpretation of the clock drawing as "normal" or "abnormal" may suffice (See Mini-Cog)
Prevent Cognitive Decline
Epidemiologic evidence suggests that when combined, these risk factors are responsible for 40% of dementia cases worldwide:
- Hypertension
- A systematic review and meta-analysis of 7 studies found that systolic BP >160 mm Hg was associated with a 25% increase in risk for Alzheimer disease. Systolic BP >140 mm Hg was associated with an 18% increased risk.
- Less education
- In general, studies find higher educational attainment to be protective against cognitive decline in older adults
- A meta-analysis including 13 longitudinal studies found that low educational level (≤8 years) increased risk for dementia or cognitive impairment by 1.8 times
- Smoking
- smoking is the third most important modifiable risk factor for dementia, behind hypertension and less education.
- A recent meta-analysis involving >900 000 cases showed that whereas smokers clearly had an increased risk of dementia, quitting smoking decreased that risk to close to the level of never smokers
- Air pollution
- Alcohol misuse
- Depression
- Depression appears to be a risk factor for dementia, yet dementia is also a risk factor for depression in older age
- Diabetes Mellitus
- Hearing Loss
- In a meta-analysis of 36 cross-sectional and longitudinal studies, age-related hearing loss was associated with both cognitive impairment and dementia
- Hyperlipidemia
- Obesity
- Physical inactivity
- Social isolation
- Social isolation is defined as having little or no social contact or a diminished social network; loneliness is the subjective feeling related to isolation
- Traumatic brain injury
This is what has evidence to help with cognitive decline:
- Physical Activity - 30-45min of cardio, 4-5d/wk
- Cognitive Exercises - Reading, puzzles, social games, learning
- Social stimulation - Weekly social activities
- Diet - A Mediterranean diet is recommended
Life's Simple 7 (Modifiable risk factors for cognitive decline):
- Blood Pressure Control
- No Smoking
- Regular Physical Activity
- Reduce Diabetes Risk
- Healthy Diet
- Weight Control
- Lipid Control
Reference:
- Am Fam Physician. 2022;105(1):13-14
Study: A Primary Care Agenda for Brain Health
A healthy brain is critical for living a longer and fuller life. The projected aging of the population, however, raises new challenges in maintaining quality of life. As we age, there is increasing compromise of neuronal activity that affects functions such as cognition, also making the brain vulnerable to disease. Once pathology-induced decline begins, few therapeutic options are available.
Prevention is therefore paramount, and primary care can play a critical role. The purpose of this American Heart Association scientific statement is to provide an up-to-date summary for primary care providers in the assessment and modification of risk factors at the individual level that maintain brain health and prevent cognitive impairment.
Building on the 2017 American Heart Association/American Stroke Association presidential advisory on defining brain health that included "Life's Simple 7," we describe here modifiable risk factors for cognitive decline, including depression, hypertension, physical inactivity, diabetes, obesity, hyperlipidemia, poor diet, smoking, social isolation, excessive alcohol use, sleep disorders, and hearing loss. These risk factors include behaviors, conditions, and lifestyles that can emerge before adulthood and can be routinely identified and managed by primary care clinicians.
Reference:
- Lazar RM, Howard VJ, Kernan WN, Aparicio HJ, Levine DA, Viera AJ, Jordan LC, Nyenhuis DL, Possin KL, Sorond FA, White CL; American Heart Association Stroke Council. A Primary Care Agenda for Brain Health: A Scientific Statement From the American Heart Association. Stroke. 2021 Jun;52(6):e295-e308. doi: 10.1161/STR.0000000000000367. Epub 2021 Mar 15. PMID: 33719523; PMCID: PMC8995075.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8995075/
Checklist to Screen for
Checklist to screen for factors which may contribute to cognitive impairment.
- Vitamin B12 deficiency and thyroid disease
- Use of sedating and anticholinergic medications
- Sleep apnea
- Depression
- Alcohol and drug use
- Hearing and vision loss
Reference:
- AFP Vol 11 No 5 May 2025
Mild Cognitive Impairment / Dementia
These impairments suggest cognitive decline:
- Activities of daily living
- Bathing
- Dressing
- Toileting/continence
- Transferring/ambulation
- Eating
- Instrumental activities of daily living
- Ability to use the telephone
- Shopping
- Food preparation
- Housekeeping
- Laundry
- Mode of transportation
- Responsibility for own medication
- Ability to handle finances
The difference between MCI and dementia is a patient's functional status.
- Dementia core criteria are cognitive or neurobehavioral symptoms that:
- Interfere with work or usual daily function
- Represent a change from the prior baseline function
- Are not explained by delirium or a psychiatric illness
- Include detectable impairment in 2 cognitive domains
Cognitive domains:
- Complex attention
- Executive function
- Learning and momory
- Language
- Visuospacial
- Social cognition
MCI Subtypes:
- Amnestic MCI single domain if only memory is affected
- Amnestic MCI multiple domain, if memory and any other cognitive domains are affected
- Non-amnestic MCI single domain, if any other cognitive domain is the only one affected
- Non-amnestic MCI multiple domain, if multiple domains other than memory are affected
Medications associated with cognitive impairment
- Anticholinergics (diphenhydramine, hydroxyzine, meclizine, promethazine)
- Antidepressants (TCAs, particularly those with anticholinergic effects such as amitriptyline; paroxetine)
- Benzodiazepines (class effect, worse with long acting agents)
- Digoxin
- H2-receptor antagonists
- Nonbenzodiazepine, benzodiazepine receptor agonist hypnotics (zolpidem)
Elderly patients with depression commonly complain of memory impairment.
References:
- JFP Vol 66 No 11 Nov 2017
- Modifiable risk factors for dementia
12 Modifiable Risk Factors
- Diabetes
- Hypertension
- High cholesterol
- Smoking
- Obesity
- Physical inactivity
- Depression
- Coronary heart disease
- Kidney disease
- Diet
- Alcohol
- Mental activity
Factors that reduce dementia risk:
- High cognitive activity
- Healthy diet or Mediterranean diet
- Low-moderate alcohol intake
References:
- Family Practice News Sep 2017
Activities Of Daily Living
| INSTRUMENTAL ACTIVITIES OF DAILY LIVING | BASIC ACTIVITIES OF DAILY LIVING |
|---|---|
| Shopping and social functioning | Dressing |
| Housework and hobbies | Eating |
| Accounting (banking, bills, taxes, handling cash) | Ambulation |
| Food preparation | Toileting |
| Telephone, tools, and transportation | Hygiene |
| Medication management |
References:
Dementia Testing - Clock
How to Administer the Clock Drawing Test
| Step 1 | Find a table and chair in a room that is familiar or free of distractions. Sit your loved one down at the table and provide a single sheet of paper (a blank 8.5-by-11-inches sheet is fine) and a writing utensil. It is best to provide a pencil with an eraser as this may help to lessen any frustration for the test taker. Note that it's also OK to pre-draw a 10-inch circle for your loved one, rather than starting with a blank page. Check out Provide the Circle? in the information box located below the steps. |
| Step 2 | Say "Draw a clock that shows the time as 10 minutes after 11." If further prompting is needed, it's OK to be more specific: "Draw a circle to represent the face of the clock, then add the numbers, and then the hands." The test will still work this way. |
| Step 3 | Allow as much time as needed to complete the task. Rarely will the task take more than 10 minutes. It is suggested that one might put themselves out of the visual range of the test taker in order to discourage questions. If questions are asked, either refrain from answering or simply say "just do as you think best". |
| Step 4 | Assess the clock, looking for abnormalities. If your loved one is distracted, or refuses to draw after having agreed to do so, you might consider these actions as a failure and seek a further assessment from a doctor. More on how to assess the Clock-Drawing Test results below. |
Interpreting the Results
- The Size of the Clock.
- Patients with Parkinson's disease dementia and Huntington's disease, a rarer dementia that can develop in a person's 30s and 40s, are prone to draw a smaller clock (less than two inches), while people with Alzheimer's disease tend to draw bigger (more than 10 inches) clocks. This is because size awareness is affected differently depending on which illness is present.
- Fixating on Time.
- If the person being tested is focused mostly on the time aspect—getting the hands pointed the right way so the clock is correct—to the detriment of the rest of the clock, this is more common in Alzheimer's disease and Parkinson's disease dementia than with other dementias.
- Graphical Errors.
- If the clock looks essentially correct, but is messy (wavy or broken lines), this is more common in Huntington's disease and vascular dementia than Alzheimer's disease.
- Radical Wrongness.
- If the clock doesn't even look like a clock, like if there are letters or incorrect shapes added, this suggests confusion that is more indicative of Alzheimer's disease than Huntington's, Parkinson's, vascular dementia or frontotemporal dementia.
- Spatial Errors.
- If there are big gaps, numbers outside the circle, or numbers on only one side of the circle, this is more common in Parkinson's disease with dementia, Lewy body dementia and vascular dementia, and less common in people with Alzheimer's.
References:
Driving safety edit
Driving safety a physician should evaluate the patient in three main areas:
- vision
- cognition
- neuromuscular functioning
The cognitive tests most associated with driving ability are the clock drawing test and the Trail Making Test (TMT).
- The TMT has two parts (A and B), and part B measures working memory and the ability to shift attention.
- Impairments in clock drawing and TMT are predictive of poor driving skill, but a behind-the-wheel assessment should still be recommended when clinicians have uncertainty around the decision to recommend against driving.
End of Life Care
General recommendations:
- Opiates should be used to treat dyspnea (LOE B)
- Haloperidol and risperidone are effective in treating delerium (LOE C)
- Corticosteroids should be used in management of bowel obstruction caused by malignancy (LOE B)
- Octreotide has limited benefit
- Hyoscyamine or atropine ophthalmic drops can be used to treat excessive oropharyngeal secretions (LOE C)
Common medications (Hospice Comfort Kit)
| Class | Medication | Initial dose |
|---|---|---|
| Antipsychotics | Haloperidol or risperidone | 0.5-1mg sublingually or rectally every 4h as needed for agitation or nausea |
| Each 2mg/mL | ||
| Antipyretics | Acetaminophen suppository (650mg) | 650mg orally or rectally every 4h as needed for fever |
| Benzodiazepines | Lorazepam (2mg/mL) | 0.5-1mg subliingually or rectally every 4h as needed for anxiety |
| Opiates | Morphine or oxycodone (20mg/mL) | 5-10mg sublingually every 3h as needed for pain or shortness of breath |
| Secretion meds | Hyoscyamin (0.125mg/sublingual or liq) | 0.125mg of hyoscyamine or 2-3 drops of atroping sublingually every 6h |
| Atropine ophthalmic 1% drops | as needed for oropharyngeal secretions |
Constipation in End-of-life:
- Docusate
- 1-2 tab 2x a day
- Lactulose
- 15-30 mL orally 2-3x a day
- Magnesium hydroxide
- 30-60 mL orally at bedtime
- Polythylene glycol (Miralax)
- 1 tablespoon (17g) dissolved in 4-8oz of fluid orally per day
- Senna with docusate
- 1-2 taba orally 2-4x a day
References:
- AFP Vol 95 No 6 Mar 2017
Falls
Medications associated with falls:
- Anticonvulsants
- Antidepressants
- Antihypertensives
- Antiparkinsonian drugs
- Antipsychotics
- Benzodiazepines
- Digoxin
- Diuretics
- Laxatives
- Opioids
- Nonbenzodiazepine, benzodiazepine receptor agonist hypnotics
- NSAIDs
- Sedatives and hypnotics
References:
- AFP Vol 96 No 4 Aug 2017
Get up and Go Test
Steps:
- Rise from sitting position
- Walk 10 feet
- Turn around
- Return to chair and sit down
Interpretation:
- >12 seconds is high risk of falling
- Patient takes <20 seconds to complete test
- Adequate for independent transfers and mobility
- Patient requires >30 seconds to complete test
- Suggests higher dependence and risk of of falls
References:
- Posiadlo (1991) J Am Geriatr Soc 39:142-8 [PubMed]
- Am Fam Physician. 2018;97(12):776-784
30 second chair stand test
Patient performs as many sit-to-stand sequences without hands as they can in 30 seconds while evaluator counts complete cycles.
| Age | Men | Women |
|---|---|---|
| 60-64 | <14 | <12 |
| 65-69 | <12 | <11 |
| 70-74 | <12 | <10 |
| 75-79 | <11 | <10 |
| 80-84 | <10 | <9 |
| 85-89 | <8 | <8 |
| 90-94 | <7 | <4 |
Reference:
- AFP Vol 109 No 5 May 2024
- https://www.cdc.gov/steadi/media/pdfs/STEADI-Assessment-30Sec-508.pdf
4 Stage balance test
Assessment of static balance using 4 different foot positions (should hold for 10 sec)
- feet together
- feet together with 1 foot a few inches forward
- Tandem stance (1 foot directly in front of the other)
- Single leg stance
Loss of balance during any of the 4 stages indicates an increased risk of falls
Reference:
- AFP Vol 109 No 5 May 2024
Gait Evaluations
- Timed Up and Go Test
- Stand up, walk 10 feet, turn, walk back and sit down
- 12 seconds or longer = increased fall risk
- 4 Stage Balance Test
- Assess ability to stand in 4 positions for 10 seconds
- Feet side by side
- Instep of 1 foot touching big toe of other foot
- 1 foot in front of the other
- On 1 foot
- Assess ability to stand in 4 positions for 10 seconds
- 30 Second Cair Stand Test
- Sit in middle of chair, hands on opposite shoulders, feet flat on floor and back straight, rise to full standing and sit back down, repeat for 30 seconds
30 Second Chair Stand Below Average Scores
| AGE | MEN | WOMEN |
| 60-64 | <14 | <12 |
| 65-69 | <12 | <11 |
| 70-74 | <12 | <10 |
| 75-79 | <11 | <10 |
| 80-84 | <10 | <9 |
| 85-89 | <8 | <8 |
| 90-94 | <7 | <4 |
Geriatric Assistive Devices
For patients who need one upper extremities for weight bearing or balance:
- Minimal need:
- Standard cane
- Intermittent need:
- Offset cane
- Need Often:
- Quadripod cane
For patients who need both upper extremities for weight bearing or balance:
- Minimal need:
- Four-wheeled walker (rollator)
- Intermittent need:
- Front-wheeled walker or
- Forearm crutches
- Need Often:
- Front-wheeled walker or
- Standard walker
- Constant need:
- Standard or front-wheeled walker
Frailty
Frailty Strength Training Prescription
- Two to three nonconsecutive days per week
- Moderate intensity (5 to 6 on a 10-point scale)
- Target the major muscle groups with eight to 10 exercises per session
- 8 to 15 repetitions per exercise; at least one set of repetitions per exercise
- Gradually increase weight and repetitions based on tolerability
- Strength training exercises:
- Sit to stand
- Heel lifts
- Toe lifts
- Lunges
- Front arm raises
- Side arm raises
- Wall push-ups
Frailty Balance Training Prescription
- Two or more hours per week, initially under close supervision to reduce fall risk
- Begin with less challenging positions
- Maintain each exercise for a minimum of five to 10 seconds, with at least one repetition per exercise
- Start on flat surfaces and gradually advance the level of difficulty*
- Flat surface exercises:
- Side-by-side stance
- Semi-tandem stance
- Tandem stance
- Single limb stance
- Heel stance
- Toe stance
- Uneven surface exercises:
- Step up, step down without hand support
- Forward and backward walking
- Sideways walking
- Change directions while walking
- Complex task exercises:
- Navigate obstacles while walking
- Pick up objects from the floor while walking
- Carry objects of variable weight and size while walking
- Incorporate head turns while reaching in different directions
- Carry on conversation while walking
- Conduct simple mathematical calculations while walking
References:
- AFP Feb 2021 Vol 103 No 4
Hospice
Consider Hospice if 2 or more:
- Dependent in 2-3 of 6 ADLS
- SOB or fatigue at rest/minimal exertion
- Multiple ED visits or hospitalizations
- 10% weight loss in 6 mo
- Recurrent falls with injury
- Decreased tolerance in physical activity
Diagnosis Specific Eligibility Guidelines
- ALS
- In end-stage ALS, two factors are critical in determining prognosis: ability to breathe and ability to swallow.
- BOTH rapid progression of ALS and critically impaired ventilatory capacity or
- BOTH rapid progression of ALS and critical nutritional impairment with a decision not to receive artificial feeding or
- BOTH rapid progression of ALS and life-threatening complications such as:
- Recurrent aspiration pneumonia
- Decubitus ulcers, multiple, stage 3-4, particularly if infected
- Upper urinary tract infection, e.g., pyelonephritis
- Sepsis
- Fever recurrent after antibiotics
- Alzheimer's and Dementia
- When patients with dementia or Alzheimer's can no longer move around, get dressed, bathe, or speak, they may be eligible for hospice care.
- Unable to ambulate without assistance
- Unable to dress without assistance
- Unable to bathe properly
- Incontinence of bowel and bladder
- Unable to speak or communicate meaningfully (ability to speak is limited to approximately a half dozen or fewer intelligible and different words)
- COPD and Lung Disease
- One of the major characteristics that a COPD patient may be hospice-eligible is dyspnea at rest or with minimal exertion.
- Dyspnea at rest and/or with minimal exertion while on oxygen therapy
- Dyspnea unresponsive or poorly responsive to bronchodilator therapy
- Progression of chronic pulmonary disease as evidenced by one or more of the following:
- Frequent use of medical services, including hospitalizations, ED visits and/or physician outpatient visits, due to symptoms of pulmonary disease
- Frequent episodes of bronchitis or pneumonia
- Unintentional weight loss of ≥ 10 percent body weight over the preceding six months
- Progressive inability to independently perform various activities of daily living (ADLs) or an increasing dependency with ADLs, resulting in a progressively lower performance status
- Heart Disease
- Hospice care for heart disease addresses a wide range of symptoms, including shortness of breath, chest pain, weakness, functional decline and the management of fluid status.
- New York Heart Association (NYHA) Class III if any of the following symptoms are present during less-than-normal activity (i.e. patient is comfortable only at rest):
- Fatigue
- Palpitations
- Angina or dyspnea with exercise
- NYHA Class IV as manifested by any of the following symptoms:
- Dyspnea and/or other symptoms at rest or with minimal exertion
- Inability to carry out physical activity without dyspnea and/or other symptoms
- If physical activity is undertaken, dyspnea and/or other symptoms worsen
- The patient is being optimally treated for congestive heart failure with diuretics and vasodilators, such as ACE inhibitors, or they are maximally medically managed and have no available surgical options.
- HIV and AIDS
- Low CD4 counts, decreased performance on the KPS scale, and documentation of certain factors are all signs that your HIV/AIDS patient may be ready for hospice.
- Liver Disease
- Liver disease patients may be appropriate for hospice care if they have persistent symptoms of hepatic failure, such as ascites, hepatic encephalopathy or recurrent varicella bleeding, and meet other guidelines.
- Neurological Disease
- Neurological diseases such as coma, stroke, Parkinson's disease and multiple sclerosis are life-altering conditions that can lead to permanent deterioration of the nervous system.
- Severely compromised breathing, marked by inability to clear respiratory secretions, persistent cough, or recurring aspiration pneumonia
- Increased shortness of breath, even at rest or on oxygen
- Inability to swallow liquids or soft food without choking or coughing; progression to a mainly pureed diet
- Spends most of the time in the same room, chair or bed
- Barely intelligible speech
- Continued weight loss
- Inability to manage most activities of daily living
- Oncology
- In oncology, the biggest predictor of hospice eligibility is the patient's functional status, which is determined by the Eastern Cooperative Oncology Group (ECOG) scale or the Palliative Performance Scale (PPS).
- Renal Disease
- More patients and families are choosing not to start or to withdraw dialysis for multiple reasons, particularly in patients older than 60 years.
- Sepsis and Concomitant End-Stage Disease
- Sepsis is one of the most deadly U.S. conditions, with about 250,000 deaths each year. The estimated annual cost of sepsis readmissions is more than $3.5 billion.
Reference:
Indications for Mental Health Referral
Indications for Mental Health Referral for terminal illness:
- Diagnostic uncertainty
- Other significant psychiatric comorbidities
- Psychosis
- Psychotherapy referral
- SI or request for physician assisted dying
- Unresponsive or intolerant to initial treatment trials
References:
- AFP Vol 86 No 3 2012
Early Signs of Dementia vs Normal Cognitive Changes Related to Aging
| Domain | Early signs of dementia | Normal cognitive changes related to aging |
|---|---|---|
| Familiar tasks | Struggling with daily tasks or driving | Needing help with microwave or television settings |
| Judgment | Poor financial decisions or hygiene | Occasional bad decisions |
| Language and communication | Trouble with conversations or vocabulary | Trouble with finding the right word occasionally |
| Memory loss | Forgetting recent information; repeating questions | Forgetting names but remembering later |
| Misplacing items | Unable to retrace steps | Misplacing items, able to retrace steps |
| Mood and personality changes | Becoming anxious or suspicious easily | Irritable with routine changes |
| Planning and problem solving | Difficulty with plans, numbers, recipes | Occasional financial errors |
| Social withdrawal | Withdrawing from activities or hobbies | Feeling uninterested occasionally |
| Time and place orientation | Losing track of dates or locations | Confused about the day of the week |
| Visual perception | Difficulty with balance or reading | Vision changes from cataracts |
Reference:
- Am Fam Physician. 2025;112(6):657-667
Insomnia in Geriatrics
Recent systematic reviews and network meta-analyses reinforce that among pharmacologic options, low-dose doxepin (3–6 mg) demonstrates the most favorable balance of efficacy and safety for geriatric insomnia, particularly for improving total sleep time and sleep efficiency, with an adverse event profile comparable to placebo in older adults.
Eszopiclone and zaleplon may offer greater efficacy for specific sleep parameters (e.g., sleep onset latency), but their use is limited by increased risks of cognitive impairment, falls, and other adverse effects in the elderly.
Reference:
- Chiu HY, Lee HC, Liu JW, et al. Comparative Efficacy and Safety of Hypnotics for Insomnia in Older Adults: A Systematic Review and Network Meta-Analysis. Sleep. 2021;44(5):zsaa260. https://doi.org/10.1093/sleep/zsaa260.
- Schroeck JL, Ford J, Conway EL, et al. Review of Safety and Efficacy of Sleep Medicines in Older Adults. Clinical Therapeutics. 2016;38(11):2340-2372. https://doi.org/10.1016/j.clinthera.2016.09.010.
Medications in Geriatrics
See also:
Mobility Assist Devices
When mobility deficit impairs ADLs at home and patient can operate assistive device safely:
- If mobility deficit can be resolved with a cane or walker
- One UE needed for weight bearing or balance:
- Minimal frequency of weight bearing:
- Standard cane
- Intermittent frequency of weight bearing:
- Offset cane
- Often frequency of weight bearing:
- Quadripod cane
- Minimal frequency of weight bearing:
- Both UE needed for weight bearing or balance:
- No frequency of weight bearing:
- Four-wheel walker (rollator)
- Intermittent frequency of weight bearing:
- 2-wheel or standard walker
- Often frequency of weight bearing:
- 2-wheel walker or fore-arm crutches
- Constant frequency of weight bearing:
- Standard or 2-wheel walker
- No frequency of weight bearing:
- One UE needed for weight bearing or balance:
- If mobility deficit cannot be resolved with a cane or walker
- If patient has sufficient upper body strength for a manual wheelchair
- Manual wheelchair
- If patient has sufficient strength and postural stability to operate a scooter
- Scooter
- If patient is unable to operate a manual wheelchair or needs feaures provided with a power wheelchair
- Power wheelchair
- If patient has sufficient upper body strength for a manual wheelchair
Reference:
- AFP Jun 2021 Vol 103 No 12
One-legged Stand
Successful 10-second one-legged stance performance predicts survival in middle-aged and older individuals
- During a median follow-up of 7 years:
- 7.2% died, with 4.6% (YES) and 17.5% (NO) on the 10-s OLS
- HR of all-cause mortality was higher for NO individuals
- HR 1.84 (95% CI: 1.23 to 2.78) (p<0.001)
- Within the limitations of uncontrolled variables such as recent history of falls and physical activity, the ability to successfully complete the 10-s OLS is independently associated with all-cause mortality and adds relevant prognostic information beyond age, sex and several other anthropometric and clinical variables
- Reference:
- Araujo CG, de Souza e Silva CG, Laukkanen JA, et al. Successful 10-second one-legged stance performance predicts survival in middle-aged and older individuals British Journal of Sports Medicine. Published Online First: 21 June 2022. doi: 10.1136/bjsports-2021-105360
Osteoporosis
Bone Mineral Density:
- Normal: T-score > -1.0
- Osteopenia: BMD between -1.0 and -2.5
- Osteoporosis: BMD at or below -2.5
- Severe or established osteoporosis: -25 or lower + fragility fracture
Consider Pharmacologic Therapy:
- Postmenopausal women and men >50 with a Hip or Vertebral fragility fracture
- T-score < -2.5 Femoral neck, total hip, or spine
- T-score between -1.0 and -2.5 and FRAX scores:
- Major > 20% or Hip 3% 10-yr fracture risk
Recommendations:
- First line antiresorptive agents: Offer to women with osteoporosis (strong rec; high-quality evidence):
- alendronate
- risedronate
- zoledronic acid (Reclast) (IV qyr)
- denosumab (SC q6mo)
- First line anabolic agents:
- teriparatide (Forteo)
- Once initiated, pharmacologic treatment should be continued for 5 years (weak rec; low-quality evidence)
- Bisphosphonates should be offered to men with osteoporosis (weak rec; low-quality evidence)
- Bone density should not be monitored during the 5 year treatment period for women with osteoporosis (weak rec; low-quality evidence)
Resources:
- FRAX s
References:
- FMX 2016
- JFP Vol 67 No 2 Feb 2018
- JAMA Vol 310 No 10 Mar 2018
- AFP Vol 107 No 3 Mar 2023
Screening
Screen:
- All women 65+
- Women who are postmenopausal and <65yo with increased risk
Screen men with scores >6:
| Risk Factor | Points |
|---|---|
| Age: | |
| <55 yo | 0 |
| 56-74yo | 3 |
| >75 | 4 |
| COPD | 3 |
| Weight: | |
| <154 lbs | 6 |
| 155-176 | 4 |
| >176lbs | 0 |
Ref:
- AFP Vol 82 No 5 Sep 2010
Recommendations
To prevent bone loss and falls:
- Strength training for major muscle goups >2/wk
- Balance challenges daily
- Mod-Vigorous aerobic physical activity >150min/wk or 20-30min/d
To reduce spine loads:
- Exercises for back extensor muscles daily
- Spine sparing strategies
- Hip hinge for bending
- Step to turn instead of twisting
- Holding loads close to body
Ref:
- FMX 2016
- Fit to Fracture
Vertebral compression fractures
Medications:
| Medication | Dosage | Cost |
|---|---|---|
| Acetaminophen | 500-1000mg q4-q8 (max 3g/d) | $15 |
| Calcitonin | 200 IU/d intranasally | $45 |
| Lidocaine 5% patch | Apply to affected areas q12 | $220 |
| Muscle relaxants | 10mg q8 | Varies |
| Narcotics | Varies | Varies |
| Ibuprofen | 200-800mg q8 | $11 |
| Naproxen | 500mg q12 | $4 |
Ref:
- AFP Vol 94 No 1 2016
Osteoporosis
Risk factors for osteoporosis
- Age ≥ 65 y
- Early menopause
- Excessive alcohol use
- Family history of osteoporosis
- Female sex
- Low body weight (< 127 lb)
- Physical inactivity
- Smoking
Fracture risk can be assessed with any of a number of tools, including:
- Simplified Calculated Osteoporosis Risk Estimation (SCORE): www.medicalalgorithms.com/simplified-calculated-osteoporosis-risk-estimation-tool
- Osteoporosis Risk Assessment Instrument (ORAI): www.physiopedia.com/TheOsteoporosisRiskAssessmentInstrument(ORAI)
- Osteoporosis Index of Risk (OSIRIS): https ://www.tandfonline.com/doi/abs/10.1080/gye.16.3.245.250?journalCode=igye20
- Osteoporosis Self-Assessment Tool (OST): www.ncbi.nlm.nih.gov/books/NBK45516/figure/ch10.f2/
- FRAX tool5: www.sheffield.ac.uk/
FRAX.
The FRAX tool is widely used. It assesses a patient's 10-year risk of fracture
Diagnosis of osteoporosis is based on any 1 or more of the following criteria:
- a history of fragility fracture not explained by metabolic bone disease
- T-score ≤ –2.5 (lumbar, hip, femoral neck, or 33% radius)
- a nation-specific FRAX score (in the absence of access to DXA).
Measures to prevent osteoporosis
- Avoid smoking
- Reduce alcohol intake
- Increase physical activity, including a regular regimen of weight-bearing
- exercises
- Maintain a blood level of 25‐hydroxyvitamin D of ≥ 30 ng/mL (75 nmoL/L)
- Ensure adequate intake of calcium (1000-1200 mg/d)
Indications for pharmacotherapy for osteoporosis in older adults
- Osteopenia or low bone mass and a history of fragility fracture of the hip or spine
- T-score of –2.5 or lower in the spine, femoral neck, total hip, or 33% radius
- T-score between –1.0 and –2.5 in the spine, femoral neck, total hip, or 33% radius, if the FRAX 10-year probability for major osteoporotic fracture is ≥ 20% or the 10-year probability of hip fracture is ≥ 3% (in the United States) or above the country-specific threshold in other countries or regions
- The country-specific FRAX score indicates treatment for osteoporosis where bone mineral density assessment by dual-energy X-ray absorptiometry is unavailable
Reference:
- J Fam Pract. 2021 June;70(5):220-228 | 10.12788/jfp.0201
Preoperative Evaluation and Frailty Assessment in Older Patients edit
Key Components of the Preoperative Evaluation in Older Patients
- Cognitive status
- Patient's life goals
- PHQ-2 and PHQ-9, if indicated
- Risk Analysis Index
- Social and living situation
Questions to Ask Older Patients Considering Surgery: Quality-of-life assessment
- How might my life be different right after surgery or three to six months later?
- How might surgery affect my independence?
- What serious complications could arise?
- Will surgery affect my life expectancy?
- Will surgery make me feel better?
References:
- AFP Vol 102 No 12 Dec 2020
Study: Abdominal fat depots are related to lower cognitive functioning and brain volumes in middle-aged males at high Alzheimer's risk
Objective:
- High BMI, which poorly represents specific fat depots, is linked to poorer cognition and higher dementia risk, with different associations between sexes. This study examined associations of abdominal fat depots with cognition and brain volumes and whether sex modifies this association.
Methods:
- A total of 204 healthy middle-aged offspring of Alzheimer's dementia patients (mean age = 59.44, 60% females) underwent abdominal magnetic resonance imaging to quantify hepatic, pancreatic, visceral, and subcutaneous adipose tissue and to assess cognition and brain volumes.
Results:
- In the whole sample, higher hepatic fat percentage was associated with lower total gray matter volume (β = -0.17, p < 0.01).
- Primarily in males
- higher pancreatic fat percentage was associated with lower global cognition (males: β = -0.27, p = 0.03; females: β = 0.01, p = 0.93)
- executive function (males: β = -0.27, p = 0.03; females: β = 0.02, p = 0.87)
- episodic memory (males: β = -0.28, p = 0.03; females: β = 0.07, p = 0.48)
- inferior frontal gyrus volume (males: β = -0.28, p = 0.02; females: β = 0.10, p = 0.33)
- Visceral and subcutaneous adipose tissue was inversely associated with middle frontal and superior frontal gyrus volumes in males and females.
Conclusions:
- In middle-aged males at high Alzheimer's dementia risk, but not in females, higher pancreatic fat was associated with lower cognition and brain volumes. These findings suggest a potential sex-specific link between distinct abdominal fat with brain health.
Reference:
- Golan Shekhtman S, Boccara E, Ravona-Springer R, Inbar Y, Zelicha H, Livny A, Bendlin BB, Lesman-Segev O, Yore I, Heymann A, Sano M, Mardor Y, Azuri J, Schnaider Beeri M. Abdominal fat depots are related to lower cognitive functioning and brain volumes in middle-aged males at high Alzheimer's risk. Obesity (Silver Spring). 2024 Feb 27. doi: 10.1002/oby.24004. Epub ahead of print. PMID: 38410053.
Study: Hypertension linked to Alzheimer's disease via stroke: Mendelian randomization
This study aimed to investigate the relationship between hypertension and Alzheimer's disease (AD) and demonstrate the key role of stroke in this relationship using mediating Mendelian randomization. AD, a neurodegenerative disease characterized by memory loss, cognitive impairment, and behavioral abnormalities, severely affects the quality of life of patients. Hypertension is an important risk factor for AD. However, the precise mechanism underlying this relationship is unclear.
To investigate the relationship between hypertension and AD, we used a mediated Mendelian randomization method and screened for mediating variables between hypertension and AD by setting instrumental variables.
The results of the mediated analysis showed that stroke, as a mediating variable, plays an important role in the causal relationship between hypertension and AD. Specifically, the mediated indirect effect value for stroke obtained using multivariate mediated MR analysis was 54.9%.
This implies that approximately 55% of the risk of AD owing to hypertension can be attributed to stroke. The results suggest that the increased risk of AD owing to hypertension is mediated through stroke.
The finding not only sheds light on the relationship between hypertension and AD but also indicates novel methods for the prevention and treatment of AD. By identifying the critical role of stroke in the link between hypertension and AD, this study provides insights into potential interventions that could mitigate the impact of hypertension on AD. This could help develop personalized treatments and help improve the quality of life of patients with AD who suffer from hypertension.
Reference:
- Tang C, Ma Y, Lei X, Ding Y, Yang S, He D. Hypertension linked to Alzheimer's disease via stroke: Mendelian randomization. Sci Rep. 2023 Dec 7;13(1):21606. doi: 10.1038/s41598-023-49087-0. PMID: 38062190; PMCID: PMC10703897.
Study: Hypertension and Alzheimer's disease pathology at autopsy: A systematic review
Hypertension is an important risk factor for Alzheimer's disease (AD) and all-cause dementia. The mechanisms underlying this association are unclear. Hypertension may be associated with AD neuropathological changes (ADNC), but reports are sparse and inconsistent.
This systematic review included 15 autopsy studies (n = 5879) from observational cohorts. Studies were highly heterogeneous regarding populations, follow-up duration, hypertension operationalization, neuropathological methods, and statistical analyses.
- Hypertension seems associated with higher plaque and tangle burden, but results are inconsistent.
- Four studies (n = 3993/5879; 68%), reported clear associations between hypertension and ADNC.
- Another four suggested that antihypertensive medication may protect against ADNC.
- Larger studies with longer follow-up reported the strongest relationships.
Our findings suggest a positive association between hypertension and ADNC, but effects may be modest, and possibly attenuate with higher hypertension age and antihypertensive medication use. Investigating interactions among plaques, tangles, cerebrovascular pathology, and dementia may be key in better understanding hypertension's role in dementia development.
Reference:
- Abdulrahman H, van Dalen JW, den Brok M, Latimer CS, Larson EB, Richard E. Hypertension and Alzheimer's disease pathology at autopsy: A systematic review. Alzheimers Dement. 2022 Nov;18(11):2308-2326. doi: 10.1002/alz.12707. Epub 2022 Jun 27. PMID: 35758526; PMCID: PMC9796086.
Study: Blood Pressure, Antihypertensive Use, and Late-Life Alzheimer and Non-Alzheimer Dementia Risk: An Individual Participant Data Meta-Analysis
Background and objectives:
- Previous randomized controlled trials and longitudinal studies have indicated that ongoing antihypertensive use in late life reduces all-cause dementia risk, but the specific impact on Alzheimer dementia (AD) and non-AD risk remains unclear. This study investigates whether previous hypertension or antihypertensive use modifies AD or non-AD risk in late life and the ideal blood pressure (BP) for risk reduction in a diverse consortium of cohort studies.
Methods:
- This individual participant data meta-analysis included community-based longitudinal studies of aging from a preexisting consortium. The main outcomes were risk of developing AD and non-AD. The main exposures were hypertension history/antihypertensive use and baseline systolic BP/diastolic BP. Mixed-effects Cox proportional hazards models were used to assess risk and natural splines were applied to model the relationship between BP and the dementia outcomes. The main model controlled for age, age2, sex, education, ethnoracial group, and study cohort. Supplementary analyses included a fully adjusted model, an analysis restricting to those with >5 years of follow-up and models that examined the moderating effect of age, sex, and ethnoracial group.
Results:
- There were 31,250 participants from 14 nations in the analysis (41% male) with a mean baseline age of 72 (SD 7.5, range 60-110) years.
- Participants with untreated hypertension had a 36% (hazard ratio [HR] 1.36, 95% CI 1.01-1.83, p = 0.0406) and 42% (HR 1.42, 95% CI 1.08-1.87, p = 0.0135) increased risk of AD compared with "healthy controls" and those with treated hypertension, respectively.
- Compared with "healthy controls" both those with treated (HR 1.29, 95% CI 1.03-1.60, p = 0.0267) and untreated hypertension (HR 1.69, 95% CI 1.19-2.40, p = 0.0032) had greater non-AD risk, but there was no difference between the treated and untreated groups.
- Baseline diastolic BP had a significant U-shaped relationship (p = 0.0227) with non-AD risk in an analysis restricted to those with 5-year follow-up, but otherwise there was no significant relationship between baseline BP and either AD or non-AD risk.
Discussion:
- Antihypertensive use was associated with decreased AD but not non-AD risk throughout late life.
- This suggests that treating hypertension throughout late life continues to be crucial in AD risk mitigation.
- A single measure of BP was not associated with AD risk, but DBP may have a U-shaped relationship with non-AD risk over longer periods in late life.
Reference:
- Lennon MJ, Lipnicki DM, Lam BCP, Crawford JD, Schutte AE, Peters R, Rydberg-Sterner T, Najar J, Skoog I, Riedel-Heller SG, Röhr S, Pabst A, Lobo A, De-la-Cámara C, Lobo E, Lipton RB, Katz MJ, Derby CA, Kim KW, Han JW, Oh DJ, Rolandi E, Davin A, Rossi M, Scarmeas N, Yannakoulia M, Dardiotis T, Hendrie HC, Gao S, Carriere I, Ritchie K, Anstey KJ, Cherbuin N, Xiao S, Yue L, Li W, Guerchet M, Preux PM, Aboyans V, Haan MN, Aiello A, Scazufca M, Sachdev PS; as the Cohort Studies of Memory in an International Consortium (COSMIC) Group. Blood Pressure, Antihypertensive Use, and Late-Life Alzheimer and Non-Alzheimer Dementia Risk: An Individual Participant Data Meta-Analysis. Neurology. 2024 Sep 10;103(5):e209715. doi: 10.1212/WNL.0000000000209715. Epub 2024 Aug 14. PMID: 39141884; PMCID: PMC11329294.
Study: Heavy resistance training at retirement age induces 4-year lasting beneficial effects in muscle strength: a long-term follow-up of an RCT
Objectives:
- Muscle function and size decline with age, but long-term effects of resistance training in older adults are largely unknown. Here, we explored the long-lasting (3 years) effects of 1 year of supervised resistance training with heavy loads.
Methods:
- The LIve active Successful Ageing (LISA) study was a parallel group randomised controlled trial at a university hospital in Denmark. Older adults (n=451) at retirement age were randomised to 1 year of heavy resistance training (HRT), moderate-intensity training (MIT) or a non-exercising control group (CON). Primary outcome measure was leg extensor power. Secondary outcomes included maximal isometric quadriceps torque (isometric leg strength) and body composition (dual-energy X-ray absorptiometry (DXA)). Participants completed test procedures at baseline, following the 1-year intervention, and 2 and 4 years post study start.
Results:
- At the 4-year assessment, 369 participants attended (mean age=71 years, 61% women).
- The main finding was that across all four time points, there was a significant group×time interaction in isometric leg strength (F6,1049=8.607, p<0.001, η2 =0.05).
- Individuals in HRT maintained baseline performance in isometric leg strength (Baseline: 149.7±51.5 Nm, 4 years: 151.5±51.1 Nm, t(1050)=1.005, p=1.00) while participants in CON and MIT decreased.
Conclusion:
- In well-functioning older adults at retirement age, 1 year of HRT may induce long-lasting beneficial effects by preserving muscle function.
Reference:
- Bloch-Ibenfeldt M, Theil Gates A, Karlog K, Demnitz N, Kjaer M, Boraxbekk CJ. Heavy resistance training at retirement age induces 4-year lasting beneficial effects in muscle strength: a long-term follow-up of an RCT. BMJ Open Sport Exerc Med. 2024 Jun 18;10(2):e001899. doi: 10.1136/bmjsem-2024-001899. PMID: 38911477; PMCID: PMC11191791.
Study: Galantamine for Alzheimer's disease and mild cognitive impairment edit
BLUF:
- Galantamine improves global and cognitive symptoms at doses of 16 mg/day or greater, in people with mild to moderate Alzheimer's disease, for at least 6 months
- Alzheimer's disease is a progressive neurodegenerative illness, affecting thinking and memory. Galantamine is a reversible cholinesterase inhibitor that inhibits the degradation of the neurotransmitter acetylcholine, and may have other actions on nicotinic receptors as well. The review finds that galantamine was more effective than placebo in improving cognitive function. A greater proportion of people taking galantamine than of those taking placebo was rated as improved or not changed after three to six months. There was evidence of improvement on measures of activities of daily living and behavioral symptoms. Longer‐term controlled studies have yet to be performed or published.
- Data from the two MCI trials suggest marginal clinical benefit, but a yet unexplained excess in death rate.
Background:
- Galantamine is a specific, competitive, and reversible acetylcholinesterase inhibitor.
Objectives:
- To assess the clinical effects of galantamine in patients with mild cognitive impairment (MCI), probable or possible Alzheimer's disease (AD), and potential moderators of effect.
Search strategy:
- The trials were identified from a search of the Specialized Register of the Cochrane Dementia and Cognitive Improvement Group, last updated on 25 April 2005 using the terms galanthamin*, galantamin* and Reminyl. Published reviews were inspected for further sources. Additional information was collected from unpublished clinical research reports for galantamine obtained from Janssen and from http://www.clinicalstudyresults.org/.
Selection criteria:
- Trials selected were randomised, double-blind, parallel-group comparisons of galantamine with placebo for a treatment duration of greater than 4 weeks in subjects with MCI or AD.
Data collection and analysis:
- Data were extracted independently by the reviewers and pooled where appropriate and possible. Outcomes of interest include the clinical global impression of change (CIBIC-plus or CGIC), Alzheimer's Disease Assessment Scale-cognitive sub scale (ADAS-cog), Alzheimer's Disease Cooperative Study/Activities of Daily Living (ADCS-ADL), Disability Assessment for Dementia scale (DAD) and Neuropsychiatric Inventory (NPI). Potential moderating variables of treatment effect assessed included trial duration, dose, and diagnosis of possible versus probable Alzheimer's disease.
Main results:
- Ten trials with a total 6805 subjects were included in the analysis. Treatment with galantamine led to a significantly greater proportion of subjects with improved or unchanged global rating scale rating (k = 8 studies), at all dosing levels except for 8 mg/d . Confidence intervals for the ORs overlapped across the dose range of 16 mg to 36 mg per day, with point estimates of 1.6 - 1.8 when analysed with the intention-to-treat sample. Treatment with galantamine also led to significantly greater reduction in ADAS-cog score at all dosing levels (k = 8), with greater effect over six months compared to three months. Confidence intervals again overlapped. Point estimate of effect was lower for 8 mg/d but similar for 16 mg to 36 mg per day. For example, treatment effect for 24 mg/d over six months was 3.1 point reduction in ADAS-cog (95%CI 2.6-3.7, k = 4, ITT).ADCS-ADL, DAD and NPI were reported only in a small proportion of trials: all showed significant treatment effect in some individual trials at least. Confidence interval of treatment effect for the one trial recruiting patients with possible AD overlapped with the other seven recruiting patients with probable AD. Galantamine's adverse effects appeared similar to those of other cholinesterase inhibitors and to be dose related. Prolong release / once daily formulation of galantamine at 16 - 24mg/d was found to have similar efficacy and side-effect profile as the equivalent twice-daily regime. Data from the two MCI trials suggest marginal clinical benefit, but a yet unexplained excess in death rate.
Authors' conclusions:
- Subjects in these trials were similar to those seen in earlier anti dementia AD trials, consisting primarily of mildly to moderately impaired outpatients. Galantamine's effect on more severely impaired subjects has not yet been assessed.Nevertheless, this review shows consistent positive effects for galantamine for trials of three to six months' duration. Although there was not a statistically significant dose-response effect, doses above 8 mg/d were, for the most part, consistently statistically significant. Galantamine's safety profile in AD is similar to that of other cholinesterase inhibitors with respect to cholinergically mediated gastrointestinal symptoms. It appears that doses of 16 mg/d were best tolerated in the single trial where medication was titrated over a four week period, and because this dose showed statistically indistinguishable efficacy with higher doses, it is probably most preferable initially. Longer term use of galantamine has not been assessed in a controlled fashion. Galantamine use in MCI is not recommended due to its association with an excess death rate.
Reference:
- Loy C, Schneider L. Galantamine for Alzheimer's disease and mild cognitive impairment. Cochrane Database Syst Rev. 2006 Jan 25;2006(1):CD001747. doi: 10.1002/14651858.CD001747.pub3. Update in: Cochrane Database Syst Rev. 2024 Nov 5;11:CD001747. doi: 10.1002/14651858.CD001747.pub4. PMID: 16437436; PMCID: PMC8961200.
Study: Nonlinear dynamics of multi-omics profiles during human aging
Aging is a complex process associated with nearly all diseases. Understanding the molecular changes underlying aging and identifying therapeutic targets for aging-related diseases are crucial for increasing healthspan. Although many studies have explored linear changes during aging, the prevalence of aging-related diseases and mortality risk accelerates after specific time points, indicating the importance of studying nonlinear molecular changes.
In this study, we performed comprehensive multi-omics profiling on a longitudinal human cohort of 108 participants, aged between 25 years and 75 years. The participants resided in California, United States, and were tracked for a median period of 1.7 years, with a maximum follow-up duration of 6.8 years.
The analysis revealed consistent nonlinear patterns in molecular markers of aging, with substantial dysregulation occurring at two major periods occurring at approximately 44 years and 60 years of chronological age.
Distinct molecules and functional pathways associated with these periods were also identified, such as immune regulation and carbohydrate metabolism that shifted during the 60-year transition and cardiovascular disease, lipid and alcohol metabolism changes at the 40-year transition.
Overall, this research demonstrates that functions and risks of aging-related diseases change nonlinearly across the human lifespan and provides insights into the molecular and biological pathways involved in these changes.
Reference:
- Shen X, Wang C, Zhou X, Zhou W, Hornburg D, Wu S, Snyder MP. Nonlinear dynamics of multi-omics profiles during human aging. Nat Aging. 2024 Nov;4(11):1619-1634. doi: 10.1038/s43587-024-00692-2. Epub 2024 Aug 14. PMID: 39143318; PMCID: PMC11564093.
Study: What Is the Association Between Music-Related Leisure Activities and Dementia Risk? A Cohort Study
Key points
- Always listening to music was associated with a 39% reduced dementia risk and better global cognition and memory scores.
- Playing an instrument was associated with a 35% reduced dementia risk, but no significant association with CIND risk or changes in cognitive test scores over time.
- Regularly engaging in both music listening and playing was associated with a 33% decreased risk of dementia and 22% decreased risk of cognitive impairment no dementia (CIND).
- Engagement in music-related activities showed no significant association with subjective cognitive wellbeing.
- Music engagement benefits were strongest in those with higher education (16+ years) but showed inconsistent results in the middle education group (12–15 years).
- This large prospective cohort study (n = 10,893) suggests music activities may be an accessible strategy for maintaining cognitive health in older adults, though causation cannot be established.
-—
Objectives
- To determine whether engagement in music-related leisure activities is associated with a reduced risk of dementia and cognitive impairment no dementia (CIND), as well as better cognitive wellbeing in initially cognitively healthy older adults. Here, cognitive wellbeing includes maintaining good cognitive function as well as quality of life. Potential effect modification by education was also investigated.
Methods
- This study used secondary data from the ASPirin in Reducing Events in the Elderly (ASPREE) study, and the ASPREE Longitudinal Study of Older Persons (ALSOP) sub-study. Included were 10,893 community-dwelling Australian adults who were 70 years and older, without dementia diagnosis at recruitment to the study. Cox proportional hazard regression models were used to determine the association between level of music engagement (listening to music, playing an instrument, and a combination of both) and dementia risk from year 3 onwards. Linear mixed models were used to investigate the association with cognitive wellbeing. Analyses adjusted for age, gender and level of education completed.
Results
- Always listening to music, compared with never/rarely/sometimes, was associated with a 39% decreased risk of dementia (95% CI = 0.45,0.82, p = 0.001), and a 17% decreased risk of CIND (95% CI = 0.74, 0.92, p = 0.001).
- Playing an instrument (often/always) was associated with a 35% decreased dementia risk only (95% CI = 0.42,0.99, p = 0.047).
- Participants who both listened to and played music had a 33% decreased dementia risk (95% CI = 0.51,0.89, p = 0.006) and a 22% decreased CIND risk (95% CI = 0.65,0.92, p = 0.004).
- Always listening to music was associated with better global cognition and memory over time (p < 0.001, p = 0.004, respectively), but not the other cognitive domains.
- Engagement in music-related activities was not associated with changes in subjective cognitive wellbeing. In general, findings were stronger in individuals with over 16 years of education.
Conclusion
- These results highlight music as a potential promising, accessible strategy to help reduce cognitive impairment and delay the onset of dementia in later life.
Reference:
- Jaffa E, Wu Z, Owen A, Phyo AAZ, Woods RL, Orchard SG, T-J Chong T, Shah RC, Murray A, Ryan J. What Is the Association Between Music-Related Leisure Activities and Dementia Risk? A Cohort Study. Int J Geriatr Psychiatry. 2025 Oct;40(10):e70163. doi: 10.1002/gps.70163. PMID: 41088732.
Study: Topological turning points across the human lifespan edit
Structural topology develops non-linearly across the lifespan and is strongly related to cognitive trajectories. We gathered diffusion imaging from datasets with a collective age range of zero to 90 years old (N=4,216). We analyzed how 12 graph theory metrics of organization change with age and projected these data into manifold spaces using Uniform Manifold Projection and Approximation. With these manifolds, we identified four major topological turning points across the lifespan – around nine, 32, 66, and 83 years old. These ages defined five major epochs of topological development, each with distinctive age-related changes in topology. These lifespan epochs each have a distinct direction of topological development and specific changes in the organizational properties driving the age-topology relationship. This study underscores the complex, non-linear nature of human development, with unique phases of topological maturation, which can only be illuminated with a multivariate, lifespan, population-level perspective.
Reference:
- Mousley, A., Bethlehem, R.A.I., Yeh, FC. et al. Topological turning points across the human lifespan. Nat Commun 16, 10055 (2025). https://doi.org/10.1038/s41467-025-65974-8
Hematology/Oncology
Abnormal bleeding or bruising
Steps:
- Rule out trauma or medications
- Labs: CBC, peripheral blood smear, PT, PTT, renal and liver function tests
- If abnormal platelet shape/size and no specific disorder evident -> Heme referral for light transmission aggregometry
- If abnoramlly low platelet count -> Thrombocytopenia
- If normal PT and normal PTT ->
- Order Factor VIII, von Willebrand factor Ag, von Willenbrand factor activity
- If all normal -> Heme referral for light transmission aggregometry
- If abnormal -> von Willebrand disease
- If normal PT and abnormal PTT ->
- Order PTT mixing study
- If it corrects ->
- Order Factor VIII, IX, XI assays - If VIII is low check von Willebrand labs
- If it does not correct ->
- Lupus anticoagulant and Factor VIII inhibitor
- If abnormal PT and normal PTT ->
- Give vit K ->
- If corrects - Malnutrition
- If it does not correct - Factor VII assay
- Give vit K ->
- If normal PT and abnormal PTT ->
- Order LFTs, Fibrinoge, Consider factor assays
- Liver disease, Disseminated intravascular coagulation, Factor deficiency
- Order LFTs, Fibrinoge, Consider factor assays
References:
- AFP Vol 93 No 4 Feb 2016
Anemia
Microcytic Anemia
- Ferritin <30ng/mL
- Fe Def likely -> treat and recheck -> If no improvement check for other causes, ongoing loss, or compliance
- Ferritin >30ng/mL
- If suspect anemia of chronic disease and Ferritin >70ng/mL -> treat underlying cause
- If suspect anemia of chronic disease and Ferritin <70ng/mL -> consider concominant Fe def
- CRP high -> treat for Fe def anemia
- CRP low -> unlikely Fe def - treat as ACD
- If suspect thalassemia -> electropheresis
References:
- Consultant p838 Nov 2014
Macrocytic Anemia
Causes:
- Megaloblastic anemia
- Folate deficiency
- B12 deficiency
- Nonmegaloblastic anemia
- Bone marrow disorders
- Hepatic dysfunction
- Infection
- Thyroid dysfunction
Reference:
- Dec 2024 Vol 110 No 6
CBC with differential
- Red blood cells (RBCs)
- White blood cells (WBCs)
- Neutrophils (bacterial/fungal infections)
- Lymphocytes - produce antibodies against bacteria, viruses, and other invaders
- Infection, including bacterial, viral or other type of infection.
- Cancer of the blood or lymphatic system.
- An autoimmune disease causing ongoing, called chronic, swelling and irritation, called inflammation.
- Monocytes (viral infections) - isolate and clean up microorganisms
- Prolonged stress can cause monocytosis.
- May be a biomarker for depression and other mental health conditions
- Eosinophils (allergies/parasites)
- Basophils - secrete chemicals to help mediate the body's response to allergies and infectious agents.
- Platelets
Eosinophilia
| Class | Examples |
|---|---|
| Antibiotics | PCN, cephalosporins, tetracycline |
| NSAIDs | ASA, ibuprofen |
| Antiepileptic agents | Phenytoin, carbamazepine |
| Antihypertensive | HCTZ |
| Other | Ranitidine, allopurinol, sulfasalazine, cyclosporine, nevirapine |
Reference:
- JFP Vol 65 No 10 Oct 2016
Leukocytosis
If elevated:
- Basophils
- Allergic conditions
- Leukemias
- Eosinophils
- Allergic conditions
- Dermatologic conditions
- Eosinophilic esophagitis
- Idiopathic hypereosinophilic syndrome
- Malignancies
- Medication reactions
- Parasitic infections
- Lymphocytes
- Acute/chronic leukemia
- Hypersensitivity reaction
- Infections (viral, pertussis)
- Monocytes
- Autoimmune disease
- Infections (EBV, fungal, protozoan, rickettsial, tuberculosis)
- Splenectomy
- Neutrophils
- Bone marrow stimulation
- Chronic inflammation
- Congenital infection
- Medication induced
- Reactive
- Splenectomy
References:
- AFP Vol 92 No 11 Dec 2015
Leukemia
| Subtype | Description | Groups affected | Common features | 5yr survival rates by age |
|---|---|---|---|---|
| Acute lymphoblastic leukemia | >20% lymphoblasts on bone marrow | Children and young adults (60% <20yo) | Symptoms: easy bruising or bleeding, fatigue, fever, joint pain, pallor | <20: 87% |
| Signs: hepatosplenomegaly and lymphadenopathy | 50-64: 30% | |||
| >=65: 15% | ||||
| Acute Myelopgenous leukemia | >20% myeloblasts on peripheral blood smear or bone marrow | Adultes (Median Dx 68yo) | Symptoms: CNS palsies, fever, pallor, thrombocytopenia | <50: 55% |
| Auer rods on peripheral smear | Signs: flow murmur, hepatosplenomegaly, lymphadenopathy | 50-64: 30% | ||
| >=65: 7% | ||||
| Chronic Lymphocytic Leukemia | >=5000 per mcl monoclonal B lymphocytes on blood smear | Older adults (70% Dx >65 yo) | Asymptomatic (70%) | <50: 93% |
| Hepatosplenomegaly and lymphadenopathy | 50-64: 91% | |||
| >=65: 80% | ||||
| Chronic Myelogenous Leukemia | Philadelphia chromosome (BCR-ABL1 fusion gene) | Adults | Asymptomatic (50%) | <50: 86% |
| Splenomegaly (46-76%) | 50-64: 77% | |||
| >=65: 42% |
Reference:
- AFP Vol 107 No 4 Apr 2023
False A1c Readings
Falsely lower A1c:
- Acute blood loss
- Chronic liver disease
- Hemodialysis
- Antiretroviral therapy
- Pregnancy
- Vitamins E and C
Lower or Elevate A1c:
- Hemoglobinopathies or hemoglobin variants
- Malnutrition
Falsely elevate A1c:
- Aplastic anemias
- Hyperbilirubinemia
- Hypertrglyceridemia
- Fe Deficiency anemias
- Renal failure
- Splenectomy
References:
- AFP Vol 93 No 2 Jan 2016
A different view:
| Factor | False lower | False Elevated |
|---|---|---|
| Erythrocyte life span | Hemolytic anemia | Splenectomy |
| Recent blood transfusion | ||
| Splenomegaly | ||
| Erythropoiesis | Reticulocytosis | Fe/B12 deficiency |
| Erythropoitin | ||
| Assay interference | Severe hypertriglyceridemia | Chronic alcoholism |
| Glycation | High dose Vit C or E | Chronic Kidney Disease |
References:
- JAMA Vol 315, No 6 Feb 2016
Gastric Cancer
Risk Factors:
- First degree relative with gastric cancer
- RR=2.71 (2.08-3.53)
- Helicobacter pylori infection
- OR=2.56 (2.18-3.00)
- Pernicious anemia
- OR=2.18 (1.94-2.45)
- Obesity
- RR=1.93 (1.52-2.45)
- Smoking
- OR=1.61 (1.49-1.75)
- High salt intake
- OR=1.55 (1.45-1.64)
- Alcohol consumption
- OR=1.20 (1.12-1.27)
Protective Factors:
- Mediterranean diet
- OR=0.43 (0.29-0.63)
- Fruit intake >2 times per week
- OR=0.48 (0.37-0.63)
- Vegetable intake >2 times per week
- OR=0.62 (0.49-0.79)
| SEER Stage | Definition | 5-yr survival, % (95% CI) |
|---|---|---|
| Localized | No evidence that cancer has spread outside of the stomach. | 75 (74-79) |
| Regional | Cancer has spread to nearby organs or lymph nodes. | 37 (35-40) |
| Distant | Cancer has spread beyond nearby structures. | 6.5 (5.6-7.6) |
| Unstaged | Not applicable. | 32 (29-36) |
Reference:
- AFP Vol 111 No 2 Feb 2025
Hemoglobin C Disease edit
Hemoglobin analysis reveals three different patterns of normal hemoglobin in an adult. These are Hb A (95 to 98%) containing two alpha and two beta chains, Hb A2 (2% to 3%) containing two alpha and two delta chains, and Hb F (less than 1%) containing two alpha and two gamma chains.
Hemoglobin C (Hb C), on the other hand, is one of the common structural variants of normal hemoglobin in which lysine is substituted for the glutamate in the sixth position of the beta-globin chain making it less soluble than Hb A. Hemoglobin C can either be in the homozygous states (Hb CC) or in the heterozygous states (Hb SC, Hb AC). Persons with hemoglobin C trait (Hb AC) are phenotypically normal and generally do not show any symptoms while persons with hemoglobin C disease (Hb CC) may present with mild chronic hemolysis, splenomegaly, and jaundice.
As with chronic hemolysis, body stores of folic acid can get depleted; thus, folic acid is indicated, which helps produce new red cells and improve the symptoms of anemia. Despite splenomegaly, the splenic function remains normal, and hence long-term antibiotic prophylaxis is not indicated.
Overall people with hemoglobin C have normal growth and development and a normal life expectancy.
From:
- Karna B, Jha SK, Al Zaabi E. Hemoglobin C Disease. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559043/
Iron (Fe) Deficiency Anemia
- Serum ferritin is the most reliable single test for diagnosing iron deficiency, with levels <15 ng/mL being highly specific; levels <30 ng/mL suggest deficiency, while levels >100 ng/mL make deficiency unlikely, especially in inflammatory conditions.
- Serum iron is typically low, but its measurement is unreliable due to daily fluctuations and influences from oral iron intake or inflammation.
- Total iron-binding capacity (TIBC) is usually elevated, and transferrin saturation is decreased, though both can be affected by inflammation, aging, or poor nutrition.
- Mean corpuscular volume (MCV) is often less than 80 fL, indicating microcytosis, but this is a late finding; normocytic anemia can occur in early or mild iron deficiency.
- Red cell distribution width (RDW) is frequently increased, reflecting anisocytosis and can be an early indicator of iron deficiency before MCV changes.
- The anemia of iron deficiency is classically microcytic and hypochromic, but these findings are not specific, as thalassemia and anemia of chronic disease can present similarly.
| Lab | Notes |
|---|---|
| Ferritin | <15 |
| Serum Fe | Typically low |
| TIBC | Elevated |
| Transferrin | Decreased |
| MCV | <80 |
| RDW | Increased |
| Hb | Low |
Lung Cancer Screening
Screen those over age 50 with 20-pack-year history of smoking, using low-dose CT scannign
- Expected to reduce annual mortality from lung cancer by additional 3% or more (from 9.8% to 13%)
References:
- JFP Vol 70 No 7 Sep 2021
- USPSTF
Lymphadenopathy Causes
MAGIC Causes
- M - Malignancy (lymphoma [Hodkin vs non-Hodkin], solid organ cancers, acute and chronic leukemia, Waldenstrom macroglobulinemia, metastatic spread), systemic mastocytosis
- A - Allergic alveiolitis (hypersensitivity pneumonitis), autoimmune diseases
- G - Granulomatous diseases (sarcoidosis, Wegner granulomatosis, berylliosis)
- I - Infection (bacterial [tuberculosis, melioidosis, cat-scratch disease], viral [HIV, Epstein-Barr virus], fungal [coccidioidomycosis, histoplasmosis], parasitic, mycobacterial, atypical bacterial), Iatrogenic (drug-induced lymphadenopathy)
- C - COPD including bronchiectasis; Congestive heart failure, other chronic diseases leading to reactive lymphadenopathy
Laboratory Studies to Consider by Possible Etiology:
- Autoimmune diseases
- Anti-cyclic citrullinated peptide antibody
- Antinuclear antibody
- Complement levels
- C-reactive protein level
- Double-stranded DNA antibodies
- ESR
- RF
- Infectious diseases
- Chlamydia and gonococcal PCR
- CBC with dif
- Cytomegalovirus PCR
- Hepatitis B surface antigen
- HIV-1/HIV-2
- Quantiferon-TB
- Mononucleosis spot test and EBV serrology
- Purified protein derivative skin test
- Throat swab and culture
- Treponemal antibody
Reference:
- Consultant Nov 2016
- AFP Sep 2025 Vol 112 No 3
Silicone Lymphadenopathy (Siliconoma)
Silicone implants are associated with axillary lymphadenopathy primarily due to the migration of silicone particles from the implant to the regional lymph nodes. This phenomenon, known as silicone lymphadenopathy or siliconoma, can occur due to silicone bleed, leak, or rupture of the implant.
A retrospective study conducted at the Shamir-Assaf Harofeh Medical Center found that the incidence of siliconomas was 13.6% among women with silicone implants. Key risk factors included older age, older implant age, ruptured implants, subpectoral placement, severe capsular contracture, and the use of specific implant brands such as Mentor and Poly Implant Prothèse (PIP).
Histologically, silicone lymphadenopathy is characterized by the presence of foamy macrophages and refractile silicone material within the lymph nodes. This was confirmed in a study using laser-Raman microprobe spectroscopy and Fourier transform infrared microspectroscopy, which identified silicone in the lymph nodes of patients with breast implants.
Clinically, patients with silicone lymphadenopathy may present with painless or painful lymphadenopathy. The axillary region is the most commonly affected area, followed by internal mammary, cervical/supraclavicular, and mediastinal regions.[3] Imaging modalities such as ultrasonography (US) and magnetic resonance imaging (MRI) are used for diagnosis. The "snowstorm" appearance on US is particularly sensitive for detecting silicone within lymph nodes.
The American College of Radiology (ACR) recommends that unexplained axillary adenopathy in patients with silicone implants be evaluated initially with mammography or US, with US being particularly useful for diagnosing silicone adenitis. In summary, silicone implants can lead to axillary lymphadenopathy due to silicone migration, especially in cases of implant rupture or other risk factors. Diagnosis is primarily through imaging and histological examination, with management tailored to the patient's clinical presentation.
For the evaluation of axillary lymphadenopathy in patients with silicone implants, the American College of Radiology (ACR) recommends initial imaging with ultrasound (US) and/or mammography, depending on the patient's age and clinical presentation.
Ultrasound is particularly useful for diagnosing silicone lymphadenopathy, as it can identify the characteristic "snowstorm" appearance of silicone within lymph nodes, which is highly sensitive and specific for this condition.[3] Mammography can also detect silicone within low axillary nodes and is often used in conjunction with US for a comprehensive evaluation.
If the initial imaging is inconclusive or if there is a high clinical suspicion of other pathologies, further evaluation with magnetic resonance imaging (MRI) may be considered. However, MRI is generally less sensitive than US for detecting silicone lymphadenopathy.
In cases where imaging findings are suspicious or highly suggestive of malignancy, a core needle biopsy of the lymph nodes is recommended to confirm the diagnosis and rule out other conditions such as metastatic disease or lymphoma.
In summary, the recommended diagnostic tests for axillary lymphadenopathy in patients with silicone implants include:
- Ultrasound (US): First-line imaging to identify the "snowstorm" sign of silicone lymphadenopathy.
- Mammography: Complementary to US, especially useful for detecting silicone in low axillary nodes.
- Magnetic Resonance Imaging (MRI): Considered if initial imaging is inconclusive or further confirmation is needed.
- Core Needle Biopsy: Recommended for suspicious or highly suggestive imaging findings to confirm the diagnosis and rule out malignancy.
Reference:
- These recommendations are based on guidelines from the American College of Radiology (ACR) and supported by clinical studies
- OpenEvidence Search
Meat Consumption and Cancer edit
IARC/WHO does not assess the size of risk
- The International Agency for Cancer Research (IARC) used clearly defined guidelines to identify hazards (qualitative evaluation), i.e. whether an agent can cause cancer, but IARC does not assess level or the magnitude of risk (quantative assessment).
- In other words, the IARC/WHO evaluates the evidence not risk.
- As stated by the Director of IARC Christopher Wild, "The IARC evaluations are important in enabling governments and international regulatory agencies to conduct risk assessments, in order to balance the risks and benefits of eating red meat and processed meat and to provide the best possible dietary recommendations."
- As an example, the US Dietary Guidelines Committee issued a review of diet and health earlier this year; among the conclusions was that consumption of red meat should be low for both human and planet health.
Smoking vs. high consumption of processed meat
- Even though smoking is in the same category as processed meat (Group 1 carcinogen), the magnitude or level of risk associated with smoking is considerably higher (e.g., for lung cancer about 20 fold or 2000% increased risk) from those associated with processed meat – an analysis of data from 10 studies, cited in the IARC report showed an 18 percent increased risk in colorectal cancer per 50g processed meat increase per day.
- To put this in perspective, according to the Global Disease Burden Project 2012:
- over 34,000 cancer deaths per year worldwide are attributable to high processed meat intake
- 1 million deaths per year attributable to tobacco smoke
High consumption of red or processed meat also increases risk of other chronic diseases and mortality
- It is important to keep in mind that the above estimates pertain to cancer deaths only. It is well known that besides increasing the risk of some cancers, high red and processed meat intake can also increase risk of other chronic and potentially life threatening diseases such as coronary heart disease, stroke and type II diabetes compared to other protein sources such as poultry, legumes and fish.
- According to 2013 data from the Global Burden of Disease Project, the number of total deaths (including deaths from cardiovascular disease or diabetes and colorectal cancers) attributable to a diet high in processed meat was 644,000.
The media has reported that 50g/day consumption of processed meat can risk for colorectal cancer from an average 5 percent lifetime risk to 6 percent. This does not sound like much of an increase in risk.
- 50g processed meat is equivalent to about 6 slices of bacon or one hot dog.
- The 5 percent to 6 percent increase in risk of colorectal cancer reported in the media is a population average, but this estimate does not take into account that for certain subgroups (e.g., those who are also obese, are physically inactive or consume diets high in sugar, saturated fat etc., or are more genetically susceptible) the absolute risk can be higher
Reference:
Unprocessed Red Meat and Processed Meat Consumption: Dietary Guideline Recommendations From the Nutritional Recommendations (NutriRECS) Consortium edit
Description:
- Dietary guideline recommendations require consideration of the certainty in the evidence, the magnitude of potential benefits and harms, and explicit consideration of people's values and preferences. A set of recommendations on red meat and processed meat consumption was developed on the basis of 5 de novo systematic reviews that considered all of these issues.
Methods:
- The recommendations were developed by using the Nutritional Recommendations (NutriRECS) guideline development process, which includes rigorous systematic review methodology, and GRADE methods to rate the certainty of evidence for each outcome and to move from evidence to recommendations. A panel of 14 members, including 3 community members, from 7 countries voted on the final recommendations. Strict criteria limited the conflicts of interest among panel members. Considerations of environmental impact or animal welfare did not bear on the recommendations. Four systematic reviews addressed the health effects associated with red meat and processed meat consumption, and 1 systematic review addressed people's health-related values and preferences regarding meat consumption.
Recommendations:
- The panel suggests that adults continue current unprocessed red meat consumption (weak recommendation, low-certainty evidence). Similarly, the panel suggests adults continue current processed meat consumption (weak recommendation, low-certainty evidence).
Points:
- Dose– response meta-analysis results from 23 cohort studies with 1.4 million participants provided low- to very low- certainty evidence that decreasing unprocessed red meat intake may result in a very small reduction in the risk for major cardiovascular outcomes (cardiovascular disease, stroke, and myocardial infarction) and type 2 diabetes (range, 1 fewer to 6 fewer events per 1000 persons with a decrease of 3 servings/wk), with no statistically significant differences in 2 additional outcomes (all-cause mortality and cardiovascular mortality)
- Dose–response meta-analysis results from 17 cohorts with 2.2 million participants provided low-certainty evidence that decreasing unprocessed red meat intake may result in a very small reduction of overall lifetime cancer mortal- ity (7 fewer events per 1000 persons with a decrease of 3 servings/wk), with no statistically significant differences for 8 additional cancer outcomes (prostate cancer mortality and the incidence of overall, breast, colorectal, esopha- geal, gastric, pancreatic, and prostate cancer)
- In terms of how to interpret our weak recommendation, it indicates that the panel believed that for the majority of individuals, the desirable effects (a potential lowered risk for cancer and cardiometabolic outcomes) associated with reducing meat consumption probably do not outweigh the undesirable effects (impact on quality of life, burden of modifying cultural and per- sonal meal preparation and eating habits). The weak recommendation reflects the panel's awareness that values and preferences differ widely, and that as a re- sult, a minority of fully informed individuals will choose to reduce meat consumption.
| Outcome | Unprocessed Red Meat | Processed Meat | Dietary Patterns | |||
|---|---|---|---|---|---|---|
| Risk Difference | Certainty of Evidence | Risk Difference | Certainty of Evidence | Risk Difference | Certainty of Evidence | |
| Cardiovascular mortality | 4 fewer per 1000 persons (from 5 fewer to 4 fewer) over 10.8 y | Very low | 4 fewer per 1000 persons (from 7 fewer to 1 fewer) over 10.8 y | Very low | 6 fewer per 1000 persons (from 9 fewer to 2 fewer) over 10.8 y | Very low |
| Type 2 diabetes | 6 fewer per 1000 persons (from 7 fewer to 4 fewer) over 10.8 y | Low | 12 fewer per 1000 persons (from 16 fewer to 9 fewer) over 10.8 y | Very low | 14 fewer per 1000 persons (from 18 fewer to 8 fewer) over 10.8 y | Very low |
| Overall cancer mortality | 7 fewer per 1000 persons (from 9 fewer to 6 fewer) over lifetime | Low | 8 fewer per 1000 persons (from 12 fewer to 6 fewer) over lifetime | Low | 12 fewer per 1000 persons (from 18 fewer to 4 fewer) over lifetime | Very low |
Reference:
- Johnston BC, Zeraatkar D, Han MA, Vernooij RWM, Valli C, El Dib R, Marshall C, Stover PJ, Fairweather-Taitt S, Wójcik G, Bhatia F, de Souza R, Brotons C, Meerpohl JJ, Patel CJ, Djulbegovic B, Alonso-Coello P, Bala MM, Guyatt GH. Unprocessed Red Meat and Processed Meat Consumption: Dietary Guideline Recommendations From the Nutritional Recommendations (NutriRECS) Consortium. Ann Intern Med. 2019 Nov 19;171(10):756-764. doi: 10.7326/M19-1621. Epub 2019 Oct 1. PMID: 31569235.
- https://www.acpjournals.org/doi/suppl/10.7326/M19-1621/suppl_file/AIME201911190-M191621-v1.pdf
Consumption of red meat and processed meat and cancer incidence: a systematic review and meta-analysis of prospective studies edit
Red meat and processed meat consumption has been hypothesized to increase risk of cancer, but the evidence is inconsistent.
We performed a systematic review and meta-analysis of prospective studies to summarize the evidence of associations between consumption of red meat (unprocessed), processed meat, and total red and processed meat with the incidence of various cancer types. We searched in MEDLINE and EMBASE databases through December 2020. Using a random-effect meta-analysis, we calculated the pooled relative risk (RR) and 95% confidence intervals (CI) of the highest versus the lowest category of red meat, processed meat, and total red and processed meat consumption in relation to incidence of various cancers. We identified 148 published articles.
Results:
- Red meat consumption was significantly associated with greater risk of:
- Breast cancer (RR = 1.09; 95% CI = 1.03-1.15)
- Endometrial cancer (RR = 1.25; 95% CI = 1.01-1.56)
- Colorectal cancer (RR = 1.10; 95% CI = 1.03-1.17)
- Colon cancer (RR = 1.17; 95% CI = 1.09-1.25)
- Rectal cancer (RR = 1.22; 95% CI = 1.01-1.46)
- Lung cancer (RR = 1.26; 95% CI = 1.09-1.44)
- Hepatocellular carcinoma (RR = 1.22; 95% CI = 1.01-1.46)
- Processed meat consumption was significantly associated with:
- A 6% greater breast cancer risk
- An 18% greater colorectal cancer risk
- A 21% greater colon cancer risk
- A 22% greater rectal cancer risk
- A 12% greater lung cancer risk
- Total red and processed meat consumption was significantly associated with greater risk of:
- Colorectal cancer (RR = 1.17; 95% CI = 1.08-1.26)
- Colon cancer (RR = 1.21; 95% CI = 1.09-1.34)
- Rectal cancer (RR = 1.26; 95% CI = 1.09-1.45)
- Lung cancer (RR = 1.20; 95% CI = 1.09-1.33)
- Renal cell cancer (RR = 1.19; 95% CI = 1.04-1.37)
My notes:
- See also: Lifetime Risk of Developing or Dying From Cancer
- For example: RR increase for colon cancer from total red and processed meat consumption (RR = 1.21) for a male with a baseline risk of 4.3% (or 1 in 23) is:
- 4.3*1.21 = 5.02%.
- Absolute risk increase is 0.7% to develop colon cancer
- For example: RR increase for colon cancer from total red and processed meat consumption (RR = 1.21) for a male with a baseline risk of 4.3% (or 1 in 23) is:
Conclusion:
- This comprehensive systematic review and meta-analysis study showed that high red meat intake was positively associated with risk of breast cancer, endometrial cancer, colorectal cancer, colon cancer, rectal cancer, lung cancer, and hepatocellular carcinoma
- High processed meat intake was positively associated with risk of breast, colorectal, colon, rectal, and lung cancers.
- Higher risk of colorectal, colon, rectal, lung, and renal cell cancers were also observed with high total red and processed meat consumption.
Reference:
- Farvid MS, Sidahmed E, Spence ND, Mante Angua K, Rosner BA, Barnett JB. Consumption of red meat and processed meat and cancer incidence: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol. 2021 Sep;36(9):937-951. doi: 10.1007/s10654-021-00741-9. Epub 2021 Aug 29. PMID: 34455534.
- https://pubmed.ncbi.nlm.nih.gov/34455534/
Lifetime Risk of Developing or Dying From Cancer
| Risk of developing | Risk of dying from | |||
|---|---|---|---|---|
| Males | % | 1 in | % | 1 in |
| Any cancer | 40.9 | 2 | 20.2 | 5 |
| Bladder (includes in situ) | 3.86 | 28 | 0.9 | 111 |
| Brain and nervous system | 0.7 | 147 | 0.5 | 189 |
| Breast | 0.1 | 727 | <0.1 | 3312 |
| Colon and rectum | 4.3 | 23 | 1.7 | 578 |
| Esophagus | 0.8 | 128 | 0.7 | 138 |
| Hodgkin lymphoma | 0.2 | 435 | <0.1 | 2899 |
| Kidney and renal pelvis | 2.3 | 44 | 0.6 | 177 |
| Larynx (voice box) | 0.5 | 200 | 0.2 | 570 |
| Leukemia | 1.8 | 55 | 0.9 | 108 |
| Liver and bile duct | 1.5 | 66 | 1 | 96 |
| Lung and bronchus | 6.2 | 16 | 4.7 | 21 |
| Melanoma of the skin* | 3.5 | 28 | 0.4 | 240 |
| Multiple myeloma | 0.9 | 106 | 0.5 | 219 |
| Non-Hodgkin lymphoma | 2.3 | 43 | 0.8 | 128 |
| Oral cavity and pharynx (mouth and throat) | 1.7 | 60 | 0.4 | 240 |
| Pancreas | 1.7 | 59 | 1.4 | 71 |
| Prostate | 12.6 | 8 | 2.4 | 41 |
| Stomach | 1 | 102 | 0.4 | 246 |
| Testicles | 0.4 | 246 | <0.1 | 4966 |
| Thyroid | 0.6 | 155 | 0.1 | 1706 |
| Risk of developing | Risk of dying from | |||
| Females | % | 1 in | % | 1 in |
| Any cancer | 39.1 | 3 | 17.7 | 6 |
| Bladder (includes in situ) | 1.1 | 91 | 0.3 | 294 |
| Brain and nervous system | 0.5 | 188 | 0.4 | 241 |
| Breast | 12.9 | 8 | 2.5 | 39 |
| Cervix | 0.7 | 153 | 0.2 | 466 |
| Colon and rectum | 3.9 | 26 | 1.6 | 63 |
| Esophagus | 0.2 | 439 | 0.2 | 524 |
| Hodgkin lymphoma | 0.2 | 532 | <0.1 | 3819 |
| Kidney and renal pelvis | 1.3 | 75 | 0.3 | 316 |
| Larynx (voice box) | 0.1 | 852 | <0.1 | 2346 |
| Leukemia | 1.3 | 78 | 0.7 | 152 |
| Liver and bile duct | 0.7 | 146 | 0.6 | 181 |
| Lung and bronchus | 5.8 | 17 | 4 | 25 |
| Melanoma of the skin* | 2.4 | 41 | 0.2 | 465 |
| Multiple myeloma | 0.7 | 134 | 0.4 | 275 |
| Non-Hodgkin lymphoma | 1.9 | 53 | 0.6 | 167 |
| Oral cavity and pharynx (mouth and throat) | 0.7 | 141 | 0.2 | 537 |
| Ovary | 1.1 | 88 | 0.8 | 123 |
| Pancreas | 1.6 | 61 | 1.4 | 73 |
| Stomach | 0.6 | 157 | 0.3 | 359 |
| Thyroid | 1.7 | 59 | 0.1 | 1440 |
| Uterus | 3.1 | 33 | 0.7 | 152 |
Reference:
Multiple Myeloma
Diagnostic Tests:
- Initial tests
- CBC
- Serum albumin, calcium, creatinine, BUN, electrolytes
- Confirmatory tests
- 24-hr urine protein
- Beta2-microglobulin
- Lactate dehydrogenase
- Serum free light chain assay
- Serum immunofixation electrophoresis
- Serum protein electrophoresis (http://www.aafp.org/afp/2005/0101/p105.html)
- Serum quantitative immunoglobulins
- Skeletal survey
- Urine immunofixation electrophoresis
- Urine protein electrophoresis
- Test by oncology consultants
- Bone marrow aspirate and biopsy with cytogenetics, flow cytometry, fluorescence in situ hybridization, and/or immunohistochemistry
- Tests for special circumstances
- Bone densitometry
- PET/CT or whole-body MRI
- Serum viscosity
- Tissue biopsy of bony or other lesion
Findings on presentation:
- Anemia (Hg<12g/dl) (73% of patients)
- Bone pain (58% of patients)
- Elevated creatinine (>1.3mg/dL) (48% of patients)
- Fatigue or generalized weakness (32% of patients)
- Hypercalcemia (Ca >10.1 mg/dL) (28% of patients)
- Weight loss (24% of patients)
References:
- AFP Vol 95, No 6 Mar 2017
Neutropenia
| Suspected etiology | Laboratory testing | Clinical context |
|---|---|---|
| Autoimmune neutropenia | CBC with differential; Antineutrophil antibodies | Consider in patients with signs or symptoms of chronic systemic illness or history of recurrent infections |
| Cyclic neutropenia | CBC with differential | Evaluate for other cytopenias and review past CBCs; If cyclic neutropenia is a concern, serial CBCs should be performed two times per week for at least 6 weeks to document two nadirs with return-to-normal neutrophil counts in between |
| Hematologic malignancy | Peripheral blood smear | Evaluate for immature or abnormal neutrophils or leukocytes |
| Infection | Viral serology | Concern for HIV, hepatitis B or C, Epstein-Barr virus, cytomegalovirus, or influenza |
| Nutritional deficiency | Vitamin B12, folate, copper | Alcoholism, growth faltering, malabsorption syndromes, history of bariatric surgery, concern for megaloblastic anemia |
| Rheumatoid arthritis | C-reactive protein, rheumatoid factor, anti-cyclic citrullinated peptide antibody | Criteria used in diagnosis of rheumatoid arthritis; Consider secondary autoimmune neutropenia |
| Sjogren syndrome | Antinuclear, anti-SS-A (Ro), and anti-SS-B (La) antibodies; rheumatoid factor | Antibodies to anti-SS-A and anti-SS-B antigens are used in the Revised International Classification Criteria for Sjogren syndrome; Consider secondary autoimmune neutropenia |
| Systemic lupus erythematosus | Antinuclear antibody; anti-dsDNA, anti-Smith, anti- cardiolipin antibodies | Laboratory criteria used in the diagnosis of systemic lupus erythematosus; Consider secondary autoimmune neutropenia |
| Presentation | Evaluation |
|---|---|
| All patients | Complete blood cell count, blood cultures, lactic acid, comprehensive |
| metabolic panel | |
| Abdominal pain, nausea, vomiting, diarrhea | Abdomen and pelvis CT with contrast |
| Cough, shortness of breath, wheezing, rhonchi | Chest radiography, sputum cultures |
| Erythema, fluctuance, tender soft tissue | Ultrasonography or CT to evaluate for abscess |
| Neurologic deficits, headache, photophobia, encephalopathy, seizures | Lumbar puncture, head CT without contrast, brain magnetic resonance; imaging with and without contrast |
| Urinary symptoms, flank pain, suprapubic pain | Urinalysis with culture |
Reference:
- Am Fam Physician. 2025;112(6):618-628
Peripheral Lymphadenopathy (LAP) edit
Use acronym "CHICAGO" to consider all causes
- C - Cancers:
- Hematologic malignancies: Hodgkin's disease, Non-Hodgkin's lymphoma, Leukemia
- Metastatic: Breast tumor, Lung, Kidney, others
- H - Hypersensitivity syndromes: Serum sickness, Drugs
- I - Infections: Viral (Epstein-Barr virus, cytomegalovirus, HIV), Bacterial (TB,) Fungal, Protozoan, Rickettsial (Typhus), Helminthes
- C - Connective Tissue disorders: Systemic lupus erythematosus, Rheumatoid arthritis, Dermatomyositis
- A - Atypical lymphoproliferative disorders: Castleman's Disease, Wegener
- G - Granulomatous: Histoplasmosis, Mycobacterial infections, Cryptococcus, Berylliosis, Cat scratch disease, Silicosis
- O - Others
Labs:
- If more work-up is needed, the first step is to obtain complete blood count (CBC).
- If autoimmune diseases are suspected, CBC, antinuclear antibody, dsDNA antibody, ESR, and rheumatoid factor and complement level should be checked
Imaging:
- Ultrasonography is a useful imaging tool in the assessment of the number, size, site, shape, margins, and internal structure in patients with peripheral LAP
- A normal or reactive node is usually oval with a hilum, whereas metastatic and lymphomatous lymph nodes generally emerge as round lesions.
- A low long axis to short axis of lymph nodes (L/S ratio) is a significant sign of lymphoma and metastatic cancer
- L/S ratio less than 2 was indicative of metastatic lymph nodes with 95% accuracy
- A normal or reactive node is usually oval with a hilum, whereas metastatic and lymphomatous lymph nodes generally emerge as round lesions.
- CT scan and magnetic resonance imaging (MRI) are more useful in the evaluation of the thoracic and abdominopelvic cavity and their accuracy mainly depends on the size of the lymph nodes
| Shape | Border | L/s Ratio* | Internal Echogenicity | Hilum | RI** | PI*** | Blood Flow Distribution | |
|---|---|---|---|---|---|---|---|---|
| Benign Disorders | ovoid | various | High>2 | Isoechoic | Present-Normal | Low<0.8 | <1.5 | Hilar |
| Neoplastic Disorders | Round | sharp† | Low<2 | Hypoechoic | Absent | High> 0.8 | >1.5 | Peripheral or miscellaneous |
*Long axis to short axis (L/S); **Resistive index (RI); ***Pulsatility index (PI); †In matted lymph nodes, the border is not sharp. The data of the table are derived from references cited in the text.
Notes:
- Lymph nodes are generally considered abnormal if their diameter exceeds 1 cm.
- The cervical region is the most frequent site involved in peripheral LAP at any age.
- Generalized LAP usually is indicative of an underlying disease. Some important causes include the Epstein-Barr virus, HIV, lymphoma, and autoimmune disorders.
- Ultrasound can assess the number, size, site, shape, margins, and pattern of vascularity and the internal structure of a lymph node.
- FNAC is more powerful in diagnosing metastatic cancers than lymphomas. Ultrasonography-guided FNAC offers more accurate information than does blinded FNAC.
- Needle biopsy can be used as the first step in the diagnostic approach to lymphomas, but excisional biopsy of enlarged lymph nodes is still the gold standard procedure.
- Age more than 40 years, multiple sites of LAP, supraclavicular lymph nodes, nodal diameter greater than 2 cm, firm or hard texture, fixed nodes, lack of tenderness, and abnormal chest X-ray are factors that propel the physician into tissue sampling.
- If none of the predictive risks for malignancy is present, patients with peripheral LAP can be observed for 3 to 4 weeks before lymph node biopsy.
| Historical clues | Suggested diagnoses | Initial testing |
|---|---|---|
| Fever, night sweats, weight loss, or node located in supraclavicular, popliteal, or iliac region, bruising, splenomegaly | Leukemia, lymphoma, solid tumor metastasis | CBC, nodal biopsy or bone marrow biopsy; imaging with ultrasonography or computed tomography may be considered but should not delay referral for biopsy |
| Fever, chills, malaise, sore throat, nausea, vomiting, diarrhea; no other red flag symptoms | Bacterial or viral pharyngitis, hepatitis, influenza, mononucleosis, tuberculosis (if exposed), rubella | Limited illnesses may not require any additional testing; depending on clinical assessment, consider CBC, monospot test, liver function tests, cultures, and disease-specific serologies as needed |
| High-risk sexual behavior | Chancroid, HIV infection, lymphogranuloma venereum, syphilis | HIV-1/HIV-2 immunoassay, rapid plasma reagin, culture of lesions, nucleic acid amplification for chlamydia, migration inhibitory factor test |
| Animal or food contact | ||
| - Cats | Cat-scratch disease (Bartonella) | Serology and polymerase chain reaction |
| Toxoplasmosis | Serology | |
| - Rabbits, or sheep or cattle wool, hair, or hides | Anthrax | Per CDC guidelines |
| Brucellosis | Serology and polymerase chain reaction | |
| Tularemia | Blood culture and serology | |
| - Undercooked meat | Anthrax | Per CDC guidelines |
| Brucellosis | Serology and polymerase chain reaction | |
| Toxoplasmosis | Serology | |
| Recent travel, insect bites | Diagnoses based on endemic region | Serology and testing as indicated by suspected exposure |
| Arthralgias, rash, joint stiffness, fever, chills, muscle weakness | Rheumatoid arthritis, Sjögren syndrome, dermatomyositis, systemic lupus erythematosus | Antinuclear antibody, anti-doubled-stranded DNA, erythrocyte sedimentation rate, CBC, rheumatoid factor, creatine kinase, electromyography, or muscle biopsy as indicated |
Risk Factors for Malignancy
- Age older than 40 years
- Duration of lymphadenopathy greater than four to six weeks
- Generalized lymphadenopathy (two or more regions involved)
- Male sex
- Node not returned to baseline after eight to 12 weeks
- Supraclavicular location
- Systemic signs: fever, night sweats, weight loss, hepatosplenomegaly
- White race
| Location | Lymphatic drainage | Causes |
|---|---|---|
| Submandibular | Tongue, submaxillary gland, lips and mouth, conjunctivae | Infections of head, neck, sinuses, ears, eyes, scalp, pharynx |
| Submental | Lower lip, floor of mouth, tip of tongue, skin of cheek | Mononucleosis syndromes, Epstein-Barr virus, cytomegalovirus, toxoplasmosiss |
| Jugular | Tongue, tonsil, pinna, parotid | Pharyngitis organisms, rubella |
| Posterior cervical | Scalp and neck, skin of arms and pectorals, thorax, cervical and axillary nodes | Tuberculosis, lymphoma, head and neck malignancy |
| Suboccipital | Scalp and head | Local infection |
| Postauricular | External auditory meatus, pinna, scalp | Local infection |
| Preauricular | Eyelids and conjunctivae, temporal region, pinna | External auditory canal |
| Right supraclavicular node | Mediastinum, lungs, esophagus | Lung, retroperitoneal or gastrointestinal cancer |
| Left supraclavicular node | Thorax, abdomen via thoracic duct | Lymphoma, thoracic or retroperitoneal cancer, bacterial or fungal infection |
| Axillary | Arm, thoracic wall, breast | Infections, cat-scratch disease, lymphoma, breast cancer, silicone implants, brucellosis, melanoma |
| Epitrochlear | Ulnar aspect of forearm and hand | Infections, lymphoma, sarcoidosis, tularemia, secondary syphilis |
| Inguinal | Penis, scrotum, vulva, vagina, perineum, gluteal region, lower abdominal wall, lower anal canal | Infections of the leg or foot, STDs (e.g., herpes simplex virus, gonococcal infection, syphilis, chancroid, granuloma inguinale, lymphogranuloma venereum), lymphoma, pelvic malignancy, bubonic plague |
If lymph nodes are detected, note and describe:
- Size.
- Nodes are generally considered to be normal if they are up to 1 cm in diameter; however, some authors suggest that epitrochlear nodes larger than 0.5 cm or inguinal nodes larger than 1.5 cm should be considered abnormal.7,8 Little information exists to suggest that a specific diagnosis can be based on node size. However, in one series10 of 213 adults with unexplained lymphadenopathy, no patient with a lymph node smaller than 1 cm2 (1 cm × 1 cm) had cancer, while cancer was present in 8 percent of those with nodes from 1 cm2 to 2.25 cm2 (1 cm × 1 cm to 1.5 cm × 1.5 cm) in size, and in 38 percent of those with nodes larger than 2.25 cm2 (1.5 cm × 1.5 cm). In children, lymph nodes larger than 2 cm in diameter (along with an abnormal chest radiograph and the absence of ear, nose and throat symptoms) were predictive of granulomatous diseases (i.e., tuberculosis, cat-scratch disease or sarcoidosis) or cancer (predominantly lymphomas).
- Pain/Tenderness.
- When a lymph node rapidly increases in size, its capsule stretches and causes pain. Pain is usually the result of an inflammatory process or suppuration, but pain may also result from hemorrhage into the necrotic center of a malignant node. The presence or absence of tenderness does not reliably differentiate benign from malignant nodes.
- Consistency.
- Stony-hard nodes are typically a sign of cancer, usually metastatic. Very firm, rubbery nodes suggest lymphoma. Softer nodes are the result of infections or inflammatory conditions. Suppurant nodes may be fluctuant. The term "shotty" refers to small nodes that feel like buckshot under the skin, as found in the cervical nodes of children with viral illnesses.
- Matting.
- A group of nodes that feels connected and seems to move as a unit is said to be "matted." Nodes that are matted can be either benign (e.g., tuberculosis, sarcoidosis or lymphogranuloma venereum) or malignant (e.g., metastatic carcinoma or lymphomas).
- Location.
- The anatomic location of localized adenopathy will sometimes be helpful in narrowing the differential diagnosis. For example, cat-scratch disease typically causes cervical or axillary adenopathy, infectious mononucleosis causes cervical adenopathy and a number of sexually transmitted diseases are associated with inguinal adenopathy.
References:
- Habermann TM, Steensma DP. Lymphadenopathy. Mayo Clin Proc. 2000;75:723–32. doi: 10.1016/S0025-6196(11)64620-X. PubMed PMID: 10907389.
- Mohseni S, Shojaiefard A, Khorgami Z, Alinejad S, Ghorbani A, Ghafouri A. Peripheral lymphadenopathy: approach and diagnostic tools. Iran J Med Sci. 2014;39(2 Suppl):158-170.
- Am Fam Physician. 2016 Dec 1;94(11):896-903.
- Am Fam Physician. 1998 Oct 15;58(6):1313-1320.
Polycythemia Vera
2016 Revised World Health Organization Diagnostic Criteria for Polycythemia Vera
- Must meet all three major criteria or the first two major criteria and the minor criterion
- Major criteria
- Hemoglobin > 165 g per L (16.5 g per dL) in men or > 160 g per L (16.0 g per dL) in women or Hematocrit > 49% in men or > 48% in women or Increased red blood cell mass (> 25% above normal)
- Bone marrow with tri-lineage proliferation with pleomorphic mature megakaryocytes
- Presence of Janus kinase 2 mutation
- Minor criterion
- Subnormal erythropoietin level
- Major criteria
| Symptom/finding | Percentage with finding |
|---|---|
| Fatigue | 91 |
| Insomnia | 68 |
| Pruritus on contact with water | 36 to 68 |
| Concentration problems | 61 |
| Splenomegaly | 36 |
| Erythromelalgia | 29 |
| Arterial thrombosis | 16 |
| Venous thrombosis | 7.4 |
| Major hemorrhage | 4.2 |
Treatment:
- All patients should receive phlebotomy with a goal hematocrit level of less than 45%.18–20
- All patients should receive daily low-dose aspirin (40 to 100 mg) in the absence of contraindications.20,21
- Hydroxyurea is the first-line agent for cytoreductive therapy in PV.20
- First-line therapy for associated pruritis includes aspirin, antihistamines, and paroxetine (Paxil).22,31,32
- Follow-up appointments every three to six months are recommended for routine history, physical examination, and complete blood count.15
- Smoking cessation decreases the risk of thrombosis.39
Reference:
- AFP Jun 2021 Vol 103 No 11
Prostate Cancer
Prostate Cancer Screening
See also:
The snags of PSA screening from this study are
- At baseline, prostate cancer is rarely deadly and often slow-growing
- Screening is most likely to pick up low-risk tumors
- Older men are many times more likely to die of other causes
- Once a PSA is positive it is hard not to act, and action can result in complications, such as incontinence and impotence
Prostate cancer is the most commonly diagnosed cancer in men, but it is not a common cause of death.
- About 1 in 8 men will be diagnosed with prostate cancer during their lifetime
- Only about 1 in 41 will die from it
After 23 years, the prostate cancer mortality was 13% lower in the screening group (Rate ratio 0.87 95% CI 0.80-0.95).
- The absolute rates of prostate cancer deaths were 1.4% vs 1.6% in the screened vs control arm.
- So the absolute risk reduction (ARR) was 0.2%.
- This means that the number needed to screen to prevent one prostate cancer death is approximately 500.
- (499 out of 500 men get no benefit from being invited to be screened)
Screening detects 30% more prostate cancer, though on an absolute scale it is only an excess of 27 cases of prostate cancer per 1000 men (2.7%).
- Screening is 2x more likely to find low-risk cancer, and 44% less likely to find high-risk cancer.
The overall mortality curves are identical. Prostate cancer detection does not prolong life, because other-cause mortality is 49% in both groups.
Reference:
PIRADS Score
| Score | Significance |
|---|---|
| 1 | Clinically significant disease is highly unlikely to be present |
| 2 | Clinically significant disease is unlikely to be present |
| 3 | Clinically significant cancer is equivocal |
| 4 | Clinically significant cancer is likely to be present |
| 5 | Clinically significant cancer is highly likely to be present |
| PI-RADS Category | Lesion-Level CDR | Lesion-Level 95% CI | Patient-Level CDR | Patient-Level 95% CI |
|---|---|---|---|---|
| 1 | 2% | 0–8% | 6% | 0–20% |
| 2 | 4% | 1–9% | 9% | 5–13% |
| 3 | 20% | 13–27% | 16% | 7–27% |
| 4 | 52% | 43–61% | 59% | 39–78% |
| 5 | 89% | 76–97% | 85% | 73–94% |
- CDR = Cancer Detection Rate (clinically significant cancer)
- n lesions = 1,946
- n patients = 1,268
- Higher categories significantly associated with higher CDR (P < 0.001)
Notes:
- Lesion level means the cancer detection rate is calculated per suspicious area identified on the MRI. For example, if a PI-RADS 4 lesion is biopsied and found to be cancerous, that counts as one positive lesion.
- Patient level means the rate is calculated per person. If a patient has at least one PI-RADS 4 lesion that turns out to be cancerous, the entire patient is counted as a positive case, even if other lesions are benign.
- This is why detection rates are often higher at the lesion level: a single patient may have multiple lesions, but only one needs to be cancerous to count at the patient level.
Reference:
- Liddell H, Jyoti R, Haxhimolla HZ. mp-MRI Prostate Characterised PIRADS 3 Lesions are Associated with a Low Risk of Clinically Significant Prostate Cancer - A Retrospective Review of 92 Biopsied PIRADS 3 Lesions. Curr Urol. 2015 Jul;8(2):96-100. doi: 10.1159/000365697. Epub 2015 Jul 10. PMID: 26889125; PMCID: PMC4748763.
- Oerther, B., Engel, H., Bamberg, F. et al. Cancer detection rates of the PI-RADSv2.1 assessment categories: systematic review and meta-analysis on lesion level and patient level. Prostate Cancer Prostatic Dis 25, 256–263 (2022). https://doi.org/10.1038/s41391-021-00417-1
Study: European Study of Prostate Cancer Screening — 23-Year Follow-up
Background
- The European Randomized Study of Screening for Prostate Cancer (ERSPC) was initiated in 1993 to assess the effect of prostate-specific antigen (PSA) testing on prostate cancer mortality. Because deaths from prostate cancer are expected to rise worldwide owing to increased life expectancy and population growth, a final analysis of the long-term outcomes of prostate cancer screening is essential to understanding the benefits and harms of PSA testing.
Methods
- We updated the findings from ERSPC, a multicenter, randomized study conducted across eight European countries with a focus on a predefined core age group of 162,236 men who were 55 to 69 years of age at the time of randomization. Participants were randomly assigned to the screening group and offered repeated PSA testing or to the control group and not invited for screening. The primary outcome was prostate cancer mortality.
Results
- After a median follow-up of 23 years, prostate cancer mortality was 13% lower in the screening group (rate ratio, 0.87; 95% confidence interval [CI], 0.80 to 0.95), and the absolute risk reduction was 0.22% (95% CI, 0.10 to 0.34). The cumulative incidence of prostate cancer was higher in the screening group than in the control group (rate ratio, 1.30; 95% CI, 1.26 to 1.33).
- At a median of 23 years of follow-up, one death from prostate cancer was prevented for every 456 men (95% CI, 306 to 943) who were invited for screening, and one death from prostate cancer was averted for every 12 men (95% CI, 8 to 26) in whom prostate cancer was diagnosed, as compared with one death from prostate cancer prevented for every 628 men (95% CI, 419 to 1481) and one death averted for every 18 men (95% CI, 12 to 45) at 16 years of follow-up.
Conclusions
- Long-term follow-up confirms a sustained reduction in deaths from prostate cancer with PSA testing, alongside an improved harm–benefit ratio. Future screening strategies should adopt risk-based approaches to minimize overdiagnosis while maintaining clinical benefits. (Funded by the Dutch Cancer Society and others; ERSPC ISRCTN registry number, ISRCTN49127736.)
Reference:
- Roobol MJ, de Vos II, Månsson M, Godtman RA, Talala KM, den Hond E, Nelen V, Villers A, Poinas G, Kwiatkowski M, Wyler S, Recker F, Puliti D, Gorini G, Zappa M, Paez A, Lujan M, Bangma CH, Tammela T, Schröder FH, Remmers S, Hugosson J, Auvinen A; ERSPC Investigators. European Study of Prostate Cancer Screening - 23-Year Follow-up. N Engl J Med. 2025 Oct 30;393(17):1669-1680. doi: 10.1056/NEJMoa2503223. PMID: 41160819.
Study: Projected Lifetime Cancer Risks From Current Computed Tomography Imaging
Notes:
- Projected Cancers:
- By age:
- Cancer risk in girls younger than 1 year were 20 cancers per 1000 examinations (1900 of 97,000)
- 2 per 1000 in girls aged 15 to 17 years (1100 of 483,600)
- By type:
- Abdomen and pelvis CT was estimated to contribute the largest number of projected cancers (40%) in adults (37,500 [90% UL, 32,900-42,600] cases)
- Head CT contributed the largest number of cancers (53%) in children (5100 [90% UL, 3700-7100)
- By age:
- Projected Risk
- CT utilization in the United States in 2023 was estimated to result in 102,700 (90% UL, 96,400-109,500) projected lifetime cancers, including 93,000 (90% UL, 86,900-99,600) in adults and 9,700 (90% UL, 8100-11,600) in children
- The leading cancers in adults were lung cancer (21,400 [90% UL, 19,200-24,000]), colon cancer (8400 [90% UL, 7500-9400]), and leukemia (7400 [90% UL, 6100-8900])
- The most frequent projected cancers in children were thyroid (3500 [90% UL, 2300-5500]), lung (990 [90% UL, 870-1100]), and breast (630 [90% UL, 550-730]) cancer.
- Lung and thyroid cancer incidence were higher in female patients, whereas incidence of most other cancers was similar by sex or slightly higher in male patients
Key Points
- Question
- How many future cancers could result from radiation exposure from annual computed tomography (CT) examinations in the United States?
- Findings
- In this risk model, the 93 million CT examinations performed in 62 million patients in 2023 were projected to result in approximately 103,000 future cancers. Although the per-examination cancer risk was higher in children, higher CT utilization among adults accounted for the majority of the projected cancers.
- Meaning
- These findings suggest that if current radiation dosing and utilization practices continue, CT-associated cancers could eventually account for 5% of all new cancer diagnoses annually.
Abstract
- Importance
- Approximately 93 million computed tomography (CT) examinations are performed on 62 million patients annually in the United States, and ionizing radiation from CT is a known carcinogen.
- Objective
- To project the number of future lifetime cancers in the US population associated with CT imaging in 2023.
- Design, Setting, and Participants
- This risk model used a multicenter sample of CT examinations prospectively assembled between January 2018 and December 2020 from the University of California San Francisco International CT Dose Registry. Data analysis was conducted from October 2023 to October 2024.
- Main Outcomes and Measures
- Distributions of CT examinations and associated organ-specific radiation doses were estimated by patient age, sex, and CT category and scaled to the US population based on the number of examinations in 2023, quantified by the IMV national survey. Lifetime radiation-induced cancer incidence and 90% uncertainty limits (UL) were estimated by age, sex, and CT category using National Cancer Institute software based on the National Research Council's Biological Effects of Ionizing Radiation VII models and projected to the US population using scaled examination counts.
- Results
- An estimated 61,510,000 patients underwent 93,000,000 CT examinations in 2023, including 2,570,000 (4.2%) children, 58,940,000 (95.8%) adults, 32,600,000 (53.0%) female patients, and 28,910,000 (47.0%) male patients. Approximately 103,000 (90% UL, 96,400-109,500) radiation-induced cancers were projected to result from these examinations. Estimated radiation-induced cancer risks were higher in children and adolescents, yet higher CT utilization in adults accounted for most (93,000; 90% UL, 86,900-99,600
[0%]) radiation-induced cancers. The most common cancers were lung cancer (22,400 cases; 90% UL, 20,200-25,000 cases), colon cancer (8700 cases; 90% UL, 7800-9700 cases), leukemia (7900 cases; 90% UL, 6700-9500 cases), and bladder cancer (7100 cases, 90% UL, 6000-8500 cases) overall, while in female patients, breast was second most common (5700 cases; 90% UL, 5000-6500 cases). The largest number of cancers was projected to result from abdomen and pelvis CT in adults, reflecting 37,500 of 103,000 cancers (37%) and 30 million of 93 million CT examinations (32%), followed by chest CT (21,500 cancers[0%]; 20 million examinations[0%]). Estimates remained large over a variety of sensitivity analyses, which resulted in a range of 80,000 to 127,000 projected cancers across analyses.
- An estimated 61,510,000 patients underwent 93,000,000 CT examinations in 2023, including 2,570,000 (4.2%) children, 58,940,000 (95.8%) adults, 32,600,000 (53.0%) female patients, and 28,910,000 (47.0%) male patients. Approximately 103,000 (90% UL, 96,400-109,500) radiation-induced cancers were projected to result from these examinations. Estimated radiation-induced cancer risks were higher in children and adolescents, yet higher CT utilization in adults accounted for most (93,000; 90% UL, 86,900-99,600
- Conclusions and Relevance
- This study found that at current utilization and radiation dose levels, CT examinations in 2023 were projected to result in approximately 103,000 future cancers over the course of the lifetime of exposed patients. If current practices persist, CT-associated cancer could eventually account for 5% of all new cancer diagnoses annually.
Reference:
- Smith-Bindman R, Chu PW, Azman Firdaus H, et al. Projected Lifetime Cancer Risks From Current Computed Tomography Imaging. JAMA Intern Med. Published online April 14, 2025. https://doi.org/10.1001/jamainternmed.2025.0505
Study: The Association Between Smartphone Use and Breast Cancer Risk Among Taiwanese Women: A Case-Control Study edit
Introduction
- Breast cancer is a common malignancy worldwide. Smartphones have gradually become indispensable to our modern lives and have already changed lifestyles of human beings. To our best knowledge, no study has investigated the relationship between smartphone use and breast cancer. This case-control study purposely investigated the relationship between smartphone use and breast cancer risk.
Materials and Methods
- This was a case-control study comprising 894 healthy controls and 211 patients with breast cancer. All participants were asked to respond to standard questionnaires to collect information on sleep quality, smartphone addiction, and smartphone use.
Results
- Participants with smartphone addiction had a significantly higher 1.43-fold risk of breast cancer.
- Individuals with the habitual behavior of smartphone use >4.5 minutes before bedtime had a significantly increased 5.27-fold risk of breast cancer compared to those who used a smartphone for ≤4.5 minutes before bedtime.
- Additionally, a closer distance between the smartphone and the breasts when using the smartphone exhibited a significantly increased 1.59-fold risk.
- Participants who carried their smartphone near their chest or waist-abdomen area had significantly increased 5.03-fold and 4.06-fold risks of breast cancer, respectively, compared to those who carried the smartphone below the waist.
- Moreover, there was a synergistic effect of smartphone addiction and smartphone use of >4.5 minutes before bedtime which increased the breast cancer risk.
Conclusion
- Excessive smartphone use significantly increased the risk of breast cancer, particularly for participants with smartphone addiction, a close distance between the breasts and smartphone, and the habit of smartphone use before bedtime.
Reference:
- Shih YW, Hung CS, Huang CC, Chou KR, Niu SF, Chan S, Tsai HT. The Association Between Smartphone Use and Breast Cancer Risk Among Taiwanese Women: A Case-Control Study. Cancer Manag Res. 2020 Oct 29;12:10799-10807. doi: 10.2147/CMAR.S267415. PMID: 33149685; PMCID: PMC7605549.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7605549/
Infectious Disease
Acute Bacterial Rhinosinusitis (ABRS)
Defined as any of the following 3 presentations:
- Symptoms lasting for 10d and not improving
- Symptoms that are severe with fever over 39C, nasal discharge, and facial pain lasting 3-4d
- Worsening symptoms with new fever, headache, or increased nasal discharge, typically after viral URI lasting 5-6d after initially seeming to improve
Most common organisms:
- Streptococcus pneumoniae (38%)
- Haemophilus influenzae (35%)
- Moraxella catarrhalis (16%)
Treatment:
- Amoxacillin-clavulanate (500mg/125mg tid or 850mg/125mg bid)
- Doxycycline (100mg bid for 5-7d)
- If resistance -> Levofloxacin (500mg qd) or amoxicillin-clavulanate (2000mg/125mg bid) for 10d
- Antibiotics can shorten the time to cure. 5 more people per 100 will improve more quickly at any point between 7 and 14 days if they recieve antibiotics vs placebo. Given the potential harms of antibiotics, it is NOT recommended to use antibiotics for uncomplicated acute rhinosinusitis.
References:
- Consultant Feb 2016
Acute Gastroenteritis
See also:
What to do for viral gastroenteritis:
- Drink plenty of fluids to avoid dehydration; You need to drink more than usual to replace the fluids lost from vomiting and diarrhea. Water is best, and you should drink fluids slowly in frequent, small amounts
- Get plenty of rest
- Take acetaminophen (Tylenol) for any fever or aches and pains
- For nausea/vomiting and diarrhea, you can also use bismuth subsalicylate (Pepto-Bismol)
- If you feel like eating, try small amounts of plain foods, such as soup, rice, pasta and bread
- You can use loperamide 2 mg after every loose stool to help with diarrhea
As symptoms start to ease:
- Gradually ease food back into the your diet.
- Start with bland, easy-to-digest food such as crackers, bananas, toast, rice, and chicken
- Avoid dairy, caffeine, and alcohol until recovery is complete
Prevention
- Stay off work, school or nursery until at least 48 hours after the symptoms have passed
- Wash your hands frequently and thoroughly with soap and water – don't rely on alcohol hand gels, as they're not always effective
- Disinfect any surfaces or objects that could be contaminated – it's best to use a bleach-based household cleaner
- Wash contaminated items of clothing or bedding separately on a hot wash
- Practice good food hygiene: make sure food is properly refrigerated, always cook your food thoroughly, and never eat food that is past its use-by date
Acute Respiratory Tract Infections
See also:
- Acute Bacterial Rhinosinusitis
- Influenza
- Pharyngitis
- Pneumonia (Community Acquired)
- Post Infectious Cough
Exercise:
- For adults,
- Regular exercise may reduce the overall severity of acute respiratory tract infections and the number of days with symptoms
- But there is no evidence that exercise reduces the overall occurrence or duration of these infections. (SOR B)
References:
- AFP Feb 2021 Vol 103 No 3
Comparison of different Acute Upper Respiratory Infections
| Condition | Signs and symptoms | Treatment |
|---|---|---|
| Acute otitis media | Fever, earache, ear drainage, middle ear effusion, signs of middle ear inflammation | Analgesics, amoxicillin |
| Acute rhinosinusitis | Fever, purulent nasal discharge, facial pain, headache | Watchful waiting for most, Augmentin for severe or complicated |
| Common cold | Low-grade fever, myalgieas, headache, nasal congestion, rhinorrhea, sneezing, sore throat, cough | Supportive car4e, OTC analgesics, antihistampine/decongestant combinations for adults |
| COVID-19 | Fever, chills, cough, SOB, sore throat, loss taste/smell, headache, rhinorrhea, congestion, malaise, myalgieas, GI symptoms | Supportive care in general |
| Epiglottitis | Fever, inspiratory stridor, drooling, muffled voice, preference for sitting forward, sore throat, odynophagia, dysphagia | Supplemental humidified O2 and IV 3rd gen cephalosporin (ceftriaxone or cefotaxime) |
| Influenza | Abrupt onset of fever/cough, chills, congestion, rhinorrhea, sore throat, headache, myalgias, fatigue | Supportive care, neuraminidase inhibitors (oseltamivir) |
| Laryngitis | Hoarse voice, sore throat, nasal congestion, fever | Supportive care |
| Pharyngitis | Sore throat, pain with swallowing, fever, absence of cough | Supportive care, PCN or amoxicillin for +cultre or Centor 4-5 |
Reference:
- AFP Vol 106 No 6 Dec 2022
CDC Outpatient Antibiotic Recommendations edit
Conditions:
- Acute rhinosinusitis
- Epidemiology
- About 1 out of 8 adults (12%) in 2012 reported receiving a diagnosis of rhinosinusitis in the previous 12 months, resulting in more than 30 million diagnoses
- Ninety–98% of rhinosinusitis cases are viral, and antibiotics are not guaranteed to help even if the causative agent is bacterial.
- Diagnosis
- Diagnose acute bacterial rhinosinusitis based on symptoms that are:
- Severe (>3-4 days), such as a fever ≥39°C (102°F) and purulent nasal discharge or facial pain;
- Persistent (>10 days) without improvement, such as nasal discharge or daytime cough; or
- Worsening (3-4 days) such as worsening or new onset fever, daytime cough, or nasal discharge after initial improvement of a viral upper respiratory infections (URI) lasting 5-6 days.
- Sinus radiographs are not routinely recommended.
- Diagnose acute bacterial rhinosinusitis based on symptoms that are:
- Management
If a bacterial infection is established:
- Watchful waiting is encouraged for uncomplicated cases for which reliable follow-up is available.
- Amoxicillin or amoxicillin/clavulanate is the recommended first-line therapy.
- Macrolides such as azithromycin are not recommended due to high levels of Streptococcus pneumoniae antibiotic resistance (~40%).
- For penicillin-allergic patients, doxycycline or a respiratory fluoroquinolone (levofloxacin or moxifloxacin) are recommended as alternative agents.
- Epidemiology
- Acute uncomplicated bronchitis
- Epidemiology
- Cough is the most common symptom for which adult patients visit their primary care provider, and acute bronchitis is the most common diagnosis in these patients.
- Diagnosis
- Evaluation should focus on ruling out pneumonia, which is rare among otherwise healthy adults in the absence of abnormal vital signs (heart rate ≥ 100 beats/min, respiratory rate ≥ 24 breaths/min, or oral temperature≥ 38 °C) and abnormal lung examination findings (focal consolidation, egophony, fremitus).
- Colored sputum does not indicate bacterial infection.
- For most cases, chest radiography is not indicated.
- Management
Routine treatment of uncomplicated acute bronchitis with antibiotics is not recommended, regardless of cough duration.
- Options for symptomatic therapy include:
- Cough suppressants (codeine, dextromethorphan);
- First-generation antihistamines (diphenhydramine);
- Decongestants (phenylephrine).
- Evidence supporting specific symptomatic therapies is limited.
- Options for symptomatic therapy include:
- Epidemiology
- Common cold or non-specific upper respiratory tract infection (URI)
- Epidemiology
- The common cold is the third most frequent diagnosis in office visits, and most adults experience two to four colds annually.
- At least 200 viruses can cause the common cold.
- Diagnosis
- Prominent cold symptoms include fever, cough, rhinorrhea, nasal congestion, postnasal drip, sore throat, headache, and myalgias.
Management
- Decongestants (pseudoephedrine and phenylephrine) combined with a first-generation antihistamine may provide short-term symptom relief of nasal symptoms and cough.
- Non-steroidal anti-inflammatory drugs can be given to relieve symptoms.
- Evidence is lacking to support antihistamines (as monotherapy), opioids, intranasal corticosteroids, and nasal saline irrigation as effective treatments for cold symptom relief.
Providers and patients must weigh the benefits and harms of symptomatic therapy.
- Epidemiology
- Pharyngitis
- Epidemiology
- Group A beta-hemolytic streptococcal (GAS) infection is the only common indication for antibiotic therapy for sore throat cases.
- Only 5–10% of adult sore throat cases are caused by GAS.
- Diagnosis
- Clinical features alone do not distinguish between GAS and viral pharyngitis; a rapid antigen detection test (RADT) is necessary to establish a GAS pharyngitis diagnosis
- Those who meet two or more Centor criteria (e.g., fever, tonsillar exudates, tender cervical lymphadenopathy, absence of cough) should receive a RADT. Throat cultures are not routinely recommended for adults.
- Management
- Antibiotic treatment is NOT recommended for patients with negative RADT results.
- Amoxicillin and penicillin remain first-line therapy due to their reliable antibiotic activity against GAS.
- For penicillin-allergic patients, cephalexin, cefadroxil, clindamycin, or macrolides are recommended.
- GAS antibiotic resistance to azithromycin and clindamycin are increasingly common.
- Recommended treatment course for all oral beta lactams is 10 days.
- For specific treatment recommendations and dosing, visit the Pharyngitis (Strep Throat) page for clinicians.
- Epidemiology
- Acute uncomplicated cystitis
Epidemiology
- Cystitis is among the most common infections in women and is usually caused by E. coli.
- Diagnosis
- Classic symptoms include dysuria, frequent voiding of small volumes, and urinary urgency. Hematuria and suprapubic discomfort are less common.
- Nitrites and leukocyte esterase are the most accurate indicators of acute uncomplicated cystitis
- Management
For acute uncomplicated cystitis in healthy adult non-pregnant, premenopausal women:
- Nitrofurantoin, trimethoprim/sulfamethoxazole (TMP-SMX, where local resistance is <20%), and fosfomycin are appropriate first-line agents.
- Fluoroquinolones (e.g. ciprofloxacin) should be reserved for situations in which other agents are not appropriate.
Reference:
CDC Treatment for Common Illnesses edit
Influenza vs Common cold edit
Influenza and the common cold are both viral respiratory infections, but they differ significantly in their clinical presentation, severity, and potential complications.
| Feature | Influenza | Common Cold |
|---|---|---|
| Onset | Abrupt | Gradual |
| Severity | More Severe | Milder |
| Systemic Symptoms | High fever, chills, myalgias, malaise, severe fatigue | Low-grade fever (if present), less pronounced myalgias/fatigue |
| Fever | Common, high | Rare, low-grade (if present) |
| Common Symptoms | High fever, chills, myalgias, headache, malaise, nonproductive cough, sore throat, rhinitis, nausea, vomiting, diarrhea (especially in children) | Sore throat, nasal congestion, rhinorrhea, sneezing, cough |
| Complications | Primary/Secondary Viral Pneumonia, Myocarditis, Exacerbation of Underlying Conditions | Typically Self-Limiting |
| Disease Burden | Substantial morbidity and mortality, especially in high-risk populations | Generally self-limiting |
Influenza is characterized by an abrupt onset of symptoms, including high fever, chills, myalgias, headache, malaise, nonproductive cough, sore throat, and rhinitis. Gastrointestinal symptoms such as nausea, vomiting, and diarrhea can also occur, particularly in children. Influenza can lead to severe complications such as primary viral pneumonia, secondary bacterial pneumonia, myocarditis, and exacerbation of underlying medical conditions. The disease burden of influenza is substantial, with significant morbidity and mortality, especially in high-risk populations such as the elderly, young children, and individuals with chronic health conditions.[1-2]
The common cold, typically caused by rhinoviruses, coronaviruses, and other respiratory viruses, presents with milder symptoms compared to influenza. Common cold symptoms include sore throat, nasal congestion, rhinorrhea, sneezing, and cough. Fever is less common and, if present, is usually low-grade. The onset of symptoms is more gradual, and systemic symptoms like myalgias and severe fatigue are less pronounced. The common cold is generally self-limiting and rarely leads to severe complications.[3-4]
In summary, the key differences between influenza and the common cold are:
- Onset and severity: Influenza has a sudden onset with more severe systemic symptoms, while the common cold has a gradual onset with milder symptoms.
- Fever: High fever is common in influenza but rare in the common cold.
- Complications: Influenza can lead to serious complications, whereas the common cold is typically self-limiting.
These distinctions are crucial for clinical diagnosis and management of these respiratory infections
| Signs and Symptoms | Cold | Influenza (Flu) |
|---|---|---|
| Symptom onset | Gradual | Abrupt |
| Fever | Rare | Common; lasts 3-4 days |
| Aches | Slight | Common; often severe |
| Chills | Uncommon | Fairly common |
| Fatigue, weakness | Sometimes | Usual |
| Sneezing | Common | Sometimes |
| Chest discomfort, cough | Mild to moderate; hacking cough | Common; can be severe |
| Stuffy nose | Common | Sometimes |
| Sore throat | Common | Sometimes |
| Headache | Rare | Common |
I have a few questions:
- How fast did symptoms begin?
- Do you have any fevers, chills, muscle aches, or joint pains?
- Any fatigue or weakness?
- What about sneezing or chest discomfort/cough?
- Have you had any headaches?
Reference:
- Christine Szablewski, Michael Daugherty, Eduardo Azziz-Baumgartner Influenza. CDC Yellow Book
- Treanor JJ. Influenza Vaccination. The New England Journal of Medicine. 2016;375(13):1261-8. https://doi.org/10.1056/NEJMcp1512870.
- Iyadorai T, Lim SH, Wong PL, et al. Clinical Symptoms, Comorbidities and Health Outcomes Among Outpatients Infected With the Common Cold Coronaviruses Versus Influenza Virus. Virology Journal. 2024;21(1):251. https://doi.org/10.1186/s12985-024-02524-6.
- Eccles R. Understanding the Symptoms of the Common Cold and Influenza. The Lancet. Infectious Diseases. 2005;5(11):718-25. https://doi.org/10.1016/S1473-3099(05)70270-X.
Additional Reference:
Common Cold EBM
- ipratropium
- OTC analgesics
- decongestants
- zinc (75 mg zinc acetate or gluconate lozenges daily) - resolves cough and nasal discharge
- Start within 24 hours of symptom onset
Influenza
When to use an antiviral:
- Severe, complicated, or progressive illness
- Hospitalization required
- High risk for complications
- Children <2yrs
- Adults >64yrs
- Individuals with
- COPD
- Asthma
- CV (except HTN alone) disease
- Renal disease
- Hepatic disease
- Hematologic disease
- Stroke
- Intellectual disability
- Muscular dystrophy
- Spinal cord injury
- Individuals with immunosuppression
- Women who are pregnant or postpartum
- Individuals <19 who are receiving long-term aspirin therapy
- American Indians/Alaska natives
- Individuals who are morbidly obese
- Residents of nursing homes and other chronic care facilities
Reference:
- JFP Vol 66 No 9 Sep 2017
Coronavirus Disease 2019 (COVID-19)
| Clinical Recommendation | LOE |
|---|---|
| Close contacts of patients with COVID-19 should quarantine for 14 days with daily monitoring for fever and other symptoms.8 | C |
| Telehealth can be used for initial triage of patients with respiratory symptoms of COVID-19; further care should be based on vital signs, physical examination findings, social considerations, and risk factors.11,17 | C |
| Infection with severe acute respiratory syndrome coronavirus 2 should be confirmed by polymerase chain reaction testing using a nasopharyngeal swab.38 | C |
| Management of COVID-19 in the outpatient setting is focused on supportive care and reducing the risk of transmission via isolating at home.41 | C |
| Dexamethasone, 6 mg per day for 10 days, reduces mortality in hospitalized patients with COVID-19 who require supplemental oxygen (NNT = 29) and mechanical ventilation (NNT = 9), but not in hospitalized patients or outpatients who do not require supplemental oxygen.46 | B |
| Remdesivir (Veklury) shortens time to recovery in hospitalized patients with COVID-19 but has not been proven to reduce mortality.48,49 | B |
Signs and Symptoms of Coronavirus Disease 2019
- Adults
- Anosmia or altered taste (64%)
- Fever (56% to 99%)
- Cough (55% to 82%)
- Anorexia (40%)
- Fatigue (38% to 70%)
- Sputum production (27% to 34%)
- Shortness of breath (19% to 57%)
- Chills (12% to 15%)
- Myalgias (11% to 45%)
- Dizziness (8% to 9%)
- Sore throat (5% to 14%)
- Headache (3% to 14%)
- Diarrhea (2% to 24%)
- Chest pain (2% to 15%)
- Nasal congestion or rhinorrhea (2% to 5%)
- Rash or skin discoloration (1% to 20%)
- Nausea and vomiting (1% to 19%)
- Hemoptysis (1% to 2%)
- Conjunctivitis (1%)
- Children
- Pharyngeal erythema (46%)
- Cough (44% to 54%)
- Fever (41% to 56%)
- Diarrhea (8%)
- Fatigue (8%)
- Rhinorrhea (8%)
- Vomiting
Remote patient monitoring via telehealth can be used to detect red flag symptoms that warrant urgent assessment, such as:
- Fever above 100.4°F (38°C)
- Heart rate greater than 100 beats per minute with new confusion
- Oxygen saturation less than 95%
- Respiratory rate greater than 20 breaths per minute
COVID-19 Resources
- BMJ's COVID-19 hub
- European Centre for Disease Prevention and Control: contact tracing for COVID-19
- Infectious Diseases Society of America: COVID-19 treatment guidelines
- National Institutes of Health: COVID-19 treatment guidelines
- World Health Organization: Interim guidance on clinical management of COVID-19
References:
- AFP Oct 2020 Vol 102 No 8
FLCCC - Prevention Protocol (COVID-19)
Prevention Protocol:
- Ivermectin
- Chronic Prevention
- 0.2 mg/kg per dose (take with or after a meal) — twice a week for as long as disease risk is elevated in your community. Alternative: Hydroxychloroquine – 200 mg tablet daily.
- Post COVID-19 Exposure Prevention
- 0.4 mg/kg per dose (take with or after a meal) — one dose today, repeat after 48 hours.
- Alternative: Hydroxychloroquine – 400 mg twice day on day 1, then 200 mg twice a day on Days 2 and 3.
- Chronic Prevention
- Gargle mouthwash
- 2 x daily – gargle (do not swallow) antiseptic mouthwash with cetylpyridinium chloride (e.g. ScopeTM, ActTM, CrestTM), 1% povidone/iodine solution or ListerineTM with essential oils.
Immune Fortifying / Supportive Therapy
- Vitamin D3 Optimal approach to dosing requires testing of 25(OH)D level. For dosing guidance, see Table 1 if level is known and Table 2 if level is unknown.
- Vitamin C 500–1,000 mg 2 x daily
- Quercetin 250 mg/day
- Zinc 30–40 mg/day (elemental zinc)
- Melatonin 6 mg before bedtime (causes drowsiness)
FLCCC - Early Outpatient Treatment Protocol (COVID-19)
First line agents
- Antiviral:
- Ivermectin: 0.4–0.6 mg/kg per dose (take with or after a meal) — one dose daily, take for 5 days or until recovered. Use upper dose if: 1) in regions with aggressive variants (e.g. Delta); 2) treatment started on or after day 5 of symptoms or in pulmonary phase; or 3) multiple comorbidities/risk factors.
- and/or Hydroxychloroquine (preferred for Omicron): 200 mg PO twice daily; take for 5 days or until recovered.
- Ivermectin: 0.4–0.6 mg/kg per dose (take with or after a meal) — one dose daily, take for 5 days or until recovered. Use upper dose if: 1) in regions with aggressive variants (e.g. Delta); 2) treatment started on or after day 5 of symptoms or in pulmonary phase; or 3) multiple comorbidities/risk factors.
- Antiseptic
- Antiviral mouthwash: Gargle 3 x daily (do not swallow; must contain chlorhexidine, povidone-iodine, or cetylpyridinium chloride).
- Iodine nasal spray/drops: Use 1 % povidone-iodine commercial product as per instructions 2–3 x daily. If 1 %-product not available, must first dilute the more widely available 10 %-solution and apply 4–5 drops to each nostril every 4 hours. (No more than 5 days in pregnancy.)
- Anticoagulation/Immune fortifying
- Aspirin 325 mg daily (unless contraindicated)
- Vitamin D3 Optimal approach to dosing requires testing of 25(OH)D level. For dosing guidance, see Table 1 if level is known and Table 2 if level is unknown.
- Melatonin 10 mg before bedtime (causes drowsiness)
- Synergistic Therapies
- Quercetin 250 mg 2 x daily
- Zinc 100 mg/day (elemental zinc)
- Vitamin C 500–1,000 mg 2 x daily
- Nutritional (for 14 days)
- Curcumin (turmeric) 500 mg 2 x daily
- Nigella Sativa (black cumin seed) 80 mg/kg daily
- Honey 1 gram/kg daily
- Pulse Ox
Second line (if 1) ≥ 5 days of symptoms; 2) Poor response to therapies above; 3) Significant comorbidities):
- Dual anti-androgen therapies
- Spironolactone 100 mg 2 x daily for ten days.
- Dutasteride 2 mg on day 1, followed by 1 mg daily for 10 days.
- If Dutasteride not available, use Finasteride 10 mg daily for 10 days
- Fluvoxamine
- 50 mg 2 x daily for 10 days 7
- Consider Fluoxetine 30 mg daily for 10 days as an alternative (it is often better tolerated). Avoid if patient is already on an SSRI.
- Monoclonal Antibodies
- Sotrovimab 500 mg each in a single intravenous infusion.
- Antibody therapy is for patients within 5 days of first symptoms, non-severe symptoms, and one or more risk factors as: Age>55y; BMI>25; pregnancy; chronic lung, heart, or kidney disease; diabetes.
- Sotrovimab 500 mg each in a single intravenous infusion.
Third Line:
- Corticosteroids
- Prednisone or Methylprednisolone 1 mg/kg daily for 5 days followed by slow taper or escalation according to patient response.
- Criteria: After day 7–10 from first symptoms and patient has either:
- abnormal chest x-ray
- shortness of breath
- or oxygen saturations of 88–94 %.
- If oxygen saturation is lower than 88 %, emergency room evaluation should be sought
Reference:
- Vitamin D Dosing for COVID-19
Table 115: Longer-term maintenance of serum 25(OH)D concentrations above 50 ng/mL based on body weight Body-weight category Dose (IU) kg/day Daily dose (IU) Once a week (IU) BMI ≤ 19 (under-weight) 40 – 70 2,000 – 4,000 25,000 BMI 20–29 (non-obese person) 70 – 100 5,000 – 7,000 50,000 BMI 30–39 (obese persons) 100 – 150 9,000 – 15,000 75,000 BMI ≥ 40 (morbidly obese persons) 150 – 200 16,000 – 30,000 100,000 - Pulse Ox for COVID-19
In symptomatic patients, monitoring with home pulse oximetry is recommended (due to asymptomatic hypoxia). The limitations of home pulse oximeters should be recognized, and validated devices are preferred. Multiple readings should be taken over the course of the day, and a downward trend should be regarded as ominous.
Baseline or ambulatory desaturation < 94% should prompt hospital admission.
The following guidance is suggested:
- Use the index or middle finger; avoid the toes or ear lobe.
- Only accept values associated with a strong pulse signal.
- Observe readings for 30–60 seconds to identify the most common value.
- Remove nail polish from the finger on which measurements are made.
- Warm cold extremities prior to measurement.
- Calculation for ivermectin dose (0.2 mg per kg) for COVID-19
Body weight lbs Body weight Kg Dose 0.2 mg/kg ≈ 0.09 mg/lb (Each tablet = 3 mg; doses rounded to nearest half tablet above) 70–90 lb 32–40 kg 8 mg (3 tablets = 9 mg) 91–110 lb 41–50 kg 10 mg (3.5 tablets) 111–130 lb 51–59 kg 12 mg (4 tablets) 131–150 lb 60–68 kg 13.5 mg (4.5 tablets) 151–170 lb 69–77 kg 15 mg (5 tablets) 171–190 lb 78–86 kg 16 mg (5.5 tablets) 191–210 lb 87–95 kg 18 mg (6 tablets) 211–230 lb 96–104 kg 20 mg (7 tablets = 21 mg) 231–250 lb 105–113 kg 22 mg (7.5 tablets=22.5 mg) 251–270 lb 114–122 kg 24 mg (8 tablets) 271–290 lb 123–131 kg 26 mg (9 tablets = 27 mg) 291–310 lb 132–140 kg 28 mg (9.5 tablets=28.5 mg) For higher doses used in our I-MASK+ Protocol please multiply the value found in the table for 0.2 mg/kg, e.g.:
- 0.4 mg/kg: double the 0.2 mg/kg dose
- 0.6 mg/kg: triple the 0.2 mg/kg dose
COVID Risk factors for Death and Hospitalization (Medicare Population)
| Covariates | COVID-19–Related Death – OR (CI) | COVID-19 Hospitalization - OR (CI) |
|---|---|---|
| Male sex (reference: female) | 1.77 (1.71–1.84) | 1.48 (1.45–1.52) |
| Aged into Medicare (reference: not aged into Medicare) | 0.72 (.68–.76) | 0.74 (.72–.77) |
| ADI national rank (reference: ADI of 1) | ||
| 50 | 0.97 (.91–1.03) | 1.08 (1.04–1.12) |
| 100 | 1.09 (1.00–1.18) | 1.23 (1.16–1.29) |
| Logged COVID-19 circulation rate per 100,000(a) (change by 2×) | 1.98 (1.94–2.01) | 1.94 (1.92–1.96) |
| Logged population density by county(b) (change by 2×) | 1.00 (.99–1.01) | 1.02(1.01–1.03) |
| Influenza vaccination status (reference: nonvaccinated) | ||
| Standard-dose inactivated vaccine (FLUAD) | 1.04 (.96–1.11) | 1.01 (.96–1.06) |
| High-dose inactivated vaccine (Fluzone High-Dose) | 0.91 (.87–.95) | 0.95 (.92–.98) |
| Other influenza vaccine or administration code | 1.05 (1.00–1.10) | 1.05 (1.01–1.09) |
| Presence of medical conditions(c) | ||
| Hypertension | 1.02 (.97–1.07) | 1.13 (1.09–1.16) |
| Obesity | 1.10 (1.05–1.16) | 1.16 (1.13–1.20) |
| Diabetes | 1.23 (1.18–1.29) | 1.28 (1.24–1.32) |
| Hospitalized for stroke or TIA | 1.07 (.91–1.25) | 0.94 (.84–1.06) |
| Coronary revascularization | 1.03 (.85–1.26) | 0.86 (.74–1.00) |
| Atrial fibrillation | 0.97 (.92–1.01) | 0.98 (.95–1.01) |
| Congestive heart failure | 1.30 (1.23–1.36) | 1.15 (1.11–1.19) |
| Hospitalized for AMI | 0.99 (.85–1.16) | 0.89 (.79–1.00) |
| Other cerebrovascular disease | 0.90 (.85–.95) | 0.91 (.87–.94) |
| COPD | 1.14 (1.08–1.20) | 1.10 (1.06–1.14) |
| Asthma without COPD | 0.93 (.85–1.03) | 1.06 (1.00–1.13) |
| Interstitial lung disease | 1.08 (.97–1.20) | 0.95 (.88–1.03) |
| Hypersensitivity pneumonitis | 1.11 (.83–1.48) | 1.00 (.81–1.25) |
| Bronchiectasis | 0.85 (.73–1.00) | 0.89 (.80–.99) |
| Chronic liver disease | 1.07 (.97–1.19) | 1.07 (1.00–1.14) |
| Neurological or neurodevelopmental conditions | 1.08 (1.02–1.14) | 1.14 (1.10–1.19) |
| Frailty conditions | ||
| Impaired mobility | 1.45 (1.29–1.65) | 1.40 (1.27–1.54) |
| Depression | 1.32 (1.26–1.38) | 1.26 (1.22–1.30) |
| Parkinson disease | 1.27 (1.17–1.39) | 1.23 (1.15–1.32) |
| Arthritis | 0.97 (.93–1.01) | 0.99 (.97–1.02) |
| Cognitive impairment | 3.16 (3.02–3.31) | 2.24 (2.16–2.32) |
| Paranoia | 1.66 (1.54–1.80) | 1.63 (1.54–1.73) |
| Chronic skin ulcer | 1.12 (1.05–1.20) | 1.06 (1.01–1.11) |
| Skin and soft-tissue infection | 1.13 (1.06–1.20) | 1.12 (1.07–1.17) |
| Mycoses | 1.57 (1.51–1.64) | 1.47 (1.43–1.51) |
| Gout | 1.06 (.99–1.14) | 1.02 (.97–1.07) |
| Falls | 1.37 (1.30–1.46) | 1.36 (1.31–1.42) |
| Musculoskeletal problems | 0.96 (.92–1.00) | 1.01 (.98–1.03) |
| Urinary tract infection | 1.22 (1.17–1.28) | 1.19 (1.15–1.23) |
| Pneumonia | 1.89 (1.79–2.00) | 1.94 (1.86–2.02) |
| Charlson Comorbidity Index >0 | 1.08 (1.03–1.14) | 1.09 (1.06–1.13) |
| Hospital admission in past 6 mo | 1.43 (1.35–1.51) | 1.55 (1.49–1.61) |
| Immunocompromised status (reference: nonimmunocompromised) | 1.43 (1.34–1.53) | 1.24 (1.18–1.30) |
| Estimated overall interaction effects of age, dual eligibility, and race(d) | ||
| Age 80 vs 65 y | 3.09 (2.94–3.25) | 1.74 (1.68–1.80) |
| Dual eligible vs non–dual eligible | 2.17 (1.92–2.44) | 2.23 (2.08–2.39) |
| Nonwhites vs whites | ||
| Black | 2.47 (2.17–2.81) | 2.81 (2.62–3.02) |
| Hispanic | 3.11 (2.37–4.08) | 3.31 (2.83–3.87) |
| North American Native | 5.82 (3.25–10.43) | 4.22 (2.90–6.16) |
| Asian | 1.32 (.93–1.87) | 1.50 (1.23–1.82) |
| Other/unknown | 1.19 (.95–1.50) | 1.16 (1.01–1.32) |
| Effects of dual eligibility, by race | ||
| White (dual vs non-dual eligible) | 2.25 (1.97–2.55) | 2.35 (2.18–2.54) |
| Black | 1.79 (1.54–2.09) | 1.60 (1.46–1.74) |
| Hispanic | 1.46 (1.14–1.87) | 1.34 (1.16–1.54) |
| North American Native | 3.09 (1.75–5.46) | 2.44 (1.66–3.59) |
| Asian | 1.28 (.90–1.82) | 1.12 (.91–1.37) |
| Other/unknown | 2.00 (1.52–2.63) | 2.15 (1.83–2.53) |
| Nonwhites vs whites, non–dual eligible | ||
| Black | 2.53 (2.21–2.89) | 2.92 (2.71–3.14) |
| Hispanic | 3.23 (2.44–4.29) | 3.49 (2.96–4.10) |
| North American Native | 5.65 (3.09–10.32) | 4.21 (2.85–6.21) |
| Asian | 1.39 (.98–1.99) | 1.60 (1.31–1.97) |
| Other/unknown | 1.21 (.95–1.53) | 1.17 (1.01–1.34) |
| Nonwhites vs whites, dual eligible | ||
| Black | 2.02 (1.74–2.35) | 1.98 (1.81–2.16) |
| Hispanic | 2.10 (1.64–2.69) | 1.99 (1.72–2.29) |
| North American Native | 7.77 (4.39–13.75) | 4.37 (2.97–6.43) |
| Asian | 0.80 (.56–1.13) | 0.76 (.62–.94) |
| Other/unknown | 1.08 (.82–1.41) | 1.07 (.91–1.25) |
- (a) - County-level circulation rate log-transformed using a base of 2, where the OR is interpreted as the estimated OR of doubling the circulation rate.
- (b) - County-level population density log-transformed using a base of 2, where the OR is interpreted as the estimated OR of doubling the circulation rate.
- (c) - ORs obtained from logistic regression models. For the OR for the COPD and asthma without COPD groups, the reference group is people with no COPD or asthma.
- (d) - Interaction effects estimated at median age of the cohort (73 years old), except for the effects of age.
Abbreviation:
- ADI, area deprivation index;
- AMI, acute myocardial infarction;
- CI, confidence interval;
- COPD, chronic obstructive pulmonary disease;
- COVID-19, coronavirus disease 2019;
- OR, odds ratio;
- TIA, transient ischemic attack.
- Dual-eligible: Persons who are eligible for both Medicare and Medicaid are called "dual eligibles", or sometimes, Medicare-Medicaid enrollees.
Reference:
- Hector S Izurieta, David J Graham, Yixin Jiao, Mao Hu, Yun Lu, Yue Wu, Yoganand Chillarige, Michael Wernecke, Mikhail Menis, Douglas Pratt, Jeffrey Kelman, Richard Forshee, Natural History of Coronavirus Disease 2019: Risk Factors for Hospitalizations and Deaths Among >26 Million US Medicare Beneficiaries, The Journal of Infectious Diseases, 2020;, jiaa767, https://doi.org/10.1093/infdis/jiaa767
COVID Ideas/Opinions
- When Vanden Bossche initially reviewed the high vaccination rates in Israel, Vanden Bossche warned the absence of a natural immunity population to fight the virus would lead to an uncontrollable spread of the virus in the vaccinated community. The higher the vaccination rates, the more serious the spread of the virus amid the population that only carries the immune system protection provided by the vaccine.
- "The widespread vaccination rate is creating pressure on the virus to mutate into variants with higher levels of contagion. The unvaccinated group has been keeping the pressure down by defeating the virus and carrying natural immunity. However, as the unvaccinated population is increasingly made smaller, the pressure on the virus to mutate increases. Subsequently, these mutations stay at higher or more effective levels of infection."
- Geert Vanden Bossche
COVID Treatments
- OTC COVID Precautions
For: Prevention, Post-exposure, and Symptomatic
- Use a Mouthwash 2x per day
- Gargle, do not swallow
- Choose any mouthwash with Cetylpyridinium Chloride(CPC):
- ACT
- Scope
- Crest
- Or choose an essential oil based mouthwash like Listerine made from:
- Thymol (thyme)
- Menthol
- Eucalyptus
- Choose any mouthwash with Cetylpyridinium Chloride(CPC):
- Monoclonal Antibodies:
The new analyses show REGEN-COV reduced the risk of contracting COVID-19 (i.e., laboratory-confirmed symptomatic SARS-CoV-2 infections) by 81.6% during the pre-specified follow-up period (months 2 - 8 ), maintaining the 81.4% risk reduction during the first month after administration, which was previously reported in The New England Journal of Medicine (https://www.nejm.org/doi/full/10.1056/NEJMoa2109682).
But in this trial of prophylactic use, the antibodies were delivered by subcutaneous injections, not infusions
And eight months was the end of the study. Not necessarily the end of protection by the antibodies.
- Press Release
Single dose of REGEN-COV (1,200 mg subcutaneous) reduced the risk of COVID-19 by 81.6% during the pre-specified follow-up period (months 2-8), maintaining the 81.4% risk reduction previously reported during month 1
During the 8-month assessment period there were 0 hospitalizations for COVID-19 in the REGEN-COV group and 6 in the placebo group
The fully human antibodies in REGEN-COV were developed to provide long-lasting protective effects without any artificial mutations or sequences
- Press Release
- COVID Pills
- Merck and Ridgeback Biotherapeutics
- Drug Name: molnupiravir
- MOA: Inhibits the replication of the coronavirus inside the body
- Study Population: Every participant was unvaccinated and had at least one underlying factor that put them at greater risk of developing a more severe case of the virus
- Adverse events:
- Comparable in the molnupiravir and placebo groups, with around 10% reporting adverse events.
- Just 1.3% of the molnupiravir group discontinued therapy due to an adverse event - less than the 3.4% of the placebo group who did so
- Results:
- 7.3% of patients treated with molnupiravir were hospitalized within 29 days. Of the patients who received a placebo, 14.1% were hospitalized or died by day 29.
- No deaths were reported in patients who were given molnupiravir within the 29-day period, while eight deaths were reported in placebo-treated patients
- Reduces the risk of hospitalization or death by around 50% for patients with mild or moderate cases of Covid
Molnupiravir reduced the risk of hospitalization and/or death across all key subgroups; efficacy was not affected by timing of symptom onset or underlying risk factor. Additionally, based on the participants with available viral sequencing data (approximately 40% of participants), molnupiravir demonstrated consistent efficacy across viral variants Gamma, Delta, and Mu.
Table 117: Original data Group Hospitalization Death Total Treatment 28 0 385 Control 53 8 377 NNT 14.7 47.6 PEEV 14.06% 2.12% ARR 6.8% 2.1% RRR 48.3% Table 118: Updated Nov 2021 Group Hospitalization Death Total Treatment 48 1 709 Control 68 9 699 NNT 33.3 90.9 PEEV 9.73% 1.29% ARR 3% 1.1% RRR 30.4% 89%
Reference:
- https://www.merck.com/news/merck-and-ridgebacks-investigational-oral-antiviral-molnupiravir-reduced-the-risk-of-hospitalization-or-death-by-approximately-50-percent-compared-to-placebo-for-patients-with-mild-or-moderat/
- https://www.merck.com/news/merck-and-ridgeback-biotherapeutics-provide-update-on-results-from-move-out-study-of-molnupiravir-an-investigational-oral-antiviral-medicine-in-at-risk-adults-with-mild-to-moderate-covid-19/
- Pfizer
- Drug Name: PF-07321332 (Paxlovid)
- MOA: Protease inhibitor - works by inhibiting an enzyme the virus needs to replicate in human cells
- Used along with an HIV drug, which helps slow the metabolism of Pfizer's pill in order for it to remain active in the body for longer periods of time at higher concentrations
- Results:
- Used with an HIV drug, cut the risk of hospitalization or death by 89% in high-risk adults who've been exposed to the virus
- Study of 1,219 adults
6 hospitalizations and 0 deaths out of the 607 trial participants who received the pill in combination with the HIV drug within five days of symptom onset. That compares with 41 hospitalizations and 10 deaths out of the 612 people who received a placebo.
Group Hospitalizations Deaths Total Treatment 6 0 607 Control 41 10 612 NNT 17.5 62.5 PEEV 6.7% 1.63% ARR 5.7% 1.6% RRR 85.2% 100%
Reference:
- Merck and Ridgeback Biotherapeutics
- Current Authorized COVID-19 Outpatient Therapeutics
Treatment Guidelines: https://www.covid19treatmentguidelines.nih.gov/therapies/anti-sars-cov-2-antibody-products/anti-sars-cov-2-monoclonal-antibodies/
- Monoclonal Antibodies (MABs) for Pre-Exposure Prophylaxis
- Evusheld (tixagevimap co-packaged and administered together with cilgavimab; intramuscular injection)
- MABs for Post-Exposure Prophylaxis
- Bamlanivimab plus etesevimab (Intravenous (IV) infusion)
- Casirivimab plus imdevimab (IV infusion or subcutaneous (SQ) injection)
- Sotrovimab (IV infusion)
- MABs for Early Treamtent of COVID-19
- Bamlanivimab plus etsevimab (IV infusion)
- Casirivimab plus imdevimab (IV infusion or SQ injection)
- Sotrovimab (IV infusion)
Ref:
- Florida Department of Health Dec 16, 2021
- Monoclonal Antibodies (MABs) for Pre-Exposure Prophylaxis
- COVID-19 Treatments Pending FDA Approval
- In November 2021, Merck released study results about an oral antiviral drug to treat COVID-19. The Antimicrobial Drugs Advisory Committee to the Food and Drug Administration (FDA) recommended emergency use authorization (EUA) for molnupiravir. FDA approval is pending.
- In December 2021, Pfizer released study results for their oral antiviral treatment called Paxlovid. Pfizer has submitted its data, and FDA approval is pending.
Ref:
- Florida Department of Health Dec 16, 2021
- Emerging Treatment Options for COVID-19
- Fluvoxamine
- Recent evidence shows a potential therapeutic role of fluvoxamine (administered orally) for COVID-19. See these links for more information: JAMA Network; Lancet Global Health
- https://jamanetwork.com/journals/jama/fullarticle/2773108
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8550952/
- Budesonide
- Recent evidence shows a potential therapeutic role of budesonide (an inhaled glucocorticoid) for COVID-19. See these links for more information: The Lancet; The Lancet Respiratory Medicine
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)01744-X/fulltext
- https://www.thelancet.com/article/S2213-2600(21)00160-0/fulltext
Ref:
- Florida Department of Health Dec 16, 2021
- Fluvoxamine
- HCQ and COVID 19
No evidence of benefit in COVID-19:
- Prophylaxis
- Efficacy and Safety of Hydroxychloroquine vs Placebo for Pre-exposure SARS-CoV-2 Prophylaxis Among Health Care Workers Randomized Clinical Trial
- Abella BS, Jolkovsky EL, Biney BT, et al. Efficacy and Safety of Hydroxychloroquine vs Placebo for Pre-exposure SARS-CoV-2 Prophylaxis Among Health Care Workers: A Randomized Clinical Trial. JAMA Intern Med. Published online September 30, 2020. https://doi.org/10.1001/jamainternmed.2020.6319
- Treatment
- Effect of Hydroxychloroquine on Clinical Status at 14 Days in Hospitalized Patients With COVID-19A Randomized Clinical Trial
- Interventions Patients were randomly assigned to hydroxychloroquine (400 mg twice daily for 2 doses, then 200 mg twice daily for 8 doses) (n = 242) or placebo (n = 237).
- In this randomized clinical trial that included 479 hospitalized adults with respiratory symptoms from COVID-19, the distribution of the day 14 clinical status score (measured using a 7-category ordinal scale) was not significantly different for patients randomized to receive hydroxychloroquine compared with placebo (adjusted odds ratio, 1.02).
- Meaning: These findings do not support the use of hydroxychloroquine for treatment of COVID-19 among hospitalized adults.
- Self WH, Semler MW, Leither LM, et al. Effect of Hydroxychloroquine on Clinical Status at 14 Days in Hospitalized Patients With COVID-19: A Randomized Clinical Trial. JAMA. 2020;324(21):2165–2176. https://doi.org/10.1001/jama.2020.22240
References:
- Abella BS, Jolkovsky EL, Biney BT, et al. Efficacy and Safety of Hydroxychloroquine vs Placebo for Pre-exposure SARS-CoV-2 Prophylaxis Among Health Care Workers: A Randomized Clinical Trial. JAMA Intern Med. Published online September 30, 2020. https://doi.org/10.1001/jamainternmed.2020.6319
- Self WH, Semler MW, Leither LM, et al. Effect of Hydroxychloroquine on Clinical Status at 14 Days in Hospitalized Patients With COVID-19: A Randomized Clinical Trial. JAMA. 2020;324(21):2165–2176. https://doi.org/10.1001/jama.2020.22240
- Prophylaxis
- COVID Ivermectin
- Total with COVID-19: 41608
- Ivermectin: 1072
- Remdesivir: 40536
Ivermectin reduced mortality vs remdesivir: OR = 0.308 p = <0.0001
- 70% less likely to die if treated with ivermectin than remdesivir
Total: 159561
COVID 19 RR Died RR Hops Ivermectin 4311 3.7% 0.56 25 0.8% 0.32 44 No ivermectin 3034 6.6% 79 2.6% 99 Small dose (0.2mg/kg/d x2d/2wk)
- 44% reduction in infection rate RR 0.56
- 68% reduction in mortality rate p = <0.0001
- 56% reduction in hospitalization rate p = <0.0001
Reference:
- I. Efimenko, S. Nackeeran, S. Jabori, J.A. Gonzalez Zamora, S. Danker, D. Singh, Treatment with Ivermectin Is Associated with Decreased Mortality in COVID-19 Patients: Analysis of a National Federated Database, International Journal of Infectious Diseases, Volume 116, Supplement, 2022, Page S40, ISSN 1201-9712, https://doi.org/10.1016/j.ijid.2021.12.096. (https://www.sciencedirect.com/science/article/pii/S1201971221009887)
COVID Vaccines
- COVID-19 Vaccines
Vaccine developer: Pfizer Moderna AstraZeneca Johnson & Johnson When approved/expected approval Dec. 11 Dec. 18 Could submit application for emergency use authorization in late March. Submitted application for emergency use authorization on Feb. 5. What percentage of people did it protect from getting infected in clinical studies? 95% 94.1% 70% 66% How many shots do you need? Two doses, 3 weeks apart Two doses, 4 weeks apart Two doses, a month apart One dose What are the side effects? Fatigue, headache, chills, muscle pain, especially after the second dose. Fever, muscle aches, headaches lasting a few days. Effects worse after second dose. Injection site pain, fever, muscle aches, headache. Not yet available. How many doses will be available, and when? 50 million, starting Dec. 18; 1.3 billion in 2021. 20 million, starting Dec. 21; 80 million for U.S. in 2021. 3 billion planned for 2021. Not yet available. Who is it recommended for? People 16 years and older. People 18 years and older. Not yet available. Not yet available. What about pregnant women and nursing moms? Pregnant women or nursing moms who want the COVID-19 vaccine should get one, experts say. The vaccine has not yet been studied in pregnant women. Read guidelines here. There's limited data. Studies in rats who were immunized before and during pregnancy found no safety concerns. The CDC says pregnant women may choose to receive the vaccine. Not yet available. Not yet available. Is there anyone who shouldn't get the vaccine? People with a history of serious allergic reactions, anyone with a history of allergic reactions to vaccine ingredients including polyethylene glycol, and anyone with a history of allergic reactions to polysorbate. People with a history of serious allergic reactions, anyone with a history of allergic reactions to vaccine ingredients including polyethylene glycol, and anyone with a history of allergic reactions to polysorbate. Not yet available. Not yet available. Any significant side effects? 50 cases of anaphylaxis in people who received the vaccine, mostly women. Four cases of Bell's palsy, a type of temporary facial paralysis, reported in people who received the vaccine. This is not more than would be expected in the general population. 21 cases of anaphylaxis in people who received the vaccine, all in women. Four cases of Bell's palsy reported in the clinical trials including 3 in the vaccine group, and 1 in the placebo group. This is not more than would be expected in the general population. Four total serious side effects, including two cases of transverse myelitis. One person went to the hospital for fever associated with the vaccine. Four other serious cases were not related to the vaccine. What about people with lowered immune function? Ok for people whose immune function is lowered by HIV or immunosuppressing drugs if they have no other reasons to avoid it. There is limited safety data in this group. Ok for people whose immune function is lowered by HIV or immunosuppressing drugs if they have no other reasons to avoid it. There is limited safety data in this group. Not yet available. Not yet available. What about people with autoimmune diseases? No data are available on the safety or effectiveness of mRNA vaccines in people with autoimmune disease. People with autoimmune conditions may still get the shots if they have no other reasons to avoid vaccination. No data are available on the safety or effectiveness of mRNA vaccines in people with autoimmune disease. People with autoimmune conditions may still get the shots if they have no other reasons to avoid vaccination. Not yet available. Not yet available. Is the vaccine safe for people with a history of Guillain-Barre Syndrome (GBS)? To date, no cases of GBS have been seen in people vaccinated for COVID-19. The CDC says a history of GBS is not a reason to avoid vaccination. To date, no cases of GBS have been seen in people vaccinated for COVID-19. The CDC says a history of GBS is not a reason to avoid vaccination. Not yet available. Not yet available. Reference:
- Moderna
https://www.fda.gov/media/144434/download
The Moderna COVID-19 Vaccine, mRNA-1273 (100μg) is administered intramuscularly as a series of two doses (0.5 mL each), given 28 days apart.
Study mRNA-1273-P301 is an ongoing randomized, stratified, observer-blind, placebo-controlled study to evaluate the efficacy, safety and immunogenicity of mRNA-1273 administered in 2 doses 28 days apart in adults 18 years of age and older. The study took place in 99 sites in the United States. Participants (N=30,351) were randomized 1:1 to receive intramuscular injections of either 100 μg of mRNA-1273 vaccine (n=15,181) or placebo (n=15,170) on Day 1 and Day 29. Participants were stratified by age and health risk into one of three groups: 18 to <65 years of age and not at risk for progression to severe COVID-19, 18 to <65 years of age and at risk for progression to severe COVID-19, and ≥65 years of age, with the latter two groups consisting of 41.4% of the study population. Participants were considered at risk for progression to severe COVID-19 if they had underlying comorbidities including diabetes, chronic lung disease, severe obesity, significant cardiovascular disease, liver disease, or infection with HIV. The study included 24,907 (82.1%) participants considered at occupational risk for acquiring SARS-CoV-2 infection, of whom 7,613 (25.1%) were healthcare workers. Other essential workers were also represented. The primary efficacy endpoint was efficacy of the vaccine to prevent protocol-defined COVID-19 occurring at least 14 days after the second dose in participants with negative SARS-CoV-2 status at baseline (i.e., negative RT-PCR and negative serology against SARS-CoV-2 nucleocapsid on Day 1).
Primary Efficacy Endpoint
The primary efficacy endpoint was efficacy of the vaccine to prevent protocol-defined COVID-19 occurring at least 14 days after the second dose in participants with negative SARS-CoV-2 status at baseline (i.e., negative RT-PCR and negative serology against SARS-CoV-2 nucleocapsid on Day 1). The primary analysis was based on the Per-Protocol Set, defined as all randomized, baseline SARS-CoV-2 negative participants who received planned doses per schedule and have no major protocol deviations. For the primary efficacy endpoint, the case definition for a confirmed COVID-19 case was defined as:-At least TWO of the following systemic symptoms: Fever (≥38ºC), chills, myalgia, headache, sore throat, new olfactory and taste disorder(s), or -At least ONE of the following respiratory signs/ symptoms: cough, shortness of breath or difficulty breathing, OR clinical or radiographical evidence of pneumonia; and -NP swab, nasal swab, or saliva sample (or respiratory sample, if hospitalized) positive for SARS-CoV-2 by RT-PCR
Table 119: Table 9. Interim Analysisa for Primary Efficacy Endpoint, COVID-19 Starting 14 Days After the 2nd Dose, Per-Protocol Set Primary Endpoint: COVID-19 (per adjudication committee assessment) Vaccine Group N=13934 Cases n (%)(Incidence rate per 1,000 person-years) Placebo Group N=13883 Cases n (%)(Incidence rate per 1,000 person-years) Vaccine Efficacy (VE)% (95%CI)* Met Predefined Success Criterion** All participants 5 (<0.1)1.840 90 (0.6)33.365 94.5% (86.5%, 97.8%) Yes 18 to <65 5 / 10407 (<0.1)2.504 75 / 10384 (0.7)37.788 93.4% (83.7%, 97.3%) NA 65 and older 0 / 3527 15/3499(0.4)21.046 100% NA COVID-19: symptomatic COVID-19 requiring positive RT-PCR result and at least 2 systemic symptoms or 1 respiratory symptom. Cases starting 14 days after the 2nd dose. All potential COVID-19 cases starting 14 days after the 2nd dose in the clinical database as of 07-Nov-2020 have been sent to adjudication committee, and have been adjudicated for this analysis (07-Nov-2020 is the datacutoff date for efficacy). One case (in the placebo group) was assessed as a case by the adjudication committee but did not meet case definition based on statistical analysis plan (participant had body aches, nasal congestion, rhinorrhea, which were not protocol defined symptoms).
*VE is calculated as 1-ratio of incidence rates (mRNA-1273/placebo) and 95% CI from the stratified Cox proportional hazard model.
**The one-sided p-value is <0.0001 from the stratified Cox proportional hazard model to test the null hypothesis of VE≤3 0%, achieving the pre-specified efficacy boundary: the one-sided nominal alpha of 0.0049 based on 95 cases using the Lan-DeMets O'Brien-Fleming spending function
(My Calculations)
Absolute Risk Reduction (95% CI) -0.006 (-0.007 to -0.005) Relative Risk Reduction (95% CI) -0.945 (0.022 to 0.135) Number Needed to Treat -166.7 Odds Ratio 0.055 Relative Risk 0.055 Patient Expected Event Rate: 0.65%
- Pfizer
Phase 3 trials of the Pfizer-BioNTech vaccine, eight of the 17,411 people who were given the vaccine wound up becoming sick with COVID-19, compared with 162 of the 17,511 who got the placebo. Using that and other data, researchers determined that the vaccine was 95% effective at preventing COVID-19.
Table 6. Final Analysis of Efficacy of BNT162b2 Against Confirmed COVID-19 From 7 Days AfterDose 2 in Participants Without Evidence of Prior SARS-CoV-2 Infection - Evaluable Efficacy Population
Pre-specified Age Group BNT162b2 N(a) = 18198 Cases n1(b) Surveillance Time(c)(n2(d)) Placebo N(a) =18325 Cases n1(b) Surveillance Time(c)(n2(d)) Vaccine Efficacy %(95% CI) Met Predefined Success Criterion(*) All participants 8 2.214 (17411) 162 2.222 (17511) 95.0(90.3, 97.6)(e) Yes 16 to 55 years 5 1.234 (9897) 114 1.239 (9955) 95.6(89.4, 98.6)(f) NA > 55 years and older 3 0.980 (7500) 48 0.983 (7543) 93.7(80.6, 98.8)(f) NA - (*) Success criterion: the posterior probability that true vaccine efficacy > 30% conditioning on the available data is >99.5% at the final analysis
- (a) N = number of participants in the specified group.
- (b) n1 = Number of participants meeting the endpoint definition.
- (c) Total surveillance time in 1000 person-years for the given endpoint across all participants within each group at risk for the endpoint. Time period for COVID-19 case accrual is from 7 days after Dose 2 to the end of the surveillance period.
- (d) n2 = Number of participants at risk for the endpoint.
- (e) Credible interval for VE was calculated using a beta-binomial model with prior beta (0.700102, 1) adjusted for surveillance time.
- (f) Confidence interval (CI) for VE is derived based on the Clopper and Pearson method adjusted to the surveillance time
(My Calculations)
Absolute Risk Reduction (95% CI) -0.008 (-0.009 to -0.007) Relative Risk Reduction (95% CI) -0.951 (0.024 to 0.100) Number Needed to Treat -125 Odds Ratio 0.049 Relative Risk 0.049 Patient Expected Event Rate: 0.89%
- Adverse Events
Cumulatively, through 28 February 2021 (3 months of use)
Table 120: Table 1: General Overview: Selected Characteristics of All Cases Received During the Reporting Interval Characteristics Relevant cases (N=42086) Gender: Female 29914 Male 9182 No Data 2990 Age range (years): 0.01 -107 years Mean = 50.9 years n = 34952 ≤ 17 175 18-30 4953 31-50 13886 51-64 7884 65-74 3098 ≥ 75 5214 Unknown 6876 Case outcome: Recovered/Recovering 19582 Recovered with sequelae 520 Not recovered at the time of report 11361 Fatal 1223 Unknown 9400 Reference:
- Johnson & Johnson
Released Stats:
- Vaccine Candidate 72% Effective in the US and 66% Effective Overall at Preventing Moderate to Severe COVID-19, 28 Days after Vaccination
- 85% Effective Overall in Preventing Severe Disease and Demonstrated Complete Protection Against COVID-19 related Hospitalization and Death as of Day 28
- Protection Against Severe Disease Across Geographies, Ages, and Multiple Virus Variants, including the SARS-CoV-2 Variant from the B.1.351 Lineage[1] Observed in South Africa
- Single-shot compatible with standard vaccine distribution channels provides important tool in pandemic setting
The Janssen vaccine is a recombinant vector vaccine that uses a human adenovirus to express the SARS-CoV-2 spike protein. SARS-CoV-2 is the virus that causes COVID-19. Adenoviruses are a group of viruses that cause infections in the respiratory and gastrointestinal tracts; the adenovirus vector used in the experimental vaccine has been modified, so that it can no longer replicate in humans and cause illness. In developing the vaccine, Janssen employed the same vector used in the first dose of its prime-boost vaccine regimen against Ebola virus disease (Ad26 ZEBOV and MVN-BN-Filo), developed under a long-standing partnership with BARDA and granted marketing authorization by the European Commission in July 2020. Unlike the two COVID-19 vaccines currently authorized by the U.S. Food and Drug Administration for emergency use (Pfizer and Moderna vaccines), the Janssen investigational vaccine requires only a single vaccination.
The Phase 3 ENSEMBLE study is a randomized, double-blind, placebo-controlled clinical trial designed to evaluate the safety and efficacy of a single vaccine dose versus placebo in up to 60,000 adults 18 years old and older, including significant representation from those that are over age 60. The study was designed to evaluate the safety and efficacy of the Janssen investigational vaccine in protecting against both moderate and severe COVID-19 disease, with assessment of efficacy as of day 14 and as of day 28 as co-primary endpoints.
Overall, the results indicate that the J&J vaccine is 66% effective for the prevention of moderate and severe illness, and was shown to be effective against emerging viral variants at day 28. Level of protection varied based on geographical location:
- United States: 72%
- Latin American countries: 66%
- South Africa: 57%
The primary efficacy analysis was based on the per-protocol set, which consisted of all vaccinated participants who were SARS-CoV-2 seronegative at time of vaccination and who had no major protocol deviations.
Table 121: Table 10. Vaccine Efficacy Against Centrally Confirmed Moderate to Severe/Critical COVID-19 With Onset at Least 14 and at Least 28 Days After Vaccination, Per-Protocol Set, Study 3001 Onset at Least: 14 Days 14 Days 14 Days 28 Days 28 Days 28 Days Co-primary Endpoint Subgroup Ad26.COV2.S Cases (N)aPerson-yrsb Placebo Cases (N)Person-yrs VE% (95% CI) Ad26.COV2.S Cases (N)Person-yrs Placebo Cases (N)Person-yrs VE%(95% CI) All participants 116(19514) 3116.6 348(19544) 3096.1 66.9%(59.0, 73.4) 66 (19306) 3102.0 193(19178) 3070.7 66.1%(55.0,74.8) Age 18-59 years 95(12750) 2106.8 260(12782) 2095.0 63.7%(53.9, 71.6) 52(12617) 2097.6 152(12527) 2077.0 66.1%(53.3,75.8) Age ≥60 years 21(6764) 1009.8 88(6762) 1001.2 76.3%(61.6, 86.0) 14(6689)1004.4 41(6651)993.6 66.2%(36.7,83.0)
(My Calculations)
Table 122: At 14 Days Absolute Risk Reduction (95% CI) -0.012 (-0.014 to -0.010) Relative Risk Reduction (95% CI) -0.666 (0.271 to 0.412) Number Needed to Treat -83.3 Odds Ratio 0.330 Relative Risk 0.334 Patient Expected Event Rate (PEER): 1.78% (COVID Prevalence during study)
Secondary Efficacy Analyses
Efficacy Against Any Symptomatic COVID-19 Efficacy against any symptomatic COVID-19 (including mild disease) and efficacy based on a less restrictive case definition (FDA harmonized case definition), with onset at least 14 days or 28 days after vaccination, were overall similar to results obtained for the primary efficacy endpoint of efficacy against moderate to severe/critical COVID-19.
Table 123: Table 15. Vaccine Efficacy Against Centrally Confirmed COVID-19a With Onset at Least 14 or at Least 28 Days After Vaccination, Per-Protocol Set, Study 3001 Onset at Least: 14 Days 14 Days 14 Days 28 Days 28 Days 28 Days Ad26.COV2.S Cases (N)Person-yrs Placebo Cases (N)Person-yrs VE% (95% CI) Ad26.COV2.S Cases (N)Person-yrs Placebo Cases (N)Person-yrs VE%(95% CI) Symptomatic COVID-19, any severity(a) 117 (19514) 3116.5 351 (19544) 3095.9 66.9% (59.1, 73.4) 66 (19306) 3102.0 195 (19178) 3070.5 66.5% (55.5,75.1) FDA harmonized COVID-19 cases 114 (19514) 3116.6 345 (19544) 3096.3 67.2% (59.3,73.7) 65 (19306) 3102.0 193 (19178) 3070.6 66.7% (55.6, 75.2) a Includes mild, moderate, and severe/critical cases
COVID-19 Requiring Medical Intervention
The endpoint of COVID-19 requiring medical intervention is defined as participant requiring hospitalization, ICU admission, mechanical ventilation, and/or ECMO, linked to objective measures such as decreased oxygenation, X-ray or computed tomography (CT) findings, andlinked to any molecularly confirmed, COVID-19 with onset at least 14 days and at least 28 days post-vaccination.
Table 124: Table 17. Vaccine Efficacy of First Occurrence COVID-19 Requiring Medical Intervention Based on MRU, With Onset at Least 14 or at Least 28 Days After Vaccination, Per-Protocol Set, Study 3001 Onset at Least: 14 Days 14 Days 14 Days 28 Days 28 Days 28 Days Ad26.COV2.S Cases (N)Person-yrs Placebo Cases (N)Person-yrs VE% (95% CI) Ad26.COV2.S Cases (N)Person-yrs Placebo Cases (N)Person-yrs VE%(95% CI) Centrally Confirmed 2 (19514)3126.9 8 (19544) 3126.1 75.0%(-25.3, 97.4) 0 (19306)3106.4 5(19178) 3084.4 Any positive PCR 2 (19514)3125.9 14 (19544)3125.8 85.7% (37.8,98.4) 0 (19306)3106.4 7 (19178)3084.4 100%(31.1, 100.0)
(My Calculations)
Table 125: Of COVID Positive people, number to vaccinate for medical intervention Absolute Risk Reduction (95% CI) -0.023 (-0.054 to 0.008) Relative Risk Reduction (95% CI) -0.571 (0.099 to 1.860) Number Needed to Treat -43.5 Odds Ratio 0.419 Relative Risk 0.429 (Vaccinated: 2 of 116; and Control: 14 of 348)
References:
- NovaVax
Primary End Point
- The aim of the trial was to estimate, as the primary end point, the efficacy of NVX-CoV2373 for the prevention of a first occurrence of reverse-transcriptase–polymerase-chain-reaction (RT-PCR)–confirmed symptomatic mild, moderate, or severe Covid-19
Results:
- Among the 25,452 participants in the per-protocol efficacy analysis population who were followed through April 19, 2021 (median follow-up for efficacy, approximately 3 months), 77 central laboratory–confirmed Covid-19 cases occurred: 14 cases in NVX-CoV2373 recipients and 63 in placebo recipients (incidence, 3.3 cases per 1000 person-years [95% CI, 1.6 to 6.9] and 34.0 cases per 1000 person-years [95% CI, 20.7 to 55.9], respectively). These results yielded a vaccine efficacy of 90.4% (95% CI, 82.9 to 94.6; P<0.001)
- All the cases reported in NVX-CoV2373 recipients were mild in severity, whereas 14 moderate-to-severe cases (10 moderate and 4 severe) occurred in the placebo group, yielding a vaccine efficacy against moderate-to-severe Covid-19 of 100% (95% CI, 87.0 to 100)
- Vaccine efficacy against confirmed Covid-19 meeting the definition of the primary end point among participants who were at high risk for acquisition or complications of Covid-19 was 91.0% (95% CI, 83.6 to 95.0)
Side Effects:
- After each dose, the most frequently reported solicited local adverse events were tenderness and injection-site pain.
- The median duration of these events was 2 days or less
- Severe (grade ≥3) local reactions were infrequent overall but were more common among NVX-CoV2373 recipients than among placebo recipients, particularly after dose 2 (1.1% of NVX-CoV2373 recipients and <1% of placebo recipients after dose 1 and 6.7% and <1%, respectively, after dose 2)
- The most common solicited systemic adverse events were headache, myalgia, fatigue, and malaise, which were detected more frequently among NVX-CoV2373 recipients and after the second injection and lasted for a median duration of 1 day or less.
Conclusion:
- NVX-CoV2373 was safe and effective for the prevention of Covid-19. Most breakthrough cases were caused by contemporary variant strains.
—
(My Calculations)
Table 126: After 3 Months Absolute Risk Reduction (95% CI) -0.007 (-0.009 to -0.005) Relative Risk Reduction (95% CI) -0.896 (0.058 to 0.185) Number Needed to Treat -142.9 Odds Ratio 0.104 Relative Risk 0.104 Patient Expected Event Rate: 0.77 % PEER (COVID Prevalence during study)
Reference:
- Efficacy and Safety of NVX-CoV2373 in Adults in the United States and Mexico
- Moderna
- COVID Vaccine Comparison edit
Pfizer Moderna J&J Novavax RRR 95.1 % 94.5 % 66.7 % 91 % NNT 125 167 83 143 ARR 0.8 % 0.6 % 1.2 % 0.7 % PEER 0.89 % 0.65 % 1.78 % 0.77 % - COVID Vaccine Adverse Effects
Pfizer vaccine (after 2nd dose):
- 66% reported pain
- 60% fatigue
- 52% headache
- 38% muscle pain
- 22% joint pain
- 16% fever
- 2% vomiting.
Moderna vaccine (after 2nd dose):
- 88% experienced pain
- 16% fever, including 1.4% severe cases
- 59% headache
- 66% fatigue
- 43% joint pain
- 19% vomiting.
Novavax:
- tenderness at the injection site for 73% of participants
- pain upon and after vaccination for 60% of participants
- fatigue for 50% of the participants
- muscle pain for 48% of participants
- headache for 44% of participants
- malaise for 39% of participants
- fever for 6% of participants, including severe cases for 0.37%
- nausea and vomiting for 11% of participants, including severe cases for 0.23%
- joint pain for 22% of participants, including severe cases for 2.44%
- COVID Vaccine Adverse Effects
- COVID Vaccine Efficacy Calculations
Table 127: Risk for COVID-19 Infection, Hospitalization, and Death By Age Group Rate compared to 18-29 years old 0-4 years old 5-17 years old 18-29 years old 30-39 years old 40-49 years old 50-64 years old 65-74 years old 75-84 years old 85+ years old Cases <1x 1x Reference group 1x 1x 1x 1x 1x 1x Hospitalization <1x <1x Reference group 2x 2x 4x 5x 8x 10x Death <1x <1x Reference group 4x 10x 25x 65x 150x 370x - All rates are relative to the 18- to 29-year-old age category. This group was selected as the reference group because it has accounted for the largest cumulative number of COVID-19 cases compared to other age groups. Sample interpretation: Compared with 18- to 29-year-olds, the rate of death is four times higher in 30- to 39-year-olds, and 370 times higher in those who are 85 years and older. (In the table, a rate of 1x indicates no difference compared to the 18- to 29-year-old age category.)
- https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html
- Updated Nov. 22, 2021
Table 128: Risk for COVID-19 Infection, Hospitalization, and Death By Race/Ethnicity Rate ratios compared to White, Non-Hispanic persons American Indian or Alaska Native, Non-Hispanic persons Asian, Non-Hispanic persons Black or African American, Non-Hispanic persons Hispanic or Latino persons Cases 1.6x 0.6x 1.0x 1.6x Hospitalization 3.3x 0.8x 2.6x 2.5x Death 2.2x 0.9x 1.9x 2.1x - Race and ethnicity are risk markers for other underlying conditions that affect health, including socioeconomic status, access to health care, and exposure to the virus related to occupation, e.g., frontline, essential, and critical infrastructure workers.
- https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html
- Updated Nov. 22, 2021
Table 129: Estimated rates of COVID-19 disease outcomes per 100,000, by age group — United States, February 2020-September 2021 Infection rate per 100,000 Symptomatic Illness rate per 100,000 Hospitalization rate per 100,000 Death rate per 100,000 Age group Estimate Rate % 95% UI Estimate Rate % 95% UI Estimate Rate % 95% UI Estimate Rate % 95% UI 0-17 years 35490 0.3549 29,335 – 43,414 30253 0.3025 26,240 – 35,295 366 0.00366 309 – 434 0.9 0.000009 0.7-1.6 18-49 years 54860 0.5486 45,740 – 66,055 46724 0.4672 41,213 – 53,525 1457 0.01457 1,255 – 1,704 43.7 0.000437 41.0 – 46.6 50-64 years 43656 0.4366 36,428 – 52,439 37239 0.3724 32,859 – 42,526 3200 0.03200 2,822 – 3,671 253.5 0.002535 246.2 – 261.3 65+ years 32363 0.3236 26,101 – 40,895 26278 0.2628 23,200 – 30,085 5807 0.05807 5,146 – 6,617 1296.5 0.012965 1274.5 – 1319.1 All ages 44650 0.4465 38,374 – 52,262 37764 0.3776 33,821 – 42,630 2286 0.02286 2,046 – 2,579 280.7 0.002807 275.0 – 286.7 - Adjusted rates are presented in two parts: an uncertainty interval [UI] and a point estimate. The uncertainty interval provides a range in which the true number or rate of COVID-19 infections, symptomatic illnesses, hospitalizations, or deaths would be expected to fall if the same study was repeated many times, and it gives an idea of the precision of the point estimate. A 95% uncertainty interval means that if the study were repeated 100 times, then 95 out of 100 times the uncertainty interval would contain the true point estimate. Conversely, in only 5 times out of a 100 would the uncertainty interval not contain the true point estimate.
- https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/burden.html
Table 130: Baseline COVID Rates Infection Symptomatic Illness Hospitalization Death Age group Rate % Rate % Rate % Rate % 0-17 years 0.3549 0.3025 0.00366 0.000009 18-49 years 0.5486 0.4672 0.01457 0.000437 50-64 years 0.4366 0.3724 0.03200 0.002535 65+ years 0.3236 0.2628 0.05807 0.012965 All ages 0.4465 0.3776 0.02286 0.002807 Death:
- Patients aged > 75 years (OR 3.25 [95% CI 1.91, 5.52])
- Male patients (OR 1.81 [95% CI 1.02, 3.19])
- Those with concomitant neurological disorders (OR 2.07 [95% CI 1.15, 3.74])
- Renal disease (OR 1.91 [95% CI 0.82, 4.45])
- Pulmonary disease (OR 1.83 [95% CI 1.05, 3.20])
- Diabetes (OR 1.62 [95% CI 0.95, 2.76])
- Cancer (OR 1.52 [95% CI 0.85, 2.70])
- Those who required oxygen by face mask (OR 2.05 [95% CI 1.25, 3.38]) had a higher risk of death in our cohort
- The risk of death was also high in those with higher CRP (OR 1.25 [95% CI 1.08, 1.45], 50 mg/L increase)
- Serum creatinine (OR 1.09 [95% CI 0.98, 1.21], 50 μmol/L increase) levels
- Those with low hemoglobin (OR 1.14 [95% CI 0.99, 1.32], 1 g/L decrease)
- Platelet (OR 1.46 [95% CI 1.04, 2.04], 100 G/L decrease) count
ICU hospitalization.
- Patients aged ≤ 75 years (OR 2.79 [95% CI 1.67, 4.66])
- those with concomitant pulmonary disease (OR 1.64 [95% CI 0.96, 2.78])
- those without dementia (OR 3.57 [95% CI 0.8, 15.9])
- those requiring oxygen by face mask (OR 1.53 [95% CI 0.97, 2.42]) were at higher risk of being hospitalized in the ICU.
- Higher CRP (OR 1.47 [95% CI 1.28, 1.68], 50 mg/L increase)
- hemoglobin (OR 1.31 [95% CI 1.14, 1.52], 1 g/L increase)
- serum creatinine (OR 1.20 [95% CI 1.10, 1.32], 50 μmol/L increase) levels also increased the risk of ICU hospitalization.
Ref:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8260549/
- Martinot M, Eyriey M, Gravier S, et al. Predictors of mortality, ICU hospitalization, and extrapulmonary complications in COVID-19 patients. Infect Dis Now. 2021;51(6):518-525. https://doi.org/10.1016/j.idnow.2021.07.002
Moderna
Absolute Risk Reduction (95% CI) -0.006 (-0.007 to -0.005) Relative Risk Reduction (95% CI) -0.945 (0.022 to 0.135) Number Needed to Treat -166.7 Odds Ratio 0.055 Relative Risk 0.055 Patient Expected Event Rate: 0.65%
Pfizer
Absolute Risk Reduction (95% CI) -0.008 (-0.009 to -0.007) Relative Risk Reduction (95% CI) -0.950 (0.025 to 0.102) Number Needed to Treat -125 Odds Ratio 0.049 Relative Risk 0.050 Patient Expected Event Rate: 0.88%
J&J
Absolute Risk Reduction (95% CI) -0.012 (-0.014 to -0.010) Relative Risk Reduction (95% CI) -0.666 (0.271 to 0.412) Number Needed to Treat -83.3 Odds Ratio 0.330 Relative Risk 0.334 Patient Expected Event Rate (PEER): 1.78% (COVID Prevalence during study)
Moderna Pfizer J&J PEEV 0.65% 0.88% 1.78% ARR -0.6% -0.8% -1.2% NNV 167 125 83 Baseline(/10k) 65 88 178 With Vaccine 3 4.4 59.5 From Pfizer:
Absolute Risk Reduction (95% CI) -0.008 (-0.009 to -0.007) Relative Risk Reduction (95% CI) -0.951 (0.024 to 0.100) Number Needed to Treat -125.0 Odds Ratio 0.049 Relative Risk 0.049 Patient Expected Event Rate: 0.89%
COVID -COVID Vaccine 8 18190 18198 Placebo 162 18163 18325 Vaccine + Placebo 170 36353 36523 For Pfizer:
- Baseline Risk of Infection during study: 0.89%
- Baseline risk of severe disease during study: 0.016%
- Risk of infection with vaccine: 0.04%
- Risk of severe disease with vaccine: 0.005%
- COVID Vaccines do not prevent disease
Open up the spreadsheet and click on sheet 1b
You will see that vaccination increases risk for omnicron variant of COVID:
- Not vaccinated: 1 (reference)
- 1 dose 14+ days ago: 1.57x
- 2 doses 14+ days ago: 2.26x
- 3 doses 14+ days ago: 4.45x
—
Vaccinations do not prevent disease:
- Nearly 50 Passengers Aboard Royal Caribbean Cruise Ship Test Positive for COVID-19 in Miami
- 95% were fully vaccinated, and that of those who tested positive, 98% were fully vaccinated
- https://people.com/travel/covid-cruise-royal-caribbean-miami-50-passengers-test-positive/
- 55 People Aboard Second Royal Caribbean Cruise Ship Test Positive for COVID-19
- A spokesperson added that the 55 people who tested positive "are fully vaccinated and mildly symptomatic or asymptomatic."
- https://people.com/travel/55-people-aboard-royal-caribbean-cruise-ship-test-positive-for-covid-19/
- J&J
Cases of TTS following administration of the Janssen COVID-19 Vaccine have been reported in males and females, in a wide age range of individuals 18 years and older, with the highest reporting rate (approximately 8 cases per 1,000,000 doses administered) in females ages 30-49 years; overall, approximately 15% of TTS cases have been fatal. Currently available evidence supports a causal relationship between TTS and the Janssen COVID-19 Vaccine. The clinical course of these events shares features with autoimmune heparin-induced thrombocytopenia. In individuals with suspected TTS following administration of the Janssen COVID-19 Vaccine, the use of heparin may be harmful and alternative treatments may be needed. Consultation with hematology specialists is strongly recommended. The American Society of Hematology has published considerations relevant to the diagnosis and treatment of TTS following administration of the Janssen COVID-19 Vaccine (https://www.hematology.org/covid-19/vaccine-induced-immune-thrombotic-thrombocytopenia)
- Vaccine-induced Immune Thrombotic Thrombocytopenia (VITT)
Definitive Diagnosis (must meet all five criteria):
- COVID vaccine 4 to 42 days prior to symptom onset#
- Any venous or arterial thrombosis (often cerebral or abdominal)
- Thrombocytopenia (platelet count < 150 x 109/L)*
- Positive PF4 "HIT" (heparin-induced thrombocytopenia) ELISA
- Markedly elevated D-dimer (> 4 times upper limit of normal)
Urgent medical evaluation for VITT is indicated if any of the following develop 4 to 42 days after vaccination:
- Severe headache
- Visual changes
- Abdominal pain
- Nausea and vomiting
- Back pain
- Shortness of breath
- Leg pain or swelling
- Petechiae, easy bruising, or bleeding
Initial work-up (a normal platelet count is less concerning for VITT*):
- CBC with platelet count and peripheral smear
- Imaging for thrombosis based on signs/symptoms
- PF4-ELISA (HIT assay); draw blood prior to any therapies
- Fibrinogen and D-dimer
Initiate therapy with intravenous immunoglobin and nonheparin anticoagulation pending PF4 ELISA results if: Confirmed thrombosis AND at least one of the following
- Low platelets* OR
- Markedly elevated D-dimer OR
- Both
OR:
- If thrombocytopenia and very high D-Dimer in absence of known thrombosis, particularly in the presence of severe headache, check PF4 ELISA, and consider treatment (see Q2)
- If thrombocytopenia but no thrombosis and negative PF4 ELISA: likely ITP
- Avoid platelet transfusions unless other treatments have been initiated AND life-threatening bleeding or imminent surgery
- Consider referral to tertiary care center if VITT is confirmed.
References:
- Vaccine-induced Immune Thrombotic Thrombocytopenia (VITT)
EUA
To be considered for an EAU, a Phase 3 vaccine trial should include "well over 3,000" participants, and at least half of them should be tracked for at least two months after receiving their final dose
An EUA can last only as long as a public health emergency is in effect. But scientists anticipate that the coronavirus will continue to circulate in humans even after the COVID-19 pandemic ends. In that case, vaccine makers that want to keep their products on the market will need to have regular FDA approval — and to get it, they'll need to keep their Phase 3 clinical trials going.
Masks
https://themodelhealthshow.com/maskfacts/
Definition of a significant exposure to Covid-19 as face-to-face contact within 6 feet with a patient with symptomatic Covid-19 that is sustained for at least a few minutes (and some say more than 10 minutes or even 30 minutes)
Covid-19 virus is 120 nanometers in size while the filtration potential of a N95 mask is 150-300 nanometers.
Penetration of cloth masks by particles was almost 97% and medical masks 44%.
- MacIntyre CR, Seale H, Dung TC, et al A cluster randomised trial of cloth masks compared with medical masks in healthcare workers BMJ Open 2015;5:e006577. doi: 10.1136/bmjopen-2014-006577
Face mask use in health care workers has not been demonstrated to provide benefit in terms of cold symptoms or getting colds
- Jacobs JL, Ohde S, Takahashi O, Tokuda Y, Omata F, Fukui T. Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: a randomized controlled trial. Am J Infect Control. 2009 Jun;37(5):417-419. doi: 10.1016/j.ajic.2008.11.002. Epub 2009 Feb 12. PMID: 19216002.
Our analysis confirms the effectiveness of medical masks and respirators against SARS. Disposable, cotton, or paper masks are not recommended. We found no clear benefit of either medical masks or N95 respirators against pH1N1.
- Vittoria Offeddu, Chee Fu Yung, Mabel Sheau Fong Low, Clarence C Tam, Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis, Clinical Infectious Diseases, Volume 65, Issue 11, 1 December 2017, Pages 1934–1942, https://doi.org/10.1093/cid/cix681
Norway's Institute for Public Health reported that if masks did work then any difference in infection rates would be small when infection rates are low: assuming 20% asymptomatics and a risk reduction of 40% for wearing masks, 200 000 people would need to wear one to prevent one new infection per week
- Iversen BG, Vestrheim DF, Flottorp S, Denison E, Oxman AD. COVID-19:
Should individuals in the community without respiratory symptoms wear facemasks to reduce the spread of COVID-19? [Covid-19: Bør personer i samfunnet bruke ansiktsmasker for å redusere spredningen av covid-19? Hurtigoversikt 2020] Oslo: Norwegian Institute of Public Health, 2020
Median (range) aerosol particle number emission rates were (Figure 2): 135 (85-691) particles/s for breathing, 270 (120–1380) particles/s for normal talking, 570 (180–1760) particles/s for loud talking, 690 (320–2870) particles/s for normal singing, 980 (390–2870) particles/s for loud singing, and 1480 (500-2820) particles/s for loud singing with exaggerated diction. For loud singing with a face mask, the emission rate was 410 (200–1150) particles/s. Median number of emitted particles in the size range 0.54–10 µm per second for the 12 singers. Nevertheless, many of the largest droplets travel a limited distance (<0.5 m) before their movement become vertical due to sedimentation.
- M. Alsved, A. Matamis, R. Bohlin, M. Richter, P.-E. Bengtsson, C.-J. Fraenkel, P. Medstrand & J. Löndahl (2020) Exhaled respiratory particles during singing and talking, Aerosol Science and Technology, 54:11, 1245-1248, DOI: 10.1080/02786826.2020.1812502
In this community-based, randomized controlled trial conducted in a setting where mask wearing was uncommon and was not among other recommended public health measures related to COVID-19, a recommendation to wear a surgical mask when outside the home among others did not reduce, at conventional levels of statistical significance, incident SARS-CoV-2 infection compared with no mask recommendation.
- Henning Bundgaard, Johan Skov Bundgaard, Daniel Emil Tadeusz Raaschou-Pedersen, et al. Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers: A Randomized Controlled Trial. Ann Intern Med.2021;174:335-343. [Epub ahead of print 18 November 2020]. https://doi.org/10.7326/M20-6817
Random Stats Stuff
- COVID Shorten life - 5 days not 1 year
Analysts estimate that, on average, a death from Covid-19 robs its victim of around 12 years of life. Approximately 400,000 Americans died Covid-19 in 2020, meaning about 4.8 million years of life collectively vanished. Spread that ghastly number across the U.S. population of 330 million and it comes out to 0.014 years of life lost per person. That's 5.3 days. There were other excess deaths in 2020, so maybe the answer is seven days lost per person.
Outpatient COVID-19 Management
Budesonide:
- Inhaled budesonide 800 mg bid significantly reduces the likelihood that patients with early COVID-19 will require emergency department evaluation or hospitalization (NNT = 7-8) (LOB 1b-)
- budesonide 400 mcg actuations - 2 actuations twice daily
Aspirin:
- Observational cohort study of 412 adult patients with COVID-19, aspirin use was associated with a significantly lower rate of
- Reaching mechanical ventilation by 44%
- ICU admissions by 43%
- Overall in-hospital mortality by 47%
Fluvoxamine ($10):
- Treatment with fluvoxamine (100 mg twice daily for 10 days) among high-risk outpatients with early diagnosed COVID-19 reduced the need for hospitalisation defined as retention in a COVID-19 emergency setting or transfer to a tertiary hospital.
- This placebo-controlled, randomised, adaptive platform trial done among high-risk symptomatic Brazilian adults confirmed positive for SARS-CoV-2 included eligible patients from 11 clinical sites in Brazil with a known risk factor for progression to severe disease. Patients were randomly assigned (1:1) to either fluvoxamine (100 mg twice daily for 10 days) or placebo.
Molnupiravir:
- $700
- At the Interim Analysis, 7.3 Percent of Patients Who Received Molnupiravir Were Hospitalized Through Day 29, Compared With 14.1 Percent of Placebo-Treated Patients Who were Hospitalized or Died
- The MOVe-OUT trial (MK-4482-002) (NCT04575597) was a global Phase 3, randomized, placebo-controlled, double-blind, multi-site study of non-hospitalized adult patients with laboratory-confirmed mild to moderate COVID-19, at least one risk factor associated with poor disease outcomes, and symptom onset within five days prior to randomization.
- Orally administered form of a potent ribonucleoside analog that inhibits the replication of SARS-CoV-2
References:
- AFP Vol 104 No 2 Aug 2021
- Chow, J.H., et al. (2021) Aspirin Use Is Associated With Decreased Mechanical Ventilation, Intensive Care Unit Admission, and In-Hospital Mortality in Hospitalized Patients With Coronavirus Disease 2019. Anesthesia & Analgesia. doi.org/10.1213/ANE.0000000000005292.
- G Reis E A dos S Moreira-Silva et al. Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial. Lancet Glob Health 2021 Published Online October 27, 2021 https://doi.org/10.1016/S2214-109X(21)00448-4
- Lenze EJ Mattar C Zorumski CF et al. Fluvoxamine vs placebo and clinical deterioration in outpatients with symptomatic COVID-19: a randomized clinical trial. JAMA. 2020; 324: 2292-2300
- https://www.merck.com/news/merck-and-ridgebacks-investigational-oral-antiviral-molnupiravir-reduced-the-risk-of-hospitalization-or-death-by-approximately-50-percent-compared-to-placebo-for-patients-with-mild-or-moderat/
Testing Guidance for COVID-19 - Jan 2022 edit
If you get symptoms, you should avoid contact with others. A positive COVID-19 test result will not change this recommendation.
There are certain groups who are at an increased risk for severe illness from COVID-19. Severe illness means that an individual diagnosed with COVID-19 may need hospitalization, intensive care, or that they may even die.
Groups at increased risk for severe illness from COVID-19 include:
- Older adults, especially those age 65 and older.
- Individuals with certain medical conditions, including cancer, diabetes, chronic lung diseases, heart conditions, and a weakened immune system (immunocompromised).
- Pregnant or recently pregnant individuals.
- Individuals with Symptoms and Risk Factors
Individuals with symptoms of COVID-19 and who are at an increased risk for severe illness from COVID-19:
- Should get tested for COVID-19 soon after symptom onset.
- Should seek early monoclonal antibody or antiviral drug treatment and seek other medical treatment as necessary.
- Individuals with Symptoms and No Risk Factors
Individuals with symptoms and who are not at an increased risk for severe illness from COVID- 19:
- Consider getting tested for COVID-19 soon after symptom onset.
- Seek medical treatment only as necessary.
- Individuals with No Symptoms
Individuals who may have been exposed to COVID-19, but have no symptoms:
- COVID-19 testing is unlikely to have any clinical benefits.
Mortality Stuff
| Country | Expected Age-standardised Mortality 2020 (per 100,000) | Age-standardised total mortality per 100,000 | Absolute excess age-standardised mortality per 100,000 | Percentage increase in Mortality per Age-Adjusted 100,000 |
|---|---|---|---|---|
| Austria | 938 | 1009 | 71 | 7.60% |
| Belgium | 956 | 1072 | 116 | 12.20% |
| Bulgaria | 1597 | 1788 | 191 | 12.00% |
| Canada | 709 | 751 | 42 | 6.00% |
| Chile* | 1041 | 1184 | 143 | 13.80% |
| Czechia | 1147 | 1258 | 111 | 9.70% |
| Denmark | 1016 | 972 | -44 | -4.30% |
| England & Wales | 960 | 1060 | 100 | 10.50% |
| Estonia | 1178 | 1178 | 0 | 0.00% |
| Finland | 948 | 919 | -29 | -3.10% |
| France | 839 | 895 | 56 | 6.70% |
| Germany* | 1016 | 1049 | 33 | 3.30% |
| Greece* | 912 | 957 | 45 | 4.90% |
| Hungary | 1420 | 1473 | 53 | 3.70% |
| Iceland | 755 | 724 | -31 | -4.10% |
| Israel | 864 | 920 | 56 | 6.50% |
| Italy | 728 | 792 | 63 | 8.7 |
| Latvia | 1446 | 1414 | -32 | -2.20% |
| Lithuania | 1393 | 1468 | 75 | 5.40% |
| Luxembourg | 842 | 852 | 9.5 | 1.10% |
| Netherlands | 971 | 1040 | 70 | 7.20% |
| Norway | 893 | 861 | -32 | -3.60% |
| Poland | 1216 | 1391 | 175 | 14.40% |
| Portugal | 977 | 1043 | 66 | 6.80% |
| Scotland | 1134 | 1219 | 85 | 7.50% |
| Slovakia | 1219 | 1236 | 17 | 1.40% |
| Slovenia | 996 | 1116 | 120 | 12.00% |
| South Korea | 779 | 757 | -22 | -2.90% |
| Spain | 838 | 946 | 108 | 12.90% |
| Sweden | 883 | 896 | 13 | 1.50% |
| Switzerland | 783 | 817 | 34 | 4.30% |
| USA | 1020 | 1152 | 132 | 12.90% |
The USA which has often been cited as the worse affected country (often using the total number of COVID-19 deaths) has relative excess of 12.9% which although one of the highest, is below some with even higher relative excess mortality such as Poland and Chile.
Relative standardised excess mortality is one method of measuring the impact of the SARS-nCOV2 pandemic. It is superior to comparing the total numbers of COVID-19 deaths and arguably more useful than comparing the COVID-19 death rate per 100k as it overcomes the recording bias and measures both direct and indirect consequences of the pandemic. But it has limitations. We have noted that defining the expected number of deaths and thus the excess can vary according to whether a four or five year average is used. In addition, using simple averages of historical mortality data could underestimate if there is a significant downward trend in mortality or overestimated if there are upward trends.
Ref:
Vaccine Stuff
- Sensible Public Health Vaccine Policy
- There is just no question that vaccinating low-risk cohorts (including the recovered) is not only pointless, but also dangerous. These aren't the people who end up in the hospital dying of Corona anyway. And because the vaccinated sooner or later end up driving transmission, there is only downside and no upside here.
- All the vaccines are good for, is reducing the likelihood of severe disease among the old and the vulnerable. It follows that only the old and the vulnerable should be vaccinated.
- In these groups, carefully timed annual vaccinations, like flu shots, might well provide good protection at the height of the winter coronavirus season and limit mortality. Even here, though, you'd have to proceed carefully, to avoid causing case spikes in the newly vaccinated during that brief period where their vulnerability to infection is heightened.
Ref:
- Adverse Effects
- Compared with other vaccines
Table 132: VAERS Summary for COVID-19 Vaccines through 10/1/2021 High-Level Summary COVID19 vaccines (Dec'2020 – present) All other vaccines 1990-present US Data Only COVID19 vaccines (Dec'2020 – present) US Data Only All other vaccines 1990-present Number of Adverse Reactions 778685 824864 593728 723780 Number of Life-Threatening Events 17618 13634 9011 9725 Number of Hospitalizations 75605 78604 34880 38211 Number of Deaths 16,310* 9155 7437 5129 # of Permanent Disabilities after vaccination 23712 19638 8628 12467 Number of Office Visits 121304 43674 111693 42348 # of Emergency Room/Department Visits 87758 209950 74464 200967 # of Birth Defects after vaccination 528 141 330 90 Ref:
- Myocarditis risk in Young Males (Japan)
- As of November 14, out of every one million males who had the Moderna vaccine, such side effects were reported in 81.79 males aged 10 to 19 and 48.76 males in their 20s.
- The figures were 15.66 and 13.32 respectively for those who had the Pfizer vaccine.
Ref:
- Vaccine Negatives?
The vaccines appear to induce negative efficacy against infection.
This probably arises from a combination of
- minimally symptomatic super-spreading among the vaccinated
- the selective pressure that vaccine-elicited antibodies place upon the virus
- the narrow immunity against an obsolete arrangement of the spike protein that the vaccines confer.
- For a period of several weeks after dose 1 (and likely dose 3)
- They also make the vaccinated more susceptible to infection
- and mass vaccination campaigns have induced case spikes across many countries
Ref:
- Compared with other vaccines
- Natural Immunity vs Vaccine
- 138 Research Studies Affirm Naturally Acquired Immunity to Covid-19: Documented, Linked, and Quoted
Study/report title, author, and year published and interactive url link Predominant finding on natural immunity 1) Necessity of COVID-19 vaccination in previously infected individuals, Shrestha, 2021 "Cumulative incidence of COVID-19 was examined among 52,238 employees in an American healthcare system. The cumulative incidence of SARS-CoV-2 infection remained almost zero among previously infected unvaccinated subjects, previously infected subjects who were vaccinated, and previously uninfected subjects who were vaccinated, compared with a steady increase in cumulative incidence among previously uninfected subjects who remained unvaccinated. Not one of the 1359 previously infected subjects who remained unvaccinated had a SARS-CoV-2 infection over the duration of the study. Individuals who have had SARS-CoV-2 infection are unlikely to benefit from COVID-19 vaccination…" 2) SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls, Le Bert, 2020 "Studied T cell responses against the structural (nucleocapsid (N) protein) and non-structural (NSP7 and NSP13 of ORF1) regions of SARS-CoV-2 in individuals convalescing from coronavirus disease 2019 (COVID-19) (n = 36). In all of these individuals, we found CD4 and CD8 T cells that recognized multiple regions of the N protein…showed that patients (n = 23) who recovered from SARS possess long-lasting memory T cells that are reactive to the N protein of SARS-CoV 17 years after the outbreak of SARS in 2003; these T cells displayed robust cross-reactivity to the N protein of SARS-CoV-2." 3) Comparing SARS-CoV-2 natural immunity to vaccine-induced immunity: reinfections versus breakthrough infections,Gazit, 2021 "A retrospective observational study comparing three groups: (1) SARS-CoV-2-naïve individuals who received a two-dose regimen of the BioNTech/Pfizer mRNA BNT162b2 vaccine, (2) previously infected individuals who have not been vaccinated, and (3) previously infected and single dose vaccinated individuals found para a 13 fold increased risk of breakthrough Delta infections in double vaccinated persons, and a 27 fold increased risk for symptomatic breakthrough infection in the double vaccinated relative to the natural immunity recovered persons…the risk of hospitalization was 8 times higher in the double vaccinated (para)…this analysis demonstrated that natural immunity affords longer lasting and stronger protection against infection, symptomatic disease and hospitalization due to the Delta variant of SARS-CoV-2, compared to the BNT162b2 two-dose vaccine-induced immunity." 4) Highly functional virus-specific cellular immune response in asymptomatic SARS-CoV-2 infection, Le Bert, 2021 "Studied SARS-CoV-2–specific T cells in a cohort of asymptomatic (n = 85) and symptomatic (n = 75) COVID-19 patients after seroconversion…thus, asymptomatic SARS-CoV-2–infected individuals are not characterized by weak antiviral immunity; on the contrary, they mount a highly functional virus-specific cellular immune response." 5) Large-scale study of antibody titer decay following BNT162b2 mRNA vaccine or SARS-CoV-2 infection, Israel, 2021 "A total of 2,653 individuals fully vaccinated by two doses of vaccine during the study period and 4,361 convalescent patients were included. Higher SARS-CoV-2 IgG antibody titers were observed in vaccinated individuals (median 1581 AU/mL IQR [533.8-5644.6]) after the second vaccination, than in convalescent individuals (median 355.3 AU/mL IQR [141.2-998.7]; p<0.001). In vaccinated subjects, antibody titers decreased by up to 40% each subsequent month while in convalescents they decreased by less than 5% per month…this study demonstrates individuals who received the Pfizer-BioNTech mRNA vaccine have different kinetics of antibody levels compared to patients who had been infected with the SARS-CoV-2 virus, with higher initial levels but a much faster exponential decrease in the first group". 6) SARS-CoV-2 re-infection risk in Austria, Pilz, 2021 Researchers recorded "40 tentative re-infections in 14, 840 COVID-19 survivors of the first wave (0.27%) and 253 581 infections in 8, 885, 640 individuals of the remaining general population (2.85%) translating into an odds ratio (95% confidence interval) of 0.09 (0.07 to 0.13)…relatively low re-infection rate of SARS-CoV-2 in Austria. Protection against SARS-CoV-2 after natural infection is comparable with the highest available estimates on vaccine efficacies." Additionally, hospitalization in only five out of 14,840 (0.03%) people and death in one out of 14,840 (0.01%) (tentative re-infection). 7) mRNA vaccine-induced SARS-CoV-2-specific T cells recognize B.1.1.7 and B.1.351 variants but differ in longevity and homing properties depending on prior infection status, Neidleman, 2021 "Spike-specific T cells from convalescent vaccinees differed strikingly from those of infection-naïve vaccinees, with phenotypic features suggesting superior long-term persistence and ability to home to the respiratory tract including the nasopharynx. These results provide reassurance that vaccine-elicited T cells respond robustly to the B.1.1.7 and B.1.351 variants, confirm that convalescents may not need a second vaccine dose." 8) Good news: Mild COVID-19 induces lasting antibody protection, Bhandari, 2021 "Months after recovering from mild cases of COVID-19, people still have immune cells in their body pumping out antibodies against the virus that causes COVID-19, according to a study from researchers at Washington University School of Medicine in St. Louis. Such cells could persist for a lifetime, churning out antibodies all the while. The findings, published May 24 in the journal Nature, suggest that mild cases of COVID-19 leave those infected with lasting antibody protection and that repeated bouts of illness are likely to be uncommon." 9) Robust neutralizing antibodies to SARS-CoV-2 infection persist for months, Wajnberg, 2021 "Neutralizing antibody titers against the SARS-CoV-2 spike protein persisted for at least 5 months after infection. Although continued monitoring of this cohort will be needed to confirm the longevity and potency of this response, these preliminary results suggest that the chance of reinfection may be lower than is currently feared." 10) Evolution of Antibody Immunity to SARS-CoV-2, Gaebler, 2020 "Concurrently, neutralizing activity in plasma decreases by five-fold in pseudo-type virus assays. In contrast, the number of RBD-specific memory B cells is unchanged. Memory B cells display clonal turnover after 6.2 months, and the antibodies they express have greater somatic hypermutation, increased potency and resistance to RBD mutations, indicative of continued evolution of the humoral response…we conclude that the memory B cell response to SARS-CoV-2 evolves between 1.3 and 6.2 months after infection in a manner that is consistent with antigen persistence." 11) Persistence of neutralizing antibodies a year after SARS-CoV-2 infection in humans, Haveri, 2021 "Assessed the persistence of serum antibodies following WT SARS-CoV-2 infection at 8 and 13 months after diagnosis in 367 individuals…found that NAb against the WT virus persisted in 89% and S-IgG in 97% of subjects for at least 13 months after infection." 12) Quantifying the risk of SARS‐CoV‐2 reinfection over time, Murchu, 2021 "Eleven large cohort studies were identified that estimated the risk of SARS‐CoV‐2 reinfection over time, including three that enrolled healthcare workers and two that enrolled residents and staff of elderly care homes. Across studies, the total number of PCR‐positive or antibody‐positive participants at baseline was 615,777, and the maximum duration of follow‐up was more than 10 months in three studies. Reinfection was an uncommon event (absolute rate 0%–1.1%), with no study reporting an increase in the risk of reinfection over time." 13) Natural immunity to covid is powerful. Policymakers seem afraid to say so, Makary, 2021 Makary writes "it's okay to have an incorrect scientific hypothesis. But when new data proves it wrong, you have to adapt. Unfortunately, many elected leaders and public health officials have held on far too long to the hypothesis that natural immunity offers unreliable protection against covid-19 — a contention that is being rapidly debunked by science. More than 15 studies have demonstrated the power of immunity acquired by previously having the virus. A 700,000-person study from Israel two weeks ago found that those who had experienced prior infections were 27 times less likely to get a second symptomatic covid infection than those who were vaccinated. This affirmed a June Cleveland Clinic study of health-care workers (who are often exposed to the virus), in which none who had previously tested positive for the coronavirus got reinfected. The study authors concluded that "individuals who have had SARS-CoV-2 infection are unlikely to benefit from covid-19 vaccination." And in May, a Washington University study found that even a mild covid infection resulted in long-lasting immunity." The Western Journal-Makary "The data on natural immunity are now overwhelming," Makary told the Morning Wire. "It turns out the hypothesis that our public health leaders had that vaccinated immunity is better and stronger than natural immunity was wrong. They got it backwards. And now we've got data from Israel showing that natural immunity is 27 times more effective than vaccinated immunity." 14) SARS-CoV-2 elicits robust adaptive immune responses regardless of disease severity, Nielsen, 2021 "203 recovered SARS-CoV-2 infected patients in Denmark between April 3rd and July 9th 2020, at least 14 days after COVID-19 symptom recovery… report broad serological profiles within the cohort, detecting antibody binding to other human coronaviruses… the viral surface spike protein was identified as the dominant target for both neutralizing antibodies and CD8+ T-cell responses. Overall, the majority of patients had robust adaptive immune responses, regardless of their disease severity." 15) Protection of previous SARS-CoV-2 infection is similar to that of BNT162b2 vaccine protection: A three-month nationwide experience from Israel, Goldberg, 2021 "Analyze an updated individual-level database of the entire population of Israel to assess the protection efficacy of both prior infection and vaccination in preventing subsequent SARS-CoV-2 infection, hospitalization with COVID-19, severe disease, and death due to COVID-19… vaccination was highly effective with overall estimated efficacy for documented infection of 92·8% (CI:[92·6, 93·0]); hospitalization 94·2% (CI:[93·6, 94·7]); severe illness 94·4% (CI:[93·6, 95·0]); and death 93·7% (CI:[92·5, 94·7]). Similarly, the overall estimated level of protection from prior SARS-CoV-2 infection for documented infection is 94·8% (CI: [94·4, 95·1]); hospitalization 94·1% (CI: [91·9, 95·7]); and severe illness 96·4% (CI: [92·5, 98·3])…results question the need to vaccinate previously-infected individuals." 16) Incidence of Severe Acute Respiratory Syndrome Coronavirus-2 infection among previously infected or vaccinated employees, Kojima, 2021 "Employees were divided into three groups: (1) SARS-CoV-2 naïve and unvaccinated, (2) previous SARS-CoV-2 infection, and (3) vaccinated. Person-days were measured from the date of the employee first test and truncated at the end of the observation period. SARS-CoV-2 infection was defined as two positive SARS-CoV-2 PCR tests in a 30-day period… 4313, 254 and 739 employee records for groups 1, 2, and 3…previous SARS-CoV-2 infection and vaccination for SARS-CoV-2 were associated with decreased risk for infection or re-infection with SARS-CoV-2 in a routinely screened workforce. The was no difference in the infection incidence between vaccinated individuals and individuals with previous infection." 17) Having SARS-CoV-2 once confers much greater immunity than a vaccine—but vaccination remains vital, Wadman, 2021 "Israelis who had an infection were more protected against the Delta coronavirus variant than those who had an already highly effective COVID-19 vaccine…the newly released data show people who once had a SARS-CoV-2 infection were much less likely than never-infected, vaccinated people to get Delta, develop symptoms from it, or become hospitalized with serious COVID-19." 18) One-year sustained cellular and humoral immunities of COVID-19 convalescents, Zhang, 2021 "A systematic antigen-specific immune evaluation in 101 COVID-19 convalescents; SARS-CoV-2-specific IgG antibodies, and also NAb can persist among over 95% COVID-19 convalescents from 6 months to 12 months after disease onset. At least 19/71 (26%) of COVID-19 convalescents (double positive in ELISA and MCLIA) had detectable circulating IgM antibody against SARS-CoV-2 at 12m post-disease onset. Notably, the percentages of convalescents with positive SARS-CoV-2-specific T-cell responses (at least one of the SARS-CoV-2 antigen S1, S2, M and N protein) were 71/76 (93%) and 67/73 (92%) at 6m and 12m, respectively." 19) Functional SARS-CoV-2-Specific Immune Memory Persists after Mild COVID-19, Rodda, 2021 "Recovered individuals developed SARS-CoV-2-specific immunoglobulin (IgG) antibodies, neutralizing plasma, and memory B and memory T cells that persisted for at least 3 months. Our data further reveal that SARS-CoV-2-specific IgG memory B cells increased over time. Additionally, SARS-CoV-2-specific memory lymphocytes exhibited characteristics associated with potent antiviral function: memory T cells secreted cytokines and expanded upon antigen re-encounter, whereas memory B cells expressed receptors capable of neutralizing virus when expressed as monoclonal antibodies. Therefore, mild COVID-19 elicits memory lymphocytes that persist and display functional hallmarks of antiviral immunity." 20) Discrete Immune Response Signature to SARS-CoV-2 mRNA Vaccination Versus Infection, Ivanova, 2021 "Performed multimodal single-cell sequencing on peripheral blood of patients with acute COVID-19 and healthy volunteers before and after receiving the SARS-CoV-2 BNT162b2 mRNA vaccine to compare the immune responses elicited by the virus and by this vaccine…both infection and vaccination induced robust innate and adaptive immune responses, our analysis revealed significant qualitative differences between the two types of immune challenges. In COVID-19 patients, immune responses were characterized by a highly augmented interferon response which was largely absent in vaccine recipients. Increased interferon signaling likely contributed to the observed dramatic upregulation of cytotoxic genes in the peripheral T cells and innate-like lymphocytes in patients but not in immunized subjects. Analysis of B and T cell receptor repertoires revealed that while the majority of clonal B and T cells in COVID-19 patients were effector cells, in vaccine recipients clonally expanded cells were primarily circulating memory cells…we observed the presence of cytotoxic CD4 T cells in COVID-19 patients that were largely absent in healthy volunteers following immunization. While hyper-activation of inflammatory responses and cytotoxic cells may contribute to immunopathology in severe illness, in mild and moderate disease, these features are indicative of protective immune responses and resolution of infection." 21) SARS-CoV-2 infection induces long-lived bone marrow plasma cells in humans, Turner, 2021 "Bone marrow plasma cells (BMPCs) are a persistent and essential source of protective antibodies… durable serum antibody titres are maintained by long-lived plasma cells—non-replicating, antigen-specific plasma cells that are detected in the bone marrow long after the clearance of the antigen … S-binding BMPCs are quiescent, which suggests that they are part of a stable compartment. Consistently, circulating resting memory B cells directed against SARS-CoV-2 S were detected in the convalescent individuals. Overall, our results indicate that mild infection with SARS-CoV-2 induces robust antigen-specific, long-lived humoral immune memory in humans…overall, our data provide strong evidence that SARS-CoV-2 infection in humans robustly establishes the two arms of humoral immune memory: long-lived bone marrow plasma cells (BMPCs) and memory B-cells." 22) SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative health-care workers in England: a large, multicentre, prospective cohort study (SIREN), Jane Hall, 2021 "The SARS-CoV-2 Immunity and Reinfection Evaluation study… 30 625 participants were enrolled into the study… a previous history of SARS-CoV-2 infection was associated with an 84% lower risk of infection, with median protective effect observed 7 months following primary infection. This time period is the minimum probable effect because seroconversions were not included. This study shows that previous infection with SARS-CoV-2 induces effective immunity to future infections in most individuals." 23) Pandemic peak SARS-CoV-2 infection and seroconversion rates in London frontline health-care workers, Houlihan, 2020 "Enrolled 200 patient-facing HCWs between March 26 and April 8, 2020…represents a 13% infection rate (i.e. 14 of 112 HCWs) within the 1 month of follow-up in those with no evidence of antibodies or viral shedding at enrolment. By contrast, of 33 HCWs who tested positive by serology but tested negative by RT-PCR at enrolment, 32 remained negative by RT-PCR through follow-up, and one tested positive by RT-PCR on days 8 and 13 after enrolment." 24) Antibodies to SARS-CoV-2 are associated with protection against reinfection, Lumley, 2021 "Critical to understand whether infection with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) protects from subsequent reinfection… 12219 HCWs participated…prior SARS-CoV-2 infection that generated antibody responses offered protection from reinfection for most people in the six months following infection." 25) Longitudinal analysis shows durable and broad immune memory after SARS-CoV-2 infection with persisting antibody responses and memory B and T cells, Cohen, 2021 "Evaluate 254 COVID-19 patients longitudinally up to 8 months and find durable broad-based immune responses. SARS-CoV-2 spike binding and neutralizing antibodies exhibit a bi-phasic decay with an extended half-life of >200 days suggesting the generation of longer-lived plasma cells… most recovered COVID-19 patients mount broad, durable immunity after infection, spike IgG+ memory B cells increase and persist post-infection, durable polyfunctional CD4 and CD8 T cells recognize distinct viral epitope regions." 26) Single cell profiling of T and B cell repertoires following SARS-CoV-2 mRNA vaccine, Sureshchandra, 2021 "Used single-cell RNA sequencing and functional assays to compare humoral and cellular responses to two doses of mRNA vaccine with responses observed in convalescent individuals with asymptomatic disease… natural infection induced expansion of larger CD8 T cell clones occupied distinct clusters, likely due to the recognition of a broader set of viral epitopes presented by the virus not seen in the mRNA vaccine." 27) SARS-CoV-2 antibody-positivity protects against reinfection for at least seven months with 95% efficacy, Abu-Raddad, 2021 "SARS-CoV-2 antibody-positive persons from April 16 to December 31, 2020 with a PCR-positive swab ≥14 days after the first-positive antibody test were investigated for evidence of reinfection, 43,044 antibody-positive persons who were followed for a median of 16.3 weeks…reinfection is rare in the young and international population of Qatar. Natural infection appears to elicit strong protection against reinfection with an efficacy ~95% for at least seven months." 28) Orthogonal SARS-CoV-2 Serological Assays Enable Surveillance of Low-Prevalence Communities and Reveal Durable Humoral Immunity, Ripperger, 2020 "Conducted a serological study to define correlates of immunity against SARS-CoV-2. Compared to those with mild coronavirus disease 2019 (COVID-19) cases, individuals with severe disease exhibited elevated virus-neutralizing titers and antibodies against the nucleocapsid (N) and the receptor binding domain (RBD) of the spike protein…neutralizing and spike-specific antibody production persists for at least 5–7 months… nucleocapsid antibodies frequently become undetectable by 5–7 months." 29) Anti-spike antibody response to natural SARS-CoV-2 infection in the general population, Wei, 2021 "In the general population using representative data from 7,256 United Kingdom COVID-19 infection survey participants who had positive swab SARS-CoV-2 PCR tests from 26-April-2020 to 14-June-2021…we estimated antibody levels associated with protection against reinfection likely last 1.5-2 years on average, with levels associated with protection from severe infection present for several years. These estimates could inform planning for vaccination booster strategies." 30) Researchers find long-lived immunity to 1918 pandemic virus, CIDRAP, 2008 "A study of the blood of older people who survived the 1918 influenza pandemic reveals that antibodies to the strain have lasted a lifetime and can perhaps be engineered to protect future generations against similar strains…the group collected blood samples from 32 pandemic survivors aged 91 to 101..the people recruited for the study were 2 to 12 years old in 1918 and many recalled sick family members in their households, which suggests they were directly exposed to the virus, the authors report. The group found that 100% of the subjects had serum-neutralizing activity against the 1918 virus and 94% showed serologic reactivity to the 1918 hemagglutinin. The investigators generated B lymphoblastic cell lines from the peripheral blood mononuclear cells of eight subjects. Transformed cells from the blood of 7 of the 8 donors yielded secreting antibodies that bound the 1918 hemagglutinin." and the actual 2008 NATURE journal publication by Yu Yu: "here we show that of the 32 individuals tested that were born in or before 1915, each showed sero-reactivity with the 1918 virus, nearly 90 years after the pandemic. Seven of the eight donor samples tested had circulating B cells that secreted antibodies that bound the 1918 HA. We isolated B cells from subjects and generated five monoclonal antibodies that showed potent neutralizing activity against 1918 virus from three separate donors. These antibodies also cross-reacted with the genetically similar HA of a 1930 swine H1N1 influenza strain." 31) Live virus neutralisation testing in convalescent patients and subjects vaccinated against 19A, 20B, 20I/501Y.V1 and 20H/501Y.V2 isolates of SARS-CoV-2, Gonzalez, 2021 "No significant difference was observed between the 20B and 19A isolates for HCWs with mild COVID-19 and critical patients. However, a significant decrease in neutralisation ability was found for 20I/501Y.V1 in comparison with 19A isolate for critical patients and HCWs 6-months post infection. Concerning 20H/501Y.V2, all populations had a significant reduction in neutralising antibody titres in comparison with the 19A isolate. Interestingly, a significant difference in neutralisation capacity was observed for vaccinated HCWs between the two variants whereas it was not significant for the convalescent groups…the reduced neutralising response observed towards the 20H/501Y.V2 in comparison with the 19A and 20I/501Y.V1 isolates in fully immunized subjects with the BNT162b2 vaccine is a striking finding of the study." 32) Differential effects of the second SARS-CoV-2 mRNA vaccine dose on T cell immunity in naïve and COVID-19 recovered individuals, Camara, 2021 "Characterized SARS-CoV-2 spike-specific humoral and cellular immunity in naïve and previously infected individuals during full BNT162b2 vaccination…results demonstrate that the second dose increases both the humoral and cellular immunity in naïve individuals. On the contrary, the second BNT162b2 vaccine dose results in a reduction of cellular immunity in COVID-19 recovered individuals." 33) Op-Ed: Quit Ignoring Natural COVID Immunity, Klausner, 2021 "Epidemiologists estimate over 160 million people worldwide have recovered from COVID-19. Those who have recovered have an astonishingly low frequency of repeat infection, disease, or death." 34) Association of SARS-CoV-2 Seropositive Antibody Test With Risk of Future Infection, Harvey, 2021 "To evaluate evidence of SARS-CoV-2 infection based on diagnostic nucleic acid amplification test (NAAT) among patients with positive vs negative test results for antibodies in an observational descriptive cohort study of clinical laboratory and linked claims data…the cohort included 3 257 478 unique patients with an index antibody test…patients with positive antibody test results were initially more likely to have positive NAAT results, consistent with prolonged RNA shedding, but became markedly less likely to have positive NAAT results over time, suggesting that seropositivity is associated with protection from infection." 35) SARS-CoV-2 seropositivity and subsequent infection risk in healthy young adults: a prospective cohort study, Letizia, 2021 "Investigated the risk of subsequent SARS-CoV-2 infection among young adults (CHARM marine study) seropositive for a previous infection…enrolled 3249 participants, of whom 3168 (98%) continued into the 2-week quarantine period. 3076 (95%) participants…Among 189 seropositive participants, 19 (10%) had at least one positive PCR test for SARS-CoV-2 during the 6-week follow-up (1·1 cases per person-year). In contrast, 1079 (48%) of 2247 seronegative participants tested positive (6·2 cases per person-year). The incidence rate ratio was 0·18 (95% CI 0·11–0·28; p<0·001)…infected seropositive participants had viral loads that were about 10-times lower than those of infected seronegative participants (ORF1ab gene cycle threshold difference 3·95 [95% CI 1·23–6·67]; p=0·004)." 36) Associations of Vaccination and of Prior Infection With Positive PCR Test Results for SARS-CoV-2 in Airline Passengers Arriving in Qatar, Bertollini, 2021 "Of 9,180 individuals with no record of vaccination but with a record of prior infection at least 90 days before the PCR test (group 3), 7694 could be matched to individuals with no record of vaccination or prior infection (group 2), among whom PCR positivity was 1.01% (95% CI, 0.80%-1.26%) and 3.81% (95% CI, 3.39%-4.26%), respectively. The relative risk for PCR positivity was 0.22 (95% CI, 0.17-0.28) for vaccinated individuals and 0.26 (95% CI, 0.21-0.34) for individuals with prior infection compared with no record of vaccination or prior infection." 37) Natural immunity against COVID-19 significantly reduces the risk of reinfection: findings from a cohort of sero-survey participants, Mishra, 2021 "Followed up with a subsample of our previous sero-survey participants to assess whether natural immunity against SARS-CoV-2 was associated with a reduced risk of re-infection (India)… out of the 2238 participants, 1170 were sero-positive and 1068 were sero-negative for antibody against COVID-19. Our survey found that only 3 individuals in the sero-positive group got infected with COVID-19 whereas 127 individuals reported contracting the infection the sero-negative group…from the 3 sero-positives re-infected with COVID-19, one had hospitalization, but did not require oxygen support or critical care…development of antibody following natural infection not only protects against re-infection by the virus to a great extent, but also safeguards against progression to severe COVID-19 disease." 38) Lasting immunity found after recovery from COVID-19, NIH, 2021 "The researchers found durable immune responses in the majority of people studied. Antibodies against the spike protein of SARS-CoV-2, which the virus uses to get inside cells, were found in 98% of participants one month after symptom onset. As seen in previous studies, the number of antibodies ranged widely between individuals. But, promisingly, their levels remained fairly stable over time, declining only modestly at 6 to 8 months after infection… virus-specific B cells increased over time. People had more memory B cells six months after symptom onset than at one month afterwards… levels of T cells for the virus also remained high after infection. Six months after symptom onset, 92% of participants had CD4+ T cells that recognized the virus… 95% of the people had at least 3 out of 5 immune-system components that could recognize SARS-CoV-2 up to 8 months after infection." 39) SARS-CoV-2 Natural Antibody Response Persists for at Least 12 Months in a Nationwide Study From the Faroe Islands, Petersen, 2021 "The seropositive rate in the convalescent individuals was above 95% at all sampling time points for both assays and remained stable over time; that is, almost all convalescent individuals developed antibodies… results show that SARS-CoV-2 antibodies persisted at least 12 months after symptom onset and maybe even longer, indicating that COVID-19-convalescent individuals may be protected from reinfection." 40) SARS-CoV-2-specific T cell memory is sustained in COVID-19 convalescent patients for 10 months with successful development of stem cell-like memory T cells, Jung, 2021 "ex vivo assays to evaluate SARS-CoV-2-specific CD4+ and CD8+ T cell responses in COVID-19 convalescent patients up to 317 days post-symptom onset (DPSO), and find that memory T cell responses are maintained during the study period regardless of the severity of COVID-19. In particular, we observe sustained polyfunctionality and proliferation capacity of SARS-CoV-2-specific T cells. Among SARS-CoV-2-specific CD4+ and CD8+ T cells detected by activation-induced markers, the proportion of stem cell-like memory T (TSCM) cells is increased, peaking at approximately 120 DPSO." 41) Immune Memory in Mild COVID-19 Patients and Unexposed Donors Reveals Persistent T Cell Responses After SARS-CoV-2 Infection, Ansari, 2021 "Analyzed 42 unexposed healthy donors and 28 mild COVID-19 subjects up to 5 months from the recovery for SARS-CoV-2 specific immunological memory. Using HLA class II predicted peptide megapools, we identified SARS-CoV-2 cross-reactive CD4+ T cells in around 66% of the unexposed individuals. Moreover, we found detectable immune memory in mild COVID-19 patients several months after recovery in the crucial arms of protective adaptive immunity; CD4+ T cells and B cells, with a minimal contribution from CD8+ T cells. Interestingly, the persistent immune memory in COVID-19 patients is predominantly targeted towards the Spike glycoprotein of the SARS-CoV-2. This study provides the evidence of both high magnitude pre-existing and persistent immune memory in Indian population." 42) COVID-19 natural immunity, WHO, 2021 "Current evidence points to most individuals developing strong protective immune responses following natural infection with SARSCoV-2. Within 4 weeks following infection, 90-99% of individuals infected with the SARS-CoV-2 virus develop detectable neutralizing antibodies. The strength and duration of the immune responses to SARS-CoV-2 are not completely understood and currently available data suggests that it varies by age and the severity of symptoms. Available scientific data suggests that in most people immune responses remain robust and protective against reinfection for at least 6-8 months after infection (the longest follow up with strong scientific evidence is currently approximately 8 months)." 43) Antibody Evolution after SARS-CoV-2 mRNA Vaccination, Cho, 2021 "We conclude that memory antibodies selected over time by natural infection have greater potency and breadth than antibodies elicited by vaccination…boosting vaccinated individuals with currently available mRNA vaccines would produce a quantitative increase in plasma neutralizing activity but not the qualitative advantage against variants obtained by vaccinating convalescent individuals." 44) Humoral Immune Response to SARS-CoV-2 in Iceland, Gudbjartsson, 2020 "Measured antibodies in serum samples from 30,576 persons in Iceland…of the 1797 persons who had recovered from SARS-CoV-2 infection, 1107 of the 1215 who were tested (91.1%) were seropositive…results indicate risk of death from infection was 0.3% and that antiviral antibodies against SARS-CoV-2 did not decline within 4 months after diagnosis (para)." 45) Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection, Dan, 2021 "Analyzed multiple compartments of circulating immune memory to SARS-CoV-2 in 254 samples from 188 COVID-19 cases, including 43 samples at ≥ 6 months post-infection…IgG to the Spike protein was relatively stable over 6+ months. Spike-specific memory B cells were more abundant at 6 months than at 1 month post symptom onset." 46) The prevalence of adaptive immunity to COVID-19 and reinfection after recovery – a comprehensive systematic review and meta-analysis of 12 011 447 individuals, Chivese, 2021 "Fifty-four studies, from 18 countries, with a total of 12 011 447 individuals, followed up to 8 months after recovery, were included. At 6-8 months after recovery, the prevalence of detectable SARS-CoV-2 specific immunological memory remained high; IgG – 90.4%… pooled prevalence of reinfection was 0.2% (95%CI 0.0 – 0.7, I2 = 98.8, 9 studies). Individuals who recovered from COVID-19 had an 81% reduction in odds of a reinfection (OR 0.19, 95% CI 0.1 – 0.3, I2 = 90.5%, 5 studies)." 47) Reinfection Rates among Patients who Previously Tested Positive for COVID-19: a Retrospective Cohort Study, Sheehan, 2021 "Retrospective cohort study of one multi-hospital health system included 150,325 patients tested for COVID-19 infection…prior infection in patients with COVID-19 was highly protective against reinfection and symptomatic disease. This protection increased over time, suggesting that viral shedding or ongoing immune response may persist beyond 90 days and may not represent true reinfection." 48) Assessment of SARS-CoV-2 Reinfection 1 Year After Primary Infection in a Population in Lombardy, Italy, Vitale, 2020 "The study results suggest that reinfections are rare events and patients who have recovered from COVID-19 have a lower risk of reinfection. Natural immunity to SARS-CoV-2 appears to confer a protective effect for at least a year, which is similar to the protection reported in recent vaccine studies." 49) Prior SARS-CoV-2 infection is associated with protection against symptomatic reinfection, Hanrath, 2021 "We observed no symptomatic reinfections in a cohort of healthcare workers…this apparent immunity to re-infection was maintained for at least 6 months…test positivity rates were 0% (0/128 [95% CI: 0–2.9]) in those with previous infection compared to 13.7% (290/2115 [95% CI: 12.3–15.2]) in those without (P<0.0001 χ2 test)." 50) Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals, Grifoni, 2020 "Using HLA class I and II predicted peptide "megapools," circulating SARS-CoV-2-specific CD8+ and CD4+ T cells were identified in ∼70% and 100% of COVID-19 convalescent patients, respectively. CD4+ T cell responses to spike, the main target of most vaccine efforts, were robust and correlated with the magnitude of the anti-SARS-CoV-2 IgG and IgA titers. The M, spike, and N proteins each accounted for 11%–27% of the total CD4+ response, with additional responses commonly targeting nsp3, nsp4, ORF3a, and ORF8, among others. For CD8+ T cells, spike and M were recognized, with at least eight SARS-CoV-2 ORFs targeted." 51) NIH Director's Blog: Immune T Cells May Offer Lasting Protection Against COVID-19, Collins, 2021 "Much of the study on the immune response to SARS-CoV-2, the novel coronavirus that causes COVID-19, has focused on the production of antibodies. But, in fact, immune cells known as memory T cells also play an important role in the ability of our immune systems to protect us against many viral infections, including—it now appears—COVID-19.An intriguing new study of these memory T cells suggests they might protect some people newly infected with SARS-CoV-2 by remembering past encounters with other human coronaviruses. This might potentially explain why some people seem to fend off the virus and may be less susceptible to becoming severely ill with COVID-19." 52) Ultrapotent antibodies against diverse and highly transmissible SARS-CoV-2 variants, Wang, 2021 "Our study demonstrates that convalescent subjects previously infected with ancestral variant SARS-CoV-2 produce antibodies that cross-neutralize emerging VOCs with high potency…potent against 23 variants, including variants of concern." 53) Why COVID-19 Vaccines Should Not Be Required for All Americans, Makary, 2021 "Requiring the vaccine in people who are already immune with natural immunity has no scientific support. While vaccinating those people may be beneficial – and it's a reasonable hypothesis that vaccination may bolster the longevity of their immunity – to argue dogmatically that they must get vaccinated has zero clinical outcome data to back it. As a matter of fact, we have data to the contrary: A Cleveland Clinic study found that vaccinating people with natural immunity did not add to their level of protection." 54) Protracted yet coordinated differentiation of long-lived SARS-CoV-2-specific CD8+ T cells during COVID-19 convalescence, Ma, 2021 "Screened 21 well-characterized, longitudinally-sampled convalescent donors that recovered from mild COVID-19…following a typical case of mild COVID-19, SARS-CoV-2-specific CD8+ T cells not only persist but continuously differentiate in a coordinated fashion well into convalescence, into a state characteristic of long-lived, self-renewing memory." 55) Decrease in Measles Virus-Specific CD4 T Cell Memory in Vaccinated Subjects, Naniche, 2004 "Characterized the profiles of measles vaccine (MV) vaccine-induced antigen-specific T cells over time since vaccination. In a cross-sectional study of healthy subjects with a history of MV vaccination, we found that MV-specific CD4 and CD8 T cells could be detected up to 34 years after vaccination. The levels of MV-specific CD8 T cells and MV-specific IgG remained stable, whereas the level of MV-specific CD4 T cells decreased significantly in subjects who had been vaccinated >21 years earlier." 56) Remembrance of Things Past: Long-Term B Cell Memory After Infection and Vaccination, Palm, 2019 "The success of vaccines is dependent on the generation and maintenance of immunological memory. The immune system can remember previously encountered pathogens, and memory B and T cells are critical in secondary responses to infection. Studies in mice have helped to understand how different memory B cell populations are generated following antigen exposure and how affinity for the antigen is determinant to B cell fate… upon re-exposure to an antigen the memory recall response will be faster, stronger, and more specific than a naïve response. Protective memory depends first on circulating antibodies secreted by LLPCs. When these are not sufficient for immediate pathogen neutralization and elimination, memory B cells are recalled." 57) SARS-CoV-2 specific memory B-cells from individuals with diverse disease severities recognize SARS-CoV-2 variants of concern, Lyski, 2021 "Examined the magnitude, breadth, and durability of SARS-CoV-2 specific antibodies in two distinct B-cell compartments: long-lived plasma cell-derived antibodies in the plasma, and peripheral memory B-cells along with their associated antibody profiles elicited after in vitro stimulation. We found that magnitude varied amongst individuals, but was the highest in hospitalized subjects. Variants of concern (VoC) -RBD-reactive antibodies were found in the plasma of 72% of samples in this investigation, and VoC-RBD-reactive memory B-cells were found in all but 1 subject at a single time-point. This finding, that VoC-RBD-reactive MBCs are present in the peripheral blood of all subjects including those that experienced asymptomatic or mild disease, provides a reason for optimism regarding the capacity of vaccination, prior infection, and/or both, to limit disease severity and transmission of variants of concern as they continue to arise and circulate." 58) Exposure to SARS-CoV-2 generates T-cell memory in the absence of a detectable viral infection, Wang, 2021 "T-cell immunity is important for recovery from COVID-19 and provides heightened immunity for re-infection. However, little is known about the SARS-CoV-2-specific T-cell immunity in virus-exposed individuals…report virus-specific CD4+ and CD8+ T-cell memory in recovered COVID-19 patients and close contacts…close contacts are able to gain T-cell immunity against SARS-CoV-2 despite lacking a detectable infection." 59) CD8+ T-Cell Responses in COVID-19 Convalescent Individuals Target Conserved Epitopes From Multiple Prominent SARS-CoV-2 Circulating Variants, Redd, 2021and Lee, 2021 "The CD4 and CD8 responses generated after natural infection are equally robust, showing activity against multiple "epitopes" (little segments) of the spike protein of the virus. For instance, CD8 cells responds to 52 epitopes and CD4 cells respond to 57 epitopes across the spike protein, so that a few mutations in the variants cannot knock out such a robust and in-breadth T cell response…only 1 mutation found in Beta variant-spike overlapped with a previously identified epitope (1/52), suggesting that virtually all anti-SARS-CoV-2 CD8+ T-cell responses should recognize these newly described variants." 60) Exposure to common cold coronaviruses can teach the immune system to recognize SARS-CoV-2,La Jolla, Crotty and Sette, 2020 "Exposure to common cold coronaviruses can teach the immune system to recognize SARS-CoV-2" 61) Selective and cross-reactive SARS-CoV-2 T cell epitopes in unexposed humans, Mateus, 2020 "Found that the pre-existing reactivity against SARS-CoV-2 comes from memory T cells and that cross-reactive T cells can specifically recognize a SARS-CoV-2 epitope as well as the homologous epitope from a common cold coronavirus. These findings underline the importance of determining the impacts of pre-existing immune memory in COVID-19 disease severity." 62) Longitudinal observation of antibody responses for 14 months after SARS-CoV-2 infection, Dehgani-Mobaraki, 2021 "Better understanding of antibody responses against SARS-CoV-2 after natural infection might provide valuable insights into the future implementation of vaccination policies. Longitudinal analysis of IgG antibody titers was carried out in 32 recovered COVID-19 patients based in the Umbria region of Italy for 14 months after Mild and Moderately-Severe infection…study findings are consistent with recent studies reporting antibody persistency suggesting that induced SARS-CoV-2 immunity through natural infection, might be very efficacious against re-infection (>90%) and could persist for more than six months. Our study followed up patients up to 14 months demonstrating the presence of anti-S-RBD IgG in 96.8% of recovered COVID-19 subjects." 63) Humoral and circulating follicular helper T cell responses in recovered patients with COVID-19, Juno, 2020 "Characterized humoral and circulating follicular helper T cell (cTFH) immunity against spike in recovered patients with coronavirus disease 2019 (COVID-19). We found that S-specific antibodies, memory B cells and cTFH are consistently elicited after SARS-CoV-2 infection, demarking robust humoral immunity and positively associated with plasma neutralizing activity." 64) Convergent antibody responses to SARS-CoV-2 in convalescent individuals, Robbiani, 2020 "149 COVID-19-convalescent individuals…antibody sequencing revealed the expansion of clones of RBD-specific memory B cells that expressed closely related antibodies in different individuals. Despite low plasma titres, antibodies to three distinct epitopes on the RBD neutralized the virus with half-maximal inhibitory concentrations (IC50 values) as low as 2 ng ml−1." 65) Rapid generation of durable B cell memory to SARS-CoV-2 spike and nucleocapsid proteins in COVID-19 and convalescence, Hartley, 2020 "COVID-19 patients rapidly generate B cell memory to both the spike and nucleocapsid antigens following SARS-CoV-2 infection…RBD- and NCP-specific IgG and Bmem cells were detected in all 25 patients with a history of COVID-19." 66) Had COVID? You'll probably make antibodies for a lifetime, Callaway, 2021 "People who recover from mild COVID-19 have bone-marrow cells that can churn out antibodies for decades…the study provides evidence that immunity triggered by SARS-CoV-2 infection will be extraordinarily long-lasting." 67) A majority of uninfected adults show preexisting antibody reactivity against SARS-CoV-2, Majdoubi, 2021 In greater Vancouver Canada, "using a highly sensitive multiplex assay and positive/negative thresholds established in infants in whom maternal antibodies have waned, we determined that more than 90% of uninfected adults showed antibody reactivity against the spike protein, receptor-binding domain (RBD), N-terminal domain (NTD), or the nucleocapsid (N) protein from SARS-CoV-2." 68) SARS-CoV-2-reactive T cells in healthy donors and patients with COVID-19, Braun, 2020 "The results indicate that spike-protein cross-reactive T cells are present, which were probably generated during previous encounters with endemic coronaviruses." Presence of SARS-CoV-2-reactive T cells in COVID-19 patients and healthy donors, Braun, 2020 "The presence of pre-existing SARS-CoV-2-reactive T cells in a subset of SARS-CoV-2 naïve HD is of high interest." 69) Naturally enhanced neutralizing breadth against SARS-CoV-2 one year after infection, Wang, 2021 "A cohort of 63 individuals who have recovered from COVID-19 assessed at 1.3, 6.2 and 12 months after SARS-CoV-2 infection…the data suggest that immunity in convalescent individuals will be very long lasting." 70) One Year after Mild COVID-19: The Majority of Patients Maintain Specific Immunity, But One in Four Still Suffer from Long-Term Symptoms, Rank, 2021 "Long-lasting immunological memory against SARS-CoV-2 after mild COVID-19… activation-induced marker assays identified specific T-helper cells and central memory T-cells in 80% of participants at a 12-month follow-up." 71) IDSA, 2021 "Immune responses to SARS-CoV-2 following natural infection can persist for at least 11 months… natural infection (as determined by a prior positive antibody or PCR-test result) can confer protection against SARS-CoV-2 infection." 72) Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: a population-level observational study, Holm Hansen, 2021 Denmark, "during the first surge (ie, before June, 2020), 533 381 people were tested, of whom 11 727 (2·20%) were PCR positive, and 525 339 were eligible for follow-up in the second surge, of whom 11 068 (2·11%) had tested positive during the first surge. Among eligible PCR-positive individuals from the first surge of the epidemic, 72 (0·65% [95% CI 0·51–0·82]) tested positive again during the second surge compared with 16 819 (3·27% [3·22–3·32]) of 514 271 who tested negative during the first surge (adjusted RR 0·195 [95% CI 0·155–0·246])." 73) Antigen-Specific Adaptive Immunity to SARS-CoV-2 in Acute COVID-19 and Associations with Age and Disease Severity, Moderbacher, 2020 "Adaptive immune responses limit COVID-19 disease severity…multiple coordinated arms of adaptive immunity control better than partial responses…completed a combined examination of all three branches of adaptive immunity at the level of SARS-CoV-2-specific CD4+ and CD8+ T cell and neutralizing antibody responses in acute and convalescent subjects. SARS-CoV-2-specific CD4+ and CD8+ T cells were each associated with milder disease. Coordinated SARS-CoV-2-specific adaptive immune responses were associated with milder disease, suggesting roles for both CD4+ and CD8+ T cells in protective immunity in COVID-19." 74) Detection of SARS-CoV-2-Specific Humoral and Cellular Immunity in COVID-19 Convalescent Individuals, Ni, 2020 "Collected blood from COVID-19 patients who have recently become virus-free, and therefore were discharged, and detected SARS-CoV-2-specific humoral and cellular immunity in eight newly discharged patients. Follow-up analysis on another cohort of six patients 2 weeks post discharge also revealed high titers of immunoglobulin G (IgG) antibodies. In all 14 patients tested, 13 displayed serum-neutralizing activities in a pseudotype entry assay. Notably, there was a strong correlation between neutralization antibody titers and the numbers of virus-specific T cells." 75) Robust SARS-CoV-2-specific T-cell immunity is maintained at 6 months following primary infection, Zuo, 2020 "Analysed the magnitude and phenotype of the SARS-CoV-2 cellular immune response in 100 donors at six months following primary infection and related this to the profile of antibody level against spike, nucleoprotein and RBD over the previous six months. T-cell immune responses to SARS-CoV-2 were present by ELISPOT and/or ICS analysis in all donors and are characterised by predominant CD4+ T cell responses with strong IL-2 cytokine expression… functional SARS-CoV-2-specific T-cell responses are retained at six months following infection." 76) Negligible impact of SARS-CoV-2 variants on CD4+ and CD8+ T cell reactivity in COVID-19 exposed donors and vaccinees, Tarke, 2021 "Performed a comprehensive analysis of SARS-CoV-2-specific CD4+ and CD8+ T cell responses from COVID-19 convalescent subjects recognizing the ancestral strain, compared to variant lineages B.1.1.7, B.1.351, P.1, and CAL.20C as well as recipients of the Moderna (mRNA-1273) or Pfizer/BioNTech (BNT162b2) COVID-19 vaccines… the sequences of the vast majority of SARS-CoV-2 T cell epitopes are not affected by the mutations found in the variants analyzed. Overall, the results demonstrate that CD4+ and CD8+ T cell responses in convalescent COVID-19 subjects or COVID-19 mRNA vaccinees are not substantially affected by mutations." 77) A 1 to 1000 SARS-CoV-2 reinfection proportion in members of a large healthcare provider in Israel: a preliminary report, Perez, 2021 Israel, "out of 149,735 individuals with a documented positive PCR test between March 2020 and January 2021, 154 had two positive PCR tests at least 100 days apart, reflecting a reinfection proportion of 1 per 1000." 78) Persistence and decay of human antibody responses to the receptor binding domain of SARS-CoV-2 spike protein in COVID-19 patients, Iyer, 2020 "Measured plasma and/or serum antibody responses to the receptor-binding domain (RBD) of the spike (S) protein of SARS-CoV-2 in 343 North American patients infected with SARS-CoV-2 (of which 93% required hospitalization) up to 122 days after symptom onset and compared them to responses in 1548 individuals whose blood samples were obtained prior to the pandemic…IgG antibodies persisted at detectable levels in patients beyond 90 days after symptom onset, and seroreversion was only observed in a small percentage of individuals. The concentration of these anti-RBD IgG antibodies was also highly correlated with pseudovirus NAb titers, which also demonstrated minimal decay. The observation that IgG and neutralizing antibody responses persist is encouraging, and suggests the development of robust systemic immune memory in individuals with severe infection." 79) A population-based analysis of the longevity of SARS-CoV-2 antibody seropositivity in the United States, Alfego, 2021 "To track population-based SARS-CoV-2 antibody seropositivity duration across the United States using observational data from a national clinical laboratory registry of patients tested by nucleic acid amplification (NAAT) and serologic assays… specimens from 39,086 individuals with confirmed positive COVID-19…both S and N SARS-CoV-2 antibody results offer an encouraging view of how long humans may have protective antibodies against COVID-19, with curve smoothing showing population seropositivity reaching 90% within three weeks, regardless of whether the assay detects N or S-antibodies. Most importantly, this level of seropositivity was sustained with little decay through ten months after initial positive PCR." 80) What are the roles of antibodies versus a durable, high- quality T-cell response in protective immunity against SARS-CoV-2? Hellerstein, 2020 "Progress in laboratory markers for SARS-CoV2 has been made with identification of epitopes on CD4 and CD8 T-cells in convalescent blood. These are much less dominated by spike protein than in previous coronavirus infections. Although most vaccine candidates are focusing on spike protein as antigen, natural infection by SARS-CoV-2 induces broad epitope coverage, cross-reactive with other betacoronviruses." 81) Broad and strong memory CD4+ and CD8+ T cells induced by SARS-CoV-2 in UK convalescent COVID-19 patients, Peng, 2020 "Study of 42 patients following recovery from COVID-19, including 28 mild and 14 severe cases, comparing their T cell responses to those of 16 control donors…found the breadth, magnitude and frequency of memory T cell responses from COVID-19 were significantly higher in severe compared to mild COVID-19 cases, and this effect was most marked in response to spike, membrane, and ORF3a proteins…total and spike-specific T cell responses correlated with the anti-Spike, anti-Receptor Binding Domain (RBD) as well as anti-Nucleoprotein (NP) endpoint antibody titre…furthermore showed a higher ratio of SARS-CoV-2-specific CD8+ to CD4+ T cell responses…immunodominant epitope clusters and peptides containing T cell epitopes identified in this study will provide critical tools to study the role of virus-specific T cells in control and resolution of SARS-CoV-2 infections." 82) Robust T Cell Immunity in Convalescent Individuals with Asymptomatic or Mild COVID-19, Sekine, 2020 "SARS-CoV-2-specific memory T cells will likely prove critical for long-term immune protection against COVID-19…mapped the functional and phenotypic landscape of SARS-CoV-2-specific T cell responses in unexposed individuals, exposed family members, and individuals with acute or convalescent COVID-19…collective dataset shows that SARS-CoV-2 elicits broadly directed and functionally replete memory T cell responses, suggesting that natural exposure or infection may prevent recurrent episodes of severe COVID-19." 83) Potent SARS-CoV-2-Specific T Cell Immunity and Low Anaphylatoxin Levels Correlate With Mild Disease Progression in COVID-19 Patients, Lafron, 2021 "Provide a full picture of cellular and humoral immune responses of COVID-19 patients and prove that robust polyfunctional CD8+ T cell responses concomitant with low anaphylatoxin levels correlate with mild infections." 84) SARS-CoV-2 T-cell epitopes define heterologous and COVID-19 induced T-cell recognition, Nelde, 2020 "The first work identifying and characterizing SARS-CoV-2-specific and cross-reactive HLA class I and HLA-DR T-cell epitopes in SARS-CoV-2 convalescents (n = 180) as well as unexposed individuals (n = 185) and confirming their relevance for immunity and COVID-19 disease course…cross-reactive SARS-CoV-2 T-cell epitopes revealed pre-existing T-cell responses in 81% of unexposed individuals, and validation of similarity to common cold human coronaviruses provided a functional basis for postulated heterologous immunity in SARS-CoV-2 infection…intensity of T-cell responses and recognition rate of T-cell epitopes was significantly higher in the convalescent donors compared to unexposed individuals, suggesting that not only expansion, but also diversity spread of SARS-CoV-2 T-cell responses occur upon active infection." 85) Karl Friston: up to 80% not even susceptible to Covid-19, Sayers, 2020 "Results have just been published of a study suggesting that 40%-60% of people who have not been exposed to coronavirus have resistance at the T-cell level from other similar coronaviruses like the common cold…the true portion of people who are not even susceptible to Covid-19 may be as high as 80%." 86) CD8+ T cells specific for an immunodominant SARS-CoV-2 nucleocapsid epitope cross-react with selective seasonal coronaviruses, Lineburg, 2021 "Screening of SARS-CoV-2 peptide pools revealed that the nucleocapsid (N) protein induced an immunodominant response in HLA-B7+ COVID-19-recovered individuals that was also detectable in unexposed donors…the basis of selective T cell cross-reactivity for an immunodominant SARS-CoV-2 epitope and its homologs from seasonal coronaviruses, suggesting long-lasting protective immunity." 87) SARS-CoV-2 genome-wide mapping of CD8 T cell recognition reveals strong immunodominance and substantial CD8 T cell activation in COVID-19 patients, Saini, 2020 "COVID-19 patients showed strong T cell responses, with up to 25% of all CD8+ lymphocytes specific to SARS-CoV-2-derived immunodominant epitopes, derived from ORF1 (open reading frame 1), ORF3, and Nucleocapsid (N) protein. A strong signature of T cell activation was observed in COVID-19 patients, while no T cell activation was seen in the 'non-exposed' and 'high exposure risk' healthy donors." 88) Equivalency of Protection from Natural Immunity in COVID-19 Recovered Versus Fully Vaccinated Persons: A Systematic Review and Pooled Analysis, Shenai, 2021 "Systematic review and pooled analysis of clinical studies to date, that (1) specifically compare the protection of natural immunity in the COVID-recovered versus the efficacy of full vaccination in the COVID-naive, and (2) the added benefit of vaccination in the COVID-recovered, for prevention of subsequent SARS-CoV-2 infection…review demonstrates that natural immunity in COVID-recovered individuals is, at least, equivalent to the protection afforded by full vaccination of COVID-naïve populations. There is a modest and incremental relative benefit to vaccination in COVID-recovered individuals; however, the net benefit is marginal on an absolute basis." 89) ChAdOx1nCoV-19 effectiveness during an unprecedented surge in SARS CoV-2 infections, Satwik, 2021 "The third key finding is that previous infections with SARS-CoV-2 were significantly protective against all studied outcomes, with an effectiveness of 93% (87 to 96%) seen against symptomatic infections, 89% (57 to 97%) against moderate to severe disease and 85% (-9 to 98%) against supplemental oxygen therapy. All deaths occurred in previously uninfected individuals. This was higher protection than that offered by single or double dose vaccine." 90) SARS-CoV-2 specific T cells and antibodies in COVID-19 protection: a prospective study, Molodtsov, 2021 "Explore the impact of T cells and to quantify the protective levels of the immune responses…5,340 Moscow residents were evaluated for the antibody and cellular immune responses to SARS-CoV-2 and monitored for COVID-19 up to 300 days. The antibody and cellular responses were tightly interconnected, their magnitude inversely correlated with infection probability. Similar maximal level of protection was reached by individuals positive for both types of responses and by individuals with antibodies alone…T cells in the absence of antibodies provided an intermediate level of protection." 91) Anti- SARS-CoV-2 Receptor Binding Domain Antibody Evolution after mRNA Vaccination, Cho, 2021 "SARS-CoV-2 infection produces B-cell responses that continue to evolve for at least one year. During that time, memory B cells express increasingly broad and potent antibodies that are resistant to mutations found in variants of concern." 92) Seven-month kinetics of SARS-CoV-2 antibodies and role of pre-existing antibodies to human coronaviruses, Ortega, 2021 "Impact of pre-existing antibodies to human coronaviruses causing common cold (HCoVs), is essential to understand protective immunity to COVID-19 and devise effective surveillance strategies…after the peak response, anti-spike antibody levels increase from ~150 days post-symptom onset in all individuals (73% for IgG), in the absence of any evidence of re-exposure. IgG and IgA to HCoV are significantly higher in asymptomatic than symptomatic seropositive individuals. Thus, pre-existing cross-reactive HCoVs antibodies could have a protective effect against SARS-CoV-2 infection and COVID-19 disease." 93) Immunodominant T-cell epitopes from the SARS-CoV-2 spike antigen reveal robust pre-existing T-cell immunity in unexposed individuals, Mahajan, 2021 "Findings suggest that SARS-CoV-2 reactive T-cells are likely to be present in many individuals because of prior exposure to flu and CMV viruses." 94) Neutralizing Antibody Responses to Severe Acute Respiratory Syndrome Coronavirus 2 in Coronavirus Disease 2019 Inpatients and Convalescent Patients, Wang, 2020 "117 blood samples were collected from 70 COVID-19 inpatients and convalescent patients…the neutralizing antibodies were detected even at the early stage of disease, and a significant response was shown in convalescent patients." 95) Not just antibodies: B cells and T cells mediate immunity to COVID-19, Cox, 2020 "Reports that antibodies to SARS-CoV-2 are not maintained in the serum following recovery from the virus have caused alarm…the absence of specific antibodies in the serum does not necessarily mean an absence of immune memory." 96) T cell immunity to SARS-CoV-2 following natural infection and vaccination, DiPiazza, 2020 "Although T cell durability to SARS-CoV-2 remains to be determined, current data and past experience from human infection with other CoVs demonstrate the potential for persistence and the capacity to control viral replication and host disease, and importance in vaccine-induced protection." 97) Durable SARS-CoV-2 B cell immunity after mild or severe disease, Ogega, 2021 "Multiple studies have shown loss of severe acute respiratory syndrome coronavirus 2-specific (SARS-CoV-2-specific) antibodies over time after infection, raising concern that humoral immunity against the virus is not durable. If immunity wanes quickly, millions of people may be at risk for reinfection after recovery from coronavirus disease 2019 (COVID-19). However, memory B cells (MBCs) could provide durable humoral immunity even if serum neutralizing antibody titers decline… data indicate that most SARS-CoV-2-infected individuals develop S-RBD-specific, class-switched rMBCs that resemble germinal center-derived B cells induced by effective vaccination against other pathogens, providing evidence for durable B cell-mediated immunity against SARS-CoV-2 after mild or severe disease." 98) Memory T cell responses targeting the SARS coronavirus persist up to 11 years post-infection., Ng, 2016 "All memory T cell responses detected target the SARS-Co-V structural proteins… these responses were found to persist up to 11 years post-infection… knowledge of the persistence of SARS-specific cellular immunity targeting the viral structural proteins in SARS-recovered individuals is important." 99) Adaptive immunity to SARS-CoV-2 and COVID-19, Sette, 2021 "The adaptive immune system is important for control of most viral infections. The three fundamental components of the adaptive immune system are B cells (the source of antibodies), CD4+ T cells, and CD8+ T cells…a picture has begun to emerge that reveals that CD4+ T cells, CD8+ T cells, and neutralizing antibodies all contribute to control of SARS-CoV-2 in both non-hospitalized and hospitalized cases of COVID-19." 100) Early induction of functional SARS-CoV-2-specific T cells associates with rapid viral clearance and mild disease in COVID-19 patients, Tan, 2021 "These findings provide support for the prognostic value of early functional SARS-CoV-2-specific T cells with important implications in vaccine design and immune monitoring." 101) SARS-CoV-2–specific CD8+ T cell responses in convalescent COVID-19 individuals, Kared, 2021 "A multiplexed peptide-MHC tetramer approach was used to screen 408 SARS-CoV-2 candidate epitopes for CD8+ T cell recognition in a cross-sectional sample of 30 coronavirus disease 2019 convalescent individuals…Modelling demonstrated a coordinated and dynamic immune response characterized by a decrease in inflammation, increase in neutralizing antibody titer, and differentiation of a specific CD8+ T cell response. Overall, T cells exhibited distinct differentiation into stem cell and transitional memory states (subsets), which may be key to developing durable protection." 102) S Protein-Reactive IgG and Memory B Cell Production after Human SARS-CoV-2 Infection Includes Broad Reactivity to the S2 Subunit, Nguyen-Contant, 2021 "Most importantly, we demonstrate that infection generates both IgG and IgG MBCs against the novel receptor binding domain and the conserved S2 subunit of the SARS-CoV-2 spike protein. Thus, even if antibody levels wane, long-lived MBCs remain to mediate rapid antibody production. Our study results also suggest that SARS-CoV-2 infection strengthens pre-existing broad coronavirus protection through S2-reactive antibody and MBC formation." 103) Persistence of Antibody and Cellular Immune Responses in Coronavirus Disease 2019 Patients Over Nine Months After Infection, Yao, 2021 "A cross-sectional study to assess the virus-specific antibody and memory T and B cell responses in coronavirus disease 2019 (COVID-19) patients up to 343 days after infection…found that approximately 90% of patients still have detectable immunoglobulin (Ig)G antibodies against spike and nucleocapsid proteins and neutralizing antibodies against pseudovirus, whereas ~60% of patients had detectable IgG antibodies against receptor-binding domain and surrogate virus-neutralizing antibodies…SARS-CoV-2-specific IgG+ memory B cell and interferon-γ-secreting T cell responses were detectable in more than 70% of patients…coronavirus 2-specific immune memory response persists in most patients approximately 1 year after infection, which provides a promising sign for prevention from reinfection and vaccination strategy." 104) Naturally Acquired SARS-CoV-2 Immunity Persists for Up to 11 Months Following Infection, De Giorgi, 2021 "A prospective, longitudinal analysis of COVID-19 convalescent plasma donors at multiple time points over an 11-month period to determine how circulating antibody levels change over time following natural infection… data suggest that immunological memory is acquired in most individuals infected with SARS-CoV-2 and is sustained in a majority of patients." 105) Decreasing Seroprevalence of Measles Antibodies after Vaccination – Possible Gap in Measles Protection in Adults in the Czech Republic, Smetana, 2017 "A long-term high rate of seropositivity persists after natural measles infection. By contrast, it decreases over time after vaccination. Similarly, the concentrations of antibodies in persons with measles history persist for a longer time at a higher level than in vaccinated persons." 106) Broadly cross-reactive antibodies dominate the human B cell response against 2009 pandemic H1N1 influenza virus infection, Wrammert, 2011 "The expansion of these rare types of memory B cells may explain why most people did not become severely ill, even in the absence of pre-existing protective antibody titers"…found "extraordinarily" powerful antibodies in the blood of nine people who caught the swine flu naturally and recovered from it."…unlike antibodies elicited by annual influenza vaccinations, most neutralizing antibodies induced by pandemic H1N1 infection were broadly cross-reactive against epitopes in the hemagglutinin (HA) stalk and head domain of multiple influenza strains. The antibodies were from cells that had undergone extensive affinity maturation." 107) Reinfection With Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in Patients Undergoing Serial Laboratory Testing, Qureshi, 2021 "Reinfection was identified in 0.7% (n = 63, 95% confidence interval [CI]: .5%–.9%) during follow-up of 9119 patients with SARS-CoV-2 infection." 108) Distinct antibody and memory B cell responses in SARS-CoV-2 naïve and recovered individuals following mRNA vaccination, Goel, 2021 "Interrogated antibody and antigen-specific memory B cells over time in 33 SARS-CoV-2 naïve and 11 SARS-CoV-2 recovered subjects… In SARS-CoV-2 recovered individuals, antibody and memory B cell responses were significantly boosted after the first vaccine dose; however, there was no increase in circulating antibodies, neutralizing titers, or antigen-specific memory B cells after the second dose. This robust boosting after the first vaccine dose strongly correlated with levels of pre-existing memory B cells in recovered individuals, identifying a key role for memory B cells in mounting recall responses to SARS-CoV-2 antigens." 109) Covid-19: Do many people have pre-existing immunity? Doshi, 2020 "Six studies have reported T cell reactivity against SARS-CoV-2 in 20% to 50% of people with no known exposure to the virus… in a study of donor blood specimens obtained in the US between 2015 and 2018, 50% displayed various forms of T cell reactivity to SARS-CoV-2… Researchers are also confident that they have made solid inroads into ascertaining the origins of the immune responses. "Our hypothesis, of course, was that it's so called 'common cold' coronaviruses, because they're closely related…we have really shown that this is a true immune memory and it is derived in part from common cold viruses." 110) Pre-existing and de novo humoral immunity to SARS-CoV-2 in humans, Ng, 2020 "We demonstrate the presence of pre-existing humoral immunity in uninfected and unexposed humans to the new coronavirus. SARS-CoV-2 S-reactive antibodies were readily detectable by a sensitive flow cytometry-based method in SARS-CoV-2-uninfected individuals and were particularly prevalent in children and adolescents." 111) Phenotype of SARS-CoV-2-specific T-cells in COVID-19 patients with acute respiratory distress syndrome, Weiskopf, 2020 "We detected SARS-CoV-2-specific CD4+ and CD8+ T cells in 100% and 80% of COVID-19 patients, respectively. We also detected low levels of SARS-CoV-2-reactive T-cells in 20% of the healthy controls, not previously exposed to SARS-CoV-2 and indicative of cross-reactivity due to infection with 'common cold' coronaviruses." 112) Pre-existing immunity to SARS-CoV-2: the knowns and unknowns, Sette, 2020 "T cell reactivity against SARS-CoV-2 was observed in unexposed people…it is speculated that this reflects T cell memory to circulating 'common cold' coronaviruses." 113) Pre-existing immunity against swine-origin H1N1 influenza viruses in the general human population, Greenbaum, 2009 "Memory T-cell immunity against S-OIV is present in the adult population and that such memory is of similar magnitude as the pre-existing memory against seasonal H1N1 influenza…the conservation of a large fraction of T-cell epitopes suggests that the severity of an S-OIV infection, as far as it is determined by susceptibility of the virus to immune attack, would not differ much from that of seasonal flu." 114) Cellular immune correlates of protection against symptomatic pandemic influenza, Sridhar, 2013 "The 2009 H1N1 pandemic (pH1N1) provided a unique natural experiment to determine whether cross-reactive cellular immunity limits symptomatic illness in antibody-naive individuals… Higher frequencies of pre-existing T cells to conserved CD8 epitopes were found in individuals who developed less severe illness, with total symptom score having the strongest inverse correlation with the frequency of interferon-γ (IFN-γ)( ) interleukin-2 (IL-2)(-) CD8() T cells (r = -0.6, P = 0.004)… CD8(+) T cells specific to conserved viral epitopes correlated with cross-protection against symptomatic influenza."115) Preexisting influenza-specific CD4+ T cells correlate with disease protection against influenza challenge in humans, Wilkinson, 2012 "Precise role of T cells in human influenza immunity is uncertain. We conducted influenza infection studies in healthy volunteers with no detectable antibodies to the challenge viruses H3N2 or H1N1…mapped T cell responses to influenza before and during infection…found a large increase in influenza-specific T cell responses by day 7, when virus was completely cleared from nasal samples and serum antibodies were still undetectable. Pre-existing CD4+, but not CD8+, T cells responding to influenza internal proteins were associated with lower virus shedding and less severe illness. These CD4+ cells also responded to pandemic H1N1 (A/CA/07/2009) peptides and showed evidence of cytotoxic activity." 116) Serum cross-reactive antibody response to a novel influenza A (H1N1) virus after vaccination with seasonal influenza vaccine, CDC, MMWR, 2009 "No increase in cross-reactive antibody response to the novel influenza A (H1N1) virus was observed among adults aged >60 years. These data suggest that receipt of recent (2005–2009) seasonal influenza vaccines is unlikely to elicit a protective antibody response to the novel influenza A (H1N1) virus." 117) No one is naive: the significance of heterologous T-cell immunity, Welsh, 2002 "Memory T cells that are specific for one virus can become activated during infection with an unrelated heterologous virus, and might have roles in protective immunity and immunopathology. The course of each infection is influenced by the T-cell memory pool that has been laid down by a host's history of previous infections, and with each successive infection, T-cell memory to previously encountered agents is modified." 118) Intrafamilial Exposure to SARS-CoV-2 Induces Cellular Immune Response without Seroconversion, Gallais, 2020 "Individuals belonging to households with an index COVID-19 patient, reported symptoms of COVID-19 but discrepant serology results… All index patients recovered from a mild COVID-19. They all developed anti-SARS-CoV-2 antibodies and a significant T cell response detectable up to 69 days after symptom onset. Six of the eight contacts reported COVID-19 symptoms within 1 to 7 days after the index patients but all were SARS-CoV-2 seronegative… exposure to SARS-CoV-2 can induce virus-specific T cell responses without seroconversion. T cell responses may be more sensitive indicators of SARS-Co-V-2 exposure than antibodies…results indicate that epidemiological data relying only on the detection of SARS-CoV-2 antibodies may lead to a substantial underestimation of prior exposure to the virus." 119) Protective immunity after recovery from SARS-CoV-2 infection, Kojima, 2021 "It important to note that antibodies are incomplete predictors of protection. After vaccination or infection, many mechanisms of immunity exist within an individual not only at the antibody level, but also at the level of cellular immunity. It is known that SARS-CoV-2 infection induces specific and durable T-cell immunity, which has multiple SARS-CoV-2 spike protein targets (or epitopes) as well as other SARS-CoV-2 protein targets. The broad diversity of T-cell viral recognition serves to enhance protection to SARS-CoV-2 variants, with recognition of at least the alpha (B.1.1.7), beta (B.1.351), and gamma (P.1) variants of SARS-CoV-2. Researchers have also found that people who recovered from SARS-CoV infection in 2002–03 continue to have memory T cells that are reactive to SARS-CoV proteins 17 years after that outbreak. Additionally, a memory B-cell response to SARS-CoV-2 evolves between 1·3 and 6·2 months after infection, which is consistent with longer-term protection." 120) This 'super antibody' for COVID fights off multiple coronaviruses, Kwon, 2021 "This 'super antibody' for COVID fights off multiple coronaviruses…12 antibodies…that was involved in the study, isolated from people who had been infected with either SARS-CoV-2 or its close relative SARS-CoV." 121) SARS-CoV-2 infection induces sustained humoral immune responses in convalescent patients following symptomatic COVID-19, Wu, 2020 "Taken together, our data indicate sustained humoral immunity in recovered patients who suffer from symptomatic COVID-19, suggesting prolonged immunity." 122) Evidence for sustained mucosal and systemic antibody responses to SARS-CoV-2 antigens in COVID-19 patients, Isho, 2020 "Whereas anti-CoV-2 IgA antibodies rapidly decayed, IgG antibodies remained relatively stable up to 115 days PSO in both biofluids. Importantly, IgG responses in saliva and serum were correlated, suggesting that antibodies in the saliva may serve as a surrogate measure of systemic immunity." 123) The T-cell response to SARS-CoV-2: kinetic and quantitative aspects and the case for their protective role, Bertoletti, 2021 "Early appearance, multi-specificity and functionality of SARS-CoV-2-specific T cells are associated with accelerated viral clearance and with protection from severe COVID-19." 124) The longitudinal kinetics of antibodies in COVID-19 recovered patients over 14 months, Eyran, 2020 "Found a significantly faster decay in naïve vaccinees compared to recovered patients suggesting that the serological memory following natural infection is more robust compared to vaccination. Our data highlights the differences between serological memory induced by natural infection vs. vaccination." 125) Continued Effectiveness of COVID-19 Vaccination among Urban Healthcare Workers during Delta Variant Predominance, Lan, 2021 "Followed a population of urban Massachusetts HCWs…we found no re-infection among those with prior COVID-19, contributing to 74,557 re-infection-free person-days, adding to the evidence base for the robustness of naturally acquired immunity." 126) Immunity to COVID-19 in India through vaccination and natural infection, Sarraf, 2021 "Compared the vaccination induced immune response profile with that of natural infection, evaluating thereby if individuals infected during the first wave retained virus specific immunity…the overall immune response resulting from natural infection in and around Kolkata is not only to a certain degree better than that generated by vaccination, especially in the case of the Delta variant, but cell mediated immunity to SARS-CoV-2 also lasts for at least ten months after the viral infection." 127) Asymptomatic or mild symptomatic SARS-CoV-2 infection elicits durable neutralizing antibody responses in children and adolescents, Garrido, 2021 "Evaluated humoral immune responses in 69 children and adolescents with asymptomatic or mild symptomatic SARS-CoV-2 infection. We detected robust IgM, IgG, and IgA antibody responses to a broad array of SARS-CoV-2 antigens at the time of acute infection and 2 and 4 months after acute infection in all participants. Notably, these antibody responses were associated with virus-neutralizing activity that was still detectable 4 months after acute infection in 94% of children. Moreover, antibody responses and neutralizing activity in sera from children and adolescents were comparable or superior to those observed in sera from 24 adults with mild symptomatic infection. Taken together, these findings indicate that children and adolescents with mild or asymptomatic SARS-CoV-2 infection generate robust and durable humoral immune responses that can likely contribute to protection from reinfection." 128) T cell response to SARS-CoV-2 infection in humans: A systematic review, Shrotri, 2021 "Symptomatic adult COVID-19 cases consistently show peripheral T cell lymphopenia, which positively correlates with increased disease severity, duration of RNA positivity, and non-survival; while asymptomatic and paediatric cases display preserved counts. People with severe or critical disease generally develop more robust, virus-specific T cell responses. T cell memory and effector function has been demonstrated against multiple viral epitopes, and, cross-reactive T cell responses have been demonstrated in unexposed and uninfected adults, but the significance for protection and susceptibility, respectively, remains unclear." 129) Severity of SARS-CoV-2 Reinfections as Compared with Primary Infections, Abu-Raddad, 2021 "Reinfections had 90% lower odds of resulting in hospitalization or death than primary infections. Four reinfections were severe enough to lead to acute care hospitalization. None led to hospitalization in an ICU, and none ended in death. Reinfections were rare and were generally mild, perhaps because of the primed immune system after primary infection." 130) Assessment of the Risk of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Reinfection in an Intense Re-exposure Setting, Abu-Raddad, 2021 "SARS-CoV-2 reinfection can occur but is a rare phenomenon suggestive of protective immunity against reinfection that lasts for at least a few months post primary infection." 131) Increased risk of infection with SARS-CoV-2 Beta, Gamma, and Delta variant compared to Alpha variant in vaccinated individuals, Andeweg, 2021 "Analyzed 28,578 sequenced SARS-CoV-2 samples from individuals with known immune status obtained through national community testing in the Netherlands from March to August 2021. They found evidence for an "increased risk of infection by the Beta (B.1.351), Gamma (P.1), or Delta (B.1.617.2) variants compared to the Alpha (B.1.1.7) variant after vaccination. No clear differences were found between vaccines. However, the effect was larger in the first 14-59 days after complete vaccination compared to 60 days and longer. In contrast to vaccine-induced immunity, no increased risk for reinfection with Beta, Gamma or Delta variants relative to Alpha variant was found in individuals with infection-induced immunity." 132) Prior COVID-19 protects against reinfection, even in the absence of detectable antibodies, Breathnach, 2021 "Studies did not address whether prior infection is protective in the absence of a detectable humoral immune response. Patients with primary or secondary antibody deficiency syndrome and reduced or absent B cells can recover from COVID-19…Although there have been few mechanistic studies, preliminary data show that such individuals generate striking T-cell immune responses against SARS-CoV-2 peptide pools…SARS-CoV-2 specific T cell immune responses but not neutralising antibodies are associated with reduced disease severity suggesting the immune system may have considerable redundancy or compensation following COVID-19…our results add to the emerging evidence that detectable serum antibody may be an incomplete marker of protection against reinfection. This could have implications for public health and policy-making, for example if using seroprevalence data to assess population immunity, or if serum antibody levels were to be taken as official evidence of immunity – a minority of truly immune patients have no detectable antibody and could be disadvantaged as a result. Our findings highlight the need for further studies of immune correlates of protection from infection with SARS-CoV-2, which may in turn enhance development of effective vaccines and treatments." 133) Natural infection vs vaccination: Which gives more protection?, Rosenberg, 2021 "With a total of 835,792 Israelis known to have recovered from the virus, the 72 instances of reinfection amount to 0.0086% of people who were already infected with COVID…By contrast, Israelis who were vaccinated were 6.72 times more likely to get infected after the shot than after natural infection, with over 3,000 of the 5,193,499, or 0.0578%, of Israelis who were vaccinated getting infected in the latest wave." 134) Community transmission and viral load kinetics of the SARS-CoV-2 delta (B.1.617.2) variant in vaccinated and unvaccinated individuals in the UK: a prospective, longitudinal, cohort study, Singanayagam, 2021 "Nonetheless, fully vaccinated individuals with breakthrough infections have peak viral load similar to unvaccinated cases and can efficiently transmit infection in household settings, including to fully vaccinated contacts." 135) Antibodies elicited by mRNA-1273 vaccination bind more broadly to the receptor binding domain than do those from SARS-CoV-2 infection, Greaney, 2021 "The neutralizing activity of vaccine-elicited antibodies was more targeted to the receptor-binding domain (RBD) of the SARS-CoV-2 spike protein compared to antibodies elicited by natural infection. However, within the RBD, binding of vaccine-elicited antibodies was more broadly distributed across epitopes compared to infection-elicited antibodies. This greater binding breadth means that single RBD mutations have less impact on neutralization by vaccine sera compared to convalescent sera. Therefore, antibody immunity acquired by natural infection or different modes of vaccination may have a differing susceptibility to erosion by SARS-CoV-2 evolution." 136) Antigen-Specific Adaptive Immunity to SARS-CoV-2 in Acute COVID-19 and Associations with Age and Disease Severity, Moderbacker, 2020 "Limited knowledge is available on the relationship between antigen-specific immune responses and COVID-19 disease severity. We completed a combined examination of all three branches of adaptive immunity at the level of SARS-CoV-2-specific CD4+ and CD8+ T cell and neutralizing antibody responses in acute and convalescent subjects. SARS-CoV-2-specific CD4+ and CD8+ T cells were each associated with milder disease. Coordinated SARS-CoV-2-specific adaptive immune responses were associated with milder disease, suggesting roles for both CD4+ and CD8+ T cells in protective immunity in COVID-19. Notably, coordination of SARS-CoV-2 antigen-specific responses was disrupted in individuals ≥ 65 years old. Scarcity of naive T cells was also associated with aging and poor disease outcomes. A parsimonious explanation is that coordinated CD4+ T cell, CD8+ T cell, and antibody responses are protective, but uncoordinated responses frequently fail to control disease, with a connection between aging and impaired adaptive immune responses to SARS-CoV-2." 137) Protection and waning of natural and hybrid COVID-19 immunity, Goldberg, 2021 "Protection from reinfection decreases with time since previous infection, but is, nevertheless, higher than that conferred by vaccination with two doses at a similar time since the last immunity-conferring event." 138) A Systematic Review of the Protective Effect of Prior SARS-CoV-2 Infection on Repeat Infection, Kojima, 202 "The protective effect of prior SARS-CoV-2 infection on re-infection is high and similar to the protective effect of vaccination." Ref:
- Study: Protection and waning of natural and hybrid COVID-19 immunity
Natural immunity - the protection following infection and recovery - lasts much longer, the study shows.
In fact, people who had already had Covid once had better protection from the virus more than a year later than people who had been vaccinated only three months before.
The gap was even larger in cases of severe infection.
Vaccinated people were more than five times as likely to develop severe infections than people with natural immunity. Only 25 out of roughly 300,000 Israelis with natural immunity developed severe Covid infections in the summer wave - compared to almost 1,400 vaccinated Israelis.
The researchers found that the highest rates of infection by far came in people who had been vaccinated at least six months before. They had a nearly 3 percent chance of being infected per month (the researchers present the figure as 89 per 100,000 "person-days.")
Those people were four times as likely to be infected as newly vaccinated people. They were also seven times as likely to be infected as people who had natural immunity from an infection six to eight months before, and three times as likely as those who had natural immunity from an infection more than year before.
A single vaccination dose in people with natural immunity temporarily produced strong protection, the researchers found. But after six months, the advantage had faded to within the margin of statistical error. In other words, so-called hybrid immunity hardly appeared to exist after six months - natural immunity was once again providing the protection.
Table 133: Table 2. Summary of the results regarding confirmed infections of the Poisson regression analysis for all sub-cohorts. For each sub-cohort, the table shows the estimated covariate-adjusted (to the Israeli population during the study period, August 1, 2021, to September 30, 2021) confirmed infection rates per 100,000 person days, as well as the rate ratio of confirmed infections between individuals with a fresh second dose vaccination (up to two months) who were not previously infected relative to each of the other sub-cohorts. 95% confidence intervals without adjustment for multiplicity are given in square brackets. The Recovered 12+ sub-cohort includes the period 12-18 months. Sub-cohort Adjusted Confirmed Infection Rate Per 100000 Rate ratio of reference relative to sub-cohort Recovered 4-6 10.5 [8.8,12.4] 2.0 [1.7,2.4] Recovered 6-8 14.0 [13.3,14.8] 1.5 [1.4,1.6] Recovered 8-10 20.6 [19.2,22.1] 1.0 [0.9,1.1] Recovered 10-12 28.5 [26.9,30.2] 0.7 [0.7,0.8] Recovered 12+ 30.2 [28.5,32] 0.7 [0.6,0.8] Booster 0-2 8.2 [8.0,8.5] 2.6 [2.4,2.7] Vaccinated 0-2 21.1 [20,22.4] Reference Vaccinated 2-4 45.0 [43.7,46.4] 0.5 [0.4,0.5] Vaccinated 4-6 69.2 [68.6,69.8] 0.3 [0.3,0.3] Vaccinated 6-8 88.9 [88.3,89.6] 0.2 [0.2,0.3] Recovered then Vaccinated 0-2 3.7 [3.1,4.5] 5.7 [4.6,6.9] Recovered then Vaccinated 2-4 4.3 [3.5,5.2] 5.0 [4.0,6.1] Recovered then Vaccinated 4-6 10.3 [9.4,11.4] 2.0 [1.8,2.3] Recovered then Vaccinated 6-8 11.6 [10.0,13.5] 1.8 [1.5,2.1] Vaccinated then Recovered 4-6 12.8 [9.9,16.6] 1.7 [1.3,2.1] Vaccinated then Recovered 6-8 17.2 [15.2,19.2] 1.2 [1.1,1.4] Study Conclusion: Protection from reinfection decreases with time since previous infection, but is, nevertheless, higher than that conferred by vaccination with two doses at a similar time since the last immunity-conferring event. A single vaccine dose after infection helps to restore protection.
Ref:
- 138 Research Studies Affirm Naturally Acquired Immunity to Covid-19: Documented, Linked, and Quoted
- Vaccines temporary
A retrospective cohort study was conducted using Swedish nationwide registries.
- The cohort comprised 842,974 pairs (N=1,684,958), including individuals vaccinated with 2 doses of ChAdOx1 nCoV-19, mRNA-1273, or BNT162b2, and matched unvaccinated individuals.
- Cases of symptomatic infection and severe Covid-19 (hospitalization or 30-day mortality after confirmed infection) were collected from 12 January to 4 October 2021.
Results:
- Vaccine effectiveness of BNT162b2 against infection waned progressively from 92% (95% CI, 92-93, P<0·001) at day 15-30 to 47% (95% CI, 39-55, P<0·001) at day 121-180, and from day 211 and onwards no effectiveness could be detected (23%; 95% CI, -2-41, P=0·07).
- The effectiveness waned slightly slower for mRNA-1273, being estimated to 59% (95% CI, 18-79) from day 181 and onwards.
- In contrast, effectiveness of ChAdOx1 nCoV-19 was generally lower and waned faster, with no effectiveness detected from day 121 and onwards (-19%, 95% CI, -97-28), whereas effectiveness from heterologous ChAdOx1 nCoV-19 / mRNA was maintained from 121 days and onwards (66%; 95% CI, 41-80).
- Overall:
- vaccine effectiveness was lower and waned faster among men and older individuals
- For the outcome severe Covid-19, effectiveness waned from 89% (95% CI, 82-93, P<0·001) at day 15-30 to 42% (95% CI, -35-75, P=0·21) from day 181 and onwards, with sensitivity analyses showing notable waning among men, older frail individuals, and individuals with comorbidities.
Conclusion:
- Vaccine effectiveness against symptomatic Covid-19 infection wanes progressively over time across all subgroups, but at different rate according to type of vaccine, and faster for men and older frail individuals. The effectiveness against severe illness seems to remain high through 9 months, although not for men, older frail individuals, and individuals with comorbidities. This strengthens the evidence-based rationale for administration of a third booster dose.
Thoughts:
- the downslope in efficacy against symptomatic infection is just starting right where pfizer and moderna ended their trials and vaccinated the control groups to make future comparison impossible. (red vertical line added by me)
- out around 240 days it goes negative.
- raises questions about whether the vaccines ever provide ANY sterilizing immunity at all or if they merely prevent symptoms. recall that both the mRNA drug trials only tested those reporting symptoms for covid to assess efficacy.
Ref:
- Nordström, Peter and Ballin, Marcel and Nordström, Anna, Effectiveness of Covid-19 Vaccination Against Risk of Symptomatic Infection, Hospitalization, and Death Up to 9 Months: A Swedish Total-Population Cohort Study. Available at SSRN: https://ssrn.com/abstract=3949410 or http://dx.doi.org/10.2139/ssrn.3949410
- https://boriquagato.substack.com/p/swedish-study-shows-covid-vaccines
- Unvaccinated vs Vaccinated
- The epidemiological relevance of the COVID-19-vaccinated population is increasing
High COVID-19 vaccination rates were expected to reduce transmission of SARS-CoV-2 in populations by reducing the number of possible sources for transmission and thereby to reduce the burden of COVID-19 disease. Recent data, however, indicate that the epidemiological relevance of COVID-19 vaccinated individuals is increasing.
- In the UK it was described that secondary attack rates among household contacts exposed to fully vaccinated index cases was similar to household contacts exposed to unvaccinated index cases (25% for vaccinated vs 23% for unvaccinated).
- 12 of 31 infections in fully vaccinated household contacts (39%) arose from fully vaccinated epidemiologically linked index cases. Peak viral load did not differ by vaccination status or variant type.
- In Germany, the rate of symptomatic COVID-19 cases among the fully vaccinated ("breakthrough infections") is reported weekly since 21 July 2021 and was 16.9% at that time among patients of 60 years and older
- This proportion is increasing week by week and was 58.9% on 27 October 2021 (Figure 1) providing clear evidence of the increasing relevance of the fully vaccinated as a possible source of transmission.
- A similar situation was described for the UK. Between week 39 and 42, a total of 100.160 COVID-19 cases were reported among citizens of 60 years or older. 89.821 occurred among the fully vaccinated (89.7%), 3.395 among the unvaccinated (3.4%).
- One week before, the COVID-19 case rate per 100.000 was higher among the subgroup of the vaccinated compared to the subgroup of the unvaccinated in all age groups of 30 years or more.
- In Israel a nosocomial outbreak was reported involving 16 healthcare workers, 23 exposed patients and two family members. The source was a fully vaccinated COVID-19 patient. The vaccination rate was 96.2% among all exposed individuals (151 healthcare workers and 97 patients). Fourteen fully vaccinated patients became severely ill or died, the two unvaccinated patients developed mild disease.
- The US Centres for Disease Control and Prevention (CDC) identifies four of the top five counties with the highest percentage of fully vaccinated population (99.9–84.3%) as "high" transmission counties.
Many decisionmakers assume that the vaccinated can be excluded as a source of transmission. It appears to be grossly negligent to ignore the vaccinated population as a possible and relevant source of transmission when deciding about public health control measures.
Ref:
- COVID-19: stigmatising the unvaccinated is not justified
The claim of: "the unvaccinated threaten the vaccinated for COVID-19"
Vaccinated individuals continue to have a relevant role in transmission.
- In Massachusetts, USA, a total of 469 new COVID-19 cases were detected during various events in July, 2021, and 346 (74%) of these cases were in people who were fully or partly vaccinated, 274 (79%) of whom were symptomatic. Cycle threshold values were similarly low between people who were fully vaccinated (median 22.8) and people who were unvaccinated, not fully vaccinated, or whose vaccination status was unknown (median 21.5), indicating a high viral load even among people who were fully vaccinated.
- In the USA, a total of 10262 COVID-19 cases were reported in vaccinated people by April 30, 2021, of whom 2725 (26·6%) were asymptomatic, 995 (9.7%) were hospitalised, and 160 (1.6%) died.
- In Germany, 55.4% of symptomatic COVID-19 cases in patients aged 60 years or older were in fully vaccinated individuals
- In Münster, Germany, new cases of COVID-19 occurred in at least 85 (22%) of 380 people who were fully vaccinated or who had recovered from COVID-19 and who attended a nightclub.
People who are vaccinated have a lower risk of severe disease but are still a relevant part of the pandemic.
- It is therefore wrong and dangerous to speak of a pandemic of the unvaccinated.
Ref:
- The epidemiological relevance of the COVID-19-vaccinated population is increasing
Cutaneous Larva Migrans
Hookworm larvae of a cat or dog (Anxylostoma braziliense or caninum)
Transmitted by wlaking barefoot on contaminated sand or soil
Presents as erythmatous papule that progresses to papules in a serpentine pattern on the lower extremity
References:
- AFP Dec 2019 Vol 100, No 12
Dog and Cat Bites
Antibiotic Prophylaxis
- Adults
- 1st line: amoxicillin/clav 875/125mg bid
- Alt: clindamycin 300 mg tid plus ciprofloxacin 500 mg bid
- Children
- 1st line: amoxicillin/clav 45 mg per Kg divided bid
- Alt: clindamycin 10-20 mg/Kg divided q6-8 plus trimethoprim/sulfamethoxazole 8-10 mg/Kg of trimethoprim div bid
- Pregnant patients allergic to PCN
- 1st line: clindamycin 300 mg tid plus timethoprim/sulfamethoxazole 160 mg of trimethoprim bid
- Alt: azithromycin 250 mg to 500 mg daily (high failure rate)
Reference:
- AFP Nov 2023 Vol 108 No 5
FL Prevent Mosquito's edit
Prevent Mosquito-Borne Illness
Immediately following a storm, flooding may occur. Mosquito eggs laid in the soil during previous floods can hatch and result in very large populations. Most of these mosquitoes are considered nuisance mosquitoes, however it's essential to protect yourself and your family from mosquito breeding and mosquito-borne illness.
The risk of disease transmission through bites of infected mosquitoes to humans often increases during the warm, rainy months. To protect against mosquitoes, the Department urges the public to "Drain and Cover:"
- DRAIN standing water stop mosquitoes from multiplying.
- Drain water from garbage cans, buckets, pool covers, coolers, toys, flowerpots or any other containers where sprinkler or rainwater has collected.
- Discard old tires, drums, bottles, cans, pots and pans, broken appliances and other items that aren't being used.
- Empty and clean birdbaths and pet's water bowls at least once a week.
- Protect boats and vehicles from rain with tarps that don't accumulate water.
- Maintain swimming pools in good condition and appropriately chlorinated. Empty plastic swimming pools when not in use.
- COVER your skin with clothing or repellent to reduce mosquito bites.
- Clothing - If you must be outside when mosquitoes are active, cover up. Wear shoes, socks, long pants and long sleeves.
- Repellent - Apply mosquito repellent to bare skin and clothing. Always use repellents according to the label. Repellents with DEET, picaridin, oil of lemon eucalyptus, and IR3535 are effective.
- Use mosquito netting to protect children younger than 2 months old.
- COVER doors and windows with screens to keep mosquitoes out of your home.
- Repair broken screening on windows, doors, porches and patios.
Tips on Eliminating Mosquito Breeding Sites:
- Clean out troughs and gutters.
- Remove old tires or drill holes in those used in playgrounds to drain.
- Turn over or remove empty plastic pots.
- Pick up all beverage containers and cups.
- Check tarps on boats or other equipment that may collect water.
- Replace water in birdbaths and pet or other animal feeding dishes at least once a week.
- Change water in plant trays, including hanging plants, at least once a week.
- Remove vegetation or obstructions in drainage ditches that prevent the flow of water.
Foodborne Pathogens
The CDC estimates that norovirus is the top foodborne pathogen, sickening an average of 5.5 million people a year.
- Followed by:
- campylobacter (1.87 million illnesses)
- salmonella (1.28 million)
- Salmonella is estimated to be the top pathogen that results in deaths, followed by the campylobacter bacteria.
- clostridium perfringens (889K)
- STEC known commonly as “E. coli" (357K)
- listeria (1,250)
- Norovirus is the top pathogen that leads to the most hospitalizations.
Fever:
- Characteristically associated with:
- Campylobacter jejuni
- Shigella
- Vibrio cholerae non-O1
- Often associated:
- Norwalk virus
- Salmonella
- Vibrio parahaemolyticus
Vomiting:
- Characteristically associated with:
- Bacillus cereus (emetic syndrome)
- Norwalk virus
- Staphylococcus aureus
- Often associated:
- Clostidium botulinum
- V. cholerae O-1
- V. parahaemolyticus
Prevention:
- Washing your hands, surfaces, and cooking tools
- Separating raw foods from each other
- Cooking food long enough / to high enough temperatures
- Storing chilled and frozen foods properly
| Food | Major organisms involved |
|---|---|
| Unpasteurized milk, cheese, and other dairy products | Salmonella, Campylobacter, Escherichia coli O157, Listeria, Mycobacterium bovis, Brucella |
| Unpasteurized fruit or vegetable juices | E. coli O157, Salmonella, Clostridium botulinum |
| Eggs | Salmonella |
| Raw or undercooked meat, poultry | Salmonella, Campylobacter, E. coli O157, Yersinia, Listeria, Toxoplasma, Brucella, Trichinosis |
| Raw fish and shellfish | Vibrios, norovirus, hepatitis A, many other pathogens, toxins and parasites |
| Fresh fruits and vegetables | Cryptosporidium, Cyclospora, calicivirus, norovirus, Giardia, Shigella, E coli O157, other E coli species, hepatitis A |
| Sprouts (alfalfa, mung bean) | Salmonella, E coli O157, hepatitis A |
| Honey | C. botulinum |
| Cream-filled pastry; potato, egg, or other salad with creamy dressing | Staphylococcus aureus, Bacillus cereus |
References:
- AFP Vol 92, No 5 Sep 2015
- How many people get sick from foodborne illness in the US? | USAFacts
- Donkor ES. Cockroaches and Food-borne Pathogens. Environ Health Insights. 2020 Apr 30;14:1178630220913365. doi: 10.1177/1178630220913365. PMID: 32425541; PMCID: PMC7218330.
Hepatitis B
| Lab | Result | Meaning |
|---|---|---|
| HBsAg | negative | Susceptible |
| anti-HBc | negative | |
| anti-HBs | negative |
| Lab | Result | Meaning |
|---|---|---|
| HBsAg | negative | Immune due to natural infection |
| anti-HBc | positive | |
| anti-HBs | positive |
| Lab | Result | Meaning |
|---|---|---|
| HBsAg | negative | Immune due to hepatitis B vaccination |
| anti-HBc | negative | |
| anti-HBs | positive |
| Lab | Result | Meaning |
|---|---|---|
| HBsAg | positive | Acutely infected |
| anti-HBc | positive | |
| IgM anti-HBc | positive | |
| anti-HBs | negative |
| Lab | Result | Meaning |
|---|---|---|
| HBsAg | positive | Chronically infected |
| anti-HBc | positive | |
| IgM anti-HBc | negative | |
| anti-HBs | negative |
| Lab | Result | Meaning |
|---|---|---|
| HBsAg | negative | Interpretation unclear; four possibilities: |
| anti-HBc | positive | 1. Resolved infection (most common) |
| anti-HBs | negative | 2. False-positive anti-HBc, thus susceptible |
| 3. "Low level" chronic infection | ||
| 4. Resolving acute infection |
| Lab | Result | Meaning |
|---|---|---|
| HBsAg | negative | Resolved infection |
| anti-HBc | positive | |
| anti-HBs | positive | |
| IgM anti-HBc | negative |
- Hepatitis B surface antigen (HBsAg): A protein on the surface of hepatitis B virus; it can be detected in high levels in serum during acute or chronic hepatitis B virus infection. The presence of HBsAg indicates that the person is infectious. The body normally produces antibodies to HBsAg as part of the normal immune response to infection. HBsAg is the antigen used to make hepatitis B vaccine.
- Hepatitis B surface antibody (anti-HBs): The presence of anti-HBs is generally interpreted as indicating recovery and immunity from hepatitis B virus infection. Anti-HBs also develops in a person who has been successfully vaccinated against hepatitis B.
- Total hepatitis B core antibody (anti-HBc): Appears at the onset of symptoms in acute hepatitis B and persists for life. The presence of anti-HBc indicates previous or ongoing infection with hepatitis B virus in an undefined time frame.
- IgM antibody to hepatitis B core antigen (IgM anti-HBc): Positivity indicates recent infection with hepatitis B virus (<6 mos). Its presence indicates acute infection.
Quick summary:
- Screen infection: HBsAg (Positive = Infected)
- Screen immunity: anti-HBs (Positive = Immune)
Reference:
- https://www.cdc.gov/hepatitis/hbv/pdfs/SerologicChartv8.pdf
- JFP Vol 72 No 6 July 2023
Hepatitis C
Who to screen:
- Once to all persons 18-79yo (2020 USPSTF update)
- Periodic to those with continued risk for HCV
- Screening test: anti-HCV Ab followed by HCV RNA if positive
Those with:
- IV drug use
- Intranasal drug use
- Long-term hemodialysis
- Tatoos from unregulated settings
- Born to HCV pos mother
- Long-term partner of an HCV-infected indv
- Health care-assoc exposure to infected blood
- H/o incarceration
- HIV infection
- Abnormal liver blood tests
- H/o of blood product transfusion or organ transplant prior to 1992
Tests to order before therapy:
- Quantitative HCV RNA (viral load) test
- HCV genotype and subtype testing
- Screen for other viral infections
- HBV
- HBsAg
- anti-HBs
- anti-HBc
- HIV-1
- HBV
Tests to conduct 12 weeks before starting therapy:
- CBC - low plts could indicate cirrhosis
- INR - high INR could indicate liver disease
- LFTs
- Low albumin could indicate cirrhosis
- Elevated bilirubin could indicate cirrhosis
- ALT and AST are nonspecific markers of liver inflammation
- High Alk Phos could indicate blockage in the biliary tract
- eGFR
- HCV NS5A (depending on therapy choice)
Assess fibrosis staging:
- AST to platelet ratio index (APRI)
- APRI = [(AST/40)/Platelet]*100
- AST units: IU/L
- AST Upper Level of Normal = 40 IU/L
- Platelets: 109/L
- APRI > 1.0 has sensitivity 76% and specificity 72% for cirrhosis
- APRI > 0.7 has sensitivity 77% and specificity 72% for cirrhosis
- APRI = [(AST/40)/Platelet]*100
- FibroScan
Assess treatment response:
- If HCV is UNDETECTABLE at Week 4
- No further RNA testing is necessary while on treatment
- If HCV is DETECTABLE at Week 4
- Repeat test after additional 2 weeks
- If HCV is UNDETECTABLE
- No further RNA testing is necessary while on treatment
- If HCV has INCREASED BY >10-Fold at Week 6 or later
- Discontinue therapy
- If HCV is UNDETECTABLE
- Repeat test after additional 2 weeks
Tests to conduct after Week 4 of therapy:
- CBC
- LFTs
- If over 10-Fold increase in ALT -> Discontinue therapy and monitor liver toxicity
- If <10-Fold increase in ALT in SYMPTOMATIC patient -> Discontinue therapy
- IF <10-Fold increase in ALT in ASYMPTOMATIC patient -> Monitor and repeat ALT in 6 weeks and 8 weeks
- eGFR
Assess Treatment:
- HCV RNA test at end of treatment (optional)
- HCV RNA test at 12 weeks after end of treatment (CURED! if no detectable HCV)
If Cure (Sustained Virologic Response - SVR):
- Zero to mod fibrosis (F0-F2) - no special monitoring of follow-up HCV treatment or liver care
- Advanced fibrosis or cirrhosis (F3-F4) - Monitored for HCC with twice yearly Ultrasound
- Endoscopy recommended for patients with cirrhosis (F4 fibrosis) to screen for varices
- Those with ongoing risk for HCV reinfection - Assessed periodically (with HCV RNA) and counseled on prevention
- Persistently abnormal liver tests - Evaluated for other causes (alcohol use, iron overload, fatty liver)
If cure not achieved:
- Monitor HCV patients every 6-12 months (LFTs, CBC, INR)
- Those with cirrhosis - recommended screening for esophageal varices
- Advanced fibrosis or cirrhosis (F3-F4) - Screen for HCC via ultrasound every 6 months
Medications:
- Ledispasvir/sofosbuvir (Harvoni)
- Elbasvir/grazoprevir (Zepatier)
- Ombitasvir/paritaprevir/Ritonavir/Dasabuvir (Viekira Pak)
- Ombitasvir/paritaprevir/Ritonavir (Technivie)
- Sofosbuvir/velpatasvir (Epclusa): Combination therapy is required because monotherapy with either agent is not efficacious.
Resources:
- AASLD/IDSA HCV Guidelines: www.hcvguidelines.com
- CDC HCV Recs: www.cdc.gov/hepatitis/hcv
- JFP Vol 64, No 9 Sep 2015
HIV
- Test everyone
- Undetectable = Untransmissable
ART = 2 NRTIs + one of these:
- Boosted PI
- INSTI (preferred)
- NNRTI
Pre-ART:
- Labs:
- HIV Ab
- CD4
- Plasma HIV RNA
- CBC, CMP, UA
- Hepatitis A, B, C
- Lipids
- Genotypic resistance testing
- HLA-B*5701 allele
- G6PD screening
- Assess:
- High risk behaviors
- Substance abuse
- Social support
- Mental illness
- Comorbidities
- Economic factors
- Medical insurance status
- Discussion of risk reduction
Antiretroviral Therapy for HIV (ART) EDIT
Key Recommendations:
- Initiation of ART is recommended as soon as possible after HIV diagnosis, including immediately after diagnosis if the patient is ready to commit to treatment (evidence rating: AIa)
- Structural barriers that delay receipt of ART should be removed to allow newly diagnosed persons to receive ART at the first clinic visit after diagnosis if they and their clinicians determine that this approach is appropriate (evidence rating: AIa)
- Initiation of ART is recommended within 2 weeks of initiation of treatment for most opportunistic infections (evidence rating: AIa), except:
- For individuals with tuberculosis and CD4 cell counts of 50/£gL or above, ART should be initiated within 2 to 8 weeks of initiation of tuberculosis treatment (evidence rating: AIa)
- For individuals with cryptococcal meningitis, ART should be initiated within 4 to 6 weeks after starting antifungal therapy (evidence rating: BIa)
- Initiation of ART is recommended immediately in the setting of a new diagnosis of cancer with attention to drug-drug interactions (evidence rating: BIIa)
References:
- JAMA Oct 202 Vol 324, No 16
- Recommended Initial Antiretroviral Therapy (ART) Regimens
Recommended initial regimens consist of 3 drugs: 2 nucleoside reverse transcriptase inhibitors (nRTIs) and an integrase strand transfer inhibitor (InSTI) or a 2-drug regimen of dolutegravir/lamivudine.
Recommended for Most People With HIV (a)
- Bictegravir/tenofovir alafenamide/emtricitabine (evidence rating: AIa)
- Dolutegravir plus (all evidence ratings: AIa)
- Tenofovir alafenamide/emtricitabine
- Tenofovir disoproxil fumarate/emtricitabine
- Tenofovir disoproxil fumarate/lamivudine
- Dolutegravir/lamivudine with caveats (b) (evidence rating: AIa)
Recommended in the Setting of Opportunistic Infection Treatment
- Dolutegravir (50 mg twice daily), efavirenz (600 mg/d), or raltegravir (800 mg twice daily) plus 2 nucleoside reverse transcription inhibitors is recommended for initial ART in people with HIV who have active tuberculosis and are receiving a rifamycin-based tuberculosis treatment regimen (evidence rating: AIa)
- Bictegravir with rifampin is not recommended due to drug-drug interactions (evidence rating: AIIa)
- Boosted protease inhibitors are recommended only if an integrase strand transfer inhibitor¡Vbased or efavirenz-based regimen is not an option (evidence rating: AIa); if possible, rifabutin (150 mg/d) should be substituted for rifampin in the tuberculosis treatment regimen if a protease inhibitor¡Vbased regimen must be used (evidence rating: BIII)
Recommended During Pregnancy (c)
- Atazanavir/ritonavir (evidence rating: AIIa) (d)
- Darunavir/ritonavir (evidence rating: AIIa) (d)
- Dolutegravir (evidence rating: AIb) (d),(e)
- Efavirenz (evidence rating: BIa) (d)
- Raltegravir (evidence rating: AIIa) (d)
- Rilpivirine (evidence rating: BIIa) (f)
a Listed in alphabetical order by integrase strand transfer inhibitor component. Drug components separated with a virgule indicate these are available as co-formulations.
b Not recommended for rapid start because baseline laboratory evaluation results must be reviewed before initiation. Also not recommended for patients with chronic hepatitis B or HIV RNA level above 500,000 copies/mL, and perhaps a CD4 cell count below 200/£gL, although the latter is unclear. Close monitoring for adherence and virological response is needed. Not recommended for patients being treated for an active opportunistic infection.
c Listed in alphabetical order. Drug components separated with a virgule indicate these are available as co-formulations.
d Combined with either tenofovir disoproxil fumarate/emtricitabine or tenofovir disoproxil fumarate/lamivudine. There are data supporting the use of dolutegravir plus tenofovir alafenamide/emtricitabine during pregnancy (evidence rating: AIb).
e Women who are taking this drug when they become pregnant do not necessarily have to switch ART.
f May be used as a component of the regimen during pregnancy. Abacavir/lamivudine (evidence rating: BIIa) may be used in place of one of the other dual-nucleoside reverse transcription inhibitor components during pregnancy, but data and experience for either are more limited.
References:
- JAMA Oct 202 Vol 324, No 16
- Recommended initial HIV regimens
(Information from FAFP CME and Package inserts)
Single Tablet Regimens
- Biktarvy (bictegravir 50mg/emtricitabine 200mg/tenofovir alafenamide 25mg) by Gilead
- INSTI plus 2 NRTIs
- 1 tablet, 1 time a day, with no food requirements and no booster
- Indications:
- Complete regimen for treatment of HIV-1 in those with no antiretroviral treatment history
- Replace the current ARV regimen in those who are virologically suppressed (HIV-1 RNA <50/mL) on a stable ARV regimen for >3mo with no history of treatment failure and no known resistance to components of Biktarvy
- Cautions and Warnings:
- Do NOT use in those with CrCl <30 mL/min (Renal disease)
- Discontinue if evidence of lactic acidosis or hepatomegaly and steatosis (Liver disease)
- Contraindicated with:
- difetilide
- rifampin
- Most common adverse reactions:
- Diarrhea (6%)
- Nausea (6%)
- Headache (5%)
- Prior to initiation:
- Test for:
- HBV infection
- Renal function
- Urine glucose/protein
- Test for:
- dolutegravir/abacavir/lamivudine (DTG/ABC/3TC)
- INSTI plus 2 NRTIs
- Only for those with a negative HLA-B*5701 allele
- 3TC may be substituted for FTC and vice versa
- No food considerations
- Consider DTG for those in high cardiac risk and those with adherence concerns
- elvitegravir/cobicistat/tenofovir/emtricitabine (EVG/c/tenofovir/FTC)
- Must be taken with food
- TDF: Avoid in those with CKD or osteoporosis
Other Regimens:
- dolutegravir/tenofovir/emtricitabine (DTG plus tenofovir/FTC)
- 3TC may be substituted for FTC and vice versa
- tenofovir as either TAF or TDF.
- TAF has fewer bone and kidney toxicities
- TDF is associated with lower lipid levels
- TDF: Avoid in those with CKD or osteoporosis
- Consider DTG for those in high cardiac risk and those with adherence concerns
- HBV coinfection: Use TAF or TDF with FTC or 3TC
- raltegravir/tenofovir/emtricitabine (RAL plus tenofovir/FTC)
- RAL can be given as 400mg BID or 1200mg once daily
- No food considerations
- TDF: Avoid in those with CKD or osteoporosis
- HBV coinfection: Use TAF or TDF with FTC or 3TC
- Biktarvy (bictegravir 50mg/emtricitabine 200mg/tenofovir alafenamide 25mg) by Gilead
- Recommended ART regimens for treatment-naive patients
Recommended ART regimens for treatment-naive patients with HIV infection are INSTI-based, and are as follows:
- Bictegravir/tenofovir alafenamide/emtricitabine - Brand: Biktarvy
- Test for Hep B infection, GFR, urine glucose
- Dolutegravir/abacavir/lamivudine (only for patients who are HLA-B*5701 negative and do not have chronic hepatitis B (HBV) co-infection) - Brand: Triumeq or Triumeq PD
- Screen HLA-B*5701 before initiating
- Screen integrase strand transfer inhibitor resistance (ISTI)
- Dolutegravir plus either emtricitabine or lamivudine, plus either tenofovir disoproxil fumarate (DF) or tenofovir alafenamide (AF) - Brand: Stribild or Genvoya
- Dolutegravir/lamivudine [3] (only if HIV RNA < 500,000 copies/mL, there is no HBV co-infection, or in cases where ART is started prior to known HIV genotype resistance testing and HBV testing)
For patients with HIV who have used long acting cabotegravir as PrEP, INSTI resistance testing should be done before starting ART.
If ART is started before the genotype test results are known, then the following regimen is recommended:
- Boosted darunivir plus either tenofovir alafenamide or tenofovir disoproxil fumarate, plus either emtricitabine or lamivudine
Reference:
- Bictegravir/tenofovir alafenamide/emtricitabine - Brand: Biktarvy
Opportunistic diseases associated with low CD4 levels
- Candidiasis
- Cryptococcus infection
- Cryptosporidium infection
- Cytomegalovirus infection
- HIV associated neurocognitive disorders
- Herpes simplex virus infections
- Herpes zoster virus infections
- Karposi sarcoma
- Mycobacterium avium complex infection
- Non-Hodgkin lymphoma
- Pneumocystis jirovecii infection
- Progressive multifocal leukoencephalopathy
- Toxoplasmosis infection
- Wasting syndrome
Consultant Apr 2016
Pre Exposure Prophylaxis (PrEP)
Free PrEP for uninsured: https://getyourprep.com
Strong adherence to PrEP is associated with a risk reduction of 90-100%
- Patient Assistance:
- Clinician Consultation Center:
- NC AIDS Trianing and Education Center:
- CDC:
Steps to start PrEP:
- Assess Risk
- Risk for sexual transmission:
- Condomless sex in prior 6mo
- Any STI in past 6mo
- Not in monogamous relationship with HIV-neg partner
- Relationship with HIV-pos partner(s)
- Commercial sex work
- Risk for non-sexual transmission:
- Shared injection equipment
- Known HIV-pos injecting partner(s)
- Recent drug treatment
- Sexually active with injecting partner(s)
- Risk for sexual transmission:
- Determine clinical eligibility
- Within 30d of starting PrEP: Viral hepatitis status and renal function
- Hep B surface antigen and antibody (sAg and sAb) - must be Hep B sAg neg
- Serum creatinine, eCrCl (must be >60mL/min), UA, LFT's
- Within 7d before starting PrEP:
- HIV test using one of these (must be HIV neg):
- HIV RNA
- Antigen/Antibody combination assay
- Rapid test with fingerstick
- Traditional blood test with ELISA and reflex confirmatory testing
- Any symptoms in last 1mo? (Must be free of symptoms in last month)
- Fever
- Fatigue
- Skin rash
- Pharyngitis
- Cervical adenopathy
- HIV test using one of these (must be HIV neg):
- Within 30d of starting PrEP: Viral hepatitis status and renal function
- Other tests to consider
- If not done in last 6-12 mo
- Serum RPR
- NAATs for gonorrhea and chlamydia
- NAAT for Trichomonas vaginalis
- Hep C Ab for those who inject drugs, has sex with an IDU, and MSM
- If not done in last 6-12 mo
- Patient counseling
- Startup syndrome
- Some patients develop mild headaches, nausea, or flatulence, resolves in 1st mo for most
- Notify provider of any unexpected reactions, especially rashes
- Adherence strategies
- Pair pill taking with daily tasks
- Set an alarm, use a pill box, keep extra dose handy, etc
- Anticipatory guidance
- Dose can be safely taken 3-4 hrs before or after dosing time
- No interactions with alcohol or recreational drugs, avoid sex under the influence
- Startup syndrome
- Prescribe, monitor, support
- Fist prescription:
- Truvada, 1 tab by mouth daily, dispense #30, no refills
- Return to clinic in 3-4 weeks: assess adherence, adverse effects, and risk-reduction behaviors
- Subsequent prescriptions:
- Truvada, 1 tab by mouth daily, dispense #30, 2 refills
- Every 3 months
- Repeat HIV testing for all patients
- Assess adherence, adverse effects, and risk-reduction behaviors
- For women: pregnancy test
- Refill only if pt returns for visit and is confirmed HIV neg
- For injection drug users: link to drug treatment services and needle exchange programs
- Every 6 months
- Check Cr and CrCl - Do not use if eCrCl <60
- Check for STIs if not done in interim
- Throat/Rectum/Urethral G/C
- Assess ongoing need for PrEP
- Every 12 months
- UA
- Fist prescription:
ICD10 Codes:
- PrEP
- Z20.6 Contact with and (suspected) exposure to HIV
- Z20.2 Contact with and (suspected) exposure to infections with a predominantly sexual mode of transmission
- Z11.3 Encounter for screening for infections with a predominantly sexual mode of transmission
- Z11.4 Encounter for screening for human immunodeficiency virus
- Z11.59 Encounter for screening for other viral diseases
- Z20.5 Contact with and (suspected) exposure to viral hepatitis
- Z71.7 Encounter for HIV counseling
- PEP
- Z20.6 Contact with and (suspected) exposure to HIV
- Z20.2 Contact with and (suspected) exposure to infections with a predominantly sexual mode of transmission
- Z20.5 Contact with and (suspected) exposure to viral hepatitis
- Z77.21 Contact with and (suspected) exposure to potentially hazardous body fluids
References:
- JFP Vol 65 No 1 Jan 2016
- JAMA Vol 319 No 12 Mar 2018
PrEP and PEP edit
Key Recommendations for the Use of Preexposure Prophylaxis (PrEP) and Postexposure Prophylaxis (PEP)
- PrEP is recommended for individuals at risk for HIV infection (evidence rating: AIa)
- Initiation of PrEP is recommended as soon as feasible for individuals who have chosen to use it (evidence rating: AIII)
- Tenofovir disoproxil fumerate/emtricitabine once daily is recommended for oral PrEP (evidence rating: AIa).
- For men who have sex with men (MSM), a double dose (2 pills) of tenofovir disoproxil fumerate/emtricitabine is recommended on the first day (evidence rating: AIIa)
- For MSM with or at risk for kidney dysfunction, osteopenia, or osteoporosis, daily tenofovir alafenamide/emtricitabine is recommended (evidence rating: BIa)
- Oral PrEP dosing using the 2-1-1 (or on-demand) method is recommended only for MSM (evidence rating: AIa)
- Injectable cabotegravir every 8 weeks (see text for details) is recommended (pending approval by regulatory agencies and availability) as PrEP for cisgender men and transgender women who have sex with men (evidence rating: AIb)a
Recommended Monitoring for Oral PrEP
Prior to Initiation
- Combined HIV antibody and antigen testing (HIV RNA level if clinical suspicion of acute HIV)b (evidence rating: AIa)
- Serum creatinine level (evidence rating: AIIa)
- Hepatitis B surface antigen (evidence rating: AIIa)
- Hepatitis C IgG antibody (if not known to be previously positive; if known positive, hepatitis C virus RNA should be confirmed if not recently known; evidence rating: AIIa)
- Hepatitis A IgG antibody for MSM and people who inject drugs (if not known to be immune; evidence rating: AIIa)
- Genital and nongenital Neisseria gonorrhea and Chlamydia trachomatis testing by nucleic acid amplification test (NAAT) (evidence rating: AIIa)
- Syphilis testing (evidence rating: AIIa)
During PrEP
- At 1 month:
- Combined HIV antibody and antigen test (evidence rating: BIII)
- Quarterly:
- Combined HIV antibody and antigen test (evidence rating: AIa)
- Estimated creatinine clearance rate (at first quarterly visit and annually thereafter; evidence rating: AIIa); every 3 to 6 months for patients with or at risk for kidney injury (evidence rating: BIIa)
- Genital and nongenital N gonorrhea and C trachomatis testing by NAAT (evidence rating: AIIa)
- Syphilis testing (evidence rating: AIIa)
- Pregnancy testing for individuals of childbearing potential (evidence rating: AIIa)
- Annually:
- Combined HIV antibody and antigen test (evidence rating: AIa)
- Estimated creatinine clearance rate (evidence rating: AIIa)
- Hepatitis C virus antibody test (every 3-6 months for people who inject drugs and MSM who use recreational drugs at the time of sex if liver function test results are abnormal) (evidence rating: BIIa)
- For individuals who have ceased PrEP for 7 or more consecutive days, the combined HIV antibody and antigen test is recommended prior to restarting PrEP (evidence rating: BIII)
- In the setting of substantial nonadherence to PrEPc and high-risk exposure, discontinuation of PrEP and initiation of a 28-day course of 3-drug PEP is recommended (evidence rating: CIII)
- Use of exogenous estrogens or androgen blockers by transfeminine persons may result in a reduction of approximately 30% in tenofovir/tenofovir metabolite concentrations and reduced protection is possible; additional measures to support maximal adherence to daily dosing is recommended (evidence rating: BIII)
For PEP
- A 3-drug ART regimen is recommended for PEP within the first 24 hours (ideally) to 72 hours after an exposure and continued for 28 days (evidence rating: BIIa)
- In the event of HIV acquisition while receiving PrEP, a transition to a dolutegravir-, bictegravir-, or ritonavir-boosted darunavir¡Vbased regimen is recommended initially (evidence rating: AIIb), which can be subsequently tailored according to clinical resistance test results
References:
- JAMA Oct 202 Vol 324, No 16
HIV PrEP
Florida PrEP: Call 1-850-245-4422 for more information about Florida's PrEP Drug Assistance program and participating health department clinics.
PrEP Telemedicine: https://files.hiv.gov/s3fs-public/2023-11/PAP-CAP-Resources-for-Accessing-PrEP-telemedicine.pdf
To find out whether your health plan covers PrEP medications without charge:
- If you have private health insurance through your employer or have purchased it yourself: Check with your health insurance company about coverage for PrEP medications, or look on their drug formulary (drug list) online to find information about coverage for the drugs approved for PrEP.
- If you purchased your health plan through HealthCare.gov or a state-based Marketplace: This NASTAD tip sheetExit Disclaimer can help you verify whether your plan covers PrEP medications.
- If you are on Medicaid: Check with your benefits counselor.
- If you are on Medicare: Find which plans cover your drugs.
- If you are eligible to receive care through the Indian Health Service (IHS): PrEP services are available with no out-of-pocket costs at IHS health centers most tribal health clinics. For more information, visit IHS.gov.
- If you are eligible to receive care from Veterans Programs: PrEP is available for Veterans who use VA for their health care. For information, visit myhealth.VA.gov.
Reference:
ICD10 for PrEP and PEP edit
PrEP
- Z20.6 Contact with and (suspected) exposure to HIV
- Z20.2 Contact with and (suspected) exposure to infections with a predominantly sexual mode of transmission
- Z11.3 Encounter for screening for infections with a predominantly sexual mode of transmission
- Z11.4 Encounter for screening for human immunodeficiency virus
- Z11.59 Encounter for screening for other viral diseases
- Z20.5 Contact with and (suspected) exposure to viral hepatitis
- Z71.7 Encounter for HIV counseling
PEP
- Z20.6 Contact with and (suspected) exposure to HIV
- Z20.2 Contact with and (suspected) exposure to infections with a predominantly sexual mode of transmission
- Z20.5 Contact with and (suspected) exposure to viral hepatitis
- Z77.21 Contact with and (suspected) exposure to potentially hazardous body fluids
Reference:
H. pylori
Per ACG: In adults who are not previously treated:
- 14 days of optimized bismuth quadruple therapy
- Proton pump inhibitor, twice daily
- Bismuth subcitrate, 120 to 300 mg, four times daily or Bismuth subsalicylate 300 mg 4 times daily
- tetracycline, 500 mg, four times daily (NOT doxycycline)
- metronidazole, 500 mg, three or four times daily
Reference:
- AFP Mar 2025 Vol 111 No 3
Immunizations and Vaccines
Insect Repellents
| Repellent | Brand Name | Formulation | Duration against | Duration against |
|---|---|---|---|---|
| Mosquitoes | Ticks | |||
| DEET | Cutter Skinsations | 7% pump spray | 1-3 hrs | 6hrs |
| Off Deep Woods III | 25% aerosol spray | 8hrs | 5hrs | |
| Ultrathon* | 34% lotion | 12hrs | NA | |
| Picaridin | Cutter Advanced | 5.75% wipes | 8hrs | 5hrs |
| Natrapel 8hour* | 20% pump spray | 8hrs | 8hrs | |
| IR3535 | Avon Skin So Soft | 7.5% lotion | 2hrs | 2hrs |
| Bug Guard Plus IR3535 | ||||
| Coleman Skin Smart* | 20% pump spray | 8hrs | 8hrs | |
| Oil of lemon eucalyptus | Repel Lemon Eucalyptus* | 30% pump spray | 7-8hrs | 7hrs |
| Permethrin | Sawyer Premium | 0.5% pump spray | ||
| Permethrin Clothing | ||||
| Repel Permethrin | 0.5% aerosol spray | |||
| Clothing and Gear |
*'s indicate my personal preference
Notes:
- Ultrathon formulation developed for US Military
- Picaridin 19.2% prevented mosquito bites as effectively as long-acting 33% DEET used by US Military per a field study
- Multiple studies found 7.5% IR3535 to be ineffective (Concentrations >10% are effective)
- Citronella oil protects against mosquitoes not ticks for 1.5 to 5 hours
- CDC considers EPA-registered formulations of DEET, picaridin, IR3535, and OLE safe for use during pregnancy
For use with sunscreens:
- Use repellent after sunscreen.
- DEET has been shown to reduce the SPF but applying after DEET could increase absorption of DEET
See also: Skin Protection
Reference:
- JAMA Vol 316 No 7 Aug 2016
Insects
Hymenoptera
Medically Relevant Hymenoptera in the USA
- Fire ants
- Honeybee, bublebee
- Hornet
- Wasp
- Yellow jacket
References:
- AFP Aug 2022 Vol 106 No 2
Arthropods
Medically Relevant Biting Arthropods in the USA
- Bed bugs (no associated vector borne diseases)
- Biting midges
- Mansonellosis (Africa and tropical Americas)
- Brown recluse spider (no associated vector borne diseases)
- Fleas
- Cat scratch fever
- flea-borne (murine) typhus
- plague
- Horseflies and Deer flies
- Anthrax
- loiasis
- tularemia
- Mites and Chiggers
- Rickettsialpox
- Scrub typhus (Asia-Pacific region)
- Mosquitoes
- Japanese encephalitis
- lymphatic filariasis
- malaria
- West Nile virus
- St Louis encephalitis
- Western equine encephalitis
- Venezuelan equine encephalitis
- Ross River virus
- Rift valley fever virus
- dengue
- yellow fever
- chikungunya
- zika
- Sandliess
- Leismaniasis
- Sanfly fever
- Bartonellosis
- Papataci fever (three day fever)
- Ticks
- Lyme disease
- Rocky Mountain spotted fever
- Rickettsia disease
- Anapalasmosis
- ehrlichiosis
- babesiosis
- Colorado tick fever
- tickborne relapsing fever
- tularemia
- Widow spiders (no associated vector borne diseases)
References:
- AFP Aug 2022 Vol 106 No 2
Patient Messaging
It could be bed bug. Here is information on getting rid of bed bugs:
Monkeypox
Member of Orthopoxvirus genus in the family Poxviridae
Transmitted is through:
- Direct skin to skin contact with infectious lesions
- Contact with materials used by a person with monkeypox including clothing, bedding, or sex toys may lead to transmission
- It is NOT transmitted through casual contact
Incubation period:
- Mean: 7.6 days from exposure to first symptom
- 95% develop symptoms within 17.1 days
Prodrome:
- flulike illness with fever, malaise, headaceh, and fatigue
- Commonly also Lymphadenopathy
After prodrome:
- Rash
- Lesions as macules that progress to papules, vesicles, and then pustules before scabbing
- In current (2022) outbreask:
- anorectal pain, proctitis with bleeding, and penile edema with balanitis and phimosis
- Sore throat, odynophagia, epiglottitis, and tonsilitis as well
Most individuals, monkeypox is not life-threatening. Complications include:
- pneumonia
- encephalitis
- eye infections (usually in <8yo, immunocompromised, and pregnant women)
Management
- Maintain in isolation for duration of illness (usually 2-4 weeks)
- Symptomatic
- tecovirimat (antiviral for smallpox) is available via expanded access Investigational New Drug protocol
- Recommended for those with severe disease and those with 1 or more complications
Vaccines:
- 2 vaccine options
- JYNNEOS
- Vaccine Biden admin is working to increase availability of
- FDA approved for smallpox and monkeypox
- Live attenuated vaccinia virus incapable of replicating
- 2 dose series
- 85% effective at preventing monkeypox
- Can be administered as post exposure prophylaxis
- If within 4 days of exposure, can prevent disease
- If within up to 2 weeks, can reduce symptom severity
- ACAM2000
- Live vaccinia virus capable of replicating
- 1 dose
- 85% effective at preventing monkeypox
- Associated with unexpectedly high rate of myocarditis and pericarditis
- Can be administered as post exposure prophylaxis
- If within 4 days of exposure, can prevent disease
- If within up to 2 weeks, can reduce symptom severity
- JYNNEOS
Preventing spread
- Health care
- Low risk
- Workers should wear a gown, gloves, eye protection, and N95 mask
- Patients with possible monkeypox should be masked immediately, have lesions covered with gown or sheet, and placed i isolation in single person room
- Persons with monkeypox should
- Avoid close contact with others until skin lesions are completely healed (several weeks)
- Individuals already infected should not be prioritized for vaccination (possible immunity)
Reference:
- JAMA Vol 328 No 10 Sep 2022
Otitis Externa
- Prescribe topical antibiotics for uncomplicated otitis externa, reserving systemic agents for infection extending outside the ear canal, necrotizing otitis externa, or patients who are immunodeficient. LOE C
- Avoid clearing cerumen if a patient is asymptomatic and advise patients/parents on Do's and Don'ts for ear wax accumulation. LOE C
- Consider flooding the ear canal with xylocaine, alcohol, or mineral oil before attempting insect removal. LOE C
References:
- JFP Jul 2020 Vol 69, No 6
Paronychia Home Care Instructions
Acute paronychia:
If you have been diagnosed with paronychia, which is an infection or inflammation of the skin around your fingernail or toenail, here are some important steps to help you manage it at home and know when to seek further care:
For Acute Paronychia (recent onset, usually less than 6 weeks):
- Warm Soaks: Soak the affected finger or toe in warm water for 15-20 minutes, 3-4 times a day. This helps reduce swelling and pain, and can encourage drainage if there is any pus.
- Keep the Area Clean and Dry: After soaking, gently dry the area. Avoid picking at the nail or cuticle.
- Topical Treatments: If the swelling and redness do not improve after a few days of soaks, we could try a topical antibiotic cream
- Abscess (Pus Collection): If you notice a pocket of pus, or if the area becomes very swollen, painful, or red, you may need a minor procedure to drain the pus. This is usually done in a clinic and helps the infection heal faster. I recommend avoiding, though if we are able to.
- Oral Antibiotics: Most people do not need oral antibiotics unless the infection is severe, spreading, or if you have a weakened immune system. Let me know if it worsens.
- Pain Relief: Over-the-counter pain relievers like acetaminophen 1000 mg every 4 hours or ibuprofen 400 mg every 4 hours can help with pain/discomfort.
Prevention Tips:
- Avoid biting or picking at your nails and cuticles.
- Keep nails trimmed and clean.
- Wear gloves when working with water or chemicals.
- Moisturize your hands regularly.
Chronic paronychia:
If you have been diagnosed with paronychia, which is an infection or inflammation of the skin around your fingernail or toenail, here are some important steps to help you manage it at home and know when to seek further care:
For Chronic Paronychia (lasting more than 6 weeks):
- Avoid Irritants: Chronic paronychia is often caused by repeated exposure to water, soaps, or chemicals. Try to keep your hands dry and wear gloves when doing wet work or using cleaning products.
- Topical Steroids: We could use a steroid cream or ointment to reduce inflammation. This is often more effective than antifungal medications, even if yeast is present.
- Moisturize: Use a gentle, fragrance-free moisturizer on your hands and nails to help restore the skin barrier.
- Antifungal Creams: Sometimes, a topical antifungal may be recommended if there is evidence of a yeast infection.
- Patience: Chronic paronychia can take weeks to months to fully heal, even with proper treatment.
Let me know:
- If the redness, swelling, or pain gets worse or spreads up the finger or toe.
- If you develop a fever or feel generally unwell.
- If you see pus that does not drain on its own.
Prevention Tips:
- Avoid biting or picking at your nails and cuticles.
- Keep nails trimmed and clean.
- Wear gloves when working with water or chemicals.
- Moisturize your hands regularly.
References:
- Acute and Chronic Paronychia. Leggit JC. American Family Physician. 2017;96(1):44-51.
- Acute and Chronic Paronychia. Rigopoulos D, Larios G, Gregoriou S, Alevizos A. American Family Physician. 2008;77(3):339-46.
- Acute and Chronic Paronychia. Rockwell PG. American Family Physician. 2001;63(6):1113-6.
- Acute and Chronic Paronychia of the Hand. Shafritz AB, Coppage JM. The Journal of the American Academy of Orthopaedic Surgeons. 2014;22(3):165-74. https://doi.org/10.5435/JAAOS-22-03-165.
- Common Acute Hand Infections. Clark DC. American Family Physician. 2003;68(11):2167-76.
- Homogenization of the Management of Acute Paronychia With Abscess Formation Within the Context of an Evaluation of Professional Practices. Matter-Parrat V, Lazarus P, Goldammer F, et al. Orthopaedics & Traumatology, Surgery & Research : OTSR. 2021;107(5):102982. https://doi.org/10.1016/j.otsr.2021.102982.
- Topical Steroids Versus Systemic Antifungals in the Treatment of Chronic Paronychia: An Open, Randomized Double-Blind and Double Dummy Study. Tosti A, Piraccini BM, Ghetti E, Colombo MD. Journal of the American Academy of Dermatology. 2002;47(1):73-6. https://doi.org/10.1067/mjd.2002.122191.
Pet Related Diseases
- Parasitic
- Toxoplasmosis -
- Ingestion of oocysts in soil/fomites, undercooked meat
- Visceral larva migrans
- Ingestion of Toxocara spp eggs in soil or feces
- Ocular larva migrans
- Ingestion of Toxocara spp eggs in soil or feces
- Cutaneous larva migrans
- Skin contact with soil
- Cystic echinococcosis
- Ingestion of animal feves containing Echinococcus eggs
- Alveolar echinococcosis
- Ingestion of animal feves containing Echinococcus eggs
- Dipylidiasis
- Ingestion of infected fleas
- Cryptosporidiosis
- Contact with infected pet feces (dog, cat, ferret, rodent)
- Giardiasis
- Contact with infected pet feces (dog, cat, ferret, rodent) -
- Toxoplasmosis -
- Fungal
- Tinea corporis/capitis
- Physical contact/petting
- Tinea corporis/capitis
- Bacterial
- Campylobacteriosis
- Ingestion through contact
- Salmonellosis
- Ingestion through contact
- Cat-scratch
- Scratch or bite
- Psittacosis
- Inhalation of bird droppings or nasal secretions
- Leptospirosis
- Contact with infected dogs
- MRSA
- Contact with infected animal
- Lyme
- Ticks from pet
- Plague
- Contact with infected cats
- Tularemia
- Ticks, contact with infected cats
- Fish Tank granuloma
- Contact with fish aquarium
- Campylobacteriosis
- Arthropod
- Scabies
- Contact
- Scabies
- Viral
- Rabies
- Bites, scratches
- Lymphocytic choriomeningitis
- Petting, kissing animal (guinea pigs, other rodents)
- Monkeypox
- Direct contact with infected rodents
- Rabies
AFP Vol 76 No 9 Nov 2007
Dog and Cat Zoonotic Infections in USA
| Disease | Organism | Cat | Dog | Transmission Mode |
|---|---|---|---|---|
| Arthropod-borne | Anaplasma phagocytophilum | Y | Y | Bite from an arthropod that |
| shared by pets and people | Ehrlichia spp. | Y | Y | previously fed on an |
| Leishmania infantum | Y | Y | infected animal. | |
| Rickettsia spp. | Y | Y | ||
| Bartonellosis | Bartonella henselae | Y | N | Cat scratch |
| Enteric | Campylobacter spp. | Y | N | Ingestion after contact with |
| Escherichia coli | Y | N | feces | |
| Salmonella spp. | Y | N | ||
| Giardiasis | Giardia spp. | Y | Y | Ingestion after contact with |
| feces | ||||
| Influenza | Influenza A virus | Y | Y | Direct contact with aerosols |
| from infected animals | ||||
| Leptospirosis | Leptospira spp. | N | Y | Direct contact with infected |
| urine | ||||
| MRSA | Staphylococcus spp. | Y | Y | Direct contact with infected |
| wounds | ||||
| Ocular and visceral larva | Toxocara spp. | Y | Y | Ingestion after contact with |
| migrans | infected feces | |||
| Plague | Yersinia pestis | Y | N | Direct contact with secretions |
| or flea transmitted | ||||
| Rabies | Rabies virus | Y | Y | Bite |
| Ringworm | Dermatophytes | Y | Y | Direct contact with cutaneous |
| lesions | ||||
| Toxoplasmosis | Toxoplasma gondii | Y | N | Ingestion after contact with |
| infected fees | ||||
| Tularemia | Francisella tularensis | Y | N | Direct contact with secretions |
| or arthropod transmitted |
AFP Vol 93 No5 Mar 2016
Pharyngitis
- Modified Centor Decision Rule
| Criteria | Points |
|---|---|
| Absence of cough | 1 |
| Swollen, tender ant cervical LA | 1 |
| Temp >100.4F | 1 |
| Tonisllar exudate | 1 |
| Age: | |
| 3-14yo | 1 |
| 15-44yo | 0 |
| >45 | -1 |
| Score | Risk | Next step |
|---|---|---|
| 0 | 1-2.5% | No further testing or Antibioics |
| 1 | 5-10% | No further testing or antibiotics |
| 2 | 11-17% | Throat culture or rapid antigen testing |
| Treat if positive | ||
| 3 | 28-35% | Throat culture or rapid antigen testing |
| Treat if positive | ||
| 4 | 51-53% | Consider empiric antibiotics |
(Table modified as I think there was an editorial error in the table information)
Recommended antibiotics for GABHS Pharyngitis:
- 5 days of 800 mg penicillin 4 times a day is non inferior to 10 days of 1000 mg PCN tid
First Line
| Medication | Duration | Cost |
|---|---|---|
| Amoxicillin | 10 d | $4 |
| Pen G benz | 1 dose | Varies |
| Pen V | 10 d | $5 |
For Type IV PCN reaction
| Medication | Duration | Cost |
|---|---|---|
| Cephalexin | 10d | $4 |
For Type I PCN reaction
| Medication | Duration | Cost |
|---|---|---|
| Azithromycin | 5d | $10 |
| Clarithromycin | 10d | $23 |
| Clindamycin | 10d | $17 |
References:
- AFP Vol 94 No 1 2016
- AFP Vol 101 No 7 Apr 2020
Pneumonia (Community Acquired)
Management for Outpatients:
- Without comorbidities:
- Most effective oral treatment for community-acquired pneumonia is levofloxacin
- Amoxicillin or doxycycline (SR - Strong Recommendation)
- Alt: Macrolide monotherapy (Azithromycin or clarithromycin)
- With comorbidities (chronic heart, lung, liver, renal disease, diabetes, alcoholism, malignancy, asplenia):
- Amoxicillin/clavulanate or cephalosporin plus a macrolide (SR)
- Amoxicillin/clavulanate or doxycyclnie
- Alt: Monotherapy with fluoroquinolone (Levaquin) for 5-7 days
No evidence that corticosteroids improve outcomes in mild to mod CAP
References:
- JAMA Mar 2020 Vol 323, No 9
- AFP Jul 2025 Vol 112 No 1
Postexposure Doxycycline to Prevent Bacterial Sexually Transmitted Infections edit
Background
- Interventions to reduce sexually transmitted infections (STIs) among men who have sex with men (MSM) are needed.
Methods
- We conducted an open-label, randomized study involving MSM and transgender women who were taking preexposure prophylaxis (PrEP) against human immunodeficiency virus (HIV) infection (PrEP cohort) or living with HIV infection (persons living with HIV infection [PLWH] cohort) and who had had Neisseria gonorrhoeae (gonorrhea), Chlamydia trachomatis (chlamydia), or syphilis in the past year.
- Participants were randomly assigned in a 2:1 ratio to take 200 mg of doxycycline within 72 hours after condomless sex (doxycycline postexposure prophylaxis) or receive standard care without doxycycline.
- STI testing was performed quarterly.
- The primary end point was the incidence of at least one STI per follow-up quarter.
Results
- Of 501 participants (327 in the PrEP cohort and 174 in the PLWH cohort), 67% were White, 7% Black, 11% Asian or Pacific Islander, and 30% Hispanic or Latino.
- In the PrEP cohort, an STI was diagnosed in 61 of 570 quarterly visits (10.7%) in the doxycycline group and 82 of 257 quarterly visits (31.9%) in the standard-care group, for an absolute difference of −21.2 percentage points and a relative risk of 0.34 (95% confidence interval [CI], 0.24 to 0.46; P<0.001).
- In the PLWH cohort, an STI was diagnosed in 36 of 305 quarterly visits (11.8%) in the doxycycline group and 39 of 128 quarterly visits (30.5%) in the standard-care group, for an absolute difference of −18.7 percentage points and a relative risk of 0.38 (95% CI, 0.24 to 0.60; P<0.001).
- The incidences of the three evaluated STIs were lower with doxycycline than with standard care; in the PrEP cohort, the relative risks were 0.45 (95% CI, 0.32 to 0.65) for gonorrhea, 0.12 (95% CI, 0.05 to 0.25) for chlamydia, and 0.13 (95% CI, 0.03 to 0.59) for syphilis, and in the PLWH cohort, the relative risks were 0.43 (95% CI, 0.26 to 0.71), 0.26 (95% CI, 0.12 to 0.57), and 0.23 (95% CI, 0.04 to 1.29), respectively.
- Five grade 3 adverse events and no serious adverse events were attributed to doxycycline. Of the participants with gonorrhea culture available, tetracycline-resistant gonorrhea occurred in 5 of 13 in the doxycycline groups and 2 of 16 in the standard-care groups.
Conclusions
- The combined incidence of gonorrhea, chlamydia, and syphilis was lower by two thirds with doxycycline postexposure prophylaxis than with standard care, a finding that supports its use among MSM with recent bacterial STIs. (Funded by the National Institutes of Health; DoxyPEP ClinicalTrials.gov number, NCT03980223. opens in new tab.)
Reference:
- Luetkemeyer AF, Donnell D, Dombrowski JC, Cohen S, Grabow C, Brown CE, Malinski C, Perkins R, Nasser M, Lopez C, Vittinghoff E, Buchbinder SP, Scott H, Charlebois ED, Havlir DV, Soge OO, Celum C; DoxyPEP Study Team. Postexposure Doxycycline to Prevent Bacterial Sexually Transmitted Infections. N Engl J Med. 2023 Apr 6;388(14):1296-1306. doi: 10.1056/NEJMoa2211934. PMID: 37018493; PMCID: PMC10140182.
- https://www.nejm.org/doi/full/10.1056/NEJMoa2211934
Post Infectious Cough
This cough is expected to last for only one or two weeks, but persists for more than 3 weeks and up to many months.
PPC is reported to 11–25% of all cases of chronic cough.
Persistent tickling or irritating sensation in the throat which leads to paroxysms of coughing.
PPC is stimulated by cigarette smoke, chemical fumes, aerosol sprays, dust, perfumes, drinking, eating, talking, laughing, and breathing cold air.
Study:
- The first group received a jam-like paste consisting of 500 g of honey and 70 g of original instant coffee (honey coffee, HC).
- This means that each person took 20.8 g of honey and 2.9 g of coffee three times daily.
Findings:
- Take 1 tablespoon of honey (21 g) mixed with half teaspoon (3 g) of instant coffee, in a glass (200 ml) of warm water, 3 times a day, for at least 1 week.
Procalcitonin
| Pro-calc (ug/L) | Recommendation |
|---|---|
| <0.10 | Bact infection highly unlikely |
| Strongly recommend AGAINST antibiotics | |
| 0.10-<0.25 | Bact inftection unlikely |
| Recommend against antibiotics | |
| 0.25 - 0.50 | Bacterial inftection likely |
| Recommend antibiotics | |
| >0.50 | Bacterial infection very likely |
| Strongly recommend antibiotics |
Recommend discontinuation of antibiotics when levels decreased by 80-90% or <0.25ug/L
References:
- AFP Vol 94 No 1 2016
- AFP Vol 92, No 7 Oct 2015
Red flags in a child with diarrhea
- Decreased tearing, sunken eyes, decreased urine output dry mucous membranes
- Fever >100.4 in <3mo
- Fever >102.2 in children 3-36mo
- Frequent and substantial episodes of diarrhea
- H/o prematurity, chronic medical conditions, accompanying illness
- Mental status changes
- Persistent vomiting
- Poor response to oral rehydration or inability to rehydrate
- Visible blood in stool
- Young (<6mo) or low body weight
References:
- AFP Vol 85 No 11 Jun 2012
Scabies
Treatment:
- Benzyl benzoatate 25% - More effective than permethrin 5% with number needed to treat = 2
- Permethrin 5% cream (first line)
- Ivermictin 1% cream
- Ivermictin pill 200mcg/Kg single or double dose
References:
- JFP Vol 69, No 1 Jan/Feb 2020
- AFP Jul 2025 Vol 112 No 1
Sepsis
Notes:
- Pneumonia is most common etiology
- Fever is most common manifestation
Overall Approach:
- Airway and respiratory stabilization
- Sepsis bundle (within first 3 hours)
- Fluid resuscitation
- IV Crystalloid (LR or NS) at 30 mL/Kg within first 3 hrs
- Infuse 1 L bolus over first 30 min, followed by repeat bolus infusions
- Enhances preload and cardiac output -> O2 delivery
- Frequent assessment of fluid balance
- Dynamic BP response
- Tissue perfusion (lactate clearance)
- Urine output (should be 0.5 mL/Kg/hr or more)
- Restrict in later phases of sepsis management
- At 72 hours - net balance goal is 0 to negative
- Antibiotics
- Start broad and empirical antibiotics within 3 hours based on suspected infection site
- 7 to 10 days is sufficient for most infections associated with sepsis
- Lactate measurement (See below)
- Cultures (See below)
- Fluid resuscitation
- Vasopressor therapy if hypotensive despite fluid resuscitation
- Restore mean arterial pressure (MAP) to 65 mmHg or more
- Infuse vasopressors through central venous catheter with dynamic BP measurements through an arterial line
- Medications:
- Norepinephrine should be initiated at 2 to 5 mcg/min and titrated up to 35 to 90 per min to achieve MAP >65 mmHg
- Vasopressin (up to 0.03 units/min) can be added as second line
- Epinephrine (20-50 mcg/min) if needed
- Infection source control
Laboratory testing:
- CBC with dif
- BMP
- Lactate
- An indirect marker of tissue perfusion
- > 18 mg/dL (2mmol per L) is diagnostic for septic shock in Sepsis-3
- Measure every 4-6 hours until levels have normalized
- Procalcitonin
- Marker for inflammation produced by cytokines and bacterial endotoxins
- < 0.05 ng/mL is normal
- < 0.25 ng/mL is low likelihood of bacterial sepsis
- Levels rise within 4 hours after onset of an infection and peak at 12 to 48 hrs
- LFT
- Coagulation studies
- Urinalysis
- Art or Venous blood sampling for Acid-base
- 2 sets of peripheral blood cultures, and urine, stool, sputum, and skin cultures
Imaging:
- CXR
- Additional as indicated
Other:
- Blood Products
- PRBCs only when Hg is <7 g/dL
- Platelets when <10 regardless of bleeding risk, <20 when bleeding risk is significant - goal is platelets >50
- Corticosteroids
- Hydrocortisone 200 mg/day is recommended for septic shock not responsive to vasopressor therapy and fluid resuscitation
- Glycemic control
- Insulin recommended when 2 consecutive glucose >180 mg/dL
- Monitor glucose every 1 to 2 hours then every 4 hours once stable
- Nutrition
- Enteral nutrition should be used instead of parenteral nutrition
- Dextrose infusion should be administered over the first 7 days
- Sodium bicarbonate therapy
- Not recommended in patients with hypoperfusion-induced lactic acidemia with a pH >7.15
Reference:
- AFP Vol 101 No 7 Apr 2020
SIRS Criteria
SIRS defined as 2 or more of:
- Temp >100.4 F or <96.8 F
- Heart rate >90 bpm
- Resp rate >20 breaths/min or
- WBC >12 or <4 or >10% immature forms
Reference:
- AFP Vol 101 No 7 Apr 2020
qSOFA (Quick Sequential Organ Failure Assessment)
2 out 3:
- Respiratory rate of >22 breaths/min
- Altered mental status
- Systolic BP <100 mmHg
Reference:
- AFP Vol 101 No 7 Apr 2020
Sepsis NEWS score
- Respiration rate
- Oxygen saturation
- Systolic blood pressure
- Pulse rate
- Level of consciousness
- Temperature
5 or more, think Sepsis
Tick Borne Diseases
- Lyme disease
- Lyme disease is caused by a bacterium called Borrelia burgdorferi. In the southeastern U.S. the black-legged tick transmits the disease. About 15–20 cases are reported each year in people who were exposed in Florida.
- SYMPTOMS: Most people, though not all, will get a red "bull's eye" rash three to 30 days after being bitten by an infected tick. This rash does not always appear at the site of the bite, and may occur on another part of the body. Other symptoms can include fever, headache, chills, fatigue, stiff neck or muscle aches. If you do not treat the infection, it can spread to joints, the heart and the nervous system.
- Rocky Mountain spotted fever
- Rocky Mountain spotted fever (RMSF) is a serious disease caused by the bacterium Rickettsia rickettsii. The main type of tick that carries RMSF in this area is the American dog tick. About 10–15 cases are reported each year in people who were exposed in Florida.
- SYMPTOMS: Symptoms usually begin 5 to 10 days after a tick bite, and can include fever, headache, vomiting, muscle aches, and lack of appetite. A rash may appear 2–5 days or longer after symptoms first begin. The rash is often seen on the arms, legs, hands and feet, but not everyone who is infected will see a rash. Later signs include stomach pain, joint pain, and diarrhea. Three to five percent of cases may die from the disease.
- Ehrlichiosis/anaplasmosis
- Ehrlichiosis and anaplasmosis are tickborne diseases that infect blood cells. Ehrlichiosis is spread by the lone star tick. The black-legged tick carries anaplasmosis. Ehrlichiosis is more common in Florida. Each year there are about 15–25 cases in people who were exposed in Florida.
- SYMPTOMS: Symptoms of both diseases usually begin 5 to 10 days after a tick bite, and can include fever, headache, fatigue, and muscle aches. Other signs include cough, nausea, vomiting, joint pain, diarrhea, and confusion. A rash can be present, but is not common.
- Other tick-borne diseases
- Other tick-borne diseases may also be in Florida. If you have a tick bite and become ill, you should call your doctor.
People treated with antibiotics early after becoming ill usually get better quickly. Those who find out they have a tick-borne disease later on are more likely to have severe symptoms. People with severe illness caused by RMSF, ehrlichiosis, or anaplasmosis can die from the disease. If you are sick, you should tell your doctor about any recent tick bites or exposure to ticks or tick habitats. Fortunately, most tick bites do not make people ill. Treatment is not recommended unless a person starts to show signs of illness.
Prevention:
- Apply repellent to help prevent ticks from attaching to your skin. EPA registered repellents containing DEET (N,N-diethylmeta-toluamide, or N,N-diethyl-3-methylbenzamide), picaridin or IR3535 can give you several hours of protection.
- Repellents with permethrin can be used on clothing, shoes, tents and gear. You should not put permethrin directly on the skin. Always follow product instructions when applying repellent!
- Dress so your skin is covered in white or light-colored clothing when you are in an area where ticks might be present. This will help you see if any ticks are crawling on your clothes. Tuck your pants legs into your socks so that ticks cannot crawl up the inside of your pants.
- Walk in the center of the trail or path to avoid touching plants in tick-infested areas.
- Check your body and your child's body for ticks after spending time in a place where ticks are likely to be found. Look carefully at your feet and legs, as some ticks are small enough to crawl into shoes and through socks.
- Check your pets for ticks.Talk to your veterinarian about products that keep ticks off your pets. Be sure to follow package directions and keep your pet under the care of a vet.
- Prevent tick infestations around your home by landscaping your yard to be a tick-free zone. For details on how you can control ticks around the home, visit http://www.cdc.gov.
Reference:
Patient Messaging: Tick bites
The adult female Lone Star Tick displays a white spot near the center of her back while the male has white streaks or spots along the margin on the top side of its body. They are found throughout most of Florida and the Southeastern United States with populations spreading to the Midwest and the Northeast.The adult female Lone Star Tick displays a white spot near the center of her back while the male has white streaks or spots along the margin on the top side of its body. They are found throughout most of Florida and the Southeastern United States with populations spreading to the Midwest and the Northeast.
Lone Star Ticks are known to carry several pathogens including Rickettsiosis, Ehrlichiosis and Tularemia. They have also been said, by some scientists, to be carriers of Southern Tick Associated Rash Illness (STARI).
The lone star tick is the most common tick reported to bite humans in the southeastern and southcentral US (Masters et al. 2008). Various pathogens have been shown to enter the tick by blood feeding; however, most are not transmitted because the tick is not a competent vector (Goddard and Varela-Stokes 2009). An unknown pathogen has been implicated in causing Southern tick-associated rash illness (STARI) in humans, but etiology, pathogenicity and identification are pending (CDC 2011a). Several pathogens are known to be transmitted by the lone star tick and given the proper circumstances they may manifest into disease. These include ehrlichiosis, rickettsiosis, tularemia and protozoan infections. The causative agents of ehrlichiosis, rickettsiosis, and anaplasmosis are all tick-borne bacterial infections that are readily treatable in humans, but the causative agent can be difficult to determine because the similarities among the pathogens.
Recently, in three case studies, including one specifically identified as a result of a bite by a lone star tick, tick bites may have been involved in producing or generating an immune response that caused a food allergy to red meat proteins (Wolver et al. 2009). Heavy infestations of lone star ticks also have been associated with increased mortality in white-tailed deer fawns in Oklahoma (Bolte et al. 1970).
Do you have any symptoms of illness?
While these ticks are vectors for some diseases, they are not good at doing it so the current recommendations are to treat those who show signs of illness such as rash, fever, nausea, vomiting, muscle pains, etc
Reference:
Traveler's Diarrhea
Treatment:
- Ciprofloxacin 500 mg bid x3 days
Check resistance of area and cautions
| Drug | Dose |
|---|---|
| Bismuth subsalicylate | 2 tabs qid |
| Ofloxacin | 300mg qd |
| Norfloxacin | 400mg qd |
| Ciprofloxacin | 500mg qd |
| Levofloxacin | 500mg qd |
| Rifamiximin | 200mg bid to 600mg qd |
References:
- FP Essentials #370
Tropical Diseases from geographic areas
| Area | Most common |
|---|---|
| Caribbean | Dengue, malaria |
| Central America | Dengue, malaria (mostly P vivax) |
| South America | Dengue, malaria (mostly P vivax) |
| South Central Asia | Dengue, enteric, malaria (mostly non-P falciparum) |
| Southeast Asia | Dengue, malaria (mostly non-P falciparum) |
| Sub-Sahara Africa | Malaria (mostly P falciparum), tick-borne rickettsiae, acute schistosomiasis, filiriasis |
References:
- AFP Vol 88, No 8 Oct 15, 2013
Uncomplicated Cystitis (UTI)
See also:
Recommended first-line antimicrobials by IDSA:
- Nitrofurantoin 100mg twice a day for 5 days
- Avoid if early pyelonephritis is suspected and those with low creatinine clearance
- Trimethoprim-sulfamethoxazole 160/800 mg twice a day for 3 days
- Avoid if resistance prevalence is known to exceed 20% or if used for UTI in last 3mo
- Fosfomycin 3g single dose
- Lower efficacy than some other agents, avoid if early pyelonephritis is suspected
Recurrent UTIs:
- Probiotics reduce the likelihood of recurrent UTIs of women with frequent UTIs
- Those containing lactobacillus
- Vaginal probiotics outperform oral probiotics alone
References:
- Consultant Aug 2017
- AFP Jul 2025 Vol 112 No 1
Waterborne Illnesses
Per CDC estimates, the five most common waterborne illnesses in the US are:
- Otitis externa or "swimmer's ear": A bacterial infection that typically occurs when water stays in the outer ear canal for too long. Although more prevalent among children, anyone can get swimmer's ear. It's not contagious.
- Norovirus: A highly contagious virus that spreads through contaminated food or water — it's considered both a foodborne and waterborne illness. It often spreads when an infected person handles food without washing their hands first.
- Giardiasis: A waterborne illness triggered by the microscopic parasite Giardia duodenalis. Giardia parasites spreads by being ingested in contaminated water or food. After infection, the parasite lives in the intestines and can be passed through fecal matter.
- Cryptosporidiosis: Cryptosporidium, often called “Crypto,” is a microscopic parasite that causes the diarrheal disease cryptosporidiosis. The primary symptom of a Cryptosporidium infection is watery diarrhea. Other symptoms include stomach cramps or pain, dehydration, nausea, vomiting, fever, and weight loss. It can be spread through drinking contaminated water or coming in contact with contaminated fecal matter.
- Campylobacteriosis: An illness caused by the bacteria Campylobacter, and the most common bacterial cause of diarrheal illness in the United States. Campylobacter spreads mainly through consumption of raw or undercooked poultry, or foods that have been in contact with raw poultry. It can also be transmitted through other foods, contact with infected animals, and untreated water.
Reference:
Wounds
WOUND CLASSIFICATION
- Acute wound: a wound which occurs suddenly and progresses through the stages of healing as expected
- Chronic wound: a wound which fails to progress or progresses slowly through the stages of healing. Healing can be greater than 4-6 weeks.
- Surgical wound: a wound which is secondary to surgical intervention e.g. scalpel incision, surgical drain
- Non-surgical wound: an acute or chronic wound which is not secondary to surgical intervention
Tissue is usually described by colour.
- Epithelial tissue: Appears pink or pearly white and wrinkles when touched. Occurs in the final stage of healing when the wound is covered by healthy epithelium.
- Granulating tissue: Appears red and moist. Occurs when healthy tissue is formed in the remodelling phase that is well vascularised and bleeds easily.
- Slough tissue: Appears yellow, brown or grey. Slough is devitalised tissue made of dead cells or debris.
- Necrotic tissue: Appears hard, dry and black. Necrotic tissue is dead tissue that prevents wound healing.
- Hyper granulating tissue: Appears red, uneven or granular. Occurs in the proliferative phase when tissue is over grown.
Inflammation is an essential part of wound healing; however, infection causes tissue damage and impedes wound healing.
- Contamination: The presence of microorganisms that are contained and do not multiply. It does not provoke a host response so healing is not impaired. Antimicrobials are not indicated.
- Colonisation: Microorganisms multiply but do not provoke a host response. The infection is contained but wound healing may be delayed. Antimicrobials are not indicated.
- Local infection: Invasion by an agent that, under favourable conditions, multiplies and produces effects that are injurious to the patient. When microorganisms and bacteria move into the wound tissue and invokes a host response. Healing is impaired and can lead to wound breakdown. Topical antimicrobials are indicated.
- Spreading and systemic infection: Microorganisms spread from the wound through the vascular and or lymphatic systems and involves either a part of the body (spreading) or the whole body (systemic). Healing is impaired. A systemic approach is needed e.g. topical antimicrobials and the use of antibiotics to prevent sepsis.
- Biofilms: represent a survival mechanism of microorganisms and are therefore ubiquitous in nature. They are complex, slime-encased communities of microbes which are often seen as slime layers on objects in water or at water-air interfaces. The degree of bioburden in the wound from the microorganisms is indicated by a poor response to antimicrobial or antibiotic treatment, delayed wound healing or increase in exudate or inflammation.
Wound healing may be by:
- Primary intention: the wound edges can be pulled together e.g. surgical incision (using sutures, staples, steristrips or glue), small wounds, paper cuts
- Secondary intention: the wound edges don't come together and need dressing products to promote granulation
- Tertiary intention/ delayed primary intention: the wound is cleaned before it can be closed due to a high risk of infection e.g. contaminated wounds
- Negative pressure wound therapy: Topical negative pressure or vacuum assisted closure (VAC) is a foam dressing attached to a device to assist with wound closure, proliferation, moisture removal and stabilisation of the wound environment. Typically used in open or dehisced wounds, grafts, flaps or pressure injuries.
Causes of ulceration
- Vascular (venous, arterial, lymphatic, vasculitis)
- Neuropathic (for example, diabetes, spina bifida, leprosy)
- Metabolic (for example, diabetes, gout)
- Connective tissue disease (for example, rheumatoid arthritis, scleroderma, systemic lupus erythematosus)
- Pyoderma gangrenosum (often reflection of systemic disorder)
- Haematological disease (red blood cell disorders (for example, sickle cell disease); white blood cell disorders (for example, leukaemia); platelet disorders (for example, thrombocytosis))
- Dysproteinaemias (for example, cryoglobulinaemia, amyloidosis)
- Immunodeficiency (for example, HIV, immunosuppressive therapy)
- Neoplastic (for example, basal cell carcinoma, squamous cell carcinoma, metastatic disease)
- Infectious (bacterial, fungal, viral)
- Panniculitis (for example, necrobiosis lipoidica)
- Traumatic (for example, pressure ulcer, radiation damage)
- Iatrogenic (for example, drugs)
- Factitious (self harm, "dermatitis artefacta")
- Others (for example, sarcoidosis)
| Lab Investigation | Rationale |
|---|---|
| Haemoglobin | Anaemia may delay healing |
| White cell count | Infection |
| Platelet count | Thrombocytopenia |
| Erythrocyte sedimentation rate; C reactive protein | Non-specific markers of infection and inflammation; useful in diagnosis and monitoring treatment of infectious or inflammatory ulceration |
| Urea and creatinine | High urea impairs wound healing. Renal function important when using antibiotics |
| Albumin | Protein loss delays healing |
| Glucose, haemoglobin A1C | Diabetes mellitus |
| Markers of autoimmune disease (such as rheumatoid factor, antinuclear antibodies, anticardiolipin antibodies, lupus anticoagulant) | Indicative of rheumatoid disease, systemic lupus erythematosus, and other connective tissue disorders |
| Cryoglobulins, cryofibrinogens, prothrombin time, partial thromboplastin time | Haematological disease |
| Deficiency or defect of antithrombin III, protein C, protein S, factor V Leiden | Vascular thrombosis |
| Haemoglobinopathy screen | Sickle cell anaemia, thalassaemia |
| HIV status | Kaposi's sarcoma |
| Serum protein electrophoresis; Bence-Jones proteins | Myeloma |
| Urine analysis | Useful in connective tissue disease |
| Wound swab | Not routine; all ulcers colonised (not the same as infection); swab only when clinical signs of infection |
| Edges | Type of ulcer |
|---|---|
| Sloping | Venous ulcer |
| Punched out | Arterial or vasculitic ulcer |
| Rolled | Basal cell carcinoma |
| Everted | Squamous cell carcinoma |
| Undermining | Tuberculosis, syphilis |
| Purple | Vasculitic (such as pyoderma gangrenosum) |
| Site | Type of ulcer |
|---|---|
| Gaiter area of the leg | Venous ulcer |
| Sacrum, greater trochanter, heel | Pressure ulcer |
| Dorsum of the foot | Arterial or vasculitic ulcer |
| Shin | Necrobiosis lipoidica |
| Lateral malleolus | Venous, arterial, or pressure ulcer or hydroxyurea induced ulceration |
| Plantar and lateral aspect of foot and toes | Diabetic ulcer |
| Sun exposed areas | Basal cell carcinoma; squamous cell carcinoma |
Wound Exudate
- Wound exudate may be serous, serosanguinous, or sanguinous
- The quantity of exudate is usually classified as heavy (
+(dressing soaked)), medium (+ (dressing wet)), or minimal ((dressing dry)) - Excessive exudate may be due to wound infection or gross oedema in the wound area and may complicate wound healing
- The exudate should be controlled with the use of dressings appropriate for the level of exudate and any infection treated
- Barrier films applied to the surrounding skin help to prevent further maceration (see the ninth article in the series)
- The oedematous leg should be raised when the patient is seated
Clinical features of non-healing wounds
- Absence of healthy granulation tissue - Lack of adequate blood supply
- Failure of re-epithelialisation
- Presence of necrotic and unhealthy tissue in the wound bed - Cyclical or persistent pain
- Recurrent breakdown of wound
- Clinical or subclinical infection
- Excess exudate and slough
References:
- https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Wound_assessment_and_management/
- Grey JE, Enoch S, Harding KG. Wound assessment. BMJ. 2006 Feb 4;332(7536):285-8. doi: 10.1136/bmj.332.7536.285. PMID: 16455730; PMCID: PMC1360405.
Ways to prevent wounds
Principles of preventive sand care include:
- Avoid positioning patient over an area of erythema.
- Keep the skin clean and dry.
- Do not massage or vigorously rub skin that is risk for pressure injury.
- Develop an individualized continence plan.
- Protect the skin from exposure to excessive moisture and friction.
- Careful patient positioning
- Use of protective devices
- Judicial use of supportive surfaces
Study: Upper Respiratory Tract Infection edit
Upper respiratory tract infection (URI) is a general term for a heterogeneous group of illnesses caused by numerous etiologic agents that affect the mucosal lining of the upper respiratory tract, including the middle-ear cavity and paranasal sinuses. URIs are primarily caused by viruses, rhinoviruses being the most common etiological agents. Respiratory viruses transmit easily via direct contact or aerosols. The incidence of URI is highest in children who suffer 6–8 infections per year. The main symptoms of URI are nasal blockage and discharge, sneezing, sore throat, and cough. Fever occurs variably, most commonly in children. Viral URIs often predispose to bacterial complications. Acute otitis media is the most common complication in children, whereas sinusitis and pneumonia are more frequent in adults and the elderly. The treatment of URI is mainly symptomatic because specific antivirals are available only for influenza viruses. Antibiotics have no efficacy for viral URI but are commonly used for treating acute otitis media and sinusitis. Most URIs are self-limited illnesses with an average duration of 7–10 days and an excellent prognosis.
Young children suffer on average 6–8 and adults 2–4 URIs per year. The occurrence of URI displays a clear seasonal variation. The highest incidence rates are observed in the autumn and winter in temperate regions of the northern hemisphere. In tropical countries, most URIs occur during the rainy season.
On an annual level, rhinoviruses are estimated to account for approximately 30–50% of all respiratory illnesses, but this percentage may rise to 80% during the autumn peak season.
The treatment of URI is largely symptomatic and aimed at relieving the most unpleasant symptoms of the illness. Nasal stuffiness can be effectively reduced with intranasally or orally administered decongestants. First-generation (but not second-generation) antihistamines reduce sneezing and nasal discharge. This effect is probably more likely due to the anticholinergic rather than the antihistamine features of these drugs. Locally administered ipratropium has also been shown to reduce nasal discharge. Nonsteroidal anti-inflammatory drugs reduce fever and soreness of the throat. Cough medications are commonly used but their efficacy has not been demonstrated convincingly. Despite corticosteroids being potent anti-inflammatory agents, their intranasal or oral use has not resulted in any clinical benefits. The use of intranasal steroids in children during rhinovirus infection may even increase the risk of AOM. Data on the efficacy of zinc, vitamin C, or echinacea extracts in the treatment of URI are inconclusive. Although it is well known that antibiotics are not effective against viruses and that unnecessary use of antibiotics increases bacterial resistance, antibiotics are frequently used in the treatment of uncomplicated URIs. Specific antiviral treatments for respiratory viruses are currently available only for influenza viruses (oseltamivir, zanamivir, amantadine, and rimantadine). However, antiviral drugs for some other respiratory viruses (e.g., RSV, rhinoviruses, enteroviruses) are currently being developed.
Reference:
- Heikkinen T, Ruuskanen O. UPPER RESPIRATORY TRACT INFECTION. Encyclopedia of Respiratory Medicine. 2006:385–8. doi: 10.1016/B0-12-370879-6/00416-6. Epub 2006 May 13. PMCID: PMC7204877.
Misc Medicine
Animals:
2024 Anchor Imaging edit
| SimonMed Imaging | Orlando Diagnostic Center | |
|---|---|---|
| Agreement | Self-Pay | |
| MRI/MRA w & w/o contrast | 425 | 300 |
| MRA / MRI w/o contrast | 325 | 250 |
| MRI/MRA w/ contrast | 375 | |
| Breast MRI | 525 | |
| CT/CTA w/o contrast | 215 | 200 |
| CT/CTA w & w /o contrast | 275 | 250 |
| CT/CTA w/ contrast | 230 | |
| CT Lung Screen | 150 | |
| CCTA | 450 (Longwood only) | |
| CCTA w/Calcium score | 500 (Longwood only) | |
| Mammo screening | 180 | |
| Mammo DX unilateral | 150 | |
| Mammo DX bilateral | 200 | |
| PETSkull to midthigh (excludes axumin, netspot, amyvid and vizamyl ) | 1,795 | |
| PET Whole Body (excludes axumin, netspot, amyvid and vizamyl ) | 1,930 | |
| Ultrasound w/ Elastography | 130 | |
| Ultrasound pelvic TA & TV (w/or w/o Doppler) | 300 | |
| Whole Breast / Breast Ultrasound (per slide) | 115 | |
| CT Cardiac Score | 99 | 99 (Longwood only) |
| Ultrasound | 115 | 125 |
| Echocardiogram | 235 | 240 |
| Dexa Scan | 75 | 80 |
| Xray (excludes fluroscopy exams; each body part) | 40 | 30 |
25 Most Common Diagnoses
- Hypertension
- Hyperlipidemia
- Diabetes
- Back pain
- Anxiety
- Obesity
- Allergic rhinitis
- Reflux esophagitis
- Respiratory problems
- Hypothyroidism
- Visual refractive errors
- General medical exam
- Osteoarthritis
- Fibromyalgia / myositis
- Malaise and fatigue
- Pain in joint
- Acute laryngopharyngitis
- Acute maxillary sinusitis
- Major depressive disorder
- Acute bronchitis
- Asthma
- Depressive disorder
- Nail fungus
- Coronary atherosclerosis
- Urinary tract infection
AAFP Online Help edit
- Google Search: afp:
- AAFP Algorithms
- AAFP Videos
- AAFP Handouts
Advanced Directives
A Florida advance directive is a combination of forms used to outline an individual's health care plans and identify an agent to act in their best interests in the event they can no longer speak for themselves. Also, it outlines end-of-life medical requests and organ donation.
Once signed, with at least two (2) witnesses, it may be used immediately.
Advance Directives Include:
- Living Will – Set out life-ending treatment options.
- Health Care Surrogate Form – A 'medical power of attorney' electing someone to handle healthcare-related needs.
- Do Not Resuscitate Form (DNR) – Used to inform medical personnel NOT to perform life-saving procedures.
- Donor Form – List organ donation preferences.
- Wallet Card – To have in the chance of an emergency.
Art and Philosophy of Medicine
10 practical ways to boost your EQ
- Clarify your intention for the day
- Practice self-care
- Perform an emotional checkup
- Pause before responding to emotional situations
- Be curious instead of making assumptions
- Be open about mistakes and weaknesses
- Pay attention to your environment
- Build relationships by making time for those around you
- Be accountable, and apologize when needed
- Start and end your workday with a positive ritual
References:
- Fam Pract Manag. 2018 Jan-Feb;25(1):11-14.
Art of Caring
Florence Nightingale's Notes on Nursing
- Observe the sick.
- Never let a patient be waked out of his sleep.
- Avoid unnecessary noise: Whisper outside the room.
- View and sunlight are matters of first importance to the sick.
- Leading questions are useless or misleading.
- Obtain accurate information
- Be confidential.
- Children are much more susceptible than grown people to noxious Influences.
Medical statements:
Quotes from forgotten sources:
- The difference you will make as a physician is in making the common problems rare
- The good physicians are never as good as they could be
- The average physician is worse than he appears to be
- At the end of the day, it is outcomes that matter
Rounds presentation
This is a [age] yo [gender] with a h/o [major hx ->ab, sx, pert ob/gyn hx] who presented on [date] with [major symptoms -> pelvic pain, fever, etc] and found to have [working dx].
[Tests done] showed [results]. Yesterday the pt [state inpatient changes, new plan, new tx/med/tests].
This AM the pt feels [state pt words].
The physical exam is significant for [state major findings].
The plan is…
Rules of Considerate Conduct for Healers
- Pay attention
- Acknowledge others
- Think the best
- Listen
- Be inclusive
- Speak kindly
- Do not speak ill
- Accept and give praise
- Respect even a subtle "no"
- Respect others' opinions
- Mind your body
- Be agreeable
- Keep it down (and rediescover silence)
- Respect other people's time
- Respect other people's spae
- Apologize earnestly
- Assert yourself
- Avoid (unnecessary) personal questions
- Care for your guests
- Be a considerate guest
- Think twice before asking for favors
- Refrain from idle complaints
- Accept and give constructive criticism
- Respect the environment and be gentle to animals
- Don't shift responsibility and blame
25 rules collected from Richard Colgan, MD and published in Consultant Apr 2016
See also: http://www.advicetotheyoungphysician.com
Tips for faster chart completion
- Let go of perfection. The EHR can be a minefield for perfectionists and compulsive "box-checkers." Not all boxes need checking, and not all categories need filling on every visit. Know which ones do, and leave the rest alone.
- Forget the opus. The clinical note serves as neither biography nor ethnography. Be brief and focused. In the plan section of the note, be clear and concise enough that the next person looking at your note will be able to understand your clinical reasoning and follow the plan.
References:
- Fam Pract Manag. 2016 Mar-Apr;23(2):40.
Benefits of a dog edit
- Physical Activity
- More than 50% of annual (preventable) deaths result from adverse lifestyle choices, with poor diet and physical inactivity being the most important
- dog ownership resulted in a 4 times greater chance of meeting these physical activity guidelines compared with people without a dog
- Owning a dog, with its walking obligation, is strongly associated with a lower risk of cardiovascular conditions and death (hazard ratio=0.77, 95% confidence interval=0.73-0.80)
- Allergies and Autoimmune Diseases
- Children living on farms, especially those younger than 5 years old, who are exposed to bacteria in barns, animal feed, manure, and mud are much less likely to develop allergies or autoimmune diseases compared to nonrural children.
- This "farming effect" is evident throughout the world and appears to protect children from asthma (odds ratio=0.48, 95% confidence interval=0.31-0.76) and allergic diseases.
- And if the child does not live on a farm, exposure to innocuous microbes that protect against allergic diseases is also obtained by having a dog at home and playing outside in the dirt. Dogs share numerous favorable microorganisms on their coats and mouth with children.
- Mental Health
- Loneliness and social isolation are significantly associated with a 50% increased risk of dementia, 29% increased risk of heart disease, 32% increased risk of stroke, and a greater risk of all causes of premature death.
- Dog ownership does reduce depression and has positive effects on well-being in certain subgroups, including single individuals, women, homeless kids, older individuals who suffer a loss of spouse or divorce, elderly women, and people who are more attached to their dog
References:
- Robinson LA. Dog Ownership Is the Best Preventive 'Medicine' for Patients. Am J Med. 2021 Jun;134(6):710-712. doi: 10.1016/j.amjmed.2021.01.033. Epub 2021 Feb 21. PMID: 33621539.
Biostatistics
Definitions:
- Sensitivity: (Sn) - % of patients with the disease who have a POS test for the disease
- Specificity: (Sp) - % of patients without the disease who have a NEG test for the disease
- Pre/Post test probability: Probability of disease before/after a test is performed
- Likelihood ratio: (LR) - LR>1 indicates increased likelihood of disease. The most helpful tests have a ratio less than 0.2 or over 5.
- Control Event Rate: (CER) - #events/#control group
- Experimental Event Rate: (EER) - #events/#exp group
- Relative Risk: (RR) - EER/CER
- Relative risk reduction: (RRR) - The % difference in risk or outcomes between treatment and control groups. Ex: If mortality is 30% in controls and 20% with treatment - RRR=(30-20)/30=33%
- Absolute risk reduction: (ARR) - Arithmetic difference in risk or outcomes between treatment and control groups. Ex: If mortality is 30% in controls and 20% with treatment - ARR=(30-20)=10%
- Number needed to treat: Number of patients who need to receive an intervention instead of the alt in order for 1 additional patient to benefit. NNT=1/ARR; If ARR is 4% -> NNT=1/4%=1/0.04=25
- 95% confidence interval: An estimate of certainty. It is 95% certain that the tru value lies within the given range. A narrow CI is good - if CI spans 1.0 makes the results seem questionable.
Clinical significance is best assessed using ARR and NNT rather than RRR. RRR can exaggerate perceptions and be misleading:
- Consider a drug, that reduces mortality from 40 to 30% if taken for 1 year.
- RRR is 25%
- [(40-30)/40]*100
- ARR is 10%
- 40-30
- NNT is 10 for 1 year
- 1/ARR -> 1/10% -> 1/0.10 = 10 people
- RRR is 25%
- Consider a drug with a lower baseline risk of dying (reduces mortality from 1.00 to 0.75% if taken for 1yr)
- RRR is 25%
- [(1.00-0.75)/1.00]*100
- ARR is only 0.25%
- 1.00-0.75
- NNT is 400
- 1/ARR -> 1/0.25% -> 1/0.0025 = 400
- RRR is 25%
NNT can also be determined with Patient Expected Event Rate (PEER - might be prevalence in some cases) (if known or estimated) and Odds Ratio:
- NNT = (1 - [PEER × (1–OR)]) / ((1 - PEER) × PEER × (1–OR))
Reference:
- AFP Vol 82 No 1 Jul 2010
- https://ebmh.bmj.com/content/ebmental/13/4/g1.full.pdf
Key Concepts When Looking At Research Studies
- Bias
- Confounding variables bias. These are characteristics that are distributed differently among study groups and that can affect the outcome being assessed.
- Exclusion bias. Excluding patients in whom the study drug has already failed biases the study in favor of that drug. If these patients had been included (e.g., a random sample of patients), the response rate to the study drug would have been less than observed.
- History bias. Controlling for temporal trends in disease incidence is important when doing a comparison between contemporary and historical groups.
- Industry bias. This refers to the fact that studies and reviews published by industry are more likely to present positive (favorable) outcomes. Look for non–industry-sponsored studies—they are less likely to have publication bias or use inappropriate comparisons.
- Interrupted time series design bias. Studies with an interrupted time series design, also known as "before and after" studies, are subject to numerous potential confounders because of uncontrolled changes that occur in the study environment over time.
- Lack of placebo bias. Failure to use a true placebo may jeopardize the validity of the results of a trial. In one study, parents who got an empty syringe knew their child was not getting treatment and may have been biased toward a more negative interpretation when they answered follow-up questions regarding their child's cough and sleep quality. Almost anything will look better than placebo. A study should compare the study drug with a real-world scenario, such as (in the case of another study) increasing the dose, switching antidepressants, or using another drug for augmentation.
- Lead-time bias is an important consideration when evaluating a screening intervention. Diagnosing disease earlier with a screening test can appear to prolong survival without actually changing outcomes. The only thing that changes is the period of time during which the patient is diagnosed with the disease, not the actual survival time.
- Observation bias (also known as the Hawthorne effect) occurs when individuals temporarily modify their behavior (and consequently change study outcomes) when they know they are being observed. Gains achieved during the study period often regress when the study ends.
- Open-label study bias occurs when patients' or researchers' knowledge of the condition or treatment can influence their judgment. An example is when a researcher is adjudicating an outcome, and knows which treatment group a patient was assigned to. A stronger study is blinded for patients, researchers, and, if used, evaluators.
- Publication bias. Studies that show treatments in a positive light are more likely to be submitted for publication. For example, the published studies on levalbuterol look good. But if you look at all of the studies submitted to the U.S. Food and Drug Administration, levalbuterol and albuterol are equivalent, and albuterol costs less. Negative studies are less likely to get published than positive studies, and this results in the overwhelmingly positive nature of the literature. Even when negative studies are published, they are less likely to receive the attention by the media and medical establishment that positive studies do. In addition, more and more information is being hidden in online supplemental protocol information or in appendices.
- Review bias occurs when the reader of a test (e.g., radiologist, electrocardiographer) knows the patient's history. The history may change the way a test is read.
- Run-in bias. Run-in periods to assess compliance and ensure treatment responsiveness create a bias in favor of the treatment in question, and yield results in a patient population that will not be the same as in your patients. Thus, the results of these studies may not be generalizable.
- Sampling bias. Representative inclusion of all possible study participants helps to eliminate differences between groups so that more appropriate comparisons can be made. If only some subsets of patients are included (i.e., "sampled"), they are less likely to represent the general population.
- Selection bias occurs when the patients in a study are not representative of the patients you see in practice.
- Spectrum bias occurs when the group being studied is either sicker or not as sick as the patients you see in your practice. A diagnostic test can perform differently in dissimilar patient populations. You cannot apply a test standardized in an inpatient population to your outpatient population (or vice versa) and expect it to have the same sensitivity and specificity.
- Straw man comparison bias. In head-to-head treatment trials, watch out for the straw man comparison. For example, make sure that an article that evaluates treatments uses equipotent dosages of the drugs being compared. Obviously, if you use an adequate dose of a study drug and a suboptimal comparison, the study drug is going to win. In one study, the doses of prasugrel and clopidogrel were not equivalent. As a corollary, a placebo-controlled trial should not typically change your practice; any drug comparison should be against a known effective therapy, if one exists.
- Verification bias or workup bias exists when not everyone in a study gets the definitive, criterion standard test. This generally makes the new test look better because real cases of disease are missed when patients with a negative new test are sent home.
- Causation
- Causation vs. association. A risk factor and outcome are associated if they occur together. Case-control studies can suggest an association, but not causation. Causation is more difficult to establish and generally requires a prospective randomized study.
- Case-control studies may not be able to control for all patient variables. This is a potential source of error. A good example of this would be case-control studies that suggested that postmenopausal estrogen was cardioprotective. Subsequent randomized controlled trials proved that this is not the case.
- An association does not confer causation. But when multiple criteria are met (e.g., strength of association, consistency, specificity, temporality, dose-response relationship, biologic plausibility, coherence, experimental evidence, analogy), the likelihood of a causal relationship increases.
- Hill's criteria for causation (listed above) are a broadly accepted set of nine criteria to establish causality between an exposure or incidence and an effect or consequence. In general, the more criteria that are met, the more likely the relationship is causal.
- Reverse causation. A reverse causality error occurs when the outcome, or some component of it, causes the intervention or exposure in question. For example, in nonrandomized studies, participants may select their "intervention" behavior based on early symptoms or prior knowledge, which then may affect the outcome in question.
- Industry "Spin"
- Watch for "spins" promoted by pharmaceutical salespersons. Testimonials, isolated experiences, small company-sponsored studies with surrogate markers or "fuzzy" end points, and selected reprints are often used to try to convince physicians to use a certain drug or intervention.
- Be skeptical of industry-sponsored studies. These studies are often "spun" to favor the sponsor's drug.
- NNT and NNH
- The number needed to treat (NNT), number needed to harm (NNH), and the magnitude of the benefit are critical information if you are going to make an educated decision about treatment options. NNT and NNH are powerful tools in documenting an intervention's effect.
- Whenever you see an NNT, look for the corresponding NNH.
- Calculate NNT and NNH. They tell you the real magnitude of benefit and harm. P values only tell you that there is a difference between two groups; this difference can be clinically meaningless. NNT gives a better sense of the strength of treatment effect.
- How to calculate NNT or NNH: 1/(absolute difference in treated vs. untreated patients). For example, if 5% of treated patients have a heart attack and 10% of untreated patients have a heart attack, the NNT calculation is 1/(0.10 − 0.05), equals 1/0.05, equals 100/5, equals 20. Ignoring percent signs, the calculation simplifies to 100/absolute difference, equals 100/10 − 5, equals 100/5, equals 20.
- Let your patients know the magnitude of benefit and risk in language that is easy for them to understand. For instance, in one study, 33 patients need to be treated for one year to prevent one hospitalization, at a risk of one in 41 patients developing pneumonia.
- Large numbers of patients are typically required to demonstrate a deleterious side effect of a drug or intervention (i.e., the NNH).
- Noninferiority
- Noninferiority trials are designed to show that an alternative treatment is not substantially worse than the standard intervention. They do not meet the same rigorous design and statistical format of traditional superiority trials.
- Showing that one drug is noninferior to another does not mean that these drugs are equivalent.
- Authors of noninferiority trials must declare a margin of how far outside the acceptable outcome the treatment can perform and still be considered noninferior to the standard treatment.
- The noninferiority margin allows researchers to choose their own benchmark for what is considered a clinically significant difference between two drugs. This can lead to a drug being called noninferior when other researchers not associated with the study would call it inferior.
- The efficacy of the standard treatment (for instance, warfarin) shown in the trials that established its efficacy must be preserved in any noninferiority trials. In a study comparing warfarin and rivaroxaban, time in therapeutic range was not within established norms for many of the patients—this would make warfarin perform worse and allow rivaroxaban to appear noninferior.
- Odds Ratio / Relative Risk
- An odds ratio tells us the odds of an outcome in one group compared with another group, but does not give us the magnitude of this changed outcome. It is usually used in case-control studies and not in randomized trials, where relative risk and absolute risk are used instead.
- Case-control studies are not interventional studies and are retrospective, so we use odds ratio rather than relative risk as a measure of the association. Odds ratio is calculated by dividing the odds of disease in those who were exposed to a given factor by the odds of disease in those who were not exposed.
- Relative risk is the ratio of the probability of an event in an exposed population to the probability in an unexposed population. This calculation is useful in comparisons in which there is a low probability of the event occurring.
- Attributable risk is the difference in the rate of an event between an exposed population and an unexposed population. This is usually calculated in cohort studies.
- Patient-Oriented Evidence Vs. Disease-Oriented Evidence
- Remember the difference between disease-oriented evidence (DOE) and patient-oriented evidence that matters (POEMs).
- POEMs refers to clinical outcomes that mean something to patients (e.g., death, fracture, myocardial infarction). DOE is an indirect measure of a pathologic or physiologic process that may or may not correlate with clinical outcomes (such as changes in blood glucose, electrocardiogram abnormalities, carotid intima thickening). Family physicians should concentrate on POEMs because it has a direct influence on patients' health.
- A lot of studies use surrogate markers as outcomes (e.g., fasting or postprandial blood glucose, FEV1). These are DOEs. What we care about are POEMs (e.g., stroke rates, myocardial infarction rates, quality of life). Be wary of DOEs; they are surrogate markers of disease and may or may not correlate with important clinical end points, such as morbidity and mortality. For example, in certain clinical situations, it is possible to lower blood pressure, but not help patients. It could even harm them.
- A study should change your practice only if it is applicable to your patient population (e.g., study patients presented to a family physician or the emergency department, not a subspecialist).
- Statistical Significance Vs. Clinical Significance
- Recognize that end points can be statistically significant without being clinically significant (e.g., A1C difference of 0.08%). Another example: in one study, 23 mg of donepezil was statistically better than 10 mg, but only in one of three tests, and by only two points on a 100-point scale. This is clinically imperceptible, yet it will be touted as superior by pharmaceutical companies.
- When reviewing a study, you must know what the scale measures, whether the scale has been validated, and what change in the scale is actually clinically significant.
- Study Interpretation
- Absolute risk reduction quantifies the actual difference between two outcomes; this is what the physician should be interested in. Relative risk reduction demonstrates the change in outcome relative to a baseline or control; it will often exaggerate a benefit.
- Abstracts of articles should not be relied on when deciding whether a therapy is good, because they often have misleading information and conclusions. The data and conclusion in the abstract of an article may not be the same as the data in the paper. If you read only the abstract, you may be misled.
- Blinding is ensuring that participants, clinicians, and/or investigators do not know which participants are assigned to each study group. Using seemingly identical products (in terms of taste, appearance, odor, and even texture) with the same dosing regimen is a common practice to help achieve blinding.
- Clinical scoring systems should be externally validated ("road tested") before widespread implementation.
- Dates of the study. Look at the dates that data were generated and not the date of publication. If the data are old, updates in technology and treatments may affect the outcomes.
- "Double-dummy" design is used when the two drugs being tested look different from each other, so that group assignment cannot be blinded. In a double-dummy design, there are matching placebos for both administered drugs (two "dummy" drugs) and every patient gets an active drug and a placebo.
- Durability of an intervention (i.e., the ability to provide sustained results) is an important concept when considering implementing the intervention based on a study's results.
- Efficacy is how a test or drug performs in a study setting. Effectiveness is how it performs in the general population. Usually, results are better for efficacy than for effectiveness.
- External validity refers to the ability to generalize the results of a study to other settings. The demonstrated efficacy of a drug or intervention in a clinical trial may not translate to effectiveness in the community or in your particular practice. Check to see if the population in the study is similar to the population you see in your practice. For example, the average age of patients in a certain study was 77 years. These findings should only be generalized to younger patients with caution.
- Internal validity means you have evidence that what you did in the study (i.e., the treatment) caused what you observed (i.e., the outcome). Internal validity can be threatened by confounding variables.
- Kappa is a measure of interobserver reliability (e.g., the probability that two radiologists reading the same film will get the same answer beyond chance alone). It is generally scored as: 0 = no agreement; 0 to 0.2 = slight agreement; 0.2 to 0.4 = fair agreement; 0.4 to 0.6 = moderate agreement; 0.6 to 0.8 = substantial agreement; and 0.8 to 1.0 = almost perfect agreement. Although in such a study, which would be more or less methodologically sound, a better strategy would have been to have two readers read each film, then have a third party adjudicate if the first two readers disagreed. This is generally accepted methodology.
- Logistic regression attempts to control for confounders between the experimental groups or participants. However, it is at best inexact and cannot control for every potential confounder.
- Multiple comparisons. As the number of comparisons increases, it becomes more likely that the groups being compared will appear to differ in at least one attribute, if only by chance alone.
- Observational studies are not the best design for testing some hypotheses. If we really wanted to know how good electrocardiography is, for example, we would design a study in which initial electrocardiography was performed in the emergency department, followed by cardiac catheterization in all of the patients. This is the only way to get the true sensitivity and specificity of electrocardiography. Observational studies let things take their course without a prescribed, randomized intervention. This adds a lot of uncertainty to the data (in this hypothetical case) by not controlling the subsequent workup.
- Post hoc cutoff values are often selected to maximize the sensitivity and specificity of a test. The test may not perform as well in another group of patients. Receiver operating characteristic curves are used to figure out the cutoff values to achieve optimal sensitivity vs. specificity.
- Post-marketing monitoring is often required to find a difference in adverse outcomes that are associated with the drugs.
- Power of a study is the probability of finding a real difference when one exists, and is based on the minimum number of participants needed to show a difference, the size of the treatment effect desired, and a predetermined level of significance. When you have fewer events in a study than you expect, you need to increase the number of participants, not decrease it.
- Prevalence of a disease in a population changes the interpretation of a test (i.e., the positive and negative predictive values).
- Retraction Watch (http://www.retractionwatch.com) is a blog about retractions in the scientific literature. There is currently no database that catalogs retractions.
- Type II (falsely negative) errors often occur when a study is too small to find a real difference between two treatments. A type I error occurs when the study shows a difference when in fact there is none (falsely positive).
- True- And False-Positive/Negative Study Results
- All tests follow a Bayesian model. They are more likely to be true-positive in a sick patient and false-positive in a well patient.
- Sensitivity and specificity only tell part of the story. Always look at the false-positive and false-negative rates of a test.
- False-positive studies. How many patients who really don't have the disease are you treating simply because the test was positive? One study showed that 42% of low-risk patients had a positive result on chest computed tomography, but no evidence of pulmonary embolism on any confirmatory test. If the chest computed tomography result had been accepted as valid, a significant number of these patients would have been needlessly exposed to anticoagulation.
- False-negative studies. How many patients with true disease are you missing and not treating because the test was negative?
- Types Of Study Analysis
- Intention-to-treat analysis. This type of analysis evaluates all patients in the group to which they were assigned, whether or not they completed the study. Thus, persons who didn't tolerate a treatment, for example, are still analyzed in their original group. This reflects our real-world experience. Some of our patients are going to do badly or stop a medication. They still need to be included in our equation when we decide whether to use a drug. This gives a more realistic sense of the treatment's effectiveness efficacy, and reduces bias that would otherwise make the treatment look better than it actually is. Make sure that a study protocol makes sense. Don't assume that a study uses an appropriate dose or schedule of a drug.
- Per-protocol analysis allows the researcher to throw out any data from patients who don't tolerate a drug (for example). So a per-protocol analysis may not reflect the kind of results we will see in our practice and typically overestimates the net benefit of an intervention. Avoid basing your clinical decisions on articles that use per-protocol analysis.
- Post hoc and subgroup analyses should only be used to generate a hypothesis (the derivation set). This hypothesis then needs to be tested in a separate randomized study (the validation set), and should not be used to show the harm or benefit of a therapy.
- Power analysis ensures that there are enough participants enrolled in a study to find a difference, if there is one. This avoids a type II error, which is when there are not enough participants to find a difference, producing a false-negative result.
- Sensitivity analysis excludes outliers, such as large, heavily weighted studies and studies of marginal quality, to check whether the results are the same.
Reference:
PICOTS for the Trial:
PICOTS is an acronym similar to PICO used in evidenced-based medicine and represents the following:
- (P) for patient population
- (I) for the intervention of interest
- (C) for comparative intervention
- (O) for the outcome
- (T) for the timing of the intervention
- (S) for the setting
Example PICOTS:
- P = Adults with class II - IV heart failure and EF < 40% on standard therapy
- I = Angiotensin-neprilysin inhibition(LCZ696) at doses of 200 mg twice a day
- C = Enalapril 10 mg twice daily
- O = CV related mortality, all-cause mortality, and hospitalizations for heart failure
- T = Over a period a median of 27 months
- S = Outpatient
EBM Consult uses PICOTS because it is more complete and appropriate.
Every study has a PICO or PICOTS and appropriate application of this content should be compared to the PICO or PICOTS being asked by the clinician.
- Mehta's Example Of A Study Evaluation
E-cigarette's users twice as likely to quit smoking
- Population: RCT of 886 adults in UK
- Intervention: Patients randomized to receive Nicotine Replacement (pt choice) or E-cigarette for 3 months, along with weekly behavioral counseling for first 4 weeks.
- Primary outcome: Sustained abstinence for 1 year, which was validated biochemically at the final visit
- Results: 1-year abstinence rate was 18.0% in the e-cigarette group, as compared with 9.9% in the nicotine-replacement group (relative risk, 1.83; 95% confidence interval [CI], 1.30 to 2.58; P<0.001).
- Conclusion: E-cigarettes were more effective for smoking cessation than nicotine-replacement therapy, when both products were accompanied by behavioral support.
Reference:
Cancer Screening Definitions
Overdiagnosis:
- When testing results in finding asymptomatic disease that would not have been clinically important during the patient's lifetime and would not have impacted morbidity and mortality
Lead-time bias:
- When screening results in diagnosis of the disease leading to an apparent increase in survival time (as measured from diagnosis) despite no change in overall mortality and possibly no change in person's life length
Length-time bias:
- When screening is more likely to detect slow growing tumors than aggressive, rapidly growing tumors leading to an apparent increase in survival
Healthy participant bias:
- When those who choose to be screened are in better health and have healthier habits in general leading to improvements in survival and other outcomes unrelated to screening
References:
- AFP Vol 93 No 8 Apr 2016
Example of Interpreting A Study Results (Just a 1% difference)
Example of interpreting a study results:
"In 1993, the GUSTO trial provided highly statistically significant results that showed that 30-day mortality among Activase-treated patients was 6.3% versus 7.3% for streptokinase and the 24-hour mortality rates were 2.4% and 2.9%, respectively."
7.3% –> 6.3%
- 1% change in mortality is a 13.7% improvement
- Percent change = (new value - old value)/old value = (7.3-6.3)/7.3 = 1/7.3 = 0.136986 = 13.7%
"When … 100 people would die on the old drug, only 86 would die on the new Genentech drug."
"Was the additional $2,000 worth the better patient outcomes? For me, the answer is clear. Giving Activase instead of streptokinase to 1,000 patients would, based on these results, cost an extra $2 million and save ten patients (1,000 x 0.073 – 1,000 x 0.063 = 10), for an effective cost per life saved of $200,000 (1993 dollars). In today’s dollars, the amount would be $448,000, or about 5% of the value the Environmental Protection Agency uses to value an American life."
Notes:
- EPA recommends that the central estimate of $7.4 million ($2006), updated to the year of the analysis, be used in all benefits analyses that seek to quantify mortality risk reduction benefits regardless of the age, income, or other population characteristics of the affected population until revised guidance becomes available.
Reference:
Random Statistics in Medicine edit
65% of deaths and 35% of years of life lost to premature mortality or lived with disability in USA are from:
- Tobacco use
- Obesity
- Unhealthy diet
- Lack of physical activity
References:
- JAMA 2013;310(6):591-608
Christakis and Fowler found using the Framingham network:
- If a person became obese, the likelihood his friend would also become obese was 171%.
- When smokers quit, their friends are 36% more likely to also quit. (Although this effect diminishes as the separation between contacts grow, and loses its efficacy at four degrees of separation.)
- Happy friends increased the likelihood of an individual being happy by 8%.
Obesity stats:
- 2/3 of all adults and 1/3 of children are currently overweight or obese.
- 72% of older men and 67% of older women are now overweight or obese
- Obesity is linked to more than 60 chronic diseases
References:
- (Consultant Jan 2016)
Men's Health:
- 48% do not regularly engage in physical activity
- 33% obese
- 32% have had 5+ alcoholic drinks in 1d in last 1y
- 31% have hypertension
- 22% smoke
- 12% rate overall health as fair or poor
References:
- AFP Vol 85 No 10 May 2012
15% of reproductive age women use antidepressants.
- Ages 35-44
- Most comonly: sertraline, burpropion, and citalopram
- Morb Mort Wkly Rep 2016 Jan 29;65:41-6
Family Medicine
- 1 in 5 Americans report no usual source of health care (Jetty A. Fewer Americans Report a Personal Physician as Their Usual Source of Health Care. AFP 2015 Vol 92 No 12)
- Complexity:
- Complexity per hour is 33% high than cardiologists and 5x higher than psychiatrists
- (Katerndahl D, Wood R, Jaen CR. Family medicine outpatient encounters are nore complex than those of cardiology and psychiatry. J Am Board Fam Med. 2011;24:6-15)
What did 95 Percent effective mean (COVID) edit
"95% effective" means that 95% of the patients who had Covid symptoms and a positive test were in the control group. Five percent were in the test group.
Here's what "95% effective" did not mean: if you take the shots, then you will have a 95% lower chance of getting covid. But that is how most people understood it because that is what the words mean in normal English.
Would you take a drug that could reduce the incidence of a rare disease by 50%? From 10 per 1 million to 5 per 1 million is an 50% RRR and an 0.0005% ARR.
The 95% figure cited for the covid injections is the relative risk. The absolute risk reduction was 0.84%. In a slide deck from the Canadian Covid Care Alliance (CCCA), slide 11 shows how the 91% was achieved (it is 91%, not 95%, because the it refers to an earlier version of the study):
The research paper COVID-19 vaccine efficacy and effectiveness—the elephant (not) in the room puts the ARR in the 1% range. The CCCA slide deck gives an ARR of 0.84%, though it is not clear how they reached this number, based on the other numbers in their slides.
A clinical trial finding of a 1% ARR means that 99% of the people who take the drug either did not experience the condition that the drug treats, or they did experience it, but were not helped by the drug. The 1% both had the condition and were helped by the drug. Another way of saying this is the Number Needed to Treat (NNT). NNT is the reciprocal of the ARR and is the number of people who must take the drug to help one person reach the endpoint. An ARR of 1% corresponds to an NNT of 100 people.
Biostat Terms
| Sensitivity | Sn | Percentage of patients with disease who have a positive test for the disease in question |
| Specificity | Sp | Percentage of patients without disease who have a negative test for the disease in question |
| Predictive value (positive and negative) | PV+ | Percentage of patients with a positive or negative test for a disease who do or do not have the disease in question |
| PV- | Percentage of patients with a positive or negative test for a disease who do or do not have the disease in question | |
| Pretest probability | Probability of disease before a test is performed | |
| Post-test probability | Probability of disease after a test is performed | |
| Likelihood ratio | LR | LR >1 indicates an increased likelihood of disease |
| LR <1 indicates a decreased likelihood of disease. | ||
| The most helpful tests generally have a ratio of less than 0.2 or greater than 5. | ||
| Relative risk reduction | RRR | The percentage difference in risk or outcomes between treatment and control groups. Example: if mortality is 30% in controls and 20% with treatment, RRR is (30-20)/30 = 33 percent. |
| Absolute risk reduction | ARR | The arithmetic difference in risk or outcomes between treatment and control groups. Example: if mortality is 30% in controls and 20% with treatment, ARR is 30-20=10%. |
| Number needed to treat | NNT | The number of patients who need to receive an intervention instead of the alternative in order for one additional patient to benefit. The NNT is calculated as: 1/ARR. Example: if the ARR is 4%, the NNT = 1/4% = 1/0.04 = 25. |
| 95 percent confidence interval | 95% CI | An estimate of certainty. It is 95% certain that the true value lies within the given range. A narrow CI is good. A CI that spans 1.0 calls into question the validity of the result. |
| Systematic review | A type of review article that uses explicit methods to comprehensively analyze and qualitatively synthesize information from multiple studies | |
| Meta-analysis | A type of systematic review that uses rigorous statistical methods to quantitatively synthesize the results of multiple similar studies |
Reference:
- Spn vs Sn edit
- Specificity: Tru negative rate - % without disease who have neg test
- Total true neg/(Total true neg + Total false positive)
- SpPIN - high Specificity rule IN with a positive result
- Sensitivity - % of patients with a disease who have a positive test
- SnNOUT - highly Sensitive test is Negative helps to rule OUT disease
- OR or RR - measure of the association between an exposure and disease
- LR - clinical impression of how well a test rules in or out a disease
- Specificity: Tru negative rate - % without disease who have neg test
Shared Decision Making And Using Numbers
Recommendations:
- Use numerical data to describe risks
- Use absolute risk rather than relative risk
- Risk increased from 1:1000 to 2:1000 rather than "it doubles"
- Use natural frequencies
- 10 in 100 rather than 10%
- Be consistent when using data; use the same denominator comparing risks
- 7:100 and 20:100 rather than 1:14 and 1:5
- Present risk over a defined period of time (months or years)
- If 100 people have treatment for 1 year, 10 will have this adverse effect
- Use positive and negative framing
- Treatment will be successful for 97 out of 100 people, and it will be unsuccessful for 3 out of 100 people
References:
- AFP Aug 2022 Vol 106 No 2
Safety Statistics
- Motorcycles
Motorcycle fatality trends for 2021. The majority of motorcyclist fatalities occurred:
- On urban roads (67%)
- In good weather (83%)
- During the nighttime (50%)
- In crashes involving two vehicles (53%)
- When wearing helmets (59%)
- 72% of the motorcycle operators involved in fatal crashes were NOT alcohol-impaired
Reference:
- Study: Disparities in Activity and Traffic Fatalities by Race/Ethnicity
Introduction
- Traffic fatalities remain a major public health challenge despite progress made during recent decades. This study develops exposure-based estimates of fatalities per mile traveled for pedestrians, cyclists, and light-duty vehicle occupants and describes disparities by race/ethnicity, including a subanalysis of fatality rates during darkness and in urban areas.
Methods
- Estimates of person-miles traveled by mode and race/ethnicity group were derived from the 2017 National Household Travel Survey using replicate weights. Three-year average (2016‒2018) traffic fatalities were measured by mode and race/ethnicity group with the U.S. Fatality Analysis Reporting System. Fatality rates per mile traveled and CIs were calculated for each subgroup as well as separately for trips occurring during darkness and in urban areas. Analysis was conducted in 2021‒2022.
Results
- Exposure to traffic fatality differs by race/ethnicity group and by mode, indicating that adjustment for differential exposure is needed when estimating disparities.
- The authors find that fatality rates per 100 million miles traveled are systematically higher for Black and Hispanic Americans for all modes
- Notably higher for vulnerable modes
- Black Americans died at
- More than 4 times the rate for White Americans while cycling, 33.71 [95% CI: 21.84, 73.83] compared with 7.53 [95% CI: 6.64, 8.69]
- More than 2 times the rate while walking, 40.92 [95% CI: 36.58, 46.44] compared with 18.77 [95% CI: 17.30, 20.51])
- Black Americans died at
- Previous estimates that do not adjust for differential exposure may underestimate disparities by race/ethnicity. Observed disparities remained when considering only urban areas and appear to be exacerbated during darkness.
Conclusions
- Traffic fatalities are a substantial and preventable public health challenge in America. Black and Hispanic Americans have higher traffic fatality rates per mile traveled than White Americans across the transportation system, requiring urgent attention.
Reference:
- Raifman MA, Choma EF. Disparities in Activity and Traffic Fatalities by Race/Ethnicity. Am J Prev Med. 2022;63(2):160-167. https://doi.org/10.1016/j.amepre.2022.03.012
- https://www.ajpmonline.org/article/S0749-3797(22)00155-6/fulltext
Life Expectancy
| Age | Men | Women |
|---|---|---|
| Birth | 76.3 | 81.1 |
| 65 | 17.8 | 20.3 |
| 70 | 14.3 | 16.5 |
| 75 | 11.1 | 12.9 |
| 80 | 8.2 | 9.6 |
| 85 | 5.9 | 6.9 |
| 90 | 4.1 | 4.8 |
| 95 | 2.9 | 3.3 |
| 100 | 2.1 | 2.3 |
| Disease | Age | Life expectancy |
|---|---|---|
| Alzheimer disease | Unspecified | Men: 4.2 years |
| Women: 5.7 years | ||
| Hip fracture | 80yo | 5.4 years |
| Heart Failure | >75yo | Men: 3.9 years |
| Women: 4.5 years | ||
| Myocardial Infarction | Unspecified | 11.3 years |
| Cancer | 50 yo | 70 yo | 75 yo | 80 yo | 85 yo | 90 yo |
|---|---|---|---|---|---|---|
| Breast | 3.1 | 2.2 | 1.8 | 1.5 | 1.2 | 0.8 |
| Colorectal (men) | 2.3 | 2.1 | 1.9 | 1.8 | 1.6 | 1.1 |
| Colorectal (women) | 2.2 | 2.0 | 1.9 | 1.8 | 1.6 | 1 |
| Cervical | 0.26 | 0.15 | 0.12 | 0.10 | 0.07 | 0.05 |
References:
- AFP Vol 93 No 8 Apr 2016
- AFP Vol 78 No 12 Dec 2008
- CDC
p values
P-values
- P-values are a measure of how likely it is that you'd observe the results you did if your intervention didn't actually work.
- The smaller your p-value, the less likely you are to have observed the results you did by mere luck.
- Conversely, the larger your p-value, the more likely it is that you'd observe the results you did by mere luck.
- A p-value is not the probability that the null hypothesis is true. The opposite is also true: a p-value is not the probability that your intervention is effective.
- Just because you haven't observed an effect, it doesn't mean there isn't one.
- If you run the same experiment many times, you'll eventually see a p-value below 0.05, even if the null hypothesis is true.
- Looking for an effect until you find one is an effective way to make sure you get a small p-value, but it's bad practice unless you're looking for an easy way to sell books.
- A p-value below 0.05 is usually considered "statistically significant". Although it's not a magic number, it's a rule of thumb that has been around for a while.
Reference:
Study: The (Mis)Reporting Of Statistical Results In Psychology Journals
In order to study the prevalence, nature (direction), and causes of reporting errors in psychology, we checked the consistency of reported test statistics, degrees of freedom, and p values in a random sample of high- and low-impact psychology journals. In a second study, we established the generality of reporting errors in a random sample of recent psychological articles.
Our results, on the basis of 281 articles, indicate that
- around 18% of statistical results in the psychological literature are incorrectly reported. Inconsistencies were more common in low-impact journals than in high-impact journals.
- Moreover, around 15% of the articles contained at least one statistical conclusion that proved, upon recalculation, to be incorrect; that is, recalculation rendered the previously significant result insignificant, or vice versa.
- These errors were often in line with researchers' expectations.
We classified the most common errors and contacted authors to shed light on the origins of the errors.
Reference:
- Bakker M, Wicherts JM. The (mis)reporting of statistical results in psychology journals. Behav Res Methods. 2011 Sep;43(3):666-78. doi: 10.3758/s13428-011-0089-5. PMID: 21494917; PMCID: PMC3174372.
Books For Patients To Read From Library
- Breakfast with Seneca: A Stoic Guide to the Art of Living by David Fideler
- Tell Yourself a Better Lie: Use the power of Rapid Transformational Therapy to edit your story and rewrite your life. by Marisa Peer
- Meditation for Fidgety Skeptics: A 10% Happier How-to Book by Dan Harris
- Understanding Other People: The Five Secrets to Human Behavior by Beverly Flaxington
- Cognitive Behavioral Therapy: Techniques for Retraining Your Brain by Jason M. Satterfield
- The Book of Job: When Bad Things Happened to a Good Person by Harold S. Kushner
- Confidence and Success with CBT: Small steps to achieve your big goals with cognitive behavior therapy by Avy Joseph
Chloride Levels
Some reasons for high chloride (>106 MEq/L):
- Metabolic acidosis, which can happen with health conditions or substances that cause acid to build up in the body
- Dehydration
- Kidney disease
- Some forms of diarrhea
- Some medications, like NSAIDs or estrogen
Some medications that may increase chloride levels include:
- Cortisone
- Estrogen
- Ammonium chloride
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin) and naproxen (Aleve)
Some reasons for low chloride (<96 MEq/L):
- Heart failure
- Vomiting or diarrhea
- Some medications, like diuretics
- Addison's disease
- Chronic lung disease
- Some forms of kidney disease
- Metabolic alkalosis, which can happen with severe dehydration, laxative use, and certain medical conditions like cystic fibrosis
- Burns
Coding
Codes to help with radiology
- ICD-10
- Head
- Dizziness/vertigo R42.
- Headache R51.
- Vascular G44.1
- Migraine, unspecified G43.909
- Pituitary Tumor D44.3
- Sinusitis, acute J01.90
- Chronic J32.9
- Tinnitus H93.19
- Trauma, unspecified injury S09.90XA
- Other specified head injury S09.8XXA
- Vision, blurred H53.8
- Disturbance/loss H53.9
- Neck
- Mass/lump/swelling R22.1
- Parotid tumor, benign D11.0
- Thyroid nodule E04.1
- Elevated TSH R94.6
- Chest
- Chest pain, atypical, other R07.89
- Precordial chest pain R07.2
- Cough R05.
- Lung nodule R91.1
- Mass, abnormal imaging finding R91.8
- SOB R06.02
- Abdomen
- Liver lesion, other specified disorder K76.89
- Abnormal liver function studies R94.5
- Pain,
- Generalized R10.84
- Epigastric R10.13
- RUQ R10.11
- RLQ R10.31
- LUQ R10.12
- LLQ R10.32
- Pelvis
- DUB N93.8
- Menorrhagia N92.0
- Premenopausal N92.4
- Postmenopausal bleeding N95.0
- Pelvic and/or perineal pain R10.2
- Perineal other spec. conditions assoc. w/ female genital organs and menstrual cycle N94.89
- Chronic bladder pain R39.82
- Disorder of prostate unspec N42.9
- Spine
- Cervical
- Arthropathy M46.92
- Disc disease M50.30
- Herniation M50.20
- Pain M54.2
- Radiculopathy M54.12
- Spondylosis M47.812
- Stenosis M48.02
- Thoracic
- Disc disease M51.34
- Herniation M51.24
- Pain M54.6
- Radiculopathy M54.14
- Spondylosis M47.814
- Stenosis M48.04
- Lumbar
- Arthropathy M46.96
- Disc disease M51.36
- Herniation M51.26
- Pain M54.5
- Radiculopathy M54.16
- Sciatica M54.3
- Spondylosis M47.816
- Stenosis M48.06
- Coccyx, pain M53.3
- Lumbosacral Spondylosis M47.817
- Cervical
- Extremities
- Effusion
- Ankle M25.471 (R)/.472 (L)
- Foot M25.474 (R)/.475 (L)
- Knee M25.461 (R)/.462 (L)
- Hip M25.451 (R)/.452 (L)
- Hand M25.441 (R)/.442 (L)
- Wrist M25.431 (R)/.432 (L)
- Elbow M25.421 (R)/.422 (L)
- Shoulder M25.411 (R)/.412 (L)
- Pain
- Toe M79.674 (R)/.675 (L)
- Foot M79.671 (R)/.672 (L)
- Ankle M25.571 (R)/.572 (L)
- Lower leg M79.661 (R)/.662 (L)
- Knee M25.561 (R)/.562 (L)
- Hip M25.551 (R)/.552 (L)
- Finger M79.644 (R)/.645 (L)
- Hand M79.641 (R)/.642 (L)
- Wrist M25.531 (R)/.532 (L)
- Elbow M25.521 (R)/.522 (L)
- Shoulder M25.511 (R)/.512 (L)
- Injury
- Rotator cuff tear/rupture
- no trauma M75.101 (R)/.102 (L)
- Derangement of meniscus,
- old injury M23.2
- Meniscus Tear, current injury S83.2
- Sprain unspecified ligament knee S83.5
- Ankle/foot injury unspecified S99.9
- Effusion
- Breast
- Routine screening Z12.31
- Breast lump N63.
- Personal history of breast cancer Z85.3
- Abnormal findings
- diagnostic imaging R92.8
- Breast pain (Mastodynia) N64.4
Reference:
- Head
- CPT Codes
- X-Ray
- Skull, Facial Bones, and Jaw
- Skull less than 4 views 70250
- Skull min. 4 views 70260
- Facial Bones less than 3 views 70140
- Facial Bones min. 3 views 70150
- Mandible less than 4 views 70100
- Mandible min. 4 views 70110
- Jaw joint unilateral (TMJ) 70328
- Jaw joint bilateral (TMJ) 70330
- Orbits, Eyes, Sinus, and Nasal
- Orbits complete 70200
- Eye for foreign body 70030
- Sinuses less than 3 views 70210
- Sinuses min 3 views 70220
- Nasal Bones 70160
- Neck
- Neck soft tissue 70360
- Upper Extremity
- SI joints less than 3 views 72200
- SI joints 3 or more views 72202
- Sacrum/Coccyx 72220
- Clavicle 73000
- Scapula 73010
- Shoulder 1 view 73020
- Shoulder min 2 views 73030
- AC joints bilateral 73050
- Humerus 73060
- Elbow min 2 views 73070
- Elbow min 3 views 73080
- Forearm 73090
- Wrist 2 views 73100
- Wrist 3 views 73110
- Hand 2 views 73120
- Hand 3 views 73130
- Finger(s) 73140
- Scoliosis and Spine
- Scoliosis Evaluation 2-3 views 72082
- Spine 1 view 72020
- Cervical Spine
- Cervical Spine 2 or 3 views 72040
- Cervical Spine 4 or 5 views 72050
- Cervical Spine 6 or more views 72052
- 2020 X-RAY CPT CODES*
- Thoracic Spine
- Thoracic Spine 2 views 72070
- Thoracic Spine 3 views 72072
- Thoracic Spine min 4 views 72074
- Thoracic Lumbar Spine 2 views 72080
- Lumbar Spine
- Lumbar Spine 2 or 3 views 72100
- Lumbar Spine min 4 views 72110
- Lumbar Spine complete bending
- min 6 views 72114
- Lumbosacral, bend only 2-3 views 72120
- Lower Extremity
- Hip unilateral 1 view 73501
- Hip unilateral 2 or 3 views 73502
- Femur 1 view 73551
- Femur min 2 views 73552
- Knee 1 or 2 views 73560
- Knee 3 views 73562
- Knee 4 or more views 73564
- Both Knees standing 1 view 73565
- Lower Leg Tibia and Fibula 73590
- Leg Infant 73592
- Ankle 2 views 73600
- Ankle 3 views 73610
- Foot 2 views 73620
- Foot 3 views 73630
- Heel 2 views 73650
- Toe(s) 73660
- Chest
- Chest 1 view 71045
- Chest 2 views (PA & Lateral) 71046
- Chest (front, lat, w/apical) 3 views 71047
- Chest (PA lat & Obliques) 71047 or 71048
- Chest complete 4 view 71048
- Ribs/Chest min 4 views 71111
- Sternum min 2 views 71120
- Abdomen
- Abdomen single AP view 74018
- Abdomen AP/Oblique/Cone view 2 views 74019
- Abdomen complete min 6 views 74021
- Abdomen obstruct series 74022
- Pelvis
- Pelvis Complete min 3 views 72190
Bone Age Study
- Bone Age Study 77072
Reference:
- Skull, Facial Bones, and Jaw
- Ultrasound
- Head & Extracranial
- Echo Head (Echoencephalography) 76506
- Head & Neck soft tissue (thyroid) 76536
- Extracranial complete bilateral duplex study 93880
- Extracranial limited or unilateral duplex study 93882
- Chest & Abdomen
- Chest 76604
- Abdomen complete 76700
- Abdomen limited 76705
- Renal
- Renal complete (Retroperitoneal) 76770
- Renal limited (Retroperitoneal) 76775
- Pelvic
- Pelvic complete 76856
- Pelvic limited / follow-up 76857
- Scrotum & Extremity Soft Tissue
- Scrotum 76870
- Extremity soft tissue complete 76881
- Duplex Vascular
- Duplex Vascular Abdominal/Pelvic/Scrotal/Retroperitoneal complete 93975
- Duplex Vascular Abdominal/Pelvic/Scrotal/Retroperitoneal limited 93976
- Duplex Vascular Aorta/IVC/Iliac Vascular/Bypass grafts complete 93978
- Paracentesis & Thoracentesis
- Paracentesis with imaging guidance 49083
- Thoracentesis with imaging guidance 32555
- Arterial & Venous
- Extremity Arterial doppler limited 93922
- Extremity Arterial doppler complete 93923
- Arterial Lower Extremity duplex study complete bilateral 93925
- Arterial Lower Extremity duplex study limited or unilateral 93926
- Arterial Upper Extremity duplex complete bilateral 93930
- Arterial Upper Extremity duplex limited or unilateral 93931
- Venous Duplex Extremity Imt. or unilateral 93971
- Venous Duplex Extremity comp. bilateral 93970
- OB, Pregnant Uterus, & Transvaginal
- OB complete 1st Trimester single gestation 76801
- Pregnant Uterus > 14 weeks single gestation 76805
- Pregnant Uterus multiple > 14 weeks 76810
- Pregnant Uterus limited 76815
- Pregnant Uterus repeat / follow-up 76816
- Transvaginal non-OB 76830
- OB Transvaginal 76817
- Breast
- Breast unilateral complete 76641
- Guided Breast Cyst Aspiration (puncture) 19000
- MRI Breast bilateral with and/or
- without contrast 77049
- Digital Mammogram screening; bilateral 77067
- Diagnostic Mammogram; unilateral 77065
- Each Additional Cyst + 19001
- Diagnostic Mammogram; bilateral 77066
- Needle Localization
- Placement of breast localization device ONLY, first lesion (includes mammo. guidance) 19281
- Each Additional Lesion + 19282
- Placement of breast localization device ONLY, first lesion (includes US guidance) 19285
- Each Additional Lesion + 19286
- Placement of breast localization device ONLY, first lesion (includes MRI guidance) 19287
- Each Additional Lesion + 19288
- Stereotactic Guided Biopsy
- Biopsy w/ stereotactic guidance, first lesion (incl. local/device placement/specimen imaging) 19081
- Each Additional Lesion + 19082
- x2 Bilateral 19082
- Ultrasound Guided Biopsy
- Biopsy w/ ultrasound guidance, first lesion (incl. local/device placement/specimen imaging) 19083
- Each Additional Lesion + 19084
- x2 Bilateral 19084
- MRI Guided Biopsy
- Biopsy w/ MRI guidance, first lesion (incl. local/device placement/specimen imaging) 19085
- Diagnostic Mammogram; unilateral + 19086
- x2 Bilateral 19086
- Galactogram
- Single Duct (injection) 19030
Bone Density
- DEXA Scan Hip & Lumbar Spine 77080
Reference:
- Head & Extracranial
- CT
- Head (Brain)
- w 70460
- wo 70450
- w/wo 70470
- CTA Head (Brain) w/wo 70496
- Orbits (Temporal Bones)
- w 70481
- wo 70480
- w/wo 70482
- Maxillofacial (Sinus Complete)
- w 70487
- wo 70486
- w/wo 70488
- Neck (Soft Tissues)
- w 70491
- wo 70490
- w/wo 70492
- CTA Neck (Carotid) w/wo 70492
- Upper Extremity
- w 73201
- wo 73200
- w/wo 73202
- CTA Upper Extremity w/wo 73206
- Lower Extremity
- w 73701
- wo 73700
- w/wo 73702
- CTA Lower Extremity w/wo 73706
- Cervical Spine
- w 72126
- wo 72125
- w/wo 72127
- Thoracic Spine
- w 72129
- wo 72128
- w/wo 72130
- Lumbar Spine
- w 72132
- wo 72131
- w/wo 72133
- Virtual Colonoscopy
- w/wo 74263
- Calcium Score (Coronary Calcium Score)
- 75571
- Chest
- w 71260
- wo 71250
- w/wo 71270
- CTA/PE study 71275
- Chest/Abdo/Pelvis w/wo 71275 & 74178
- Abdomen
- w 74160
- wo 74150
- w/wo 74170
- CTA Abdomen (Renal arteries) w/wo 74175
- CTA Abdomen/Pelvis w/wo 74174
- Pelvis
- w 72193
- wo 72192
- w/wo 72194
- CTA Pelvis w/wo 72191
- CTV Pelvis w 72191
- COMBINATION CODES
- Abdomen & Pelvis
- Abdomen & Pelvis (w) 74177
- Abdomen & Pelvis (wo) 74176
- Abdomen & Pelvis (w/wo) 74178
- CTA
- Coronary Arteries 75574
- Runoff 75635
- Low Dose Lung Nodule
- Low Dose Lung Nodule 71250
- Abdomen & Pelvis
- Bone Density (QCT)
- Bone Density (QCT) 77078
Contrast Code
- Contrast Code Q9967
Reference:
- Head (Brain)
- MRI
- TMJ/Orbits/Face/Neck
- TMJ(s) 70336
- w 70542
- wo 70540
- w/wo 70543
- Head
- w 70545
- wo 70544
- w/wo 70546
- Neck
- w 70548
- wo 70547
- w/wo 70549
- Brain
- w 70552
- wo 70551
- w/wo 70553
- Brain, Spectroscopy 76390
- Upper Extremity (Non-Joint/Joint)
- Non-Joint w 73219
- Non-Joint wo 73218
- Non-Joint w/wo 73220
- Joint w 73222
- Joint wo 73221
- Joint w/wo 73223
- MRA Upper Extremity w/wo 73225
- Lower Extremity (Non-Joint/Joint)
- Non-Joint w 73719
- Non-Joint wo 73718
- Non-Joint w/wo 73720
- Joint w 73722
- Joint wo 73721
- Joint w/wo 73723
- MRA Lower Extremity w/wo 73725
- Cervical Spine
- w 72142
- wo 72141
- w/wo 72156
- Thoracic Spine
- w 72147
- wo 72146
- w/wo 72157
- Lumbar Spine
- w 72149
- wo 72148
- w/wo 72158
- Breast (Bilateral)
- w and/or wo 77049
- Chest
- w 71551
- wo 71550
- w/wo 71552
- MRA Chest w/wo 71555
- Abdomen
- w 74182
- wo 74181
- w/wo 74183
- MRA Abdomen w/wo 74185
- Pelvis
- w 72196
- wo 72195
- w/wo 72197
- MRA Pelvis w/wo 72198
- MRI Guidance & Arthrogram
- MRI Guidance for needle placement S&I 77021
- Arthrogram shoulder injection/joint 23350
- Arthrogram knee injection/joint 27369
- Arthrogram wrist injection/joint 25246
- 3D Rendering & Interpretation
- CT or MRI 76376
Contrast Code
- Contrast Code A9579
UPPER EXTREMITY Non-Joint Joint Upper Arm Shoulder Lower Arm Elbow Hand Wrist Finger LOWER EXTREMITY Non-Joint Joint Femur Knee Foot Ankle Tibia/Fibula Hip Reference:
- TMJ/Orbits/Face/Neck
- PET
- Brain, Metabolic
- Brain, Metabolic 78608
- Skull to Mid-Thigh
- Tumor Imaging with concurrent CT, Skull to Mid-Thigh 78815
- Whole Body
- Tumor Imaging with concurrent CT, Whole Body 78816
FDG Injection
- FDG Injection A9552
Reference:
- Brain, Metabolic
- Nuc Med
- Endocrine
- Thyroid uptake, single study 78012
- with vascular flow 78013
- with single/multiple uptake(s)
- quantitative 78014
- Thyroid carcinoma metastases limited 78015
- whole body 78018
- Parathyroid planar 78070
- Adrenal, cortex and/or medulla 78075
- Thyroid uptake, single study 78012
- Gastrointestinal
- Liver, static only 78201
- Liver SPE 78803
- Liver-Spleen, static only 78215
- Hepatobiliary including gallbladder 78226
- Gastroesophageal reflux study 78262
- Gastric emptying 78264
- Acute GI blood loss scan 78278
- Musculoskeletal Bone Scans
- Bone and/or, limited 78300
- multiple areas 78305
- Whole body 78306
- 3 Phase study 78315
- Bone and/or, limited 78300
- Cardiovascular
- Non cardiac vascular flow 78445
- DVT imaging, Peptide (AcuTect) 78456
- Myocardial perfusion study, single 78451
- multiple studies 78452
- Myocardial perfusion planar, single 78453
- multiple studies 78454
- Cardiac Pool (MUGA), single 78472
- multiple 78473
- Respiratory
- Perfusion lung scan 78580
- Ventilation/perfusion lung 78582
- Pulmonary quantitative function 78597
Abscess/Tumor
- Localization of tumor, single 78800
- multiple 78801
- whole body, single day 78802
- requiring 2 or more days 78804
Reference:
- Localization of tumor, single 78800
- Endocrine
- X-Ray
Inpatient coding
- Admits: (992…)
- On admission: 21 or 23 - most should be 23
- Day 2: 31, 32, 33 - most should be 32
- On discharge: 38
- Observations:
- On day 1: 18 or 20 - most should be 20
- On discharge: 17
Intensive Behavioral Therapy for Obesity
For Medicare beneficiaries with obesity, defined as a BMI greater than or equal to 30; who are competent and alert at the time that counseling is provided; and whose counseling is furnished by a qualified primary care physician or other primary care practitioner in a primary care setting, CMS will cover intensive behavioral therapy for obesity. This service is described as follows:
- One face-to-face visit every week for the first month
- One face-to-face visit every other week for months 2–6
- One face-to-face visit every month for months 7–12, if the beneficiary meets the 3kg (6.6 lbs) weight loss requirement during the first 6 months as discussed below
Coding:
- HCPCS code G0447 (Face-to-face behavioral counseling for obesity, 15 minutes) may be reported for this service.
- HCPCS code G0473 (Face-to-face behavioral counseling for obesity, group (2–10), 30 minutes), may be reported if the counseling is performed in a group session.
Additional information on the Medicare policy for treatment of obesity may be accessed at
Home Health Care Benefit Qualifications
To qualify for for the Medicare home health care benefit, a patient must:
- Be confined to the home
- Be under the care of a physician
- Be receiving services under a plan of care established and periodically reviewed bya physician
- Be in need of skilled nursing care on an intermittent basis or physical therapy or speech language pathology; or continuing need for occupational therapy
- Have a face-to-face encounter with a medical provider as mandated by the Affordable CAre Act for the initial episode of care
Outpatient coding
- Advanced Care Planning
- 99497 - Advanced care planning first 30 min ($82)
- 99498 - Each additional 30min ($72)
- Chronic Care Management
- 99490 - CCM services 20 min ($42)
- 99487 - Complex CCM services 60 min ($93)
- Gyn procedure codes:
- 99499 No charge E&M
- 57452 Colpo
- 57455 Colpo with cerv bx
- 57454 Colpo with cerv bx and ECC
- 57456 Colpo with ECC
- 57505 ECC alone (no colpo)
- 58100 Endometrial biopsy
- 11981 Nexplanon insertion
- 11982 Nexplanon removal
- 58300 IUD insertion
- 58301 IUD removal
- Medicare patients
- GE Modifier if faculty did not see patient. Faculty Attestation must be present stating faculty discussed patient with resident and agrees with plan.
- GC Modifier if faculty was face to face with patient for visit/procedure. Faculty Attestation must be present stating faculty saw the patient and participated in key components of service/procedure. (Required participation for billing higher than a 99213).
- OB codes:
- IOB – 0501F
- ROB/antenatal visit – 0502F
- Post-partum – 0503F
- Obesity
- E66.01 - Morbid obesity from excess calories
- E66.9 - Unspecified obesity (Do not use unless necessary)
- Attach BMI codes to obesity codes
- BMI codes are Z68.BMI -> example: BMI 31 = Z68.31
- Other
- 99050 - Services provided in the office at times other than regularly scheduled office hours, or days when the office is normally closed (holidays, Sat, Sun)
- 99051 - Services provided in the office during regularly scheduled evening, weekend, or holiday office hours - when seen during regular office hours that occur outside of traditional office hours
- 99058 - Services provided on an emergency basis in the office, which dirupts other scheduled office services
- 99053 - Services provided between 10pm and 8am at 24-hr facility
- Post-op
- 99024
- Preventive Visits (Established)
- 99391 - Established Inf
- 99392 - Established 1-4
- 99393 - Established 5-11
- 99394 - Established 12-17
- 99395 - Established 18-39
- 99396 - Established 40-64
- 99397 - Established 65+
- Preventive Visits (New)
- 99381 - New Inf
- 99382 - New 1-4
- 99383 - New 5-11
- 99384 - New 12-17
- 99385 - New 18-39
- 99386 - New 40-64
- 99387 - New 65+
- Prolonged Services
- 99354 - Prolonged services in an office or other outpatient setting with direct patient contact first hour - ($131)
- 99355 - Each additional 30min
- 99358 - Prolonged without direct patient contact ($113)
- 99339 - Each additional 30min
- Routine Visits:
- 99213
- 99214
- 99215
- Smoking cessation codes
- G0436 - Smoking and tobacco use cessation counseling visit; intermediae, greater than 3min up to 10 min
- G0437 - Smoking and tobacco use cessation counseling visit; intermediae, greater than 3min up to 10 min
- Telephone Visits
- 99441 (0-10 min)
- 99442 (11-20 min)
- 99443 (21-30 min)
- Transitional Care Management (TCM)
- 99495 - TCM with moderate mod decision complexity and face-to-face visit within 14 days of discharge ($165)
- 99496 - TCM with moderate high decision complexity and face-to-face visit within 7 days of discharge ($233)
- Video Visits
- G9847 (15 min)
- G9848 (25 min)
- G9849 (40 min)
For a single procedure done in a procedure only appointment:
- CPT (done as an order in Epic, not sure in Athena) + no charge E&M code
- Ex: IUD in Gyn clinic, Single excision in Skin clinic, Circumcision clinic
For multiple procedures done in a procedure only appointment:
- CPTs (order the most lucrative one first) + 59 modifiers added to each additional procedure + no charge
- Ex: Skin excision + freeze AKs, EMB + colpo, spirometry + nebulizer during combined
For a procedure done during an office visit where evaluation and counseling of options has occurred or other conditions are discussed:
- E&M code (99213, etc) + 25 modifier attached to the E&M + CPT code
- Ex: asthma eval + neb tx, knee or shoulder eval + injection, pre-op + EKG, WWE + pap
For multiple procedures done during an office visit where evaluation and counseling of options has occurred or other conditions are discussed:
- E&M code (99213, etc) + 25 modifier attached to the E&M + CPT codes (in descending cost order) + 59 modifiers to each additional procedure
- Exception: use a 50 modifier if bilateral procedure (both knees)
- If the patient is there for an office visit (a skin spot, knee pain, etc) and you decide a procedure is necessary, make sure to code for the office visit (99213 or 4) with a 25 modifier and the CPT for the procedure
- Please make sure that your chief complaint is not "biopsy" "knee injection" or "IUD placement" unless they are specifically there for that reason. If you try to charge an office visit for chief complaint of "knee injection," it will likely get rejected by insurance as they feel the pt is only there for procedure itself. Use knee pain, skin lesion, etc for the CC.
- If they are there just for the procedure (skin clinic, IUD placement), then you bill a global/no charge with a 25 modifier and the CPT for the procedure if you address no other issues at the visit
- Do not forget that most skin procedures have a global period of 10 days associated with them so we cannot bill an office visit for removing sutures (that we placed) or repacking an I&D or doing a wound check for the first 10 days after the procedure. These should all be global/no charges if no other complaints were addressed, not 99213s etc.
- If you do a multi-layer closure, there is a CPT code for this as well. (ex 12032 for 3 cm wound on back - $483)
References:
- Medical Economics Jul 2017
ICD10: Pre-op edit
- Z01.810, "Encounter for preprocedural cardiovascular examination."
- Z01.811, "Encounter for preprocedural respiratory examination."
- Z01.812, "Encounter for preprocedural laboratory examination."
- Z01.818, "Encounter for other preprocedural examination."
DCF Contact edit 2024
- Abuse Hotline - 1-800-962-2873
- Suicide Prevention - 1-800-273-8255
- Domestic Violence Hotline - 1-800-500-1119
- Background Screening - 1-888-352-2849
Human Trafficking (Orange/Osceola)
- Sue Aboul-hosn, BSSW, CSW
- Regional Human Trafficking Coordinator
- 400 West Robinson Street, South Tower 936K, Orlando, FL 32801
- sue.aboul-hosn@myflfamilies.com
- P: (407) 719-4228
- Katelyn Lee
- Regional Human Trafficking Coordinator
- 882 South Kirkman Road, Suite 200, Orlando, FL 32811
- Katelyn.Lee@myflfamilies.com
- P: (863) 838-1829
Reference:
Disability Tools edit
- Psychosocial impact
- Fear-Avoidance Beliefs Questionnaire
- Assesses fear-avoidance beliefs about physical activity that contribute to back pain and disability
- https://www.sralab.org/rehabilitation-measures/fear-avoidance-beliefs-questionnaire
- Patient Health Questionnaire-9
- Used to diagnose depression and grade severity of symptoms
- https://www.mdcalc.com/calc/1725/phq9-patient-health-questionnaire9
- Fear-Avoidance Beliefs Questionnaire
- Patient-reported outcome measures
- Disabilities of the Arm, Shoulder, and Hand
- Measures severity of symptoms and ability to complete tasks using the upper extremities
- https://dash.iwh.on.ca/about-dash
- Health and Work Questionnaire
- Assesses workplace productivity in relation to worker health
- https://tobaccocontrol.bmj.com/content/suppl/2001/09/13/10.3.233.DC1/halpern.pdf
- Medical Outcomes Study 36-item short-form survey
- Measures quality of life
- https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form/survey-instrument.html
- Neck Disability Index
- Measures how neck pain affects ADL
- https://www.smcnd.org/assets/docs/pt/neck_disability_index.pdf
- Örebro Musculoskeletal Pain Questionnaire
- Predicts long-term disability and work absenteeism in adults with acute and chronic musculoskeletal pain following injury
- https://aci.health.nsw.gov.au/__data/assets/pdf_file/0004/212908/Orebro_musculoskeletal_pain_questionnaire_Final.pdf
- Oswestry Disability Index
- Measures permanent functional disability in ADL due to low back pain
- https://www.aaos.org/globalassets/quality-and-practice-resources/patient-reported-outcome-measures/spine/oswestry-2.pdf
- Pain Disability Index
- Measures disruptions to ADL due to chronic pain
- https://www.med.umich.edu/1info/FHP/practiceguides/pain/detpdi.pdf
- Patient-Reported Outcomes Measurement Information System
- Evaluates and monitors physical, mental, and social health
- https://www.healthmeasures.net/index.php
- Patient-Specific Functional Scale
- Quantifies activity limitations and measures functional outcomes for patients with orthopedic conditions
- https://www.sralab.org/sites/default/files/2017-06/Patient-specific.pdf
- Roland Morris Disability Questionnaire
- Measures disability related to low back pain
- https://www.rmdq.org
- Tampa Scale of Kinesiophobia
- Evaluates fear of movement or physical activity and fear-related avoidance in patients with chronic musculoskeletal pain
- https://novopsych.com.au/assessments/health/tampa-scale-of-kinesiophobia-tsk
- Work Ability Index
- Assesses work ability
- https://workbox.chrodis.eu/repository/pdf/WAI_Work-Ability-Index.pdf
- Disabilities of the Arm, Shoulder, and Hand
- Activity limitations, participation restrictions
- Functional capacity evaluation
- Evaluates functional capacity in relation to job demands
- https://www.physio-pedia.com/Functional_Capacity_Evaluation
- Functional capacity evaluation
Reference:
- Am Fam Physician. 2023;107(5):490-498
Executive Physical Exam edit
An executive check-up typically includes a comprehensive set of tests and assessments tailored to the individual's age, sex, medical history, and lifestyle factors.
Below is a list of commonly ordered tests and procedures during an executive check-up:
- Physical Examination: A physician conducts a thorough assessment of overall health, observing general appearance, signs of distress, and overall demeanor.
- Complete Blood Count (CBC): This test evaluates different components of the blood, such as red and white blood cells and platelets, helping detect conditions like anemia or infections.
- Urinalysis: This test checks for abnormalities in the urine, which may indicate infections, diabetes, or kidney issues.
- Fecal Occult Blood Test: This test detects hidden blood in the stool, which can be a sign of gastrointestinal issues or colorectal cancer.
- Lipid Profile: This test measures cholesterol and triglyceride levels, which are important indicators of cardiovascular health.
- Fasting Blood Sugar: This test assesses blood glucose levels to screen for diabetes or prediabetes.
- Oral Glucose Tolerance Test: This test measures how well the body processes sugar over time and is used to diagnose diabetes.
- Electrocardiogram (ECG): This test evaluates heart function and can detect potential heart problems such as arrhythmias or previous heart attacks.
- Chest X-ray: This imaging test is used to examine the lungs and heart, identifying issues such as infections, tumors, or heart enlargement.
- Creatinine Test: This test measures kidney function by evaluating creatinine levels in the blood.
- Liver Function Tests: These tests assess liver health by measuring levels of bilirubin and other substances in the blood.
- Thyroid Function Tests: These tests evaluate thyroid hormone levels to detect hypothyroidism or hyperthyroidism.
- Pap Smear: This test screens for cervical cancer in women and may include HPV testing.
- Mammogram: This imaging test is used for breast cancer screening in women.
- Prostate-Specific Antigen (PSA) Test: This blood test screens for prostate cancer in men.
- Colonoscopy: This procedure examines the large intestine for signs of cancer or other abnormalities, especially recommended for individuals with a family history of colon cancer or gastrointestinal symptoms.
- Ultrasound: This imaging technique can evaluate various organs, such as the thyroid, breasts, or abdomen, depending on individual risk factors.
- Computed Tomography (CT) Scan: This imaging test can detect issues in muscles, bones, and internal organs, including tumors or blood clots.
- Magnetic Resonance Imaging (MRI): This imaging technique provides detailed images of organs and tissues, useful for evaluating the brain, spinal cord, and other areas.
- Bone Density Test: This test measures bone mineral density to assess for osteoporosis, especially in older adults.
- Vision and Hearing Tests: These assessments evaluate sensory functions and can identify early signs of deterioration.
These tests are designed to provide a comprehensive overview of an individual's health, detect early signs of disease, and guide preventive care strategies. The specific tests included may vary depending on the healthcare provider and the individual's unique health profile.
Family Medicine and AAFP
Family Medicine in Florida:
- $12.7 billion in Direct and Indirect Economic Output
- 81,322 of Jobs/Direct and Indirect Positions
- $5.7 billion in Direct and Indirect Wages and Benefits
- Average FP has 84 total patient encounters
Health is Primary
Only 3% of health care spending is tied to prevention and public health 75% of health care costs are spent treating preventable disease
Triple Aim - cost, quality, patient experience
- Better Health
- Areas with more PCP/person have lower death rates for cancer, heart disease, stroke, and less likely to be hospitalized
- Better Care
- Increase of 1 PCP/10,000 reduces outpatient visits by 5%, inpatient admissions by 5.5%, ER visits by 10.9%, and surgeries by 7.2%
- Primary care is associated with a more equitable distribution of health in populations
- Lower Costs
- US Adults with a PCP have 33% lower health care costs
Movie Medicine
- Hodor from Game of Thrones = Brocas aphasia
General Differential Diagnosis
DDx:
- Vascular
- Infection
- Neoplastic
- Degenerative
- Iatrogenic/Intoxication
- Congenital
- Autoimmune
- Traumatic
- Endocrine/Metabolic
Top 7 Diagnoses in FM
- HTN
- HLD
- CHF
- CAD
- Asthma/COPD
- DM
- Depression
Top 10 Diagnoses
- HTN
- HLD
- CHF
- CAD
- Asthma/COPD
- DM
- Depression
- Pain management
- Weight management
- Tobacco
Top 20 admitting diagnoses at Community Hospitals
- Coronary atherosclerosis and other heart disease
- PNA
- CHF
- Acute MI
- Trauma to perineum and vulva
- Acute cerebrovascular disease
- Affective disorders and substance abuse
- Cardiac dysarrhythmias
- COPD and bronchiectasis
- Spondylosis, intervertebral disc disorders, and other back problems
- Nonspecific chest pain
- Fluid and electrolyte disorders
- Biliary tract disorders
- Complication of device, implant, or graft
- Septicemia
- Asthma
- Osteoarthritis
- Urinary tract infections
- Diabetes mellitus
- Fracture of neck of femur
References:
- 2000 Agency for Healthcare Research and Quality
Journals that publish case reports
| Family Practice Journals | Publish Case Reports? | Notes |
|---|---|---|
| American Family Physician | Yes | Case reports are not featured as articles, although, a |
| brief case summary may be submitted in the form of a Letter to the Editor. | ||
| Family Medicine | No | |
| The Journal of Family Practice | Yes | Photo Rounds |
| Annals of Family Medicine | No | |
| The Journal of the American Medical Association | Yes | |
| The American Journal of Medicine | Yes | |
| The New England Journal of Medicine | Yes | |
| British Medical Journal | Yes | |
| Journal of the American Osteopathic Association | Yes | |
| Annals of Emergency Medicine | Yes |
Fun medical words
- Borborygmi - a rumbling or gurgling sound caused by the movement of gas in the intestines
- Echolalia
- Erythema ab igne - "red from fire" - reticulated, hyperpigmented patch caused by repeated exposure of the skin to a low-intensity heat source that is insufficient to burn the skin
- Piloerections - Goosebumps
- Melassasia furfur
- Bezoar -
- Plagiocephaly - funny shaped head
Favorite Patient Quotes
- "I need a refill on my birthday control"
- "My girlfriend is super hot and young"
- "I can picnic up water pills."
- "Please update his shit form…"
- "I want weightless shots"
- "thsnk yoy"
- "liquid bawl movement"
Federal Poverty Guidelines For 2023
| Persons In Family Household | Poverty Guideline Salary per year |
|---|---|
| 1 | $14,580 |
| 2 | $19,720 |
| 3 | $24,860 |
| 4 | $30,000 |
| 5 | $35,140 |
| 6 | $40,280 |
| 7 | $45,420 |
| 8 | $50,560 |
First Aid Kits edit 2025
The Red Cross recommends that all first aid kits for a family of four include the following:
- 2 absorbent compress dressings (5 x 9 inches)
- 25 adhesive bandages (assorted sizes), also found within our Family First Aid Kit
- 1 adhesive cloth tape (10 yards x 1 inch)
- 5 antibiotic ointment packets (approximately 1 gram)
- 5 antiseptic wipe packets
- 2 packets of aspirin (81 mg each)
- 1 emergency blanket
- 1 breathing barrier (with one-way valve)
- 1 instant cold compress
- 2 pair of nonlatex gloves (size: large)
- 2 hydrocortisone ointment packets (approximately 1 gram each)
- 1 3 in. gauze roll (roller) bandage
- 1 roller bandage (4 inches wide)
- 5 3 in. x 3 in. sterile gauze pads
- 5 sterile gauze pads (4 x 4 inches)
- Oral thermometer (non-mercury/nonglass)
- 2 triangular bandages
- Tweezers
- Emergency First Aid instructions
Reference:
FL Emergency Kit Components edit
FL Emergency Kit:
- Water:
- Enough for drinking, cooking and sanitation purposes—pack a minimum of 1 gallon daily per person for 7 days.
- Food:
- Non-perishable packaged or canned food and juices, snacks and foods for those with dietary restrictions (e.g., infants and people with diabetes).
- Cooking Supplies:
- Manual can opener, cooking tools and fuel, paper plates, and plastic utensils.
- Flashlight and Extra Batteries
- Pillows, Blankets and/or Sleeping Bags
- Clothing:
- Complete change of clothes suitable for the current climate and include sturdy shoes to protect feet from debris or other sharp objects post-storm.
- First Aid Kit, Prescription Medication, and Other Medicines:
- Include a first aid kit and plan to bring medications that you need. After a storm, you may have limited supplies of your prescription medications and your local pharmacy may close. Keep an updated list of each medication you take, its dosing instructions, and the name and contact information of the prescribing doctor.
- Radio:
- Battery operated and NOAA weather radio.
- Toiletries
- Cleaning Supplies:
- Garbage bags, moisture wipes and other items.
- Cash:
- Banks and ATMs may not be open or available for extended periods following a disaster.
- Important Documents:
- Store all critical documents in a waterproof container and save electronically. Documents like insurance, medical records, bank account numbers, Social Security card, etc.
- Contact List:
- Keep an updated list of all important contacts, including doctors, friends, relatives, out-of-state friends, or relatives.
- Special Items:
- Assess all family member needs. Plan for infants, elderly and individuals with access and functional needs (e.g., medical items and baby bottles).
- Pet Care Items:
- Proper identification, immunization records, ample supply of food and water, carrier or cage, medications, muzzle and leash, and a photo of you and your pet together to validate ownership.
Contact: During severe weather and other emergencies, the State Assistance Information Line (SAIL), a toll-free hotline, is activated to provide accurate and up-to-date information on emergency or disaster situations impacting the State of Florida.
- The SAIL hotline is: 1-800-342-3557
You can also get helpful information from the Department's Emergency Information webpage. Additionally, one of the fastest ways to receive accurate health-related information is to monitor @HealthyFla on Twitter and on Facebook.
Reference:
- Florida Division of Emergency Management
- 2555 Shumard Oak Blvd. Tallahassee, Florida 32399-2100
- Phone: 850-815-4000
- https://www.floridadisaster.org/planprepare/hurricane-supply-checklist/
Florida Things that Bite edit
- Spiders
- Widow Spiders
- There are four species of widow spiders in Florida:
- Latrodectus mactans, the southern black widow
- Latrodectus bishopi, the red widow
- Latrodectus variolus, the northern black widow
- Latrodectus geometricus, the brown widow
- There are four species of widow spiders in Florida:
- Recluse Spiders
- The brown recluse has been found in Alachua, Bay, Duval, Jefferson and Leon counties. It typically has a dark violin-shaped mark, although the color is variable.
- The Mediterranean recluse has been found in Dade, Escambia, Orange and Osceola counties. It is very similar in appearance to the brown recluse, but the violin mark tends to be lighter in color and has parallel sides.
- The Chilean recluse has only recently been found in Florida, in Polk County. It is the largest and most dangerous of the recluse species. The violin mark of this species is dark and wider in front than behind.
- Widow Spiders
- Ticks
- Most people are infected by nymphal stages during the spring and summer. Nymphs are often small enough to escape notice and so can stay attached longer than adults, increasing risk of disease transmission.
Reference:
Fun Medical Definitions
- obdormition
- Numbness of an extremity due to pressure on the sensory nerve.
- From wikipedia: Obdormition (ˌɒbdɔːrˈmɪʃən; from Latin obdormire "to fall asleep") is a medical term describing numbness in a limb, often caused by constant pressure on nerves or lack of movement.[1] This is colloquially referred to as the limb "going to sleep" and is usually followed by paresthesia, colloquially called "pins and needles".
- https://en.wikipedia.org/wiki/Obdormition
Grandmother's Rules of Life edit
See also:
Rules of Life
- Get enough sleep - 7-9 hrs a night
- Eat vegetables
- Have friends - Be social
- Be active
- Don't smoke
- Avoid EtOH
- Everything in moderation
- Sicker people get sicker
Reference:
- Dennis M
Health Insurance Analysis (Opinionated)
| HDHP | Silver | Gold | |
|---|---|---|---|
| Monthly Rate | $ | $$ | $$$ |
| Deductible | $$$ | $$ | $ |
| Year Out of Pocket | $ | $$ | $$$ |
- Typical Best Coverage:
- HDHP + DPC +/- HSA
- Typical Second Best
- DPC + Health Share Plan
- DPC + Supplemental Health Insurance
- Ok Coverage
- DPC (Primary Care only)
Homeless Resources
- Homeless Shelter Directory
- National Domestic Violence Hotline (800-799-7233)
- Health Care for the Homeless
Reference:
- AFP Vol 106 No 6 Dec 2022
HSA Is OK With DPC Edit
- So the irs document 213(d) https://bit.ly/3esjusv
- Makes it very clear that payments to physicians are an allowed deductible insurance.
- Then if you look at IRS document 502, http://www.irs.gov/pub/irs-pdf/p502.pdf
- Medical expenses are the costs of diagnosis, cure, mitigation, treatment, or prevention of disease, and the costs for treatments affecting any part or function of the body. These expenses include payments for legal medical services rendered by physicians, surgeons, dentists, and other medical practitioners. They include the costs of equipment, supplies, and diagnostic devices needed for these purposes.
- So for those reasons, we are confident that HSAs can be used in combination with DPC.
Human Trafficking edit
If the patient answers yes to the assessment questions or your findings suggest that the individual may be a victim of human trafficking, you should call the National Human Trafficking Hotline at 1-888-373-7888 or via text telephone by dialing 711. You can also send a text message to 233733. You will be asked to provide basic information regarding the situation, including (National Human Trafficking Hotline, n.d.):
- the location of the suspected trafficking
- the name of the suspected trafficker if possible
- your city and state
- how you learned about the hotline
Since health care professionals are mandated reporters under child abuse and neglect laws, practitioners who know or suspect that a minor is being abused, neglected, or abandoned should immediately report their concerns to law enforcement or the appropriate child welfare agency. The Florida Department of Children and Families Abuse Hotline can be reached by calling 1-800-96-ABUSE or by using the online reporting tool (Florida Department of Children and Families, n.d.).
Human Trafficking edit
- Free the Slaves:
- Polaris Project:
- Stop the Traffik:
Resources for Providers
- National Human Trafficking Resource Center's referral database
Emergency Shelter and Crisis Services
Abuse Counseling and Treatment, Inc.
Hotline: 239-939-3112
Phone: 239-939-2553
P.O. Box 60401
Fort Meyers, FL 33906
Website: http://www.actabuse.com/
Ark of Freedom Alliance
Hotline: 954-778-2871
Phone: 954-778-2871
101 NE Third Avenue, Suite 1500
Fort Lauderdale, FL 33301
Website: www.aofalliance.org/
Camillus House
Phone: 305-374-1065
Overnight Shelter
1603 NW Seventh Avenue
Miami, FL 33136
Camillus Health
336 NW Fifth Street
Miami, FL 33128
Capital City Youth
Hotline: 850-576-6000
Phone: 850-576-6000
2407 Roberts Avenue
Tallahassee, FL 32310
Website: http://www.ccys.org/
Children's Home Society
Main Office: 321-397-3000
482 Keller Rd.
Orlando, FL 32810
To locate nearest local office: https://www.chsfl.org/find-your-location/
Created Gainesville, Inc.
Phone: 352-870-8481
Hotline: 855-4-BE-FREE
P.O. Box 6013
Gainesville, FL 32627
Website: https://www.createdgainesville.com/
Created Women, Inc.
Phone: 813-379-2975
Hotline: 813-379-2975
P.O. Box 5717
Tampa, FL 33675
Website: http://www.createdwomen.com/
Florida Department of Children and Families
Phone: 850-300-4323
Hotline: 800-962-2873
1317 Winewood Blvd.
Tallahassee, FL 32399
Website: https://www.myflfamilies.com/
International Rescue Committee
Phone: 305-640-9881
P.O. Box 453504
Miami, FL 33245
Website: https://www.rescue.org/united-states/miami-fl
Miami-Dade County Coordinated Victims Assistance Center
Phone: 305-285-5900
More Too Life, Inc.
Phone: 941-227-1012
Hotline: 888-544-2872
1750 17th Street, Building F
Sarasota, FL 34234
Website: https://moretoolife.org/
Nancy J. Cotterman Center
400 N.E. Fourth Street
Fort Lauderdale, FL 33301
Phone: 954-357-5775
Website: https://www.broward.org/nancyjcottermancenter/
121 Hope (Northland Church)
Phone: 407-949-7200
530 Dog Track Road
Longwood, FL 32750
Website: http://www.121hope.com/
One More Child
Phone: 863-687-8811
P.O. Box 8190
Lakeland, FL 33802
Website: https://onemorechild.org/
Path2Freedom, Inc.
Phone: 239-398-9961
1200 Goodlette Road N. #9916
Naples, FL 94101
Website: https://www.path2freedom.org/
Greater Orlando Human Trafficking Task Force
Phone: 407-836-7200
The Shelter for Abused Women and Children
Hotline: 239-775-1101
Naples Administration and Outreach Office: 239-775-3862
Immokalee Outreach Office: 239-657-5700
P.O. Box 10102
Naples, FL 34101
Website: https://naplesshelter.org/
United Abolitionists
Hotline: 833-9-STOP-HT
Phone: 407-495-5846
P.O. Box 536832
Orlando, FL 32853
Website: https://www.unitedabolitionists.com/
Legal Services
Abuse Counseling and Treatment, Inc.
Hotline: 239-939-3112
Phone: 239-939-2553
P.O. Box 60401
Fort Meyers, FL 33906
Website: http://www.actabuse.com/
Americans for Immigrant Justice
Phone: 305-573-1106
6355 NW 36th Street, Suite 2201
Miami, FL 33166
Website: http://www.aijustice.org/
Catholic Charities
Palm Beach Diocese
Phone: 561-345-2000
P.O. Box 109650
Palm Beach Gardens, FL 33410
Website: https://www.ccdpb.org/
Diocese of Venice
239-334-2234 (Fort Meyers)
239-390-2928 (Bonita Springs)
Website: https://catholiccharitiesdov.org/
Gulf Coast Legal Services
Phone:
Pinellas Office 727-821-0726
Manasota Office 941-746-6151
Wimauma Office 727-821-0726
Lealman Office 727-821-0726
Website: https://gulfcoastlegal.org/
International Rescue Committee
Phone: 305-640-9881
P.O. Box 453504
Miami, FL 33245
Website: https://www.rescue.org/united-states/miami-fl
Lutheran Services Florida
Phone: 813-875-1408
3627 W. Waters Ave.
Tampa, FL 33614
Website: https://www.lsfnet.org/
Miami-Dade County Coordinated Victims Assistance Center
Phone: 305-285-5900
More Too Life, Inc.
Phone: 941-227-1012
Hotline: 888-544-2872
1750 17th Street, Building F
Sarasota, FL 34234
Website: https://moretoolife.org/
Greater Orlando Human Trafficking Task Force
Phone: 407-836-7200
The Shelter for Abused Women and Children
Hotline: 239-775-1101
Naples Administration and Outreach Office: 239-775-3862
Immokalee Outreach Office: 239-657-5700
P.O. Box 10102
Naples, FL 34101
Website: https://naplesshelter.org/
Mental Health Services
Abuse Counseling and Treatment, Inc.
Hotline: 239-939-3112
Phone: 239-939-2553
P.O. Box 60401
Fort Meyers, FL 33906
Website: http://www.actabuse.com/
Ark of Freedom Alliance
Hotline: 954-778-2871
Phone: 954-778-2871
101 NE Third Avenue, Suite 1500
Fort Lauderdale, FL 33301
Website: www.aofalliance.org/
Bikers Against Trafficking
Phone: 407-300-8971
1349 S. International Parkway, Suite 2421
Lake Mary, FL 32746
Website: https://bikersagainsttrafficking.org/
Capital City Youth
Hotline: 850-576-6000
Phone: 850-576-6000
2407 Roberts Avenue
Tallahassee, FL 32310
Website: http://www.ccys.org/
Catholic Charities
Palm Beach Diocese
Phone: 561-345-2000
P.O. Box 109650
Palm Beach Gardens, FL 33410
Website: https://www.ccdpb.org/
Diocese of Venice
239-334-2234 (Fort Meyers)
239-390-2928 (Bonita Springs)
Website: https://catholiccharitiesdov.org/
Children's Home Society
Main Office: 321-397-3000
482 Keller Rd.
Orlando, FL 32810
To locate nearest local office: https://www.chsfl.org/find-your-location/
Created Gainesville, Inc.
Phone: 352-870-8481
Hotline: 855-4-BE-FREE
P.O. Box 6013
Gainesville, FL 32627
Website: https://www.createdgainesville.com/
Created Women, Inc.
Phone: 813-379-2975
Hotline: 813-379-2975
P.O. Box 5717
Tampa, FL 33675
Website: http://www.createdwomen.com/
Devereux Advanced Behavioral Health
Phone: 800-338-3738 ext. 77130
Locations throughout Florida
Website: https://www.devereux.org/site/SPageServer/
Glory House
Miami, FL
Phone: 786-505-4681
Website: https://www.gloryhouseofmiami.org/
Hepzibah House
Phone: 561-386-0031
1530 W. Boynton Beach Blvd., #3863
Boynton Beach, FL 33424
Website: https://hepzibahhouse.org/
International Rescue Committee
Phone: 305-640-9881
P.O. Box 453504
Miami, FL 33245
Website: https://www.rescue.org/united-states/miami-fl
Kristi House
Phone: 305-547-6800
1265 NW 12th Ave.
Miami, FL 33136
Website: https://kristihouse.org/
Miami-Dade County Coordinated Victims Assistance Center
Phone: 305-285-5900
More Too Life, Inc.
Phone: 941-227-1012
Hotline: 888-544-2872
1750 17th Street, Building F
Sarasota, FL 34234
Website: https://moretoolife.org/
Nancy J. Cotterman Center
400 N.E. Fourth Street
Fort Lauderdale, FL 33301
Phone: 954-357-5775
Website: https://www.broward.org/nancyjcottermancenter/
121 Hope (Northland Church)
Phone: 407-949-7200
530 Dog Track Road
Longwood, FL 32750
Website: http://www.121hope.com/
One More Child
Phone: 863-687-8811
P.O. Box 8190
Lakeland, FL 33802
Website: https://onemorechild.org/
Path2Freedom, Inc.
Phone: 239-398-9961
1200 Goodlette Road N. #9916
Naples, FL 94101
Website: https://www.path2freedom.org/
Selah Freedom
Phone: 888-8-FREE-ME
P.O. Box 21415
Sarasota, FL 34276
Website: https://www.selahfreedom.com/
Greater Orlando Human Trafficking Task Force
Phone: 407-836-7200
The Shelter for Abused Women and Children
Hotline: 239-775-1101
Naples Administration and Outreach Office: 239-775-3862
Immokalee Outreach Office: 239-657-5700
P.O. Box 10102
Naples, FL 34101
Website: https://naplesshelter.org/
United Abolitionists
Hotline: 833-9-STOP-HT
Phone: 407-495-5846
P.O. Box 536832
Orlando, FL 32853
Website: https://www.unitedabolitionists.com/
Wings of Shelter
Phone: 239-340-2980
21301 S. Tamiami Trail, Suite 320
Estero, FL 33928
Website: http://wingsofshelter.com/index.html
Miscellaneous Services
Addiction Treatment/Services Health Care Case Management Child Care Education/Job Training Family Reunification Interpretation/Translation Long-term Housing Repatriation Survivor Leadership Transitional Housing Transportation Assistance
(Contact provider for specific services offered.)
Abuse Counseling and Treatment, Inc.
Hotline: 239-939-3112
Phone: 239-939-2553
P.O. Box 60401
Fort Meyers, FL 33906
Website: http://www.actabuse.com/
Ark of Freedom Alliance
Hotline: 954-778-2871
Phone: 954-778-2871
101 NE Third Avenue, Suite 1500
Fort Lauderdale, FL 33301
Website: www.aofalliance.org/
Bethany Christian Services
Central Florida: 407-877-4006
South Florida: 954-315-1759
Gulf Coast: 850-478-6789
Website: https://bethany.org/
Bikers Against Trafficking
Phone: 407-300-8971
1349 S. International Parkway, Suite 2421
Lake Mary, FL 32746
Website: https://bikersagainsttrafficking.org/
Camillus House
Phone: 305-374-1065
Overnight Shelter
1603 NW Seventh Avenue
Miami, FL 33136
Camillus Health
336 NW Fifth Street
Miami, FL 33128
Capital City Youth
Hotline: 850-576-6000
Phone: 850-576-6000
2407 Roberts Avenue
Tallahassee, FL 32310
Website: http://www.ccys.org/
Catholic Charities
Palm Beach Diocese
Phone: 561-345-2000
P.O. Box 109650
Palm Beach Gardens, FL 33410
Website: https://www.ccdpb.org/
Diocese of Venice
239-334-2234 (Fort Meyers)
239-390-2928 (Bonita Springs)
Website: https://catholiccharitiesdov.org/
Children's Home Society
Main Office: 321-397-3000
482 Keller Rd.
Orlando, FL 32810
To locate nearest local office: https://www.chsfl.org/find-your-location/
Created Gainesville, Inc.
Phone: 352-870-8481
Hotline: 855-4-BE-FREE
P.O. Box 6013
Gainesville, FL 32627
Website: https://www.createdgainesville.com/
Created Women, Inc.
Phone: 813-379-2975
Hotline: 813-379-2975
P.O. Box 5717
Tampa, FL 33675
Website: http://www.createdwomen.com/
Devereux Advanced Behavioral Health
Phone: 800-338-3738 ext. 77130
Locations throughout Florida
Website: https://www.devereux.org/site/SPageServer/
Florida Department of Children and Families
Phone: 850-300-4323
Hotline: 800-962-2873
1317 Winewood Blvd.
Tallahassee, FL 32399
Website: https://www.myflfamilies.com/
Glory House
Miami, FL
Phone: 786-505-4681
Website: https://www.gloryhouseofmiami.org/
Greater Orlando Human Trafficking Task Force
Phone: 407-836-7200
Gulf Coast Legal Services
Phone:
Pinellas Office 727-821-0726
Manasota Office 941-746-6151
Wimauma Office 727-821-0726
Lealman Office 727-821-0726
Website: https://gulfcoastlegal.org/
Hepzibah House
Phone: 561-386-0031
1530 W. Boynton Beach Blvd., #3863
Boynton Beach, FL 33424
Website: https://hepzibahhouse.org/
International Rescue Committee
Phone: 305-640-9881
P.O. Box 453504
Miami, FL 33245
Website: https://www.rescue.org/united-states/miami-fl
Kristi House
Phone: 305-547-6800
1265 NW 12th Ave.
Miami, FL 33136
Website: https://kristihouse.org/
Lutheran Services Florida
Phone: 813-875-1408
3627 W. Waters Ave.
Tampa, FL 33614
Website: https://www.lsfnet.org/
Miami-Dade County Coordinated Victims Assistance Center
Phone: 305-285-5900
More Too Life, Inc.
Phone: 941-227-1012
Hotline: 888-544-2872
1750 17th Street, Building F
Sarasota, FL 34234
Website: https://moretoolife.org/
Nancy J. Cotterman Center
400 N.E. Fourth Street
Fort Lauderdale, FL 33301
Phone: 954-357-5775
Website: https://www.broward.org/nancyjcottermancenter/
121 Hope (Northland Church)
Phone: 407-949-7200
530 Dog Track Road
Longwood, FL 32750
Website: http://www.121hope.com/
One More Child
Phone: 863-687-8811
P.O. Box 8190
Lakeland, FL 33802
Website: https://onemorechild.org/
Path2Freedom, Inc.
Phone: 239-398-9961
1200 Goodlette Road N. #9916
Naples, FL 94101
Website: https://www.path2freedom.org/
Selah Freedom
Phone: 888-8-FREE-ME
P.O. Box 21415
Sarasota, FL 34276
Website: https://www.selahfreedom.com/
Survive and Thrive Advocacy Center
Phone: 850-597-2080
Website: https://www.surviveandthriveadvocacy.org/
The Shelter for Abused Women and Children
Hotline: 239-775-1101
Naples Administration and Outreach Office: 239-775-3862
Immokalee Outreach Office: 239-657-5700
P.O. Box 10102
Naples, FL 34101
Website: https://naplesshelter.org/
United Abolitionists
Hotline: 833-9-STOP-HT
Phone: 407-495-5846
P.O. Box 536832
Orlando, FL 32853
Website: https://www.unitedabolitionists.com/
Victim Service Center of Central Florida
Hotline: 407-500-HEAL
Website: https://www.victimservicecenter.org/
Wings of Shelter
Phone: 239-340-2980
21301 S. Tamiami Trail, Suite 320
Estero, FL 33928
Website: http://wingsofshelter.com/index.html
Human Trafficking edit
Human Trafficking edit
If the patient answers yes to the assessment questions or your findings suggest that the individual may be a victim of human trafficking, you should call the National Human Trafficking Hotline at 1-888-373-7888 or via text telephone by dialing 711. You can also send a text message to 233733. You will be asked to provide basic information regarding the situation, including (National Human Trafficking Hotline, n.d.):
- the location of the suspected trafficking
- the name of the suspected trafficker if possible
- your city and state
- how you learned about the hotline
Since health care professionals are mandated reporters under child abuse and neglect laws, practitioners who know or suspect that a minor is being abused, neglected, or abandoned should immediately report their concerns to law enforcement or the appropriate child welfare agency. The Florida Department of Children and Families Abuse Hotline can be reached by calling 1-800-96-ABUSE or by using the online reporting tool (Florida Department of Children and Families, n.d.).
Human Trafficking edit
- Free the Slaves:
- Polaris Project:
- Stop the Traffik:
Resources for Providers
- National Human Trafficking Resource Center's referral database
Emergency Shelter and Crisis Services
Abuse Counseling and Treatment, Inc.
Hotline: 239-939-3112
Phone: 239-939-2553
P.O. Box 60401
Fort Meyers, FL 33906
Website: http://www.actabuse.com/
Ark of Freedom Alliance
Hotline: 954-778-2871
Phone: 954-778-2871
101 NE Third Avenue, Suite 1500
Fort Lauderdale, FL 33301
Website: www.aofalliance.org/
Camillus House
Phone: 305-374-1065
Overnight Shelter
1603 NW Seventh Avenue
Miami, FL 33136
Camillus Health
336 NW Fifth Street
Miami, FL 33128
Capital City Youth
Hotline: 850-576-6000
Phone: 850-576-6000
2407 Roberts Avenue
Tallahassee, FL 32310
Website: http://www.ccys.org/
Children's Home Society
Main Office: 321-397-3000
482 Keller Rd.
Orlando, FL 32810
To locate nearest local office: https://www.chsfl.org/find-your-location/
Created Gainesville, Inc.
Phone: 352-870-8481
Hotline: 855-4-BE-FREE
P.O. Box 6013
Gainesville, FL 32627
Website: https://www.createdgainesville.com/
Created Women, Inc.
Phone: 813-379-2975
Hotline: 813-379-2975
P.O. Box 5717
Tampa, FL 33675
Website: http://www.createdwomen.com/
Florida Department of Children and Families
Phone: 850-300-4323
Hotline: 800-962-2873
1317 Winewood Blvd.
Tallahassee, FL 32399
Website: https://www.myflfamilies.com/
International Rescue Committee
Phone: 305-640-9881
P.O. Box 453504
Miami, FL 33245
Website: https://www.rescue.org/united-states/miami-fl
Miami-Dade County Coordinated Victims Assistance Center
Phone: 305-285-5900
More Too Life, Inc.
Phone: 941-227-1012
Hotline: 888-544-2872
1750 17th Street, Building F
Sarasota, FL 34234
Website: https://moretoolife.org/
Nancy J. Cotterman Center
400 N.E. Fourth Street
Fort Lauderdale, FL 33301
Phone: 954-357-5775
Website: https://www.broward.org/nancyjcottermancenter/
121 Hope (Northland Church)
Phone: 407-949-7200
530 Dog Track Road
Longwood, FL 32750
Website: http://www.121hope.com/
One More Child
Phone: 863-687-8811
P.O. Box 8190
Lakeland, FL 33802
Website: https://onemorechild.org/
Path2Freedom, Inc.
Phone: 239-398-9961
1200 Goodlette Road N. #9916
Naples, FL 94101
Website: https://www.path2freedom.org/
Greater Orlando Human Trafficking Task Force
Phone: 407-836-7200
The Shelter for Abused Women and Children
Hotline: 239-775-1101
Naples Administration and Outreach Office: 239-775-3862
Immokalee Outreach Office: 239-657-5700
P.O. Box 10102
Naples, FL 34101
Website: https://naplesshelter.org/
United Abolitionists
Hotline: 833-9-STOP-HT
Phone: 407-495-5846
P.O. Box 536832
Orlando, FL 32853
Website: https://www.unitedabolitionists.com/
Legal Services
Abuse Counseling and Treatment, Inc.
Hotline: 239-939-3112
Phone: 239-939-2553
P.O. Box 60401
Fort Meyers, FL 33906
Website: http://www.actabuse.com/
Americans for Immigrant Justice
Phone: 305-573-1106
6355 NW 36th Street, Suite 2201
Miami, FL 33166
Website: http://www.aijustice.org/
Catholic Charities
Palm Beach Diocese
Phone: 561-345-2000
P.O. Box 109650
Palm Beach Gardens, FL 33410
Website: https://www.ccdpb.org/
Diocese of Venice
239-334-2234 (Fort Meyers)
239-390-2928 (Bonita Springs)
Website: https://catholiccharitiesdov.org/
Gulf Coast Legal Services
Phone:
Pinellas Office 727-821-0726
Manasota Office 941-746-6151
Wimauma Office 727-821-0726
Lealman Office 727-821-0726
Website: https://gulfcoastlegal.org/
International Rescue Committee
Phone: 305-640-9881
P.O. Box 453504
Miami, FL 33245
Website: https://www.rescue.org/united-states/miami-fl
Lutheran Services Florida
Phone: 813-875-1408
3627 W. Waters Ave.
Tampa, FL 33614
Website: https://www.lsfnet.org/
Miami-Dade County Coordinated Victims Assistance Center
Phone: 305-285-5900
More Too Life, Inc.
Phone: 941-227-1012
Hotline: 888-544-2872
1750 17th Street, Building F
Sarasota, FL 34234
Website: https://moretoolife.org/
Greater Orlando Human Trafficking Task Force
Phone: 407-836-7200
The Shelter for Abused Women and Children
Hotline: 239-775-1101
Naples Administration and Outreach Office: 239-775-3862
Immokalee Outreach Office: 239-657-5700
P.O. Box 10102
Naples, FL 34101
Website: https://naplesshelter.org/
Mental Health Services
Abuse Counseling and Treatment, Inc.
Hotline: 239-939-3112
Phone: 239-939-2553
P.O. Box 60401
Fort Meyers, FL 33906
Website: http://www.actabuse.com/
Ark of Freedom Alliance
Hotline: 954-778-2871
Phone: 954-778-2871
101 NE Third Avenue, Suite 1500
Fort Lauderdale, FL 33301
Website: www.aofalliance.org/
Bikers Against Trafficking
Phone: 407-300-8971
1349 S. International Parkway, Suite 2421
Lake Mary, FL 32746
Website: https://bikersagainsttrafficking.org/
Capital City Youth
Hotline: 850-576-6000
Phone: 850-576-6000
2407 Roberts Avenue
Tallahassee, FL 32310
Website: http://www.ccys.org/
Catholic Charities
Palm Beach Diocese
Phone: 561-345-2000
P.O. Box 109650
Palm Beach Gardens, FL 33410
Website: https://www.ccdpb.org/
Diocese of Venice
239-334-2234 (Fort Meyers)
239-390-2928 (Bonita Springs)
Website: https://catholiccharitiesdov.org/
Children's Home Society
Main Office: 321-397-3000
482 Keller Rd.
Orlando, FL 32810
To locate nearest local office: https://www.chsfl.org/find-your-location/
Created Gainesville, Inc.
Phone: 352-870-8481
Hotline: 855-4-BE-FREE
P.O. Box 6013
Gainesville, FL 32627
Website: https://www.createdgainesville.com/
Created Women, Inc.
Phone: 813-379-2975
Hotline: 813-379-2975
P.O. Box 5717
Tampa, FL 33675
Website: http://www.createdwomen.com/
Devereux Advanced Behavioral Health
Phone: 800-338-3738 ext. 77130
Locations throughout Florida
Website: https://www.devereux.org/site/SPageServer/
Glory House
Miami, FL
Phone: 786-505-4681
Website: https://www.gloryhouseofmiami.org/
Hepzibah House
Phone: 561-386-0031
1530 W. Boynton Beach Blvd., #3863
Boynton Beach, FL 33424
Website: https://hepzibahhouse.org/
International Rescue Committee
Phone: 305-640-9881
P.O. Box 453504
Miami, FL 33245
Website: https://www.rescue.org/united-states/miami-fl
Kristi House
Phone: 305-547-6800
1265 NW 12th Ave.
Miami, FL 33136
Website: https://kristihouse.org/
Miami-Dade County Coordinated Victims Assistance Center
Phone: 305-285-5900
More Too Life, Inc.
Phone: 941-227-1012
Hotline: 888-544-2872
1750 17th Street, Building F
Sarasota, FL 34234
Website: https://moretoolife.org/
Nancy J. Cotterman Center
400 N.E. Fourth Street
Fort Lauderdale, FL 33301
Phone: 954-357-5775
Website: https://www.broward.org/nancyjcottermancenter/
121 Hope (Northland Church)
Phone: 407-949-7200
530 Dog Track Road
Longwood, FL 32750
Website: http://www.121hope.com/
One More Child
Phone: 863-687-8811
P.O. Box 8190
Lakeland, FL 33802
Website: https://onemorechild.org/
Path2Freedom, Inc.
Phone: 239-398-9961
1200 Goodlette Road N. #9916
Naples, FL 94101
Website: https://www.path2freedom.org/
Selah Freedom
Phone: 888-8-FREE-ME
P.O. Box 21415
Sarasota, FL 34276
Website: https://www.selahfreedom.com/
Greater Orlando Human Trafficking Task Force
Phone: 407-836-7200
The Shelter for Abused Women and Children
Hotline: 239-775-1101
Naples Administration and Outreach Office: 239-775-3862
Immokalee Outreach Office: 239-657-5700
P.O. Box 10102
Naples, FL 34101
Website: https://naplesshelter.org/
United Abolitionists
Hotline: 833-9-STOP-HT
Phone: 407-495-5846
P.O. Box 536832
Orlando, FL 32853
Website: https://www.unitedabolitionists.com/
Wings of Shelter
Phone: 239-340-2980
21301 S. Tamiami Trail, Suite 320
Estero, FL 33928
Website: http://wingsofshelter.com/index.html
Miscellaneous Services
- Addiction Treatment/Services
- Health Care
- Case Management
- Child Care
- Education/Job Training
- Family Reunification
- Interpretation/Translation
- Long-term Housing
- Repatriation
- Survivor Leadership
- Transitional Housing
- Transportation Assistance
(Contact provider for specific services offered.)
Abuse Counseling and Treatment, Inc.
Hotline: 239-939-3112
Phone: 239-939-2553
P.O. Box 60401
Fort Meyers, FL 33906
Website: http://www.actabuse.com/
Ark of Freedom Alliance
Hotline: 954-778-2871
Phone: 954-778-2871
101 NE Third Avenue, Suite 1500
Fort Lauderdale, FL 33301
Website: www.aofalliance.org/
Bethany Christian Services
Central Florida: 407-877-4006
South Florida: 954-315-1759
Gulf Coast: 850-478-6789
Website: https://bethany.org/
Bikers Against Trafficking
Phone: 407-300-8971
1349 S. International Parkway, Suite 2421
Lake Mary, FL 32746
Website: https://bikersagainsttrafficking.org/
Camillus House
Phone: 305-374-1065
Overnight Shelter
1603 NW Seventh Avenue
Miami, FL 33136
Camillus Health
336 NW Fifth Street
Miami, FL 33128
Capital City Youth
Hotline: 850-576-6000
Phone: 850-576-6000
2407 Roberts Avenue
Tallahassee, FL 32310
Website: http://www.ccys.org/
Catholic Charities
Palm Beach Diocese
Phone: 561-345-2000
P.O. Box 109650
Palm Beach Gardens, FL 33410
Website: https://www.ccdpb.org/
Diocese of Venice
239-334-2234 (Fort Meyers)
239-390-2928 (Bonita Springs)
Website: https://catholiccharitiesdov.org/
Children's Home Society
Main Office: 321-397-3000
482 Keller Rd.
Orlando, FL 32810
To locate nearest local office: https://www.chsfl.org/find-your-location/
Created Gainesville, Inc.
Phone: 352-870-8481
Hotline: 855-4-BE-FREE
P.O. Box 6013
Gainesville, FL 32627
Website: https://www.createdgainesville.com/
Created Women, Inc.
Phone: 813-379-2975
Hotline: 813-379-2975
P.O. Box 5717
Tampa, FL 33675
Website: http://www.createdwomen.com/
Devereux Advanced Behavioral Health
Phone: 800-338-3738 ext. 77130
Locations throughout Florida
Website: https://www.devereux.org/site/SPageServer/
Florida Department of Children and Families
Phone: 850-300-4323
Hotline: 800-962-2873
1317 Winewood Blvd.
Tallahassee, FL 32399
Website: https://www.myflfamilies.com/
Glory House
Miami, FL
Phone: 786-505-4681
Website: https://www.gloryhouseofmiami.org/
Greater Orlando Human Trafficking Task Force
Phone: 407-836-7200
Gulf Coast Legal Services
Phone:
Pinellas Office 727-821-0726
Manasota Office 941-746-6151
Wimauma Office 727-821-0726
Lealman Office 727-821-0726
Website: https://gulfcoastlegal.org/
Hepzibah House
Phone: 561-386-0031
1530 W. Boynton Beach Blvd., #3863
Boynton Beach, FL 33424
Website: https://hepzibahhouse.org/
International Rescue Committee
Phone: 305-640-9881
P.O. Box 453504
Miami, FL 33245
Website: https://www.rescue.org/united-states/miami-fl
Kristi House
Phone: 305-547-6800
1265 NW 12th Ave.
Miami, FL 33136
Website: https://kristihouse.org/
Lutheran Services Florida
Phone: 813-875-1408
3627 W. Waters Ave.
Tampa, FL 33614
Website: https://www.lsfnet.org/
Miami-Dade County Coordinated Victims Assistance Center
Phone: 305-285-5900
More Too Life, Inc.
Phone: 941-227-1012
Hotline: 888-544-2872
1750 17th Street, Building F
Sarasota, FL 34234
Website: https://moretoolife.org/
Nancy J. Cotterman Center
400 N.E. Fourth Street
Fort Lauderdale, FL 33301
Phone: 954-357-5775
Website: https://www.broward.org/nancyjcottermancenter/
121 Hope (Northland Church)
Phone: 407-949-7200
530 Dog Track Road
Longwood, FL 32750
Website: http://www.121hope.com/
One More Child
Phone: 863-687-8811
P.O. Box 8190
Lakeland, FL 33802
Website: https://onemorechild.org/
Path2Freedom, Inc.
Phone: 239-398-9961
1200 Goodlette Road N. #9916
Naples, FL 94101
Website: https://www.path2freedom.org/
Selah Freedom
Phone: 888-8-FREE-ME
P.O. Box 21415
Sarasota, FL 34276
Website: https://www.selahfreedom.com/
Survive and Thrive Advocacy Center
Phone: 850-597-2080
Website: https://www.surviveandthriveadvocacy.org/
The Shelter for Abused Women and Children
Hotline: 239-775-1101
Naples Administration and Outreach Office: 239-775-3862
Immokalee Outreach Office: 239-657-5700
P.O. Box 10102
Naples, FL 34101
Website: https://naplesshelter.org/
United Abolitionists
Hotline: 833-9-STOP-HT
Phone: 407-495-5846
P.O. Box 536832
Orlando, FL 32853
Website: https://www.unitedabolitionists.com/
Victim Service Center of Central Florida
Hotline: 407-500-HEAL
Website: https://www.victimservicecenter.org/
Wings of Shelter
Phone: 239-340-2980
21301 S. Tamiami Trail, Suite 320
Estero, FL 33928
Website: http://wingsofshelter.com/index.html
Informed Consent 2025
Obtain informed consent prior to performing a treatment and/or procedure. In the communications process, disclose and discuss with your patient:
- The patient's diagnosis, if known;
- The nature and purpose of a proposed treatment or procedure;
- The risks and benefits of a proposed treatment or procedure;
- Alternatives (regardless of their cost or the extent to which the treatment options are covered by health insurance);
- The risks and benefits of the alternative treatment or procedure; and
- The risks and benefits of not receiving or undergoing a treatment or procedure.
Informed consent is not the signing of a document, rather a process that leads to shared decision making between the patient and the provider. The form is merely an affirmation that the process has taken place.
Insurance Notes edit
| Can see any Doctor | Require referrals for specialists | |
|---|---|---|
| PPO | Yes | No |
| HMO | No | Yes |
| HMO vs. PPO | HMO | PPO |
|---|---|---|
| Lower out-of-pocket costs, premiums, and deductibles | X | |
| Need to go through a primary care physician | X | |
| Can receive at least limited coverage with an out-of-network provider | X | |
| Can receive at least limited coverage for prescriptions at any pharmacy | X | |
| Provider or policyholder must file a claim to receive payment of benefits | X |
| HMO Insurance Referrals | Accept In-network Providers Referrals | Accept Out-of-network Provider Referrals | Notes |
|---|---|---|---|
| In-network Specialists | YES | Usually | Depends on the HMO plan and individual needs |
| In-network Imaging Orders | YES | Usually | Depends on the HMO plan and individual needs |
| In-network Lab Orders | YES | Usually | Depends on the HMO plan and individual needs |
| HMO Insurance Physicians | Out of pocket cost | Direct Pay Option | Notes |
| Out-of-network Primary Care Physician | Out-of-network rates per HMO plan. | Yes, but not advised | Generally, HMO's make it difficult to retain a private physician |
| Out-of-network Specialist | Out-of-network rates per HMO plan. | Yes, but not advised | HMO's make it difficult and more expensive to work with out-of-network specialists. |
| Medicare Referrals | Accept Medicare Provider Referrals | Accept Opted-Out Provider Referrals | Notes |
|---|---|---|---|
| Specialists | YES | YES | |
| Imaging Orders | YES | YES | |
| In-network Lab Orders | YES | YES | |
| Medicare Physicians | Out of pocket cost | Direct Pay Option | |
| Opted Out Primary Care Physician | Free market pricing, fee for service | YES, only if provider is opted out of Medicare | Direct Primary Care is a model of payment whereby the patient pays a membership fee in exchange comprehensive primary care services |
| Opted Out Specialist | Free Market, Fee for Service | YES, only if provider is opted out; | Only select markets have specialty care membership models |
| Health Sharing/Cost Sharing - Referrals | Accept In-network Provider Referrals | Accept Out-of-network Provider Referrals | Notes |
|---|---|---|---|
| Specialists | n/a | n/a | Since health share plans are not insurance and not network-based, one can see any specialist |
| Imaging Orders | n/a | n/a | Able to go to any imaging center |
| Lab Orders | n/a | n/a | Able to go to any lab |
| Health Cost/Health Sharing - Physicians | Out of pocket cost | Direct Pay Option | |
| Primary Care Physicians | Cash Price, Fee for Service, Membership Pricing Initial Unshared Amount (IUA); | YES | Health share plans pair well with DPC practices, often saving people 40-50% vs. traditional insurance plans |
| Specialist | Cash Price, Fee for Service, Membership Pricing; Initial Unshared Amount (IUA) | YES |
Reference:
Insurance Stuff
Insurance: Employer group coverage ideas
PPO > HMO
Self Funded Plans:
- Aetna Funding Advantage
- 855-565-2129
- https://www.discoveraetna.com/afa
- https://www.youtube.com/watch?v=k6D76Mq7dSM
- Savings they advertise:
- Savings of up to 25%* on monthly payments
- Opportunity for shared savings
- Employee-funded Individual HSA by PayFlex
- Humana - Level-funded premium (LFP)
Health Shares:
- Sedera Employer Type Plans
- https://sedera.com/
- (800) 473-5472 Option 1
- Brad (Regional Contact)
High Deductible Health Plans (Catastrophic): HSA Eligible
- Humana
- Aetna Small Group Broker
- 844-241-0209
- Florida Blue
- Oscar
Medicare Donut Hole
- The first $3700 on medicine is spent with patient copay and medicare
- The next $4000 are out of pocket split 49% paid by patient and 51% by medicare
- Then they reach catastrophic and everything is $19
Legal Stuff
Good Samaritan Law
In order to qualify, a person must:
- Act in good faith
- Not engage in gross misconduct
- Not receive specific compensation
Key reasons to "fire" a patient
- Persistent failure to keep scheduled appointments or adhere to agreed-upon treatment plans
- Repeated failure to pay reasonable medical bills
- Ongoing rude, disruptive, or unreasonably demanding behavior
- Habitual noncompliance
- Falsifying or providing misleading medical history
- Seductive behavior toward physician or staff
- Sentinel incident (eg, verbal threat, violence, criminal activity)
Reference:
- Kodner C. FP Essentials. 2008.3 Harris S. Am Med News. 2008.
Legal assistance for patients
- If you have a patient that needs legal assistance related to a medical condition, remember we have the Partners in Healing program. Cindy Carlson is the contact person. Cindy.Carlson@flhosp.org
- Center for Independent Living in Central Florida has a grant to provide home modifications for disabled accessibility for patients with disabilities who meet several criteria:
· Orange County residents · Own their own home (or live with a family member who does) · Meet income requirements of 120 % or less of poverty level (CIL can assess this) · Can be a condo; can't be a mobile home
Diane has the application and information, or call: Dan Ryan at Center for Independent Living, 407-623-1070.
Patient Identifiers
Patient identifiers:
- Account numbers
- All dates related to an individual (except years)
- Biometric identifiers
- License or birth certificate numbers
- Serial numbers or medical device numbers
- E-mails
- Fax numbers
- Full-face photographs or specifically identifiable images
- Geographical location or subdivisions smaller than states
- Health plan beneficiary numbers
- IP address numbers
- Medical record numbers
- Names or any derivative including initials
- Phone numbers
- Social security numbers
- Vehicle identifiers and serial numbers including license plate numbers
- URLs
- Any other unique identifying number, characteristic, or code
References:
- JAMA Vol 317 No 23 Jun 2017
Lifestyle Medicine
EBM Lifestyle Medicine 6 Key Therapeutic Interventions:
- Nutrition: A whole food, plant-based eating pattern
- Regular physical activity
- 150-300 min mod intensity/week
- +2 days of strength training
- Sleep Management
- <6-8 hrs increases risk early death by 12%
- Protects from oxidative stress
- Stress management/Well being
- Mind-body, CBT
- Social Support: Positive Social connection
- Unhealthy social relationships, isolation and loneliness are associated with increased mortality and morbidity
- Micro-moments of human connectivity are correlated with physiologic response
- Substance Use
- Avoidance of risky substances
Quadruple Aim:
- Better outcomes
- Better patient experience
- Lower costs
- Better clinician satisfaction
Nutrition
"For the treatment, reversal and prevention of lifestyle-related chronic disease, an eating plan based predominantly on a variety of minimally processed vegetables, fruits, whole grains, legumes, nuts and seeds is recommended." ACLM
Drink of choice: Water
We eat foods, not nutrients.
EAT-Lancet 2019
- Limited intake
- Red meat
- Starchy vegetables
- Optional foods
- Eggs
- Poultry
- Dairy
- Emphasized foods
- Fish
- Vegetables
- Fruit
- Legumes
- Whole grains
- Nuts
Tips:
- Focus on adding foods instead of restricting
- Make simple swaps
- Re-imagine what meals look like
- Add umami
- Identify support network
- Prepare for challenges - social situations, travel, busy weeknights
- Encourage progress not perfection
- Sources of macros is more important than ratios
- Macro: Carbs
- high quality carbs
- Fruits and vegetables
- Whole grains
- Beans and Legumes
Fiber:
- 14g/1000 cal
- M: >38g/d
- F: >25g/d
GI:
- High >70
- Blending can also increase
- Low <55
Added sugars
- Many forms
- high quality carbs
- Macro: Fats
Polyunsaturated:
- Omega-3
- Omega-6 (in nuts/oils)
Monounsaturated fats
- When swapped for saturated and trans fats and refined carbs: May lower LDL and raise HDL
Saturated Fats (solid at Room Temp)- Minimize (<13g)
Trans Fats- Significantly increase CVD
- Partially hydrogenated oils in foods
Replacing Animal based fats with plant based fats:
- Decreases risk of some cancers
- Lowers risk of heart disease
- Lowers risk of DM
- Reduces excess adipose stores
- Reduces inflammation
- Increases insulin sensitivity
- Macro: Protein
Recommended amount: 10-35% of calories or 0.8g/Kg of body weight
Plant foods high in protein:
- Soy foods
- Legumes
- Nuts and seeds
- Quinoa
- Micro: Vitamins
B12
- Fortified foods
- Supplement
Calcium
Vit D:
- Sun exposure between 10a-2pm for 15-20 min/d
Iron:
- Avoid tea and coffee with meals
- Avoid Ca supplements with meals
- Consume Vit C foods with iron foods
Zinc
List of Physician Side Hustles
From: https://www.whitecoatinvestor.com/list-of-physician-side-hustles/
- Make Extra Money Using Your Medical Degree (Non-Clinical)
- Medical Consulting – McKinsey
- Retail Consulting – Advisor for retail/cosmetic company
- Physician Advisor – R1
- Telemedicine – American Telemedicine Association, MDlive, Doctor On Demand, HealthTap. I also wrote a review on a great course to get you started in telemedicine.
- Expert Witness – SEAK, American Medical Experts
- Chart/Utilization Review – SEAK, Dane Street, Advanced Medical Reviews
- Pharm / Clinical Trials
- Review and offer opinions on medical cases – Best Doctors
- Medical Surveys – InCrowd, ZoomRX (For a complete list, check out our Paid Medical Surveys page)
- Review Health Insurance Claims – NAIRO
- Disability Insurance Evaluation – ABIME, IAIME
- Clinical
- Locum Tenens – National Assoc. of Locum Tenens Org., Equal Access Health
- Pick up shifts at an urgent care center or start your own
- On Demand Doctor visits – Heal, Pager
- Concierge Doctor – SignatureMD
- Physicals for the military – MEPS
- Medical Review Officer – Drug & Alcohol Testing – AAMRO
- Medical Director – home health/hospice, infusion centers, IV hydration clinics
- Clinical Lab director
- Educate Others
- Write a book – You can take a course like this to get started. Some examples of books by doctors: The House of God, Complications, Drug Dealer, MD
- Write an eBook – Self-publish
- Create an online course – Kajabi, Udemy, Teachable
- Create guides to help students with exams – ex. First Aid for the USMLE
- Create online quiz banks
- Teach at a university or medical school
- Tutoring
- Real Estate Opportunities
- Invest in direct ownership of rental property – Single Family, Multifamily (Apartments)
- Invest in Crowdfunding Real Estate – CrowdStreet, EquityMultiple. (Check out our list of the Best Real Estate Crowdfunding Sites.)
- Invest in Syndications
- Invest in Private Equity Real Estate Funds
- Learn how to invest in Syndications & Funds by joining the Passive Real Estate Academy.*
- Rent out your own home – Airbnb
- Invest in Tax Liens
- Get your real estate license
- Businesses
- Purchase a franchise
- Start a multi-level marketing business
- Start a Locum Tenens company
- Online Businesses
- Start a Blog – How to start a Blog.
- Affiliate Marketing – Amazon Affiliates, CJ Affiliate, Affiliate Marketing Course
- Sell items on Etsy or eBay
- Direct to consumer products – ex. L3O Soaps
- Create online store / dropshipping – Like this blogger, My Wife Quit Her Job
- Patent / Invention
- Create invention & patent it, collect royalties, ex. BareEase
- Create an app – Can use BuildFire, iBuildApp. ex. CallSimplified
- Patent an idea for a Medical Device specifically
- Investing in Companies
- Angel Investing – AngelList, Microventures
- Venture Capitalist – Work and consult for a venture capital firm that funds medical innovation – Artiman Ventures
- Stock Market
- Invest in the stock market
- Day Trade
- Writing
- Medical Writing – SEAK
- CME content writer
- Medical Journal Editor
- Traditional Media / Online Media / Social Media
- Medical expert on air or radio – ex. Dr. Sanjay Gupta, Dr. Kien Vuu
- Social Media Influencer – ex. Dr. Mike
- Podcasting – ex. 10 Podcasts Doctors Should Really Be Listening To
- YouTube & Video Blogging – ex. ZDoggMD
- Public Speaking
- Pharmaceutical industry lecturer
- Paid guest lecturer at conferences
- Aesthetics
- Start a Medi Spa
- Aesthetics clinic – Aesthetics Pro Workshop
- Create your own skincare line – ex. MD Glam
- Transportation
- Drive Uber or Lyft (Believe it or not, I've actually heard of some docs doing this.)
- Rent out ad space on car – Wrapify
- Rent out your car – Turo, Getaround
- Coaching
- Athletes, Training, & Nutrition – ex. AthletesRX
- Weight Loss – ex. Dr. Katrina Ubell
- Health and Wellness
- Life / Business / Career – Life Coach School, Dr. Sunny Smith (Empowering Women Physicians)
- How to get into med school – Medical School Headquarters
- Just about anything and sites to get started on:
- Blinktoll.com
- GLG
- Clarity.fm
- Lending
- Invest in peer-to-peer lending – Lending Club, Prosper
- Be a Hard Money Lender
- Freelancing
- Upwork
- Fiverr
- Others
- Teach Yoga / Pilates
- Photography
- Other online surveys – Swagbucks, Survey Junkie
- Make money by referring student loan refinancing companies to your friends
Local Women's Shelter Resources
Low Income Resources Central Florida edit
Primary Care Access Network edit
- Apopka (NW)
- Apopka Family Health Center
- 225 East 7th Street
- Apopka, FL 32703
- (407) 905-8827
- East Orlando (NE)
- Central Florida Family Health Center, Inc.
- 11881-A East Colonial Drive
- (at Alafaya Trail)
- Orlando, FL 32826
- (407) 322-8645
- East Orlando (SE)
- Lake Underhill Family Health Center
- 5730 Lake Underhill Road
- Orlando, FL 32807
- (407) 322-8645
- Eatonville (NW)
- Eatonville Family Health Center
- 434 West Kennedy Blvd. Suite D
- (near Lakeside Alternatives)
- Eatonville, FL 32810
- (407) 905-8827
- Orange Blossom Family Health Center (SW)
- 234 North Orange Blossom Trail
- Orlando, FL 32805
- (407) 428-5751
- Pine Hills (NW)
- Pine Hills Family Health Center
- 1800 Mercy Drive
- Orlando, Fl 32808
- (407) 905-8827
- Southeast Orlando (SE)
- Central Florida Family Health Center, Inc.
- 5449 South Semoran Blvd. Suite 14 (at
- Hoffner Ave.)
- Orlando, FL 32822
- (407) 322-8645
- Prenatal Care
- (407) 207-7757
- Dental Care, Suite 19B
- (407) 207-7290
- Southwest Orlando (SW)
- Orange County Southside Family Health Center
- 6101 Lake Ellenor Drive
- Orlando, FL 32809
- (407) 322-8645
- Winter Garden (NW)
- Health Alliance Family Care Center
- 1210 East Plant St. Winter
- Garden, FL 34787
- (407) 905-8827
- Bithlo Family Health Center (SE)
- 19108 E Colonial Dr.
- Orlando, FL 32820
- (407) 905-8827
- Meadow Woods Family Health Center (SE)
- 849 Greenway Professional Court
- Orlando, Florida 32824
- (407) 905-8827
- Grace Medical Home (13)
- 51 Pennsylvania Ave
- Orlando, Fl 32806
- (407) 936-2785
Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI) edit
Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI) are federal programs
Social Security Disability Insurance (SSDI)
- SSDI works similarly to an insurance program.
- To receive the benefit, applicants will have had to work for a specific period of time, paying into a Social Security Trust Fund through payroll taxes.
- In addition, applicants need to meet the following SSDI prerequisites:
- You can no longer do the type of work you did before
- You have worked and paid into Social Security earning satisfactory work credits
- You cannot easily adjust to another type of work because of your medical condition
- Your disability has lasted or is expected to last for at least one year or result in death
Supplemental Security Income (SSI)
- A program meant to cover the gap in Social Security retirement and disability programs, SSI is often used by those who cannot receive SSDI or retirement benefits because of the work history requirement.
- To qualify, applicants must identify and present proof of one of the following:
- 65 years of age or older, blind, or disabled.
- Other requirements include:
- Limited income or resources
- U.S. citizenship, national, or an alien in a certain category
- Inability to work due to age or disability
- Residence within the U.S. but not confined at the State's expense (correctional or psychiatric facilities, etc)
To get disability, make sure you qualify and then start the application.
Here is the website: https://www.usa.gov/social-security-disability
Counseling Orlando edit
Free Counseling Services in Orlando Greater Orlando Trauma Response Network (TRN) Greater Orlando EMDR International Association Regional Network 5458 Lake Howell Rd Winter Park, FL 32792
The Trauma Recovery Network provides free EMDR (Eye Movement Desensitization and Reprocessing) therapy services to residents of the Greater Orlando area that have recently been impacted by community-wide traumatic experiences. Currently, TRN is offering up to five free EMDR sessions for those impacted by COVID-19 and by the death of George Floyd.
Outlook Clinic Mental Health Association of Central Florida 1525 E Robinson Street Orlando, FL 32801 407-898-0110
Outlook Clinic offers counseling in Orlando for adults 18 years and older. There is specific admission criteria to qualify for counseling services. If you don't qualify for counseling through Outlook, you will be referred to another counseling service in Orlando that can meet your needs.
Orange County Family Counseling 1728 E. Michigan Street Orlando, FL 32806 407-254-9370
Orange County Family services offers 3 months of free counseling in Orlando to children, adolescents, teenagers (ages 6-17) that are having difficulties. The children must be residents of Orange County in order to qualify for free counseling.
Neighborhood Center for Families 2100 East Michigan Street Orlando, FL 32806 407-836-7610
Neighborhood Center for Families offers counseling in Orlando in multiple locations. They see children and adults and provide individual counseling, relationship counseling, couples therapy, and marriage and family counseling. Clients must provide proof of residence in Orange County.
University of Central Florida 12494 University Blvd Orlando, FL 32816 407-823-2052
UCF Community Resource Center offers counseling in Orlando to children and adults for individual counseling, relationship counseling, couples therapy, and marriage and family counseling. Counseling services are provided by supervised graduate level interns.
Victim Service Center 2111 E. Michigan Street Orlando, FL 32806 407-254-9415
Victim Service Center provides counseling to children 12 years and older and adults who have experienced a traumatic event, including sexual abuse and domestic violence. They provide counseling services in Orange, Osceola, and Seminole counties.
Positive Behavioral Solutions 7635 Ashley Park Ct #503 Orlando, FL 32835 321-299-9415
Positive Behavioral Solutions offers counseling in Orlando to all ages for individual counseling, relationship counseling, couples counseling, and marriage and family counseling. Positive Behavioral Solutions offers free counseling with their graduate-level counselors. They offer sliding scale fee options, as well. Counselors are graduate-level, registered interns, and licensed counselors.
Sliding Scale Fee Counseling in Orlando Jewish Family Services 2100 Lee Road Orlando, FL 32789 407-644-7593
JFS offers counseling in Orlando to children and adults. They provide individual counseling, relationship counseling couples therapy, and marriage and family counseling. They offer a sliding scale fee based off of income. The counselors are registered interns or licensed counselors.
Everyone's Counseling Center 1600 E Robinson Street #250 Orlando, FL 32803 407-423-3327
Everyone's Counseling Center offers counseling in Orlando to children (as young as 4) and adults for individual counseling, relationship counseling, couples counseling, and marriage and family counseling. They have offices in Orlando, Titusville, Melbourne, St. Cloud, and Apopka. The counselors at Everyone's Counseling Center are graduate level counselors, register interns, and licensed counselors.
Discovery Counseling of Orlando 1180 Springs Centre Blvd #212 Altamonte Springs, FL 32714 407-376-3773
Discovery Counseling offers counseling in Orlando to adolescents (12 years and older) and adults for individual counseling, relationship counseling, couples counseling, and marriage and family counseling. They have offices in Altamonte Springs and Winter Garden. Their rates are based on the level of therapist. The counselors are graduate level interns, registered interns, and licensed counselors.
Hope Counseling Clinic 410 North Dillard Street #103 Winter Garden, FL 34787 407-654-5700
Hope Counseling Clinic offers counseling in Winter Garden to people of all ages for individual counseling, relationship counseling, couples therapy, marriage and family counseling. They have graduate level counselors, counseling interns, and licensed professionals. They offer sliding scale and have scholarships for children.
HD Counseling 612 East Colonial Drive Orlando, FL 32803 407-504-1869
HD Counseling offers counseling in Orlando to children and adults for individual counseling, relationship counseling, couples counseling, and marriage and family counseling. They offer sliding scale fees. The counselors at HD Counseling are graduate level counselors, registered interns, and licensed counselors.
Lutheran Counseling Services 1505 Orchid Avenue Winter Park, FL 32789 407-644-4692
Lutheran Counseling Services offers faith based counseling in Orlando to children and adults for individual counseling, relationship counseling, couples therapy, marriage and family counseling. They offer sliding scale fee that is based off of income. Their main office is in Winter Park and they have offices across Orlando
Orange Blossom Family Health 232 N Orange Blossom Trail Orlando, FL 32805 407-428-5751
Orange Blossom Family Health provides counseling at a sliding scale rate to the patients of their medical practice. They also provide outpatient substance abuse counseling. Clients must be 18 years or older.
Orlando Counseling Services 1817 Crescent Blvd, Ste 102 Orlando, FL 32817 407-808-1444
Orlando Counseling Services offers counseling near UCF to people of all ages for individual counseling, relationship counseling, couples therapy, marriage and family counseling. They have graduate level counselors, counseling interns, and licensed counselors. They have a sliding scale fee and offer reduced rates for students.
Open Path Collective Open Path Collective is a reduced rate online directory where you can find an counselor in Orlando. You pay a lifetime membership fee of $49, and then you can schedule an appointment with one of the counselors on the directory for a session fee ranging from $30-$50 for individual counseling and $30-$80 for couples counseling.
If you weren't able to find a provider that meets your needs on this list, you can contact Mental Health Association of Central Florida for referrals for more providers that offer counseling in Orlando.
Sliding Scale Medical Clinics edit
- TrueHealth - Central Florida Family Health Center
- Lake Underhill, Alafaya, Hoffner, more
- PHONE: 407-322-8645
- FAX: 833-314-0572
- OBGYN: 321-259-2229
- https://www.mytruehealth.org/
- Community Health Centers
- Apopka, Winter Garden, Clermont, more
- 13275 W Colonial Dr, Winter Garden, FL 34787
- P: 407-905-8827
- Fax: 407-660-1667
- https://www.chcfl.org/locations/winter-garden/
- Orange County Medical Clinic
- 101 S Westmoreland Drive, Orlando, FL. 32805
- PCAN Phone: (407) 836-PCAN
- Phone: (407) 836-7191
- Fax: (407) 836-9244
- https://www.orangecountyfl.net/FamiliesHealthSocialSvcs/SecondaryCareMedicalServices.aspx
- ELIGIBILITY:
- Adult Orange County resident
- U.S. citizen or resident alien
- Low Income (125% or less of the Federal Poverty Level)
- Uninsured
- No Medicare, Medicaid, or Private Insurance including Veterans Administration benefits
- Affordable Care Clinics
- Serving the Orange County area.
- 1650 Sandlake Rd, Suite 112a, Orlando, FL 32809
- P: (407) 286-1829
- FAX (407)-286-3291
- info@affordablecareclinics.com
- https://www.affordablecareclinics.com/
- Orange Blossom Family Health Center
- 232 N Orange Blossom Trail, Orlando, FL 64
- Telephone: 407-428-5751
- Fax: 407-836-9203
Malpractice Risk Knowledge
6 S's of Mental Health
- Sex
- Watch for warning signs
- Never have a relationship with a patient or former patient
- Suicide
- 5-6:1 Suicide:Homicide
- Evaluate risks
- Document conversation
- SSRI
- Follow weekly until stable
- Script Writing
- You write it you are liable
- Samples are the same as writing it
- Stop seeing a patient
- Is termination in the best interest of my patient?
- Substance Abuse
- Drugs and Alcohol masquerade as anything
- Co-occurance is 56% in bipolar, 36% in anxiety
Medical Assessment
- The medical record's primary purposes are:
- To document the course of a patient's illness and the treatment that the patient receives or to facilitate the flow of information
- To protect the patient by preserving information that may be needed for future care
- To serve as the main communication tool between all members of the healthcare team Office procedures should specify documentation requirements for telephone-based, email or texting patient encounters. All communication, either during or after office hours, should be documented in the medical record when one of the following occurs:
- Prescribing or changing medication
- Making a diagnosis
- Directing treatment
- Directing patient to another provider or facility
- Components of a well-designed test management system include:
- a process where the patient is involved in the identification process prior to any specimen collection and using two forms of patient identification, excluding the room number.
- a process for tracking pending lab results that ensures their receipt by the practice as well as a method for identifying test results that are not received.
- a mechanism to ensure that test results are reviewed and acknowledged by the provider.
- a process for patient notification of test results and for such notification being documented in the medical record.
- a process that ensures follow-up of any additional testing/monitoring required/needed.
- Informed consent prior to performing a treatment and/or procedure. In the communications process, disclose and discuss with your patient:
- The patient's diagnosis, if known;
- The nature and purpose of a proposed treatment or procedure;
- The risks and benefits of a proposed treatment or procedure;
- Alternatives (regardless of their cost or the extent to which the treatment options are covered by health insurance);
- The risks and benefits of the alternative treatment or procedure; and
- The risks and benefits of not receiving or undergoing a treatment or procedure. (American Medical Association's Opinion 8.08 - Informed Consent (2006)
Medical Emergency Codes
Roles of staff members
- Receptionist
- Acts as recorder
- Call EMS; provide patient's age and condition, and office location
- Medical Assistant
- Attach monitors
- Measure vital signs
- Provide chest compressions when instructed
- Nurse
- Administer drugs
- Start IV fluids
- Physician
- Establish airway
- Direct code
References:
- FP Essentials #338
Medicare Advantage vs Medigap (supplemental) edit
| Medicare + Medigap | Medicare Advantage | |
|---|---|---|
| Providers | Lets you see any doctor accepting Medicare, anywhere in the U.S. | Typically restricts you to in-network care |
| Care restrictions | Prior authorization and referrals not typically required | Preauthorizations and referrals are typically necessary |
| Out-of-pocket cost maximum limits | No | Yes, then you don't pay any costs for covered care for the plan year |
| Prescription coverage | Must be added with a Part D plan | Typically included in MA plans |
| Extra benefits such as vision, hearing, or dental coverage | No | Most plans include at least some of this coverage |
| U.S. travel coverage | Yes, see any doctor accepting Medicare in the U.S. | Non-emergency care outside the plan's coverage area is typically not covered. |
Here are the 6 most important points:
- Medicare Advantage plans are provided by private insurers and cover all Medicare-covered benefits, plus additional benefits like dental, vision, and prescription drugs. They have a more restricted provider network compared to Original Medicare.
- Medicare Supplement (Medigap) plans are sold by private insurers to help cover the gaps in Original Medicare, such as deductibles and coinsurance. They provide more flexibility in provider choice but do not include prescription drug coverage.
- The best time to enroll in a Medigap plan is during the 6-month Medigap Open Enrollment Period that starts when you're 65 and enrolled in Medicare Part B, as you cannot be denied coverage or charged more due to pre-existing conditions during this time.
- Medicare Advantage plans often have $0 premiums, but you must also pay the Medicare Part B premium. Medigap plans can be more expensive but provide more predictable out-of-pocket costs.
- A small percentage of Medigap plans offer non-traditional benefits like vision, dental, and hearing coverage, which are more commonly found in Medicare Advantage plans.
- You can switch between Medicare Advantage and Medigap plans, but the timing is restricted to certain enrollment periods, and you may not be able to get back the Medigap plan you had before.
Medicare Advantage:
- Provided by private insurers, covers all Medicare-covered benefits plus additional benefits
- More restricted provider network, may require referrals to see specialists
- Often have $0 premiums, but you must pay the Medicare Part B premium
- Most plans include prescription drug coverage (Part D)
- Covers vision, hearing, dental, and fitness benefits in many plans
Medigap (Medicare Supplement):
- Sold by private insurers to cover gaps in Original Medicare
- Allows you to see any provider that accepts Medicare without referrals
- Tend to have higher monthly premiums but more predictable out-of-pocket costs
- Do not include prescription drug coverage (you must enroll in a separate Part D plan)
- Only a small percentage offer non-traditional benefits like vision, dental, and hearing
- Covers one person only, spouses must buy separate policies
The key tradeoff is that Medicare Advantage plans have more restricted provider networks but often lower out-of-pocket costs, while Medigap plans offer more flexibility in provider choice but higher monthly premiums.
- Medicare Advantage (MA) plans vs. Original Medicare with Medigap:
- MA plans tend to have low/no monthly premiums but restrict provider choice and require preauthorization
- Original Medicare with Medigap offers more flexibility but higher monthly costs
- Costs and Coverage Differences:
- Original Medicare has deductibles, copays, and no annual out-of-pocket limit
- Medigap plans cover many of these costs, but have higher monthly premiums
- MA plans may include additional benefits like dental, vision, and prescription drugs
- Enrollment Deadlines and Penalties:
- Enroll in Medicare Parts A and B during the 7-month window around your 65th birthday
- Delay Part B enrollment if you have employer coverage, but face late enrollment penalties if you don't sign up later
- Enroll in Part D drug coverage during open enrollment to avoid late penalties
- Choosing Between Plans:
- Consider factors like costs, provider networks, travel needs, and health status when selecting MA or Original Medicare + Medigap
- MA plans may be more affordable for those with chronic conditions, but limit provider choice
- Original Medicare + Medigap offers more flexibility but higher monthly costs
- Switching Plans:
- You can switch between MA and Original Medicare during annual open enrollment periods
- Switching from MA to Original Medicare may require re-qualifying for Medigap coverage
- Medigap Standardization:
- Medigap plans are standardized and labeled A-N, allowing easier comparison of coverage and costs
MA plans tend to have lower premiums but more restrictions, while Medigap offers more flexibility but higher monthly costs.
Reference:
Medicine Tool Kit
CFM Race Event Supplies
Small Front Pocket:
- #10 Petroleum jelly packets
- #15 Antibiotic ointment packets
- #2 Paper tape rolls
Main Section:
- #1 Box Large gloves
- #2 Boxes Band-Aids
- #1 Box 2x3" Band-Aids
- #1 Box Alcohol prep
- #1 Package 4x4 – All-purpose sponges
- #1 Box 4x4 gauze sponges
- #2 Gauze rolls
- #3 3" ACE bandages
- #2 4" ACE bandages
- #1 H2O2 bottle
- #4 2" Coban rolls
- #1 Hand alcohol sanitizer
- #1 Albuterol inhaler
- #4 Spacers
Emergency Checklist for Medical Office
Equipment
[ ]Automated external defibrillator (AED)[ ]Bag mask ventilator (two bag sizes and three mask sizes for adult, pediatric, and infant)[ ]Blood pressure cuff (all sizes)[ ]Blood spill cleanup kit[ ]Cardiac board[ ]CPR barrier device[ ]Eye wash[ ]Glucometer[ ]Intravenous catheter/butterfly needles (18 to 24 gauge)[ ]Intravenous extension tubing and T-connectors[ ]Nasal airways (one set)[ ]Nasogastric tubes[ ]Nasal cannula for oxygen[ ]Nebulizer or metered dose inhaler with spacer and face mask[ ]Non-rebreather mask (three sizes)[ ]Oxygen mask (three sizes)[ ]Oxygen tank and flow meter[ ]Portable suction device and catheters, or bulb syringe[ ]Pulse oximeter for child and adult usage[ ]Resuscitation tape (color-coded)[ ]Universal precautions (latex-free gloves, masks, and eye protection)
Medications
[ ]Acetaminophen (rectal suppositories)[ ]Albuterol[ ]Aspirin, chewable[ ]Atropine[ ]Ceftriaxone[ ]Corticosteroids, parenteral[ ]Dextrose 25% and 50%[ ]Diazepam, parenteral[ ]Diphenhydramine, oral and parenteral[ ]Epinephrine injection[ ]Flumazenil[ ]Glucagon[ ]Lidocaine[ ]Lorazepam, sublingual[ ]Morphine[ ]Naloxone[ ]Nitroglycerin spray[ ]Saline, normal
Other
[ ]ECG Machine[ ]Condition C cards[ ]Fire extinguisher[ ]Panic button
References:
- Toback SL. Medical emergency preparedness in office practice. Am Fam Phys. 2007;75(11):1679–1684.
Home Disaster Preparedness Kit
- Water: 3 gal for each individual who would use the kit (additional 4gal per individual or pet for use if confined to the home)
- Food: 3-day supply and minimum additional 4-day supply per individual or pet for use if confined to the home
- Infants: Formula, diapers, bottles, pacifiers, powdered milk, and drugs not requiring refrigeration
- Elderly: Special foods, denture, eyeglasses, medications, other essentials.
- Kitchen accessories: Manual can opener, mess kits or disposable cups, plates and utensils, utility knife, sugar and salt, aluminum foil and plastic wrap, resealable plastic bags
- Electronics: Protable radio with extra batteries
- First Aid Kit
- Clothing: Complete change of clothes for each individual and sturdy shoes or boots
- Blankets or sleeping bag for each individual
- Sanitation and hygiene items: Shampoo, deodorant, toothpast, toothbrushes, comb, lip balm, sunscreen, contact lenses, any regular medications, toilet paper, soap, hand sanitizer, liquid detergent, feminine hygiene supplies, plastic garbage bags, disinfectant, bleach, medium-size bucket with lid
- Other essentials: Paper, pencil, needles, thread, small A,B,C class fire extinguisher
- Entertainment: Games, books
- Map of the area
- Extra set of keys and personal ID
- Other: Cash/coins, copies of credit cards, copies of medical prescriptions, matches in waterproof container, small tent, compass, and shovel
For pets:
- Food and water for at least 3 days for each pet
- Leashes, harnesses carriers as needed
- Current photo and descriptions of pets to help with identification in case of separation
References:
- FP Essentials #337
My First Aid Kit
| Location | Item | Number | Cost |
|---|---|---|---|
| Center | Gerber Seatbelt cutter | 1 | |
| Center | Laerdal Pocke Mask | 1 | |
| Center | Pharmacopoeia | 1 | |
| Center | Portable oto/ophthalmoscope | 1 | |
| Center | Sphigmomanometer | 1 | |
| Center | Stethoscope | 1 | |
| Center | Emergency Blanket | 1 | $2.97 |
| Side 1 | Alcohol Pads | 15 | |
| Side 1 | Aleve 220mg | 10 | $1.98 |
| Side 1 | Anti-itch hydrocortisone/aloe stick | 1 | |
| Side 1 | Aspirin 81mg chewable | 36 | $0.96 |
| Side 1 | Band Aids | 15 | |
| Side 1 | Diphenhydramine 50mg | 32 | $4.00 |
| Side 1 | Gerber Seatbelt cutter | 1 | |
| Side 1 | Hand snitizer | 1 | |
| Side 1 | Insect repellent spray (40% DEET) | 1 | $2.97 |
| Side 1 | Meclizine 25mg | 8 | $1.47 |
| Side 1 | Scalpel #15 | 1 | |
| Side 1 | Super glue | 1 | $2.97 |
| Side 1 | Tampon | 1 | |
| Side 1 | Tums | 12 | $1.68 |
| Side 1 | Tylenol 500mg | 10 | $1.97 |
| Side 2 | Bandana | 1 | |
| Side 2 | Boot knife | 1 | |
| Side 2 | CAT Touniquet | 1 | |
| Side 2 | Compass | 1 | |
| Side 2 | CPR Mask/Shield | 1 | |
| Side 2 | Flashlight | 1 | $1.88 |
| Side 2 | Gerber Seatbelt cutter | 1 | |
| Side 2 | Hemostats | 1 | |
| Side 2 | Needle driver | 1 | |
| Side 2 | Reflex hammer | 1 | |
| Side 2 | Thermometer | 1 | $2.96 |
| Side 2 | Tweezers | 1 |
Total sum of cost: $25.81
- This does not include the blank spots, so overall cost is much higher
- I had 3 Seatbelt cutters, only 1 is needed in my opinion
References:
POC Help
- Google (Add what you want to search for after AFP:)
- AFP Procedure Videos / YouTube
- Patient Handouts
- AFP Topics
- Practice Guidelines
- USPSTF Recommendations
- AFP Clinical Answers
- http://www.cancer.gov/bcrisktool/
References:
- AFP Mar 2021 Vol 103 No 6
- Screening tools edit
See also:
- Anxiety
- Dementia
- Depression
- Insomnia
Measure Sensitivity % Specificity % PPV % NPV % GAD-7 89 82 29 99 PHQ-9 95 67 88 83 MDQ 58 93 50 82 ISI 82.4 82.1 70 90.2 MoCA 94 42 77 76 - MDQ: https://www.sadag.org/images/pdf/mdq.pdf
- ISI: https://www.myhealth.va.gov/mhv-portal-web/insomnia-severity-index
- MoCA: https://www.mocatest.org
References:
- JFP Nov 2020 Vol 69, No 9
Sideline bag
Stethoscope Pen light Cell phone Already communicated with EMT ambulance on site Documentation resources SCAT3 card for concussions gloves Hand desanitizer
Crash kit: BP cuff Stethoscope Ophthalmoscope Otoscope Rectal thermometer scissors eye patch
Fluids: 5% Dextrose 250ml x3 NaCl 0.45% 1000ml x1 NaCl 0.9% 1000ml x4 IV catheters 16, 18, 20g
C-spine: Screwdriver Face mask cutters Bag valve mask O2 Spine board Hand cervical collars Tape
Meds: epi-pen albuterol inhaler solumedrol benadryl
Travel Medical Kit
- Adhessive bandages
- Analgesics for fever/pain
- Antacids
- Antibacterial hand wipes/solution
- Antibacterial ointments
- Antibiotics for presumptive management of travelors diarrhea
- Anticonstipation drug/laxative
- Antidiarrheal drug: bismuth subsalicylate, loperamide
- Antifungal cream, powder, or tablets: fluconazole
- Antihistamine for allergis, sleep, motion sickness
- Dental kit
- Drugs for high altitude travel
- Drugs for motion sickness
- Epinephrine auto-injector
- Essential medical records
- Health insurance cards
- Insect repellent spray
- Condoms
- Malaria prophylaxis
- Name and address of destination hospitals and clinics
- Contact info of personal physician
- Oral rehydration packets
- Sleeping drugs: melatonin
- Steroid cream
- Sunscreen 30 Sun Protective Factor and Sunburn cream (aloe)
- Thermometer
- Water purification kit/tablets
References:
- FP Essentials #370
Physiology (Misc)
Cholesterol Metabolism
- Cholesterol -> Pregnenolone -> Progesterone ->
- Dehydroepiandrosterone sulfate -> Dehydroepiandrosterone -> Androstenedione -> Testosterone ->
- Testosterone ->
- Dihydrotestosterone
- Estradiol
Reference:
- AFP Vol 78 No 9 Nov 2008
Pt quotes edit
People just don't seem to know how to be happy.
Readmission
HOSPITAL Rule
Predicts potentially avoidable hospital readmissions:
| Criteria | Score |
|---|---|
| Low Hb at discharge (<12g/dL) | 1 |
| Discharge from oncology | 2 |
| Low sodium at discharge (<135 mEq/L) | 1 |
| Procedure during hospital stay | 1 |
| Index admission type is nonelective | 1 |
| Number of admissions in previous year: | |
| - 0 | 0 |
| - 1 to 5 | 2 |
| - 6+ | 5 |
| Length of stay 5+ days | 2 |
Results:
- 0 to 4: 5.8% risk of potentially avoidable readmission
- 5 to 6: 11.9% risk of potentially avoidable readmission
- 7+: 22.8% risk of potentially avoidable readmission
Pros:
- Uses only clinical data available prior to discharge
- Validated
LACE Index
The LACE index identifies patients that are at risk for readmission or death within thirty days of discharge.
It incorporates four parameters:
- "L" stands for the length of stay of the index admission.
- "A" stands for the acuity of the admission. Specifically, if the patient is admitted through the Emergency Department vs. an elective admission.
- "C" stands for co-morbidities, incorporating the Charlson Co-Morbidity Index.
- "E" stands for the number of Emergency Department visits within the last 6 months.
LACE scores range from 1-19 and as mentioned above predict the rate of readmission or death within thirty days of discharge.
Scoring:
- 0 – 4 = Low
- 5 – 9 = Moderate
- ≥ 10 = High risk of readmission
Notes:
- A 1 point increase in LACE increases odds of readmission by 18%
- A 1 point increase in LACE increases odds of early death by 29%
Pros:
- Validated
- Uses administrative data readily available
References:
- AFP Vol 94 No 4 Aug 2016
Sample Letter From Health Care Provider: For Any Needed Accommodation
Your Health Care Provider's Letterhead
[Date]
To Whom It May Concern:
I am the treating [job title or description, such as physician, psychiatrist, psychologist, therapist, social worker, case worker, or health care professional] for [name of employee or applicant].
[Name] has [optional: name or description of employee's medical condition,] a medical condition that [substantially*] limits [Name]'s major life activities, including [fill in relevant major life activities, such as: caring for oneself, performing manual tasks, seeing, hearing, eating, sleeping, walking, standing, lifting, bending, speaking, breathing, learning, reading, concentrating, thinking, communicating, or the operation of major bodily function].
As a result of [Name]'s disability, [she/he] seeks an accommodation from [employer].
[Describe situation and how accommodation will assist employee by enabling him/her to perform job or to maintain health.]
[Name] will require this accommodation from [Start Date] to [End Date] with a possible need for extension upon evaluation.
[Example 1] As a result of [Name]'s disability, she occasionally experiences episodes of disorientation and dizziness. During these episodes, [Name] must sit or lie down for a few minutes to recover. Therefore, [Name] needs, as an accommodation, permission to take these short breaks.
[Example 2] As a result of [Name]'s disability, [she/he] is extremely sensitive to distractions, including noise, colors and light. When these distractions are present, [Name] has difficulty concentrating on [his/her] job. Therefore, [Name] needs, as an accommodation, a workspace in which these distractions are reduced.
Signature and license number
*Federal law (the ADA) requires that the condition "substantially limit" a major life activity. State law (the FEHA) requires that the condition "limit" a major life activity.
Reference:
Scope of Practice (For NP/PA) Expansion Talking Points (Opposition)
- There is no equivalency between the training and experience of a physician and a nonphysician healthcare professional.
- (11 years of education and over 20,000 hours of training compared to 5.5-7 years and 2,800-5,350).
- This lack of training and experience will result in missed diagnoses or increased costs as the inability to understand the complexity of diseases or conditions often lead to unnecessary referrals.
- Data shows patients are best served by a physician-led, clinically integrated team and, when asked, prefer to see a physician.
- "All members of the primary care team are valuable, but they are not interchangeable" (Dr. Reid Blackwelder, AAFP Past President).
- The access to care argument is workflow problem, rather than workforce shortage.
Embracing the team-based care concept will allow even greater access in both urban and rural areas.
Service Animals
See also:
Florida Statute 413.08 defines a service animal as one that is "trained to do work or perform tasks for an individual with a disability… A service animal is not a pet." These tasks are vital for the quality of life of the person with the disability. For instance, a service dog may help obtain a life-saving medication, guide the visually impaired, or help with mobility issues.
The ADA 2010 Regulations provides the following examples of work and tasks that a service dog can perform, but is not limited to:
- Guiding the blind or those with low vision
- Alerting the deaf or hard of hearing
- Providing non-violent protection or rescue work
- Pulling a wheelchair
- Assisting an individual during a seizure
- Alerting individuals to the presence of allergens
- Retrieving items
- Providing assistance to those with balance issues or disabilities related to mobility
- Helping those with psychiatric or neurological disabilities by preventing or interrupting impulsive or destructive behaviors
- Reminding a person with mental illness to take prescribed medications
- Calming a person with Post Traumatic Stress Disorder (PTSD) during an anxiety attack
To protect the service dog owner's privacy, the public can not inquire about the nature of the service animal's owner's disability. They may only ask two questions:
- Is this a service animal?
- What task has the animal been trained to perform?
Service Dog Behavior Requirements
- Service dogs must be under the control of the owner at all times.
- Service dogs can be removed or excluded from an area if the dog is out of control, is not appropriately housebroken, or is a safety issue for the public.
- Fear of animals or allergies is not a justifiable reason for the exclusion of a service animal.
- If a service animal must be removed for being a threat, the service dog owner must be provided the option of remaining without the service animal.
- Damage caused by the service animal is the responsibility of the service animal's owner.
- Any person who interferes with these rights may be subject to a misdemeanor of a second-degree in the state of Florida.
Misrepresentation of a Service Dog
- The state of Florida considers the misrepresentation of a service dog a second-degree misdemeanor.
Register Your Dog as a Service Dog
- Input the name of the service dog handler. The handler would be the name of the person who the dog performs tasks for and answers to. The handler also provides care for the dog, such as grooming, feeding, and toileting.
- Input the name of your service dog. This name would be the name a service dog typically responds to.
- Provide your email address. Some sites may need you to verify your email address afterward.
- Upload a picture of your service dog. Choose a photo that is clear and provides an accurate representation of your dog.
- Select the format of the registration. Include the registration as a paper certificate, collar tags, leash covers, and other tools.
Links:
Social Media in Healthcare
Social media is not the appropriate venue to answer medical questions. Clinicians should have a template response that explains medical questions are not answered on social media, and advise individuals to call the office, utilize a patient portal or seek emergency services.
It's important to have a written plan that includes guidelines on what information will be included on your social media site; ensuring that content is accurate, acceptable and legal.
Organizations must obtain written authorization if they plan to use someone's testimonials or photos. Just because patients posted them publicly doesn't mean an organization can use them without their explicit permission.
The following is suggested online content:
- A. Practice information and physician bios
- B. Health tips and industry news
- C. Information about upcoming events
The following are best practices for responding to negative reviews.
- Keep responses generic and anonymous
- Use standard response templates
- Recommend contacting the organization directly
Study: Examining gender-specific mental health risks after gender-affirming surgery: a national database study
Background:
- Transgender individuals face heightened psychological distress, including depression, anxiety, and suicidal ideation, partly due to stigma and lack of gender affirmation.
Aim:
- To evaluate mental health outcomes in transgender individuals with gender dysphoria who have undergone gender-affirming surgery, stratified by gender and time since surgery.
Methods:
- This retrospective study utilized the TriNetX database, analyzing U.S. patients aged ≥18 with gender dysphoria (International Classification of Diseases, Tenth Revision [ICD-10] F64) between June 2014 and June 2024. Six cohorts were created based on gender and surgery status: Cohorts A-D included patients with or without surgery, and Cohorts E-F allowed for gender comparison among those with surgery. Propensity score matching controlled for age, race, and ethnicity. Mental health outcomes included depression, anxiety, suicidal ideation, substance use disorder, and body dysmorphic disorder, assessed over two years post-surgery using clinician-verified ICD-10 codes. Body dysmorphic disorder (BDD) was analyzed separately and not conflated with gender dysphoria cohorts to ensure the distinction between these conditions. Statistical analysis employed risk ratios, with P < 0.05 deemed significant.
Outcomes:
- Primary outcomes were differences in mental health disorders, specifically depression, anxiety, suicidal ideation, body-dysmorphic disorder, and substance use disorder, among transgender individuals' post-surgery.
Results:
- From 107,583 patients, matched cohorts demonstrated that those undergoing surgery were at significantly higher risk for depression, anxiety, suicidal ideation, and substance use disorders than those without surgery.
- Males with surgery showed a higher prevalence of depression (25.4% vs. 11.5%, RR 2.203, P < 0.0001) and anxiety (12.8% vs. 2.6%, RR 4.882, P < 0.0001).
- Females exhibited similar trends, with elevated depression (22.9% vs. 14.6%, RR 1.563, P < 0.0001) and anxiety (10.5% vs. 7.1%, RR 1.478, P < 0.0001).
- Feminizing individuals demonstrated particularly high risk for depression (RR 1.783, P = 0.0298) and substance use disorders (RR 1.284, P < 0.0001).
Clinical implications:
- Findings suggest the necessity for gender-sensitive mental health support following gender-affirming surgery to address post-surgical psychological risks.
Strengths and limitations:
- By leveraging ICD-10 codes, we provide a more accurate representation of patient demographics and clinical outcomes, minimizing recall and reporting biases that often limit survey-based research.
- Limitations include the inability to account for unmeasured confounders such as social support.
Conclusion:
- Gender-affirming surgery, while beneficial in affirming gender identity, is associated with increased risk of mental health issues, underscoring the need for ongoing, gender-sensitive mental health support for transgender individuals' post-surgery.
Reference:
- Lewis JE, Patterson AR, Effirim MA, Patel MM, Lim SE, Cuello VA, Phan MH, Lee WC. Examining gender-specific mental health risks after gender-affirming surgery: a national database study. J Sex Med. 2025 Feb 25:qdaf026. doi: 10.1093/jsxmed/qdaf026. Epub ahead of print. PMID: 39996623.
Study: Racial and Ethnic Differences in Homework Time among U.S. Teens
Along with intensified competition for college admissions, U.S. teens increasingly spend more time on educational activities. Homework can be a particularly important component of educational time for economically disadvantaged and racial/ethnic minority students who have limited access to private sources of learning beyond the classroom.
This study uses data from the American Time Use Survey and the Programme for International Student Assessment to compare homework time by race/ethnicity and examine the factors that explain these differences. We extend existing literature to consider explanations beyond demographic and family background.
Our ordinary least squares (OLS) results show that family background accounts for the difference in homework time between Hispanic and White students and partially explains the difference between Black and White students, with students' academic characteristics or school fixed effects explaining the remaining gap.
While these factors partially account for Asian students' greater time spent on homework than their White peers, a substantial gap remains.
Results:
- Educational Activity Time
- Black students reported spending less time overall on educational activities per day compared with White students – 285 (4 hours 45 minutes) versus 301 minutes (5 hours 1 minute).
- Asian students reported spending substantially more time on educational activities per day – 396 minutes (6 hours 36 minutes).
- Hispanic students spent slightly more time on educational activities per day than White students – 310 minutes (5 hours 10 minutes), owing to greater time spent in classes – 249 minutes (4 hours 9 minutes).
- Homework Time
- Asian students spent 134 minutes per day.
- White students reported spending an average of 56 minutes per day on homework compared with
- 37 minutes among Black students
- 50 minutes among Hispanic students
Reference:
- Dunatchik, A., & Park, H. (2022). Racial and Ethnic Differences in Homework Time among U.S. Teens. Sociological Perspectives, 65(6), 1144-1168. https://doi.org/10.1177/07311214221101422
- https://journals.sagepub.com/doi/10.1177/07311214221101422
Teaching
RIME
- Receptor
- Interpreter
- Manager
- Educator
Exposed -> proficiency -> mastery
5-min preceptor:
- Commit to dx, w/u, tx plan
- Probe for understanding/evidence
- Teach general principles
- Reinforce correct things
- Correct mistakes
Presentation Tools
Tech Stuff
Citrix Installation
- Open the i-Extend Practice Domain
- Navigate to https://doc.adventhealth.com
- Select Central Florida and Scroll down to the Practice Domain Dropdown link
- Select Outside Hosp Practice Domain
- If the device being used is logged into Citrix Installation (For New Providers)
- Log into Cerner Store front (i-Extend page)
- Enter User name: (AdventHealth OPID)
- Enter Password
- Click Log On
- Enter User name: (AdventHealth OPID)
- Download Citrix Receiver
- Navigate to the bottom left hand of the Cerner Store front
- Click on the Download Receiver link for your device
- Install Citrix Receiver
- Find the downloaded Citrix Receiver file
- Double click to start the installation process
- When the installation is complete a window asking you to Add Account or URL may display
- Do not enter any information
- Citrix Receiver will automatically connect to the server determined by the Cerner Application
Ref:
Virtual PE edit
- VITALS: Pt reports temp of _ degrees F orally. Home BP today _. (if measured)
- Weight measured at home: _. Blood sugar measured at home: _. (if measured)
- GENERAL: Stable appearing, in no distress. Alert and oriented.
- SKIN: no visible facial rash or concerning facial lesions noted. No skin redness or discoloration seen. Patient denies seeing new skin findings on brief self-exam of arms, legs, chest, and abdomen.
- EYES: conjunctiva clear, sclera non-icteric, no eye drainage, grossly normal EOM.
- EARS: hearing grossly intact, no pain elicited with ear tugging bilaterally
- MOUTH: no visible perioral lesions, no perioral cyanosis, no lip swelling.
- NECK: Grossly normal ROM, no visible thyroid enlargement. Patient did not palpate any cervical LAD under physician-guided exam.
- HEART: Patient self-reported heart rate of _ beats per minute (measured by patient with physician instruction, or by fitness tracker HR monitor).
- LUNGS: Does not appear dyspneic. No audible wheezes or rales. No nasal flaring.
- ABDOMEN: no tenderness with patient self-palpation diffusely around abdomen under physician guidance, no pain elicited with jumping or leg lifts
- MUSCULOSKELETAL: No significant cervical kyphosis, grossly normal active ROM in upper extremities.
- NEURO: Intact recent memory. No facial or eyelid drooping. No speech impairment, answering questions appropriately.
- PSYCH: Judgment and insight good; normal mood and affect.
Travel Medicine
| Illness | % |
|---|---|
| Acute diarrhea | 16.9 |
| Viral syndrome | 4.9 |
| Irritable bowel syndrome | 4.1 |
| Malaria | 3.5 |
| Campylobacteriosis | 3.1 |
| Insect or arthropod bite or sting | 2.6 |
| Giardiasis | 2.4 |
| Chronic diarrhea | 2.3 |
| Dengue fever | 2.3 |
| Influenza-like illness | 2.1 |
Reference:
- AFP Mar 2025 Vol 111 No 3
VA Nexus Letters
4 Key Elements of a VA Nexus Letter
- VA Nexus Letter Key #1: The doctor should list any supporting evidence reviewed The nexus letter doctor should reference any medical or personnel records reviewed, such as service treatment records, VA medical records, private treatment records, DD 214, or any other existing evidence of record.
Medical Nexus Letter Key #2: The doctor must offer supporting, evidence-based rationale The most credible VA nexus letters list medical research studies, scientific journals, or previous BVA case law precedent that describes the medical etiology of the veteran's condition, and the relationship to the veteran's military service.
This is especially important for direct service connection, secondary service connection, and presumptive service connection because medical etiology, also known as a "showing of causation," is important to help a veteran prove service connection under the law.
- VA Medical Nexus Letter Key #3: The doctor should give a strong medical nexus opinion Make sure the medical professional writes one of five statements of likelihood in the VA nexus letter to help the veteran prove service connection under the law, preferably, the words "more likely than not."
VA Nexus Letter Key #4: The doctor should list his/her credentials, such as job title and specialty The doctor must sign and date their name, in addition to listing his/her medical credentials, such as, Oncologist, Orthopedic Surgeon, Sleep Specialist, PA-C, MD, etc.
This is a particularly important part of the VA nexus letter because it helps the VA Rating Official determine if it's competent and credible for VA rating purposes.
Reference:
The 5 Statements of Likelihood for a VA Nexus Letter
When asked to give an independent medical opinion as to whether a veteran's condition is related to a specific incident during military service or another service-connected disability, the medical professional should express his/her medical nexus opinion with one of the following 5 statements of likelihood:
- "Is due to" (100% sure) The VA nexus opinion "is due to" means the doctor is 100% certain that a veteran's condition was caused or made worse by active duty service or by another service-connected disability for secondary service connection.
- "More likely than not" (greater than 50%) The nexus opinion "more likely than not" means the doctor believes there is a greater than 50% chance that a veteran's condition was caused or made worse by active duty service or by another service-connected disability for secondary service connection.
"At least as likely as not" (equal to 50%) The VA nexus letter opinion "at least as likely as not" means the doctor thinks there is an approximate even balance of medical evidence for and against, and thus, there is a 50/50 chance that a veteran's condition was caused or made worse by active duty service or by another service-connected disability for secondary service connection.
This is the minimum nexus statement that will help a veteran prove service connection, because the Benefit of the Doubt always goes to the veteran according to VA law.
When all things are equal, tie goes to the veteran!
"Less likely than not" (less than 50%) The nexus opinion "less likely than not" means the doctor thinks there is a less than 50% chance that a veteran's condition was caused or made worse by active duty service or by another service-connected disability for secondary service connection.
This statement will likely cause the VA Rater to deny service connection, unless one or more other medical opinions carry more weight (higher probative value) or contain different medical opinions.
"Is not due to" (0% chance) The nexus opinion "is not due to" means the doctor thinks there is a 0% chance that a veteran's condition was caused or made worse by active duty service or by another service-connected disability for secondary service connection.
This statement will cause the VA Rater to deny service connection.
Reference:
Wellness Visits (Medicare)
Welcome to Medicare (Initial Wellness Visit)
- Health risk assessment - a self reported form that includes demographics and ADLs
- Establish PMH, PSH, SH, FH
- Review risk factors for depression, screen for depression
- Reeview functional ability and sagety risks
- Assess height, weight, BMI, BP
- List current providers and suppliers
- Assess for cognitive impairment
- Provide written screening schedule based on USPSTF
- List risk factors and medical conditions for interventions
- Health advice and referral to education or preventive counseling services
Requirements for Subsequent Annual Wellness Visit
- Update health risk assessment
- Update the PMH, PSH, SH, FH
- Assess weight and BP
- Update list of providers and suppliers
- Assess for cognitive impairment
- Update written screening schedule
- Update list of risk factors and conditions for current interventions
- Provide personalized health advice and referrals as appropriate
References:
- Florida Fam Phs 2016
Study: Commercial Insurers Paid More For Procedures At Hospital Outpatient Departments Than At Ambulatory Surgical Centers
Site neutrality in payment practices has become a salient issue in the US health care debate, as rising prices have brought increased pressure for policy action. Although Medicare has received disproportionate attention, these policies could also apply to commercial insurers, particularly to address payment differentials between hospital outpatient departments (HOPDs) and ambulatory surgical centers (ASCs).
Using 2024 Transparency in Coverage data provided by Clarify Health on commercial prices for three insurers (UnitedHealthcare, Cigna, and BlueCross BlueShield), we compared payments for thirteen common procedures across settings.
- Overall, in 2024, commercial prices were $1,489 (78 percent) higher in HOPDs than in ASCs, whereas Medicare prices were $633 (97 percent) higher.
- However, site payment differentials varied substantially across payers:
- Cigna had the lowest differentials between HOPDs and ASCs ($327)
- Cigna achieved this through provider selection, contracting with only 14 percent of HOPDs in applicable markets compared with an average of 76 percent for United and BlueCross BlueShield.
- United had the highest ($1,673).
- If United and BlueCross BlueShield paid Cigna’s average HOPD rates for these procedures, together they would save approximately $1.4 billion a year.
- Cigna had the lowest differentials between HOPDs and ASCs ($327)
Our results suggest that payers can reduce site differentials through provider selection; they also imply that larger insurers with broader networks may continue to reimburse different sites differently in the absence of either government action or a shift in market dynamics.
Reference:
- Matthew P. Maughan, Andrew M. Ryan, Nandita Radhakrishnan, and Christopher M. Whaley Commercial Insurers Paid More For Procedures At Hospital Outpatient Departments Than At Ambulatory Surgical Centers Health Affairs 2025 44:10, 1291-1297
Lab References
Notes:
Specific Labs:
- Acid/Base
- ANA+
- Biochemical Nutritional Indications
- CBC with differential
- Chloride Levels
- Copeptin
- D-Dimer increased plasma values
- Special tests to classify Diabetes
- Elevated Liver Transaminase Levels
- Eosinophilia
- False A1c Readings
- HCG Levels During Pregnancy
- Hematuria
- Hepatitis B
- homocysteine
- hsCRP
- IgG vs IgM
- MTHFR Gene/Test
- Procalcitonin
- Prostate Specific Antigen (PSA)
- Semen
- Transaminases
- Troponin Increased Plasma Values
- Urine Drug Testing
- Urine Specific Gravity
Common Lab Tests
| 1 | CBC |
| 2 | Basic metabolic panel |
| 3 | Glucose |
| 4 | Urinalysis |
| 5 | Chlamydia detection |
| 6 | HbA1C |
| 7 | Phosphorus |
| 8 | Magnesium |
| 9 | PT/INR |
| 10 | Comprehensive metabolic panel |
| 11 | TSH |
| 12 | Liver function |
| 13 | Lipid panel |
| 14 | PTT |
| 15 | Troponin-I |
| 16 | Urine culture |
| 17 | Blood group |
| 18 | Lactate |
| 19 | Antibody screen |
| 20 | Drugs of abuse screen, urine |
| 21 | Cytology |
| 22 | Syphilis |
| 23 | Surgicals |
| 24 | Blood culture |
| 25 | Pregnancy |
Despite the differences in health systems, local epidemiology, practice patterns, and resources, there are strong similarities in laboratory test utilization patterns across five hospitals in countries with very different levels of per capita income.
Reference:
- Susan Horton, Kenneth A Fleming, Modupe Kuti, Lai-Meng Looi, Sanjay A Pai, Shahin Sayed, Michael L Wilson, The Top 25 Laboratory Tests by Volume and Revenue in Five Different Countries, American Journal of Clinical Pathology, Volume 151, Issue 5, May 2019, Pages 446–451, https://doi.org/10.1093/ajcp/aqy165
MTHFR Gene/Test edit
See also:
Normally, your body quickly breaks down homocysteine, so you have very little in your bloodstream. But if you have a change in an MTHFR gene, the MTHFR proteins your body makes may not process folate as well as they should. As a result, you may have increased levels of homocysteine in your blood.
In general, researchers aren't certain that increased homocysteine levels directly cause health problems. But some studies have linked too much homocysteine to damage to the inside of your blood vessels. This may increase the risk for blood clots, heart disease, and stroke. Also, the risk of having a baby with neural tube defects is slightly higher if homocysteine levels are high during pregnancy.
Even if a homocysteine blood test shows that your homocysteine levels are higher than normal, an MTHFR gene test is generally not needed. That's because the treatment for high homocysteine levels is the same whether or not it's caused by a common change in your MTHFR gene.
To lower homocysteine levels, your health care provider will usually recommend taking vitamin B supplements that include folic acid, which is a form of folate. However, if you have the gene variant MTHFR, your provider may recommend methylfolate (5-MTHF) instead since your body may be able to use this form more easily. The extra vitamins can make up for an MTHFR gene that's not fully working. Your provider may recommend eating more foods with folate, too. Before making changes in your health habits, talk with your provider.
Studies show that taking folic acid greatly reduces the risk of neural tube defects in babies. So, even if you have the MTHFR gene variant, the U.S. Centers for Disease Control and Prevention (CDC) recommends folic acid supplements for everyone who may become pregnant. Folic acid may also decrease the risk of stroke from a blood clot in adults. But this treatment doesn't appear to decrease the risk of heart disease.
Other names: methylenetetrahydrofolate reductase mutation, C677T and A1298C, MTHFR DNA assay, MTHFR DNA testing, MTHFR gene variants, MTHFR gene polymorphisms 677T>C & 1298A>C mutations
In general, medical experts do not recommend testing for common MTHFR gene changes.
But the test may be ordered if:
- You had a blood test that showed higher than normal levels of homocysteine
- A close relative was diagnosed with an MTHFR gene change
- You and/or close family members have early heart or blood vessel disease
Reference:
Copeptin
Copeptin and AVP
TLDR:
- For Nephrogenic Diabetes Insipidus
- NOT for SAIDH
- Study: Copeptin and its role in the diagnosis of diabetes insipidus and the syndrome of inappropriate antidiuresis
Copeptin is secreted in an equimolar amount to arginine vasopressin (AVP) but can easily be measured in plasma or serum with a sandwich immunoassay. The main stimuli for copeptin are similar to AVP, that is an increase in osmolality and a decrease in arterial blood volume and pressure. A high correlation between copeptin and AVP has been shown. Accordingly, copeptin mirrors the amount of AVP in the circulation. Copeptin has, therefore, been evaluated as diagnostic biomarker in vasopressin-dependent disorders of body fluid homeostasis.
Disorders of body fluid homeostasis are common and can be divided into hyper- and hypoosmolar circumstances: the classical hyperosmolar disorder is diabetes insipidus, while the most common hypoosmolar disorder is the syndrome of inappropriate antidiuresis (SIAD).
Copeptin measurement has led to a “revival” of the direct test in the differential diagnosis of diabetes insipidus. Baseline copeptin levels, without prior thirsting, unequivocally identify patients with nephrogenic diabetes insipidus.
In contrast, for the difficult differentiation between central diabetes insipidus and primary polydipsia, a stimulated copeptin level of 4.9 pmol/L upon hypertonic saline infusion differentiates these two entities with a high diagnostic accuracy and is clearly superior to the classical water deprivation test.
On the contrary, in the SIADH, copeptin measurement is of only little diagnostic value. Copeptin levels widely overlap in patients with hyponatraemia and emphasize the heterogeneity of the disease. Additionally, a variety of factors lead to unspecific copeptin elevations in the acute setting further complicating its interpretation. The broad use of copeptin as diagnostic marker in hyponatraemia and specifically to detect cancer-related disease in SIADH patients can, therefore, not be recommended.
Reference:
- Refardt J, Winzeler B, Christ-Crain M. Copeptin and its role in the diagnosis of diabetes insipidus and the syndrome of inappropriate antidiuresis. Clin Endocrinol (Oxf). 2019 Jul;91(1):22-32. doi: 10.1111/cen.13991. Epub 2019 May 8. PMID: 31004513; PMCID: PMC6850413.
hsCRP
hs-CRP is a general marker of systemic inflammation, but its elevation is associated with cardiovascular risk. For lowering high-sensitivity C-reactive protein (hs-CRP) levels, (which reflect inflammation in blood vessels such as coronary arteries):
- General strategies noted to lower hsCRP include:
- Regular exercise
- Healthy diet rich in antioxidants
- Managing underlying conditions like obesity or metabolic syndrome
- Some studies suggest that certain supplements, such as omega-3 fatty acids, may help lower hs-CRP
Musculoskeletal/Orthopedics
52 WALKING FUN FACTS edit
https://acewebcontent.azureedge.net/assetportfoliodownloads/WalkingFunFacts-2015.pdf
- Walking is good medicine: It can help you reduce the risk of coronary heart disease.
- Dog owners walk significantly more than their non-pooch owning counterparts.
- A 15-minute walk can curb chocolate and sugar cravings.
- The fastest 5k (3.1 miles) time for walking is 21:58 (about a 7-minute mile) for a woman and 19:09 (about a 6-minute mile) for a man—faster than most runners!
- The first Wednesday in April is National Walking Day.
- Walking can boost creativity by up to 60 percent.
- People who track their steps take an average of 2,500 more steps each day.
- Replacing 1½ miles of driving with walking will reduce the amount of greenhouse gases produced by about 75 percent.
- Walking is good medicine: It can help you improve blood pressure and blood sugar levels.
- About 2,000 steps equal one mile.
- A lunchtime walk can make you more productive at work.
- The risk of exercise-related injuries is 1 to 5 percent for walkers compared to 20 to 70 percent for runners.
- Taking less than 5,000 steps each day is considered sedentary.
- Your walking speed can predict how long you'll live.
- Jobs that get you moving: waiters (23,000 steps a day), nurses (16,000) and retail workers (15,000).
- Race walking made its Olympic debut in 1908.
- Walking is good medicine: It can help elevate your mood and enhance mental well-being.
- Interval walkers lost six times more weight than walkers who maintained a steady pace, according to a Danish study.
- The claim that you'll burn 100 calories whether you walk or run a mile is false. Your speed and body weight affect the amount of calories you burn. The faster and heavier you are, the more calories you'll burn.
- Walk to the beat of "Shut Up and Dance" and you'll be going about 3.5 mph. If you can keep up with "Shake It Off," you'll be cruising at more than 5 mph.
- Walking just 21 minutes a day can cut your risk of heart disease by 30 percent.
- Focusing on an object ahead of you can increase your speed by as much as 23 percent.
- Walking is good medicine: It can help you reduce the risk of breast and colon cancer.
- Walking uphill activates three times more muscle fibers than walking on flat terrain. It also burns up to 60 percent more calories.
- The ultimate calorie burner: stair climbing. You'll burn calories two to three times faster than walking without an incline.
- Australians walk the most, taking an average of 9,695 steps each day. Americans stroll the least (5,117 steps each day) of all the industrial countries surveyed.
- Walking is good medicine: It can help you avoid osteoporosis and osteoarthritis.
- Being short doesn't have to slow you down: At the 2008 Olympics, 5'2½" Olga Kaniskina of Russia beat out Norway's 5'8" Kjersti Plätzer for the gold in the women's 20k race walk.
- The longest uninterrupted walk was 19,019 miles from the southern tip of South America to the northern most part of Alaska and took 2,425 days.
- It would take a person walking nonstop at a 3-mph pace approximately 347 days to walk around the world.
- A typical pair of athletic shoes will last for approximately 500 miles of walking.
- Walking is good medicine: It can help you maintain body weight and lower your risk of obesity.
- Babies typically begin to walk around 12 to 13 months of age, though some may start as early as 9 or 10 months and as late as 15 or 16 months.
- Walking is the most popular form of exercise in the U.S.
- Today, less than one out of seven children walk to school. In 1970, two out of three children walked to school.
- The average walking speed for the typical adult is approximately 3 mph.
- Eliminating just 10 miles of driving each week would eliminate roughly 500 pounds of carbon dioxide per year.
- The average person will walk an estimated 65,000 miles in his or her lifetime—the equivalent of three trips around the world.
- A person needs to walk the length of a football field to burn enough calories to offset eating a single piece of candy-coated chocolate.
- Adding 150 minutes of brisk walking to your routine each week can add a little over three years to your lifespan.
- Walking is good medicine: It improves cerebral blood flow and lowers the risk of vascular disease that may help you avoid dementia later in life.
- You use an estimated 200 muscles during walking.
- You need to walk roughly 13 miles or the equivalent of a half marathon to burn off a super-sized meal.
- Walking a typical 18-hole golf course equates to about 12,000 steps.
- During a typical day of walking, the cumulative impact forces on the feet can total several hundred tons—so invest in good quality footwear.
- Hippocrates had it right—"walking is man's best medicine."
- Consider getting a wearable device to track your steps taken or distance covered. Watching your improvement over time can be a great source of motivation.
- To get a rough estimate of how fast you walk, count the number of steps you take in a minute and divide by 30.
- Listening to music while walking has been observed to improve mood, motivation and performance.
- A significant difference between walking and running is the amount of time each foot contacts the ground. During walking, at least one foot is in contact with the ground at any given time, and the length of time the foot is in contact is longer than while running.
- Since the days of Socrates, walking has been linked to enhanced cognitive functioning and creativity.
- Thomas Jefferson, who lived to be 83 when life expectancy was 40, walked four miles a day.
90 Second MSK Sceening
| Instruction | Observation |
|---|---|
| Stand facing examiner | AC joints: general habitus |
| Look at ceiling, floor, over both shoulders, touch ears to shoulders | Cervical spine motion |
| Shrug shoulders | Trapezius strength |
| Abduct shoulders to 90 | Deltoid strength |
| Full external rotation of arms | Shoulder motion |
| Flex and extend elbows | Elbow motion |
| Arms at sides, elbows at 90 flexed; pronate and supinate wrists | Elbow and wrist motion |
| Spread fingers; make a fist | Hand/finger motion, strength, deformities |
| Tighten quadriceps | Symetry and knee effusions, ankle effusion |
| "Duck Walk" | hip, knee, and ankle motions |
| Back to examiner | Shoulder symmetry; scoliosis |
| Knees straight, touch toes | scoliosis, hip motion, hamstring tightness |
| Raise up on toes, heel | Calf symmetry, leg strength |
References:
- J Fam Prac Vol 52, No 2 Feb 2003
Acute Pain from Non-Low Back Musculoskeletal Injuries
- Topical NSAIDs are the most effective intervention and only to to improve all measured outcomes
- Improve pain within 2 hrs
- Although oral NSAID and acetaminophen are effective, combining them does not improve effectiveness
- Acetaminophen reduces pain at 2 hrs and over 1 wk (like NSAIDs) but without increasing physical function, symptom relief, or patient satisfaction
- Opioids are moderately effective - they increase gastrointestinal and nuerologic adverse effects and lead to long-term use in 6% of people treated
- Avoid for short term pain relief
- Acupressure and TENS techniques are effective nonpharmacologic options
References:
- AFP Vol 102, No 11 Dec 2020
Ankle Pain
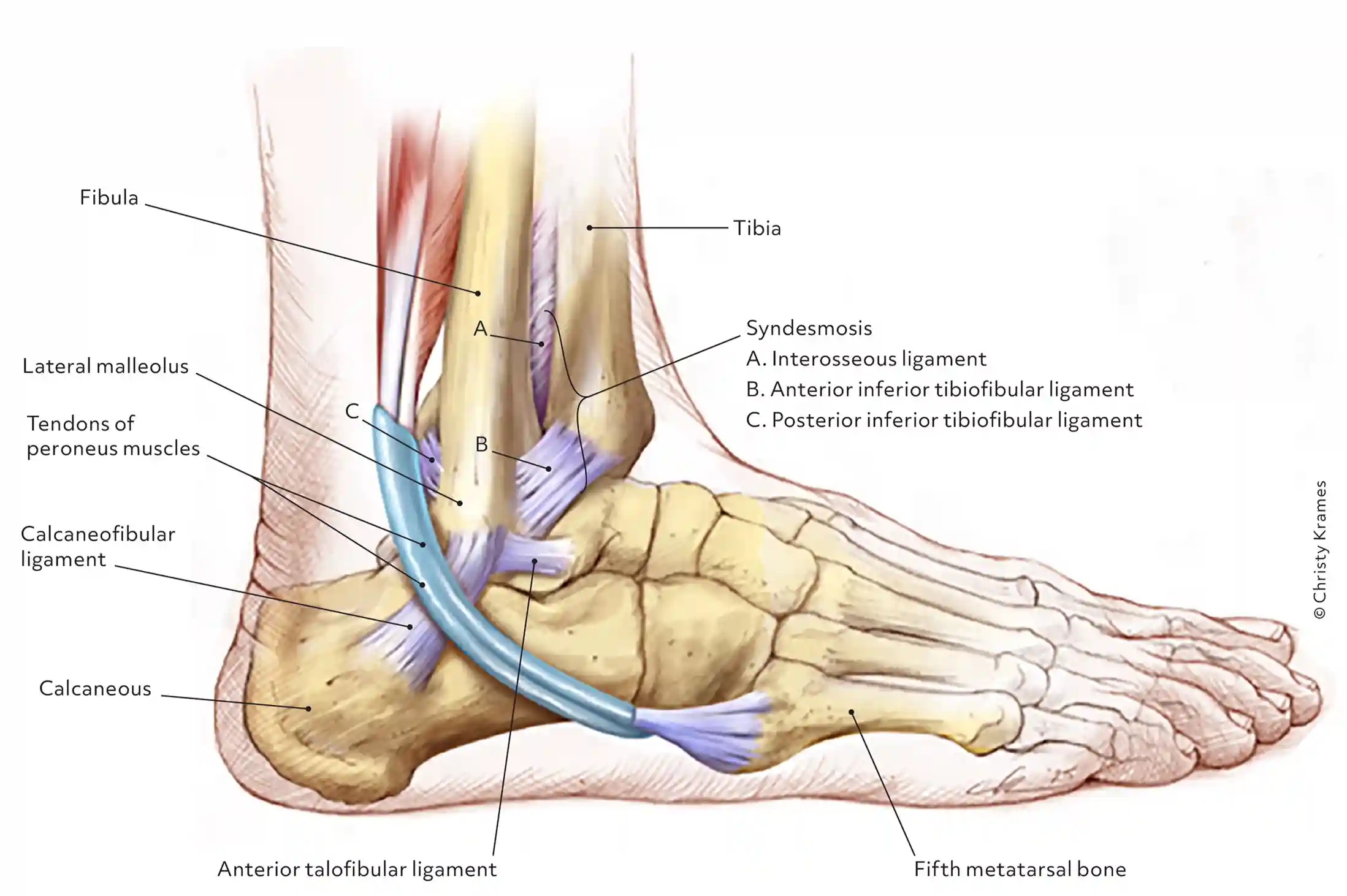
| Anterior | Lateral | Medial | Posterior |
|---|---|---|---|
| Osteochondritis dissecans | Lateral ankle sprain | Medial ankle sprain | Achilles tendinopathy |
| Anterior impingement | Distal fibular fracture | Distal tibia fracture | Flexor hallucis dysfunction |
| Tibiotalar arthritis | Peroneal tendinopathy | Posterior tibialis subluxation | Os trigonum syndrome |
| Tibialis anterior tendinopathy | Peroneal tendon subluxation | Posterior tibialis tendinopaty | |
| Syndesmotic sprain | Peroneal nerve entrapment | Tarsal tunnel syndrome |
Achilles tendon rupture
- pain at the Achilles tendon—2 to 6 cm above the insertion into the calcaneus—and an inability to fully bear weight
- edema, bruising, and a palpable gap within the tendon, 2 to 6 cm proximal to insertion.
- A diagnosis of Achilles tendon rupture is supported when at least 2 of the following conditions are met4,5:
- positive Thompson test
- decreased strength during plantar flexion of the ankle
- palpable gap or pain at the typical location (2-6 cm above insertion)
- increased passive ankle dorsiflexion upon gentle ranging of the ankle joint.
Injury to the syndesmosis
- "high ankle sprain," a syndesmotic injury is present in as many as 20% of ankle fractures and 5% to 10% of ankle sprains.
- Recovery is typically prolonged (ie, twice as long as recovery from a lateral ankle sprain).
- present with ankle pain, swelling, instability, pain when walking on uneven terrain, and pain upon push-off
- Exam:
- Squeeze test. The patient sits with the knee on the affected side bent at a 90° degree angle while the examiner applies compression, with one or both hands, to the tibia and fibula at midcalf. The test is positive when pain is elicited at the level of the syndesmosis just above the ankle joint.9,11
- External rotation test. External rotation of the foot and ankle relative to the tibia reproduces pain.
- Crossed leg test. The affected ankle is crossed over the opposite knee in a figure-4 position. The test is positive when pain is elicited at the syndesmosis.10
- Cotton test. The proximal lower leg is steadied with 1 hand and the plantar heel grasped with the other hand. Pain when the heel is externally rotated (and radiographic widening of the syndesmosis under fluoroscopy) signal syndesmotic instability.
- Fibular translation test. When anterior or posterior drawer force is applied to the fibula, pain and increased translation of the fibula (compared to the contralateral side) suggest instability.
- Imaging typically involves anteroposterior [AP], lateral, and mortise plain films of the ankle and weight-bearing AP and lateral views of the tibia and fibula.9 Important measures on weight-bearing AP x-rays are the tibiofibular clear space (abnormal, > 6 mm) and the tibiofibular overlap (abnormal, < 6 mm)
- Management:
- Grade 1 injury is a sprain without diastasis on imaging. Management is conservative, with immobilization in a splint or boot for 1 to 3 weeks, followed by functional rehabilitation over 3 to 6 weeks.10
- Grade 2 injury is demonstrated by diastasis on a stress radiograph. Although evidence to guide successful identification of a grade 2 injury is lacking, it is clinically important to make that identification because these injuries might require surgical intervention, due to instability. Because the diagnosis of this injury can be challenging in primary care, high clinical suspicion of a grade 2 injury makes it appropriate to defer further evaluation to an orthopedic surgeon. On the other hand, if suspicion of a grade 2 injury is low, a trial of conservative management, with weekly clinical assessment, can be considered. A diagnosis of grade 2 injury can be inferred when a patient is unable to perform a single-leg hop after 3 weeks of immobilization; referral to an orthopedic surgeon is then indicated.12
- Grade 3 injury is frank separation at the distal tibiofibular joint that is detectable on a routine plain film. Management—surgical intervention to address instability—is often provided concurrently with the treatment for a Danis-Weber B or C fracture, which tends to coexist with grade 3 syndesmotic injury. (The Danis-Weber A–B–C classification of lateral ankle fracture will be discussed in a bit.)
Ankle fracture
- Management
- Type A fractures (distal to the level of the tibial plafond) are managed with ankle stabilization bracing without immobilization.
- Nondisplaced type B and C fractures (at the level of the tibial plafond and proximal to it, respectively) should be treated with 6 weeks of immobilization in a walking boot; close follow-up within 1 week of injury is recommended to ensure that no displacement of fragments has occurred. Type B and C fractures need to be followed until bony union is achieved.
- If there is radiologic evidence of a fracture line after 3 months, referral to an orthopedic surgeon is indicated for management of delayed union.
- Talar fracture: Although talar fracture is rare, the injury is important to detect because a limited blood supply places fragments at risk of avascular necrosis
Lisfranc injury
- a spectrum of midfoot injuries in which 1 or more metatarsals are displaced from the tarsus.
- typically result from a direct blow to the midfoot or excessive pronation or supination in a plantarflexed foot
- pain while walking down stairs
- reveal plantar ecchymosis, which is considered pathognomonic
- Diagnosed on weight-bearing x-rays;
- as many as one-half of cases are missed when only non-weight-bearing films are obtained.
- If initial weight-bearing cannot be tolerated by the patient, another attempt at imaging can be made after 1 week of rest
- Management
- Stable injury without diastasis can be managed conservatively with immobilization in a short walker boot and limited weight-bearing for 2 weeks, followed by weight-bearing as tolerated in the boot if tenderness has improved.24 After 6 to 8 weeks, if the patient is pain-free with abduction stress, weight-bearing without the boot (but with a rigid-sole shoe) is permissible for an additional 6 months.
Proximal fifth-metatarsal fractures
- present with lateral foot pain and tenderness at the base of the fifth metatarsal, made worse by inversion of the foot, and inability to bear weight on the lateral aspect of the foot.
- Most fractures are revealed on standing AP, oblique, and lateral x-rays.
- Management
- nondisplaced tuberosity avulsion fracture:
- compressive dressings or casting for pain control and weight-bearing and
- range-of-motion exercises as tolerated.
- Follow-up every 2 to 3 weeks is recommended to ensure appropriate healing—ie, pain nearly resolved by 3 weeks post-injury and radiographic union evident at 8 weeks. If displacement is > 3 mm, > 60% of the metatarsal–cuboid joint surface is affected, or there is a 1 to 2 mm step-off on the cuboid articular surface, consider referral to an orthopedist.
- Jones fractures can be managed
- initially with posterior splinting, non-weight-bearing, and close follow-up.
- Surgical referral is indicated in all cases of diaphysial stress fracture because of the high rate of nonunion and refracture.
- nondisplaced tuberosity avulsion fracture:
References:
- JFP Vol 66 No 5 May 2017
- JFP Vol 69, No 5 Jun 2020
Ankle Sprains
Assessment:
- Delaying the examination until 4 to 7 days postinjury increases diagnostic accuracy of sprain severity.
- As part of the physical examination, a combination of ankle-specific tests should be used to evaluate ligaments.
- In the acute setting, the Ottawa Foot and Ankle rules can help determine when radiography does not need to be ordered to evaluate for fracture.
Management:
- Management of acute ankle sprains should include:
- joint protection
- pain control
- external ankle supports for 5 to 10 days
- early functional activity
- targeted rehabilitation exercises
POLICE (Initial management)
- Protection
- Optimal loading
- Ice
- Compression
- Elevation
PEACE and LOVE (Initial management and recovery)
- Protection
- Elevation
- Avoid anti-inflammatory drugs (in initial management)
- Compression
- Education and load
- Optimism
- Vascularization
- Exercise
Pain Management:
- Oral medications such as acetaminophen, nonsteroidal anti-inflammatory drugs, and opioids are equally effective in managing pain.
Recovery:
- Recovery includes the use of external ankle supports (eg, semirigid braces) and a targeted neuromuscular rehabilitation program for 8 to 12 weeks.
- Continuing functional exercises and the use of external ankle support during sport after recovery can aid in the prevention of recurrent ankle sprains.
- If an ankle sprain does not follow the expected course of recovery, further evaluation with magnetic resonance imaging should be performed to evaluate for other causes of acute lateral ankle injuries, such as talar fractures and peroneal tendon injuries.
PAASSS (Return to Play)
- Pain severity: after the last 24 hours, including activity
- [Ankle] impairment: in range of motion, strength
- Athlete perception: comfort, stability, readiness to return
- Sensorimotor control: proprioception, balance
- Sport or functional performance: in sport-specific exercises, can participate in practice
| Test | Targeted structure | Technique | Positive finding |
|---|---|---|---|
| Anterior drawer test | Anterior talofibular ligament | Patient is seated or supine; stabilize the distal tibia and fibula with one hand and use the other hand to grasp the heel, with the ankle in 10-20 degrees plantar flexion, and apply firm anterior force to the heel, attempting to translate the talus forward | Increased anterior translation of talus relative to tibia compared with uninjured ankle |
| Dorsiflexion external rotation stress test (Kleiger test) | Syndesmosis | Patient is seated with knee flexed to 90 degrees; stabilize the distal tibia and fibula with one hand while the other hand applies external rotation stress onthe foot while ankle is in slight dorsiflexion position | Pain over syndesmosis area or sense of instability |
| Squeeze test | Syndesmosis | Patient is seated or supine; firmly squeeze the tibia and fibula together around the midcalf region | Reproduces pain in distal tibiofibular syndesmosis area |
| Talar tilt test (dorsiflexion) | Calcaneofibular ligament | Patient is seated or supine; grasp the lower leg with one hand to stabilize the tibia and fibula and use the other hand to grasp the heel; while holding the ankle in a neutral position, apply varus force to the talus and invert the foot | Increased tilt translation of the talus, pain, or sense of instability compared with uninjured ankle |
| Talar tilt test (plantar flexion) | Anterior talofibular ligament | Patient is seated or supine; grasp the lower leg with one hand to stabilize the tibia and fibula and use the other hand to grasp the heel; while holding the ankle in 10-20 degrees plantar flexion, apply varus force to talus and invert foot | Increased tilt translation of the talus, pain, or sense of instability compared with uninjured ankle |
Reference:
- Am Fam Physician. 2025;112(6):609-617
Ottowa Ankle Rules
For Ankle Pain – Ask These Questions:
- Is the bony bump on the outside of your ankle (lateral malleolus) tender when you press it?
- Is the bony bump on the inside of your ankle (medial malleolus) painful when you touch it?
- Does the bony area on the top of your midfoot (near the arch) hurt when you press it?
- Is the base of the small toe (fifth metatarsal) tender when touched?
- Right after the injury, were you unable to stand on it or take a few steps? Are you able to walk on it now (even if you’re limping or in pain)?
Benefits of exercise
- Those who are more active (8000 MET/min/wk) had:
- 14% reduced risk of breast cancer
- 21% reduced risk of colon cancer
- 28% reduced risk of diabetes
- 25% reduced risk of ischemic heart disease
- 26% reduced risk of ischemic stroke
References:
- BMJ. 2016;354:i3857
Bone Stress Injury Prediction Rule
| Finding | Points |
|---|---|
| Bony tenderness | 3 |
| History of bone stress injury | 2 |
| Pes Cavus | 2 |
| Increased walking or running volume | 1 |
A cutoff score of 3 to diagnose bone stress injury (98% sensitivity, 54% specificity, 98% NPPV)
Reference:
- Dec 2024 Vol 110 No 6
Carpal Tunnel Syndrome
Splinting:
- Goal: Minimize wrist movement to decrease any concomitant swelling in carpal tunnel contributing to compression
- Orthoses:
- Neutral wrist splint
- Cock-up wrist splint (20 deg wrist extension)
- Use continuously for 2-4 weeks
- At minimum nocturnal use
Surgery versus splinting long-term three months and greater follow-up.
- Benefits
- Clinical improvement after initial surgery
- Number needed to treat: 4
- To reduce risk for further surgery after initial surgery
- Number needed to treat: 3
- Clinical improvement after initial surgery
- Harms
- Uncertain or insufficient evidence to draw conclusions
Surgery versus corticosteroid injection long-term over three months follow-up
- Uncertain or insufficient evidence to draw conclusions
References:
- JFP Vol 67 No 11 Nov 2018
- AFP Jul 2025 Vol 112 No 1
Cervical Radiculopathy
Cervical radiculopathy describes pain in one or both of the upper extremities, often in the setting of neck pain, secondary to compression or irritation of nerve roots in the cervical spine.
Accompanied by motor, sensory, or reflex deficits and is most prevalent in persons 50 to 54 years of age.
Common examination findings:
- painful neck movements
- muscle spasm
- Diminished deep tendon reflexes, particularly of the triceps (most common neurologic finding)
- The Spurling test, shoulder abduction test, and upper limb tension test can be used to confirm the diagnosis.
Imaging is not required unless there is a history of trauma, persistent symptoms, or red flags for malignancy, myelopathy, or abscess.
Most cases will resolve regardless of the type of treatment
- Nonoperative treatment includes:
- physical therapy involving strengthening, stretching, and potentially traction
- nonsteroidal anti-inflammatory drugs, muscle relaxants, and massage
- Epidural steroid injections may be helpful but have higher risks of serious complications.
Those with red flag symptoms or persistent symptoms after 4-6 weeks of treatment:
- magnetic resonance imaging can identify pathology amenable to epidural steroid injections or surgery
Reference:
- Childress MA, Becker BA. Nonoperative Management of Cervical Radiculopathy. Am Fam Physician. 2016 May 1;93(9):746-54. PMID: 27175952.
de Quervain tendinopathy
Splinting:
- Goal: Immobilize the affected tendons to reduce irritation and/or inflammation
- Orthoses:
- Thumb spica splint
- Better if used early in disease but does not alter natural disease course
References:
- JFP Vol 67 No 11 Nov 2018
EBM: Massage Therapy edit
Low Back Pain
- Several evaluations of massage for low-back pain have found only weak evidence that it may be helpful.
- The Agency for Healthcare Research and Quality, in a 2016 evaluation of nondrug therapies for low-back pain, examined 20 studies that compared massage to usual care or other interventions and found that there was evidence that massage was helpful for chronic low-back pain but the strength of the evidence was low. The agency also looked at six studies that compared different types of massage but found that the evidence was insufficient to show whether any types were more effective than others.
- A 2015 review of 25 studies with a total of 3,096 participants found that in both acute and chronic low-back pain, there were short-term improvements in pain after massage therapy. However, because the quality of the studies was low, the investigators who conducted the review concluded that they had "very little confidence" that massage is an effective treatment for low-back pain.
- Clinical practice guidelines (guidance for health care providers) issued by the American College of Physicians in 2017 included massage therapy as an option for treating acute/subacute low-back pain but did not include massage therapy among the options for treating chronic low-back pain.
Neck and Shoulder Pain
- Massage therapy may be helpful for neck or shoulder pain, but the benefits may only last for a short time.
- A 2013 review of 12 studies (757 total participants) found that massage therapy was more helpful for both neck and shoulder pain than inactive therapies but was not more effective than other active therapies. For shoulder pain, massage therapy had short-term benefits only.
- A 2016 review of 4 studies conducted in the United States (519 participants) found that massage could provide short-term relief of neck pain if massage sessions were long enough and frequent enough.
Osteoarthritis of the Knee
- The small amount of research that's been done on massage therapy for osteoarthritis of the knee suggests that it may have short-term benefits in relieving knee pain.
- Of 6 studies that evaluated massage therapy for osteoarthritis of the knee (408 total participants), 5 found that it provided short-term pain relief. Two of the studies that showed pain relief (149 participants) involved the use of essential oils (aromatherapy massage).
Headaches
- Only a small number of studies of massage for headache have been completed. These studies looked at different types of massage and different types of headache, and their results are not consistent.
- A 2016 study with 64 participants evaluated 2 types of massage (lymphatic drainage and traditional massage), once a week for 8 weeks, in patients with migraine. The frequency of migraines decreased in both groups, compared with people on a waiting list.
- In a 2015 study, 56 people with tension headaches were assigned to receive massage at myofascial trigger points or an inactive treatment (detuned ultrasound) twice a week for 6 weeks or to be on a waiting list. People who received either massage or the inactive treatment had a decrease in the frequency of headaches, but there was no difference between the two groups.
- A 2011 study evaluated the effect of adding hand massage to multimodal behavior treatment of migraine in 83 people. Hand massage had no effect on migraine frequency.
Fibromyalgia
- Massage therapy may be helpful for some fibromyalgia symptoms if it's continued for long enough.
- A 2014 evaluation of 9 studies (404 total participants) concluded that massage therapy, if continued for at least 5 weeks, improved pain, anxiety, and depression in people with fibromyalgia but did not have an effect on sleep disturbance.
- A 2015 evaluation of 10 studies (478 total participants) compared the effects of different kinds of massage therapy and found that most styles of massage had beneficial effects on quality of life in people with fibromyalgia. Swedish massage may be an exception; 2 studies of this type of massage (56 total participants) did not show benefits.
Reference:
Endurance Athletes Common Conditions
- Exercise-induced asthma
- Exercise-associated collapse and hyponatremia
- Overtraining syndrome
- Rest for weeks to months, then gradually resume training program
Endurance Athletes Overuse Injuries
- Patellofemoral pain syndrome
- History: Ant knee pain worsened with running, jumping, cycling; pain with stairs; pain with prolonged sitting with knees flexed
- PE: Patellofemoral malalignment; "J" sign with patella; tenderness with patellar compression; crepitus with active extension
- Imaging: None indicated
- Treatment: Relative rest and activity modification; ice; NSAIDs; patellar tracking exercise program; Consider knee sleeve or patellar taping
- Illiotibial band friction syndrome
- History: Lat knee pain worse with running, jumping, cycling; Aggravated with prolonged hill running, slanted road, too much unidirectional track
- PE: TTP along lateral femoral condyle or aprox 2cm above lat joint line; tight IT band with Ober's test
- Imaging: Usually not indicated
- Treatment: Relative rest and activity modification; ice; NSAIDs; hip abductor strengthening, IT band stretching
- Medial tibial stress syndrome (shin splints)
- History: Activity associated shin pain described as dull ache along mid-distal tibia
- PE: TTP posteromedial border of mid - distal tibia - Focal TTP over ant tibia could indicate stress fracture
- Imaging: MRI or bone scan if suspected stress fracture
- Treatment: Relative rest; ice; NSAIDs; stretching; consider insoles or othotics for pes cavus or hyperpronation
- Achilles tendinopathy
- History: Gradual onset of pain in achilles
- PE: TTP 2-6cm prox to attachment; Crepitus suggests acute tenosynovitis; Thompso's test if rupture suspected
- Imaging: Not usually indicated - Sono may be useful
- Treatment: Relative rest, ice, NSAIDs, stretching, heel lifts; short-term walking boots; Eccentric strength training is key
- Plantar fasciitis
- History: Pain in plantar heel or arch worse with first steps in AM
- PE: TTP at medial plantar calcaneal tuberosity and along medial arch; pain with dorsiflexion of toes; pes planus or cavus
- Imaging: Not indicated
- Treatment: Relative rest, ice, massage, NSAIDs, shoe inserts, heel cord and plantar fascia stretching, tension night splints, occ injections
- Stress fracture
- History: Progressive pain over bony structure worse with weight-bearing activity; pain at rest; high suspicion of stress fracture in long distance runners with musculoskeletal pain
- PE: Focal TTP over bony structure
- Imaging: MRI or bone scan; DEXA if osteoporosis is suspected
- Treatment: Relative rest; specialized care
References:
- AFP Vol 76 No 2 Jul 2007
Finger injuries
See also:
Trigger finger
- Definition:
- Impingement of the flexor tendon at the level of the Q1 pulley
- Cause:
- Thickening of the A1 pulley or a nodule on the flexor tendon cuases the tendon to catch on the A1 pulley
- Presentation:
- Pain over the colar MCP joing
- Presence of clicking, catching, or locking of the affected digit
- Exam:
- Pain, nodule, or both at the volar MCP joint
- Repeated finger flexion or slowly opening clenched fist can provoke triggering
- Imaging
- Radiographs are not necessary - if ordered will be negative
- Management
- Corticosteroid injection into the flexor tendon sheath
- Consider splinting if the patient is poor candidate for injection
- Refer to surgery if no improvment after 2-3 injections
Jersey finger
- Definition:
- Avulsion of the flexor digitorum profundus tendon from the distal phalanx
- Cause
- Flexes finger is forced into extension
- Ring finger is commonly affected
- Presentation
- Inability to actively flex DIP
- Exam
- Affected finger might lie in extension
- DIP joint can be passively but not actively flexed
- Might have tenderness over the distal phalynx
- Imaging
- Radiographs might show avulsio fragment from the dorsal base of the distal phalynx
- Management
- Refer for surgery
Mallet finger
- Definition
- Disruption of the extensor tendon due to injury or laceration of the tendon
- Cause
- Usually due to a forced flexion or hyperextension injury
- Can occur after laceration of the dorsal surface of the finger
- Presentation
- Pain and swelling at the DIP joint
- Inability to actively extend the DIP
- Exam
- DIP is flexed and can be passively but not actively extended
- Imaging
- Radiographs might show fracture at dorsal base of the distal phalanx if injury is d/t hyperextension
- Management
- 6-8 weeks of splinting the DIP in extension - splint must be worn continuously
- Refer for surgery if there is subluxation of the distal phalanx or a fracture greater than 1/3 of the articular surface, or the fexor tendon is lacerated
Skiers thumb
- Definition
- Tear of the thumb UCL at the MCP joint
- Cause
- Vlagus force hyperabducts the thumb
- Presentation
- Swelling and pain at the MCP joint
- Weakness of the grip or pinch
- Exam
- Stress exam of the thumb UCL reveals laxity or a soft endpoint, or both; a firm endpoint is found in Grade 2 injury
- Stener lesion (palpable mass over the ulnar side of the MCP joint) might be palpable if the tear is Grade 3
- Imaging
- Order radiographs to evaluate for subluxation of the proximal phalanx
- Order MRI if stres exam is equivocal
- Management
- Grades 1 and 2 - manage with a thumb spica splint for 4-6 weeks
- Grade 3 - Refer for surgery
References:
- AFP Vol 107 No 3 Mar 2023
Foot Fractures
Forefoot
- Great toe
- Ortho referral:
- Lesser toes
- Ortho referral:
- 1st Metatarsal shaft
- Ortho referral:
- Lesser metatarsal shaft
- Ortho referral:
- 5th metatarsal shaft
- Ortho referral:
- Proximal metatarsal
- Ortho referral:
Reference:
- AFP Vol 109 No 2 Feb 2024
Fractures: Foot
Management is determined by the location of the fracture and its effect on balance and weight bearing.
- Metatarsal shaft fractures are initially treated with a posterior splint and avoidance of weight-bearing activities; subsequent treatment consists of a short leg walking cast or boot for four to six weeks.
- Nondisplaced acute metatarsal shaft fractures generally heal well without complications
- Minimally displaced (less than 3 mm) fractures of the second to fifth metatarsal shafts (Figure 2) and fractures with less than 10° of dorsoplantar angulation in the absence of other injuries can generally be managed in the same manner as nondisplaced fractures
- Initial management includes immobilization in a posterior splint, use of crutches, and avoidance of weight-bearing activities.
- Indications for surgical referral include open fractures, fracture-dislocations, multiple metatarsal fractures, intra-articular fractures, and fractures of the second to fifth metatarsal shaft with at least 3 mm displacement or more than 10° angulation in the dorsoplantar plane. Indications for referral of patients with first metatarsal fractures are different because the first metatarsal has a vital role in weight bearing and arch support. Referral is indicated for patients with first metatarsal fractures with any displacement or angulation.
- Metatarsal shaft fractures near the head or base of the first to fourth metatarsal with any degree of displacement or angulation are often associated with concomitant injuries and generally take longer to heal. Patients with these fractures should be referred to an orthopedist.
- Proximal fifth metatarsal fractures have different treatments depending on the location of the fracture.
- A fifth metatarsal tuberosity avulsion fracture can be treated acutely with a compressive dressing, then the patient can be transitioned to a short leg walking boot for two weeks, with progressive mobility as tolerated after initial immobilization.
- A Jones fracture has a higher risk of nonunion and requires at least six to eight weeks in a short leg non–weight-bearing cast; healing time can be as long as 10 to 12 weeks.
- Great toe fractures are treated with a short leg walking boot or cast with toe plate for two to three weeks, then a rigid-sole shoe for an additional three to four weeks.
- Range-of-motion exercises can generally be initiated at four weeks.
- Repeat radiography is indicated and should be obtained one week post-fracture if there was intra-articular involvement or if a reduction was required.
- Healing time is typically four to six weeks. However, return to work and sport can generally take six to eight weeks depending on activity level; some high-level athletes may require more time
- Lesser toe fractures can be treated with buddy taping and a rigid-sole shoe for four to six weeks.
- Indications for referral of toe fractures include a fracture-dislocation, displaced intra-articular fractures, nondisplaced intra-articular fractures involving more than 25% of the joint, and physis (growth plate) fractures. Patients with lesser toe fractures with angulation of more than 20° in the dorsoplantar plane, more than 10° in the mediolateral plane, or more than 20° rotational deformity should also be referred
Reference:
- Am Fam Physician. 2016;93(3):183-191
Fractures in children
Salter-Harris:
- I - through hypertrophic cartilage - point tenderness at epiphysial plate
- II - through both physis and metaphysis - most common
- III - through physis and epiphysis - chronic sequelae as disrupt articulating area but usually no deformities and good prognosis
- IV - cross epiphysis, physis, and metaphysis - high risk of chronic disability
- V - least common and worst prognosis - axial force with compression of epiphysial plate without overt fracture of epiphysis or metaphysis
Heel Pain
Most patients with heel pain improve with conservative treatment, and surgical management should be reserved for recalcitrant cases.
Magnetic resonance imaging is the most accurate test for the diagnosis of most causes of heel pain, but ultrasonography is being used more often as it becomes more readily available at the point of care.
Pain catastrophizing and kinesiophobia are associated with diminished foot function and poorer prognosis.
Notes: In os trigonum syndrome, athletes such as soccer players, gymnasts, and dancers who are engaged in repetitive plantar flexion commonly present with worsening posterior ankle pain and an antalgic gait.
Causes of Heel Pain by Location
Posterior
- Achilles tendinopathy
- Achy, sharp pain with tenderness along the tendon; Worsens with increased activity; Occasional palpable prominence from tendon thickening; Worsens with passive dorsiflexion
- Activity modification, rest and weight-bearing as tolerated, decrease pressure to affected area, heel lifts or orthotics, NSAIDs or analgesics, deep friction massage, ankle bracing, and eccentric exercises
- Haglund deformity
- Pain at the superior aspect of the posterior calcaneus; Radiography may show early deformities
- Decrease pressure to affected area and NSAIDs or analgesics
- Retrocalcaneal bursitis
- Pain, erythema, and swelling around the Achilles tendon; Tenderness on direct palpation
- Decrease pressure to affected area, NSAIDs or analgesics, and corticosteroid injections (preferably ultrasound guided)
- Notes: Retrocalcaneal bursitis is more common in women 40 to 60 years of age with Haglund deformity and a thickened Achilles tendon.
- Calcaneal apophysitis (Sever disease)
- Pain in adolescents that worsens with increased activity or during growth spurt; Tenderness at Achilles insertion; Pain with passive dorsiflexion and mediolateral calcaneal compression
- Activity modification, NSAIDs or analgesics, ice, stretching and strengthening exercises, and orthotics or shoe modifications
- Notes: Calcaneal apophysitis (Sever disease) is the most common cause of heel pain in active children and adolescents; in the outpatient setting, it accounts for up to 16% of musculoskeletal conditions in children.
Inferior
- Calcaneal stress fracture
- Commonly occurs following an increase in activity level or a change to harder walking surfaces; Pain with activity that progressively worsens to pain at rest; Diagnosed with imaging
- Sensations of burning or tingling; Painful lump with palpation
- Heel pad syndrome
- Deep, bruise-like pain and tenderness at middle of heel
- Decrease pressure to affected area, NSAIDs or analgesics, heel cups, taping, and proper footwear
- Heel spurs
- Radiographic findings at site of pain
- Decrease pressure to affected area
- Nerve entrapment (medial or lateral plantar nerve,nerve to or trauma abductor digiti minimi)
- Sensations of burning, tingling, or numbness; Occasionally preceded by increased activity or trauma
- Decrease pressure to affected area, NSAIDs or analgesics, ice, and stretching exercises
- Neuroma
- Activity modification with occasional non-weight-bearing activity, heel pads, walking boots, crutches, or a controlled ankle motion walker
- Decrease pressure to affected area
- Plantar fasciitis
- Pain with first steps after prolonged rest; Tenderness on medial calcaneal tuberosity and plantar fascia
- Rest and activity modification, stretching and strengthening exercises, NSAIDs or analgesics, ice massage, and arch support
- Midfoot (medial)
- Flexor digitorum longus tendinopathy
- Tenderness posterior to medial malleolus and obliquely across sole of foot to base of distal phalanges of lateral toes
- Activity modification, decrease pressure to affected area, NSAIDs or analgesics, and eccentric exercises
- Flexor hallucis longus tendinopathy
- Tenderness posterior to medial malleolus and on plantar surface of great toe
- Activity modification, decrease pressure to affected area, NSAIDs or analgesics, and eccentric exercises
- Posterior tibialis tendinopathy
- Tenderness at navicular and medial cuneiform
- Activity modification, decrease pressure to affected area, NSAIDs or analgesics, and eccentric exercises
- Tarsal tunnel syndrome
- Burning, tingling, or shooting pain and numbness in posteromedial ankle and heel (may extend to toes) that worsens with standing and activity; Positive Tinel sign; Muscle atrophy in severe cases
- Activity modification, orthotics, NSAIDs, neuromodulator therapy, and corticosteroid injections
Midfoot (lateral)
- Peroneal tendinopathy
- Tenderness in lateral calcaneus along path to base of fifth metatarsal
- Activity modification, decrease pressure to affected area, NSAIDs or analgesics, and eccentric exercises
- Notes: Risk factors for peroneal tendon injuries include corticosteroid injections into the peroneal sheath, use of fluoroquinolones, rheumatoid arthritis, hyperparathyroidism, and diabetes.
- Sinus tarsi syndrome
- Pain in lateral calcaneus and ankle; Feeling of foot or ankle instability; Worse after exercise or on uneven surfaces; May have history of repeated ankle sprains
- Orthotics, ice massage, NSAIDs or analgesics, physical therapy (eg, balance/proprioception, strengthening exercises), and corticosteroid injections
Reference:
- Am Fam Physician. 2025;112(6):648-656
Hip Pain in Adults
| Type of pain | History | Physical examination |
|---|---|---|
| Anterior | ||
| Referred | ||
| - Intra-abdominal or intrapelvic | Pain associated with urinary or bowel symptoms, cyclic pain associated with menses | Abdominal and/or pelvic examination |
| Extra-articular | ||
| - Flexor tendon | Overuse activities, acute strain or injury with hip flexion activities | Pain over the hip bony prominence, anterior superior iliac spine, anterior inferior iliac spine, or pubic symphysis; pain with hip flexion strength testing |
| Intra-articular | ||
| - Femoroacetabular impingement | Young, athletic patient; gradual onset; pain with hip range of motion; history of slipped capital femoral epiphysis or developmental dysplasia | Positive FADDIR and FABER test results |
| - Labral tear | Young, athletic patient; acute injury (vs. gradual onset); pain with hip range of motion; mechanical symptoms | Positive FADDIR and FABER test results |
| Femoral neck stress fracture | Overuse/overtraining, energy imbalance in athletes | Antalgic gait, pain with range of motion and ambulating |
| - Avascular necrosis | Middle or older age, smoking, alcohol use, systemic corticosteroid use, hemoglobinopathies, chemotherapy, metabolic syndrome, and obesity | Antalgic gait, pain with range of motion, limited range of motion |
| - Osteoarthritis | Older age, gradual onset, pain with sitting or ambulating for long periods | Antalgic gait, pain with flexion and internal and external rotation, limited range of motion |
| - Hip fracture | Older age, osteoporosis, fall/trauma | Inability to walk on the affected limb; shortened, externally rotated, abducted leg |
| Lateral | ||
| Greater trochanteric pain syndrome, including bursitis, gluteus medius tendinopathy or tear, external snapping, or iliotibial band friction | No injury, middle age, female sex, overweight, pain with sleeping on affected hip, pain aggravated by physical activity or sitting for long periods | Tenderness to palpation over the lateral hip/greater trochanter, Trendelenburg gait or positive Trendelenburg test, positive resisted external derotation test |
| Posterior | ||
| Referred pain | ||
| - Intra-abdominal or intrapelvic | Pain associated with urinary or bowel symptoms, cyclic pain associated with menses | Abdominal and/or pelvic examination |
| Deep gluteal syndrome | Deep buttock pain; no injury; worse with sitting, especially in a car; sciatica (burning pain shooting down the leg) | Seated piriformis stretch test |
| - Ischiofemoral impingement | Gradual onset of deep buttock pain that worsens with activities requiring a long stride (e.g., running) | Long-stride walking test |
| - Lumbar spine or muscle | Pain in the low back (above L5) and hip/buttock, history of lumbar spinal problems | Tenderness over the lumbar spine or lumbar musculature above L5 |
| - Sacroiliac joint pain | No history of lumbar spinal issues | Tenderness over the sacroiliac joint, no tenderness above L5 |
| - Proximal hamstring tendinopathy or tear | Overuse injury with hip extension activities (vs. acute injury with forceful hip extension) | Tenderness to palpation over the ischial tuberosity, pain with hamstring strength testing; acute tears cause ecchymosis of the posterior thigh |
FABER:
- Flexion abduction external rotation test. The examiner (A) passively flexes and then (B) abducts and externally rotates the hip. The result is positive if pain is reproduced in the anterior hip/groin area. This test has been shown to have 42% to 81% sensitivity and 18% to 25% specificity for intra-articular hip pathology.
FADDIR:
- Flexion adduction internal rotation test. The examiner (A) passively flexes then (B) adducts and internally rotates the hip.[corrected] The result is positive if pain is reproduced in the anterior hip/groin area. This test has been shown to have a sensitivity of 59% to 100% and specificity of 4% to 75% for intra-articular hip pathology.
Tests for gluteal tendinopathy.
- Modified Trendelenburg test.
- Patients are instructed to stand on the affected leg/hip and lift the other leg for 30 seconds. The result is positive if the iliac crest falls below the standing side, showing weakness in hip abductors (gluteus muscles). A positive finding on the Trendelenburg test has been shown to have 23% to 97% sensitivity and 77% to 96% specificity for gluteal tendinopathy.4,7
- Resisted external derotation test.
- While the patient lies on a table, the hip is passively flexed to 90 degrees, then externally rotated.[corrected] The patient is asked to return the leg to the same axis as the table (0 degrees rotation), pushing against the examiner's (resisting) hand. The result is positive if pain is reproduced over the lateral hip. This test has been shown to have 88% sensitivity and 97% specificity for gluteal tendinopathy
Posterior Hip Pain
- Piriformis and Deep Gluteal Syndrome
- Seated piriformis stretch test. The patient is seated with 90 degrees of hip flexion. The examiner extends the knee and passively moves the hip into adduction and internal rotation while palpating just lateral to the ischium. The result is positive if pain is reproduced at the piriformis muscle. This test has been shown to have a 91% sensitivity and 80% specificity for deep gluteal syndrome.
- Ischiofemoral Impingement
- Long-stride walking test. The patient is instructed to take a long step on the unaffected leg with the hip pointed forward. This narrows the space between the lesser trochanter and ischium on the posterior (affected) hip, which can reproduce pain caused by ischiofemoral impingement. This test has been shown to have a sensitivity of 94% and specificity of 85% for ischiofemoral impingement.
Reference:
- AFP Jan 2021 Vol 103 No 2
Joint Injections
Specific Corticosteroid Injections:
- Carpal tunnel syndrome
- Can be considered for those wanting to avoid or delay surgery (LOE B)
- D-80 injection reduces proression to surgery at one year (SOR B)
- After injections, 14% progress to surgery in 1 year, and 33% in 5 years (SOR B)
- deQuervan tenosynovitis and trigger finger
- Effective early in therapy (LOE B)
- Epicondylitis
- Short-term improvement in lateral and medial epicondylitis
- High rate of recurrence and are no better than other options in the long term (LOE B)
- Knee and Hip Osteoarthritis
- Short-term relief in those wanting to delay surgery (LOE B)
- Shoulder
- Short-term benefits in adhesive capsulitis and subacromial impingement syndrome (LOE B)
Possible adverse effects of corticosteroid injections
- Anaphylaxis
- Depigmentation of skin
- Elevated blood glucose
- Infection
- Nerve injury
- Pain at injection site
- Subcutaneous fatty atrophy/necrosis
- Tendon/fascial ruptures
References:
- AFP Vol 92 No 8 Oct 2015
- JFP Vol 65 No 2 Feb 2016
- JFP Vol 66 No 8 Aug 2017
Joint Aspiration
Routine synovial fluid analysis:
- Crystals, Synovial Fluid: Test Code 4563
- Cell Count and Differential, Synovial Fluid: Test Code 4562
- Culture, Aerobic and Anaerobic: Test Code 4446
Gram Stain: Test Code 497Culture, Blood: Test Code 389
| Noninflammatory*: <2000 WBC per mm3 (2 x 109 per L) | Inflammatory: >2000 WBC per mm3 |
|---|---|
| Osteoarthritis | Septic arthritis |
| Trauma | Crystal-induced monoarthritis (eg, gout, pseudogout) |
| Avascular necrosis | Rheumatoid arthritis and juvenile idiopathic arthritis |
| Charcot's arthropathy | Spondyloarthritis |
| Hemochromatosis | Systemic lupus erythematosus |
| Pigmented villonodular synovitis | Lyme disease |
| Noninflammatory (such as osteoarthritis) | Inflammatory (such as rheumatoid arthritis) | Septic | Hemorrhagic | |
|---|---|---|---|---|
| WBC count (cells/microL) | <2000 | 2000 to 20,000 | >20,000 | Up to 1 WBC for every 1000 RBCs |
| Percent neutrophils | <25% | 50 to 75% | >75% | <50% |
| Crystal examination by polarized microscopy | Negative | May demonstrate uric acid or CPPD crystals | Negative | Bloody |
| Stain, culture for microorganisms | Negative | Negative | May be positive (depending on organism, prior antibiotic exposure) | Negative |
Procedure
- The patient is supine on the table with the knee extended (some physicians prefer that the knee be bent to 90 degrees). Some physicians prefer the medial approach for smaller effusions, but the lateral approach will be discussed here. The knee is examined to determine the amount of joint fluid present and to check for overlying cellulitis or coexisting pathology in the joint or surrounding tissues.
- The superior lateral aspect of the patella is palpated. The skin is marked with a pen, one fingerbreadth above and one fingerbreadth lateral to this site. This location provides the most direct access to the synovium.
- The skin is washed with povidone-iodine solution. The physician should be gloved, although there is no consensus as to whether sterile gloves must be used. A 21-gauge, 1-inch needle is attached to a 5- to 20-mL syringe, depending on the anticipated amount of fluid present for removal.
- The needle is inserted through stretched skin. Some physicians administer lidocaine (Xylocaine) into the skin, but stretching the pain fibers in the skin with the nondominant hand can also reduce needle-insertion discomfort. The needle is directed at a 45-degree angle distally and 45 degrees into the knee, tilted below the patella (Figure 1).
- Once the needle has been inserted 1 to ¼ inches, aspiration is performed, and the syringe should fill with fluid. Using the nondominant hand to compress the opposite side of the joint or the patella may aid in arthrocentesis.
- Once the syringe has filled, a hemostat can be placed on the hub of the needle. With the needle stabilized with the hemostat, the syringe can be disconnected and the fluid sent for studies. Care should be taken not to touch the needle tip against the joint surfaces when removing the syringe. A syringe filled with corticosteroid medication can then be attached to the needle.
- For injection, use betamethasone (Celestone, 6 mg per mL), 1 mL, mixed with 3 to 5 mL of 1 percent lidocaine. Alternately, methylprednisolone (Depo-Medrol, 40 mg per mL), 1 mL, mixed with 3 to 5 mL of 1 percent lidocaine can be used. After injection of the medication, the needle and syringe are withdrawn.
- The skin is cleansed, and a bandage is is applied over the needle-puncture site. The patient is warned to avoid forceful activity on the joint while it is anesthetized.
| Type | Appearance | WBCs | PMNs | Crystals |
|---|---|---|---|---|
| Normal | Clear | <150 | <25% | None |
| Noninflammatory | Clear | <3000 | <25% | None |
| Inflammatory | Cloudy | >3000 | >50% | Many or None |
| Septic | Cloudy | >50000 | >90% | None |
| Hemorrhagic | Bloody | >2000 | <25% | None |
Reference:
- Am Fam Physician. 2002;66(8):1497-1501
- Akbarnia H, Saber AY, Zahn E. Knee Arthrocentesis. [Updated 2022 Aug 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470229/
- UTD
- Seidman AJ, Limaiem F. Synovial Fluid Analysis. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537114/
Joint Injections
Other references:
| Joint | Needle | Length (in) | Steroid | Analgesic |
|---|---|---|---|---|
| Knee | 22g | 1.5 | 20 mg triamcinolone | 2-4 mL 1% lidocaine |
| Glenohumeral | 22g | 1.5 | 20 mg triamcinolone | 2-4 mL 1% lidocaine |
| Plantar fascia | 25g | 10 mg triamcinolone | 0.5-1 mL 1% lidocaine | |
| Lateral epicondyle | 25g | 20 mg triamcinolone | 1 mL lidocaine | |
| Trigger finger | 25g | 1-1.5 | 10-20 mg triamcinolone | 0.3-0.5 mL 1% lidocaine |
| DeQuervain's | 25g | 1-1.5 | 20 mg triamcinolone | 1 mL 1% lidocaine |
| Trochanteric bursa | 22g | 1.5 | 20 mg triamcinolone | 2-4 mL 1% lidocaine |
| Trigger point | 25g | 0 mg triamcinolone | 1-1.5 mL 1% lidocaine | |
| Carpal tunnel | 25g | 1-1.5 | 20 mg triamcinolone | 1 mL 1% lidocaine |
| Acromioclavicular | 25g | 1-1.5 | 10-20 mg triamcinolone | 0.5 mL 1% lidocaine |
| Location | Gauge | Length (in) |
|---|---|---|
| Shoulder (rotator interval or posterior approach) | 22 | 1.5 > 3.5 |
| Shoulder (anterior approach) | 22 | 3.5 |
| Elbow | 25 | 1.5 |
| Wrist | 25 | 1.5 |
| Hip | 22 | 3.5 > 6 |
| Knee | 22 | 1.5 >> 3.5 |
| Ankle | 25 | 1.5 |
Recent evidence: Lower doses of corticosteroid (20 mg) are as effective as higher doses (40 mg).
References:
- Nate Falk, MD
- AFP Vol 108 No 2 Aug 2023
- Rastogi AK, Davis KW, Ross A, Rosas HG. Fundamentals of Joint Injection. AJR Am J Roentgenol. 2016 Sep;207(3):484-94. doi: 10.2214/AJR.16.16243. Epub 2016 Jun 8. PMID: 27276101.
- AFP Vol 109 No 1 Jan 2024
Knee Pain
Ligament injuries are classified as Grades 1 to 3:
- Grade 1 sprains. The ligament is stretched, but there is no macroscopic tearing; joint stability is maintained.
- Grade 2 sprains. There are partial macroscopic ligament tears. There is joint laxity due to the partial loss of the ligament's structural integrity.
- Grade 3 sprains. The ligament is fully avulsed or ruptured with resultant gross joint instability.
When to consider surgery:
- Neurovascular injury following dislocation
- Unstable fractures
- Joint instability or laxity
- Major tendon rupture
- Locked knee or meniscus tear
- "Bucket handle" meniscus tear
- Osteochondritis dessecans
- Septic arthritis
Reference:
- JFP Vol 72 No 6 July 2023
Ottowa Knee Rules
Criteria for Ordering Radiographs
Radiography is recommended if any one of the following five criteria is present:
- Age ≥ 55 years – Older patients have a higher risk of fractures due to decreased bone density.
- Isolated patellar tenderness – Tenderness directly on the kneecap (patella) without other bone tenderness.
- Tenderness at the fibular head – Pain when pressing on the lateral side of the knee at the top of the fibula.
- Inability to flex the knee to 90 degrees – Measured objectively, often with a goniometer.
- Inability to bear weight – Both immediately after injury and in the emergency department, defined as inability to take four weight-bearing steps, regardless of limping.
Performance and Use
- Sensitivity: ~100% – effectively rules out fractures when negative.
- Specificity: Lower (~39–40%) – some patients without fractures will still be imaged.
- Impact: Reduces unnecessary radiographs by up to 35%, decreasing radiation exposure and healthcare costs.
- Setting: Validated for use in emergency departments and primary care, but not recommended for patients under 18 due to different injury patterns.
Reference:
- Ketelslegers E, Collard X, Vande Berg B, Danse E, El-Gariani A, Poilvache P, Maldague B. Validation of the Ottawa knee rules in an emergency teaching centre. Eur Radiol. 2002 May;12(5):1218-20. doi: 10.1007/s00330-001-1198-9. Epub 2001 Nov 14. PMID: 11976870.
Knee Effusion
| Condition | Mechanism & historical features | Common symptoms | Key examination findings | Additional comments |
|---|---|---|---|---|
| Activity related | ||||
| Chronic osteochondral defect | Mild repetitive trauma (running/jumping) | Diffuse knee pain worse with and after activity | Activity related effusion | Radiographs or advanced imaging (MRI) needed for diagnosis |
| Knee osteoarthritis | Usually adults 50 years or older Activity-related pain; brief stiffness after inactivity | Diffuse knee pain Delayed swelling (12 to 24 hours post activity) | Effusion present Ligaments stable; meniscus testing equivocal Inability to fully flex or extend knee common | Weight bearing radiographs show sclerosis, osteophytes, and joint space narrowing |
| Not activity related | ||||
| Crystal arthropathy | Acute knee pain and effusion No trauma or recent activity | Diffuse knee pain and swelling Weight bearing can be difficult | Erythema, warmth, tenderness, and swelling of knee Knee flexion limited by effusion and pain | Joint aspiration required for diagnosis Serum uric acid level should not be used for diagnosis |
| Infectious arthritis | Acute knee pain and effusion No trauma or recent activity | Diffuse knee pain and swelling Weight bearing can be difficult | Erythema, warmth, tenderness, and swelling of knee Knee flexion limited by effusion and pain | Medical emergency Joint aspiration critical for diagnosis |
| Systemic rheumatic disease | Include RA, SLE, Sjögren's syndrome, systemic sclerosis, spondyloarthropathy, polymyositis, and dermatomyositis RA is most prevalent | Systemic symptoms (fever, night sweats, fatigue, weight loss) and polyarthralgia common | Examination findings highly variable | Consider in oligoarticular or polyarticular joint disease, pain with swelling, systemic symptoms, or a positive family history |
Red Flags
- Fever
- Non-weight bearing
- Loss of distal pulses
- Loss of sensation distal to the knee
- Open fractures
- Cellulitis overlying the knee
Laboratory Evaluation
- Synovial Fluid Aspirate Analysis
- Complete cell count with differential (white blood cell [WBC], polymorphonuclear leukocytes)
- Quest: 4562
- Crystal examination of synovial fluid
- Quest: 4563
- Bacterial Culture and Gram staining of synovial fluid
- Quest: 4550
- Viscosity (RA: expect decreased viscosity and poor mucin clot formation)
- Glucose
- A low level of synovial-fluid glucose is suggestive of an infected joint, but low glucose levels are present in only about 50% of patients with septic joints and can also occur in rheumatoid arthritis.
- Fasting glucose levels are usually reduced to less than half of the simultaneously obtained blood levels.
- Quest: 4410
- The presence of crystals cannot exclude septic arthritis with certainty.[8] Septic arthritis occurs concurrently with gout or pseudogout in less than 5% of cases.
- Complete cell count with differential (white blood cell [WBC], polymorphonuclear leukocytes)
- Septic Arthritis
- Joint fluid appears cloudy or purulent.
- A cell count with WBC greater than 50,000 is considered diagnostic for septic arthritis. However, lower counts may still indicate infection (not sensitive).[9]
- A prosthetic joint with WBC greater than 1100 is considered septic.
- Gram stains only identify infective organisms one-third of the time.
- Glucose will be less than 50% of the serum level.
- Non-Inflammatory Synovial Fluid
- It contains less than 60 to 180 cells per mL, most of which should be mononuclear.
- Synovial fluid is considered non-inflammatory if it contains less than 2000 cells/mL, but most samples of synovial fluids from pts with osteoarthritis contain less than 500 cells per ml.
- The most common cause of non-inflammatory effusions of the knee (synovial fluid white blood cell count less than 2000 cells/mcL) is osteoarthritis; other causes include osteonecrosis, Charcot arthropathy, sarcoidosis, amyloidosis, hypothyroidism, and acromegaly. Inflammatory arthritis (synovial fluid white blood cells greater than 2000 cells/mL) can be caused by infection, autoimmune disease, and crystal-induced arthritis. Aspiration of dark brown serosanguinous fluid should raise the possibility of pigmented villonodular synovitis.
- Inflammatory Synovial Fluid
- Greater than 2000 leukocytes/mL
- Traumatic: Less than 5000 (w/RBCs)
- Toxic Synovitis: 5000 to 15,000 and less than 25% polymorphs
- Acute Rheumatic Fever: 10,000 to 15,000 and 50% polymorphs
- JRA 15,000 to 80,000 and 75% polymorphs
- Greater 50,000 leukocytes/mL;
- Although other diseases, including trauma, may produce WBC cells in joint fluid, levels greater than 50,000/mm3 are usually due to infectious arthritis.
- Usually causes most intense synovial fluid leukocytosis, w/ 50,000 to 200,000 cells/mL and usually over 90% PMNs.
- Lower leukocyte counts are more common early in bacterial arthritis and in patients with disseminated gonococcal infection.
- Non-infectious conditions such as gout, pseudogout, acute rheumatic fever, reactive arthritis, and RA can cause a markedly inflammatory synovial effusion. A finding of greater than 90% PMNs despite a relatively low total leukocyte count should prompt concern about infection or crystal-induced disease. However, the presence of crystals cannot exclude septic arthritis with certainty[10]
- Septic arthritis 80,000 to 200,000 and greater than 75% polymorphs
- In synovial fluid, WBC count and percentage of polymorphonuclear cells from arthrocentesis are the most powerful predictors for septic arthritis. The LR is increased as the synovial fluid WBC count increases.
- For counts greater than 50,000/microL (LR, 7.7; 95% CI, 5.7-11.0) and for counts greater than 100,000/microL (LR, 28.0; 95% CI, 12.0-66.0). On the same synovial fluid sample, a polymorphonuclear cell count of at least 90% suggests septic arthritis with an LR of 3.4 (95% CI, 2.8-4.2), while a PMN cell count of less than 90% lowers the likelihood (LR, 0.34; 95% CI, 0.25-0.47)[6]
Treatment
- Septic joint: Once the lab studies have been sent, start intravenous (IV) antibiotics for the suspected infective agent. The most common bacterial causes include staphylococci (40%), streptococci (28%), gram-negative bacilli (19%), mycobacteria (8 percent), gram-negative cocci (3%), gram-positive bacilli (1%), and anaerobes (1%). Also, an orthopedic consult may be necessary. Drainage of the joint is associated with rapid recovery and low morbidity. Arthroscopy allows visualization of the joint, provides the ability to lyse adhesions, drains any purulent pockets, and can facilitate the debridement of necrotic material if needed.[14]
- Ligamentous injuries: The patient can be placed in a knee brace with an outpatient referral to an orthopedic surgeon.
- Fractures: These may need a referral to a surgeon depending on severity. The Salter-Harris classification can be used for pediatric fractures involving the growth plate.
- Rheumatologic conditions: Anti-inflammatories (NSAIDs) or acetaminophen can be used, and the patient should be referred to a rheumatologist.
- Reactive Arthritis: The primary infection should be treated with the appropriate antibiotic. NSAIDs and acetaminophen can be used for pain.
Reference:
- Gerena LA, Mabrouk A, DeCastro A. Knee Effusion. [Updated 2022 Nov 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532279/
- UpToDate
Knee Pain: Anterior - DDx
- Superior to patella
- Quadriceps tendonitis
- Lateral
- ITB Syndrome (Most common)
- Lateral meniscus tear
- LCL injury
- Medial
- MCL sprain (Most common - Usually <50 yo)
- Medial meniscus tear
- Arthritis
- Patellar
- Patellofemoral Pain Syndrome (Most common)
- Chondromalacia Patella (Usually <40yo)
- Arthritis (Usually >60yo)
- Housemaids knee (inflammation of prepatellar bursa - common in people who kneel a lot)
- Distal to patella
- Patellar tendonitis (Most common)
- Osgood schlatters disease
- Osteochondritis dissecans
- Sinding-Larsen-Johansson disease (like OSD but just below patella)
- Medial/distal to patella
- Medial plica syndrome
- Pes anserine bursitis (Pain about 2 in below the knee)
| Etiology | Comment |
|---|---|
| Articular cartilage injury | May describe history of trauma; mechanical symptoms may occur if loose body present; may have effusion; may have tenderness of involved structure (e.g., femoral condyles, patella) |
| Bone tumors | Pain may be insidious; may have tenderness of bony structures |
| Chondromalacia patellae | Retropatellar pain; may have history of trauma; may have effusion on examination |
| Hoffa's disease | Pain and tenderness localized to infrapatellar fat pad |
| Iliotibial band syndrome | Typically presents with lateral pain and tenderness over lateral femoral epicondyle |
| Loose bodies | Symptoms variable; may have intermittent sharp pain, locking, or effusion |
| Osgood-Schlatter disease | Tenderness and swelling at insertion of patellar tendon at tibial tubercle in an adolescent |
| Osteochondritis dissecans | Symptoms variable; may have intermittent pain, swelling, or locking |
| Patellar instability/subluxation | Intermittent pain with sensation of instability or movement of patella; may have swelling; locking can occur with loose body formation; may have tenderness over medial retinaculum |
| Patellar stress fracture | May have tenderness directly over patella |
| Patellar tendinopathy | Tenderness of tendon; tendon may be thickened if chronic |
| Patellofemoral osteoarthritis | May have crepitus or effusion; characteristic radiographic findings |
| Patellofemoral pain syndrome | Anterior knee pain “behind” or around patella; usually no effusion; may have findings of patellar maltracking |
| Pes anserine bursitis | Pain usually described as medial rather than anterior; tenderness over pes anserine bursa |
| Plica synovialis | May be medial or lateral to patella; if symptomatic, tenderness can be demonstrated on examination |
| Prepatellar bursitis | Characteristic swelling anterior to patella following trauma |
| Quadriceps tendinopathy | Tenderness over tendon |
| Referred pain from the lumbar spine or hip joint pathology | Symptoms depend on origin of pain; knee examination usually normal |
| Saphenous neuritis | Pain usually medial but poorly localized; may have history of surgery |
| Sinding-Larsen-Johansson syndrome | Tenderness at patellar tendon insertion at inferior pole of patella in an adolescent |
| Symptomatic bipartite patella | May have tenderness directly over patella with characteristic radiographic findings |
| Feature | Runner's Knee (PFPS) | Jumper's Knee (Patellar Tendonitis) |
|---|---|---|
| Medical Name | Patellofemoral Pain Syndrome (PFPS) | Patellar Tendinopathy / Tendonitis |
| Primary Location | Behind or around the kneecap | Below the kneecap (on the tendon) |
| Pain Description | Dull, aching, and diffuse | Sharp and localized (pinpoint) |
| Main Cause | Poor kneecap "tracking" or alignment | Overuse/tears of the patellar tendon |
| Common Trigger | Running, walking up/down stairs | Jumping, landing, explosive movements |
| Aggravating Factor | Prolonged sitting with bent knees | Quick starts, stops, or deep squats |
| Physical Signs | Clicking, popping, or grinding sounds | Localized swelling or tenderness on the tendon |
| Primary Rehab | Hip, glute, and quad strengthening | Progressive tendon loading (isometrics) |
Notes:
- The "Theater Sign:" Runner's knee is famous for causing pain after sitting for long periods (like at a movie theater or on a plane). Jumper’s knee usually doesn't flare up from sitting, but rather from explosive "loading" of the leg.
- The Warm-Up Effect:
- Jumper’s knee pain sometimes decreases once you start moving and the tendon "warms up," only to return much sharper after you stop.
- Runner’s knee tends to get progressively worse the longer you perform the activity.
- Anatomy:
- Runner's Knee is like a friction/alignment issue between the kneecap and the thigh bone
- Jumper's Knee is like a wear-and-tear issue on the "rope" (tendon) that connects the kneecap to the shin
Reference:
- Am Fam Physician. 2007;75(2):194-202
Knee Pain: Posterior - DDx
- Behind knee
- Bakers cyst (Most common)
- Arthritis
- ACL tear
- PCL tear
- Hyperextension
- Posterolateral
- Biceps femoris tendinopathy (Often misdiagnosed as ITBS)
- Pesteromedial
- Hamstring tendinopathy
- Lateral pain below knee
- Lateral head gastrocnemius tear
- Medial pain below knee
- Medial head gastrocnemius tear
- Pain below the knee
- Calf muscle cramps
- Calf tear
- DVT
Lateral ankle sprain
Splinting:
- Goal: Provide lateral stability
- Orthoses:
- Stirrup bracing for treatment of grade 1 and 2 injuries
- Use during at-risk activities (more important intervention to reduce recurrence)
- Early mobilization should be integrated into treatment plan
References:
- JFP Vol 67 No 11 Nov 2018
Lateral/medial epicondyle pain
Splinting:
- Goal: Dampen or disperse the forces at the painful area via a counterforce brace
- Orthoses:
- Counterforce brace
- Additionally brace to reduce wrist use - specifically extension or flexion
- Use for less than 30 days
- Avoid use of a volar wrist brace
References:
- JFP Vol 67 No 11 Nov 2018
Leg Cramps
The diagnostic workup for leg cramps focuses on identifying underlying causes through history, physical examination, and targeted laboratory testing, while management emphasizes non-pharmacologic approaches and evidence-based pharmacologic options when necessary.
Diagnostic Workup
The evaluation should identify potential causes including neurologic conditions (ALS, peripheral neuropathies, cramp-fasciculation syndrome), metabolic abnormalities (hypomagnesemia, hypocalcemia, hypothyroidism), renal or liver dysfunction, pregnancy, or medication-related triggers.[1] Medications strongly associated with leg cramps include intravenous iron sucrose, conjugated estrogens, raloxifene, naproxen, and teriparatide.[2] A history and physical examination are usually sufficient to differentiate nocturnal leg cramps from conditions like restless legs syndrome, claudication, myositis, and peripheral neuropathy.[2] Laboratory evaluation and specialized testing are typically unnecessary unless the history or examination suggests a specific underlying disorder.[2]
Management Recommendations
- Non-Pharmacologic Approaches
Combined calf and hamstring stretching for six weeks may reduce cramp severity (mean difference -1.30 cm on a 10-cm visual analogue scale) in adults over 55 years, though evidence for frequency reduction remains uncertain.[3] Calf stretching alone for 12 weeks shows little to no difference in cramp frequency compared to sham stretching.[3] Patient-reported effective non-pharmacologic treatments include massage, stretching, and walking.[4]
- Pharmacologic Options
The American Academy of Neurology provides the following evidence-based recommendations:[1]
Quinine derivatives (200-500 mg daily) are likely effective but should be avoided for routine use due to toxicity concerns. While they reduce cramp number by 28%, intensity by 10%, and cramp days by 20%, the FDA has warned against off-label use citing 665 reports of serious adverse events including 93 deaths since 1969.[5][1] Quinine may be considered only in select patients for an individual therapeutic trial after discussing potential side effects, with a 0.12% risk of thrombocytopenia.[5]
Alternative agents that are possibly effective include:[1]
- Vitamin B complex (including 30 mg/day of vitamin B6) - induced remission in 86% of treated patients in one study
- Diltiazem (30 mg) - reduced cramp frequency (p=0.04) but not intensity
Magnesium supplementation shows minimal benefit for idiopathic nocturnal leg cramps in older adults. Multiple trials found no statistically significant difference between magnesium and placebo in cramp frequency at four weeks (mean difference -0.18 cramps/week, 95% CI -0.84 to 0.49).[6][7] Evidence for pregnancy-associated leg cramps remains conflicting.[6][8]
Vitamin K2 represents an emerging option, with a 2024 trial demonstrating effectiveness in reducing frequency, severity, and duration of nocturnal leg cramps with a favorable safety profile.[9]
The American Academy of Neurology found insufficient evidence to recommend vitamin E, as trials failed to demonstrate significant benefit.[1] While gabapentin, levetiracetam, verapamil, and lidocaine showed promise in open-label studies, these lack sufficient evidence for formal recommendations.[1]
Over-the-counter analgesics are the most commonly used pharmacologic treatment among patients, though nearly one-third seek treatment information online, highlighting the need for evidence-based counseling.[4]
- References
- Assessment: Symptomatic Treatment for Muscle Cramps (An Evidence-Based Review): Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Katzberg HD, Khan AH, So YT. Neurology. 2010;74(8):691-6. https://doi.org/10.1212/WNL.0b013e3181d0ccca.
- Nocturnal Leg Cramps. Allen RE, Kirby KA. American Family Physician. 2012;86(4):350-5.
- Non-Drug Therapies for the Secondary Prevention of Lower Limb Muscle Cramps. Hawke F, Sadler SG, Katzberg HD, et al. The Cochrane Database of Systematic Reviews. 2021;5:CD008496. https://doi.org/10.1002/14651858.CD008496.pub3.
- Patient-Reported Leg Cramp Treatments and Their Effectiveness. Khandalavala B, Geske J, Karloff M. Journal of the American Board of Family Medicine : JABFM. 2024 Nov-Dec;37(6):1123-1129. https://doi.org/10.3122/jabfm.2023.230310R1.
- Quinine for Muscle Cramps. El-Tawil S, Al Musa T, Valli H, et al. The Cochrane Database of Systematic Reviews. 2015;(4):CD005044. https://doi.org/10.1002/14651858.CD005044.pub3.
- Magnesium for Skeletal Muscle Cramps. Garrison SR, Korownyk CS, Kolber MR, et al. The Cochrane Database of Systematic Reviews. 2020;9:CD009402. https://doi.org/10.1002/14651858.CD009402.pub3.
- Effect of Magnesium Oxide Supplementation on Nocturnal Leg Cramps: A Randomized Clinical Trial. Roguin Maor N, Alperin M, Shturman E, et al. JAMA Internal Medicine. 2017;177(5):617-623. https://doi.org/10.1001/jamainternmed.2016.9261.
- Interventions for Leg Cramps in Pregnancy. Luo L, Zhou K, Zhang J, Xu L, Yin W. The Cochrane Database of Systematic Reviews. 2020;12:CD010655. https://doi.org/10.1002/14651858.CD010655.pub3.
- Vitamin K2 in Managing Nocturnal Leg Cramps: A Randomized Clinical Trial. Tan J, Zhu R, Li Y, et al. JAMA Internal Medicine. 2024;184(12):1443-1447. https://doi.org/10.1001/jamainternmed.2024.5726.
Patient Messaging
Options to treat leg cramps (charlie horses):
- Combined calf and hamstring stretching for six weeks may reduce cramp severity
- Supplements:
- Quinine derivatives (200-500 mg daily) are likely effective but should be avoided for routine use due to toxicity concerns.
- Vitamin B complex (including 30 mg/day of vitamin B6) - induced remission in 86% of treated patients in one study
- Magnesium supplementation shows minimal benefit for idiopathic nocturnal leg cramps in older adults.
- Vitamin K2 represents an emerging option, with a 2024 trial demonstrating effectiveness in reducing frequency, severity, and duration of nocturnal leg cramps with a favorable safety profile.
- Medications
- Diltiazem 30 mg - reduced cramp frequency (p=0.04) but not intensity
Low back pain
History: Look for red flags:
- Cauda equina syndrome
- Progressive motor or sensory loss, new urinary retention or overflow incontinence, new fecal incontinence
- Exam:
- Saddle anesthesia
- Loss of anal sphincter tone
- Significant motor deficits encompassing multiple nerve roots
- Fracture
- Significant trauma relative to age, prolonged corticosteroid use, age >50, osteoporosis
- Exam:
- Contusions or abrasions
- Infection
- Spinal procedure in past 12mo, IV drug use, immunosuppression, distant lumbar surgery
- Exam:
- Fever, wound in spinal region
- Localized pain and tenderness
- Malignancy
- History of metastatic cancer, Unexplained weight loss, Age >50, Progressive pain or night pain
- Exam:
- Focal tenderness and localized pain in the setting of risk factors
Physical Exam:
- Evaluation of strength, sensation, and reflexes of lower extremities
- Inspection, palpation, and range-of-motion testing of lumbosacral musculature
- Identify point tenderness, restriction, and spasm
- Straight leg raise
- Ipsilateral pain at <60 degrees is positive for lumbar disk herniation
- Contralateral pain using the crossed straight leg raise is positive for lumbar disk herniation
Differential Diagnosis of Mechanical LBP
- Lumbosacral muscle strains/sprains (70%)
- Often following isolated traumatic incidents or repetitive overuse
- Pain worse with movement, relieved by rest
- Exam might show:
- restricted range of motion
- muscle tenderness
- trigger point
- Lumbar spondylosis (10%)
- More common in persons older than 40 years
- Pain is worse with activity
- Pain may worsen with lumbar spine extension or rotation
- Neurologic examination is usually normal
- Pain may be present in or radiate from the hips
- Disk herniation (5%-10%)
- Most often involves the L5 or S1 nerve root, at L4–L5 or L5–S1 in 90%-95% of cases
- Symptoms may include:
- pain
- paresthesia
- sensory change
- loss of strength or reflexes
- Spondylolysis (<5%)
- Common in young athletes
- Occurs in less than 5% of the general population but in up to 50% of preadolescent and adolescent athletes
- Symptoms often develop insidiously
- Pain with activities involving lumbar extension
- Imaging is diagnostic (early imaging without red flags is not usually necessary)
- Usually occurs in a lower lumbar vertebra, most often L5
- Common in young athletes
- Vertebral compression fracture (4%)
- Risk factors:
- increased age
- history of trauma
- chronic steroid use
- osteoporosis
- Presents:
- localized back pain
- worse with flexion
- often point tenderness on palpation
- Fracture may occur slowly over time or acutely with mild trauma
- Plain radiography should be obtained to confirm diagnosis
- Acute episodes usually resolve in 4-6 weeks
- Risk factors:
- Spondylolisthesis (3%-4%)
- Pain radiates into the buttocks or posterior thigh
- Leg pain may be worse than back pain
- Presents with:
- paresthesias
- numbness
- weakness
- Occurs at L5 in 90% of cases
- Spinal stenosis (3%)
- Presents as back pain
- Sometimes with sensory loss or weakness in the legs
- Calf pain with ambulation and relieved with rest/sitting (pseudoclaudication)
- Neurologic examination findings are normal
- Imaging is diagnostic
- Presents as back pain
Treatment options:
- NSAIDs like ibuprofen or naproxen
- Effective for short term relief without radiculopathy
- Topiramate
- More effective than placebo in chronic low back pain
- Effective for short term relief of nonspecific chronic low back pain
- Avoid opioids as much as possible to reduce misuse, abuse, and dependence
- Effective for short term relief of nonspecific chronic low back pain
- Duloxetine (Cymbalta) effective in those with depression and chronic pain
- Acetaminophen (Tylenol)
- Not more effective than placebo for chronic low back pain
- Topical lidocaine
- Not more effective than placebo for chronic low back pain
- Skeletal muscle relaxants
- More effective pain relief and global efficacy in acute chronic nonspecific low back pain
- No additional benefit when added to naproxen
- Gabapentinoids
- Significant adverse effects without benefits in low pack pain
Consider referral to physical therapy for McKenzie method techniques to reduce he risk of recurrence
References:
- AFP Vol 98 No 7 Oct 2018
- AFP Vol 100 No 11 Dec 2019
Patient Messaging: Low Back Pain
For your back pain:
- Use heat on area for 20 min multiple times a day
- Diclofenac gel 1% OTC apply topically to most painful area once a day
- Ibuprofen 400 mg every 4 hours as needed
- Stay active: Keep moving and stretching
- Muscle relaxers as needed
Here are some general instructions that may be helpful for low back pain:
Immediate Relief (First 24-48 hours)
- Rest: Avoid heavy lifting, bending, or physical activity to prevent further strain on the back.
- Ice: Apply ice packs or a cold compress to the affected area for 15-20 minutes, several times a day, to reduce pain and inflammation.
- Over-the-counter pain relievers: Take acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) as directed on the label to help manage pain and reduce fever.
- Stretching: Gentle stretching exercises can help relieve muscle tension and improve flexibility. Try:
- Knee to chest stretch: Lie on your back, bring one knee towards your chest, and hold for 30 seconds.
- Pelvic tilt: Lie on your back with knees bent and feet flat on the floor. Tilt pelvis upwards and then back down again. Repeat for 10-15 repetitions.
- Knee to shoulder stretch: Stand with feet hip-width apart, then bend one knee towards your chest and hold for 30 seconds. Switch legs.
Short-term Relief (Days 2-7)
- Heat or cold therapy: Apply heat or cold packs to the affected area to reduce pain and inflammation. Heat can help relax muscles, while cold can reduce pain and inflammation.
- Good posture: Maintain good posture by standing up straight, with shoulders back and weight evenly distributed on both feet.
- Lose weight: If you're overweight or obese, losing weight can help alleviate pressure on the lower back.
- Improve sleep: Establish a consistent sleep schedule, avoid lying down after meals, and create a relaxing bedtime routine to improve sleep quality.
- Exercise regularly: Engage in low-impact exercises like yoga, swimming, or cycling to improve flexibility, strength, and overall spinal health.
- Strengthen core muscles: Weak core muscles can contribute to lower back pain. Engage in exercises that strengthen your core, such as planks, bridges, or pelvic tilts.
- Manage stress: High levels of stress can exacerbate low back pain. Practice stress-reducing techniques like meditation, deep breathing, or progressive muscle relaxation.
Long-term Prevention (Ongoing)
- Maintain a healthy weight: Excess weight can put additional strain on the lower back.
- Improve posture: Continue to practice good posture throughout the day, especially when sitting or standing for long periods.
- Engage in regular exercise: Regular physical activity can help improve spinal health and reduce the risk of low back pain.
- Consider physical therapy: A physical therapist can help you develop a personalized exercise program and provide guidance on proper posture and body mechanics.
Risk to progress to chronic low back pain
Scoring: Agree = 1; Disagree = 0
Questions:
- My back pain has spread down my legs some
- I have had pain in the shoulder or neck some time
- I have only walked short distances because of my back pain
- I have dressed more slowly than usual because of back pain
- It's not really safe for a person with a condition like mine to be physically active
- Worrying thoughts have been going through my mind a lot of the time
- I feel that my back pain is terrible and it's never going to get any better
- In general, I have not enjoyed all the things I used to enjoy
- Overall, how bothersome has your back pain been in the past 2 weeks?
- Not at all (0)
- Slightly (0)
- Moderately (0)
- Very much (10
- Extremely (1)
Scores 3 or less are low risk to progress to chronic low back pain
References:
- AFP Vol 100 No 11 Dec 2019
Links to differrent guidelines and society recommendations on Low back pain
- AAFP: https://www.aafp.org/family-physician/patient-care/clinical-recommendations/all-clinical-recommendations/back-pain.html
- ACP: https://www.acpjournals.org/doi/10.7326/M16-2367
- AAPMR: https://www.choosingwisely.org/clinician-lists/aapmr-opiates-for-low-back-pain/
- Europe: https://link.springer.com/article/10.1007/s00586-018-5673-2
- AAOS: https://www.choosingwisely.org/clinician-lists/aaos-avoid-routine-use-of-opioids-for-treatment-of-knee-osteoarthritis-hip-osteoarthritis-low-back-pain-or-rotator-cuff-injury/
- NASS: https://www.choosingwisely.org/clinician-lists/north-american-spine-society-bed-rest-for-more-than-48-hours/
- NASS: https://www.choosingwisely.org/clinician-lists/nass-opioids-for-acute-or-chronic-low-back-pain/
Lumbar Spinal Stenosis
Signs and symptoms of lumbar spinal stenosis:
- Older age at onset
- Longer duration of symptoms
- Symptoms that worsen with walking or standing
- Numbness of the lower legs with activity
- Symptoms that improve with bending forward
- Symptoms that worsen with bending backward
The most strongly suggesting symptoms:
- Improve with bending forward
- Urinary disturbance
- Intermittent claudication
| Patient-reported signs and symptoms | Sensitivity (%) | Specificity (%) | LR+ | LR– |
|---|---|---|---|---|
| History of urinary symptoms | 14 | 98 | 7 | 0.14 |
| Symptoms improve when bending forward | 52 | 92 | 6.5 | 0.52 |
| Intermittent claudication | 82 | 78 | 3.7 | 0.23 |
| Symptoms worsen when standing up | 68 | 70 | 2.3 | 0.46 |
| Bilateral plantar numbness | 27 | 87 | 2.1 | 0.84 |
| Symptoms induced when bending backward | 70 | 55 | 1.6 | 0.55 |
| Findings | Points |
|---|---|
| Age | |
| - < 60 years | 0 |
| - 60 to 70 years | 2 |
| - > 70 years | 3 |
| Onset of symptoms occurred more than six months ago | 1 |
| Symptoms improve when bending forward | 2 |
| Symptoms improve when bending backward | –2 |
| Symptoms worsen when standing up | 2 |
| Intermittent claudication present | 1 |
| Urinary incontinence present | 1 |
| Total: |
Scoring:
- Probability of lumbar spinal stenosis
- ≤ 2: 11/66 (16.7%)
- 3 or 4: 35/120 (29.2%)
- 5 or 6: 78/151 (51.7%)
- ≥ 7: 98/131 (74.8%)
Surgery?
- Decompression surgery may improve short and long term function and pain in patients with lumbar spinal stenosis but is associated with a higher risk of complications
References:
- https://www.aafp.org/pubs/afp/issues/2009/1115/p1145.html
- AFP Vol 110 No 2 Aug 2024
Medial Collateral Ligament injury (MCL)
Splinting:
- Goals/Orthoses:
- Hinged knee brace
- Allows for full extension but limited valgus and varus stress
- Hinged knee brace
- Isolated grades 1 to 2 MCL injuries can be treated conservatively
References:
- JFP Vol 67 No 11 Nov 2018
Morton's Neuroma
Conservative treatment for Morton's Neuroma:
- Decreasing pressure on the metatarsal heads by using a padded shoe insert
- Proper placement of the inserts just in front of (proximal to) the metatarsal head is important
- Treatment inserts are often placed in both shoes, even when symptoms are unilateral, to ensure that you can walk evenly
- Symptomatic relief often begins within a few days of insert use and pain may completely subside over several weeks.
A broad-toed shoe that allows spreading of the metatarsal heads may be helpful.
Here is some information to read more about Morton's Neuroma: https://medlineplus.gov/ency/article/007286.htm
MSK Exams
Elbow
- Inspection
- Look for subtle bicep ruptures
- Palpation
- ROM
- Flexion/Extension
- Pronation/Supination
- Strength
- Neurovascular
- Ulnar nerve tinel
- Posterior interosseous/Radial nerve
- Special Tests
- Anterior - Hook test
- Lateral - resisted wrist and middle finger extension
- Medial - Milking maneuver, moving valgus stress test
Knee Exam
- Inspection
- Palpation
- Joint lines, Quad/Patellar tendon, Patellar facets
- ROM
- Flex/extension
- Strength
- Straight leg raise
- Neurovascular
- Special Tests
- Major ligaments
- ACL (Lachman, Ant drawer)
- PCL (Posterior drawer, sag sign)
- MCL/LCL (varus and valgus stress)
- Menisci (McMurray, Thessaly)
- PFPS (Patellar grind/shrug, patellar movement, single-leg squat)
- Iliotibial band (Ober test)
- Major ligaments
Shoulder Exam
- Inspection - Don't forget the scapula
- Palpation
- SC to AC joints
- ROM
- Abduction, flexiion, ER, IR (measured by spinal level)
- Strength
- SITS muscles (full can, external rotation, belly press)
- Neurovascular
- Shoulder Special Tests
- Impingement (Neer's, Hawkin's)
- AC joint (1-finger sign, O'Brien's active compression)
- Labrum (Bicep load 2, Load/Shift, Crank, O'Brien's, Passive distraction)
- Bicep (Speed's, Yergason's)
- Instability (Apprehension, sulcus)
- Shoulder Special Tests
- Empty Can Test
- Commonly used orthopedic examination test for supraspinatus impingement or integrity of the supraspinatus muscle and tendon
- The Empty Can Test is considered positive if there is significant pain and/or weakness.
- The test is more accurate for detecting a tear in the muscle or tendon if very significant weakness is present.
- Drop Arm Test
- Supraspinatus tendon
- The patient is asked to actively lower their arm from abduction to their side in a slow and controlled manner.
- A positive test is determined by the patient's inability to smoothly control the lowering of their arm or the inability to hold the arm in 90 degrees of abduction. In a positive test that starts above 90 degrees of abduction, the patient will tend to have difficulty controlling the movement around 90 degrees of abduction. There may or may not be pain reported. Pain alone is not a positive test.
- Neer Test
- subacromial impingement of rotator cuff tendons
- From the starting position, the examiner internally rotates the patient's arm and forcefully moves the arm through the full range of forward flexion or until reports of pain.
- The Neer test is considered positive if pain is reported in the anterior – lateral aspect of the shoulder.
- Negative Likelihood Ratio = .35
- Sensitivity: 75% for subacromial bursitis, 85% for rotator cuff pathology
- Hawkins Test
- Structures:
- supraspinatus tendon
- the most likely involved structure in a positive test
- subacromial bursa
- long head of biceps tendon
- not as likely involved as supraspinatus tendon
- a-c joint
- pain during this test may also be the result of an injury to the acromioclavicular joint
- supraspinatus tendon
- The examiner moves the arm of the shoulder to be tested such that the arm is in 90 degrees of forward flexion and the elbow is flexed to 90 degrees.
- The Hawkins Kennedy test is considered positive if pain is reported in the superior – lateral aspect of the shoulder.
- Specificity: 62%
- Sensitivity: 92% for subacromial bursitis, 88% rotator cuff tear
- Structures:
- Speed's Test
- Long Head Biceps Tendonitis
- The test is best performed with the patient in a relaxed sitting position. The arm to be tested should be in about 60 degrees of front flexion with the forearm supinated and the elbow fully extended.
- In the starting position the examiner forcefully presses down on the patient's arm at the forearm. The patient attempts to resist the pressure of the examiner. Alternatively the patient attempts to forward flex the shoulder while the examiner resists.
- Positive:
- Speed's Test is considered positive if pain is reported in the bicipital groove. Weakness in maintaining the forward flexion position will also likely be noted.
- A positive test is indicative of biceps tendon instability or tendonitis.
- Tenderness on palpation of the bicipital groove is also and indicator of bicipital tendonitis.
- When the therapist stops pushing down on the arm a sudden jerking motion may result. Pain at this point may indicate a positive test for sub-acromial bursitis.
- O'Brien's Test
- glenohumeral joint labral tears (and more specifically for SLAP Lesions; superior labral tear from anterior to posterior)
- The test is best performed with the patient in a relaxed sitting position but can also be performed in standing. The arm to be tested should be in 90 degrees of flexion and about 10 degrees of adduction. The patient then internally rotates the arm, pronating at the elbow and essentially pointing the thumb to the ground.
- The examiner provides a downward force distally on the arm while the patient resists with an upward force. The examiner can also instruct the patient to simultaneously externally rotate the arm while the examiner resists this as well. The test is then repeated but with the arm in neutral rotation.
- The test is considered positive if there is pain and/or clicking when the arm is in full internal rotation but not when the arm is in neutral rotation. Pain over the acromioclavicular joint (a-c joint) indicates pathology at that joint while pain felt 'deeper' in the shoulder is more indicative of glenoid labrum pathology. In the event of a-c joint pathology the patient will likely complain of pain in both positions of the test.
- Bear Hug Test
- Subscapularis
- This test is usually performed with the patient in sitting. The patient's arm is placed with the open hand of the affected side placed just in front of the shoulder on the opposite site.
- In this position, the examiner attempts to pull the affected arm forward, away from the patient's chest/shoulder as the patient attempts to resist the movement.
- The Bear Hug Test is considered positive if the patient has significant weakness and/or pain.
- The Bear Hug Test for integrity of the subscapularis is considered to have very high sensitivity and negative predictive value. Sensitivity 75%, specificity 56%, positive predictive value 62%, negative predictive value 70% and accuracy 65%.
- Gerber's Lift Off Test
- subscapularis tendon or subscapularis tendonitis
- The patient's arm is placed in internal rotation with the hand behind the small of the back/mid-lumbar spine. The dorsum of the hand (back of the hand) is against the patient's lumbar spine.
- In this position, the patient attempts to move the hand away from the lower back by extending and further internally rotating the arm. The examiner can also provide resistance to this movement if the patient is able to complete the movement.
- The Lift-Off Test is considered positive if the patient is unable to move the hand away from the back or is very weak in doing so. The test is also positive if pain is reported
- Specificity of this test has been shown to be 92%.
- Hornblower's Test
- Muscles:
- teres minor muscle
- teres minor tendon
- infraspinatus muscle
- infraspinatus tendon
- The arm to be tested is elevated to 90 degrees of shoulder abduction in the scapular plane. The elbow is to be in 90 degrees of flexion and is externally rotated.
- In the starting position the examiner applies an internal rotation force to the forearm or wrist. The patient is asked to resist movement, thereby attempting to externally rotate (laterally rotate) the shoulder.
- The Hornblower's test is considered positive if pain is reported by the patient and/or significant weakness is noted by the examiner.
- Hornblower's Sign: it is generally considered positive if the patient is unable to hold the arm themselves in the text position; holding the arm up with the hand to the mouth as if blowing a horn.
- Likelihood ratio: 4.81
- SDpecificity: 96%
- Muscles:
- Yergason's Test
- Structures:
- biceps tendon
- glenoid labrum
- transverse humeral ligament
- On the side to be tested the one of the examiner's hands palpates the bicipital groove. The arm to be tested is relaxed at the person's side. The elbow is flexed to 90 degrees and the forearm is in neutral position or is pronated.
- The examiner's other hand applies downward pressure on the patient's forearm (attempt to extend the patient's elbow) while also attempting to move the patient's forearm into further pronation. The patient forcefully resists these movements.
- Yergason's Test is considered positive for bicipital tendinopathy if there is pain in the area of the bicipital groove. The test is positive for transverse ligament pathology if there is a snapping of the bicipital tendon.
- The test can also appear positive when the pathology is related to the glenoid labrum; e.g. SLAP lesion.
- Structures:
Table 159: Diagnostic Accuracy of Special Tests in Rotator Cuff Tear Diagnosis Number of Patients with Tear Sensitivity (%) (95% CI) Specificity (%) (95% CI) Likelihood Ratio (+) (95% CI) Test Yield (%) SUBSCAPULARIS Lift off test 60 22 (12–33) 94 (90–99) 3.81 (1.53–9.49) 97.0 Passive lift off 60 19 (9–29) 95 (91–99) 3.77 (1.38–10.31) 98.2 Belly-press test 66 28 (17–39) 87 (81–94) 2.23 (1.19–4.17) 98.3 Belly-off sign 63 18 (8–27) 96 (93–100) 4.79 (1.59–14.41) 98.8 Bear hug 64 32 (20–43) 81 (74–88) 1.69 (1.0–2.87) 99.4 INFRASPINATUS External rotation lag sign at 0° 67 10 (3–18) 98 (96–100) 6.06 (1.30–28.33) 100 External rotation lag sign at 90 ° 63 8 (1–15) 100 (100–100) - 99.4 Hornblower's sign 65 17 (8–26) 96 (93–100) 4.81 (1.60–14.49) 98.9 SUPRASPINATUS Jobe's test 67 88 (80–96) 62 (53–71) 2.30 (1.79–2.95) 99.5 Full can test 65 70 (59–82) 81 (74–88) 3.75 (2.47–5.69) 99.4 Drop arm test 67 24 (14–34) 96 (93–100) 6.45 (2.25–18.47) 100 Neer's sign 68 60 (48–71) 58 (49–67) 1.42 (1.06–1.91) 99.4 Hawkin's sign 68 64 (53–76) 48 (38–57) 1.23 (0.95–1.58) 99.4 BICEPS PATHOLOGY Speed's test 16 75 (54–96) 45 (37–52) 1.35 (0.99–1.86) 99.4 Bicipital groove tenderness 16 69 (46–91) 57 (50–65) 1.61 (1.11–2.35) 100 Reference:
- Jain NB, Luz J, Higgins LD, Dong Y, Warner JJ, Matzkin E, Katz JN. The Diagnostic Accuracy of Special Tests for Rotator Cuff Tear: The ROW Cohort Study. Am J Phys Med Rehabil. 2017 Mar;96(3):176-183. doi: 10.1097/PHM.0000000000000566. PMID: 27386812; PMCID: PMC5218987.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5218987/
- Empty Can Test
- Rotator Cuff
- Supraspinatus
- Patient lifts an object in the plane of scaption (90 degrees of abduction and approximately 30 degrees of forward flexion)
- Patient fully abducts the arm and then slowly reverses the motion in the same arc. Test is positive for rotator cuff tear if arm drops suddenly or patient has severe pain (drop-arm sign)
- Infraspinatus and teres minor
- Patient lies on unaffected side and externally rotates against gravity or with an object
- Subscapularis
- With the patient facing to the side and the arm internally rotated behind the back, the patient lifts the hand away from the back against gravity (lift-off test)
References:
- AFP Feb 2021 Vol 103 No 3
- Supraspinatus
Hip Exam
- Inspection
- Gait, hip height, leg lengths
- Palpation
- Greater trochanter
- ROM
- Flex/extension, IR/ER (prone IR for kids), abduction/adduction
- Strength
- Neurovascular
- Special Tests
- FABER
- FADIR +/- axial load (FADaxl)
- Ober test
- Modified Thomas test (Quad and hip flexor tightness)
Lower Extremity
- FABER (Patrick) test
- While the patient is lying on their back, the hip is flexed, abducted to the side, and externally rotated into a "figure of four" position
- Sacroiliac joint or intra-articular pathology (depending on localization of pain)
- FADIR test
- While the patient is lying on their back, the hip is flexed, adducted toward midline, and internally rotated
- Pain suggests intra-articular pathology
- Trendelenburg test
- Patient stands facing away from camera and balances on one foot for 30 seconds
- Inability to maintain pelvis stability parallel to the ground suggests pelvic instability (stance leg)
References:
- AFP Feb 2021 Vol 103 No 3
Hand and Wrist
- Finkelstein test
- Patient grasps a weighted object and tilts wrist down (ulnar deviation) against gravity
- Pain with this maneuver suggests de Quervain tenosynovitis
- Froment sign
- Patient grasps a piece of paper between thumb and index finger on affected side and attempts to pull it out with opposite hand
- Difficulty holding paper suggests ulnar nerve injury
- Phalen test
- With arms raised to the level of shoulders, patient brings dorsum of hands together in midline, holding in forced flexion for 30 to 60 seconds
- Burning, numbness, or tingling in the median nerve distribution suggests carpal tunnel syndrome
- Press test
- Seated patient pushes their body weight up off a chair using affected wristA1
- Focal ulnar wrist pain with this maneuver suggests triangular fibrocartilage complex injuries
- Reverse Phalen test
- With arms raised to the level of shoulders, patient brings palms together in midline, holding in forced flexion for 30 to 60 seconds
- Carpal tunnel syndrome (same as Phalen test)
References:
- AFP Feb 2021 Vol 103 No 3
MSK Tests
SI Joint
- +Faber (Figure 4 test) (hip pathology or SI joint affected)
- like piriformis stretch while supine
- positive if affected (crossed) leg cannot be lower than other leg
- TTP or pain along SI joint line
Nocturnal Leg Cramps
Associated Medical Conditions:
- Cancer treatment
- Cardiovascular disease
- Cirrhosis
- End stage renal disease and hemodialysis
- Lumbar canal stenosis
- Neurologic deficit
- Osteoarthritis
- Peripheral neuropathy
- Peripheral vascular disease
- Pregnancy
- Venous insufficiency
Management:
- Treat underlying alternative diagnosis
- Trial of exercise, stretching, massage
- Trial of magnesium, calcium channel blocker, muscle relaxant, vit B12
- Consider diagnosis and management of Restless Leg Syndrome
Differential Diagnosis:
- Claudication
- Pain with ex, relieved with rest
- Modfy risk factors
- Graded exercise
- Exercise-associated muscle cramping
- Graded exercise and stretching
- Hypnic myoclonus
- sudden involuntary jerking at onset of sleep
- Reassurance
- Myositis, myalgias
- pain unrelated to exertion
- Treat underlying cause
- Periodic limb movement disorder
- Nonpainful, repetitive, rhythmic, slow dorsiflexion of toes, knees, and hips during sleep, with pt unaware
- Sleep modification
- Peripheral neuropathy
- Treat underlying condition
- Pain medications, anticonvulsants, TCAs
- Restless leg syndrome
- Irresistible urge to move or shake the legs, relieved with movement
- Dopaminergic drugs
References:
- AFP Vol 86 No 4 Aug 2012
Osteoarthritis
Treat pain from knee osteoarthritis (OA) with weight management and low-impact exercise to decrease the risk of disease progression. (SOR A)
Stepped-Care Approach:
- Encourage regular exercise and weight loss. Consider physical therapy, bracing, and splinting. (SOR B)
- Begin with acetaminophen (SOR A)
- Start oral or topical NSAID therapy (SOR A)
- Add combination glucosamine and chondroitin - discontinue if no change after 3 months (SOR B)
- Consider opioid therapy but monitor closely
- Consider corticosteroid injection for acute exacerbation of knee OA (SOR A)
- Consider hyaluronic acid injection for persistent knee OA (SOR B)
- Discuss total joint replacement for OA of the hip,knee, or shoulder if steps are unsuccessful (SOR B)
Splinting:
- Goals/Orthoses:
- Simple knee sleeve (mild-mod OA to improve functional scores)
- warmth and proprioception
- Valgus unloader brace (inconclusive evidence - reserve for advanced OA)
- valgus stress to open and unload the medial compartment
- Recommend a medial unloading (valgus) knee brace for short-term relief of medial knee OA. (SOR B)
- Simple knee sleeve (mild-mod OA to improve functional scores)
Risk Factors:
- Advancing age
- Increased BMI
- Prior injury (ACL or meniscus tear)
- Occupation involving high physical workload
- Female gender
- Knee malalignment
- Genetic variables
References:
- AFP Vol 85 No 1 Jan 2012
- JFP Vol 67 No 11 Nov 2018
- JFP Sep 2020 Vol 69 No 7
Overtraining Syndrome
| Term | Synonym | Definition | Performance Decrement | Outcome |
|---|---|---|---|---|
| Functional overreaching | Short-term overreaching | Increased training leading to a temporary performance decrement and with improved performance after rest | Days to weeks | Positive (super- compensation) |
| Nonfunctional overreaching | Long-term overreaching | Intense training leading to a longer performance decrement but with full recovery after rest; accompanied by increased psychologic and/or neuroendocrinologic symptoms | Weeks to months | Negative due to symptoms and loss of training time |
| Overtraining syndrome | Consistent with extreme nonfunctional overreaching but with (1) longer performance decrement (> 2 months), (2) more severe symptomatology and maladapted physiology (psychologic, neurologic, endocrinologic, immunologic systems), (3) and an additional stressor not explained by other disease | Months | Negative due to symptoms and possible end to athletic career |
| Parasympathetic Alterations | Sympathetic Alterations | Other |
|---|---|---|
| (more common aerobic sports) | (more common anaerobic sports) | |
| Fatigue | Insomnia | Anorexia |
| Depression | Irritability | Weight loss |
| Bradycardia | Agitation | Lack of mental concentration |
| Loss of motivation | Tachycardia | Heavy, sore, stiff muscles |
| Hypertension | Anxiety | |
| Restlessness | Awakening unrefreshed |
Potential triggers of overtraining syndrome
- Increased training load without adequate recovery
- Monotony of training
- Excessive number of competitions
- Sleep disturbances
- Stressors including personal life (family, relationships) and occupational
- Previous illness
- Altitude exposure
- Heat injury episode
- Severe "bonk"
Diagnosis: Diagnosis of OTS is clinical and accomplished through history, which should demonstrate the following:
- Decreased performance persisting despite weeks to months of recovery
- Disturbances in mood
- Lack of signs/symptoms or diagnosis of other possible causes of underperformance
The list of organic diseases that can result in underperformance is extensive and not limited to the following:
- Undiagnosed asthma/bronchial hyperreactivity
- Thyroid disease
- Adrenal disease
- Diabetes mellitus or insipidus
- Iron deficiency with or without anemia
- Infection (myocarditis, hepatitis, HIV, etc)
- Malnutrition (due to eating disorders, celiac sprue, etc).
Workup
- History
- An extensive nutrition history should be obtained along with an assessment of caloric expenditure
- Labs
- comprehensive metabolic panel (including kidney function, potassium, magnesium, and glucose)
- complete blood count
- erythrocyte sedimentation rate
- C-reactive protein
- iron studies
- creatine kinase
- thyroid stimulating hormone
Stages of Overtraining Syndrome:
- Stage 1: Overreaching (physical symptoms, no significant decline in performance)
- Stage 2: Sympathetic Overtraining Syndrome (physical and mental symptoms, increased stress response)
- Stage 3: Parasympathetic Overtraining Syndrome (most severe, prolonged recovery period)
Treatment
- Treatment of NFO and OTS is rest; however, some propose that relative rest is more appropriate.3 It is recommended to build up volume prior to intensity, starting from 5 to 10 minutes daily until 1 hour is tolerated.3 It is unclear which strategy is best, so the motivation for exercise, internal versus external, should be considered when recommending complete versus relative rest. Given the significant psychological overlay, one may consider involving a sports psychologist or other mental health expert in multidisciplinary management.30 If stress, depression, and/or anxiety are increased with full rest, relative rest with well-defined expectations should be provided.30
- Treatment with selective serotonin reuptake inhibitor is suggested by some based on similarities between neuroendocrinologic changes between depression and OTS.2,38 However, one should be cautious of increased heat stress and possible decreased performance with antidepressant treatment in athletes. In addition, if sleep complaints are prominent, treatment with trazodone or amitriptyline could be considered.38
Preventative measures for nonfunctional overreaching/overtraining syndrome.
- Periodization of training
- Tapering for competition
- Adjust training volume and intensity based on performance and mood
- Ensure adequate calories for training load
- Ensure adequate hydration
- Ensure adequate carbohydrate ingestion during exercise
- Ensure adequate sleep
- Promoting mental toughness or resilience as buffer
- Rest period of greater than 6 hours between exercise bouts
- Abstinence of training following infection, heat stroke/stress, periods of high stress
- Avoid extreme environmental conditions
- Utilize Profile of Mood States (or stress level) and alter training load
Reference:
- Kreher JB, Schwartz JB. Overtraining syndrome: a practical guide. Sports Health. 2012 Mar;4(2):128-38. doi: 10.1177/1941738111434406. PMID: 23016079; PMCID: PMC3435910.
Overtraining Syndrome (Review for accuracy) edit
Overtraining syndrome, also known as burnout, is a chronic maladaptive condition resulting from excessive, prolonged training with inadequate recovery time. It affects athletes and individuals who engage in intense physical activity, leading to a decline in performance, mood changes, and physical symptoms.
Common Symptoms:
- Decreased performance and efficiency during exercise
- Chronic fatigue and exhaustion
- Mood changes, including depression, anxiety, and irritability
- Sleep disturbances and insomnia
- Increased resting and delayed recovery heart rate
- Decreased body mass and muscle loss
- Sustained muscle and joint pain
- Lack of appetite and decreased nutrient intake
- Increased sensitivity to illnesses and infections
- Emotional instability and fear
Risk Factors:
- Specializing in a single sport
- Sudden increases in training intensity or volume
- Participation in endurance sports
- Low self-esteem
- Parental and coaching pressure to perform
- Insufficient recovery time between training sessions
Diagnosis:
- Based on an athlete's history and symptoms
- Absence of alternative explanations for symptoms
- No single test exists for overtraining syndrome; diagnosis relies on a combination of clinical evaluation and laboratory tests
Treatment:
- Rest and cessation of training for a set period (4-12 weeks)
- Low-intensity aerobic exercise to maintain fitness during the recovery period
- Gradual return to training when symptoms resolve
- Flexibility in training regimens with planned breaks and longer breaks every few months
- Supportive environment from parents and coaches
- Awareness of body cues indicating a need to slow down or change training routines
Prevention:
- Monitor heart rate at rest and during exercise
- Note changes in heart rate and adjust training accordingly
- Incorporate variety and flexibility in training regimens
- Prioritize recovery time and listen to body cues
- Make training fun and engaging to maintain motivation and enjoyment
Stages of Overtraining Syndrome:
- Stage 1: Overreaching (physical symptoms, no significant decline in performance)
- Stage 2: Sympathetic Overtraining Syndrome (physical and mental symptoms, increased stress response)
- Stage 3: Parasympathetic Overtraining Syndrome (most severe, prolonged recovery period)
By understanding the symptoms, risk factors, diagnosis, treatment, and prevention strategies, individuals can take proactive steps to avoid overtraining syndrome and maintain optimal physical and mental well-being.
Peripheral nerve entrapment (Upper Extremity)
| Joint function | Cervical root | Muscles | Nerves |
| Shoulder abduction | C5 | Deltoid | Axillary |
| Elbow flexion | C5, C6 | Biceps | Musculocutaneous |
| Elbow extension | C7 | Triceps | Radial |
| Forearm pronation | C6, C7 | Pronator teres | Median |
| Forearm supination | C6 | Supinator | Radial |
| Wrist flexion | C7 | Flexor carpi radialis, flexor carpi ulnaris | Median and ulnar |
| Wrist extension | C6, C7 | Extensor carpi radialis brevis, extensor carpi radialis longus | Radial |
| Finger flexion | C8 | Flexor digitorum profundus, flexor digitorum superficialis | Ulnar and median |
| Finger extension | C7, C8 | Extensor digitorum, extensor indicis, extensor digiti minimi | Radial (posterior interosseous) |
| Thumb abduction | C7, C8 | Abductor pollicis longus | Radial (posterior interosseous) |
| Thumb flexion | C8, T1 | Flexor pollicis longus | Median (anterior interosseous) |
| Finger abduction or adduction | T1 | Intrinsic hand muscles | Ulnar |
References:
- AFP Col 103 No 5 Mar 2021
Physical activity
Running
- Running as little as 5-10 min a day can greatly reduce mortality risk adding potentially 3 years to a life expectancy.
- Same benefits for those running <1hr/wk as >3hrs/wk.
Walking
- Lowers systolic blood pressure by 4.11 mm Hg (95% CI, 3.01 to 5.22 mm Hg)
- Lowers diastolic blood pressure by 1.79 mm Hg (95% CI, 1.07 to 2.51 mm Hg) and resting heart rate by 2.76 beats per minute (bpm; 95% CI, 0.95 to 4.57 bpm) (SOR: C)
Needed for Maximum Cardiovascular Benefit:
- Walk: Brisk 1 hour walk 5 days a week
- Run: Jog at 10 min/mile pace for 30 min twice a week
- Running at 6mph for 30min 2x/wk (10-metabolic equivalent of task hours) is associated with 40% reduction in cardiovascular disease mortality
- Additional exercise does not demonstrate additional mortality reduction
- It is ok to cram weeks worth of activity into the weekend (Comparable reduction in risk as to those who exercise throughout the week: 40% to 41%)
Mortality benefits:
- 15 min of mod-intensity physical activity daily is associated with 14% reduction in relative risk of all cause mortality and 19% reduction in death from cardiovascular disease
- Each additional 15 min of moderate exercise further reduced mortality by 4%
Stand:
- Those who stood for 2-5 hours a day have 10% lower risk of all-cause mortality than those who stood for <2 hrs a day
- Stadning for 5-8 hours a day is associated with 15% relative risk reduction
- Standing for >8 hrs a day is 24% relative risk reduction
Reference:
- Fam Prac News Vol 50 No 3 Mar 2020
- J Am Coll Cardiol. 2014;64(5):472-481
- JAMA Intern Med.1 2017 Mar 1;177[3]:335-42
- Lancet 2011 Oct 1;378[9798]:1244-53
- Prev Med. 2014 Dec;69:187-91
- AFP Jan 2022 Vol 105 No 1
2018 Physical Activity Guidelines for Americans
- Key Guidelines for Preschool-Aged Children:
- Preschool-aged children (ages 3 through 5 years) should be physically active throughout the day to enhance growth and development.
- Adult caregivers of preschool-aged children should encourage active play that includes a variety of activity types.
- Key Guidelines for Children and Adolescents:
- It is important to provide young people opportunities and encouragement to participate in physical activities that are appropriate for their age, that are enjoyable, and that offer variety.
- Children and adolescents ages 6 through 17 years should do 60 minutes (1 hour) or more of moderate-to-vigorous physical activity daily:
- Aerobic:
- Most of the 60 minutes or more per day should be either moderate- or vigorous-intensity aerobic physical activity and should include vigorous-intensity physical activity on at least 3 days a week.
- Muscle-strengthening:
- As part of their 60 minutes or more of daily physical activity, children and adolescents should include muscle-strengthening physical activity on at least 3 days a week.
- Bone-strengthening:
- As part of their 60 minutes or more of daily physical activity, children and adolescents should include bone-strengthening physical activity on at least 3 days a week.
- Aerobic:
- Key Guidelines for Adults:
- Adults should move more and sit less throughout the day. Some physical activity is better than none. Adults who sit less and do any amount of moderate-to-vigorous physical activity gain some health benefits.
- For substantial health benefits, adults should do at least 150 minutes (2 hours and 30 minutes) to 300 minutes (5 hours) a week of moderate-intensity, or 75 minutes (1 hour and 15 minutes) to 150 minutes (2 hours and 30 minutes) a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. Preferably, aerobic activity should be spread throughout the week.
- Additional health benefits are gained by engaging in physical activity beyond the equivalent of 300 minutes (5 hours) of moderate-intensity physical activity a week.
- Adults should also do muscle-strengthening activities of moderate or greater intensity and that involve all major muscle groups on 2 or more days a week, as these activities provide additional health benefits.
- Key Guidelines for Older Adults - The key guidelines for adults also apply to older adults. In addition, the following key guidelines are just for older adults:
- As part of their weekly physical activity, older adults should do multicomponent physical activity that includes balance training as well as aerobic and muscle-strengthening activities.
- Older adults should determine their level of effort for physical activity relative to their level of fitness.
- Older adults with chronic conditions should understand whether and how their conditions affect their ability to do regular physical activity safely.
- When older adults cannot do 150 minutes of moderate-intensity aerobic activity a week because of chronic conditions, they should be as physically active as their abilities and conditions allow.
- Key Guidelines for Women During Pregnancy and the Postpartum Period:
- Women should do at least 150 minutes (2 hours and 30 minutes) of moderate-intensity aerobic activity a week during pregnancy and the postpartum period. Preferably, aerobic activity should be spread throughout the week.
- Women who habitually engaged in vigorous-intensity aerobic activity or who were physically active before pregnancy can continue these activities during pregnancy and the postpartum period.
- Women who are pregnant should be under the care of a health care provider who can monitor the progress of the pregnancy. Women who are pregnant can consult their health care provider about whether or how to adjust their physical activity during pregnancy and after the baby is born.
- Key Guidelines for Adults With Chronic Health Conditions and Adults With Disabilities:
- Adults with chronic conditions or disabilities, who are able, should do at least 150 minutes (2 hours and 30 minutes) to 300 minutes (5 hours) a week of moderate-intensity, or 75 minutes (1 hour and 15 minutes) to 150 minutes (2 hours and 30 minutes) a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. Preferably, aerobic activity should be spread throughout the week.
- Adults with chronic conditions or disabilities, who are able, should also do muscle-strengthening activities of moderate or greater intensity and that involve all major muscle groups on 2 or more days a week, as these activities provide additional health benefits.
- When adults with chronic conditions or disabilities are not able to meet the above key guidelines, they should engage in regular physical activity according to their abilities and should avoid inactivity.
- Adults with chronic conditions or symptoms should be under the care of a health care provider. People with chronic conditions can consult a health care professional or physical activity specialist about the types and amounts of activity appropriate for their abilities and chronic conditions.
- Key Guidelines for Safe Physical Activity - to do physical activity safely and reduce risk of injuries and other adverse events, people should:
- Understand the risks, yet be confident that physical activity can be safe for almost everyone.
- Choose types of physical activity that are appropriate for their current fitness level and health goals, because some activities are safer than others.
- Increase physical activity gradually over time to meet key guidelines or health goals. Inactive people should "start low and go slow" by starting with lower intensity activities and gradually increasing how often and how long activities are done.
- Protect themselves by using appropriate gear and sports equipment, choosing safe environments, following rules and policies, and making sensible choices about when, where, and how to be active.
- Be under the care of a health care provider if they have chronic conditions or symptoms. People with chronic conditions and symptoms can consult a health care professional or physical activity specialist about the types and amounts of activity appropriate for them.
- Benefits of Exercise:
- Benefit from small amounts of moderate-to-vigorous physical activity throughout the day.
- Physical activity has immediate health benefits. For example, physical activity can reduce anxiety and blood pressure and improve quality of sleep and insulin sensitivity.
- Long-term health benefits:
- For youth, physical activity can help improve cognition, bone health, fitness, and heart health. It can also reduce the risk of depression.
- For adults, physical activity helps prevent 8 types of cancer (bladder, breast, colon, endometrium, esophagus, kidney, stomach, and lung); reduces the risk of dementia (including Alzheimer's disease), all-cause mortality, heart disease, stroke, high blood pressure, type 2 diabetes, and depression; and improves bone health, physical function, and quality of life.
- For older adults, physical activity also lowers the risk of falls and injuries from falls.
- For pregnant women, physical activity reduces the risk of postpartum depression.
- For all groups, physical activity reduces the risk of excessive weight gain and helps people maintain a healthy weight.
- Improved management of health conditions that Americans already have:
- Physical activity can decrease pain for those with osteoarthritis, reduce disease progression for hypertension and type 2 diabetes, reduce symptoms of anxiety and depression, and improve cognition for those with dementia, multiple sclerosis, ADHD, and Parkinson's disease.
References:
METS
Calories = METS x weight (kg) x time (hours)
- For example, to estimate how many calories a 150 lb. (~70 kg) person would burn during 30 minutes of gardening (5 METS), use the calculation below:
- Calories burned = 5 x 68.2 kg x .5 hour = 170.5
See also: Metabolic Equivalents (METS)
Plantar fasciitis
- Stretching the gastrocnemius and soleus muscles, and especially the plantar fascia, reduces pain and disability in plantar fasciitis.
- Strengthening exercises for toe flexors, ankle everters and inverters, and the gastrocnemius improve pain and function more than stretching alone.
- Dry needling of the gastrocnemius, soleus, and plantar muscles improves pain and reduces disability for up to six months.
Reference:
- AFP Vol 111 No 2 Feb 2025
Here is a great resource to learn more about plantar fasciitis and what to do about it: https://www.nhs.uk/conditions/plantar-fasciitis/
I recommend:
- Gentle stretching of the fascia before getting out of bed using a towel to pull the foot back
- Using a cold can (can be any can placed in refrigerator) to roll under the foot several times a day to both ice and stretch the area
- Apply ice for 15 to 20 minutes for 3 times per day
Platelet-rich Plasma (PRP)
Consider using PRP:
- Knee OA (SOR B)
- Rotator cuff tendinopathy (for short term pain relief) (SOR B)
- Patellar tendinopathy (for return to sport) (SOR B)
- Lateral epicondylitis (SOR B)
Additional research is needed:
- Ankle OA (SOR B)
- Hip OA (SOR B)
Do not use:
- Achilled tendinopathy (SOR B)
Reference:
- JFP Vol 72 No 5 Jun 2023
Prolotherapy
Achilles tendinopathy (non-insertional)
- When added to eccentric exercise results in faster and sustained improvement in pain and function
- SOR A
Knee OA
- Improves pain scores and flexion ROM
- SOR A
Low back pain (mechanical)
- No evidence for use in subacute or chronic low back pain
- SOR A
Epicondylosis (lateral)
- Single study shows better than saline for pain and pain control at 1 yr
- SOR B
Osgood-Schlatter disease
- Single study improved overall pain and pain with specific sport activity
- SOR B
Plantar fasciosis
- Small studies show it can improve pain at rest and during activity
- SOR B
Chondromalacia patella/PFPS
- Evidence lacking
- SOR C
References:
- JFP Vol 64 No 12 Dec 2015
Rehab
SI Joint Strengthening Exercises
Hip Extension Exercise
- Begin standing up straight and, if needed, hold on to a wall or table for balance
- Keep your left leg straight and squeeze your buttocks and extend your right leg behind your body
- Hold this position for 2 to 3 seconds
- Slowly return to the starting position
- Alternate sides
- Aim for 10 repetitions of this exercise on each side
Bridge Exercise
- Begin by lying on your back with your knees bent and feet placed flat on the floor with your arms positioned beside your upper body
- Push your heels into the floor, tighten your gluteal and abdominal muscles, and slightly lift your pelvis off of the floor
- Hold this position for 2 to 3 seconds
- Slowly return to the starting position
- Aim for 10 repetitions of this exercise
Bird Dog Exercise
- Begin on your hands and knees on the floor
- Slowly raise your right arm and reach forward until it is inline with your torso, and at the same time extend your left leg backward until it is in line with your torso
- Hold this position for 2 to 3 seconds
- Slowly return to the starting position
- Repeat on the opposite side
- Aim for 10 repetitions of this exercise on each side
Supermans
- Begin lying on your stomach on the floor
- Extend both of your arms straight above your head
- Slowly raise both your arms and legs off the floor
- Hold this position for 2 to 3 seconds
- Slowly return to the starting position
- Aim for 10 repetitions of this exercise
Lunge
- Begin standing with both of your feet together
- Step forward, about 2 feet, with your left foot
- Bend both of your knees to lower yourself toward the ground, ensuring that your back remains straight
- Hold this position for 2 to 3 seconds
- Slowly return to the starting position
- Alternate sides
- Aim for 10 repetitions of this exercise on each side
Avoid these exercises:
- Crunches or sit-ups
- Any exercise or activity that involves a lot of twisting or turning at the hips such as golf or tennis
- Heavy weight lifting, especially those involving the lower back
- Contact sports that could further injure your SI joint such as football or basketball
- Excessive biking or long rides can actually cause more harm than good by putting extra pressure on the sacroiliac joints
Stretching
- Stretching before exercise doe not reduce the risk of injury. (SOR B)
- Stretching may slightly reduce postexercise muscle soreness (SOR B)
Reference:
- AFP Vol 94 No 7 Oct 2016
Prescribing Physical Therapy
Acute (<72hrs)
- Modality: cold application, electrical stimulation, pulsed ultrasound
- Exercse: isometric, gentle active range of motion
- Manual therapy: gentle massage -> Daily for 5d -> Goals:
- Decrease edema
- Decrease pain
- Improve healing
- Increase range of motion
Subacute (3-14 days)
- Modality: heat appication, electrical stimulation, low-level laser therapy, iontrophoresis
- Exercise: isotonic, active range of motion
- Manual therapy: massage, joint mobilization -> 3/wk for 2 weeks -> Goals:
- Improve flexibility
- Improve functional moility
- Increase muscle tone
Chronic (>2 wks)
- Modality: transcutaneous electrical nerve stimulation, continuous ultrasound
- Exercise: strengthening, stabilization
- Manual therapy: myofascial release -> 2/wk for 4 wks -> Goals:
- Functional improvement of activities of daily living
- Restore normal tissue length
References:
- AFP Vol 76 No 11 Dec 2007
At-Home Exercises for common MSK Complaints edit
- Have patients apply ice to an acute injury for 15 to 20 minutes at a time to help control inflammation, and prescribe an anti-inflammatory medication, if indicated. A
- Reserve heat application for use following the acute phase of injury to decrease stiffness. A
- Instruct patients who have an acute lateral ankle sprain to begin "ankle ABCs" and other range-of-motion exercises once acute pain subsides. C
- Consider recommending an eccentric heel stretch to help alleviate plantar fasciitis symptoms. C
General rehabilitation principles
- Once pain is sufficiently controlled, have patients begin basic rehabilitation with simple range-of-motion exercises that move the injured region through normal patterns, as tolerated. Later, the patient can progress through more specific exercises to return the injured region to full functional capacity.
- Explain to patients that it takes about 7 to 10 days of consistent care to decrease inflammation, but that they should begin prescribed exercises once they are able to tolerate them. Plan a follow-up visit in 2 to 3 weeks to check on the patient's response to prescribed care.
Ice
- Ice should be applied for 15 to 20 minutes at a time, once an hour.
Heat
- Heat will help relax and loosen muscles and is a preferred treatment for older injuries, chronic pain, muscle tension, and spasms.
- A heating pad or a warm, wet towel can be applied for up to 20 minutes at a time to help relieve pain and tension
NSAIDs
- A good suggestion is to have the patient take the scheduled NSAID with food for 7 to 10 days or until symptoms subside.
Topical Medications
- Acceptable topical medications include NSAIDs, lidocaine, menthol, and arnica
Lateral ankle sprain
- Phase 1: Immediately following injury, have the patient protect the injured area with rest, ice, compression, and elevation (RICE)
- Exercises to regain range of motion, such as stretching and doing ankle "ABCs," should begin within 48 to 72 hours of the initial injury
- Phase 2: Once the patient has achieved full range of motion and pain is controlled, begin the process of regaining strength.
- Phase 3: Once your patient is able to bear full weight with little to no pain, begin a balance program
- For most lateral ankle sprains, patients can expect time to recovery to range from 2 to 8 weeks.
Plantar fasciitis
- A conservative management program that focuses on reducing pain and inflammation, reducing tissue stress, and restoring strength and flexibility has been shown to be effective for this type of injury.
- Deep-tissue massage and cryotherapy are easy ways to help with pain and inflammation. Deep-tissue massage can be accomplished by rolling the bottom of the foot on a golf or lacrosse ball. A favorite recommendation of ours to reduce inflammation is to use the ice-cup massage, mentioned earlier, for 5 minutes. Or rolling the bottom of the foot on a frozen water bottle will accomplish both tasks at once
- Step 2: Reduce tissue stress. Management tools commonly used to reduce tissue stress are OTC orthotics and night splints. The night splint has been shown to improve symptoms,but patients often stop using it due to discomfort.
- Step 3: Restore muscle strength and flexibility
- an eccentric heel stretch can help to alleviate PF symptoms
- A reasonable timeline for follow-up on newly diagnosed PF is 4 to 6 weeks.
Patellofemoral pain syndrome
- vague anterior knee pain, or pain that worsens with activities such as climbing hills or stairs, or with long sitting or when fatigued
- In general, unbalanced patellar tracking within the trochlear groove likely leads to this pain.
- Specifically, weakness in hip external rotators and abductors is associated with abnormal lower extremity mechanics
- Non-weightbearing standing hip abduction
- Side-lying hip abduction
- Clams
- Forward lunge
- Single-leg squat
- Explain to patients that the recovery process may take several month
Neck pain
- A mainstay in treating mechanical neck pain is alleviating trapezial tightness or spasm.
- A simple self-care tool is using a tennis ball to massage the trapezial muscles. This can be accomplished by having the patient position the tennis ball along the upper trapezial muscles, holding it in place by leaning against a wall, and initiating self-massage.
- Another method of self-massage is to put 2 tennis balls in an athletic tube sock and tie off the end, place the sock on the floor, and lie on it in the supine position.
- There is also evidence that exercise of any kind can help control neck pain
- The easiest exercises one can offer a patient with neck stiffness, or even mild cervical strains, is self-directed stretching through gentle pressure applied in all 4 directions on the neck. This technique can be repeated hourly both at work and at home
MSK conditions in helping patients on the road to recovery. After the acute phase, advise patients to
- apply heat to the affected area before exercising. This can help bring blood flow to the region and promote ease of movement.
- continue icing the area following rehabilitation exercises in order to control exercise-induced inflammation.
- report any changing symptoms such as worsening pain, numbness, or weakness.
References:
- JFP Dec 2020 Vol 69 No 10
Relative Energy Deficiency in Sport (red-s) (Formerly Female Triad)
Low Energy Availability (LEA): The Cause of RED-S
- The underlying etiology of RED-S is LEA, which occurs when dietary intake is inadequate for an athlete's level of physical activity. Energy availability (EA) as noted earlier is defined as energy from dietary intake minus exercise energy expenditure (30, 31).
- Energy availability (EA) = Energy Intake (EI;kcal) − Exercise Energy Expenditure (EEE;kcal/Fat − FreeMass[FFM;kg])
- N.B., 1 kcal=4.184 kJ
Obtaining a valid FFM measure provides the most accurate EA estimation.
- The use of body composition devices such as Dual Energy X-Ray Absorptiometry (DXA) or bioelectrical impedance analysis (BIA) can be utilized to measure FFM for EA calculations as well as to monitor body composition changes over time.
- If available, the DXA provides a more valid measurement, but BIA may be more accessible in many situations.
- However, BIA may underestimate FFM, especially in athletic populations, so greater caution should be taken when using BIA to measure FFM to determine EA estimates
For athletes, EA is a more advantageous concept than energy balance, which is the difference between energy intake and total energy expenditure
- To this end, overall health, activities of daily living, and physiological processes are dependent on the amount of dietary energy remaining after exercise training is accounted for.
- In healthy adults, a value of 45 kcal/kg FFM/day provides sufficient energy
When an athlete has LEA, there is insufficient energy to support the physiological functions necessary to maintain optimal health and performance.
Proposed clinical thresholds for LEA:
- An EA <30 kcal/kg FFM/day for females
- EA <25 kcal/kg FFM/day for males
- It is recommended athletes should keep their EA above 30 kcal/kg FFM/day, even if they trying to lose body weight or body fat.
- Clinical studies have exhibited negative health implications from LEA in as little as five days of <30 kcal/kg FFM/day
Reference:
- Cabre HE, Moore SR, Smith-Ryan AE, Hackney AC. Relative Energy Deficiency in Sport (RED-S): Scientific, Clinical, and Practical Implications for the Female Athlete. Dtsch Z Sportmed. 2022;73(7):225-234. doi: 10.5960/dzsm.2022.546. Epub 2022 Nov 1. PMID: 36479178; PMCID: PMC9724109.
Restless Leg Syndrome
Diagnosis
Essential diagnostic criteria:
- U - Urge to move
- R - Rest induced
- G - Gets better with activity
- E - Evening and night accentuation
Supportive features:
- Family history (1st degree relative)
- Improvement with dopaminergic therapy
- Periodic leg movements during sleep (<50yo)
- Periodic leg movements while awake (all ages)
Associated features:
- Clinical course with progression that varies with age of onset
- Sleep disturbances
- No physical findings in primary/idiopathic RLS
Reference:
- JFP Vol 58 No 8 Aug 2009
Differential Diagnosis
- Akathisia
- Internal desire to move
- Symptoms not worse at night
- Most commonly with neuroleptic medications
- Desire to move is not associated with discomfort
- Nocturnal leg cramps
- Peripheral neuropathy
- Peripheral vascular disease
Reference:
- AFP Vol 78 No 2 Jul 2008
Management of RLS
Treatment algorythm RLS:
- Evaluate medications
- Fe to Fe-def patients
- Ferritin <50mcg/L
- Iron sucrose (FeSO4 325mg tid + Vit C 300mg tid - Venofer)
- Mental alerting acivities
- Abstnence from caffeine, nicotine, and alcohol
- Carbidopa/levodopa or Dopamine agonists
- Low potency opioids
- Benzodiazepines
Daily RLS:
- Dopamine agonists (ropinirole (Requip), pramipexole (Mirapex))
- Gabapentin
- Low potency opioids
Refractory RLS:
- Change to different dopamine agonist
- Change to gabapentin
- Change to high-potency opioid or tramadol
- Consider a second agent
Reference:
- AFP Vol 78 No 2 Jul 2008
- AFP Vol 58 No 8 Aug 2009
Medications that exacerbate RLS
- Antihistimines
- Caffeine
- Dopamine agonists including neuroleptics and antiemetics
- Lithium
- SSRI's
- TCA's
Reference:
- AFP Vol 78 No 2 Jul 2008
Running injuries
- IT Band syndrome
- Patello-femoral Stress Syndrome
- Shin splints
- Achilles tendonitis
- Plantar fasciitis
- Metatarsalgia
- Hammer toes
- Bunions
- Morton's neuroma
Overuse running injury treatment
Recommended:
- Decrease weekly mileage
- Avoid hard surface running
- Shorten running stride
- Ice daily for at least 20min
- Ibuprofen for NSAID therapy
- Daily stretching exercises
Sacroiliac (SI) Joint Pain
Things that can be done for SI joint pain:
- Avoid doing the things that make you hurt
- Modify or avoid activities that worsen your pain to help reduce inflammation in the SI joint
- Stretching exercises (https://healthy.kaiserpermanente.org/health-wellness/health-encyclopedia/he.sacroiliac-pain-exercises.zp4465)
- NSAID medications help with pain
- Physical therapy can be helpful
- Joint injections
Prevention is key to avoiding recurrence:
- Proper lifting techniques
- Good posture during sitting, standing, moving, and sleeping
- Regular exercise with stretching /strengthening
- An ergonomic work area
- Good nutrition, healthy weight, lean body mass
- Stress management and relaxation techniques
- No smoking
You can read more about SI joint pathology here:
Shoulder
See also:
Shoulder dislocation
- Conservative management in patients >30 years and those with uncomplicated injuries (SOR B)
- Discourage strict immobilization - utility is debated and may not change outcomes (SOR B)
- Recommend a progressive rehabilitation program after the acute shoulder injury (SOR B)
- Consider surgical management for patients younger than 30 who have complicated injuries with bone or cartilage loss, rotator cuff tears, or recurrent instability or for the highly physical active individual (SOR B)
References:
- JFP Vol 70 No 2 Mar 2021
Shoulder Impingement PT edit
Physical therapy exercises for shoulder impingement focus on strengthening the rotator cuff and improving shoulder stability and mobility. Here are some recommended exercises:
- Isometric Shoulder Internal and External Rotation:
- Place a rolled-up towel under the arm of the shoulder that is experiencing pain.
- Stand at the corner of a wall with your elbow bent at a 90-degree angle in front of you.
- With a flat hand, push into the wall at 25- to 50-percent pressure.
- Hold the push for 10 seconds, repeating the exercise 10 times. This is the internal rotation.
- Then turn your body so you can press the outside of your hand into the wall. Push into the wall with the outside of your hand at 25- to 50-percent pressure.
- Hold the push for 10 seconds, repeating the exercise 10 times. This is the external rotation.
- Lying External Rotation:
- Use the same rolled-up towel under your arm as in the first exercise. (The towel makes the arm position more efficient and helps prevent overcompensation.)
- Lie on your non-injured side with your head resting on a pillow in a neutral position.
- With your top arm bent at a 90-degree angle in front of you, lift a light weight (Consider starting with a one-pound water bottle) from the surface you're on straight up until it is in line with your shoulder.
- Lower it slowly back down.
- Repeat the lift for three sets of 10 or, if your body can tolerate it, go straight through to 30. Eventually, you can increase the weight up to five pounds.
- Lying Internal Rotation:
- Lie on your side with your affected shoulder underneath your body.
- Keep your elbow bent at 90 degrees and pivot your elbow toward your stomach so your hand points to the ceiling.
- Perform 10 to 15 repetitions.
- Shoulder Scaption Exercise
- In a standing position, hold a water bottle or light weight in one hand by your injured side.
- Slowly lift that arm until it is fully extended at a 45-degree angle away from your body.
- Slowly lower the arm back down to your side.
- Repeat the lift for three sets of 10, pausing between sets if needed to decrease shoulder burn, or go straight through to 30. Gradually, you can increase the weight up to five pounds.
- Wall Angels:
- Stand straight or in a squatting position with your back against the wall.
- Place the back of your hands against the wall and slowly slide your arms up the wall in a V shape, then slide them back down the wall.
- Keep your back and head against the wall the entire time.
- Repeat 5 to 10 times.
These exercises can help alleviate shoulder impingement pain and improve shoulder function.
Sports Physicals
Study: Incidence of Cardiac Arrest During Sports Among Women RARE
Incidence of Cardiac Arrest During Sports Among Women in the European Union
- BACKGROUND
- Women represent a growing proportion of sports participants. Still, few original data regarding sudden cardiac arrest during sports (Sr-SCA) in women are available.
- OBJECTIVES
- The authors sought to assess the incidence, characteristics, and outcomes of women presenting with Sr-SCA.
- METHODS
- Data were analyzed from 3 population-based European registries (ESCAPE-NET 2020 Horizon Program) that prospectively and exhaustively collect every case of SCA: SDEC (Paris-Sudden Death Expertise Center), ARREST (AmsteRdam REsuscitation Studies), and SRCR (Swedish Register for Cardiopulmonary Resuscitation). Sr-SCA was defined as SCA during or #1 hour after cessation of sports activity.
- RESULTS
- Of 34,826 SCA between 2006 and 2017, 760 Sr-SCA (2.2%) were identified, including 54 in women.
- The average annual incidence of Sr-SCA in women in the 3 registries ranged from 0.10 per million (95% CI: 0.01-0.71 per million) to 0.38 per million (95% CI: 0.14-1.04 per million).
- Overall, the average annual incidence rate of Sr-SCA in women was 0.19 per million (95% CI: 0.14-0.24 per million), >10-fold lower compared with men (2.63 per million [95% CI: 2.45-2.83 per million]; P < 0.0001).
- When extrapolating to the total European population and accounting for age and sex, this yields 98 cases per year (95% CI: 72-123 cases per year) in women and 1,350 cases per year (95% CI: 1,256-1,451 cases per year) in men.
- Subject characteristics and circumstances of occurrence were similar in women vs men. Bystander response, time to defibrillation, and survival rate at hospital admission (58.8% vs 58.5%; P ¼ 0.99) and 30 days did not differ significantly between women and men.
- CONCLUSIONS
- These findings emphasize the dramatically lower risk of Sr-SCA in women compared with men, despite similar subject characteristics. This should be considered in designing preparticipation screening strategies in the future.
Reference:
- Weizman O, Empana JP, Blom M, et al. Incidence of Cardiac Arrest During Sports Among Women in the European Union. J Am Coll Cardiol. 2023;81(11):1021-1031. https://doi.org/10.1016/j.jacc.2023.01.015
- https://www.jacc.org/doi/pdf/10.1016/j.jacc.2023.01.015
Study: Diagnosis, treatment and prevention of ankle sprains: Update Of An Evidence-Based Clinical Guideline
This guideline aimed to advance current understandings regarding the diagnosis, prevention and therapeutic interventions for ankle sprains by updating the existing guideline and incorporate new research. A secondary objective was to provide an update related to the cost-effectiveness of diagnostic procedures, therapeutic interventions and prevention strategies. It was posited that subsequent interaction of clinicians with this guideline could help reduce health impairments and patient burden associated with this prevalent musculoskeletal injury.
The previous guideline provided evidence that the severity of ligament damage can be assessed most reliably by delayed physical examination (4–5 days post trauma).
After correct diagnosis, it can be stated that even though a short time of immobilisation may be helpful in relieving pain and swelling, the patient with an acute lateral ankle ligament rupture benefits most from use of tape or a brace in combination with an exercise programme.
New in this update:
- Participation in certain sports is associated with a heightened risk of sustaining a lateral ankle sprain. Care should be taken with non-steroidal anti-inflammatory drugs (NSAIDs) usage after an ankle sprain. They may be used to reduce pain and swelling, but usage is not without complications and NSAIDs may suppress the natural healing process.
- Concerning treatment, supervised exercise-based programmes preferred over passive modalities as it stimulates the recovery of functional joint stability.
- Surgery should be reserved for cases that do not respond to thorough and comprehensive exercise-based treatment.
- For the prevention of recurrent lateral ankle sprains, ankle braces should be considered as an efficacious option.
Reference:
- Vuurberg G, Hoorntje A, Wink LM, van der Doelen BFW, van den Bekerom MP, Dekker R, van Dijk CN, Krips R, Loogman MCM, Ridderikhof ML, Smithuis FF, Stufkens SAS, Verhagen EALM, de Bie RA, Kerkhoffs GMMJ. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. Br J Sports Med. 2018 Aug;52(15):956. doi: 10.1136/bjsports-2017-098106. Epub 2018 Mar 7. PMID: 29514819.
Study: Exercise Is the Only Intervention to Provide Long-Term Improvement in Patients with Chronic Low Back Pain
The interventions that are better than control in achieving at least a 30% reduction in pain are:
- Exercise
- Oral Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- Duloxetine (Cymbalta)
- Opioids
- (but discontinuations of the latter two treatments were common)
Lower-quality data suggest that manipulation and topical capsaicin are also effective. (Level of Evidence = 1a–)
- The authors performed 15 individual systematic reviews focusing on individual interventions for managing patients with chronic (at least three months' duration) low back pain. They searched the Medline, EMBASE, and Cochrane databases, as well as clinical trials registries to identify randomized trials. Two authors independently evaluated potential studies for inclusion and risk of bias. They included 63 trials with more than 16,000 participants. Several interventions resulted in no search results because they lacked a responder analysis: acetaminophen, cannabinoids, muscle relaxants, and antidepressants other than duloxetine. The quality of the included studies was mixed.
- The authors reported meaningful reductions in pain (at least a 30% reduction) as the primary outcome for the included studies.
- They included 18 studies of exercise, most commonly guided by a physiotherapist. After pooling, they estimated that 50% of exercising patients and 35% of control patients achieved meaningful pain relief (number needed to treat [NNT] = 7; 95% CI, 6 to 10). They reported that a significant proportion of patients who were randomized to receive an exercise intervention had sustained relief even after the intervention was completed (NNT = 6; 95% CI, 5 to 9).
- In four trials, oral NSAIDs were more effective than control (NNT = 6; 95% CI, 5 to 8) while patients were taking them.
- Four trials of duloxetine also found it to be more effective than control (NNT = 10; 95% CI, 7 to 18), but discontinuation of treatment due to adverse effects was more common with duloxetine (number needed to harm [NNH] = 11).
- Spinal manipulation (five trials; low-quality evidence) was more effective than control in achieving pain relief (57% vs. 39%; NNT = 6; 95% CI, 4 to 10).
- Three trials (overall lower quality) evaluated topical capsaicin for three weeks. It was effective (NNT = 6; 95% CI, 4 to 10) at the cost of a superficial burning.
- Acupuncture was more effective than control in eight trials (54% vs. 35%; NNT = 6; 95% CI, 5 to 7); however, when only higher-quality studies were included, it was no better than control.
- The authors identified six opioid trials lasting four to 12 weeks, which found that 39% of patients achieved relief compared with 32% of control patients (NNT = 16; 95% CI, 10 to 35), but discontinuation due to side effects was more common with opioids (27% vs. 5%; NNH = 5).
- In 10 trials of corticosteroid injections (overall poor quality), there was no difference in pain relief compared with controls.
- The authors found significant heterogeneity for many of the interventions. One trial each of gabapentin (Neurontin) and topical flurbiprofen (in tape form) found neither to be effective in achieving pain relief. The authors did not address function in their analyses.
Reference:
- Am Fam Physician. 2021 Jun 1;103(11):696-697.
Tendinopathy
Tendinosis:
- Most tendon conditions resulting from overuse
- A degenerative condition induced by chronic overuse
- Recommend eccdntric exercises - Effective and safe
- Use corticosteroids with caution
Tendinitis:
- An acute inflammatory condition (3% of all tendon disorders)
- Acute onset of pain and swelling
Paratenonitis:
- Acute duration
- Caused by injury or overuse
- Inflammation surrounding the tendon
- Swollen and erythematous tendon like de Quervain disease
Tenosynovitis:
- Inflammation of the paratendon and the synovial sheath
- Acute or chronic casued typically from overuse
Treatments:
- First line:
- Relative rest
- activity modification
- cryotherapy
- bracing
- NSAIDs
- Provide pain relief in the short term (7-14 days)
- Use for <2 wks
- Rehab (Eccentric exercises and deep-friction massage)
References:
- JFP Vol 69 No 3 Apr 2020
Trigger Finger
- Recommend splinting as a first-line conservative treatment for trigger finger if there is not a fixed contracture (SOR B)
- Goal is to keep the affected digit in extension
- Recommended length of splinting is 3 - 12 weeks (average of 6 weeks)
- Can compromise with night only splinting
- Massage and physical therapy should be considered as less invasive first line treatments
- Prescribe corticosteroids which may completely resolve the trigger finger in majority of patients without diabetes (SOR A)
- 70% of trigger digits had complete resolution of symptoms at a mean follow-up of 8 years after 1 injection (n=43)
- Refer patients for surgical release if they do not respond to conservative management - surgical success rate is as high as 99%. (SOR A)
Green's Classification System
| Grade | Symptoms |
|---|---|
| I (pre-triggering) | Tenderness and pain at A1 pulley |
| II (active) | Catching with active full extension |
| IIIA (passive) | Catching requiring passive extension |
| IIIB (passive) | Inability to actively flex |
| IV (contracture) | Catching with fixed flexion contracture of PIPJ |
References:
- AFP Vol 107 No 6 Jun 2023
- JFP Vol 70 No 7 Sep 2021
VO2 Max
One easy way to estimate VO2 max at home is using the Heart Rate Ratio Method:
VO2 max=15×(HRmax/HRrest)
- HRmax is your maximum heart rate
- HRrest is your resting heart rate
There are a couple ways to estimate your maximum heart rate:
- Subtract your age from 220
- Some research suggests a more accurate formula is HRmax = 205.8 – (0.685 × age)
Your resting heart rate can be measured by counting your pulse for 60 seconds while at rest. You can also count for 10 seconds and multiply by 6.
Alternatively, if you want to run, you can calculate it with this "Cooper Test":
Run for 12 minutes and measure the distance in miles.
VO2 max = (35.97 x your distance in miles) – 11.29
Reference:
- Uth N, Sørensen H, Overgaard K, Pedersen PK. Estimation of VO2max from the ratio between HRmax and HRrest–the Heart Rate Ratio Method. Eur J Appl Physiol. 2004 Jan;91(1):111-5. doi: 10.1007/s00421-003-0988-y. Epub 2003 Nov 18. Erratum in: Eur J Appl Physiol. 2005 Jan;93(4):508-9. PMID: 14624296.
Walking/Steps Evidence
Study: Walking 7000 steps per day may slash mortality risk by 70%
- Steps per Day and All-Cause Mortality in Middle-aged Adults in the Coronary Artery Risk Development in Young Adults Study
- This prospective cohort study was part of the Coronary Artery Risk Development in Young Adults (CARDIA) study. Participants were aged 38 to 50 years and wore an accelerometer from 2005 to 2006. Participants were followed for a mean (SD) of 10.8 (0.9) years. Data were analyzed in 2020 and 2021.
- In this cohort study of 2110 adults with a mean follow-up of 10.8 years, participants taking at least 7000 steps/d, compared with those taking fewer than 7000 steps/d, had a 50% to 70% lower risk of mortality.
- There was no association of step intensity with mortality regardless of adjustment for step volume.
Reference:
- Paluch AE, Gabriel KP, Fulton JE, et al. Steps per Day and All-Cause Mortality in Middle-aged Adults in the Coronary Artery Risk Development in Young Adults Study. JAMA Netw Open. 2021;4(9):e2124516. https://doi.org/10.1001/jamanetworkopen.2021.24516
Muscle Spasms edit
For muscle spasms:
- Use a heating pad as often as you can
- Take NSAIDs like ibuprofen regularly (400 mg every 4 hours or 800 mg every 8 hours)
- You can use a muscle relaxer (like cyclobenzaprine 10 mg) up to twice a day, but since they can make you sleepy, I recommend using at night
- Stretch often and Continue to be active - don't avoid movement because it hurts
Things will usually improve through the day, but then worsen again overnight as you lay still
Patient Messaging: Physical Therapy Library edit
Stretches:
- Pigeon Pose:
- Start on all fours.
- Bring your right knee forward behind your right wrist, angling your leg out to the side.
- Extend your left leg straight back, keeping it flat.
- Square your hips towards the front of your mat and gently lower your torso towards the floor.
- Hold for 30-60 seconds, then switch sides.
- Butterfly Stretch:
- Sit on the floor with the soles of your feet together.
- Gently press down on your knees with your hands to bring them closer to the floor.
- Keep your back straight and relax your shoulders.
- Hold for 30-60 seconds.
- Figure-Four Stretch:
- Lie on your back with knees bent and feet flat.
- Cross your right ankle over your left thigh, just above the knee.
- Gently pull your left thigh towards your chest until you feel a stretch in your right hip.
- Hold for 30-60 seconds, then switch sides.
- Hip Flexor Stretch:
- Kneel on one knee with the other foot flat on the floor in front of you.
- Push your hips forward and feel the stretch in the front of your hip.
- Hold for 30-60 seconds, then switch sides.
- Hamstring Stretch:
- Stand with feet hip-width apart.
- Extend one leg straight out in front of you, keeping your toes pointed upwards.
- Bend forward at the waist, reaching towards your toes.
- Hold for 30-60 seconds, then switch sides.
- Single knee-to-chest stretch
- Lie on your back with your knees bent and your feet flat on the floor. You can put a small pillow under your head and neck if it is more comfortable.
- Clasp your hands under one knee and bring the knee to your chest. Keep your other foot flat on the floor.
- Keep your lower back pressed to the floor. Hold the stretch for at least 15 to 30 seconds.
- Relax and lower the knee to the starting position.
- Repeat 2 to 4 times with each leg.
- Double knee-to-chest stretch
- Lie on your back with your knees bent and your feet flat on the floor. You can put a small pillow under your head and neck if it is more comfortable.
- Bring your knees to your chest and hold them with your hands. Or you can hold at the fronts of your shins or behind your thighs.
- Keep your lower back pressed to the floor. Hold the stretch for 15 to 30 seconds.
- Relax, and lower your knees to the starting position.
- Repeat 2 to 4 times.
Exercises:
- Clamshells:
- Lie on your side with knees bent and feet together.
- Keeping your feet together, raise your top knee as high as you can without moving your hips.
- Slowly lower your knee back down. Repeat for 10-15 reps.
- Bridges:
- Lie on your back with knees bent and feet flat on the floor.
- Lift your hips off the ground until your body forms a straight line from shoulders to knees.
- Squeeze your glutes at the top of the movement, then slowly lower back down. Repeat for 10-15 reps.
- Side-Lying Hip Abduction:
- Lie on your side with legs extended and hips aligned.
- Keeping your feet together, lift your top leg as high as you can without arching your back.
- Slowly lower your leg back down. Repeat for 10-15 reps.
- Squats:
- Stand with feet shoulder-width apart and toes slightly pointed out.
- Lower your hips as if sitting in a chair, keeping your back straight and core engaged.
- Push through your heels to stand back up. Repeat for 10-15 reps. (Modifications: Use a chair or wall for support)
- Lunges:
- Step forward with one leg, lowering your hips until both knees are bent at a 90-degree angle.
- Keep your front knee aligned with your ankle and your back straight.
- Push off with your front foot to return to standing position. Repeat for 10-15 reps per leg.
- Alternate arm and leg (bird dog)
- Start on the floor, on your hands and knees.
- Tighten your belly muscles by pulling your belly button in toward your spine. Be sure you continue to breathe normally and do not hold your breath.
- Keeping your back and neck straight, raise one arm off the floor and hold it straight out in front of you. Be careful not to let your shoulder drop down, because that will twist your trunk.
- Hold for about 6 seconds, then lower your arm and switch to your other arm. Over time, work up to holding for 10 to 30 seconds each time.
- Repeat 8 to 12 times with each arm.
- Notes:
- When you feel steady and strong doing this exercise with your arms, try doing the exercise with your legs instead. Raise one leg and hold it straight out behind you. Be careful not to let your hip drop down, because that will twist your trunk.
- When holding your leg straight out becomes easier, try raising your opposite arm at the same time.
- Bridging (feet flat)
- Lie on your back with both knees bent and your feet flat on the floor. Your knees should be bent about 90 degrees.
- Tighten your belly muscles by pulling your belly button in toward your spine. Keep breathing normally and don't hold your breath.
- Push your feet into the floor, squeeze your buttocks, and lift your hips off the floor until your shoulders, hips, and knees are all in a straight line. Keep your hips level.
- Hold for about 6 seconds.
- Slowly lower your hips back to the floor.
- Repeat 8 to 12 times.
- Curl-up (arms crossed)
- Lie on your back on the floor, with your knees bent and your feet flat on the floor. (Or you can lie on any flat surface, such as a bed.)
- Cross your arms over your chest. If this bothers your neck, try putting your hands behind your neck (not your head), with your elbows spread apart.
- Slowly tighten your belly muscles and raise your head and shoulder blades off the floor. Keep breathing normally and don't hold your breath.
- Keep your neck straight and do not press your chin to your chest.
- Hold for 1 to 2 seconds. Then slowly lower yourself back to the floor.
- Repeat 8 to 12 times.
- Front plank (beginner)
- Lie on your stomach, supporting your body with your forearms. Keep your elbows under your shoulders.
- Press down on your forearms and lift your hips off the floor so that you are supporting your body on your elbows and knees.
- Keep your body straight by tightening your belly and buttocks muscles.
- Hold for about 6 seconds. Over time, build up to about 30 seconds.
- Rest for up to 10 seconds.
- Repeat 3 to 5 times.
- Front plank (intermediate)
- Get into the front plank position, resting on your elbows and toes, with your body straight.
- Keep your body straight by tightening your belly and buttocks muscles. Keep breathing normally and don't hold your breath.
- Hold for about 6 seconds, and then rest. Over time, build up to about 30 seconds.
- Repeat 3 to 5 times.
Notes:
- Start slowly and gradually increase intensity. Listen to your body and stop if you experience pain.
- Focus on proper form.
- Be consistent
Nephrology
Acid/Base
Step 1: Determine the primary process
pH PaCO2 HCO3 Primary process ↓ ↓ ↓ Metabolic acidosis ↑ ↑ ↑ Metabolic alkalosis ↓ ↑ ↑ Respiratory acidosis ↑ ↓ ↓ Respiratory alkalosis Step 2: Determine compensation
Table 163: Compensation Rules: Primary acid-base disorder Expected compensation Metabolic acidosis PaCO2 = HCO3 + 15 Metabolic alkalosis PaCO2 = 40 + [0.7 * (HCO3 - 24)] Respiratory acidosis (acute) HCO3 = 24 + [1 * (PaCO2 - 40)/10] Respiratory acidosis (chronic) HCO3 = 24 + [3.5 * (PaCO2 - 40)/10] Respiratory alkalosis (acute) HCO3 = 24 - [2*40-PaCO2)/10] Respiratory alkalosis (chronic) HCO3 = 24 - [5*40-PaCO2)/10]
Reference:
- AFP Vol 111 No 2 Feb 2025
Acute Kidney Injury
Staging of AKI
| Stage | Serum creatinine level | Urine output |
|---|---|---|
| 1 | 1.5–1.9 times baseline or ≥ 0.3 mg/dL (≥ 26.5 μmol/L) increase | < 0.5 mL/kg/h for 6–12 hours |
| 2 | 2.0–2.9 times baseline | < 0.5 mL/kg/h for ≥ 12 hours |
| 33.0 times baseline or Increase in serum creatinine to ≥ 4.0 mg/dL (≥ 353.6 μmol/L) or Initiation of renal replacement therapy or, in patients < 18 years, decrease in eGFR to < 35 mL/min per 1.73 m2 | < 0.3 mL/kg/h for ≥ 24 hours or Anuria for ≥ 12 hours |
Causes:
- Prerenal
- Increased intra-abdominal pressure
- Abdominal compartment syndrome
- Intravascular volume depletion
- Hemorrhage, gastrointestinal losses, renal losses, skin and mucous membrane losses, nephrotic syndrome, cirrhosis, capillary leak
- Peripheral vasodilation
- Sepsis, cirrhosis, anaphylaxis, pharmacologic adverse effects
- Reduced cardiac output
- Cardiogenic shock, pericardial diseases, congestive heart failure, valvular diseases, pulmonary diseases, sepsis
- Renal vasoconstriction
- Early sepsis, hepatorenal syndrome, acute hypercalcemia, pharmacologic adverse effects, iodinated contrast media
- Increased intra-abdominal pressure
- Intrinsic renal
- Glomerular injury
- Pharmacologic adverse effects
- Hematologic disorders: hemolytic uremic syndrome, thrombotic thrombocytopenic purpura
- Inflammation: anti–glomerular basement membrane disease, antineutrophil cytoplasmic antibody disease, infection, cryoglobulinemia, membranoproliferative glomerulonephritis, immunoglobulin A nephropathy, systemic lupus erythematosus, Henoch-Schönlein purpura, polyarteritis nodosa
- Renal microvasculature
- Malignant hypertension, toxemia of pregnancy, hypercalcemia, radiocontrast media, scleroderma, pharmacologic adverse effects
- Tubular injury
- Endogenous toxins: myoglobin, hemoglobin, paraproteinemia, uric acid
- Exogenous toxins: antibiotics, chemotherapy agents, radiocontrast media, phosphate preparations
- Ischemia due to hypoperfusion
- Tubulointerstitial injury
- Acute allergic interstitial nephritis
- Infections: Legionella, Leptospira, Rickettsia, Hantavirus, Candida, Plasmodium, tuberculosis
- Infiltration
- Vascular causes (e.g., large vessel diseases, such as renal artery thrombosis; embolism; stenosis; and operative renal arterial clamping)
- Arterial thrombosis, vasculitis, dissection, thromboembolism, venous thrombosis, compression, trauma
- Glomerular injury
- Postrenal
- Lower urinary tract causes
- Bladder: neck obstruction, calculi, carcinoma, infection (schistosomiasis)
- Functional: neurogenic bladder, diabetes, multiple sclerosis, stroke, pharmacologic adverse effects (anticholinergics, antidepressants)
- Prostate: benign prostatic hypertrophy, carcinoma, infection
- Urethral: posterior urethral valves, strictures, trauma, infections, tuberculosis, tumors
- Upper urinary tract extrinsic causes
- Retroperitoneal space tumors, pelvic or intra-abdominal tumors, retroperitoneal fibrosis, ureteral ligation or surgical trauma, granulomatous disease, hematoma
- Upper urinary tract intrinsic causes
- Nephrolithiasis, strictures, edema, debris, blood clots, sloughed papillae, fungal ball, malignancy
- Lower urinary tract causes
References:
- AFP Vol 100 No 11 Dec 2019
Chronic Kidney Disease
Initial workup
- Albumin/creatinine ratio
- A1c
- Lipid panel
- Renal US
- Serum electrolytes
- UA/urine microscopy
If CKD defined as eGFR < 60 or urine albumin:Cr >30 mg/g (mg/mmol) for > 3 mo
- Start ACEI or ARB if HTN or urine albumin:Cr >30
- Start SGLT2-inhib if eGFR >20, urine albumin:Cr >200 mg/g (20 mg/mmol), or HF
- Start a statin if pt >50 yo or 18-49 with any of the following:
- Diabetes
- CVD
- Prior ischemic stroke
- 10-yr CV score > 10%
- If Type 2 DM:
- Start GLP-1 agonist if A1c above goal
- Start nonsteroidal mineralcorticoid receptor antagonist (finerenone) if urine albumin:Cr >30 and eGFR >25
Reference:
- AFP Dec 2023 Vol 108 No 6
- AFP Mar 2025 Vol 111 No 3
eGFR
eGFR = estimated GFR
- The conventional measure of precision has been the P30, which describes the percent of GFR estimates that are within 30% of the measured GFR. For even the most accurate estimating equations, only about 90% of GFR estimates are within 30% of the measured GFR of the study population (P30), with varying accuracy across populations.
- For example, if an estimating equation has a P30 value of 90% in a population, then for an individual within that population with measured GFR of 55 ml/min/1.73m2, there is an approximately 90% chance that the person’s eGFR will fall between 38.5 and 71.5 ml/min/1.73m2 of the mGFR.
- The average BSA today is near 1.83, ~ 1.91 in men and 1.71 in women. Thus, for any printout showing eGFR in an American male, one can assume that the true eGFR is almost 10% higher. And for a smaller woman, the reported eGFR could be 5% lower than the true GFR.
| A1 | A2 | A3 | ||
|---|---|---|---|---|
| <30 mg/g | 30-300 mg/g | >300 mg/g | ||
| G3a | 45-59 | 1 | 2 | 3 |
| G3b | 30-44 | 2 | 3 | 3 |
| G4 | 15-29 | 3 | 3 | 4+ |
| G5 | <15 | 4+ | 4+ | 4+ |
| Age | Avg GFR |
|---|---|
| 20-29 | 116 mL/min/1.73 m2 |
| 30-39 | 107 mL/min/1.73 m2 |
| 40-49 | 99 mL/min/1.73 m2 |
| 50-59 | 93 mL/min/1.73 m2 |
| 60-69 | 85 mL/min/1.73 m2 |
| 70+ | 75 mL/min/1.73 m2 |
Suggestions and recommendations:
- The eGFR should never be reported to decimal precision.
- Involved clinicians should be periodically reminded that the “e” in eGFR stands for estimated.
- Leaders in Clinical Chemistry should strongly consider to modernize the index BSA to 1.83 m2.
- eGFR must never be reported for patients on dialysis.
- eGFR should not be reported for patients in acute renal failure.
Reference:
- AFP Dec 2023 Vol 108 No 6
- AFP Mar 2025 Vol 111 No 3
- Factors Affecting eGFR Accuracy - NIDDK
CKD Anemia
For those with:
- Creatinine >2mg/dL
- Male and post-menopausal females with Hb <12g/dL
- Premenopausal females with Hb <11g/dL
Order:
- CBC
- Ferritin
- TIBC/TSAT
- Reticulocyte
- B12
- Folate
- Stool guaiac
- Serum Fe
If Fe deficient:
- R/o occult GI malignancy; if none -> start Fe therapy
- Start ESA (erythropoietin-stimulating agents) if Hb <10g/dL
- Monitor Fe stores periodically
If B12/folate deficient:
- Supplement
If unclear/malignancy
- Refer to hematology
References:
- JFP Vol 59 No 1 Jan 2010
CKD Interventions
Dietary recommendations:
- Limit sodium to <2,300 mg/day
- Limit protein intake to 0.6 - 0.8 g/Kg/day (For stages 3b-5)
Blood Pressure:
- ACE or Arb
Diabetes:
- Metformin reduces mortality - continue until GFR <30
- SGLT-2 and GLP-1 improve outcomes
Anemia
- Stage: All
- Assess:
- CBC
- Reticulocyte
- Fe, Ferritin, Transferrin
- Frequency: Annual
Malnutrition
- Stage: 3a-5
- Assess:
- Weight
- Albumin
- Dietary history
- Frequency:
- q6-12mo while stage 3a/b
- q1-3mo while stage 4 or 5
- Consider nutrition referral at stage 4
Mineral and bone disorder
- Stage: 3a-5
- Assess:
- Alk Phos
- Once in stage 3a/b
- q12mo in stage 4 or 5
- Ca++ and Phosphorus
- q3-6 for stage 3a/b and 4
- q1-3mo for stage 5
- DEXA - No specific recommendations
- 25-hydroxyvitamin D
- Once, then as indicated in stage 3a/b; q3-6mo in stage 4; q1-3mo in stage 5
- Parathyroid
- Alk Phos
- Frequency:
- Once, then as indicated in stage 3a/b; q3-6mo in stage 4; q1-3mo in stage 5
Neuropathy
- Stage: 3a-5
- Assess:
- Paresthesia
- Mental status
- Sleep distrubances
- Consider Sleep Study and Nerve Conduction Study
- Frequency:
- As indicated
Reduced level of functioning and well-being
- Stage: 3a-5
- Assess:
- Health literacy assessment
- Social support
- Standardized self-administered instruments
- Frequency:
- Once, then as indicated
References:
- AFP Vol 96 No 12 Dec 2017
- AFP Vol 102 No 6 Sep 2020
CKD Stages
NKF KOQI guideline recommends using MDRD Study calculator for adults.
| CKD | GFR | Description | Action Plan |
|---|---|---|---|
| 1 | 90+ | Kidney damage with normal GFR | Diagnose and treat CKD and comorbid conditions; slow progression; reduce CV risk |
| 2 | 60-89 | Kidney damage with mild GFR | Estimate progression |
| 3a | 45-59 | Mild - Mod GFR | Evaluate and treat complications |
| 3b | 30-44 | Moderate GFR | Evaluate and treat complications |
| 4 | 15-29 | Severe GFR | Prepare for renal replacement therapy |
| 5 | <15 | Kidney failure | Renal replacement therapy if uremia present |
References:
- AFP Vol 96 No 12 Dec 2017
- NKF KIDOQI clinical practice guideline
Indications for considering Nephrology Referral
Diagnosis of CKD cause
- Acute kidney injury (unresponsive to initial management)
- Anemia of CKD
- Family history of kidney disease
- Presence of red blood cell casts in the urine
- Progression of CKD
Management of CKD complications
- Anemia of chronic kidney disease when hemoglobin < 10 g per dL (100 g per L)
- CKD and refractory hypertension
- Mineral and bone disorder of CKD
- Persistent abnormalities in serum
- Persistent elevated albuminuria (albumin/creatinine ratio > 300 mg per g [> 30 mg per mmol]) or refractory proteinuria (urinary protein/creatinine ratio > 500 to 1,000 mg per g [> 50 to 100 mg per mmol])
- Recurrent nephrolithiasis or concern for nephrocalcinosis
Preparation for renal replacement therapy
- GFR < 30 mL per minute per 1.73 m2 (KDIGO GFR categories G4 and G5)
References:
- AFP Vol 96 No 12 Dec 2017
CKD-EPI Calculator for Adults (SI Units)
Better kidney function calculator: https://www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-management/kidney-disease/laboratory-evaluation/glomerular-filtration-rate-calculators/ckd-epi-adults-si-units
This CKD-EPI equation calculator should be used when Scr is reported in µmol/L. This equation is recommended when eGFR values above 60 mL/min/1.73 m² are desired.
GFR = 141 × min(Scr/κ, 1)α × max(Scr/κ, 1)-1.209 × 0.993Age × 1.018 [if female] × 1.159 [if African American]
- where:
- Scr is serum creatinine in µmol/L,
- κ is 61.9 for females and 79.6 for males,
- α is -0.329 for females and -0.411 for males,
- min indicates the minimum of Scr/κ or 1, and
- max indicates the maximum of Scr/κ or 1
Microscopic hematuria
Notes:
- Repeat microscopic urinalysis
- Further evaluation is recommended for individuals with 3+ red blood cells per high-power field in a properly collected urine specimen in the absence of infection.
- Computed tomography urography is the preferred method for radiologic imaging in the evaluation of microscopic hematuria.
Reference:
- Am Fam Physician. 2013;88(11):747-754
Nephrolithiases
Risk Factor for Recurrent Symptomatic Stones:
- Male
- Younger age
- Obesity
- Pregnancy
- FH of kidney stones
Acute Management:
- Fluids
- At least 2L/24hrs
- 0.9% NS if BP low
- 5% dextrose in water and 0.45% NS if calciuria
- Antispasmotics
- Alpha blockers
- Tamsulosin 0.4mg qd 2-4 weeks
- Improves clearance of stones >5mm
- Shortens expulsion times
- Reduces hospitalization
- Doxazosin 4mg qd
- Tamsulosin 0.4mg qd 2-4 weeks
- Calcium channel blocker
- Nifedipine 30mg qd
- Alpha blockers
- Pain Management
- NSAIDS for mild to moderate pain
- Opiates q4-6 prn for severe pain
- Surgery
- For stones >10 mm or those with uncontrolled pain/nausea, only 1 functioning kidney, or haven't passed stones after 4-6 weeks
Prevention of recurrent stones:
- Increase fluid intake
- Eat a low sodium, normal calcium, moderate protein diet
- May benefit from thiazide diuretic medication and potassium citrate
References:
- AFP Vol 84 No 11 Dec 2011
- AFP Vol 102, No 11 Dec 2020
- JAMA Sep 2022 Vol 328 No 9
Renal Tubular Acidosis
Evaluate when normal anion gap (hyperchloremic) metabolic acidosis
- Plasma HCO3 Levels:
- Type 1: Less than 10 to 20 mEq/L
- Type 2: 12 to 18 mEq/L
- Type 4: Greater than 17 mEq/L
- Plasma Potassium:
- Low in type 1 and type 2
- High in type 4, type 1 (due to decreased reabsorption of Na in distal tubule) [14]
- BUN/Cr:
- Normal or near normal (rules out renal failure as the cause of acidosis)
- Urinalysis:
- Urine pH
- inappropriately alkaline (greater than 5.5) despite metabolic acidosis in type 1, also in type 2 if HCO3 above reabsorptive threshold (12 to 18 mEq/L)
- acidic (less than 5.5) in type 2 and 4
- Urine pH
- Urine culture:
- Rule out urinary tract infection with the urea-splitting organism as it may elevate urine pH
- Urine anion gap ([Na + K] - Cl):
- Positive gap signifies low NH4Cl excretion which causes decrease chloride in urine along with hyperchloremic metabolic acidosis suggesting RTA
Subtypes are as follows:
- Type 1: Distal RTA
- Etiologies:
- Autoimmune diseases are the commonest cause in adults: Systemic lupus erythematosus (SLE), Sjogren syndrome, rheumatoid arthritis, systemic sclerosis, thyroiditis, hepatitis, primary biliary cirrhosis [2].
- Inherited, AD or AR: Genetic primary causes of distal RTA include mutations of genes that encode the chloride-bicarbonate exchanger (AE1) or subunits of the H-ATPase pump respectively
- Genetic associations: Marfan syndrome, Ehler Danlos syndrome, sickle cell disease, congenital obstruction of the urinary tract
- Nephrocalcinosis: Chronic hypercalcemia, medullary sponge kidney
- Tubulointerstitial diseases: chronic pyelonephritis, chronic interstitial nephritis, obstructive uropathy, renal transplant rejection
- Hypergammaglobulinemic states: Monoclonal gammopathy, multiple myeloma, amyloidosis, cryoglobulinemia, chronic liver disease
- Drugs: Lithium, amphotericin B, NSAIDs, lead, antivirals
- Miscellaneous: Idiopathic, familial hypercalciuria, glue sniffing (toluene inhalation in recreational drug abuse) [3]
- Etiologies:
- Type 2: Proximal RTA
- Etiologies:
- Hypergammaglobulinemic states: Most common cause in adults-monoclonal gammopathy(light chain), multiple myeloma, amyloidosis
- Inherited: AD or AR putative mutations in Na-H antiporter in apical membrane and Na-HCO3 cotransporter in the basolateral membrane of proximal tubular cells respectively
- Drugs: Lead or other heavy metals, carbonic anhydrase inhibitors (e.g., acetazolamide, topiramate) [4], out of date tetracyclines, aminoglycosides, valproate, mercury, tenofovir, and ifosfamide (nephrotoxic)
- Autoimmune: Sjogren syndrome, systemic lupus erythematosus (SLE)
- Miscellaneous: Interstitial nephritis, Fanconi syndrome, vitamin D deficiency, secondary hyperparathyroidism, chronic hepatitis, idiopathic
- Etiologies:
- Type 3: Mixed RTA
- Etiologies:
- Inherited: Mutations in carbonic anhydrase II (mostly affecting children from Arabic, North African, and Middle Eastern descent)
- Etiologies:
- Type 4:Hyporeninemic hypoaldosteronism RTA (Most Common in USA)
- Etiologies:
- Hyporeninemic hypoaldosteronism: most common cause in adults is diabetic nephropathy - destruction of JG apparatus due to vascular hyalinosis [5]
- Drugs: Potassium-sparing diuretics, beta blockers, NSAIDs, calcineurin inhibitors (cyclosporine, tacrolimus), ACEi, ARBs, renin inhibitors, heparin, TMP/SMX
- Autoimmune: SLE
- Genetic: Sickle cell disease, pseudohypoaldosteronism
- Miscellaneous: Interstitial nephritis, chronic obstruction of the urinary tract, adrenal insensitivity to angiotensin II, renal insufficiency
- Etiologies:
Reference:
Uremia (and complaints of a urea smell)
Most Likely Diagnoses:
- Uremia: Uremia, a condition associated with advanced chronic kidney disease (CKD), can cause a characteristic uremic odor due to the accumulation of urea and other waste products in the body. This is often seen in patients with CKD stages 3-4.
- Chronic Kidney Disease (CKD): CKD can lead to the accumulation of urea and other nitrogenous wastes in the body, which can manifest as a uremic odor. This is particularly relevant in advanced stages of CKD.
- Urinary Tract Infection (UTI): UTIs can sometimes cause changes in the odor of urine, which may be perceived as a uremic smell. This is more common in recurrent or severe infections.
- Dehydration: Severe dehydration can lead to the concentration of urea in the body, potentially causing a uremic odor. This is particularly relevant in children and the elderly.
- Diabetes Mellitus: Poorly controlled diabetes can lead to diabetic ketoacidosis (DKA), which can cause a fruity or acetone-like odor, sometimes confused with a uremic smell.
Most Important Not to Miss Diagnoses:
- Liver Failure: Liver failure can lead to the accumulation of various toxins, including ammonia, which can cause a characteristic odor. Assessment of liver function tests is crucial.
- Sepsis: Sepsis can cause metabolic derangements and organ dysfunction, including renal impairment, which can lead to a uremic odor. Early identification and treatment are critical.
- Metabolic Acidosis: Metabolic acidosis, particularly in the context of renal failure, can lead to the accumulation of urea and other waste products, causing a uremic odor. Evaluation of acid-base status and serum electrolytes is essential.
Key pieces of additional history and/or follow-up tests needed:
- Renal Function Tests: Serum creatinine, blood urea nitrogen (BUN), and glomerular filtration rate (GFR) to assess kidney function.
- Urinalysis: To check for signs of infection or other abnormalities.
- Liver Function Tests: Including serum bilirubin, aspartate aminotransferase (AST), alanine transaminase (ALT), and albumin.
- Blood Glucose and Ketone Levels: To rule out diabetic ketoacidosis.
- Complete Blood Count (CBC) and Blood Cultures: To evaluate for signs of infection or sepsis.
- Electrolyte Panel and Arterial Blood Gas (ABG): To assess for metabolic acidosis.
The treatment options for uremia, particularly in the context of advanced chronic kidney disease (CKD), include both kidney replacement therapies (KRT) and conservative management strategies.
Kidney Replacement Therapy (KRT):
- Hemodialysis: This can be performed either in-center or at home. It involves the extracorporeal removal of waste products and excess fluid from the blood.
- Peritoneal Dialysis: This is a home-based therapy where the peritoneal membrane acts as a filter to clear waste products from the blood.
- Kidney Transplant: This is the definitive treatment for end-stage kidney disease (ESKD) and involves the surgical placement of a healthy kidney from a donor.
Conservative Management:
- Dietary Modifications: A low-protein diet can help reduce the production of uremic toxins. Plant-based diets and very low-protein diets are recommended to decrease the generation of uremic toxins.
- Medications: AST-120, an oral adsorbent, has been shown to reduce circulating levels of certain uremic toxins like indoxyl sulfate and p-cresol sulfate.
- Probiotics and Prebiotics: These can modulate the gut microbiota to reduce the production of uremic toxins.
- Symptom Management: Addressing symptoms such as pruritus, nausea, and poor appetite through pharmacological and non-pharmacological means is crucial. The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines recommend a multidisciplinary approach to manage these symptoms.
Emerging Therapies:
- Intestinal Dialysis: Techniques such as colonic perfusion and the use of oral sorbents to enhance bowel elimination of uremic toxins are being explored.
- Activated Charcoal: This can be used to manage uremic pruritus and reduce uremic toxin levels.
In summary, the treatment of uremia in advanced CKD involves a combination of KRT and conservative management strategies, tailored to the patient's clinical status and preferences. The KDIGO guidelines emphasize the importance of patient-centered care and symptom management.
Urine Specific Gravity
Urine specific gravity is a laboratory test that measures the concentration of solutes in urine compared to water. It helps assess kidney function and hydration status.
The test compares the density of urine to the density of water, with a specific gravity of 1.000 representing pure water. Urine specific gravity typically ranges from 1.003 to 1.030, with values outside this range indicating potential health issues.
- High urine specific gravity suggests that the urine is too concentrated
- Low urine specific gravity indicates that the urine is too diluted
Increased urine specific gravity may be due to conditions such as:
- Adrenal glands do not produce enough hormones (such as Addison disease)
- Glucose in the urine
- Heart failure
- High sodium level in the blood
- Loss of body fluids (dehydration)
- Narrowing of the kidney artery (renal artery stenosis)
- Shock
- Syndrome of inappropriate ADH secretion (SIADH)
Decreased urine specific gravity may be due to:
- Damage to kidney tubule cells (renal tubular necrosis)
- Diabetes insipidus
- Drinking too much fluid
- Kidney failure
- Low sodium level in the blood
- Severe kidney infection (pyelonephritis)
Neurology
Altitude Sickness edit
Prophylaxis:
- acetazolamide 250 mg bid starting 24-48 hours early
Bell's Palsy edit
Presentation:
- Bell palsy presents as mouth droop, flattening of the nasolabial fold, inability to close the eye, and smoothing of the brow on one side of the face
- Symptoms of Bell palsy are rarely bilateral
- Symptoms typically develop acutely (over 1-3 days), peak within the first week, and gradually resolve over weeks to months
- Additional evaluation should be considered in patients with ipsilateral recurrent Bell palsy because this could suggest an underlying tumor
Physical examination maneuvers to demonstrate the degree and extent of facial weakness include:
- Raise their eyebrows
- Smile
Interpretation:
- If they cannot raise their eyebrows and cannot move the lower portion of their face they have Bell's palsy and should be given steroids +/- antivirals
- If the lower portion of the face is paralyzed but the eyebrows rise symmetrically, then you have to be concerned for a stroke and should get imaging and further consideration of treatment (depending on time of presentation and cause)
House-Brackmann scale (severity):
- Grade I, normal severity: normal facial function in all areas.
- Grade II, slight severity: slight weakness on close inspection, slight synkinesis, complete eyelid closure with minimal effort.
- Grade III, moderate severity: Obvious but not disfiguring facial asymmetry, synkinesis is noticeable but not severe, may have hemifacial spasm or contracture, complete eyelid closure with effort, mouth is slightly weak with maximal effort.
- Grade IV, moderately severe: Disfiguring facial asymmetry or obvious facial weakness, forehead cannot move, incomplete eyelid closure, mouth is asymmetrical with maximal effort.
- Grade V, total paralysis: no facial movement.
Treatment:
- Patients with Bell palsy should be treated with oral corticosteroids, which have been shown to improve rates of full recovery (NNT = 10)
- Prednisone 50 to 60 mg per day for 5 days with 5-day taper
- Combination therapy (steroid and antiviral) consistently leads to lower rates of synkinesis (NNT = 12)
- Valacyclovir, 1 g 3 times per day for 7 days
- Acyclovir, 400 mg 5 times per day for 10 days
- Patients with Bell palsy should not be treated with antivirals alone.
- Patients with Bell palsy who are not able to close an eye should be educated about eye protection measures (e.g., administration of liquid tears or lubricating gel, eyelid taping at night)
- Signs or symptoms of keratitis warrant referral to an eye specialist
Alternative diagnoses should be considered in those with (because they indicate an upper motor neuron lesion or a lesion involving more than just cranial nerve VII):
- bilateral involvement
- sparing of the forehead
- abnormal extraocular movements
- hearing loss
- tinnitus
- vertigo
Alternative diagnoses should be considered in patients with:
- gradual onset of symptoms
- prolonged course (more than three months without improvement)
- limb or bulbar weakness
- systemic or localized facial skin cancer
- signs of infection
- risk of infection
Reference:
- Dalrymple SN, Row JH, Gazewood J. Bell Palsy: Rapid Evidence Review. Am Fam Physician. 2023;107(4):415-420.
- https://www.ebmconsult.com/articles/anatomy-stroke-vs-bells-palsy
Bells Palsy
Bell's Palsy:
- Sudden onset (usually over hours) of unilateral facial paralysis. Common findings include the eyebrow sagging, inability to close the eye, disappearance of the nasolabial fold, and drooping at the affected corner of the mouth, which is drawn to the unaffected side
Exam:
- Facial movement is assessed by observing the response to command for closing the eyes, elevating the brow, frowning, showing the teeth, puckering the lips, and tensing the soft tissues of the neck to observe for platysma activation. The evaluation also includes a general physical examination and neurologic examination. Particular attention is directed at the external ear to look for vesicles or scabbing (which indicates zoster) and for mass lesions within the parotid gland.
Diagnosis:
- There is a diffuse facial nerve involvement manifested by paralysis of the facial muscles, with or without loss of taste on the anterior two-thirds of the tongue or altered secretion of the lacrimal and salivary glands. (See 'Peripheral versus central lesions' below.)
- Onset is acute, over a day or two; the course is progressive, reaching maximal clinical weakness/paralysis within three weeks or less from the first day of visible weakness; and recovery or some degree of function is present within six months.
- An associated prodrome, ear pain, or dysacusis is variable.
Differential Diagnosis of Facial nerve palsy:
- Bell's palsy
- herpes zoster infection
- Guillain-Barré syndrome (GBS)
- otitis media
- Lyme disease (neuroborreliosis)
- HIV infection
A "peripheral" pattern of facial weakness involving the forehead and all muscles of facial expression can be caused by a central lesion, such as a stroke, that involves the ipsilateral facial nerve nucleus or facial nerve tract in the pons. Usually a CVA spares the forehead muscles.
Etiologies: Herpes simplex virus activation is the likely cause of Bell's palsy in most cases. Nevertheless, most patients with peripheral facial palsy are labeled as having Bell's palsy because there is no established method of confirming herpes simplex virus as the mechanism in clinical practice. Herpes zoster is probably the second most common viral infection associated with facial palsy.
Further evaluation warranted: Patients with a typical Bell's palsy that is incomplete and recovers do not need further study. However, imaging of the brain, temporal bone, and parotid gland with high-resolution contrast-enhanced computed tomography (CT) or gadolinium-enhanced magnetic resonance imaging (MRI) is warranted if the physical signs are atypical, if there is slow progression beyond three weeks, or if there is no improvement at four months. In patients with clinically complete lesions, electrodiagnostic studies may be useful for prognostic purposes. Serologic testing for Lyme disease is recommended for adults with acute-onset facial palsy when there is the possibility of exposure in Lyme-endemic areas during the spring through autumn seasons, particularly for those with bilateral facial palsy or other clinical manifestations of Lyme disease.
Treatment:
- Glucocorticoids (all patients)
- prednisone (60 to 80 mg/day) for one week
- Antiviral therapy (severe facial palsy)
- coadministration of oral valacyclovir or acyclovir
- valacyclovir 1000 mg three times daily for one week
- Acyclovir 400 mg five times daily for 10 days
- Eye care to prevent corneal injury
- All patients with Bell's palsy should be assessed for the completeness of eyelid closure. For those with incomplete closure
- Waking hours
- Artificial tear drops (liquid or gel) four times daily and up to hourly if needed
- Protective glasses or goggles can be worn to physically protect the eye from external trauma
- Some patients may prefer to tape the eyelid closed during the day to prevent exposure
- During sleep
- ointment formulation of artificial tears
- the eye can be carefully taped shut using a medical-grade waterproof transparent dressing or tape
- Patching without taping is not generally recommended
Recovery:
- 70 percent of patients are expected to recover spontaneously by three to six months
- Recurrent attacks of Bell's palsy on either the ipsilateral or contralateral side have been observed in 7 to 15 percent of patients
Reference:
- UpToDate 2022
BPPV
- Epley Maneuver
- Turn your head 45 deg toward the side that causes vertigo
- Quickly lay down on your back with your head in the same position just off the edge of the table.
- Wait 30 seconds
- Turn your head 90 deg to the opposite direction without raising it
- Wait 30 seconds
- Rotate the rest of your body and head another 90 deg in that same direction
- Wait 30 seconds
- Sit upright on the side of the bed
- Brandt-Daroff maneuver
- For right and left-sided posterior canalithiasis.
- The seated patient begins by rapidly lying on one side and waits until any provoked vertigo subsides.
- The patient then sits up again, and waits once more for vertigo to subside.
- The next move is to rapidly lie on the other side, wait for any vertigo to subside, and then sit up again.
- The sequence is repeated 10 to 20 times, up to three times a day, until the patient is asymptomatic.
- The symmetry of this maneuver makes it appropriate for either left or right-sided pathology, and it also makes this maneuver useful when one is uncertain as to the side of the canalithiasis.
- Modified Semont maneuver (for left posterior canalithiasis):
- The seated patient begins by turning the head 45° to the right.
- The patient then quickly drops the trunk to the left side with the head turned 45° to the right. This position is held for at least 30 seconds or until any provoked vertigo subsides.
- The patient then quickly sits up and lies down on the right side without stopping in the upright position, all the while keeping the head turned 45° to the right so that the head now faces partly down into the bed. This position is held for 30 seconds or until vertigo subsides.
- Then patient returns to the upright position.
- This maneuver is repeated three times a day until the patient is asymptomatic.
- For right posterior canalithiasis, the maneuver must be performed in the opposite direction, starting with the head turned toward the left.
Reference:
- UTD
Cerebral Vascular Accident
ABCD2 Scoring System:
| Risk | Cat | Score | |
|---|---|---|---|
| A | Age | >60yo | 1 |
| <60yo | 0 | ||
| B | BP | >140/90 | 1 |
| <140/90 | 0 | ||
| C | Clinical | Unilateral weakness | 2 |
| Speech disturbance | 1 | ||
| Other | 1 | ||
| D | Duration | >60 min | 2 |
| 10-59min | 1 | ||
| <10min | 0 | ||
| D | Diabetes | Yes | 1 |
| No | 0 |
ABCD2 Score:
| Score | 2-Day Stroke risk | 7-day | 90-day |
|---|---|---|---|
| 0-3 (Low) | 1% | 1.2% | 3.1% |
| 4-5 (Mod) | 4.1% | 5.9% | 9.8% |
| 6-7 (High) | 8.1% | 12% | 18% |
Testing:
- Brain imaging
- Head CT - imaging of choice for acute stroke
- Brain MRI without gadolinium is most sensitive and specific for acute ischemia
- Vascular imaging
- CTA and MRA of head and neck (gadolinium is not necessary for MRA) preferred over carotid US
- CBC, INR, PTT
- Assess for infection, thrombocytosis, polycythemia, anemia, blood dyscrasias, and bleeding risk
- CMP
- Assess for metabolic derangements, liver failure, renal dysfunction.
- Troponin
- Assess for MI
- Fasting lipid
- Assess for dyslipidemia
- HbA1c/Fasting Glucose
- Assess for DM or impaired fasting glucose
- EKG
- Assess for underlying arrhythmia and/or MI
- TTE
- Assess for wall motion abnormality, apical hypokinesis, mitral or aortic valve pathologies, cardiomyopathy, and heart failure.
- Telemetry
- Assess for paroxysmal atrial fibrillation
Presenting symptom/neuroanatomic correlate:
| Symptom | Neuroanatomic correlate |
|---|---|
| Hemiparesis | Corticospinal tracts (travel primary motor cortex to spinal cord) |
| Hemisensory loss | Ascending sensory tracts (travel up from spinal cord to primary |
| somatosensory cortex) | |
| Aphasia | Dominant hemisphere, cortical |
| Neglect | Non-dominant hemisphere, cortical |
| Loss of vision | Monocular = retinal artery embolism |
| Hemianopia/quadrantanopias = occipital lobe or visual pathways | |
| Ataxia, dysmetria, | Cerebellum and its connections |
| nystagmus, dysarthria, | |
| vertigo | |
| Diplopia, dysphagia, | Brainstem |
| dysarthria, vertigo |
Secondary stroke prevention
- Large artery atherosclerosis (~15% - 20%)
- Extracranial (Carotid or vertebral artery stenosis, nonstenotic ulceration/thrombus)
- ASA +/- clopidogrel
- High intensity statin
- BP goal <140/90 mmHg (post-procedure)
- Lifestyle modification
- CEA/stenting within 2 weeks of TIA or minor/non-disabling CVA
- Intracranial (70%-90% stenotic, symptomatic, atherosclerotic disease)
- ASA +/- clopidogrel for 90 days then ASA alone
- High intensity statin
- BP goal <140/90 mmHg (<130/80 if DM)
- Lifestyle modification
- Angioplasty/stenting considered for medical treatment failures
- Extracranial (Carotid or vertebral artery stenosis, nonstenotic ulceration/thrombus)
- Cardiac emboli (~25% - 30%)
- High risk source of emboli (AF, LV/LA thrombus, HF with EF <30%, acute anterior wall MI, mitral valve disease, mechanical valves)
- Oral anticoagulation
- Rate control in AF
- BP goal <140/90 mm Hg
- LDL goal <100 mg/dL
- Lifestyle modification
- Valve repair/replacement
- Low risk source of emboli (PFO, mitral valve prolapse, focal wall motion abnormalities)
- ASA
- BP goal <140/90 mm Hg
- LDL goal <100 mg/dL
- Lifestyle modification
- Anticoagulation or closure may be recommended for PFO in select cases
- High risk source of emboli (AF, LV/LA thrombus, HF with EF <30%, acute anterior wall MI, mitral valve disease, mechanical valves)
- Small vessel disease (~20% - 30%) - Lacune
- ASA
- High intensity statin
- BP goal <130/80 mmHg
- Lifestyle modification
- Cryptogenic (~30% - 40%)
- Consider vascular neurologist referral
- ASA
- Low dose statin
- BP goal <140/90 mmHg
- Lifestyle modification
- Other identified source (~5%) - arterial dissection, infectious endocarditis, systemic hypercoagulability
- Target identified cause
- Refer to appropriate specialist
BP Management following CVA:
- Prefer ACEIs, ARBs, and thiazide
- Unless a compelling indication for use, B-blockers should not be used to prevent recurrent strokes
Blood pressure targets after CVA:
- Ischemic stroke, non-thrombolysis
- <220/120 mmHg for first 24-48hrs then gradual to normotension over days
- Ischemic stroke, given thrombolytics
- <185/110 mmHg prior to tPA
- Maintain <180/105 for 24hr post tPA
- Then gradual reduction to normotension over days
- Intracranial hemorrhage
- Acute lowering to <160/100 mmHg
- Subarachnoid hemorrhage
- Acute lowering to <140/90 mmHg
Refernces:
- JFP Vol 66 No 6 Jun 2017
- JFP Vol 66 No 7 Jul 2017
Cervical Nerve Roots
- Nerve root C4
- Interspace: C3-C4
- Pain distribution: Lower neck, trapezius
- Motor: None
- Sensory: Cape distribution
- Reflex: None
- Nerve root C5
- Interspace: C4-C5
- Pain distribution: Lateral arm, neck, shoulder
- Motor: Deltoid, elbow flexion
- Sensory: Lateral arm
- Reflex: Biceps
- Nerve root C6
- Interspace: C5-C6 $
- Pain distribution: Dorsolateral arm, neck, thumb $
- Motor: Biceps, wrist extension $
- Sensory: Lateral forearm, thumb $
- Reflex: Brachioradialis
- Nerve root C7
- Interspace: C6-C7 $
- Pain distribution: Dorsolateral forearm, middle finger, neck $
- Motor: Triceps, wrist flexion $
- Sensory: Dorsal forearm, long finger $
- Reflex: Triceps
- Nerve root C8
- Interspace: C7-C8 $
- Pain distribution: Medial forearm, neck, ulnar digits $
- Motor: Finger flexors $
- Sensory: Medial forearm, ulnar digits $
- Reflex: None
- Nerve root T1
- Interspace: C8-T1 $
- Pain distribution: Ulnar forearm $
- Motor: Finger intrinsics $
- Sensory: Ulnar forearm $
- Reflex: None
Tests:
- Spurling (highly specific and sensitive)
- Passively moving patient's neck into lateral flexion and extension and applying gentle axial compression - positive test is reproduction of radicular symptoms
- Shoulder abduction test
- Place palm of the affected limb on top of the patient's head - positive test is relief of radicular symptoms
References:
- AFP Vol 93 No 9 May 2016
Concussions
Common Signs/Symptoms:
- Appears dazed
- Noticeable balance problems
- Answers questions slowly
- Frequent sleep interruptions
- Changes in mood or behavior
- HA or pressure in the head
- Nausea
- Dizziness
- Problems remembering or concentrating
- Sensitive to light or noise
Cognitive and Physical Rest and Aerobic Treatment
- Healthcare providers should counsel patients to observe more restrictive physical and cognitive activity during the first several days following mTBI in children.
- Following these first several days, healthcare providers should counsel patients and families to resume a gradual schedule of activity that does not exacerbate symptoms, with close monitoring of symptom expression (number, severity).
- Following the successful resumption of a gradually increased schedule of activity, healthcare providers should offer an active rehabilitation program of progressive reintroduction of noncontact aerobic activity that does not exacerbate symptoms, with close monitoring of symptom expression (number, severity).
- Healthcare providers should counsel patients to return to full activity when they return to premorbid performance if they have remained symptom-free at rest, and with increasing levels of physical exertion.
Return to School
- To assist children returning to school following mTBI, medical and school-based teams should counsel the student and family regarding the process of gradually increasing the duration and intensity of academic activities as tolerated, with the goal of increasing participation without significantly exacerbating symptoms.
- Return to school protocols should be customized based on the severity of postconcussion symptoms in children with mTBI as determined jointly by medical and school-based teams.
- For any student with prolonged symptoms that interfere with academic performance, school-based teams should assess the educational needs of that student and determine the student's need for additional educational supports, including those described under pertinent federal statutes.
- Postconcussion symptoms and academic progress in school should be monitored collaboratively by the student, family, healthcare provider, and school teams, who jointly determine which modifications or accommodations are needed to maintain an academic workload without significantly exacerbating symptoms.
- The provision of educational supports should be monitored and adjusted on an ongoing basis by the school-based team until the student's academic performance has returned to pre-injury levels. - For students who demonstrate prolonged symptoms and academic difficulties despite an active treatment approach, healthcare providers should refer the child for a formal evaluation by a specialist in pediatric mTBI.
Post-traumatic Headache Treatment and Management:
- Healthcare providers in the emergency department should clinically observe and consider obtaining a head CT in children presenting with a severe and worsening headache, along with other symptoms or risk factors, following mTBI to evaluate for ICI requiring further management in accordance with validated clinical decision making rules.
- Children undergoing observation periods for headache with acutely-worsening symptoms should undergo emergent neuroimaging.
- Healthcare providers and caregivers should offer non- narcotic analgesia to children with a painful headache following acute mTBI, but also provide counseling to the family regarding the risks of analgesic overuse, including a rebound headache.
- There is insufficient evidence to recommend the administration of 3% hypertonic saline as a treatment for an acute headache following mTBI in children. Healthcare providers should not administer this medication to children with mTBI for treatment of symptoms outside of a research setting at this time.
- Chronic headache following mTBI is likely to be multifactorial; therefore, healthcare providers should refer children with chronic headache after mTBI for multidisciplinary evaluation and treatment, with consideration of analgesic overuse as a contributory factor.
Healthcare providers should identify and tailor treatment plans/referrals to address:
- Acutely worsening headache: consider neuroimaging
- Chronic headache: nonopioid analgesia (monitor for overuse), multidisciplinary evaluation
- Vestibulo-ocular dysfunction: vestibular rehabilitation Healthcare providers should identify and tailor treatment plans/referrals to address:
- Worsening sleep problems: sleep hygiene, sleep specialist
- Cognitive impairment: treatment directed at etiology, neuropsychological evaluation
- Emotional dysfunction: psychotherapeutic evaluation and treatment
Vestibulo-ocular Motor Dysfunction:
- Dizziness is another potentially debilitating symptom of mTBI, and limited evidence suggests that early vestibular physical therapy may benefit patients experiencing dizziness. Painful headaches are one of the most common symptoms in children after mTBI and may require intervention.
- Healthcare providers may refer children with subjective or objective evidence of persistent vestibulo-ocular motor dysfunction following mTBI to a program of vestibular rehabilitation.
Sleep Treatment and Management:
- Sleep disturbances after mTBI are common and may exacerbate ongoing problems. Adequate sleep has been shown to improve overall health and should be an important part of treatment for children with mTBI.
- Healthcare providers should provide guidance on proper sleep hygiene methods to facilitate recovery from pediatric mTBI.
- If sleep problems emerge or continue, despite appropriate sleep hygiene measures, healthcare providers may refer children with mTBI to a sleep disorder specialist for further assessment.
Cognitive Impairment Treatment and Management:
- Problems with attention, memory and learning, response speed, and other cognitive impairment can occur following mTBI. These disturbances can result in significant problems with learning in school, or social interactions.
- Healthcare providers should attempt to determine the etiology of cognitive dysfunction within the context of other mTBI symptoms.
- Healthcare providers should recommend treatment for cognitive dysfunction that reflects its presumed etiology.
- Healthcare providers may refer children with persisting complaints related to cognitive function for a formal neuropsychological evaluation to help determine etiology, and to recommend targeted treatment.
Evaluation form:
Reference:
- https://www.cdc.gov/traumaticbraininjury/pdf/pediatricmtbiguidelineeducationaltools/2018-mTBI_AtAGlance_Treatment-508.pdf
- Centers for Disease Control and Prevention (U.S.). Heads up; facts for physicians about mild traumatic brain injury (MTBI). 2/17/09;2009; https://stacks.cdc.gov/view/cdc/12340
- Centers for Disease Control and Prevention (U.S.). A Fact sheet for sports officials. August 2022. https://stacks.cdc.gov/view/cdc/131303
- AFP Oct 2024 Vol 110 No 4
Assessment Tools
Tools:
- Sport Concussion Office Assessment Tool (SCOAT6) - 13+yo
- Sport Concussion Office Assessment Tool (SCOAT6) - 8-12yo
| Test | Sen | Spe | Details | Notes |
|---|---|---|---|---|
| Balance Error Scoring System | 34-64% | 91% | Stability in various leg positions | + Objective test |
| (BESS) | - Most accurate with baseline, takes time and proficiency | |||
| Neurophychological | 71-88% | Paper or computer | + Objective test | |
| - Most accurate with baseline, expensive | ||||
| Symptom checklist | 64-89% | 91-100% | Self report or by medical staff | + Fast, without staff admin time |
| - Subjective | ||||
| Standard Assessment | 80-94% | 76-91% | 6 min, orientation, | + Multiple items measured, nonphysician |
| immediate/delayed memory, concentration | - Staff admin time | |||
| Sensory Organization | 48-61% | 85-90% | Force plate for equilibrium | + Objetive test |
| - Exensive, time needed for testing | ||||
| King-Devick | 86% | 90% | Vision based rapid number naming | + Low cost |
| - Baseline required |
Reference:
- FMX 2016
- AFP Oct 2024 Vol 110 No 4
Management
General Management
- Rest from physical and mental activities
- TV, computers, music limited or stopped
- No sports participation
- Increase fluids; Eat regularly
Most concussion symptoms resolve in 7-10 days
Return to Play ONLY when (See RTP notes):
- Asymptomatic
- Normal neurologic exam
- Off medications related to concussion
- Returned to normal classroom activity
- Neuropsychological testing (as available) has returned to baseline
Note: Early aerobic exercise for symptoms of concussion more than 72 hours after injury may decrease symptom severity and frequency and time to recovery from the day of injury.
Return to activity advice
- Relative rest for the first 24-48 hours after an mTBI is recommended, the goal is to alleviate symptoms and reduce metabolic demands on the brain. Complete rest, such as lying in a dark room and avoiding all sensory stimuli (eg, reading, interacting with family and friends, etc) does not accelerate recovery and is therefore not advisable.
- After an initial period of relative rest and symptom stabilization, patients should be encouraged to gradually resume normal daily activities (including screen time) as tolerated.
- This means that physical and cognitive activities can be progressively resumed at a pace that does not significantly worsen existing symptoms or generate new symptoms.
- Environmental conditions with high sensory stimulation can also be gradually reintroduced. Clinicians may provide more detailed, structured guidance for a graduated activity progression with return to school, sport, or military service.
- Students who are returning to school with residual symptoms may benefit from pragmatic accommodations.
General Approach
- Follow-up primary care should target specific symptoms.
- Underlying this approach is an assumption that mTBI symptoms that persist past the acute period (2 weeks for adults and 4 weeks for school-aged children and adolescents) usually do not have a single etiology. Symptoms result from a complex interplay of biopsychosocial factors, many of which are not unique to mTBI. Two key principles guide treatment.
- First, treatment algorithms that have a substantial evidence base in primary medical or psychiatric disorders generally do not require modification to treat symptoms that occur after an mTBI.
- Second, clinicians should prioritize the treatment of symptoms that are most amenable to intervention and most likely to bring about improvement in other symptoms. Priority symptoms in the subacute to chronic stage of mTBI recovery include headaches, insomnia, anxiety, and depression.27
Headaches
- Posttraumatic headaches do not have a unique location pattern or character but instead mimic primary headache types such as migraine, tension, cervicogenic, and those with mixed features.
- Early management should include avoidance of fasting (skipping meals) and maintaining adequate hydration. During the immediate postinjury period, acetaminophen may be preferred over aspirin and certain other nonsteroidal anti-inflammatory agents that confer a slightly increased risk of hemorrhagic stroke.
- Consider prescription medications when headaches are refractory to lifestyle interventions and occasional over-the-counter analgesics. Medication choice should be based on the primary headache type that the posttraumatic headache most closely resembles.
- Note that opioids, in almost all cases, should be avoided.
- Medication overuse can perpetuate posttraumatic headache.
- Excessive use of rescue pain medications (generally >10 days a month for opiates and triptans or >15 days a month for simple analgesics) for prolonged periods should be discouraged.
- The clinician can initiate a prophylactic bridge (eg, topiramate) along with advice to taper use of rescue medication and keep a daily headache diary before referring to a specialist for medication overuse headache.
Sleep disturbance
- Both hypersomnia and insomnia are common after mTBI. The goal of treatment is to normalize the sleep-wake cycle.
- Initial management of sleep disturbance should include environmental and behavioral modifications, such as setting a regular nighttime sleep schedule, limiting daytime naps, and avoiding foods or substances that may have a stimulating effect.
- If sleep disturbances become persistent, cognitive behavioral therapy is an evidence-based treatment option for primary insomnia.
- Sleep medications may help to normalize the sleep schedule but should only be used on a short-term basis while implementing behavioral strategies.
- Commonly used medications include tricyclic antidepressants, trazodone, and melatonin. Benzodiazepines should be avoided.
- Emergent obstructive sleep apnea, catalyzed by inactivity and weight gain after the injury, should be considered before treating insomnia in adults.
Psychological distress
- Patients with severe depression or anxiety disorders should be referred to a mental health provider, but mild-moderate symptoms (eg, Generalized Anxiety Disorder–7 and Patient Health Questionnaire–9 screening scores both <15) can generally be managed within primary care.
- Cognitive behavioral therapy and selective serotonin reuptake inhibitors are first line treatments for depression and anxiety disorders after mTBI.
- Alternative medications such as serotonin-norepinephrine reuptake inhibitors, tricyclics, trazodone, or mirtazapine may be appropriate, particularly if treating concurrent symptoms such as sleep disturbance, headache, or bodily pain. Several of these agents have antiheadache properties, extending their usefulness. Benzodiazepines for anxiety should be avoided.
- In general, treatment should be initiated as soon as a patient meets diagnostic criteria for a mental health disorder (eg, ≥2 weeks of persistent depressive symptoms for major depressive disorder), and effective pharmacotherapy should be maintained for at least 6 months before considering discontinuation.
Exercise as treatment
- Physical activity has pan-domain beneficial effects. Following an initial brief period symptom subsidence, aerobic exercise at insufficient intensity and duration to provoke symptoms appears safe and therapeutic.
- The preinjury activity level of the patient should be considered in making exercise recommendations, but the clinician could recommend 20 minutes of aerobic exercise 5-6 times a week, initially at light intensity (no more than [220−age]×0.7 heart beats per minute) and supervised (eg, by a physical therapist) and then at home.
Referral to a specialty clinic
- The majority of patients with mTBI can be managed effectively in primary care and need not be referred to a specialty clinic.
- Referral to individual medical specialists or to a specialized multidisciplinary mTBI clinic is appropriate for patients with persistent symptoms (lasting more than 4-6 weeks) that do not respond to treatment in a primary care setting.
- Earlier referral may be helpful when
- Patients have a high symptom burden or known risk factors for prolonged recovery, such as a preexisting mental health disorder,
- Patients are unable to progress with their return to activity or are attempting to return to high-stakes roles soon after injury (eg, competitive sport or university examinations), or (3) access to care is limited (eg, long waitlist times). mTBI clinics should have access to a physician and a multidisciplinary team of licensed health professionals who provide coordinated, evidence-based care.
- Interdisciplinary treatment may include vestibular, vision-oculomotor, behavioral health, and cognitive rehabilitation interventions that are individually tailored to a patient's symptom profile.
- Patients with 1-2 specific symptoms may only require individual disciplines rather than referral to a multidisciplinary clinic. For example, patients with primarily vestibular symptoms should be referred to physical therapy or otolaryngology.
- Musculoskeletal cervical complaints may respond to multifaceted physical therapy.
Pediatric considerations
- There is expert consensus that management of school-aged children and adolescents with mTBI should consider that
- recovery time might be slower than adults
- child-validated symptom rating scales and assessment tools, such as the Child SCAT5109 are most appropriate
- return to activity advice to prevent reinjury should include nonsport play especially in unpredictable environments (eg, schoolyard)
- successful return to school (ie, symptom-free during school activities with no accommodations) should precede return to sport.
Reference:
- https://www.archives-pmr.org/article/S0003-9993(19)31305-X/fulltext
- Early Aerobic Exercise for Postconcussion Symptoms in Adolescent Patients: October 2022
Management - Post-Concussion Headache
To manage these headaches it is also very important to:
- Drink plenty of water
- Get regular sleep
- Eat regular meals
- Decrease or manage stress
- Avoid repeat head injury
- Consider a triptan medication if severe migraine-type headache that doesn't respond to ibuprofen, or acetaminophen for teenagers with a history of migraine headaches, or migraine type post-concussion headaches.
Treatment may also include:
- Medications to treat "spikes" in headache such as acetaminophen, ibuprofen, naproxen or triptans.
- Daily supplements such as magnesium, omega-3 fatty acids, or riboflavin used to decrease headache frequency and severity.
- Daily prescription preventive headache medications to decrease headache frequency and severity.
- Complementary therapies such as physical therapy, massage, biofeedback therapy, or acupuncture.
Once a child or teen has headaches lasting longer than a few weeks after concussion, with guidance from a medical provider, it may be reasonable to consider beginning low-impact aerobic exercise ("sub-threshold" exercise, such as walking, slow swimming, slow stationary biking) that does not make headache or other symptoms worse,
There is a concern that long periods of complete rest may eventually worsen rather than help symptoms (note this is NOT "return to play").
Fortunately, even if post-concussion headaches don't get better in the first few weeks after concussion, most are better within 3 months and almost all are better within a year after injury.
Reference:
Return to Play (Student)
| Stage | Aim | Activity | Goal of Each Step |
|---|---|---|---|
| 1 | Symptom-limited activity | Usual daily activities that do not provoke symptoms | Gradual reintroduction to school and work |
| 2 | Light aerobic exercise | Walking or stationary biking at slow to medium pace without resistance. | Increase heart rate |
| 3 | Sport-specific exercise | Aerobic exercises such as running, sprinting, skating. Sport-specific warm-up and light drills. No head impact activities | Increase motion |
| 4 | Noncontact training drills | More intense training drills. May start progressive resistance training and weight lifting | Assess coordination, fitness, and concentration |
| 5 | Full contact practice | Participate in normal training activities including scrimmaging | Restore confidence and assess functional skills by coaching staff |
| 6 | Return to sport | Normal game play |
NOTE. There should be at least 24 h (or longer) for each step of the progression. If any symptoms worsen during exercise, the athlete should go back to the previous step.
Reference:
School Accommodations (Student)
| Symptom | Manifestation | Possible Accommodations |
|---|---|---|
| Decreased attention/poor concentration | Has trouble focusing during lessons and assignments. | Advise a lighter work load with shorter/modified assignments. Provide written notes of lessons. |
| Trouble remembering | Struggles holding instructions in mind, retaining information, and accessing new concepts. Trouble with reading comprehension and math calculations. | Provide written instructions, shorter reading assignments, and offer smaller amounts of new material to learn. |
| Decreased processing speed | Struggles to keep up with work demands and processes information at a slower rate. | Provide increased time for tests and/or assignments. |
| Cognitive fatigue | Decreased arousal. | Provide breaks throughout day as needed. |
| Emotional symptoms (eg, anxiety or depression) | Increased social isolation or lack of interest in participating in usual activities (eg, sports, clubs). | Provide encouragement to engage in social activities at school and outside of school. Suggest an appointment with a school counselor. |
| Headaches | Interferes with ability to concentrate and perform school work. | Breaks as needed in a quiet environment. |
| Light or noise sensitivity | Symptoms may worsen with screen time or in loud environments. | Offer written assignments vs computer-based assignments. Avoid loud settings, such as cafeteria or assemblies. |
| Symptom sensitivity | Symptoms worsen with cognitive and/or physical exertion. | Reduce cognitive or physical demands by providing rest breaks and completing work in small sections (ie, working to a point that does not elicit symptoms). |
Reference:
Return to Play (Adult)
- 2 weeks rest and symptom free
- Clearance from PCP recommended
- GTRP 24 hrs per stage
- Earliest RTP = 19 days
| Stage | Aim | Activity | Goal of each step |
|---|---|---|---|
| 1 | Symptom-limited activity | Daily activities that do not provoke symptoms | Gradual reintroduction of work/school activities |
| 2 | Light aerobic exercise | Walking or stationary cycling at slow to medium pace. No resistance training | Increase heart rate |
| 3 | Sport-specific exercise | Running or skating drills. No head impact activities | Add movement |
| 4 | Non-contact training drills | Harder training drills, eg, passing drills. May start progressive resistance training | Exercise, coordination and increased thinking |
| 5 | Full contact practice | Following medical clearance, participate in normal training activities | Restore confidence and assess functional skills by coaching staff |
| 6 | Return to sport | Normal game play |
The American Congress of Rehabilitation Medicine recommends the following stages, with at least 24 hours between each step:
- Symptom-limited activity: Engage in usual daily activities that do not provoke symptoms. The goal is the gradual reintroduction to school and work.
- Light aerobic exercise: Activities such as walking or stationary biking at a slow to medium pace without resistance. The aim is to increase heart rate.
- Sport-specific exercise: Aerobic exercises like running, sprinting, or skating, including sport-specific warm-ups and light drills, but no head impact activities. The goal is to increase motion.
- Noncontact training drills: More intense training drills, including progressive resistance training and weight lifting. This step assesses coordination, fitness, and concentration.
- Full contact practice: Participation in normal training activities, including scrimmaging. The goal is to restore confidence and assess functional skills by coaching staff.
- Return to sport: Normal game play.
If symptoms worsen at any stage, the athlete should return to the previous step and attempt progression again after 24 hours.
Notes:
- An initial period of 24–48 hours of both relative physical rest and cognitive rest is recommended before beginning the RTS progression.
- There should be at least 24 hours (or longer) for each step of the progression. If any symptoms worsen during exercise, the athlete should go back to the previous step. Resistance training should be added only in the later stages (stage 3 or 4 at the earliest). If symptoms are persistent (eg, more than 10–14 days in adults or more than 1 month in children), the athlete should be referred to a healthcare professional who is an expert in the management of concussion.
Reference:
- Silverberg ND, Iaccarino MA, Panenka WJ, et al. Management of Concussion and Mild Traumatic Brain Injury: A Synthesis of Practice Guidelines. Archives of Physical Medicine and Rehabilitation. 2020;101(2):382-393. https://doi.org/10.1016/j.apmr.2019.10.179.
- McCrory P, Meeuwisse W, Dvorak J, et al Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016 British Journal of Sports Medicine 2017;51:838-847.
- https://bjsm.bmj.com/content/51/11/838#T1
- https://resources.wftda.org/competition/safety-and-track-resources/concussions/
Study: Is rest after concussion "the best medicine?": Recommendations for activity resumption following concussion in athletes, civilians, and military service members
Practice guidelines universally recommend an initial period of rest for people who sustain a sports-related concussion or mild traumatic brain injury (MTBI) in daily life or military service. This practice is difficult to reconcile with the compelling evidence that other health conditions can be worsened by inactivity and improved by early mobilization and exercise. We review the scientific basis for the recommendation to rest after MTBI, the challenges and potential unintended negative consequences of implementing it, and how patient management could be improved by refining it.
The best available evidence suggests that complete rest exceeding 3 days is probably not helpful, gradual resumption of preinjury activities should begin as soon as tolerated (with the exception of activities that have a high MTBI exposure risk), and supervised exercise may benefit patients with persistent symptoms.
Reference:
- Silverberg ND, Iverson GL. Is rest after concussion "the best medicine?": recommendations for activity resumption following concussion in athletes, civilians, and military service members. J Head Trauma Rehabil. 2013 Jul-Aug;28(4):250-9. doi: 10.1097/HTR.0b013e31825ad658. PMID: 22688215.
Concussion Advice
CONCUSSION INJURY ADVICE (To be given to the person monitoring the concussed athlete)
This patient has received an injury to the head. A careful medical examination has been carried out and no sign of any serious complications has been found. Recovery time is variable across individuals and the patient will need monitoring for a further pe- riod by a responsible adult. Your treating physician will provide guidance as to this timeframe.
If you notice any change in behavior, vomiting, worsening headache, double vision or excessive drowsiness, please telephone your doctor or the nearest hospital emergency department immediately.
Other important points:
Initial rest: Limit physical activity to routine daily activities (avoid exercise, training, sports) and limit activities such as school, work, and screen time to a level that does not worsen symptoms.
- Avoid alcohol/drugs
- Avoid prescription or non-prescription drugs without medical supervision. Specifically:
- Avoid sleeping tablets
- Do not use aspirin, anti-inflammatory medication or stronger pain medications such as narcotics
- Do not drive until cleared by a healthcare professional.
- Return to play/sport requires clearance by a healthcare professional.
Reference:
- Davis GA, et al. Br J Sports Med 2017;0:1–8. https://doi.org/10.1136/bjsports-2017-097506SCAT5
Concussion Recognition Tool
- Visible clues of suspected concussion
- Any one or more of the following visual clues can indicate a possible concussion:
- Loss of consciousness or responsiveness
- Lying motionless on ground / Slow to get up
- Unsteady on feet / Balance problems or falling over / Incoordination
- Grabbing / Clutching of head
- Dazed, blank or vacant look
- Confused / Not aware of plays or events
- Any one or more of the following visual clues can indicate a possible concussion:
- Signs and symptoms of suspected concussion Presence of any one or more of the following signs & symptoms may suggest a concussion:
- "Don't feel right"
- "Pressure in head"
- Amnesia
- Balance problems
- Blurred vision
- Confusion
- Difficulty concentrating
- Difficulty remembering
- Dizziness
- Drowsiness
- Fatigue or low energy
- Feeling like "in a fog"
- Feeling slowed down
- Headache
- Irritability
- Loss of consciousness
- More emotional
- Nausea or vomiting
- Neck Pain
- Nervous or anxious
- Sadness
- Seizure or convulsion
- Sensitivity to light
- Sensitivity to noise
- Memory function
Failure to answer any of these questions correctly may suggest a concussion.
- "What venue are we at today?"
- "Which half is it now?"
- "Who scored last in this game?"
- "What team did you play last week / game?"
- "Did your team win the last game?"
Any athlete with a suspected concussion should be IMMEDIATELY REMOVED FROM PLAY, and should not be returned to activity until they are assessed medically. Athletes with a suspected concussion should not be left alone and should not drive a motor vehicle.
It is recommended that, in all cases of suspected concussion, the player is referred to a medical professional for diagnosis and guidance as well as return to play decisions, even if the symptoms resolve.
RED FLAGS If ANY of the following are reported then the player should be safely and immediately removed from the field. If no qualified medical professional is available, consider transporting by ambulance for urgent medical assessment:
- Athlete complains of neck pain
- Deteriorating conscious state
- Double vision
- Increasing confusion or irritability
- Repeated vomiting
- Seizure or convulsion
- Severe or increasing headache
- Unusual behaviour change
- Weakness or tingling / burning in arms or legs
Remember:
- In all cases, the basic principles of first aid (danger, response, airway, breathing, circulation) should be followed.
- Do not attempt to move the player (other than required for airway support) unless trained to so do
- Do not remove helmet (if present) unless trained to do so.
Reference:
- from McCrory et. al, Consensus Statement on Concussion in Sport. Br J Sports Med 47 (5), 2013
New Orleans criteria for CT after minor head injury
Order CT if one or more of these:
- Headache
- Vomiting
- Age >60yo
- Drug or EtOH intox
- Persistent anterograde amnesia
- Visible trauma above the clavicle
- Seizure
Classification Of Sports/Risk Categories
| Collision | Contact | Non-Contact |
|---|---|---|
| (High) | (Mod) | (Less) |
| Tackle Football | Basketball | Tennis |
| Ice Hockey | Girls Lacrosse | Golf |
| Rugby | Cheerleading | Bowling |
| Boys Lacrosse | Gymnastics | Swimming |
| Wrestling | Flag Football | Track |
| Soccer | Baseball | Cross Country |
| Roller Derby |
Military Primary Care Concussion Management
- Reduce stimulus environments
- Rest (No more than 3 days of complete rest)
- Aggressive HA management - Acetaminophen q6 for 48hrs. After 48hrs - may use naproxen prn
- Consider nortriptyline 10mg ahs or amitriptyline 25mg po qhs for persistent headache (>7d). Prescribe no more than 10 pills.
- Implement duty restrictions
- Address sleep. Zolpidem may be considered for <2wks
- Pain management as applicable
- Avoid tramadol, narcotics
Cranial Hemorrhages
Cranial Hemorrhage Types
- Intracerebral hemorrhage: Bleeding within the brain tissue itself:
- Intraparenchymal hemorrhage: bleeding within the brain parenchyma
- Intraparenchymal contusions: small, scattered areas of bleeding within the brain tissue
- Cerebral microhemorrhages: small, focal areas of bleeding within the brain tissue
- Subarachnoid hemorrhage: Bleeding between the arachnoid layer and the pia mater
- Ruptured aneurysm
- Aneurysmal rupture
- Traumatic head injury
- Epidural hemorrhage: Bleeding between the dura mater and the skull
- Traumatic head injury, especially fractures of the temporal bone
- Rupture of middle meningeal artery
- Subdural hemorrhage: Bleeding between the dura mater and the arachnoid mater
- Traumatic head injury
- Rupture of bridging veins
- Dural arteriovenous fistula (DAVF): A rare condition characterized by abnormal connections between arteries and veins in the dura mater
- Intraparenchymal hemorrhage
- Subarachnoid hemorrhage
Degenerative cervical myelopathy edit
Result in progressive spinal cord dysfunction secondary to cord compression.
Patients are typically male (3:1 male-to-female ratio), and the average age of presentation is 64 years.
Common examination findings include neck pain or stiffness, a wide-based ataxic gait, ascending paresthesia in the upper or lower extremities, lower extremity weakness, decreased hand dexterity, hyperreflexia, clonus, Babinski sign, and bowel or bladder dysfunction in severe disease.
Definitive diagnosis requires correlation of physical examination findings with imaging findings.
Magnetic resonance imaging of the cervical spine with and without contrast media is the preferred imaging modality.
Cervical spine computed tomography, computed tomography myelography, and plain radiography are helpful in certain situations.
Treatment depends on the presence and severity of symptoms.
Surgery is recommended for patients with moderate to severe symptoms or rapidly progressive disease.
- The overall goal of surgery is spinal cord decompression and stabilization in an effort to prevent further neurologic compromise
- Possible surgical complications include C5 nerve palsy (up to 30% of patients) and injuries to the recurrent laryngeal nerve (2.7%), superficial laryngeal nerve (1.3%), or vertebral artery (4.1%)
Conservative treatments with monitoring for progression may be considered in patients with mild to moderate disease.
- physical therapy
- immobilization with hard or soft cervical collars
- cervical traction
- massage
- spinal manipulation therapy
- spinal injections
- and avoidance of high-risk activities
Potential Noncompressive Etiologies for Patients with Cervical Myelopathic Signs and Symptoms
- Acute transverse myelitis
- Liver disease
- Alcohol abuse
- Multiple sclerosis
- Amyotrophic lateral sclerosis
- Paraneoplastic syndrome
- Copper or vitamin B12 deficiency
- Parkinson disease
- Cubital or carpal tunnel syndrome
- Syphilis
- Guillain-Barré syndrome
- Syringomyelia
- HIV or human T-lymphotropic virus 1 infection
- Viral encephalitis
| Spinal cord tracts | Location |
|---|---|
| Dorsal column | Located between the dorsal horns; carries ipsilateral pressure and vibration sensation |
| Lateral corticospinal tract | Lateral aspect of the spinal cord; controls ipsilateral motor function |
| Spinothalamic tract | Located in the anterior cord; carries contralateral pain and temperature sensations |
| Spinal cord pathology | Physical examination findings |
| Dorsal column syndrome | Vibratory and proprioceptive loss below a dermatomal level with preservation of other sensory modalities |
| Hemicord (Brown-Séquard) syndrome | Ipsilateral weakness, vibratory and proprioceptive loss, contralateral pain, and temperature loss |
| Posterior lateral syndrome | Decreased vibratory and proprioceptive sensation and motor control impairments |
Upper motor neuron signs/symptoms (Table 44,9,13,18,27,28) are the hallmark of cervical myelopathy, whereas lower motor neuron symptoms are manifestations of peripheral nerve pathology as seen in radiculopathies.
Upper Motor Neuron Signs and Symptoms of Degenerative Cervical Myelopathy
- Signs
- Atrophy of intrinsic hand muscles
- Babinski sign
- Clonus: Achilles tendon is more commonly affected than the patella
- Gait disturbance: wide-based ataxic gait
- Hyperreflexia of the deep tendon reflexes
- Hyporeflexia of superficial reflexes (abdominal and cremasteric)
- Lhermitte sign (27%)
- Pathologic (upper motor neuron) reflexes: Hoffmann sign inverted brachioradialis reflex, Romberg sign, and Brissaud reflex
- Pyramidal weakness: upper extremity extensors > upper and lower extremity flexors > lower extremity extensors
- Spasticity
- Synkinesis: involuntary movement in a limb associated with voluntary movement of other limbs
- Symptoms
- Ascending paresthesia in the upper and lower extremities
- Autonomic: erectile dysfunction, difficulty with elimination (44%), or bowel or bladder incontinence
- Decreased hand dexterity, changes in handwriting
- Falls
- Lower extremity stiffness, weakness, and sensory loss
- Neck pain (50%) and stiffness
- Radicular pain (38%)
- Scapular pain
References:
- AFP Vol 102 No 12 Dec 2020
Dementia
See Dementia under Geriatrics.
Dizziness
Vertigo Differential Diagnosis:
- BPPV
- Ménière disease[30]
- Inner ear concussion
- Alcohol intoxication
- Labyrinthitis or vestibular neuronitis[10]
- Vascular loop syndrome
- Positional nystagmus of central origin
- Lesion of the nodulus from conditions such as stroke, Arnold-Chiari malformation, multiple sclerosis, cerebellar degeneration, ischemia, and intoxication[10][30]
- Acoustic neuroma and meningioma
- Vertebral artery insufficiency
- Orthostatic hypotension
Types of Dizziness:
- Presyncope
- Dysrhythmia
- Vasovagal syncope
- Orthostatic hypotension
- Hypoglycemia
- Hypoxia
- Hyperventilation
- Vertigo
- Benign paroxysmal positional vertigo
- Labyrinthitis
- Vestibular migraine
- Meniere's disease
- Genetics
- Acustic neuroma
- Age-related vestibular loss
- Cerebellar infarction
- Tullio phenomenon
- Obstructive sleep apnea
- Systemic sclerosis
- Diabetes
- Disequilibrium
- Atypical ("light-headedness")
- Panic attack
- Early hyperventilation
- Toxin exposure
Reference:
- JFP Vol 64 No 11 Nov 2015
HINTS - Vertigo: Central vs Peripheral
Head Impulse:
- Face the patient
- Have them focus on your nose
- Quickly turn the patients head left and right
- If they cannot fixate forward during the test - it is positive for a peripheral lesion
Nystagmus:
- Horizontal nystagmus - if increase when pt looks in direction of fast phase of nystagmus - positive for a peripheral lesion
- Vertical or rotary nystagmus - almost always a central lesion
Test of Skew:
- Face the patient
- Have them focus on your nose
- Cover one eye and then the other. If the uncovered eye has to move up or down to refocus - positive for central lesion
References:
- JFP Vol 64 No 11 Nov 2015
BPPV Maneuvers
- Epley Maneuver
In a patient with right-sided BPPV, the Epley procedure will be done as follows:
Start with the sitting position, and the head is turned in the direction of the affected side. To move the particles, a mastoid bone oscillator is kept behind the affected ear with the help of a headband.
- Position 1 - The patient reclines slowly to the supine position, with head turned 45 degrees to the affected side. The rate is altered to achieve a point of no nystagmus and no symptoms. This usually takes approximately 30 seconds.
- Position 2 - The patient lies supine, 15 degrees Trendelenburg, and head turned 45 degrees toward the affected side. The patient reclines more to the Dix-Hallpike position on the ipsilateral side. It takes around 10 seconds. Then the patient stays in the Dix-Hallpike position for another 20 seconds with the affected ear down.
- Position 3 - The patient lies supine, 15 degrees Trendelenburg, and head turned 45 degrees toward the opposite side. After this, the patient's head is slowly turned from position 3 to the opposite side.
- Position 4 - The patient lies on the side with the opposite shoulder down, head turned 45 degrees toward the contralateral side. The body is then rolled to bring the shoulders perpendicular to the floor with the affected ear up. Next, the head is turned more so that the nose comes at an angle of 45 degrees below the horizon. This takes 40 seconds more.
- Position 5 - The patient is brought back to the sitting position, and the head is turned away from the affected side.
- Ending position - In the end, the head is brought back to the midline. At this point, the headband and the mastoid bone oscillator are removed.
Right ear BPPV patient:
- Sit on exam table with head turned 45 deg to right
- Lie down quickly onto a pillow positioned under shoulders
- After 30 seconds, turn head 90 deg to left without raising head
- After 30 seconds, turn both head and body 90 deg to the left and wait another 30 seconds
- Sit up on the left side of the table
See: http://www.neurology.org/content/vol63/issue1/images/data/150/DC1/video2.mpg
Reference:
- JFP Vol 59 No 5 May 2010
- Palmeri R, Kumar A. Benign Paroxysmal Positional Vertigo. [Updated 2022 Dec 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470308/
- Semont Maneuver
Right ear BPPV patient:
- Sit on the table with head turned 45 deg to left
- Drop rapidly to right side so head contacts the table just behind the right ear
- Wait 30 sec
- Move quickly and smoothly to the left side without stopping in the upright position so the left side of the forehead rests on the exam table
- After 30 sec, sit up again
See: http://www.neurology.org/content/vol63/issue1/images/data/150/DC1/video1.mpg
Reference:
- JFP Vol 59 No 5 May 2010
Headaches
| Tension-Type | Migraine | Cluster | |
|---|---|---|---|
| Intensity | Mild - Mod | Mod - Severe | Sev - Very Severe |
| Location | Often bilat | Often bilat | Unilateral, usually behind or around 1 eye |
| Physical activity | Not aggravated by routine physical activity | Aggravated by routine physical activity | |
| Duration | 30 min - 1 wk | 4-72 hrs | 15-180 min |
| Frequency | Infrequent to daily | Recurrent, variable freq | Once every other day to 8x/d during cluster |
| Symptoms | Light OR Sound sensitivity; Pericranial tenderness; No N/V | Light and sound sensitivity; N/V; Aura, Sensitivity to touch | Eye redness or watering/constricted pupils; Nasal congestion and facial sweating; Eyelid swelling or drooping |
| Demographics | Prevalence higher in women than in men | Prevalence in women 2-3x higher than in men | Prevalence in men 3x higher than in women |
References:
- Headache Classification Committee of the International Headache Society 2018; 38(1)
Chronic Tension Headaches
Management:
- Acetaminophen 1000 mg
- ASA 500 to 1000 mg
- Diclofenac 12.5 to 25 mg
- Ibuprofen 200 to 800 mg
- Naproxen 375 to 550 mg
- Biofeedback and TCAs are effective prophylactics (SOR B)
Prophylaxis:
- Amitriptyline 10 to 75 mg qhs
- Nortriptyline 10 to 100 mg qhs
References:
- JFP Vol 64, No 8 Aug 2015
- AFP Vol 101 No 7 Apr 2020
Cluster Headaches
Management:
- Oxygen 100%, 7 to 12 L per min for 15 min
- Sumatriptan 6mg SQ
- Zolmitriptan 5mg intranasally
Prophylaxis:
- Lithium 900 to 1200 mg daily
- Verapamil 240 to 960 mg daily
References:
- AFP Vol 101 No 7 Apr 2020
EFNS Guideline On The Treatment Of Tension-Type Headache – Report Of An EFNS Task Force
Background:
- Tension-type headache (TTH) is the most prevalent headache type and is causing a high degree of disability. Treatment of frequent TTH is often difficult.
Objectives:
- To give evidence-based or expert recommendations for the different treatment procedures in TTH based on a literature search and the consensus of an expert panel.
Methods:
- All available medical reference systems were screened for the range of clinical studies on TTH. The findings in these studies were evaluated according to the recommendations of the EFNS resulting in level A, B or C recommendations and good practice points.
Recommendations:
- Non-drug management should always be considered although the scientific basis is limited. Information, reassurance and identification of trigger factors may be rewarding.
- Electromyography (EMG) biofeedback has a documented effect in TTH, whilst cognitive-behavioural therapy and relaxation training most likely are effective.
- Simple analgesics and non-steroidal anti-inflammatory drugs are recommended for the treatment of episodic TTH.
- Combination analgesics containing caffeine are drugs of second choice. Triptans, muscle relaxants and opioids should not be used.
- It is crucial to avoid frequent and excessive use of analgesics to prevent the development of medication-overuse headache.
- Physical therapy and acupuncture may be valuable options for patients with frequent TTH, but there is no robust scientific evidence for efficacy.
- The tricyclic antidepressant amitriptyline is drug of first choice for the prophylactic treatment of chronic TTH.
- Mirtazapine and venlafaxine are drugs of second choice.
- The efficacy of the prophylactic drugs is often limited, and treatment may be hampered by side effects.
Reference:
Exertional Headaches
New or never-evaluated exercise headache should have an evaluation:
- brain imaging
- neurovascular evaluation
- MRI and MRA or CT/CTA
- Rule out:
- vascular abnormalities or other structural causes
- subarachnoid hemorrhage
- cerebral or cervical arterial dissection
- reversible cerebral vasoconstriction syndrome
- vascular abnormalities or other structural causes
Cough Headache vs Exertional Headache:
However, several clinical differences between benign cough and benign exercise headache have been identified that aid in distinguishing the two disorders:
- Cough headache is triggered by Valsalva maneuvers, while exercise headache is triggered by more sustained physical exercise
- The average age of patients afflicted with benign cough headache is 67 (± 11), while the average age of patients with benign exercise headache is 24 (± 11)
- Primary cough headache typically has a faster onset than benign exercise headache, which builds up over minutes or longer
- Primary cough headaches are shorter in duration than benign exercise headaches
- Primary cough headaches are typically sharp and stabbing in quality while benign exercise headaches are described as pulsatile
Treatment:
- Treatment of exercise headaches is usually prophylactic or preemptive when exercise is predictable.
- Indomethacin is the de facto drug of choice for benign exercise headaches, although supporting evidence is mainly anecdotal [17,18].
- The therapeutic dose may range from 25 to 150 mg per day, although higher doses up to 250 mg may be necessary.
- Indomethacin can be used daily, but we suggest dosing 30 to 60 minutes before activity/exercise unless headaches are activated on an almost daily basis.
- Propranolol [3], naproxen, phenelzine, and ergonovine have also been reported to be beneficial in some patients [20].
Migraine Headaches
See also:
- Acute Migraines in Children
- The Primary Care Management of Headache: Synopsis of the 2020 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guideline
Diagnostic criteria for migraine without aura:
- At least 5 total episodes of headache that last 4-72 hrs each
- At least 2 of the following characteristics
- Unilateral location
- Pulsing quality
- Moderate to severe pain
- Aggravation with movement
- Causes avoidance of routine activities
- At least 2 of the following
- Nausea
- Vomiting
- Photophobia
- Phonophobia
- Osmophobia
POUND Mnemonic:
- P - Pulsatile quality
- O - One day duration
- U - Unilateral location
- N - Nausea or vomiting
- D - Disabling intensity
| POUND | LR | Prob in | Prob in | Prob in |
|---|---|---|---|---|
| Male | Female | Primary Care | ||
| 4-5 | 24 | 60% | 81% | 92% |
| 3 | 3.5 | 18% | 38% | 64% |
| 0-2 | 0.41 | 2.5% | 6.7% | 17% |
Classification:
- Episodic (EM) less than 15 days per month of headache
- Low frequency EM (<10 days per month) LFEM
- High frequency EM (10-14 days per month) HFEM
- Chronic (CM) 15 or more headache days per month of which 8 or more meet criteria for migraine for at least 3 months
Risk Factor for Stroke:
- Migraine is an independent risk factor for stroke in women <45 years old
- 2-fold increase in ischemic stroke compared to women without migraine
- This increase primarily driven by the subgroup of women who have migraine with aura
- Approximately 1.5 increased risk hemorrhagic stroke in women with migraine
- Other risk factors, such as smoking, amplify this risk
References:
- JFP Vol 65 No 10 Oct 2016
- JAMA 2006;296:1274
- AFP Vol 97 No 4 Feb 2018
- AFP Vol 101 No 7 Apr 2020
- FAFP Spring 2024
- AFP Vol 111 No 4 Apr 2025
- Migraine Management
Consider Migraine Diary
Migraine Abortive therapy (Acute Treatment):
- Acetaminofen 1000 mg
- Acetaminophen NOT recommended as monotherapy
- Acetaminophen/aspirin/carreinge 500mg/500mg/130mg - LOE A
- NNT: 12
- NSAIDs - LOE A
- 1000 mg effervescent ASA = 50mg Imitrex in Sx at 2hrs and 24hr relief
- ASA 975mg (3 adult tabs) is a viable first line treatment for acute migraine. (SOR A)
- ASA 900 -1000 mg
- NNT: 8
- Consider metoclopramide 10mg with aspirin to decrease associated nausea. (SOR A)
- ASA 975mg (3 adult tabs) is a viable first line treatment for acute migraine. (SOR A)
- Ibuprofen/Naproxen/Diclofenac
- Ibuprofen 400 mg to 600 mg
- NNT: 7
- Naproxen 500 to 825 mg
- NNT: 11
- Ibuprofen 400 mg to 600 mg
- 1000 mg effervescent ASA = 50mg Imitrex in Sx at 2hrs and 24hr relief
- Triptans
- If migraine is mild to mod without improvement on nonspecific meds -> Go to triptans
- Sumatriptan (25/50/100mg tabs - $16/9 tabs) - Use 50 mg
- NNT = 3.2 - 3.4 (5 with 100 mg)
- NNH = 7.5 (25mg); 5.1 (100mg)
- Rizatriptan (5/10 mg tabs - $12/6 tabs)
- NNT: 3 (10 mg)
- Zolmitriptan (2.5-5 mg)
- NNT: 3 with 5 mg
- Combined Regimens
- Acetaminophen/aspirin/caffeine - preferred in patients with containdications to vasoconstrictors
- Sumatriptan/naproxen
- Evidence of improved therapy of sumatriptan 85 mg + naproxyn 500 mg (Can make cheaper version with sumatriptan 50mg/naproxen 500 mg)
- NNT: 3
- Dihydroergotomine, intranasal - second line - DHE Nasal Spray 2 mg
- Contraindicated in CVD, HTN, PVD
- Cannot take within 24 hrs of triptan
- Consider timolol maleate 0.5% eyedrops - 1 drop in each eye; can repeat in 10 min (SOR B)
- Gepants (CGRP receptor antagonists) - LOE A
- Rimegepant
- Ubrogepant
- Zavegepant
- Ditan (Lasmiditan - selective 5 HT-1F receptor agonist) - LOE A
- Driving restriction 8 hours
Migraine Refractory Management
- Add dexamethasone to mod-severe migraine headache (SOR A)
- A single dose of 8-24mg may prevent short-term recurrence
- Leads to less medication need and fewer repeat visits to office or ED
- Dihydroergotamine (IV)
- Do not use within 24 hours of triptan
- Severe nausea is common
- Magnesium sulfate (IV) - Used only for migraine with aura
Other notes:
- Do not use opioids or butalbital containing medications except as last resort
- Opiates are vasodilatory and can fuel HA and are associated with chronic daily HA
- Pregnancy:
- Only use Acetaminophen and Metoclopramide
- Children:
- Almotriptan (12-17yo)
- Sumatriptan with naproxen (12+yo)
- Sumatriptan nasal spray (AAN recommends 12+)
Table 172: Effectiveness of Sumatriptan for Migraine Headaches Route Dose NNT for Pain NNT for Pain relief at 2hr free at 2hr Intranasal 10 6 7 20 4 5 Oral 25 4 6 50 4 6 100 4 5 Subcutaneous 4 2 3 6 2 2 Table 173: Percentage of Patients With Headache Response (No or Mild Pain) 2 and 4 Hours Following Treatment Placebo Sumatriptan Tablets Sumatriptan Tablets Sumatriptan Tablets 2 hr 4 hr 25 mg 50 mg 100 mg 2 hr 4 hr 2 hr 4 hr 2 hr 4 hr Study 1 27% 38% 52% 67% 61% % 62% 79% (N = 94) (N = 298) (N = 296) (N = 296) Study 2 26% 38% 52% 70% 50% 68% 56% 71% (N = 65) (N = 66) (N = 62) (N = 66) Study 3 17% 19% 52% 65% 54% 72% 57% 78% (N = 47) (N = 48) (N = 46) (N = 46) Note: There were no statistically significant differences between the 50 and 100 mg dose groups in any study.
Cheapest Triptans:
- Sumatriptan 25mg, 50mg, 100mg, - $16 for 9 tabs
- Rizatriptan 5mg and 10mg - $12 for 6 tabs
Contraindications to Triptans (use acetaminophen/aspirin/caffeine instead):
- Coronary Artery Disease
- Migraine syndromes:
- Hemiplegic
- Basilar migraines
References:
- The Primary Care Management of Headache: Synopsis of the 2020 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guideline
- JFP Vol 58 No 7 Jul 2009
- JFP Vol 63 No 2 Feb 2014
- Headache 2005;45:983-991
- J Neurol 2007;254:705-712
- AFP Vol 97 No 4 Feb 2018
- AFP Vol 107 No 3 Mar 2023
- FAFP Spring 2024
- https://www.drugs.com/pro/sumatriptan.html
- AFP Vol 111 No 4 Apr 2025
- Acetaminofen 1000 mg
- Hellenic Headache Society on the diagnosis and treatment of migraine
- For mild migraine, symptomatic treatment with high dose simple analgesics is suggested
- For moderate to severe migraines triptans or non-steroidal anti-inflammatory drugs, or both, should be administered following an individually tailored therapeutic strategy.
- A rescue acute treatment option should always be advised.
- For episodic migraine prevention, metoprolol (50-200 mg/d), propranolol (40-240 mg/d), flunarizine (5-10 mg/d), valproate (500-1800 mg/d), topiramate (25-100 mg/d) and candesartan (16-32 mg/d) are the drugs of first choice.
- For chronic migraine prevention topiramate (100-200 mg/d), valproate (500-1800 mg/d), flunarizine (5-10 mg/d) and venlafaxine (150 mg/d) may be used, but the evidence is very limited.
Reference:
- Kouremenos E, Arvaniti C, Constantinidis TS, Giannouli E, Fakas N, Kalamatas T, Kararizou E, Naoumis D, Mitsikostas DD; Hellenic Headache Society. Consensus of the Hellenic Headache Society on the diagnosis and treatment of migraine. J Headache Pain. 2019 Dec 13;20(1):113. doi: 10.1186/s10194-019-1060-6. PMID: 31835997; PMCID: PMC6911284.
- For mild migraine, symptomatic treatment with high dose simple analgesics is suggested
- Alternative (CAM) Migraine Therapies
- Acupuncture - effective as prophylaxis (SOR A)
- Biofeedback - effective (SOR A)
- Botox - effective for chronic migraine but risk for averse effects (SOR A)
- Butterbur - Good quality LOE, safety concerns with hepatotoxic and carcinogenic properties (SOR A)
- CBT - probably effective and safe (SOR B)
- Feverfew - probably effective; contraindicated in pregnancy (SOR B)
- Magnesium 400mg/d - probably effective (SOR B)
- Melatonin 3mg - As effective as amytriptyline in reducing headaches and causes fewer adverse effects (SOR B)
- Physical activity - effective in reducing headache frequency if done regularly (SOR B)
- Riboflavin 400mg/d - possibly effective if used <3mo (SOR B)
References:
- JFP Vol 65, No 3 Mar 2016
- JFP Vol 66, No 5 May 2017
- Common Migraine Triggers
Common Migraine Triggers
- Additives
- Alcohol
- Artificial sweeteners
- Caffeine (over consumption and withdrawal)
- Delayed/missed meals
- Exercise
- Foods (chocolate, soft cheese)
- Light
- Menses
- Odors
- Oral contraceptives
- Psychiatric comorbidities
- Red wine
- Sleep distrubances (OSA, insomnia)
- Smoke
- Stress
- Weather changes
References:
- AFP Vol 99 No 1 Jan 2019
- Lifestyle Modification Interventions
Lifestyle Modification Interventions
- Adequate hydration
- Appropriate sleep
- Headache diary to help identify common and uncommon triggers to avoid
- Regular exercise
- Stress reduction including decreasing the fear of future migraines.
Reference:
- AFP Vol 111 No 4 Apr 2025
- Differential Diagnosis of Migraine
Conditions:
- Acute glaucoma
- Acute or chronic subdural hematoma
- Acute severe hypertension
- Benign intracranial hypertension (pseudotumor cerebri)
- Carbon monoxide poisoning
- Carotid artery dissection
- Cluster headache
- Encephalitis
- Frontal sinusitis
- Greater occipital neuralgia
- Intracranial neoplasm
- Medication induced headache
- Meningitis
- Postconcussion syndrome
- Subarachnoid hemorrhage
- Temporal arteritis
- Temporomandibular joint disorder
- Tension-type headache
- Trigeminal neuralgia
References:
- AFP Vol 97 No 4 Feb 2018
- Migraine Prophylaxis
Indications:
- Contraindications to, failure of, overuse of, or adverse effects with treatment
- Disabling headaches despite aggressive intervention
- Headache frequency of more than 2d/wk, 4 migraines/mo, or >8d/mo
- Patient desire to reduce frequency of headaches
- Presence of prolonged aura (>1hr), complex aura (basilar or hemiplegic), or migraine-induced stroke
- Hemiplegic and Basilar Migraines
Table 174: Recommended medications for prophylaxis: Medication Dose Notes First Line? Divalproex 500-1000 mg/d First line Frovatriptan First line Propranolol 80-240 mg/d First line Timolol 20-30 mg/d First line Topiramate 25-200 mg/d 50% pts achieve >50% reduction in frequency First line Sodium valproate 800-1500 mg/d 50% pts achieve >50% reduction in frequency Amitriptyline 25-150 mg/d Often causes sedation Second line Atenolol 50-200 mg Second line Venlafaxine 150 mg/d Second line Zolmitriptan Second line Butterbur 100-150 mg/d Reduces freq by 36-60%; assoc hepatic tox Botox Chronic migraine pts (>15/mo) Atogepant 10, 30, 60 mg Oral CGRP Receptor Antagonist for the prevention of episodic migraine (chronic 60mg dose) gepant Rimegepant 75 mg qod Oral CGRP Receptor Antagonist for the prevention of episodic/chronic migraine gepant erenumab 70mg or 140mg SC monthly CGRP receptor blocker fremanezumab 225mg SC monthly or 3x225mg SC quarterly (=675mg) CGRP ligand blocker galacnezumab 120mg SC monthly (requires 240mg loading dose) CGRP ligand blocker eptinezumab 100mg or 300mg IV infusion monthly CGRP ligand blocker Pearls:
- Amitriptyline - good evidence - SE include dry mouth, wt gain, and drowsiness - take at night
- Valproic Acid and Topiramate - dec freq by 1.3/28 days - expensive - caution in renal/hepatic disease
- Timolol and propranolol - 60-80% effective in reduction of HA - SE include fatigue, ex intol, bradycardia, hypotension, and sexual dysfunction
- Topiramate - avoid in patients who are pregnant, have glaucoma, kidney stones, or liver disease
References:
- Treatment of primary headache disorders; National Headache Foundation 2008:48
- AFP Vol 58 No 11 Nov 2009
- JAMA Vol 317 No 21 Jun 2017
- AFP Vol 99 No 1 Jan 2019
- AFP Vol 101 No 7 Apr 2020
- FAFP Spring 2024
- Red Flags
Symptoms indicating need for neuroimaging and/or urgent subspecialist referral:
- Change in established headache pattern or "worst headache ever"
- Neurologic signs or seizures
- New onset after 50 yrs of age
- Persistent headache after Valsalva maneuver or exertion
- Progressively increasing severity
- Symptoms of systemic disorders (such as fever, hypertension, myalgia, weight loss)
- Thunderclap headache (maximum severity at onset)
References:
- AFP Vol 97 No 4 Feb 2018
Ottowa SAH Rule
Use of this rule:
- For >15yo alert patients with new severee nontraumatic headache with max intensity within 1hr of onset
- NOT for patients with new neurologic deficits, previous aneurysms, SAH, brain tumors, or h/o recurrent HA
Investigate if 1 or more are present:
- Age >40
- Neck pain/stiffness
- Witnessed LOC
- Onset with exertion
- Thunderclap headache
- Limited neck flexion on exam
References:
- JAMA Vol 310 No 12 Sep 2013
Red flags
- HA aggravated or relieved by assuming upright or supine position
- Incracranial hemorrhage
- HA provoked by valsalva
- Arnold-Chiari malformation
- H/o sudden onset HA
- Subarachnoid hemorrhage
- Onset after age 50
- Brain neoplasm
- Papilledema
- Disorders with increased intracranial pressure
- Presence of focal or lateralizing neurologic signs
- Hemorrhagic stroke
- Presence of systemic symptoms
- Giant cell arteritis, meningitis, encephalitis
- Recent pregnancy
- Postpartum preeclampsia
- SNOOPS mneumonic (Recommend imaging CT or MRI)
- S - Systemic symptoms
- fever, weight loss
- N - Neurologic symptoms or abnormal signs (MS etc)
- Confusion, lack of alertness, impaired consciousness
- O - Onset (sudden, arupt, split-second)
- Sudden, abrupt, split-second
- O - Older (new onset or progressive, esp >50yo)
- New or progressive in pts >50yo
- P - Previous HA history (change, or new)
- 1st Ha or new or different headache
- S - Secondary RF (HIV, cancer)Am Acad of Neurology
- HIV, systemic ca
Concerning Headaches
- Thunderclap - suubarachnoid hemorrhage - if suspicious and normal CT -> LP - at 3hrs RBC in lubar area - at 12 hrs xanthochromia (yellowing from RBCs) apparent
- Brain Tumors - Metastatic and astrocytomas more likely tumors assos with HA
- HTN - occurs if severe, changing rapidly, or sustained >240/120 and hypertensicve encephalopathy
- Temp Arteritis - >50yo, new onset, dim pulse/tenderness, ESR >50, biopsy consistant - 3 = 93.5% sensitivity and 91% specificity - immediate steroids - does not affect biopsy results
References:
- Augart C, Vadini A., Headache. FP Essentials 359, 2009
- www.aan.com/globals/axon/assets/2360.pdf
- S - Systemic symptoms
Secondary causes of Headaches
- Infectious
- Intracranial pressure disorders
- Medication related
- Metabolic
- Neuralgias
- Postraumatic
- Structural
- Vascular
| Etiologies | Examples |
|---|---|
| Neoplastic | Primary or metastatic brain neoplasms |
| Infectious | Meningitis, acute sinusitis, brain abscess |
| Vascular | Subarachnoid hemorrhage, carotid or vertebral dissection, aneurysm, CVA, temporal arteritis |
| Low- or high-pressure syndromes | Intracranial hypotension or hypertension |
| Drug-induced | Medication overuse headaches |
| Idiopathic | Vasculitis, CNS lupus, CNS sarcoidosis |
SNOOP4 – When in doubt, investigate the atypical! Systemic symptoms (fever, weight loss); OR
- Systemic symptoms or Secondary risk factors: underlying disease
- Neurologic signs or symptoms: confusion, impaired alertness, or consciousness
- Onset: sudden, abrupt, or split-second - first, worst
- Older: new onset and progressive headache, especially in middle age >50 (giant cell arteritis)
- P4 Pattern change:
- Progression (first headache or different/change in type of headache)
- Postural aggravation
- Precipitated by Valsalva
- Papilledema
Reference:
- FAFP Spring 2024
Neurological Physical Examination
The patient should be asked to do the following:
- Stand with feet together
- Close eyes
- Open eyes and walk heel to toe in a straight line forwards and backwards
- test of plantar and dorsiflexion.
- Walk on tiptoes and then on heels
- test of plantar and dorsiflexion.
- Hold their arms outstretched with palms facing upwards
- normal people are able to hold their pronated arms outstretched and in the same position. Patients with a left-hemisphere lesion may show flexion of the right arm. If there is neglect, there may be downward drift.
- Hold this position for a few seconds
- normal people are able to hold their pronated arms outstretched and in the same position. Patients with a left-hemisphere lesion may show flexion of the right arm. If there is neglect, there may be downward drift.
- With eyes closed, touch the nose with the tip of the index finger that the examiner has just lightly touched. Then touch the nose with the tip of the middle finger that the examiner has just lightly touched
- the patient's index finger on one hand and the middle finger on the other should be touched, and then the patient should be asked to touch their nose with the tip of each of these fingers. Fine finger movement is a useful test of extrapyramidal function.
- Pretend to play the piano with the arms still outstretched
- good screen for ataxia. If the patient has difficulties in doing this, you can then test the more difficult way by asking them to tap rapidly and alternately the back and palm of each hand with the back and palm of the opposite hand (step 9). Most people perform this test better with their dominant hand.
- Pat the back of each hand with the opposite palm
- good screen for ataxia. If the patient has difficulties in doing this, you can then test the more difficult way by asking them to tap rapidly and alternately the back and palm of each hand with the back and palm of the opposite hand (step 9). Most people perform this test better with their dominant hand.
- While facing the examiner, screw eyes tight
- assess muscles innervated by the facial nerve. The patient's face should be watched closely for signs of asymmetry. On opening the eyes, it should be noted whether the pupils constrict. The presence of Horner's syndrome can be checked by looking for signs of ptosis, a slightly quizzical raising of the eyebrow and a constricted pupil. The latter is better seen in a darkened rather than bright room.
- Give a grin
- assess muscles innervated by the facial nerve. The patient's face should be watched closely for signs of asymmetry. On opening the eyes, it should be noted whether the pupils constrict. The presence of Horner's syndrome can be checked by looking for signs of ptosis, a slightly quizzical raising of the eyebrow and a constricted pupil. The latter is better seen in a darkened rather than bright room.
- Protrude the tongue
- test for presence of pseudobulbar palsy.
- Wiggle the tongue
- test for presence of pseudobulbar palsy.
- Stare at the examiner's face and, as the examiner wiggles one finger in each outer quadrant on the left, then on the right and then wiggles one finger on the left and right at the same time, the patient should point to the moving fingers
- The first part of step 14 (wiggling a finger in the outer quadrants to the left and then to the right of the head) achieves adequate visual-field screening. The second part of step 14 (wiggling a finger on both sides of the head at the same time) tests for inattention. If any abnormality is observed, the visual fields must be assessed more thoroughly using a red pin
- Follow the examiner's finger, with head still: the finger should move across the mid-line to shoulder width on either side and then move up and down; this procedure should be repeated on the opposite side
- tests for occulomotor palsies (cranial nerves III, IV and VI) and nystagmus.
- Sit on the examining couch while the examiner tests the patient's reflexes
- Lateralising signs indicating an upper (increased reflexes) or lower (diminished reflexes) motor neurone problem should be looked for.
- Allow the examiner to examine the fundi with an ophthalmoscope
- looks for papilloedema, optic atrophy and system vascular disease (e.g. diabetes or hypertension).
Neurologic Exam Components
My thoughts on what should be in a Neuro Exam:
- Mental status (MMSE, GCS)
- Apearance
- Behavior
- Cognition
- Thought process
- Cranial Nerves
- Speech
- Fluent
- Aphasia
- Cerebellar (coordination/proprioception)
- Gait
- Rapid Alternating Movements
- Finger to nose
- Heel/shin
- Deep tendon reflexes (0-4+)
- Patella
- Biceps
- Muscular strength (0-5)
- Hand grips/Foot pushes if bed ridden
- Sensory assessment
- 2 point descrimination
- Vibration
- Temp
- Stereognosis
Parkinson and Mimics
Parkinson Disease:
- Clinical diagnosis
- Presence of bradykinesia, rigidity, tremor, postural instability
- Gradual symptom progression
- Sustained response to therapy with levodopa
Initiate treatment once patients develop functional disability
Essential tremor:
- Symetric postural tremor;
- Worsens with movement
- Affects distal extremities, head, voice
- Family History
- Improves with alcohol and B-blockers
Vascular parkinsonism:
- Clinically similar to Parkinsons
- May have focal neurologic findings
- Stepwise progression with poor response to carbidopa/levodopa
- Presence of basal ganglia and/or thalamic infarcts on CT or MRI
Drug-induced parkinsonism:
- Clinically similar to Parkinsons
- Drug history or withdrawal
- Antiemetics and psychotropic drugs most common causative agents
Dementia with Lewy Bodies:
- Onset of motor symptoms with dementia and visual hallucinations
- Marked fluctuations in attention and cognition
- Poor response to carbidopa/levodopa
Atypical parkinsonism:
- Clinically similar to Parkinsons but other signs early in disease
- prominent gait and speech impairment
- Prominent postural instability
- Axial rigidity greater than extremity rigidity
- Absence of resting tremor and prominent autonomic dysfunction
- Poor response to carbidopa/levodopa
Treatment:
- First line:
- Carbidopa/levodopa - monotherapy to treat bradykinesia, postural instability, and rigidity
Other Management:
- Cigarette smoking, beer consumption, and high coffee intake are protective against PD
- High dietary (not supplemental) intake of vitamin E (in things like almonds, spinach, sweet potatoes, sunflower seeds, and avocados) and increased nut consumption are protective
References:
- AFP Vol 87 No 4 Feb 2013
- JFP Vol 67 No 5 May 2018
Differentiating Parkinson Disease from Essential Tremor
| Clinical features | Parkinson disease tremor | Essential tremor |
|---|---|---|
| Age at onset | > 50 years | Bimodal (2nd and 6th decade) |
| Gender | Male >= Female | Male = Female |
| Family history | 10% to 15% | 50% |
| Asymmetry | + + + | + |
| Frequency | 4 to 6 Hz | 6 to 12 Hz |
| Character | At rest; Supination-pronation | Postural, kinetic; Flexion-extension |
| Distribution | Hands, legs, chin, tongue | Hands, head, voice |
| Associated features | Bradykinesia, rigidity, postural instability, micrographia | Mild gait disorder or cerebellar signs in a minority |
Peripheral Neuropathy
Evaluation:
- Fasting glucose
- B12
- Methylmalonic acid
- Serum protein electrophoresis (SPEP) or immunofixation electrophoresis (IFE) - order on all pts >60 with LE paraethesias
(SOR C)
Management:
- Consider pregabalin for painful paraesthesias (SOR A)
- Evidence for gabapentin, valproate, amitriptyline, venlafaxine, and duloxetine is moderate
Differential Diagnosis:
- Anatomic:
- Sciatica
- Fibular nerve compression/entrapment
- Nerve dissection from surgery or accidental injury
- Systemic:
- HIV
- Carcinoma/paraneoplastic syndrome
- Monoclonal gammopathy
- Amyloidosis
- Sarcoidosis
- Sjogren's syndrome
- Tick bite
- Metabolic:
- DM
- Thyroid disease
- Renal disease
- Chronic liver disease
- Toxic:
- Vit def (B1, B6, B12)
- Vit excess (B6)
- Heavy metal poisoningg (arsenic, lead, mercury)
- Drug-induced (amiodarone, digoxin, isoniazid, lithium, metronidazole, statins)
- Organophosphate exposure
- Alcohol use
References:
- JFP Vol 64 No 12 Dec 2015
Peripheral Neuropathy
Initial evaluation:
- CBC
- CMP
- Fasting glucose
- TSH
- Vit B12
- Serum protein electrophoresis with immunofixation
Referral fro electrodiagnostic studies if:
- symptoms are worrisome (acute onset, asymmetrical, predominant motor or autonomic symptoms, rapidly progressive)
- if initial workup is normal and symptoms persist
Reference:
- AFP Vol 104 No 3 Sep 2021
Peripheral Neuropathy edit
Peripheral neuropathy, a common neurologic problem encountered by family physicians, can be classified clinically by the anatomic pattern of presenting symptoms and, if indicated, by results of electrodiagnostic studies for axonal and demyelinating disease.
The prevalence of peripheral neuropathy in the general population ranges from 1% to 7%, with higher rates among those older than 50 years.
Common identifiable causes include:
- diabetes mellitus,
- nerve compression or injury,
- alcohol use,
- toxin exposure,
- hereditary diseases,
- and nutritional deficiencies.
Peripheral neuropathy is idiopathic in 25% to 46% of cases.
Diagnosis requires a comprehensive history, physical examination, and judicious laboratory testing.
- Early peripheral neuropathy may present as sensory alterations that are often progressive, including sensory loss, numbness, pain, or burning sensations in a "stocking and glove" distribution of the extremities.
- Later stages may involve proximal numbness, distal weakness, or atrophy.
- Physical examination should include a comprehensive neurologic and musculoskeletal evaluation.
Initial laboratory evaluation includes:
- a complete blood count;
- a comprehensive metabolic profile;
- fasting blood glucose,
- vitamin B12,
- and thyroid-stimulating hormone levels;
- and serum protein electrophoresis with immunofixation.
If the initial evaluation is inconclusive, referral to a neurologist for additional testing (e.g., electrodiagnostic studies, specific antibody assays, nerve biopsy) should be considered.
Treatment of peripheral neuropathy focuses on managing the underlying etiology
- gabapentinoids
- antidepressants
References:
- AFP Vol 102 No 12 Dec 2020
Painful Diabetic Peripheral Neuropathy
First Line:
- Anticonvulsants
- Pregabalin
- Gabapentin
- Antidepressants
- Amitriptyline
- Duloxetine
Second Line:
- SNRIs
- Venlafaxine
- Desvenlafaxine
- Opioid-like drugs
- Tramadol
- Tapentadol ER
- Topical treatments
- Lidocaine 5% patch
- Capsaisin 0.075% cream
Third Line:
- SSRIs
- Citalopram
- Paroxetine
- Escitalopram
- Opioids
- Oxycodone controlled release
References:
- AFP Vol 94 No 3 Aug 2016
Seizures
Seizures edit
The investigators concluded that lamotrigine should be considered the drug of first choice for focal epilepsy and valproate for generalized epilepsy.
For patients treated for focal epilepsy, the first SANAD trail found that lamotrigine and oxcarbazepine had the longest time to treatment failure compared with carbamazepine, gabapentin, and topiramate [56]. Lamotrigine and carbamazepine were associated with the shortest times to 12-month seizure remission. In the SANAD II trial, by intention-to-treat analysis, levetiracetam did not meet noninferiority criteria compared with lamotrigine for time to 12-month seizure remission and was inferior for time to treatment failure for any reason; in contrast, zonisamide did meet the criteria for noninferiority compared with lamotrigine for time to 12-month seizure remission, but was also inferior for time to treatment failure [58]. Both levetiracetam and zonisamide were more likely to fail than lamotrigine due to adverse reactions, but not because of inadequate control of seizures.
For patients treated for generalized and unclassifiable epilepsy, the first SANAD trial found that valproate and lamotrigine were superior to topiramate in regard to time to treatment failure [57]. For time to 12-month seizure remission, valproate and topiramate were more efficacious compared with lamotrigine. In the SANAD II trial, by intention-to-treat analysis, levetiracetam did not meet noninferiority criteria compared with valproate for time to 12-month seizure remission [59].
Some general principles to consider when starting an antiseizure medication include [51-53]:
Start treatment with a single drug (monotherapy).
In general, the strategy is to gradually titrate to the highest dose that is tolerated and/or produces seizure freedom (start low and go slow). The concept is to slowly titrate up to a dose that causes persistent or recurrent side effects and then to titrate back down to a previously tolerable dose.
Using this approach, there is only one decision to make if breakthrough seizures occur, which is to add a second seizure medication; raising the dose to achieve seizure control is not a good option because the patient previously had persistent/recurrent side effects at the next dosage level up. This strategy is especially helpful with antiseizure medications that have easily identified, dose-related side effects and a narrow therapeutic index.
Monitor treatment regularly. At regular office visits, clinicians should ask and record seizure frequency and medication side effects [3].
The recommended initial dose for individual antiseizure medications and a potential titration schedule are presented separately. (See "Antiseizure medications: Mechanism of action, pharmacology, and adverse effects".)
Regular follow-up visits should be scheduled to check drug concentrations, blood counts, and hepatic and renal function, when indicated. These visits are also used to address concerns the patient may have about taking the medication and possible side effects, or psychosocial aspects of their disorder. It may be useful to obtain drug levels at least yearly, including in patients who are not having seizures and not undergoing medication dose changes.
Antiepileptic Medication Recommendations
Adult Partial Onset:
- Level A: carbamazepine, phenytoin
- Level B: valproic acid
- Level C: gabapentin, lamotrigine, phenobarbital, vigabatrin, topiramate, levetiracetam
- Levetiracetam (Keppra), lamotrigine (Lamictal), and carbamazepine (Tegretol) - associated with the longest time to treatment withdrawal (SOR:A)
Elderly Partial Onset:
- Level A: gabapentin, lamotrigine, levetiracetam
- Level B: none
- Level C: carbamazepine
Generalized Onset Tonic-Clonic Adult
- Level A: none
- Level B: none
- Level C: carbamazepine, phenytoin, lamotrigine, oxcabazepine, phenobarbital, topiramate, valproic acid
- Valproic acid - associated with the longest time to treatment withdrawal (SOR:A)
References:
- ILAE treatment guidelines 2006
- AFP Vol 97 No 9 May 2018
Syncope
Causes of syncope:
- Reflex (neurogenic: 35-48% of cases)
- Carotid sinus hypersensitivity - 1%
- Situational - 5%
- Occurs during or after defecation, urination, coughin, or after eating or exercise
- Absence of heart disease; Patient might have had previous experiences
- Vasovagal - 18%
- Inappropriate vasodilation and bradycardia; caused by fear, pain, noxious stimuli, heat, or stress
- Cardiac (5-21% of cases)
- Arrythmia - 14%
- Structural disease - 4%
- Valvular
- Aortic, mitral, or pulmonic stenosis
- Vascular (may be associated with EKG changes)
- AMI, Aortic dissection, PE
- Orthostatic - (4-24% of cases)
- Autonomic failure
- Drug induced
- Anticholinergics
- Diuretics
- Antihypertensives
- Dopaminergics
- opiates
- Antipsychotics
- Sedatives
- TCAs
- Postural orthostatic tachycardia syndrome
- Volume depletion
Risk stratification:
- Associated with Higher Risk
- History suggestive of arrhythmia
- Comorbidities
- EKG history suggestive of arrythmia
- Family History of sudden death
- Hypotension (SBP <90)
- Persistent bradycardia <40 bpm in absence of physical training
- Suggestions of GI bleeding
- Prev undiagnosed systolic murmur
- Older age
- Severe structural heart or CAD
- Associated with chest pain, SOB, abdominal pain, HA
- Associated with sudden onset palpitations
- Lack of prodrome
- Male patient
- Occurs during exertion
- Occurs while sitting or supine
- Associated with Lower Risk (Outpatient evaluation)
- Age <50
- No history of cardiovascular disease
- Normal EKG
- Symptoms consistent with neurally mediated or orthostatic syncope
- Unremarkable cardiovascular exam
- History of recurrent episodes with similar low-risk features
- After prolonged standing
- During or after a meal
- Caused by head rotation or pressure on carotid sinus
- Caused by positional change from supine or sitting to standing
- With a prodrome typical of reflex syncope
- With a trigger such as cough, defecation, or micturition
Diagnostic evaluation:
- Basic labs
- Carotid sinus massage - for unknown etiology in patients >40yo
- EKG - All patients with syncope (diagnostic yield is 3-5%)
- Telemetry
- Echocardiogram
- Electrophysiology - in those with underlying heart disease
- Exercise testing
- Neurologic testing - 20-30% of seizures with transient LOC could be result of syncope
- Orthostatic BP
- Psychiatric evaluation
- Tilt-table testing - distinguish between neurally mediated and orthostatic
| Feature | Possible diagnosis |
|---|---|
| Preexisting disease | |
| Alcoholism, DM, parkinsons | Orthostatic hypotension syndrome |
| FH of sudden cardiac death | Cardiac syncope |
| Heart disease | Cardiac syncope |
| H/o freq and prolonged syncopal events | Psychogenic pseudosyncope, cardiac syncope |
| Psychiatric illness | Psychogenic pseudosyncope |
| Prodrome | |
| Abdominal pain, diaphoresis, nausea | Neurally mediated syncope (vasovagal) |
| Aura | Seizure |
| Blurred vision, dizziness, vertigo | Neurally mediated syncope, orthostatic |
| Chest pain, dyspnea | Cardiac syncope |
| Fluttering or palpitations | Cardiac syncope |
| Focal neurologic deficit | Cerebrovascular accident, TIA |
| Headache | Subarachnoid hemorrhage |
| Slow pulse | Neurally mediated synocpe, cardiac syncope |
| Tonic-clonic movement or posture | Seizure |
| None | Vasovagal or cardiac syncope in older adults, cardiac syncope in younger adults |
| Category | Comment | Points |
|---|---|---|
| Predisposition to vasovagal symptoms | Triggered by being in warm/crowded place, prolonged standing, fear, emotion, or pain | -1 |
| History of heart disease | CAD, AF or flutter, HF, valvular disease, nonsinus rhythm | 1 |
| SBP <90 or >180 mmHg | 2 | |
| Elevated troponin levels | >99th % of normal population | 2 |
| Abnormal QRS axis | <30 or >100 degrees | 1 |
| QRS duration >130 ms | 1 | |
| Corrected QT interval >480 ms | 2 | |
| ED diagnosis | Vasovagal syncope | -2 |
| Cardiac syncope | 2 | |
| Neither | 0 |
| Total score | Risk or arrhythmia or death | Risk Category |
|---|---|---|
| -2 to 0 | 0.2% to 0.9% | Very low |
| 1 | 1.9% | Low |
| 2 to 3 | 3.8% to 7.5% | Medium |
| 4 to 5 | 14.3% to 25.4% | High |
| 6 to 8 | 41.1% to 74.5% | Very high |
References:
- AFP Vol 84 No 6 Sep 2011
- AFP Vol 95 No 5 Mar 2017
- AFP Nov 2023 Vol 108 No 5
Vasovagal Syncope
Syncope is defined as a transient loss of consciousness, associated with an inability to maintain postural tone, rapid and spontaneous recovery, and the absence of clinical features specific for another form of transient loss of consciousness such as epileptic seizure.
Vasovagal syncope is defined as a syncope syndrome that usually
- occurs with upright posture held for more than 30 seconds or with exposure to emotional stress, pain, or medical settings
- features diaphoresis, warmth, nausea, and pallor
- is associated with hypotension and relative bradycardia, when known
- is followed by fatigue
Investigation of Vasovagal Syncope
- Tilt-table testing can be useful for assessing patients with suspected vasovagal syncope who lack a confident diagnosis after the initial assessment.
- Tilt-table testing is a reasonable option for differentiating between convulsive syncope and epilepsy, for establishing a diagnosis of pseudosyncope, and for testing patients with suspected vasovagal syncope but without clear diagnostic features.
- Implantable loop recorders (ILRs) can be useful for assessing older patients with recurrent and troublesome syncope who lack a clear diagnosis and are at low risk of a fatal outcome.
- Tilt testing is not recommended for predicting the response to specific medical treatments for vasovagal syncope.
Lifestyle and Medical Treatment for Vasovagal Syncope
- Education, reassurance, and promoting salt and fluid intake are indicated for patients with vasovagal syncope, unless contraindicated.
- Reducing or withdrawing medications that can cause hypotension can be beneficial for patients with vasovagal syncope.
- Physical counterpressure maneuvers can be useful for patients with vasovagal syncope who have a sufficiently long prodromal period.
- The use of fludrocortisone seems reasonable for patients with frequent vasovagal syncope who lack contraindications for its use.
- Beta-blockers may be considered for patients older than 40 years with frequent vasovagal syncope.
- The use of midodrine seems reasonable for patients with frequent vasovagal syncope and no hypertension or urinary retention.
For patients with only an occasional syncope: Reassure patients, stress fluid and salt intake, and teach counterpressure maneuvers. Do not treat patients who have not fainted in the past year.
Pacemakers for Syncope
- Dual-chamber pacing can be effective for patients 40 years of age or older with recurrent and unpredictable syncope who have a documented pause ≥3 seconds during clinical syncope or an asymptomatic pause ≥6 seconds.
- Tilt-table testing may be considered to identify patients with a hypotensive response who would be less likely to respond to permanent cardiac pacing.
- Pacing may be considered for pediatric patients with recurrent syncope with documented symptomatic asystole who are refractory to medical therapy.
- Dual-chamber pacing may be considered in adenosine-susceptible older patients who have unexplained syncope without a prodrome, a normal ECG, and no structural heart disease.
Reference:
- Sheldon RS, Grubb BP 2nd, Olshansky B, Shen WK, Calkins H, Brignole M, Raj SR, Krahn AD, Morillo CA, Stewart JM, Sutton R, Sandroni P, Friday KJ, Hachul DT, Cohen MI, Lau DH, Mayuga KA, Moak JP, Sandhu RK, Kanjwal K. 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015 Jun;12(6):e41-63. doi: 10.1016/j.hrthm.2015.03.029. Epub 2015 May 14. PMID: 25980576; PMCID: PMC5267948.
Tension Headache edit
Definitions:
- Tension-type headache
- At least 10 previous headache episodes fulfilling the following criteria; number of days with such headaches: less than 180 per year or 15 per month
- Headaches lasting from 30 minutes to 7 days
- At least two of the following pain characteristics:
- Pressing or tightening (nonpulsating) quality
- Mild to moderate intensity (nonprohibitive)
- Bilateral location
- No aggravation from walking stairs or similar routine activities
- Both of the following:
- No nausea or vomiting
- Photophobia and phonophobia absent, or only one is present
- Chronic tension-type headache
- Same as tension-type headache, except number of days with such headaches: at least 15 days per month, for at least six months
- Chronic daily headache
- Features of tension-type headache
- Occurs at least 6 days per week
Indications for Neuroimaging in Patients with Headache Symptoms
- Focal neurologic finding on physical examination
- Headache starting after exertion or Valsalva's maneuver
- Acute onset of severe headache
- Headache awakens patient at night
- Change in well-established headache pattern
- New-onset headache in patient >35 years of age
- New-onset headache in patient who has HIV infection or previously diagnosed cancer
Acute Treatment:
- Most commonly: OTC non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen
- A large, randomized controlled trial1 assigned patients with tension-type headache to treatment with doses of placebo, 400 mg of ibuprofen, or 1,000 mg of acetaminophen. Both medications were well tolerated and significantly more effective than placebo at relieving the symptoms of headache. Ibuprofen was more effective than acetaminophen.
- [Evidence level A, RCT]
- Ibuprofen 400 mg for Tension-type HA
- Number needed to treat = 1 in 14 patients are pain-free at two hours
- If this regimen is inadequate, the patient can try acetaminophen or aspirin combined with caffeine and butalbital.
- This combination is usually quite effective but is also the most frequent cause of chronic daily headache.
- Before initiating this regimen, patients should be informed of the possibility of chronic daily headache and instructed to limit their use of the combination to twice weekly.
Prophylaxis of Frequent Tension Headaches
- Amitriptyline (Elavil) is the most researched of the prophylactic agents for chronic tension-type headache.
- It is typically used in doses of 10 to 75 mg
- 1-2 hours before bedtime to minimize grogginess on awakening
- Evidence level A, RCT
- Double-blind randomized controlled studies confirm its use in patients with chronic tension-type headache.
- Anticholinergic side effects (dry mouth, blurred vision, orthostasis) and weight gain can limit its usefulness in some persons.
- Selective serotonin reuptake inhibitors (SSRIs)
- Have shown their efficacy in the prophylaxis of chronic tension-type headache in small studies.
- The beneficial effect of fluoxetine only manifested after two months of treatment and was slightly inferior to the effect of amitriptyline.
- fluoxetine [Prozac])
- paroxetine [Paxil]
- venlafaxine [Effexor]
- Have shown their efficacy in the prophylaxis of chronic tension-type headache in small studies.
References:
- Am Fam Physician. 2002 Sep 1;66(5):797-805.
- Am Fam Physician. 2016 May 1;93(9):online.
Trigeminal Neuralgia
- Brain MRI should be obtained when suspecting trigeminal neuralgia.
- Carbamazepine is in the initial drug of choice.
Diagnostic criteria:
- Recurrent paroxysms of unilateral facial pain in the distribution of one or more divisions of the trigeminal nerve with no radiation beyond and fulfilling criteria B(2) and C(3).
- Pain has all of the following characteristics:
- Lasting from a fraction of a second to two minutes
- Severe intensity
- Electric shock-like, shooting, stabbing, or sharp quality
- Precipitated by a innocuous stimuli with the affected trigeminal distribution
- Not better accounted for by another ICHD3 diagnosis.
Atypical features suggesting secondary trigeminal neuralgia or alternative diagnosis:
- Abnormal neurologic examination
- Abnormal oral
- Dental or ear examination
- Age less than 40
- Bilateral symptoms
- Dizziness or vertigo
- Hearing loss or abnormality
- Numbness
- Pain episodes persisting longer than two minutes
- Pain outside of trigeminal nerve distribution
- Vision changes
Differential Diagnosis
- Cluster headache
- Dental pain
- Giant cell arteritis
- Glossopharyngeal neuralgia
- Intracranial tumors
- Migraine
- Multiple sclerosis
- Otitis media
- Paroxysmal hemicrania
- Post-harapatic neuralgia
- Sinusitis
- Temporal mandibular joint syndrome
- Trigeminal neuropathy
Reference:
- AFP Vol 111 No 5 May 2025
Temporal Arteritis (Giant Cell Arteritis)
Temporal Arteritis (Giant cell arteritis)
- Initial tests:
- ESR
- CRP
- CBC
- LFTs
- TA biopsy or US
- TA biopsy - most definitive test to establish dx
- High dose prednisone - highly effective therapy, do not delay treatment while awaiting biopsy
- If NO visual issues:
- Immediately start prednisone 1 mg/kg/day orally x 4 weeks, max 80 mg/day. Taper over months once remission occurs (may be 1-2 years)
- IF visual issues:
- Methylprednisolone pulse therapy
Reference:
- FAFP Spring 2024
Diagnostic Criteria
The American College of Rheumatology (ACR) and EULAR updated classification criteria for GCA (2022)
Patient age of 50 years or older is a mandatory requirement for the diagnosis.
Additionally, the following weighted criteria must total 6 points or higher for a diagnosis of GCA:
- Positive temporal artery biopsy or temporal artery halo sign on ultrasonography (5 points)
- ESR ≥50 mm/hr or CRP level ≥10 mg/L (3 points)
- Sudden visual loss (3 points)
- Morning stiffness in shoulders or neck (2 points)
- Jaw or tongue claudication (2 points)
- New temporal headache (2 points)
- Scalp tenderness (2 points)
- Temporal artery abnormality on vascular examination (2 points)
- Bilateral axillary involvement on imaging (2 points)
- Fluorodeoxyglucose-PET activity throughout the aorta (2 points)
These criteria have a sensitivity of 87.0% and a specificity of 94.8%.
Laboratory Workup
Essential laboratory tests for giant cell arteritis (GCA) workup include erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), complete blood count with platelet count, and comprehensive metabolic panel.
ESR and CRP are the cornerstone inflammatory markers, with combined sensitivity of 96-97% for GCA diagnosis.[2][3] While specificity is relatively low (21-30%), normal values of both markers make GCA unlikely, occurring in only 3-4% of confirmed cases.[2][4] ESR >50-60 mm/h and CRP >2.5 mg/dL have negative likelihood ratios of 0.18-0.48, making them useful for ruling out disease when normal.[5]
Platelet count >400 × 10³/μL has diagnostic value with a positive likelihood ratio of 3.75 and specificity of 79%, though sensitivity is only 49%.[5][4] Thrombocytosis and mild anemia of chronic disease are common findings.[2][3]
The American College of Rheumatology recommends obtaining these inflammatory markers as part of clinical monitoring.[6] A comprehensive metabolic panel helps assess for liver function abnormalities (present in approximately one-third of patients) and evaluate overall metabolic status.[2][7]
If clinical suspicion remains high despite normal inflammatory markers, interleukin-6 measurement may be considered, as it can be elevated when ESR and CRP are normal.[8][7] However, this is not routinely recommended in standard practice.[2]
Additional testing may include autoantibody assays (ANCA, anti-CCP) or serum electrophoresis if alternative diagnoses need exclusion, and blood cultures if fever of unknown origin is present.[2]
References:
- Polymyalgia Rheumatica and Giant Cell Arteritis: A Systematic Review. Buttgereit F, Dejaco C, Matteson EL, Dasgupta B. JAMA. 2016;315(22):2442-58. https://doi.org/10.1001/jama.2016.5444.
- Giant-Cell Arteritis and Polymyalgia Rheumatica. Weyand CM, Goronzy JJ. The New England Journal of Medicine. 2014;371(1):50-7. https://doi.org/10.1056/NEJMcp1214825.
- Ischemic Optic Neuropathies. Biousse V, Newman NJ. The New England Journal of Medicine. 2015;372(25):2428-36. https://doi.org/10.1056/NEJMra1413352.
- Population-Based Performance of Inflammatory Markers in Giant Cell Arteritis. Castillejo Becerra CM, Crowson CS, Langenfeld HE, et al. American Journal of Ophthalmology. 2025;275:47-51. https://doi.org/10.1016/j.ajo.2025.03.022.
- Diagnostic Accuracy of Symptoms, Physical Signs, and Laboratory Tests for Giant Cell Arteritis: A Systematic Review and Meta-analysis. van der Geest KSM, Sandovici M, Brouwer E, Mackie SL. JAMA Internal Medicine. 2020;180(10):1295-1304. https://doi.org/10.1001/jamainternmed.2020.3050.
- 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Giant Cell Arteritis and Takayasu Arteritis. Maz M, Chung SA, Abril A, et al. Arthritis Care & Research. 2021;73(8):1071-1087. https://doi.org/10.1002/acr.24632.
- Polymyalgia Rheumatica and Giant-Cell Arteritis. Salvarani C, Cantini F, Boiardi L, Hunder GG. The New England Journal of Medicine. 2002;347(4):261-71. https://doi.org/10.1056/NEJMra011913.
- Polymyalgia Rheumatica and Giant Cell Arteritis: Rapid Evidence Review. Raleigh MF, Stoddard J, Darrow HJ. American Family Physician. 2022;106(4):420-426.
Ultrasound for Diagnosis
Color Doppler ultrasound (CDUS) is the type of ultrasound needed for diagnosing giant cell arteritis. This technique allows visualization of both the vessel wall and blood flow, enabling detection of the characteristic halo sign and compression sign.
The halo sign---hypoechoic (dark) circumferential wall thickening that is non-compressible—is the hallmark finding of acute GCA on ultrasound.[1][2] The compression sign, where the inflamed vessel wall remains visible despite probe compression, has demonstrated excellent specificity of 100% for GCA diagnosis.[3][4]
Bilateral examination of temporal and axillary arteries is recommended as the standard imaging protocol.[1][5] The temporal arteries are assessed along their length, while axillary arteries are particularly important as they increase diagnostic sensitivity and can detect extracranial involvement. Adding large vessel assessment (at least axillary and subclavian arteries) to temporal artery examination increases sensitivity from 84% to 97% and improves negative predictive value from 89% to 98%.[5]
The ultrasound should ideally be performed within 7 days of starting corticosteroids, as the halo sign can disappear rapidly with treatment—typically within 2-4 weeks, though sometimes as early as 2 days.[6][7] Bilateral halos in both temporal and axillary arteries enhance diagnostic performance and can achieve specificities approaching 100%.[1][3]
While ultrasound expertise varies by region, with greater experience in Europe than the US, it offers advantages of being non-invasive, widely available, and more sensitive than temporal artery biopsy for detecting this systemic disease.[8][2]
References:
- Large-Vessel Vasculitis. Cacoub P, Vieira M, Langford CA, Tazi Mezalek Z, Saadoun D. Lancet (London, England). 2025;406(10514):2017-2032. https://doi.org/10.1016/S0140-6736(25)01436-9.
- Ultrasound in the Diagnosis and Management of Giant Cell Arteritis. Schmidt WA. Rheumatology (Oxford, England). 2018;57(suppl2):ii22-ii31. https://doi.org/10.1093/rheumatology/kex461.
- The Use of Ultrasound to Assess Giant Cell Arteritis: Review of the Current Evidence and Practical Guide for the Rheumatologist. Monti S, Floris A, Ponte C, et al. Rheumatology (Oxford, England). 2018;57(2):227-235. https://doi.org/10.1093/rheumatology/kex173.
- Polymyalgia Rheumatica and Giant Cell Arteritis: A Systematic Review. Buttgereit F, Dejaco C, Matteson EL, Dasgupta B. JAMA. 2016;315(22):2442-58. https://doi.org/10.1001/jama.2016.5444.
- Diagnostic Validity of Ultrasound Including Extra-Cranial Arteries in Giant Cell Arteritis. Henry IM, Fernández Fernández E, Peiteado D, Balsa A, de Miguel E. Clinical Rheumatology. 2023;42(4):1163-1169. https://doi.org/10.1007/s10067-022-06420-8.
- Evolution of Ultrasound in Giant Cell Arteritis. Kirby C, Flood R, Mullan R, Murphy G, Kane D. Frontiers in Medicine. 2022;9:981659. https://doi.org/10.3389/fmed.2022.981659.
- Ultrasonography in the Diagnosis and Follow-Up of Giant Cell Arteritis. Coath FL, Mukhtyar C. Rheumatology (Oxford, England). 2021;60(6):2528-2536. https://doi.org/10.1093/rheumatology/keab179.
- 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Giant Cell Arteritis and Takayasu Arteritis. Maz M, Chung SA, Abril A, et al. Arthritis Care & Research. 2021;73(8):1071-1087. https://doi.org/10.1002/acr.24632.
Tremor
Classification:
| Type | Description |
|---|---|
| Action Tremors | Occurs with voluntary contraction of muscle |
| - Postural | Occurs with body part is maintained against gravity (includes essential, physiologic, cerebellar, dystonic, and drug-induced tremors) |
| - Isometric | Occurs as a result of muscle contraction against a rigid stationary object |
| - Kinetic | Occurs with any form of voluntary movement (includes classic essential, cerebellar, dystonic, and drug-induced tremors) |
| - Intention | Subtype of kinetic tremor amplified as target is reached (Presence of this type implies there is a disturbance of the cerebellum or its pathways) |
| Rest Tremors | Occurs in a body part that is relaxed and completely supported against gravity (Most commonly caused by Parkinsonism, but also in severe essential tremor) |
Diagnosis:
- Is tremor physiologic?
- Enhanced physiologic tremor
- Evaluate for anxiety, caffeine, glucose, LFTs, TSH
- Enhanced physiologic tremor
- Is there a medication associated with tremor?
- Drug-induced
- Try off the medication
- Drug-induced
- Is it relieved with distraction?
- Psychogenic
- Send to Mental Health for evaluation
- Psychogenic
- Organic cause
Clues:
- Tremor in older patients and gradual onset are more likely to be Parkinson disease or essential tremor.
- Sudden onset of tremor is more likely to be caused by medication use, toxins, a psychogenic cause, or, in rare cases, a brain tumor.
Common Tremor Syndromes:
- Cerebellar tremor
- Clinical Features
- Intention or postural tremor
- Ipsilateral involvement to lesion
- Abnormal finger-to-nose test
- Imbalance
- Abnormal heel-to-shin test
- Hypotonia
- Diagnostic test
- Head CT or MRI
- Treatment
- Treat underlying cause
- Deep brain stimulation
- Clinical Features
- Enhanced physiologic tremor
- Clinical Features
- Postural tremor
- Low amplitude
- Use of exacerbating medication
- Diagnostic test
- Serum glucose level, TSH, LFTs
- Patient history for anxiety and caffeine use
- Treatment
- Treat underlying cause
- Reassurance
- Clinical Features
- Essential tremor
- Clinical Features
- Postural tremor
- Symmetric
- Involves hands, wrists, lower extremities, head, or voice
- Family history
- Improves with alcohol
- Diagnostic test
- None
- CBC, TSH, CMP
- Treatment
- Propranolol
- Primidone
- Clinical Features
- Parkinsonian tremor
- Clinical Features
- Rest tremor
- Asymmetric
- Involves distal extremities
- Decreases with voluntary movement
- bradykinesia
- Postural instability
- Rigidity
- Diagnostic test
- None
- PET scan for atypical presentation
- Treatment
- Dopamine agonists
- Anticholinergics
- Clinical Features
- Psychogenic tremor
- Clinical Features
- Abrupt onset
- Spontaneous remission
- Extinction with distraction
- Changing tremor characteristics
- Diagnostic test
- Careful history
- Treatment
- Mental health counseling
- Clinical Features
References:
- AFP Vol 83 No 6 Mar 2011
Nutrition
Good nutrition is simply about designing a life where healthy choices are ones that are easy and that you stick to for years:
- Whole foods like fruits, nuts, and vegetables
- Modest portions
- Share meals with people you like
See: Nutrition and Diet
- Limit added sugars to less than 10% of calories per day for ages 2 and older and to avoid added sugars for infants and toddlers;
- Limiting saturated fat to less than 10% of calories per day starting at age 2;
- Limiting sodium intake to less than 2,300 mg per day (or even less if younger than 14);
- Limiting alcoholic beverages (if consumed) to 2 drinks or less a day for men and 1 drink or less a day for women.
Reference:
Beans/Legumes edit
United States Department of Agriculture (USDA) suggests tweaking the Dietary Guidelines for Americans to recommend that people have at least 2.5 cups of beans and lentils a week.
| Red Lentils | Black Beans | Chickpeas | |
|---|---|---|---|
| Calories (per ½ cup) | 343.5 | 331 | 378 |
| Fat | 2 grams | 1.38 grams | 6 grams |
| Protein | 23 grams | 21 grams | 20.5 grams |
| Fiber | 10.35 grams | 15 grams | 12.2 grams |
| Carbohydrates | 60.5 grams | 60.5 grams | 63 grams |
Reference:
Biochemical Nutritional Indications
- Serum Albumin:
- Indicator of long-term depleted protein status, half life = 14-20 days, levels affected by rate of synthesis (liver disease may reduce levels, look for extra loss)
- Serum Transferrin:
- Half-life = 8-9 days, levels change w/other factors-iron status, stress
- Serum Pre-albumin:
- Aka transthyretin and thyroxine-binding prealbumin, short half life =2-3d; returns to normal at beginning of nutritional therapy, so not a good endpoint
- Total Lymphocyte Count = (%lymp on CBC w/diff x WBC)x100,
- Normal = 1200-1800 cells/mm3,
- Moderate protein-calorie malnutrition (PCM) = 800-1200,
- Severe PCM = < 800
Calories in Drinks and Popular Beverages
- Soda
- Serving: 12 ounces
- Calories: 124-189
- Diet soda
- Serving: 12 ounces
- Calories: 0-7
- Bottled sweet tea
- Serving: 12 ounces
- Calories: 129-143
- Unsweetened tea
- Serving: 12 ounces
- Calories: 4
- Orange juice, unsweetened
- Serving: 12 ounces
- Calories: 157-168
- Apple juice, unsweetened
- Serving: 12 ounces
- Calories: 169-175
- Tomato/vegetable juice
- Serving: 12 ounces
- Calories: 80
- Cranberry juice cocktail
- Serving: 12 ounces
- Calories: 205
- Whole milk
- Serving: 12 ounces
- Calories: 220
- 2% low-fat milk
- Serving: 12 ounces
- Calories: 183
- 1% low-fat milk
- Serving: 12 ounces
- Calories: 154
- Nonfat (skim) milk
- Serving: 12 ounces
- Calories: 125
- Soy milk
- Serving: 12 ounces
- Calories: 147-191
- Coffee, black
- Serving: 12 ounces
- Calories: 0-4
- Coffee with cream (2 tablespoons half-and-half)
- Serving: 12 ounces
- Calories: 39-43
- Coffee with whipped cream (2 tablespoons from can)
- Serving: 12 ounces
- Calories: 15-19
- Coffee with heavy whipping cream (2 tablespoons)
- Serving: 12 ounces
- Calories: 104-108
- Latte (espresso coffee) with whole milk
- Serving: 12 ounces
- Calories: 122
- Latte (espresso coffee) with 2% milk
- Serving: 12 ounces
- Calories: 101
- Latte (espresso coffee) with skim (fat-free) milk
- Serving: 12 ounces
- Calories: 69
- Sports drink
- Serving: 12 ounces
- Calories: 94
- Energy drink
- Serving: 1 can (8.3 ounces)
- Calories: 105-112
- Beer, regular
- Serving: 12 ounces
- Calories: 155
- Beer, light
- Serving: 12 ounces
- Calories: 104
- Red wine
- Serving: 5 ounces
- Calories: 125
- White wine
- Serving: 5 ounces
- Calories: 122
Hard liquor (vodka, rum, whiskey, gin; 80 proof)
- Serving: 1.5 ounces
- Calories: 96
Reference:
Dietary Guidelines for Americans (2015-2020)
Healthy diet consists of:
- Vegetables of all types
- Fruits
- Grains - 50% or more being whole grains
- Fat-free or low-fat dairy
- Protein
- Oils
Other points:
- Limit saturated and trans-fats
- Saturated fats should be <10% of daily calories
- Sugars should be <10% of daily calories
- Sodium should be <2300mg daily
Needs:
- Protein needs = 1.4g/kg/day (baseline) to 2g/kg/day (stress)
- Fluid requirements = 40ml/kg/day
References:
- AFP Vol 93 No 6 Mar 2016
Dietary patterns and changes
Dietary patterns and changes:
| Ask About Dietary Pattern | Resonable change | Example |
|---|---|---|
| - Fast food meals or snacks | Decrease by 1 fast food meal | Replace 1 fast food meal per week with prepared |
| per month | per week | food from grocery store or sandwhich from home |
| - Servings of fruit per day | Increase by 1 serving per day | Add fresh, froze, or canned fruit to yogurt |
| - Servings of vegetables | Increase by 1 serving per day | Add fresh, froze, or canned vegetables to yogurt |
| per day | ||
| - Regular sodas, juices, or | Decrease by 1 sugary beverage | Replace a sugared soda with water or flavored |
| other sugary beverages per | per day | water, lightly sweetened tea, or coffee |
| day | ||
| - Servings of beans, nuts, | Increase fish/seafood by around | Replace a fast food entree or processed meat |
| chicken, or fish per week | 1 per week | sandwhich with tuna fish sandwhich |
| - Regular snack chips or | Decrease by 1 serving per week | Replace 1 serving of snack chips or crackers |
| crackers per week | with a handful of nuts | |
| - Desserts and other sweets | Decrease by 1 serving per week | Replace 1 sugary sweet or dessert with a fruit |
| per week | or a handful of nuts | |
| - Use of butter or meat fat | Decrease trans and saturated | Replace butter with light drizzle of olive oil |
| fats as seasoning | and/or spices |
Reference:
- JAMA Vol 318, No 12 Sep 2017
Eat Nuts!
Eat at least 20g of nuts daily
Relative Risk Reduction per 28g/d increase in nut consumption:
- Coronary heart disease: 24%
- Stroke: 11%
- CVD: 19%
- Total ca: 18%
- All-cause mortality: 19%
Relative Risk Reduction per 1 serving:
- Mortality from respiratory disease: 52%
- Mortality from DM: 39%
- Mortality from ID: 75%
- Nut consumtion and risk of cardiovascular disease, total cancer, all-cause martality: a systematic review and dose-response meta-analysis of prospective studies. BMC Med. 2016;14(1):207
- Consultant Feb 2017
Reference:
EBM Food Intake and Diet
Evidence Based Recommendations:
- Fruits and Vegetables: 1/2 of every meal
- Whole grains: 1/4 of every meal
- Legumes and/or animal proteins: 1/4 of every meal
- Water: Primary beverage
- Nuts: Small handful daily
- Oils/fats: In moderation
- Salt: 2,500 mg daily
Dietary Serving Sizes:
- Fruits:
- 1/2 cup
- 1 medium fruit
- Grains:
- 1/2 cup cooked rice, corn, or pasta
- 1/2 cup cooked cereal
- 1 cup ready-to-eat cereal
- 1 slice of bread
- Nuts
- 1/4 cup (1 oz)
- Oils/fats:
- 1 tablespoon
- Protein
- 2-3 oz cooked lean meat, poultry, or fish
- 1 egg
- 1/2 cup cooked beans
- 1/2 cup tofu
- 1/4 cup hummus
- 1 oz nuts
- Vegetables
- 1/2 cup (1 cup leafy greens)
Reference:
Fats and Lipids
Types of dietary fats:
- Monounsaturated fats ('healthy' fats)
- Usually liquid at room temperature
- Peanut butter, almonds, cashews, hazelnuts, peanuts and pistachios.
- Rapeseed oil, olive oil, olives and avocados.
- Polyunsaturated fats ('healthy' fats)
- These are the omega-3 fatty acids and omega-6 fatty acids
- Oily fish like kippers, mackerel and salmon.
- Rapeseed oil, sunflower oil and corn oil.
- Some nuts like walnuts, pine nuts, sesame seeds and sunflower seeds.
- Saturated fats ('unhealthy' fats)
- Most of the foods that contain these types of fats are solid at room temperature
- Processed and fatty meats like sausages, ham, burgers and bacon.
- Hard cheeses like cheddar. Whole milk, cream and ice cream. Butter, lard, ghee, suet, palm oil and coconut oil.
- Trans fats ('unhealthy' fats)
- Fried foods and takeaways.
- Snacks like biscuits, cakes, pies and pastries.
- Hard margarines made with hydrogenated oil.
Dietary goals:
- Men: < 30g Of Saturated Fat Per Day
- Women: < 20g Of Saturated Fat Per Day
- Men And Women: < 5g Of Trans Fat Per Day
- Children: should have less trans fat and saturated fat per day than adults
Low fat foods:
- Sometimes, the fat will be replaced with more sugar or salt to make it taste like the original product. This might not make the lower fat option healthier.
- Check the amount of 'total fat' and the amount of 'saturated fat' per serving on the label.
Easy tips to help you reduce unhealthy fats:
- Cook with vegetable oils and spreads like olive oil, rapeseed oil and sunflower oil.
- Measure the amount of oil you use with a teaspoon or use a spray bottle.
- Make your sandwich fillers healthier by using spreads made from vegetable oils and nuts. And swap hard cheese and processed meat for oily fish and vegetables like avocado, and lettuce.
- Reduce your intake of processed meats like hamburgers and sausages. Choose lean meats (meats with less fat) like skinless chicken, turkey and fish. Or plant-based protein like lentils, beans or Quorn.
- Snack on unsalted nuts and fruit, rather than biscuits, cakes and crisps. Or make your own healthy snacks like homemade fresh fruit scones.
- Use semi-skimmed, skimmed or 1% milk. Or no added sugar, plant-based milk like almond milk, soya milk, oat milk and cashew milk.
- Use lower fat cheeses like feta, mozzarella, half-fat cheddar, edam and ricotta, rather than cheeses like halloumi and cheddar. Or grate your cheese to make it go further in your meal.
- Check the amount of saturated fat per serving on your foods labels to help you keep to the recommended daily intake.
To improve the health benefits of your family's meals
- Choose fish, poultry and lean meats
- Create your own healthy cooking spray
- Use oven-bake method for crispy cravings
- Extend meals with healthy choices
- Add mixed vegetables for both lunch and dinner
Doctors associate a higher TC/HDL ratio with increased insulin resistance and heart problems.
- A high TC to high-density lipoprotein (HDL) ratio is the best predictor of cardiovascular risk (hence this calculation, not LDL, is used in recognised cardiovascular risk calculators such as that from Framingham).
- A high TC to HDL ratio is also a surrogate marker for insulin resistance (ie, chronically elevated serum insulin at the root of heart disease, type 2 diabetes and obesity).
- And in those over 60 years, a recent systematic review concluded that LDL cholesterol is not associated with cardiovascular disease and is inversely associated with all-cause mortality.
- A high TC to HDL ratio drops rapidly with dietary changes such as replacing refined carbohydrates with healthy high fat foods.
Reference:
- https://www.bhf.org.uk/informationsupport/support/healthy-living/healthy-eating/fats-explained
- https://www.dietaryguidelines.gov/resources/2020-2025-dietary-guidelines-online-materials
- https://www.scripps.org/news_items/4359-good-fats-vs-bad-fats
- Malhotra A, Redberg RF, Meier PSaturated fat does not clog the arteries: coronary heart disease is a chronic inflammatory condition, the risk of which can be effectively reduced from healthy lifestyle interventionsBritish Journal of Sports Medicine 2017;51:1111-1112.
Fiber
Sources of Insoluble Fiber:
- Whole grains, such as wheat bran, oats, and barley
- Fruits, such as berries, apples, and bananas (peels and pulp)
- Vegetables, such as broccoli, carrots, and potatoes (skins and pulp)
- Legumes, such as beans and lentils
- Nuts and seeds, such as almonds and flaxseeds
Sources of Soluble Fiber:
- Fruits: apples, bananas, berries, citrus fruits
- Vegetables: carrots, broccoli, Brussels sprouts, sweet potatoes
- Whole grains: oats, barley, wheat bran, brown rice
- Legumes: beans, lentils, peas
- Nuts and seeds: chia seeds, flaxseeds, almonds
Study: Dietary fiber in irritable bowel syndrome
Irritable bowel syndrome (IBS) is a common chronic gastrointestinal disorder.
It is widely believed that IBS is caused by a deficient intake of dietary fiber, and most physicians recommend that patients with IBS increase their intake of dietary fiber in order to relieve their symptoms.
However, different types of dietary fiber exhibit marked differences in physical and chemical properties, and the associated health benefits are specific for each fiber type.
- Short-chain soluble and highly fermentable dietary fiber, such as oligosaccharides results in rapid gas production that can cause abdominal pain/discomfort, abdominal bloating/distension and flatulence in patients with IBS.
- Long-chain, intermediate viscous, soluble and moderately fermentable dietary fiber, such as psyllium results in a low gas production and the absence of the symptoms related to excessive gas production.
The effects of type of fiber have been documented in the management of IBS, and it is known to improve the overall symptoms in patients with IBS. Dietary fiber acts on the gastrointestinal tract through several mechanisms, including increased fecal mass with mechanical stimulation/irritation of the colonic mucosa with increasing secretion and peristalsis, and the actions of fermentation byproducts, particularly short-chain fatty acids, on the intestinal microbiota, immune system and the neuroendocrine system of the gastrointestinal tract.
Fiber supplementation, particularly psyllium, is both safe and effective in improving IBS symptoms globally. Dietary fiber also has other health benefits, such as lowering blood cholesterol levels, improving glycemic control and body weight management.
Reference:
- El-Salhy M, Ystad SO, Mazzawi T, Gundersen D. Dietary fiber in irritable bowel syndrome (Review). Int J Mol Med. 2017;40(3):607-613. https://doi.org/10.3892/ijmm.2017.3072
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5548066/
Study: Dietary Fiber And Body Weight
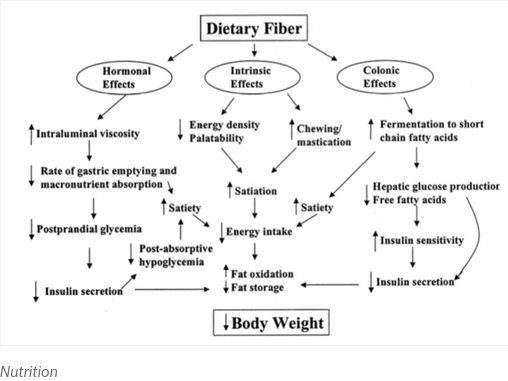
Objective
- This review provides an update of recent studies of dietary fiber and weight and includes a discussion of potential mechanisms of how dietary fiber can aid weight loss and weight maintenance.
Methods
- Human studies published on dietary fiber and body weight were reviewed and summarized. Dietary fiber content of popular low-carbohydrate diets were calculated and are presented.
Results
- Epidemiologic support that dietary fiber intake prevents obesity is strong. Fiber intake is inversely associated with body weight and body fat. In addition, fiber intake is inversely associated with body mass index at all levels of fat intake after adjusting for confounding factors. Results from intervention studies are more mixed, although the addition of dietary fiber generally decreases food intake and, hence, body weight. Many mechanisms have been suggested for how dietary fiber aids in weight management, including promoting satiation, decreasing absorption of macronutrients, and altering secretion of gut hormones.
Conclusion
- The average fiber intake of adults in the United States is less than half recommended levels and is lower still among those who follow currently popular low-carbohydrate diets, such as Atkins and South Beach. Increasing consumption of dietary fiber with fruits, vegetables, whole grains, and legumes across the life cycle is a critical step in stemming the epidemic of obesity found in developed countries. The addition of functional fiber to weight-loss diets should also be considered as a tool to improve success.
Reference:
- Slavin JL. Dietary fiber and body weight. Nutrition. 2005 Mar;21(3):411-8. doi: 10.1016/j.nut.2004.08.018. PMID: 15797686.
IBS Fiber
Soluble vs. Insoluble Fiber: How to Know What's Right for You if You Have IBS
By attracting water, soluble fiber removes excess fluid, which is how it helps decrease diarrhea. Majumdar recommends that her patients with IBS who are dealing with diarrhea increase their intake of these soluble fiber-rich fruits and vegetables:
Higher in soluble fiber (for diarrhea):
- Apples
- Oranges
- Pears
- Strawberries
- Blueberries
- Peas
- Avocados
- Sweet Potatoes
- Carrots
- Turnips
- Oats
- Beans
- Bran
- Barley
Insoluble fiber, on the other hand, does not dissolve in water, so it stays intact as it moves through your digestive system. "This is something that can be helpful for constipation because it adds bulk to the stool and can get things moving, almost like a laxative effect," says Majumdar, who is also a spokesperson for the Academy of Nutrition and Dietetics.
Higher in insoluble fiber (for constipation):
- Zucchini
- Broccoli
- Cabbage
- Leafy Greens
- Cauliflower
- Blackberries
- Flaxseed
- Chia Seeds
- Whole Grains
- Bran
- Brown Rice
- Cereals
- Rolled Oats
A meta-analysis published in September 2014 in The American Journal of Gastroenterology evaluated the use of dietary fiber supplementation in 14 randomized, controlled clinical trials involving 906 people living with IBS. The authors concluded that fiber supplementation — especially with psyllium, a soluble fiber — was effective in improving symptoms of IBS when compared with a placebo.
FODMAP
FODMAP:
- fermentable oligo-, di-, mono-saccharides, and polyols,
- collection of short-chain carbohydrates found in many common foods
- results in increased volume of liquid and gas in the small and large intestine
- contributing to symptoms such as abdominal pain, gas, and bloating, and the motility problems of diarrhea and constipation
High in FODMAPs:
- Fruits:
- Apples
- Apricots
- Blackberries
- Cherries
- Grapefruit
- Mango
- Nectarines
- Peaches
- Pears
- Plums and prunes
- Pomegranates
- Watermelon
- High concentration of fructose from canned fruit, dried fruit or fruit juice
- Grains
- Barley
- Couscous
- Farro
- Rye
- Semolina
- Wheat
- Lactose-Containing Foods
- Buttermilk
- Cream
- Custard
- Ice cream
- Margarine
- Milk (cow, goat, sheep)
- Soft cheese, including cottage cheese and ricotta
- Yogurt (regular and Greek)
- Dairy Substitutes
- Oat milk (although a 1/8 serving is considered low-FODMAP)
- Soy milk (U.S.)
- Legumes
- Baked beans
- Black-eyed peas
- Butter beans
- Chickpeas
- Lentils
- Kidney beans
- Lima beans
- Soybeans
- Split peas
- Sweeteners
- Agave
- Fructose
- High fructose corn syrup
- Honey
- Isomalt
- Maltitol
- Mannitol
- Molasses
- Sorbitol
- Xylitol
- Vegetables
- Artichokes
- Asparagus
- Beets
- Brussels sprouts
- Cauliflower
- Celery
- Garlic
- Leeks
- Mushrooms
- Okra
- Onions
- Peas
- Scallions (white parts)
- Shallots
- Snow peas
- Sugar snap peas
Low in FODMAPs:
- Fruits
- Avocado (limit 1/8 of whole)
- Banana
- Blueberry
- Cantaloupe
- Grapes
- Honeydew melon
- Kiwi
- Lemon
- Lime
- Mandarin oranges
- Olives
- Orange
- Papaya
- Plantain
- Pineapple
- Raspberry
- Rhubarb
- Strawberry
- Tangelo
- Sweeteners
- Artificial sweeteners that do not end in -ol
- Brown sugar
- Glucose
- Maple syrup
- Powdered sugar
- Sugar (sucrose)
- Dairy and Alternatives
- Almond milk
- Coconut milk (limit 1/2 cup)
- Hemp milk
- Rice milk
- Butter
- Certain cheeses, such as brie, camembert, mozzarella, Parmesan
- Lactose-free products, such as lactose-free milk, ice cream, and yogurt
- Vegetables
- Arugula (rocket lettuce)
- Bamboo shoots
- Bell peppers
- Broccoli
- Bok choy
- Carrots
- Celeriac
- Collard greens
- Common Cabbage
- Corn (half a cob)
- Eggplant
- Endive
- Fennel
- Green beans
- Kale
- Lettuce
- Parsley
- Parsnip
- Potato
- Radicchio
- Scallions (green parts only)
- Spinach, baby
- Squash
- Sweet potato
- Swiss chard
- Tomato
- Turnip
- Water chestnut
- Zucchini
- Grains
- Amaranth
- Brown rice
- Bulgur wheat (limit to 1/4 cup cooked)
- Oats
- Gluten-free products
- Quinoa
- Spelt products
- Nuts
- Almonds (limit 10)
- Brazil nuts
- Hazelnuts (limit 10)
- Macadamia nuts
- Peanuts
- Pecan
- Pine nuts
- Walnuts
- Seeds
- Caraway
- Chia
- Pumpkin
- Sesame
- Sunflower
- Protein Sources
- Beef
- Chicken
- Eggs
- Fish
- Lamb
- Pork
- Shellfish
- Tofu and tempeh
- Turkey
Food Intake Planning/Diets
Calorie deficit: 500-1000kcal/day (2-4mJ)
- Focus on number of calories to subtract rather than total in
IOM Acceptable Macronutrient
- Carbs: 45-65%
- Fat: 20-35%
- Protein: 10-35%
Diet ideas:
- Mediterranean-type diet
- Average weight loss was 3.8-10.1 Kg after 1 year vs a loss of 5 to a gain of 2.9 Kg with a low-fat diet. (LOE 1A-)
- Reference:
- AFP Vol 94 No 1 2016
- 3-4-5 Diet (1200kcal - 1500kcal)
- Breakfast (300kcal)
- Snack (150kcal)
- Lunch (400kcal)
- Snack (150kcal)
- Dinner (500kcal)
- Breakfast (300kcal)
- 4-4-4-4 Diet (1600kcal)
- 4 Meals of 400kcal
- 5-3-2-1-almost none plan
- 5 - Eat >5 servings of fruits and vegetables
- 3 - Have 3 structured meals
- 2 - Limit TV/Video game use to <2hrs
- 1 - Engage in >1hr of moderate to vigorous physical activity
- 0 - Limit sugar-sweetened drinks to almost none
Guidance
Drinking 500 mL of water 30 min before all meals lost 9.48 lbs over 12 weeks.
- (Parretti, H. M., Aveyard, P., Blannin, A., Clifford, S. J., Coleman, S. J., Roalfe, A. and Daley, A. J. (2015), Efficacy of water preloading before main meals as a strategy for weight loss in primary care patients with obesity: RCT. Obesity, 23: 1785–1791. doi: 10.1002/oby.21167)
Decreasing fats over carbs leads to greater body fat loss.
- More fat is burned on low carb diets but more fat is lost in low fat diets.
- Low carb diets lead to decreased insulin secretion and substantial sustained increase in net fat oxidation compared to baseline energy balanced diets.
- Reference:
- (Hall, Kevin D. et al. Calorie for Calorie, Dietary Fat Restriction Results in More Body Fat Loss than Carbohydrate Restriction in People with Obesity. Cell Metabolism , Volume 22 , Issue 3 , 427 - 436)
General Tips
- Use smaller dinner plates
- Do not skip meals
- Eat more of the daily calories earlier in day and fewer later in the day
- Keep a food diary
- Look for clues to unhealthy eating
- Serve meals on plates and not by putting dishes on the table
- Do not injest calories in response to thirst
- Avoid the feeling of starvation
- Do not shop for food when hungry
- Use a small bowl or dish, do not eat straight out of the container
- Reduce size of composition of meals
- Do not eat in front of the TV
- Eat a small, healthy snack if you get hungry inbetween meals
- Eat regularly to become hungry but not ravenous
- Decrease poor food choices and volume
- Do not keep tempting, unhealthy foods or snacks in the house
- Eat slowly and stop when no longer hungry
- Place cutlery down between bites
- Pause during meal
- Chew thoroughly
- Try to reduce the energy density of eaten foods
- Increase soups and salad consumption (low calorie density)
References:
- FamilyDoctor.org
How Intermittent Fasting Affects Your Cells and Hormones
When you fast, several things happen in your body on the cellular and molecular level.
- For example, your body changes hormone levels to make stored body fat more accessible.
- Your cells also initiate important repair processes, and change the expression of genes.
Here are some changes that occur in your body when you fast:
- Human Growth Hormone (HGH): The levels of growth hormone skyrocket, increasing as much as 5-fold. This has benefits for fat loss and muscle gain, to name a few (4, 5, 6, 7).
- Insulin: Insulin sensitivity improves and levels of insulin drop dramatically. Lower insulin levels make stored body fat more accessible (8).
- Cellular repair: When fasted, your cells initiate cellular repair processes. This includes autophagy, where cells digest and remove old and dysfunctional proteins that build up inside cells (9, 10)
- Gene expression: There are changes in the function of genes related to longevity and protection against disease (11, 12).
These changes in hormone levels, cell function and gene expression are responsible for the health benefits of intermittent fast
The 5:2 Diet
- For five days a week, you eat normally and don't have to think about restricting calories.
- Then, on the other two days, you reduce your calorie intake to a quarter of your daily needs. This is about 500 calories per day for women, and 600 for men.
- You can choose whichever two days of the week you prefer, as long as there is at least 1 non-fasting day in between.
- A common way of planning the week is to fast on Mondays and Thursdays, with 2 or 3 small meals, then eating normally for the rest of the week.
Insulin and Weight
There are really only two ways that insulin increases. Either:
- We eat more foods that stimulate insulin
- We eat the same insulin-stimulating foods, but more frequently
Controlling insulin requires a change in our diet, which is composed of two factors — how high the insulin levels are after meals, and how long they persist. This boils down to two simple factors:
- What we eat
- Determines how high insulin spikes
- When we eat
- Determines how persistent insulin is
Don't eat all the time.
Losing weight by lowering insulin exposure
Don't eat all the time.
There are really only two ways that insulin increases. Either:
- We eat more foods that stimulate insulin, or;
- We eat the same insulin-stimulating foods, but more frequently.
Controlling insulin requires a change in our diet, which is composed of two factors — how high the insulin levels are after meals, and how long they persist. This boils down to two simple factors:
- What we eat — which determines how high insulin spikes
- When we eat — which determines how persistent insulin is
Reducing insulin depends mostly upon 2 things:
- What you eat
- Macronutrients
- Carbohydrates, particularly refined carbohydrates raise insulin the most.
- Protein also raises insulin significantly, although blood glucose remains stable. Animal proteins stimulate more insulin release compared to plant proteins.
- Dietary fat raises neither glucose nor insulin.
- Rules:
- Avoid added sugar – causes insulin resistance and high insulin
- Eat less refined grains – High insulin effect
- Moderate protein – excessive consumption can be fattening
- Don't be afraid of eating natural fats – Low insulin effect
- Eat real unprocessed foods – refining increases insulin effects
- Macronutrients
- When you eat
- Insulin
- Insulin cycle
- High insulin leads to insulin resistance
- Insulin resistance leads to higher insulin.
- High insulin level depends on 2 things.
- High insulin levels
- Persistence of those high levels
- Providing extended periods of low insulin levels can prevent the development of insulin resistance.
- Use a daily period of fasting.
- Insulin cycle
- Rules:
- Don't eat all the time (time-restricted eating or intermittent fasting). Stop snacking.
- If you want to lose more weight – increase the fasting periods
- Insulin
Ketogenic Diet
The ketogenic diet was developed by Dr. Russell Wilder in the 1920s to treat drug-resistant epilepsy in children. His diet provides at least 90% of calories from fat and has been shown to mimic the beneficial effects of starvation on seizures.
The exact mechanisms behind the ketogenic diet's antiseizure effects remain unknown.
Ketogenic diet:
- Carb intake is limited to 50 grams or fewer per day.
- Protein is often restricted.
- A major goal is to increase ketone blood levels.
On a standard low carb diet, the brain will still largely depend on glucose, the sugar found in your blood, for fuel. However, the brain may burn more ketones than on a regular diet. On a ketogenic diet, the brain is mainly fueled by ketones. The liver produces ketones when carb intake is very low.
Following a ketogenic diet is the most effective way to enter ketosis. Generally, this involves limiting carb consumption to around 20 to 50 grams per day and filling up on fats, such as meat, fish, eggs, nuts, and healthy oils
Practicing intermittent fasting could also help you enter ketosis faster. There are many different forms of intermittent fasting, but the most common method involves limiting food intake to around 8 hours per day and fasting for the remaining 16 hours.
In general, you can eat from the following food groups:
- Fats & Oils. Try to get your fat from natural sources like meat and nuts. Supplement with saturated and monounsaturated fats like coconut oil, butter, and olive oil.
- Protein. Try to stick with organic, pasture-raised and grass-fed meat where possible. Most meats don't have added sugar in them, so they can be consumed in moderate quantity. Remember that too much protein on a ketogenic diet is not a good thing.
- Vegetables. Fresh or frozen doesn't matter. Stick with above ground vegetables, leaning toward leafy/green items.
- Dairy. Most dairy is fine, but make sure to buy full-fat dairy items. Harder cheeses typically have fewer carbs.
- Nuts and Seeds. In moderation, nuts and seeds can be used to create some fantastic textures. Try to use fattier nuts like macadamias and almonds.
- Beverages. Stay simple and stick to mostly water. You can flavor it if needed with stevia-based flavorings or lemon/lime juice.
Do Not Eat:
- Grains – wheat, corn, rice, cereal, etc.
- Sugar – honey, agave, maple syrup, etc.
- Fruit – apples, bananas, oranges, etc.
- Tubers – potato, yams (sweet potato), etc.
Do Eat:
- Meats – fish, beef, lamb, poultry, eggs, etc.
- Leafy Greens – spinach, kale, etc.
- Above-ground veggies & leafy greens — Spinach, kale, cauliflower, broccoli, etc.
- High Fat Dairy – hard cheeses, high fat cream, butter, etc.
- Nuts and seeds – macadamias, walnuts, sunflower seeds, etc.
- Avocado and berries – raspberries, blackberries, and other low glycemic impact berries
- Sweeteners – stevia
- Some fruits — Avocados, berries, etc.
- Other fats – coconut oil, high-fat salad dressing, saturated fats, etc.
Sample calculations of daily energy requirements for the 3:1 classic ketogenic diet for a 18 kg patient.
- Daily caloric requirement
- Total body weight × 68 cal/kg/day
- 18 kg × 68 cal/kg/day = 1224 cal/day
- Daily number of dietary units
- For 3:1 (fat:protein/carbohydrate)
- 3 g fat/unit × 9 cal/g fat -> 27 calories
- 1 g protein or CHO/unit × 4 cal/g protein or carbohydrate (CHO) = 4 calories
- 27 + 4 = 31 calories/unit
- Daily caloric requirement ÷ calories/unit = dietary units/day
- 1224 ÷ 31 = 39 units/day
- For 3:1 (fat:protein/carbohydrate)
- Daily fat content
- Dietary units/day × g fat/unit = g fat/day
- 39 units/day × 3 g fat/unit = 117 g fat/day
- Daily protein and CHO content (combined)
- Dietary units/day × g protein or CHO/unit = g protein or CHO/day
- 39 units/day × 1 g protein or CHO/unit = 39 g protein and CHO/day
- Daily protein content = 1 g/kg/day
- 1 g/kg/day × 18 kg = 18 g/day
- Daily carbohydrate content
- Combined protein and CHO content − daily protein content = daily carbohydrate content
- 39 g protein and CHO/day − 18 g protein/day = 21 g CHO/day
- Divide allotment into 3 meals
- Fat: 117 ÷ 3 = 39 g/meal
- Protein: 18 ÷ 3 = 6 g/meal
- CHO: 21 ÷ 3 = 7 g/meal
References:
Low Glycemic Index
How to implement a Low Glycemic Index Diet
The Low Glycemic Diet will work with your current diet plan. You will continue your current calorie and carbohydrate levels. The only thing you will be doing different is making smarter (Low GI) food choices based on the glycemic index of different foods.
- Step #1 - Make a list of the main carbohydrates (vegetables, fruits, breads, grains, cereals, pasta, rice, juices, beans, soups, baked goods, etc.) in your diet and note the number of times a week you eat that particular food.
- Step #2 - Now look up the Glycemic Index for each food on your list. If you can't find a particular food listed, consider the foods ingredients. If they are all highly processed (refined white flour, sugar, corn syrup) rank the food HIGH. If the food has some processed and some unprocessed ingredients, rank it a MEDIUM. If almost all the ingredients are in their natural state, rank the food as LOW. This is a good rule of thumb, but it's not exact. Also, overcooked foods will tend to have a higher GI than undercooked foods. This is especially true for pasta, vegetables, grains, and cereals.
- Step #3 - Identify the high glycemic foods in your diet, foods with a G.I. over 70 and try to eliminate as many as you can. Pick out some of the medium GI foods (GI between 55 and 70) you can do without.
- Step #4 - Then, using the GI Food List, find low G.I. substitute foods you enjoy and start working them into your every day diet. If you're eating out and have to select a high GI food try to offset it by ordering something with a very low GI. Or, consider ordering a vinaigrette dressing on a salad to bring the average GI of your meal lower. Remember, this isn't an "all or nothing" diet. No one eats perfectly all the time. Just do the best you can and watch what happens.
Is the Altman Rule a proxy for glycemic load?
The Altman Rule:
Grams of fiber (>=3g) + grams of protein must be > grams of sugar
A food is a healthier option:
- Have 3g or more of fiber
- Grams of fiber + protein is more than grams sugar
Background:
- The Altman Rule, a simple tool for consumers seeking to make healthier packaged food choices at the point of sale, applies to packaged carbohydrates.
- According to the Altman Rule, a food is a healthier option if it has at least 3 g of fiber per serving and the grams of fiber plus the grams of protein exceed the grams of sugar per serving.
- This study sought to evaluate whether the Altman Rule is a valid proxy for glycemic load (GL).
Methods:
- We compared the binary outcome of whether a food item meets the Altman Rule with the GL of all foods categorized as cereals, chips, crackers, and granola bars in the Nutrition Data System for Research Database (University of Minnesota, Version 2010). We examined the percentage of foods in low-, medium-, and high-GL categories that met the Altman Rule.
Results:
- There were 1235 foods (342 cereals, 305 chips, 379 crackers, and 209 granola bars) in this analysis.
- There was a significant relationship between the GL of foods and the Altman Rule (P < .001) in that:
- most low-GL (68%) met the criteria of the rule
- almost half of medium-GL (48%) met the criteria of the rule
- very few high-GL (7%) foods met the criteria of the rule
Conclusions:
- The Altman Rule is a reasonable proxy for GL and can be a useful and accessible tool for consumers interested in buying healthier packaged carbohydrate foods.
Reference:
- Dong KR, Eustis S, Hawkins K, Altman W. Is the Altman Rule a proxy for glycemic load? J Fam Pract. 2023 Sep;72(7):286-291. doi: 10.12788/jfp.0656. PMID: 37729141.
- https://www.mdedge.com/familymedicine/article/265249/mixed-topics/altman-rule-proxy-glycemic-load
Low Glycemic Index Foods
| Food Category | Food | GI Value |
|---|---|---|
| Fruits | Apple | 38 |
| Fruits | Apricots, canned | 64 |
| Fruits | Apricots, dried | 30 |
| Fruits | Apricots, fresh | 57 |
| Fruits | Banana | 52 |
| Fruits | Cantaloupe | 65 |
| Fruits | Cherries | 22 |
| Fruits | Dates | 103 |
| Fruits | Figs, dried | 61 |
| Fruits | Fruit Cocktail | 55 |
| Fruits | Grapefruit | 25 |
| Fruits | Grapes | 46 |
| Fruits | Kiwi | 58 |
| Fruits | Mango | 51 |
| Fruits | Orange, Navel | 42 |
| Fruits | Papaya | 56 |
| Fruits | Peach, canned in juice | 38 |
| Fruits | Peach, fresh | 42 |
| Fruits | Pear, canned | 43 |
| Fruits | Pear, fresh | 38 |
| Fruits | Pineapple, fresh | 66 |
| Fruits | Plum | 39 |
| Fruits | Prunes | 29 |
| Fruits | Raisins | 56 |
| Fruits | Strawberries | 40 |
| Fruits | Watermelon | 72 |
| Vegetables | Beets | 64 |
| Vegetables | Broccoli | 10 |
| Vegetables | Cabbage | 10 |
| Vegetables | Carrots | 49 |
| Vegetables | Corn, fresh | 60 |
| Vegetables | Green peas | 48 |
| Vegetables | Lettuce | 10 |
| Vegetables | Mushrooms | 10 |
| Vegetables | Onions | 10 |
| Vegetables | Parsnips | 97 |
| Vegetables | Pumpkin | 75 |
| Vegetables | Red Peppers | 10 |
| Beans | Baked Beans | 48 |
| Beans | Blackeyed Peas, canned | 42 |
| Beans | Chana Dal | 8 |
| Beans | Chickpeas, canned | 42 |
| Beans | Chickpeas, dried | 28 |
| Beans | Kidney Beans, canned | 52 |
| Beans | Kidney Beans, dried | 28 |
| Beans | Lentils | 29 |
| Beans | Lima Beans (frozen) | 32 |
| Beans | Yellow Split Peas | 32 |
| Potatoes | Baked | 85 |
| Potatoes | Canned | 65 |
| Potatoes | Instant Mashed | 86 |
| Potatoes | French Fries | 75 |
| Potatoes | New | 57 |
| Potatoes | Red Skinned, boiled | 88 |
| Potatoes | Sweet | 44 |
| Potatoes | White skinned mashed | 70 |
| Potatoes | Yam | 37 |
| Rice | Aborio | 69 |
| Rice | Basmati | 58 |
| Rice | Barley, pearled | 25 |
| Rice | Brown | 55 |
| Rice | Buckwheat | 54 |
| Rice | Converted, White | 38 |
| Rice | Cornmeal | 68 |
| Rice | Couscous | 65 |
| Rice | Glutinous (Sticky) | 98 |
| Rice | Instant, White | 87 |
| Rice | Long grain, White | 44 |
| Rice | Short grain, White | 72 |
| Rice | Wild rice | 87 |
| Soups | Black Bean | 64 |
| Soups | Lentil | 44 |
| Soups | Minestrone | 39 |
| Soups | Pea | 66 |
| Soups | Tomato | 38 |
| Pasta | Capellini | 45 |
| Pasta | Fettuccini (egg) | 32 |
| Pasta | Linguine | 46 |
| Pasta | Macaroni | 47 |
| Pasta | Spaghetti, white | 38 |
| Pasta | Spaghetti, whole wheat | 37 |
| Pasta | Spiral Pasta | 43 |
| Pasta | Star Pastina | 38 |
| Pasta | Rice vermicelli | 58 |
| Breads | Bagel | 72 |
| Breads | Bread stuffing | 74 |
| Breads | Croissant | 67 |
| Breads | French Baguette | 95 |
| Breads | Hamburger bun | 61 |
| Breads | Kaiser roll | 73 |
| Breads | Pita, whole wheat | 57 |
| Breads | Pumpernickel | 41 |
| Breads | Sourdough | 53 |
| Breads | Stone Ground whole wheat | 53 |
| Breads | Taco Shell | 68 |
| Breads | White | 70 |
| Breads | Whole Meal Rye | 58 |
| Breads | Whole Wheat (100%) | 77 |
| Bakery | Angel Food Cake | 67 |
| Bakery | Blueberry Muffin | 59 |
| Bakery | Bran Muffin | 60 |
| Bakery | Carrot Muffin | 62 |
| Bakery | Doughnut | 76 |
| Bakery | Pastry Pie Crust | 59 |
| Bakery | Pound Cake | 54 |
| Bakery | Scones | 92 |
| Bakery | Sponge Cake | 46 |
| Crackers | Graham Crackers | 74 |
| Crackers | Kavli Crispbread | 71 |
| Crackers | Melba Toast | 70 |
| Crackers | Rice Cakes | 82 |
| Crackers | Rice Crackers | 91 |
| Crackers | Ryvita Crispbread | 69 |
| Crackers | Soda Crackers | 74 |
| Crackers | Stoned Wheat Thins | 67 |
| Crackers | Water crackers | 78 |
| Breakfast and cereals | All Bran with Fiber | 38 |
| Breakfast and cereals | Bran Buds | 47 |
| Breakfast and cereals | Bran Chex | 58 |
| Breakfast and cereals | Bran Flakes | 74 |
| Breakfast and cereals | Cheerios | 74 |
| Breakfast and cereals | Corn Chex | 83 |
| Breakfast and cereals | Corn Flakes | 92 |
| Breakfast and cereals | Cream of Wheat | 66 |
| Breakfast and cereals | Cream of Wheat Instant | 74 |
| Breakfast and cereals | Grapenuts | 71 |
| Breakfast and cereals | Muesli | 43 |
| Breakfast and cereals | Oat Bran | 55 |
| Breakfast and cereals | Pancakes | 67 |
| Breakfast and cereals | Puffed Wheat | 67 |
| Breakfast and cereals | Quick (One Minute) Oats | 66 |
| Breakfast and cereals | Raisin Bran | 61 |
| Breakfast and cereals | Rice Krispies | 82 |
| Breakfast and cereals | Shredded Wheat | 75 |
| Breakfast and cereals | Special K | 69 |
| Breakfast and cereals | Waffles | 76 |
| Dairy | Ice cream, low fat | 43 |
| Dairy | Ice cream, premium | 38 |
| Dairy | Skim milk | 32 |
| Dairy | Whole milk | 31 |
| Dairy | Yogurt, artificially sweetened | 14 |
| Dairy | Yogurt, sweetened | 33 |
| Cookies | Butter | 47 |
| Cookies | Chocolate Chip | 44 |
| Cookies | Fudge | 57 |
| Cookies | Oatmeal | 55 |
| Cookies | Shortbread | 64 |
| Cookies | Vanilla Crème Filled Wafers | 50 |
| Snacks | Cashews | 22 |
| Snacks | Corn Chips | 63 |
| Snacks | Hummus | 6 |
| Snacks | Kudos Bar | 62 |
| Snacks | Jelly Beans | 78 |
| Snacks | M & M Peanut Candies | 33 |
| Snacks | Milk Chocolate | 43 |
| Snacks | Peanuts | 15 |
| Snacks | Popcorn | 72 |
| Snacks | Potato Chips | 57 |
| Snacks | Pretzels | 83 |
| Snacks | Walnuts | 15 |
| Juices | Apple | 40 |
| Juices | Cranberry Juice Cocktail | 68 |
| Juices | Grapefuit | 48 |
| Juices | Orange | 53 |
| Juices | Pineapple | 46 |
| Juices | Tomato | 38 |
Macronutrient Composition of Diet
| Source | Protein | Fat | Carbohydrate |
|---|---|---|---|
| North America [9] | 10–30 youth | 25–35 youth | 45–65 |
| 10–35 adults | 20–35 adults | 45–65 | |
| United Kingdom [10] | − | <35 | 50 |
| New Zealand and Australia [8] | 15–25 | 20–35 | 45–65 |
| World Health Organization [11] | 10–15 | 15–30 | 55–75 |
Reference:
- Venn BJ. Macronutrients and Human Health for the 21st Century. Nutrients. 2020 Aug 7;12(8):2363. doi: 10.3390/nu12082363. PMID: 32784664; PMCID: PMC7468865.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7468865/
The dietary recommendation for macronutrient diet composition for the prevention of chronic disease is:
- Carbs: 50%
- Fat: 20-35%
- Protein: 10-35%
Macronutrient Ranges edit
| Macronutrient | 1-3yo | 4-18yo | Adults |
|---|---|---|---|
| Fats | |||
| n-6 polyunsaturated fats | 30-40 | 25-35 | 20-35 |
| n-3 polyunsaturated fats | 5-10 | 5-10 | 5-10 |
| Carbohydrates | 45-65 | 45-65 | 45-65 |
| Protein | 5-20 | 10-30 | 10-35 |
| Macro's | Cal | Grams | Cal | Grams |
|---|---|---|---|---|
| Fats | 425. | 47.222222 | 765. | 225. |
| Carbohydrates | 765. | 225. | 1105. | 325. |
| Protein | 170. | 50. | 595. | 175. |
| 1700 | 1360. | 322.22222 | 2465. | 725. |
Grams per day
- Fats (25-45%): 55 - 100
- Carbohydrates (45-65%): 225 - 325
- Protein (10-35%): 50 - 175
- Fats (25%): 52 g (468 cal)
- Carbohydrates (40%): 190 g (760 cal)
- Protein (35%): 166 g (665 cal)
Reference:
- Institute of Medicine. 2006. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. Washington, DC: The National Academies Press. https://doi.org/10.17226/11537.
- https://nap.nationalacademies.org/catalog/11537/dietary-reference-intakes-the-essential-guide-to-nutrient-requirements
Mediterranean Diet edit
Mediterranean Diet Simplified
- Eat lots of vegetables. From a simple plate of sliced fresh tomatoes drizzled with olive oil and crumbled feta cheese to stunning salads, garlicky greens, fragrant soups and stews, healthy pizzas, or oven-roasted medleys, vegetables are vitally important to the fresh tastes and delicious flavors of the Med Diet.
- Change the way you think about meat. If you eat meat, have smaller amounts – small strips of sirloin in a vegetable sauté, or a dish of pasta garnished with diced prosciutto.
- Enjoy some dairy products. Eat Greek or plain yogurt, and try smaller amounts of a variety of cheeses.
- Eat seafood twice a week. Fish such as tuna, herring, salmon, and sardines are rich in omega-3 fatty acids, and shellfish including mussels, oysters, and clams have similar benefits for brain and heart health.
- Cook a vegetarian meal one night a week. Build meals around beans, whole grains, and vegetables, and heighten the flavor with fragrant herbs and spices. Down the road, try two nights per week.
- Use good fats. Include sources of healthy fats in daily meals, especially extra-virgin olive oil, nuts, peanuts, sunflower seeds, olives, and avocados.
- Switch to whole grains. Whole grains are naturally rich in many important nutrients; their fuller, nuttier taste and extra fiber keep you satisfied for hours. Cook traditional Mediterranean grains like bulgur, barley, farro and brown, black or red rice, and favor products made with whole grain flour.
- For dessert, eat fresh fruit. Choose from a wide range of delicious fresh fruits — from fresh figs and oranges to pomegranates, grapes and apples. Instead of daily ice cream or cookies, save sweets for a special treat or celebration.
Mediterranean Diet Principles
- Cook with Olive Oil
- Eat More Fish
- Eat Veggies All Day Long
- Help Yourself to Whole Grains
- Snack on Nuts
- Enjoy Fruit for Dessert
- Savor Every Bite
Mediterranean Diet Foods List
- Olive oil
- Fish, including canned and frozen fish
- Beans and lentils
- Fresh and frozen fruits and vegetables
- Herbs
- Whole grains, like oatmeal, quinoa, whole-wheat pasta and brown rice
- Red wine, in moderation
- Nuts, seeds and nut butters
- Eggs
- Fermented dairy, like kefir and nonfat plain Greek yogurt
Mediterranean Diet Principles AI version
The Mediterranean diet is a way of eating that emphasizes whole, unprocessed foods and is characterized by a high intake of fruits, vegetables, whole grains, and healthy fats, such as those found in olive oil. The diet is based on the traditional dietary patterns of countries bordering the Mediterranean Sea, including Greece, Italy, and Spain.
- Emphasis on whole foods: The Mediterranean diet focuses on whole, unprocessed foods, such as fruits, vegetables, whole grains, legumes, nuts, and seeds. These foods are rich in essential nutrients, fiber, and antioxidants.
- High intake of healthy fats: The Mediterranean diet is characterized by a high intake of healthy fats, such as those found in olive oil, avocados, and nuts. These fats are rich in monounsaturated and polyunsaturated fats, which can help lower cholesterol levels and reduce the risk of heart disease.
- Low intake of red meat: The Mediterranean diet recommends a low intake of red meat, which is high in saturated fat and cholesterol. Instead, lean protein sources, such as poultry, fish, and legumes, are emphasized.
- High intake of fruits and vegetables: Fruits and vegetables are a staple of the Mediterranean diet, and are consumed in abundance. A variety of colors and types are recommended to ensure a broad range of nutrients.
- Whole grains: Whole grains, such as brown rice, quinoa, and whole-wheat bread, are a key component of the Mediterranean diet. They provide fiber, vitamins, and minerals.
- Legumes: Legumes, such as lentils, chickpeas, and fava beans, are a good source of protein, fiber, and complex carbohydrates.
- Nuts and seeds: Nuts and seeds, such as almonds, walnuts, and pumpkin seeds, are a good source of healthy fats, protein, and fiber.
- Herbs and spices: Herbs and spices, such as oregano, thyme, and rosemary, are used to add flavor to dishes instead of salt and sugar.
- Red wine in moderation: Red wine is consumed in moderation as part of the Mediterranean diet, as it is believed to have health benefits when consumed in moderation.
- Emphasis on social eating: The Mediterranean diet is not just about food, but also about the social aspect of eating. Meals are often shared with family and friends, and are a time for socializing and relaxation.
Michi's Ladder of Healthy Food Choices edit
Michi's Ladder is a Diet Guideline
If you only ate from Tiers 1 & 2, you would have a near-perfect diet!
Consumption:
- Tier 1/2: Daily Intake
- Tier 3: Treats
- Tier 4/5: Special Occasions only
| Apples, with skin | Egg whites | Peppers |
| Artichokes | Endive | Plantains |
| Arugula | Fish, cold water (salmon, mackerel, sardines) | Prunes |
| Asparagus | Fish, freshwater | Radishes |
| Avocados | Flaxseed | Raspberries |
| Beans | Garlic, fresh | Refried beans, nonfat |
| Beets | Granola, raw, | Rice, brown |
| Bok choy | no sugar | Salsa, natural, no sugar |
| Boysenberries | Hemp seed | Seitan |
| Bran | Kale | Spinach |
| Broccoli | Lettuce, romaine, green or red leaf | Squash |
| Broccoli sprouts | Milk, nonfat | Strawberries |
| Brussels sprouts | Milk, soy | Sweet potatoes |
| Cabbage | Muesli, raw, | Tea, green or black |
| Carrots | no sugar | Tempeh |
| Cauliflower | Mushrooms | Tofu |
| Celery | Mustard | Tomato sauce, no sugar |
| Cereal, whole grain | Nectarines | Tomatoes |
| Chard | Oatmeal | Vinegar |
| Cherries | Olive oil | Water |
| Citrus fruits | Olives | Yams |
| Collard greens | Onions | Yogurt, nonfat, no sugar |
| Cottage cheese, nonfat | Pears, with skin | |
| Cucumbers | Peas |
| Apples, skinless | Milk, 1% |
| Bananas | Nuts, raw |
| Blueberries | Ostrich |
| Bread, whole grain | Pancakes, buckwheat |
| Cantaloupe | Papayas |
| Cheese, nonfat | Peaches |
| Chicken, skinless white meat | Pineapple |
| Coffee, black or cappuccino with nonfat milk | Plums |
| Corn | Raisins |
| Cottage cheese, low-fat | Ricotta cheese, nonfat |
| Cream cheese, nonfat | Soy nuts |
| Duck, free-range | Soy sauce |
| Eggplant | Squid |
| Fish, farmed | String beans |
| Granola or energy bar | Sunflower seeds |
| Grapes | Tortillas, whole wheat |
| Hummus | Turkey breast |
| Juice, fresh-squeezed with pulp, no sugar | Vegetable juice |
| Kiwifruit | Veggie burger |
| Mangoes | Venison, free-range |
| Meal replacement bar | Watermelon |
| Melon, honeydew | Zucchini |
| Yogurt, no sugar |
| A1 Steak Sauce | Lamb, lean |
| Angel food cake | Lettuce, iceberg |
| Applesauce | Lobster |
| Bagels | Mayonnaise |
| Beef, eye of round | Milk, 2% |
| Beef, London | Muesli |
| Beef, top round | Oatmeal, flavored |
| Canola oil | Oysters |
| Cheese, low-fat | Pancakes |
| Chicken, dark meat | Pasta, plain |
| Chicken sandwich, broiled | Peanut butter, raw |
| Chicken taco, baked | Popcorn, plain |
| Clams | Pork tenderloin |
| Coffee, cappuccino with whole milk | Potatoes, baked or boiled |
| Crab | Pretzels |
| Cream cheese, low-fat | Refried beans, low-fat |
| Eggs, whole | Rice cakes |
| French fries, baked | Rice, white |
| Fruit, dried | Sauerkraut |
| Graham crackers | Soup, canned broth |
| Granola | Steak, lean |
| Honey | Sweet-and-sour sauce |
| Jam or marmalade | Veal cutlet |
| Jerky, turkey | Wine, red |
| Juice, from concentrate | Yogurt, frozen, nonfat |
| Ketchup |
| Animal crackers | Macaroni and cheese |
| Beef, filet mignon | Margarine |
| Beef, lean ground | Meat loaf |
| Beef, sirloin | Mexican food |
| Beef Stroganoff | Milk, whole |
| Beer | Muffins |
| Bread, refined flour | Nuts, salted or roasted |
| Buffalo | Peanut butter, not raw |
| Butter | Pepper, stuffed |
| Caesar salad, with chicken | Pizza, meatless or Hawaiian style |
| Canadian bacon | Popcorn, with salt and butter |
| Cheese (including bleu and goat) | Pork chop |
| Chili | Potato salad or macaroni salad |
| Chinese food | Pudding, with low-fat milk |
| Chips, low-fat, baked | Reuben sandwich |
| Coconut | Sherbet |
| Coffee, iced mocha latte with nonfat milk | Shrimp |
| Coffee, latte with whole milk | Sloppy Joe, lean beef or turkey |
| Coffee cake | Soft drinks, diet |
| Crackers | Soup, canned creamy |
| Grilled cheese sandwich | Spaghetti, with meatballs |
| Ham | Sub sandwich |
| Hot dogs, turkey | Taco salad, with chicken |
| Ice cream, sugar-free or fat-free | Tortilla, refined flour or corn |
| Jell-O | Tuna salad or chicken salad |
| Juice, sweetened | Vegetable oil |
| Lamb chops | Wine, white |
| Lasagna, with meat | Yogurt, frozen |
| Alcohol, hard liquor | French fries |
| Bacon | Gravy |
| Baked beans | Hamburger, fast food |
| Beef, ground, regular | Hot dogs |
| Beef taco, fried | Ice cream |
| Breakfast sandwich, fast food | Jerky, beef, pork, or venison |
| Cakes | Juice, sugar added |
| Candy | Lobster Newburg |
| Cereal, sugared | Nachos |
| Chicken a la King | Onion rings |
| Chicken, buffalo wings or nuggets | Pastries |
| Chicken or fish sandwich, fried | Pies |
| Chips, potato or corn | Potato skins, fried |
| Chocolate | Potatoes, fried |
| Cinnamon bun | Potpie |
| Coffee, mocha, macchiato, ice blended, frappé, triple caramel vanilla buzz bomb, etc. | Refried beans, with lard |
| Cookies | Salad dressing, creamy |
| Cream cheese | Sausage |
| Creamed veggies | Soft drinks, sugared |
| Creamer, nondairy | Tater tots |
| Doughnuts | Toaster pastries |
Nutrition and Diet
3 commandments that cross over all types of weight-loss approaches:
- Eat more vegetables (fiber)
- They fill you up for very few calories, and they flood your body with the nutrients it needs
- Eat less sugar
- Whether you call it agave, cane juice, maple syrup, brown rice syrup, fruit juice concentrate, date sugar or any of the many names for added sugar
- Eat more whole foods
- Whole foods include fruits, vegetables, beans, nuts, seeds, whole grains, eggs, seafood, chicken
Strategies:
- Time-restricted feeding, or TRF - the approach is simple:
- Eat more or less what you want, but don't consume anything before or after the allotted time.
- Eat within a 8-10 hr window
Instead of Counting Calories
- Eat smaller portions
- One caveat: there's no reason to eat fewer vegetables; they're much less calorie dense than other foods (they contain fewer calories per gram).
- Choose foods that use more calories
- High-fiber, protein foods - might save about 12 to 15 calories per day, the same amount someone could expend by walking for about four minutes
- Consume the right kind of calories
- Nutrient-dense choices like fruit, vegetables, and whole grain
Reference:
Dining/Eating Out Strategies
Strategies for Eating Out
- Look at menu before you go and have a plan
- Choose a protein and vegetable combo
- If you have a starch, choose one with a lower Glycemic Index
- Immediately cut dish in half and ask for a box
- Do not feel like you need to clean your plate
- When you feel full, throw your napkin (or salt) on your left over food
- Drink water or unsweet tea
Optimizing foods for satiety edit
Highlights
- Foods high in protein and fiber are satiating.
- Sensory and cognitive signals generated during consumption are important for satiety.
- Satiety is moderated a combination of cognitive, sensory and physiological signals.
- Food products can be manipulated to enhance the consumer's experience of satiety.
Reference:
Patient Messaging: General Nutrition Information
Websites:
Evidence Based Recommendations:
- Fruits and Vegetables: 1/2 of every meal
- Whole grains: 1/4 of every meal
- Legumes and/or animal proteins: 1/4 of every meal
- Water: Primary beverage
- Nuts: Small handful daily
- Oils/fats: In moderation
- Salt: 2,500 mg daily
3 commandments that cross over all types of weight-loss approaches:
- Eat more vegetables
- They fill you up for very few calories, and they flood your body with the nutrients it needs
- Eat less sugar
- Whether you call it agave, cane juice, maple syrup, brown rice syrup, fruit juice concentrate, date sugar or any of the many names for added sugar
- Eat more whole foods
- Whole foods include fruits, vegetables, beans, nuts, seeds, whole grains, eggs, seafood, chicken
In general:
- Avoid added sugar
- Eat less refined grains
- Moderate protein
- Eat real unprocessed foods
Patient Messaging: Healthy food: 7 Affordable Ideas
- Brown Rice
- One serving of rice can cost you as little as 9 cents and is rich with B vitamins and other healthy nutrients
- Whole Chicken
- A pound of chicken averages at $1.28 per pound, and Moore says you can use this as your main protein source for meals
- Sweet Potatoes
- Sweet potatoes can go for about a dollar a pound if purchased in bulk.
- Use them to make sweet potato fries in the oven, mashed sweet potatoes or even roasted sweet potatoes
- Ground Turkey or Chicken
- Ground turkey can cost as little as 3 dollars and some change per pound and the options for meals are endless
- Beans
- A bag of dry beans, pinto, black, kidney or even lentils can give you 11 servings for about $1.39 or less.
- Rolled Oats
- You can get 13 servings of oats for about $2.50.
- Oatmeal doesn't just have to be a breakfast food either; you can make sweet and savory oats.
- Fruits and Vegetables
- Buy fruit and vegetables that are in season, as they will be cheaper than those that aren't.
- Picking up frozen fruits and veggies is also a great idea and just as healthy as the non-frozen kind.
Patient Messaging: Intermittent Fasting (IF)
There are several ways to do Intermittent Fasting (IF), and any fasting time frame between 10-16 hours is safe. I like the 16:8 IF (fast lasting 16 hours per day, with all foods consumption during the remaining 8 hours).
Common Eating Time Frames:
- 9 am to 5 pm
- 10 am to 6 pm
- 12 pm to 8 pm
While, people commonly do not do dietary restrictions during IF, I still recommend tracking your calories.
Patient Messaging: Portion control
4 Strategies for Portion Control:
- Use smaller plates. Folks will often eat what's placed in front of them, so using smaller dinnerware has been shown to help people eat less.[1]
- Drink a glass of water before your meal. If you chug a glass of water 30 minutes before you plan on eating, the H20 will take up some room in your stomach. This might help you eat less.[2]
- Take it slow. It can take about 20 minutes for your body to come around to the fact that it's full, so slowing down your meals can help you eat less.[3]
- Use a food journal. Recording everything you eat and drink is a great way to become aware of portions, which can help you control them.[4] In fact, one of the first missions we have Nerd Fitness Prime members complete is creating a food journal.
Focus your portion control strategy on:
- Protein
- A serving of protein is about the size and thickness of your palm
- Vegetables (technically carbs, but important enough to deserve their own category)
- A serving of veggies is about the size of your fist
- Carbohydrates (think starches and fruit)
- A serving of carbohydrates is about two hands cupped together
- Fat
- Here is a serving of fat, roughly the size of your thumb!
Food Portion Size (how much to eat at a time):
- Meat - 1 portion is size of deck of cards
- Rice, pasta, fruit - 1 portion is size of a fist
- Vegetables - 1 portion is size of a baseball
We've learned that using your hand as a guide is the most helpful strategy for portion control:
- You might not always have access to small plates.
- You might forget to drink water before each meal.
- You might have a short lunch break without the luxury of eating slowly.
- You might grow tired of logging all your food intake.
Make sure you get a proper serving of protein and vegetables every time you sit down to eat.
When it comes to portion control, we need to pay close attention to carbohydrates and fats, because this is where people have the tendency to overeat.
Portions
Simple Portion Guides
Use Your (not large) Plate as a Portion Guide:
- Vegetables or salad: Half a plate
- High-quality protein: Quarter of a plate (includes meat, poultry, fish, eggs, dairy, tofu, and beans)
- Complex carbs: Quarter of a plate (such as whole grains and starchy vegetables)
- High-fat foods: Half a tablespoon (7 grams) (including cheese, oils and butter)
Use Your Hands as a Serving Guide:
- Vegetables and salads: Fist-sized portion: 1 for women, 2 for men
- High-protein foods (such as meat, fish, poultry and beans): Palm-sized serving: 1 for women, 2 for men
- High-carb foods (such as whole grains and starchy vegetables): Cupped-hand portion: 1 for women, 2 for men
- High-fat foods (such as butter, oils and nuts): Thumb-sized portion: 1 for women, 2 for men
Here's a simple way to plan for portions:
- 1/2 Plate Vegetables: Fill half your plate with a colorful assortment of different vegetables
- 1/4 Plate Proteins: Bake, broil, or grill your way to a delicious and healthy meal.
- 1/4 Plate Starches: Whole-grain starches are good for your heart and keep you feeling fuller longer. Foods like yams, potatoes and corn (though considered vegetables), are high in starch and should be placed on this part of your plate.
Additional reference:
Portion controlled meal substitution diets work
Meal plan with portion controlled prepackaged food promotes greater weight and fat loss than standard self-selected diets.
Reference:
- Consultant July 2016
How can I manage portions when eating out?
Although it may be easier to manage your portions when you cook and eat at home, most people eat out from time to time—and some people eat out often. Try these tips to keep your food portions in check when you're away from home.
- Share a meal with a friend or take half your meal home.
- Avoid all-you-can-eat buffets. Instead, choose restaurants that offer some healthy food choices in controlled portions.
- Order one or two healthy appetizers or side dishes instead of a whole meal. Options include steamed or grilled—instead of fried—seafood or chicken, a salad with dressing on the side, or roasted vegetables.
- Ask to have the basket of bread or chips removed from the table.
- If you have a choice, pick the small-sized—rather than large-sized—drink, salad, or frozen yogurt.
- Look for calorie information next to food and drink items on menus and menu boards to understand how many calories are in a standard restaurant portion.
- Stop eating and drinking when you're full. Put down your fork and glass. Focus on enjoying the setting and company for the rest of the meal.
Reference:
How can I manage food portions at home?
You don't need to measure and count everything you eat or drink for the rest of your life. You may only want to do so long enough to learn typical serving and portion sizes. Try these tips to control portions at home.
- Take one serving according to the food label and eat it off a plate instead of straight out of the box or bag.
- Avoid eating in front of the TV, while driving or walking, or while you are busy with other activities.
- Focus on what you are eating, chew your food well, and fully enjoy the smell and taste of your food.
- Eat slowly so your brain has time to realize your stomach is full, which may take at least 15 minutes.
- Use smaller dishes, bowls, and glasses so you eat and drink less.
- Eat fewer high-fat, high-calorie foods, such as desserts, chips, sauces, and prepackaged snacks.
- Freeze food you won't serve or eat right away if you make too much. That way, you won't be tempted to finish the whole batch. If you freeze leftovers in single- or family-sized servings, you'll have ready-made meals for another day.
- Eat meals at regular times. Delaying meals or skipping meals altogether may cause you to overeat later in the day.
- Buy snacks, such as fruit or single-serving prepackaged foods that are lower in calories. If you buy bigger bags or boxes of snacks, divide the items into single-serving packages right away so you aren't tempted to overeat.
Reference:
Portion and Serving Sizes
Portions:
- 1/2 PLATE VEGETABLES:
- Fill half your plate with a colorful assortment of different vegetables
- 1/4 PLATE PROTEINS:
- Bake, broil, or grill your way to a delicious and healthy meal.
- 1/4 PLATE STARCHES:
- Whole-grain starches are good for your heart and keep you feeling fuller longer.
- Foods like yams, potatoes and corn (though considered vegetables), are high in starch and should be placed on this part of your plate
Servings:
- Basic Guidelines:
- 1 cup = baseball
- ½ cup = lightbulb
- 1 oz or 2 tbsp = golf ball
- 1 tbsp = poker chip
- 3 oz chicken or meat = deck of cards
- 3 oz fish = checkbook
- Grains:
- 1 cup of cereal flakes = baseball
- 1 pancake = compact disc
- ½ cup cooked rice = lightbulb
- ½ cup cooked pasta = lightbulb
- 1 slice bread = cassette tape
- 1 bagel = 6 oz can of tuna
- 3 cups popcorn = 3 baseballs
- Dairy and Cheese:
- 1 ½ oz cheese = 3 stacked dice
- 1 cup yogurt = baseball
- ½ cup of frozen yogurt = lightbulb
- ½ cup of ice cream = lightbulb
- Fats and Oils:
- 1 tbsp butter or spread = poker chip
- 1 tbsp salad dressing = poker chip
- 1 tbsp mayonnaise = poker chip
- 1 tbsp oil = poker chip
- Fruits and Vegetables:
- 1 medium fruit = baseball
- ½ cup grapes = about 16 grapes
- 1 cup strawberries = about 12 berries
- 1 cup of salad greens = baseball
- 1 cup carrots = about 12 baby carrots
- 1 cup cooked vegetables = baseball
- 1 baked potato = computer mouse
- Meats, Fish, and Nuts
- 3 oz lean meat = deck of cards
- 3 oz fish = checkbook
- 3 oz tofu = deck of cards
- 2 tbsp peanut butter = golf ball
- 2 tbsp hummus = golf ball
- ¼ cup almonds = 23 almonds
- ¼ cup pistachios = 24 pistachios
- Mixed dishes:
- 1 hamburger (without bun) = deck of cards
- 1 cup fries = about 10 fries
- 4 oz nachos = about 7 chips
- 3 oz meatloaf = deck of cards
- 1 cup chili = baseball
- 1 sub sandwich = about 6 inches
- 1 burrito = about 6 inches
Reference:
Serving Sizes for Fruits and Vegetables
- One large banana (about eight inches long) is equal to one serving of fruit.
- 100 calories
- 8 large strawberries will give you one day's serving of fruit.
- 50 calories
- 2 large plums count as one serving of fruit.
- 60 calories
- 32 grapes should count as one serving of fruit.
- 150 calories
- 1/2 cup of raisins is 1 serving of fruit.
- 200 calories
- 1 small apple (a little under three inches in diameter) counts as a serving of fruit.
- 75 calories
- 1 whole peach (just under three inches in diameter) also counts as a serving of fruits.
- 70 calories
- 1 cup of orange juice - eight ounces is a serving of fruit
- 120 calories
- 3 Broccoli Spears
- 30 calories
- 12 Baby Carrots
- 40 calories
- 1 Large Tomato
- 35 calories
- 1 Cup Vegetable Juice
- 1 Large Sweet Potato
- 125 calories
- 1 Large Ear of Corn
- 2 Large Celery Stalks
- 20 calories
- 2 Cups of Raw Greens
- 14 calories
- 1 Cup Cooked Greens
- 1 Large Red Pepper
Recommended Daily Allowance for Macronutrients
The Recommended Dietary Allowance (RDA) for macronutrients provides guidelines on the minimum amount of each macronutrient needed for healthy individuals. Here are the RDAs and Acceptable Macronutrient Distribution Ranges (AMDR) for macronutrients:
- Carbohydrates: The RDA for carbohydrates is 130 grams per day for children and adults, based on the average minimum amount of glucose used by the brain. The AMDR for carbohydrates is 45-65% of total daily calories.
- Protein: There is no specific RDA for protein, but the AMDR is 10-35% of total daily calories for adults. For children, the range is 5-20% for those aged 1-3 and 10-30% for those aged 4-18. The RDA for protein is at least 0.36 grams per pound (0.8 grams per kg) of body weight for adults.
- Fat: There is no RDA for total fat intake, but the AMDR is 20-35% of total daily calories for adults. For children, the AMDR varies by age, starting at 30-40% for those aged 1-3 and gradually approaching the adult range.
Recommended Nutrition For Muscle Injury
According to the American College of Sports Medicine, a high-protein diet is essential for muscle repair, with an intake of approximately 1.2-2.0 g/kg/day of protein being beneficial.[1]
During the initial phase of injury, it is crucial to maintain energy balance to prevent muscle atrophy. Higher protein intakes, around 2-2.5 g/kg/day, may be warranted during periods of immobilization to counteract muscle loss.[2] Additionally, omega-3 fatty acids and creatine supplementation show promising results in reducing muscle loss and enhancing muscle hypertrophy, respectively.[2-3]
Carbohydrate intake is also important to provide the necessary energy for recovery processes. A balanced diet rich in whole, minimally processed foods is recommended to ensure adequate intake of all essential nutrients.[2][4]
In summary, the key nutritional strategies for a torn muscle include:
- High protein intake: 1.2-2.5 g/kg/day depending on the phase of recovery.[2]
- Balanced energy intake: To prevent muscle atrophy and support recovery.[2][4]
- Omega-3 fatty acids and creatine: Potential supplements to enhance recovery.[2-3]
- Carbohydrates: To provide energy for recovery processes.[2][4]
Reference:
- Rodriguez NR, Di Marco NM, Langley S. American College of Sports Medicine Position Stand. Nutrition and Athletic Performance. Medicine and Science in Sports and Exercise. 2009;41(3):709-31. https://doi.org/10.1249/MSS.0b013e31890eb86.
- Tipton KD. Nutritional Support for Exercise-Induced Injuries. Sports Medicine (Auckland, N.Z.). 2015;45 Suppl 1:S93-104. https://doi.org/10.1007/s40279-015-0398-4.
- Giraldo-Vallejo JE, Cardona-Guzmán MÁ, Rodríguez-Alcivar EJ, et al. Nutritional Strategies in the Rehabilitation of Musculoskeletal Injuries in Athletes: A Systematic Integrative Review. Nutrients. 2023;15(4):819. https://doi.org/10.3390/nu15040819.
- Papadopoulou SK. Rehabilitation Nutrition for Injury Recovery of Athletes: The Role of Macronutrient Intake. Nutrients. 2020;12(8):E2449. https://doi.org/10.3390/nu12082449.
Renal Diet/Lifestyle
Ways to protect your kidneys:
- Manage blood pressure
- Goal is less than 130/80
- Low Sodium Intake
- Goal is less than 2300 mg/day
- Avoid foods that have more than 300mg sodium per serving
- Eat small portions of protein foods.
- Limit alcohol intake
- No more than 1-2 drinks per day
- Choose foods with less phosphorus
- Too much phosphorus in your blood pulls calcium from your bones, making your bones thin, weak, and more likely to break.
- Choose foods with less potassium
- Damaged kidneys allow potassium to build up in your blood, which can cause serious heart problems.
Ways to eat lower sodium:
- Buy fresh food often. Sodium (a part of salt) is added to many prepared or packaged foods you buy at the supermarket or at restaurants.
- Cook foods from scratch instead of eating prepared foods, "fast" foods, frozen dinners, and canned foods that are higher in sodium. When you prepare your own food, you control what goes into it.
- Use spices, herbs, and sodium-free seasonings in place of salt.
- Check for sodium on the Nutrition Facts label of food packages. A Daily Value of 20 percent or more means the food is high in sodium.
- Try lower-sodium versions of frozen dinners and other convenience foods.
- Rinse canned vegetables, beans, meats, and fish with water before eating.
Foods Lower in Phosphorus
- Fresh fruits and vegetables
- Breads, pasta, rice
- Rice milk (not enriched)
- Corn and rice cereals
- Light-colored sodas/pop, such as lemon-lime or homemade iced tea
Foods Lower in Potassium
- Apples, peaches
- Carrots, green beans
- White bread and pasta
- White rice
- Rice milk (not enriched)
- Cooked rice and wheat cereals, grits
- Apple, grape, or cranberry juice
Reference:
Study: Coffee and tea consumption and mortality from all causes, cardiovascular disease and cancer: a pooled analysis of prospective studies from the Asia Cohort Consortium
Background:
- Accumulating evidence suggests that consuming coffee may lower the risk of death, but evidence regarding tea consumption in Asians is limited. We examined the association between coffee and tea consumption and mortality in Asian populations.
Methods:
- We used data from 12 prospective cohort studies including 248 050 men and 280 454 women from the Asia Cohort Consortium conducted in China, Japan, Korea and Singapore. We estimated the study-specific association of coffee, green tea and black tea consumption with mortality using Cox proportional-hazards regression models and the pooled study-specific hazard ratios (HRs) using a random-effects model.
Results:
- In total, 94,744 deaths were identified during the follow-up, which ranged from an average of 6.5 to 22.7 years.
- Compared with coffee non-drinkers, men and women who drank at least five cups of coffee per day had a 24% [95% confidence interval (CI) 17%, 29%] and a 28% (95% CI 19%, 37%) lower risk of all-cause mortality, respectively.
- Similarly, we found inverse associations for coffee consumption with cardiovascular disease (CVD)-specific and cancer-specific mortality among both men and women.
- Green tea consumption was associated with lower risk of mortality from all causes, CVD and other causes but not from cancer.
- The association of drinking green tea with CVD-specific mortality was particularly strong, with HRs (95% CIs) of 0.79 (0.68, 0.91) for men and 0.78 (0.68, 0.90) for women who drank at least five cups per day of green tea compared with non-drinkers.
- The association between black tea consumption and mortality was weak, with no clear trends noted across the categories of consumption.
Conclusions:
- In Asian populations, coffee consumption is associated with a lower risk of death overall and with lower risks of death from CVD and cancer.
- Green tea consumption is associated with lower risks of death from all causes and CVD.
Reference:
- Shin S, Lee JE, Loftfield E, Shu XO, Abe SK, Rahman MS, Saito E, Islam MR, Tsugane S, Sawada N, Tsuji I, Kanemura S, Sugawara Y, Tomata Y, Sadakane A, Ozasa K, Oze I, Ito H, Shin MH, Ahn YO, Park SK, Shin A, Xiang YB, Cai H, Koh WP, Yuan JM, Yoo KY, Chia KS, Boffetta P, Ahsan H, Zheng W, Inoue M, Kang D, Potter JD, Matsuo K, Qiao YL, Rothman N, Sinha R. Coffee and tea consumption and mortality from all causes, cardiovascular disease and cancer: a pooled analysis of prospective studies from the Asia Cohort Consortium. Int J Epidemiol. 2022 May 9;51(2):626-640. doi: 10.1093/ije/dyab161. PMID: 34468722; PMCID: PMC9308394.
Study: Detox diets for toxin elimination and weight management: a critical review of the evidence
Abstract Detox diets are popular dieting strategies that claim to facilitate toxin elimination and weight loss, thereby promoting health and well-being. The present review examines whether detox diets are necessary, what they involve, whether they are effective and whether they present any dangers. Although the detox industry is booming, there is very little clinical evidence to support the use of these diets.
A handful of clinical studies have shown that commercial detox diets enhance liver detoxification and eliminate persistent organic pollutants from the body, although these studies are hampered by flawed methodologies and small sample sizes.
There is preliminary evidence to suggest that certain foods such as coriander, nori and olestra have detoxification properties, although the majority of these studies have been performed in animals.
To the best of our knowledge, no randomised controlled trials have been conducted to assess the effectiveness of commercial detox diets in humans. This is an area that deserves attention so that consumers can be informed of the potential benefits and risks of detox programmes.
Reference:
- Klein AV, Kiat H. Detox diets for toxin elimination and weight management: a critical review of the evidence. J Hum Nutr Diet. 2015 Dec;28(6):675-86. doi: 10.1111/jhn.12286. Epub 2014 Dec 18. PMID: 25522674.
Study: Dietary Sugar Intake and Incident Type 2 Diabetes Risk: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies
The dose-response relationship between dietary sugar and type 2 diabetes (T2D) risk is uncertain.
MEDLINE, Embase, CINAHL, Web of Science and Cochrane databases were searched through July 9, 2024 for prospective cohort studies reporting relative measures of incident T2D risk by categories of dietary sugar (total, free, added, fructose, sucrose) or 2 beverage sources (non-diet sugar-sweetened beverages [SSBs], fruit juice) in healthy adults.
Linear and restricted cubic spline dose-response models were fitted for each exposure, and study-specific slopes and confidence intervals (CIs) were calculated. Heterogeneity was evaluated using Q-statistics. Risk of bias was evaluated using the Risk of Bias in Non-randomized Studies of Exposures (ROBINS-E) tool. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was applied to assess the certainty of evidence.
Of 10,384 studies, 29 cohorts were included: SSB: 18 (n = 541,288); fruit juice: 14 (n = 490,413); sucrose: 7 (n = 223,238); total sugar: 4 (n = 109,858); fructose: 5 (n = 158,136); and added sugar: 2 (n = 31,004). Studies were conducted in Europe (13), United States (11), Asia (6), Australia (4), and Latin America (3).
Each additional serving of SSB and fruit juice was associated with a higher risk of T2D (risk ratio [RR]: 1.25; 95% CI: 1.17, 1.35 and RR: 1.05; 95% CI: >1.00, 1.11, respectively; moderate certainty).
In contrast, 20 g/d intakes of total sugar and sucrose were inversely associated with T2D (RR: 0.96; 95% CI: 0.94, 0.98; low certainty; and RR: 0.95; 95% CI: 0.91, <1.00; moderate certainty, respectively).
No associations were found for added sugar (RR: 0.99; 95% CI: 0.96, 1.01; low certainty) or fructose (RR: 0.98; 95% CI: 0.83, 1.15; very low certainty).
These findings suggest that dietary sugar consumed as a beverage (SSB and fruit juice) is associated with incident T2D risk. The results do not support the common assumption that dietary sugar (i.e., total sugar and sucrose), irrespective of type and amount, is consistently associated with increased T2D risk.
Reference:
- Karen A Della Corte, Tyler Bosler, Cole McClure, Anette E Buyken, James D LeCheminant, Lukas Schwingshackl, Dennis Della Corte, Dietary Sugar Intake and Incident Type 2 Diabetes Risk: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies, Advances in Nutrition, Volume 16, Issue 5, 2025, 100413, ISSN 2161-8313, https://doi.org/10.1016/j.advnut.2025.100413. (https://www.sciencedirect.com/science/article/pii/S2161831325000493)
Study: Effect of Calorie Restriction on Mood, Quality of Life, Sleep, and Sexual Function in Healthy Nonobese Adults: The CALERIE 2 Randomized Clinical Trial
Importance:
- Calorie restriction (CR) increases longevity in many species and reduces risk factors for chronic diseases. In humans, CR may improve health span, yet concerns remain about potential negative effects of CR.
Objective:
- To test the effect of CR on mood, quality of life (QOL), sleep, and sexual function in healthy nonobese adults.
Design, setting, and participants:
- A multisite randomized clinical trial (Comprehensive Assessment of Long-term Effects of Reducing Intake of Energy Phase 2 [CALERIE 2]) was conducted at 3 academic research institutions. Adult men and women (N = 220) with body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) of 22.0 to 28.0 were randomized to 2 years of 25% CR or an ad libitum (AL) control group in a 2:1 ratio favoring CR. Data were collected at baseline, 12 months, and 24 months and examined using intent-to-treat analysis. The study was conducted from January 22, 2007, to March 6, 2012. Data analysis was performed from July 18, 2012, to October 27, 2015.
Interventions:
- Two years of 25% CR or AL.
Main outcomes and measures:
- Self-report questionnaires were administered to measure mood (Beck Depression Inventory-II [BDI-II], score range 0-63, higher scores indicating worse mood, and Profile of Mood States [POMS], with a total mood disturbance score range of -32 to 200 and higher scores indicating higher levels of the constructs measured), QOL (Rand 36-Item Short Form, score range 0-100, higher scores reflecting better QOL, and Perceived Stress Scale, score range 0-40, higher scores indicating higher levels of stress), sleep (Pittsburgh Sleep Quality Index [PSQI], total score range 0-21, higher scores reflecting worse sleep quality), and sexual function (Derogatis Interview for Sexual Function-Self-report, total score range 24-188, higher scores indicating better sexual functioning).
Results:
- In all, 218 participants (152 women [69.7%]; mean [SD] age, 37.9 (7.2) years; mean [SD] BMI, 25.1 [1.6]) were included in the analyses.
- The CR and AL groups lost a mean (SE) of 7.6 (0.3) kg and 0.4 (0.5) kg, respectively, at month 24 (P < .001).
- Compared with the AL group, the CR group had significantly improved mood (BDI-II: between-group difference [BGD], -0.76; 95% CI, -1.41 to -0.11; effect size [ES], -0.35), reduced tension (POMS: BGD, -0.79; 95% CI, -1.38 to -0.19; ES, -0.39), and improved general health (BGD, 6.45; 95% CI, 3.93 to 8.98; ES, 0.75) and sexual drive and relationship (BGD, 1.06; 95% CI, 0.11 to 2.01; ES, 0.35) at month 24 as well as improved sleep duration at month 12 (BGD, -0.26; 95% CI, -0.49 to -0.02; ES, -0.32) (all P < .05).
- Greater percent weight loss in the CR group at month 24 was associated with increased vigor (Spearman correlation coefficient, ρ = -0.30) and less mood disturbance (ρ = 0.27) measured with the POMS, improved general health (ρ = -0.27) measured with the SF-36, and better sleep quality per the PSQI total score (ρ = 0.28) (all P < .01).
Conclusions and relevance:
- In nonobese adults, CR had some positive effects and no negative effects on health-related QOL.
Reference:
- Martin CK, Bhapkar M, Pittas AG, Pieper CF, Das SK, Williamson DA, Scott T, Redman LM, Stein R, Gilhooly CH, Stewart T, Robinson L, Roberts SB; Comprehensive Assessment of Long-term Effects of Reducing Intake of Energy (CALERIE) Phase 2 Study Group. Effect of Calorie Restriction on Mood, Quality of Life, Sleep, and Sexual Function in Healthy Nonobese Adults: The CALERIE 2 Randomized Clinical Trial. JAMA Intern Med. 2016 Jun 1;176(6):743-52. doi: 10.1001/jamainternmed.2016.1189. PMID: 27136347; PMCID: PMC4905696.
Study: Optimal dietary patterns for healthy aging
As the global population ages, it is critical to identify diets that, beyond preventing noncommunicable diseases, optimally promote healthy aging. Here, using longitudinal questionnaire data from the Nurses' Health Study (1986-2016) and the Health Professionals Follow-Up Study (1986-2016), we examined the association of long-term adherence to eight dietary patterns and ultraprocessed food consumption with healthy aging, as assessed according to measures of cognitive, physical and mental health, as well as living to 70 years of age free of chronic diseases.
After up to 30 years of follow-up, 9,771 (9.3%) of 105,015 participants (66% women, mean age = 53 years (s.d. = 8)) achieved healthy aging.
For each dietary pattern, higher adherence was associated with greater odds of healthy aging and its domains.
- The odds ratios for the highest quintile versus the lowest ranged from 1.45 (95% confidence interval (CI) = 1.35-1.57; healthful plant-based diet) to 1.86 (95% CI = 1.71-2.01; Alternative Healthy Eating Index).
- When the age threshold for healthy aging was shifted to 75 years, the Alternative Healthy Eating Index diet showed the strongest association with healthy aging, with an odds ratio of 2.24 (95% CI = 2.01-2.50).
- Higher intakes of fruits, vegetables, whole grains, unsaturated fats, nuts, legumes and low-fat dairy products were linked to greater odds of healthy aging, whereas higher intakes of trans fats, sodium, sugary beverages and red or processed meats (or both) were inversely associated.
Our findings suggest that dietary patterns rich in plant-based foods, with moderate inclusion of healthy animal-based foods, may enhance overall healthy aging, guiding future dietary guidelines.
Reference:
- Tessier AJ, Wang F, Korat AA, Eliassen AH, Chavarro J, Grodstein F, Li J, Liang L, Willett WC, Sun Q, Stampfer MJ, Hu FB, Guasch-Ferré M. Optimal dietary patterns for healthy aging. Nat Med. 2025 Mar 24. doi: 10.1038/s41591-025-03570-5. Epub ahead of print. PMID: 40128348.
Study: Salad and satiety: energy density and portion size of a first-course salad affect energy intake at lunch
Objective:
- We tested the effect on meal intake of varying the energy density and portion size of a compulsory first-course salad.
Design:
- The study used a randomized crossover design.
Subjects/setting:
- Forty-two women from the State College, PA, university community ate lunch in the laboratory once per week for 7 weeks.
Intervention:
- Lunch comprised one of six first-course salads, or no salad in the control condition, followed by a main course of pasta. Subjects were required to consume the entire salad, but ate as much pasta as they wanted. The salads varied in energy density (0.33, 0.67, or 1.33 kcal/g) and portion size (150 or 300 g). The energy density of the salad was reduced by changing the amount and type of dressing and cheese.
Main outcome measures:
- Energy intake and ratings of hunger, satiety, and food characteristics were measured.
Statistical analyses performed:
- Outcomes were analyzed using a linear mixed model with repeated measures.
Results:
- Compared with having no first course, consuming the low-energy-dense salads reduced meal energy intake (by 7% for the small portion and 12% for the large), and consuming the high-energy-dense salads increased intake (by 8% for the small portion and 17% for the large).
- When two salads with the same number of calories were compared, meal intake was decreased when the large portion of the lower-energy-dense salad was consumed.
Conclusions:
- Eating a low-energy-dense first course enhances satiety and reduces meal energy intake.
- Consuming a large portion of a low-energy-dense food at the start of a meal may be an effective strategy for weight management.
Reference:
- Rolls BJ, Roe LS, Meengs JS. Salad and satiety: energy density and portion size of a first-course salad affect energy intake at lunch. J Am Diet Assoc. 2004 Oct;104(10):1570-6. doi: 10.1016/j.jada.2004.07.001. PMID: 15389416.
Sugar
Avoid added sugars. Avoid foods with any of these in the first 3 ingredients:
- Sucrose
- Agave Nectar
- Evaporated Cane Juice
- High-Fructose Corn Syrup
- Corn Syrup
- Dextrose
- Honey
- Maple Syrup
- Malt Syrup
- Molasses
- Turbinado
Shop the perimeter of the grocery store to avoid foods highest in added sugars.
Reference:
- JAMA Vol 315 No 11 Mar 2016
Dangers of Added Sugar
Added Sugar:
- Every extra 150 calories of sugar (compared with identical 150 cal from fat or protein) increases the rate of DM 2 by 11x.
- This is independent of the persons weight and activity levels.
Reference:
- (Malhotra A, Noakes T, Phinney S. It is time to bust the myth of physical inactivity and obesity: you cannot outrun a bad diet. British J Sports Med. 2015 Apr.)
Sugar Sweetened Beverages
Daily consumption of 1-2 sugar sweetened beverages (SSB) is associated with:
- 26% increased rate of developing Diabetes Type 2
- 35% increased risk of MI or fatal heart disease
- 16% increased risk of CVA
Reference:
- (Consultant Nov 2015)
Glucose vs Fructose
Glucose vs Fructose:
- Glucose is absorbed directly in the blood stream.
- Fructose is metabolized in the liver and converted to triglycerides which can lead to fatty liver disease and insulin resistance.
Reference:
- (Consultant Nov 2015)
Vegetarian Diets
Types:
- Vegan (no animal products)
- Macrobiotics (whole grain, brown rice, fruits, vegetables; No white meat or fish to twice a week)
- Lacto vegetarian (allows milk products)
- Ovo vegetarian (allows eggs but no meat, dairy, or fish)
- Pescitarian (allows fish but no meats, dairy, or eggs)
- Semi-vegitarian (restrics meat)
Nutrients to Discuss:
- Protein
- Iron
- Calcium
- Vit B12
- Vit D
The recommended dietary allowance for protein is about 0.8 g/kg of bodyweight (or 0.36 g/lb)
- Equates to about 52 g of protein per day for a 145-lb woman and 65 g for a 180-lb man
The recommended daily allowances for protein are easily met by consuming a variety of whole plant foods, including a variety of minimally processed vegetables, fruits, whole grains, legumes, nuts, and seeds.
- One cup of cooked red lentils or black beans, for example, contains between 15 g and 18 g of protein
- A quarter cup of almonds contains about 7 g of protein and one cup of cooked oats has 5 g
OB/GYN
g#p#:
- TPAL
- T = term births (after 37 weeks gestation)
- P = premature births
- A = abortions
- L = living children
Advanced Lifesaving in Obstetrics (ALSO)
ALSO Abruption
Sher Classification
- Mild
- Moderate
- Severe
ALSO Biophysical Profile
- A reactive Nonstress Test
- Fetal breathing movements consisting of one or more episodes within 30 minutes and lasting 30 seconds or more
- Fetal movement consisting of three or more discrete body or limb movements within 30 minutes
- Fetal tone defined as one or more episodes of limb extension with return to flexion within 30 minutes
- Adequate amniotic fluid volume defined as one or more 1 cm or larger pockets of fluid two perpendicular planes.
- For each of the five components, a normal observation is given a score of 2 and an abnormal observation is given a score of 0.
- In the absence of oligohydramnios, a score of 8 or 10 is normal, 6 is equivocal, and a score of 4 or less is abnormal.
- It is important to note that falsely abnormal tests are more common in preterm fetus.
ALSO DIC
- No single clinical finding or lab test can confirm the diagnosis of DIC
Diagnosis is based on:
- Presence of underlying disease that predisposes to DIC
- Clinical findings suggestive of either bleeding or intravascular thrombosis (bruising, petechiae, oozing from needle puncture sites, mucosal surfaces, surgical incisions, or laceration repairs)
- Lab studies consistent with diagnosis
- Platelet <100,000 mm3
- Fibrinogen <300 mg/dL
- Fibrin split products >40 mg/dL
- PT >14 seconds
- PTT >40 seconds
- D-dimer = early indicator of DIC
ALSO FHR Monitoring
DR C Bravado
- DR - Determine the Risk:
- premature, IUGR, smoking, htn disease
- C - Contractions:
- frequency, strength, regular, association with progression.
- Hyperstim (now called tachy systole)= >7 in 15 min (or >6 in 10 minutes)
- Normal: less than or equal to 5 contractions per 10 minutes (averaged over 30 minutes)
- Tachysystole: greater than 5 contractions per 10 minutes (averaged over 30 minutes)
- Bra - Baseline RAte:
- normal 110-160
- mild bradycardia 100-110
- mod-severe bradycardia <100
- severe bradycardia?<80
- tachycardia >160 (premature, anemia, etc)
- >180+fever=chorio
- >200=fetal arrhythmia
- V - Variability:
- Minimal0-5 BPM
- moderate6-25
- marked>25
- normal= 10-15 over baseline
- A - Accelerations
- normal = 15 bpm for 15 seconds
- D - Decelerations
- Early: begin & end with contractions, fall from baseline <60 bpm and rarely go <100 bpm
- Variable: rapid, with a sharp decent & recovery
- Are present in 50-80% of labors during 2nd stage
- Benign if "shoulders" & good baseline variability
- Mild >80 bpm for <30 sec
- Mod 70-80 bpm, 30-60 sec
- Severe <70 bpm, >60 sec
- Kubli's Ceritia for varible decels
- FHT <30 sec 30-60 sec>60 sec
- >80mildmildmild
- 70-80mildmodmod
- <70mildmodsevere
- Late: begin after contraction
- Watch out for subtle, shallow late decelerations with poor baseline varibility
- O - Overall assessment
- Reassuring vs Nonreassuring
Category I – "Normal" ALL of following:
- Baseline FHR: 110-160
- Baseline FHR variability; moderate
- Late or variable decelerations: absent
- Early decelerations: present or absent
- Accelerations: present or absent
Category II – "Indeterminate"
- Everything between Cat I and III
Category III – "Abnormal" include EITHER
- Absent baseline FHR variability AND any of the following:
- Recurrent late decelerations
- Recurrent variable decelerations
- Bradycardia
- Or: Sinusoidal pattern
Things to do to address
- Materal Position change
- Oxygen 6-10 liters/min
- IV Fluid bolus
- Vaginal exam (cord, scalp stim, dilation, pH sam)
- Pitocin off
- Terbutaline 0.25 mg subcutaneously
- Amnio-infusion (meconium, variable deceleration, oligohydramnios)
Scalp pH
- >7.25 normal
- 7.20-25 border low
- <7.2 abnormal
ALSO Forceps Application
- A - Anesthia
- B - Bladder empty
- C - Cervix fully dilated
- D - Determine position of head / think Dystocia, and prepare for Shoulder Dystocia
- E - Equipment check
- F - Forceps ready - Position For Safety
- P - Posterior fontanelle <1cm above
- F - Fennestration - only fingertip
- S - Sutures - Sagittal suture midline Lambdoidal suture above and equidistant from superior surface of blade
- G - Gentle traction
- H - Handles elevated in J curve (Pajot's Maneuver)
- I - Incision / Episiotomy
- J - remove forceps when Jaw visible
ALSO Postpartum Hemorrhage
4T's:
- T - Tissue (retained placenta)
- T - Trauma (vaginal,cervical,uterine)
- T - Tone (Pitocin, Methergine, Hemobate)
- T - Thrombin (clotting deficiency)
Don't forget BLS and ATLS protocals:
- ABC's
- 2 Large bore IV's
- Blood-Type / Screen 2 to 4 units
- Clotting studies
ALSO Preterm Contractions
Cervical thinning via U/S premature labor</=25mm
+FFN (Fetal fibrinectin) >/=50 ng/ml (24-28 weeks) -> substantial risk of spontaneous preterm labor
Treatment of Bacterial Vaginosis with Flagyl & Erythromycin reduces risk of preterm labor. Tx with Flagyl alone does not decrease risk.
Treatment:
- Terbutaline 0.25 mg subcutaneously q 1-4 hours prn contractions & safe maternal heart rate.
- Procardia 10-20 mg po q6h or q8h
Magnesium sulfate
- Load 4-6 grams over 20 minutes
- Continuous infusion: 2-3 grams/hour
Corticosteriods
- Betamethasone 12 mg IM x2, 24 hours apart
- Dexamethasone 6 mg IM x4, 12 hours apart
ALSO Shoulder Dystocia
HELPERRR
- H - call for Help
- E Evaluate for Episiotomy
- L Legs back (McRobert's maneuver)
- P external, suprapubic Pressure
- E Enter vagina - pressure behind
- Posterior aspect of Anterior Shoulder
- R Remove posterior arm
- R Roll to hands / knees (Gaskin Maneuver); deliver posterior shoulder
- R Replace head in uterus / C-section Zavanelli Manueuver
ALSO Ultrasound (Limited)
- L - Lie (Longitudinal, Tranverse)/ Living (FHT)
- M - Masses / Fetal Movements
- N - Number (Single vs Twin)
- O - Occupant (Anatomic Survey)
- P - Placenta / Presentation (Vtx, Breech, Face) / Position (ROA, LOA)
- Q - Quantity (Amniotic Fluid Index)
Age:
- Add 6.5 to CRL in cm=GA in weeks
Cervical length
- Starting @ 16 wks for those with hx of LEEP & continuing q2wks until 24 wks.
- IF at 24 wks the cervical length is <3.5 cm, continue q2wk measurements until 32 wks & transition to fetal fibronectin from there
AFI:
- Oligohydramniosis = AFI <5
- Polyhydramniosis = AFI >20
- Equivical=AFI 5-8 (repeat in 1-2 days)
ALSO Vacuum Extractor
- A - Anesthesia
- B - Bladder empty
- C - Cervix fully dilated
- D - Determine position, Think Dystocia, and plan for Shoulder Dystocia
- E - Equipment check
- F - Fontanelle - Apply cup near posterior Fontanelle / check for maternal tissue
- G - Gentle traction
- H - Halt:
- Halt between contractions;
- Halt if cup disengages 3 times or no progess in 3 pulls, or not delivered in 30 minutes
- I - evaluate for Incision
- J - remove when Jaw is visible
Breast Cancer Risk Tool
- Excellent tool developed by National Cancer Institute to estimate a woman's risk of developing invasive breast cancer.
- Great way to educate women about their specific and individual risk of cancer relative to other women their age.
Reference:
Nordic Cochrane Mammogram Leaflet
Courtesy of Dr. Guthrie, from Nordic Cochrane Group:
Summary:
- If 2000 women are screened regularly for 10 years, 1 will benefit from screening, as she will avoid dying from breast cancer because the screening detected the cancer earlier.
- If 2000 women are screened regularly for 10 years, 10 healthy women will be turned into cancer patients and will be treated unnecessarily.
- If 2000 women are screened regularly for 10 years, about 200 healthy women will experience a false alarm.
Reference:
Breast Exam edit
- Inspection
- Abnormalities in the overall shape of the breasts
- Changes in skin color
- Skin dimpling / retractions
- Spontaneous nipple discharge
- Palpation
- Shape: the most common benign lesions, like a cyst or a fibroadenoma, have very regular borders while cancerous nodules tend almost always to be irregular in shape
- Consistency: a mass that feels rock hard or otherwise very firm is probably malignant, while a rubbery or elastic consistency is typical of a benign lesion
- Relation to the skin: a lesion that is very fixed to skin is usually malignant
- Changes over time: rapid changes of a lesion over weeks to months raise suspicion for cancer
- Tenderness: cancerous nodules tend to be nontender, while benign lesions are often particularly tender. A mass that changes in tenderness during the menstrual cycle is most likely benign
- Document any masses: size, shape, texture, mobility, delimitation, tenderness, and approximate depth
- Lymph Node Exam
- Document number, size, texture, mobility, and delimitation of any palpable lymph nodes
Documentation:
- Symmetrical or asymmetrical
- Shape (ptotic, pendulous, any scars or deformities with descriptions)
- Texture (soft, nodular, fibrocystic, dense, presence of inframammary ridge in large breasts)
- Masses (described as indicated above versus no masses evident)
- Absent
- Present: size, consistency, distance from areolar edge, clock position
- Nipple-areolar complex (pink, brown, everted, inverted, discharge present/absent with description, presence of dry, scaly texture concerning for Paget's disease)
- Skin (warm, dry, presence/absence of erythema, edema, peau d'orange appearance, open sores, draining fluid collections)
- Symmetrical or asymmetrical
- Shape:
- ptotic
- pendulous
- any scars or deformities with descriptions
- Texture:
- soft
- nodular
- fibrocystic
- dense
- presence of inframammary ridge in large breasts
- Masses:
- Absent
- Present: size, consistency, distance from areolar edge, clock position
- Nipple-areolar complex:
- pink, brown
- everted, inverted
- discharge present/absent with description
- presence of dry, scaly texture concerning for Paget's disease
- Skin:
- warm
- dry
- presence/absence of erythema, edema, peau d'orange appearance, open sores, draining fluid collections
Reference:
- https://meded.ucsd.edu/clinicalmed/breast.html
- Henderson JA, Duffee D, Ferguson T. Breast Examination Techniques. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459179/
- https://stanfordmedicine25.stanford.edu/the25/BreastExam.html
Breastfeeding
Health risks for mothers who do not breastfeed:
- Breast ca
- Diabetes Mellitus
- Hyperlipidemia
- Hypertension
- Myocardial infarction
- Obesity
- Ovarian ca
References:
- AFP Vol 91 No 9 May 2015
Cervical Disease
Notes:
- Do not perform cervical cytoloty or HPV in immunocompetent women <21yo
- Do not perform screening for cervical ca in low risk women 65+ yo or women with total hysterectomy for benign disease
Timing:
- Normal cervix -> HPV-infected cervix (8-24 months)
- HPV-infected cervix -> Precancer -> Cervical cancer (10-20 years)
Risk Factors for Cervical Squamous Cell Carcinoma
- Number of sex partners
- 2-5 - RR 2.00(95% CI 1.91-2.09)
- 6+ - RR 2.98(95% CI 2.62-3.40)
- Age at first intercourse <18yo
- RR 2.24(95% CI 2.11-2.38)
- Number of full-term pregnancies
- 1-2 - RR 1.00(95% CI 0.94-1.07)
- 3-4 - RR 1.50(95% CI 1.43-1.59)
- 5+ - RR 2.08(95% CI 1.95-2.23)
- Age at first parity
- 17-19 - RR 2.16(95% CI 2.03-2.30)
- <17 - RR 2.72(95% CI 2.42-3.05)
- Current smoker
- RR 1.50(95% CI 1.38-1.63)
- Other
- Black or hispanic race
- OCP over 5yrs
- H/o STD
- Immunosuppression
- Low socioeconomic status
- Family history
HPV Genotypes
- High risk
- Type 16
- Causes 50% of all squamous cell carcinomas of the cervix and 55%-60% of all cervical cancers worldwide
- Type 18
- Causes 20% of cervical adenocarcinomas
- Other (31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68)
- All types combined cause 25% of cervical cancers
- Type 16
- Low risk (wart causing)
- Types 6, 11
- Cause 90-95% of anogenital warts
- Types 6, 11
References:
- AFP Vol 97 No 7 Apr 2018
Chronic Pelvic Pain
- Chronic pelvic pain is most often associated with endometriosis, bladder pain syndrome, or both but also shares the multifactorial aspects of other chronic pain syndromes.
- Neuromuscular pain conditions are common in chronic pelvic pain and can be diagnosed with palpation for pelvic floor muscle tenderness and with the FABER and Carnett tests for sources outside the pelvic floor.
- Pelvic floor physical therapy and trigger point injections can both improve vaginal pain and dyspareunia from neuromuscular chronic pelvic pain.
- Surgical interventions appear to offer no benefit in chronic pelvic pain.
Guideline:
- Available at: https://journals.lww.com/greenjournal/Abstract/2020/03000/Chronic_Pelvic_Pain__ACOG_Practice_Bulletin,.48.aspx
References:
- AFP Feb 2021 Vol 103 No 3
Colposcope Prediction: REID Index
Colposcopic prediction of histologic diagnosis using the Reid Colposcopic Index (RCI)
| Colposcopic signs | Zero point | One point | Two points |
|---|---|---|---|
| Colour | Low-intensity acetowhitening (not completely opaque) | Intermediate shade | Dull, opaque, oyster white |
| Indistinct acetowhitening | - grey/white colour and shiny surface | Grey | |
| Transparent or translucent acetowhitening | (most lesions should be scored in this category) | ||
| Acetowhitening beyond the margin of the transformation zonePure snow-white colour with intense surface shine | |||
| Lesion margin and surface configuration | Microcondylomatous or micropapillary contour | Regular-shaped, symmetrical lesions with smooth, straight outlines | Rolled, peeling edges |
| Flat lesions with indistinct margins | Internal demarcations between areas of differing colposcopic appearance | ||
| Feathered or finely scalloped margins | - a central area of high-grade change and peripheral area of low-grade change | ||
| Angular, jagged lesions | |||
| Satellite lesions beyond the margin of the transformation zone | |||
| Vessels | Fine/uniform-calibre vessels - closely and uniformly placed | Absent vessels | Well defined coarse punctation or mosaic, sharply demarcated |
| Poorly formed patterns of fine punctation and/or mosaic | - and randomly and widely placed | ||
| Vessels beyond the margin of the transformation zone | |||
| Fine vessels within microcondylomatous or micropapillary lesions | |||
| Iodine staining | Positive iodine uptake giving mahogany-brown color | Partial iodine uptake - variegated, speckled appearance | Negative iodine uptake of significant lesion |
| Negative uptake of insignificant lesion | - i.e., yellow staining by a lesion already scoring 4+ on the first 3 criteria | ||
| - i.e., yellow staining by a lesion scoring 3 points or less on the first 3 criteria | |||
| Areas beyond the margin of the transformation zone, conspicuous on colposcopy, evident as iodine-negative areas | |||
| - such areas are frequently due to parakeratosis |
| RCI (overall score) | Histology |
|---|---|
| 0 - 2 | Likely to be CIN 1 |
| 3 - 4 | Overlapping lesion: likely to be CIN 1 or CIN 2 |
| 5 - 8 | Likely to be CIN 2-3 |
References:
Contraindications to vaginal delivery
- Active HSV or prodromal symptoms
- Certain malpresentations
- Complete placenta previa
- Previsou vertical uterine incision or transfundal uterine surgery
- Mother does not wnat VBAC
Dysmenorrhea
Combined OCPs (SOR A)
- Combined oral contraceptives reduce pain associated with primary dysmenorrhea compared with placebo (standardized mean difference [SMD] = −0.58; 95% CI, −0.74 to −0.41).
- Increase the risk of any adverse effects when compared with placebo (number needed to harm [NNH] = 5; 95% CI, 4 to 8)
Combined OCPs vs Placebo
- Benefits
- 1:6 had less pain
- 1:7 had reduced use of additional pain medications (analgesics)
- 1:8 had fewer absences from work or school
- Harms:
- 1:5 had an increase in any adverse event
- 1:3 had increased irregular bleeding
- 1:11 had headaches
- 1:16 had nausea
Low-dose combined continuous OCP vs low dose combined standard OCPs
- Harms
- 1:13 had an increase in any adverse event
- 1:8 had an increase in irregular bleeding
Reference:
- AFP Vol 109 No 6 Jun 2024
Dyspareunia
Causes:
- Superficial:
- Atrophy
- Condylomas
- Infectious lesions
- Provoked vestibulodynia
- Trauma
- Vulvodynia
- Vulvovaginitis
- Deep:
- Adenomyosis
- Endometriosis
- High-tone pelvic floor dysfunction
- Interstitial cystitis
- Irritable bowel syndrome
- Pelvic adhesive disease
- Pelvic congestion syndrome
- Pelvic inflammatory disease
- Sexual abuse history
- Uterine leiomyomas
- Uterine retroversion
- Other generalized pain disorders
References:
- JFP Vol 66 No 12 Dec 2017
EAB
Abortion in Florida
State Abortion Restrictions (2022):
- A patient must receive state-directed counseling that includes information designed to discourage the patient from having an abortion, and then wait 24hours before the procedure is provided. Counseling must be provided in person and must take place before the waiting period begins, thereby necessitating two trips to the facility.
- Health plans offered in the state's health exchange under the Affordable Care Act can only cover abortion in cases of life endangerment, rape or incest, unless individuals purchase an optional rider at an additional cost.
- The parent of a minor must be notified before an abortion can take place.
- Public funding is available for abortion only in cases of life endangerment, rape or incest.
- A woman must undergo an ultrasound before obtaining an abortion and must be given the option to view the image.
- An abortion cannot be performed at or after 24 weeks from the last menstrual period unless the mother's life or health is endangered.
| Reason | Total | 1st Trimester | 2nd Trimester | 3rd Trimester |
|---|---|---|---|---|
| Elective Abortion | 59257 | 56409 | 2848 | 0 |
| Abortion Performed due to Social or Economic Reasons | 16983 | 15687 | 1296 | 0 |
| Abortion Performed due to Emotional/Psychological Health of the Mother | 1505 | 1392 | 113 | 0 |
| Abortion Performed due to Physical Health of Mother that is not Life Endangering | 1070 | 999 | 71 | 0 |
| Abortion Performed due to a Life Endangering Physical Condition | 119 | 98 | 21 | 0 |
| Abortion Performed due to Serious Fetal Genetic Defect, Deformity or Abnormality | 757 | 273 | 484 | 0 |
| Abortion Performed due to Incest | 8 | 5 | 3 | 0 |
| Abortion Performed due to Rape | 118 | 104 | 3 | 0 |
| Florida Totals: | 79817 | 74967 | 4850 | 0 |
| 2020 | 2017 | 2014 | 2011 | 2008 | 2005 |
| 77,400 | 71,050 | 75,990 | 84,990 | 94,360 | 92,300 |
| 2020 | 2017 | 2014 | 2011 | 2008 | 2005 | |
| FL | 19.7 | 18.6 | 20.6 | 23.7 | 27.2 | 26.8 |
| U.S. | 14.4 | 13.5 | 14.6 | 16.9 | 19.4 | 19.4 |
For 2020: 8.3% of all U.S. abortions occurred in Florida
Who chooses?
- The demographic characteristic most associated with the decision to terminate an unintended pregnancy is marital status (in 2007, 84% of all abortions were performed on unmarried women). (28)
- Women living with a partner to whom they are not married account for 25% of abortions but only about 10% of women in the population. (29)
- The highest abortion rate, 40 abortions per 1,000 women in the age-group, occurred among women aged 20 to 24 years. (28)
- The percentage of teenagers' unintended pregnancies terminated by abortion (about 40%) was lower than that among US women generally (48%). (26)
- The (abortion) rate among Black women is more than four times as high (as White women). (29)
- (The abortion rate) of Hispanic women lies between that of Black and White women. (29)
- The abortion rate of women with Medicaid coverage is three times as high as that of other women. (30)
- The abortion rate of non-metropolitan women is about half that of women who live in metropolitan counties. (32)
- More than 23% of US abortions occur in California (roughly 12% of the US population lives in California). (136)
- Women seeking abortion are generally young and healthy. (252)
- Most women choose abortion for reasons other than threat to maternal health. (78)
- One per cent (of aborting women) reported that they were the survivors of rape. (28)
- In 2004, 47% of US women obtaining abortions had had a prior induced abortion. (27)
- Women who terminate a pregnancy differ from those who do not in ways that affect reproductive health. For example, they are more likely to smoke and (more likely) to be exposed to sexually transmitted infections [because they've had a] greater number of sexual partners, (and an) earlier age at first sex… (253)
Women of races other than White are more than twice as likely to die from induced abortion (in the US). About one-fifth of the excess mortality risk among minority-race women is because of their later gestational age at the time of abortion.
Florida Abortions (2020):
- Ages:
- women ages 20 to 24: 27%
- women ages 25 to 29: 29%
- women ages 30-39: 33%
- women ages 40 and older: 4%
- Races
- white women: 47%
- black women: 37%
- Florida's black abortion rate was 33.4 abortions per 1,000 women of childbearing age (almost 3x the white rate)
- other races: 9%
- unknown race: 6%, and six percent were on women of unknown race.
- Ethnicity
- Hispanic women: 27%
- non-Hispanic women: 67%
- unreported ethnicity: 6%
- Marriage
- married women: 13%
- unmarried women: 73%
- unknown: 14%while 14 percent were obtained by women whose marital status was not reported.
- Previous birth status
- no previous live births: 37%
- women with one live birth: 25%
- women with two or more live births: 37%
- Prior abortion
- No prior abortions: 56%
- 1 abortion: 25%
- more than one previous abortion: 19%
- Method
- chemical: 56%
- curettage procedures: 40%
- a different or unreported method: 4%
- hysterotomy or hysterectomy: 6 abortions
- Dates
- six weeks post-fertilization or earlier: 75%
- between seven and eight weeks: 12%
- between nine and 10 weeks: 5%
- between 11 and 12 weeks: 3%
- between 13 and 14 weeks: 2%
- between 15 and 17 weeks: 1%
- at 18 weeks post-fertilization or later: 1.2% (923 abortions)
- Reason
- elective: 75%
- for social or economic reasons: 20%
- for the mother's emotional or psychological health: 2%
- for the mother's physical health: 1.5%
- because the unborn baby had an abnormality: 1%
- because of risk to the mother's life: 0.2% (146 abortions)
- due to rape: 0.1% (112 abortions)
- due to incest: 9 abortions
- 7 babies were reported to have been born alive during abortions in Florida in 2020. The report does not include information about these babies' outcomes.
Resources:
References:
Study: Abortion, substance abuse and mental health in early adulthood: Thirteen-year longitudinal evidence from the United States
Objective
- To examine the links between pregnancy outcomes (birth, abortion, or involuntary pregnancy loss) and mental health outcomes for US women during the transition into adulthood to determine the extent of increased risk, if any, associated with exposure to induced abortion.
Method
- Panel data on pregnancy history and mental health history for a nationally representative cohort of 8005 women at (average) ages 15, 22, and 28 years from the National Longitudinal Study of Adolescent to Adult Health were examined for risk of depression, anxiety, suicidal ideation, alcohol abuse, drug abuse, cannabis abuse, and nicotine dependence by pregnancy outcome (birth, abortion, and involuntary pregnancy loss). Risk ratios were estimated for time-dynamic outcomes from population-averaged longitudinal logistic and Poisson regression models.
Results
- After extensive adjustment for confounding, other pregnancy outcomes, and sociodemographic differences, abortion was consistently associated with increased risk of mental health disorder.
- Overall risk was elevated 45% (risk ratio, 1.45; 95% confidence interval, 1.30-1.62; p < 0.0001).
- Risk of mental health disorder with pregnancy loss was mixed, but also elevated 24% (risk ratio, 1.24; 95% confidence interval, 1.13-1.37; p < 0.0001) overall.
- Birth was weakly associated with reduced mental disorders.
- One-eleventh (8.7%; 95% confidence interval, 6.0-11.3) of the prevalence of mental disorders examined over the period were attributable to abortion.
Conclusion
- Evidence from the United States confirms previous findings from Norway and New Zealand that, unlike other pregnancy outcomes, abortion is consistently associated with a moderate increase in risk of mental health disorders during late adolescence and early adulthood.
Reference:
- Sullins DP. Abortion, substance abuse and mental health in early adulthood: Thirteen-year longitudinal evidence from the United States. SAGE Open Med. 2016 Sep 23;4:2050312116665997. doi: 10.1177/2050312116665997. PMID: 27781096; PMCID: PMC5066584.
Study: Emotions over five years after denial of abortion in the United States: Contextualizing the effects of abortion denial on women's health and lives
Background:
- The Turnaway Study was the first to follow women denied abortions because of state law or facility policy over five years. The study has found negative effects on women's socioeconomic status, physical health, and on their children's wellbeing.
- However, women did not suffer lasting mental health consequences, prompting questions about the effects of denial on women's emotions.
Methods:
- In this mixed methods study, we used quantitative and qualitative interview data from the Turnaway Study to offer insight into these findings.
- We surveyed 161 women who were denied abortions at 30 facilities across the United States between 2008 and 2010 one week after the abortion denial and semiannually over five years.
- Mixed-effects regression analyses examined emotions about having been denied the abortion over time. To contextualize the quantitative findings, we draw on in-depth qualitative interviews with 15 participants, conducted in 2014-2015, for their accounts of their emotions and feelings over time.
Results:
- Survey participants reported both negative and positive emotions about the abortion denial one week after.
- Emotions became significantly less negative and more positive over their pregnancy and after childbirth.
- In multivariable models, lower social support, more difficulty deciding to seek abortion, and placing the baby for adoption were associated with reporting more negative emotions.
- Interviews revealed how, for some, belief in antiabortion narratives contributed to initial positive emotions.
- Subsequent positive life events and bonding with the child also led to positive retrospective evaluations of the denial.
Conclusions:
- Findings of emergent positive emotions about having been denied an abortion suggest that individuals are able to cope emotionally with an abortion denial, although evidence that policies leading to abortion denial cause significant health and socioeconomic harms remains.
Reference:
- Rocca CH, Moseson H, Gould H, Foster DG, Kimport K. Emotions over five years after denial of abortion in the United States: Contextualizing the effects of abortion denial on women's health and lives. Soc Sci Med. 2021 Jan;269:113567. doi: 10.1016/j.socscimed.2020.113567. Epub 2020 Nov 29. PMID: 33309441.
- https://pubmed.ncbi.nlm.nih.gov/33309441/
Study: Global prevalence of post-abortion depression: systematic review and Meta-analysis
Background:
- Depression after abortion is a common problem for all women of reproductive age. However, there are not any data on post-abortion depression at a global level. Consequently, the purpose of this study was to find out the global prevalence of post-abortion depression.
Methods
- The present study involved a comprehensive search of several databases, including Science Direct, Scopus, EMBSE, Google Scholar, and PubMed. The search was conducted between February 1, 2023, and March 10, 2023. The data was extracted using Microsoft Excel (version 14) and analyzed using STATA statistical software. To evaluate publication bias, a forest plot, Begg's test, and Egger's test were employed. Heterogeneity was assessed using I2, and a pooled estimated analysis was conducted. Additionally, subgroup analysis was performed based on the study continent/region, World Bank income group, screening instrument, and study design.
Results
- This analysis included 15 papers with a total of 18,207 research participants out of a total of 657 articles. The overall pooled prevalence of post-abortion depression was found to be 34.5% (95% CI 23.34, 45.68), with an I2 value of 71.6%. The prevalence of post-abortion depression varied based on geographic location, World Health Organization (WHO) regions, World Bank income category, screening approach, and study design. The highest proportion of post-abortion depression was observed in Asia (37.5%), while the WHO's Eastern Mediterranean region had the greatest rate of post-abortion depression (43.1%). Lower-middle-income countries had the highest frequency of post-abortion depression (42.91%) based on World Bank economic classification. The Center of Epidemiological Studies Depression Scale was found to have the highest incidence of reported depression prevalence (30%) across diagnostic tools. Furthermore, the prevalence of depression was higher in cross-sectional study designs (36.42%) compared to cohort studies (22.7%).
Conclusion
- In conclusion, the occurrence of post-abortion depression has been observed to be widespread globally. The prevalence of post-abortion is found to be influenced by several factors, including the methodology employed in the study, the diagnostic tool utilized, the geographical location, and the socioeconomic status of the population. Healthcare providers should prioritize the provision of post-abortion counseling, care, and emotional support to women.
Reference:
- Gebeyehu NA, Tegegne KD, Abebe K, Asefa Y, Assfaw BB, Adella GA, Alemu BW, Sewyew DA. Global prevalence of post-abortion depression: systematic review and Meta-analysis. BMC Psychiatry. 2023 Oct 26;23(1):786. doi: 10.1186/s12888-023-05278-7. PMID: 37884930; PMCID: PMC10605843.
Study: Perceived stress and emotional social support among women who are denied or receive abortions in the United States: a prospective cohort study edit
Background:
- Examining women's stress and social support following denial and receipt of abortion furthers understanding of the effects of unwanted childbearing and abortion on women's well-being. This study investigated perceived stress and emotional social support over time among women who were denied wanted abortions and who received abortions, and compared outcomes between the groups.
Methods:
- The Turnaway Study is a prospective cohort study of women who sought abortions at 30 abortion facilities across the United States, and follows women via semiannual phone interviews for five years.
- Participants include 956 English or Spanish speaking women aged 15 and over who sought abortions between 2008 and 2010 and whose gestation in pregnancy fit one of three groups: women who presented up to three weeks beyond a facility's gestational age limit and were denied an abortion; women presenting within two weeks below the limit who received an abortion; and women who received a first trimester abortion.
- The outcomes were modified versions of the Perceived Stress Scale and the Multidimensional Scale of Perceived Social Support. Longitudinal mixed effects models were used to assess differences in outcomes between study groups over 30 months.
Results:
- Women denied abortions initially had higher perceived stress than women receiving abortions near gestational age limits (1.0 unit difference on 0-16 scale, P = 0.003).
- Women receiving first-trimester abortions initially had lower perceived stress than women receiving abortions near gestational age limits (0.6 difference, P = 0.045).
- By six months, all groups' levels of perceived stress were similar, and levels remained similar through 30 months.
- Emotional social support scores did not differ among women receiving abortions near gestational limits versus women denied abortions or women having first trimester abortions initially or over time.
Conclusions:
- Soon after being denied abortions, women experienced higher perceived stress than women who received abortions.
- The study found no longer-term differences in perceived stress or emotional social support between women who received versus were denied abortions.
Reference:
- Harris LF, Roberts SC, Biggs MA, Rocca CH, Foster DG. Perceived stress and emotional social support among women who are denied or receive abortions in the United States: a prospective cohort study. BMC Womens Health. 2014 Jun 19;14:76. doi: 10.1186/1472-6874-14-76. PMID: 24946971; PMCID: PMC4080695.
- https://pubmed.ncbi.nlm.nih.gov/24946971/
Study: Socioeconomic Outcomes of Women Who Receive and Women Who Are Denied Wanted Abortions in the United States edit
Objectives:
- To determine the socioeconomic consequences of receipt versus denial of abortion.
Methods:
- Women who presented for abortion just before or after the gestational age limit of 30 abortion facilities across the United States between 2008 and 2010 were recruited and followed for 5 years via semiannual telephone interviews. Using mixed effects models, we evaluated socioeconomic outcomes for 813 women by receipt or denial of abortion care.
Results:
- In analyses that adjusted for the few baseline differences, women denied abortions who gave birth had higher odds of poverty 6 months after denial (adjusted odds ratio [AOR] = 3.77; P < .001) than did women who received abortions; women denied abortions were also more likely to be in poverty for 4 years after denial of abortion. Six months after denial of abortion, women were less likely to be employed full time (AOR = 0.37; P = .001) and were more likely to receive public assistance (AOR = 6.26; P < .001) than were women who obtained abortions, differences that remained significant for 4 years.
Conclusions:
- Women denied an abortion were more likely than were women who received an abortion to experience economic hardship and insecurity lasting years.
- Laws that restrict access to abortion may result in worsened economic outcomes for women [ for 4 years, but lose significant difference by 5 years ].
Reference:
- Foster DG, Biggs MA, Ralph L, Gerdts C, Roberts S, Glymour MM. Socioeconomic Outcomes of Women Who Receive and Women Who Are Denied Wanted Abortions in the United States. Am J Public Health. 2018 Mar;108(3):407-413. doi: 10.2105/AJPH.2017.304247. Epub 2018 Jan 18. PMID: 29345993; PMCID: PMC5803812.
- https://pubmed.ncbi.nlm.nih.gov/29345993/
Study: Suicide risks associated with pregnancy outcomes: a national cross-sectional survey of American females 41-45 years of age
Objective
- Numerous studies have linked abortion to an elevated risk of suicide. One hypothesis is that this association is entirely incidental and most likely fully explained by preexisting mental illness. This hypothesis can be tested by examining women's own self-assessments of the degree, if any, that abortion and other pregnancy outcomes contributed to suicidal thoughts and behaviors.
Methods
- A topic blind survey was distributed to 2829 American females 41-45 years of age. Respondents were asked about any history of attempted suicide(s) and reproductive histories. Grouped by reproductive history, respondents were then asked to rank on visual analog scales the degree, if any, to which their pregnancy outcome contributed to suicidal thoughts, self-destructive behaviors, and any attempted suicides.
Results
- Aborting women were twice as likely to have attempted suicide compared to other women.
- Aborting women, especially those who underwent coerced or unwanted abortions, were significantly more likely to say their pregnancy outcomes directly contributed to suicidal thoughts and behaviors compared to women in all other groups.
Conclusions
- The hypothesis that higher rates of suicide following abortion can be entirely explained by preexisting mental health problems is inconsistent with women's own self-assessments of the degree their abortions directly contributed to suicidal and self-destructive behaviors.
Reference:
- Reardon DC. Suicide risks associated with pregnancy outcomes: a national cross-sectional survey of American females 41-45 years of age. J Psychosom Obstet Gynaecol. 2025 Dec;46(1):2455086. doi: 10.1080/0167482X.2025.2455086. Epub 2025 Jan 21. PMID: 39838528.
Endometrial Biopsy
Endometrial biopsy should be performed for patients with abnormal uterine bleeding who are 45 years or older and in younger patients with a significant history of unopposed estrogen exposure, persistent bleeding, or in whom medical management is ineffective. Patients with postmenopausal bleeding but no risk factors for endometrial hyperplasia or cancer may have transvaginal ultrasonography or endometrial biopsy as a first-line approach to evaluation.
Reference:
- AFP Jun 2021 Vol 103 No 12
- https://www.aafp.org/afp/2020/0501/p551.html
Endometrial Thickness
Normal endometrial thickness
- Premenopausal
- Immediately postmenses: Homogenous 1-4 mm
- Proliferative: Triple-layer structure 7-10 mm
- Luteal phase: Hyperechogenic 8-16 mm (>18 mm thickness suggests endometrial disease)
- Postmenopausal: <5 mm (>10 mm thickness strongly suggests endometrial cancer)
Fetal Monitoring
| Category | Description |
|---|---|
| 1 | Normal baselien (110-160bpm), mod variability, no variable or late decelerations |
| 2 | Anything not category 1 or 3 |
| 3 | Absent variability with recurrent variable decelss, recurrent late decels or bradycardia, or sinusoidal pattern |
GDM
3hr 100g oral GTT criteria (diagnosis when 2+ meet or exceed cutoff values):
- Fasting =/> 95mg/dL
- 1hr =/> 180mg/dL
- 2hr =/> 155mg/dL
- 3hr =/> 140mg/dL
If the fasting is >125 automatically GDM
Glucose treatment goals:
- Fasting: <96mg/dL
- 1h pp: <140mg/dL
- 2h pp: <120-127mg/dL
Insulin management:
- Typically started as 0.7units/Kg per pre-pregnancy weight
- Given in divided doses
- 2/3 insulin in AM (2/3 NPH and 1/3 Regular)
- 1/3 insulin before dinner (1:1 NPH:Regular)
Possible Oral Agents:
- Glyburide
- Metformin
References:
- FP Essentials #358
- AFP Vol 80 No 1 Jul 2009
HCG Levels During Pregnancy
| Length of pregnancy | Average hCG levels in blood during pregnancy |
|---|---|
| 4 weeks | 0 - 750 µ/L |
| 5 weeks | 200 - 7,000 µ/L |
| 6 weeks | 200 - 32,000 µ/L |
| 7 weeks | 3,000 - 160,000 µ/L |
| 8 - 12 weeks | 32,000 - 210,000 µ/L |
| 13 - 16 weeks | 9,000 - 210,000 µ/L |
| 16 - 29 weeks (second trimester) | 1,400 - 53,000 µ/L |
| 29 - 41 weeks (third trimester) | 940 - 60,000 µ/L |
Reference:
Hormonal Contraceptives
Initiate of OCPs
- Initiation — OCs can be started anytime during the cycle.
- They prefer the quick start method in which the woman begins taking OCs on the day that she is given the prescription, as long as pregnancy is reasonably excluded.
- An alternative is the Sunday start approach where the woman starts the pill on the first Sunday after her period begins (because most pill packs are arranged for a Sunday start to avoid withdrawal bleeding on a weekend).
- Some form of back-up contraception is needed for the first seven days of use if one chooses the quick or Sunday start methods because the full contraceptive effect might not be provided immediately.
- The US Selected Practice Recommendations for Contraceptive Use suggests that if the pill is started >5 days after the onset of menses, back-up contraception should be used for the first seven days
Reference:
- UpToDate
Oral Contraceptives:
- Progestin mg / Estrogen (mcg)
- Combination extended cycle
- Levonorgestrel/ethinyl estradiol
- Seasonale (0.15/30)
- Seasonique (0.15/30, -/10)
- Levonorgestrel/ethinyl estradiol
- Combination monophasic
- Norethindrone/ethinyl estradiol
- Lo Loestrin Fe (1/10, -/10)
- Microgestin 1/20
- Necon (0.5/35)
- Necon (1/35)
- Ortho-Novum 1/35
- Ethynodiol diacetate/ethinyl estradiol
- Zovia (1/35)
- Zovia (1/50)
- Desogestrel/ethinyl estradiol
- Desogen (0.15/30)
- Drospirenone/ethinyl estradiol
- Yasmin (3/30)
- Yaz (3/20)
- Norgestimate/ethinyl estradiol
- Ortho-Cyclen (0.25/35)
- Sprintec (0.25/35)
- Norethindrone/ethinyl estradiol
- Combination biphasic
- Necon 10/11 (0.5/35, 1/35)
- Combination triphasic
- Desogestrel/ethinyl estradiol
- Cyclessa (0.1/25, 0.125/25, 0.15/25)
- Norethindrone/ethinyl estradiol
- Ortho-Novum 7/7/7 (0.5/35, 0.75/35, 1/35)
- Norgestimate/ethinyl estradiol
- Ortho Tri-Cyclen Lo (0.18/25, 0.215/25, 0.25/25)
- Levonorgestrel/ethinyl estradiol
- Trivora (0.05/30, 0.075/40, 0.125/30)
- Desogestrel/ethinyl estradiol
- Combination extended cycle
- Progestin-only
- Camila (0.35)
- Errin (0.35)
- Jolivette (0.35)
- Ortho Micronor (0.35)
Which methods to avoid in whom
| Those with: | Avoid: |
|---|---|
| Uterine cavity anatomic abnormalities | IUD |
| Breast Ca | All hormonal contraceptives |
| Breastfeeding <6mo postpartum | Combined OCP, Ortho Evra, Nuvaring |
| Cardiovascular disease risk factors | Combined OCP, Ortho Evra, Nuvaring |
| Cervical Ca (untreated) | IUD initiation (can continue if already placed) |
| Chlamydia, gonorrhea, or current purulent cervicitis | IUD initiation (can continue if already placed) |
| Cirrhosis (severe) | Combined OCP, Ortho Evra, Nuvaring |
| DVT | Combined OCP, Ortho Evra, Nuvaring |
| DM with organ damage | Combined OCP, Ortho Evra, Nuvaring |
| Endometrial Ca | IUD initiation (can continue if already placed) |
| Gestational trophoblastic disease | IUD |
| Hepatocellular adenoma or carcinoma | Combined OCP, Ortho Evra, Nuvaring |
| SBP >160 mmHg or DBP >100 mmHg | Combined OCP, Ortho Evra, Nuvaring |
| Ischemic heart disease | Combined OCP, Ortho Evra, Nuvaring |
| Leimomyomas with uterine cavity distortion | IUD |
| Major surgery with prolonged immobilization | Combined OCP, Ortho Evra, Nuvaring |
| Migraine with aura | Combined OCP, Ortho Evra, Nuvaring |
| Migraine without aura in >35yo | Ortho Evra, Nuvaring (can continue OCP if in use) |
| Pelvic inflammatory disease | Initiation of IUD |
| Postpartum sepsis | IUD |
| Septic abortion | IUD |
| Smoking >15cig/d in >35yo | Combined OCP, Ortho Evra, Nuvaring |
| Stroke | Combined OCP, Ortho Evra, Nuvaring |
| Systemic lupus erythematosus with + or ? antibodies | Combined OCP, Ortho Evra, Nuvaring |
| Thrombotic mutations (factor V l=Leiden, prothrombin | Combined OCP, Ortho Evra, Nuvaring |
| protein C, protein S, or antitrhombin deficiencies) | |
| Tuberculosis with pelvic involvement | Initiation of IUD |
| Unexplained vaginal bleeding before evaluation | IUD |
| Valvular heart disease | Combined OCP, Ortho Evra, Nuvaring |
| Viral hepatitis (acute or flare) | Initiation of Combined OCP, Ortho Evra, Nuvaring |
| (can continue if in use) |
Reference:
- AFP Vol 82 No 12 Dec 2010
Management of Adverse Effects of Hormonal Contraceptives
- Combined Oral Contraceptives
- Adverse effect: Breakthrough bleeding
- Treatment:
- Reassurance - cycle will likely resolve in 3 to 5 cycles
- Increase estrogen dose if less than 20mcg per day
- Treatment:
- Adverse effect: Decreased libido
- Treatment:
- Reassurance
- Consider increasing estrogen dose if current dose is very low
- Consider 10mcg estrogen during placebo week if patient is perimenopausal
- Look for alternative reasons for decreased libido
- Treatment:
- Adverse effect: Depressed mood
- Treatment:
- Reassure mood changes will improve with time
- Treatment:
- Adverse effect: Headache
- Treatment:
- Discontinue if headache is migraine with aura
- Reassure patient headache will likely resolve after the first few cycles
- If HA is during placebo week in a patient over 40yo, add 10mcg ethinyl estradiol per day during 5 days of placebo week
- Treatment:
- Adverse effect: Weight gain
- Treatment:
- Combined oral contraceptives are not associated with weight gain
- Consider lifestyle factors that may be causing weight gain
- Treatment:
- Adverse effect: Breakthrough bleeding
- Combined Oral Contraceptives (Extended Cycle)
- Adverse effect: Breakthrough bleeding
- Treatment:
- Reassurance - cycle will likely diminish by month 4
- Consider hormone-free interval of 3 to 4 days beginning on the 1st day of breakthrough bleeding
- Consider changing progestin from levonorgestrel to norethindrone
- Treatment:
- Adverse effect: Breakthrough bleeding
- Depo-Provera
- Adverse effect: Acne
- Treatment:
- Consider changing to combined method
- Treatment:
- Adverse effect: Amenorrhea
- Treatment:
- Reassurance
- Treatment:
- Adverse effect: Hirsutism
- Treatment:
- Consider changing to combined method
- Treatment:
- Adverse effect: Weight gain
- Treatment:
- Careful adherence to diet and exercise regimen
- Treatment:
- Adverse effect: Acne
- Emergency contraceptive regimens
- Adverse effect: Nausea
- Treatment:
- Metoclopramide 10mg or meclizine 50mg 1hr before taking emergency contraceptive
- Use progestin only emergency contraceptive
- Treatment:
- Adverse effect: Nausea
- Implanon
- Adverse effect: Breakthrough bleeding (single episode)
- Treatment:
- Mifepristone 25mg twice a day then ehinyl estradiol one 10mg tablet twice a day for 4 days, beginning onthe first doy of bleeding
- Treatment:
- Adverse effect: Breakthrough bleeding (continuous)
- Treatment:
- No treatment is effective
- Consider changing contraceptive method
- Treatment:
- Adverse effect: Heavy menses
- Treatment:
- Reassurance - but unclear if it will improve over time
- Change method if persistent
- Treatment:
- Adverse effect: Breakthrough bleeding (single episode)
- Nuvaring (standard use)
- Adverse effect: Increased vaginal discharge
- Treatment:
- Reassurance - discharge usually does not mean pathology
- Consider changing to nonvaginal contraceptive
- Treatment:
- Adverse effect: Increased vaginal discharge
- Nuvaring (continuous use)
- Adverse effect: Breakthrough bleeding
- Treatment:
- Remove the ring for 4 dyas at the start of the bleeding, then replace for remainder of month
- Treatment:
- Adverse effect: Breakthrough bleeding
- Ortho Evra Patch
- Adverse effect: Breast tenderness
- Treatment:
- Consider changing to a combined oral contraceptive
- Treatment:
- Adverse effect: Breast tenderness
- Progestin-only Pills
- Adverse effect: Acne
- Treatment:
- Change to a combined oral contraceptive if able
- Treatment:
- Adverse effect: Breakthrough bleeding
- Treatment:
- Change to a combined oral contraceptive if able
- Treatment:
- Adverse effect: Hirsutism
- Treatment:
- Change to a combined oral contraceptive if able
- Treatment:
- Adverse effect: Acne
Reference:
- AFP Vol 82 No 12 Dec 2010
Hysterectomy Types
- Simple/extrafascial
- Uterus is removed with cervix, but without parametria or vagina (class I)
- Modified radical
- Uterus is removed with the cervix, parametria and upper 25% of vagina (class II)
- Radical
- Uterus is removed with the cervix and:
- Additional parametria and upper 50% of vagina (class III)
- Upper 75% of vagina (class IV)
- Additional resection of a portion of the bladder (class V)
- Uterus is removed with the cervix and:
References:
- AFP Vol 97 No 7 Apr 2018
Infertility
See also: Infertility (Male)
Workup after 12 mo of infertility:
- Male evaluation:
- Semen analysis
- Female evaluation:
- Evaluate ovulation (day 21 progesterone level)
- If <5ng/mL -> evaluate for cause
- TSH, prolactin, FSH, estradiol -> Treat underlying cause
- Consider Clomid
- If 5ng/mL or more -> indicates ovulation
- Assess for tubal patency, uterine abnormalities (hysterosalpingography or laparoscopy)
Indicators of Diminished Ovarian Reserve
- Antimullerian hormone <1.0 ng per mL
- Antral follicle count <5-7
- Follicle stimulating hormone >10 mIU per mL
References:
- AFP Vol 91, No 5 Mar 2015
Infertility Work-Up in PCP Office
The following tests are useful in most couples with infertility:
- Male:
- H/P
- Sexual developmental history, including testicular descent, pubertal development, loss of body hair, or decrease in shaving frequency
- Chronic severe systemic illness and history of major head or pelvic trauma
- Infections, such as mumps orchitis, sinopulmonary symptoms, sexually transmitted infections, and genitourinary tract infections (including prostatitis)
- Surgical procedures involving the inguinal and scrotal areas, such as vasectomy or orchiectomy
- Drugs and environmental exposures, including alcohol, tobacco, marijuana, opioids, radiation therapy, anabolic steroids, corticosteroids, cytotoxic chemotherapy (current or past), drugs that cause hyperprolactinemia, and exposure to toxic chemicals (eg, pesticides)
- Sexual history, including libido, frequency of intercourse, and previous fertility assessments of the man and his partner
- Semen analysis to assess male factors
- Endocrine testing (In low sperm count)
- Low testosterone, and high FSH and LH – Primary (hypergonadotropic) hypogonadism (affecting both spermatogenesis and Leydig cell function). These men should have a karyotype performed. (See 'Chromosomal anomalies' below.)
- Normal testosterone and LH, and high FSH – Primary (hypergonadotropic) hypogonadism (seminiferous tubule damage without Leydig cell dysfunction). (See "Causes of male infertility", section on 'Primary testicular defects in spermatogenesis'.)
- Low testosterone, but FSH and LH not elevated (normal or low) – Secondary (hypogonadotropic) hypogonadism. Serum prolactin should be measured in men with a low serum testosterone concentration and normal to low serum LH. Some men may need additional evaluation for a sellar mass and secondary hypothyroidism and hypoadrenalism. (See "Clinical features and diagnosis of male hypogonadism".)
- High testosterone and LH, but normal FSH – Partial androgen resistance. (See "Pathogenesis and clinical features of disorders of androgen action".)
- Normal testosterone, LH, and FSH – Further evaluation depends upon findings on semen analysis (eg, azoospermia, oligozoospermia, asthenozoospermia, or teratozoospermia). (See "Treatments for male infertility", section on 'Normal serum T, normal LH and FSH'.)
- Men with normal endocrine testing who also have azoospermia should be evaluated for ejaculatory duct obstruction. (See "Treatments for male infertility", section on 'Obstruction of epididymis or ejaculatory duct'.)
- Most infertile men who have normal serum testosterone concentrations, normal serum gonadotropin concentrations, and a primary defect in spermatogenesis have sperm in the ejaculate, but the numbers of sperm with normal motility and/or normal morphology are low. Clinicians may consider infertile men with oligozoospermia and normal serum hormones in the same category as men with idiopathic infertility (ie, men with normal semen analyses and normal serum hormones). There is no clearly effective medical therapy for these men. Strategies include continuation of attempts at natural conception or ART. (See "Treatments for male infertility", section on 'Assisted reproductive technologies'.)
- Low sperm count and very low LH in a man who is very muscular – Suspicious for androgen abuse.
- H/P
- Female:
- H/P
- Duration of infertility and results of previous evaluation and therapy.
- Menstrual history (cycle length and characteristics), which helps in determining ovulatory status. For example, regular monthly cycles with molimina (breast tenderness, ovulatory pain, bloating) suggest that the patient is ovulatory, and characteristics such as severe dysmenorrhea suggest endometriosis. Menstrual cycle length may also be a general indicator of ovarian reserve. A meta-analysis including over 12,000 females reported that short menstrual cycle length (21 to 27 days) was associated with reduced ovarian reserve, including lower anti-müllerian hormone levels and antral follicle counts, compared with normal (28 to 31 days) and long (32 to 35 days) cycle lengths [3].
- If cycles not clear - Ovulation is most easily documented by a mid-luteal phase serum progesterone level, which should be obtained approximately one week before the expected menses. For a typical 28-day cycle, the test would be obtained on day 21. A progesterone level >3 ng/mL is evidence of recent ovulation [6].
- If the mid-luteal progesterone concentration is <3 ng/mL, the patient is evaluated for causes of anovulation. The minimal work-up includes serum prolactin, thyroid-stimulating hormone (TSH), FSH, and assessment for polycystic ovary syndrome (PCOS).
- Medical, surgical, and gynecologic history (including sexually transmitted infections, pelvic inflammatory disease, and treatment of abnormal Pap smears) to look for conditions, procedures, or medications potentially associated with infertility. At a minimum, the review of systems should determine whether the patient has symptoms of thyroid disease, galactorrhea, hirsutism, pelvic or abdominal pain, dysmenorrhea, or dyspareunia. Young women who have undergone unilateral oophorectomy generally do not have reduced fertility since young women have many primordial follicles per ovary; however, prior unilateral oophorectomy may impact fertility in older women as they may develop diminished ovarian reserve sooner than women with two ovaries [4].
- Obstetric history to assess for events potentially associated with subsequent infertility or adverse outcome in a future pregnancy.
- Sexual history, including sexual dysfunction and frequency of coitus. Infrequent or ineffective coitus can be an explanation for infertility.
- Family history, including family members with infertility, birth defects, genetic mutations, or intellectual disability. Women with fragile X premutation may develop premature ovarian failure, while males may have learning problems, developmental delay, or autistic features.
- Personal and lifestyle history including age, occupation, exercise, stress, dieting/changes in weight, smoking, and alcohol use, all of which can affect fertility.
- Menstrual history, assessment of luteinizing hormone surge in urine prior to ovulation, and/or luteal phase progesterone level to assess ovulatory function.
- Hysterosalpingogram or sonohysterogram with a test of tubal patency such as hysterosalpingo-contrast-sonography to assess tubal patency and the uterine cavity.
- Assessment of ovarian reserve with day 3 serum follicle-stimulating hormone and estradiol levels, anti-müllerian hormone, and/or antral follicle count.
- Thyroid-stimulating hormone.
- H/P
In select couples, the following additional tests may be warranted:
- Pelvic ultrasound to assess for uterine myomas and ovarian cysts.
- Laparoscopy to identify endometriosis or other pelvic pathology.
Infertility Workup
- Evaluate for clinical evidence of ovulation
- Regular menstrual cycles
- Premenstrual symptoms
- If NO clinical evidence of ovulation
- Evaluate for ovulatory dysfunction
- Check labs
- TSH
- Prolactin
- FSH
- LH
- PCOS testing indicated in women with irregular menses or symptoms of hyperandrogenism
- Treat underlying causes
- Consider ovulation induction x3 cycles
- After treatment of hypothyroidism or hyperprolactinoma if indicated
- Evaluate for ovulatory dysfunction
- If clinical evidence of ovulation
- Ovarian reserve testing
- Evaluate for tubal patency
- Hysterosalpingogram
- Evaluate for uterine anatomic abnormalities
- Transvaginal US or Sonohysterography as indicated
- Evaluate quality and quantity of partner's sperm
- Evaluate and treat underlying causes
- Assess need for surgical correction for uterine anatomic abnormalities or tubal obstruction
- Further male testing as indicated
- In women >40yo
- After treatment for above conditions, consider ovulation induction and intrauterine insemination x3 cycles or immediate in vitro fertilization
- Unclear ovulation history
- Serum progesterone on day 21 of menstrual cycle
- Progesterone <3 ng/mL
- Evaluate as ovulatory infertility (anovulation)
- Progesterone >=3 ng/mL
- Evaluate for other causes of infertility
- Serum progesterone on day 21 of menstrual cycle
References:
- JAMA Jul 2021 Vol 326 No 1
Ovarian Reserve
See also:
Testing ovarian reserve
Normal AMH values often exceed:
- 2 ng/mL at 30 yo
- 1.5 ng/mL at 35 yo
- 1 ng/mL at 40 yo
Rates of miscarriage are approximately:
- 12% in women aged 20 to 29 years
- 25% by 40 years
- 40% by 43 years
- 65% in females 45 years and older
Cumulative live birth rates:
- 28.1% in women with AMH levels of 0.91 - <1 ng/mL
- 10.9% in women with AMH < 0.10 ng/mL
When considering both age and AMH, cumulative live birth rates:
- 22% - 41% for women younger than 35 years
- 1% - 4% for women older than 42 years
Reference:
- Seifer DB, Feinberg EC, Hsu AL. Ovarian Aging and Fertility. JAMA. 2024;332(20):1750–1751. https://doi.org/10.1001/jama.2024.18207
- Deadmond A, Koch CA, Parry JP. Ovarian Reserve Testing. [Updated 2022 Dec 21]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279058/
IUD and Depression/Anxiety edit
Study: Levonorgestrel intrauterine device and depression: A Swedish register-based cohort study
Background: The levonorgestrel intrauterine device (LNG-IUD) is traditionally viewed as a safe contraceptive with limited systemic effects. However, three recent studies have indicated an increased risk of depression subsequent to LNG-IUD use. This study aimed to examine the potential associated risk between LNG-IUDs and depression, and determine which women are at risk.
Methods: This longitudinal cohort study was based on data from seven Swedish national population-based registers. All Nordic-born women aged 15-24 years residing in Sweden between 2010 and 2017 were included. Cox regression was implemented to estimate the adjusted hazard ratio (AHR) for developing depression, defined as first depression diagnosis or redeemed prescription for antidepressant treatment. We adjusted for age, education level, parental country of origin, parental psychiatric health, previous hormonal contraceptive use and medical indications for contraceptive use.
Findings: 703,157 women were included in the analysis. The LNG-IUD was associated with 57% increased risk of depression [AHR 1.57 (95 % CI 1.51-1.64)]. The greatest risk increase was seen in adolescent women [AHR 2.57, (95 % CI 2.36-2.80)] and women who used the LNG-IUD as their first hormonal contraceptive method [AHR 1.63, (95 % CI 1.50-1.78)]. The risk of depression decreased at the end of study period [AHR 1.43, (95 % CI 1.36-1.51)], once the LNG-IUD became more widely accessible among nulliparous women.
Conclusions: Adolescent women who use the LNG-IUD as their first-ever hormonal contraceptive are at increased risk of developing depression. However, additional impact from confounding factors is likely as risk estimates decreased over the study period. Further research needs to determine if there is a causal relationship between LNG-IUDs and depression.
Reference:
- Stenhammar E, Wikman P, Gemzell Danielsson K, Kopp-Kallner H, Sundström Poromaa I. Levonorgestrel intrauterine device and depression: A Swedish register-based cohort study. Int J Psychophysiol. 2023 Nov;193:112230. doi: 10.1016/j.ijpsycho.2023.08.003. Epub 2023 Aug 21. PMID: 37611669.
Study: The potential association between psychiatric symptoms and the use of levonorgestrel intrauterine devices (LNG-IUDs): A systematic review
Background: Levonorgestrel (LNG)-intrauterine devices (IUDs) are an effective method of contraception; however, there is growing evidence regarding potential psychiatric side effects such as depressive symptoms, anxiety, and suicidal thoughts. Therefore, we conducted this systematic review to summarise the psychiatric effects of using LNG-IUDs.
Methods: We searched six databases (MEDLINE, Web of Science, Scopus, Science Direct, Cochrane Library, and PsycInfo), and we included all study designs. The included studies were extracted, quality assessed, and qualitatively summarised.
Results: Out of the screened studies, only 22 were finally included. While ten studies showed increased depressive symptoms, two studies showed reduced symptoms. Moreover, one study showed increased anxiety, another one reported an increased risk of suicide, four studies concluded no association with depressive symptoms, and four other studies showed uncertainty about a potential association but mentioned other psychiatric symptoms.
Conclusion: Despite unreliable data, many studies report psychiatric symptoms associated with LNG-IUDs, predominantly depression. Gynaecologists, general practitioners, and psychiatrists should therefore be aware of these potential risks, especially depressive symptoms and suicidality. Counselling patients about these risks should be mandatory. Further studies should investigate the absolute risk of mental disorders associated with LNG-IUDs and other hormonal contraceptives.KEY MESSAGESMany researchers are reporting adverse psychiatric events associated with levonorgestrel intrauterine devices (LNG-IUDs).Despite their effectiveness, a proper psychiatric assessment should be done before inserting LNG-IUDs.Proper counselling regarding the depressive symptoms and suicidality should be done by the treating obstetrician.Further studies should investigate the absolute risk of mental disorders associated with LNG-IUDs and other hormonal contraceptives.
Reference:
- Elsayed M, Dardeer KT, Khehra N, Padda I, Graf H, Soliman A, Makram AM, Zeiss R, Schönfeldt-Lecuona C. The potential association between psychiatric symptoms and the use of levonorgestrel intrauterine devices (LNG-IUDs): A systematic review. World J Biol Psychiatry. 2023 Jun-Jul;24(6):457-475. doi: 10.1080/15622975.2022.2145354. Epub 2022 Nov 25. PMID: 36426589.
Study: Association Between Intrauterine System Hormone Dosage and Depression Risk
Objective: The authors compared the associated risk of incident depression between first-time users of low-, medium-, and high-dose levonorgestrel-releasing intrauterine systems (LNG-IUSs).
Methods: This national cohort study was based on Danish register data on first-time users of LNG-IUSs, 15-44 years of age, between 2000 and 2022. Cox regression and a G-formula estimator were used to report 1-year average absolute risks, risk differences, and risk ratios of incident depression, defined as initiation of an antidepressant or receipt of a depression diagnosis, standardized for calendar year, age, education level, parental history of mental disorders, endometriosis, menorrhagia, polycystic ovary syndrome, dysmenorrhea, leiomyoma, and postpartum initiation.
Results: In total, 149,200 women started using an LNG-IUS, among whom 22,029 started a low-dose one (mean age, 22.9 years [SD=4.5]), 47,712 a medium-dose one (mean age, 25.2 years [SD=6.2]), and 79,459 a high-dose one (mean age, 30.2 years [SD=5.6]). The associated subsequent 1-year adjusted absolute risks of incident depression were 1.21% (95% CI=1.06-1.36), 1.46% (95% CI=1.33-1.59), and 1.84% (95% CI=1.72-1.96), respectively. For the users of high-dose LNG-IUSs, the risk ratios were 1.52 (95% CI=1.30-1.74) and 1.26 (95% CI=1.10-1.41) compared with users of the low- and medium-dose LNG-IUSs, respectively. For users of medium-dose LNG-IUSs, the risk ratio was 1.21 (95% CI=1.03-1.39) compared with users of low-dose LNG-IUSs.
Conclusions: First-time use of an LNG-IUS was positively associated with incident depression in an LNG-dose-dependent manner across low-, medium-, and high-dose LNG-IUSs. Although the observational design of the study does not permit causal inference, the dose-response relationship contributes to the body of evidence suggesting a relationship between levonorgestrel exposure and risk of depression.
Reference:
- Larsen SV, Mikkelsen AP, Ozenne B, Munk-Olsen T, Lidegaard Ø, Frokjaer VG. Association Between Intrauterine System Hormone Dosage and Depression Risk. Am J Psychiatry. 2024 Sep 1;181(9):834-841. doi: 10.1176/appi.ajp.20230909. Epub 2024 Jul 10. PMID: 38982827.
Study: Cohort Study of Psychiatric Adverse Events Following Exposure to Levonorgestrel-Containing Intrauterine Devices in UK General Practice
Introduction: Intrauterine devices are implantable contraceptives of which some brands steadily release levonorgestrel over an extended time period. Exposure to a levonorgestrel-releasing intrauterine device has been associated with depression and, more recently, a connection to anxiety, panic attacks, sleep problems and restlessness has been suggested. This study uses data from the THIN database of UK general practice to investigate these suggestions.
Methods: A cohort study was performed to compare the incidence of psychiatric adverse events between groups of women who were new users of levonorgestrel-releasing and non-hormonal intrauterine devices. Hazard ratios for the first occurrence of psychiatric symptoms or prescriptions of disease-specific treatments were calculated on an intention-to-treat basis using a proportional hazards model.
Results: Significant associations were found between levonorgestrel exposure and records of anxiety (hazard ratio = 1.18; 95% confidence interval 1.08-1.29) and sleep problems (hazard ratio = 1.22; 95% confidence interval 1.08-1.38) in women without a prior record of these events. No significant associations were found for panic attacks or restlessness. Clear baseline differences in clinical characteristics and age between the groups were present. These were included in the model as potential confounding factors.
Conclusion: Statistically significant associations of levonorgestrel exposure with anxiety and sleep problems were observed. Substantive differences in baseline characteristics of the treated groups make robust conclusions difficult but the results strongly suggest that additional studies are warranted.
Reference:
- Slattery J, Morales D, Pinheiro L, Kurz X. Cohort Study of Psychiatric Adverse Events Following Exposure to Levonorgestrel-Containing Intrauterine Devices in UK General Practice. Drug Saf. 2018 Oct;41(10):951-958. doi: 10.1007/s40264-018-0683-x. PMID: 29785475.
IUD Comparisons edit
| Brand Name | Paraguard | Liletta | Mirena | Kyleena | Skyla |
| Years effective | 12 | 8 | 8 | 5 | 3 |
| Total LNG dose (mg) | -- | 52 | 52 | 19.5 | 13.5 |
| Daily LNG dose (mcg/d) | -- | 20 | 20 | 17.5 | 14 |
| Size (mm) | 32x36 | 32x32 | 32x32 | 28x30 | 28x30 |
| String color | White | Blue | Brown | Blue | Brown |
| Silver ring? | N | N | N | Y | Y |
Reference:
Kegel Instructions
How to do Kegel exercises:
- Find the right muscles. To identify your pelvic floor muscles, stop urination in midstream. Once you've identified your pelvic floor muscles you can do the exercises in any position, although you might find it easiest to do them lying down at first.
- Perfect your technique. To do Kegels, imagine you are sitting on a marble and tighten your pelvic muscles as if you're lifting the marble. Try it for three seconds at a time, then relax for a count of three.
- Maintain your focus. For best results, focus on tightening only your pelvic floor muscles. Be careful not to flex the muscles in your abdomen, thighs or buttocks. Avoid holding your breath. Instead, breathe freely during the exercises.
Don't make a habit of using Kegel exercises to start and stop your urine stream. Doing Kegel exercises while emptying your bladder can actually lead to incomplete emptying of the bladder — which increases the risk of a urinary tract infection.
Perform 3 sets of 10 pelvic floor contractions held for 10 seconds each per day.
Reference:
- JAMA Vol 318 No 16 Oct 2017
Limited OB Ultrasound (ALSO)
L, M, N, O, P, Q memory tool:
- L:
- Lie (longitudinal, transverse, oblique)
- Living (fetal heart motion / rate)
- M:
- Masses (fetal or uterine)
- Fetal movements
- Measurements (CRL, BPD, Femur, Circum)
- N:
- Name of patient correct
- Number (singe, twin, triplets)
- O:
- Occupant (anatomic survey)
- P:
- Placenta
- Presentation (vtx, breech, face)
- Position (ROA, LOA)
- Q:
- Quantity (amniotic fluid index)
References:
- From ALSO Course
Mammograms
| 40 yo | 50 yo | 60 yo | |
|---|---|---|---|
| Diagnosed with invasive breast ca | 147 | 231 | 345 |
| Breast ca deaths | 32 | 62 | 88 |
| Deaths averted because of mammogram | 3 | 10 | 43 |
| >1 False positive | 6130 | 6130 | 4970 |
| >1 unnecessary biopsy | 700 | 940 | 980 |
| Overdiagnosed | 28 | 44 | 66 |
- Starting at age 40 saves most lives and causes most harms
- USPSTF recommends age 50-74yo biennial (q2yrs) screening
Potential benefits and harms for 1000 women who start mammography at age 40 vs 50:
- 1 woman diagnosed with breast cancer will not die (1/1000)
- 576 more women will have false positive test results
- 67 more women will have breast biopsies with normal results
- 2 women will be diagnosed and treated for breast tumors that would never have caused symptoms or problems or needed treatment
References:
- AFP Vol 93 No 8 Apr 2016
- JAMA Vol 319 No 17 May 2018
Reading Mammograms
- Ensure the mammogram is technically ok
- The image must be free from blur and artifacts. The trabeculae should be sharp
- Each breast nipple should be in profile in at least one view
- The 3 S's. Get a general overview looking at:
- breast size
- symmetry
- any evidence of prior surgery.
- Compare with prior studies.
- Mediolateral oblique (MLO) Shade symmetry
- Compare the right and left breasts looking only at 1/3 of the breast at a time.
- Next, magnify the breast and repeat the shade symmetry comparison looking for calcifications.
- MLO 5 Spots
- These are either common areas or tricky areas where breast cancer can hide.
- This includes the
- axilla
- subareolar region
- glandular interface
- fatty 'danger zones'
- the whitest thing in the breast.
- Craniocaudal (CC) view Shade symmetry on the CC view.
- Compare the right and left breasts looking only at 1/3 of the breast at a time.
- Next, magnify the breast and repeat the shade symmetry comparison looking for calcifications on the CC view.
- CC 5 SpotsLook at the 5 "Do Not Miss" spots on the CC view.
- These are either common areas or difficult locations where breast cancer can hide.
- This includes the:
- lateral breast
- subareolar region
- glandular interface
- fatty 'danger zones'
- the whitest thing in the breast
- Scroll through the tomosynthesis cine images
- The primary goal of these images is to identify any areas of architectural distortion.
- Check the Computer Aided Detection (CAD).
- Almost every exam will have some markings, most will be ignored.
- But is is worth a quick second glance at each marked area.
Notes:
- Calcifications are best viewed at 1:1 or higher magnification
- Architectural distortion is best seen when the whole breast is visualized
SCREENING MAMMOGRAM SEARCH FOR: mass, calcifications, architectural distortion, asymmetry
- Mass - new or increasing are of concern, particularly if irregular, high density, not circumscribed
- Calcifications - assess stability, morphology, distribution. new or increasing are of concern when not typically benign morphology ie when fine linear, fine linear branching, fine pleomorphic, coarse heterogeneous, amorphous. Suspicious distribution includes segmental, linear, grouped, regional
- Architectural Distortion:
- Normal breast architecture is distorted with no definite mass
- Thin straight lines of spiculations radiating from a point; focal retraction, distortion, straightening at the anterior or posterior edge of the parenchyma
- May also be seen in association with asymmetry or calcifications
- Determine if concordant history of trauma or surgery
- DDx for architectural distortion = Cancer, Radial scar, Posttraumatic/Surgical scar
- Asymmetry: Unilateral deposits of fibroglandular tissue not conforming to the definition of a radiodense mass. Four types:
- ASYMMETRY - visible in only one mammographic projection. Typically summation artefact
- GLOBAL ASYMMETRY - large amount of fibroglandular-density tissue over a substantial portion of breast (at least a quadrant) compared to contralateral breast. Usually normal variant
- FOCAL ASYMMETRY - relatively small amount of fibroglandular-density tissue over a confined portion of breast (< a quadrant). Concave borders and interspersed fat distinguish from mass. DDx Superimposition of two normal structures, Mass
- DEVELOPING ASYMMETRY - focal asymmetry that is new, larger, or more conspicuous than previously. 15% are CA. Therefore developing asymmetry can not be assigned BI-RADS® CATEGORY 3
Reference:
BI-RADS Score Assessment
BI-RADS categories:
- Category 0:
- A category 0 BI-RADS score generally implies an incomplete result. It might indicate the test results were challenging to read for various reasons, and that additional testing may be necessary.
- Category 1:
- A BI-RADS assessment category 1 result is essentially a "negative" result, which means the mammogram didn't detect any abnormalities.
- It can also indicate your breasts are symmetrical with equal densities.
- Category 2:
- A category 2 result is also a "normal" result, with no cancer signs.
- It may indicate a benign finding like cysts, lymph nodes in the breast tissues or calcifications.
- Category 3:
- With a category 3 result, the findings indicate a "probably benign" result.
- The chances of cancer are still minor, at around 2%, and the findings are not likely to change over time.
- Since the results are not 100%, you and your provider should note these and compare them at the next visit.
- Category 4:
- A category 4 mammogram result indicates a suspicion of abnormalities or possibilities of cancerous findings.
- The chances of cancer are still only at 20 to 35%.
- Generally a biopsy of the suspicious tissue.
- This mid-range category also comes with an additional rating of A, B or C:
- A indicating the lowest suspicion of cancerous tissues
- C indicating a higher level of concern for the possibility of cancer
- Category 5:
- At a BI-RADS category 5 score, a high suspicion of cancer is present.
- Biopsy of any questionable tissue
- Category 6:
- For those who have already had a cancer diagnosis, with biopsies to confirm previous mammogram results.
- Used to compare previous screenings and assess how the cancer is responding to the current treatment plan
Reference:
Menopause
- 12 Consequtive months of amenorrhea
- Average age 51yo
Risk Factors for Earlier Menopause:
- Smoking (up to 2 years)
- Nulliparous
- Hysterectomy
- Fragile X carrier
- Autoimmune disorder
- Living at high altitude
- Exposure to chemo/radiation
Reference:
- FAFP Spring 2024 - Dr Simpkins
Perimenopause
Perimenopause can begin 5-10 years before menopause
Symptoms
- Vasomotor symptoms - Thermoregulatory set point lowered
- HRT is the most effective treatment for severe hot flushes
- Transdermal or transvaginal route should be considered
- Venlafaxine 37.5 mg, Paroxetine 7.5 mg, Gabapentin 300 mg qhs, Escitalopram 10 mg also effective
- HRT is the most effective treatment for severe hot flushes
- Genitourinary Symptoms (GSM) - Marked hormonal fluctuations with decreasing estrogen levels
- Thinning of vaginal and urethral epithelium
- Symptoms will not improve over time without treatment
- Mild to moderate symptoms (first line)
- Nonhormonal lubricants with sexual activity
- Vaginal moisturisers used regularly (Not just for sexual activity - several times/wk)
- Not supported by clinical trials - stretching exercises, sexual activity
- Prescription low dose vaginal estrogens, vaginal DHEA inserts, oral SERM
- Moderate to Severe symptoms
- Transdermal and oral HT are effective
- Vaginally preferred when only GSM symptoms present
- Selective Estrogen Receptor Modulators (SERMs) - ospemifene
- Symptoms reduction may take 1-2 months
- Pelvic floor PT may be beneficial
- Transdermal and oral HT are effective
- Estrogen Treatment Most Effective for Vaginal Symptoms
- Local vaginal therapy highly effective for treating atrophy – Success rates > 80%
- Controversial in women with hx of breast cancer
- NO concomitant progestogen therapy required – But no long-term safety trials
- Formulations vary: Beware FEMring (estradiol acetate) delivers systemic dose
- Affordable treatment:
- Vaginal Estrogen needed is ~ 0.1mg
- Can use 1/4 tab of Estrace 0.5 mg (0.125 mg) PV qhs for 2 weeks, then 1-3 times a week
- Mood disturbances- Serotonin levels decreased
- Sleep disturbance
- Cognitive changes
Sexual Function in Menopause
- Transdermal Estrogen Therapy may be preferable over oral ET - Minimal effect on sex hormone-binding globulin and free testosterone levels.
- Filbanserin (Addyi) – pink Viagra - Not indicated for postmenopausal women
- Testosterone:
- Limited data to support or recommend use for GSM
- Some evidence of increase in sexual desire
- High risk profile of AE such as effects on lipid parameters, clitoromegaly, hirsutism, and acne
- No long term safety
- For postmenopausal women who are not using concurrent estrogen therapy
- Topical compounded 1% testosterone cream, ointment, or gel.
- Pt applies approximately 0.5 grams daily to the skin of the arms, legs, or abdomen
- Transdermal testosterone (daily dose of 150 or 300 mcg)
- Transdermal testosterone dose of 300 mcg/day for six months is safe and effective in women who are receiving concomitant estrogen therapy
- Topical compounded 1% testosterone cream, ointment, or gel.
Reference:
- FAFP Spring 2024 - Dr Simpkins
- UTD
Labs
Blood tests are NOT required!
Can check:
- Estradiol
- Follicle-stimulating hormone (FSH)
- Luteinizing hormone (LH)
At menopause, the ovaries become less responsive to FSH and LH hormones, so the body makes more of these hormones to compensate. Estradiol and other hormones decrease around menopause as well.
Hormone Replacement Therapy
Criticism of HERS and WHI trials
- HERS – average age 67, with known CHD
- 75% new users to hormones
- WHI – average age 63
- 36% on anti-hypertensives, 20% on aspirin
- Both trials used 0.625 mg conjugated estrogens alone or with 2.5 mg medroxyprogesterone acetate per day for less than 5 years
Notes:
- Not same age group for seeking treatment – late 40's to 50's
- Overall risks of HRT in younger postmenopausal women are considerably lower than those for older women
Contraindications for HRT
- Unexplained vaginal bleeding
- Hormone sensitive cancers
- Past history of thromboembolus
- Hypertriglyceridemia
- Chronic liver disease
- Active or Recent Stroke or AMI
Progestins should be used with systemic estrogen in all females with an intact uterus:
- Continuous combined
- estrogen and progesterone every day
- Cyclic
- estrogen every day and progestin daily for 12 to 14 days monthly
Lifestyle:
- Weight loss only thing to help with symptoms
HRT:
- estradiol 0.05 mg patch twice a week
- progesterone 200 mg capsule
How long to treat?
- Generally not more that 5 years of use or not beyond age 60
- Hot flashes can last 10 years or more in many women
- For women who experience recurrent, bothersome hot flashes after stopping estrogen
- Try non hormonal options before resuming estrogen
- For those who do not get adequate relief with nonhormonal therapies consider extended use
Reference:
- FAFP Spring 2024 - Dr Simpkins
- ESTROGENS
- The lowest dosage of estrogen therapy that provides bone protection or relief from symptoms should be used.
- A reduction in dosage should be considered as the patient ages.
Common regimens include:
- conjugated equine estrogen or synthesized conjugated estrogen (0.3 to 0.625 mg)
- micronized 17β-estradiol administered orally (0.5 to 1 mg) or intramuscularly, transdermal estradiol (25 to 100 mcg)
- ethinyl estradiol (0.01 to 0.02 mg)
- topical estradiol preparations
- vaginal estrogenic preparations (vaginal estradiol ring, conjugated equine estrogen cream, estradiol cream)
There are few differences among the treatment methods, although the oral and transdermal routes are most commonly used.
The choice of estrogen should be based on patient preference and prior experience.
- However, the transdermal route is recommended for certain clinical situations, such as in women with hypertension, hypertriglyceridemia, and an increased risk of cholelithiasis, and possibly to reduce the risk of thromboembolic disease.
- Transvaginal estrogen may be considered to provide topical effects with less systemic absorption.
- PROGESTATIONAL AGENTS
- If a progestational agent is used in conjunction with estrogen, it should be taken a minimum of 10 to 14 days per month.
- Although amenorrhea may be achieved with daily use of a low-dose progestational agent, it is not recommended because recent studies have shown adverse breast outcomes with continuous therapy.
- Long-cycle use of progestational agents (14 days every three months) may be considered to reduce breast exposure, although the evidence is lacking.
Common choices of progestational agents include:
- micronized progesterone (100 mg daily or 200 mg for 10 to 12 days per month)
- medroxyprogesterone (2.5 mg daily or 5 mg for 10 to 12 days per month)
- norethindrone (0.35 mg daily or 5 mg for 10 to 12 days per month), drospirenone (3 mg daily)
- levonorgestrel (0.075 mg daily)
- BIOIDENTICAL HORMONE THERAPY
- Compounded bioidentical hormone therapies are claimed to be identical in structure to human hormones. However, in many cases, this has not been biochemically substantiated, and the compounded therapies are not regulated by the FDA.
- Although some FDA-approved bioidentical hormone preparations may be considered for menopausal symptoms, there is little evidence that they are safer or more effective than traditional menopausal hormone therapy.
- Risks
- CANCER
- Unopposed estrogen therapy has been associated with the development of endometrial cancer, and therefore a progestational agent should be added to prevent hyperplasia and endometrial cancer. Although data are conflicting, physicians should discuss with patients the possible relationship between menopausal hormone therapy and breast cancer.
- Evidence suggests that this potential relationship is stronger with estrogen/progestational agent combinations than with estrogen alone.
- Using micronized progesterone rather than medroxyprogesterone and avoiding combined continuous therapy may be associated with a lower risk.
- Although study results regarding the effect of menopausal hormone therapy on the risk of ovarian cancer have been inconsistent, women should be advised that there is a possible increase in ovarian epithelial tumors after more than 10 years of therapy.
- Studies have demonstrated a decrease in the incidence of colon cancer and related mortality in women taking menopausal hormone therapy.
- VENOUS THROMBOEMBOLIC DISEASE
- Estrogen therapy has been associated with an increased risk of venous thromboembolic disease within one to two years of initiation.
- Women at increased risk of disease should not take estrogen-containing therapy, although recent research suggests that transdermal estrogen may be safe. Aggressive smoking cessation is recommended for smokers who are considering menopausal hormone therapy because smoking increases the risk of venous thromboembolic disease in those who are taking estrogen.
- STROKE
- Some evidence shows that women on menopausal hormone therapy have more strokes, especially older women.
- OSTEOPOROSIS
- Menopausal hormone therapy should be used to prevent and treat osteoporosis when appropriate, after considering the risks versus benefits in the individual patient.
- Although nonhormonal therapies are available, randomized controlled trials have substantiated the benefits of estrogen in preserving bone mass and, less consistently, in preventing fractures.
- DEMENTIA
- Menopausal hormone therapy has not been shown to affect the risk of dementia and is not recommended to prevent or treat the condition.
- CARDIOVASCULAR DISEASE
- Menopausal hormone therapy should not be used in the primary or secondary prevention of cardiovascular disease. Lipid profiles, smoking history, and diabetes mellitus history should be considered before initiating therapy to determine individual cardiovascular risk. Smoking cessation is strongly advised for smokers who are considering menopausal hormone therapy because smoking increases the risk of cardiovascular disease in those who are taking estrogen.
Reference:
- CANCER
Vaginal Atrophy
Most affordable protocol:
- Estradiol 1 mg tablets
Here is how to use them:
- Using a water based lubricant, insert the tablet vaginally every night for 2 weeks.
- After 2 weeks, go to every other night for 2 weeks
- After those 2 weeks, you can use the tabs as needed basis
Hot flashes
Diet changes:
- Avoid caffeine, alcohol, and spicy foods
- Eat soy containing foods. Soy contains estrogen
Get plenty of calcium and vitamin D in food or supplements
Avoid potential hot-flash triggers:
- Using hair dryers
- Taking hot showers
- Caffeine
- Hot or spicy foods
- Hot drinks
- Alcohol
- Cigarette smoking
General Techniques:
- Wear loose-fitting cotton clothing in layers that can be removed.
- Keep ice water at hand. Lower room temperatures or use a fan.
- Night sweats:
- Take a cool shower before bed
- Wear light cotton pajamas as they are easier to change than sheets
- Keep a frozen ice pack under the pillow, and turn the pillow often so your head rests on a cool surface.
- Try paced respiration:
- Slow, deep abdominal breaths in through your nose and released through your mouth
- Once or twice a day or at the beginning of a hot flash
Menstrual Irregularities
| Term | Definition |
|---|---|
| Anovulatory Cycle | Women who experience uterine bleeding but have not ovulated (ovulation cannot be detected by urinary LH surge or has not been confirmed by hormone concentrations via blood sample analysis). |
| Eumenorrhea | Women who experience menstrual cycle lengths ≥ 21 days and ≤ 35 days, resulting in 9 or more consecutive periods per year, plus recent evidence of a LH surge, correct hormonal profile, and no EHC use in the past 3 months. |
| Normal Menstruating | Women who experience menstruation, with menstrual cycle lengths ≥ 21 days and ≤ 35 days, but without confirmed ovulation (i.e., ovulation has not been confirmed by urinary LH surge or verified by hormone concentrations via blood sample analysis). |
| Oligomenorrhea | Women who experience fewer than 9 menstrual cycles per year or menstrual cycle length that is > 35 days. |
| Ovulatory Cycle | Women who experience menstrual bleeding with a confirmed urinary LH surge which indicates ovulation has occurred. |
| Polymenorrhea | Women who experience menstrual cycle length that is < 21 days on a regular basis. |
| Primary amenorrhea | Failure of a girl to reach menarche by age 15 years when the development of secondary sexual characteristics is evident, or by age 14 years when no secondary sexual characteristics are present. |
| Secondary amenorrhea | The absence of ≥ 3 consecutive menstrual periods in a non-pregnant woman who has a past normal menses history. |
Reference:
- Cabre HE, Moore SR, Smith-Ryan AE, Hackney AC. Relative Energy Deficiency in Sport (RED-S): Scientific, Clinical, and Practical Implications for the Female Athlete. Dtsch Z Sportmed. 2022;73(7):225-234. doi: 10.5960/dzsm.2022.546. Epub 2022 Nov 1. PMID: 36479178; PMCID: PMC9724109.
Bloating during Ovulation
Diet
- Smaller, frequent meals: Eat smaller, more frequent meals to help manage bloating.
- Hydration: Drink plenty of water to help flush out excess sodium and improve digestion. Aim for at least eight cups a day, but consult your doctor for personalized advice.
- Limit salt: Reduce the intake of salty foods, as they can worsen fluid retention.
- Low-FODMAP diet: Avoid high-FODMAP foods such as wheat, onions, garlic, cauliflower, apples, beans, and watermelon, which can trigger digestive symptoms like bloating.
- High-potassium foods: Incorporate potassium-rich foods like bananas and potatoes to help balance sodium levels and reduce water retention.
- Magnesium: Consuming magnesium-rich foods like fish, almonds, and avocados can help. You may also consider a magnesium supplement, but only after consulting with your doctor.
- Natural diuretics: Include foods like ginger, cucumbers, and pineapple, which act as natural diuretics and help reduce water retention.
Supplements
- Probiotics: Taking probiotic supplements that contain strains like Lactobacillus acidophilus and Bifidobacterium lactis can help improve gut health and reduce bloating.
- Peppermint oil: Enteric-coated peppermint oil capsules can soothe the digestive system, reducing gas, bloating, diarrhea, and constipation.
- Digestive enzymes: Enzymes such as lactase (for dairy) and alpha-galactosidase ( for high-fiber foods) can aid digestion and alleviate bloating.
Reference:
Menorrhagia
| Menstrual cycle terms | Descriptive terms | Definition |
|---|---|---|
| Frequency (interval between start of each cycle) | Infrequent | >38 d |
| Normal | 24-38 d | |
| Frequent | <24 d | |
| Regularity (variation of cycle length measured over 12 months) | Regular | +/- 2-20 d over 12 mo |
| Irregular | >20 d over 12 mo | |
| Duration of menstruation | Shortened | <4.5 d |
| Normal | 4.5-8 d | |
| Prolonged | >8 d | |
| Volume (total blood loss per cycle) | Light | <5 ml |
| Normal | 5-80 ml | |
| Heavy | >80 ml | |
| Other | Amenorrhea | No bleeding for 90 d |
| Primary amenorrhea | Absent menarche by 15yo | |
| Secondary amenorrhea | Amenorrhea for 6 mo with prev regular cycles | |
| Menopause | Amenorrhea for 12 mo without apparent cause | |
| Precocious menstruation | Menarche before 9yo |
Reference:
- Am Fam Physician. 2019;99(7):435-443
Risk Factors for Endometrial Cancer
Risk Factors for Endometrial Cancer:
- Major
- Long term use of unopposed estrogen
- RR: 10-20
- Hereditary nonpolyposis colorectal cancer (Lynch syndrome)
- RR: 6-20
- Estrogen-producing tumor
- RR: >5
- Long term use of unopposed estrogen
- Minor
- Obesity
- RR: 2-5
- Nulliparity
- RR: 3
- PCOS
- RR: 3
- History of infertility
- RR: 2-3
- Late menopause
- RR: 2-3
- Tamoxifen use
- RR: 2-3
- Type 2 DM, HTN, Gallbladder disease, Thyroid disease
- RR: 1.3-3
- Obesity
Reference:
- Am Fam Physician. 2019;99(7):435-443
Causes of Abnormal Uterine Bleeding
- Structural
- Endometrial polyps
- Adenomyosis
- Leiomyoma
- Malignancy and hyperplasia
- Nonstructural
- Coagulopathy
- Ovulatory dysfunction
- Endometrial dysfunction
- Iatrogenic (hormone contraceptions is most common)
- Not otherwise classifies
Reference:
- AFP Feb 2024 Vol 109 No 2
Amenorrhea and Oligomenorrhea
- Pregnancy should be excluded in all patients presenting with amenorrhea
- In the evaluation of amenorrhea, hormone-induced withdrawal bleeding has poor sensitivity and specificity for ovarian function
- In patients with functional hypothalamic amenorrhea (especially with the female athlete triad), the primary treatment is weight restoration through nutritional rehabilitation and decreased exercise
- In patients with functional hypothalamic amenorrhea, combined oral contraceptives do not improve bone density and should not be used solely for this purpose
- Patients with polycystic ovary syndrome who are overweight should be evaluated for glucose intolerance, dyslipidemia, and overall cardiovascular risk
- Metformin (Glucophage) may improve abnormal menstruation in patients with polycystic ovary syndrome
Primary Workup:
- Preg test, LH, FSH, TSH, prolactin, pelvic US if indicated
- Pregnancy
- TSH abnormality -> thyroid function tests
- prolactin abnormality -> MRI to exclude adenoma, consider medications
- If uterus
- Low FSH and LH
- Functional amenorrhea if energy deficit
- constitutional delay
- (Rare) primary GnRH def
- Normal FSH and LH
- Consider outflow obstruction
- Other causes
- Elevated FSH and LH
- Primary ovarian failure -> Karyotype (Truner or lack of Y)
- Low FSH and LH
- If no Uterus
- Karyotype, Free and Total Test
- 46,XX
- Mullerian agenesis - expect female Test range
- 46,XY
- Androgen insensitivity syndrome - expect male Test range
- 46,XX
- Karyotype, Free and Total Test
Secondary Workup:
- Preg test, LH, FSH, TSH, prolactin, pelvic US if indicated
- Pregnancy
- TSH abnormality -> thyroid function tests
- prolactin abnormality -> MRI to exclude adenoma, consider medications
- Elevated FSH and LH
- Repeat in 1 month
- Consider Estradiol
- Primary ovarian failure -> Karyotype (Truner or lack of Y)
- Normal or Low FSH and LH
- Evidence of disordered eating; excessive exercise; poor nutritional status
- Most likely Functional amenorrhea
- Consider chronic illness
- Evidence of high intracraneal pressure
- Consider MRI of head to eval neoplasm
- Evidence of hyperandrogenism
- Testosterone, DHEA-S, 17-hydroxyprogesterone
- Eevated 17-hydroxyprogesterone
- Consider late onset congenital adrenal hyperplasia
- PCOS
- Rapid onset of symptoms or very high androgen levels
- Consider adrenal and ovarian imaging
- Eevated 17-hydroxyprogesterone
- Testosterone, DHEA-S, 17-hydroxyprogesterone
- Evidence of disordered eating; excessive exercise; poor nutritional status
- H/o OB/GYN procedures
- Consider induction of withdrawal bleed or hysteroscopy (for Ashermans syndrome)
Reference:
Natural Family Planning
Most effective method: Cervical Mucous Monitoring - LOE B
Two day method: If yes to either question - assume fertile:
- Did I note secretions today?
- Did I note secretions yesterday?
Calendar method:
- Beginning of fertile time - subtract 18 days from the shortest of the previous 6-12 cycles
- End of fertile time - subtract 11 days from the longest cycle
- If perfect 28d cycle - this predicts an 8day fertile period from days 10-17
Standard days method:
- Simplified calendar = assumes a cycle from 26 to 32 days and sets 12 day fertile period from days 8 to 19
Effectiveness of method with use:
- Gives % of women with unintended pregnancy in 1st year of use
| Method | Typical | Perfect |
|---|---|---|
| None | 85% | - |
| Spermicides | 28% | 18% |
| Withdrawal | 22% | 4% |
| Condom | 18% | 2% |
| Diaphragm | 12% | 6% |
| OCP | 9% | <1% |
| Depo-Prov | 6% | <1% |
| IUD | <1% | <1% |
| Standard Days | 8-25% | 5% |
| Two Day | 14% | 4% |
| Creighton Model | 2-5% | <1% |
References:
- AFP Vol 86 No 10 Nov 2012
Nipple discharge
| Characteristic | Etiologies |
|---|---|
| Galactorrhea (Bilat/multiductal) | Hyperprolactinemia due to drugs, |
| hypothyroidism, chronic renal disease, | |
| or pituitary tumor | |
| Multiductal; provoked; bloody or | Ductal ectasia, Fibrocystic change |
| nonbloody; bilateral; green, | |
| yellow, or brown | |
| Uniductal, bloody or occult | Intraductal papilloma, ductal carcinoma |
| blood, provoked or spontaneous, | in situ, Paget's disease of the breast |
| serosanguinous |
References:
- FP Essentaials #341
Oral Contraception
See Also: Contraception (in Drugs
Pap Recommendations
USPSTF recommendations:
- Screen women ages 21-29 every 3 years with cervical cytology
- Women ages 30-65:
- Screen with either cervical cytology alone 3 three years, high-risk HPV (hrHPV) testing alone every 5 years, or hrHPV testing in combination with cytology every 5 years
- Do not screen:
- Women younger than 21
- Women older than 65 who previously have been adequately screened
- Certain women who have had a hysterectomy
Reference:
Pelvic Exams
- No evidence exists to support a clinical benefit from annual pelvic examinations for asymptomatic women who receive Pap smears every 3 to 5 years. However, the American College of Obstetricians and Gynecologists (ACOG) committee on gynecologic practice recommends annual pelvic exams (strength of recommendation [SOR]: C, expert opinion).
- Urine testing alone reliably diagnoses gonorrhea and chlamydia (SOR: A, systematic review of cohort studies).
- Pelvic examinations unreliably detect adnexal masses (SOR: B, single cohort study); pelvic exams accompanied by ultrasound fail to affect outcomes in ovarian cancer screening (SOR: B, cohort studies).
- Pelvic exams aren't necessary before prescribing oral contraceptive pills (OCPs) (SOR: C, expert opinion).
- Vulvar carcinoma has a low prevalence and is usually symptomatic (SOR: B, ecologic study and a case series).
References:
- J Fam Pract. 2015 January;64(1):51-52,65.
Pelvic Pain (Acute)
Defined: Lower abdominal or pelvic pain <3mo
Non-preg reproductive aged women (order of commonness)
- Idiopathic pelvic pain
- PID
- Acute appendicitis
- Conditions related to ovarian cysts
- Endometriosis
Reproductive Age (not pregnant)
Common:
- Endometriosis
- Idiopathic
- Ovarian cyst (ruptured)
- Ovarian torsion
- PID
Less common:
- Adenomyosis
- Dysmenorrhea
- Endometritis (post op)
- Imperforate hymen
- IUD perforation
- Leiomyoma
- Mittelschmerz
Rare:
- Endosalpingiosis
- Round ligament mass (lipoma, teratoma)
- Transverse vaginal septum
Reproductive age (pregnancy related)
Common:
- Corpus luteum cyst
- Ectopic
- Endometritis (postpart)
- Normal labor
- Ovarian torsion
- PID
- Placental abruption
- Preterm labor
- Spont AB
Less common:
- Leiomyoma
- Pubic symphysis separation
- Subchorionic hemorrhage
Rare:
- Incarcerated gravid uterus
- Ovarian vein thrombosis
- Uterine rupture
Reproductive age (fertility treatment)
- Ectopic preg
- Ovarian follicular cyst
- Ovarian hyperstimulation syndrome
- Ovarian torsion
- Heterotopic pregnancy
Postmenopausal
Common:
- Malignancy
Less common:
- Ischemic colitis
Rare:
- Endometriosis
- PID
- Retained IUD
All groups:
Common:
- Appendicitis
- Diverticulitis
- Inflammatory bowel disease
- Irritable bowel syndrome
- Musculoskeletal (abdominal wall)
- UTI
- Urolithiasis
Less common:
- Bowel obstruction
- Inguinal hernia
- Interstitial cystitis
- Pelvic adhesions
- Perirectal abscess
- Urethral diverticulum
- Urinary retention
Rare:
- Mesenteric adenitis
References:
- AFP Vol 93 No 1 Jan 2016
Polycystic Ovarian Syndrome (PCOS)
Diagnosis (2 out of these 3):
- Hyperandrogenism
- presence of excessive acne, androgenic alopecia, or hirsutism (terminal hair in a male-pattern distribution) OR
- by elevated serum levels of total, bioavailable, or free testosterone or dehydroepiandrosterone sulfate
- Ovulatory dysfunction refers to
- oligomenorrhea (cycles more than 35 days apart but less than six months apart) OR
- amenorrhea (absence of menstruation for six to 12 months after a cyclic pattern has been established)
- A polycystic ovary or elevated antimullerian hormone levels
- defined as an ovary containing 12 or more follicles measuring 2 to 9 mm in diameter OR
- an ovary that has a volume of greater than 10 mL on ultrasonography
- a single ovary meeting either or both of these definitions is sufficient for diagnosis of polycystic ovaries
Labs:
- Upon Diagnosis:
- pregnancy test - r/o pregnancy
- TSH - r/o thyroid dysfunction
- prolactin - r/o hyperprolactinemia
- 17-hydroxyprogesterone - r/o nonclassic congenital adrenal hyperplasia
- If labs normal:
- Change in hat/glove size, protruding jaw, impaired vision
- Insuline like grwoth factor 1 to r/o acromegaly
- Dorsocervical fat pad, purple striae, hypertension
- Cortisol (saliva or urine) or dexamethasone suppression test to r/o Cushing Syndrome
- Severe virilization
- Totl testosteron and dehydroepiandrosterone sulfate; then ovarian US or adreanl gland CT or MRI to r/o androgen secreting tumor
- Hot flashes, urogenital symptoms
- FSH and estradiol to r/o primary ovarian insufficiency
- Low body weight, eating d/o, or excessive exercise
- Serum LH, FSH, and estradiol to r/o hypothalamic amenorrhea
- Change in hat/glove size, protruding jaw, impaired vision
Management:
- If desires pregnancy
- Anovulation or infertility
- First line: letrozole
- 2nd: clomiphene
- 3rd: metformin
- Insulin resistance
- First line: lifestyle modification
- 2nd: metformin
- Overweight or obesity
- First line: lifestyle modification
- Hirsutism
- First line: electrolysis
- Acne
- First line: standard topical acne therapy (retinoids, antibiotics, and benzoyl peroxide)
- Anovulation or infertility
- If does not want pregnancy
- Anovulation or menstrual irregularities
- First line: hormonal contraception (including IUD or periodic progesterone withdrawal)
- 2nd: metformin
- Insulin resistance
- First line: lifestyle modification
- 2nd: metformin
- Overweight or obesity
- First line: lifestyle modification; metformin
- 2nd: antiobesity medications (glp-1)
- Hirsutism
- First line: hormonal contraception
- 2nd: antiandrogen medications (spironolactone 25-100 mg qd)
- 3rd: metformin
- Acne
- First line: hormonal contraception with or without standard topical acne therapy
- 2nd: antiandrogen medications (spironolactone)
- Anovulation or menstrual irregularities
Reference:
- AFP Vol 94 No 2 2016
- AFP Vol 107 No 3 Mar 2023
- AFP Vol 110 No 5 Nov 2024
Pregnancy status
CDC criteria for pregnancy without urine test:
- Must meet at least one of the following criteria to be reasonably certain a woman is not pregnant:
- Is <8 days after the start of a normal menses
- Has not had sexual intercourse since the start of last normal menses
- Has been correctly and consistently using a reliable method of contraception
- Is <8 days after spontaneous or induced abortion
- Is within 4 weeks postpartum
- Is fully or nearly fully breastfeeding (exclusively breastfeeding or the vast majority >85% of feeds), amenorrheic, and <6 months postpartum
References:
- JFP Vol 66 No 11 Nov 2017
Premenstrual Syndrome (PMS)
Affective symptoms:
- angry outbursts
- anxiety
- confusion
- depression
- irritability
- social withdrawal
Somatic symptoms:
- abdominal bloating
- breast tenderness or swelling
- headache
- joint or muscle pain
- swelling of extremities
- weight gain
PMS can be diagnosed if the patient reports at least one affective or somatic symptom during the five days before menses in at least two previous menstrual cycles.
Symptoms must resolve within four days of onset of menses without recurrence until at least day 13 of cycle and must be present in the absence of pharmacologic therapy, hormone therapy, or drug or alcohol use.
Treat
- SSRI (LOE A)
- Exercise (LOE B)
- CBT (LOE B)
Reference:
- AFP Vol 111 No 4 Apr 2025
Prenatal Care
Estimated date of confinement (EDC) is based on the first day of the last menstrual period plus 280 days
Ultrasound dating is considered accurate to within:
- four to seven days in the first trimester
- 10 to 14 days in the second trimester
- 21 days in the third trimester
Pregnancy dating should be confirmed with:
- auscultation of fetal heart tones between 10 and 12 weeks
- with fetal quickening between 16 and 18 weeks in women who have been pregnant before or
- between 18 and 19 weeks in first pregnancies.
To prevent pre-eclampsia:
- Use Aspirin
- Recommended for moderate and high risk
- Treat through post-partum visit
Chronic HTN
- Treatment goal is <160/90
- Avoid overtreatment as that can result in IUGR
- Prefered medications:
- Labetolol
- Nifedipine
- Methyldopa
GDM
- Goal is be physiologic
- Preferred medications
- insulin
- metformin
- glyburide
Mental health
- Treat mother
- Risk of medication < Risk of untreated mother
UTI
- After 2 UTI's requires prophylaxis for pregnancy
- Make diagnosis with symptoms
- After treatment, perform test of cure
Drugs in pregnancy:
References:
- 2019 Spring FAFP
Home Birth
A planned home birth is associated with an average absolute increased risk of perinatal death of up to 2 deaths per 1000 patients.
Reference:
- AFP Vol 109 No 6 Jun 2024
Dietary Guidelines in Pregnancy
- Minimize artificial sweeteners
- Limit caffeine intake to less than 300 mg per day
- Association with high caffeine and SAB/low birth weight
- Caloric increase of only 300-400 cal/day
- Avoid unpasteurized dairy products and soft cheeses
- Risk of Toxoplasma and Listeria
- Avoid raw eggs
- Risk of salmonella
- Take 400 mcg Folic Acid even 4 weeks before conception
- Decrease neural tube defects
- Avoid teas containing chamomile, licorice, peppermint, or raspberry leaf
- Associated with adverse outcomes
Reference:
- AFP Vol 108 No 2 Aug 2023
Prenatal Pregnancy Labs
| Quest | Test | Checks For | Price ($) |
|---|---|---|---|
| 1759 | Complete blood count | Anemia (low iron in the blood) | 1.82 |
| 7788 | Blood type, Rh, antibodies | Blood type, Rh status, blood group antibodies | 12 |
| 36126 | RPR | Syphilis, a sexually transmitted disease | 2.39 |
| 802 | Rubella antibody | Immunity to German measles | 8.8 |
| 91431 | HIV antibody | Virus that causes AIDS | 22.12 |
| 498 | HBs Ag testing | Hepatitis B | 8.86 |
| 7909/395 | Urinalysis/Urine Culture | Infections and kidney disease | 10.8 |
| 11363 | Chlamydia | Chlamydia | 24.66 |
| Pap | Cervical Cancer | ||
| Total: | 101.45 | ||
| Total (w/o STI): | 52.28 |
Depending on your health history, you may also be offered tests to check for:
- Immunity to chickenpox
- Sickle cell trait or disease, a certain type of anemia
- Blood sugar levels to see if you are diabetic or pre-diabetic
Optional Genetic Testing:
- First Trimester Screen, hCG (16145) - To screen for Down Syndrome and Trisomy 18 at 10.0-13.9 weeks gestation.
- $138.22
- Quad Screen (30294) - prenatal screening of Down syndrome (Trisomy 21), Trisomy 18 (Edwards syndrome), and open neural tube defects (ONTD).
- Should be performed between 14.0 and 22.9 weeks gestational age, although the optimal period is 15.0-16.9 weeks
- $648.63
Notes:
- Down syndrome (trisomy 21 syndrome) occurs in one per 1,440 births in women 20 years of age and one per 32 births in women 45 years of age
- Invasive genetic testing (amniocentesis or chorionic villous sampling) should be offered to women who are 35 years or older.
- At 35 years of age, the risk of Down syndrome (one per 338 births) is similar to that of fetal loss due to amniocentesis
- All screening tests have a positive rate of approximately 5% (most of which are false positives) and a detection rate of 69% to 87%
- Invasive genetic testing (amniocentesis or chorionic villous sampling) should be offered to women who are 35 years or older.
- Neural tube defects affect 1.5 per 1,000 pregnancies and can be detected by testing maternal serum α-fetoprotein levels (sensitivity = 85.7%, specificity = 97.6%)
- Folic acid, 400 mcg daily, started before pregnancy and continued until six to 12 weeks gestation reduces the rate of neural tube defects by nearly 75%
References:
- General Prenatal Advice
Here is some general prenatal advice:
- Take a daily prenatal vitamin with at least 400 mcg of folic acid and 30 mg of elemental iron to promote neurologic and musculoskeletal fetal development
- EDIT WEIGHT GAIN:
- Your weight gain in pregnancy should be 28 to 40 lb (underweight)
- Your weight gain in pregnancy should be 25 to 35 lb (normal weight)
- Your weight gain in pregnancy should be 15 to 25 lb (overweight)
- Your weight gain in pregnancy should be 11 to 20 lb (obese)
- Consume a well-balanced diet including omega-3 fatty acids (like in low mercury fish)
- Avoid unpasteurized foods
- Caffeine intake should be limited to 200 mg per day (about two small cups of coffee)
- Avoid artificial sweeteners
- Continue regular cardiovascular activity for at least 150 minutes per week
- Bed rest is not recommended.
- Sex can be continued throughout an uncomplicated pregnancy.
- Avoidance of alcohol and marijuana is recommended
Reference:
Prenatal Summary edit
- The First Two Weeks
Shortly after a woman's period begins, her body begins preparing for the possibility of pregnancy.
Approximately 2 weeks into her cycle, a woman releases an egg from one of her ovaries into her adjacent fallopian tube. Conception is now possible for the next 24 hours or so8 and signifies the beginning of pregnancy.9
The single-cell embryo has a diameter of approximately 4 thousandths of an inch.10
- 2 to 4 Weeks
The cells of the embryo repeatedly divide as the embryo moves through the Fallopian tube into the woman's uterus or womb. Implantation, the process whereby the embryo embeds itself into the wall of the womb, begins by the end of the third week and is completed during the fourth week of pregnancy.11
The 4-week embryo is less than 1/100th of an inch long.
- 4 to 6 Weeks
By 5 weeks, development of the brain, spinal cord,12 and heart13 is well underway.
The heart begins beating at 5 weeks and one day14 and is visible by ultrasound almost immediately.15
By 6 weeks, the heart is pumping the embryo's own blood to his or her brain and body.16 All four chambers of the heart are present17 and more than 1 million heartbeats have occurred.18 The head, as well as the chest and abdominal cavities have formed19 and the beginnings of the arms and legs are easily seen.20
The 6-week embryo measures less than ¼ of an inch long from head to rump.
- 6 to 8 Weeks
Rapid brain development continues with the appearance of the cerebral hemispheres at 6½ weeks.21
The embryo reflexively turns away in response to light touch on the face at 7½ weeks.22
Fingers are beginning to form on the hand.23
By 8 weeks the developing human measures about a ½ inch from head to rump.
- 8 to 10 Weeks
Brainwaves have been measured and recorded before 8½ weeks.24
Also by 8½ weeks, the bones of the jaw and collar bone begin to harden.25
By 9 weeks the hands move, the neck turns,26 and hiccups begin.27 Girls now have ovaries28 and boys have testes.29 The embryo's heart rate peaks at about 170 beats per minute30 and will gradually slow down until birth.
Electrical recordings of the heart at 9½ weeks are very similar to the EKG tracing of a newborn.31 The heart is nearly fully formed.32
By 10 weeks kidneys begin to produce and release urine,33 and intermittent breathing motions begin.34 All fingers and toes are free and fully formed,35 and several hundred muscles are present.36 The hands and feet move frequently and most embryos show the first signs of right- or left-handedness.37
Experts estimate the 10-week embryo possesses approximately 90% of the 4,500 body parts found in adults.38 This means that approximately 4,000 permanent body parts are present just eight weeks after conception.
Incredibly, this highly complex 10-week embryo weighs about 1/10th of an ounce and measures slightly less than 1¼ inches from head to rump.
- 10 to 12 Weeks
After 10 weeks, the developing human is called a fetus, which means "little one" or "unborn offspring."39
The eyelids are temporarily fused together by 10½ weeks.40
By 11 weeks the head moves forward and back, the jaw actively opens and closes, and the fetus periodically sighs41 and stretches.42 The face, palms of the hands, and soles of the feet are sensitive to light touch.43 Thumb sucking44 and swallowing amniotic fluid begin.45 Girls' ovaries now contain reproductive cells46 which will give rise to eggs later in life. Also in girls, the uterus is now present.47
Yawning begins at 11½ weeks.48
The number of heartbeats now exceeds 10 million.
Fingerprints start forming at 12 weeks49 while fingernails and toenails begin to grow.50
The bones are hardening in many locations.51
The 12-week fetus weighs less than 1 ounce and measures about 3 inches from head to heel. The Original Fetal Position Crossed Ankles Left Knee and Hip Flexion Hands on Cheeks Hand Near Mouth
- 12 to 14 Weeks
By 13 weeks the lips and nose are fully formed52 and the fetus can make complex facial expressions.53
By 14 weeks taste buds are present all over the mouth and tongue.54
The fetus now produces a wide variety of hormones.55
Arms reach final proportion to body size.56
The 14-week fetus weighs about 2 ounces and measures slightly less than 5 inches from head to heel. Joints of the Fingers Sole of the Right Foot Touching Thumbs Fingertips of Right Hand Palmar Surface of Right Hand
- 14 to 16 Weeks
By 15 weeks the entire fetus (except for parts of the scalp) responds to light touch.57 Tooth development is underway.58
Gender differences emerge at 16 weeks when girl fetuses move their jaws more often than boys.59
A pregnant woman may begin to feel fetal movement at this time.60
The 16-week fetus weighs about 4 ounces and measures slightly less than 7 inches from head to heel.
- 16 to 18 Weeks
Production of a variety of digestive enzymes is well underway.61
Around 17 weeks blood cell formation moves to its permanent location inside the bone marrow62 and the fetus begins storing energy in the form of body fat.63
By 18 weeks formation of the breathing passages, called the bronchial tree, is complete.64 The fetus releases stress hormones in response to being poked with a needle.65
The 18-week fetus weighs around 6 ounces and measures about 8 inches from head to heel.
- 18 to 20 Weeks
By 19 weeks, more than 20 million heartbeats have occurred.
By 20 weeks the larynx or voice box begins moving in a way similar to the movement seen during crying after birth.66 The skin has developed sweat glands67 and is covered by a greasy white substance called "vernix,"68 which provides protection from the amniotic fluid.69
The 20-week fetus weighs about 9 ounces and measures about 10 inches from head to heel. The Mouth and Nose A Smile Slightly Open Right Eye No Worries Yawning
- 20 to 22 Weeks
At 21 weeks breathing patterns, body movements, and heart rate begin to follow daily cycles called circadian rhythms.70
By 22 weeks the sense of hearing begins to function and the fetus starts responding to various sounds.71 The cochlea, the organ of hearing, reaches adult size.72 All skin layers and structures are complete.73
With specialized medical care some fetuses can survive outside the womb by 22 weeks with survival rates reported as high as 40%74 in some medical centers.
The 22-week fetus weighs slightly less than 1 pound and measures about 11 inches from head to heel.
- 22 to 24 Weeks
Between 20 and 23 weeks rapid eye movements begin. These eye movements are similar to those seen when children and adults have dreams.75
By 24 weeks more than 30 million heartbeats have occurred.
The 24-week fetus weighs about 1¼ pounds and measures about 12 inches from head to heel.
- 24 to 26 Weeks
By 25 weeks, breathing motions may occur up to 44 times per minute.76
By 26 weeks sudden, loud noises may trigger a blink-startle response,77 which may increase movement, heart rate, and swallowing.78
The lungs produce a substance necessary for breathing after birth.79
The 26-week fetus weighs almost 2 pounds and measures about 14 inches from head to heel.
- 26 to 28 Weeks
By 27 weeks the thigh bones and the foot bones are each about two inches long (about 5 cm).80
By 28 weeks the sense of smell is functioning81 and eyes produce tears.82
The 28-week fetus weighs more than 2½ pounds and measures about 15 inches from head to heel.
- 28 to 30 Weeks
By 29 weeks, pupils of the eyes react to light.83
The 30-week fetus weighs about 3¼ pounds and measures about 16 inches from head to heel.
- 30 to 32 Weeks
By 31 weeks more than 40 million heartbeats have occurred. Wrinkles in the skin are disappearing as more and more fat deposits are formed.84
By 32 weeks breathing movements occur up to 40 percent of the time.85
The 32-week fetus weighs about 4 pounds and measures about 17 inches from head to heel.
- 32 to 34 Weeks
By 34 weeks true alveoli, or "air pocket" cells, begin developing in the lungs.86
The 34-week fetus weighs about 5 pounds and measures about 18 inches from head to heel.
- 34 to 36 Weeks
The 36-week fetus weighs about 5¾ pounds and measures about 18½ inches from head to heel.
- 36 to 38 Weeks
By 37 weeks the fetus has a firm hand grip87 and the heart has beat more than 50 million times.
The 38-week fetus weighs about 6¾ pounds and measures about 19 inches from head to heel.
- 38 to 40 Weeks
At term, the umbilical cord is typically 20 to 24 inches long.88
Labor is initiated by the fetus,89 ideally around 40 weeks, leading to childbirth.
At full-term birth, newborn babies typically weigh between 6 and 9 pounds and measure between 18 and 21 inches from head to heel.90
Medications during Pregnancy
- Pain or headache
- Acetaminophen (Tylenol; category B) is the drug of choice for pain during pregnancy. It's widely used with very few documented adverse effects.
- Aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs), on the other hand, should be avoided during pregnancy.
- NSAIDs include:
- ibuprofen (Advil, Motrin)
- ketoprofen (Orudis)
- naproxen (Aleve)
- NSAIDs include:
- That said, opioid use during pregnancy does carry the risk of withdrawal, called neonatal abstinence syndrome (NAS), after delivery.
- Colds
- Safe options include:
- plain cough syrup, such as Vicks
- dextromethorphan (Robitussin; category C) and dextromethorphan-guaifenesin (Robitussin DM; category C) cough syrups
- cough expectorant during the day
- cough suppressant at night
- acetaminophen (Tylenol; category B) to relieve pain and fever
- Home treatments before taking medications:
- Get plenty of rest.
- Stay hydrated by drinking water and warm liquids, like chicken soup or tea.
- Gargle salt water to ease sore throat.
- Use saline nose drops to fight stuffiness.
- Humidify the air in your room.
- Use menthol rub on your chest.
- Try nasal strips to open airways.
- Suck on cough drops or lozenges.
- Safe options include:
- Heartburn
- generally safe during pregnancy:
- aluminum hydroxide-magnesium hydroxide (Maalox; category B)
- calcium carbonate (Tums; category C)
- simethicone (Mylanta; category C)
- famotidine (Pepcid; category B)
- For severe heartburn, your doctor may suggest taking H2 blockers, such as:
- ranitidine (Zantac; category B)
- cimetidine (Tagamet; category B)
- Lifestyle changes may also help take the edge off heartburn:
- Wear loose-fitting clothing that doesn't put pressure on your abdomen.
- Try keeping a food diary to help identify certain foods that may trigger your reflux.
- Wait three hours to lie down after meals. Avoid late meals right before bedtime.
- Sleep with your head elevated at night.
- Eat small meals throughout the day.
- generally safe during pregnancy:
- Allergies
- generally considered safe:
- diphenhydramine (Benadryl; category B)
- chlorpheniramine (Chlor-Trimeton; category B)
- loratadine (Claritin, Alavert; category B)
- cetirizine (Zyrtec; category B)
- If your allergies are more severe, your doctor may suggest taking an OTC corticosteroid spray at a low dose along with an oral antihistamine. Options include:
- budesonide (Rhinocort Allergy; category C)
- fluticasone (Flonase; category C)
- mometasone (Nasonex; category C)
- You may also try the following lifestyle changes:
- Avoid going outdoors or opening windows on high pollen days.
- Take off clothing you've been wearing outdoors. Rinse off pollen from skin and hair with a quick shower.
- Wear a mask while completing outdoor chores or enlist the help of someone else for tasks like mowing.
- Rinse nasal passages with saline spray or a neti pot.
- generally considered safe:
- Constipation
- Stool softeners are generally considered safe during pregnancy. Options include Colace or Surfak.
- Laxatives, like Senokot, Dulcolax, or Milk of Magnesia, may also help, but speak with your doctor before trying any of these medications.
- Other treatment options for constipation include the following:
- Drink more water and fluids. Prune juice is another good choice.
- Add more exercise to each day.
- Eat more fiber. You can find fiber in fruits and vegetables (with skins, if possible), beans, and whole grains.
- Ask your doctor about fiber supplements, like Metamucil.
- Morning sickness
- Try home remedies, like eating small meals throughout the day or sipping ginger ale, before reaching for medications.
- You might try:
- vitamin B-6, 25 milligrams by mouth three times a day
- doxylamine succinate (Unisom; category B)
- dimenhydrinate (Dramamine; category B)
- There are medications your doctor may prescribe if you're experiencing severe nausea and vomiting (hyperemesis gravidarum):
- doxylamine succinate-pyridoxine hydrochloride (Diclegis; category A)
- ondansetron (Zofran; category B)
- Hemorrhoids
- Safe treatment options include:
- Tucks pads or other witch hazel pads
- Preparation H
- Anusol
- You may want to try other methods first:
- Soak the hemorrhoids by filling a tub with warm water. Don't add soap or bubble bath.
- Stand or lie on your side when possible.
- Try a ring cushion or hemorrhoid pillow for when you must sit.
- Treat constipation by taking stool softeners, drinking more fluids, getting more exercise, and eating more fiber.
- Safe treatment options include:
- Yeast infections
- Safe medications include:
- miconazole (Monistat; category C)
- clotrimazole (Lotrimin; category C)
- butoconazole (Femstat; category C)
- Safe medications include:
- Insomnia
- Safe medications for insomnia are those in the diphenhydramine (category B) family, including:
- Sominex
- Nytol
- Doxylamine succinate (Unisom; category B) is another possibility that may also be used if you're experiencing insomnia.
- If OTC methods don't work, your doctor may prescribe the following after weighing the benefits and risks:
- sedating tricyclic antidepressants (Amitriptyline, Nortriptyline; category C)
- benzodiazepines (Ativan, Klonopin; category D)
- Benzodiazepines may be associated with risk of cleft or lip palate. Use in later pregnancy may not carry this risk.
- Lifestyle changes you can try include the following:
- Schedule sleep for consistent wake and bedtimes.
- Get regular exercise.
- Limit napping to no more than 30 minutes per day.
- Skip caffeine and other stimulants.
- Create a nighttime ritual. For example, take a bath, listen to music, or do yoga.
- Explore alternative treatments, such as meditation or acupuncture.
- Safe medications for insomnia are those in the diphenhydramine (category B) family, including:
From: https://www.healthline.com/health/pregnancy/what-medicines-are-safe-during-pregnancy
When to change dates based on US
| Gest. Age | Diff in EDC |
|---|---|
| <8 6/7 | 5 |
| 9 0/7 - 15 6/7 | 7 |
| 16 0/7 - 21 6/7 | 10 |
| 22 0/7 - 27 6/7 | 14 |
| >28 | 21 |
References:
- Obsetet Gynecol. 2014; 124(4):864
Progesterone Use edit
- INDUCTION OF WITHDRAWAL BLEEDING IN SECONDARY AMENORRHEA
- Short courses of orally administered medroxyprogesterone acetate (5 mg twice daily for five days) have produced withdrawal bleeding in 93 percent of amenorrheic women
- oral micronized progesterone (300 mg per day) produced withdrawal bleeding in 90 percent of women with oligomenorrhea or amenorrhea
- TREATMENT OF DYSFUNCTIONAL UTERINE BLEEDING
- In most adolescents, the bleeding can be controlled with cyclic progestins (medroxyprogesterone acetate, 5 to 10 mg per day for 10 to 12 days of the month) or low-dose oral contraceptive pills (with the added advantage of contraception). It is important to administer therapy for short periods (three to six months) and then reevaluate the patient. As many as 93 percent of adolescents with dysfunctional uterine bleeding respond to medical therapy
- Dysfunctional uterine bleeding in perimenopausal women is generally related to declining β-estradiol levels. In this age group, it is particularly important to rule out endometrial atypia and cancer before initiating therapy. However, patient age is not as important as duration of exposure to unopposed estrogens.
- Endometrial hyper-stimulation resulting from unopposed estrogen administration can be reduced by adding a progestin in postmenopausal women. Therapy with a progestin for 12 or more days each month can prevent new cases of endometrial hyperplasia and significantly reduce the risk of endometrial carcinoma
- A regimen consisting of low-dose micronized progesterone (100 mg per day) and micronized estradiol (Estrace; 1.5 mg per day) for 25 days each month controls endometrial proliferation but does not fully suppress mitotic activity.27 Consequently, amenorrhea is induced without irregular spotting
- No increase in the risk for cerebral thromboembolic events has been reported for progestin-only oral contraceptive pills
- For retention of efficacy, progestin-only oral contraceptive pills must be taken at the same time each day. If a pill is taken more than three hours late, a backup method of contraception should be used for at least the next 48 hours.
- PROGESTIN-ONLY EMERGENCY CONTRACEPTION
- Until recently in the United States, the progestin dose needed for emergency contraception could only be obtained by taking 20 0.075-mg norgestrel tablets. The FDA has now labeled Plan B (800–330–1271), which consists of two 0.75-mg levonorgestrel tablets. One tablet is taken as soon as possible but no later than 72 hours after unprotected sexual intercourse; the second tablet is taken 12 hours after the first dose.
Reference:
- Am Fam Physician. 2000;62(8):1839-1846
- https://www.aafp.org/pubs/afp/issues/2000/1015/p1839.html
Risk factors for post partum hemorrhage
- Augmented labor
- Chorioamnionitis
- History of postpartum hemorrhage
- Operative delivery
- Overdistended uterus
- Preeclampsia
- Prolonged labor
- Rapid labor
- 3rd stage lasting >18min
Sexual Dysfunction In Women
- Bupropion (Wellbutrin) in higher dosages (150 mg twice daily) has been shown to be effective as an adjunct for antidepressant-induced sexual dysfunction in women. (LOE B)
- Sildenafil (Viagra) may benefit women with sexual dysfunction induced by selective serotonin reuptake inhibitor or serotonin-norepinephrine reuptake inhibitor use. (LOE B)
- Female genital sexual pain disorders are complex and most effectively managed with a comprehensive, multidisciplinary approach that addresses contributing biopsychosocial factors. (LOE C)
- Group cognitive behavior therapy has been shown to effectively treat low sexual desire. (LOE C)
- Mindfulness-based interventions have been shown to effectively treat low sexual desire and arousal, and acquired anorgasmia. (LOE B)
- Directed masturbation is recommended for lifelong anorgasmia. (LOE A)
- Local vaginal estrogen therapy is recommended and preferred over systemic estrogen therapy for treatment of genitourinary syndrome of menopause and related dyspareunia when vaginal dryness is the primary concern. Because of potential adverse effects, the use of estrogens, especially systemic estrogens, should be limited to the shortest duration compatible with treatment goals. (LOE A)
- 0.625 mcg vaginal estrogen cream +/- 1 mgtestosterone
- Ospemifene (Osphena) is modestly effective for treatment of dyspareunia. (LOE B)
- Transdermal testosterone, with or without concomitant estrogen therapy, has been shown to be effective for short-term treatment of low sexual desire or arousal in natural and surgically induced menopause. (LOE B)
- 300 mcg patch to 1 mg transdermal
Endocrine Society recommends consideration of 3-6 mo course of testosterone specifically for postmenopausal women with low sexual desire
Reference:
- Am Fam Physician. 2015;92(4):281-288
- AFP Vol 111 No 5 May 2025
Uterine Bleeding
Conditions:
- Menorrhagia
- Prolonged (>7d) or excessive bleeding at regular intervals (>80ml/cycle)
- Metrorrhagia
- Irregular, frequent bleeding of varying amounts but not excessive
- Menometrorrhagia
- Prolonged (>7d) or excessive bleeding at irregular intervals (>80ml/cycle)
- Polymenorrhea
- Regular bleedig at intervals <21 days
- Oligomenorrhea
- Bleeding at intervals >35 days in adults; >45 days in adolescents
- Primary amenorrhea
- No spontaneous menses in a female 16yo or older
- Secondary amenorrhea
- No uterine bleeding for 6mo or more
- Intermentrual bleeding
- Irregular bleeding between regular cycles
- Postmenopausal bleeding
- Bleeding occuring >1yr after cessation of menses or at unanticipated times for women taking cyclic hormone therapy
Estrogen
- Promotes endometrial growth
Progesterone
- Promotes differentiation of endometrium
Management of Heavy Uterine Bleeding
- Acute heavy bleeding
- Conjugated estrogen: 25mg IV q4 for up to 24hrs
- Stops bleeding in 75% of patients within 5 hours
- Monophasic OCP: Norethindrone 1mg, ethinyl estradiol 35mcg: 1 pill tid for 1 wk, then 1 pill daily for 21 days. Repeat 21 day regimen after a 7 day interval
- Stops bleeding in most patients within 3 days
- Progestins: Norethindrone 5mg po tid for 21 day and repeat after 7 day interval OR Medroxyprogesterone 20mg tid for 7 days, then 20mg daily for 21 days and repeat after 7 day interval
- Stops bleeding in most patients within 3 days
- Conjugated estrogen: 25mg IV q4 for up to 24hrs
- Stable heavy bleeding
- OCP: Daily monthly
- Reduces bleeding by 50% with long term use
- Progestins: Medroxyprogesterone 10mg/d for 14-21 days monthly OR Norethindrone 5mg daily for 14-21 days monthly
- 87% mean reduction in blood loss with long term use
- NSAIDs: Naproxen
- 29% mean reduction in blood loss
- Levonorgestrel IUD: 20mcg/24hrs for 5 yrs
- 94% mean reduction in blood loss
- OCP: Daily monthly
Postmenopausal bleeding
Work-up:
- Transvaginal Ultrasound
- <4 mm endometrial thickness
- Monitor at 4 and 12 months; repeat US if bleeding persists
- >4 mm endometrial thickness
- Consider Saline Infusion Sonography
- Diffusely thickened -> Endometrial biopsy
- Focal mass or thickening -> Hysteroscopy and biopsy
- Consider Saline Infusion Sonography
- Focal thickening of endometrium
- Hysteroscopy
- <4 mm endometrial thickness
- Overall approach to OCP associated uterine bleeding
- Consider Abnormal Uterine Bleeding evaluation
- Evaluate for missed OCP doses
- Pregnancy Test
- Counsel on compliance
- Anticipate uterine bleeding in first 3 months
- Offer anticipatory guidance
- Consider adjuncts to Oral Contraceptive
- Ibuprofen 800 mg PO tid for 1-2 weeks
- Supplemental Estrogen for 1-2 weeks
- Premarin 0.625 to 1.25 qd
- Ethinyl Estradiol 20 ug qd
- Estradiol (Estrace) 0.5 to 1 mg qd
- Consider alternative Oral Contraceptive
- Change Progesterone type as listed below
- Switch from Levonorgestrel to Norethindrone containing Oral Contraceptives
- If on Seasonal Contraception, stop for 3-4 days when breakthrough bleeding occurs
- Increasing Estrogen to 50 ug does not appear effective at reducing bleeding
- Moreau (2007) Obstet Gynecol 109(6):1277-85 [PubMed]
Reference:
- Early Cycle Breakthrough Bleeding (Days 1-9) or all month
- Progestin characteristics
- Higher Estrogenic Activity
- Consider increasing Estrogen to 50 mcg Monophasic
- Ovcon 50
- Ortho-Novum 1/50
- Demulen 1/50
- Temporarily add Estrogen prn breakthrough bleeding
- Ethinyl Estradiol 0.02 mg PO qd for 7 days prn
Reference:
- Progestin characteristics
- Late Cycle Breakthrough Bleeding (Days 10-21)
- OCP Characteristics
- Higher Progestin Activity
- Higher Endometrial Activity
- Examples
- Loestrin 1.5/30
- Loestrin 1/20
- Demulen 1/35
Reference:
- OCP Characteristics
- Menorrhagia or Dysmenorrhea
- OCP Characteristics
- Higher Progestin Activity
- Lower Estrogenic Activity
- Examples
- Loestrin 1.5/30
Reference:
- OCP Characteristics
- Amenorrhea or Menses too light
- Check Pregnancy Test!
- OCP Characteristics
- Lower Progestin Activity
- Higher Estrogenic Activity
- Higher Endometrial Activity
- Examples
- Loestrin 1.5/30
- Loestrin 1/20
- Demulen 1/35
- Consider additional Estrogen initially
- Premarin 0.625 mg qd for 7 days
- Start at beginning of next cycle
Reference:
- Seasonal OCP
- Typical monophasic Oral Contraceptive used in Seasonal Contraception (e.g. Loestrin 1/20, Alesse, Aviane)
- Low dose Estrogen (20-30 mcg Ethinyl Estradiol) and
- Progestin (e.g. Levonorgestrel, Norethindrone)
- Simply do not take Placebo pills
Reference:
- Typical monophasic Oral Contraceptive used in Seasonal Contraception (e.g. Loestrin 1/20, Alesse, Aviane)
Vaginitis
Diagnosis:
- Bacterial vaginosis
- Etiology: Anaerobic bacteria (Prevotell, Mobiluncus Garderella vaginalis, Ureaplasma, Mycoplasma)
- Symptoms:
- Fishy odor
- Thin, homongenous discharge that may worsen after intercourse
- Pelvic discomfort possible
- Signs:
- No inflammation
- Other risks:
- Increased risk of HIV, gonorrhea, chlamydia, and herpes infections
- Risk factors:
- Low socioeconomic status
- Vaginal douching
- Smoking
- New or multiple partners
- Unprotected intercourse
- Women who have sex with women
- Vulvovaginal candidiasis
- Etiology: Candida albicans
- Symptoms:
- White, thick, cheesy, or curdy discharge
- Vulvar itching or burning
- No odor
- Signs:
- Vulvar erythema and edema
- Risk factors:
- Recent antibiotic use
- Pregnancy
- Uncontrolled diabetes mellitis
- AIDS
- Corticosteroid use
- Immunosuppression
- Trichomoniasis
- Etiology: Trichomonas vaginalis
- Symptoms:
- Green or yellow, frothy discharge
- Foul odor
- Vaginal pain or soreness
- Signs:
- Inflammation; strawberry cervix
- Other risks:
- Increased risk of HIV infection (should be screen for other STDs)
- Increased risk of preterm labor
- Risk factors:
- Low socioeconomic status
- Multiple sex partners
- Other STDs
- Unprotected intercourse
- Drug use
- Smoking
- Atrophic vaginitis
- Etiology: Estrogen deficiency
- Symptoms:
- Thin, clear discharge
- Vaginal dryness
- Dyspareunia
- Itching
- Signs:
- Inflammation
- Thin, friable vaginal mucosa
- Risk factors:
- Menopause
- Lactation
- Oopherectomy
- Radiation/Chemo therapy
- Immunologic disorders
- Premature ovarian failure
- Endocrine disorders
- Antiestrogen medications
- Irritant/allergic vaginitis
- Etiology: Contact irritation or allergic reactino
- Symptoms:
- Burning, soreness
- Signs:
- Vulvar erythema
- Risk factors:
- Soaps
- Tampons
- Condoms, diaphragms, sex toys
- Pessaries
- Douching
- Fastidious cleansing
- Medications
- Clothing
- Inflammatory vaginitis
- Etiology: Possibly autoimmune
- Symptoms:
- Purulent vaginal discharge
- Burning
- Dyspareunia
- Signs:
- Vaginal atrophy and inflammation
- Other risks:
- Associated with low estrogen levels
- Risk factors:
- Sperm
- Douching
- Latex condoms or diaphragms
- Tampons
- Topical products
- Medications
- Clothing
- Atopic history
References:
- AFP Vol 97 No 5 Mar 2018
Amsel Diagnostic Criteria for Bacterial Vaginosis
3 out of 4 criteria must be met:
- Thin, homogenous discharge
- Positive Whiff test (Amine odor produced after 10% KOH with vaginal discharge sample
- Clue cells present on microscopy (Vaginal epithelial cells with borders obscured by adherent coccobacilli on wet-mount)
- Vaginal pH > 4.5
References:
- AFP Vol 97 No 5 Mar 2018
Weight gain in Pregnancy
Recommended weight gain from pre-pregnancy weight:
| Recommendation | Underweight | Normal Weight | Overweight | Obese |
|---|---|---|---|---|
| BMI | <18.5 | 18.5-24.9 | 25-29.9 | >30 |
| Total wt gain range | 28-40 lbs | 25-35 lbs | 15-25 lbs | 11-20 lbs |
| (12.5-18 kg) | (11.5-16 kg) | (7-11.5 kg) | (5-9 kg) |
Reference:
- JAMA Vol 317 No 21 Jun 2017
Ophthalmology
Acute Red Eye (Conjunctivitis)
Best predictors of serious eye disease:
- Eliciting photophobia via pupillary constriction
- Presence of anisocoria (>1mm)
- Prompt referral (LOE 2A-)
| Bacterial | Viral | Allergic | |
|---|---|---|---|
| Systemic symptoms. | Usually none. | May be part of a viral prodrome followed by adenopathy, fever, pharyngitis, and upper respiratory tract infection. There may be an enlarged and tender preauricular node. | Nasal congestion, sneezing, wheezing. |
| Itching. | Limited to none. | Limited to none. Primary complaint is grittiness, burning or irritation. | Primary complaint. May also report grittiness, burning, or irritation. |
| Ocular discharge. | Purulent, may be yellow, white, or green. Recurs at lid margins and corners of the eye within minutes of wiping lids. | Watery with strands of mucus. | Watery. |
| Conjunctival appearance. | Pink or red. | Pink or red. Very rarely hemorrhagic. Tarsal conjunctiva may have a follicular or "bumpy" appearance. | Pink. Bulbar conjunctiva may be chemotic (puffy). Tarsal conjunctiva may have a follicular or "bumpy" appearance. |
Bacterial conjunctivitis
- erythromycin ophthalmic ointment 0.5% 3.5 g
- 0.5 inch (1.25 cm) 4 times daily for 5 to 7 days
- Ciprofloxacin 0.3% ophthalmic drops (preferred agent in contact lens wearer)
- 1 to 2 drops 4 times daily for 5 to 7 days
- Ofloxacin 0.3% ophthalmic drops (preferred agent in contact lens wearer)
- 1 to 2 drops 4 times daily for 5 to 7 days
- Moderate-certainty evidence showed that, compared with placebo, antibiotics were more likely to achieve a clinical cure (i.e., resolution of clinical symptoms or signs of infection) after a treatment course of varying duration (risk ratio [RR] = 1.26; 95% CI, 1.09 to 1.46; absolute risk difference [ARD] = 15%; number needed to treat = 7).
- A subgroup analysis showed no difference by antibiotic class (fluoroquinolone vs. nonfluoroquinolone) or treatment duration (three to five days vs. more than five days).
- 1/7 Helped: Clinical cure
- 1/32 Harmed: Ocular adverse effects
Viral conjunctivitis
- Antihistamine/decongestant drops (OTC)
- 1 to 2 drops 4 times daily as needed for no more than 3 weeks
| Drug | Dose | Cost |
|---|---|---|
| Antihistamines: | ||
| - Bepotastine | bid | $180 |
| - Emedastine | qid | $120 |
| - Epinastine | bid | $38 |
| Mast Cell Stab: | ||
| - Lodoxamide | qid | $150 |
| - Nedocromil | bid | $190 |
| - Pemirolast | qid | $115 |
| Combinations: | ||
| - Azelastine | qid | $40 |
| - Ketotifen | bid | $15 |
| - Olopatadine | bid | $50 |
References:
- AFP Vol 93 No 7 Apr 2016
- AFP Vol 93 No 11 Jun 2016
Reference:
- Am Fam Physician. 2023;107(6):online
- UptoDate.com
Eye drops/lubrication
Emollient Eye Drops
- Bausch+Lomb SootheXP with Restoryl Mineral oils
Eye Emergencies
- Patients with a central retinal artery occlusion should receive a workup for stroke consisting of echocardiography, electrocardiography, and carotid artery ultrasonography. LOE C
- A chemical eye injury should be irrigated with normal saline or lactated Ringer solution until the ocular surface pH has normalized. LOE B
- Patients with a suspected mechanical globe injury should have a metal shield placed over the eye, be given antiemetics, and be referred immediately to an ophthalmologist for surgical repair. LOE C
- Prophylactic systemic antibiotics should be administered to patients to prevent endophthalmitis after a mechanical globe rupture or laceration. LOE C
- Patients with new symptomatic floaters, flashing lights, and visual field defect should be referred within 24 hours to an ophthalmologist for evaluation of a retinal tear or detachment. LOE C
References:
- AFP Nov 2020 Vol 102, No 9
Eyelid Inflammation
Stye Information:
- Spontaneous drainage occurs 3-4 days following formation
- Use hot compresses applied for 5-10 min 2-4 times a day - I suggest using a wet washcloth and microwaving for a few seconds to make it hot (but not to burn your skin). You will need to reheat a few times as the temperature is important.
- Topical antibiotics can be effective - I can send a prescription (erythromycin) in for you - If it doesn't improve with the hot compresses, where do you want me to send an antibiotic?
Internal Hordeolum
Etiology:
- Infection within the meibomian gland
- Most commonly caused by Staphylococcus aureus
- Associated with:
- Rosacea
- Trichiasis (inward-turned eyelashes)
- Ectropion
Management:
- Warm compresses applied for 5-10 min 2-4 times a day
- The heat softens the granuloma and lipids, allowing it to drain more easily
- Effective temperature is 40.5C - washcloths need frequent reheating
- Topical antibiotics are NOT effective
- Penicillinase-resistant penicillins:
- dicloxacillin 125-250mg q6
- amoxicillin clavulanate 250mg q8
- Alternative oral antibiotics:
- levofloxacin 500mg daily
- trimethoprim-sulfamethoxazole 200mg daily
- cephalexin 250-500mg q6 for 1-2 wks
- If unresolved - surgical incision and drainage
References:
- Consultant May 2017
External Hordeolum
Etiology:
- Glands of Moll or Zeis are infected
- Infection occurs in lumen of either gland causing tender, erythematous swelling near lid margin
- Anterior to tarsal plate and muscle tissue - abcess can be seen without eyelid eversion
- Associacet with blepharitis, fatigue, poor diet, and stress
- Can be recurrent
Management:
- Spontaneous drainage occurs 3-4d following formation
- Warm compresses applied for 5-10 min 2-4 times a day
- The heat softens the granuloma and lipids, allowing it to drain more easily
- Effective temperature is 40.5C - washcloths need frequent reheating
- Topical antibiotics ARE effective
- bacitracin
- erythromycin ophthalmic 4 times a day in acute phase and twice a day for 1 week
- Penicillinase-resistant penicillins:
- dicloxacillin 125-250mg q6
- Alternative oral antibiotics:
- cephalexin 250-500mg q6 for 1-2 wks
- If unresolved - surgical incision and drainage
References:
- Consultant May 2017
Chalazion
Etiology:
- Obstruction and inflammation of the sebaceous glands of eyelid - can be either meibomian glands or glands of Zeis
- Marginal chalazion on lid maergin are from gland of Zeis
- NOT infectious - chronic, sterile lipogranulomatous inflammation within the glands
- Can come from unresolved hordeolum
- Associated with:
- seborrheic blepharitis
- rosacea
Unlike hordeolum, chalazia are hard, immobile, and painless
Management:
- Warm compresses applied for 5-10 min 2-4 times a day
- The heat softens the granuloma and lipids, allowing it to drain more easily
- Effective temperature is 40.5C - washcloths need frequent reheating
- Lid massages
- Topical and oral antibiotics are NOT effective
- Oral tetracyclines can help by stabalizing free fatty acids produced as meibomnian lipids break down - reducing the stimuli for granuloma formation
- Oral doxycycline 50-100mg bid
- Oral tetracycline 250mg q6 for 3-4 weeks
- Corticosteroid intralesional or subcutaneous injections
- triamcinolone 40mg/mL (0.10-0.20mL)
- Resolution occusrs 1-2wks after 1 injection
- Aspirate for blood before injection. Inject slowly.
References:
- Consultant May 2017
Sudden Vision Loss
- Autoimmune conditions in self or family
- Optic neuritis
- Chronic therapeutic anticoagulation
- Vitreous hemorrhage
- Constitutional symptoms
- Giant cell arteritis
- Curtain like visual field defect
- Retinal detachment
- Disproportionate change in color perception
- Optic neuritis
- Eye pain at rest
- Acute angle-closure glaucoma, uveitis, endophthalmitis
- Headache
- Optic neuritis, migraine with aura, idiopathic intracranial hypertension
- High myopia (nearsightedness)
- Retinal detachment
- Jaw claudication, scalp tenderness, polymyalgia rheumatica
- Giant cell arteritis
- Long lasting (>24 hrs) vision loss
- Retinal artery occlusion, retinal vein occlusion, giant cell arteritis, vitreous hemorrhage, retinal detachment, Optic neuritis, sudden discovery of preexisting unilateral vision losss, stroke, toxins
- Multiple dark floaters
- Vitreous hemorrhage
- Pain with eye movements
- Optic neuritis
- Partial visual field loss in both eyes
- Cerebral ischemia, intracerebral hemorrhage, brain tumor
- Recent intraocular interventions
- Endophthalmitis, hypotony maculopathy, choroidal effusion
- Transient (<1hr) vision loss
- Amorosis fugax, transient ischemic attack, stroke, migraine, giant cell arteritis, syncope
- Vascular risk factors
- Amorosis fugax, transient ischemic attack, stroke, retinal artery occlusion, branch retinal vein occlusion, vitreous hemorrhage
Reference:
- AFP Jan 2025 Vol 111 No 1
Refractory Eye Surgery
Patient selection criteria for LASIK:
- Age over 18yo
- Stable refraction for at least 1 year
- Astigmatism no worse than 5 D
- Hyperopia no worse than +6 D
- Myopia no worse than -12 D
Expected visual acuity with LASIK
| UCVA | UCVA | Predictable | Predictable | Patient |
|---|---|---|---|---|
| 20/20 | 20/40 | correction | correction | satisfaction |
| within 0.5 D | within 1 D | |||
| >90% | 98% | >80% | >95% | 97% |
- UCVA = Uncorrected visual acuity
Contraindications to LASIK:
- Absolute contraindications:
- Corneal abnormalities
- External eye disease
- Pregnancy, lactation
- Significant cataract
- Uncontrolled diabetes mellitis
- Uncontrolled glaucoma
- Uncontrolled systemic autoimmune disease
- Unrealistic patient expectations
- Possible contraindications:
- Abnormal wound healing
- Controlled diabetes
- Glaucoma
- History of herpetic keratitis
- Systemic autoimmune disease
Potential complications:
- Dry eyes (20-40%)
- Peaks at 3mo, resolves by 6-12mo
- Persistent in 2-3%
- Diffuse lamellar keratitis (2-4%)
- Epithelial disruption from debris at edge of flap; also called Sands of Sahara
- Epithelial ingrowth (1-3%)
- Self limited; may need laser to treat ectopic cells
- Flap wrinkles (0.2-4%)
- Free cap (0.1-1%)
- Infection (bacterial, fungal) (0.1-0.1%)
- Usually resolves with treatment
References:
- AFP Vol 81 No 1 Jan 2010
- AFP Vol 95 No 10 May 2017
Pain
Chronic Musculoskeletal Pain
- Regular exercise is recommended for patients with chronic musculoskeletal pain.10–12,18–23 Because no specific type of exercise is clearly superior, patients should be encouraged to engage in the type of low-impact exercise they prefer. (LOE B)
- Encourage yoga for patients with chronic low back pain, lumbar radiculopathy, knee osteoarthritis, or fibromyalgia. (LOE B)
- Encourage cognitive behavior therapy for patients with chronic low back pain or fibromyalgia. (LOE B)
- Encourage mindfulness-based stress reduction for patients with chronic low back pain or fibromyalgia. (LOE B)
- Consider spinal manipulation for patients with chronic low back pain or neck pain. (LOE B)
- Consider acupuncture for patients with chronic low back pain, neck pain, or fibromyalgia. (LOE B)
- Consider massage or myofascial release for low back pain, neck pain, hip and knee osteoarthritis, and fibromyalgia. (LOE B)
- Consider multi- or interdisciplinary rehabilitation for patients with chronic low back pain or fibromyalgia that does not respond to initial therapies, or who have a significant psychological component. (LOE B)
References:
- AFP Oct 2020 Vol 102 No 8
Facial pain
Extraoral:
- Musculoskeletal
- Temporalmandibular disorders
- Neuropathic
- Trigeminal neuralgia
- Post-traumatic trigeminal pain
- Glossopharyngeal neuralgia
- Postherpetic neuralgia
- Numb chin syndrome
- Vascular
- Giant cell arteritis
- Malignancy
- Atypical
- Persistent idiopathic facial pain
Oral:
- Dental
- Caries
- Pulpitis
- Periapical disease
- Cracked tooth
- Sensitivity
- Alveolar osteitis
- Periodontal disease
- Pericoronitis
- Nondental
- Salivary gland disorders
- Sinusitis
- Cancer
- Mucosal disorders
- Burning mouth syndrome
- Atypical odontalgia
References:
- JFP Vol 64,No 9 Sep 2015
Common Dental Emergencies
- Abscess
- Localized bacterial infection
- Localized pain and swelling
- Treatment: incision and drainage, root canal, or extraction
- Cellulitis
- Diffuse bacterial infection of soft tissue
- Pain, erythema, and swelling
- Treatment: antibiotics, root canal, or extraction
- Irreversible pulpitis
- Inflammation of the tooth pulp
- Poorly localized pain
- Treatment: root canal or extraction
- Pericoronitis
- Inflammed gum over incompletely erupted tooth
- Pain, erythmea, and swelling
- Treatment: irrigation; antibiotics for concurrent cellulitis
- Reversible pulpitis
- Inflammation of the tooth pulp
- Hot/cold sensitivity
- Treatment: filling
- Tooth avulsion
- Missing tooth
- Treatment: reimplantation or splinting
- Tooth fracture
- Broken tooth
- Visible fracture; confirm with radiography
- Treatment: filling, root canal, or extraction
- Tooth luxation
- Loose tooth
- Confirm with radiography
- Treatment: splinting, root canal, or extraction
References:
- AFP Vol 98 No 11 Dec 2018
Antibiotics Commonly Used for Odontogenic Infections
- Amoxicillin
- 500mg tid or 1g po bid
- Amoxicillin/clavulanate
- 500/125mg po tid or 875/125mg po bid
- Clindamycin
- 300 to 600mg po tid
- Penicillin
- 1.2 to 2.4 million units/d IM or IV
- 250 to 500 mg po qid
References:
- AFP Vol 98 No 11 Dec 2018
Back pain
Red Flags:
- Abnormal gait with lack of heel to toe ambulation
- Absence of perineal reflex
- Acute presentation of bilateral sciatica
- Acute urinary retention
- Drop foot or inability to dorsiflex the foot
- Intravenous drug abuse
- Progressive neuromotor or sensory loss
- Recent diagnosis of malignancy
- Recent infection
- Recumbent worsening of pain
- Saddle block anesthesia
- Urinary and/or bowel incontinence
Back Pain Differencial Diagnosis:
- AAA
- Ankylosing spondylitis
- Epidural abscess
- Fracture of the pars interarticularis
- Metastatic malignancy
- Osteoarthritis of the hip
- Osteoporosis
- Piriformis syndrome
- Radiculitis
- Sacroiliac joint dysfunction
- Traumatic fracture
- Trochanteric bursitis
- Varicella zoster virus
Treatment:
- NSAIDs (MA/RCT), opioids (MA/RCT), and topiramate (RCT) are more efective than placebo in the short term for nonspecific low back pain - LOE A
- Acetaminophen, muscle relaxants, lidocaine patches, and TENS are NOT more effetive than placebo in the treatment of chronic low back pain - LOE B
References:
- AFP Vol 91 No 10 May 2015
Causes/Red Flags
- Mechanical back pain
- Strain: Trauma, motor deficit, age >50yrs
- Herniated disc: Trauma motor defecit
- Osteoporosis, spinal stenosis, fractures: Age >50yrs, trauma, steroid use
- Scoliosis, kyphosis, lordosis: Age >50yrs
- Nonmechanical back pain
- Neopastic (multiple myeloma, metastatic carcinoma, lymphoma, leukemia, spinal cord tumors): Fever, weight loss, age >50yrs, history of malignancy, motor defecit
- Infection (osteolyelitis, septic discitis, epidural abscess, bacterial endocarditis): Fever, illicit drug use, steroid use, elevated ESR, motor defecit
- Inflammatory conditions (ankylosing spondylitis, psoriatic spondylitis, Reiter's syndrome, inflammatory bowel disease): Fever, elevated ESR, weight loss, age >50yrs
- Paget's disease: Fever, age >50yrs
References:
- J Fam Pract. 2015 Feb;64(2):110-112.
Modified Duty Recommendations
Mild Severity:
- Clerical (up to 20lbs)
- 0 days
- Manual (up to 50lbs)
- 7-10 days
Severe Severity:
- Clerical (up to 20lbs)
- 0-3 days
- Manual (up to 50lbs)
- 14-17 days
- Heavy manual (over 50lbs)
- 35 days
References:
- AFP Vol 76 No 10 Nov 2007
Causes/Red flags
Mechanical back pain
- Strain: Trauma, motor deficit, age >50yrs
- Herniated disc: Trauma motor defecit
- Osteoporosis, spinal stenosis, fractures: Age >50yrs, trauma, steroid use
- Scoliosis, kyphosis, lordosis: Age >50yrs
Nonmechanical back pain
- Neopastic (multiple myeloma, metastatic carcinoma, lymphoma, leukemia, spinal cord tumors): Fever, weight loss, age >50yrs, history of malignancy, motor defecit
- Infection (osteolyelitis, septic discitis, epidural abscess, bacterial endocarditis): Fever, illicit drug use, steroid use, elevated ESR, motor defecit
- Inflammatory conditions (ankylosing spondylitis, psoriatic spondylitis, Reiter's syndrome, inflammatory bowel disease): Fever, elevated ESR, weight loss, age >50yrs
- Paget's disease: Fever, age >50yrs
References:
- J Fam Pract. 2015 Feb;64(2):110-112.
Knee pain
Nontraumatic Knee Pain Differential Diagnosis:
- Patellofemoral pain syndrome
- Chronic dislocation
- Patellar tendinopathy
- Iliotibial band syndrome
- Plica syndrome
- Anserine bursitis
- Poplitial cyst
- Knee effusion
MSK Pain Guidelines edit
- Topical NSAIDs are the most effective intervention for acute musculoskeletal pain other than low back pain.
- Although oral NSAIDs and acetaminophen are effective for acute pain relief, combining them does not improve effectiveness.
- Although moderately effective for pain relief, opioids increase gastrointestinal and neurologic adverse effects and lead to long-term use in 6% of people treated.
- Acupressure and TENS techniques are effective nonpharmacologic options for acute pain.
Non-narcotic Medications
Gabapentin:
- Oral gabapentin (1200-3600 mg/d for 4-12 weeks) for moderate to severe neuropathic pain from postherpetic neuralgia or painful diabetic neuropathy is associated with pain reduction of at least 50% in 14%-17% more patients than placebo
References:
- JAMA Vol 319 No 8 Feb 2018
- J Fam Pract. 2023 September;72(7):320-321 | doi: 10.12788/jfp.0654
Opioids
See also:
Elements of optimal opioid prescribing:
- Gather patient history (include patient interview) and conduct a physical exam.
- Assess pain.
- Employ risk-mitigation strategies.
- Confirm use of prescribed and illicit substances using PDMP and UDT.
- Clarify indications for opioid therapy and medical necessity.
- Enact a controlled-substance agreement with the patient.
- Set goals and optimize nonopioid and nonpharmacologic
- Initiate appropriate agents at appropriate doses (prescribe naloxone to accompany opioid prescriptions).
- Follow-up, monitor, and evaluate progress toward goal of therapy.
- Discontinue therapy when indicated and follow tapering regimen.
References:
- JFP Jul 2020 Vol 69, No 6
Opioid Response Monitoring
At every visit, use the five As:
- Analgesia
- Activities of daily living
- Adverse or side effects
- Apparent drug related behaviors
- Affect
Signs and symptoms that may suggest a problematic response:
- excessive sleeping or days and nights turned around
- diminished appetite
- short attention span or inability to concentrate
- mood volatility, especially irritability
- lack of involvement with others
- impaired functioning due to drug effects
- use of the opioid to regress instead of re-engaging in life
- lack of attention to hygiene and appearance
| Monitoring Tool | Low Risk | Med Risk | High Risk |
|---|---|---|---|
| Urine drug test | 1-2 yrs | 6-12 mo | 3-6 mo |
| State Prescription Drug Monitoring Program | 2x/yr | 3x/yr | 4x/yr |
PEG scale for assessing pain and function
PEG score = average of 3 individual question scores (30% improvement from baseline is clinically meaningful)
- Q1: What number, from 0-10, best describes your pain in the past week?
- 0 = "no pain," 10 = "worst you can imagine"
- Q2: What number from 0-10 best describes how, during the past week, pain has interfered with your enjoyment in life?
- 0 = "not at all," 10 = "complete interference"
- Q3: What number from 0-10 describes how, during the past week, pain has interfered with your general activity?
- 0 = "not at all," 10 = "complete interference
References:
- JFP Jul 2020 Vol 69, No 6
Opioid Prescribing FL Law
Per HB 21 Florida Law - Effective July 1, 2018
- Acute pain - Schedule II opioid prescription limited to 3 days supply unless prescriber believes there is a medically necessary reason to prescribe up to a 7 day supply
- Does not apply to cancer, terminal illness, for palliative care, or trauma patients with Injury Severity Score of >9
- Applies after discharge and not inpatient
- Before prescribing a controlled substance, the provider must consult the Prescription Drug Monitoring Program (PDMP) also referenced as e-forsce
- All practitioners must complete a 2 hour CME before January 31, 2019
Electronic-Florida Online Reporting of Controlled Substance Evaluation Program (E-FORCSE): https://flpdm-ph.hidinc.com/fllogappl/bdflpdmqlog/pmqhome.html
Opioid Conversion Factor
| Morphine | 1 mg |
|---|---|
| Buprenorphine film/tablet | 3 (mg) 30 |
| Buprenorphine patch 4 (mcg/hr) | 12.6 mg |
| Buprenorphine film (mcg) | 0.03 mg |
| Butorphanol (mg) | 7 mg |
| Codeine (mg) | 0.15 mg |
| Dihydrocodeine (mg) | 0.25 mg |
| Fentanyl buccal or SL tablets, or lozenge/troche 5 (mcg) | 0.13 mg |
| Fentanyl film or oral spray 6 (mcg) | 0.18 mg |
| Fentanyl nasal spray 7 (mcg) | 0.16 mg |
| Fentanyl patch 8 (mcg) | 7.2 mg mg |
| Hydrocodone (mg) | 1 mg |
| Hydromorphone (mg) | 4 mg |
| Levorphanol tartrate (mg) | 11 mg |
| Meperidine hydrochloride (mg) | 0.1 mg |
| Methadone 9 (mg) | 3 mg |
| >0, <= 20 | 4 mg |
| >20, <=40 | 8 mg |
| >40, <=60 | 10 mg |
| >60 | 12 mg |
| Morphine (mg) | 1 mg |
| Opium (mg) | 1 mg |
| Oxycodone (mg) | 1.5 mg |
| Oxymorphone (mg) | 3 mg |
| Pentazocine (mg) | 0.37 mg |
| Tapentadol 10 (mg) | 0.4 mg |
| Tramadol (mg) | 0.1 mg |
Risk:
- >50 MME/Day is high risk
- >90 MME/Day requires referral
Do not use the calculated dose in MMEs to determine dosage for converting one opioid to another—the new opioid should be lower to avoid unintentional overdose caused by incomplete cross-tolerance and individual differences in opioid pharmacokinetics. Consult the medication label.
References:
Opioid Tapering/Withdrawal
Recommendations for discontinuing and tapering opioids
- Engage the patient in all discussions regarding discontinuation/tapering.
- Consider switching patient from IR to ER opioids on a fixed-dose schedule to assist some patients in adhering to the taper/discontinuation plan.
- Collaborate with a multidisciplinary team to assist with scheduling dose reductions.
- Gradually reduce 5%-10% of the original MME every 1-4 weeks until 30% of the original dose is reached, followed by a weekly reduction of 10% of the remaining dose.
- Increase the taper rate when opioid doses reach a low level (eg, < 15 mg/d MME), since formulations of opioids may not be available to allow smaller decreases.
- Use a schedule for tapering, including planned dates, doses, frequency, total dose/d, and quantities that will be required for the prescription.
- Do not reverse the taper in cases of withdrawal symptoms; rate may be slowed or paused while monitoring for and managing withdrawal symptoms.
- Manage opioid abstinence syndrome with clonidine 0.1-0.2 mg orally every 6 h or transdermal clonidine patch 0.1 mg/24 h weekly during the taper.
Consider tapering:
- Failure to provide significant analgesia despite incremental increasing doses
- Lack of functional improvements over time
- Prescription of high dosages of opioids (MME >90/d)
- Significant risk factors
- OSA
- Prolonged QT
- Pulmonary disease
- Adverse effects of medication interfere with quality of life
- Dangerous coprescribing: benzodiazepines, muscle relaxants, other sedatives
- Patient request
Velocity:
- Standard recommendation is decrease MME by 5-10% every 1-2 weeks
- Most can tolerate less than 5% every month
- Try to keep the same dosing cadence (bid, tid, etc)
- Breaks in taper are appropriate
Validation
- Body pain will worsen each time opioid is decreased but with time and body adjusting to new dose (approx 4 weeks), the pain level will return to baseline
Behavioral Health:
- Practice Mindfulness
- Opposite Action skills
Opioid withdrawal symptoms:
- Abdominal cramping
- Agitation
- Anxiety
- Diarrhea
- Dilated pupils
- Dysphoria
- Goose bumps
- Insomnia
- Irritability
- Lacrimation
- Myalgias
- Nausea
- Rhinorrhea
- Sweating
- Vomiting
- Yawning
Medications to relieve opioid withdrawal:
- Abdominal cramping
- dicyclomine 20 mg q6-8 prn
- Anxiety
- Hydroxyzine 25-50 mg q6-8 prn
- diphenhydramine 25 mg q6 prn
- Autonomic symptoms such as rhinorrhea, diarrhea, sweating, tachycardia, hypertension
- Clonidine 0.1-0.3 mg q6-8 prn
- baclofen 5-10 mg q8 prn
- gabapentin 100-300 mg q8 prn
- Diarrhea
- Antidiarrheal agents (loperamide 2-4 mg)
- Insomnia
- trazodone 100-300 mg qhs prn
- Hydroxyzine 25-50 mg q6-8 prn
- Irritability, pain, sleep disturbance:
- Antidepressants (trazodone)
- Myalgia
- NSAIDs - ibuprofen 400 mg q4
- acetaminophen 650 mg q6 prn
- Nausea
- prochlorperazine 10 mg q4 prn
- Neuropathic pain
- Antiepileptics
References:
- AFP Vol 101 No 1 Jan 2020
- JFP Jul 2020 Vol 69, No 6
- Additional resource: https://www.cdc.gov/drugoverdose/pdf/clinical_pocket_guide_tapering-a.pdf
- AFP Vol 111 No 6 Jun 2025
Postherpetic neuralgia
Treatment:
- Topical therapy with lidocaine or capsaicin
- Systemic therapy with gabapentin, pregabalin, or TCAs
References:
- NEJM 371;16 Oct 2014
Resources
Providers' Clinical Support System http://pcss-o.org
Butrans (Buprenorphine Waiver Notification)
Notification of Intent to Use Schedule III, IV, or V Opioid Drugs for the Maintenance and Detoxification Treatment of Opiate Addiction by a "Qualifying Physician" under 21 USC § 823(g)(2) Note: Notification is required by § 303(g)(2), Controlled Substances Act (21 USC § 823(g)(2)). See instructions below.
SMA-167 Form Approved: 0930-0234
Date: 01/31/2023
See OMB Statement Below
Your Waiver Notification has been successfully submitted. Please check your spam/junk folders. If you do not see an email attachment in your inbox within 45 days, please contact the Buprenorphine Center at 866-BUP-CSAT (866-287-2728). If you submitted an increase waiver DO NOT send your training certificate. If this is your first time applying and you did not upload your training, please forward via email to infobuprenorphine@samhsa.hhs.gov.
CDC Opioids
When CONSIDERING long-term opioid therapy
- Set realistic goals for pain and function based on diagnosis
- (eg, walk around the block).
- Check that non-opioid therapies tried and optimized.
- Discuss benefits and risks (eg, addiction, overdose) with patient.
- Evaluate risk of harm or misuse.
- Discuss risk factors with patient.
- Check prescription drug monitoring program (PDMP) data.
- Check urine drug screen.
- Set criteria for stopping or continuing opioids.
- Assess baseline pain and function (eg, PEG scale).
- Schedule initial reassessment within 1– 4 weeks.
- Prescribe short-acting opioids using lowest dosage on product labeling;
- match duration to scheduled reassessment.
If RENEWING without patient visit
- Check that return visit is scheduled ≤ 3 months from last visit.
When REASSESSING at return visit
- Continue opioids only after confirming clinically meaningful improvements
- in pain and function without significant risks or harm.
- Assess pain and function (eg, PEG); compare results to baseline.
- Evaluate risk of harm or misuse:
- Observe patient for signs of over-sedation or overdose risk.
- If yes: Taper dose.
- Check PDMP.
- Check for opioid use disorder if indicated (eg, difficulty controlling use).
- If yes: Refer for treatment.
- Observe patient for signs of over-sedation or overdose risk.
- Check that non-opioid therapies optimized.
- Determine whether to continue, adjust, taper, or stop opioids.
- Calculate opioid dosage morphine milligram equivalent (MME).
- If ≥50 MME /day total (≥50 mg hydrocodone; ≥33 mg oxycodone),
- increase frequency of follow-up; consider offering naloxone.
- Avoid ≥90 MME /day total (≥90 mg hydrocodone; ≥60 mg oxycodone),
- or carefully justify; consider specialist referral.
- Schedule reassessment at regular intervals (≤ 3 months).
EVIDENCE ABOUT OPIOID THERAPY
- - Benefits of long-term opioid therapy for chronic pain not well supported by evidence.
- - Short-term benefits small to moderate for pain; inconsistent for function.
- - Insufficient evidence for long-term benefits in low back pain, headache, and fibromyalgia.
NON-OPIOID THERAPIES
- Use alone or combined with opioids, as indicated:
- - Non-opioid medications (eg, NSAIDs, TCAs, SNRIs, anti-convulsants).
- - Physical treatments (eg, exercise therapy, weight loss).
- - Behavioral treatment (eg, CBT).
- - Procedures (eg, intra-articular corticosteroids).
EVALUATING RISK OF HARM OR MISUSE
- Known risk factors include:
- - Illegal drug use; prescription drug use for nonmedical reasons.
- - History of substance use disorder or overdose.
- - Mental health conditions (eg, depression, anxiety).
- - Sleep-disordered breathing.
- - Concurrent benzodiazepine use.
- Urine drug testing: Check to confirm presence of prescribed substances and for undisclosed prescription drug or illicit substance use.
- Prescription drug monitoring program (PDMP): Check for opioids or benzodiazepines from other sources.
ASSESSING PAIN & FUNCTION USING PEG SCALE
- PEG score = average 3 individual question scores (30% improvement from baseline is clinically meaningful)
- Q1: What number from 0 –10 best describes your pain in the past week?
- 0 = "no pain", 10 = "worst you can imagine"
- Q2: What number from 0 –10 describes how, during the past week, pain has interfered with your enjoyment of life?
- 0 = "not at all", 10 = "complete interference"
- Q3: What number from 0 –10 describes how, during the past week, pain has interfered with your general activity?
- 0 = "not at all", 10 = "complete interference"
- Q1: What number from 0 –10 best describes your pain in the past week?
| MEDICATION | MAGNITUDE OF BENEFITS | HARMS | COMMENTS |
|---|---|---|---|
| Acetaminophen | Small | Hepatotoxic, particularly at higher doses | First-line analgesic, probably less effective than NSAIDs |
| NSAIDs | Small-moderate | Cardiac, GI, renal | First-line analgesic, COX-2 selective NSAIDs less GI toxicity |
| Gabapentin/pregabalin | Small-moderate | Sedation, dizziness, ataxia | First-line agent for neuropathic pain; pregabalin approved for fibromyalgia |
| Tricyclic antidepressants and serotonin/norephinephrine reuptake inhibitors | Small-moderate | TCAs have anticholinergic and cardiac toxicities; SNRIs safer and better tolerated | First-line for neuropathic pain; TCAs and SNRIs for fibromyalgia, TCAs for headaches |
| Topical agents (lidocaine, capsaicin, NSAIDs) | Small-moderate | Capsaicin initial flare/burning, irritation of mucus membranes | Consider as alternative first-line, thought to be safer than systemic medications. Lidocaine for neuropathic pain, topical NSAIDs for localized osteoarthritis, topical capsaicin for musculoskeletal and neuropathic pain |
Low back pain
- Self-care and education in all patients; advise patients to remain active and limit bedrest
- Nonpharmacological treatments: Exercise, cognitive behavioral therapy, interdisciplinary rehabilitation
- Medications
- First-line: acetaminophen, non-steroidal anti inflammatory drugs (NSAIDs)
- Second-line: Serotonin and norepinephrine reuptake inhibitors (SNRIs)/tricyclic antidepressants (TCAs)
Migraine
- Preventive treatments
- Beta-blockers
- TCAs
- Antiseizure medications
- Calcium channel blockers
- Non-pharmacological treatments (Cognitive behavioral therapy, relaxation, biofeedback, exercise therapy)
- Avoid migraine triggers
- Acute treatments
- Aspirin, acetaminophen, NSAIDs (may be combined with caffeine)
- Antinausea medication
- Triptans-migraine-specific
Neuropathic pain
- Medications: TCAs, SNRIs, gabapentin/pregabalin, topical lidocaine
Osteoarthritis
- Nonpharmacological treatments: Exercise, weight loss, patient education
- Medications
- First-line: Acetamionphen, oral NSAIDs, topical NSAIDs
- Second-line: Intra-articular hyaluronic acid, capsaicin (limited number of intra-articular glucocorticoid injections if acetaminophen and NSAIDs insufficient)
Fibromyalgia
- Patient education: Address diagnosis, treatment, and the patient's role in treatment
- Nonpharmacological treatments: Low-impact aerobic exercise (e.g., brisk walking, swimming, water aerobics, or bicycling), cognitive behavioral therapy, biofeedback, interdisciplinary rehabilitation
- Medications
- FDA-approved: Pregabalin, duloxetine, milnacipran
- Other options: TCAs, gabapentin
When to conduct urine drug testing:
- All patients on long-term opioid therapy should have periodic urine drug tests (UDT). Medical experts agree that an annual UDT for all patients should be standard practicei. Subsequent UDTs should be determined on an individual patient basis, at the discretion of the clinician. Before ordering a UDT, have a plan for responding to unexpected results.
- IMMUNOASSAY
- Will show false positives: poppy seeds, quinolone antibiotics, over-the-counter medications
- Screens for presence of drugs or a panel of drugs: amphetamine, marijuana, PCP, cocaine, natural opiates (morphine/ codeine/thebaine but without differentiation). Heroin is metabolized to morphine and can therefore be detected; a separate screening assay specific to heroin is also available.
Reference:
Controlled Meds edit
SCH. II
| BRAND | GENERIC | FUNCTION |
| Percocet® | Oxycodone | |
| + APAP | Pain Relief | |
| Oxycontin® | Oxycodone | Pain Relief |
| Concerta® | Methylphenidate | ADHD |
| Adderall® | Amphetamine + | |
| Dextroamphetamine | ADHD | |
| Vyvanse® | Lisdexamfetamine | ADHD |
| Duragesic® | Fentanyl Patch | Pain Relief |
| Methadose® | Methadone | Opoid Recovery |
SCH. III
| BRAND | GENERIC | FUNCTION |
| Vicodin® | APAP + | |
| Hydrocodone | Pain Relief | |
| Tylenol 3® | Codeine + APAP | Pain Relief |
| Suboxone® | Buprenorphine | Opoid Recovery |
| Tussionex® | Hydrocodone + | |
| Chlorpheniramine | Cough suppressant | |
| + Antihistamine |
SCH. IV
| BRAND | GENERIC | FUNCTION |
| Xanax® | Alprazolam | Benzodiazepine |
| Ambiem® | Zolpidem | Sleep Aid |
| Klonopin® | Clonazepam | Benzodiazepine |
| Ativan® | Lorazepam | Benzodiazepine |
| Darvocet® | Propoxyphene + APAP | Pain Relief |
| Valium® | Diazepam | Benzodiazepine |
| Restoril® | Temazepam | Sleep Aid |
| Adipex® | Phentermine | Appetite Supressant |
| Lunesta® | Eszopiclone | Sleep Aid |
| Soma® | Carisoprodol | Muscle relaxer |
Buprenorphone edit
Buprenorphine is safer than Schedule II opioids in patients with chronic pain who have an increased risk of life-threatening opioid-related adverse events (e.g., high BMI/obstructive sleep apnea, a comorbid psychiatric diagnosis, pulmonary disease, concomitant use of drugs known to increase risk [benzodiazepines, gabapentin, pregabalin, muscle relaxants, alcohol], and those taking high morphine milligram equivalents [MME]). The risk of respiratory depression with buprenorphine monotherapy is very low. However, when buprenorphine is used in combination with nonopioid sedatives or anticonvulsants, respiratory depression is an important risk to consider. Many people have incorrectly characterized buprenorphine as less effective for pain because it is considered a partial µ-opioid agonist. In studies it has shown equal and sometimes greater efficacy in pain control than full µ-opioid receptor agonists. Buprenorphine is a full agonist at the opioid receptor-like 1 (ORL1). In addition, it is an antagonist at the δ- and k-opioid receptors, which lessen constipation, dysphoria, and abuse potential.
A recent guideline recommended consideration of buprenorphine for patients in the following categories:
- Lack of efficacy (including tolerance or hyperalgesia)
- Risk of adverse events
- Concern from health care providers regarding risk of addiction, misuse, and/or overdose death
- The limited ability to utilize oral formulations in patients with altered gastrointestinal motility/function
- A patient is receiving immediate-release treatment and would benefit from a longer-acting analgesic with a relatively favorable safety profile
A protocol that has been recommended for transition of this patient who is taking less than 90 MME would be:
- Discontinuing oxycodone after the last nighttime dose.
- Considering initiating an adrenergic α2-agonist (e.g., clonidine, lofexidine) or an immediate-release opioid (e.g., current opioid) to reduce the symptoms of withdrawal.
- Initiating buprenorphine the following morning per the prescribing information, as either 10-µg/h transdermal buprenorphine or 150-µg buccal buprenorphine twice daily. Titrate buprenorphine as needed for pain per recommendations in the prescribing information.
For those taking more than 90 MME, the dose of buprenorphine would be double the above recommendation.
Spinal manipulative therapy for acute low‐back pain edit
Low‐back pain is a common and disabling disorder, representing a great burden both to the individual and society. It often results in reduced quality of life, time lost from work, and substantial medical expense. Spinal manipulative therapy (SMT) is widely practised by a variety of healthcare professionals worldwide and is a common choice for the treatment of low‐back pain. The effectiveness of this form of therapy for the management of acute low‐back pain is, however, not without dispute.
For this review, acute low‐back pain was defined as pain lasting less than six weeks. Only cases of low‐back pain not caused by a known underlying condition, for example, infection, tumour, or fracture, were included. Also included were patients whose pain was predominantly in the lower back but may also have radiated (spread) into the buttocks and legs.
SMT is known as a 'hands‐on' treatment directed towards the spine, which includes both manipulation and mobilization. The therapist applies manual mobilization by passively moving the spinal joints within the patient's range of motion using slow, passive movements, beginning with a small range and gradually increasing to a larger range of motion. Manipulation is a passive technique whereby the therapist applies a specifically directed manual impulse, or thrust, to a joint at or near the end of the passive (or physiological) range of motion. This is often accompanied by an audible 'crack'.
In this review, a total of 20 randomized controlled trials (RCTs) (representing 2674 participants) assessing the effects of SMT in patients with acute low‐back pain were identified. Treatment was delivered by a variety of practitioners, including chiropractors, manual therapists, and osteopaths. Approximately one‐third of the trials were considered to be of high methodological quality, meaning these studies provided a high level of confidence in the outcome of SMT.
Overall, we found generally low to very low quality evidence suggesting that SMT is no more effective in the treatment of patients with acute low‐back pain than inert interventions, sham (or fake) SMT, or when added to another treatment such as standard medical care. SMT also appears to be no more effective than other recommended therapies. SMT appears to be safe when compared to other treatment options but other considerations include costs of care.
Reference:
Understanding Buprenorphine for Use in Chronic Pain: Expert Opinion edit
Objective
An expert panel convened to reach a consensus on common misconceptions surrounding buprenorphine, a Schedule III partial µ-opioid receptor agonist indicated for chronic pain. The panel also provided clinical recommendations on the appropriate use of buprenorphine and conversion strategies for switching to buprenorphine from a full µ-opioid receptor agonist for chronic pain management. Methods
The consensus panel met on March 25, 2019, to discuss relevant literature and provide recommendations on interpreting buprenorphine as a partial µ-opioid receptor agonist, prescribing buprenorphine before some Schedule II, III, or IV options, perioperative/trauma management of patients taking buprenorphine, and converting patients from a full µ-opioid receptor agonist to buprenorphine. Results
The panel recommended that buprenorphine's classification as a partial µ-opioid receptor agonist not be clinically translated to mean partial analgesic efficacy. The panel also recommended that buprenorphine be considered before some Schedule II, III, or IV opioids in patients with a favorable risk/benefit profile on the basis of metabolic factors, abuse potential, and tolerability and that buprenorphine be continued during the perioperative/trauma period. In addition, switching patients from a full µ-opioid receptor agonist to buprenorphine should be considered with no weaning period at starting doses that are based on the previous opioid dose. Conclusions
These recommendations provide a framework for clinicians to address most clinical scenarios regarding buprenorphine use. The overall consensus of the panel was that buprenorphine is a unique Schedule III opioid with favorable pharmacologic properties and a safety profile that may be desirable for chronic pain management.
Reference:
Urine Drug Testing edit
Immunoassays for opioids reliably detect morphine, heroin, and codeine but do not reliably detect synthetic and semisynthetic opioids (e.g., oxycodone, fentanyl, methadone, tramadol).
If it is important to confirm if a patient is taking a synthetic or semisynthetic opioid, another test is needed.
Some common medications that cause false-positive results on UDT include:
- Amphetamines: bupropion, phenylephrine, promethazine, pseudoephedrine, ranitidine, trazodone
- Benzodiazepines: sertraline, oxaprozin
- Cannabinoids: dronabinol, efavirenz, proton pump inhibitors, NSAIDs
- Phencyclidine: dextromethorphan, diphenhydramine, doxylamine, ibuprofen, tramadol, venlafaxine
The immunoassay for cocaine is highly sensitive and specific for cocaine and its metabolite benzoylecgonine. A positive test for cocaine almost always signals cocaine use and a negative test reliably rules it out.
Secondhand marijuana smoke is not sufficient to result in a positive UDT for cannabis at the typical cutoffs for office-based immunoassays. Similarly, eating baked goods covered with poppy seeds is not typically sufficient to result in a positive UDT for opioids.
Reference:
Medication edit
| Term | Definition |
|---|---|
| Addiction | Neurobiologic, multifactorial disease characterized by impaired control, compulsive drug use, and continued use despite harm |
| Physical dependence | Normal adaptive state that results in withdrawal symptoms if the drug is abruptly stopped or decreased |
| Pseudoaddiction | Relief-seeking behaviors misinterpreted as drug-seeking behaviors that resolve upon institution of effective analgesic therapy |
| Substance abuse | Use of any substance for purposes that are non-therapeutic or are not those for which it is prescribed |
| Tolerance | Physiologic state from regular drug use in which an increased dosage is needed to produce the same effect |
Reference:
Monitoring Medication for Chronic Nonmalignant Pain edit
Six A's for Monitoring Patients with Chronic Nonmalignant Pain Taking Controlled Substances
- Analgesia (assess pain relief)
- Affect (evaluate mood)
- Activities (evaluate activities of daily living, function, and quality of life)
- Adjuncts (nonpharmacologic or nonopioid treatments)
- Adverse effects (side effects of treatments)
- Aberrant behavior (tolerance, dependence, and addiction)
Reference:
Opioid Appropriate Documentation of Follow-up Visits edit
If the patient is on a stable dose of medication and is doing well, then a visit every 1 to 2 months is generally considered reasonable. If the patient is on a relatively low dose of opioids, then 3 months is often adequate. If the patient has significant psychosocial issues, is a recovering addict, has exhibited difficulty with compliance, has a new additional pain issue, or the dose is being adjusted, etc., then the patient may need to be seen weekly, and, at times, there may even need to be telephone contact in between the visits.
The frequency of a detailed physical exam focuses on the diagnosis (not a comprehensive physical exam involving the entire body), depending on the patient's stability.
Because insurance companies generally pay for only 30-day quantities of a medication and the Drug Enforcement Agency (DEA) does not permit Schedule II prescriptions to have any refills on them, the question arises about what to do for the second month (the month between appointments) for stable patients who medically need to be seen only every 2 months. Published guidelines do not mandate an office visit when a patient needs a prescription for a controlled substance. The DEA permits writing multiple prescriptions for Schedule II drugs for up to 90 days as long they are dated on the date they were written. Within the body of the second and subsequent prescriptions, write "Do not fill until . . . ." Pharmacists are not permitted to fill a prescription before that date.
Document the 5 A's:
- Analgesia: The level of pain, such as on a scale of 1 to 10.
- Activities of daily living: What the patient actually does (be as specific as possible: "Walking the dog for 15 minutes, about half a mile.")
- Adverse effects: For example, ask about constipation, which can be an ongoing problem.
- Aberrant drug-related behaviors: For example, "Ran out early because. . ." or "Leaving on vacation, needs early refill," or "Urine positive for cocaine."
Reference:
CDC Opioid Recommendations edit
Key Recommendations
- Nonpharmacologic and nonopioid pharmacologic therapies are preferred for chronic pain. Opioid therapy should be considered only when benefits for both pain and function are anticipated to outweigh the risks. If opioids are used, they should be combined with nonpharmacologic and nonopioid pharmacologic therapy as appropriate.
- Realistic treatment goals for pain and function should be established before initiation of opioid therapy. Opioid treatment should be continued only if there is meaningful improvement in pain and function that outweighs risk.
- When starting opioid therapy for chronic pain, the lowest effective dose of immediate-release opioids should be prescribed instead of extended-release/long-active (ER/LA) opioids.
- Benefits and risks should be reassessed when increasing dosages to ≥50 morphine milligram equivalents (MME)/day. Dosages ≥90 MME/day should be carefully justified or avoided if possible.
- For acute pain, the lowest effective dose of immediate-release opioids should be prescribed in no greater quantity than is needed for severe pain.
- Benefits and harms should be evaluated with patients within one to four weeks of initiating or escalating dose of opioids for chronic pain and at least every three months thereafter. If benefits do not outweigh the harms, a plan to taper opioids and optimize other therapies should be developed.
- Risk factors for opioid-related harms should be evaluated prior to initiation and periodically during treatment. Strategies to mitigate risk should be developed, including offering naloxone to those at increased risk for overdose.
- A patient's history of controlled substance prescriptions using a prescription drug monitoring program (PDMP). PDMP data should be reviewed when starting opioid therapy and periodically during treatment.
- Urine drug testing may be used prior to initiating opioid therapy and periodically during treatment to asses for controlled prescription medications as well as illicit drugs.
- Co-prescription of opioids and benzodiazepines should be avoided whenever possible.
- Evidence-based treatment including medication-assisted treatment with buprenorphine or methadone and behavioral therapies should be offered to patients with opioid use disorder.
Reference:
Cannabis-Based Products for Chronic Pain edit
Background:
- Contemporary data are needed about the utility of cannabinoids in chronic pain.
Purpose:
- To evaluate the benefits and harms of cannabinoids for chronic pain.
Data Sources:
- Ovid MEDLINE, PsycINFO, EMBASE, the Cochrane Library, and Scopus to January 2022.
Study Selection:
- English-language, randomized, placebo-controlled trials and cohort studies (≥1 month duration) of cannabinoids for chronic pain.
Data Extraction:
- Data abstraction, risk of bias, and strength of evidence assessments were dually reviewed. Cannabinoids were categorized by THC-to-CBD ratio (high, comparable, or low) and source (synthetic, extract or purified, or whole plant).
Data Synthesis:
- Eighteen randomized, placebo-controlled trials (n = 1740) and 7 cohort studies (n = 13 095) assessed cannabinoids.
- Studies were primarily short term (1 to 6 months); 56% enrolled patients with neuropathic pain, with 3% to 89% female patients.
- Synthetic products with high THC-to-CBD ratios (>98% THC) may be associated with moderate improvement in pain severity and response (≥30% improvement) and an increased risk for sedation and are probably associated with a large increased risk for dizziness.
- Extracted products with high THC-to-CBD ratios (range, 3:1 to 47:1) may be associated with large increased risk for study withdrawal due to adverse events and dizziness.
- Sublingual spray with comparable THC-to-CBD ratio (1.1:1) probably is associated with small improvement in pain severity and overall function and may be associated with large increased risk for dizziness and sedation and moderate increased risk for nausea.
- Evidence for other products and outcomes, including longer-term harms, were not reported or were insufficient.
Limitation:
- Variation in interventions; lack of study details, including unclear availability in the United States; and inadequate evidence for some products.
Conclusion:
- Oral, synthetic cannabis products with high THC-to-CBD ratios and sublingual, extracted cannabis products with comparable THC-to-CBD ratios may be associated with short-term improvements in chronic pain and increased risk for dizziness and sedation.
- Studies are needed on long-term outcomes and further evaluation of product formulation effects.
Reference:
- McDonagh MS, Morasco BJ, Wagner J, Ahmed AY, Fu R, Kansagara D, Chou R. Cannabis-Based Products for Chronic Pain : A Systematic Review. Ann Intern Med. 2022 Aug;175(8):1143-1153. doi: 10.7326/M21-4520. Epub 2022 Jun 7. PMID: 35667066.
- https://www.acpjournals.org/doi/full/10.7326/M21-4520
Study: Physician Empathy and Chronic Pain Outcomes edit
Key Points
- Question
- Is physician empathy associated with the outcomes of patients with chronic pain?
- Findings
- In this cohort study that included 1470 adults with chronic low back pain, patients treated by very empathic physicians reported having significantly better and clinically relevant outcomes pertaining to pain, function, and health-related quality of life over 12 months compared with patients treated by slightly empathic physicians. Physician empathy was more strongly associated with favorable outcomes than were nonpharmacological treatments, opioid therapy, and lumbar spine surgery.
- Meaning
- These findings suggest that physician empathy is an important aspect of the patient-physician relationship and was associated with better outcomes among patients with chronic pain.
Abstract
- Importance
- Empathy is an aspect of the patient-physician relationship that may be particularly important in patients with chronic pain.
- Objective
- To measure the association of physician empathy with pain, function, and health-related quality of life (HRQOL) among patients with chronic low back pain.
- Design, Setting, and Participants
- This cohort study included adult enrollees from the Pain Registry for Epidemiological, Clinical, and Interventional Studies and Innovation national pain research registry. Study dates were from April 1, 2016, to July 25, 2023, with up to 12 months of follow-up.
- Exposure
- Physician empathy was assessed with the Consultation and Relational Empathy measure and dichotomized to yield very empathic physician and slightly empathic physician groups.
- Main Outcomes and Measures
- Main outcomes were patient-reported pain, function, and HRQOL measured with a numerical rating scale for low back pain intensity, the Roland-Morris Disability Questionnaire for back-related disability, and the Patient-Reported Outcomes Measurement Information System for HRQOL deficits pertaining to anxiety, depression, fatigue, sleep disturbance, and pain interference. Data were collected at 5 quarterly encounters from registry enrollment through 12 months and analyzed with generalized estimating equations, including multivariable models to measure temporal trends and to adjust for baseline and longitudinal covariates.
- Results
- Among the 1470 patients, the mean (SD) age was 53.1 (13.2) years, and 1093 (74.4%) were female. Patients completed 5943 encounters in which multivariable analyses demonstrated that greater physician empathy was inversely associated with pain intensity (β = −0.014; 95% CI, −0.022 to −0.006; P < .001), back-related disability (β = −0.062; 95% CI, −0.085 to −0.040; P < .001), and HRQOL deficits on each measure (eg, pain interference: β = −0.080; 95% CI, −0.111 to −0.049; P < .001). Correspondingly, compared with the slightly empathic physician group, the very empathic physician group reported lower mean pain intensity (6.3; 95% CI, 6.1-6.5 vs 6.7; 95% CI, 6.5-6.9; P < .001), less mean back-related disability (14.9; 95% CI, 14.2-15.6 vs 16.8; 95% CI, 16.0-17.6; P < .001), and fewer HRQOL deficits on each measure (eg, fatigue: 57.3; 95% CI, 56.1-58.5 vs 60.4; 95% CI, 59.0-61.7; P < .001). All physician empathy group differences were clinically relevant, with Cohen d statistics ranging from 0.21 for pain intensity to 0.30 for back-related disability, fatigue, and pain interference. Physician empathy was associated with more favorable outcomes than non-pharmacological treatments, opioid therapy, and lumbar spine surgery.
- Conclusions and Relevance
- In this cohort study of adult patients with chronic pain, physician empathy was associated with better outcomes over 12 months. Greater efforts to cultivate and improve physician empathy appear warranted.
Reference:
- Licciardone JC, Tran Y, Ngo K, Toledo D, Peddireddy N, Aryal S. Physician Empathy and Chronic Pain Outcomes. JAMA Netw Open. 2024;7(4):e246026. https://doi.org/10.1001/jamanetworkopen.2024.6026
- https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2817441
PDMP Overdose Risk Score edit
The score was designed such that the risk of overdose death doubles approximately every 100 pts.
| ORS | Risk of Death |
|---|---|
| 200 | 1x |
| 300 | 2x |
| 400 | 4x |
| 500 | 8x |
| 600 | 16x |
| 700 | 32x |
| 800 | 64x |
| 900 | 128x |
An Odds Ratio for 100 point scoring groups using 000-190 as the referent group can also be used to quantify risk.
Patient's with an ORS of 900-990 are more than 300x likely to die of an overdose than patients with a score of less than 200.
| Overdose Risk Score | Odds Ratio of Unintentional Overdose Death |
|---|---|
| 000-190 | 1 |
| 200-290 | 10 |
| 300-390 | 12 |
| 400-490 | 25 |
| 500-590 | 44 |
| 600-690 | 85 |
| 700-790 | 141 |
| 800-890 | 194 |
| 900-990 | 329 |
Reference:
Pediatrics
2023 Childhood Immunizations Edit
Combined 7-Series Vaccines - The series includes vaccines to protect against:
- Chickenpox (varicella): 1 or more doses
- Diphtheria, lockjaw (tetanus), and whooping cough (pertussis): 4 or more doses, commonly of the DTaP vaccine
- Hepatitis B: three or more doses
- Hib infections: three to four or more doses, depending on the vaccine
- Measles: one or more doses, commonly of the MMR vaccine
- Pneumococcal diseases: four or more doses, commonly of the PCV vaccine
- Polio: three or more doses
Vaccines by age:
Birth:
- Hepatitis B (HepB) #1
2 months:
- HepB #2 (can be done at 1 month also)
- Rotavirus (RV) #1
- DTaP #1
- HiB #1
- Pneumococcal (PCV13) #1
- Inactivated polio (IPV) #1
4 months:
- RV #2
- DTaP #2
- Hib #2
- PCV13 #2
- IPV #2
6 months:
- HepB #3 (Can be done between 6 months and 18 months)
- DTaP #3
- PCV13 #3
- IPV #3 (can be done between 6 and 18 months)
- Influenza (annual)
12 months:
- PCV13 #4 (Can be done 12 - 15 months)
- Hib #3 (Can be done 12 - 15 months)
- MMR #1 (Can be done 12 - 15 months)
- Varicella (VAR) #1 (Can be done 12 - 15 months)
- Hepatitis A #1 (2 dose series 6 month interval 12-23 months)
15 months:
- DTaP #4 (Can be done 15 - 18 months)
4-6 years:
- DTaP #5
- IPV #4
- MMR #2
- VAR #2
11-12 years:
- Tdap #1
- Meningococal #1
- HPV #1 and #2
16 years:
- Meningococal #2
Reference:
Combination Vaccines
| Vaccine | Trade Name | Abbreviation | Manufacturer | Route | Doses in Routine Series | Approved Ages | Comments |
|---|---|---|---|---|---|---|---|
| DTaP, Polio | Kinrix® | DTaP-IPV | GlaxoSmithKline | IM | 1 | 4-6 years | Inactivated, Adj.: Approved as 5th DTaP and 4th IPV. |
| Quadracel® | DTaP-IPV | Sanofi | IM | 1 | 4-6 years | Inactivated, Adj.: Approved as 5th DTaP and 4th IPV. | |
| DTaP, Hepatitis B, Polio | Pediarix® | DTaP-HepB-IPV | GlaxoSmithKline | IM | 3 | 6 weeks-6 years | Inactivated, Adj.: Approved for 2, 4, 6 month doses. |
| DTaP, Polio, Haemophilus influenzae type b | Pentacel® | DTaP-IPV/Hib | Sanofi | IM | 4 | 6 weeks-4 years | Inactivated, Adj.: Approved for 2, 4, 6, 15-18 month doses. |
| DTaP, Polio, Haemophilus influenzae type b, Hepatitis B | Vaxelis® | DTap-IPV-Hib-HepB | Sanofi | IM | 3 | 6 weeks-4 years | Recombinant |
| Hepatitis A, Hepatitis B | Twinrix® | HepA-HepB | GlaxoSmithKline | IM | 3 | ≥18 years | Inactivated/Recombinant, Adj. Pediatric HepA + Adult HepB |
| Measles, Mumps, Rubella, Varicella | ProQuad® | MMRV | Merck | SC | 2 | 12 months- 12 years | Live Attenuated |
Reference:
Vaccines - Childhood Special Situations
- Premature babies weighing >2000 g should receive immunizations based on chronological age
- Premature babies weighing <2000 g should have the Hep B schedule modified with vaccination delayed if the mother is known to be HBsQg-negative
- Seasonal flu vaccine should be administered to all infants over 6 mo
Ref:
Vaccines and Autism
Original idea was the measles component of the MMR vaccine might be linked to autism
- Began with a small, now-retracted 1998 study in the journal The Lancet. That research looked at 12 children with developmental delays, and eight of the kids had autism. It's since come to light that the lead researcher had several conflicts of interest: He had been paid by a law firm that wanted to sue the vaccine manufacturer, and he had a patent for a "safer" measles vaccine that he had developed before doing the 1998 study, according to a 2011 report in the journal The BMJ.
Much better and larger studies demonstrate MMR does not cause Autism:
- 2002 study: A population-based study of measles, mumps, and rubella vaccination and autism
- Research looked at 537,000 children born in Denmark between 1991 and 1998.
- But after the publication of that study, Hviid heard from concerned parents and so-called anti-vaxxers who questioned whether "susceptible" children might be at risk for autism after receiving the MMR vaccine.
- Madsen KM, Hviid A, Vestergaard M, Schendel D, Wohlfahrt J, Thorsen P, Olsen J, Melbye M. A population-based study of measles, mumps, and rubella vaccination and autism. N Engl J Med. 2002 Nov 7;347(19):1477-82. doi: 10.1056/NEJMoa021134. PMID: 12421889.
- 2019 Study: Measles, Mumps, Rubella Vaccination and Autism: A Nationwide Cohort Study
- researchers looked at whether the vaccine increased risk in the following groups: boys, girls, children who develop "regressive autism" when they're older and children whose siblings have autism (the condition is partly genetic, so these children already have a greater risk of developing autism than the general public does).
- The scientists also looked at individuals' birth years, whether other childhood vaccines were received and when, and each child's autism risk factors based on the child's disease risk score, the researchers reported in the study.
- In the results, none of the subgroups that received the MMR vaccine showed any increased risk for autism, the researchers found. Interestingly, the vaccine was even associated with a slightly lower risk of autism in girls and in children born from 1999 to 2001, the researchers reported.
- The study strongly supports that MMR vaccination does not increase the risk for autism, does not trigger autism in susceptible children, and is not associated with clustering of autism cases after vaccination. It adds to previous studies through significant additional statistical power and by addressing hypotheses of susceptible subgroups and clustering of cases.
- Hviid A, Hansen JV, Frisch M, Melbye M. Measles, Mumps, Rubella Vaccination and Autism: A Nationwide Cohort Study. Ann Intern Med. 2019 Apr 16;170(8):513-520. doi: 10.7326/M18-2101. Epub 2019 Mar 5. PMID: 30831578.
Patient Messaging: re: The Dr. Paul Thomas Approved Vaccine Plan
I've heard of him before. I am ok with his schedule in general, but I disagree with some of it as well.
My main concerns are the schedule does not including polio, hepatitis B, nor rotavirus.
- Polio is low risk here in the US, but the vaccine is a dead virus, the baby cannot get the disease from it, and it will protect them throughout their life even if they travel to a part of the World where it still is endemic
- Hepatitis B continues to be a risk here in the USA for all ages. The vaccine safety is well demonstrated historically - I am not sure why he recommends avoiding it entirely
- Rotavirus has a troubled historical past (1980s) where it was removed from the market. A new and different version was released when I was in medical school and it has not shown the same dangers. This is the one I would be most supportive of skipping entirely.
Reference:
- www.integrativepediatricsonline.com/uploads/1/0/9/2/109222957/thevaccine-friendlyplan.pdf
Acute Gastroenteritis in Children
- Noninflammatory agents
- Viruses
- Rotavirus
- Enteric adenovirus
- Calicivirus
- Astrovirus
- Viruses
- Inflammatory agents
- Bacteria
- Salmonella
- Shigella
- Campylobacter jejuni
- Yersinia enterocolitica
- Enterohemorrhagic Escherichia coli (including O157:H7)
- Other E. coli
- Clostridium difficile
- Parasites
- Giardia intestinalis
- Cryptosporidium
- Bacteria
References:
- AFP Vol 85 No 11 Jun 2012
Acute Migraines in Children
First-line acute migraine treatment in children is ibuprofen;
Adolescents may benefit from sumatriptan/naproxen (Treximet) tablets, zolmitriptan (Zomig) nasal spray, sumatriptan (Imitrex) nasal spray, rizatriptan (Maxalt), or almotriptan (Axert).
ADHD Pediatric Management
Medication options for pediatric attention-deficit/hyperactivity disorder (ADHD) include both stimulant and non-stimulant medications.
Stimulants are the first-line treatment and include:
- Amphetamines: These increase extracellular synaptic levels of dopamine and norepinephrine. Preparations include extended-release amphetamines (XR-OS liquid oral suspension, orally disintegrating tablets), dextroamphetamine sulfate (tablet, solution, extended-release capsule), lisdexamfetamine (capsule, chewable tablet), methamphetamine (tablet), mixed amphetamine salts (tablet, extended-release capsule), racemic amphetamine sulfate (tablet, orally disintegrating tablet), and triple-bead mixed amphetamine salts (extended-release capsule).
- Methylphenidate: This increases extracellular synaptic levels of dopamine and norepinephrine. Preparations include dexmethylphenidate (tablet, extended-release capsule), methylphenidate (immediate-release tablet, solution, chewable tablet, extended-release tablet, chewable tablet, long-acting capsule, controlled-delivery capsule, transdermal patch, delayed-release and extended-release capsule, osmotic-release oral system tablet, extended-release orally disintegrating tablet, extended-release suspension, multilayer extended-release capsule).
Non-stimulants are considered when stimulants are not effective or cause significant side effects:
- Atomoxetine: This selectively inhibits the norepinephrine transporter and is available as a capsule.
- Extended-release clonidine: This stimulates postsynaptic α2-adrenergic receptors and is available as a tablet.
- Extended-release guanfacine: This stimulates postsynaptic α2A-adrenergic receptors and is available as a tablet.
These medications are approved by the FDA for the treatment of ADHD in pediatric patients and are supported by clinical evidence for their efficacy and safety profiles.
Reference:
- Cortese S. Pharmacologic Treatment of Attention Deficit–Hyperactivity Disorder. Published September 2020
Bruising/Non-accidental Trauma
TEN-4 Bruise Clinical Decision Rule for Predicting Nonaccidental Trauma in Children Four Years and Younger
- Torso (including abdomen, back, buttocks, chest, genitourinary area, hip)
- Ear
- Neck
- Anywhere on child under 4 mo
Any 1 indicates increased likelihood of nonaccidental trauma
Reference:
- Pierce MC, Kaczor K, Aldridge S, et al. Bruising characteristics discriminating physical child abuse from accidental trauma [published correction appears in Pediatrics. 2010;125(4):861]. Pediatrics. 2010;125(1):67-74.
Child Development
| Age | Gross Motor | Fine Motor | Language | Social |
|---|---|---|---|---|
| 2mo | Holds head up | Swipes at objects | Coos | Social Smile |
| 4mo | Rolls over | Grasps objects | Orients to voice | Laughs |
| 6mo | Sits without support | Transfers objects | Babbles | Stanger Anxiety |
| Monosyllable | Peek-a-boo | |||
| 9mo | Crawl/pull to stand | Pincer grasp | Mama-Dada non-specific | Responds to name |
| 12mo | Stands | Mature pincer | Mama-Dada specific | Picture book |
| 15mo | Walks | Uses cup | 4-6 words | Temper Tantrum |
| 18mo | Walks up steps | Spoon for solids | 2 words together | Begin toilet training |
| Throws ball | ||||
| 24mo | Walks down steps | Spoon for semi-solids | 50 words / 2-3 word sent | Follows 2 step command |
| 36mo | Tricycle | Eats neatly with utensils | 3-4 word sentences | Toilet trained |
| Asks who, what, where, and why | Dresses with help |
Midparental height:
- Females:
- In cm: (paternal height-13+maternal height)/2
- In in: (paternal height-5+maternal height)/2
- Males
- In cm: (paternal height+13+maternal height)/2
- In in: (paternal height+5+maternal height)/2
Children (<3 yo) with a Fever
Neonates younger than 28 days with a fever higher than 100.4°F (38°C) should have a diagnostic evaluation, including a thorough history, physical examination, complete blood count, blood cultures, lumbar puncture, urinalysis, and urine culture. For febrile children older than 28 days but younger than three months, diagnostic evaluation should include a thorough history, physical examination, urinalysis, and risk assessment tools that may include additional tests such as a complete blood count, procalcitonin, and C-reactive protein. Lumbar puncture may be considered but is not suggested for all infants in this age range. In febrile children older than 28 days, the need for chest radiography is determined by clinical presentation and laboratory examinations. Radiography is not recommended for wheezing suggestive of bronchiolitis or asthma. Febrile children older than two months but younger than three years should be assessed for possible urinary tract infection if no other source of fever has been identified.
Reference:
- AFP Jun 2021 Vol 103 No 12
- https://www.aafp.org/afp/2020/0615/p721.html
Constipation (Newborn)
If your newborn truly is constipated and his stool is hard, there are some solutions that are safe and effective.
- Start by giving 1 ounce of straight water.
- If that doesn't work after 4 hours, give 1 ounce of straight prune juice.
- If you still don't get results 4 hours later, give 1 ounce of water and 1 ounce of prune juice.
- If it's still not working after another 4 hours, give a pediatric glycerin suppository.
Other things to try:
- Also, try massaging the abdomen in a circular motion close to their belly button. Alternatively, you can try bicycling his legs to see if that helps
- Do a warm bath
Reference:
Constipation (Pediatric)
Evidence statements:
- Digital rectal examination and abdominal radiography should not be performed routinely in children with suspected functional constipation.
- Increasing fiber or fluid intake above usual daily recommendations does not improve constipation in children. (LOE A)
- Probiotics are not beneficial in the treatment of constipation in children. (LOE A)
- Referring children with functional constipation to a child psychologist can improve some constipation outcomes. (LOE B)
- Polyethylene glycol (Miralax) is first-line treatment for functional constipation in children.
Reference:
- Am Fam Physician. 2022;105(5):469-478
Croup
General info:
- Diagnosis is based on clinical findings of: (LOE C)
- Barking cough
- Stridor
- Hoarseness
- Humidified air inhalation does not improve symptoms in moderate croup (LOE B)
- Corticosteroids should be administered to patients with croup of any severity (LOE A)
- Epinephrine should be given to those with moderate to severe croup (LOE A)
- Parainfluenza virus (types 1-3) account for 75% of cases
- Human parainfluenza virus 1 is most common type
Differential:
- Bacterial tracheitis
- Typical age: <6yo
- Presentation: High fever, barking cough, respiratory distress, rapid deterioration
- Croup
- Typical age: 6mo-3yo
- Presentation: Acute onset of barking cough, stridor, and hoarseness
- Epiglottitis
- Typical age: 3-12yo
- Presentation: Acute onset of dysphagia, odynophagia, drooling, high fever, anxiety, and muffled voice
- Foreign body aspiration
- Typical age: <3yo
- Presentation: Acute onset of choking and/or drooling
- Hemangioma
- Typical age: <6mo
- Presentation: Stridor worse with crying
- Large airway lesions (subglottic stenosis, laryngeal cleft, tracheomalacia, and laryngomalacia)
- Typical age: <6mo to 4.5yo
- Presentation: Recurrent episodes of barking cough and stridor
- Neoplasm
- Typical age: No age predeliction
- Presentation: Progressive airway symptoms
- Peritonsillar abscess
- Typical age: 6mo to 3.5yo
- Presentation: Sore throat, fever, "hot potato" voice
- Retropharyngeal abcsess
- Typical age: 2-4yo
- Presentation: Fever, drooling, dysphagia, odynophagia, and neck pain
- Thermal injury/smoke inhalation
- Typical age: No age predeliction
- Presentation: Exposure to heat, smoke, or chemical
References:
- AFP Vol 97 No 9 May 2018
Westley Croup Score
| Sign | Score |
|---|---|
| LOC | |
| Normal | 0 |
| Disoriented | 5 |
| Cyanosis | |
| None | 0 |
| With agitation | 4 |
| At rest | 5 |
| Stridor | |
| None | 0 |
| When agitated | 1 |
| At rest | 2 |
| Air entry | |
| Normal | 0 |
| Decreased | 1 |
| Markedly decreased | 2 |
| Retractions | |
| None | 0 |
| Mild | 1 |
| Moderate | 2 |
| Severe | 3 |
Scoring:
| Total | Croup severity |
|---|---|
| 0-2 | Mild |
| 3-7 | Moderate |
| 8-11 | Severe |
| 12+ | Impending respiratory failure |
References:
- AFP Vol 97 No 9 May 2018
Dermatologic Concerns
See also:
Childhood Rashes
- Roseola Infantum (Exanthema Subitum)
Roseola is most commonly caused by human herpesvirus 6 and affects infants and children younger than three years.2 It is characterized by the abrupt onset of high fever lasting one to five days. During this period, children often appear well with no focal clinical signs except possible mild cough, rhinorrhea, or mild diarrhea. Once the fever resolves, an erythematous macular to maculopapular rash usually appears, starting on the trunk and spreading peripherally. This rash is similar in appearance to that of rubeola (measles). In contrast with roseola, the rash associated with measles starts on the face (usually behind the ear) or mouth (Koplik spots) and moves downward.3 Children with roseola usually appear well, whereas those with measles are typically more ill-appearing. Roseola is a self-limited illness requiring no treatment, and the diagnosis is clinical.4
References:
- Am Fam Physician. 2015;92(3):211-216
- Pityriasis Rosea
Approximately 80% of patients with pityriasis rosea present with a single oval-shaped, rose-colored patch, usually on the trunk. This lesion, commonly known as the herald patch, is typically 2 to 10 cm in diameter and may have a peripheral scale5 (Figure 1). It may be present for a few weeks before the development of smaller lesions that are similar to the herald patch, maintaining a classic peripheral scale overlying pink thin papules.
The herald patch may be misdiagnosed as tinea corporis because of the annular lesion with raised edges, fine scale, and central clearing. There is usually a single plaque with tinea corporis, without eruptions of smaller lesions typical with pityriasis rosea. The rash of pityriasis rosea is usually bilateral and symmetric, distributed parallel to the Langer lines in a Christmas tree pattern. Children with pityriasis rosea may have a history of mild upper respiratory tract infection symptoms, and up to one-half have pruritus.6 A potassium hydroxide preparation can help distinguish pityriasis rosea from tinea infection or other rashes. The rash associated with pityriasis rosea may be present for two to 12 weeks, and treatment is supportive.6 Although the etiology is not fully known, it is thought to be infectious, with some studies implicating human herpesvirus 6 and 7.5,7
References:
- Am Fam Physician. 2015;92(3):211-216
- Scarlet Fever
Scarlet fever is diagnosed in 10% of children presenting with streptococcal tonsillopharyngitis.8 It is caused by certain strains of group A beta-hemolytic streptococci that release a streptococcal pyrogenic exotoxin (erythrogenic toxin). Patients who have a hypersensitivity to the toxin may develop the characteristic rash associated with scarlet fever.
Most children have a fever and sore throat one to two days before the rash develops on the upper trunk. The rash spreads throughout the body, sparing the palms and soles, with characteristic circumoral pallor. This differs from some viral exanthems that develop more slowly. The rash is characterized by confluent, erythematous, blanching, fine macules, resembling a sunburn, and sandpaper-like papules (Figure 2). In skinfolds, such as the axilla, antecubital fossa, and buttock creases, an erythematous, nonblanching linear eruption (Pastia lines) may develop. Petechiae on the palate may occur, as well as erythematous, swollen papillae with a white coating on the tongue (white strawberry tongue). Red strawberry tongue occurs after desquamation of the white coating. After several weeks, the rash fades and is followed by desquamation of the skin, especially on the face, in skin-folds, and on the hands and feet, potentially lasting four to six weeks.9
With a sensitivity of 90% to 95%, throat culture is the first-choice method for diagnosis of group A streptococcal infection, but this is not always practical.8 Rapid antigen tests are routinely used in clinicians' offices and have a sensitivity of approximately 86%.10 Cultures may be ordered when the suspicion for group A streptococcal infection is high, but the rapid antigen test result is negative.11
Penicillin is the therapy of choice for streptococcal infection. Those allergic to penicillin and cephalosporins may be treated with oral macrolides (erythromycin, azithromycin [Zithromax]) or clindamycin.10.
References:
- Am Fam Physician. 2015;92(3):211-216
- Erythema Infectiosum
Erythema infectiosum, or fifth disease, is caused by parvovirus B19. It is a common childhood infection characterized by a prodrome of low-grade fever, malaise, sore throat, headache, and nausea followed several days later by an erythematous "slapped cheek" facial rash (Figure 4). After two to four days, the facial rash fades. In the second stage of the disease process, pink patches and macules may develop in a lacy, reticular pattern, most often on the extremities. After one to six weeks, the rash resolves but may reappear with sun exposure, heat, or stress. Arthralgias occur in approximately 8% of young children with the disease but are much more common in teens and young adults. Patients are no longer considered infectious once the rash appears. Treatment is symptomatic and includes nonsteroidal anti-inflammatory drugs for arthralgias and antihistamines for pruritus.13
References:
- Am Fam Physician. 2015;92(3):211-216
- Molluscum Contagiosum
Molluscum contagiosum is a skin infection caused by a poxvirus. This highly contagious viral infection most commonly affects children two to 11 years of age.14 It also occurs in sexually active adolescents. The lesions are flesh-colored or pearly white, small papules with central umbilication (Figure 5). The oral mucosa is rarely affected, but lesions may appear on the genital region and conjunctiva. Typically, children have 10 to 20 lesions, but occasionally there may be up to hundreds.14 Molluscum may also occur in conjunction with dermatitis. It can erupt and spread quickly in a child with underlying atopic dermatitis, or it can induce dermatitis in a child with previously clear skin (molluscum dermatitis).
The diagnosis of molluscum contagiosum is made clinically. The condition is self-limited, but clinicians should advise parents to use gentle skin care products on the patient and that lesions may last for months or up to two to four years. Treatment options, including cryotherapy, imiquimod (Aldara), and intralesional immunotherapy, are available if physical appearance is a concern. Dermatitis (occurring as molluscum dermatitis or a flare-up of atopic dermatitis) requires treatment to resolve pruritus and limit spread of the molluscum.14
References:
- Am Fam Physician. 2015;92(3):211-216
- Impetigo
Impetigo is a primary or secondary bacterial infection of the epidermis of the skin. Primary infections occur when bacteria enter breaks in the skin, whereas secondary infections develop at the site of an existing dermatosis. There are bullous and nonbullous forms of the infection, with the bullous form typically occurring in neonates and the nonbullous form most common in preschool- and school-aged children.12 Although Streptococcus pyogenes was once the most common cause of nonbullous impetigo, Staphylococcus aureus has surpassed it in more recent years. However, S. pyogenes may still be the predominant cause in warm and humid climates. S. aureus is the main source of bullous impetigo. Initially, children may develop vesicles or pustules that form a thick, yellow crust (Figure 3). With autoinoculation, the lesions may quickly spread. The face and extremities are most commonly affected. Although impetigo is usually a self-limited disease, antibiotics are often prescribed to prevent complications and spread of the infection.12
References:
- Am Fam Physician. 2015;92(3):211-216
- Tinea Infection
Tinea is a common fungal skin infection in children that may affect the scalp (tinea capitis), body (tinea corporis), groin (tinea cruris), feet (tinea pedis), hands (tinea manus), or nails (tinea unguium). The diagnosis is based on physical examination findings and is confirmed by potassium hydroxide microscopy, periodic acid–Schiff staining of hair follicles, or fungal culture.
References:
- Am Fam Physician. 2015;92(3):211-216
- Atopic Dermatitis
Atopic dermatitis is a common childhood inflammatory skin disease that affects approximately 20% of children in the United States.16 This chronic, pruritic skin disease is relapsing in nature. Atopic dermatitis typically presents in infancy and early childhood and may persist into adulthood. Children may present with a variety of skin changes, including erythematous plaques and papules, excoriations, severely dry skin, scaling, and vesicular lesions (Figure 8).
References:
- Am Fam Physician. 2015;92(3):211-216
Neonatal jaundice
Within 24hr of birth:
- Hemolysis
- Sepsis
Within 48hr of birth:
- Hemolysis
- Infetion
- Physiologic
After 48hrs of birth:
- Infection
- Hemolysis
- Breast milk
- Congenital malformation
- Hepatitis
Other notes:
- Jaundice AT birth is ALWAYS pathologic
Documentation: Newborn Exam
- GEN: Normal general appearance; NAD
- HEAD: NCAT; No cephalohematoma; AFOSF
- EENT: Red reflex present bilaterally; Normal ext ears, nose, lips
- MOUTH: MMM; Normal gums, mucosa, palate, OP
- NECK: Supple
- CV: RRR, no m/r/g; Normal femoral pulses
- LUNGS: CTAB, no w/r/c
- ABD: Soft, NT/ND, NBS, no masses or organomegaly; Normal umbilicus
- GU: Normal _male genitalia; Testes descended bilaterally
- MSK: Normal extremities & spine; No hip clicks or clunks; No clavicular fracture
- NEURO: MAE symmetrically; Normal moro & suck reflexes; Normal muscle tone
- SKIN: WWP; No jaundice, new skin rashes, or abnormal lesions; No sacral dimple
Reference:
Febrile Seizures
Prediction of Recurrent Febrile Seizures
| Risk Factor | Points |
|---|---|
| Age <18 mo | 1 |
| Temp <104F at time of seizure | 1 |
| Duration of fever <1 hr | 1 |
| Family history of febrile seizure | 1 |
Scoring:
- 0 = 13%
- 1 = 23%
- 2 = 32%
- 3 = 62%
- 4 = 76%
Overall risk for recurrence is 32%.
Reference:
- AFP Vol 101 no 8 Apr 2020
Feeding schedule
| Age | Number | Volume/feeding |
|---|---|---|
| Birth - 1wk | 6 - 10 | 1 - 3oz |
| 1wk - 1mo | 7 - 8 | 2 - 4oz |
| 1mo - 3mo | 5 - 7 | 4 - 6oz |
| 3mo - 6mo | 4 - 5 | 6 - 7oz |
| 6mo - 9mo | 3 - 4 | 7 - 8oz |
| 10mo - 12mo | 3 | 7 - 8oz |
Functional Abdominal Pain in Children
An organic cause (Table 25–8 ) is found in 5% to 10% of children with recurrent abdominal pain (RAP).9 If RAP is not associated with an anatomic, metabolic, infectious, inflammatory, or neoplastic disorder, it is considered functional (nonorganic) abdominal pain.10 The worldwide pooled prevalence of functional abdominal pain in children is 13.5% (95% confidence interval [CI], 11.8% to 15.3%).11 Functional abdominal pain is a clinical diagnosis and does not require a diagnostic workup.
These criteria include functional abdominal pain disorder, which is further divided into functional dyspepsia, irritable bowel syndrome (IBS), functional abdominal pain–not otherwise specified, and abdominal migraine. Among children with functional abdominal pain disorder in primary care, functional abdominal pain–not otherwise specified is most common (53.8%), followed by IBS (38.5%) and functional dyspepsia (7.7%).12
Simple laboratory tests to consider include a complete blood count for anemia or infection, erythrocyte sedimentation rate or C-reactive protein level for infection or inflammatory conditions, urinalysis for urinary tract infections, fecal guaiac testing for gastrointestinal blood loss, and fecal ova and parasite testing for protozoal gastrointestinal infections (eTable A). Pregnancy testing and screening for sexually transmitted infections should be considered in adolescents or if there are concerns about sexual abuse.
Labs:
- CBC
- ESR or CRP
- Fecal calprotectin
- Fecal guaiac
- Fecal ova and parasite
- Tissue translutaminase Ab testing (anti–tissue transglutaminase immunoglobulin A [IgA] level) and overall IgA level
- Urinalysis/Urine culture
In children with functional abdominal pain, the use of probiotics, such as Lactobacillus, reduces the intensity and frequency of abdominal pain and is safe in children.
Systematic reviews show that cognitive behavior therapy and hypnotherapy improve abdominal pain in children with functional abdominal pain disorders.
ORGANIC CAUSES
cid Reflux. Antacids and histamine H2 antagonists are used in children, although their benefit has not been well studied.6,50
Dyspepsia. Proton pump inhibitors, including lansoprazole (Prevacid) and pantoprazole (Protonix), are safe and effective for the treatment of dyspepsia in children and adolescents, with improved pain in more than 70% of patients.51
Celiac Disease. A gluten-free diet should be initiated. Children with inflammatory bowel disease should be referred to a pediatric gastroenterologist for anti-inflammatory medications and biologics.9
Chronic Constipation. Treatment includes dietary interventions, such as increased fluids, fiber, and prune, pear, and apple juices; behavioral interventions, including regular toilet time for five or 10 minutes after meals and use of stool diaries; reward systems; and parental education.52,53 Polyethylene glycol (Miralax) is a first-line therapy in children, safe for resolving fecal impaction, and better accepted in children than non–polyethylene glycol laxatives such as magnesium hydroxide.53 Severe constipation may require manual disimpaction, enemas (e.g., saline, mineral oil, polyethylene glycol), suppositories (e.g., bisacodyl [Dulcolax], glycerin), or other laxatives (e.g., magnesium citrate, lactulose, sorbitol, docusate [Colace], mineral oil).53 Stimulant laxatives such as bisacodyl and senna should be reserved for short-term use and discontinued once regular stooling habits are maintained.52
Functional Dyspepsia. Similar to acid reflux disease, functional dyspepsia is treated with antacids, H2 antagonists, and proton pump inhibitors.6,51
Irritable Bowel Syndrome. For diarrhea-predominant IBS, 5 g of partially hydrolyzed guar gum (a fiber from guar beans used in the food industry as a food thickener) may reduce abdominal pain and other symptoms.31 Antispasmodics have not been shown to be beneficial in low-quality studies.50 A small study showed that one or two peppermint oil capsules taken three times per day for two weeks can reduce diarrhea by 75%.1,54 Loperamide (Imodium), an opiate analogue, may reduce diarrhea but not abdominal pain and has not been studied in children as comprehensively as in adults.55 The use of antibiotics for treatment of IBS is controversial.55 In a small study of children with IBS, treatment with 600 mg of rifaximin (Xifaxan) improved abdominal pain, constipation, diarrhea, bloating, and flatulence.56 Treatment of constipation-predominant IBS is similar to that of constipation in children.
Abdominal Migraines. Treatment in children is similar to that in adults, including simple analgesics (e.g., acetaminophen, ibuprofen) for headaches and antiemetics (e.g., ondansetron [Zofran]) for nausea. Case reports suggest that nasal sumatriptan (Imitrex) is effective.57 Rizatriptan (Maxalt) is approved by the U.S. Food and Drug Administration for children six to 17 years of age, and almotriptan (Axert), sumatriptan/naproxen (Treximet), and nasal zolmitriptan (Zomig) are approved for those 12 years and older. Injectable sumatriptan (Zembrace) and nasal sumatriptan have also been studied for acute migraine management in children six to 17 years of age. Prophylaxis with cyproheptadine, an H1 antagonist, or propranolol can be considered if symptoms are severe, frequent, and disrupt the child's daily routine.58
Functional Abdominal Pain–Not Otherwise Specified. There is little evidence supporting the use of a variety of medications commonly tried in children with functional abdominal pain–not otherwise specified.59 Fiber supplementation is not beneficial.31 Amitriptyline does not improve abdominal pain,60 and citalopram (Celexa) does not improve pain, depression, anxiety, or somatization in children with functional abdominal pain–not otherwise specified.61 Other medications lacking data to support routine use in children for pain or dyspepsia include muscle relaxants,17 dopamine receptor antagonists (e.g., metoclopramide [Reglan], domperidone [not available in the United States]), and erythromycin.62 Cyproheptadine improves patient and parent assessment of abdominal pain.63 Famotidine (Pepcid), an H2 antagonist, subjectively improves pain when children are asked after using the medication whether it was helpful. However, when objectively measured based on pain frequency, pain severity, management of symptoms (e.g., nausea, vomiting, epigastric pain), and relationship of pain to meals, treatment with famotidine does not show improvement.64
References:
Hypertension (Pediatric)
See also:
| Population and test | Instructions and rationale |
|---|---|
| All patients | |
| Chemistry panel | Include measurement of electrolytes, blood urea nitrogen, and creatinine |
| Echocardiogram | Order only when pharmacotherapeutic intervention is being considered |
| Lipid panel | Specimen can be drawn in a fasting or nonfasting state |
| Urinalysis | |
| Obese patients | |
| Alanine aminotransferase and aspartate aminotransferase | Screen for fatty liver disease |
| Fasting lipid panel | Screen for dyslipidemia |
| Hemoglobin A1C | Screen for diabetes |
| Optional | |
| Complete blood count | Order when a history of growth delay has been reported or results of renal function testing are abnormal |
| Drug screen | Order when the history suggests substance abuse |
| Fasting serum glucose | Order when the patient is at high risk of diabetes |
| Renal doppler ultrasound | Should be performed in a child < 6 y or who has abnormal urinalysis or renal function |
| Consider performing in a normal-weight child ≥ 8 y in whom renovascular hypertension is suspected | |
| Sleep study | Order when a history of loud snoring or daytime sleepiness has been reported |
| Thyroid-stimulating hormone |
Etiologies
- Primary hypertension
- Essential
- Family history of hypertension
- Overweight, obesity
- Essential
- Secondary hypertensiona
- Coarctation
- Diminished femoral pulses, heart murmur, lower blood pressure in a leg than in either arm
- Cushing syndrome
- Family history of an endocrine disorder
- Acne, hirsutism, moon facies, striae, truncal obesity
- Drug- and substance-induced
- Cocaine, corticosteroids, decongestants, diet aids, oral contraceptives, stimulants (amphetamines, caffeine)
- Hyperthyroidism
- Family history of thyroid disorder
- Heat intolerance, pallor, rash, sweating, tachycardia, weight loss
- Mineralocorticoid excess
- Family history of an endocrine disorder
- Ambiguous genitalia, muscle weakness
- Pheochromocytoma
- Flushing, pallor, palpitations, tachycardia
- Renal artery stenosis
- History of umbilical artery catheterization
- Abdominal bruit
- Renal parenchymal disease
- Family history of renal disease
- Abdominal mass, edema, enuresis, fatigue, gross hematuria, growth retardation, recurrent urinary tract infection
- Rheumatologic disorder
- Family history of autoimmune disease
- Fatigue, friction rub, joint pain or swelling, rash
- Sleep-disordered breathing
- Family history of obstructive sleep apnea
- Snoring, tonsillar hypertrophy
- Coarctation
- J Fam Pract. 2021 June;70(5):220-228 | 10.12788/jfp.0201
Reference:
Orlando Pediatric Resources
Early Steps
- Who: Infants from birth –36months with significant delays or an established condition that may result in delay
- What: Provides families with services to enhance their child's development so they are ready to learn when they enter school
- Where:
- Early Steps Program of Central Florida
- 407-317-7430 Ext 2121
- May also contact: 1800-654-4440
- Fax 407-648-4150
- Early Steps Program of Central Florida
- How: Athena "Early Intervention Referral" must write "Early Steps" in internal note
Early Intervention
- Who: Children between the ages of 3-5 who you have concerns for development (speech, milestones, cognition or suspicion for Autism, concern for behavioral problems)
- What: Preschool diagnostic intervention services (PDIS) assists families in the identification of learning delays and disabilities through screening and evaluation, development of an individualized education plan and referral to programs and services. Support to families and school staff is provided through training, professional development and consultation.
- Where:
- 3130 Edgewater Drive
- Orlando, Fl 32804
- Office 407-317-3503
- Fax 407-317-3552
- How: Athena "Early Childhood Intervention Referral"
CARDS
- Who: Child of any age with concerns for Autism or other behavioral or developmental problems.
- What: Center for Autism and Related disabilities. Provides resources only.
- Where:
- University of Central Florida
- PO Box 1662202
- Orlando, Florida 32816
- Main line: 407-823-601
- Fax: 407-823-6012
- University of Central Florida
- How: Provide patient with phone number and have them contact center.
Healthy 100 Program
- Who: Overweight and obese pediatric patients
- What: Team of pediatric specialist led by Dr. Angela Fal who work to provide support and education to pediatric patients and their family to pursue healthy lifestyle. Team includes: Board certified pediatrician and bariatric physician, child psychologist, exercise physiologist and licensed nutritionist.
- Where:
- Main office
- 1801 Lee Rd, Suite 307
- Winter Park, FL 32789
- Phone: 407-303-9200
- Fax: 407-303-9201
- YMCA Aquatic Center
- 8422 International Dr.
- Orlando, FL 328219
- Phone: 407-303-9200
- Fax: 407-303-9201
- YMCA Blanchard Park Family Center
- 10501 J. Blanchard Trail
- Orlando, FL 32817
- Phone: 407-303-9200
- Fax: 407-303-9201
- Main office
- How: Athena "Weight management referral" Must write for Healthy 100 program or Dr. Fals in the internal note section
Parenting
See also:
General Tips
- Catch them being good
- Look for opportunities and take 5-10 seconds to acknowledge good behavior throughout the day
- Let them help you
- Involve your children in activities during which they can help you
- Establish home routines
- Establish clear, consistent, orderly, and predictable routines
- Eat dinner as a family and encourage open communication
- Monitor your children
- Hand out discipline in a consistent and matter-of-fact manner
- Be calm when you discipline
- Save long talks and lectures for good behavior
- Threats and nagging often result in worse behavior
- Talk with your children, not at them
- Show sympathy when you discipline
- Be a good role model
- Children learn from what they watch and hear
- Be a parent, not a martyr
- Occasionally take time away from your children using a trusted family member or babysitter. Focus on the relationship with your significant other and recharge your batteries.
- As a parent, understand that you are also a teacher
- Actively look for opportunities to teach, model, and reinforce positive behaviors
- Monitor your children's use of electronic media
- Avoid fast-paced, distracting, or violent content
- Turn off the TV and other electronic devices when not in use
- Avoid using media as the single method to calm a child
- Monitor your child's media use
- Keep mealtimes, bedrooms, and parent-child playtimes screen free
- Avoid screen time for 1 hr before bedtime and remove devices from bedroom before bed
References:
- AFP Vol 97 No 10 May 2018
Stop Thumb Sucking
- Praise children when they don't such their thumb
- Find alternative ways of comforting and soothing for children (like a stuffed toy)
- Provide reminders or negative reinforcement fo thumb sucking (like bitter liquids or band-aid on thumb)
- Involve older children in ways in which they can stop sucking (they can create their own reward system)
Reference:
- AFP Vol 80 No 2 Jul 2009
Strategies to Reduce Picky Eating
- Follow the rule of 10s:
- Introduce a food 10 times before deciding a child does not like it
- Offer foods frequently and in different settings
- Expand food choices by offering other oods with similar properties
- Offer calm, pleasant mealtimes
- Offer peer modeling of eating (older sibling)
- Combine foods, even if in illogical combinations - adjusting how it is presented can change palatability
- Limit mild to 16 to 24oz per day - too much milk can decrease appetite and lead to iron deficiency and other nutrient imbalances
- Limit juice to no more than 4 to 6oz per day - juices can represent a large amount of sugar and calories in a child's diet
- Emphasize quality over quantity
- Offer the child only foods that parents wish the child to eat - do not indulge the child's wishes
Reference:
- AFP Vol 80 No 2 Jul 2009
Safety Counseling
Safety:
- Firearms
- Firearms and ammunition should be kept in separate locked cabinets
- Sports
- Appropriate sports-specific safety equipment should be worn
- Protective equipment for skating and skateboarding should be emphasized
- Traffic
- Seat belts worn during all car rides
- Booster seats until child fits properly in adult seat belt
- No one in bed of pickup truck
- Persons <16yo should not drive ATV
- Bicycle helmets should be worn on all bike rides
- Water
- Children 5 and older should learn to swim
- Personal floatation devices should be worn while boating
References:
- AFP Vol 83 No 6 Mar 2011
Pediatric Depression edit
| Medication | Age (in years) | Diagnosis |
|---|---|---|
| Escitalopram (Lexapro) | 12 and older | Major depressive disorder |
| Fluoxetine (Prozac) | 8 and older | Major depressive disorder |
| Olanzapine and fluoxetine, combination drug (Symbyax) | 10 and older | Bipolar depression |
| Duloxetine (Cymbalta) | 7 and older | Generalized anxiety disorder |
| Clomipramine (Anafranil) | 10 and older | Obsessive-compulsive disorder (OCD) |
| Fluvoxamine | 8 and older | OCD |
| Sertraline (Zoloft) | 6 and older | OCD |
| Fluoxetine (Prozac) | 7 and older | OCD |
The FDA reported that an extensive analysis of clinical trials showed that antidepressants may cause or worsen suicidal thinking or behavior in a small number of children and teens. The analysis showed that children and teens taking antidepressants had a small increase in suicidal thoughts, compared with those taking a sugar pill (placebo).
None of the children in any of the studies actually took his or her own life. Still, the FDA considered the findings concerning enough to issue a public health advisory and require manufacturers to label antidepressants with strong warnings about the link to suicidal thinking and behavior in children, adolescents and young adults under 25.
The highest risk of suicidal thinking and behavior occurs:
- During the first few months of treatment with an antidepressant
- When the dosage is increased or decreased
Pediatric Dosing: acetaminophen
| Child's weight (lbs) | 6-11 | 12-17 | 18-23 | 24-35 | 36-47 | 48-59 | 60-71 | 72-95 | 96+ | lbs |
|---|---|---|---|---|---|---|---|---|---|---|
| Liquid 160 mg/ 5 mL | 1.25 | 2.5 | 3.75 | 5 | 7.5 | 10 | 12.5 | 15 | 20 | mL |
| Liquid 160 mg/ 1 tsp | -- | 1/2 | 3/4 | 1 | 1.5 | 2 | 2.5 | 3 | 4 | tsp |
| Chewable 160 mg tab | -- | -- | -- | 1 | 1.5 | 2 | 2.5 | 3 | 4 | tabs |
| Adult 325 mg tab | -- | -- | -- | -- | -- | 1 | 1 | 1.5 | 2 | tabs |
| Adult 500 mg tab | -- | -- | -- | -- | -- | -- | -- | 1 | 1 | tab |
Reference:
Pediatric Dosing: cetirizine
| Child's AGE (years) | 2-5 | 6-11 | 12+ | years |
|---|---|---|---|---|
| Liquid 5 mg/ 5 mL | 2.5 | 5 | 10 | mL |
| Liquid 5 mg/ 1 teaspoon (tsp) | ½ | 1 | 2 | tsp |
| Chewable 5 mg tablets | -- | 1 | 2 | tablets |
| Tablets 10 mg | -- | -- | 1 | tablet |
Reference:
Pediatric Dosing: dextromethorphan
| Child's weight (pounds) | 30-47 | 48-63 | 64-79 | 80-95 | 96-129 | 130+ | lbs |
|---|---|---|---|---|---|---|---|
| Liquid 5 mg/ 5 milliliters (mL) | 5 | 7.5 | 10 | 12.5 | 15 | -- | mL |
| Liquid 5 mg/ 1 teaspoon (tsp) | 1 | 1½ | 2 | 2½ | 3 | -- | tsp |
| Liquid 7.5 mg/ 5 milliliters (mL) | -- | 5 | 5 | 7.5 | 10 | 15 | mL |
| Liquid 7.5 mg/ 1 teaspoon (tsp) | -- | 1 | 1 | 1½ | 2 | 3 | tsp |
| Liquid 10 mg/ 5 milliliters (mL) | -- | -- | 5 | 5 | 7.5 | 10 | mL |
| Liquid 10 mg/ 1 teaspoon (tsp) | -- | -- | 1 | 1 | 1½ | 2 | tsp |
Reference:
Pediatric Dosing: diphenhydramine
| Child's weight (pounds) | 20-24 | 25-37 | 38-49 | 50-99 | 100+ | lbs. |
|---|---|---|---|---|---|---|
| Liquid 12.5 mg/ 5 milliliters (mL) | 4 | 5 | 7.5 | 10 | 20 | mL |
| Liquid 12.5 mg/ 1 teaspoon (tsp) | ¾ | 1 | 1½ | 2 | 4 | tsp |
| Chewable 12.5 mg | -- | 1 | 1½ | 2 | 4 | tablets |
| Tablets 25 mg | -- | ½ | ½ | 1 | 2 | tablets |
| Capsules 25 mg | -- | -- | -- | 1 | 2 | caps |
Reference:
Pediatric Dosing: ibuprophen
| Child's weight (pounds) | 12-17 | 18-23 | 24-35 | 36-47 | 48-59 | 60-71 | 72-95 | 96+ | lbs |
|---|---|---|---|---|---|---|---|---|---|
| Infant Drops 50 mg/ 1.25 mL | 1.25 | 1.875 | 2.5 | 3.75 | 5 | -- | -- | -- | mL |
| Liquid 100 mg/ 5 milliliters (mL) | 2.5 | 3.75 | 5 | 7.5 | 10 | 12.5 | 15 | 20 | mL |
| Liquid 100 mg/ 1 teaspoon (tsp) | ½ | ¾ | 1 | 1½ | 2 | 2½ | 3 | 4 | tsp |
| Chewable 100 mg tablets | -- | -- | 1 | 1½ | 2 | 2½ | 3 | 4 | tabs |
| Junior-strength 100 mg tablets | -- | -- | -- | -- | 2 | 2½ | 3 | 4 | tabs |
| Adult 200 mg tablets | -- | -- | -- | -- | 1 | 1 | 1½ | 2 | tabs |
Reference:
Pediatric Dosing: loratadine
| Child's AGE (years) | 2-5 | 6-11 | 12+ | years |
|---|---|---|---|---|
| Liquid 5 mg/ 5 milliliters (mL) | 2.5 | 5 | 10 | mL |
| Liquid 5 mg/ 1 teaspoon (tsp) | ½ | 1 | 2 | tsp |
| Chewable 5 mg tablets | -- | 1 | 2 | tablets |
| Tablets 10 mg | -- | -- | 1 | tablet |
Reference:
Sleep
Transgender and Pediatrics
Transgender Interventions Harm Children (From ACP)
No Evidence that Transgender Interventions are Safe for Children
- There is not a single long-term study to demonstrate the safety or efficacy of puberty blockers, cross-sex hormones and surgeries for transgender-believing youth. This means that youth transition is experimental, and therefore, parents cannot provide informed consent, nor can minors provide assent for these interventions. Moreover, the best long-term evidence we have among adults shows that medical intervention fails to reduce suicide.
Puberty blockers may cause mental illness
- Puberty blockers may actually cause depression and other emotional disturbances related to suicide. In fact, the package insert for Lupron, the number one prescribed puberty blocker in America, lists "emotional instability" as a side effect and warns prescribers to "Monitor for development or worsening of psychiatric symptoms during treatment." Similarly, discussing an experimental trial of puberty blockers in the U.K., Oxford University Professor Michael Biggs wrote, "There was no statistically significant difference in psychosocial functioning between the group given blockers and the group given only psychological support. In addition, there is unpublished evidence that after a year on [puberty blockers] children reported greater self-harm, and the girls also experienced more behavioral and emotional problems and expressed greater dissatisfaction with their body—so puberty blockers exacerbated gender dysphoria."
Puberty blockers may cause permanent physical harm
- Temporary use of Lupron has also been associated with and may be the cause of many serious permanent side effects including osteoporosis, mood disorders, seizures, cognitive impairment and, when combined with cross-sex hormones, sterility.
Cross-sex hormones (testosterone for women; estrogen for men) may disrupt mental health
- Women who identify as men are given enough testosterone to raise their levels 10-40 times above the female reference range. Past studies have documented multiple psychiatric problems with similar high doses of anabolic steroids like testosterone such that 23% of subjects met DSM criteria for a major mood syndrome such as mania, hypomania, and major depression, and 3.4-12% developed psychotic symptoms. Estrogen also impacts mood in complex ways. Post menopausal women treated with estrogen often experience severe anxiety despite being placed on physiologic doses of the hormone. Men who identify as women are given supraphysiologic doses of estrogen; theoretically, this has the potential to worsen both depression and anxiety.
Other health risks are correlated with puberty blockers and cross-sex hormones
- Temporary use of puberty blocker Lupron has also been associated with and may be the cause of many serious permanent side effects including osteoporosis, mood disorders, seizures, cognitive impairment and, when combined with cross-sex hormones, sterility. In addition to the harm from Lupron, cross-sex hormones put youth at an increased risk of heart attacks, stroke, diabetes, blood clots and cancers across their lifespan. Add to this the fact that physically healthy transgender-believing girls are being given double mastectomies at 13 and hysterectomies at 16, while their male counterparts are referred for surgical castration and penectomies at 16 and 17, respectively, and it becomes clear that affirming transition in children is about mutilating and sterilizing emotionally troubled youth.
Transgender interventions for children are experimental and dangerous
- Many medical organizations around the world, including the Australian College of Physicians, the Royal College of General Practitioners in the United Kingdom, and the Swedish National Council for Medical Ethics have characterized these interventions in children as experimental and dangerous. World renowned Swedish psychiatrist Dr. Christopher Gillberg has said that pediatric transition is "possibly one of the greatest scandals in medical history" and called for "an immediate moratorium on th
Reference:
Myth About Suicide and Gender Dysphoric Children (From ACP)
- Suicide risk among trans-identified youth is less than or comparable to that of other at-risk groups of youth.4
- Being trans-identified increases suicide risk by a factor of 13
- Anorexia increases risk by a factor of 18-31
- Depression multiplies it by a factor of 20
- Autism raises the risk by a factor of 8
- Children with gender dysphoria often also have depression, anorexia, autism, and other psychological conditions predisposing them to suicide. 5 Suicide among trans-identified youth may be due to the dysphoria, but maybe not – it could stem from the other psychological conditions or a combination of both.
- Prevention of suicide for trans-identified youth is the same as for other youth: talk therapy and FDA-approved psychiatric medications.6 As reported by the American Foundation for Suicide Prevention, "Ninety percent of people who die by suicide have an underlying — and potentially treatable — mental health condition."7 One study found that 96% of U.S. adolescents who attempt suicide suffer from at least one mental illness.8 There is no evidence trans-identified children who commit suicide are any different.
- The most up-to-date research shows the effectiveness of psychotherapy for resolving gender dysphoria in children and adolescents.9 A 2019 study confirms the findings of 16 studies dated 1969-2012, all showing that psychotherapy can be highly effective in treating underlying causes of gender incongruence such that trans- identifying patients embrace their biological sex. 10
- Puberty blockers actually cause depression and other emotional disturbances related to suicide.11 Discussing an experimental trial of puberty- blockers in the U.K., Oxford University Professor Michael Biggs wrote, "There was no statistically significant difference in psychosocial functioning between the group given blockers and the group given only psychological support. In addition, there is unpublished evidence that after a year on [puberty blockers] children reported greater self-harm, and that girls experienced more behavioral and emotional problems and expressed greater dissatisfaction with their body—so puberty blockers exacerbated gender dysphoria."12
- Cross-sex hormones (testosterone for women; estrogen for men) may disrupt mental health. Women who identify as men are given enough testosterone to raise their levels 10-40 times above the female reference range. Past studies have documented multiple psychiatric problems with similar high doses of anabolic steroids like testosterone such that 23% of subjects met DSM criteria for a major mood syndrome such as mania, hypomania, and major depression, and 3.4-12% developed psychotic symptoms.13 Estrogen also impacts mood in complex ways. Post menopausal women treated with estrogen often experience severe anxiety despite being placed on physiologic doses of the hormone. 14 Men who identify as women are given supraphysiologic doses of estrogen; theoretically, this has the potential to worsen both depression and anxiety.
- The most reliable research shows that in the long run, medical transition does not reduce and may even exacerbate the psychological distress that could lead to suicide. "The two largest and most complete studies (one from the Netherlands and one from Sweden), which show significantly elevated rates of completed suicides among gender-dysphoric individuals, both studied adults who had already transitioned to imitation of the opposite sex."15 These studies thus support the conclusion that transitioning does not reduce the risk of suicide and may even increase it. Transitioning merely masks the underlying psychological problems that are producing the dysphoria – it treats the symptoms rather than the disease.
- Suicide is prone to social contagion, meaning the more it occurs and is talked about, the more likely vulnerable kids will kill themselves.16 One medical researcher (an epidemiologist who himself transitioned to feminized male until he detransitioned after 13 years) calls out the manipulative use of the suicide threat to bully parents and legislators: "The trans industry's insistence and hype that [trans-identified adolescents] are constantly on the brink of transphobia-related suicide at rates that far exceed those of other highly relevant populations is a shameful social engineering strategy to keep society's focus preferentially on transgenderism – perhaps to cast themselves as visionary pioneers in the field. . . . trans activist adults and some clinicians effectively threaten suicide on behalf of the young people. They do this to socially-engineer, manipulate and intimidate non-industry doctors, politicians, community leaders and families of [these adolescents]. They are well aware of the emotional responses they will get with this rhetoric."
- Trans-identified teens may be encouraged, by social media and members of the transgender industry, to threaten suicide if their parents resist medical transition. Psychotherapist Dr. Wallace Wong offered such advice during a presentation in Canada: ""So what you need is, you know what? Pull a stunt. Suicide, every time, [then] they will give you what you need." Wong added that trans-identified kids "learn that. They learn it very fast."
Reference:
Urinary Tract Infections in Children
DUTY Clinical Decision Rules
| Characteristic | Points |
|---|---|
| Pain/Crying when passing urine | 2 |
| Smelly urine per parents | 2 |
| Previous UTI | 1 |
| Absence of severe cough | 2 |
| Severe illness present | 2 |
| Points | UIT Dx/Total Pts | LR |
|---|---|---|
| 0-2 | 9/2003 (0.45%) | 0.20 |
| 3-4 | 20/562 (3.6%) | 1.6 |
| 5+ | 31/175 (17.7%) | 9.6 |
| Characteristic | Points |
|---|---|
| Pain/Crying when passing urine | 2 |
| Smelly urine per parents | 2 |
| Previous UTI | 1 |
| Absence of severe cough | 2 |
| Severe illness present | 2 |
| Dipstick positive for: | |
| - Leukocytes | 2 |
| - Nitrites | 3 |
| - Blood | 1 |
| Points | UIT Dx/Total Pts | LR |
|---|---|---|
| 0-5 | 13/2444 (0.53%) | 0.24 |
| 6-8 | 18/240 (7.5%) | 3.6 |
| 9+ | 29/56 (51.8%) | 48 |
- Likelihood Ratio <1 = less likely to be UTI
- Likelihood Ratio >1 = more likely to be UTI
References:
- AFP Vol 97 No 4 Feb 2018
Vital Signs
Pediatric Blood Pressure:
- NB Systolic = 60 – 70
- Systolic = 70 + (2 x age)
- Diastolic = 2/3 systolic
Normal Vital Signs
| Age | Pulse | Resp |
|---|---|---|
| NB | 120 – 160 | 30 – 60 |
| < 1yo | 120 – 140 | 30 – 50 |
| 1-2 yo | 100 – 140 | 30 – 40 |
| 3-5 yo | 100 – 120 | 20 – 30 |
| 6-10 yo | 80 – 100 | 16 – 20 |
See also:
Normal pediatric vital signs
| Age | Pulse | Resp |
|---|---|---|
| NB | 120 - 160 | 30 - 60 |
| <1yo | 120 - 140 | 30 - 50 |
| 1-2yo | 100 - 140 | 30 - 40 |
| 3-5yo | 100 - 120 | 20 - 30 |
| 6-10yo | 80 - 100 | 16 - 20 |
BP:
- NB Systolic = 60 -70
- Systolic = 70 + (2 x age)
- Diastolic = 2/3 systolic
Down's Syndrome
Common physical characteristics with Down syndrome:
- Arched palate
- Brachycephaly (flattened head, usually occiput)
- Brushfield spots (hypopigmented iris spots)
- Clinodactyly (curved fifth finger)
- Ear abnormalities (low-set or folded)
- Epicanthal folds
- Excessive skin on nape of neck
- Flat facial profile (midface hypoplasia)
- Global muscular hypotonia
- Hyperflexibility
- Macroglossia (relative, secondary to midface hypoplasia)
- Microcephaly
- Short, broad hands
- Short fifth finger
- Short neck
- Single palmar crease
- Small nose
- Upward slant to eyes
- Widened gap between first and second toes (sandal sign)
Reference:
- AFP Mar 2025 Vol 111 No 5
Study: Epinephrine metered-dose inhaler for pediatric croup
Spoon Feed Epinephrine administration via metered-dose inhaler (MDI) for the treatment of croup in children may be a safe and effective alternative to nebulization.
Why does this matter? Croup is a common presentation in pediatric patients, especially during respiratory virus season. During the COVID-19 era, concern was raised over nebulization as an aerosol-generating procedure – can we effectively deliver epinephrine via MDI for children with croup?
'Sealing' the deal A quality assurance network of nine pediatric emergency departments (PEDs) in Canada developed algorithms for assessment and dosing of epinephrine MDI (i.e. over-the-counter Primatene Mist), with valved spacer device, for croup. Initially, five puffs of epinephrine MDI (125μg/puff) were administered. Patients were reassessed 10 minutes later using the Westley Croup Score (WCS), and adverse effects were recorded. Additional administration was recommended, up to 15 total puffs, if there was minimal change in WCS (<2 points) and no adverse effects.
Data were collected from seven PEDs from August 2020 to October 2021, including 210 children. The mean age was 36.4 (±29.27) months. Pre-treatment WCS was mild (0-2) in 27 children (12.9%), moderate (3-4) in 118 (56.2%), severe (5-7) in 60 (28.6%), and near respiratory failure (≥8) in five (2.4%). The median croup scores of pre- versus post-treatment were 4 and 1, with a median change of 2 (IQR 1-3) within 60 minutes of treatment (p < 0.001). There were two reports of agitation (0.7%), and two children had continued pre-existing tachycardia. No other adverse events were reported.
This study is limited by lack of a control group, though previous studies of nebulized racemic epinephrine show similar improvements in WCS.
Reference:
- Meckler GD, Alqurashi W, Eltorki M, Curtis SJ, Doyle E, Kam AJ, Lim R, MacPhee S, Schuh S, Wright B, Johnson DW. Epinephrine metered-dose inhaler for pediatric croup. Acad Emerg Med. 2023 Feb;30(2):144-146. doi: 10.1111/acem.14616. Epub 2022 Dec 7. PMID: 36307996.
Psychiatry
Addiction and Dependence
Principles of Effective Treatment Based on scientific research since the mid-1970s, the following key principles should form the basis of any effective treatment program:
- Addiction is a complex but treatable disease that affects brain function and behavior.
- No single treatment is right for everyone.
- People need to have quick access to treatment.
- Effective treatment addresses all of the patient's needs, not just his or her drug use.
- Staying in treatment long enough is critical.
- Counseling and other behavioral therapies are the most commonly used forms of treatment.
- Medications are often an important part of treatment, especially when combined with behavioral therapies.
- Treatment plans must be reviewed often and modified to fit the patient's changing needs.
- Treatment should address other possible mental disorders.
- Medically assisted detoxification is only the first stage of treatment.
- Treatment doesn't need to be voluntary to be effective.
- Drug use during treatment must be monitored continuously.
- Treatment programs should test patients for HIV/AIDS, hepatitis B and C, tuberculosis, and other infectious diseases as well as teach them about steps they can take to reduce their risk of these illnesses.
Medications used to treat dependence:
- Opioid
- Methadone
- Buprenorphine
- Extended-release naltrexone
- Lofexidine
- Nicotine
- Nicotine replacement therapies (available as a patch, inhaler, or gum)
- Bupropion
- Varenicline
- Alcohol
- Naltrexone
- Disulfiram
- Acamprosate
Behavioral Therapies:
- Cognitive-behavioral therapy seeks to help patients recognize, avoid, and cope with the situations in which they're most likely to use drugs.
- Contingency management uses positive reinforcement such as providing rewards or privileges for remaining drugfree, for attending and participating in counseling sessions, or for taking treatment medications as prescribed.
- Motivational enhancement therapy uses strategies to make the most of people's readiness to change their behavior and enter treatment.
- Family therapy helps people (especially young people) with drug use problems, as well as their families, address influences on drug use patterns and improve overall family functioning.
- Twelve-step facilitation (TSF) is an individual therapy typically delivered in 12 weekly session to prepare people to become engaged in 12-step mutual support programs. 12-step programs, like Alcoholic Anonymous, are not medical treatments, but provide social and complementary support to those treatments. TSF follows the 12-step themes of acceptance, surrender, and active involvement in recovery.
Resources:
- https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery
- https://americanaddictioncenters.org/adderall/how-to-quit
- https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/preface
- https://www.drugabuse.gov/publications/drugfacts/treatment-approaches-drug-addiction
Alcohol Use Disorder
According to the CDC, excessive drinking includes:
- Binge drinking (defined as 4+ drinks on a single occasion for women; 5+ for men)
- Heavy drinking (defined as 8+ drinks per week for women; 15+ for men)
| Medication | FDA | Cost | |
|---|---|---|---|
| Acamprosate | Yes | $55 | 1st line |
| Topiramate | No | $10 | 2nd line |
| Ondansetron | No | $20 | 2nd line |
| Disulfram | Yes | 2nd line | |
| Naltrexone | Yes | $45 |
For patients with alcohol use disorder:
- Naltrexone decreases alcohol consumption (LOE A)
- Reduces heavy drinking days and helps promote abstinence. Also helps manage cravings in some people.
- Once daily 50 mg pill or once monthly injection
- Acamprosate increases abstinence rates (LOE A)
- Reduces heavy drinking and maintains abstinence once someone is already sober. Also helps manage cravings in some people.
- Topiramate may decrease alcohol intake (LOE B)
- Ondansetron may decrease alcohol intake (LOE B)
- There is inconsistant evidence that Disulfram decreases alcohol intake (LOE B)
- Blocks the breakdown of alcohol in the body and causes unpleasant symptoms (Nausea)
- Symptoms can help some people not to drink alcohol
References:
- AFP Vol 93 No 6 Mar 2016
- JAMA Vol 325 No 6 Feb 2021
- AFP Mar 2016
Benzodiazepines edit
Stimulants
Steps in Stimulant Detox:
- With the help of a medical professional, set up a slow weaning schedule.
- Seek emotional support and guidance from a mental health professional during detox.
- Keep busy to distract from drug cravings.
- Maintain a healthy eating and sleeping schedule, and take all prescribed medications or supplements.
- Attend support groups, meetings, counseling sessions, family therapy, and aftercare programs.
Stimulant withdrawal symptoms:
- Insomnia
- Change in appetite
- Fatigue
- Irritability
- Depression
- Mood swings
- Anxiety
- Suicidal thoughts
- Tremors
- Headache
- Drug cravings
- Trouble concentrating
- Lack of motivation
- Seizures
- Muscle aches
References:
ADHD
Resources:
- ADHD Guidelines
- ADHD Diagnosis for pediatrics: Vanderbilt Assessment Scales
- ADHD Therapists: Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD)
See also:
Medications for Adult ADHD:
- Stimulants
- Methylphenidate
- Dextroamphetamine
- Dexmethylphenidate
- Mixed amphetamines (Adderall 5 mg bid; Adderall XR 10mg qAM)
- Lisdexamfetamine 30 mg qd
- Non-Stimulants
- Atomoxetine 40 mg qd
- The most common side effects of atomoxetine are nausea, decreased appetite (in 15%–20% of patients), insomnia, slightly increased diastolic blood pressure and heart rate, decreased libido, sweating, and dysuria.
- Guanfacine 1mg qhs
- Guanfacine is effective treatment for symptoms of ADHD. It is especially helpful for patients with liability for abuse of stimulants
- Clonidine 0.1 mg qhs
- Has effect on symptoms of hyperactivity and impulsivity, but not those of inattention.
- May be useful in some patients with comorbidity, particularly in the treatment of patients with comorbid ADHD and Tourette’s syndrome and other tic disorders
- Bupropion 150 mg qd
- Starting dose is usually 150 mg per day, and maximum daily dosage is 450 mg per day
- desipramine
- Tricyclic antidepressants improve mood and decrease hyperactivity, but do not improve concentration and cognitive tasks
- Therapy should start with a dose of 50 mg and every 7 days this dose can be increased by 50 mg until the optimal benefit are seen. The maximum dose is 300 mg per day
- Atomoxetine 40 mg qd
Notes:
- Most patients will respond to both drugs. However, 36% of patients respond preferentially to amphetamine compounds while 26% of patients respond preferentially to methylphenidate compounds.
- If short-acting methylphenidate or dextroamphetamine is used, the starting dose is 10 mg for methylphenidate or 5 mg for dextroamphetamine. This dose should be titrated upward for 10 mg or 5 mg every 7 days until the optimal benefit or until side effects prevent increases.
- If long-acting stimulant preparations are used, starting dose for extend released MPH (Concerta) is 18 mg, for the controlled released MPH (Biphentin) is 10 mg, and 5 mg for mixed amphetamine salts XR (Adderall XR).
Reference:
- Kolar D, Keller A, Golfinopoulos M, Cumyn L, Syer C, Hechtman L. Treatment of adults with attention-deficit/hyperactivity disorder. Neuropsychiatr Dis Treat. 2008 Apr;4(2):389-403. doi: 10.2147/ndt.s6985. PMID: 18728745; PMCID: PMC2518387.
ADHD Systems
Developing strategies for success is crucial for individuals with Attention Deficit Hyperactivity Disorder (ADHD). Here's a list of system ideas that can help:
- Task Management:
- Use a planner, app, or digital calendar to organize tasks and appointments.
- Break down large tasks into smaller, manageable chunks.
- Prioritize tasks based on importance and deadlines.
- Time Management:
- Set specific times for tasks, breaks, and leisure activities.
- Use the Pomodoro Technique: work for 25 minutes, then take a 5-minute break.
- Schedule regular check-ins with yourself to stay on track.
- Leave time between engagements to gather thoughts and help ease transitions.
- Organization:
- Designate a "launching pad" (e.g., a specific spot near the door) for essential items like keys, wallet, and bag.
- Use baskets, bins, or shelves to categorize and contain belongings.
- Implement a "one-touch rule": handle each piece of paper or task only once.
- Memory Aids:
- Create mental or visual reminders (e.g., post-it notes) for important events or deadlines.
- Use mnemonics or acronyms to help remember key information.
- Keep a "brain dump" journal to record thoughts and ideas as they come up.
- Self-Monitoring:
- Set daily goals and track progress using a habit tracker or journal.
- Use self-monitoring tools, such as a checklist or a timer, to stay focused.
- Develop a "stoplight system": green for go, yellow for caution, red for stop (helps with decision-making).
- Environmental Adjustments:
- Create a conducive work environment by controlling lighting, temperature, and noise levels.
- Use visual aids like diagrams, charts, or mind maps to understand complex information.
- Maintain a clutter-free desk or work area.
- Implement the "5-S" system: Sort, Set in order, Shine, Standardize, and Sustain (for organizing physical space).
- Technology Support:
- Utilize digital tools like apps, extensions, or browser plugins to stay organized and focused.
- Use text-to-speech software or a voice assistant to streamline tasks.
- Implement password management systems to reduce stress.
- Prioritization:
- Identify and prioritize most important tasks (MITs) for the day.
- Use the "Eisenhower Matrix" to categorize tasks based on urgency and importance.
- Focus on completing one task at a time to avoid overwhelm.
- Self-Care:
- Schedule regular self-care activities, such as exercise, breathing exercises, or meditation.
- Prioritize sleep and establish a consistent bedtime routine.
- Engage in activities that bring joy and relaxation (e.g., hobbies, reading).
- Accountability:
- Share goals and progress with a trusted friend, family member, or coach for support.
- Join a community group or online forum to connect with others who understand ADHD challenges.
- Schedule regular check-ins with a therapist or counselor.
- Flexibility
- Embrace the concept of "good enough" when perfection is not feasible.
- Develop a growth mindset and be open to learning from mistakes.
- Prioritize self-compassion and practice self-forgiveness when things don't go as planned.
Everyone with ADHD is unique, so it's essential to experiment and find the systems that work best for you. Be patient, stay flexible, and celebrate small victories along the way!
ADHD and depression
If depression is severe, it needs to be treated prior to treating ADHD. The best strategy for treating ADHD with comorbid depression is a combination of stimulant and antidepressant medications. SSRIs combined with stimulants can be safe and effective, while the chance for potential drug interactions is small
In patients with manic episode or bipolar disorder and ADHD, therapy with mood stabilizers and/or atypical antipsychotics is indicated before the treatment with stimulants. Bupropion could be a first choice medication for this comorbidity.
Reference:
- Kolar D, Keller A, Golfinopoulos M, Cumyn L, Syer C, Hechtman L. Treatment of adults with attention-deficit/hyperactivity disorder. Neuropsychiatr Dis Treat. 2008 Apr;4(2):389-403. doi: 10.2147/ndt.s6985. PMID: 18728745; PMCID: PMC2518387.
ADHD and anxiety disorders
Stimulant medications should be the first therapeutic intervention. Anxiety symptoms generally do not worsen on stimulant medication. A second treatment intervention would be specific therapy for anxiety disorders either with SSRIs or cognitive-behavioral therapy (CBT). The most beneficial treatment option is combined therapy.
Patients who received both dextroamphetamine and paroxetine improved in both ADHD and anxiety/depressive symptoms but not to the same extent as with monotherapy and they had more severe adverse events
Reference:
- Kolar D, Keller A, Golfinopoulos M, Cumyn L, Syer C, Hechtman L. Treatment of adults with attention-deficit/hyperactivity disorder. Neuropsychiatr Dis Treat. 2008 Apr;4(2):389-403. doi: 10.2147/ndt.s6985. PMID: 18728745; PMCID: PMC2518387.
ADHD Management
Children ages 4-6 years
- The first line of treatment should include
- Parent training in behavior management; and/or
- Behavioral classroom interventions (if available).
- Methylphenidate may be used if behavioral interventions do not provide significant improvement and the child continues to have serious problems.
Children and adolescents 6-18 years
- Recommended treatment for children and adolescents includes
- FDA-approved medications along with
- Parent training in behavior management and/or
- Behavioral classroom interventions.
- Treatments often work best when used together.
For all children attending school, the school is a necessary part of any treatment plan. These plans can include
- Educational interventions; and
- Individual school supports, such as school environment and behavioral supports.
School treatment plans often include an Individualized Education Program (IEP) or a 504 plan that describes accommodations.
Reference:
ADHD Resources
Adult ADHD
- Regular 61 Question version: http://www1.psykiatristod.se/Global/Psykiatristod/Bilagor/ADHD/WURS_ADHD_.pdf
- Short 25 Question version: https://www.uvm.edu/medicine/ahec/documents/Wender_Utah_Rating_Scale.pdf
- Adult ADHD Self-Report Scale Symptom Checklist (WHO): https://add.org/wp-content/uploads/2015/03/adhd-questionnaire-ASRS111.pdf
ADHD Accomodations edit
Does ADHD mean I am:
- Distractible or Superobservant?
- Internal Distractions or Rich Imagination?
- Hyperfocusing or Enormous Capacity to Concentrate?
- Impulsive or Capable of Quick Responses?
- Hyperactivity or High Energy Level?
- Inattention to Detail or Capacity to See the Big Picture?
- Easily Bored or Tremendous Capacity for Innovation?
Here are suggestions for getting started from an employee's perspective:
- Analyze the task that is giving you difficulty (be exact about the nature of the problem or barrier)
- What aspect of your ADHD contributes to this difficulty,
- Brainstorm solutions around work environment, work style, communication style, between yourself and supervisor, and the job itself,
- Implement one solution at a time,
- Assess whether the accommodation is meeting your needs, meet with the supervisor to share feedback, implement necessary adjustments in work routines in order to sustain your progress.
Self directed Accomodations for ADHDers
Simple Accommodations Can Make a Difference
- Strategies to Consider:
- Request a standardized template for recurring reports that include necessary formulas
- Accommodations can make a difference
- Color-coding: multi-color pens, highlighters and folders
- Request instructions, questions and memos in writing when possible
- Make a habit of taking notes at meetings and typing notes to keep as electronic reference files
- Create specific folders in email and on desktop
- Become cognizant of things that trip you up – like having multiple copies of the same document, not printing work for a visual review before submitting
- Utilize electronic calendars, reminder features
- Ask for accommodations tailored to the work that you do (an example would be to ask for staff to add specific email titles to emails so the search function would be more receptive)
- For routine duties with intricate instructions, develop a Project Instructions document that can be easily referenced for use
- Eraser marker board – color code; list recurring duties on marker board and locate it near you
- Create a checklist, place it in a visible place and use it
- Disclose your ADHD to other coworkers as needed
Below is a non-exhaustive list of accommodations many adults with ADHD like you have found helpful. Keep an open mind and work with your employer to "experiment" with different accommodations. If an approach helps, keep it. If it doesn't, move on to something else.
- Inattention and Distractibility
ADHDers cannot filter noises, interruptions, and even movement around the office as well as those who don't have ADHD. People with ADHD also are easily distracted by their own thoughts. They may find it challenging to pay attention to a conversation when there are too many distractions in the environment. The following strategies can help alleviate this problem:
- Using earphones for listening to music or white noise.
- Working in unused space when completing work that requires focus or attention to details.
- Transferring phone calls directly to voicemail, and responding to them in batches at specific times in the day.
- Keeping a notebook on your desk to jot down ideas and thoughts to avoid interrupting your work flow.
- Keeping a list of ideas that come to you during meetings to avoid interrupting people.
- Staying away from multitasking and performing one task at a time. Humans cannot really pay attention to more then one task at a time.
- Requesting a private office, taking work home, or working when others are not in the office.
- Creating a no-interruption period in the day that you communicate to colleagues.
- Impulsivity
- Creating scripts and working with a coach to role-play appropriate responses to recurrent challenging situations.
- Learning to monitor impulsive actions by using self-talk.
- Requesting regular, constructive feedback.
- Engaging in relaxation and meditation techniques.
- Anticipating triggers to impulsive reactions and developing new ways of coping with them.
- Time Management
- Using a day planner that you carry with you (ideally use an application that synchronizes with your smart phone) to keep track of meetings and tasks.
- Using wall or desk charts to break large projects into smaller pieces.
- Assigning due dates to each task.
- Using notifications (such as alarms on your computer or devices).
- Scheduling travel time to meetings and appointments and setting alerts taking them into account in your electronic calendar.
- Programming your computer to beep ten or fifteen minutes before you need to leave for a meeting on the calendar.
- Scheduling buffer time in your calendar for unexpected delays or interruptions in your day.
- Avoiding over-scheduling the day by overestimating how long each task or meeting will take.
- Poor Working Memory
- Recording (on a tape recorder, or your smart phone) "notes-to-self" or meetings instead of taking copious notes at meetings.
- Writing checklists or recording complicated tasks and processes.
- Using visual ways to remember information such as a bulletin board.
- Having auditory reminders on your computer for announcements and other memory triggers.
- Using a day planner that you carry with you (ideally use an application that synchronizes with your smart phone) to keep track of meetings and tasks.
- Writing notes on sticky pads and putting them in a highly visible place.
- Managing complex or long-term projects
- Breaking projects up into milestones with closer due dates and breaking milestones into tasks.
- Striving to shorten the time allowed on a project to better utilize "sprinting abilities."
- Asking a coach or your supervisor to assist you in identifying priorities.
- Looking for work or choosing assignments that requires only short-term tasks.
- Partnering with a co-worker with good organizational skills.
- Paperwork & Details
- Requesting an administrative assistant to handle or to double-check detailed paperwork.
- Making it a rule to handle each piece of paper only once.
- Keeping only those papers that are currently in use; purging the rest.
- Using color-coded folders and catchy labels to make filing more compelling.
- Adding the task of reviewing your detailed paperwork when you are less tired.
- Challenges with Boring Tasks
Adults with ADHD almost always have challenges when faced with long, boring tasks or tasks that require a lot of detail because these tasks do not stimulate the ADHD brain enough to allow focus. You can inject interest into tasks by:
- Setting a timer for, say, 30 minutes and racing the timer to stay on task.
- Breaking up long tasks into shorter ones.
- Taking multiple breaks, then getting up and walking around.
- Finding a job where most of your work is stimulating to you.
- Bartering or exchanging work with a colleague who likes the type of tasks that bore you for tasks you prefer doing.
- Interpersonal and Social Activities
Individuals with ADHD sometimes interrupt others and are too blunt, talk too much, and don't listen or pay attention to what others are saying. This is often interpreted as rude or uncaring behavior. You can reduce these challenges by:
- Asking a trusted colleague to provide kind but constructive feedback when interacting with others.
- Asking a trusted co-worker to provide discrete cues when you're crossing the line. Eventually, you'll get better at picking up social cues.
- Working with a coach to identify situations that often lead to interpersonal/social issues and creating a plan to overcome them.
- If working with others is challenging for you, you may want to find a position with greater fewer interactions with others.
- Procrastination
- Asking a supervisor to set deadlines for tasks and hold you accountable.
- Teaming with another person who can be your accountability buddy.
- Breaking project into tasks and finding ways to reward yourself as you accomplish each task.
- Hyperactivity
- Taking intermittent breaks from long tasks by choosing shorter, more physical, tasks like filing, delivering mail to others, or by taking a short walk between tasks.
- Taking active notes in meetings or when you are reading long documents to prevent restlessness.
- Moving around when you begin to feel restless. Exercising or taking a walk at lunch or during breaks.
Reference:
ADHD Accomodations edit
Accommodations
IEP and 504 Plans can offer accommodations for students to help them manage their ADHD, including:
- Extra time on tests;
- Instruction and assignments tailored to the child;
- Positive reinforcement and feedback;
- Using technology to assist with tasks;
- Allowing breaks or time to move around;
- Changes to the environment to limit distraction; and
- Extra help with staying organized.
Did you know?
Parents of children with ADHD report receiving more services through an IEP than through a 504 plan.2
There is limited information about which types of accommodations are effective for children with ADHD.3 However, there is evidence that setting clear expectations, providing immediate positive feedback, and communicating daily with parents through a daily report card can help.4
Here are some tips for classroom success. Communication
- Give frequent feedback and attention to positive behavior;
- Be sensitive to the influence of ADHD on emotions, such as self-esteem issues or difficulty regulating feelings;
- Provide extra warnings before transitions and changes in routines; and
- Understand that children with ADHD may become deeply absorbed in activities that interest them (hyper-focus) and may need extra assistance shifting their attention.
Assignments and Tasks
- Make assignments clear—check with the student to see if they understand what they need to do;
- Provide choices to show mastery (for example, let the student choose among written essay, oral report, online quiz, or hands-on project;
- Make sure assignments are not long and repetitive. Shorter assignments that provide a little challenge without being too hard may work well;
- Allow breaks—for children with ADHD, paying attention takes extra effort and can be very tiring;
- Allow time to move and exercise;
- Minimize distractions in the classroom; and
- Use organizational tools, such as a homework folder, to limit the number of things the child has to track.
Develop a Plan That Fits the Child
- Observe and talk with the student about what helps or distracts them (for example, fidget tools, limiting eye contact when listening, background music, or moving while learning can be beneficial or distracting depending on the child);
- Communicate with parents on a regular basis; and
- Involve the school counselor or psychologist.
Close collaboration between the school, parents, and healthcare providers will help ensure the child gets the right support.
College Accomodations and ADHD What Students with ADHD Can Provide for Themselves
Students with ADHD can set themselves up for a great college experience when they advocate for themselves and get the support they need. Here are a few important ways they can do so: Make Good Choices
Choose a college with reasonable accommodations and support groups for students with ADHD Ensure the college you decide on has a large number of ADHD-LD specialists Choose a college with many registered ADHD students Disclose your ADHD diagnosis at the earliest possible opportunity to trusted student services staff and advisors Request appropriate accommodations, including those that the school may not readily offer
Contact Your Support Team
School's office of disability: Get familiar with its resources Health officials: Get documentation that proves your ADHD status and proof that ADHD affects your academic performance Writing center: Fully utilize your school's writing center for help with written assignments Professors: Make use of office hours to meet your professors and set up appointments to clarify assignments.
Find Resources
Access support from tutors, whether on campus or online Find a healthy study environment early on, free of distractions Time management resources, including a schedule that includes time for studying, socializing, and exercising Find a study buddy or study group. Sign up for classes with friends, or make friends in the classes you have, to support each other in and out of class Consider an academic coach (through the college counseling office or privately) that will check in with you throughout the week to ensure success
Improve Your Skills and Habits to Manage ADHD in College
Self-advocacy skills to build self-esteem and avoid frustrations Socializing time and social skills Perspective on your future goals and carrier Perseverance and procrastination Sleep habits to be able to get up early in the morning to catch your classes Self-expectations: ADHD is with you for life, so you will continue to need support and treatment through college and beyond.
College Accommodations and ADHD
ADHD is one of the most under-recognized and underserved neurodevelopmental disorders in adults. Untreated, its impact on adults is severe. Success Comes with Support and Accommodations
To succeed, students with ADHD need a comprehensive system of support that fosters academic engagement, clear academic goals, student success, and career preparation. Training in time management, planning, organization, and knowledge management promotes persistence among students with weaknesses in these areas.
College students must seek out the support they need and construct their own scaffolding in this new environment. It is exceedingly important that college students learn to advocate for themselves and seek out support to ensure success in the classroom and beyond.
-—
What Students with ADHD Can Provide for Themselves
Students with ADHD can set themselves up for a great college experience when they advocate for themselves and get the support they need. Here are a few important ways they can do so: Make Good Choices
Choose a college with reasonable accommodations and support groups for students with ADHD Ensure the college you decide on has a large number of ADHD-LD specialists Choose a college with many registered ADHD students Disclose your ADHD diagnosis at the earliest possible opportunity to trusted student services staff and advisors Request appropriate accommodations, including those that the school may not readily offer
Contact Your Support Team
School's office of disability: Get familiar with its resources Health officials: Get documentation that proves your ADHD status and proof that ADHD affects your academic performance Writing center: Fully utilize your school's writing center for help with written assignments Professors: Make use of office hours to meet your professors and set up appointments to clarify assignments.
Find Resources
Access support from tutors, whether on campus or online Find a healthy study environment early on, free of distractions Time management resources, including a schedule that includes time for studying, socializing, and exercising Find a study buddy or study group. Sign up for classes with friends, or make friends in the classes you have, to support each other in and out of class Consider an academic coach (through the college counseling office or privately) that will check in with you throughout the week to ensure success
Improve Your Skills and Habits to Manage ADHD in College
Self-advocacy skills to build self-esteem and avoid frustrations Socializing time and social skills Perspective on your future goals and carrier Perseverance and procrastination Sleep habits to be able to get up early in the morning to catch your classes Self-expectations: ADHD is with you for life, so you will continue to need support and treatment through college and beyond.
Reference:
Accommodations That Can Help Students with ADHD edit
Examples of accommodations which teachers can make to adapt to the needs of students with ADHD.
- Seat student in quiet area
- Seat student near good role model
- Seat student near teacher
- Seat student near "study buddy"
- Increase distance between desks
- Allow extra time to complete assigned work
- Shorten assignments or work periods to coincide with span of attention; use timer
- Break long assignments into smaller parts so student can see end to work
- Assist student in setting short term goals
- Give assignments one at a time to avoid work overload
- Require fewer correct responses for grade
- Reduce amount of homework
- Instruct student in self-monitoring of behavior using cueing (i.e. hand raising, calling out)
- Pair written instructions with oral instructions
- Provide peer assistance in note taking
- Give clear, concise instructions
- Seek to involve student in lesson presentation
- Cue student to stay on task (i.e. private signal)
- Ignore minor, inappropriate behavior
- Increase immediacy of rewards and consequences
- Use time-out procedure for misbehavior
- Supervise closely during transition times
- Use "prudent" reprimands for misbehavior (i.e. avoid lecturing or criticism)
- Attend to positive behavior with compliments etc.
- Set up behavior contract
- Call on only when hand is raised in appropriate manner
- Praise when hand raised to answer question
- Allow student to stand at times while working
- Provide opportunity for "seat breaks" (i.e. run errands, etc.)
- Provide short break between assignments
- Remind student to check over work product if performance is rushed and careless
- Give extra time to complete tasks (especially for students with slow motor tempo)
- Provide reassurance and encouragement
- Frequently compliment positive behavior and work product
- Speak softly in non-threatening manner if student shows nervousness
- Review instructions when giving new assignments to make sure student comprehends directions
- Look for opportunities for student to display leadership role in class
- Conference frequently with parents to learn about student's interests & achievements outside of school
- Send positive notes home
- Make time to talk alone with student
- Encourage social interactions with classmates if student is withdrawn or excessively shy
- Reinforce frequently when signs of frustration are noticed
- Look for signs of stress build up and provide encouragement or reduced work load to alleviate pressure and avoid temper outburst
- Spend more time talking to students who seem pent up or display anger easily
- Provide brief training in anger control: encourage student to walk away; use calming strategies; tell nearby adult if getting angry
- If reading is weak: provide additional reading time; use "previewing" strategies; select text with less on a page; shorten amount of required reading; avoid oral reading
- If oral expression is weak: accept all oral responses; substitute display for oral report; encourage student to tell about new ideas or experiences; pick topics easy for student to talk about
- If written language is weak: accept non-written forms for reports (i.e. displays, oral, projects); accept use of typewriter, word processor, tape recorder; do not assign large quantity of written work; test with multiple choice or fill-in questions
- If math is weak: allow use of calculator; use graph paper to space numbers; provide additional math time; provide immediate correctness feedback and instruction via modeling of the correct computational procedure
- Ask for parental help in encouraging organization
- Provide organization rules
- Encourage student to have notebook with dividers and folders for work
- Provide student with homework assignment book
- Supervise writing down of homework assignments
- Send daily/weekly progress reports home
- Regularly check desk and notebook for neatness, encourage neatness rather than penalize sloppiness
- Allow student to have extra set of books at home
- Do not penalize for poor handwriting if visual-motor defects are present
- Encourage learning of keyboarding skills
- Allow student to tape record assignments or homework
- Praise compliant and appropriate behavior
- Provide immediate feedback
- Use teacher attention to reinforce positive behaviors
- Acknowledge positive behavior of nearby student
- Implement classroom behavior management system
- Monitor social interactions
- Set up social behavior goals with student and implement a reward program
- Prompt appropriate social behavior either verbally or with private signal
- Encourage cooperative learning tasks with other students
- Provide small group social skills training
- Praise student frequently
- Assign special responsibilities to student so others observe student in a positive light
Reference:
- Revisions made from original article; original provided by Attention Deficit Disorder Resources. Article by Harvey C. Parker, Ph.D, a clinical psychologist and co-founder of CHADD (Children & Adults with ADD)
- https://prntexas.org/wp-content/uploads/2017/11/72-Accommodations-That-Can-Help-Students-with-ADHD-TA.pdf
Anxiety
Treatment:
- Measure symptom severity with GAD-7
- Repeat measurement each visit to track disease severity and assess treatment response
- 1 of every 3 patients with anxiety disorders will relapse with discontinuation of antidepressant (LOE: A-)
- 1 out of 6 patients with anxiety disorders previously successfully treated will replapse despite continued treatment (LOE: A- )
- Mindfulness and Opposite Action Skills
Stepped care:
- Lifestyle interventions
- Physical exercise
- Mindfulness stress reduction
- Patient education
- Pharmacotherapy or cognitive behavioral therapies or both
- Antidepressant (SSRI or SNRI)
- Trial period 8-10 weeks including 2 weeks at highest tolerated dose. If effective, maintain for 9-12 months before taper is considered
- NNT = 7 for 50% reduction
- CBT by qualified therapist
- Education
- Self monitoring
- Cognitive restructuring
- Exposure therapy
- Breathing retraining or relaxation
- Antidepressant (SSRI or SNRI)
- If inadequate response
- Switch treatment strategy (CBT, antidepressant, etc)
- Change antidepressant
- Refer to psychiatrist for advanced medication management
References:
- JAMA Vol 318 No 3 Jul 2017
- AFP VOl 97 No 9 May 2018
- AFP Oct 2025 Vol 112 No 4
Botanicals and Supplements
Botanicals
- Ashwagandha
- Appears effective based on systematic review of RCTs
- Chamomile extract
- Appears effective based on systematic review and meta-analysis of RCTs
- Kava kava
- Possible modest effect
- Lavender extract
- Appears effective based on systematic review of RCTs
- Passion flower
- Evidence inconclusive
- St John's Wort
- Evidence inconclusive - most evidence is with depression
- Valerian
- Evidence inconclusive
Supplements
- 5-hydroxytryptophan
- Evidence inconclusive
- Magnesium
- Appears effective based on systematic review and meta analysis of RCTs
Reference:
- AFP Aug 2022 Vol 106 No 2
GAD-7 Assessment for Generalized Anxiety Disorder
First Line: SSRIs or SNRIs
Over the previous 2 weeks, how often has the patient been bothered by the following problems?
- Feeling nervous, anxious, or on edge
- Not being able to stop or control worrying
- Worrying too much about different things
- Trouble relaxing
- Being so restless that it is hard to sit still
- Becoming easily annoyed or irritable
- Feeling afraid as if something awful might happen
Questions are answered as:
- Not at all = 0pts
- Several days = 1pt
- More than half the days = 2pts
- Nearly every day = 3pts
GAD7 Scoring
| Score | Symptom Severity | Comments |
| 5-9 | Mild | Monitor |
| 10-14 | Moderate | Possible clinically significant condition |
| >15 | Severe | Active treatment probably warranted |
NOTE: For Panic Disorder, Social Phobia, & PTSD, cutoff score of 8 may be used for optimal sensitivity/specificity (see Evidence section).
Reference:
- JFP Vol 65 No 4 Apr 2016
- JFP Vol 69 No 7 Sep 2020
Panic Disorder
Screen for Panic Disorder
| Question | 0 | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| When nervous, how often do you think you will pass out? | Never | Rare | 1/2 time | Usually | Always | |
| In last 7d, how much have you been bothered by pains in the chest? | Not | A little | Mod | Quite a bit | Extreme | |
| To what degree is your CP tiring or exhausting? | None | Mild | Mod | Severe |
- 67% with score <5 will not have panic disorder
- 71% with >4 will have panic disorder
Effective medications:
- benzodiazepines
- TCAs
- SSRIs (best balance of effectiveness vs risk)
Reference:
- AFP Vol 106 No 6 Dec 2022
- JFP Vol 63, No 5 May 2015
Autism
The DSM5 criteria for autism spectrum disorder require deficits in three areas of communication and social interaction across multiple settings, with at least two restricted or repetitive behaviors, not explained by another condition, and causing functional impairment.
AAP recommends screening at ages 18 and 24 months. Screening in adults is not recommended.
Autistic individuals have a 20-30 yr lower life expectancy than nonautistic people and experience higher rates of many chronic conditions, such as diabetes, epilepsy, gastrointestinal concerns, feeding disorders, and mental health disorders.
Treatment of children with autism spectrum disorder focuses on minimizing core deficits, maximizing functional independence, and preventing problem behaviors.
Pharmacologic therapy may be indicated for related conditions or symptoms, such as sleep disorders, seizures, mental health conditions, behavior problems, and gastrointestinal issues.
Melatonin effectively reduces sleep symptoms and improves daytime behaviors with minimal adverse effects.
The SPACE (sensory, predictability, acceptance, communication, empathy) framework provides specific interventions that make health care more accessible and affirming to autistic patients.
Reference:
- Am Fam Physician. 2025;112(3):294-300
Medication Management for Autism
- Selective serotonin re-uptake inhibitors (SSRIs)
This group of antidepressants treats some problems that result from imbalances in the body's chemical systems.
- SSRIs might reduce the frequency and intensity of
- repetitive behaviors
- decrease anxiety
- irritability, tantrums, and aggressive behavior
- improve eye contact
- Most common: fluoxetine and sertraline
- SSRIs might reduce the frequency and intensity of
- Tricyclics These medications are another type of antidepressant used to treat depression and obsessive-compulsive behaviors. These drugs seem to cause more minor side effects than do SSRIs. They are sometimes more effective than SSRIs for treating certain people and certain symptoms.
- Psychoactive or anti-psychotic medications These types of medications affect the brain of the person taking them. The anti-psychotic drug risperidone is approved for reducing irritability in 5-to-16-year-olds with autism. These medications can decrease hyperactivity, reduce stereotyped behaviors, and minimize withdrawal and aggression among people with autism.
- Stimulants This group of medications can help to increase focus and decrease hyperactivity in people with autism. They are particularly helpful for those with mild ASD symptoms.
- Anti-anxiety medications This group of medications can help relieve anxiety and panic disorders, which are often associated with ASD.
- Anticonvulsants These medications treat seizures and seizure disorders, such as epilepsy. (Seizures are attacks of jerking or staring and seeming frozen.) Almost one-third of people with autism symptoms have seizures or seizure disorders.
References:
SPACE Framework
Sensory, Predictability, Acceptance, Communication, Empathy Sensory
- Sight
- Turn off or down artificial lights
- Avoid flickering or oscillating environmental features
- Avoid highly stimulating decor
- Promote the use of sunglasses
- Sound
- Consider environmental sounds
- Reduce auditory clutter
- Avoid conversation in noisy environment
- Promote the use of noise-canceling headphones near plugs
- Smell
- Avoid wearing perfume or highly-sensitive cosmetics or toiletries
- Avoid aerosols or chemical air fresheners
- Avoid highly-sensitive cleaning products
- Consider ventilation
- Open windows where possible
- Taste
- Respect sensory preferences when considering nutrition
- Consider taste and texture of medications
- Consider non-standard medication formulations where necessary
- Touch
- Ask about tactile preferences and modify examination technique
- Avoid casual touch
- Promote sensory-friendly clothing choices
- Consider using sensory aids such as weighted blankets
- Proprioception
- Understand the need for proprioceptive input
- Avoid making inferences from unusual body posture
- Temperature
- Consider environmental temperature
- Adjust temperature where required
- Interoception and pain
- Ask directly about internal sensations but understand that answering may be difficult
- Pay attention to verbal reports of pain where possible
- Be aware that non-verbal expression of pain may be different
- Consider the need for adapted pain scales
- Predictability
- Give realistic information in advance
- Ensure clear and accurate directional signage in physical spaces
- Provide photographs or videos of the physical environment and staff
- Allow waiting in a familiar environment
- Ensure care is provided by staff familiar with the patient where possible
- Acceptance
- Neurodiversity-affirmative approach, beneficial
- Understand autistic-stimming and monotropic thinking patterns
- Facilitate need for detailed information
- Understand distressed behavior
- Communication
- Understand autistic-verbal and non-verbal communication differences
- Know that communication ability is reduced by anxiety and sensory stress
- Clear and ambiguous communication required
- Avoid phone-based appointment systems
- Promote the use of augmentative and alternative communication
- Empathy
- Recognize that autistic people feel empathy but may display it differently
- Empathy towards autistic patients may be more challenging for non-autistic healthcare professionals
- Physical space
- Expect a need for increased personal space Avoid proximity to other people where possible
- Temporal space
- Allow increased time to respond to questions Allow increased time for decision making
- Emotional space
- Expect differences in emotional expression Allow restorative solitude to recover without additional input if distressed
Reference:
- Am Fam Physician. 2025;112(3):294-300
Bipolar Disorder
- Screen all patients 12 years and older for depression, including all pregnant patients in the perinatal period; screening should be implemented with adequate systems in place to support accurate diagnosis, psychotherapy, and follow-up. LOE B
- Lithium, valproic acid (Depakote), and some antipsychotics are effective single agents for acute mania. LOE A
- Effective combination therapies for acute mania include lithium or valproic acid with quetiapine (Seroquel) or risperidone (Risperdal). LOE A
- Quetiapine and cariprazine (Vraylar) are effective single agents for the treatment of acute bipolar depression. LOE A
- Lurasidone (Latuda) combined with lithium or valproic acid is an effective treatment for acute bipolar depression. LOE A
- Lithium, quetiapine, or a combination of quetiapine and lithium or valproic acid is effective for maintenance of bipolar disorder. LOE A
| Medication | Type I Maint | Type II Main | Acute Mania | Acute Depression |
|---|---|---|---|---|
| Aripiprazole | + + | + + | + + | - |
| Carbamazepine | + + + | + + + | + + | - |
| Lamotrigine | + + + | + + + | - | + |
| Lithium | + + + | + + + | + + + | No |
| Lurasidone | - | - | + | + + + |
| Olanzapine | + + | + | + + + | + + |
| Olanzapine/fluoxetine | - | - | - | + + + |
| Oxcarbazepine | + + + | + + + | + | - |
| Quetiapine | + | + | + + + | + + + |
| Risperidone | + + | + | + + + | - |
| Valproic acid | + + + | + + + | + + + | - |
| Ziprasidone | + + | + | + + + | - |
Recommended First line for Bipolar I:
- Monotherapy:
- Quetiapine 50mg d1, 100 mg d2, 200mg d3 - goal dose 300-600 mg/d
- Lithium 150-300 mg po qhs
- For breakthrough add:
- lurasidone, lamotrigine, or quetiapine
- For breakthrough add:
- Lamotrigine 25mg x14d, 50 mg for 14 d, then 100 mg for 7d, then 200 mg/d
- Lurasidone
- Combination:
- Olanzapine 5 mg plus fluoxetine 20 mg
Maintenance for bipolar I:
- Quetiapine
- Lithium
- Aripiprazole
- Risperidone
- Olanzapine
| Medication | Acute depression | Acute Mania | Depression prevention | Mania prevention | Notes |
|---|---|---|---|---|---|
| Quetiapine | Yes | Yes | Yes | Yes | Fatigue, weight gain |
| Lithium | No | Yes | Yes | Yes | Tremors, Weight gain, safest in pregnancy |
| Lamotrigine | No | No | Yes | No | Most effective preventing depression |
| Olanzapine | Yes | Yes | Yes | Yes | Most weight gain |
| Drug type | Drug | Starting dosage | Cost* | Manic | Mixed | Maintenance | Depression |
|---|---|---|---|---|---|---|---|
| Salts | Lithium | 300 mg twice daily, titrated to a therapeutic level | $5.00 | Yes | No | Yes | No |
| Atypical antipsychotics | Aripiprazole (Abilify) | 1 mg daily | $20 ($1,200) | Yes | Yes | Yes | No |
| Atypical antipsychotics | Asenapine (Saphris) | 2.5 mg sublingually twice daily | NA ($600) | Yes | Yes | No | No |
| Atypical antipsychotics | Cariprazine (Vraylar) | 1.5 mg daily | NA ($1,220) | Yes | Yes | No | No |
| Atypical antipsychotics | Lurasidone (Latuda) | 20 mg daily | NA ($1,300) | No | No | No | Yes |
| Atypical antipsychotics | Olanzapine (Zyprexa) | 10 mg daily | $10 ($650) | Yes | Yes | Yes | Yes |
| Atypical antipsychotics | Olanzapine/fluoxetine (Symbyax) | 6 mg/25 mg daily | $75 ($405) | No | No | No | Yes |
| Atypical antipsychotics | Quetiapine (Seroquel) and quetiapine ER (Seroquel XR) | 300 mg daily | $20 ($575) $20 ($450) | Yes | Yes | Yes | Yes |
| Atypical antipsychotics | Risperidone (Risperdal) | 2 to 3 mg daily | $10 ($1,800) | Yes | Yes | No | No |
| Atypical antipsychotics | Ziprasidone (Geodon) | 40 mg twice daily | $20 ($1,200) | Yes | Yes | No | No |
| Anticonvulsants | Carbamazepine (Tegretol) | 100 mg twice daily | $65 ($330) | Yes | Yes | No | No |
| Anticonvulsants | Valproic acid (Depakote) or valproate (Depacon) | 15 to 20 mg per kg divided in two doses | $30 ($1,100) | Yes | No | No | No |
| Anticonvulsants | Lamotrigine (Lamictal) | 200 mg daily | $10 ($550) | No | No | Yes | No |
Differential:
- Bipolar disorder type I
- At least 1 manic episode causing social or occupational impairment with varying degrees of depression
- Bipolar disorder type II
- Varying degree of chronic depression with at least 1 hypomanic episode, often more.
- No overt manic episodes.
- Cyclothyic disorder
- Recurrent hypomanic or depressive symptoms, but never meeting criteria for hypomanic or depressive episode
- Sympomts span at least 2 years
- Symptoms never absent for more than 2 months at a time
- Generalized anxiety disorder
- Generalized worry, with or without depression
- Depressive disorder
- Depressed or anhedonic mood with no history of hypomania or mania
- Posttraumatic stress disorder
- History of trauma and severe anxiety, depressed mood
- No history of mania or hypomania
- Psychotic disorder
- Hallucinations and/or delusions without mania or depression
- Substance use disorder/acute intoxication
- Possible hypomania, mania, or depressed mood
- Linked to a substance either by history or testing
- Borderline personality disorder
- Symptoms similar to mania, hypomania, or depressed mood
References:
- JFP Vol 66 No 6 Jun 2017
- JFP Vol 69 No 7 Sep 2020
- AFP Feb 2021 Vol 103 No 4
- AFP Vol 109 No 6 Jun 2024
Cognitive Behavior Therapy
Consists of:
- One 60-90min session per week for 8-12 weeks
- Symptom measures are collected freq
- Treatment is goal oriented and collaborative - patient is active participant
- Treatment is focused on changing current problematic or maladaptive thoughts or behaviors
- Weekly homework assignments
Resources:
- Academy of Cognistive Therapy - Therapist locator: www.academyofct.org
- American Psychological Association - Therapist locator: locator.apa.org
- Psychology Today - Therapist locator: therapists.psychologytoday.com/rms/profsearch.php
Reference:
- AFP Vol 2 No 9 Nov 2015
Dialectal Behavior Therapy
Apps:
DBT interventions:
- Mindfulness: Living in the moment without fear of the future or worry from the past
- Wise Mind: Emotion mind is when we use feelings alone to determine our decisions and behavior, whereas Logic mind is when we use only logic/reasoning, ignoring our feelings. With wise mind, we recognize and respect our feelings while responding to them in a rational way.
- Focus shifts to experience, getting things done, and use of intuition. Example, "I'm feeling insecure and alone because they have not responded, but they are probably just busy at work. I need to take a little extra care of myself when I feel this way. I'll take a 10 minute walk."
- Wise Mind: DBT skill | Worksheet | Therapist Aid
“what” and “how” skills are the components of mindfulness. “What” skills refer to what someone actually does to be mindful, while “how” skills refer to the mindset they bring to these actions.
“What” skills include: “How” skills include: Observe Nonjudgmentally Describe One-mindfully Participate Effectively
- Wise Mind: Emotion mind is when we use feelings alone to determine our decisions and behavior, whereas Logic mind is when we use only logic/reasoning, ignoring our feelings. With wise mind, we recognize and respect our feelings while responding to them in a rational way.
- Distress tolerance: Managing challenging emotional experiences through distraction and living in the moment
- Radical Acceptance
- Accept things as they are, not as you wish them to be.
- Disappointment, pain, and setbacks are a normal part of life.
- You have the ability to determine why life is worth living.
- Accept things as they are, not as you wish them to be.
- Self-Soothe with Senses
- Use the five senses to experience or think about something relaxing, comforting, awe-inspiring, or pleasant to you to induce calmness.
- For example, "I can ground myself in the present moment by noticing five things that I can see, hear, smell, and touch."
- Distraction (ACCEPTS) - DBT Skill: ACCEPTS | Worksheet | Therapist Aid
- Activities
- Do an activity that requires thought and concentration
- Contributing
- Do something that allows you to focus on another person
- Comparisons
- Put your situation perspective by comparing it to something more painful or distressing
- Emotions
- do something to create a new emotion that will compete with your distressing emotion
- Pushing Away
- Avoid a painful situation or block it from your mind using a technique such as imagery
- Thoughts
- Use a mental strategy or activity to shift your thoughts to something neutral
- Sensations
- Find safe physical sensations to distract you from distressing emotions
- Activities
- 4 skills that clients can use as a mental health first-aid kit when in distress (DBT-TIPP)
- Temperature (cold): Slows heart rate and distracts from intrusive thoughts and intense emotions
- Intense exercise: Lowers stress hormones and increases feel-good neurotransmitters
- Paced breathing: Increases oxygen intake and lowers heart rate and blood pressure
- Progressive muscle relaxation: Helps the body let go of stress and triggers the relaxation response
- Radical Acceptance
- Emotional regulation: Emotions are valuable to our lived experience; learn to name, manage, and accept emotions
- 4 Skills:
- Act Opposite
- If you have a powerful negative emotion, do the opposite of your initial inclination.
- If you are angry, do something kind.
- If you are unmotivated, engage in an activity.
- If you are afraid, confidently move forward.
- If you are sad, smile at someone.
- If you have a powerful negative emotion, do the opposite of your initial inclination.
- Check the Facts - Ask yourself the following questions when you notice a strong emotional brewing.
- What event triggered my emotion?
- What interpretations or assumptions am I making about the event?
- Does the intensity of my emotion match the facts of the situation or just my assumptions?
- PLEASE - 5 Healthy Habits
- Treat Physical illness
- Eat healthy
- Avoid mood-altering drugs
- Sleep well
- Exercise
- Pay Attention to Positive Events - Positive but accurate self-talk.
- Positive self-talk is realistic, accurate, balanced, and useful.
- Choose an activity that is generally enjoyable and make a point to focus on the positives without getting hung up on the negative details.
- Try extending the positive outlook to more and more situations in life.
- Act Opposite
- 4 Skills:
- Interpersonal effectiveness: Ensure that your needs are met, develop meaningful relationships, and end toxic ones
- 3 categories of social skills:
- Objective effectiveness: Your ability to achieve objectives during social interactions. The acronym DEAR MAN offers specific steps to achieve your goals.
- Describe:
- Clearly and concisely describe the facts of the situation - No opinions or interpretations.
- Express:
- State your feelings clearly to let others know how a situation affects you. Don't expect others to read your mind.
- Try the phrase: I feel XX because XX
- Assert:
- Be direct. Say what you need clearly and concisely
- Reinforce:
- Explain why it would be helpful to agree to your request. Express thanks if they consider it.
- (Be) Mindful:
- Stay focused on the objective of the interaction and avoid being reactive or defensive. If necessary, calmly repeat your request.
- Appear confident:
- Use body language to project confidence even if you don't feel it.
- Negotiate:
- Know the limits of what you're willing to accept but be willing to compromise within them.
- Describe:
- Relationship effectiveness: Your ability to have pleasant interactions, build a relationship, or maintain a good relationship. The acronym GIVE teaches skills for nurturing strong relationships.
- (Be) Gentle:
- Always be kind and respectful. Don't attack, threaten, or express judgment during your interactions. People tend to respond better to gentleness than harshness.
- (Show) Interest:
- Listen to the other person without interrupting. Instead of mind-reading, ask follow-up questions. Make it your goal to understand the other person, even when you disagree.
- Validate:
- Outwardly acknowledge the other person's thoughts and feelings. You can do this with words or actions.
- (Use an) Easy manner:
- Laugh, smile, and be lighthearted. No one wants to be pushed around or bullied. Being relaxed and likable is more likely to help you achieve your goals.
- (Be) Gentle:
- Self-respect effectiveness: Your ability to stay true to your values during social interactions. The acronym FAST teaches skills for protecting your self-respect.
- (Be) Fair:
- Consider each person's perspective and be fair. Don't take advantage of others and say no if you believe others are taking advantage of you.
- (No) Apologies:
- Don't over-apologize. You never need to apologize for making a request or for disagreeing. Save apologies for when you've made a mistake.
- (Stick to your) Values:
- Develop an understanding of your values, the things that matter most to you and your morals. Know your red lines and be willing to stand for them.
- (Be) Truthful:
- Avoid dishonesty such as exaggeration, manipulation, and outright lying. There might be a time and place for white lies, but even these should be used carefully.
- (Be) Fair:
- Objective effectiveness: Your ability to achieve objectives during social interactions. The acronym DEAR MAN offers specific steps to achieve your goals.
- 3 categories of social skills:
Reference:
- AFP Jul 2025 Vol 112 No 1
- Therapy Worksheets, Tools, and Handouts | Therapist Aid
Depression
See also:
SIG: E(nergy) CAPS
- S - Sleep changes: increase during day or decreased sleep at night
- I - Interest (loss): of interest in activities that used to interest them
- G - Guilt (worthless): depressed elderly tend to devalue themselves
- E - Energy (lack): common presenting symptom (fatigue)
- C - Cognition/C oncentration: reduced cognition &/or difficulty concentrating
- A - Appetite (wt. loss); usually declined, occasionally increased
- P - Psychomotor: agitation (anxiety) or retardations (lethargic)
- S - Suicide/Homocidal Ideations
PHQ-9:
- Over the previous 2 weeks, how often have you been bothered by the following: (Not at all - 0, Several days - 1, More than half the days - 2, Nearly every day - 3)
- Little interest or pleasure in doing things
- Feeling down, depressed, or hopeless
- Trouble falling or staying asleep, or sleeping too much
- Feeling tired or having little energy
- Poor appetite or overeating
- Feeling bad about yourself - or that you are a failure or have let yourself or your family down
- Trouble concentrating on things, such as reading the newspaper or watching television
- Moving or speaking so slowly that other people may have noticed, or being so fidgety or restless that you have been moving around a lot more than usual
- Thoughts that you would be better off dead, or of hurting yourself in some way
- Add up all scores
| Total Score | Depression Severity |
|---|---|
| 1-4 | Minimal depression |
| 5-9 | Mild depression |
| 10-14 | Moderate depression |
| 15-19 | Moderately severe depression |
| 20-27 | Severe depression |
References:
- JFP Vol 66 No 4 Apr 2017
Anti-depression Pharmacotherapy
See also:
Choice of antidepressant:
- Women: Fair evidence that SSRI's work better (EBM B)
- Men: Fair evidence tricyclics work better (EBM B)
- Overweight/Obesity: Bupropion - not inferior and weight neutral
- For >65yo: First line SSRIs, SNRIs, mirtazapine, and bupropion
- SNRIs have higher rates of adverse events - duloxetine is associated with increased falls
SSRI Choices:
- Select sertraline or escitalopram as first line for those not previously treated when initiating therapy. They are more effective and better tolerated than other "new generation" antidepressants. (SOR A)
- Escitalopram, sertraline, and fluoxetine produce modest improvements (5-10%) without a significant increase is suicide related outcomes in adolescent patients with moderate severity depression. (SOR A)
- A national guideline recommends psychological therapy for adolescents with mild depression. Combined psychotherapy and fluoxetine for moderate or severe depression, with sertraline as second-line. (SOR A)
Common antidepressants:
Selective Serotonin Reuptake Inhibitors
- Medications:
- Citalopram 20-60mg
- Escitalopram 10-20mg
- Sertraline 50-200mg
- Fluoxetine 10-40mg
- Paroxetine 20-50mg
- Generally safe in pregnancy
- Good for comorbid anxiety
- Adverse effects:
- Decreased sexual libido
- Diarrhea, nausea, vomiting
- Emotional blunting
- Bruising (platelet function inhibition)
- Possible serotonin syndrome
Serotonin-Norepinephrine Reuptake Inhibitors
- Medications:
- Duloxetine 30-60mg
- Venlaflaxine 150-375mg
- Good for comorbid neuropathic pain
- Good for comorbid anxiety
- Adverse effects:
- Same as SSRI's
- May elevated BP
Tricyclic Antidepressants
- Medications:
- Amitriptyline 100-300mg
- Nortiptyline 40-200mg
- Imipramine 50-150mg
- Effective with chronic pain, diabetic neuropathy, migraines, fibromyalgia
- Adverse effects:
- Anticholinergic effects
- Sedation
- Constipation
- Urinary retention
- Orthostatic hypotension
- Risk of fatal arrhythmia in overdose
- Anticholinergic effects
Norepinephrine-Dopamine Reuptake Inhibitors
- Medications:
- Bupropion 200-400mg
- Good for ADHD symptoms
- Good for tobacco users
- No sexual adverse effects
- Weight neutral/losing
- Adverse effects:
- Headaches
- Insomnia
- Tremors
- Lowers seizure threshold
- Worsens anxiety
Noradrenergic and Specific Serotonergic Antidepressants
- Medications:
- Mirtazapine 15-30mg
- Good for insomnia and poor appetite
- No sexual adverse effects
- Adverse effects:
- Somnolence
- Weight gain
Augmentation / Combinations
- Augmentation of antidepressant offers little benefit
- In treatment-resistant depression:
- Consider CBT
- Do not prescribe lithium before a trial of aripiprazole
- In treatment-resistant depression:
- Use a combination of a presynaptic a2 autoreceptor antagonist (mirtazapine or trazodone) and SSRI/SNRI/or TCA for acute depression
- SOR A
- Systematic review with meta analysis
- SOR A
Notes:
- If the reason for stopping fluoxetine is QTc prolongation, then duloxetine or desvenlafaxine should be selected as the subsequent drug.
- In patients with other severe adverse drug reactions that require abrupt cessation of fluoxetine, a different SSRI or an SNRI should generally be selected since they can be initiated at therapeutic doses without titration. Conversely, bupropion is generally not appropriate for immediate switching, since it may not mitigate withdrawal symptoms.
- In most cases, if fluoxetine is discontinued abruptly due to a severe adverse drug reaction, the new antidepressant is initiated after 2 to 3 days, rather than the next day.
References:
- JFP Vol 58 No 7 Jul 2009
- JFP Vol 65 No 9 Sep 2016
- Lancet 2009;373:746-758
- AFP Vol 101 No 3 Feb 2020
- AFP Vol 102, No 11 Dec 2020
- UpToDate
Antidepressants Comparisons
| More Effective (ORs 1.19-1.96) | Less Effective (ORs 0.51-0.84) |
|---|---|
| agomelatine | fluoxetine |
| amitriptyline | fluvoxamine |
| escitalopram | reboxetine |
| mirtazapine | trazodone |
| paroxetine | |
| venlafaxine | |
| vortioxetine |
| More Acceptable (ORs 0.43-0.77) | Higher Dropout Rates (ORs 1.30-2.32) |
|---|---|
| agomelatine | amitriptyline |
| citalopram | clomipramine |
| escitalopram | duloxetine |
| fluoxetine | fluvoxamine |
| sertraline | reboxetine |
| vortioxetine | trazodone |
| venlafaxine |
See also:
Reasons to avoid different medications
- Bupropion ER
- Creatinine clearance or non-normalized eGFR <15 mL/min or receiving hemodialysis or peritoneal dialysis
- Child-Pugh class C cirrhosis
- Anorexia nervosa or bulimia
- Seizure disorder or condition predisposing to seizures (eg, brain tumor)
- Use of a monoamine oxidase inhibitor (MAOI) currently or in the past 2 weeks
- Planned withdrawal of an antiseizure medication, barbiturate, benzodiazepine, or alcohol (or at risk for abrupt withdrawal of these drugs)
- Planned use of linezolid
- Citalopram
- Prolonged QTc or risk factors for prolonged QTc, specifically bradycardia, decompensated heart failure, recent myocardial infarction, uncorrected hypokalemia, or hypomagnesemia, or use of other drugs that prolong the QTc
- Receiving hemodialysis or peritoneal dialysis
- Use of a MAOI currently or in the past 2 weeks
- Planned use of linezolid
- Sexual dysfunction
- Desvenlafaxine
- Use of a MAOI currently or in the past 2 weeks
- Planned use of linezolid
- Duloxetine
- Creatinine clearance or non-normalized eGFR <30 mL/min
- Hepatic impairment
- Poorly controlled narrow-angle glaucoma
- Use of a MAOI currently or in the past 2 weeks
- Planned use of linezolid
- Escitalopram
- Prolonged QTc or risk factors for prolonged QTc, specifically bradycardia, decompensated heart failure, recent myocardial infarction, uncorrected hypokalemia, or hypomagnesemia, or use of other drugs that prolong the QTc
- Receiving hemodialysis or peritoneal dialysis
- Use of a MAOI currently or in the past 2 weeks
- Planned use of linezolid
- Sexual dysfunction
- Fluoxetine
- Use of a MAOI currently or in the past 2 weeks, or use of thioridazine
- Planned use of linezolid
- Sexual dysfunction
- Levomilnacipran
- Angle-closure glaucoma
- Bladder outlet obstruction
- End-stage kidney disease
- Hypertension
- Tachyarrhythmia
- Planned use of linezolid
- Use of a MAOI currently or in the past 2 weeks
- Milnacipran
- Alcohol use disorder
- Angle-closure glaucoma
- Cirrhosis
- Creatinine clearance or non-normalized eGFR <15 mL/min
- Receiving hemodialysis or peritoneal dialysis
- Planned use of linezolid
- Use of a MAOI currently or in the past 2 weeks
- Mirtazapine
- Planned use of linezolid
- Use of a MAOI currently or in the past 2 weeks
- Paroxetine
- Age >65 years (due to anticholinergic effects)
- History of adherence difficulties (discontinuation symptoms may be severe)
- Planned used of linezolid
- Pregnancy
- Sexual dysfunction
- Use of a MAOI currently or in the past 2 weeks
- Sertraline
- Moderate to severe hepatic impairment
- Use of a MAOI currently or in the past 2 weeks
- Sexual dysfunction
- Venlafaxine ER
- Planned use of linezolid
- Use of a MAOI currently or in the past 2 weeks
- Sexual dysfunction
- Vilazodone
- Planned use of linezolid
- Use of a MAOI currently or in the past 2 weeks
- Vortioxetine
- Planned use of linezolid
- Use of a MAOI currently or in the past 2 weeks
References:
- Study: Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis
Notes:
- The most effective antidepressant, Amitriptyline, had an "Odds Ratio" of 2.13, which converts to an effect size of 0.417, which is "small-medium" according to Cohen's recommendations.
Background
- Major depressive disorder is one of the most common, burdensome, and costly psychiatric disorders worldwide in adults. Pharmacological and non-pharmacological treatments are available; however, because of inadequate resources, antidepressants are used more frequently than psychological interventions. Prescription of these agents should be informed by the best available evidence. Therefore, we aimed to update and expand our previous work to compare and rank antidepressants for the acute treatment of adults with unipolar major depressive disorder.
Methods
- We did a systematic review and network meta-analysis. We searched Cochrane Central Register of Controlled Trials, CINAHL, Embase, LILACS database, MEDLINE, MEDLINE In-Process, PsycINFO, the websites of regulatory agencies, and international registers for published and unpublished, double-blind, randomised controlled trials from their inception to Jan 8, 2016. We included placebo-controlled and head-to-head trials of 21 antidepressants used for the acute treatment of adults (≥18 years old and of both sexes) with major depressive disorder diagnosed according to standard operationalised criteria. We excluded quasi-randomised trials and trials that were incomplete or included 20% or more of participants with bipolar disorder, psychotic depression, or treatment-resistant depression; or patients with a serious concomitant medical illness. We extracted data following a predefined hierarchy. In network meta-analysis, we used group-level data. We assessed the studies' risk of bias in accordance to the Cochrane Handbook for Systematic Reviews of Interventions, and certainty of evidence using the Grading of Recommendations Assessment, Development and Evaluation framework. Primary outcomes were efficacy (response rate) and acceptability (treatment discontinuations due to any cause). We estimated summary odds ratios (ORs) using pairwise and network meta-analysis with random effects. This study is registered with PROSPERO, number CRD42012002291.
Findings
- We identified 28,552 citations and of these included 522 trials comprising 116,477 participants.
- In terms of efficacy, all antidepressants were more effective than placebo, with ORs ranging between 2.13 (95% credible interval [CrI] 1.89–2.41) for amitriptyline and 1.37 (1.16–1.63) for reboxetine.
- For acceptability, only agomelatine (OR 0.84, 95% CrI 0.72–0.97) and fluoxetine (0.88, 0.80–0.96) were associated with fewer dropouts than placebo, whereas clomipramine was worse than placebo (1.30, 1.01–1.68).
- When all trials were considered, differences in ORs between antidepressants ranged from 1.15 to 1.55 for efficacy and from 0.64 to 0.83 for acceptability, with wide CrIs on most of the comparative analyses.
- In head-to-head studies, agomelatine, amitriptyline, escitalopram, mirtazapine, paroxetine, venlafaxine, and vortioxetine were more effective than other antidepressants (range of ORs 1.19–1.96), whereas fluoxetine, fluvoxamine, reboxetine, and trazodone were the least efficacious drugs (0.51–0.84).
- For acceptability, agomelatine, citalopram, escitalopram, fluoxetine, sertraline, and vortioxetine were more tolerable than other antidepressants (range of ORs 0.43–0.77), whereas amitriptyline, clomipramine, duloxetine, fluvoxamine, reboxetine, trazodone, and venlafaxine had the highest dropout rates (1.30–2.32). 46 (9%) of 522 trials were rated as high risk of bias, 380 (73%) trials as moderate, and 96 (18%) as low; and the certainty of evidence was moderate to very low.
Interpretation
- All antidepressants were more efficacious than placebo in adults with major depressive disorder. Smaller differences between active drugs were found when placebo-controlled trials were included in the analysis, whereas there was more variability in efficacy and acceptability in head-to-head trials. These results should serve evidence-based practice and inform patients, physicians, guideline developers, and policy makers on the relative merits of the different antidepressants.
Reference:
- Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, Leucht S, Ruhe HG, Turner EH, Higgins JPT, Egger M, Takeshima N, Hayasaka Y, Imai H, Shinohara K, Tajika A, Ioannidis JPA, Geddes JR. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018 Apr 7;391(10128):1357-1366. doi: 10.1016/S0140-6736(17)32802-7. Epub 2018 Feb 21. PMID: 29477251; PMCID: PMC5889788.
- Antidepressants and health-related quality of life (HRQoL) for patients with depression: Analysis of the medical expenditure panel survey from the United States
Background
- Despite the empirical literature demonstrating the efficacy of antidepressant medications for treatment of depression disorder, these medications' effect on patients' overall well-being and health-related quality of life (HRQoL) remains controversial. This study investigates the effect of antidepressant medication use on patient-reported HRQoL for patients who have depression.
Methods
- A comparative cohort, secondary database analysis was conducted using data from the United States' Medical Expenditures Panel Survey for patients who had depression. HRQoL was measured using the SF-12 and reported as physical and mental component summaries (PCS and MCS). A cohort of patients that used antidepressant medications were compared to a cohort of patients that did not. Univariate and multivariate difference-in-differences (D-I-D) analyses were used to assess the significance of the mean difference of change on the PCS and MCS from baseline to follow-up.
Results
- On average, 17.5 million adults were diagnosed with depression disorder each year during the period 2005–2016. The majority were female (67.9%), a larger proportion of whom received antidepressant medications (60.5% vs. 51.5% of males).
- Although use of antidepressants was associated with some improvement on the MCS, D-I-D univariate analysis revealed no significant difference between the two cohorts in PCS (–0.35 vs. –0.34, p = 0.9595) or MCS (1.28 vs. 1.13, p = 0.6405). The multivariate D-I-D analyses ensured the robustness of these results.
Conclusion
- The real-world effect of using antidepressant medications does not continue to improve patients' HRQoL over time.
- Future studies should not only focus on the short-term effect of pharmacotherapy, it should rather investigate the long-term impact of pharmacological and non-pharmacological interventions on these patients' HRQoL.
Reference:
Complimentary and Alternative Medicine
See also:
Complimentary and Alternative Medicine
- Exercise
- Works for both unipolar depression and anxiety
- Meditation
- Clinically meaningful moderate reductions in anxiety
- Beneficial as adjunctive for depression
- St John's Wort (Hypericum perforatum
- Depression: Superior to placebo and similar rates of remission in mild-mod depression compared with SSRI/SNRI
- Anxiety: Not supported with evidence
- Methylfolate (version that crosses blood/brain barrier)
- MTHFR gene leads to lower folate
- L-methylfolate 15 mg/d
- Folate itself - RCTs do not support efficacy
- S-adenosyl methionine (SAMe)
- 800 mg bid in unipolar depression adjunct with SSRI
- Vit D
- Might improve anxiety and depression in those with low levels
- Music Therapy
- Effective with mod quality evidence in the first 3 months added to standard care
- SOR B
References:
- JFP Jun 2020 Vol 69, No 5
- AFP Mar 2020 Vol 101, No 5
Depression quotes, thoughts, and ideas edit
- Don't take advice from someone you wouldn't trade places with
- Imagine your day as quadrants - each is a new start
- If your morning is shot, you have 3 more chances to have a good day
Exercise as treatment for depression
- Exercise reduces symptoms of depression when used as monotherapy (SOR B)
- It is as effective as cognitive behavioral therapy (SOR B)
- Resistance and mixed exercise (resistance and aerobic) are better than aerobic alone (SOR B)
- High frequency exercise is better than low frequency (SOR B)
- Mindfulness exercise (Meditative like tai chi and yoga) reduce symptoms (SOR B)
References:
- JFP Vol 59 No 9 Sep 2010
Organic causes of depression
Organic causes of depression
- Anemia, leukocytosis
- CBC
- Metabolic/electrolyte abnormalities, poor renal function
- BMP
- Hormone abnormalities
- TSH, ACTH stimulation test, dexamethasone suppression test
- Substance use
- Urine drug screen, blood alcohol level
- Pregnancy
- Urine hCG
- Nutritional deficiencies
- Vit B12, Vit D
- Sleep apnea
- Polysomnogram
References:
- JFP Vol 66 No 4 Apr 2017
Pediatric Depression
Adolescents should be screened annually (LOE B)
Children and adolescents with moderate or severe depression or persistent mild depression should be treated with:
- Fluoxetine or escitalopram in conjunction with cognitive behavior therapy or other talk therapy
- LOE A
References:
- AFP Vol 100 No 10 Nov 2019
Treatment Resistant Depression
See also:
In patients with treatment-resistant depression, augmenting therapy with atypical antipsychotics can be effective.
- Adding quetiapine (Seroquel) to antidepressant therapy reduces symptoms below the remission threshold (number needed to treat [NNT] = 9), whereas the number of people who stop using the medicine (dropouts) increases only at the highest dosage.
- Augmentation with cariprazine (Vraylar) or ziprasidone (Geodon) improves the clinical response; however, the benefit is offset by increased dropouts. (Strength of Recommendation: C, based on disease-oriented outcomes.)
Second generation anti-psychotics (FDA Approved):
- Aripiprazole
- Typical dose: 10-20mg/d
- High dose: 20-40mg/d
- AE: Akathisia; EP
- Olanzapine
- Typical dose: 10-20mg/d
- High dose: 30-40mg/d
- AE: Weight gain, Sedation, EP
- Quetiapine XR
- Typical dose: 150-300mg/d
- High dose: 300-600mg/d
- AE: Sedation
- Olanzapine/Fluoxetine (Symbyax)
Monitor patients on second generation anti-psychotics:
- Baseline/Yearly:
- Personal/Family history
- BMI
- Waist circumference
- BP
- Fasting glucose/lipids
- 12wks:
- BMI
- BP
- Fasting glucose/lipids
References:
- Consultant Mar 2016
- Am Fam Physician. 2021 Jan 1;103(1):16-18.
Yoga - anxiety and depression
- Yoga can reduce symptoms of anxiety and depression (SOR B)
- Yoga typically improves overall symptom scores for anxiety and depression by about 40%, both by itself and as an adjunctive treatment.
- It produces no reported harmful side effects.
- Yoga produced overall reductions of symptoms between 12% and 76%, with an average of 39% net reduction in symptom scores across measures in depression, anxiety, and stress.
References:
- J Fam Pract. 2014 July;63(7):398-399,407.
Drugs that can cause psychosis
- Adrenergics
- Alcohol, benzos, barbs
- Antiarrhythmics
- Anticholinergics
- Antihistamines
- Antimalarials
- Antihistamines
- Antituberculars
- Cannabis, ketamine, bath salts
- Cocaine, meth, 3,4-methylenedioxymethamphetamine
- Corticosteroids
- Dextromethorphan
- Dopamine agonists
- HEavy metals
- Organophosphates
- St John's Wort
- Thyroid hormones
AFP Vol 91, No 12 Jun 2015
Eating Disorders
Binge Eating Disorder (BED)
- Most common eating disorder
- Often obese
Criteria:
- Recurrent episodes of binge eating marked by:
- Eating large amount of food in a discreet period of time
- A sense of lack of control with eating during the episode
- Associated with 3+ of the following:
- Eating more rapidly than normal
- Eating until uncomfortably full
- Eating large amounts of food when not physically hungry
- Hiding eating behavior because embarrassed by behavior (indicates worse pathology)
- Feeling disgusted, depressed, guilty after episode
- Occurs, on average, at least 1x/wk for 3 months
- Not associated with compensatory purging behaviors
Treatment:
- Treat BED before obesity
- CBT is first line
- Medicines can be used first line if patient's preference:
- Topiramate, zonisamide, bupropion
- lisdexamfetamine (Vyvanse)
- CBT plus topiramate may work best
Reference:
- OMA Review Course 2016
- Binge Eating Disorder Screening
VA Binge Eating Screener:
- On average, how often have you eaten extremely large amounts of food at one time and felt that your eating was out of control at that time?
- Never
- <1 time/wk
- 1 time/wk
- 2-4 times/wk
- 5+ times/wk
If 2+ times/wk:
- Sensitivity: 88.9%
- Specificity: 83.2%
Reference:
- JFP Vol 70 No 3 Apr 2021
- On average, how often have you eaten extremely large amounts of food at one time and felt that your eating was out of control at that time?
Night Eating Syndrome (NES)
- Second most common eating disorder
- Usually high intake of carbs (7:1 CHO:ptn)
- Up to 40% of NES engage in binge eating
Management
- Highly responsive to sertraline
- Selective serotonin reuptake inhibitors (SSRIs), particularly sertraline, have the strongest evidence for efficacy in treating night eating syndrome (NES)
- Randomized controlled trials demonstrate that sertraline (flexible dosing, 50–200 mg/day) significantly reduces NES symptoms, nocturnal ingestions, and associated weight, with response rates up to 71% compared to 18% for placebo.
- Open-label data also support the use of escitalopram, which has shown significant reductions in night eating symptoms, nocturnal ingestions, and weight over 12 weeks
- Encourage regular meal consumption earlier in daytime; increase protein
Defined:
- Morning anorexia
- Evening hyperphagia
- Insomnia
Other notes:
- Nocturnal awakenings to eat are common.
- Often with evening tension, stress
- Consume 25-50% daily calories after evening meal
Reference:
- OMA Review Course 2016
- O'Reardon JP, Allison KC, Martino NS, et al. A Randomized, Placebo-Controlled Trial of Sertraline in the Treatment of Night Eating Syndrome. The American Journal of Psychiatry. 2006;163(5):893-8. https://doi.org/10.1176/ajp.2006.163.5.893.
- Allison KC, Studt SK, Berkowitz RI, et al. An Open-Label Efficacy Trial of Escitalopram for Night Eating Syndrome. Eating Behaviors. 2013;14(2):199-203. https://doi.org/10.1016/j.eatbeh.2013.02.001.
Bulemia Nervosea (BN)
- Recurrent episodes of binge eating
- Recurrent inappropriate compensatory behavior to prevent weight gain
- At least 1x/wk for 3 months
- History of sexual abuse 25%
- 80% are normal weight
Treatment:
- CBT most effective psychological treatment
- SSRIs effective (fluoxetine)
- Combination CBT and SSRI superior
- NOT bupripion as may cause seizures
Reference:
- OMA Review Course 2016
Anorexia Nervosa (AN)
- 90% Females ages 15-19yo
- 35-85% recovery rate
- Usually higher socio-economic status
- Dysfunctional family common
Criteria:
- Restriction of energy intake leading to low weight
- Defined as BMI <18.5
- Intense fear of gaining weight
- Or persistent behavior preventing weight gain despite being underweight
- Distorted body image
- Typically focused on shape and weight
- Denial of the medical seriousness of their low weight
Specifiers:
- Restricting type
- Binge eating/purging
Severity:
- Mild - BMI > 17
- Moderate - BMI 16-16.99
- Severe - BMI 15-15.99
- Extreme - BMI <15
Reference:
- OMA Review Course 2016
SCOFF Questionnaire - Screening in Adults
- Do you make yourself sick because you feel uncomfortably full?
- Do you worry you have lost control over how much you eat?
- Have you recently lost more than one stone (14lbs) in a 3mo period?
- Do you believe yourself to be fat when others say you are too thin?
- Would you say that food dominates yourlife?
- 1 point for every yes. Score 2 or more indicates patient likely has anorexia or bulemia nervosa.
Reference:
- AFP Vol 91 No 1 Jan 2015
Eating Disorders edit
- In patients with eating disorders, early intervention and symptom improvement decrease the risk of a protracted course with long-term pathology. LOE C
- Most patients with eating disorders receive optimal care in an outpatient setting. The outpatient care team should include an experienced therapist, a dietitian, and a clinician knowledgeable about eating disorder–specific medical evaluations. LOE C
- Family-based therapy should be a first-line treatment for youths with anorexia nervosa and bulimia nervosa. LOE A
- Medications should not be used as monotherapy in the treatment of anorexia nervosa or bulimia nervosa. LOE B
- Lisdexamfetamine (Vyvanse) can be effective in reducing binge-eating behaviors. LOE B
- Contraceptives should be offered to patients with disordered eating who want to prevent pregnancy, but they have not been associated with improved bone mineral density and may mask resumption of menses. LOE C
- Caregivers and clinicians should focus on positive body image instead of weight or dieting to prevent disordered eating. LOE C
Characteristics of Eating and Feeding Disorders
Anorexia nervosa
- Restriction of food eaten, leading to significantly low body weight
- Intense fear of gaining weight or being "fat"
- Body image distortion
- Types: restrictive or binge eating/purging
- Alternative diagnosis: atypical anorexia nervosa (i.e., weight is not significantly low)*
Bulimia nervosa
- Binge eating (i.e., eating more food than peers [e.g., over a two-hour period] accompanied by a perceived loss of control)
- Repeated use of unhealthy behaviors to prevent weight gain, such as vomiting, misuse of laxatives or diuretics, food restriction, or excessive exercise
- Self-worth is overly based on body shape and weight
- Behaviors occur at least weekly for at least three months and are distinctly separate from anorexia nervosa
- Alternative diagnoses: bulimia nervosa of low frequency and/or limited duration*; purging disorder (i.e., recurrent purging to lose weight without binge eating)*
Binge-eating disorder
- Recurrent episodes of binge eating (i.e., eating more food than peers [e.g., over a two-hour period] accompanied by a perceived loss of control)
- Associated with three of the following: eating faster than normal, eating until feeling uncomfortable, eating large quantities of food when not hungry, feeling bad because of embarrassment about eating behaviors, or eating followed by negative emotions
- No behaviors to prevent weight gain
- Behaviors occur at least weekly for at least three months and are distinctly separate from anorexia nervosa or bulimia nervosa
- Alternative diagnosis: binge-eating disorder of low frequency and/or limited duration*
Avoidant/restrictive food intake disorder
- Avoidance of food intake because of one of the following: lack of interest, sensory characteristics of food, concern about consequences of eating that lead to unmet nutritional or energy needs
- Associated with significant weight loss, inadequate weight gain during growth, nutritional deficiency, interference with psychosocial functioning, or dependence on supplemental feeding
- Not explained by food availability, culturally sanctioned practice, or other medical or mental health condition
- No disturbance in how body weight or shape is experienced by the person
Rumination disorder
- Repeated regurgitation of food for at least one month
- Not attributable to a gastrointestinal or other medical condition
- Does not occur exclusively with another eating disorder
Pica
- Eating nonnutritive, nonfood substances for at least one month
- Eating behavior is developmentally inappropriate
- Not part of a culturally supported or socially normative practice
SCOFF Questionnaire: Screening for Eating Disorders
- Do you make yourself Sick because you feel uncomfortably full?
- Do you worry you have lost Control over how much you eat?
- Have you recently lost more than One stone (14 lb [6 kg]) in a three-month period?
- Do you believe yourself to be Fat when others say you are too thin?
- Would you say that Food dominates your life?
One point is given for every "yes" answer; a score of 2 or more indicates the patient likely has anorexia nervosa or bulimia nervosa.
Online resources are available for family members (https://www.feast-ed.org), clinicians (https://www.aedweb.org), and patients with disordered eating (https://www.nationaleatingdisorders.org).
Recommended Studies in Persons with Suspected or Diagnosed Eating Disorders
| Laboratory testing* | Findings of concern and associations |
|---|---|
| Amylase | Increased (may suggest purging) |
| Basic metabolic panel | Decreased sodium (water-loading), potassium, chloride, glucose; indications of metabolic acidosis (laxatives) or alkalosis (vomiting); acute renal injury |
| Calcium | Decreased |
| Cholesterol | Increased |
| Complete blood count | Bone marrow hypoplasia (thrombocytopenia, anemia, leukopenia) |
| Magnesium | Decreased |
| Phosphorus | Decreased |
Principles of Major Psychotherapy Modalities for Patients with Eating Disorders
| Psychotherapy modality | General treatment principles | Typical treatment timelines |
|---|---|---|
| Cognitive behavior therapy | Individual-focused therapy that targets the patient's distorted cognitions and associated problematic eating behaviors Identify psychological issues and determine how dietary/emotional factors affect behaviors May involve meal planning, challenging dysfunctional automatic thoughts (e.g., all-or-nothing thinking), behavior experiments, exposure to feared foods, and relapse prevention Completion of food records may be helpful in binge-eating disorder Recommended for use in patients with bulimia nervosa, anorexia nervosa, and binge-eating disorder | Weekly sessions over four to 12 months depending on condition Early stages may include sessions two times per week Can be completed in individual or group environments |
| Family-based therapy | Treatment plan focused on behaviors and education within a family unit. Family members are not to blame, should conceptualize and frame the eating disorder as separate from the person, and are vital to therapeutic success by "uniting" against the disorder. Phase 1: empowers parents in promoting healthy eating behaviors and to restore patient's weight Phase 2: autonomy in feeding is gradually shifted back to patient Phase 3: facilitates improved family communication and independence Recommended for use in adolescents and young adults with anorexia nervosa and bulimia nervosa | Occurs over six to 12 months, consisting of 18 to 20 sessions |
| Self-guided treatment | Utilizes cognitive behavior therapy principles in self-driven format Self-monitoring of eating behaviors and inward reflection of their underlying causes Components of treatment include nutrition education about healthy eating and development of coping strategies to triggering situations and to decrease the risk of relapse Treatment can be delivered via internet, mobile application, or written material Recommended for use in bulimia nervosa and binge-eating disorder | Typical timeline: self-paced course, between four and 12 months Consider supplementing self-help programming with brief, in-person sessions Progress to alternative therapy if ineffective after four weeks |
| Specialist supportive clinical management | Psychoeducation model based on "gentle coaching" Patient-driven therapy founded on therapeutic relationship Education provided on mutually agreed-upon symptom targets Goal-directed therapy to decrease these symptoms Aims to link symptoms and abnormal eating behaviors Recommended for use in adults with anorexia nervosa; low-quality studies suggest benefit in bulimia nervosa | Typically consists of 20 or more weekly sessions spread out over one year |
References:
- AFP Jan 2021 Vol 103 No 1
Emotional Support Animals in Florida
See also: Service Animals
A wide range of health care practitioners are permitted to provide ESA letters in Florida, including:
- Psychologists
- Doctors
- Mental health counselors
- Marriage and family therapists
- Social workers
- Psychiatrists
- Registered nurses
These are the basic Florida emotional support animal letter requirements for ESA owners:
- A licensed mental health professional needs to determine that you have an emotional disability
- Your mental disability is in the Diagnostic and Statistical Manual of Mental Disorders
- The identified condition substantially limits your ability to participate in at least one major life activity
- The professional has to determine that an emotional support animal would help treat the condition or ease your symptoms
- You need to get an emotional support animal letter which can be thought of as a prescription for an ESA
- The letter must come from a licensed mental health professional
- Your letter must be on your therapist's official letterhead
- The letter must include your therapist's license details, issue date, and state
You might qualify for an ESA in Florida if you have one or more issues listed below:
- Depression
- Anxiety
- PTSD
- Sleep issues
- Learning difficulties
- Phobias
- Panic disorders
- Personality disorders
Landlords are not permitted:
- To request information that details the diagnosis or severity of the tenant's disability
- They cannot request any medical records relating to the tenant's disability
Sample letters:
Airline
[Date] To Whom It May Concern: [Full Name of Tenant] is my patient, and has been under my care since [date]. I am intimately familiar with his/her history and with the functional limitations imposed by his/her emotional/mental related illness. Due to this emotional/mental disability, [first name] has certain limitations related to [social interaction/coping with stress/anxiety, etc.]. In order to help alleviate these difficulties, and to enhance his/her ability to function independently, I have prescribed [first name] to obtain a pet or emotional support animal. The presence of this animal is necessary for the emotional/mental health of [patient name] because its presence will mitigate the symptoms he/she is currently experiencing. Please allow (patient's full name) to be accompanied by his/her emotional support animal in the cabin of the aircraft, in accordance with the Air Carrier Access Act (49 U.S.C. 41705 and 14 C.F.R. 382). I am licensed by the state of (state) to practice (medicine/psychiatry/therapy–choose applicable). My license number is (license number). Sincerely, (Physician's name and title)
General
[Date] To Whom It May Concern: [Full Name of Patient] is my patient and has been under my care since [date]. I am intimately familiar with his/her history and with the functional limitations imposed by his/her emotional/mental health-related issue. Due to this emotional disability, [patient first name] has certain limitations coping with what would otherwise be considered normal, but significant day to day situations. To help alleviate these challenges and to enhance his/her day to day functionality, I have prescribed [patient first name] to obtain an emotional support animal. The presence of this animal is necessary for the emotional/mental health of [patient name] because its presence will mitigate the symptoms he/she is currently experiencing. Sincerely, (Physician's name and title)
Housing:
[Date] Dear [Name of Housing Authority/Landlord]: [Full Name of Tenant] is my patient, and has been under my care since [date]. I am intimately familiar with his/her history and with the functional limitations imposed by his/her emotional/mental related illness. He/She meets the definition of disability under the Americans with Disabilities Act, the Fair Housing Act, and the Rehabilitation Act of 1973. Due to this emotional/mental disability, [first name] has certain limitations related to [social interaction/coping with stress/anxiety, etc.]. In order to help alleviate these difficulties, and to enhance his/her ability to live independently and to fully use and enjoy the dwelling unit you own and/or administer, I have prescribed [first name] to obtain a pet or emotional support animal. The presence of this animal is necessary for the emotional/mental health of [patient name] because its presence will mitigate the symptoms he/she is currently experiencing. Sincerely, (Physician's name and title)
For flights: Please allow (patient's full name) to be accompanied by his/her emotional support animal in the cabin of the aircraft, in accordance with the Air Carrier Access Act (49 U.S.C. 41705 and 14 C.F.R. 382).
For housing: He/She meets the definition of disability under the Americans with Disabilities Act, the Fair Housing Act, and the Rehabilitation Act of 1973.
Response to Requests:
This kind of thing has strict legal definitions here in Florida.
I need to know what specific medical condition you need the animal for to put in a letter.
It needs to meet one of the following definitions: disability under the Americans with Disabilities Act, the Fair Housing Act, and the Rehabilitation Act of 1973.
It also helps to have a good description of the specific animal: type, breed, color, approx age, etc
Generic ADHD Stimulants edit
- Adderall XR
- Dexedrine spansules
- Focalin XR
- Ritalin LA
- Vyvanse
Illness Anxiety Disorder (Hypochondriasis)
Most of the patients with IAD belong to one of the two types:
- A care-seeking type. These patients frequently utilize the health care system and keep changing their doctors. They may ask for multiple investigations and treatments.[1]
- A care-avoidant type. These patients avoid medical care. They have severe anxiety with the belief that the primary doctor or laboratory testing will reveal a life-threatening illness (e.g., cancer).[1]
Management
- Primary care providers should aim to establish a rapport and therapeutic alliance with their patients so that patients feel comfortable in discussing their health concerns
- atients should be scheduled for regular follow-ups with their primary care physician along with the psychiatrist. Frequent follow-ups will reduce visits to the emergency department or other physicians. It will also allow the physician to assess new complaints and associated triggers and stresses critically
- Psychotherapy is the first-line treatment for IAD.[1] Cognitive-behavioral therapy (CBT) is a type of psychotherapy that focuses on treating the patient's dysfunctional maladaptive cognitive beliefs by behavioral modification strategies. I
- Pharmacological drugs are the second-line treatment for IAD. Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are proven to be effective in this condition.[2] Patients who respond to antidepressant therapy are recommended to receive maintenance treatment for at least 6 to 12 months. Most patients require a combination of psychotherapy and pharmacological agents.
DDx:
- Anxiety disorders
- Body dysmorphic disorder
- Conversion disorders
- Delusional disorder
- Depression
- Generalized anxiety disorder
- Obsessive-compulsive disorder
- Personality disorders
- Schizophrenia
- Somatic symptom disorder
Reference:
- French JH, Hameed S. Illness Anxiety Disorder. [Updated 2023 Jul 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554399/
- https://www.ncbi.nlm.nih.gov/books/NBK554399/
All-Cause and Cause-Specific Mortality Among Individuals With Hypochondriasis
Importance
- Hypochondriasis, also known as health anxiety disorder, is a prevalent, yet underdiagnosed psychiatric disorder characterized by persistent preoccupation about having serious and progressive physical disorders. The risk of mortality among individuals with hypochondriasis is unknown.
Objective
- To investigate all-cause and cause-specific mortality among a large cohort of individuals with hypochondriasis.
Design, Setting, and Participants
- This Swedish nationwide matched-cohort study included 4129 individuals with a validated International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) diagnosis of hypochondriasis assigned between January 1, 1997, and December 31, 2020, and 41,290 demographically matched individuals without hypochondriasis. Individuals with diagnoses of dysmorphophobia (body dysmorphic disorder) assigned during the same period were excluded from the cohort. Statistical analyses were conducted between May 5 and September 27, 2023.
Exposure
- Validated ICD-10 diagnoses of hypochondriasis in the National Patient Register.
Main Outcome and Measures
- All-cause and cause-specific mortality in the Cause of Death Register. Covariates included birth year, sex, county of residence, country of birth (Sweden vs abroad), latest recorded education, civil status, family income, and lifetime psychiatric comorbidities. Stratified Cox proportional hazards regression models were used to estimate the hazard ratios (HRs) and 95% CIs of all-cause and cause-specific mortality.
Results
- Of the 4129 individuals with hypochondriasis (2342 women [56.7%]; median age at first diagnosis, 34.5 years [IQR, 26.3-46.1 years]) and 41,290 demographically matched individuals without hypochondriasis (23,420 women [56.7%]; median age at matching, 34.5 years [IQR, 26.4-46.2 years]) in the study, 268 individuals with hypochondriasis and 1761 individuals without hypochondriasis died during the study period, corresponding to crude mortality rates of 8.5 and 5.5 per 1000 person-years, respectively.
- In models adjusted for sociodemographic variables, an increased rate of all-cause mortality was observed among individuals with hypochondriasis compared with individuals without hypochondriasis (HR, 1.69; 95% CI, 1.47-1.93).
- An increased rate was observed for both natural (HR, 1.60; 95% CI, 1.38-1.85) and unnatural (HR, 2.43; 95% CI, 1.61-3.68) causes of death.
- Most deaths from unnatural causes were attributed to suicide (HR, 4.14; 95% CI, 2.44-7.03).
- The results were generally robust to additional adjustment for lifetime psychiatric disorders.
Conclusions and Relevance
- This cohort study suggests that individuals with hypochondriasis have an increased risk of death from both natural and unnatural causes, particularly suicide, compared with individuals from the general population without hypochondriasis.
- Improved detection and access to evidence-based care should be prioritized.
Reference:
- Mataix-Cols D, Isomura K, Sidorchuk A, Rautio D, Ivanov VZ, Rück C, Österman S, Lichtenstein P, Larsson H, Kuja-Halkola R, Chang Z, Brickell I, Hedman-Lagerlöf E, Fernández de la Cruz L. All-Cause and Cause-Specific Mortality Among Individuals With Hypochondriasis. JAMA Psychiatry. 2023 Dec 13:e234744. doi: 10.1001/jamapsychiatry.2023.4744. Epub ahead of print. PMID: 38091000; PMCID: PMC10719832.
- https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2812786
Obsessive Compulsive Disorder (OCD)
Screening questions:
- Do you wash or clan a lot?
- Do you check things a lot?
- Is there any thought that keeps bothering you that you would like to get rid of but cannot?
- Do your daily activities take a long time to finish?
- Are you concerned about putting things in a special order or are you very upset by mess?
- Do these problems trouble you?
Commonly misdiagnosed as OCD:
- ADHD
- Anxiety
- Autism
- Depression
- Psychotic disorder
- Tourette syndrome
Pharmacology management (first line SSRI):
- fluoxetine
- Starting 20 mg
- Target dose: 40-80 mg
- paroxetine
- Starting 20 mg
- Target dose: 40-60 mg
- sertraline
- Starting 50 mg
- Target dose: 100-200 mg
Reference:
- AFP Oct 2024 Vol 110 No 4
Yale-Brown Obsessive Compulsive Scale (Y-BOCS)
- Description
- The Yale-Brown Obsessive Compulsive Scale (Y-BOCS) is a 10-item scale designed to measure the severity and type of symptoms in people with obsessive-compulsive disorder (OCD) over the past seven days. The symptoms assessed are obsessions and compulsions. This scale is useful in tracking OCD symptoms at intake and during/after treatment.
- Validity
- This scale was validated by Goodman et al. (1989b) who found that the Y-BOCS was significantly correlated with two independent measures of OCD. The same study also showed that the Y-BOCS is sensitive to changes in OCD symptoms. The Y-BOCS also has high internal consistency and high interrater reliability (Goodman et al., 1989a).
- Interpretation
- Total Y-BOCS scores range from 0 to 40, with higher scores indicating greater severity of OCD symptoms. Scores on the obsession and compulsion subscales range from 0 to 20, but only the total Y-BOCS score is interpreted. Total scores can be split into five categories, based on severity of symptoms. People who have a total Y-BOCS score:
- Under 7 are likely to be subclinical,
- 8-15 are likely to have a mild case of OCD,
- 16-23 are likely to have a moderate case of OCD,
- 24-31 are likely to have a severe case of OCD,
- 32-40 are likely to have an extreme case of OCD.
- Total Y-BOCS scores range from 0 to 40, with higher scores indicating greater severity of OCD symptoms. Scores on the obsession and compulsion subscales range from 0 to 20, but only the total Y-BOCS score is interpreted. Total scores can be split into five categories, based on severity of symptoms. People who have a total Y-BOCS score:
- Developer
- Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., Hill, C. L., … Charney, D. S. (1989a). The Yale-Brown Obsessive-Compulsive Scale. I. Development, Use, and Reliability. Archives of General Psychiatry, 46(11), 1006-1011.
Y-BOCS Test
- Score 0 to 4 points for each question.
- Total out of 40 points.
Answer each question based on the average occurrence of each item over the past week. The first 5 questions relate to obsessive thoughts, the last 5 questions relate to compulsive behaviors.
- How much of your time is occupied by obsessive thoughts?
- None
- Less than 1 hour per day
- 1-3 hours per day
- 3-8 hours per day
- More than 8 hours per day
- How much do your obsessive thoughts interfere with functioning in your social, work, or other roles?
- None
- Slight interference, but no impairment
- Definite interference, but managable
- Substantial intereference
- Extreme intereference, incapacitating
- How much distress do your obsessive thoughts cause you?
- None
- Mild, not too disturbing
- Moderate, disturbing, but still manageable
- Severe, very disturbing
- Extreme, near constant and disabling distress
- How much of an effort do you make to resist the obsessive thoughts?
- Always make an effort to resist, or don't even need to resist
- Try to resist most of the time
- Make some effort to resist
- Reluctantly yield to all obsessive thoughts
- Completely and willingly yield to all obsessions
- How much control do you have over your obsessive thoughts?
- Complete control
- Much control, usually able to stop or divert obsessions with some effort and concentration
- Moderate control, sometimes able to stop or divert obsessions
- Little control, rarely successful in stopping or dismissing obsessions
- No control, rarely able to even momentarily alter obsessive thinking
- How much time do you spend performing compulsive behaviors?
- None
- Less than 1 hour per day
- 1-3 hours per day
- 3-8 hours per day
- More than 8 hours per day
- How much do your compulsive behaviors interfere with functioning in your social, work, or other roles?
- None
- Slight interference, but no impairment
- Definite interference, but managable
- Substantial intereference
- Extreme intereference, incapacitating
- How anxious would you become if you were prevented from performing your compulsive behaviors?
- No anxiety
- Only slightly anxious
- Some anxiety, but managable
- Prominent and disturbing anxiety
- Extreme, incapacitating anxiety
- How much of an effort do you make to resist the compulsions?
- Always make an effort to resist, or don't even need to resist
- Try to resist most of the time
- Make some effort to resist
- Reluctantly yield to all complusions
- Completely and willingly yield to all complusions
- How much control do you have over the compulsions?
- Complete control
- Much control, usually able to stop or divert compulsive behavior with some effort and concentration
- Moderate control, sometimes able to stop or divert compulsive behavior
- Little control, rarely successful in stopping or dismissing compulsive behavior
- No control, rarely able to even momentarily alter compulsive behavior
Personality Disorders
| Disorder | Features |
|---|---|
| Paranoid | Distrus and suspicious - others are seen as malevolent |
| Schizoid | Detached from social relationships - restricted emotions |
| Schizotypal | Reduced capacity for interpersonal relationships - eccentric |
| Antisocial | Violates rights of others - impulsive - no remorse |
| Borderline | Unstable interpersonal relationships - unstable identity - impulsive |
| Histrionic | Excessive but superficial emotionality - seeks attention |
| Narcissistic | Grandiose fantasies - need for admiration |
| Avoidant | Social inhibition - fear or criticism or rejection |
| Dependent | Submissive and clingy - excessive need for advice and reassuranve |
| Obsessive-compulsive | Preoccupied with order, perfectionism, and control |
- Prevalence in community is 4.4%-14.8%
- Up to 24% of primary care patients potentially meet criteria.
Reference:
- JFP Vol 63, No 12 Dec 2014
Personality Disorders
A personality disorder is an enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual's culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is unchanging over time, and leads to distress or impairment in social or occupational functioning.
| Cluster A | Cluster B | Cluster C |
|---|---|---|
| Paranoid | Antisocial | Avoidant |
| Schizoid | Borderline | Dependent |
| Schizotypal | Histrionic | Obsessive-compulsive |
| Narcissistic |
Clues to cluster A disorders
- The patient has no peer relationships outside immediate family.
- The patient almost always chooses solitary activities for work and personal enjoyment.
Cluster B clues
- Hypersensitivity to treatment disagreements or cancelled appointments are common (and likely experienced as rejection).
- Mood changes occur very quickly, even during a single visit.
- There is a history of many failed relationships with providers and others.
- The patient will describe an individual as both "wonderful" and "terrible" (ie, splitting) and may do so during the course of one visit.
- The patient may also split groups (eg, medical staff ) by affective extremes (eg, adoration and hatred).
- The patient may hint at suicide or acts of self-harm.
Cluster C clues
- There is an excessive dependency on family, friends, or providers.
- Significant anxiety is experienced when the patient has to make an independent decision.
- There is a fear of relationship loss and resultant vulnerability to exploitation or abuse.
- Pervasive perfectionism makes treatment planning or course changes difficult.
- Anxiety and fear are unrelieved despite support and ample information.
Management Tips: Cluster A approaches
- Recommend treatment that respects the patient's need for relative isolation.
- Don't be personally offended by your patient's flat or disinterested affect or concrete thinking; don't let it diminish the emotional support you provide.
- Consult with a health psychologist (who has expertise in physical health conditions, brief treatments, and the medical system) to connect the patient with a long-term therapist. It is better to focus on fundamental changes, rather than employing brief behavioral techniques, for symptom relief. Patients with personality disorders tend to have better outcomes with long-term psychological care.
Cluster B approaches
- Set boundaries—eg, specific time limits for visits—and keep them.
- Schedule brief, more frequent, appointments to reduce perceived feelings of abandonment.
- Coordinate plans with the entire clinic team to avoid splitting and blaming.
- Avoid providing patients with personal information, as it may provide fodder for splitting behavior.
- Do not take things personally. Let patients "own" their own distress. These patients often take an emotional toll on the provider.
- Engage the help of a health psychologist to reduce burnout and for more long-term continuity of care. A health psychologist who specializes in dialectical behavioral therapy to work on emotion regulation, distress tolerance, and interpersonal effectiveness would be ideal.
Cluster C approaches
- Engage the help of family and other trusted individuals in supporting treatment plans
- Try to provide just 2 treatment choices to the patient and reinforce his or her responsibility to help make the decision collaboratively. This step is important since it is difficult to enhance autonomy in these patients.
- Engage the help of a cognitive behavioral therapist who can work on assertiveness and problem solving skills.
- Be empathetic with the patient and patiently build a trusting relationship, rather than "arguing" with the patient about each specific worry.
- Make only one change at a time. Give small assignments to the patient, such as monitoring symptoms or reading up on their condition. These can help the patient feel more in control.
- Present information in brief, clear terms. Avoid "grey areas" to reduce anxiety.
- Engage a behavioral health provider to reduce rigid expectations and ideally increase feelings of self- esteem; this has been shown to predict better treatment outcomes.
Reference:
- J Fam Pract. 2021 June;70(5):220-228 | 10.12788/jfp.0201
Phobias
Exposure Therapy
- Identify different methods of exposure to the fear-evoking stimulus
- (Example: height phobia)
- Climbing a step ladder
- Looking over a balcony
- Riding a glass elevator
- (Example: height phobia)
- Rank the methods from least to most fear evoking
- Have the patient engage in each method of exposure, starting with the least fearful method and moving to the next method only when the lesser method no longer produces a phobic response
- Have the patient continue regular in vivo exposure for maintenance of recovery
References:
- JFP Jan/Feb 2020 Vol 69, No 1
Psychological Examination
Elements of a psychological examination:
- General Appearance and Behavior (GAB)
General appearance should be assessed for unspoken clues to underlying conditions. For example, patients' appearance can help determine whether they
- Are unable to care for themselves (eg, they appear undernourished, disheveled, or dressed inappropriately for the weather or have significant body odor)
- Are unable or unwilling to comply with social norms (eg, they are garbed in socially inappropriate clothing)
- Have engaged in substance use or attempted self-harm (eg, they have an odor of alcohol, scars suggesting IV drug abuse or self-inflicted injury)
- Speech
Speech can be assessed by noting spontaneity, syntax, rate, and volume. A patient with depression may speak slowly and softly, whereas a patient with mania may speak rapidly and loudly. Abnormalities such as dysarthrias and aphasias may indicate a physical cause of mental status changes, such as head injury, stroke, brain tumor, or multiple sclerosis.
- The mechanics of talking
- What is the rate and volume?
- Is it monotone?
- What is the rhythm?
- Is there dysarthria?
- Is there an increase in latency (normal time to respond is 3-5 secs)?
- Is the amount of speech increased or decreased (e.g. mute, poverty of speech)?
- Is it spontaneous or does the patient only talk when a question is asked?
- Is the speech stilted?
- What is the level of the vocabulary?
- Are there neologisms, word approximations, phonemic or semantic paraphasias?
- The mechanics of talking
Flow of Thought" (FOT) Thinking and perception can be assessed by noticing not only what is communicated but also how it is communicated. Abnormal content may take the form of the following:
- Delusions (false, fixed beliefs)
- Ideas of reference (notions that everyday occurrences have special meaning or significance personally intended for or directed to the patient)
- Obsessions (recurrent, persistent, unwanted, and intrusive thoughts, urges, or images)
The physician can assess whether ideas seem to be linked and goal-directed and whether transitions from one thought to the next are logical. Psychotic or manic patients may have disorganized thoughts or an abrupt flight of ideas.
This section describes how thoughts are connected to each other. A general rule of thumb is that if you have to ask the patient to explain himself or if you find yourself saying, "I think he means this" then the patient probably has a thought disorder and is having difficulties in explaining himself. Patterns of thought flow:
- Circumstantial speech involves inclusion of too many trivial details. For the most part it is logical and sequential. Thus the connection between ideas is easily understood. In addition if the patient is given enough time he/she will also reach the goal (usually the answer to your question). Circumstantial speech is not necessarily pathological. It tends to be seen more commonly in the elderly (e.g. a patient starting back in 1914 and going through his/her whole life story to tell you why he/she looks both ways when crossing the street.)
- Tangential speech is used to refer to the situation in which a patient's response to specific questions is oblique or irrelevant. It should not be used to refer to abnormalities in spontaneous speech.
- Derailment (a.k.a. LOA) is used to describe spontaneous speech in which ideas slip off the track and onto another one that is obliquely related. Thus, it is comparable to tangential speech, but tangential is used to describe the phenomenon when it occurs as the immediate response to a question. Loosening of Associations is an older term for derailment, but is no longer recommended.
- Flight of Ideas describes derailment in which one idea is quickly followed by another (e.g. in the context of pressured speech). Use of this term, historically, is used to indicate the FOT in a manic and thus one should be careful in its use in non-manics, lest it be misinterpreted by others.
- Incoherence (a.k.a. word salad, jargon aphasia, schizophasia, paragrammatism) denotes a pattern of speech that is more severely affected than derailment. In contrast to derailment, where the slippage occurs between ideas or sentences, the slippage in incoherence occurs between words or phrases. At times it can be difficult to differentiate incoherence from Wernicke's aphasia.
- Clanging (choice of words based on their sounds), rhyming, puns may be present.
- Echolalia (repeating what is said by others in an echoing fashion).
- Perseveration (repeating the same word, phrase, or idea over and over again).
- Content of Thought (COT) or Thought Content (TC)
This section describes predominant ideas and thoughts that the patient is discussing or is occupied by. One should not simply record patient complaints (e.g. "I am seeing things" or "I want to kill myself"). Such statements are subjective and are symptoms and thus belong in the HPI. Instead when evaluating a patient's COT one should be probing and examining several aspects of a belief, for example, in order to offer evidence for or against it being a delusion. COT can be subdivided into 4 components. Each should be commented on.
- Suicidal and homicidal thoughts
- Thoughts associated with psychosis
- Non-psychotic thoughts
- Paucity/abundance of thoughts
Mood Emotional expression can be assessed by asking patients to describe their feelings. The patient's tone of voice, posture, hand gestures, and facial expressions are all considered. Mood (emotional state reported by the patient) and affect (patient's expression of emotional state as observed by the interviewer) should be assessed. Affect and its range (ie, full vs constricted) should be noted as well as the appropriateness of affect to thought content (eg, patient smiling while discussing a tragic event).
As defined by DSM-IV mood is "a pervasive and sustained emotion that colors the perception of the world." This is usually accomplished by asking the patient how he/she is (or has been) feeling, the goal being to have the patient "average" his/her mood over a certain amount of time.
- Affect
As defined by DSM-IV affect is "a pattern of observable behaviors that is the expression of a subjectively experienced feeling state (emotion)." Affect, thus, is a sign ("observable") and describes a person's emotional state at the time of the exam. There are four basic qualities that should be detailed about a person's affect.
- Type of affect
- Is it depressed, normal or elevated/euphoric/happy?
- What is its range?
- Can it be evoked with prompting (e.g. laughs after a joke)?
- An appropriate description of a patient suffering from depression might be: "Affect is depressed and restricted to the lower range though the patient will laugh to jokes."
- Other possible descriptors are anxious and irritable.
- Stability of affect
- Is the patient's affect labile?
- Does it remain stable, or does it change noticeably and quickly in response to small changes in the conversation?
- Appropriateness of affect Is the patient's affect appropriate to the conversation? Is it congruent to his stated mood? A patient's affect may be judged to be inappropriate for a number of reasons. Examples should be given.
- Amount of affect
- Blunted and flat affect is used to describe patients in whom the amount of affect is decreased (blunted) or non-existent (flat). This phenomenon is frequently seen in patients with schizophrenia. Usually patients with depression do have affect. It is just restricted to the negative emotions. In such instances a depressed patients should not be described as having a blunted or flat affect
- Type of affect
- Sensorium and Intellect
- Sensorium
- Orientation to person, place and time (day of month, month, year, day of week, season). If not oriented, give patient's answers and correct information.
- Recent and Remote Memory": - Retention and immediate recall - give three items and test in five minutes. If patient is unable to actively recall all three items at 5 minutes, provide hints. Recorded at 3/3 at 0 minutes and x/3 at 5 minutes without prompting and y/3 with prompting. - Recent memory - date of admission, brought to hospital by whom. - Remote memory - when and where born, date of marriage, names and ages of children.
- Attention Span and Concentration
- Serial Subtractions - subtract 7 from 100 and 7 from the answer and each succeeding answer (average adult has less than four errors and finishes within 60 seconds). If too difficult, use serial 3s starting at 20. Easiest is counting from 20 backwards to 1.
- Other - If the patient cannot do the mathematical tasks, try verbal ones. Saying the months of the year in reverse order is a reasonably difficult task that is sensitive to abnormalities in attention.
- Other possibilities are: spelling WORLD backwards, listing days of the week backwards, and citing strings of numbers forwards and backwards.
- Language
- Naming objects, ability to repeat phrases and overall vocabulary are examples of language function.
- Reading the paper or other material intended for the general public is another way to evaluate language.
- NOTE: Assessment of "Language" is NOT the same as assessment of "Speech" and must be listed separately in the Mental Status Exam.
- Computation
- Simple mathematical skills: multiply 7 x 8, divide 75 by 3. If too easy, try more difficult skills like square and square roots. If too difficult, test subtraction and addition skills.
- Fundamentals of Knowledge
- Is patient aware of current events, past history and vocabulary? Can he/she name five large cities and the last five presidents?
- Abstract Reasoning
- Ask the patient to describe the meaning of proverbs
- "Don't cry over spilled milk";
- "All that glitters is not gold";
- "A bird in the hand is worth two in the bush";
- "A rolling stone gathers no moss".
- Is the patient able to identify the abstractions involved in the proverbs?
- Contrasts and comparisons like,
- How are an apple and an orange alike?
- What is the difference between a cow and a pig?
- Ask the patient to describe the meaning of proverbs
- Constructional Ability
- Ask the patient to draw a clock face or to copy intersecting pentagons. This can detect constructional apraxia, hemineglect and perseveration.
- Sensorium
Insight and Judgment Cognitive functions include the patient's
- Level of alertness
- Attentiveness or concentration
- Orientation to person, place, and time
- Immediate, short-term, and long-term memory
- Abstract reasoning
- Insight
- Judgment
Insight and judgment are important components to determine not only in patients with psychiatric disorders but also in patients with "medical" illnesses. Studies have shown that good insight and judgment correlates with improved long-term outcome.
- Insight signifies that the patient realizes that he/she is ill and understands something of the nature of his/her illness.
- Judgment may be assessed by evaluating the patient's ability to understand social context.
Abnormalities of cognition most often occur with delirium or dementia or with substance intoxication or withdrawal but can also occur with depression.
- Level of alertness
Definitions:
- Defects in the Amount of Speech
- Poverty of Speech – restriction in the amount of spontaneous speech
- Poverty of Content of Speech – speech that conveys little information even though amount is adequate. Often uses language that is overabstract, overconcrete, vague, repetitive and stereotyped
- Pressure of Speech – increase in the amount of spontaneous speech compared to what is considered ordinary or socially customary. In addition to an increase in the amount of speech, the patient talks rapidly and is difficult to interrupt.
- Defects in Achieving the Goal of Speech (Flow of Thought)
- Distractible Speech – repeatedly stops talking in mid-sentence or idea and changes the subject in response to a nearby stimulus
- Tangentiality – replies to a question in an oblique or even irrelevant manner
- Derailment (Loose Associations) – pattern of spontaneous speech in which ideas slip off track onto one another; defect occurs between clauses and sentences
- Flight of Ideas – a nearly continuous flow of accelerated speech with abrupt changes from topic to topic that are usually based on understandable associations, distracting stimuli or plays on words
- Incoherence (Word Salad, Jargon Aphasia, Schizophasia) – pattern of speech that is incomprehensible at times in which rules of syntax and grammar are ignored; defect occurs at level of the clause or word.
- Illogicality – pattern of speech in which conclusions are reached that do not follow logically; non-sequitors; faulty inductive inferences
- Circumstantiality – pattern of speech that is very indirect and delayed in reaching its goal; tedious details and parenthetical remarks are frequently included
- Loss of Goal – failure to follow a chain of thought to its natural conclusion
- Blocking – interruption of a train of speech before a thought or idea has been completed; person cannot recall what he had been saying or meant to say
- Self-reference – individual repeatedly refers the subject under discussion back to self when someone else is talking; refers apparently neutral subjects to self when talking
- Defects Involving the Use of Words
- Clanging – pattern of speech in which sounds rather than meaning govern word choice
- Neologisms – new word formations; completely new word or phrase whose derivation cannot be understood
- Word Approximations (Paraphasia, Metonyms) – old words used in a new an unconventional way, or new words formed by conventional rules of word formation (e.g. gloves = "handshoes")
- Perseveration – persistent repetition of words, ideas or subjects in the course of speaking
- Echolalia – pattern of speech in which subject echoes words or phrases of the interviewer
- Stilted Speech – speech that has excessively formal quality; pompous, stiff
- Phonemic paraphasia – recognizable mispronunciation of words because sounds or syllables have slipped out of sequence
- Semantic paraphasia – substitution of inappropriate words during effort to say something specific; words used with wrong meaning
- Descriptions of Mood and Affect (a la DSM-IV)
- Affect – pattern of observable behaviors that is the expression of a subjectively experienced feeling state (emotion)
- DSM-IV: "In contrast to mood, which refers to a more pervasive and sustained emotional 'climate', affect refers to more fluctuating changes in emotional 'weather.'
- Common examples of affect are sadness, elation and anger.
- Disturbances of affect include: blunted, flat, inappropriate, labile and restricted.
- Mood – pervasive and sustained emotion that colors perception of the world.
- Common examples of mood include depression, elation, anger, anxiety
- Types of mood include dysphoric, elevated, euthymic, expansive and irritable
- Affect – pattern of observable behaviors that is the expression of a subjectively experienced feeling state (emotion)
- Terms Used in Content of Thought
- Delusion – a fixed false belief that is out of character for the individual's culture
- Hallucination – sensory perception that has compelling sense of reality but that occurs without external stimulation of the relevant sensory organ
- Idea of Reference – feeling that casual incidents and external events have a particular and unusual meaning that is specific to the person
- Delusions of Reference – persistence of IOR in face of evidence to the contrary
- Psychosis – no definition has achieved universal acceptance. The narrowest definition of psychotic implies the presence of delusions or prominent hallucinations, with hallucinations occurring in the absence of insight into their pathological nature. Broader definitions can include the presence of disorganized speech and behavior.
PTSD
Management:
- Consider fluoxetine, paroxetin, sertraline, and venlafaxine (SOR A)
- 2nd: mirtazapine, TCAs
- Consider prazosin for nighttime trauma related nightmares
- Screen and treat for OSA
References:
- AFP Vol 107 No 3 Mar 2023
Primary care PTSD Screen (PC-PTSD)
In your life, have you ever had any experience that was so frightening, horrile, or upsetting that, in the past month, you…
- Have had nightmares about it or thought about it when you did not want to?
- Tried hard not to think about it or went out of your way to avoid situations that remind you of it?
- Were constantly on guard, watchful, or easily startled?
- Felt numb or detached from others, activities, or your surroundings?
SOR B
- If >2 this test has a 78% sensitivity and 87% specificity
- If positive then do a PCL-C test (with all 17 items)
Prim Care Psychiatry. 2003;9:9-14
PTSD associated nightmares
- Prazosin reduces both frequency and severity of PTSD associated nightmares (SOR A)
References:
- JFP Col 64 No 12 Dec 2015 (HDA)
PTSD Pharmacotherapy
- SSRIs improve symptoms of PTSD (1st line) (SOR: A)
- Mirtazapine and amitriptyline also improve symptoms (SOR: B)
Reference:
- AFP Vol 106 No 6 Dec 2022
Sexual Dysfunction
- Female Sexual dysfunction = dysfunction + distress
- Pharmacologic options are limited
- Longer sleep –> increased sexual desire the next day
Lifestyle:
- Sleep/rest
- Exercise
- Nutrition
- Stress management
- No smoking
Somatic Symptom Disorder
Prevalence: 5-7% of general population F:M 10:1
Risk Factors:
- Childhood neglect
- Sexual abuse
- Chaotic lifestyle
- H/o alcohol and substance abuse
Diagnosis:
- Main feature is concern with physical symptoms attributed to a nonpsychiatric disease
- Distressing or resulting in significant disruption of daily life
- Persistent (>6mo)
Treatment:
- CARE MD
- Antidepressants (NNT 3)
- TCA > SSRI - but both are effective
- Amitriptyline most studied - benefits for pain, morning stiffness, global improvement, sleep, fatigue, tender point score, and functional symptoms
- Fluoxetine (Prozac) - best SSRI studied - benefits for pain, functional status, global wellbeing, sleep, morning stiffness, and tender points
AFP Vol 93 No 1 Jan 2016
CARE MD
- C - Consultation/CBT
- A - Assessment
- R - Regular visits
- E - Empathy
- M - Medical/psychiatric interface (emphasize the mind-body connection)
- D - Do no harm (limit testing and referrals; reassure)
AFP Vol 93 No 1 Jan 2016
Study: Attending live sporting events predicts subjective wellbeing and reduces loneliness edit
Introduction:
- This study explored whether attending live sporting events (LSEs) improved subjective wellbeing and loneliness, above and beyond demographic predictors.
Methods:
- Secondary data from 7,249 adults from the Taking Part 2019–20 survey (UK household survey of participation in culture and sport) were analyzed. Multiple linear regressions captured the effect of attending LSEs (yes/no) on wellbeing variables (happiness, anxiety, a sense that life is worthwhile and life satisfaction) and loneliness, with gender, Index of Multiple Deprivation (IMD), age group, health and employment as covariates.
Results:
- For life satisfaction, a sense that life is worthwhile, and loneliness, inclusion of LSE attendance in the model improved model fit significantly, although ΔR2 values were small (ΔR2 = 0.001–0.003).
- For happiness and anxiety, the inclusion of LSE attendance did not alter model fit.
- LSE attendance was associated with
- Increased life satisfaction (b = 0.171, p < 0.001)
- A greater sense of life being worthwhile (b = 0.230, p < 0.001)
- Reduced loneliness (b = −0.083, p < 0.01)
Conclusion:
- LSE attendance has positive associations with some aspects of subjective wellbeing (life satisfaction and a sense of life being worthwhile) and loneliness, above and beyond demographic predictors.
- Whilst the variance explained is small, it is comparable to demographic predictors (e.g., being in employment). As even small-sized differences in SWB can have meaningful outcomes (e.g., for mortality), we conclude that LSE attendance may still offer a scalable, accessible and effective means of improving the public's wellbeing and reducing loneliness.
Reference:
- Keyes H, Gradidge S, Gibson N, Harvey A, Roeloffs S, Zawisza M, Forwood S. Attending live sporting events predicts subjective wellbeing and reduces loneliness. Front Public Health. 2023 Jan 4;10:989706. doi: 10.3389/fpubh.2022.989706. PMID: 36684908; PMCID: PMC9848399.
- https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2022.989706/full
Study: Framing depression as a functional signal, not a disease: Rationale and initial randomized controlled trial
Explaining to patients that their depressive symptoms are an adaptation to their current circumstances, rather than a disease, may produce less stigma and greater patient acceptance and self-efficacy.
- Might be a Signal that something in a patient's life needs more attention and not as something endogenous
- Chemical imbalance explanation of depression, if true at all, may be the effect and not the cause
Highlights
- Depression is often discussed as a medical disorder.
- This framework has some benefits but also has some drawbacks.
- We compared the disease framework to a novel framing of depression as a signal.
- Framing depression as a signal led to less stigma and more hope about recovery.
- Framing depression as a signal had no impact on treatment attitudes.
Depression is often framed as a disease or dysfunctional syndrome, yet this framing has unintended negative consequences including increased stigma. Here, we consider an alternative messaging framework - that depression serves an adaptive function. We describe the historical development of popular messages about depression and draw from the fields of evolutionary psychiatry and social cognition to describe the alternative framework that depression is a "signal" that serves a purpose.
We then present data from a pre-registered, online randomized-controlled study in which participants with self-reported depression histories viewed a series of videos that explained depression as a "disease like any other" with known biopsychosocial risk factors (BPS condition), or as a signal that serves an adaptive function (Signal condition).
In the entire sample (N = 877), three of the six hypotheses were supported:
- The Signal condition led to less self-stigma
- Greater offset efficacy
- More adaptive beliefs about depression
Exploratory analyses revealed these Signal effects were stronger among females (N = 553), who also showed a greater growth mindset of depression after the Signal explanation.
Results suggest that framing depression as an adaptive signal can benefit patients and avoid harmful consequences of popular etiological presentations. We conclude that alternative framings of depression are worthy of further study.
Reference:
- Schroder HS, Devendorf A, Zikmund-Fisher BJ. Framing depression as a functional signal, not a disease: Rationale and initial randomized controlled trial. Soc Sci Med. 2023 Jul;328:115995. doi: 10.1016/j.socscimed.2023.115995. Epub 2023 Jun 3. PMID: 37301109.
Study: Ketamine versus ECT for Nonpsychotic Treatment-Resistant Major Depression
Background
- Electroconvulsive therapy (ECT) and subanesthetic intravenous ketamine are both currently used for treatment-resistant major depression, but the comparative effectiveness of the two treatments remains uncertain.
Methods
- We conducted an open-label, randomized, noninferiority trial involving patients referred to ECT clinics for treatment-resistant major depression. Patients with treatment-resistant major depression without psychosis were recruited and assigned in a 1:1 ratio to receive ketamine or ECT.
- During an initial 3-week treatment phase, patients received either ECT three times per week or ketamine (0.5 mg per kilogram of body weight over 40 minutes) twice per week.
- The primary outcome was a response to treatment (i.e., a decrease of ≥50% from baseline in the score on the 16-item Quick Inventory of Depressive Symptomatology–Self-Report; scores range from 0 to 27, with higher scores indicating greater depression). The noninferiority margin was −10 percentage points.
- Secondary outcomes included scores on memory tests and patient-reported quality of life. After the initial treatment phase, the patients who had a response were followed over a 6-month period.
Results
- A total of 403 patients underwent randomization at five clinical sites; 200 patients were assigned to the ketamine group and 203 to the ECT group. After 38 patients had withdrawn before initiation of the assigned treatment, ketamine was administered to 195 patients and ECT to 170 patients.
- A total of 55.4% of the patients in the ketamine group and 41.2% of those in the ECT group had a response (difference, 14.2 percentage points; 95% confidence interval, 3.9 to 24.2; P<0.001 for the noninferiority of ketamine to ECT).
- ECT appeared to be associated with a decrease in memory recall after 3 weeks of treatment (mean [±SE] decrease in the T-score for delayed recall on the Hopkins Verbal Learning Test–Revised, −0.9±1.1 in the ketamine group vs. −9.7±1.2 in the ECT group; scores range from −300 to 200, with higher scores indicating better function) with gradual recovery during follow-up.
- Improvement in patient-reported quality-of-life was similar in the two trial groups.
- ECT was associated with musculoskeletal adverse effects, whereas ketamine was associated with dissociation.
Conclusions
- Ketamine was noninferior to ECT as therapy for treatment-resistant major depression without psychosis. (Funded by the Patient-Centered Outcomes Research Institute; ELEKT-D ClinicalTrials.gov number, NCT03113968. opens in new tab.)
Reference:
- Anand A, Mathew SJ, Sanacora G, et al. Ketamine versus ECT for Nonpsychotic Treatment-Resistant Major Depression [published online ahead of print, 2023 May 24]. N Engl J Med. 2023;10.1056/NEJMoa2302399. https://doi.org/10.1056/NEJMoa2302399
- https://www.nejm.org/doi/full/10.1056/NEJMoa2302399#article_Abstract
Study: The brain structure, immunometabolic and genetic mechanisms underlying the association between lifestyle and depression edit
Lifestyle factors have been acknowledged to be modifiable targets that can be used to counter the increasing prevalence of depression.
This study aims to investigate combining an extensive range of lifestyle factors, that contribute to depression, and examine the underlying neurobiological mechanisms including:
- alcohol consumption
- diet
- physical activity
- sleep
- smoking
- sedentary behavior
- social connection
Over nine years of follow-up, a multivariate Cox model was utilized on 287,282 participants from UK Biobank to demonstrate the protective roles of seven lifestyle factors and combined lifestyle score on depression.
Combining genetic risk and lifestyle category in 197,344 participants, we found that a healthy lifestyle decreased the risk of depression across a population with varied genetic risk. Mendelian randomization confirmed the causal relationship between lifestyle and depression. A broad range of brain regions and peripheral biomarkers were related to lifestyle, including the pallidum, the precentral cortex, triglycerides and C-reactive protein. Structural equation modeling on 18,244 participants revealed underlying neurobiological mechanisms involving lifestyle, brain structure, immunometabolic function, genetics and depression.
Together, our findings suggest that adherence to a healthy lifestyle could aid in the prevention of depression.
Specific Results:
- Healthy sleep (7-9 hours) decreased the risk of depression by 22% (0.78, 0.75–0.81)
- Never smoking decreased the risk of depression by 20% (0.80, 0.78–0.83)
- Frequent social connection decreased the risk of depression by 18% (0.82, 0.78–0.86)
- Regular physical activity decreased the risk of depression by 14% (0.86, 0.83–0.90)
- Low-to-moderate sedentary behavior (being active) decreased the risk of depression by 13% (0.87, 0.84–0.90)
- Moderate alcohol consumption decreased the risk of depression by 11% (hazard ratio (HR) of 0.89 (95% CI, 0.85–0.92)
- Healthy diet decreased the risk of depression by 6% (0.94, 0.90–0.97)
Reference:
- Zhao, Y., Yang, L., Sahakian, B.J. et al. The brain structure, immunometabolic and genetic mechanisms underlying the association between lifestyle and depression. Nat. Mental Health 1, 736–750 (2023). https://doi.org/10.1038/s44220-023-00120-1
- https://www.nature.com/articles/s44220-023-00120-1
Study: The serotonin theory of depression: a systematic umbrella review of the evidence
The serotonin hypothesis of depression is still influential. We aimed to synthesise and evaluate evidence on whether depression is associated with lowered serotonin concentration or activity in a systematic umbrella review of the principal relevant areas of research.
PubMed, EMBASE and PsycINFO were searched using terms appropriate to each area of research, from their inception until December 2020. Systematic reviews, meta-analyses and large data-set analyses in the following areas were identified: serotonin and serotonin metabolite, 5-HIAA, concentrations in body fluids; serotonin 5-HT1A receptor binding; serotonin transporter (SERT) levels measured by imaging or at post-mortem; tryptophan depletion studies; SERT gene associations and SERT gene-environment interactions. Studies of depression associated with physical conditions and specific subtypes of depression (e.g. bipolar depression) were excluded.
Two independent reviewers extracted the data and assessed the quality of included studies using the AMSTAR-2, an adapted AMSTAR-2, or the STREGA for a large genetic study. The certainty of study results was assessed using a modified version of the GRADE. We did not synthesise results of individual meta-analyses because they included overlapping studies. The review was registered with PROSPERO (CRD42020207203).
17 studies were included:
- 12 systematic reviews and meta-analyses
- 1 collaborative meta-analysis
- 1 meta-analysis of large cohort studies
- 1 systematic review and narrative synthesis
- 1 genetic association study
- 1 umbrella review
Quality of reviews was variable with some genetic studies of high quality.
Two meta-analyses of overlapping studies examining the serotonin metabolite, 5-HIAA, showed no association with depression (largest n = 1002).
One meta-analysis of cohort studies of plasma serotonin showed no relationship with depression, and evidence that lowered serotonin concentration was associated with antidepressant use (n = 1869).
Two meta-analyses of overlapping studies examining the 5-HT1A receptor (largest n = 561), and three meta-analyses of overlapping studies examining SERT binding (largest n = 1845) showed weak and inconsistent evidence of reduced binding in some areas, which would be consistent with increased synaptic availability of serotonin in people with depression, if this was the original, causal abnormaly. However, effects of prior antidepressant use were not reliably excluded.
One meta-analysis of tryptophan depletion studies found no effect in most healthy volunteers (n = 566), but weak evidence of an effect in those with a family history of depression (n = 75).
Another systematic review (n = 342) and a sample of ten subsequent studies (n = 407) found no effect in volunteers. No systematic review of tryptophan depletion studies has been performed since 2007.
The two largest and highest quality studies of the SERT gene, one genetic association study (n = 115,257) and one collaborative meta-analysis (n = 43,165), revealed no evidence of an association with depression, or of an interaction between genotype, stress and depression.
The main areas of serotonin research provide no consistent evidence of there being an association between serotonin and depression, and no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations. Some evidence was consistent with the possibility that long-term antidepressant use reduces serotonin concentration.
—
This review suggests that the huge research effort based on the serotonin hypothesis has not produced convincing evidence of a biochemical basis to depression. This is consistent with research on many other biological markers. We suggest it is time to acknowledge that the serotonin theory of depression is not empirically substantiated.
—
Reference:
- Moncrieff J, Cooper RE, Stockmann T, Amendola S, Hengartner MP, Horowitz MA. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry. 2023 Aug;28(8):3243-3256. doi: 10.1038/s41380-022-01661-0. Epub 2022 Jul 20. PMID: 35854107; PMCID: PMC10618090.
Study: Watching sport enhances well-being: evidence from a multi-method approach
The extant literature supporting the relationship between watching sport and well-being often includes a specific sample population (e.g. sport fans), with the evidence highlighted by limited research approaches (i.e. subjectively measured well-being). It is imperative to assess the robustness of the evidence by implementing diverse methods to understand the contributions of sport-watching behavior to well-being.
The current research aimed to provide evidence on the effects of watching sport on well-being in the general population through three studies that uniquely operationalized well-being.
Study 1 examined the relationship between watching sport and well-being by analyzing publicly available open data with a large sample size (N = 20,000).
Study 2 used an online survey experiment focusing on the general Japanese population (N = 208) to show the changes in well-being after watching videos of various sports.
Study 3 conducted a neuro-imaging experiment (N = 14) using MRI to examine the effect of watching sport on brain activity and structure.
Findings from the three studies indicated that watching sport was positively associated with participants' self-reported well-being, as well as increased brain activity and the structural volume in the specific brain regions related to well-being.
Furthermore, its positive effect was intensified when watching a popular sport (e.g. baseball) compared to watching a less popular sport (e.g. golf).
The current research adds novel contributions to the literature, showing that watching sport can have a positive psychological and neurophysiological impact on human well-being.
Reference:
- Kinoshita, K., Nakagawa, K., & Sato, S. (2024). Watching sport enhances well-being: evidence from a multi-method approach. Sport Management Review, 1–25. https://doi.org/10.1080/14413523.2024.2329831
- https://www.tandfonline.com/doi/full/10.1080/14413523.2024.2329831
Study: Watching sports and depressive symptoms among older adults: a cross-sectional study from the JAGES 2019 survey
The current study investigated the relationship between the frequency of watching sports and depressive symptoms among older adults.
This study used cross-sectional data from the Japan Gerontological Evaluation Study, a nationwide mail survey of 21,317 older adults. Depressive symptoms were defined as a Geriatric Depression Scale score of ≥ 5.
Participants were queried regarding the average frequency at which they watched sports on-site and via TV/Internet over the past year. Among the 21,317 participants, 4559 (21.4%) had depressive symptoms, while 4808 (22.6%) and 16,576 (77.8%) watched sports on-site and via TV/Internet at least once a year, respectively.
Results:
- Older adults who watched sports on-site a few times/year (prevalence ratio, 0.70; 95% confidence interval, 0.65-0.74) or 1-3 times/month (0.66, 0.53-0.82) were less likely to have depressive symptoms compared to non-spectators after adjusting for frequency of playing sports, exercise activities, and other potential confounders.
- Meanwhile, a dose-response relationship was confirmed for watching via TV/Internet (prevalence ratio of 0.86, 0.79, and 0.71 for a few times/year, 1-3 times/month, and ≥ 1 time/week, respectively).
Conclusion:
- This study suggested that watching sports on-site or via TV/Internet, regardless of whether they regularly engage in sports, may reduce the risk of depressive symptoms among older adults.
Reference:
- Tsuji T, Kanamori S, Watanabe R, Yokoyama M, Miyaguni Y, Saito M, Kondo K. Watching sports and depressive symptoms among older adults: a cross-sectional study from the JAGES 2019 survey. Sci Rep. 2021 May 19;11(1):10612. doi: 10.1038/s41598-021-89994-8. PMID: 34011984; PMCID: PMC8134456.
- https://www.nature.com/articles/s41598-021-89994-8
Suicide
See also:
Risk factors:
- Risk factors
- Loss of relationship(s) or isolation
- Psychosocial stress
- Financial hardship
- Chronic mental or physical health conditions
- History of trauma
- Substance abuse
- Recent psychiatric hospitalization
- Past suicide attempt and suicidal ideation
- Constant/recurring guilt or shame
- Male gender
- American Indian/Alaskan native; non-Hispanic white race
- Veteran or active duty military
- Physician
- Rural residence
- Access to lethal means
- Exposure to others' suicidal self-injurious behavior
- Domestic violence
Protective factors:
- Supportive relationships
- Life satisfaction
- Problem-solving or coping skills
- Religious/cultural beliefs against suicide
- Participation in treatment for chronic mental or physical health conditions, or substance use
- Reduced access to lethal mean
Work with the patient to identify the following:
- Warning signs
- thoughts, images, moods, situations, or behaviors that indicate a crisis may be developing
- Coping and distraction strategies
- actions or activities that can help reduce thoughts or urges to engage in suicide behaviors. These may include individual strategies or strategies involving social support from others
- Reasons to live
- important reasons for life to have meaning and purpose
- Supportive people to contact in crisis
- family members, friends, providers, and national/local resources in the event of a crisis
- Additional strategies for safety
- ideas for reducing lethal or harmful means and instructions and contacts for psychiatric hospitalization
References:
- AFP Vol 68 No 9 Nov 2019
Suicide assessment
Risk Factors:
- Suicidality
- Prior attempts
- Hopelessness
- Mental illness
- Recent loss or crisis
- Negativity, rigidity
- Alcohol intoxication/abuse
- Elderly
- Male
- Single/living alone
- Gay/bisexual orientation
- Psychiatric symptoms
- Impulsivity or violent/aggressive behavior
- Family history of suicide
- Unemployment
Protective Factors:
- Female
- Marriage
- Children
- Pregnancy
- Interpersonal support
- Positive coping skills
- Religious activity
- Life satisfaction
Reference:
- JFP Vl 59 No 5 May 2010
Suicide Risk Factors
See also:
Risk Factors:
- Biologic
- Age (45-54 and 75-84)
- Cisgender male
- Race (White)
- Recent illness diagnosis or chronic disease
- Environmental/Social
- Access to means
- Changes in future plans (changing or establishing a will; making funeral arrangements)
- Recent suicide exposure
- Stressful life event (death of a loved one, unemployment, end of a relationship, legal issues)
- Unmarried or limited social support
- Psychological
- Feelings of social isolation
- History of suicide attempts (personal or family)
- Hopelessness
- Insomnia
- Irritability
- Psychiatric history (personal or family), such as anxiety, mood disorders, schizophrenia, borderline personality disorder
- Substance (including ethanol) misuse disorder
References:
- AFP Vol 103 No 7 Apr 2021
Study: How Breath-Control Can Change Your Life: A Systematic Review on Psycho-Physiological Correlates of Slow Breathing
Background:
- The psycho-physiological changes in brain-body interaction observed in most of meditative and relaxing practices rely on voluntary slowing down of breath frequency. However, the identification of mechanisms linking breath control to its psychophysiological effects is still under debate.
- This systematic review is aimed at unveiling psychophysiological mechanisms underlying slow breathing techniques (<10 breaths/minute) and their effects on healthy subjects.
Methods:
- A systematic search of MEDLINE and SCOPUS databases, using keywords related to both breathing techniques and to their psychophysiological outcomes, focusing on cardio-respiratory and central nervous system, has been conducted. From a pool of 2,461 abstracts only 15 articles met eligibility criteria and were included in the review. The present systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Results:
- The main effects of slow breathing techniques cover autonomic and central nervous systems activities as well as the psychological status.
- Slow breathing techniques promote autonomic changes increasing Heart Rate Variability and Respiratory Sinus Arrhythmia paralleled by Central Nervous System (CNS) activity modifications.
- EEG studies show an increase in alpha and a decrease in theta power. Anatomically, the only available fMRI study highlights increased activity in cortical (e.g., prefrontal, motor, and parietal cortices) and subcortical (e.g., pons, thalamus, sub-parabrachial nucleus, periaqueductal gray, and hypothalamus) structures.
- Psychological/behavioral outputs related to the above mentioned changes are:
- Increased comfort
- Relaxation
- Pleasantness
- Vigor and alertness
- Reduced symptoms of arousal, anxiety, depression, anger, and confusion
Conclusions:
- Slow breathing techniques act enhancing autonomic, cerebral and psychological flexibility in a scenario of mutual interactions: we found evidence of links between parasympathetic activity (increased HRV and LF power), CNS activities (increased EEG alpha power and decreased EEG theta power) related to emotional control and psychological well-being in healthy subjects.
- Our hypothesis considers two different mechanisms for explaining psychophysiological changes induced by voluntary control of slow breathing:
- one is related to a voluntary regulation of internal bodily states (enteroception),
- the other is associated to the role of mechanoceptors within the nasal vault in translating slow breathing in a modulation of olfactory bulb activity, which in turn tunes the activity of the entire cortical mantle.
Reference:
Study: A dose response relationship between accelerometer assessed daily steps and depressive symptoms in older adults: a two-year cohort study
Objectives:
- This study investigated the prospective associations of accelerometer assessed daily steps with subsequent depressive symptoms in older adults.
Methods:
- A 2-year prospective study was performed in the community. A total of 285 older adults ≥65 years (mean age = 74.5) attended the baseline assessment in 2012. The second wave of assessment was carried out in 2014 including 274 (96.1%) participants. Daily step counts were measured with a triaxial accelerometer (ActiGraph GT3X+), and participants were divided into three categories (<3,500, 3,500-6,999 and ≥ 7,000 steps/day). The 15-item Geriatric Depression Scale was used to measure depressive symptoms. Negative binomial regression models with multivariable adjustment for covariates (baseline depressive symptoms, accelerometer wear time, age, gender, education, chronic disease, activities of daily living) were conducted to examine the association between daily steps and subsequent depressive symptoms.
Results:
- Each 1,000-step increase in daily walking was linearly associated with a reduced rate of subsequent depressive symptoms (rate ratio [RR] = 0.95, 95% confidence interval [CI] = 0.92-0.98).
- Participants with daily step count in 3,500-6,999 (RR = 0.84, 95% CI = 0.70-0.99) and ≥7,000 steps (RR = 0.71, 95% CI = 0.55-0.92) per day had fewer depressive symptoms at follow-up.
- Sensitivity analyses assessing confounding and reverse causation provided further support for the stability of our findings.
Conclusion:
- Older adults engaging in more daily steps had fewer depressive symptoms after 2 years.
- Even as few as 3,500-6,999 steps a day was associated with a protecting effect.
- Accumulating ≥7,000 steps a day could provide the greatest protection against depressive symptoms.
Reference:
- Hsueh MC, Stubbs B, Lai YJ, Sun CK, Chen LJ, Ku PW. A dose response relationship between accelerometer assessed daily steps and depressive symptoms in older adults: a two-year cohort study. Age Ageing. 2021 Feb 26;50(2):519-526. doi: 10.1093/ageing/afaa162. PMID: 32980870.
Study: Daily Step Count and Depression in Adults: A Systematic Review and Meta-Analysis
Importance:
- Recent evidence syntheses have supported the protective role of daily steps in decreasing the risk of cardiovascular disease and all-cause mortality. However, step count-based recommendations should cover additional health outcomes.
Objective:
- To synthesize the associations between objectively measured daily step counts and depression in the general adult population.
Data sources:
- In this systematic review and meta-analysis, a systematic search of the PubMed, PsycINFO, Scopus, SPORTDiscus, and Web of Science databases was conducted from inception until May 18, 2024, to identify observational studies using search terms related to physical activity, measures of daily steps, and depression, among others. Supplementary search methods were also applied.
Study selection:
- All identified studies were uploaded to an online review system and were considered without restrictions on publication date or language. Included studies had objectively measured daily step counts and depression data.
Data extraction and synthesis:
- This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses and Meta-analysis of Observational Studies in Epidemiology reporting guidelines. Two independent reviewers extracted the published data.
Main outcomes and measures:
- Pooled effect sizes (correlation coefficient, standardized mean difference [SMD], and risk ratio [RR]) with 95% CIs were estimated using the Sidik-Jonkman random-effects method.
Results:
- Thirty-three studies (27 cross-sectional and 6 longitudinal [3 panel and 3 prospective cohort]) involving 96,173 adults aged 18 years or older (range of mean [SD] ages: 18.6 [0.6] to 91.2 [1.6] years) were included.
- Daily steps were inversely correlated with depressive symptoms in both cross-sectional and panel studies.
- Compared with fewer than 5000 steps/d, pooled SMDs from cross-sectional studies revealed that 10,000 or more steps/d (SMD, -0.26; 95% CI, -0.38 to -0.14), 7500 to 9999 steps/d (SMD, -0.27; 95% CI, -0.43 to -0.11), and 5000 to 7499 steps/d (SMD, -0.17; 95% CI, -0.30 to -0.04) were significantly associated with fewer depressive symptoms.
- Pooled estimates from prospective cohort studies indicated that participants with 7000 or more steps/d had reduced risk of depression compared with their counterparts with fewer than 7000 steps/d (RR, 0.69; 95% CI, 0.62-0.77).
- An increase of 1000 steps/d was associated with a lower risk of depression (RR, 0.91; 95% CI, 0.87-0.94).
Conclusions and relevance:
- In this systematic review and meta-analysis of 33 observational studies involving 96,173 adults, higher daily step counts were associated with fewer depressive symptoms in cross-sectional and longitudinal studies in the general adult population. Further prospective cohort studies are needed to clarify the potential protective role of daily steps in mitigating the risk of depression during adulthood.
Reference:
- Bizzozero-Peroni B, Díaz-Goñi V, Jiménez-López E, Rodríguez-Gutiérrez E, Sequí-Domínguez I, Núñez de Arenas-Arroyo S, López-Gil JF, Martínez-Vizcaíno V, Mesas AE. Daily Step Count and Depression in Adults: A Systematic Review and Meta-Analysis. JAMA Netw Open. 2024 Dec 2;7(12):e2451208. doi: 10.1001/jamanetworkopen.2024.51208. PMID: 39680407; PMCID: PMC11650418.
Study: Efficacy and Safety of Selective Serotonin Reuptake Inhibitors, Serotonin-Norepinephrine Reuptake Inhibitors, and Placebo for Common Psychiatric Disorders Among Children and Adolescents: A Systematic Review and Meta-analysis edit
Importance:
- Depressive disorders (DDs), anxiety disorders (ADs), obsessive-compulsive disorder (OCD), and posttraumatic stress disorder (PTSD) are common mental disorders in children and adolescents.
Objective:
- To examine the relative efficacy and safety of selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and placebo for the treatment of DD, AD, OCD, and PTSD in children and adolescents.
Data sources:
- PubMed, EMBASE, PsycINFO, Web of Science, and Cochrane Database from inception through August 7, 2016.
Study selection:
- Published and unpublished randomized clinical trials of SSRIs or SNRIs in youths with DD, AD, OCD, or PTSD were included. Trials using other antidepressants (eg, tricyclic antidepressants, monoamine oxidase inhibitors) were excluded.
Data extraction and synthesis:
- Effect sizes, calculated as standardized mean differences (Hedges g) and risk ratios (RRs) for adverse events, were assessed in a random-effects model.
Main outcomes and measures:
- Primary outcomes, as defined by authors on preintervention and postintervention data, mean change data, and adverse event data, were extracted independently by multiple observers following PRISMA guidelines.
Results:
- Thirty-six trials were eligible, including 6778 participants (3484 [51.4%] female; mean [SD] age, 12.9 [5.1] years); 17 studies for DD, 10 for AD, 8 for OCD, and 1 for PTSD.
- Analysis showed that SSRIs and SNRIs were significantly more beneficial compared with placebo, yielding a small effect size (g = 0.32; 95% CI, 0.25-0.40; P < .001).
- Anxiety disorder (g = 0.56; 95% CI, 0.40-0.72; P < .001) showed significantly larger between-group effect sizes than DD (g = 0.20; 95% CI, 0.13-0.27; P < .001).
- This difference was driven primarily by the placebo response:
- patients with DD exhibited significantly larger placebo responses (g = 1.57; 95% CI, 1.36-1.78; P < .001) compared with those with AD (g = 1.03; 95% CI, 0.84-1.21; P < .001).
- This difference was driven primarily by the placebo response:
- The SSRIs produced a relatively large effect size for ADs (g = 0.71; 95% CI, 0.45-0.97; P < .001).
- Compared with participants receiving placebo, patients receiving an antidepressant reported significantly more treatment-emergent adverse events (RR, 1.07; 95% CI, 1.01-1.12; P = .01 or RR, 1.49; 95% CI, 1.22-1.82; P < .001, depending on the reporting method), severe adverse events (RR, 1.76; 95% CI, 1.34-2.32; P < .001), and study discontinuation due to adverse events (RR, 1.79; 95% CI, 1.38-2.32; P < .001).
Conclusions and relevance:
- Compared with placebo, SSRIs and SNRIs are more beneficial than placebo in children and adolescents; however, the benefit is small and disorder specific, yielding a larger drug-placebo difference for AD than for other conditions.
- Response to placebo is large, especially in DD.
- Severe adverse events are significantly more common with SSRIs and SNRIs than placebo.
Reference:
- Locher C, Koechlin H, Zion SR, Werner C, Pine DS, Kirsch I, Kessler RC, Kossowsky J. Efficacy and Safety of Selective Serotonin Reuptake Inhibitors, Serotonin-Norepinephrine Reuptake Inhibitors, and Placebo for Common Psychiatric Disorders Among Children and Adolescents: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2017 Oct 1;74(10):1011-1020. doi: 10.1001/jamapsychiatry.2017.2432. PMID: 28854296; PMCID: PMC5667359.
Study: The efficacy of paroxetine and placebo in treating anxiety and depression: a meta-analysis of change on the Hamilton Rating Scales edit
Background:
- Previous meta-analyses of published and unpublished trials indicate that antidepressants provide modest benefits compared to placebo in the treatment of depression; some have argued that these benefits are not clinically significant. However, these meta-analyses were based only on trials submitted for the initial FDA approval of the medication and were limited to those aimed at treating depression.
- Here, for the first time, we assess the efficacy of a selective serotonin reuptake inhibitor (SSRI) in the treatment of both anxiety and depression, using a complete data set of all published and unpublished trials sponsored by the manufacturer.
Methods and findings:
- GlaxoSmithKline has been required to post the results for all sponsored clinical trials online, providing an opportunity to assess the efficacy of an SSRI (paroxetine) with a complete data set of all trials conducted.
- We examined the data from all placebo-controlled, double-blind trials of paroxetine that included change scores on the Hamilton Rating Scale for Anxiety (HRSA) and/or the Hamilton Rating Scale for Depression (HRSD).
- For the treatment of anxiety (k = 12), the efficacy difference between paroxetine and placebo was modest (d = 0.27), and independent of baseline severity of anxiety.
- Overall change in placebo-treated individuals replicated 79% of the magnitude of paroxetine response.
- Efficacy was superior for the treatment of panic disorder (d = 0.36) than for generalized anxiety disorder (d = 0.20).
- Published trials showed significantly larger drug-placebo differences than unpublished trials (d's = 0.32 and 0.17, respectively).
- In depression trials (k = 27), the benefit of paroxetine over placebo was consistent with previous meta-analyses of antidepressant efficacy (d = 0.32).
Conclusions:
- The available empirical evidence indicates that paroxetine provides only a modest advantage over placebo in treatment of anxiety and depression. Treatment implications are discussed.
Reference:
- Sugarman MA, Loree AM, Baltes BB, Grekin ER, Kirsch I. The efficacy of paroxetine and placebo in treating anxiety and depression: a meta-analysis of change on the Hamilton Rating Scales. PLoS One. 2014 Aug 27;9(8):e106337. doi: 10.1371/journal.pone.0106337. PMID: 25162656; PMCID: PMC4146610.
Study: Antidepressants versus placebo in major depression: an overview edit
Although the early antidepressant trials which included severely ill and hospitalized patients showed substantial drug-placebo differences, these robust differences have not held up in the trials of the past couple of decades, whether sponsored by pharmaceutical companies or non-profit agencies. This narrowing of the drug-placebo difference has been attributed to a number of changes in the conduct of clinical trials.
First, the advent of DSM-III and the broadening of the definition of major depression have led to the inclusion of mildly to moderately ill patients into antidepressant trials. These patients may experience a smaller magnitude of antidepressant-placebo differences.
Second, drug development regulators, such as the U.S. Food and Drug Administration and the European Medicines Agency, have had a significant, albeit underappreciated, role in determining how modern antidepressant clinical trials are designed and conducted. Their concerns about possible false positive results have led to trial designs that are poor, difficult to conduct, and complicated to analyze.
Attempts at better design and patient selection for antidepressant trials have not yielded the expected results.
As of now, antidepressant clinical trials have an effect size of 0.30, which, although similar to the effects of treatments for many other chronic illnesses, such as hypertension, asthma and diabetes, is less than impressive.
Reference:
- Khan A, Brown WA. Antidepressants versus placebo in major depression: an overview. World Psychiatry. 2015 Oct;14(3):294-300. doi: 10.1002/wps.20241. PMID: 26407778; PMCID: PMC4592645.
Study: Antidepressants versus placebo for depression in primary care edit
Effectiveness:
- TCAs: 1:9
- SSRIs: 1:7
Abstract
Background:
- Concern has been expressed about the relevance of secondary care studies to primary care patients specifically about the effectiveness of antidepressant medication. There is a need to review the evidence of only those studies that have been conducted comparing antidepressant efficacy with placebo in primary care-based samples.
Objectives:
- To determine the efficacy and tolerability of antidepressants in patients (under the age of 65 years) with depression in primary care.
Search strategy:
- All searches were conducted in September 2007.The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) Controlled Trials Register was searched, together with a supplementary search of MEDLINE, PsycINFO, EMBASE, LILACS, CINAHL and PSYNDEX. Abstracts of all possible studies for inclusion were assessed independently by two reviewers. Further trials were sought through searching the reference lists of studies initially identified and by scrutinising other relevant review papers. Selected authors and experts were also contacted.
Selection criteria:
- Studies were selected if they were randomised controlled trials of tricyclic antidepressants (TCAs) or selective serotonin reuptake inhibitors (SSRIs) versus placebo in adults. Older patients (over 65 years) were excluded. Patients had to be recruited from a primary care setting. For continuous outcomes the Hamilton Depression scale of the Montgomery Asberg Scale was requred.
Data collection and analysis:
- Data were extracted using data extraction forms by two reviewers independently, with disagreements resolved by discussion. A similar process was used for the validity assessment. Pooling of results was done using Review Manager 5. The primary outcome was depression reduction, based on a dichotomous measure of clinical response, using relative risk (RR), and on a continuous measure of depression symptoms, using the mean difference (MD), with 95% confidence intervals (CI).
Main results:
- There were fourteen studies (16 comparisons) with extractable data included in the review, of which ten studies examined TCAs, two examined SSRIs and two included both classes, all compared with placebo.
- The number of participants in the intervention groups was 1364 and in the placebo groups 919. Nearly all studies were of short duration, typically 6-8 weeks.
- Efficacy:
- Pooled estimates of efficacy data showed an RR of 1.24, 95% CI 1.11-1.38 in favour of TCAs against placebo.
- For SSRIs this was 1.28, 95% CI 1.15 to 1.43.
- The numbers needed to treat (NNT) for TCAs ranged from 7 to 16 {median NNT 9} patient expected event rate ranged from 63% to 26% respectively) and for SSRIs from 7 to 8 {median NNT 7} (patient expected event rate ranged from 48% to 42% respectively) .
- The numbers needed to harm (NNH for withdrawal due to side effects) ranged from 4 to 30 for TCAs (excluding three studies with no harmful events leading to withdrawal) and 20 to 90 for SSRIs.
Authors' conclusions:
- Both TCAs and SSRIs are effective for depression treated in primary care.
Reference:
- Arroll B, Elley CR, Fishman T, Goodyear-Smith FA, Kenealy T, Blashki G, Kerse N, Macgillivray S. Antidepressants versus placebo for depression in primary care. Cochrane Database Syst Rev. 2009 Jul 8;2009(3):CD007954. doi: 10.1002/14651858.CD007954. PMID: 19588448; PMCID: PMC10576545.
Study: Meta-analysis of the association between gratitude and loneliness edit
Abstract Gratitude is a positive social emotion that involves recognizing that others have brought benefits into one's life. Loneliness, on the other hand, is an unpleasant emotion resulting from a perceived lack of social connectedness. Although previous studies have reported an inverse association between gratitude and loneliness, these studies have not been systematically examined in a single review. To address this gap in the literature, we conducted a random-effects meta-analysis to examine the association between gratitude and loneliness. Analysis of 26 studies revealed a moderate sized effect (mean Fisher's z transformed correlation, zr = -.406, 95% confidence interval [CI] = -.463, -.349; mean back-transformed correlation, r = -.385, 95% CI = -.433, -.335). To complement these effect sizes, we calculated a probability-based common language effect size for correlations. Random-effects homogeneity testing suggested the presence of effect size heterogeneity. Analyses of both continuous and categorical moderators were non-significant, indicating that these variables did not influence effect size magnitude. Furthermore, publication bias tests suggested that our results were not influenced by unpublished studies. Finally, we proposed several statistical and clinical recommendations for future research. Regarding the latter, we offered suggestions for modifying gratitude enhancement programs with the aim of reducing loneliness.
Take Aways:
- In this meta-analysis, we found a statistically significant, moderate sized inverse association between gratitude and loneliness (overall mean Fisher zr = −.406, overall mean back-transformed correlation, r = −.385).
- One promising gratitude enhancing approach is the “three good things exercise” whereby participants list three good things that happened to them during the day and why they believe that those things happened (for an application, see Bartlett & Arpin, 2019).
- If participants are encouraged to list good things that are socially or interpersonally focused, then gratitude for relationships will be heightened which in turn should reduce loneliness.
- Another promising approach is to broaden cognitive schemas as they relate to interpersonal relationships. This recommended approach is consistent with Fredrickson's (2004, 2013) broaden-and-build theory. Consistent with this recommendation, Frinking et al. (2020) found that psychological flexibility significantly mediated the effect of dispositional gratitude on loneliness (gratitude was associated with enhanced flexibility and enhanced flexibility was associated with reduced loneliness).
- One promising gratitude enhancing approach is the “three good things exercise” whereby participants list three good things that happened to them during the day and why they believe that those things happened (for an application, see Bartlett & Arpin, 2019).
Reference:
- Hittner JB, Widholm CD. Meta-analysis of the association between gratitude and loneliness. Appl Psychol Health Well Being. 2024 Nov;16(4):2520-2535. doi: 10.1111/aphw.12549. Epub 2024 May 13. PMID: 38741417.
Suicide Risk And Documentation
The mnemonic SUICIDE is used to remind practitioners of key elements to include when documenting suicide risk. Each letter stands for a specific aspect of suicide risk assessment and management:
- S: Suicide assessment. Evaluate the patient for suicide risk factors and protective factors.
- U: Unpredictable and unpreventable. Acknowledge the limits of prediction and prevention despite comprehensive risk assessment.
- I: Interventions. Proceed with biological, psychological, and social treatment options.
- C: Clear and comprehensive documentation. Ensure detailed, accurate, and thorough daily notes.
- I: Include social support in planning for safe discharge.
- D: Educate, engage, and empathize with the patient.
- E: Ensure the patient and family members are informed about the unpredictability of suicide despite best efforts.
Attention-Deficit/Hyperactivity Disorder Medications and Long-Term Risk of Cardiovascular Diseases
Key Points
- Question
- Is long-term use of attention-deficit/hyperactivity disorder (ADHD) medication associated with an increased risk of cardiovascular disease (CVD)?
- Findings
- In this case-control study of 278 027 individuals in Sweden aged 6 to 64 years who had an incident ADHD diagnosis or ADHD medication dispensation, longer cumulative duration of ADHD medication use was associated with an increased risk of CVD, particularly hypertension and arterial disease, compared with nonuse.
- Meaning
- Findings of this study suggest that long-term exposure to ADHD medications was associated with an increased risk of CVD; therefore, the potential risks and benefits of long-term ADHD medication use should be carefully weighed.
Abstract
- Importance Use of attention-deficit/hyperactivity disorder (ADHD) medications has increased substantially over the past decades. However, the potential risk of cardiovascular disease (CVD) associated with long-term ADHD medication use remains unclear.
Objective
- To assess the association between long-term use of ADHD medication and the risk of CVD.
Design, Setting, and Participants
- This case-control study included individuals in Sweden aged 6 to 64 years who received an incident diagnosis of ADHD or ADHD medication dispensation between January 1, 2007, and December 31, 2020. Data on ADHD and CVD diagnoses and ADHD medication dispensation were obtained from the Swedish National Inpatient Register and the Swedish Prescribed Drug Register, respectively. Cases included individuals with ADHD and an incident CVD diagnosis (ischemic heart diseases, cerebrovascular diseases, hypertension, heart failure, arrhythmias, thromboembolic disease, arterial disease, and other forms of heart disease). Incidence density sampling was used to match cases with up to 5 controls without CVD based on age, sex, and calendar time. Cases and controls had the same duration of follow-up.
Exposure
- Cumulative duration of ADHD medication use up to 14 years.
Main Outcomes and Measures
- The primary outcome was incident CVD. The association between CVD and cumulative duration of ADHD medication use was measured using adjusted odds ratios (AORs) with 95% CIs.
Results
- Of 278,027 individuals with ADHD aged 6 to 64 years, 10,388 with CVD were identified (median [IQR] age, 34.6 [20.0-45.7] years; 6154 males [59.2%]) and matched with 51 672 control participants without CVD (median [IQR] age, 34.6 [19.8-45.6] years; 30 601 males [59.2%]).
- Median (IQR) follow-up time in both groups was 4.1 (1.9-6.8) years.
- Longer cumulative duration of ADHD medication use was associated with an increased risk of CVD compared with nonuse
- 0 to ≤1 year: AOR, 0.99 [95% CI, 0.93-1.06];
- 1 to ≤2 years: AOR, 1.09 [95% CI, 1.01-1.18];
- 2 to ≤3 years: AOR, 1.15 [95% CI, 1.05-1.25];
- 3 to ≤5 years: AOR, 1.27 [95% CI, 1.17-1.39];
- >5 years: AOR, 1.23 [95% CI, 1.12-1.36]
- Longer cumulative ADHD medication use was associated with an increased risk of
- hypertension
- 3 to ≤5 years: AOR, 1.72 [95% CI, 1.51-1.97]
- >5 years: AOR, 1.80 [95% CI, 1.55-2.08]
- arterial disease
- 3 to ≤5 years: AOR, 1.65 [95% CI, 1.11-2.45]
- >5 years: AOR, 1.49 [95% CI, 0.96-2.32]
- hypertension
- Across the 14-year follow-up, each 1-year increase of ADHD medication use was associated with a 4% increased risk of CVD (AOR, 1.04 [95% CI, 1.03-1.05]), with a larger increase in risk in the first 3 years of cumulative use (AOR, 1.08 [95% CI, 1.04-1.11]) and stable risk over the remaining follow-up.
- Similar patterns were observed in children and youth (aged <25 years) and adults (aged ≥25 years).
Conclusions and Relevance
- This case-control study found that long-term exposure to ADHD medications was associated with an increased risk of CVDs, especially hypertension and arterial disease. These findings highlight the importance of carefully weighing potential benefits and risks when making treatment decisions about long-term ADHD medication use. Clinicians should regularly and consistently monitor cardiovascular signs and symptoms throughout the course of treatment.
Reference:
- Zhang L, Li L, Andell P, Garcia-Argibay M, Quinn PD, D'Onofrio BM, Brikell I, Kuja-Halkola R, Lichtenstein P, Johnell K, Larsson H, Chang Z. Attention-Deficit/Hyperactivity Disorder Medications and Long-Term Risk of Cardiovascular Diseases. JAMA Psychiatry. 2023 Nov 22. doi: 10.1001/jamapsychiatry.2023.4294. Epub ahead of print. PMID: 37991787.
- https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2811812
Autism-Spectrum Quotient (AQ)
A measure of the extent of autistic traits in adults.
- In the first major trial using the test, the average score in the control group was 16.4.
- 80% of those diagnosed with autism or a related disorder scored 32 or higher.
- The test is not a means for making a diagnosis, however, and many who score above 32 and even meet the diagnostic criteria for mild autism or Asperger’s report no difficulty functioning in their everyday lives.
AQ Questions:
- I prefer to do things with others rather than on my own.
- I prefer to do things the same way over and over again.
- If I try to imagine something, I find it very easy to create a picture in my mind.
- I frequently get so strongly absorbed in one thing that I lose sight of other things.
- I often notice small sounds when others do not.
- I usually notice car number plates or similar strings of information.
- Other people frequently tell me that what I’ve said is impolite, even though I think it is polite.
- When I’m reading a story, I can easily imagine what the characters might look like.
- I am interested in the patterns or correlations of events.
- In a social group, I can easily keep track of several different people’s conversations.
- I find social situations easy.
- I tend to notice details that others do not.
- I would rather go to a library than to a party.
- I find making up stories easy.
- I find myself drawn more strongly to people than to things.
- I tend to have very strong interests, which I get upset about if I can’t pursue.
- I enjoy social chitchat.
- When I talk, it isn’t always easy for others to get a word in edgewise.
- I am fascinated by numbers.
- When I’m reading a story, I find it difficult to work out the characters’ intentions.
- I enjoy reading informative literature, but I sometimes like reading fiction as well (and might use it to learn social skills).
- I find it hard to make new friends.
- I notice patterns in things all the time.
- I would rather go to the theater than to a museum.
- It does not upset me if my daily routine is disturbed.
- I frequently find that I don’t know how to keep a conversation going.
- I find it easy to ‘read between the lines’ when someone is talking to me.
- I usually concentrate more on the whole picture, rather than on the small details.
- I am not very good at remembering information that is important to me.
- I usually notice small changes in a situation or person’s appearance.
- I know how to tell if someone listening to me is getting bored.
- I find it easy to do more than one thing at once.
- When I talk on the phone, I’m not sure when it’s my turn to speak.
- I enjoy doing things spontaneously.
- I am often the last to understand the point of a joke.
- I find it easy to work out what someone is thinking or feeling just by looking at their face.
- If there is an interruption, I can switch back to what I was doing very quickly.
- I am good at social chitchat.
- People often tell me that I keep going on and on about the same thing.
- When I was young, I used to enjoy playing games involving pretending with other children.
- I like to collect information about categories of things (e.g., types of cars, birds, trains, plants).
- I find it difficult to imagine what it would be like to be someone else.
- I like to carefully plan any activities I participate in.
- I enjoy social occasions.
- I find it difficult to work out people’s intentions.
- New situations make me anxious.
- I enjoy meeting new people.
- I am a good diplomat.
- I am not very good at remembering information that is important to me.
- I find it very easy to play games with children that involve pretending.
How to score:
- “Definitely agree” or “Slightly agree” responses to questions 2, 4, 5, 6, 7, 9, 12, 13, 16, 18, 19, 20, 21, 22, 23, 26, 33, 35, 39, 41, 42, 43, 45, 46 score 1 point.
- “Definitely disagree” or “Slightly disagree” responses to questions 1, 3, 8, 10, 11, 14, 15, 17, 24, 25, 27, 28, 29, 30, 31, 32, 34, 36, 37, 38, 40, 44, 47, 48, 49, 50 score 1 point.
Autism Spectrum Quotient For each statement below, choose one response that best describes how strongly that statement applies to you:
- I prefer to do things with others rather than on my own.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I prefer to do things the same way over and over again.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- If I try to imagine something, I find it very easy to create a picture in my mind.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I frequently get so strongly absorbed in one thing that I lose sight of other things.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I often notice small sounds when others do not.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I usually notice car number plates or similar strings of information.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- Other people frequently tell me that what I've said is impolite, even though I think it is polite.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- When I'm reading a story, I can easily imagine what the characters might look like.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I am fascinated by dates.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- In a social group, I can easily keep track of several different people's conversations.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I find social situations easy.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I tend to notice details that others do not.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I would rather go to a library than a party.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I find making up stories easy.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I find myself drawn more strongly to people than to things.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I tend to have very strong interests which I get upset about if I can't pursue.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I enjoy social chit-chat.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- When I talk, it isn't always easy for others to get a word in edgeways.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I am fascinated by numbers.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- When I'm reading a story, I find it difficult to work out the characters' intentions.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I don't particularly enjoy reading fiction.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I find it hard to make new friends.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I notice patterns in things all the time.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I would rather go to the theatre than a museum.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- It does not upset me if my daily routine is disturbed.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I frequently find that I don't know how to keep a conversation going.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I find it easy to 'read between the lines' when someone is talking to me.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I usually concentrate more on the whole picture, rather than the small details.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I am not very good at remembering phone numbers.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I don't usually notice small changes in a situation, or a person's appearance.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I know how to tell if someone listening to me is getting bored.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I find it easy to do more than one thing at once.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- When I talk on the phone, I'm not sure when it's my turn to speak.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I enjoy doing things spontaneously.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I am often the last to understand the point of a joke.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I find it easy to work out what someone is thinking or feeling just by looking at their face.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- If there is an interruption, I can switch back to what I was doing very quickly.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I am good at social chit-chat.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- People often tell me that I keep going on and on about the same thing.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- When I was young, I used to enjoy playing games involving pretending with other children.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I like to collect information about categories of things.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I find it difficult to imagine what it would be like to be someone else.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I like to plan any activities I participate in carefully.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I enjoy social occasions.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I find it difficult to work out people's intentions.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- New situations make me anxious.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I enjoy meeting new people.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I am a good diplomat.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I am not very good at remembering people's date of birth.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
- I find it very easy to play games with children that involve pretending.
- Definitely Agree
- Slightly Agree
- Slightly Disagree
- Definitely Disagree
Update with: If you take the test, please interpret the outdated questions as follows: #9. I am interested in the patterns or correlations of events. #21. I enjoy reading informative literature, but I sometimes like reading fiction as well (and might use it to learn social skills). #29. I am not very good at remembering information that is important to me. #30. I usually notice small changes in a situation or person’s appearance. #49. I am not very good at remembering information that is important to me.
Reference:
- Brugha T, Tyrer F, Leaver A, Lewis S, Seaton S, Morgan Z, Tromans S, van Rensburg K. Testing adults by questionnaire for social and communication disorders, including autism spectrum disorders, in an adult mental health service population. Int J Methods Psychiatr Res. 2020 Mar;29(1):e1814. doi: 10.1002/mpr.1814. Epub 2020 Jan 10. PMID: 31899844; PMCID: PMC7051834.
- Autism Spectrum Quotient | Embrace Autism
- Simon Baron-Cohen, et al. The Autism-Spectrum Quotient (AQ): Evidence from Asperger Syndrome/High-Functioning Autism, Males and Females, Scientists and Mathematicians. 31: Journal of Autism and Developmental Disorders 5-17. 2001.
- M Woodbury-Smith. Screening Adults for Asperger Syndrome using the AQ: a Preliminary Study of its Diagnostic Validity in Clinical Practice. 35(3): 331-335. Journal of Autism and Developmental Disorders. 2005.
- Dorothy VM Bishop, et al. Using Self-Report to Identify the Broad Phenotype in Parents of Children with Autistic Spectrum Disorders: A Study using the Autism-Spectrum Quotient. 45(8): 1431-1436. Journal of Child Psychology and Psychiatry (2004).
Autism edit
Autism, or Autism Spectrum Disorder (ASD), is a neurodevelopmental condition characterized by differences in social communication, behavior, and sensory processing. It's a spectrum, meaning it varies widely in how it affects individuals—some may need significant support, while others live independently with milder traits.
Key features include:
- Social Communication: Difficulty with social cues, such as understanding body language, maintaining conversations, or forming relationships.
- Repetitive Behaviors: Engaging in repetitive actions (e.g., hand-flapping, lining up objects) or having intense, focused interests.
- Sensory Sensitivities: Over- or under-sensitivity to sounds, lights, textures, or other sensory input.
- Cognitive and Learning Differences: Some individuals have intellectual disabilities, while others may excel in specific areas like math or memory.
ASD is typically diagnosed in early childhood, though signs can appear later. It's thought to result from a mix of genetic and environmental factors, with no single cause identified. Estimates suggest 1 in 36 children in the U.S. have ASD (based on 2023 CDC data). There's no "cure," but interventions like behavioral therapy, speech therapy, or occupational therapy can help manage challenges.
Study: Explaining the increase in the prevalence of autism spectrum disorders: the proportion attributable to changes in reporting practices
Importance
- The prevalence of autism spectrum disorders (ASDs) has increased markedly in recent decades, which researchers have suggested could be caused in part by nonetiologic factors such as changes in diagnosis reporting practices. To our knowledge, no study has quantified the degree to which changes in reporting practices might explain this increase. Danish national health registries have undergone a change in diagnostic criteria in 1994 and the inclusion of outpatient contacts to health registries in 1995.
Objective
- To quantify the effect of changes in reporting practices in Denmark on reported ASD prevalence.
Design, setting, and participants
- We used a population-based birth cohort approach that includes information on all individuals with permanent residence in Denmark. We assessed all children born alive from January 1, 1980, through December 31, 1991, in Denmark (n=677915). The children were followed up from birth until ASD diagnosis, death, emigration, or the end of follow-up on December 31, 2011, whichever occurred first. The analysis uses a stratified Cox proportional hazards regression model with the changes in reporting practices modeled as time-dependent covariates.
Exposures
- The change in diagnostic criteria in 1994 and the inclusion of outpatient diagnoses in 1995.
Main outcomes and measures
- Autism spectrum disorders.
Results
- For Danish children born during the study period:
- 33% (95% CI, 0%-70%) of the increase in reported ASD prevalence could be explained by the change in diagnostic criteria alone
- 42% (95% CI, 14%-69%), by the inclusion of outpatient contacts alone
- 60% (95% CI, 33%-87%), by the change in diagnostic criteria and the inclusion of outpatient contacts
Conclusions and relevance
- Changes in reporting practices can account for most (60%) of the increase in the observed prevalence of ASDs in children born from 1980 through 1991 in Denmark. Hence, the study supports the argument that the apparent increase in ASDs in recent years is in large part attributable to changes in reporting practices.
Reference:
- Hansen SN, Schendel DE, Parner ET. Explaining the increase in the prevalence of autism spectrum disorders: the proportion attributable to changes in reporting practices. JAMA Pediatr. 2015 Jan;169(1):56-62. doi: 10.1001/jamapediatrics.2014.1893. PMID: 25365033.
Study: Trends in Autism Prevalence: Diagnostic Substitution Revisited
There has been little evidence to support the hypothesis that diagnostic substitution may contribute to increases in the administrative prevalence of autism. We examined trends in assignment of special education codes to British Columbia (BC) school children who had an autism code in at least 1 year between 1996 and 2004, inclusive. The proportion of children with an autism code increased from 12.3/10,000 in 1996 to 43.1/10,000 in 2004; 51.9% of this increase was attributable to children switching from another special education classification to autism (16.0/10,000). Taking into account the reverse situation (children with an autism code switching to another special education category (5.9/10.000)), diagnostic substitution accounted for at least one-third of the increase in autism prevalence over the study period.
Reference:
- Coo, H., Ouellette-Kuntz, H., Lloyd, J.E.V. et al. Trends in Autism Prevalence: Diagnostic Substitution Revisited. J Autism Dev Disord 38, 1036–1046 (2008). https://doi.org/10.1007/s10803-007-0478-x
Study: Gender Dysphoria Report edit
Executive Summary
Part I: Background
- Gender dysphoria is a condition that involves distress regarding one’s sexed body and/or associated social expectations. Increasing numbers of children and adolescents in the U.S. and other countries are diagnosed with gender dysphoria. Internationally, there is intense disagreement about how best to help them.
- The term “rapid onset gender dysphoria” (ROGD) has been suggested to describe a new clinical presentation of gender dysphoria. Despite sharp disagreement about the concept’s validity, symptoms consistent with ROGD have been recorded in clinics in the U.S. and other countries.
- In the U.S., the current approach to treating pediatric gender dysphoria aligns with the “gender-affirming” model of care recommended by the World Professional Association for Transgender Health (WPATH). This model emphasizes the use of puberty blockers and cross-sex hormones, as well as surgeries, and casts suspicion on psychotherapeutic approaches for management of gender dysphoria.
- The understandable desire to avoid language that may cause discomfort to patients has, in some cases, given rise to modes of communication that lack scientific grounding, that presuppose answers to unresolved ethical controversies, and that risk misleading patients and families. This Review uses scientifically accurate and neutral terminology throughout.
- In many areas of medicine, treatments are first established as safe and effective in adults before being extended to pediatric populations. In this case, however, the opposite occurred: clinician-researchers developed the pediatric medical transition protocol in response to disappointing psychosocial outcomes in adults who underwent medical transition.
- The protocols were adopted internationally before the publication of the first outcome studies. In recent years, in response to dramatic shifts in the number and clinical profiles of minor patients, as well as to multiple systematic reviews of evidence, health authorities in an increasing number of countries have restricted access to puberty blockers and cross-sex hormones, and, in the rare cases where they were offered, surgeries for minors. These authorities now recommend psychosocial approaches, rather than hormonal or surgical interventions, as the primary treatment, and in some cases have restricted the latter to nationallyoverseen research protocols.
- There is currently no international consensus about best practices for the care of children and adolescents with gender dysphoria.
Part II: Evidence Review
- Evidence-based medicine is widely recognized by health authorities worldwide as the foundation of high-quality care. Consistent with its principles, this Review undertook a methodologically rigorous assessment of the evidence underpinning pediatric gender medicine.
- Specifically, this Review conducted an overview of systematic reviews—also known as an “umbrella review”—to evaluate the direct evidence regarding the benefits and harms of treatment for children and adolescents with gender dysphoria. Existing systematic reviews of evidence, including several that have informed health authorities in Europe, were assessed for methodological quality. The umbrella review found that the overall quality of evidence concerning the effects of any intervention on psychological outcomes, quality of life, regret, or long-term health, is very low. This indicates that the beneficial effects reported in the literature are likely to differ substantially from the true effects of the interventions.
- Evidence for harms associated with pediatric medical transition in systematic reviews is also sparse, but this finding should be interpreted with caution. Inadequate harm detection in pediatric gender medicine may reflect the relatively short period of time since the widespread adoption of the medical/surgical treatment model; the failure of existing studies to systematically track and report harms; and publication bias. Despite the lack of robust evidence from population level studies, important insights can be drawn from established knowledge about human physiology and the effects and mechanisms of the pharmacological agents used.
- The risks of pediatric medical transition include infertility/sterility, sexual dysfunction, impaired bone density accrual, adverse cognitive impacts, cardiovascular disease and metabolic disorders, psychiatric disorders, surgical complications, and regret.
Part III: Clinical Realities
- In the U.S., the most influential clinical guidelines for the treatment of pediatric gender dysphoria are published by WPATH and the Endocrine Society. A recent systematic review of international guideline quality did not recommend either guideline for clinical use after determining they “lack developmental rigour and transparency.”
- Problems with the development of WPATH’s Standards of Care, Version 8 (SOC8) extend beyond those identified in the systematic review of international guidelines. In the process of developing SOC-8, WPATH suppressed systematic reviews its leaders believed would undermine its favored treatment approach. SOC-8 developers also violated conflict of interest management requirements and eliminated nearly all recommended age minimums for medical and surgical interventions in response to political pressures.
- Although SOC-8 relaxed the eligibility criteria for access to puberty blockers, cross-sex hormones, and surgeries, there is compelling evidence that U.S. gender clinics are not adhering even to those more permissive criteria.
- The “gender-affirming” model of care, as practiced in U.S. clinics, is characterized by a child-led process in which comprehensive mental health assessments are often minimized or omitted, and the patient’s “embodiment goals” serve as the primary guide for treatment decisions. In some of the nation’s leading pediatric gender clinics, assessments are conducted in a single session lasting two hours.
- The voices of whistleblowers and detransitioners have played a critical role in drawing public attention to the risks and harms associated with pediatric medical transition. Their concerns have been discounted, dismissed, or ignored by prominent advocates and practitioners of pediatric medical transition.
- U.S. medical associations played a key role in creating a perception that there is professional consensus in support of pediatric medical transition. This apparent consensus, however, is driven primarily by a small number of specialized committees, influenced by WPATH. It is not clear that the official views of these associations are shared by the wider medical community, or even by most of their members. There is evidence that some medical and mental health associations have suppressed dissent and stifled debate about this issue among their members.
Part IV: Ethical Considerations
- The principle of autonomy in medicine establishes a moral and legal right of competent patients to refuse any medical intervention. However, there is no corollary right to receive interventions that are not beneficial. Respect for patient autonomy does not negate clinicians’ professional and ethical obligation to protect and promote their patients’ health.
- The evidence for benefit of pediatric medical transition is very uncertain, while the evidence for harm is less uncertain. When medical interventions pose unnecessary, disproportionate risks of harm, healthcare providers should refuse to offer them even when they are preferred, requested, or demanded by patients. Failure to do so increases the risk of iatrogenic harm and reduces medicine to consumerism, threatening the integrity of the profession and undermining trust in medical authority.
- Proponents of pediatric medical transition claim that regret is vanishingly rare, while critics assert that regret is increasingly common. The true rate of regret is not known and better data collection is needed. That some patients report profound regret after undergoing invasive, life-changing medical interventions is clearly of importance. However, regret alone (just like satisfaction alone) is not a valid indicator of whether an intervention is medically justified. Patients may regret medically justified treatments or feel satisfied with unjustified ones.
- A natural response to the absence of credible evidence is to call for more and better research. Even if high quality research such as randomized controlled trials on pubertal suppression or hormone therapy were feasible, however, conducting it may conflict with well-established ethical standards for human subjects research.
Part V: Psychotherapy
- The rise in youth gender dysphoria and the corresponding demand for medical interventions have occurred against the backdrop of a broader mental health crisis affecting adolescents. The relationship between these two phenomena remains a subject of scientific controversy.
- Suicidal ideation and behavior are independently associated with comorbidities common among children and adolescents diagnosed with gender dysphoria. Suicidal ideation and behavior have known psychotherapeutic management strategies. No independent association between gender dysphoria and suicidality has been found, and there is no evidence that pediatric medical transition reduces the incidence of suicide, which remains, fortunately, very low.
- There is a dearth of research on psychotherapeutic approaches to managing gender dysphoria in children and adolescents. This is due in part to the mischaracterization of such approaches as “conversion therapy.” A more robust evidence base supports psychotherapeutic approaches to managing common comorbid mental health conditions. Psychotherapy is a noninvasive alternative to endocrine and surgical interventions for the treatment of pediatric gender dysphoria. Systematic reviews of evidence have found no evidence of adverse effects of psychotherapy in this context.
Reference:
- Treatment for Pediatric Gender Dysphoria: Review of Evidence and Best Practices is a report by the U.S. Department of Health and Human Services. Published November 2025. All materials are peer-reviewed except for the Errata. The May 15, 2025 versions of these documents are superseded by the November 19, 2025 versions.
- Liberals Should Read the HHS Review of Pediatric ‘Gender Affirming’ Care | Opinion - Newsweek
Study: Mapping the genetic landscape across 14 psychiatric disorders
Notes:
- Five genetic factors explained about two-thirds of the genetic risk for individual psychiatric diagnoses. 5 major genetic factors:
- Schizophrenia–Bipolar factor
- Schizophrenia and bipolar disorder are genetically very similar.
- There are very few genes that clearly separate them.
- Internalizing factor
- Major depression, anxiety disorders, and PTSD.
- These share extensive genetic overlap and differ very little at the genetic level.
- Neurodevelopmental factor
- Autism, ADHD, and (to a degree) Tourette’s.
- Strongly tied to early brain development.
- Compulsive disorders factor
- Anorexia and OCD (with some overlap from Tourette’s and anxiety).
- Substance-use factor
- Alcohol, opioid, cannabis, and nicotine dependence.
- ADHD partially overlaps here.
- Schizophrenia–Bipolar factor
- Above those five groups, the researchers found a general genetic vulnerability to mental illness overall—sometimes called a "p-factor."
- This general risk is strongly linked to traits like:
- High emotional sensitivity
- Neuroticism
- Stress reactivity
- Loneliness
- Self-harm and suicide risk
- This general risk is strongly linked to traits like:
Abstract: Psychiatric disorders display high levels of comorbidity and genetic overlap challenging current diagnostic boundaries. For disorders for which diagnostic separation has been most debated, such as schizophrenia and bipolar disorder, genomic methods have revealed that the majority of genetic signal is shared. While over a hundred pleiotropic loci have been identified by recent cross-disorder analyses, the full scope of shared and disorder-specific genetic influences remains poorly defined. Here we addressed this gap by triangulating across a suite of cutting-edge statistical and functional genomic analyses applied to 14 childhood- and adult-onset psychiatric disorders (1,056,201 cases).
Using genetic association data from common variants, we identified and characterized five underlying genomic factors that explained the majority of the genetic variance of the individual disorders (around 66% on average) and were associated with 238 pleiotropic loci.
- The two factors defined by (1) Schizophrenia and bipolar disorders (SB factor); and (2) major depression, PTSD and anxiety (Internalizing factor) showed high levels of polygenic overlap6 and local genetic correlation and very few disorder-specific loci.
- The genetic signal shared across all 14 disorders was enriched for broad biological processes (for example, transcriptional regulation), while more specific pathways were shared at the level of the individual factors. The shared genetic signal across the SB factor was substantially enriched in genes expressed in excitatory neurons, whereas the Internalizing factor was associated with oligodendrocyte biology.
These observations may inform a more neurobiologically valid psychiatric nosology and implicate targets for therapeutic development designed to treat commonly occurring comorbid presentations.
Reference:
- Grotzinger, A.D., Werme, J., Peyrot, W.J. et al. Mapping the genetic landscape across 14 psychiatric disorders. Nature (2025). https://doi.org/10.1038/s41586-025-09820-3
Study: Exposing Worry’s Deceit: Percentage of Untrue Worries in Generalized Anxiety Disorder Treatment
Highlights
- 91.4% of worries did not come true for those with GAD (Mode = 100%).
- Higher untrue worry percentages predicted greater GAD symptom reduction in therapy.
- Attending to untrue worry percentages may be facilitate successful GAD treatment.
Theories of cognitive therapy have long proposed that those with generalized anxiety disorder (GAD) have inaccurate expectations. By challenging them with objective evidence, symptoms are thought to decrease.
To test these premises, this study used ecological momentary assessment (EMA) during the Worry Outcome Journal (WOJ) treatment to determine the percentage of GAD worries that did not come true.
We then analyzed the association between participants’ untrue worry percentages and GAD symptom change across treatment.
Twenty-nine participants with GAD recorded worries when prompted for 10 days, reviewed them online nightly, and tracked their worry outcomes across 30 days. These recordings were then coded by independent raters. Analyses applied bias-correct bootstrapping path analysis on slopes extracted from longitudinal linear mixed models.
Primary results revealed that 91.4% of worry predictions did not come true.
Higher percentages of untrue worries significantly predicted lower GAD symptoms after treatment, as well as a greater slope of symptom reduction from pre- to post-trial.
Participants’ average expected likelihoods of worries coming true were much greater than actual observed likelihoods.
The most common percentage of untrue worries per person was 100%. Thus, worries in those with GAD were mostly inaccurate.
Greater evidence of this inaccuracy predicted greater improvement in treatment. As theorized, disconfirming false expectations may significantly contribute to treatment’s effect.
Reference:
- Lucas S. LaFreniere, Michelle G. Newman, Exposing Worry’s Deceit: Percentage of Untrue Worries in Generalized Anxiety Disorder Treatment, Behavior Therapy, Volume 51, Issue 3, 2020, Pages 413-423, ISSN 0005-7894, https://doi.org/10.1016/j.beth.2019.07.003. (https://www.sciencedirect.com/science/article/pii/S0005789419300826)
Pulmonary
Asthma
Asthma Medications:
- Long-term control medications: Prevent symptoms and are taken daily
- Inhaled Corticosteroids (Including Combination Inhalers): The most consistently effective long-term control medication.
- Long-Acting Beta-Agonists (LABAs): These are used in combination with inhaled corticosteroids.
- Anticholinergics: Used as alternative controller medications.
- Cromolyn, Theophylline and Phosphodiesterase Inhibitors: Used as alternative controller medications (not preferred).
- Leukotriene Modifiers: Used as alternative controller medications.
- Immunomodulators: Monoclonal antibodies modify the allergic immune response.
- Quick-relief medications: Take only as needed for symptom relief
- Short-Acting Beta-Agonists (SABAs): relax airway muscles to give prompt relief of symptoms.
Diagnosis:
- Presence of episodic symptoms of airflow obstruction or airway hyperresponsiveness
- Objective assessment of one of the following:
- Airflow obstruction that is at least partially reversible with the use of an inhaled short-acting B-agonist as shown by one of these 3:
- Increase in FEV1 of 12% or more from baseline
- Increase in predicted FEV1 of 10% or more from baseline
- Increase in PEF of 20% or more from baseline
- Diurnal variation in PEF of more than 10%
- Airflow obstruction that is at least partially reversible with the use of an inhaled short-acting B-agonist as shown by one of these 3:
Treatment choice for mild asthma for >5yo: After establishment of Dx
- If coexisting rhinitis -> start Leukotriene receptor antagonist (LTRA)
- Can add low dose inhaled glucocorticoid if not controlled on re-evaluation
- If no rhinitis -> Start low dose inhaled glucocorticoid
- Can add LABA or LTRA if not controlled on re-evaluation
National Heart, Lung, Blood Institute Guidelines
Children 0-4yo
| Step 1 | Step 2 | Step 3 | Step 4 | Step 5 | Step 6 |
|---|---|---|---|---|---|
| SABA prn | Low-dose ICS | Med-dose ICS | Med-dose ICS | High-dose ICS | High-dose ICS |
| + | + | + | |||
| (Alt: | LABA or montelukast | LABA or montelukast | LABA or montelukast | ||
| Cromolyn or | + | ||||
| montelukast) | Oral corticosteroids |
Children 5-11yo
| Step 1 | Step 2 | Step 3 | Step 4 | Step 5 | Step 6 |
|---|---|---|---|---|---|
| SABA prn | Low-dose ICS | Low-dose ICS | Med-dose ICS | High-dose ICS | High-dose ICS |
| + | + | + | + | ||
| (Alt: | LABA, LTRA, or | LABA | LABA | LABA | |
| Cromolyn, LTRA, | theophylline | + | |||
| nedocromil, or | OR | (Alt: | (Alt: | Oral corticosteroids | |
| thophylline) | Med-dose ICS | Med-dose ICS | High-dose ICS | ||
| + | + | (Alt: | |||
| LTRA or | LTRA or | High-dose ICS | |||
| theophylline) | theophylline | + | |||
| LTRA or | |||||
| theophylline | |||||
| + | |||||
| Oral corticosteroids |
Children >12yo and Adults
| Step 1 | Step 2 | Step 3 | Step 4 | Step 5 | Step 6 |
|---|---|---|---|---|---|
| SABA prn | Low-dose ICS | Low-dose ICS | Med-dose ICS | High-dose ICS | High-dose ICS |
| + | + | + | + | ||
| (Alt: | LABA | LABA | LABA | LABA | |
| Cromolyn, LTRA, | OR | + | + | ||
| nedocromil, or | Med-dose ICS | (Alt: | Consider | Oral corticosteroids | |
| theophylline) | Med-dose ICS | omalizumab | + | ||
| (Alt: | + | for those with | Consider | ||
| Low-dose ICS | LTRA, zileuton, | allergies | omalizumab | ||
| + | or theophylline) | for those with | |||
| LTRA, theophylline, | allergies (IgE > 30 IU/ml) | ||||
| or zileuton) |
ICS: inhaled corticosteroid (fluticasone, budesonide, ciclesonide, mometasone) LABA: Long-acting beta-agonist (formoterol or salmeterol) LTRA: Leukotriene receptor antagonist (montelukast) SABA: Short-acting beta-agonist (albuterol) LAMA: Long-acting Muscarinic antagonist (like tiotropium)
Asthma Steps:
- Step 1: Mild Asthma
- Symptoms are mild and infrequent
- Peak expiratory flow (PEF) is above 80% of personal best
- No nighttime awakenings or morning symptoms
- No use of quick-relief medications
- Treatment:
- Inhaled corticosteroids (ICS) at a low dose
- As-needed use of short-acting beta2 agonists (SABA)
- Step 2: Mild Persistent Asthma
- Symptoms are mild and frequent
- PEF is 60-79% of personal best
- Some nighttime awakenings or morning symptoms
- Some use of quick-relief medications
- Treatment:
- ICS at a medium dose
- As-needed use of SABA
- Consider adding a long-acting beta2 agonist (LABA)
- Step 3: Moderate Persistent Asthma
- Symptoms are moderate and frequent
- PEF is 40-59% of personal best
- Frequent nighttime awakenings or morning symptoms
- Frequent use of quick-relief medications
- Treatment:
- ICS at a high dose
- LABA added to ICS
- As-needed use of SABA
- Consider adding an oral corticosteroid
- Step 4: Severe Persistent Asthma
- Symptoms are severe and frequent
- PEF is below 40% of personal best
- Frequent nighttime awakenings or morning symptoms
- Frequent use of quick-relief medications
- Treatment:
- High-dose ICS
- LABA and SABA as needed
- Oral corticosteroids as needed
- Consider adding other medications, such as a leukotriene modifier or a theophylline
- Step 5: Severe Asthma
- Symptoms are severe and life-threatening
- PEF is below 20% of personal best
- Frequent nighttime awakenings or morning symptoms
- Frequent use of quick-relief medications
- Treatment:
- High-dose ICS
- LABA and SABA as needed
- Oral corticosteroids as needed
- Hospitalization may be necessary
Inhaled Corticosteroids: Are considered the most effective long-term usage medication for control and management of asthma
- Beclomethasone Dipropionate
- Budesonide
- Ciclesonide
- Fluticasone Furoate
- Fluticasone Propionate
- Mometasone
- Mometasone Furoate HFA 100 or 200 mcg
References:
- AFP Vol 79 No 9 May 2009
- JFP Vol 66 No 5 May 2017
- NEJM Aug 8, 2013 369;6
- JAMA Dec 2020 Vol 324 No 22
- AFP Apr 2023 Vol 107 No 4
- Asthma Steps (Old):
Asthma Steps (Old):
- Step 1 (Intermittent Asthma)
- albuterol prn
- Preferred: low dose ICS plus formoterol as needed
- Step 2 (Persistent asthma)
- Daily low dose ICS
- SABA prn
- Alternative:
- Daily LTRA and SABA prn
- Step 3
- Daily combination low dose ICS-formoterol
- Alternative:
- Daily medium dose ICS and SABA prn
- Step 4
- Daily medium dose ICS-formoterol
- Alternative:
- Daily medium dose ICS and LAMA
- Step 5
- Daily medium to high dose ICS-LABA + LAMA and SABA prn
- Step 6
- Daily high dose ICS-LABA + oral systemic corticosteroids + SABA prn
- Step 1 (Intermittent Asthma)
Asthma Severity
| Intermittent | Mild Persistent | Moderate Persistent | Severe Persistent | |
|---|---|---|---|---|
| Symptoms | 2 or less days per week | More than 2 days per week | Daily | Throughout the day |
| Nighttime Awakenings | 2 x's per month or less | 3-4 times per month | More than once per week but not nightly | Nightly |
| Rescue Inhale Use | 2 or less days per week | More than 2 days per week but not daily | Daily | Several times per day |
| Interference with normal activity | None | Minor limitation | Some limitation | Extremely limited |
| Lung Function | FEV1 > 80% predicted and normal between exacerbations | FEV1 >80% predicted | FEV1 60-80% predicted | FEV1 less than 60% predicted |
Asthma Exacerbations
Single maintenance and reliever therapy (SMART) is preferred
- ICS/LABA recommended by guidelines - formoterol preferred LABA
| Severity | Symptoms | FEV1 |
|---|---|---|
| Mile | Dyspnea only with activity | >70% predicted or personal best |
| Moderate | Dyspnea interferes with or limits usual activity | 40-69% |
| Severe | Dyspnea at rest; interferes with conversation | <40% |
| Life-threatening | Dyspnea prevents patient from speaking; Perspiration | <25% |
Reference:
- AFP Vol 109 No 1 Jan 2024
Differential Diagnosis of Asthma
Differential:
- Upper respiratory tract
- Vocal cord dysfunction
- Congestive rhinopathy
- Postnasal drip
- Obstructive sleep apnea syndrome
- Tracheobronchomalacia
- Lower respiratory tract
- Chronic obstructive pulmonary disease
- Occupational bronchitis
- Cystic fibrosis
- Bronchiectasis
- Pneumonia
- Gastrointestinal tract
- Gastroesophageal reflux disease
- Cardiovascular system
- Congestive heart failure
- Pulmonary hypertension
- Chronic thromboempolic pulmonary disease
- Central nervous system
- Habitual cough
- Other
- Cough induced by angiotensin-converting enzyme inhibitor use
- Deconditioning
- Obesity
References:
- JAMA Vol 318 No 3 Jul 2017
- AFP Col 103 No 5 Mar 2021
Low Cost Management
With GoodRx
Rescue Inhaler:
- Albuterol 8.5g of 90 mcg 1 HFA: $18.27 at Community Walgreens and Winn-Dixie
Inhaled corticosteroids:
- Budesonide nebulized solution (1 carton of 30 ampules of 0.5mg/2ml): $35.96 at Winn-Dixie
Inhaled Corticosteroid/LABA:
- Fluticasone/salmeterol (1 respiclick inhaler, 0.45g of 55mcg/14mcg): $36.88 at CVS, $51.14 at Walgreens
- Fluticasone/salmeterol (1 respiclick inhaler, 0.45g of 113 mcg/14 mcg): $31.38 at CVS, $49.63 at Walgreens
- Fluticasone/salmeterol (1 respiclick inhaler, 0.45g of 232mcg/14mcg): $31.38 at CVS, $49.63 at Walgreens
—
- Initiation of therapy
- When treatment is started, during periods of severe asthma and while reducing or discontinuing oral glucocorticosteroids, the recommended dose of Budesonide Nebuliser Suspension is:
- Adults (including the elderly)
- Usually 1 - 2 mg twice daily. In very severe cases the dosage may be increased further.
- Pediatric population
- Children 12 years and older: Dosage as for adults.
- Children 3 months to 12 years: 0.5 – 1 mg twice daily.
- Maintenance
- The maintenance dose should be individualised and be the lowest dose which keeps the patient symptom-free.
- Adults (including the elderly and children 12 years and older)
- 0.5 - 1mg twice daily.
- Pediatric population
- Children 3 months to 12 years: 0.25 - 0.5 mg twice daily.
Cough Variant Asthma
"Cold air" and/or "talking" as cough triggers, a sign for the diagnosis of cough variant asthma
When the analysis was confined to those with a low FeNO (<22ppb) group, the sensitivity and positive predictive values of "cold air" and "talking" for the diagnosis of CVA were:
| Sensitivity | Specificity | Positive Predictive Value | |
|---|---|---|---|
| Cold Air | 36% | 81% | 70% |
| Talking | 44% | 81% | 74% |
References:
- Kanemitsu Y, Matsumoto H, Osman N, Oguma T, Nagasaki T, Izuhara Y, Ito I, Tajiri T, Iwata T, Niimi A, Mishima M. "Cold air" and/or "talking" as cough triggers, a sign for the diagnosis of cough variant asthma. Respir Investig. 2016 Nov;54(6):413-418. doi: 10.1016/j.resinv.2016.07.002. Epub 2016 Aug 24. PMID: 27886852.
Chronic Cough
A chronic cough is a cough that lasts eight weeks or longer in adults, or four weeks in children.
Top causes:
- Postnasal drip
- Treatment:
- Nonprescription decongestant or antihistamine tablets are the first step.
- Inhaling steam from a hot shower or kettle
- Nasal irrigations may also help by cleaning out irritating secretions
- Home version: First, soak a clean washcloth in a basin containing 1/8 teaspoon of table salt for each cup of water. Next, hold the dripping wet cloth up to your nostrils and sniff in the saline solution. If saline irrigations seem to help, repeat them one to three times per day.
- Treatment:
- Asthma
- Excessive mucus production, shortness of breath, and cough are the other classic symptoms of asthma. But in cough-variant asthma, coughing is the only symptom.
- Cough-variant asthma produces a persistent, dry cough that occurs around the clock but may begin at night. Exposure to allergens, dust, or cold air often triggers coughing, as does exercise.
- Gastroesophageal reflux disease (GERD)
- Avoid alcohol and foods that often trigger GERD, including those that contain chocolate, peppermint, caffeine, garlic, onions, citrus fruits, tomato sauce, or lots of fat.
- Eat small meals, and never lie down until two hours after you've eaten.
- Take liquid antacids, particularly at bedtime, and consider elevating the head of your bed or sleeping on a wedge-shaped pillow to keep your stomach's contents flowing down at night.
- Chronic bronchitis
- The most effective treatment is to quit smoking and avoid air pollutants.
- In addition, your doctor can prescribe a corticosteroid inhaler, usually with a long-acting bronchodilator
- Treatment with ACE inhibitors, used for high blood pressure
Less common causes of a nagging cough
- Airborne environmental irritants
- Aspiration during swallowing
- Heart failure
- Lung infections
- Pertussis (whooping cough)
- Lung cancer
- Other lung diseases
- Psychological disorders
- Cystic fibrosis
- Nonasthmatic eosinophilic bronchitis (airway inflammation not caused by asthma)
- Sarcoidosis (collections of inflammatory cells in different parts of your body, most commonly the lungs)
- Idiopathic pulmonary fibrosis (chronic scarring of the lungs due to an unknown cause)
Common in smokers
- Tobacco smoke itself
- Lung cancer
- Lung infections
Etiologies in Adults
| Most Common | Less Common | Least Common |
|---|---|---|
| ACE I use | Bronciectasis | Arteriovenous malformation |
| Asthma | COPD | Bronchiolitis |
| Environmental triggers | OSA | Bronchogenic carcinoma |
| GERD/LPR | Pertusis | Chronic aspiration |
| Nonasthmatic eosinophilic bronchitis | Postinfectious bronchospasm | Chronic interstitial lung disease |
| Tobacco use | Irritation of external auditory canal | |
| Upper airway cough syndrome | Persistent pneumonia | |
| Psychogenic cough | ||
| Sarcoidosis | ||
| Tuberculosis |
Etiologies in Children
| Most Common | Less Common | Least Common |
|---|---|---|
| Asthma | Environmental triggers | Chronic aspiration |
| Protracted bacterial bronchitis | Foreign body | Congenital abnormality |
| Upper airway cough syndrome (>6yo) | GERD | Cystic fibrosis |
| Pertusis | Immunodeficiency | |
| Postinfectious bronchospasm | Primary ciliary dyskinesia | |
| Psychogenic cough | ||
| Tourette sydrome/tic |
Suggested etiologies
- Wheezing on exam
- Intrathoracic airway lesions (asthma, tracheomalacia)
- Crepitations on exam
- Airway lesions (from secretions)
- Parenchymal disease (interstitial disease)
- Cardiac abnormalities
- Assosicated airway abnormalities
- Cardiac failure
- Chest pain
- Arrythmia
- Asthma
- Chest wall deformity
- Pulmonary airway
- Parenchymal disease
- Daily moist or productive cough
- Suppurative lung disease
- Digital clubbing
- Suppurative lung disease
- Dyspnea or tachypnea
- Pulmonary airway
- Parenchymal disease
- Exertional dyspnea
- Pulmonary airway
- Parenchymal disease
- Failure to thrive
- Serious systemic illness
- Feeding difficulties
- Aspiration
- Serious systemic illness
- Hemoptysis
- Suppurative lung disease
- Vascular abnormalities
- Hypoxia/cyanosis
- Pulmonary airway
- Parenchymal disease
- Cardiac disease
- Immunodeficiency
- Atypical infection
- Suppurative lung disease
- Neurodevelopmental abnormality
- Aspiration lung disease
- Recurrent pneumonia
- Atypical infection
- Congenital lung abnormality
- Immunodeficiency
- Suppurative lung disease
- Tracheoesophageal fistula
References:
- AFP Vol 96 No 9 Nov 2017
COPD
- All patients with COPD should be screened 1 time for a1-antitrypsin deficiency
- Adult Immunizations
- Influenza
- COVID-19
- PCV
- Pertussis vaccination
Classification:
- In pts with FEV1/FVC <70%
- GOLD 1 (mild): FEV1 >80% predicted
- GOLD 2 (mod): FEV1 50-79% predicted
- GOLD 3 (severe): FEV1 30-49% predicted
- GOLD 4 (very severe): FEV1 <30% predicted
Diagnosis:
- Post-bronchodilator Spirometry FEV1/FVC < 0.7
Modified Medical Research Council Dyspnea Scale (mMRC)
| Score | Description |
|---|---|
| 0 | I get breathless with strenuous exercise |
| 1 | I get SOB when hurrying on level ground or walking up a slight hill |
| 2 | On level ground, I walk slower than other people my age because of breathlessness, or I have to stop for breath walking at my pace |
| 3 | I stop for breath after walking 100m or after a few min on level ground |
| 4 | I am too breathless to leave the house, or I am breathless when dressing |
Combined assessment of COPD:
| Group | Char | Spirom Class | Exacerbations/yr | mMRC |
|---|---|---|---|---|
| A | Low risk | GOLD 1 or 2 | 0-1 | 0 or 1 |
| B | Low risk | GOLD 1 or 2 | 0-1 | 2+ |
| E | High risk | 2+ | 2+ or 1 admission | |
| High risk | GOLD 3 or 4 | 2+ | 0 or 1 | |
| High risk | GOLD 3 or 4 | 2+ | 2+ |
Treatment:
- ACP/ACCP/ATS/ERS Guidelines
- FEV1 = 60%-80% predicted: inhaled bronchodilators may be used
- FEV1 <60% predicted: long-acting anticholinergic or long-acting beta2 agonist recommended; combination therapy may be used
- Global Initiative for COPD 2023
- Group A: Long-acting anticholinergic (tiotropium) or long-acting B2 agonist (salmeterol, formoterol, aformoterol)
- LAMA
Old: Short-acting anticholinergics (ipratropium) or short-acting B2-agonist (albuterol, levalbuterol) as needed
- Group B: Long-acting anticholinergic (tiotropium) and long-acting B2 agonist (salmeterol, formoterol, aformoterol)
- LAMA/LABA
- Group E (Group C or D): Long-acting anticholinergic (LAMA) and combination of long-acting beta2 agonist plus inhaled corticosteroid (fluticasone, mometasone, budesonide, flunisolide)
- LABA + LAMA
- LAMA/LABA/ICS If blood eosinophils >= 300
- Group A: Long-acting anticholinergic (tiotropium) or long-acting B2 agonist (salmeterol, formoterol, aformoterol)
Medication Management:
- LAMA (like tiotropium) > LABA
- LAMA/LABA
- SAMA/SABA
- Try not to use: LAMA/LABA/ICS
Alpha-1 antitrypsin deficiency (AATD) screening. The World Health Organization recommends that all patients with a diagnosis of COPD should be screened once especially in areas with high AATD prevalence.33,34 A low concentration (< 20% normal) is highly suggestive of homozygous deficiency. Family members should also be screened.
References:
- Various
- AFP Vol 107 No 6 Jun 2023
- JFP Supp Vol 72 no 6 Jul 2023
Dyspnea
Management of Oropharyngeal Dysphagia
Diet modifications
- Mindful eating
- Avoiding foods likely to cause dysphagia
- Chewing carefully
- Cutting food into smaller pieces
- Drinking liquids to dilute food bolus
- Eating slowly Lubricating with sauces
- Taking smaller bites
- Mechanical soft diet to compensate for impaired chewing due to weakness or poor dentition
- Modified consistency diet to compensate for impaired swallowing (thickened food and liquids with increased viscosity and cohesiveness slow transport speed)
- Pureed diet to compensate for impaired chewing due to weakness, poor dentition, or dry mouth with impaired bolus formation
- Tasting diet
- Patient-centered approaches to feeding and environments conducive to eating should be part of usual care for all older adults with chronic debilitating illness
Swallowing rehabilitation
- Muscular reconditioning exercises to strengthen jaw, lips, and tongue
- In clinically stable patients who have potential for improvement (e.g., after a stroke), the goal is long-term change in control of swallowing via neuroplasticity
- In patients with progressive conditions (e.g., Parkinson disease), the goal is maintaining current swallowing status as long as possible
- Compensatory safe-swallow techniques (positioning to compensate for weakness and dysfunction)
- Eating upright
- Chin-tuck maneuver for patients with stroke or degenerative disease changes pharyngeal dimensions to direct the food bolus toward the pharynx and esophagus, compensates for delay of glottic closure, and reduces aspiration risk during swallowing
- Head-turn maneuver for patients with unilateral weakness (turning head toward weaker side) uses gravity to push the bolus toward the stronger side
Enteral feeding
- Nasogastric tube feeding: typically placed during the first week after stroke to allow for administration of nutrition and medication
- Percutaneous endoscopic gastronomy: used longer term if dysphagia persists after the first week; best for patients with some degree of rehabilitation potential; does not improve mortality or reduce aspiration risk
References:
- Am Fam Physician. 2021 Jan 15;103(2):97-106.
Epworth Sleepiness Scale
Rate how likely you are to doze off or fall asleep in the following situations:
- 0 = Would never doze
- 1 = Slight chance of dozing
- 2 = Moderate chance of dozing
- 3 = High chance of dozing
Situations:
- Sitting and reading
- Sitting, inactive in a public place (meeting or theatre)
- Watching TV
- As a passenger in a car for an hour without a break
- Lying down to rest in the afternoon when circumstances permit
- Sitting and talking to someone
- Sitting quietly after lunch without alcohol
- In a car, while stopped for a few minutes in the traffic
Sn=50-54%; Sp=67%
Incidental Pulmonary Nodules detected on CT Images
- Solid nodules <6mm
- Do not require routine follow-up in low-risk patients (1C)
- Pure ground-glass noduels <6mm
- No routine follow-up is recommended (1B)
- Solid nodules <6mm with suspicious morphology, upper lobe location, or pose higher risk
- Follow-up at 12 months (2A)
- Solitary solid noncalcified nodules (6-8mm) in patients of high-risk
- Initial follow-up examination recommended at 6 to 12 mo and again at 18-24 mo (1B)
- Solitary solid noncalcified nodules >8mm in diameter
- Consider 3-month follow-up
- Workup with PET and CT, tissue sampling, or combination (1A)
References:
- JAMA Vol 320 No 21 Dec 2018
Lung Ca Screening
Low dose CT Screening:
- Decreases deaths in people 40yo+ with ARR of 0.4% and NNT of 226 over 8.8 years to prevent 1 death.
- NNH 44 - overdiagnosis and false-positives
Reference:
- Cochrane May 2023
Pneumonia
Criteria to transition CAP from IV to PO Abx
- Able to ingest oral agents
- Heart rate <100 bpm and SBP >90 mmHg
- O2 sat >90%, Arterial O2 partial pressure >60mmHg on room air or low flow NC, or return to baseline
- Respiratory rate <25 breaths/min
- Return to baseline cognitive status
- Temperature <100.9F (38.3C)
Reference:
- AFP Vol 94 No 9 Nov 2016
Predicted Peak Expiratory Flow (L/min)
Men:
| Age | 60" | 65" | 70" | 75" | 80" |
|---|---|---|---|---|---|
| 20 | 554 | 602 | 649 | 693 | 740 |
| 30 | 532 | 577 | 622 | 664 | 710 |
| 40 | 509 | 552 | 596 | 636 | 680 |
| 50 | 486 | 527 | 569 | 607 | 649 |
| 60 | 463 | 502 | 542 | 578 | 618 |
| 70 | 440 | 477 | 515 | 550 | 587 |
Women:
| Age | 55" | 60" | 65" | 70" | 75" |
|---|---|---|---|---|---|
| 20 | 390 | 423 | 460 | 496 | 529 |
| 30 | 380 | 413 | 448 | 483 | 516 |
| 40 | 370 | 402 | 436 | 470 | 502 |
| 50 | 360 | 391 | 424 | 457 | 488 |
| 60 | 350 | 380 | 412 | 445 | 475 |
| 70 | 340 | 369 | 400 | 432 | 461 |
Calculation Formula:
- PEFR, children = [(Height in cm - 100) × 5] + 100
- PEFR, adult men = {[(Height in m × 5.48) + 1.58] - [Age × 0.041]} × 60
- PEFR, adult women = {[(Height in m × 3.72) + 2.24] - [Age × 0.03]} × 60
References:
- Am Rev Respir Dis. 1963 Nov;88:644-51
Pulmonary Function Tests
- Restrictive lung disesases (reduced FVC and normal FEV1/FVC)
- diminished lung parenchyma compliance
- pleural disase
- fibrosis
- conditions affecting chest wall expansion
- Obstructive disease (reduced FEV1 and increased FVC)
- Asthma
- Mixed (FVC and FEV1/FVC reduced)
- Requires further pulmonary testing
Additional Pulmonary Function Tests
- The 6-minute walk test
- Used to evaluate the treatment response for known cardiopulmonary disease
- Bronchoprovocation testing
- Identifes asthma triggered by allergens or exercise when office spirometry is normal
- Bronchoscopy
- Ventilation-perfusion scan
- May be used in the evaluation for suspected pulmonary embolus, but it is not the preferred diagnostic test in the evaluation of chronic dyspnea in a patient with normal vital signs
Pulmonary Nodules
Solitary Pulmonary Nodules
80% nodules >20mm are malignant 1% nodules between 2-5mm are malignant
Etiologies:
| Benign | Malignant |
|---|---|
| Infectious granuloma (80%) | Adenocarcinoma (60%) |
| - Atypical mycobacteria | Squamous cell ca (20%) |
| - Coccidiomycosis | Solitary metastasis (10%) |
| - Histoplasmosis | - Breast |
| - M tuberculosis | - Colon |
| - Lung abscess | - Kidney |
| Benign tumor | Small cell ca (4%) |
| - Hamartoma (10%) | Extranodal lymphoma |
| - Lipoma | Carcinoid tumor |
| - Condroma | |
| Congenital | |
| - Arteriovenous malformation | |
| - Bronchogenic cyst | |
| Immunemediated disease | |
| - Sarcoidosis | |
| - Rheumatoid arthritis | |
| Other: | |
| - Endoparenchymal lymph node | |
| - Amyloidosis |
Radiologic features:
| Feature | Sugg. benign | Sugg. Malig |
|---|---|---|
| Border | Smooth | Irregular or spiculated |
| Calcification | Concentric, central, popcorn | Typically noncalcified or eccentric calcification |
| Desity | Solid | Nonsolid, ground-glass |
| Doubling time | <30 days or >400 days | 30-400 days |
| Size | <6mm | >=6mm |
References:
- AFP Vol 92 No 12 Dec 2015
- AFP Vol 107 No 3 Mar 2023
Sleep and Insomnia
See also:
| Sleep Problem | Sleep Times | Consequences of Disturbed Sleep | Symptom Duration, |
|---|---|---|---|
| Number of awakenings | Bedtime | Fatigue or malaise | <3 months or ?3 months |
| Duration of awakenings | Duration until sleep onset | Poor attention or concentration | |
| Duration of the sleep problem | Final awakening time | Social/vocational/educational dysfunction | |
| Nap time(s) | Motor disturbance or irritability | ||
| Nap length(s) | Daytime sleepiness | ||
| Reduced motivation or energy | |||
| Increased errors or accidents | |||
| Behavioral problems | |||
| Ongoing worry |
Preference (work for both sleep onset and sleep maintenance):
- zolpidem
- daridorexant
- temazepam
| Sleep Medication | Sleep latency | Sleep maintenance | Poss dependence | Price (GoodRx) | Mechanism |
|---|---|---|---|---|---|
| temazepam (Restoril) | X | X | X | $6 | GABA-receptor agonist |
| doxepin (Silenor) | X | $8 | SNRI, H1-blocker | ||
| zolpidem (Ambien) | X | X | X | $10 | GABA-receptor agonist |
| zaleplon (Sonata) | $13 | GABA-receptor agonist | |||
| eszopiclone (Lunesta) | X | X | X | $14 | GABA-receptor agonist |
| triazolam (Halcion) | X | X | $29 | GABA-receptor agonist | |
| ramelteon (Rozerem) | X | $47 | Highly selective melatonin-receptor agonist | ||
| daridorexant (Quviviq) | X | X | X | $469 ($25) | Block OX1 and OX2 to inhibit wakefulness |
| lemborexant (Dayvigo) | X | X | X | $314 | Block OX1 and OX2 to inhibit wakefulness |
| suvorexant (Belsomra) | X | X | X | $414 | Block OX1 and OX2 to inhibit wakefulness |
Refences:
- JFP Supp Vol 69 No 7 Sep 2020
- GoodRx.com
- JFP Supp Vol 72 No 6 Jul 2023
Developmental Sleep Recommendations
Recomendations:
- Infants 4 months to 12 months should sleep 12 to 16 hours per 24 hours (including naps) on a regular basis to promote optimal health.
- Children 1 to 2 years of age should sleep 11 to 14 hours per 24 hours (including naps) on a regular basis to promote optimal health.
- Children 3 to 5 years of age should sleep 10 to 13 hours per 24 hours (including naps) on a regular basis to promote optimal health.
- Children 6 to 12 years of age should sleep 9 to 12 hours per 24 hours on a regular basis to promote optimal health.
- Teenagers 13 to 18 years of age should sleep 8 to 10 hours per 24 hours on a regular basis to promote optimal health.
Why:
- Sleeping the number of recommended hours on a regular basis is associated with better health outcomes including:
- improved attention
- behavior
- learning
- memory
- emotional regulation
- quality of life
- mental and physical health
- Regularly sleeping fewer than the number of recommended hours is associated with:
- attention
- behavior
- learning problems.
- Insufficient sleep also increases the risk of
- accidents
- injuries
- hypertension
- obesity
- diabetes
- depression
- Insufficient sleep in teenagers is associated with increased risk of
- self-harm
- suicidal thoughts
- suicide attempts
- Regularly sleeping more than the recommended hours may be associated with adverse health outcomes such as hypertension, diabetes, obesity, and mental health problems.
| DEVELOPMENTAL STAGE | AGE | DAYTIME SLEEP | NIGHTTIME SLEEP | TOTAL SLEEP |
|---|---|---|---|---|
| Newborn | 0 to 4 Months | 7–9 hours (3–5 naps) | 8–9 hours | 16–18 hours |
| Infant | 4 to 12 Months | 4–5 hours (2–3 naps) | 9–10 hours | 12–16 hours |
| Toddler | 1 to 2 Years | 2–3 hours (2 naps) | 11 hours | 11–14 hours |
| Preschool | 3 to 5 Years | 0–1 hours | 10–13 hours | 10–13 hours |
| School-Age | 6 to 12 Years | N/A | 10–11 hours | 9–12 hours |
Reference:
- Paruthi S, Brooks LJ, D'Ambrosio C, Hall WA, Kotagal S, Lloyd RM, Malow BA, Maski K, Nichols C, Quan SF, Rosen CL, Troester MM, Wise MS. Recommended Amount of Sleep for Pediatric Populations: A Consensus Statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016 Jun 15;12(6):785-6. doi: 10.5664/jcsm.5866. PMID: 27250809; PMCID: PMC4877308.
- https://www.parents.com/baby/sleep/basics/baby-and-children-sleep-chart/
Chronic Insomnia
Affects:
- 10-30% of population
Associated with:
- Cognitive difficulties
- Anxiety and depression
- Poor work performance
- Decreased quality of life
- Increased cardiovascular disease
- Increased all cause mortality
Diagnosis criteria:
- Difficulty falling asleep
- Difficulty staying asleep
- Early awakening despite the opportunity for sleep
- Symptoms associated with impaired daytime functioning
- Symptoms occur 3/wk for at least 1mo
Rule out contributing factors:
- Psychiatric and medical problems
- Medication use
- Substance abuse
Management includes:
- Cognitive behavior
- Relaxation therapy (SOR A)
- Progressive muscle relaxation
- Guided imagery
- Abdominal breathing to lower somatic and cognitive arousal states
- Sleep hygiene
Treatment:
- Behavioral interventions and address any contributing medical condition
- Determine insomnia type
- Sleep onset insomnia
- Melatonin, controlled release
- Daridorexant (Quviviq)
- Eszopiclone (Lunesta)
- Zaleplon (Sonata)
- Zolpidem (Ambien)
- Sleep maintenance insomnia
- Daridorexant (Quviviq)
- Eszopiclone
- Doxepin (Silenor)
- Zolpidem
- Insomnia in older adults
- Doxepin
- Melatonin, controlled release
- Ramelteon (Rozerem)
- Depression and insomnia
- Doxepin
- Mirtazapine (Remeron)
- Sleep onset insomnia
References:
- AFP Vol 92 No 12 Dec 2015
- JPF Vol 66 No 4 Apr 2017
- AFP Vol 96 No 1 Jul 2017
Obstructive Sleep Apnea
See also:
| Adult AHI | Pediatric AHI | |
|---|---|---|
| Mild OSA | ≥ 5 to < 15 events per hour | ≥ 1 to ≤ 5 events per hour |
| Moderate OSA | ≥ 15 to < 30 events per hour | > 5 to ≤ 10 events per hour |
| Severe OSA | ≥ 30 events per hour | > 10 events per hour |
STOP-BANG (3 or more = High Risk) (Sn=96.2-97.6%; Sp=14-12.7%)
- Do you SNORE loudly?
- Do you often feel TIRED, fatigued, or sleepy durign the day?
- Has anyone OBSERVED that you have stopped breathing while sleeping?
- Do you have or are you being treated for high blood PRESSURE?
- BMI more than 35 kg/m2?
- Are you more than 50 years of Age?
- Is your NECK 17 in or greater? (16 in for women)
- Male GENDER?
Evaluation:
- Neck
- M: >17"
- F: >16"
- Mallampati Class 3 or 4
Home sleep tests
- Home sleep tests calculate the AHI based on the total recording time, as opposed to the more precise total sleep time measured in a polysomnogram.
- As a result, at-home sleep tests often underestimate AHI by about 15%.
Sleep Hygiene Rules for the treatment of insomnia
Sleep hygiene refers to cleaning up sleep habits that interfere with good sleep. These habits often develop in response to insomnia, but are counterproductive. Practicing good sleep hygiene is recommended for all patients with insomnia.
- Sleep as much as needed to feel refreshed and healthy during the following day, but not more. Curtailing time in bed a bit seems to solidify sleep; excessively long times in bed seem related to fragmented and shallow sleep.
- Maintain a consistent, regular routine. Start by setting a routine time to wake up and get out of bed. Once your sleep improves, keep to a standard time to go to bed. This routine needs to be maintained every day of the week.
- Never try to sleep. Only go to bed when you feel sleepy and do not try to force yourself to fall asleep. This will only tend to make you more awake and is counterproductive. If you wake up in the middle of the night, let yourself fall asleep within 15-20 minutes. If you cannot fall asleep, get out of bed and sit in the dark in a chair outside your bedroom. When you are sleepy, return to bed and go to sleep.
- Use the bedroom only for sleep and intimacy. Do not watch TV, eat, drink, read, have arguments or discussions while in bed. These tend to keep you awake.
- Avoid napping unless absolutely required. Particularly avoid routine, daily naps. Napping interferes with the ability to fall asleep at night. If you need to nap for safety reasons (driving, etc) then a short 30-60 minute nap is okay.
- Avoid coffee, alcohol, and nicotine. Caffeine will tend to keep you awake. The effects of caffeine on sleep usually takes several hours to go away, however in some people the effects are prolonged. Alcohol may make some people fall asleep more quickly (but not everyone), however alcohol leads to fragmented sleep and does not provide good restful sleep. Nicotine is a stimulant and tends to reduce the quality of sleep, and nicotine withdrawal at night tends to do the same. Quiting smoking is recommended for all smokers for many reasons.
- Exercise in the late afternoon or early evening can improve sleep. Do not exercise within several hours (4-5) of attempting to go to sleep – this will keep you awake. Gentle stretching for relaxation can help you fall asleep.
- Ensure you are sleeping in a quiet, dark, comfortable environment.
- Consume a light bedtime snack (especially warm milk or similar drink) as this seems to help many individuals sleep. Hunger may disturb sleep.
- Move the bedroom clock to where you cannot see it. Some recommend removing the clock from the bedroom entirely. Looking at the clock will keep you awake; it does not help you fall asleep.
- Pad and pen next to be to write down and "hold worry"
- Take a warm, not hot, shower 1 hour before bed
- Practice diaphragm breathing for 5 breaths 3 times a day
Improving Sleep Pattern
- Bedtime routine
- Create a consistent sleep schedule with fixed sleep and wake up times, including weekends
- Create a bedtime routine that follows the same steps each night
- Practice relaxation and stress management, including meditation, mindfulness, and breathing exercises.
- Unplug from electronics 30-60 min before bedtime and dim lights to promote the production of melatonin, an essential hormone in the body that facilitates the sleep cycle
- Sleep environment
- Choose a comfortable mattress and pillow
- Make sure your bedroom is quiet. Consider ear plugs, a white noise machine, or a fan to reduce noise.
- Remove all electronics from the bedroom
- Set the bedroom thermostat to a comfortable temperature. Consider setting it to a cooler temperature, around 68 degrees or less
- Daily healthy habits
- Avoid large meals, caffeine, alcohol, or nicotine before bedtime.
- Engage in regular daily physical activity. Avoid at least 3-4 hours before bedtime.
- Get daily sunlight exposure
References:
- JFP Vol 66 No 4 Apr 2017
- JFP Vol 72 No 8 Oct 2023
Sleep Restriction Therapy:
Rationale:
In response to inadequate sleep, people with insomnia tend to increase the amount of time spent trying to sleep, but end up spending a lot of time awake while trying to sleep. Sleep that is fragmented and spread out over many hours is not as refreshing or restorative as sleep that is consolidated. For example, 6 hours of sleep in 6.5 hours time in bed is more refreshing and leads to better sleep than sleeping 6 hours while trying to sleep for 9 hours.
Rules for Sleep Restriction Therapy:
- Keep a daily sleep log which tracks the following:
- Time you lie down to go to bed
- Time you fall asleep
- Time you wake up to start your day
- When you are asleep and when you are awake at night
- The timing and duration of any naps during the day
- Calculate your total sleep time (TST) = the total number of hours of sleep in the 24 hr period.
- Calculate your time in bed (TIB) = total time from when you lie down to fall asleep and the time you get up to start your day. Also add in any naps.
- Calculate your sleep efficiency (SE) = (TST / TIB) x 100%
- Pick a wake-up time that you will use every day of the week.
- Make your new TIB your current TST. Never reduce your TST to less than 6 hours per night.
- Count backwards from your wake-up time to determine your time to lie down to go to bed.
- Keep track of your sleep efficiency for the last 7 days. When your sleep efficiency is >90%, increase your TIB by 15 minutes.
- If your sleep efficiency drops < 85%, decrease your TIB by 30 minutes.
- Only make changes to your allowed TIB once every 7 days.
- Be aware that when starting this process many people will feel sleepier during the day until your sleep improves. Be extra cautious if this occurs.
Example: John goes to bed at 9pm, falls asleep at 11pm, is awake for 1 hr in the middle of the night, and gets out of bed at 6 am.
- His TST is 6 hours
- TIB is 9 hrs
- His sleep efficiency is (6/9) x 100% = 66%.
He keeps his wake time at 6am and therefore decides to go to bed at 12 midnight. After doing this for 2 weeks, he is going to bed at 12 midnight, falling asleep within 15 minutes, and getting up at 6am.
- His current sleep efficiency is (5.75 / 6) x 100% = 95%.
- He lets himself go to bed 30 minutes earlier at 1130pm.
After several adjustments, 8 weeks after starting this program John is going to bed at 1030pm, falling asleep in 30 minutes and still gets up at 6am.
- He is getting a TST of 7 hrs with a TIB 7.5 hrs = sleep efficiency of 93%.
- He feels he is sleeping better and keeps to this schedule.
References (and modified from):
- JFP Vol 66 No Apr 2017
- Kryger et al, Principles and Practice of Sleep Medicine, 2nd Edition 2005, Chapter 61
- Morin et al. Nonpharmacologic Treatment of Chronic Insomnia. An American Academy of Sleep Medicine Review. Sleep 1999;22:1134.
The Army Quick Sleep Technique
The technique mainly involves muscle relaxation, breathing, and visualization tricks anyone can do.
How it works:
- Sit on the edge of your bed. Make sure only your bedside light is on, your phone is silenced, and your alarm is set for the morning.
- Now relax your facial muscles. First tighten them up in a wincing motion, and then slowly let your muscles naturally loosen. And let your tongue fall any which way in your mouth.
- Once your face feels like deflated putty, let gravity pull your shoulders naturally toward the ground. Let your arms dangle too, one side at a time.
- While doing this, breathe in and out, listening to the sound of your breath. With each breath, let your chest relax further and then let gravity relax your thighs and lower legs.
- Once your body feels like nothing more than a loosely formed lump of clay, try to clear your mind for 10 seconds.
- If thoughts come naturally, let them pass–just keep your body loose and limp. After a few more seconds you mind should feel clearer.
- Now picture one of the following two scenarios: you lying in a canoe in a calm lake with clear blue skies above you; or you in a velvet hammock, gently swaying in a pitch-black room.
- If you happen to be a person who isn't great at visualization, you can instead chant the mantra, "Don't think, don't think, don't think" for 10 seconds instead.
4-6-7 Breathing Technique Will Knock You Out in 10 Minutes Flat
The 4-6-7 Technique
- Breathe in and count to four
- Hold your breath for six seconds
- Breathe out slowly for seven seconds
Ways to get more sleep
- Don't use your phone before bed.
- Don't exercise at night.
- Have a snack.
- Read a physical book.
- Avoid afternoon naps.
- Write out your to-do list the night before.
- Drink chamomile tea.
- Go to bed at the same time every day.
- Have a good laugh.
- No more pets in bed.
- Have sex.
- Practice breathing.
- Be consistent.
Jet Lag edit
- Before travel
- Eastward travel
- Move bedtime and wake time 30 minutes earlier per day starting 3 days prior to departure.
- To facilitate this shift, avoid light (including electronics) in the evening and seek bright light the first 2 to 3 hours after awakening.
- Westward travel
- Move bedtime and wake time 30 minutes later per day starting 3 days prior to departure.
- To facilitate this shift, seek light in the evening and avoid bright light the first few hours after awakening.
- During travel
- Eastward travel
- Set watch to destination time.
- Avoid early morning (destination time) bright light. Use sunglasses on the plane if cabin lights are on and keep window shades down.
- Get lots of late morning and early afternoon (destination time) bright light.
- Attempt sleep during destination nighttime.
- If you cannot sleep during this period, avoid light (especially during the second half of the night) with dark sunglasses.
- Avoid sedative/hypnotic medications in flight.
- Westward travel
- Set watch to destination time.
- Get lots of late afternoon and evening (destination time) bright light.
- Avoid bright light (including electronics) during destination nighttime. Use sunglasses on the plane if cabin lights are on.
- Try to stay up to desired destination bedtime.
- Attempt sleep during destination nighttime.
- Avoid sedative/hypnotic medications in flight.
- On arrival
- Eastward travel
- Avoid early morning bright light.
- Get lots of late morning and early afternoon (destination time) bright light.
- Take melatonin at desired destination bedtime.
- Falling asleep may be difficult the first few days.
- Short naps (less than 45 minutes) and caffeine may help with alertness.
- Westward travel
- Get lots of late afternoon and evening bright light.
- Avoid bright light during destination nighttime.
- Melatonin is not helpful.
- Try to stay up to desired destination bedtime. Avoid evening nodding off.
- Staying asleep may be difficult the first few days; avoid electronics during awakenings.
- Short naps (less than 45 minutes) and caffeine may help with alertness.
General instructions are intended for eastward and westward travel across up to 7 time zones. Specific timing may vary.
Notes:
- Benzodiazepines and nonbenzodiazepine benzodiazepine receptor agonist (BzRA) medications have demonstrated efficacy in treating insomnia associated with jet lag
- Judicious use of caffeine is generally safe and can help offset daytime sleepiness associated with jet lag, but benefits may be outweighed by sleep disruption in some cases.
- Short naps (<30 minutes) at least 8 hours prior to bedtime may also help alertness without disrupting nighttime sleep
Reference:
- UptoDate.com
Sleep Study Results Explanation
The important parts are the (apnea hypopnea index (AHI) which is how often you stop breathing per hour - for you that averaged XXX times per hour while you sleep.
This means that XXX times an hour, when you are in or entering the restorative part of sleep, your body forces you to wake up slightly so you can breath again - making your sleep not as restful as it could be.
The next important part is the O2 desaturation level. Your O2 level in your blood dropped as low as XXX%. It should not dip below 94% and even though it went that low, you still averaged 97%.
Additionally, your heart rate at some point increased to XXX beats per minute, which is pretty fast for sleeping and likely was during one of your apneic events (period where you stopped breathing.
The machine we ordered should help you not have these events and thus get more restful sleep.
Feel free to ask me any questions to further clarify as I can,
Notes: Insert the following data:
- AHI
- O2 desat
- HR
Sleep Duration Recommendations
| Age Group | Age | Recommended Hours of Sleep |
|---|---|---|
| Infant | 4-12 months | 12-16 hours per 24 hours (including naps) |
| Toddler | 1-2 years | 11-14 hours per 24 hours (including naps) |
| Pre-School | 3-5 years | 10-13 hours per 24 hours (including naps) |
| School Age | 6-12 years | 9-12 hours per 24 hours |
| Teen | 13-18 years | 8-10 hours per 24 hours |
| Adult | 18-60 years | 7 or more hours per night |
CDC Habits to Improve Your Sleep
- Be consistent. Go to bed at the same time each night and get up at the same time each morning, including on the weekends.
- Make sure your bedroom is quiet, dark, relaxing, and at a comfortable temperature.
- Remove electronic devices such as TVs, computers, and phones from the bedroom.
- Avoid large meals, caffeine, and alcohol before bedtime.
- Don't use tobacco.
- Get some exercise. Being physically active during the day can help you fall asleep more easily at night.
Reference:
Study: A new method for measuring daytime sleepiness: the Epworth sleepiness scale
Notes:
- Normal patients had a mean ESS of 5.9, while patients who snored but had no sleep disorder had a mean ESS of 6.5.
- Patients with periodic limb movement disorder, OSA, narcolepsy, and idiopathic hypersomnia had ESS means of 9.2, 11.7, 17.5, and 17.9 respectively.
- Standard deviations were between 2.0 and 4.6 for each of these values.
| Condition | Epworth |
|---|---|
| Normal | 5.9 |
| Snored without d/o | 6.5 |
| Periodic limb movement | 9.2 |
| OSA | 11.7 |
| Narcolepsy | 17.5 |
| Idiopathic hypersomnia | 17.9 |
The development and use of a new scale, the Epworth sleepiness scale (ESS), is described. This is a simple, self-administered questionnaire which is shown to provide a measurement of the subject's general level of daytime sleepiness. One hundred and eighty adults answered the ESS, including 30 normal men and women as controls and 150 patients with a range of sleep disorders. They rated the chances that they would doze off or fall asleep when in eight different situations commonly encountered in daily life. Total ESS scores significantly distinguished normal subjects from patients in various diagnostic groups including obstructive sleep apnea syndrome, narcolepsy and idiopathic hypersomnia. ESS scores were significantly correlated with sleep latency measured during the multiple sleep latency test and during overnight polysomnography. In patients with obstructive sleep apnea syndrome ESS scores were significantly correlated with the respiratory disturbance index and the minimum SaO2 recorded overnight. ESS scores of patients who simply snored did not differ from controls.
Reference:
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991 Dec;14(6):540-5. doi: 10.1093/sleep/14.6.540. PMID: 1798888.
- Epworth
Epworth Questions
- Chance of dozing off while sitting and reading?
- Chance of dozing off while watching TV?
- Chance of dozing off while Sitting, inactive in a public place?
- Chance of dozing off as a passenger in a car for an hour without a break?
- Chance of dozing off while lying down to rest in the afternoon when circumstances permit?
- Chance of dozing off while sitting and talking to someone?
- Chance of dozing off while sitting quietly after lunch without alcohol?
- Chance of dozing off while in a car, while stopped for a few minutes in traffic?
Answer Options:
- Never (0)
- Slight (1)
- Moderate (2)
- High (3)
Scores:
- 0 to 10 points: Normal levels of subjective sleepiness
- 11 to 24 points: Excessive levels of subjective sleepiness
Study: Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women
Objectives:
- To evaluate associations of sleep duration with total mortality and disease-specific mortality in a Chinese population.
Design:
- Prospective study conducted from 1996 (for women)/2002 (for men) to 2010.
Setting:
- A population-based cohort study in Shanghai, China.
Intervention:
- None.
Measurements and results:
- A total of 113,138 participants (68,548 women and 44,590 men) of the Shanghai Women's and Men's Health Studies, aged 44-79 y and 40-75 y (women and men, respectively) at sleep duration assessment, were included in the study. In-person interviews were conducted to collect information on sleep duration, socioeconomic status, living conditions, history of chronic disease, participation in regular exercise, and family history of disease. The cohort has been followed using a combination of biannual in-person interviews and record linkages with Shanghai's population-based death registry. Survival status of participants on December 31, 2010 was included as the study outcome.
- Relative risks were calculated using a Cox proportional model stratified by sex and comorbidity score.
- There were 4,277 deaths (2,356 among women; 1,921 among men) during a median follow-up time of 7.12 y for women and 6.07 y for men.
- Among both women and men, sleep duration showed a J-shaped association with total mortality.
- Hazard ratios (95% confidence intervals) were 1.15 (1.01-1.32), 1.06 (0.94-1.20), 1.17 (1.04-1.32), 1.36 (1.13-1.64), and 2.11 (1.77-2.52) for women and 1.06 (0.90-1.25), 1.07 (0.94-1.23), 1.13 (1.00-1.28), 1.34 (1.10-1.62), and 1.55 (1.29-1.86) for men who slept 4-5, 6, 8, 9, and ≥ 10 h per day, respectively, compared with those who slept 7 h per day.
- Associations for disease-specific mortality, including cardiovascular disease, stroke, diabetes, and cancer, also generally followed the same J-shaped pattern.
- The sleep duration-mortality association was more evident among participants with comorbidities, but varied little by sex.
Conclusion:
- In our study population of Chinese adults, shorter and longer sleep durations were independently associated with increased risk of mortality.
- But longer sleep duration had a higher mortality risk of cardiovascular disease and diabetes than short sleep.
Reference:
- Cai H, Shu XO, Xiang YB, Yang G, Li H, Ji BT, Gao J, Gao YT, Zheng W. Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women. Sleep. 2015 Apr 1;38(4):529-36. doi: 10.5665/sleep.4564. PMID: 25348122; PMCID: PMC4355892.
Sleep Cycles and Napping edit
Here are some basic tips for healthful napping:
- Sleep for no longer than 30 minutes: The ideal nap duration is around 20 minutes and should be no longer than 30 minutes. This helps prevent the body from reaching the deeper stages of sleep, and it keeps a person from waking up feeling groggy.
- Find a quiet place to lie down and sleep: This can help a person make the most of the short time they have to nap.
- Avoid taking late naps: Taking a nap around the middle of the day or early afternoon may be best. Taking naps in the early evening may cause a person to feel very alert later into the night, which could disrupt their sleep schedule.
- Stick to a routine: Some research has found that those who nap habitually get better sleep at night.
Although 20 minutes is the ideal nap length for most people, it can vary. A person may want to take a series of test naps of around 10–45 minutes to find their ideal nap length.
- Never nap if you have problems falling asleep and staying asleep
- The ideal time for a short nap is under 30 minutes or over 90 minutes
- Try to nap in early afternoon during your circadian dip
- Understanding Sleep Cycles: Sleep is composed of different stages, and one complete sleep cycle lasts about 90 to 120 minutes. The stages include light sleep, deep sleep, and REM (rapid eye movement) sleep. These stages play different roles in memory consolidation and physical restoration.
- Ideal Nap Lengths: The effectiveness of a nap depends on its length. Short naps, around 10 to 20 minutes (often referred to as "power naps"), help prevent grogginess and can provide a quick energy boost. Longer naps may include deep sleep but can lead to sleep inertia upon waking. Napping for 90 to 120 minutes allows for a complete sleep cycle and can be refreshing but might interfere with nighttime sleep.
- Benefits of Napping: Napping, when done correctly, can offer several benefits, including improved alertness, enhanced cognitive performance, and mood regulation. Some studies even suggest that occasional napping may reduce the risk of heart disease. However, it's essential to maintain a consistent nightly sleep schedule and use naps as a supplement, not a replacement, for nighttime sleep.
To avoid disturbing your nightly sleep schedule, most sleep experts recommend napping between 1 p.m. and 3 p.m.
Study: Sleep loss and emotion: A systematic review and meta-analysis of over 50 years of experimental research
In a largely sleep-deprived society, quantifying the effects of sleep loss on emotion is critical for promoting psychological health.
This preregistered systematic review and meta-analysis quantified the effects of various forms of sleep loss on multiple aspects of emotional experiences.
Eligible studies used experimental reductions of sleep via total sleep deprivation, partial sleep restriction, or sleep fragmentation in healthy populations to examine effects on positive affect, negative affect, general mood disturbances, emotional reactivity, anxiety symptoms, and/or depressive symptoms.
In total, 1,338 effect sizes across 154 studies were included (N = 5,717; participant age range = 7-79 years).
Results:
- Random effects models were conducted, and all forms of sleep loss resulted in reduced positive affect (standardized mean difference [SMD] = -0.27 to -1.14), increased anxiety symptoms (SMD = 0.57-0.63), and blunted arousal in response to emotional stimuli (SMD = -0.20 to -0.53).
- Findings for negative affect, reports of emotional valence in response to emotional stimuli, and depressive symptoms were mixed and depended on the type of sleep loss.
- Nonlinear effects for the amount of sleep loss as well as differences based on the stage of sleep restricted (i.e., rapid eye movement sleep or slow-wave sleep) were also detected.
This study represents the most comprehensive quantitative synthesis of experimental sleep and emotion research to date and provides strong evidence that periods of extended wakefulness, shortened sleep duration, and/or nighttime awakenings adversely influence human emotional functioning. Findings provide an integrative foundation for future research on sleep and emotion and elucidate the precise ways that inadequate sleep may impact our daytime emotional lives.
Reference:
- Palmer CA, Bower JL, Cho KW, Clementi MA, Lau S, Oosterhoff B, Alfano CA. Sleep loss and emotion: A systematic review and meta-analysis of over 50 years of experimental research. Psychol Bull. 2024 Apr;150(4):440-463. doi: 10.1037/bul0000410. Epub 2023 Dec 21. PMID: 38127505.
- https://www.apa.org/pubs/journals/releases/bul-bul0000410.pdf
Patient Messaging: Avoiding Fatigue
To help avoid fatigue, I suggest:
- Sleep: Try to get 7-9 hours of sleep every night
- Nap strategy: Use short naps of only 20-25 min (no more than 30) to refresh your energy
- Fluids: Stay hydrated - being dehydrated can make you tired
- Caffeine strategy: Avoid caffeine as a way to wake you up, instead use caffeine when you feel rested as it keeps you at the level of wakefulness you are (as opposed to waking you up)
- Vitamin: B12 supplementation if you are low
Spirometry
When the ratio of forced expiratory volume in 1 second over forced vital capacity (FEV1/FVC) is less than 70% of that predicted for a matched control, it is diagnostic for a significant obstructive defect.
Criteria for assessing the severity of airflow obstruction (based on the percent predicted postbronchodilator FEV1) are as follows:
- Stage I (mild): FEV 1 80% or greater of predicted
- Stage II (moderate): FEV 1 50-79% of predicted
- Stage III (severe): FEV 1 30-49% of predicted
- Stage IV (very severe): FEV 1 less than 30% of predicted or FEV 1 less than 50% and chronic respiratory failure
Spirometry indicates the presence of an abnormality if any of the following are recorded:
- FEV1 <80% predicted normal
- FVC <80% predicted normal
- FEV1/FVC ratio <0.7
Obstructive disorder:
- FEV1 reduced (<80% predicted normal)
- FVC is usually reduced but to a lesser extent than FEV1
- FEV1/FVC ratio reduced (<0.7)
Restrictive disorder:
- FEV1 reduced (<80% predicted normal)
- FVC reduced (<80% predicted norm
Definitions:
- FVC - Largest amount of air that can be forcefully exhaled after maximal inspiration
- FEV1 - Forced expiration in 1 second
- FEV1/FVC - 80-85% is normal
Obstruction changes FEV1 -> If FEV1 and FEV1/FVC are decreased then airway obstruction
- FEV1/FVC <70% is obstruction
#CAPTION: COPD Severity Based on Spirometry
| Post-bronchodilator FEV1/FVC | Pestbronchodilator FEV1 (% of pred) | Severity |
|---|---|---|
| <0.7 | >= 80 | Mild |
| <0.7 | 50-79 | Moderate |
| <0.7 | 30-49 | Severe |
| <0.7 | <30 | Very Severe |
Restrictive changes -> FVC and FEV1 are reduced proportionally (ie 40% and 45% of predicted - FEV1/FVC normal)
- Decreased FVC -> Restrictive pattern
Assessing reversibility:
- Use a bronchodilator
- after 15 min, repeat spirometry
- If 12% improvement and absolute increase in FVC and/or FEV1 vol of 200mL -> Pos response
Flow-loop:
- Sharp peak indicates good patient effort
- The greater the degree of concavity, the more significant the obstruction
- Obstructive: Smooth concave shape (asthma) or angled (COPD)
- Restrictive: Normal height curve, but very steep and lung volume is decreased
Reference:
- AFP Vol 107 No 6 Jun 2023
Taking a nap (30/90 Rule)
Nap:
- Aim to sleep for 30 minutes or less
- Or give yourself at least 90 minutes
It's all about sleep cycles
- When we doze off, our brains cycle through different sleep phases in regular blocks of about 90 minutes
- For about the first 30 minutes after lying down, you're likely in a phase of light sleep.
- Eventually you enter a phase of deeper sleep which lasts between 30 and 75 minutes.
- Finally, before waking, you experience a period of REM sleep where you do your most intense dreaming.
- Naps of 90 to 120 minutes usually comprise all stages, including REM and deep slow-wave sleep, which helps to clear your mind, improve memory recall, and recoup lost sleep.
NASA, for instance, tested the ideal nap length to boost cognitive performance and found a snooze of 26 minutes was ideal, boosting performance on the job by 34 percent.
- The space agency found that pilots who slept in the cockpit for 26 minutes showed alertness improvements of up to 54 percent and job-performance improvements by 34 percent, compared to pilots who didn't nap.
- NASA's ultimate recommendation is power naps between 10 and 20 minutes long.
- Rosekind MR, Smith RM, Miller DL, Co EL, Gregory KB, Webbon LL, Gander PH, Lebacqz JV. Alertness management: strategic naps in operational settings. J Sleep Res. 1995 Dec;4(S2):62-66. doi: 10.1111/j.1365-2869.1995.tb00229.x. PMID: 10607214.
- Also:
- Effects of a Short Daytime Nap on the Cognitive Performance: A Systematic Review and Meta-Analysis
- Dutheil F, Danini B, Bagheri R, Fantini ML, Pereira B, Moustafa F, Trousselard M, Navel V. Effects of a Short Daytime Nap on the Cognitive Performance: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021 Sep 28;18(19):10212. doi: 10.3390/ijerph181910212. PMID: 34639511; PMCID: PMC8507757.
Tobacco (Smoking Cessation)
- Set a quit date!
- Tell people
- Can try nicotine replacement therapy
- Know your triggers
- Tips
- Drink a lot of water.
- Use gum/mints/toothpicks for cravings
- Avoid caffeine
- Wash clothes and try to remove smoke smell from house/car
- Avoid places that trigger
- Become physically active
- Use diaphramatic breathing exercises
Cytisine for Smoking Cessation, cheaper alternative to Chantix
From NEJM study & Editorial:
- Cytisine is an inexpensive drug that has been used for decades to treat smoking cessation and for which there are now current data showing its safety and effectiveness.
- Cystisine mechanism of action is similar to Chantix, it acts as a nicotinic receptor partial agonist.
- Most recent study (2014) showed that cytisine is at least equivalent to nicotine-replacement therapy in real-world practice, and superior when combined with behavioral support.
- Unfortunately, in the United States and Western Europe, cytisine is currently unavailable, and there is now no direct pathway through the regulatory and pharmaceutical market structure for easy approval.
- NEJM Editorial calls for urgent action.
- Tobacco use is now the leading preventable cause of death worldwide.
- Pharmacotherapy improves the likelihood of success for those who attempt to quit.
- Low cost option would increase pharmacotherapy access for so many patients.
- Health care costs would also benefit from a lower-cost option.
- "We can save lives by making effective treatments available to all smokers."
Reference:
E-cigarette's users twice as likely to quit smoking
E-cigarettes were more effective for smoking cessation than nicotine-replacement therapy, when both products were accompanied by behavioral support.
- Population: RCT of 886 adults in UK
- 1-year abstinence rate was 18.0% in the e-cigarette group, as compared with 9.9% in the nicotine-replacement group (relative risk, 1.83; 95% confidence interval [CI], 1.30 to 2.58; P<0.001).
References:
Health Benefits After Quitting:
Quitting by age 50 cuts risk of a smoking related death in half, and quitting by 30 almost completely negates it. (JFP Vol 65 No 1 Jan 2016)
- 20 min - BP decreases
- 8 hrs - Pa O2 normalizes
- 3 mo - Lung function improves up to 30%
- 1 yr - MI risk cut in half
- 5 yrs - Risk for mouth, throat, esophagus, and bladder ca cut in half
- 10 yrs - Risk of dying from lung ca cut in half
- 15 yrs - Risk for CAD same as a non-smoker
Quitting smoking can add 10 years to a persons life expectancy.
Management
- First line (LOE A):
- Varenicline
- Bupropion
- Nicotine replacement
- Also consider:
- Nortriptyline
- Provide counseling along with medication as this is more effective (LOE A)
- Refer patients to the Quit Line (LOE A)
References:
- JFP Vol 65 No 1 2016
Smoking and supplements
Smokers taking B-carotene supplements have increased incidence of lung cancer
Smoking USPSTF
The Task Force recommends annual screening with low-dose CT for adults aged 50 to 80 years who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years.
Reference:
Tools, Apps, Resources
http://toolsforsmokingcessation.webs.com/
Smoking cessation apps:
- QuitGuide: http://smokefree.gov/apps-quitguide
- QuitStart: http://smokefree.gov/apps-quitstart
- The quitSTART app helps you:
- Get ready to quit with tips and information to prepare you for becoming smokefree
- Monitor your progress and earn badges for smokefree milestones and other achievements
- Get back on track if you slip and smoke
- Manage cravings and bad moods in healthy ways
- Distract yourself from cravings with games and challenges
- Store helpful tips, inspirations, and challenges in your Quit Kit
- Share your progress and favorite tips through social media
- https://smokefree.gov/tools-tips/apps/quitstart
- The quitSTART app helps you:
Patient Resources:
- Tobacco Free Florida: http://www.tobaccofreeflorida.com/
- 877-u-can-now (877-822-6669)
- http://tobaccofreeflorida.com/webcoach - web coach
- http://tobaccofreeflorida.com/ahec - face-to-face
- Smoke Free: http://smokefree.gov/
- Be Tobacco Free: http://betobaccofree.hhs.gov/index.html
- American Lung Association: http://www.lung.org/stop-smoking/
Vaping and nicotine
On average, a cigarette contains about 1 gram of tobacco which is approximately 8mg of Nicotine.
- 1 cigarette = 1 g tobacco = 8 mg nicotine
- 1 ml vape juice = 100 hits
- Avg daily hits = 130
Broad guideline of the different nicotine levels compared to smoking cigarettes
- 0 mg
- People trying to cut out their nicotine dependency altogether.
- you can vape non nicotine vape juice.
- 3 mg
- Light smokers and people with lower nicotine dependency.
- 6 mg
- Light to moderate smokers and people who are, particularly used to "light" cigarettes.
- 6 mg+
- Heavy cigarette smokers and smokers of unfiltered cigarettes.
What kind of nicotine is best for vaping?
- In the study shared above, the researchers recommend 50 mg nicotine levels for heavy smokers who have recently transitioned into vaping.
- Luckily, nicotine salt fits the bill and the user-friendly devices used for nic salts are perfect for smokers who are new to vaping.
How many puffs a day is normal for Vaping?
- The median number of puffs per day was 132.
- After removing days of use with less than 5 puffs, the median rises to 140 puffs / day.
- The number of puffs per day varied considerably from one user to another.
How much vape juice is equivalent to a pack of cigarettes?
- By way of example, a 1 ml bottle of e-juice will roughly contain around 100 hits.
- This is roughly equivalent to 10 cigarettes or a half of a pack.
What vape is closest to a cigarette?
- There are two types of vaping devices:
- mouth-to-lung
- You hold it in your mouth first (like a cigarette)
- The closest to smoking a cigarette is a mouth-to-lung device
- direct-to-lung
- direct inhale (like an asthma inhaler)
- mouth-to-lung
How many cigarettes a day is considered a heavy smoker?
- Heavy smokers (those who smoke greater than or equal to 25 or more cigarettes a day ) are a subgroup who place themselves and others at risk for harmful health consequences and also are those least likely to achieve cessation.
What can smoking a pack a day do to you?
- With this study, we have found that people who smoke a pack a day develop an average of 150 extra mutations in their lungs every year, which explains why smokers have such a higher risk of developing lung cancer."
- Mutation signatures associated with tobacco smoking.
Symptoms of a Nicotine Vaping Overdose
- Nausea.
- Stomachache.
- Excessive saliva.
- Quick, heavy breathing.
- Fast heartbeat.
- High blood pressure.
- Pale skin.
- Headache.
Math:
- 1 cigarette = 1 g tobacco = 8 mg nicotine
- 1 ml vape juice = 100 hits
- Avg daily hits = 130
- We have concluded earlier that a cigarette, on average, has around 8 mg of nicotine. Using simple math, we can deduce that a 6mg nicotine strength vape juice in a 60 ml bottle equates to roughly 45 cigarettes.
- 6 mg * 60 ml / 8 mg per cig = 45 cig
Smoking Cessation Messaging
Tobacco Free Florida: Free nicotine replacement therapy like the patch
- 877-U-CAN-NOW (877-777-6534)
- tobaccofreeflorida.com/quityourway
For most people who smoke one pack per day or less, the following is a reasonable starting point:
- More than 15 cigarettes per day: 21 mg patch (Step 1)
- Seven to 15 cigarettes per day: 14 mg patch (Step 2)
- Fewer than seven cigarettes per day: 7 mg patch (Step 3).
How to use patches to stop smoking:
- Apply 1 patch daily (wear it for 24 hours) upon awakening on upper arm or shoulder
- Do not smoke while wearing the patch
- If you feel cravings, you can use gum to help with the cravings
- If you slip up and smoke while wearing the patch: Leave the patch on and throw away the cigarettes
Additional resources: You can use this app to help stop smoking: QuitStart: http://smokefree.gov/apps-quitstart
- The quitSTART app helps you:
- Get ready to quit with tips and information to prepare you for becoming smokefree
- Monitor your progress and earn badges for smokefree milestones and other achievements
- Get back on track if you slip and smoke
- Manage cravings and bad moods in healthy ways
- Distract yourself from cravings with games and challenges
- Store helpful tips, inspirations, and challenges in your Quit Kit
Smoking Cessation with patch edit
Tobacco Free Florida: Free nicotine replacement therapy like the patch
- 877-U-CAN-NOW (877-777-6534)
- tobaccofreeflorida.com/quityourway
I suggest starting with 21 mg patch for 6 weeks; then a 14 mg patch for 2 weeks; then a 7 mg patch for 2 weeks.
How:
- Apply 1 patch daily (wear it for 24 hours) upon awakening on upper arm or shoulder
- Do not smoke while wearing the patch
- If you feel cravings, you can use gum to help with the cravings
- If you slip up and smoke while wearing the patch: Leave the patch on and throw away the cigarettes
From CDC
- For best results, make sure you start on the right dose. The nicotine patch comes in three strengths (7 mg, 14 mg, 21 mg). The right dose for you depends on how much you currently smoke. If you smoke more than 10 cigarettes per day, consider starting on the 21 mg patch. Don't wear two patches at once unless directed to do so by your healthcare provider. Over time (typically after 8 to 12 weeks), you should lower the dose with the goal of stopping use of the patch completely.
- The nicotine patch is typically worn for 24 hours. The patch can even be worn when showering or bathing. When you wake up, put a fresh patch on clean skin and wear it for a full 24 hours. If you find that you are having vivid dreams or that your sleep is disturbed, you can take the patch off before bed and put a new one on the next morning.
- Put the patch on clean, dry, hair-free skin on the upper body. Usual places to put the patch are the upper chest, upper arm, shoulder, back, or inner arm. Avoid putting the patch on areas of irritated, oily, scarred, or damaged skin. Remove the patch from the foil package, peel off the protective strips, and immediately apply the patch to your skin. Press down to ensure the patch sticks to your skin.
- Wash your hands with soap and water after you apply the patch to wash away any nicotine you may have gotten on your fingers when applying the patch.
- To avoid skin irritation, put the patch on a different area of your upper body each day. Avoid wearing the patch in the same place more than once per week. If the patch loosens or falls off, replace it with a new one.
- When changing your patch, remove the patch carefully and dispose of it by folding it in half with the sticky sides touching. Then apply a new patch to a different part of your upper body.
- Keep out of reach of children and pets. Nicotine patches – even used patches – may have enough nicotine to make children and pets sick. In case of accidental use or ingestion, contact a Poison Control Center right away (1-800-222-1222).
- Combine the patch with nicotine gum or lozenge to better manage cravings. You can start using both the patch and gum or lozenge, or you can add gum or lozenge later, if you continue to have withdrawal symptoms. Patches can provide a steady level of nicotine in the body to help lessen withdrawal, while the gum or lozenge can be used to more quickly relieve cravings as they happen.
- If you have a lot of cravings while using the patch, you may not be using a strong enough dose. Consider stepping up to a higher dose. If you are already on the highest dose, talk with your doctor or other healthcare provider for help with dosing. You can also consider adding gum or lozenge, as described above.
- What if I slip up and smoke while using the patch? You do not need to stop using the patch if you slip up and smoke while wearing it. Throw away your cigarettes and get back on track with your quit attempt. Keep using the patch as directed above.
- For best results, use the nicotine patch as part of a program that includes coaching support. Talk with your healthcare provider and connect with your state tobacco quitline (1-800-QUIT-NOW) for help.
For most people who smoke one pack per day or less, the following is a reasonable starting point:
- More than 15 cigarettes per day: 21 mg patch (Step 1)
- Seven to 15 cigarettes per day: 14 mg patch (Step 2)
- Fewer than seven cigarettes per day: 7 mg patch (Step 3).
People who smoke one pack per day absorb 1.8 mg to 26.8 mg of nicotine (usually 16 mg to 20 mg), depending on how they smoke.
For a patient who smokes heavily, a good starting point is to recommend one 21 mg patch per pack of cigarettes smoked per day.
If a patient experiences symptoms of withdrawal on a 21 mg patch, the dose should be increased. Recommend that the patient increase the dose in 7 mg increments, every three to seven days.
Patients who smoke two packs per day will experience a reduction in nicotine levels if they use 42 mg of nicotine (two 21 mg patches) daily.
The Nicotine Dependence Clinic at the Centre for Addiction and Mental Health routinely uses doses from 21 mg to 42 mg (in addition to immediate-release NRT as needed). Doses as high as 84 mg (four 21 mg patches) have been used successfully with patients who smoke very heavily.
Significantly higher smoking cessation rates have been observed with high-dose nicotine patches (more than 22 mg) compared with standard dose nicotine patches (less than 22 mg) (Canadian Agency for Drugs and Technologies in Health, 2014).
Duration of NRT It is recommended that the patch and other forms of replacement should be used for as long as needed to maintain or prolong abstinence. The Lung Health study demonstrated that long-term NRT use is safe (Murray et al., 2009).
NRT product monographs recommend approximately two to three months of use, which is the length of time these products were used in early clinical trials. Many patients are not ready to stop using NRT after three months.
To prevent relapse, patients should be instructed to taper off NRT slowly. This helps them adjust to lowering nicotine levels (e.g., three to four weeks for every level).
Reference:
Vocal Cord Dysfunction
- Inspiratory wheezing/stridor
- Video for relaxation: https://youtu.be/cKHd935oRBg
Radiology
See also: Codes to help with radiology
American College of Radiology. Incidental findings. Accessed April 5, 2020. https://www.acr.org/Clinical-Resources/Incidental-Findings
| Imaging modality | Radiation dose (mSv) | Number of posteroanterior chest radiographs for equivalent exposure | Hours of commercial air travel for equivalent exposure |
|---|---|---|---|
| Plain radiography | |||
| Chest (posteroanterior view) | 0.02 | 1 | 6.7 |
| Lumbar spine (three views) | 1.5 | 75 | 500 |
| Upper gastrointestinal series | 6 | 300 | 2000 |
| Cardiac catheterization (diagnostic/stent) | 07/15/21 | 350/750 | 2,300/5,000 |
| Computed tomography | |||
| Head | 2 | 100 | 650 |
| Cervical spine | 3 | 150 | 1000 |
| Chest | 7 | 350 | 2300 |
| Virtual colonoscopy | 10 | 500 | 3300 |
| Abdomen/pelvis | 14 | 700 | 4650 |
| Pulmonary embolism protocol | 15 | 750 | 5000 |
| Cardiac angiography | 16 | 800 | 5300 |
| Dual energy x-ray absorptiometry (with computed tomography) | 0.04 | 2 | 13 |
| Mammography | 0.4 | 20 | 130 |
| Nuclear stress test (thallium) | 40.7 | 2035 | 13550 |
| Nuclear stress test (sestamibi one-day) | 9.4 | 470 | 3100 |
| Panoramic dental radiography | 0.01 | 0.5 | 3.3 |
| Organization | Description | Website |
|---|---|---|
| ACR Appropriateness Criteria | Evidence-based guidelines to assist clinicians in making appropriate imaging decisions | https://www.acr.org/Clinical-Resources/ACR-Appropriateness-Criteria |
| American Society of Radiologic Technologists | Radiation risk calculator | https://www.xrayrisk.com/calculator/calculator.php |
| Image Gently | Provides information and free educational materials to reduce unnecessary imaging studies in children | https://www.imagegently.org |
| Image Wisely | Encourages clinicians to optimize the amount of radiation used in medically necessary imaging studies and to eliminate unnecessary procedures in adults | https://www.imagewisely.org |
| Radiologyinfo.org | Patient-centered website through the ACR that gives radiation doses of conventional imaging studies | https://www.radiologyinfo.org/en/info.cfm?pg=safety-xray#safety-effective-dose-adults |
| University of California San Diego Department of Radiology | Radiation risk calculator; ideal for principal investigators and informed consent in research trials | https://ehs.ucsd.edu/Radiation_Risk/request/home |
References:
- AFP Jan 2021 Vol 103 No 1
Echocardiogram
- If LA >4 cm with AF -> More likely to stay in AF
- PAP >35 mm = Pulmonary HTN
- Ejection fraction:
- EF <40 - Heart failure with reduced EF (HFREF)
- EF >40 - Heart failure with preserved EF
IV Contrast Pre-treatment for Contrast Allergy
Pretreatment:
- prednisone, 50 mg
- 13 hr before the procedure
- 7 hr before the procedure
- 1 hr before the procedure
- diphenhydramine 50 mg
- 1 hr before the procedure.
Notes:
- Prednisone doses may be distributed unevenly to allow the patient to get a reasonable night's sleep the evening prior to the exam; however, the first dose should be taken more than 11 hours before the time the exam is scheduled to be performed.
- It is not critical to administer diphenhydramine as part of the premedication regimen (there are published regimens using corticosteroids only)
Reference:
- Greenberger PA, Patterson R, Radin RC. Two pretreatment regimens for high-risk patients receiving radiographic contrast media. J Allergy Clin Immunol. 1984 Oct;74(4 Pt 1):540-3. doi: 10.1016/0091-6749(84)90391-9. PMID: 6491099.
With or Without Contrast: CT
Indications for Non-contrast CT Contrast is not used in patients with head, extremity or spine trauma. It is also not used in patients with suspected acute stroke. Finally, imaging of the abdomen and pelvis to assess for renal stones also does not require CT contrast.
- Here is a summary of the indications for non-contrasted CT:
- Brain – Trauma, headache, bleeding, shunt check, mental status change
- Sinuses – Pain, congestion, sinusitis
- Orbits – Trauma, fracture, foreign body
- Facial Bones – Trauma, pain
- Chest – Nodule, cough, pain
- Abdomen and Pelvis – Hematuria with pain, renal stone
- Spine – Pain, trauma, fracture
- Extremities – Fracture, fusion, malunion
- Pelvis – Trauma, fracture, pain
Indications for Contrasted CT Contrast helps enhance certain body structures. Almost always, CTs should be ordered with or without contrast, not both.
- Here is an overview of the indications for contrasted CT:
- Orbits – Infection, mass
- Neck – Mass, adenopathy
- Chest – Mass, cancer/metastatic workup, lymphoma, sarcoid
- Abdomen and Pelvis – Pain, colitis, Crohn's, appendicitis, tumor, cancer, mass
Indications for CT Angiography CT Angiography, or CTA, is a type of contrasted CT scan used to evaluate the blood vessels.
- An overview of the following CTA studies and their indications:
- Abdominal Aorta (CTA Abdomen) – Aneurysm, dissection, post stent grafting, renal artery stenosis, metastatic stenosis
- Pulmonary Arteries (CTA Chest) – Aneurysm, dissection, chest pain, dyspnea, pulmonary embolism
- Thoracic Aorta (CTA Chest and Abdomen with Runoff) – Tachypnea, hemoptysis, dyspnea, pulmonary hypertension, DVT
- Lower Extremities (CTA Abdomen and Runoff) – Peripheral artery disease, DVT
- Carotid (CTA Neck) – stenosis, bruit, TIA, CVA, vascular tumor
- Brain (CTA Head) – Aneurysm, TIA, CVA, intracranial hemorrhage
| Exam | Contrast | Signs and Symptoms |
|---|---|---|
| Abdomen and Pelvis C+ | With Contrast | Generalized abdomen or pelvic pains. Colon issues. Small bowel problems (enterography) |
| Abdomen C+/C- (organ specific) Liver, Pancreas, or Kidneys | With/Without Contrast | Liver mass, acute pancreatitis, renal mass |
| Abdomen C+ | With Contrast | Upper abdomen pains, chronic pancreatitis, f/u prior scans |
| Chest/Abdomen/Pelvis C+ | With Contrast | Cancer, restaging, fevers, pains KUB (stone) History of stones, hematuria, flank pains |
| Chest C+ | With Contrast | Initial lung nodule scan, cancer |
| Chest C- | Without Contrast | Lung screening, f/u prior nodules etc. |
| Chest HIRES | Interstitial lung disease, pulmonary fibrosis, etc. | |
| CTA Chest for PE | R/o pulmonary embolism | |
| ST Neck C+ | With Contrast | Cancer, swollen glands, soft tissue pains |
| Head C- | Without Contrast | Headaches, migraines, trauma, bleed |
| Head C-/C+ | With/Without Contrast | R/o mass, abscess |
| C-Spine | Without | Trauma, cervical pains |
| L-Spine | Without | Trauma, lumbar pains |
| Heart Calcium Scoring | Without | |
| Mastoids C- | Without | |
| Sinus Landmarx Complete | Without | Pre-op |
| Sinus LTD | Without | Sinusitis |
Reference:
With or Without Contrast: MRI
| Category | Diagnosis | IV Contrast | Suggested Exam |
|---|---|---|---|
| Brain/Facial | Acoustic Neuroma/Schwannoma | Yes | MRI Brain With and Without |
| Acute CVA/TIA | No | MRI Brain Without | |
| Acute Headache | No | MRI Brain Without | |
| Aneurysm | No | MRI Brain Without | |
| Anosmia (Loss of Smell) | Yes | MRI Brain With and Without | |
| Aphasia (Speech Difficulty) | No | MRI Brain Without | |
| Arnold Chiari Malformation | No | MRI Brain Without | |
| Bells Palsy | Yes | MRI Brain With and Without | |
| Brain Tumor | Yes | MRI Brain With and Without | |
| Cancer (Any Type) | Yes | MRI Brain With and Without | |
| Concussion | No | MRI Brain Without | |
| Cushings | Yes | MRI Brain With and Without | |
| CVA/TIA | No | MRI Brain With and Without | |
| Dementia | No | MRI Brain With and Without | |
| Diplopia (Double Vision) | Yes | MRI Brain With and Without | |
| Facial Pain | Yes | MRI Brain With and Without | |
| Hearing Loss | Yes | MRI Brain With and Without | |
| Hemifacial Spasm | Yes | MRI Brain With and Without | |
| History of Cancer/Mets | Yes | MRI Brain With and Without | |
| HIV/AIDS | Yes | MRI Brain With and Without | |
| Hypogonadism | Yes | MRI Brain With and Without | |
| Infection | Yes | MRI Brain With and Without | |
| Intracranial Hemorrhage | No | MRI Brain Without | |
| Meningioma | Yes | MRI Brain With and Without | |
| Multiple Sclerosis | Yes | MRI Brain With and Without | |
| Orbit Cancer/Mass Tumor | Yes | MRI Brain With and Without | |
| Parkinsons | No | MRI Brain Without | |
| Pituitary | Yes | MRI Brain With and Without | |
| Seizure/Epilepsy | Yes | MRI Brain With and Without | |
| Syncope | No | MRI Brain Without | |
| Tic de Leroux | Yes | MRI Brain With and Without | |
| Tinnitus | Yes | MRI Brain With and Without | |
| Trauma/Hematoma | No | MRI Brain Without | |
| Trigeminal Neuralgia | Yes | MRI Brain With and Without | |
| Vertigo/Dizziness | No | MRI Brain Without | |
| Neck | All soft tissue neck protocols | Yes | MRI Neck With and Without |
| Spine | Bone Tumor/Mets | Yes | MRI Cervical, Thoracic or Lumbar With and Without |
| Discitis | Yes | MRI Cervical, Thoracic or Lumbar With and Without | |
| Extremity Numbness/Tingling | No | MRI Cervical, Thoracic or Lumbar Without | |
| History of Lumbar Surgery | Yes | MRI Lumbar With and Without | |
| Multiple Sclerosis | Yes | MRI Cervical or Thoracic With and Without | |
| Osteomyelitis/Infection | Yes | MRI Cervical, Thoracic or Lumbar With and Without | |
| Radiculopathy/Stenosis | No | MRI Cervical, Thoracic or Lumbar Without | |
| Syrinx | Yes | MRI Cervical or Thoracic With and Without | |
| Transverse Myelitis | Yes | MRI Cervical, Thoracic or Lumbar With and Without | |
| Abdomen | All Abdomen Protocols | Yes | MRI Abdomen With and Without |
| The Exception: If biliary ducts in question | No | MRCP Without – This can be done in conjunction with an abdomen without and with if needed, or just by itself. | |
| Pelvis | Bone for Cancer/mets | Yes | MRI Pelvis With and Without |
| Bone for Fracture | No | MRI Pelvis Without | |
| Fibroids | Yes | MRI Pelvis With and Without | |
| Lumbar Plexis | No | MRI Pelvis Without | |
| Mass/Tumor/Mets | Yes | MRI Pelvis With and Without | |
| Ovarian/Uterine Cancer | Yes | MRI Pelvis With and Without | |
| Pelvic Floor Dysfunction | No | MRI Pelvis Without | |
| Prostate Cancer | Yes | MRI Pelvis With and Without | |
| Pectocelle | No | MRI Pelvis Without | |
| Sciatica | No | MRI Pelvis Without | |
| Urinary Incontinence | No | MRI Pelvis Without | |
| Extremities | Bone Tumor/Mets | Yes | Appropriate Body Part With and Without |
| Lypoma | Yes | Appropriate Body Part With and Without | |
| Myositis | Yes | Appropriate Body Part With and Without | |
| Pain Muscle/Tendon Tear | No | Appropriate Body Part Without | |
| Soft Tissue Mass | Yes | Appropriate Body Part With and Without | |
| Trauma Fracture | No | Appropriate Body Part Without | |
| If Arthrogram Indicated: | Yes | Appropriate Body Part With Shoulder for Labral Tear | |
| Wrist for TFCC Tear | |||
| Hip for Labral Tear |
Ultrasound at point of care (POCUS)
Point of Care Ultrasound (POCUS)
Educational Videos:
- Intro to echocardiology: https://youtu.be/JMocr_oz1Jo
- Parasternal long-axis view: https://youtu.be/mZtK4PMdacE
- Ultrasound of the IVC: https://youtu.be/Q6CIG3v28Y
- Overview of lung ultrasound: https://youtu.be/WOIz8-km6hE
- Evaluation of the abdominal aorta: https://youtu.be/8EB0Au3I4AM
- Limited examination of the lower extremity venous system for DVT: https://youtu.be/M0JmjOOg10M
POCUS
| Protocol | Sensitivity | Specificity | Training Requirement |
|---|---|---|---|
| Evaluation of LV systolic function | 69-94% | 91-94% | 8 hrs of training or 20 practice exams |
| Evaluatino of IVC to determine volume status | 81% | 72% | 4 hrs of training or 20 practice exams |
| and predict readmission for CHF | |||
| Evaluation for pleural effusion | 94% | 98% | 3 hrs of training |
| Evaluation for pneumonia | 90-96% | 88-93% | 3 hrs of training |
| Evaluation for pulmonary edema | 86-100% | 92-98% | 5 practice exams |
| Screening exam for AAA | 100% | 100% | 50 practice exams |
| Evaluation for proximal leg DVT | 95% | 96% | 10 min to 5 hrs of training |
POCUS Use:
- Lung
- Source of acute respiratory distress
- Uterus
- R/o ectopic pregnancy
- Skin
- Differentiate cellulitis from abscess
- Reduce inappropriateness of incision and drainage and failure to resolve postdrainage
Resources to Learn:
- 5 Min Sono
- American College of Emergency Physicians
- European Society of MSK Radiology
- Sonospot
- Ultrasound Ninja
References:
- JFP Vol 67 No 2 Feb 2018
- AFP Mar 2020 Vol 101 No 5
- AFP Vol 103 No 5 Mar 2021
Ultrasound
- Sonosite learning institute: This on-line learning site includes videos, modules, and practice information (like reimbursement/coding, etc). It is free if you own a machine, but you need to create an individual account. You may use any e-mail address you would like. The "serial number" on the registration page is: 04C1TQ. The model is an X-porte.
- Education night: 2/1/2018 – Orlando Science Center
Rheumatology
Discoid Lupus Erythematosus
The best management for discoid lupus erythematosus (DLE) involves a combination of photoprotection, topical therapies, and systemic treatments.
First-line treatment includes:
- Photoprotection: Patients should be advised to use broad-spectrum sunscreens and wear protective clothing to minimize ultraviolet exposure, which can exacerbate lesions.[1-2]
- Topical corticosteroids: Potent topical corticosteroids, such as fluocinonide 0.05%, are commonly used and have been shown to be more effective than low-potency steroids like hydrocortisone 1%.[3]
- Topical calcineurin inhibitors: Agents like tacrolimus and pimecrolimus can be used, especially in areas where skin atrophy from steroids is a concern.[3]
Systemic treatments include:
- Antimalarials: Hydroxychloroquine (400 mg daily) is the first-line systemic treatment and is effective in many patients. In cases where hydroxychloroquine is ineffective, chloroquine or quinacrine can be considered.[3-5]
- Retinoids: Acitretin (initially 10 mg daily, increased to 25 mg if needed) has shown efficacy in patients who are refractory or intolerant to antimalarials.[6]
- Immunosuppressive agents: For refractory cases, medications such as methotrexate, azathioprine, mycophenolate mofetil, and cyclophosphamide may be used.[1-2]
- Thalidomide: This can be considered for chronic refractory DLE, although its use is limited due to teratogenicity and risk of polyneuropathy.[7]
Other options:
- Intravenous immunoglobulin (IVIG): This has been used successfully in refractory cases, although more research is needed to establish its efficacy.[8]
- Rapamycin: This may be considered for severe or generalized DLE resistant to conventional treatments.[9]
Overall, the choice of treatment should be individualized based on the severity of the disease, patient tolerance, and response to previous therapies.
Reference:
- Panjwani S. Early Diagnosis and Treatment of Discoid Lupus Erythematosus. Journal of the American Board of Family Medicine : JABFM. 2009 Mar-Apr;22(2):206-13. https://doi.org/10.3122/jabfm.2009.02.080075.
- Fabbri P, Cardinali C, Giomi B, Caproni M. Cutaneous Lupus Erythematosus: Diagnosis and Management. American Journal of Clinical Dermatology. 2003;4(7):449-65. https://doi.org/10.2165/00128071-200304070-00002.
- Jessop S, Whitelaw DA, Grainge MJ, Jayasekera P. Drugs for Discoid Lupus Erythematosus. The Cochrane Database of Systematic Reviews. 2017;5:CD002954. https://doi.org/10.1002/14651858.CD002954.pub3.
- Wahie S, Meggitt SJ. Long-Term Response to Hydroxychloroquine in Patients With Discoid Lupus Erythematosus. The British Journal of Dermatology. 2013;169(3):653-9. https://doi.org/10.1111/bjd.12378.
- Kuhn A, Ruland V, Bonsmann G. Cutaneous Lupus Erythematosus: Update of Therapeutic Options Part I. Journal of the American Academy of Dermatology. 2011;65(6):e179-93. https://doi.org/10.1016/j.jaad.2010.06.018.
- Laosakul K, Chiewchanvit S, Chuamanochan M, Tovanabutra N. Acitretin Treatment in Antimalarial-Refractory/Intolerant Discoid Lupus Erythematosus: A Prospective, Open-Label, Uncontrolled Study. Lupus. 2022;31(5):575-581. https://doi.org/10.1177/09612033221086878.
- Tran B, Yazdani Abyaneh MA, Wu J. Rapid Response to Treatment With Thalidomide in an Adolescent With Generalized Discoid Lupus Erythematosus. Pediatric Dermatology. 2020;37(1):244-245. https://doi.org/10.1111/pde.14067.
- Tenti S, Fabbroni M, Mancini V, et al. Intravenous Immunoglobulins as a New Opportunity to Treat Discoid Lupus Erythematosus: A Case Report and Review of the Literature. Autoimmunity Reviews. 2018;17(8):791-795. https://doi.org/10.1016/j.autrev.2018.02.010.
- Herold M, Richmond NA, Montuno MA, Wesson SK, Motaparthi K. Rapamycin for Refractory Discoid Lupus Erythematosus. Dermatologic Therapy. 2018;31(5):e12631. https://doi.org/10.1111/dth.12631.
Ehlers-Danlos Syndrome
Beighton Hypermobility Score:
- Ability to passively dorsiflex the 5th metacarpophalangeal joint 90+ degrees (1 pt right side; 1 pt left side)
- Ability to oppose the thumb to the volar aspect of the ipsilateral forearm (1 pt right side; 1 pt left side)
- Ability to hyperextend the elbow joint >10 degrees (1 pt right side; 1 pt left side)
- Ability to hyperextend the knee joint >10 degrees (1 pt right side; 1 pt left side)
- Ability to place hands flat on the floor by bending forward with knees fully extended (1 pt)
Total out of 9 points
Generalized Joint Hypermobility:
- Beighton score 6+ in prepubertal children and adolescents
- Beighton score 5+ from puberty up to 50 years
- Beighton score 4+ in persons older than 50
- Add 1 point if 5-point questionnaire is positive
- 5-Point Questionnaire: Positive if yes to 2 or more
- Can you now (or could you ever) place your hands flat on the floor without bending your knees?
- Can you now (or could you ever) bend your thumb to touch your forearm?
- As a child, did you amuse your friends by contorting your body into strange shapes or could you do the splits?
- As a child or teenager, did your shoulder or kneecap dislocate on more than one occassion?
- Do you consider yourself double-jointed?
- 5-Point Questionnaire: Positive if yes to 2 or more
Therapy Goals:
- Manage symptoms
- Prevent joint injury
- Teach patients about their condition
Use:
- Patient education
- PT/OT
- Psychological support
- Self-management
Fibromyalgia
Points for Diagnosis
- Widespread pain involving both sides of body, above and below the waist as well as the axial skeletal system for at least 3 mo
- Presence of 11 tender points amont the 9 pairs of specified sites:
- Anterior aspects of C5, C7 intertransverse spaces
- Upper border of trapezius mid portion
- Second rib space about 3cm lat to sternal border
- Muscle attachments to lateral epicondyle
- Medial fat pad of knee proximal to joint line
- Insertion of nuchal muscles into occiput
- Muscle attachments to upper medial border of scapula
- Upper outer quadrant of gluteal muscles
- Muscle attachments just posterior to greater trochanter
Notes:
- Pressure should just blanch the examiner's finger
- DDx: myofascial pain syndrome, chronic fatigue syndrome, hypothyroidism
Medications:
- Pregabalin in daily doses of 300mg, 450mg, and 600mg reduces pain (high quality evidence)
- Most effective dose is 450mg
- NNT = 9.7
- NNH = 11
- Low dose Naltrexone
- Doses as low as 5.4 mg were found to reduce pain in 95% of patients with fibromyalgia (SOR, B; single prospective dose-response study).
References:
- AFP Vol 76 No 2 Jul 2007
- J Fam Pract. 2023 September;72(7):320-321 | doi: 10.12788/jfp.0654
Fibromyalgia Management
All patients:
- Education on the disorder (LOE 1A)
- Counseling regarding the role of exercise (LOE 1A) and CBT (LOE 1A)
Pharmacology:
- All should have a good trial of a low-dose TCA (LOE 1A)
- Amitriptyline should be preferred for comorbid sleep disturbances
- amitriptyline 5-10 mg qhs (recommended dose 20-30 mg qhs)
- Those with co-morbid depression or fatigue should then try a SNRI (LOE 1A)
- Duloxetine should be preferred for comorbid depression, fatigue, and overall reduction of pain
- duloxetine 20-30 mg qAM (recommended dose 60 mg qAM)
- Those with co-morbid anxiety or sleep issues should then try a gabapentinoid (LOE 1A)
- Co-morbid peripheral pain generators can be managed with NSAIDs and acetaminophen
- Opioid are discouraged (LOE 5D)
| Efficacy | Drug | Dose |
|---|---|---|
| Strong | Amitriptyline | 25-50mg qhs |
| Cyclobenzaprine | 10-30mg qhs | |
| Modest | Duloxetine | 30-60mg qd |
| Gabapentin | 1200-2400mg qd | |
| Milnacipran | 100mg qd | |
| Pregabalin | 300-450mg qd | |
| SSRI | 20-80mg qd | |
| Tramadol | 200-300mg qd | |
| Weak | NSAID | |
| Opioids |
Fibromyalgia Management Evidence:
- Strong evidence:
- Amitriptyline 25-50 mg qhs
- Cyclobenzaprine 10-30 mg qhs
- CBT
- Patient education
- Moderate evidence:
- Duloxetine (SNRIs)
- NNT 6-10 for 30% improvement
- NNT 7-14 for 50% improvement
- Fluoxetine 20-80 mg qhs with or without a TCA
- Pregabalin
- In a systematic review of the antiepileptic medications used for fibromyalgia, only pregabalin was shown to have moderate efficacy
- NNT 6-10 for 30% improvement
- NNT 7-14 for 50% improvement
- Acupuncture
- Biofeedback
- Aerobic Exercise
- Moderate-quality evidence (based upon 2400 patients throughout 34 trials and 47 various exercise interventions) has demonstrated that aerobic exercise can decrease pain intensity, enhance physical function, and reduce the severity of fatigue.
- Strength training
tramadol 200-300 mg dailywith or without acetaminophen
- Duloxetine (SNRIs)
- No evidence:
- Corticosteroids
- Melatonin
- NSAIDs
- Opioids
- Thyroid hormone
- Flexible exercise
- Trigger point injections
References:
- AFP Vol 107 No 6 Jun 2023
- Jones EA, Asaad F, Patel N, Jain E, Abd-Elsayed A. Management of Fibromyalgia: An Update. Biomedicines. 2024 Jun 6;12(6):1266. doi: 10.3390/biomedicines12061266. PMID: 38927473; PMCID: PMC11201510.
- JAMA Vol 311 No 15 Apr 2014
- JAMA 2004;292
- AFP Vol 76 No 2 Jul 2007
- AFP Ovt 2025 Vol 112 No 4
Gout
Short term management:
- Colchicine
- NSAIDs (indomethacin)
Lifestyle changes:
- Coffee is good (as long as no sugar)
- Avoid meat and seafood
- Estrogen is protective
- Limiting alcoholic beverages and drinks sweetened with fruit sugar (fructose). Instead, drink plenty of nonalcoholic beverages, especially water.
- Limiting intake of foods high in purines, such as red meat, organ meats and seafood.
- Exercising regularly and losing weight. Keeping your body at a healthy weight reduces your risk of gout.
Certain foods have been studied for their potential to lower uric acid levels, including:
- Coffee. Studies have found an association between coffee drinking — both regular and decaffeinated coffee — and lower uric acid levels, though no study has demonstrated how or why coffee may have such an effect.
- The available evidence isn't enough to encourage noncoffee drinkers to start, but it may give researchers clues to new ways of treating gout in the future.
- Vitamin C. Supplements containing vitamin C may reduce the levels of uric acid in your blood. However, no studies have demonstrated that vitamin C affects the frequency or severity of gout attacks.
- Cherries. Cherries have been reported to lower levels of uric acid, as well as reduce the number of gout attacks. However, more research needs to be done to confirm this.
Long term management:
- Can never stop management - Once have gout, always have gout - Chronic disease
- Allopurinol
- Cut down in 100mg increments (follow monthly)
- Goal = <6
- Krystexxa (pegloticase) - recombinant uric acid enzyme, breaks down uric acid
- Infusion center (8mg IV q2wks)
- Measure G6PD Quant before prescribing
- 6mo of treatment - stop when tophi resolved
- Stop uric acid lowering medications (like allopurinol)
Reference:
- FAFP CME 2019 (pharm lunch)
Gout
Lifestyle modifications to prevent recurrent gout include reducing the consumption of high-fructose soft drinks, fruit juices, fruits, and purine-rich foods (e.g., anchovies, sardines, scallops, mussels, bacon, beef, liver, turkey, veal, venison). LOE C
A validated clinical prediction rule (Table 3) should be used to determine the likelihood of gout based on the presence of typical signs and symptoms and the uric acid level. LOE C
Nonsteroidal anti-inflammatory drugs and corticosteroids are equally effective for the treatment of acute gout, with no significant difference in pain relief or adverse effects. LOE B
In acute gout, low-dose colchicine (1.2 mg followed by 0.6 mg in 1 hour) is as effective as high-dose colchicine (1.2 mg followed by 0.6 mg every hour for 6 hours) with fewer adverse effects. LOE B
Allopurinol is the preferred first-line urate-lowering therapy to prevent recurrent gout. It is as effective as febuxostat (Uloric) in preventing gout flare-ups; however, febuxostat increases all-cause and cardiovascular mortality. LOE A
The allopurinol hypersensitivity assay, or HLA-B*58:01 test, should be considered in select patients (Korean adults with stage 3 or higher chronic kidney disease and all adults of Han or Thai descent) before initiating allopurinol therapy. LOE C
Lifestyle Therapy
- The Dietary Approaches to Stop Hypertension (DASH) diet was associated with a lower risk of developing gout in a prospective cohort study in men during 26 years of follow-up (N = 44,444; adjusted relative risk when comparing the highest fifth to the lowest fifth of the DASH dietary pattern score = 0.68; 95% CI, 0.57 to 0.80).
- Behavior modifications should be recommended, including a low-fat, low-purine diet; avoidance of alcohol; weight loss if overweight; increased exercise; and avoidance of soft drinks and foods containing fructose. Consumption of skim milk and low-fat yogurt, vegetables, soybeans, vegetable sources of protein, and cherries is recommended.
- Local ice therapy reduces pain in acute gouty arthritis.
Pharmacologic Therapy: Acute Episode
- Colchicine, nonsteroidal anti-inflammatory drugs, and corticosteroids relieve pain in adults with acute gout.
- Nonsteroidal anti-inflammatory drugs are first-line treatment unless use is contraindicated (e.g., cardiovascular disease, cerebrovascular disease, chronic kidney disease, history of gastric bypass, history of gastrointestinal bleeding, inflammatory bowel disease, peptic ulcer disease, pregnancy).
- Oral prednisolone (35 mg once daily) is equal to naproxen (500 mg twice daily) in the treatment of acute gout, with no significant difference in pain relief or adverse effects.
- In acute gout, low-dose colchicine (1.2 mg orally followed by 0.6 mg one hour later) was as effective as high-dose colchicine (1.2 mg followed by 0.6 mg every hour for six hours) and had fewer adverse effects. Nearly 77% of patients treated with high-dose colchicine reported adverse effects (mostly diarrhea) compared with 36% in the low-dose colchicine group and 27% in the placebo group.
References:
- AFP Nov 2020 Vol 102, No 9
Gout
| Portion | Relative risk (95% CI) |
|---|---|
| Alcohol: | |
| Beer 335 ml | 1.49 (1.32 to 1.70) |
| Spirits 44 ml | 1.15 (1.04 to 1.28) |
| Wine 118 ml | 1.04 (0.88 to 1.22) |
| Food: | |
| Meat | 1.21 (1.04 to 1.41) |
| Seafood (fish)* | 1.07 (1.01 to 1.12) |
| Purine rich vegetables | 0.97 (0.79 to 1.19) |
| Total dairy products | 0.82 (0.75 to 0.90) |
| Low fat dairy products | 0.79 (0.71 to 0.87) |
| High fat dairy products | 0.99 (0.89 to 1.10) |
Reference:
- Underwood M. Diagnosis and management of gout. BMJ. 2006 Jun 3;332(7553):1315-9. doi: 10.1136/bmj.332.7553.1315. PMID: 16740561; PMCID: PMC1473078.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1473078/
- Gout Diagnosis
American College of Rheumatology preliminary criteria for the clinical diagnosis of gout
Six or more of these criteria are needed to make a diagnosis:
- More than one attack of acute arthritis
- Maximum inflammation developed within one day
- Attack of monoarthritis
- Redness over joints
- Painful or swollen first metatarsophalangeal joint
- Unilateral attack on first metatarsophalangeal joint
- Unilateral attack on tarsal joint
- Tophus (proved or suspected)
- Hyperuricaemia
- Asymmetric swelling within a joint on radiograph
- Subcortical cysts without erosions on radiograph
- Joint fluid culture negative for organisms during attack
Table 220: Investigations to consider for patients with gout Test Comment Serum urate concentration Level may go down during an acute attack Full blood count To exclude myeloproliferative disorders; raised white cell count may indicate septic arthritis Renal function Hyperuricaemia can occur in renal failure; reduce dose of allopurinol Fasting lipids, glucose, and thyroid function Hyperlipidaemia, diabetes, hypothyroidism, and possibly hyperthyroidism are associated with gout13,15 Urinary urate excretion Uricosurics are contraindicated in patients with high urinary excretion of urate. Some authorities advise measuring this if the serum urate concentration is >0.8 mmol/l because of risk of renal stone formation Reference:
- Underwood M. Diagnosis and management of gout. BMJ. 2006 Jun 3;332(7553):1315-9. doi: 10.1136/bmj.332.7553.1315. PMID: 16740561; PMCID: PMC1473078.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1473078/
- Uric Acid Levels
Factors that decrease serum urate concentration
- Diet: low fat dairy products
- Drugs: xanthine oxidase inhibitors (allopurinol, febuxostat), uricosuric drugs (sulfinpyrazone), uricase drugs (rasburicase), coumarin anticoagulants, and oestrogens
Factors that increase serum urate concentration
- Diet: meat, fish, alcohol (particularly beer and spirits), obesity, and weight gain
- Drugs: including diuretics, low dose salicylates, pyrazinamide, ethambutol, cytotoxics, and lead poisoning
- Disease: increased purine turnover—myeloproliferative and lymphoproliferative disorders, chronic haemolytic anaemia, haemoglobinopathies, secondary polycythaemia, thalassaemia; increased purine synthesis—glucose-6-phosphate dehydrogenase deficiency, Lesch-Nyhan syndrome; reduced renal excretion—hypertension, hypothyroidism, sickle cell anaemia, hyperparathyroidism, chronic renal disease
Reference:
- Underwood M. Diagnosis and management of gout. BMJ. 2006 Jun 3;332(7553):1315-9. doi: 10.1136/bmj.332.7553.1315. PMID: 16740561; PMCID: PMC1473078.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1473078/
- Treatment
Treatment of acute gout
- Patients presenting with acute gouty arthritis who do not have significant renal impairment (creatinine clearance ≤ 50 ml/min or creatinine concentration ≥ 167 μmol/l) or peptic ulcer disease should be treated with one of the following:
- A non-steroidal anti-inflammatory drug
- Adrenocorticotrophic hormone or steroids (systemic or intra-articular)
- Colchicine
Prevention of recurrent gout
- Patients with gout who are obese (body mass index > 28), or who have one or more alcoholic drinks per day, should be advised to lose weight or decrease their alcohol consumption, or both
- When starting allopurinol in patients with major renal impairment, initially use a low dose (< 300 mg/day)
- When coprescribing a xanthine oxidase inhibitor with azothiaprine or 6-mercaptopurine, reduce dose of azothiaprine or 6-mercaptopirine by at least 50%
- When starting a urate lowering drug in patients with gout who do not have major renal impairment (see definition above) or peptic ulcer disease, coprescribe a non-steroidal anti-inflammatory drug or colchicine to reduce the incidence of rebound gout attacks
- Patients with asymptomatic hyperuricaemia do not need treatment
- Uricosuric drugs should not be used in patients with significant renal impairment (see definition above) or a history of renal stones
- Patients with gout and either tophaceous deposits, gouty erosive changes on radiographs, or more than two attacks per year should be offered urate lowering treatment
- Patients with gout who are taking a xanthine oxidase inhibitor should have their serum urate level checked at least once during the first six months of continued use
- Patients taking long term prophylactic oral colchicine who have major renal impairment (see definition above) should have a full blood count and creatine kinase checked at least once every six months
Tips for non-specialists
- Serum urate concentrations can go down during an attack of gout
- Oral steroids may be a safer alternative to non-steroidal anti-inflammatory drugs or colchicine for the management of acute gout
- Urate lowering drugs are usually needed only for patients with frequent attacks of gout
- Asymptomatic hyperuricaemia does not require treatment
Adherence to traditional low purine diets is poor and they are not usually recommended.
Data from the health professionals study, however, suggest that the following relatively simple changes may have an impact on incidence of recurrent gout9-11:
- Lose weight
- Eat one less portion of meat or fish a day
- Drink wine instead of beer
- Drink a glass of skimmed milk a day.
Other Notes:
- Losartan: Losartan is the only angiotensin receptor II blocker (ARB) that the ACR guideline lists as an option for reducing UA concentration.
- Fenofibrate: Fenofibrate, a fibric-acid derivative used as adjunctive therapy to diet for treatment of adults with severe hypertriglyceridemia, reduces UA concentrations by increasing the clearance of hypoxanthine and xanthine, leading to lower urate concentrations.
- Probenecid: Probenecid, a uricosuric agent, increases urinary excretion of UA and decreases serum urate concentrations
- Drug Discontinuation: Stop hctz
Reference:
- Underwood M. Diagnosis and management of gout. BMJ. 2006 Jun 3;332(7553):1315-9. doi: 10.1136/bmj.332.7553.1315. PMID: 16740561; PMCID: PMC1473078.
- https://www.uspharmacist.com/article/treatment-options-for-gout
Gout Diet Recommendations
The general principles of a gout diet follow typical healthy-diet recommendations:
- Weight loss. Being overweight increases the risk of developing gout, and losing weight lowers the risk of gout. Research suggests that reducing the number of calories and losing weight — even without a purine-restricted diet — lower uric acid levels and reduce the number of gout attacks. Losing weight also lessens the overall stress on joints.
- Complex carbs. Eat more fruits, vegetables and whole grains, which provide complex carbohydrates. Avoid foods and beverages with high-fructose corn syrup, and limit consumption of naturally sweet fruit juices.
- Water. Stay well-hydrated by drinking water.
- Fats. Cut back on saturated fats from red meat, fatty poultry and high-fat dairy products.
- Proteins. Focus on lean meat and poultry, low-fat dairy and lentils as sources of protein.
Recommendations for specific foods or supplements include:
- Red meat: Limit serving sizes of beef, lamb and pork.
- Seafood: Some types of seafood — such as anchovies, shellfish, sardines and tuna — are higher in purines than are other types. But the overall health benefits of eating fish may outweigh the risks for people with gout. Moderate portions of fish can be part of a gout diet.
- Vitamin C: Vitamin C may help lower uric acid levels. Talk to your doctor about whether a 500-milligram vitamin C supplement fits into your diet and medication plan.
- Coffee: Some research suggests that drinking coffee in moderation, especially regular caffeinated coffee, may be associated with a reduced risk of gout. Drinking coffee may not be appropriate if you have other medical conditions.
- Cherries: There is some evidence that eating cherries is associated with a reduced risk of gout attacks.
- High-purine vegetables: Studies have shown that vegetables high in purines, such as asparagus and spinach, don't increase the risk of gout or recurring gout attacks.
- Alcohol: Beer and distilled liquors are associated with an increased risk of gout and recurring attacks. Moderate consumption of wine doesn't appear to increase the risk of gout attacks. Avoid alcohol during gout attacks, and limit alcohol, especially beer, between attacks.
- Sugary foods and beverages: Limit or avoid sugar-sweetened foods such as sweetened cereals, bakery goods and candies. Limit consumption of naturally sweet fruit juices.
- Organ and glandular meats: Avoid meats such as liver, kidney and sweetbreads, which have high purine levels and contribute to high blood levels of uric acid.
Reference:
Henoch-Schonlein Purpura - HSP
Diagnostic Criteria
- At least 2 of the following:
- Palpable purpura (mandatory)
- Age =< 20y at disease onset
- Abdominal pain or GI bleeding
- Vessel wall granulocytes on biopsy
- Plus 1 of the following
- Abdominal pain
- Diffuse and colicky
- Histopathology
- Leukocytoclastic vasculitis or proliferative glomerulonephritis with predominant IgA deposition
- Arthritis or arthralgia
- Acute-onset joint pain or swelling
- Kidney involvement
- Proteinuria or hematuria
- Abdominal pain
References:
- Consultant Oct 2016
Labs - Follow up for: ANA+
Antinuclear antibody (ANA) test interpretation requires integration of titer, pattern, and clinical context.
- A negative ANA (<1:80 by indirect immunofluorescence) makes systemic autoimmune disease less likely, but does not fully exclude it, especially in early or limited disease.
- Low-titer positive ANA (≤1:160) is common in healthy individuals, especially older adults, and is often nonspecific.
- High-titer positive ANA (≥1:320) increases specificity for autoimmune diseases such as systemic lupus erythematosus (SLE), but still requires clinical correlation.
The pattern (e.g., homogeneous, speckled, nucleolar) may suggest specific autoantibody associations, but is not diagnostic alone.
- Further testing for disease-specific autoantibodies (e.g., anti-dsDNA, anti-Smith, anti-SSA/Ro) is indicated if clinical suspicion persists.
| ANA Result | Clinical Significance | Next Steps |
|---|---|---|
| Negative | Low likelihood of autoimmune disease | Consider other diagnoses |
| Low-titer Positive | Often nonspecific; common in elderly | Assess clinical context; consider repeat |
| High-titer Positive | Increased specificity for autoimmune disease | Evaluate for specific autoantibodies; correlate with symptoms |
| Specific Pattern | May suggest disease (e.g., homogeneous for SLE, speckled for Sjögren/MCTD) | Order disease-specific autoantibodies |
| Isolated Autoantibody | May be present even if ANA negative | Consider diagnosis if clinical suspicion |
| ANA Titer | % in Gen Pop |
|---|---|
| 1:40 | Up to 33% |
| 1:80 | 10-15% |
| 1:160 | 5% |
| 1:320 | 3% |
The following tests are commonly recommended:
- Anti-double-stranded DNA (anti-dsDNA): Highly specific for systemic lupus erythematosus (SLE).[1-2]
- Extractable Nuclear Antigen (ENA) Panel: Includes antibodies to SSA/Ro, SSB/La, Sm, RNP, Scl-70, and Jo-1, which can help differentiate between various connective tissue diseases such as Sjögren's syndrome, mixed connective tissue disease, and systemic sclerosis.[2-3]
- Complement Levels (C3 and C4): Low levels can indicate active SLE.[1]
- Rheumatoid Factor (RF) and Anti-Cyclic Citrullinated Peptide (anti-CCP): Useful in diagnosing rheumatoid arthritis.[2][4]
- Anticardiolipin Antibodies and Beta-2 Glycoprotein I Antibodies: Important for assessing antiphospholipid syndrome.[1]
- Lupus Anticoagulant: Another marker for antiphospholipid syndrome.[1]
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): General markers of inflammation that can provide additional information about disease activity.[2]
These tests help to confirm the diagnosis of specific autoimmune diseases and to monitor disease activity. The American College of Rheumatology and the European League Against Rheumatism recommend these follow-up tests to provide a comprehensive evaluation of patients with a positive ANA test.[1-2]
Interpreting ANA (antinuclear antibody) patterns involves understanding the distribution of staining on HEp-2 cells, which can indicate different autoimmune conditions.
Common ANA Patterns:
- Homogeneous Pattern: Often seen in patients with lupus or drug-induced lupus.
- Nucleolar Pattern: More frequently observed in patients with scleroderma or myositis.
- Speckled Pattern: Can be indicative of Sjögren's syndrome.
- Centromere Pattern: Common in limited forms of scleroderma, such as CREST syndrome.
Do NOT repeat an ANA test.
Reference:
- Al-Mughales JA. Anti-Nuclear Antibodies Patterns in Patients With Systemic Lupus Erythematosus and Their Correlation With Other Diagnostic Immunological Parameters. Frontiers in Immunology. 2022;13:850759. https://doi.org/10.3389/fimmu.2022.850759.
- Egner W. The Use of Laboratory Tests in the Diagnosis of SLE. Journal of Clinical Pathology. 2000;53(6):424-32. https://doi.org/10.1136/jcp.53.6.424.
- Bossuyt X, De Langhe E, Borghi MO, Meroni PL. Understanding and Interpreting Antinuclear Antibody Tests in Systemic Rheumatic Diseases. Nature Reviews. Rheumatology. 2020;16(12):715-726. https://doi.org/10.1038/s41584-020-00522-w.
- Meyer O. Evaluating Inflammatory Joint Disease: How and When Can Autoantibodies Help?. Joint Bone Spine. 2003;70(6):433-47. https://doi.org/10.1016/j.jbspin.2003.07.004.
Myasthenia Gravis
Lab orders for diagnosis:
- (206) Acetylcholine Receptor Binding Antibody
- (266) Striated Muscle Antibody With Reflex to Titer
Optional:
- ESR
- CRP
- ANA
- RF
- CBC
- Total Testosterone
- TSH
- Free T4
Polymyalgia Rheumatica
Early addition of methotrexate to glucocorticoid shoudl b considered in those:
- with a high risk of relapse (high baseline ESR)
- glucocorticoid related AE
- comorbidities likely to be exacerbated by glucocorticoids
- DM
- Osteoporosis
References:
- AFP Vol 107 No 3 Mar 2023
Raynaud Phenomenon
Management
- Nifedipine - trade off between benefits and harms
- Unknown effectiveness: amlodipine, diltiazem, and nicardipine
References:
- AFP Vol 90, No 6 Sep 2014
Rheumatoid Arthritis
Diagnosis/Workup:
- Criteria for diagnosis include
- having at least one joint with definite swelling that is not explained by another disease.
- The likelihood of a rheumatoid arthritis diagnosis increases with the number of small joints involved.
| Domain | Category | Points |
|---|---|---|
| A | Joint involvement (0–5 points) | |
| 1 large joint | 0 | |
| 2–10 large joints | 1 | |
| 1–3 small joints (large joints not counted) | 2 | |
| 4–10 small joints (large joints not counted) | 3 | |
| >10 joints including at least one small joint | 5 | |
| B | Serology (at least one test needed for classification; 0–3 points) | |
| Negative RF and negative ACPA | 0 | |
| Low positive RF or low positive ACPA | 2 | |
| High positive RF or high positive ACPA | 3 | |
| C | Acute-phase reactants (at least one test needed for classification; 0–1 point) | |
| Normal CRP and normal ESR | 0 | |
| Abnormal CRP or abnormal ESR | 1 | |
| D | Duration of symptoms | |
| <6 weeks | 0 | |
| ≥6 weeks | 1 |
Notes:
- The points from each of domains A through D are added and the sum is considered to be the total score.
- A total score of ≥6 is needed to classify a patient as having definite RA.
- Joint involvement refers to any swollen or tender joint on examination, which may be confirmed by imaging evidence of synovitis. DIP joints, first CMC joints and first MTP joints are excluded from assessment. Large joints refers to shoulders, elbows, hips, knees and ankles. Small joints refers to MCP joints, PIP joints, second through fifth MTP joints, thumb IP joints and wrists.
- Negative means less than or equal to the upper limit of normal (ULN); low positive means >ULN; high positive means >3× ULN.
- Normal and abnormal are determined by local laboratory standards.
- Duration of symptoms as per patient's self-report. Table adapted from Ref. [5] with permission of John Wiley and Sons Ltd.
Management:
- Hydroxychloroquine 400-600mg qd is recommended for initial treatment in those with low disease activity
- Methotrexate is recommended for initial treatment in those with mod or high disease activity
- Start with 7.5-15 mg weekly
- If started at less than 15 mg weekly, titrate to 15 mg within 6 weeks
- Give folic or folinic acid weekly to reduce AE
- In patients with RA who do not achieve low disease avtivity with MTX, triple therapy with sulfasalazine 500mg qd-bid and hydroxychloroquine is as effective as adding a biologic or targeted synthetic medication
Lab Workup
- Rheumatoid factor
- About 20% of those with confirmed RA will not have an abnormal RF test, while 5% of people who do not have RA will have an abnormal RF test. Negative levels do not exclude the disease, and positive levels do not guarantee the diagnosis.
- Anticyclic citrullinated peptide
- This test is 97% specific for RA if it is present. Once a patient develops a positive anti-CCP, it will usually remain positive, despite remission.
- About 20% of RA patients are seronegative, meaning that their RF and anti-CCP lab results both continue to come back negative. In these cases, the physician makes the diagnosis based on physical examination and imaging.
- RF and anti-CCP are not used to monitor disease activity, because they both tend to remain positive despite remission. Once the diagnosis of RA has been made and confirmed, these tests are not repeated.
- C-reactive protein and Sedimentation rate
- Both ESR and C-reactive protein are non-RA-specific measures of inflammation. Both tests are used to test disease activity; when they are high, this suggests that the disease is very active (assuming no other causes for high results, such as infection, are present)
- Complete blood count
- Complete metabolic panel - Specifically renal function
- Patients taking biologic agents should be tested for
- hepatitis B
- hepatitis C
- tuberculosis
References:
- AFP Vol 106 No 3 Sep 2022
- Am Fam Physician. 2011;84(11):1245-1252
- Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd, Birnbaum NS, Burmester GR, Bykerk VP, Cohen MD, Combe B, Costenbader KH, Dougados M, Emery P, Ferraccioli G, Hazes JM, Hobbs K, Huizinga TW, Kavanaugh A, Kay J, Kvien TK, Laing T, Mease P, Ménard HA, Moreland LW, Naden RL, Pincus T, Smolen JS, Stanislawska-Biernat E, Symmons D, Tak PP, Upchurch KS, Vencovský J, Wolfe F, Hawker G. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010 Sep;62(9):2569-81. doi: 10.1002/art.27584. PMID: 20872595.
Systemic Lupus Erythematosus (SLE)
SLE Diagnosis
| Domain[b] | Weight[c] |
|---|---|
| Clinical domains | |
| Constitutional: | |
| Fever (> 38° C) | 2 |
| Hematologic: | |
| Leukopenia (< 4000/mcL) | 3 |
| Thrombocytopenia (platelet count < 100,000/mcL) | 4 |
| Autoimmune hemolysis[d] | 4 |
| Neuropsychiatric: | |
| Delirium | 2 |
| Psychosis | 3 |
| Seizure (generalized or partial/focal) | 5 |
| Mucocutaneous: | |
| Nonscarring alopecia[e] | 2 |
| Oral ulcers[e] | 2 |
| Subacute cutaneous lupus erythematosus or discoid lupus erythematosus | 4 |
| Acute cutaneous lupus | 6 |
| Serosal: | |
| Pleural effusion or pericardial effusion | 5 |
| Acute pericarditis | 6 |
| Musculoskeletal: | |
| Joint involvement[f] | 6 |
| Renal: | |
| Proteinuria (> 0.5 g/24 hours) | 4 |
| Renal biopsy class II or V lupus nephritis | 8 |
| Renal biopsy class III or IV lupus nephritis | 10 |
| Immunologic domains | |
| Antiphospholipid antibodies: | |
| Anticardiolipin antibodies or | 2 |
| Anti-beta2 glycoprotein 1 antibodies or | |
| Lupus anticoagulant | |
| Complement proteins: | |
| Low C3 or low C4 | 3 |
| Low C3 and low C4 | 4 |
| SLE-specific antibodies: | |
| Anti-dsDNA antibody or | 6 |
| Anti-Smith antibody |
Patients are eligible for these criteria only if they have a positive ANA ≥ 1:80. Classify as Systemic Lupus Erythematosus with a score of 10 or more if entry criterion fulfilled.
[b] Criteria do not need to occur simultaneously. Only the highest-weighted criterion score within a single domain should be used. SLE must be the most likely explanation for each criterion.
[c] Each criterion is assigned a weight of 2 to 10. If the patient's score is 10 or more, and at least one clinical criterion is fulfilled, disease is classified as SLE.
[d] Evidence of autoimmune hemolysis (such as the presence of reticulocytosis, low haptoglobin, elevated indirect bilirubin, elevated lactate dehydrogenase) and a positive direct antiglobulin (direct Coombs) test.
[e] This criterion may be noted during physical examination or review of a photo.
[f] Joint involvement is defined as either synovitis involving ≥ 2 joints characterized by swelling or effusion or tenderness in ≥ 2 joints and at least 30 minutes of morning stiffness.
ANA = antinuclear antibodies; anti-dsDNA = anti–double-stranded (ds) DNA; EULAR/ACR = European League Against Rheumatism/American College of Rheumatology; SLE = systemic lupus erythematosus.
Reference:
- Adapted from Aringer M, Costenbader K, Daikh D, et al: 2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus. Arthritis Rheumatol 71(9):1400–1412, 2019. doi: 10.1002/art.40930
- Algorithm
- Suspect SLE:
- Patient with symptoms from 2 or more of the following systems:
- Constitutional
- Musculoskeletal
- Skin
- Renal
- Gastrointestinal
- Pulmonary
- Cardiac
- Reticuloendothelial
- Hematologic
- Neuropsychiatric
- Patient with symptoms from 2 or more of the following systems:
- If at least 4 ACR criteria:
- Diagnose SLE
- Check ANA (#249)
- If Negative - Low probability of SLE
- If Positive
- CBC, UA, anti-dsDNA (#255), anti-Sm (#37923), anti-cardiolipin antibodies (IgG/IgM) (#36333)
- If no organ involvement or typical lab resuls: SLE unlikely
- If high titer to anti-dsDNA or anti-Sm specific for SLE and at least 4 ACR criteria: Diagnose SLE
- CBC, UA, anti-dsDNA (#255), anti-Sm (#37923), anti-cardiolipin antibodies (IgG/IgM) (#36333)
References:
- AFP Vol 94 No 4 Aug 2016
- AFP Vol 107 No 4 Apr 2023
- Suspect SLE:
- Quest Lab references
Quest code Lab name 36333 IgG/IgM Cardiolipin Ab 37921 anti-Smith 255 dsDNA Ab 249 ANA
SLE Management
Mild SLE (No major organ involvement)
- Constitutional symptoms
- Hydroxychloroquine with or without low-dose systemic corticosteroids or methotrexate
- Then azathioprine, methotrexate, or mycophenolate
- Then rituximab or belimumab
- Discoid Lupus
- Sunscreen
- Topical corticosteroid/tacrolimus, topical acitretin, with or without hyroxychloroquine, with or without glucocorticoids
- Then add azathioprine or switch to mycophenolate or methotrexate
- Polyarthritis
- hydroxychloroquine, with or without systemic glucocorticoids
- Then add methotrexate or rituximab
- NSAIDS as adjunctive therapy
- Uncomplicated digital or cutaneous vasculitis
- Systemic glucocorticoids, with or without hydroxychloroquine, with or without methotrexate
- Then add azathioprine or mycophenolate
- Then switch to IV cyclophosphamide
Moderate to Severe SLE
- Alveolitis
- Systemic glucocorticoids + mycophenolate or IV cyclophosphamide
- Then add rituximab or IV immune globulin
- Maintain with azathioprine or mycophenolate
- Antiphospholipid syndrome
- Anticoagulation, with or without hydroxychloroquine
- Then add direct trhombin inhibitor
- Lupus nephritis
- Systemic glucocorticoids + mycophenolate
- Then IV cyclophosphamide
- Then add rituximab or switch to zazthioprine
- ACE Inhibitor and hydroxychloroquine as adjunctive therapy
- Mononeuritis/central nervous system lupus
- Systemic glucocorticoids, with or without IV cyclophosphamide
- Then add rituximab, IV immune globulin, or plasmapheresis
- Myocarditis
- Systemic glucocorticoids + IV cyclophosphamide, with or without hydroxychloroquine
- Then rituximab, belimumab, or IV immune globulin
- Pericarditis
- NSAIDs
- Then Systemic glucocorticoids + hydroxychloroquine
- Then add mycophenolate, azathioprine, or methotrexate
- Then add belimumab or rituximab
- Pulmonary artery hypertension
- Systemic glucocorticoids + IV cyclophosphamide, or mycophenolate + endothelin receptor antagonist
- Then add rituximab and PDE-5 inhibitor
- Then add prostaglandin analogue
- Maintain with prostaglandin analogue
- Thrombocytopenia
- Systemic glucocorticoids, with or without hydroxychloroquine
- Then add azathiprine or mycophenolate
- Then add rituximab or IV cyclophosphamide or IV immune globulin
References:
- AFP Vol 94 No 4 Aug 2016
- AFP Vol 107 No 4 Apr 2023
Studies: Activity and Exercise
Evidence on Running
Running Good For Knees
- Regular exercise protects against degenerative joint disorders
- Chronic, low-grade inflammation is widely implicated in the onset and progression of degenerative joint disease
- Running appears to decrease knee intra-articular pro-inflammatory cytokine concentration and facilitates the movement of COMP from the joint space to the serum.
- Hyldahl, R.D., Evans, A., Kwon, S. et al. Running decreases knee intra-articular cytokine and cartilage oligomeric matrix concentrations: a pilot study. Eur J Appl Physiol 116, 2305–2314 (2016). https://doi.org/10.1007/s00421-016-3474-z
Aerobic Exercise May Protect The Brain From Alzheimer's Disease
- Cardiorespiratory fitness increased and sedentary behavior decreased in the training program group compared with the other group. The training program group also scored better on the cognitive assessments that focused on executive function, but not the others. Lastly, the increase in cardiorespiratory fitness was correlated with increased brain glucose metabolism in an area of the brain associated with Alzheimer's disease, the posterior cingulate cortex.
- Improvement in executive function correlated with increased VO2peak.
- Gaitán, Julian M. et al. 'Brain Glucose Metabolism, Cognition, and Cardiorespiratory Fitness Following Exercise Training in Adults at Risk for Alzheimer's Disease'. 1 Jan. 2019 : 83 – 95.
Any Amount Of Running Linked To Significantly Lower Risk Of Death
- All in all, 14 studies were included, encompassing 232,149 people who had had their health tracked for periods of time between 5.5 and 35 years. Within that long time frame, 25,951 of the included study participants passed away
- Upon pooling and analyzing all of that data, researchers determined that any amount of running was associated with a 27% lower risk of death from all causes, in comparison to participants who reported never running. This held true among both genders.
- Any amount of running was also associated with a
- 30% lower chance of dying due to cardiovascular disease,
- and a 23% lower risk of cancer-related death.
- Increased rates of participation in running, regardless of its dose, would probably lead to substantial improvements in population health and longevity. Any amount of running, even just once a week, is better than no running, but higher doses of running may not necessarily be associated with greater mortality benefits.
- Pedisic Z, Shrestha N, Kovalchik S, et al. Is running associated with a lower risk of all-cause, cardiovascular and cancer mortality, and is the more the better? A systematic review and meta-analysis. British Journal of Sports Medicine 2020;54:898-905.
Jogging 40 Minutes A Day Has 'Fountain Of Youth' Effect On Cells
- Those who remained highly physically active had much longer telomeres compared to individuals who were less active. Being highly active is comparable to jogging 30 minutes at least five times a week for women, or 40 minutes for men.
- Aging causes telomeres to shorten significantly and results in gradual cell deterioration.
- Regular physical activity reduces disease risk, possibly due to the preservation of telomeres.
- Results showed that regular activity accounted for significantly longer telomeres in U.S. adults.
- The longer telomeres found in active adults accounted for 9 years of reduced cellular aging.
- Larry A. Tucker, Physical activity and telomere length in U.S. men and women: An NHANES investigation, Preventive Medicine, Volume 100, 2017, Pages 145-151, ISSN 0091-7435, https://doi.org/10.1016/j.ypmed.2017.04.027.
Evidence regarding the Q collar
From FDA:
Significant changes were found in deeper tissues of the brain involved in the transmission of electrical nerve signals (white matter regions) in 106 of the 145 (73%) participants in the no-Collar group, while no significant changes in these regions were found in 107 of the 139 (77%) of the group who wore the Q Collar. These differences appear to indicate protection of the brain associated with device use. No significant adverse events were associated with device use.
The Q-Collar does not replace, and should be worn with, other protective sports equipment associated with specific sports activities, such as helmets and shoulder pads. Wearers of the device should not depend on the device to protect them from all harmful effects of head impacts. Users should take steps to avoid direct impact to the head and neck. Data do not demonstrate that the device can prevent concussion or serious head injury. The Q-Collar should not be used if an individual has not been medically cleared to play contact sports.
From Sports Medicine Review Blog:
There are other public skeptics that have claimed individuals would take more risk if they feel they wouldn't get injured. Others do not think the "slosh" theory is validated. The FDA has approved the most popular device called the Q-collar. However, it does state that a link between the changes the studies revealed and actual brain injuries has not been "validated." FDA experts have cited a strong need currently for the prevention of traumatic brain injury and the potential benefit outweighs the risk involved.
SUMMARY In conclusion, more studies are needed to evaluate the clinical value of the jugular vein compression collar. There are many similar studies that show there are possible positive changes on diffusion tensor imaging (DTI) of the brain and the "Q-collar" has been FDA approved. These have gained some traction in the professional sports area and are becoming increasingly popular.
Reference:
Exercise As Medicine
A few things exercise is good for:
- Less depressed and anxious
- Better sleep
- Less frailty in old age
- More strength
- Able to take part in more fun activities (like long hikes)
- Being more attractive (subjectively, of course)
- Improved self perception
- Better cognitive function and memory
- Access to communities
- Less pain
- More mobility
- A stronger immune system
How exercise positively impacts your health:
- Physical Benefits:
- Reduced Risk of Chronic Diseases: Regular physical activity helps lower the risk of heart disease, stroke, type 2 diabetes, certain types of cancer, and high blood pressure.
- Improved Cardiovascular Health: Exercise strengthens the heart muscle, improves blood circulation, and lowers harmful cholesterol levels, reducing the risk of heart attacks and strokes.
- Weight Management: Exercise helps burn calories, maintain a healthy weight, and reduce the risk of obesity-related health problems.
- Stronger Bones and Muscles: Weight-bearing exercises like walking, running, and weightlifting help build and maintain strong bones, reducing the risk of osteoporosis and fractures. Exercise also increases muscle strength and endurance, improving balance and coordination.
- Boosted Immune System: Regular physical activity can enhance the immune system's ability to fight off infections and illnesses.
- Better Sleep: Exercise can improve sleep quality, making it easier to fall asleep and stay asleep throughout the night.
- Mental Benefits:
- Reduced Stress and Anxiety: Exercise releases endorphins, natural mood elevators that help reduce stress, anxiety, and depression.
- Improved Mental Clarity and Focus: Regular physical activity can enhance cognitive function, memory, and concentration.
- Enhanced Mood: Exercise can boost mood and reduce feelings of sadness and fatigue.
- Increased Self-Esteem: Achieving fitness goals and seeing physical improvements can boost self-confidence and body image.
- Additional Benefits:
- Pain Management: Exercise can help alleviate pain associated with conditions like arthritis and fibromyalgia.
- Better Digestion: Regular physical activity can improve digestion and prevent constipation.
- Increased Energy Levels: Exercise can boost energy levels and reduce fatigue.
- Longer Lifespan: Studies have shown that regular exercise can increase lifespan and improve overall quality of life.
Exercise can be prescribed as therapy for 26 different chronic diseases:
- Psychiatric diseases (e.g., depression, anxiety, stress, schizophrenia)
- Neurological diseases (e.g., dementia, Parkinson's disease, multiple sclerosis)
- Metabolic diseases (e.g., obesity, hyperlipidemia, metabolic syndrome, polycystic ovarian syndrome, type 2 diabetes, type 1 diabetes)
- Cardiovascular diseases (e.g., hypertension, coronary heart disease, heart failure, cerebral apoplexy, claudication intermittent)
- Pulmonary diseases (e.g., chronic obstructive pulmonary disease, asthma, cystic fibrosis)
- Musculoskeletal disorders (e.g., osteoarthritis, osteoporosis, back pain, rheumatoid arthritis)
- Cancer
Reference: - Pedersen BK, Saltin B. Exercise as Medicine - Evidence for Prescribing Exercise as Therapy in 26 Different Chronic Diseases. Scandinavian Journal of Medicine & Science in Sports. 2015;25 Suppl 3:1-72. doi:10.1111/sms.12581.
Exercise improves quality of life, depressive symptoms, and cognition across chronic brain disorders such as:
- Alzheimer's disease
- Huntington's disease
- multiple sclerosis
- Parkinson's disease
- schizophrenia
- Unipolar depression
Reference: - Dauwan M, Begemann MJH, Slot MIE, et al. Physical Exercise Improves Quality of Life, Depressive Symptoms, and Cognition Across Chronic Brain Disorders: A Transdiagnostic Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of Neurology. 2021;268(4):1222-1246. doi:10.1007/s00415-019-09493-9.
Exercise improves cardiorespiratory fitness and reducing cardiometabolic risk factors:
- hypertension
- glucose intolerance
- insulin resistance
- dyslipidemia
- Inflammatory markers
Reference: - Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine Position Stand. Quantity and Quality of Exercise for Developing and Maintaining Cardiorespiratory, Musculoskeletal, and Neuromotor Fitness in Apparently Healthy Adults: Guidance for Prescribing Exercise. Medicine and Science in Sports and Exercise. 2011;43(7):1334-59. doi:10.1249/MSS.0b013e318213fefb.
The American Heart Association (AHA) recommends exercise for patients with heart failure to improve functional status and reduce hospitalizations.
Reference: - Bozkurt B, Aguilar D, Deswal A, et al. Contributory Risk and Management of Comorbidities of Hypertension, Obesity, Diabetes Mellitus, Hyperlipidemia, and Metabolic Syndrome in Chronic Heart Failure: A Scientific Statement From the American Heart Association. Circulation. 2016;134(23):e535-e578. doi:10.1161/CIR.0000000000000450.
The number needed to treat (NNT) for exercise varies across different conditions:
- Depression: A systematic review and meta-analysis found that the NNT for exercise in treating depression is 2 (95% CI 1.68 to 2.59).[1]
- Heart Failure: The ExTraMATCH meta-analysis reported an NNT of 17 to prevent one death in patients with heart failure.[2]
- Anxiety: Exercise reduces anxiety symptoms, with benefits comparable to pharmacological treatments.[3]
- Type 2 Diabetes: Exercise is effective in managing type 2 diabetes, improving glycemic control and reducing cardiovascular risk factors, often comparable to pharmacological treatments.[3]
- Hypertension: Exercise is recommended for managing hypertension, with effects similar to antihypertensive medications.[3]
- Dementia: Exercise improves quality of life, depressive symptoms, and cognition in chronic brain disorders, including dementia.[4]
References: 1. Heissel A, Heinen D, Brokmeier LL, et al. Exercise as Medicine for Depressive Symptoms? A Systematic Review and Meta-Analysis With Meta-Regression. British Journal of Sports Medicine. 2023;57(16):1049-1057. doi:10.1136/bjsports-2022-106282. 2. Bozkurt B, Aguilar D, Deswal A, et al. Contributory Risk and Management of Comorbidities of Hypertension, Obesity, Diabetes Mellitus, Hyperlipidemia, and Metabolic Syndrome in Chronic Heart Failure: A Scientific Statement From the American Heart Association. Circulation. 2016;134(23):e535-e578. doi:10.1161/CIR.0000000000000450. 3. Bricca A, Harris LK, Jäger M, et al. Benefits and Harms of Exercise Therapy in People With Multimorbidity: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Ageing Research Reviews. 2020;63:101166. doi:10.1016/j.arr.2020.101166. 4. Dauwan M, Begemann MJH, Slot MIE, et al. Physical Exercise Improves Quality of Life, Depressive Symptoms, and Cognition Across Chronic Brain Disorders: A Transdiagnostic Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of Neurology. 2021;268(4):1222-1246. doi:10.1007/s00415-019-09493-9.
Patient Messaging: Exercise and Strength Building
Any exercise that takes you pretty close to failure within ~5-30 reps while stressing the target muscle(s) through a long range of motion will be good for muscle growth.
Upper Body:
- Pushups
- Dips
- Pullups
Core:
- Situps
- Crunches
- Planks
Lower body:
- Squats
- Lunges, Split squats, step ups
See:
Stair Climbing
Energy cost of walking and running at extreme uphill and downhill slopes
BLUF:
- The minimum in energy cost is similar in walking and running at ∼0.10–0.20 downhill gradient
- The optimum gradient for mountain paths is close to 0.20–0.30, both uphill and downhill, for the two gaits
- A better progression economy is expected in mountain-running athletes in the downhill range
- The running speeds adopted in downhill competition are far lower than metabolically feasible, mainly because of safety reasons.
- If athletes wish to improve their performances in competitions alternating ascent and descent phases, they should pay greatest attention to the training of movement coordination during downhill running.
Abstract
- The costs of walking (Cw) and running (Cr) were measured on 10 runners on a treadmill inclined between -0.45 to +0.45 at different speeds.
- The minimum Cw was 1.64 +/- 0.50 J. kg(-1). m(-1) at a 1.0 +/- 0.3 m/s speed on the level.
- It increased on positive slopes, attained 17.33 +/- 1.11 J. kg(-1). m(-1) at +0.45, and was reduced to 0.81 +/- 0.37 J. kg(-1). m(-1) at -0.10.
- At steeper slopes, it increased to reach 3.46 +/- 0.95 J. kg(-1). m(-1) at -0.45.
- Cr was 3.40 +/- 0.24 J. kg(-1). m(-1) on the level, independent of speed.
- It increased on positive slopes, attained 18.93 +/- 1.74 J. kg(-1). m(-1) at +0.45, and was reduced to 1.73 +/- 0.36 J. kg(-1). m(-1) at -0.20.
- At steeper slopes, it increased to reach 3.92 +/- 0.81 J. kg(-1). m(-1) at -0.45.
- The mechanical efficiencies of walking and running above +0.15 and below -0.15 attained those of concentric and eccentric muscular contraction, respectively.
- The optimum gradients for mountain paths approximated 0.20-0.30 for both gaits.
- Downhill, Cr was some 40% lower than reported in the literature for sedentary subjects.
- The estimated maximum running speeds on positive gradients corresponded to those adopted in uphill races; on negative gradients they were well above those attained in downhill competitions.
Reference:
- Minetti AE, Moia C, Roi GS, Susta D, Ferretti G. Energy cost of walking and running at extreme uphill and downhill slopes. J Appl Physiol (1985). 2002 Sep;93(3):1039-46. doi: 10.1152/japplphysiol.01177.2001. PMID: 12183501.
Study: Brief Intense Stair Climbing Improves Cardiorespiratory Fitness
Purpose
- Sprint interval training (SIT) is a time-efficient strategy to improve cardiorespiratory fitness (CRF); however, most protocols have been studied in laboratory settings and require specialized equipment. We investigated the efficacy of brief intense stair climbing as a practical model of SIT to improve CRF.
Methods
- Two separate studies, each consisting of an acute and chronic phase, were conducted in a total of 31 sedentary women (age = 24 ± 10 yr, body mass index = 23 ± 4 kg·m−2).
Results
- The acute phase of study 1 established that the mean HR, blood [lactate], and RPE were similar when participants (n = 8) performed an SIT protocol that involved 3 × 20-s "all-out" efforts of either continuously ascending stairs or cycling. The chronic phase demonstrated that CRF, as determined by peak oxygen uptake (V˙O2peak), increased by 12% or ~1 MET (8.27 ± 1.05 to 9.25 ± 1.01 METs, P = 0.002) when participants (n = 12) performed the 3 × 20-s stair climbing protocol 3 d·wk−1 for 6 wk. The acute phase of study 2 established that HR and RPE were similar when participants (n = 11) performed three different stair climbing protocols: the 3 × 20-s continuous ascent model used in study 1 and two 3 × 60-s models of ascending and descending either one or two flights of stairs (P > 0.05). The chronic phase demonstrated that V˙O2peak increased by 7% (8.91 ± 1.30 to 9.51 ± 1.52 METs, P = 0.01) when the same group of participants performed the one-flight 3 × 60-s protocol 3 d·wk−1 for 6 wk. The Cederholm index determined from an oral glucose tolerance test was 57 ± 17 and 64 ± 21 mg·L−2·mmol−1·mU−1·min−1 before and after training, respectively (P = 0.056).
Conclusion
- Brief, intense stair climbing is a practical, time-efficient strategy to improve CRF in previously untrained women.
Reference:
- ALLISON, MARY K.; BAGLOLE, JESSICA H.; MARTIN, BRIAN J.; MACINNIS, MARTIN J.; GURD, BRENDON J.; GIBALA, MARTIN J.. Brief Intense Stair Climbing Improves Cardiorespiratory Fitness. Medicine & Science in Sports & Exercise 49(2):p 298-307, February 2017. | DOI: 10.1249/MSS.0000000000001188
Study: Energy cost of stair climbing and descending on the college alumnus questionnaire
In calculating the physical activity index (PAI) on the college alumnus questionnaire, it is assumed that 8 kcal are expended for every 20 steps climbed.
- This value is equal to an energy cost of 0.40 kcal.step-1.
Since it is assumed that subjects climb and descend an equal number of stairs, the total value reflects the energy cost of stepping up (estimated at 0.30 kcal.step-1) and stepping down (estimated at 0.10 kcal.step-1). However, these values appear to be based on theoretical calculations rather than empirical observation.
The purpose of this study was to quantify the energy cost of stair climbing and stair descending by measuring oxygen uptake. Twenty subjects performed continuous stair-climbing and stair-descending on an escalator at a stepping rate of 70 step.min-1.
Heart rate was monitored by telemetry, and oxygen uptake was measured by the Douglas bag technique from 5 to 7 min.
Results showed that the gross energy cost of stair climbing is 8.6 METs, and that of stair descending is 2.9 METs.
- Thus, for a 70-kg person the gross caloric costs of ascending stairs (0.15 kcal.step-1) and descending stairs (0.05 kcal.step-1) are one-half of the values previously assumed.
In conclusion, the algorithm for calculating PAI on the college alumnus questionnaire should be modified to reflect a total cost of 0.20 kcal for going up and down one step. Even more precise estimates can be obtained by adjusting for body weight (going up and down one flight of stairs requires 1.63 MET.min).
Reference:
- Bassett DR, Vachon JA, Kirkland AO, Howley ET, Duncan GE, Johnson KR. Energy cost of stair climbing and descending on the college alumnus questionnaire. Med Sci Sports Exerc. 1997 Sep;29(9):1250-4. doi: 10.1097/00005768-199709000-00019. PMID: 9309638.
Study: The Energy Expenditure of Stair Climbing One Step and Two Steps at a Time: Estimations from Measures of Heart Rate
Stairway climbing provides a ubiquitous and inconspicuous method of burning calories. While typically two strategies are employed for climbing stairs, climbing one stair step per stride or two steps per stride, research to date has not clarified if there are any differences in energy expenditure between them.
Fourteen participants took part in two stair climbing trials whereby measures of heart rate were used to estimate energy expenditure during stairway ascent at speeds chosen by the participants.
The relationship between rate of oxygen consumption (VO2)and heart rate was calibrated for each participant using an inclined treadmill.
The trials involved climbing up and down a 14.05 m high stairway, either ascending one step per stride or ascending two stair steps per stride.
- Single-step climbing used 8.5±0.1 kcal min−1, whereas double step climbing used 9.2±0.1 kcal min−1.
- These estimations are similar to equivalent measures in all previous studies, which have all directly measured V02.
The present study findings indicate that:
- Treadmill-calibrated heart rate recordings can be used as a valid alternative to respirometry to ascertain rate of energy expenditure during stair climbing
- Two step climbing invokes a higher rate of energy expenditure; however, one step climbing is energetically more expensive in total over the entirety of a stairway.
- Therefore to expend the maximum number of calories when climbing a set of stairs the single-step strategy is better.
Reference:
- Halsey LG, Watkins DA, Duggan BM. The energy expenditure of stair climbing one step and two steps at a time: estimations from measures of heart rate. PLoS One. 2012;7(12):e51213. doi: 10.1371/journal.pone.0051213. Epub 2012 Dec 12. Erratum in: PLoS One. 2014;9(6):e100658. PMID: 23251455; PMCID: PMC3520986.
Steps Daily edit 2025
| To help | Steps | Improvement |
|---|---|---|
| Lose weight | 10000 | |
| Depression | 7000 | 31% |
| Dementia | 9800 | |
| Premature death | 8800 | 60% |
| Heart disease | 2000-3000 | |
| Preserve mentation | 3800 | 25% lower risk dementia |
| Cardiovascular health | 7126 | 51% lower risk CVD |
What happened to references?
Study: Antidepressants or running therapy: Comparing effects on mental and physical health in patients with depression and anxiety disorders
Highlights
- 141 patients with depression and/or anxiety disorder participated in this study.
- Running therapy and antidepressant medication had similar effects on mental health (remission and response rates).
- Running therapy outperformed antidepressant medication on physical health variables.
- Running therapy is a valuable treatment strategy in mental health care.
Background
- Antidepressant medication and running therapy are both effective treatments for patients with depressive and anxiety disorders. However, they may work through different pathophysiological mechanisms and could differ in their impact on physical health. This study examined effects of antidepressants versus running therapy on both mental and physical health.
Methods
- According to a partially randomized patient preference design, 141 patients with depression and/or anxiety disorder were randomized or offered preferred 16-week treatment: antidepressant medication (escitalopram or sertraline) or group-based running therapy ≥2 per week.
- Baseline (T0) and post-treatment assessment at week 16 (T16) included mental (diagnosis status and symptom severity) and physical health indicators (metabolic and immune indicators, heart rate (variability), weight, lung function, hand grip strength, fitness).
- The running sessions lasted 45 minutes
- including a 10-minute warmup
- 30 minutes of jogging
- 5 minute cooldown
- Each participant wore a heart rate monitor and the goal was to jog at an intensity of 50 to 70 percent of heart rate reserve for the first 4 weeks, and 70 to 85 percent in the final 12 weeks.
Results
- Of the 141 participants (mean age 38.2 years; 58.2 % female)
- 45 participants received antidepressant medication and 96 underwent running therapy
- Intention-to-treat analyses showed that remission rates at T16 were comparable (antidepressants: 44.8 %; running: 43.3 %; p = .881).
- However, the groups differed significantly on various changes in physical health: weight (d = 0.57; p = .001), waist circumference (d = 0.44; p = .011), systolic (d = 0.45; p = .011) and diastolic (d = 0.53; p = .002) blood pressure, heart rate (d = 0.36; p = .033) and heart rate variability (d = 0.48; p = .006).
Limitations
- A minority of the participants was willing to be randomized; the running therapy was larger due to greater preference for this intervention.
Conclusions
- While the interventions had comparable effects on mental health, running therapy outperformed antidepressants on physical health, due to both larger improvements in the running therapy group as well as larger deterioration in the antidepressant group.
Reference:
- Verhoeven JE, Han LKM, Lever-van Milligen BA, Hu MX, Révész D, Hoogendoorn AW, Batelaan NM, van Schaik DJF, van Balkom AJLM, van Oppen P, Penninx BWJH. Antidepressants or running therapy: Comparing effects on mental and physical health in patients with depression and anxiety disorders. J Affect Disord. 2023 May 15;329:19-29. doi: 10.1016/j.jad.2023.02.064. Epub 2023 Feb 23. PMID: 36828150.
- https://www.sciencedirect.com/science/article/pii/S0165032723002239
Study: Association of Daily Step Count and Intensity With Incident Dementia in 78,430 Adults Living in the UK
Key Points Question
- Is there a dose-response association of daily step count and intensity with incidence of all-cause dementia among adults living in the UK?
Findings
- This cohort study of adults assessed with wrist-worn accelerometers found that accruing more steps per day was associated with steady declines in dementia incidence risk, up to 9800 steps per day, beyond which the benefits upturned. The dose associated with 50% of maximal observed benefit was 3800 steps per day, and steps at higher intensity (cadence) were associated with lower incidence risk.
Meaning
- The findings in this study suggest that accumulating more steps per day just under the popular threshold of 10,000 steps per day and performing steps at higher intensity may be associated with lower risk of dementia onset.
Abstract
Importance
- Step-based recommendations may be appropriate for dementia-prevention guidelines. However, the association of step count and intensity with dementia incidence is unknown.
Objective
- To examine the dose-response association between daily step count and intensity and incidence of all-cause dementia among adults in the UK.
Design, Setting, and Participants
- UK Biobank prospective population-based cohort study (February 2013 to December 2015) with 6.9 years of follow-up (data analysis conducted May 2022). A total of 78,430 of 103,684 eligible adults aged 40 to 79 years with valid wrist accelerometer data were included. Registry-based dementia was ascertained through October 2021.
Exposures
- Accelerometer-derived daily step count, incidental steps (less than 40 steps per minute), purposeful steps (40 steps per minute or more), and peak 30-minute cadence (ie, mean steps per minute recorded for the 30 highest, not necessarily consecutive, minutes in a day).
Main Outcomes and Measures
- Incident dementia (fatal and nonfatal), obtained through linkage with inpatient hospitalization or primary care records or recorded as the underlying or contributory cause of death in death registers. Spline Cox regressions were used to assess dose-response associations.
Results
- The study monitored 78,430 adults (mean [SD] age, 61.1 [7.9] years; 35,040 [44.7%] male and 43,390 [55.3%] female; 881 [1.1%] were Asian, 641 [0.8%] were Black, 427 [0.5%] were of mixed race, 75,852 [96.7%] were White, and 629 [0.8%] were of another, unspecified race) over a median (IQR) follow-up of 6.9 (6.4-7.5) years, 866 of whom developed dementia (mean [SD] age, 68.3 [5.6] years; 480 [55.4%] male and 386 [54.6%] female; 5 [0.6%] Asian, 6 [0.7%] Black, 4 [0.4%] mixed race, 821 [97.6%] White, and 6 [0.7%] other).
- Analyses revealed nonlinear associations between daily steps.
- The optimal dose (ie, exposure value at which the maximum risk reduction was observed) was 9826 steps (hazard ratio [HR], 0.49; 95% CI, 0.39-0.62) and the minimal dose (ie, exposure value at which the risk reduction was 50% of the observed maximum risk reduction) was 3826 steps (HR, 0.75; 95% CI, 0.67-0.83).
- The incidental cadence optimal dose was 3677 steps (HR, 0.58; 95% CI, 0.44-0.72); purposeful cadence optimal dose was 6315 steps (HR, 0.43; 95% CI, 0.32-0.58); and peak 30-minute cadence optimal dose was 112 steps per minute (HR, 0.38; 95% CI, 0.24-0.60).
Conclusions and Relevance
- In this cohort study, a higher number of steps was associated with lower risk of all-cause dementia. The findings suggest that a dose of just under 10,000 steps per day may be optimally associated with a lower risk of dementia.
- Steps performed at higher intensity resulted in stronger associations.
Reference:
- del Pozo Cruz B, Ahmadi M, Naismith SL, Stamatakis E. Association of Daily Step Count and Intensity With Incident Dementia in 78,430 Adults Living in the UK. JAMA Neurol. 2022;79(10):1059–1063. https://doi.org/10.1001/jamaneurol.2022.2672
Study: Association of Daily Step Patterns With Mortality in US Adults
Importance
- Previous studies have shown that individuals who regularly walk, particularly 8000 daily steps or more, experience lower mortality. However, little is known about the health benefits of walking intensively only a few days a week.
Objective
- To evaluate the dose-response association between the number of days an individual takes 8000 steps or more and mortality among US adults.
Design, Setting, and Participants
- This cohort study evaluated a representative sample of participants aged 20 years or older in the National Health and Nutrition Examination Surveys 2005-2006 who wore an accelerometer for 1 week and their mortality data through December 31, 2019. Data were analyzed from April 1, 2022, to January 31, 2023.
Exposures
- Participants were grouped by the number of days per week they took 8000 steps or more (0 days, 1-2 days, and 3-7 days).
Main Outcomes and Measures
- Multivariable ordinary least squares regression models were used to estimate adjusted risk differences (aRDs) for all-cause and cardiovascular mortality during the 10-year follow-up, adjusting for potential confounders (eg, age, sex, race and ethnicity, insurance status, marital status, smoking, comorbidities, and average daily step counts).
Results
- Among 3101 participants (mean [SD] age, 50.5 [18.4] years; 1583 [51.0%] women and 1518 [49.0%] men; 666 [21.5%] Black, 734 [23.7%] Hispanic, 1579 [50.9%] White, and 122 [3.9%] other race and ethnicity), 632 (20.4%) did not take 8000 steps or more any day of the week, 532 (17.2%) took 8000 steps or more 1 to 2 days per week, and 1937 (62.5%) took 8000 steps or more 3 to 7 days per week.
- Over the 10-year follow-up, all-cause and cardiovascular deaths occurred in 439 (14.2%) and 148 (5.3%) participants, respectively.
- Compared with participants who walked 8000 steps or more 0 days per week, all-cause mortality risk was lower among those who took 8000 steps or more 1 to 2 days per week (aRD, −14.9%; 95% CI −18.8% to −10.9%) and 3 to 7 days per week (aRD, −16.5%; 95% CI, −20.4% to −12.5%).
- The dose-response association for both all-cause and cardiovascular mortality risk was curvilinear; the protective association plateaued at 3 days per week. Different thresholds for the number of daily steps between 6000 and 10,000 yielded similar results.
Conclusions and Relevance
- In this cohort study of US adults, the number of days per week taking 8000 steps or more was associated with a lower risk of all-cause and cardiovascular mortality in a curvilinear fashion.
- These findings suggest that individuals may receive substantial health benefits by walking just a couple days a week.
Reference:
- Inoue K, Tsugawa Y, Mayeda ER, Ritz B. Association of Daily Step Patterns With Mortality in US Adults. JAMA Netw Open. 2023 Mar 1;6(3):e235174. doi: 10.1001/jamanetworkopen.2023.5174. PMID: 36976556.
- https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2802810
Study: Association of Timing of Moderate-to-Vigorous Physical Activity With Changes in Glycemic Control Over 4 Years in Adults With Type 2 Diabetes From the Look AHEAD Trial
Objective:
- We aimed to determine the association of the time-of-day of bout-related moderate-to-vigorous physical activity (bMVPA) with changes in glycemic control across 4 years in adults with overweight/obesity and type 2 diabetes.
Research design and methods:
- Among 2,416 participants (57% women; mean age, 59 years) with 7-day waist-worn accelerometry recording at year 1 or 4, we assigned bMVPA timing groups based on the participants' temporal distribution of bMVPA at year 1 and recategorized them at year 4. The time-varying exposure of bMVPA (≥10-min bout) timing was defined as ≥50% of bMVPA occurring during the same time period (morning, midday, afternoon, or evening), <50% of bMVPA in any time period (mixed), and ≤1 day with bMVPA per week (inactive).
Results:
- HbA1c reduction at year 1 varied among bMVPA timing groups (P = 0.02), independent of weekly bMVPA volume and intensity.
- The afternoon group had the greatest HbA1c reduction versus inactive (-0.22% [95%CI -0.39%, -0.06%]), the magnitude of which was 30-50% larger than the other groups.
- The odds of discontinuation versus maintaining or initiating glucose-lowering medications at year 1 differed by bMVPA timing (P = 0.04). The afternoon group had the highest odds (odds ratio 2.13 [95% CI 1.29, 3.52]).
- For all the year-4 bMVPA timing groups, there were no significant changes in HbA1c between year 1 and 4.
Conclusion:
- bMVPA performed in the afternoon is associated with improvements in glycemic control in adults with diabetes, especially within the initial 12 months of an intervention. Experimental studies are needed to examine causality.
Reference:
- Qian J, Xiao Q, Walkup MP, et al. Association of Timing of Moderate-to-Vigorous Physical Activity With Changes in Glycemic Control Over 4 Years in Adults With Type 2 Diabetes From the Look AHEAD Trial [published online ahead of print, 2023 May 25]. Diabetes Care. 2023;dc222413. https://doi.org/10.2337/dc22-2413
- https://diabetesjournals.org/care/article-abstract/doi/10.2337/dc22-2413/148938/Association-of-Timing-of-Moderate-to-Vigorous
Study: Association of wearable device-measured vigorous intermittent lifestyle physical activity with mortality
Wearable devices can capture unexplored movement patterns such as brief bursts of vigorous intermittent lifestyle physical activity (VILPA) that is embedded into everyday life, rather than being done as leisure time exercise.
Here, we examined the association of VILPA with all-cause, cardiovascular disease (CVD) and cancer mortality in 25,241 nonexercisers (mean age 61.8 years, 14,178 women/11,063 men) in the UK Biobank. Over an average follow-up of 6.9 years, during which 852 deaths occurred, VILPA was inversely associated with all three of these outcomes in a near-linear fashion.
Compared with participants who engaged in no VILPA, participants who engaged in VILPA at the sample median VILPA frequency of 3 length-standardized bouts per day (lasting 1 or 2 min each) showed a 38%-40% reduction in all-cause and cancer mortality risk and a 48%-49% reduction in CVD mortality risk.
Moreover, the sample median VILPA duration of 4.4 min per day was associated with a 26%-30% reduction in all-cause and cancer mortality risk and a 32%-34% reduction in CVD mortality risk.
We obtained similar results when repeating the above analyses for vigorous physical activity (VPA) in 62,344 UK Biobank participants who exercised (1,552 deaths, 35,290 women/27,054 men).
These results indicate that small amounts of vigorous nonexercise physical activity are associated with substantially lower mortality. VILPA in nonexercisers appears to elicit similar effects to VPA in exercisers, suggesting that VILPA may be a suitable physical activity target, especially in people not able or willing to exercise.
Reference:
- Stamatakis E, Ahmadi MN, Gill JMR, Thøgersen-Ntoumani C, Gibala MJ, Doherty A, Hamer M. Association of wearable device-measured vigorous intermittent lifestyle physical activity with mortality. Nat Med. 2022 Dec;28(12):2521-2529. doi: 10.1038/s41591-022-02100-x. Epub 2022 Dec 8. PMID: 36482104; PMCID: PMC9800274.
Study: Associations between cardiorespiratory fitness in youth and the incidence of site-specific cancer in men: a cohort study with register linkage
Objectives
- To assess the associations between cardiorespiratory fitness (CRF) in young men and the incidence of site-specific cancer.
Methods
- A Swedish population-based cohort study with register linkage of men who underwent military conscription in 1968–2005 was undertaken. CRF was assessed by maximal aerobic workload cycle test at conscription. Cox regression models assessed linear associations and included CRF, age, year and site of conscription, body mass index and parental level of education. CRF was also categorised into low, moderate and high for facilitated interpretation and results comparing high and low CRF are reported.
Results
- Primary analyses were performed in 1,078,000 men, of whom 84,117 subsequently developed cancer in at least one site during a mean follow-up of 33 years.
- Higher CRF was linearly associated with a lower hazard ratio (HR) of developing cancer in the:
- head and neck (n=2738, HR 0.81, 95% CI 0.74 to 0.90)
- oesophagus (n=689, HR 0.61, 95% CI 0.50 to 0.74)
- stomach (n=902, HR 0.79, 95% CI 0.67 to 0.94)
- pancreas (n=1280, HR 0.88, 95% CI 0.76 to 1.01)
- liver (n=1111, HR 0.60, 95% CI 0.51 to 0.71)
- colon (n=3222, HR 0.82, 95% CI 0.75 to 0.90)
- rectum (n=2337, HR 0.95, 95% CI 0.85 to 1.05)
- kidney (n=1753, HR 0.80, 95% CI 0.70 to 0.90)
- lung (n=1635, HR 0.58, 95% CI 0.51 to 0.66)
- However, higher CRF predicted a higher hazard of being diagnosed with:
- prostate cancer (n=14 232, HR 1.07, 95% CI 1.03 to 1.12)
- malignant skin cancer (n=23 064, HR 1.31, 95% CI 1.27 to 1.36)
- Higher CRF was linearly associated with a lower hazard ratio (HR) of developing cancer in the:
Conclusion
- We report a number of protective associations between higher CRF in healthy young men and the subsequent hazard of site-specific cancers. These results have implications for public health policymaking, strengthening the incentive to promote health through improving CRF in youth.
Reference:
- Onerup A, Mehlig K, Geijerstam AA, Ekblom-Bak E, Kuhn HG, Lissner L, Åberg M, Börjesson M. Associations between cardiorespiratory fitness in youth and the incidence of site-specific cancer in men: a cohort study with register linkage. Br J Sports Med. 2023 Aug 15:bjsports-2022-106617. doi: 10.1136/bjsports-2022-106617. Epub ahead of print. PMID: 37582636.
- https://bjsm.bmj.com/content/early/2023/08/17/bjsports-2022-106617
Study: Cardiorespiratory fitness is a strong and consistent predictor of morbidity and mortality among adults: an overview of meta-analyses representing over 20.9 million observations from 199 unique cohort studies
Objective
- To examine and summarise evidence from meta-analyses of cohort studies that evaluated the predictive associations between baseline cardiorespiratory fitness (CRF) and health outcomes among adults.
Design: Overview of systematic reviews.
Data source: Five bibliographic databases were searched from January 2002 to March 2024.
Results
- From the 9062 papers identified, we included 26 systematic reviews. We found eight meta-analyses that described five unique mortality outcomes among general populations.
- CRF had the largest risk reduction for all-cause mortality when comparing high versus low CRF (HR=0.47; 95% CI 0.39 to 0.56).
- A dose–response relationship for every 1-metabolic equivalent of task (MET) (3.5 mL/kg/min) higher level of CRF was associated with a 11%–17% reduction in all-cause mortality (HR=0.89; 95% CI 0.86 to 0.92, and HR=0.83; 95% CI 0.78 to 0.88).
- For incident outcomes, nine meta-analyses described 12 unique outcomes.
- CRF was associated with the largest risk reduction in incident heart failure when comparing high versus low CRF (HR=0.31; 95% CI 0.19 to 0.49).
- A dose–response relationship for every 1-MET higher level of CRF was associated with a 18% reduction in heart failure (HR=0.82; 95% CI 0.79 to 0.84).
- Among those living with chronic conditions, nine meta-analyses described four unique outcomes in nine patient groups.
- CRF was associated with the largest risk reduction for cardiovascular mortality among those living with cardiovascular disease when comparing high versus low CRF (HR=0.27; 95% CI 0.16 to 0.48).
- The certainty of the evidence across all studies ranged from very low-to-moderate according to Grading of Recommendations, Assessment, Development and Evaluations.
Conclusion
- We found consistent evidence that high CRF is strongly associated with lower risk for a variety of mortality and incident chronic conditions in general and clinical populations.
- High CRF is strongly associated with lower risk of
- Premature mortality
- Incident chronic conditions
- Hypertension
- Heart Failure
- Stroke
- Atrial Fibrillation
- Dementia
- Depression
- Poor prognosis in those with existing chronic conditions
Other Notes:
- Nearly half of the variance in CRF is attributable to genetics, with the remainder modified primarily through habitual physical activity
- Brisk walking for approximately 150 min per week can result in large relative improvements in CRF among sedentary and unfit individuals. Even those with severe chronic disease can improve CRF through well-planned aerobic physical activity programmes.
- Improvements in CRF through regular physical activity results in a proportional reduction in mortality risk, regardless of the presence of other major risk factors such as higher body mass index, hypertension, type 2 diabetes, dyslipidaemia, or smoking.
Reference:
- Lang JJ, Prince SA, Merucci K, et al Cardiorespiratory fitness is a strong and consistent predictor of morbidity and mortality among adults: an overview of meta-analyses representing over 20.9 million observations from 199 unique cohort studies British Journal of Sports Medicine 2024;58:556-566.
- https://bjsm.bmj.com/content/58/10/556
Study: Clinic and Park Partnerships for childhood resilience: A prospective study of park prescriptions
Introduction:
- Pediatricians need community resources for childhood stress. We examined the association of weekly park visits and resilience amongst children receiving a park prescription at a clinic for low-income families.
Materials and methods:
- A prospective longitudinal clinical trial was conducted amongst children ages 7-17 at a safety-net primary care clinic with measures at zero, one and three months out.
- Parents reported their child's:
- park visits per week
- baseline ACE score
- parental own stress (PSS10) and coping
- children reported resilience (Brief Resiliency Scale) and stress (PSQ8-11 scale)
Results:
- Enrolled children (N = 54; mean (sd) age 10.3 (2.4) years), had a median (IQR) ACE score of 2 (1, 4).
- Child resilience improved with each one-day increase in weekly park visits (0.04 points, 95% CI 0.01, 0.08) at every level of ACEs.
- Child stress partially mediated this relationship
Conclusion:
- Parks are a community resource for pediatric resilience
- Park prescriptions may be a way to deal with pediatric stress
Reference:
- Razani N, Niknam K, Wells NM, et al. Clinic and park partnerships for childhood resilience: A prospective study of park prescriptions. Health Place. 2019;57:179-185. https://doi.org/10.1016/j.healthplace.2019.04.008
- https://pubmed.ncbi.nlm.nih.gov/31060017/
Study: Daily Step Count and Depression in Adults - A Systematic Review and Meta-Analysis
Key Points
- Question
- Are objectively measured daily steps associated with depression in adulthood?
- Findings
- In this systematic review and meta-analysis of 33 observational studies involving 96 173 adults, higher daily step counts were associated with fewer depressive symptoms in the general adult population. Compared with fewer than 5000 steps/d, achieving 5000 or more was associated with reduced depressive symptoms in cross-sectional studies, whereas a daily step count of 7000 or higher was associated with lower risk of depression in prospective studies.
- Meaning
- These findings suggest that an inclusive, comprehensive public health approach could contribute to preventing depression in adults.
Abstract
Importance
- Recent evidence syntheses have supported the protective role of daily steps in decreasing the risk of cardiovascular disease and all-cause mortality. However, step count–based recommendations should cover additional health outcomes.
Objective
- To synthesize the associations between objectively measured daily step counts and depression in the general adult population.
Data Sources
- In this systematic review and meta-analysis, a systematic search of the PubMed, PsycINFO, Scopus, SPORTDiscus, and Web of Science databases was conducted from inception until May 18, 2024, to identify observational studies using search terms related to physical activity, measures of daily steps, and depression, among others. Supplementary search methods were also applied.
Study Selection
- All identified studies were uploaded to an online review system and were considered without restrictions on publication date or language. Included studies had objectively measured daily step counts and depression data.
Data Extraction and Synthesis
- This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses and Meta-analysis of Observational Studies in Epidemiology reporting guidelines. Two independent reviewers extracted the published data.
Main Outcomes and Measures
- Pooled effect sizes (correlation coefficient, standardized mean difference [SMD], and risk ratio [RR]) with 95% CIs were estimated using the Sidik-Jonkman random-effects method.
Results
- Thirty-three studies (27 cross-sectional and 6 longitudinal [3 panel and 3 prospective cohort]) involving 96,173 adults aged 18 years or older (range of mean [SD] ages: 18.6 [0.6] to 91.2 [1.6] years) were included. Daily steps were inversely correlated with depressive symptoms in both cross-sectional and panel studies.
- Compared with fewer than 5000 steps/d, pooled SMDs from cross-sectional studies revealed that 10,000 or more steps/d (SMD, −0.26; 95% CI, −0.38 to −0.14), 7500 to 9999 steps/d (SMD, −0.27; 95% CI, −0.43 to −0.11), and 5000 to 7499 steps/d (SMD, −0.17; 95% CI, −0.30 to −0.04) were significantly associated with fewer depressive symptoms.
- Pooled estimates from prospective cohort studies indicated that participants with 7000 or more steps/d had reduced risk of depression compared with their counterparts with fewer than 7000 steps/d (RR, 0.69; 95% CI, 0.62-0.77).
- An increase of 1000 steps/d was associated with a lower risk of depression (RR, 0.91; 95% CI, 0.87-0.94).
Conclusions and Relevance
- In this systematic review and meta-analysis of 33 observational studies involving 96,173 adults, higher daily step counts were associated with fewer depressive symptoms in cross-sectional and longitudinal studies in the general adult population. Further prospective cohort studies are needed to clarify the potential protective role of daily steps in mitigating the risk of depression during adulthood.
Reference:
- Bizzozero-Peroni B, Díaz-Goñi V, Jiménez-López E, et al. Daily Step Count and Depression in Adults: A Systematic Review and Meta-Analysis. JAMA Netw Open. 2024;7(12):e2451208. https://doi.org/10.1001/jamanetworkopen.2024.51208
Study: Daily Steps And Health Outcomes In Adults: A Systematic Review And Dose-Response Meta-Analysis
Background
- Despite the rapid increase in evidence from the past decade on daily steps and health-related outcomes, existing systematic reviews primarily focused on few outcomes, such as all-cause mortality. This study synthesised the prospective dose-response relationship between daily steps and health outcomes including all-cause mortality, cardiovascular disease, cancer, type 2 diabetes, cognitive outcomes, mental health outcomes, physical function, and falls.
Methods
- For this systematic review and meta-analysis, we searched PubMed and EBSCO CINAHL for literature published between Jan 1, 2014, and Feb 14, 2025, supplemented by other search strategies. Eligible prospective studies examined the relationship between device-measured daily steps and health outcomes among adults without restrictions on language or publication type. Pairs of reviewers (BN, KO, ML, and TN) independently did the study selection, data extraction, and risk of bias assessment using the 9-point Newcastle-Ottawa Scale. Hazard ratios (HRs) from individual studies were synthesised using random-effects dose-response meta-analysis where possible. Certainty of evidence was assessed using GRADE. This trial is registered with PROSPERO (CRD42024529706).
Findings
- 57 studies from 35 cohorts were included in the systematic review and 31 studies from 24 cohorts were included in meta-analyses.
- For all-cause mortality, cardiovascular disease incidence, dementia, and falls, an inverse non-linear dose-response association was found, with inflection points at around 5000–7000 steps per day.
- An inverse linear association was found for cardiovascular disease mortality, cancer incidence, cancer mortality, type 2 diabetes incidence, and depressive symptoms.
- Based on our meta-analyses, compared with 2000 steps per day, 7000 steps per day was associated with a 47% lower risk of all-cause mortality (HR 0·53 [95% CI 0·46–0·60]; I2=36·3; 14 studies), a 25% lower risk of cardiovascular disease incidence (HR 0·75 [0·67–0·85]; I2=38·3%; six studies), a 47% lower risk of cardiovascular disease mortality (HR 0·53 [0·37–0·77]; I2=78·2%; three studies), a non-significant 6% lower risk of cancer incidence (HR 0·94 [0·87–1·01]; I2=73·7%; two studies), a 37% lower risk of cancer mortality (HR 0·63 [0·55–0·72]; I2=64·5%; three studies), a 14% lower risk of type 2 diabetes (HR 0·86 [0·74–0·99]; I2=48·5%; four studies), a 38% lower risk of dementia (HR 0·62 [0·53–0·73]; I2=0%; two studies), a 22% lower risk of depressive symptoms (HR 0·78 [0·73–0·83]; I2=36·2%; three studies), and a 28% lower risk of falls (HR 0·72 [0·65–0·81]; I2=47·5%; four studies).
- Studies on physical function (not based on meta-analysis) reported similar inverse associations.
- The evidence certainty was moderate for all outcomes except for cardiovascular disease mortality (low), cancer incidence (low), physical function (low), and falls (very low).
Interpretation
- Although 10000 steps per day can still be a viable target for those who are more active, 7000 steps per day is associated with clinically meaningful improvements in health outcomes and might be a more realistic and achievable target for some. The findings of the study should be interpreted in light of limitations, such as the small number of studies available for most outcomes, a lack of age-specific analysis and biases at the individual study level, including residual confounding.
Notes:
- In our meta-analyses, health risks generally continued to decrease with every 1000 steps per day increment across most outcomes, up to the highest analysable category of 12 000 steps per day. Although 10 000 steps per day, an unofficial target for decades without a clear evidence base,9 was associated with substantially lower risks for all-cause mortality, cardiovascular disease incidence, cancer mortality, dementia, and depressive symptoms than 7000 steps per day, the incremental improvement beyond 7000 steps per day was small, and there was no statistical difference between 7000 steps per day and a higher step count for all the other outcomes.
- Therefore, 7000 steps per day might be a more realistic and achievable recommendation for some, but 10000 steps per day can still be a viable target for those who are more active. Importantly, even a modest step count was associated with lower risk.
- For example, 4000 steps per day compared with 2000 steps per day was associated with substantial risk reduction, such as a 36% lower risk in all-cause mortality (table 2)
- Therefore, 7000 steps per day might be a more realistic and achievable recommendation for some, but 10000 steps per day can still be a viable target for those who are more active. Importantly, even a modest step count was associated with lower risk.
| All-cause mortality | Cardiovascular disease incidence | Cardiovascular disease mortality | Cancer incidence | Cancer mortality | Type 2 diabetes incidence† | Dementia | Depressive symptoms | Falls | |
|---|---|---|---|---|---|---|---|---|---|
| Number of studies | 14 | 6 | 3 | 2 | 3 | 4 | 2 | 3 | 4 |
| Number of sample size | 161,176 | 111,349 | 120,758 | 100,505 | 105,660 | 61,594 | 79,699 | 77,565 | 94,901 |
| Steps per day | |||||||||
| 2000 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| 3000 | 0·77 (0·71–0·83) | 0·93 (0·90–0·96) | 0·74 (0·60–0·91) | 0·99 (0·97–1·00) | 0·82 (0·74–0·9) | 0·97 (0·94–1·00) | 0·9 (0·86–0·93) | 0·95 (0·94–0·96) | 0·93 (0·90–0·95) |
| 4000 | 0·64 (0·57–0·73) | 0·87 (0·81–0·93) | 0·61 (0·44–0·85) | 0·97 (0·95–1·00) | 0·72 (0·63–0·82) | 0·94 (0·89–1·00) | 0·81 (0·75–0·87) | 0·91 (0·88–0·93) | 0·86 (0·81–0·91) |
| 5000 | 0·57 (0·5–0·66) | 0·82 (0·75–0·90) | 0·55 (0·37–0·80) | 0·96 (0·92–1·00) | 0·66 (0·58–0·76) | 0·91 (0·83–1·00) | 0·73 (0·66–0·81) | 0·86 (0·83–0·90) | 0·8 (0·74–0·87) |
| 6000 | 0·54 (0·47–0·62) | 0·78 (0·70–0·87) | 0·53 (0·36–0·77) | 0·95 (0·9–1·00) | 0·64 (0·56–0·73) | 0·88 (0·78–1·00) | 0·67 (0·58–0·77) | 0·82 (0·78–0·87) | 0·76 (0·69–0·84) |
| 7000 | 0·53 (0·46–0·6) | 0·75 (0·67–0·85) | 0·53 (0·37–0·77) | 0·94 (0·87–1·01) | 0·63 (0·55–0·72) | 0·86 (0·74–1·00) | 0·62 (0·53–0·73) | 0·78 (0·73–0·83) | 0·72 (0·65–0·81) |
| 8000 | 0·52 (0·46–0·6) | 0·73 (0·64–0·83) | 0·54 (0·38–0·78) | 0·93 (0·85–1·01) | 0·63 (0·54–0·72) | 0·83 (0·69–0·99) | 0·58 (0·49–0·70) | 0·74 (0·69–0·80) | 0·70 (0·62–0·79) |
| 9000 | 0·52 (0·46–0·6) | 0·71 (0·62–0·81) | 0·56 (0·39–0·79) | 0·91 (0·83–1·01) | 0·62 (0·53–0·72) | 0·81 (0·65–0·99) | 0·56 (0·47–0·67) | 0·71 (0·64–0·78) | 0·70 (0·62–0·78) |
| 10000 | 0·52 (0·45–0·59) | 0·70 (0·62–0·79) | 0·56 (0·40–0·79) | 0·90 (0·81–1·01) | 0·6 (0·51–0·70) | 0·78 (0·61–0·99) | 0·55 (0·46–0·66) | 0·67 (0·61–0·75) | 0·70 (0·63–0·79) |
| 11000 | 0·49 (0·43–0·57) | 0·69 (0·62–0·78) | 0·54 (0·38–0·76) | 0·89 (0·78–1·01) | 0·56 (0·48–0·66) | 0·76 (0·58–0·99) | 0·56 (0·47–0·67) | 0·64 (0·57–0·72) | 0·73 (0·65–0·83) |
| 12000 | 0·45 (0·39–0·53) | 0·69 (0·62–0·78) | 0·48 (0·33–0·71) | 0·88 (0·76–1·01) | 0·50 (0·41–0·60) | 0·73 (0·54–0·99) | 0·58 (0·49–0·70) | 0·61 (0·53–0·70) | 0·78 (0·67–0·92) |
Reference:
- Ding, Ding et al. Daily steps and health outcomes in adults: a systematic review and dose-response meta-analysis The Lancet Public Health, Volume 10, Issue 8, e668 - e681
Study: Do the associations of daily steps with mortality and incident cardiovascular disease differ by sedentary time levels? A device-based cohort study
Objectives
- This study aims to examine the associations of daily step count with all-cause mortality and incident cardiovascular disease (CVD) by sedentary time levels and to determine if the minimal and optimal number of daily steps is modified by high sedentary time.
Methods
- Using data from the UK Biobank, this was a prospective dose–response analysis of total daily steps across low (<10.5,hours/day) and high (≥10.5,hours/day) sedentary time (as defined by the inflection point of the adjusted absolute risk of sedentary time with the two outcomes). Mortality and incident CVD was ascertained through 31 October 2021.
Results
- Among 72,174 participants (age=61.1±7.8 years), 1633 deaths and 6190 CVD events occurred over 6.9 (±0.8) years of follow-up.
- Compared with the referent 2200 steps/day (5th percentile), the optimal dose (nadir of the curve) for all-cause mortality ranged between 9000 and 10,500 steps/day for high (HR (95% CI)=0.61 (0.51 to 0.73)) and low (0.69 (0.52 to 0.92)) sedentary time.
- For incident CVD, there was a subtle gradient of association by sedentary time level with the lowest risk observed at approximately 9700 steps/day for high (0.79 (0.72 to 0.86)) and low (0.71 (0.61 to 0.83)) sedentary time.
- The minimal dose (steps/day associated with 50% of the optimal dose) of daily steps was between 4000 and 4500 steps/day across sedentary time groups for all-cause mortality and incident CVD.
Conclusions
- Any amount of daily steps above the referent 2200 steps/day was associated with lower mortality and incident CVD risk, for low and high sedentary time.
- Accruing 9000–10,500 steps/day was associated with the lowest mortality risk independent of sedentary time.
- For a roughly equivalent number of steps/day, the risk of incident CVD was lower for low sedentary time compared with high sedentary time.
Reference:
- Ahmadi MN, Rezende LFM, Ferrari G, Del Pozo Cruz B, Lee IM, Stamatakis E. Do the associations of daily steps with mortality and incident cardiovascular disease differ by sedentary time levels? A device-based cohort study. Br J Sports Med. 2024 Mar 8;58(5):261-268. doi: 10.1136/bjsports-2023-107221. PMID: 38442950; PMCID: PMC10958308.
Study: Effectiveness and cost-effectiveness of an individualised, progressive walking and education intervention for the prevention of low back pain recurrence in Australia (WalkBack): a randomised controlled trial
Background:
- Recurrence of low back pain is common and a substantial contributor to the disease and economic burden of low back pain. Exercise is recommended to prevent recurrence, but the effectiveness and cost-effectiveness of an accessible and low-cost intervention, such as walking, is yet to be established.
- We aimed to investigate the clinical effectiveness and cost-effectiveness of an individualised, progressive walking and education intervention to prevent the recurrence of low back pain.
Methods:
- WalkBack was a two-armed, randomised controlled trial, which recruited adults (aged 18 years or older) from across Australia who had recently recovered from an episode of non-specific low back pain that was not attributed to a specific diagnosis, and which lasted for at least 24 h. Participants were randomly assigned to an individualised, progressive walking and education intervention facilitated by six sessions with a physiotherapist across 6 months or to a no treatment control group (1:1).
- The randomisation schedule comprised randomly permuted blocks of 4, 6, and 8 and was stratified by history of more than two previous episodes of low back pain and referral method. Physiotherapists and participants were not masked to allocation.
- Participants were followed for a minimum of 12 months and a maximum of 36 months, depending on the date of enrolment. The primary outcome was days to the first recurrence of an activity-limiting episode of low back pain, collected in the intention-to-treat population via monthly self-report.
- Cost-effectiveness was evaluated from the societal perspective and expressed as incremental cost per quality-adjusted life-year (QALY) gained. The trial was prospectively registered (ACTRN12619001134112).
Findings:
- Between Sept 23, 2019, and June 10, 2022, 3206 potential participants were screened for eligibility, 2505 (78%) were excluded, and 701 were randomly assigned (351 to the intervention group and 350 to the no treatment control group).
- Most participants were female (565
[0%]of 701) and the mean age of participants was 54 years (SD 12).
- Most participants were female (565
- The intervention was effective in preventing an episode of activity-limiting low back pain (hazard ratio 0·72 [95% CI 0·60-0·85], p=0·0002).
- The median days to a recurrence was 208 days (95% CI 149-295) in the intervention group and 112 days (89-140) in the control group.
- The incremental cost per QALY gained was AU$7802, giving a 94% probability that the intervention was cost-effective at a willingness-to-pay threshold of $28,000.
- Although the total number of participants experiencing at least one adverse event over 12 months was similar between the intervention and control groups (183
[0%]of 351 and 190[0%]of 350, respectively, p=0·60), there was a greater number of adverse events related to the lower extremities in the intervention group than in the control group (100 in the intervention group and 54 in the control group).
Interpretation:
- An individualised, progressive walking and education intervention significantly reduced low back pain recurrence.
- This accessible, scalable, and safe intervention could affect how low back pain is managed.
Reference:
- Pocovi NC, Lin CC, French SD, Graham PL, van Dongen JM, Latimer J, Merom D, Tiedemann A, Maher CG, Clavisi O, Tong SYK, Hancock MJ. Effectiveness and cost-effectiveness of an individualised, progressive walking and education intervention for the prevention of low back pain recurrence in Australia (WalkBack): a randomised controlled trial. Lancet. 2024 Jun 19:S0140-6736(24)00755-4. doi: 10.1016/S0140-6736(24)00755-4. Epub ahead of print. PMID: 38908392.
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(24)00755-4/fulltext
Study: Effect of Moderate to Vigorous Physical Activity on All-Cause Mortality in Middle-aged and Older Australians
Importance:
- Few studies have examined how different proportions of moderate and vigorous physical activity affect health outcomes.
Objective:
- To examine whether the proportion of total moderate to vigorous activity (MVPA) that is achieved through vigorous activity is associated with all-cause mortality independently of the total amount of MVPA.
Design, setting, and participants:
- We performed a prospective cohort study with activity data linked to all-cause mortality data from February 1, 2006, through June 15, 2014, in 204,542 adults aged 45 through 75 years from the 45 and Up population-based cohort study from New South Wales, Australia (mean [SD] follow-up, 6.52 [1.23] years). Associations between different contributions of vigorous activity to total MVPA and mortality were examined using Cox proportional hazards models, adjusted for total MVPA and sociodemographic and health covariates.
Exposures:
- Different proportions of total MVPA as vigorous activity. Physical activity was measured with the Active Australia Survey.
Main outcomes and measures:
- All-cause mortality during the follow-up period.
Results:
- During 1,444,927 person-years of follow-up, 7435 deaths were registered.
- Compared with those who reported no MVPA (crude death rate, 8.34%), the adjusted hazard ratios for all-cause mortality were 0.66 (95% CI, 0.61-0.71; crude death rate, 4.81%), 0.53 (95% CI, 0.48-0.57; crude death rate, 3.17%), and 0.46 (95% CI, 0.43-0.49; crude death rate, 2.64%) for reporting 10 through 149, 150 through 299, and 300 min/wk or more of activity, respectively.
- Among those who reported any MVPA, the proportion of vigorous activity revealed an inverse dose-response relationship with all-cause mortality: compared with those reporting no vigorous activity (crude death rate, 3.84%) the fully adjusted hazard ratio was 0.91 (95% CI, 0.84-0.98; crude death rate, 2.35%) in those who reported some vigorous activity (but <30% of total activity) and 0.87 (95% CI, 0.81-0.93; crude death rate, 2.08%) among those who reported 30% or more of activity as vigorous.
- These associations were consistent in men and women, across categories of body mass index and volume of MVPA, and in those with and without existing cardiovascular disease or diabetes mellitus.
Conclusions and relevance:
- Among people reporting any activity, there was an inverse dose-response relationship between proportion of vigorous activity and mortality.
- Our findings suggest that vigorous activities should be endorsed in clinical and public health activity guidelines to maximize the population benefits of physical activity.
Reference:
- Gebel K, Ding D, Chey T, Stamatakis E, Brown WJ, Bauman AE. Effect of Moderate to Vigorous Physical Activity on All-Cause Mortality in Middle-aged and Older Australians. JAMA Intern Med. 2015 Jun;175(6):970-7. doi: 10.1001/jamainternmed.2015.0541. Erratum in: JAMA Intern Med. 2015 Jul;175(7):1248. doi: 10.1001/jamainternmed.2015.2975. PMID: 25844882.
Study: Effects of various exercise interventions in insomnia patients: a systematic review and network meta-analysis
Objectives
- To compare the effectiveness of different exercise interventions in improving sleep quality and alleviating insomnia severity among patients with insomnia.
Design
- Our study design was a systematic review and network meta-analysis.
Eligibility criteria
- Our study eligibility criteria was restricted to include randomised controlled trials (RCTs) involving adults with insomnia that evaluated exercise-based interventions.
Data sources
- PubMed, Cochrane Library, Embase, Web of Science, SPORTDiscus, and PsycINFO databases were systematically searched from inception to 1 April 2025.
Risk of bias and certainty assessment
- Risk of bias was assessed using the Cochrane Risk of Bias 2 Tool. The certainty of the evidence was evaluated using the Confidence in Network Meta-Analysis (CINeMA) platform.
Synthesis of results
- A frequentist network meta-analysis was performed to assess the effectiveness of interventions, with outcomes presented as mean differences (MDs) and 95% confidence intervals (95% CIs). Sleep outcomes were measured using validated tools, including the Pittsburgh Sleep Quality Index (PSQI), Insomnia Severity Index (ISI), sleep diaries, and combined objective sleep measures such as polysomnography or actigraphy.
Results
- The review included 1348 participants from 22 RCTs, examining 13 distinct interventions, of which seven were exercise-based: yoga, Tai Chi, walking or jogging, aerobic plus strength exercise, strength training alone, aerobic exercise combined with therapy, and mixed aerobic exercises.
- Among the included trials, four (18%) were rated as low risk of bias, 15 (68%) had some concerns, and three (14%) were considered to have a high risk.
- Compared with active controls (eg, usual care, lifestyle modifications):
- Yoga likely results in a large increase in total sleep time (MD 110.88 minutes (min), 95% CI 58.66 to 163.09; moderate-certainty evidence) and may improve sleep efficiency (MD 15.59%, 95% CI 5.76 to 25.42; low-certainty evidence), reduce wake after sleep onset (MD −55.91 min, 95% CI −98.14 to −13.68; low-certainty evidence), and shorten sleep onset latency (MD −29.27 min, 95% CI −50.09 to −8.45; low-certainty evidence), all based on sleep diary data.
- Walking or jogging may result in a large reduction in ISI scores (MD −9.57 points, 95% CI −12.12 to −7.02; low-certainty evidence).
- Tai Chi may reduce PSQI scores (MD −4.57 points, 95% CI −7.50 to −1.63; low-certainty evidence), increase total sleep time (MD 52.07 min, 95% CI 25.53 to 78.61; low-certainty evidence), reduce wake after sleep onset (MD −36.11 min, 95% CI −62.81 to −9.42; low-certainty evidence), and shorten sleep onset latency (MD −24.76 min, 95% CI −41.07 to −8.46; low-certainty evidence), also based on sleep diary data. Additionally, Tai Chi may increase total sleep time as measured by combined objective sleep measures (MD 24.09 min, 95% CI 4.66 to 43.52; low-certainty evidence).
Conclusion
- Exercise is an effective treatment for improving sleep in patients with insomnia.
- Among the various exercise interventions, yoga, Tai Chi and walking or jogging are more effective than other exercises. To further validate and strengthen these conclusions, large-scale, high-quality and well-designed RCTs are needed.
Reference:
- Bu Z, Liu F, Shahjalal M, et al Effects of various exercise interventions in insomnia patients: a systematic review and network meta-analysis BMJ Evidence-Based Medicine Published Online First: 15 July 2025. doi: 10.1136/bmjebm-2024-113512
Study: Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men
BLUF:
- Keto diet does NOT result in increased body fat loss
- Is associated with relatively small increases in energy expenditure
Background:
- The carbohydrate-insulin model of obesity posits that habitual consumption of a high-carbohydrate diet sequesters fat within adipose tissue because of hyperinsulinemia and results in adaptive suppression of energy expenditure (EE). Therefore, isocaloric exchange of dietary carbohydrate for fat is predicted to result in increased EE, increased fat oxidation, and loss of body fat. In contrast, a more conventional view that "a calorie is a calorie" predicts that isocaloric variations in dietary carbohydrate and fat will have no physiologically important effects on EE or body fat.
Objective:
- We investigated whether an isocaloric low-carbohydrate ketogenic diet (KD) is associated with changes in EE, respiratory quotient (RQ), and body composition.
Design:
- Seventeen overweight or obese men were admitted to metabolic wards, where they consumed a high-carbohydrate baseline diet (BD) for 4 wk followed by 4 wk of an isocaloric KD with clamped protein. Subjects spent 2 consecutive days each week residing in metabolic chambers to measure changes in EE (EEchamber), sleeping EE (SEE), and RQ. Body composition changes were measured by dual-energy X-ray absorptiometry. Average EE during the final 2 wk of the BD and KD periods was measured by doubly labeled water (EEDLW).
Results:
- Subjects lost weight and body fat throughout the study corresponding to an overall negative energy balance of ∼300 kcal/d.
- Compared with BD, the KD coincided with increased EEchamber (57 ± 13 kcal/d, P = 0.0004) and SEE (89 ± 14 kcal/d, P < 0.0001) and decreased RQ (-0.111 ± 0.003, P < 0.0001).
- EEDLW increased by 151 ± 63 kcal/d (P = 0.03).
- Body fat loss slowed during the KD and coincided with increased protein utilization and loss of fat-free mass.
Conclusion:
- The isocaloric KD was not accompanied by increased body fat loss but was associated with relatively small increases in EE that were near the limits of detection with the use of state-of-the-art technology. This trial was registered at clinicaltrials.gov as NCT01967563.
Reference:
- Hall KD, Chen KY, Guo J, Lam YY, Leibel RL, Mayer LE, Reitman ML, Rosenbaum M, Smith SR, Walsh BT, Ravussin E. Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men. Am J Clin Nutr. 2016 Aug;104(2):324-33. doi: 10.3945/ajcn.116.133561. Epub 2016 Jul 6. PMID: 27385608; PMCID: PMC4962163.
Study: Exercise training enhances muscle mitochondrial metabolism in diet-resistant obesity
Background Current paradigms for predicting weight loss in response to energy restriction have general validity but a subset of individuals fail to respond adequately despite documented diet adherence. Patients in the bottom 20% for rate of weight loss following a hypocaloric diet (diet-resistant) have been found to have less type I muscle fibres and lower skeletal muscle mitochondrial function, leading to the hypothesis that physical exercise may be an effective treatment when diet alone is inadequate. In this study, we aimed to assess the efficacy of exercise training on mitochondrial function in women with obesity with a documented history of minimal diet-induced weight loss.
Methods From over 5000 patient records, 228 files were reviewed to identify baseline characteristics of weight loss response from women with obesity who were previously classified in the top or bottom 20% quintiles based on rate of weight loss in the first 6 weeks during which a 900 kcal/day meal replacement was consumed. A subset of 20 women with obesity were identified based on diet-resistance (n=10) and diet sensitivity (n=10) to undergo a 6-week supervised, progressive, combined aerobic and resistance exercise intervention.
Findings Diet-sensitive women had lower baseline adiposity, higher fasting insulin and triglycerides, and a greater number of ATP-III criteria for metabolic syndrome. Conversely in diet-resistant women, the exercise intervention improved body composition, skeletal muscle mitochondrial content and metabolism, with minimal effects in diet-sensitive women. In-depth analyses of muscle metabolomes revealed distinct group- and intervention- differences, including lower serine-associated sphingolipid synthesis in diet-resistant women following exercise training.
Interpretation Exercise preferentially enhances skeletal muscle metabolism and improves body composition in women with a history of minimal diet-induced weight loss. These clinical and metabolic mechanism insights move the field towards better personalised approaches for the treatment of distinct obesity phenotypes.
Reference:
Study: Exploring the Relationship between Walking and Emotional Health in China
Walking has a positive impact on people’s emotional health. However, in the case of serious air pollution, it is controversial whether walking exercise can still improve individuals’ emotional health.
Using data from the 2014 wave of the China Labor-Force Dynamics Survey, this study explored the relationship between walking and emotional health with different levels of environmental pollution.
The results indicated that respondents who took regular walks had better emotional health than those who did not walk regularly.
For those whose main mode of physical exercise was walking, the average number of walks per week was significantly and positively correlated with their emotional health; however, the average duration of the walk had no significant impact on their emotional health.
Moreover, for those whose main mode of physical exercise was walking and who lived in neighborhoods with a polluted environment, regular walking still had a positive impact on their emotional health.
This suggests that even if environmental pollution is serious, walking still plays an important role in regulating individuals’ mental health. We propose that in order to promote the emotional health of residents, it is necessary to create more public spaces for outdoor activities and simultaneously increase efforts to control environmental pollution.
Reference:
- Zhu Z, Chen H, Ma J, He Y, Chen J, Sun J. Exploring the Relationship between Walking and Emotional Health in China. Int J Environ Res Public Health. 2020 Nov 27;17(23):8804. doi: 10.3390/ijerph17238804. PMID: 33260796; PMCID: PMC7734587.
Study: Higher resistance training volume offsets muscle hypertrophy nonresponsiveness in older individuals
The magnitude of muscle hypertrophy in response to resistance training (RT) is highly variable between individuals (response heterogeneity). Manipulations in RT variables may modulate RT-related response heterogeneity; yet, this remains to be determined.
Using a within-subject unilateral design, we aimed to investigate the effects of RT volume manipulation on whole muscle hypertrophy [quadriceps muscle cross-sectional area (qCSA)] among nonresponders and responders to a low RT dose (single-set). We also investigated the effects of RT volume manipulation on muscle strength in these responsiveness groups.
Methods
- Eighty-five older individuals [41M/44F, age = 68 ± 4 yr; body mass index (BMI) = 26.4 ± 3.7 kg/m2] had one leg randomly allocated to a single (1)-set and the contralateral leg allocated to four sets of unilateral knee-extension RT at 8-15 repetition maximum (RM) for 10-wk 2 days/wk.
- Pre- and postintervention, participants underwent magnetic resonance imaging (MRI) and unilateral knee-extension 1-RM strength testing. MRI typical error (2× TE = 3.27%) was used to classify individuals according to responsiveness patterns. n = 51 were classified as nonresponders (≤2× TE) and n = 34 as responders (>2× TE) based on pre- to postintervention change qCSA following the single-set RT protocol.
Results
- Nonresponders to single-set training showed a dose response, with significant time × set interactions for qCSA and 1-RM strength, indicating greater gains in response to the higher volume prescription (time × set: P < 0.05 for both outcomes).
- Responders improved qCSA (time: P < 0.001), with a tendency toward higher benefit from the four sets RT protocol (time × set: P = 0.08); on the other hand, 1-RM increased similarly irrespectively of RT volume prescription (time × set: P > 0.05).
Conclusions
- Our findings support the use of higher RT volume to mitigate nonresponsiveness among older adults.
- NEW & NOTEWORTHY Using a within-subject unilateral design, we demonstrated that increasing resistance training (RT) volume may be a simple, effective strategy to improve muscle hypertrophy and strength gains among older adults who do not respond to low-volume RT. In addition, it could most likely be used to further improve hypertrophic outcomes in responders.
Reference:
- Lixandrão ME, Bamman M, Vechin FC, Conceicao MS, Telles G, Longobardi I, Damas F, Lavin KM, Drummer DJ, McAdam JS, Dungan CM, Leitão AE, Riani Costa LA, Aihara AY, Libardi CA, Gualano B, Roschel H. Higher resistance training volume offsets muscle hypertrophy nonresponsiveness in older individuals. J Appl Physiol (1985). 2024 Feb 1;136(2):421-429. doi: 10.1152/japplphysiol.00670.2023. Epub 2024 Jan 4. PMID: 38174375.
- https://pubmed.ncbi.nlm.nih.gov/38174375/
Study: Long-term time-course of strength adaptation to minimal dose resistance training: Retrospective longitudinal growth modelling of a large cohort through training records
Public health guidelines for resistance training emphasize a minimal effective dose intending for individuals to engage in these behaviors long term. However, few studies have adequately examined the longitudinal time-course of strength adaptations to resistance training.
Purpose:
- The aim of this study was to examine the time-course of strength development from minimal-dose resistance training in a large sample through retrospective training records from a private international exercise company.
Methods:
- Data were available for analysis from 14,690 participants (60% female; aged 48 ± 11 years) having undergone minimal-dose resistance training (1x/week, single sets to momentary failure of six exercises) up to 352 weeks (~6.8 years) in length. Linear-log growth models examined strength development over time allowing random intercepts and slopes by participant.
Results:
- All models demonstrated a robust linear-log relationship with the first derivatives (i.e., changes in strength with time) trending asymptotically such that by ~1-2 years strength had practically reached a "plateau."
- Sex, bodyweight, and age had minimal interaction effects.
- However, substantial strength gains were apparent; approximately ~30-50% gains over the first year reaching ~50-60% of baseline 6 years later.
Conclusion:
- It is unclear if the "plateau" can be overcome through alternative approaches, or whether over the long-term strength gains differ. Considering this, our results support public health recommendations for minimal-dose resistance training for strength adaptations in adults.
Reference:
- Steele J, Fisher JP, Giessing J, Androulakis-Korakakis P, Wolf M, Kroeske B, Reuters R. Long-Term Time-Course of Strength Adaptation to Minimal Dose Resistance Training Through Retrospective Longitudinal Growth Modeling. Res Q Exerc Sport. 2023 Dec;94(4):913-930. doi: 10.1080/02701367.2022.2070592. Epub 2022 May 19. PMID: 35591809.
- https://osf.io/preprints/sportrxiv/eq485
Study: Maximizing Muscle Hypertrophy: A Systematic Review of Advanced Resistance Training Techniques and Methods
Background:
- Effective hypertrophy-oriented resistance training (RT) should comprise a combination of mechanical tension and metabolic stress. Regarding training variables, the most effective values are widely described in the literature. However, there is still a lack of consensus regarding the efficiency of advanced RT techniques and methods in comparison to traditional approaches.
Methods:
- MEDLINE and SPORTDiscus databases were searched from 1996 to September 2019 for all studies investigating the effects of advanced RT techniques and methods on muscle hypertrophy and training variables. Thirty articles met the inclusion criteria and were consequently included for the quality assessment and data extraction.
Results:
- Concerning the time-efficiency of training, the use of agonist–antagonist, upper–lower body supersets, drop and cluster sets, sarcoplasma stimulating training, employment of fast, but controlled duration of eccentric contractions (~2s), and high-load RT supplemented with low-load RT under blood flow restriction may provide an additional stimulus and an advantage to traditional training protocols.
- With regard to the higher degree of mechanical tension, the use of accentuated eccentric loading in RT should be considered. Implementation of drop sets, sarcoplasma stimulating training, low-load RT in conjunction with low-load RT under blood flow restriction could provide time-efficient solutions to increased metabolic stress.
Conclusions:
- Due to insufficient evidence, it is difficult to provide specific guidelines for volume, intensity of effort, and frequency of previously mentioned RT techniques and methods.
- However, well-trained athletes may integrate advanced RT techniques and methods into their routines as an additional stimulus to break through plateaus and to prevent training monotony.
Reference:
- Krzysztofik M, Wilk M, Wojdała G, Gołaś A. Maximizing Muscle Hypertrophy: A Systematic Review of Advanced Resistance Training Techniques and Methods. Int J Environ Res Public Health. 2019 Dec 4;16(24):4897. doi: 10.3390/ijerph16244897. PMID: 31817252; PMCID: PMC6950543.
Study: Move less, spend more: the metabolic demands of short walking bouts
The metabolic cost of steady-state walking is well known; however, across legged animals, most walking bouts are too short to reach steady state. Here, we investigate how bout duration affects the metabolic cost of human walking with varying mechanical power, metabolic intensity and duration.
Ten participants walked for 10- to 240-s bouts on a stair climber at 0.20, 0.25 and 0.36 m s−1 and on a treadmill at 1.39 m s−1. Oxygen uptake was time-integrated and divided by bout duration to get bout average uptake (V̇O2(b)). Fitting of oxygen uptake kinetics allowed calculating non-metabolic oxygen exchange during phase-I transient and, hence, non-steady-state metabolic cost (C met(b)) and efficiency. For 240-s bouts, such variables were also calculated at steady state.
Across all conditions, shorter bouts had higher V̇O2(b) and C met(b), with proportionally greater non-metabolic oxygen exchange. As the bout duration increased, V̇O2(b), C met(b) and efficiency approached steady-state values.
Our findings show that the time-averaged oxygen uptake and metabolic cost are greater for shorter than longer bouts: 30-s bouts consume 20–60% more oxygen than steady-state extrapolations.
This is partially explained by the proportionally greater non-metabolic oxygen uptake and leads to lower efficiency for shorter bouts. Inferring metabolic cost from steady state substantially underestimates energy expenditure for short bouts.
Reference:
- Luciano F., Ruggiero L., Minetti A. E. and Pavei G. 2024Move less, spend more: the metabolic demands of short walking boutsProc. R. Soc. B.29120241220 http://doi.org/10.1098/rspb.2024.1220
Study: Movement Is Medicine: Structured Exercise Program May Lower Risk of Cancer Recurrence and Death for Some Colon Cancer Survivors
Key Findings
- Patients in both groups improved their physical function and sustained it, but it was significantly higher for patients in the structured exercise program. They had improvements that were maintained over all three years, in recreational physical activity, predicted VO2 max, and distance they could walk in six minutes.
- After a median follow-up of 7.9 years, 93 patients in the structured exercise program had their cancer recur, compared to 131 patients in the health education materials group. At five years, the disease-free survival rate was 80% in the structured exercise program and 74% in the health education materials group. Patients in the structured exercise program had a 28% lower risk of recurrent or new cancers developing than patients who only received health education materials.
- There were 41 people in the structured exercise program and 66 people in the health education materials group who died. After 8 years, overall survival was 90% in the structured exercise program and 83% in the health education materials group. Patients had a 37% lower risk of death if they participated in the structured exercise program.
Focus
- Stage III or high-risk stage II colon cancer
Population
- 889 patients from Canada and Australia with a median age of 61 years
Main Takeaway
- For patients with stage III and high-risk stage II colon cancer, a structured exercise program following surgery and adjuvant chemotherapy reduced the risk of recurrent or new cancer and increased survival.
Significance
- Colorectal cancer is the second-leading cause of cancer-related death worldwide, with the majority of these cancers being found in the colon. About 106,000 people will be diagnosed with colon cancer in the United States in 2025.
- When colon cancer is diagnosed at an earlier stage, it is easier to treat. Patients with stage III and high-risk stage II colon cancer usually have surgery to remove their tumors followed by chemotherapy to destroy any remaining cancer cells. Despite this treatment, colon cancer recurs in about 30% of these patients. After a recurrence, colon cancer can be harder to treat, and many of these patients will die of the disease.
- Many official guidelines recommend a healthy lifestyle, which includes a well-balanced diet and regular exercise. But even with these guidelines, patients usually receive minimal education and little support for incorporating exercise into their routine.
- This is the first randomized clinical trial to specifically evaluate if a structured exercise program can reduce the risk of recurrent or new cancer for a subset of patients with colon cancer.
Reference:
Study: Non-occupational physical activity and risk of cardiovascular disease, cancer and mortality outcomes:s a dose–response meta-analysis of large prospective studies
BLUF:
- 75 minutes a week of moderate-intensity exercise (which includes brisk walking) per week (11 min/day) lowered the risk of:
- Early death by 23%
- Cardiovascular disease by 17%
- Cancer by 7%
Objective
- To estimate the dose–response associations between non-occupational physical activity and several chronic disease and mortality outcomes in the general adult population.
Design
- Systematic review and cohort-level dose-response meta-analysis.
Data sources
- PubMed, Scopus, Web of Science and reference lists of published studies.
Eligibility criteria
- Prospective cohort studies with (1) general population samples >10 000 adults, (2) ≥3 physical activity categories, and (3) risk measures and CIs for all-cause mortality or incident total cardiovascular disease, coronary heart disease, stroke, heart failure, total cancer and site-specific cancers (head and neck, myeloid leukaemia, myeloma, gastric cardia, lung, liver, endometrium, colon, breast, bladder, rectum, oesophagus, prostate, kidney).
Results
- 196 articles were included, covering 94 cohorts with >30 million participants. The evidence base was largest for all-cause mortality (50 separate results; 163 415 543 person-years, 811 616 events), and incidence of cardiovascular disease (37 results; 28 884 209 person-years, 74 757 events) and cancer (31 results; 35 500 867 person-years, 185 870 events).
- In general, higher activity levels were associated with lower risk of all outcomes.
- Differences in risk were greater between 0 and 8.75 marginal metabolic equivalent of task-hours per week (mMET-hours/week) (equivalent to the recommended 150 min/week of moderate-to-vigorous aerobic physical activity), with smaller marginal differences in risk above this level to 17.5 mMET-hours/week, beyond which additional differences were small and uncertain.
- Associations were stronger for all-cause (relative risk (RR) at 8.75 mMET-hours/week: 0.69, 95% CI 0.65 to 0.73) and cardiovascular disease (RR at 8.75 mMET-hours/week: 0.71, 95% CI 0.66 to 0.77) mortality than for cancer mortality (RR at 8.75 mMET-hours/week: 0.85, 95% CI 0.81 to 0.89).
- If all insufficiently active individuals had achieved 8.75 mMET-hours/week, 15.7% (95% CI 13.1 to 18.2) of all premature deaths would have been averted.
Conclusions
- Inverse non-linear dose–response associations suggest substantial protection against a range of chronic disease outcomes from small increases in non-occupational physical activity in inactive adults.
Reference:
- Garcia L, Pearce M, Abbas A, et al Non-occupational physical activity and risk of cardiovascular disease, cancer and mortality outcomes: a dose–response meta-analysis of large prospective studies British Journal of Sports Medicine 2023;57:979-989.
Study: Oral Salt Supplementation During Ultradistance Exercise
Objective:
- The objective of this study was to determine whether sodium supplementation
- Influences changes in body weight, serum sodium [Na], and plasma volume (PV)
- Prevents hyponatremia in Ironman triathletes.
Setting:
- The study was carried out at the South African Ironman triathlon.
Participants:
- Thirty-eight athletes competing in the triathlon were given salt tablets to ingest during the race. Data collected from these athletes [salt intake group (SI)] were compared with data from athletes not given salt [no salt group (NS)].
Interventions:
- Salt tablets were given to the SI group to provide approximately 700 mg/h of sodium.
Main Outcome Measurements:
- Serum sodium, hemoglobin, and hematocrit were measured at race registration and after the race. Weights were measured before and after the race. Members of SI were retrospectively matched to subjects in NS for 1) weight change and 2) pre-race [Na].
Results:
- The SI group developed a 3.3-kg weight loss (p < 0.0001) and significantly increased their [Na] (Δ[Na] 1.52 mmol/L; p = 0.005). When matched for weight change during the race, SI increased their [Na] compared with NS (mean 1.52 versus 0.04 mmol/L), but this did not reach statistical significance (p = 0.08). When matched for pre-race [Na], SI had a significantly smaller percent body weight loss than NS (−4.3% versus −5.1%; p = 0.04). There was no significant difference in the increase of [Na] in both groups (1.57 versus 0.84 mmol/L). PV increased equally in both groups. None of the subjects finished the race with [Na] < 135 mmol/L.
Conclusions:
- Sodium ingestion was associated with a decrease in the extent of weight loss during the race.
- There was no evidence that sodium ingestion significantly influenced changes in [Na] or PV more than fluid replacement alone in the Ironman triathletes in this study.
- Sodium supplementation was not necessary to prevent the development of hyponatremia in these athletes who lost weight, indicating that they had only partially replaced their fluid and other losses during the Ironman triathlon.
Reference:
- Speedy, Dale B. MBChB, FRNZCGP, MSc, FACSM, FACSP*; Thompson, John M. D. PhD†; Rodgers, Ian BSc Hons‡; Collins, Malcolm PhD‡; Sharwood, Karen BSc Hons‡. Oral Salt Supplementation During Ultradistance Exercise. Clinical Journal of Sport Medicine 12(5):p 279-284, September 2002.
Study: Progression Models in Resistance Training for Healthy Adults
In order to stimulate further adaptation toward specific training goals, progressive resistance training (RT) protocols are necessary.
Strength Training
The optimal characteristics of strength-specific programs include the use of concentric (CON), eccentric (ECC), and isometric muscle actions and the performance of bilateral and unilateral single- and multiple-joint exercises. In addition, it is recommended that strength programs sequence exercises to optimize the preservation of exercise intensity (large before small muscle group exercises, multiple-joint exercises before single-joint exercises, and higher-intensity before lower-intensity exercises).
For novice (untrained individuals with no RT experience or who have not trained for several years) training, it is recommended that loads correspond to a repetition range of an 8-12 repetition maximum (RM).
For intermediate (individuals with approximately 6 months of consistent RT experience) to advanced (individuals with years of RT experience) training, it is recommended that individuals use a wider loading range from 1 to 12 RM in a periodized fashion with eventual emphasis on heavy loading (1-6 RM) using 3- to 5-min rest periods between sets performed at a moderate contraction velocity (1-2 s CON; 1-2 s ECC).
When training at a specific RM load, it is recommended that 2-10% increase in load be applied when the individual can perform the current workload for one to two repetitions over the desired number.
The recommendation for training frequency is 2-3 d·wk−1 for novice training, 3-4 d·wk−1 for intermediate training, and 4-5 d·wk−1 for advanced training.
Hypertrophy Training
Similar program designs are recommended for hypertrophy training with respect to exercise selection and frequency.
For loading, it is recommended that loads corresponding to 1-12 RM be used in periodized fashion with emphasis on the 6-12 RM zone using 1- to 2-min rest periods between sets at a moderate velocity.
Higher volume, multiple-set programs are recommended for maximizing hypertrophy.
- Progression in power training entails two general loading strategies:
- Strength training
- Use of light loads (0-60% of 1 RM for lower body exercises; 30-60% of 1 RM for upper body exercises) performed at a fast contraction velocity with 3-5 min of rest between sets for multiple sets per exercise (three to five sets).
- It is also recommended that emphasis be placed on multiple-joint exercises especially those involving the total body.
Local Endurance Training
For local muscular endurance training, it is recommended that light to moderate loads (40-60% of 1 RM) be performed for high repetitions (>15) using short rest periods (<90 s).
In the interpretation of this position stand as with prior ones, recommendations should be applied in context and should be contingent upon an individual's target goals, physical capacity, and training status.
Reference:
- Progression Models in Resistance Training for Healthy Adults. Medicine & Science in Sports & Exercise 41(3):p 687-708, March 2009. | DOI: 10.1249/MSS.0b013e3181915670
- https://journals.lww.com/acsm-msse/Fulltext/2009/03000/Progression_Models_in_Resistance_Training_for.26.aspx
Study: Relationship of Daily Step Counts to All-Cause Mortality and Cardiovascular Events
Background
- The minimal and optimal daily step counts for health improvements remain unclear.
Objectives
- A meta-analysis was performed to quantify dose-response associations of objectively measured step count metrics in the general population.
Methods
- Electronic databases were searched from inception to October 2022. Primary outcomes included all-cause mortality and incident cardiovascular disease (CVD). Study results were analyzed using generalized least squares and random-effects models.
Results
- In total, 111,309 individuals from 12 studies were included.
- Significant risk reductions were observed at 2,517 steps/d for all-cause mortality (adjusted HR [aHR]: 0.92; 95% CI: 0.84-0.999) and 2,735 steps/d for incident CVD (aHR: 0.89; 95% CI: 0.79-0.999) compared with 2,000 steps/d (reference).
- Additional steps resulted in nonlinear risk reductions of all-cause mortality and incident CVD with an optimal dose at 8,763 (aHR: 0.40; 95% CI: 0.38-0.43) and 7,126 steps/d (aHR: 0.49; 95% CI: 0.45-0.55), respectively.
- Increments from a low to an intermediate or a high cadence were independently associated with risk reductions of all-cause mortality. Sex did not influence the dose-response associations, but after stratification for assessment device and wear location, pronounced risk reductions were observed for hip-worn accelerometers compared with pedometers and wrist-worn accelerometers.
Conclusions
- As few as about 2,600 and about 2,800 steps/d yield significant mortality and CVD benefits, with progressive risk reductions up to about 8,800 and about 7,200 steps/d, respectively.
- Additional mortality benefits were found at a moderate to high vs a low step cadence.
- These findings can extend contemporary physical activity prescriptions given the easy-to-understand concept of step count. (Dose-Response Relationship Between Daily Step Count and Health Outcomes: A Systematic Review and Meta-Analyses; CRD42021244747)
Reference:
- Stens NA, Bakker EA, Mañas A, Buffart LM, Ortega FB, Lee DC, Thompson PD, Thijssen DHJ, Eijsvogels TMH. Relationship of Daily Step Counts to All-Cause Mortality and Cardiovascular Events. J Am Coll Cardiol. 2023 Oct 10;82(15):1483-1494. doi: 10.1016/j.jacc.2023.07.029. Epub 2023 Sep 6. PMID: 37676198.
Study: Resistance Exercise Training in Individuals With and Without Cardiovascular Disease: 2023 Update: A Scientific Statement From the American Heart Association edit
For healthy adults, regimens of 8 to 10 different exercises involving major muscle groups, each exercise performed in 1 to 3 sets of moderate-intensity loads that permits 8 to 12 repetitions per set to volitional fatigue, ≥2 times per week, is effective for achieving muscular and cardiovascular benefits.
Muscular strength is the ability of a muscle to generate force, and muscular endurance is the ability of a muscle to perform repeated contractions or maintain a contraction for a prolonged period of time. Lower repetitions (reps) with a heavier weight may better optimize muscular strength. Higher repetitions with a lighter weight may better enhance muscular endurance. Using weight loads that permit 8 to 12 repetitions, in general, will facilitate improvements in both muscular strength and endurance, provide cardiovascular health benefits, and be safe for the general population.
RT programs need not be time-consuming to be efficacious, requiring only 30 to 60 minutes per week (Figure 3). In general, a single set of 8 to 12 repetitions to volitional fatigue, using moderate weight loads of 40% to 60% of 1-RM, for 8 to 10 different exercises involving major muscle groups, performed twice per week are highly effective. Well-designed randomized controlled trials with long-term (≥6 months) interventions incorporating evidence-based behavior change and maintenance techniques are warranted and likely to reveal strategies for improved implementation of RT in clinical and nonclinical settings. Recent evidence clearly demonstrates that RT is a safe, effective, and essential component of the overall physical activity regimen for CVD risk reduction.
| Magnitude of benefit | Resistance | Aerobic | Combination | Conclusion | Summary of evidence | |
|---|---|---|---|---|---|---|
| Blood pressure | + | + | + | RT, AT, and CT have similar favorable, small to moderate effects on both systolic and diastolic BP | Systolic BP significantly reduced after RT (−1.8 mm Hg) and AT (−3.5 mm Hg), but insignificantly after CT (−1.4 mm Hg). Diastolic BP significantly reduced after RT (−3.2 mm Hg), AT (−2.5 mm Hg), and CT (−2.2 mm Hg).32 No significant differences between training types. | |
| Lipid profile | + | + | + | RT, AT, and CT have similar favorable small to moderate effects on lipids | RT, AT, and CT improve lipid profile (eg, triglyceride, HDL and LDL cholesterol) by 4%–5%. No significant differences between training types.33,34 | |
| Glycemic control | + | ++ | All modes have benefits. CT may have the strongest associations followed by AT, then RT. | In patients with type 2 diabetes, CT lowered HbA1c by 0.17% more than AT, and AT lowered HbA1c by 0.20% more than RT.35 In patients with prediabetes, CT and AT are superior to RT in reducing HbA1c and CT is most effective in controlling fasting blood glucose levels.10 | ||
| Body weight: Weight loss | 0 | + | + | AT and CT have small to moderate effects on weight loss. CT may be most beneficial for weight maintenance. | Greater reductions in body weight in CT (−2.0 kg) and AT (−1.2 kg), compared with RT.34 | |
| Weight maintenance | 0 | + | ++ | When used in combination with AT, RT may help assist with weight loss or maintenance by increasing resting metabolic rate, fat oxidation, and lean mass.36 | ||
| Body composition: Lean mass | ++ | + | RT is more beneficial for lean mass gains than AT. AT is more beneficial for fat mass loss than RT. CT provides the greatest benefits for both fat and lean mass. | Lean body mass improves more in CT (+0.9 kg) and RT (+1.3 kg), compared with AT.34 | ||
| Fat mass | 0 | ++ | Greater reductions in fat mass in CT (−1.9 kg) and AT (−1.2 kg), compared with RT.34 CT is also superior to AT or RT for reducing subcutaneous abdominal fat.37 |
Abstract: Resistance training not only can improve or maintain muscle mass and strength, but also has favorable physiological and clinical effects on cardiovascular disease and risk factors. This scientific statement is an update of the previous (2007) American Heart Association scientific statement regarding resistance training and cardiovascular disease. Since 2007, accumulating evidence suggests resistance training is a safe and effective approach for improving cardiovascular health in adults with and without cardiovascular disease. This scientific statement summarizes the benefits of resistance training alone or in combination with aerobic training for improving traditional and nontraditional cardiovascular disease risk factors. We also address the utility of resistance training for promoting cardiovascular health in varied healthy and clinical populations. Because less than one-third of US adults report participating in the recommended 2 days per week of resistance training activities, this scientific statement provides practical strategies for the promotion and prescription of resistance training.
Reference:
- Paluch AE, Boyer WR, Franklin BA, Laddu D, Lobelo F, Lee DC, McDermott MM, Swift DL, Webel AR, Lane A; on behalf the American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Epidemiology and Prevention; and Council on Peripheral Vascular Disease. Resistance Exercise Training in Individuals With and Without Cardiovascular Disease: 2023 Update: A Scientific Statement From the American Heart Association. Circulation. 2024 Jan 16;149(3):e217-e231. doi: 10.1161/CIR.0000000000001189. Epub 2023 Dec 7. PMID: 38059362; PMCID: PMC11209834.
Marathon/Ultramarathon Endurance Related
Study: Effect of Sodium Supplements and Climate on Dysnatremia During Ultramarathon Running
Objective:
- Analyze the effect of sodium supplementation, hydration, and climate on dysnatremia in ultramarathon runners.
Design:
- Prospective observational study.
Setting:
- The 2017 80 km (50 mile) stage of the 250 km (150 mile) 6-stage RacingThePlanet ultramarathon in 2017 Chilean, Patagonian, and 2018 Namibian, Mongolian, and Chilean deserts.
Participants:
- All race entrants who could understand English were invited to participate, with 266 runners enrolled, mean age of 43 years (± 9), 61 (36%) females, average weight 74 kg (± 12.5), and average race time 14.5 (± 4.1) hours. Post-race sodium collected on 174 (74%) and 164 (62%) participants with both the blood sample and post-race questionnaire.
Intervention:
- Weight change and finish line serum sodium levels were gathered.
Main outcome measures:
- Incidence of exercise-associated hyponatremia (EAH; <135 mmol·L−1) and hypernatremia (>145 mmol·L−1) by sodium ingestion and climate.
Results:
- Eleven (6.3%) runners developed EAH, and 30 (17.2%) developed hypernatremia. Those with EAH were 14 kg heavier at baseline, had significantly less training distances, and averaged 5 to 6 hours longer to cover 50 miles (80 km) than the other participants.
- Neither rate nor total ingested supplemental sodium was correlated with dysnatremia, without significant differences in drinking behaviors or type of supplement compared with normonatremic runners.
- Hypernatremic runners were more often dehydrated [8 (28%), −4.7 kg (± 9.8)] than EAH [4 (14%), −1.1 kg (± 3.8)] (P < 0.01), and EAH runners were more frequently overhydrated (6, 67%) than hypernatremia (1, 11%) (P < 0.01).
- In the 98 (56%) runners from hot races, there was EAH OR = 3.5 [95% confidence interval (CI), 0.9-25.9] and hypernatremia OR = 8.8 (95% CI, 2.9-39.5) compared with cold races.
Conclusions:
- This was the first study to show that hot race climates are an independent risk factor for EAH and hypernatremia.
- Sodium supplementation did not prevent EAH nor cause hypernatremia.
- Longer training distances, lower body mass, and avoidance of overhydration were shown to be the most important factors to prevent EAH and avoidance of dehydration to prevent hypernatremia.
Reference:
- Lipman, Grant S. MD*; Burns, Patrick MD*; Phillips, Caleb PhD†; Jensen, Jacob DO‡; Little, Colin MD§; Jurkiewicz, Carrie MD*; Jarrett, Bryan MD¶; Walker, Anne MD*; Mansfield, Nicky MD‡; Krabak, Brian J. MD║. Effect of Sodium Supplements and Climate on Dysnatremia During Ultramarathon Running. Clinical Journal of Sport Medicine 31(6):p e327-e334, November 2021. | DOI: 10.1097/JSM.0000000000000832
Study: Different Predictor Variables for Women and Men in Ultra-Marathon Running—The Wellington Urban Ultramarathon 2018
Ultra-marathon races are increasing in popularity.
- Women are now 20% of all finishers, and this number is growing.
Predictors of performance have been examined rarely for women in ultra-marathon running.
This study aimed to examine the predictors of performance for women and men in the 62 km Wellington Urban Ultramarathon 2018 (WUU2K) and create an equation to predict ultra-marathon race time.
- For women, volume of running during training per week (km) and personal best time (PBT) in 5 km, 10 km, and half-marathon (min) were all associated with race time.
- For men, age, body mass index (BMI), years running, running speed during training (min/km), marathon PBT, and 5 km PBT (min) were all associated with race time.
- For men, ultra-marathon race time might be predicted by the following equation: (r2 = 0.44, adjusted r2 = 0.35, SE = 78.15, degrees of freedom (df) = 18)
- Ultra-marathon race time (min) = −30.85 ± 0.2352 × marathon PBT + 25.37 × 5 km PBT + 17.20 × running speed of training (min/km).
- For women, ultra-marathon race time might be predicted by the following equation: (r2 = 0.83, adjusted r2 = 0.75, SE = 42.53, df = 6)
- Ultra-marathon race time (min) = −148.83 + 3.824 × (half-marathon PBT) + 9.76 × (10 km PBT) − 6.899 × (5 km PBT).
This study should help women in their preparation for performance in ultra-marathon and adds to the bulk of knowledge for ultra-marathon preparation available to men.
Reference:
- O'Loughlin E, Nikolaidis PT, Rosemann T, Knechtle B. Different Predictor Variables for Women and Men in Ultra-Marathon Running-The Wellington Urban Ultramarathon 2018. Int J Environ Res Public Health. 2019 May 24;16(10):1844. doi: 10.3390/ijerph16101844. PMID: 31137635; PMCID: PMC6571892.
- https://www.mdpi.com/1660-4601/16/10/1844
Study: Changes in Pain and Nutritional Intake Modulate Ultra-Running Performance: A Case Report edit
Ultra-endurance running provides numerous physiological, psychological, and nutritional challenges to the athlete and supporting practitioners.
We describe the changes in physiological status, psychological condition, and nutritional intake over the course of two 100-mile running races, with differing outcomes: non-completion and completion.
Athlete perception of pain, freshness, and motivation differed between events, independent of rating of perceived exertion.
Our data suggest that the integration of multiple sensations (freshness, motivation, hunger, pain, and thirst) produce performance.
Increases in carbohydrate feeding (+5 g/h) and protein intake (+0.3 g/kg) also likely contributed to successful completion of a 100-mile race, by
- reducing the fractional utilization of maximal oxygen uptake
- satiating hunger, respectively.
Nutritional data support the notion that the gut is a trainable, and critical organ with respect to ultra-endurance performance.
Finally, we propose future research to investigate the rate at which peak feeding occurs throughout ultra-endurance events, as this may further serve to personalize sports nutrition strategies.
Reference:
- Best R, Barwick B, Best A, Berger N, Harrison C, Wright M, Sparrow J. Changes in Pain and Nutritional Intake Modulate Ultra-Running Performance: A Case Report. Sports (Basel). 2018 Oct 4;6(4):111. doi: 10.3390/sports6040111. PMID: 30287789; PMCID: PMC6316849.
- https://www.mdpi.com/2075-4663/6/4/111
Study: Effects of 120 g/h of Carbohydrates Intake during a Mountain Marathon on Exercise-Induced Muscle Damage in Elite Runners
Background
- Exercise-induced muscle damage (EIMD) and internal exercise load are increased after competing in ultraendurance events such as mountain marathons. Adequate carbohydrate (CHO) intake during exercise optimizes athletic performance and could limit EIMD, reduce internal exercise load and, thus, improve recovery.
- Therefore, the aim of this study was to research into and compare the effects of high CHO intake (120 g/h) in terms of CHO intake recommendation (90 g/h) and regular CHO intake performed by ultraendurance athletes (60 g/h) during a mountain marathon, on exercise load and EIMD markers (creatine kinase (CK), lactate dehydrogenase (LDH), glutamic oxaloacetic transaminase (GOT), urea and creatinine).
Materials and Methods
- A randomized trial was carried out on 20 male elite runners who had previously undertaken nutritional and gut training, and who consumed different CHO dosages according to experimental (EXP—120 g/h), control (CON—90 g/h) and low CHO intake (LOW—60 g/h) groups during a ~4000 m cumulative slope mountain marathon. EIMD markers were analyzed before the race and 24 h afterwards. Internal exercise load was calculated based on rate of perceived exertion (RPE) during and after the marathon event.
Results
- Internal exercise load during the mountain marathon was significantly lower (p = 0.019; η2p = 0.471) in EXP (3805 ± 281 AU) compared to LOW (4688 ± 705 AU) and CON (4692 ± 716 AU).
- Moreover, results revealed that the EXP group evidenced significantly lower CK (p = 0.019; η2p = 0.373), LDH (p < 0.001; η2p = 0.615) and GOT (p = 0.003; η2p = 0.500) values 24 h after the mountain marathon race compared to LOW and CON.
- Along these lines, EIMD and exercise load evidenced a close correlation (R = 0.742; p < 0.001).
Conclusion:
- High CHO intake (120 g/h) during a mountain marathon could limit the EIMD observed by CK, LDH and GOT and internal exercise load compared to CHO ingestion of 60 and 90 g/h.
Reference:
- Viribay A, Arribalzaga S, Mielgo-Ayuso J, Castañeda-Babarro A, Seco-Calvo J, Urdampilleta A. Effects of 120 g/h of Carbohydrates Intake during a Mountain Marathon on Exercise-Induced Muscle Damage in Elite Runners. Nutrients. 2020; 12(5):1367. https://doi.org/10.3390/nu12051367
- https://www.mdpi.com/2072-6643/12/5/1367
Study: Exercise-Associated Hyponatremia, Hypernatremia, and Hydration Status in Multistage Ultramarathons
Objective:
- Dysnatremia and altered hydration status are potentially serious conditions that have not been well studied in multistage ultramarathons. The purpose of this study was to assess the incidence and prevalence of exercise-associated hyponatremia (EAH) (Na+ <135 mmol·L-1) and hypernatremia (Na+ >145 mmol·L-1) and hydration status during a multistage ultramarathon.
Methods:
- This study involved a prospective observational cohort study of runners competing in a 250-km (155-mile) multistage ultramarathon (in the Jordan, Atacama, or Gobi Desert). Prerace body weight and poststage (stage [S] 1 [42 km], S3 [126 km], and S5 [250 km]) body weight and serum sodium concentration levels were obtained from 128 runners.
Results:
- The prevalence of EAH per stage was 1.6% (S1), 4.8% (S3), and 10.1% (S5) with a cumulative incidence of 14.8%. Per-stage prevalence of hypernatremia was 35.2% (S1), 20.2% (S3), and 19.3% (S5) with a cumulative incidence of 52.3%.
- Runners became more dehydrated (weight change <-3%) throughout the race (S1=22.1%; S3=51.2%; S5=53.5%).
- Body weight gain correlated with EAH (r=-0.21, P = .02).
- Nonfinishers of S3 were significantly more likely to have EAH compared with finishers (75% vs 5%, P = .001), but there was no difference in either EAH or hypernatremia between nonfinishers and finishers of S5.
Conclusions:
- The incidence of EAH in multistage ultramarathons was similar to marathons and single-stage ultramarathons, but the cumulative incidence of hypernatremia was 3 times greater than that of EAH. EAH was associated with increased weight gain (overhydration) in early stage nonfinishers and postrace finishers.
Reference:
- Krabak BJ, Lipman GS, Waite BL, Rundell SD. Exercise-Associated Hyponatremia, Hypernatremia, and Hydration Status in Multistage Ultramarathons. Wilderness Environ Med. 2017 Dec;28(4):291-298. doi: 10.1016/j.wem.2017.05.008. Epub 2017 Aug 7. PMID: 28781178.
Study: Fluid Replacement during Marathon Running
During endurance exercise, about 75% of the energy produced from metabolism is in the form of heat, which cannot accumulate. The remaining 25% of energy available can be used for movement. As running pace increases, the rate of heat production increases. Also, the larger one's body mass, the greater the heat production at a particular pace. Sweat evaporation provides the primary cooling mechanism for the body, and for this reason athletes are encouraged to drink fluids to ensure continued fluid availability for evaporation and circulatory flow to the tissues. Elite level runners could be in danger of heat illness if they race too quickly in hot/humid conditions and may collapse at the end of their event. Most marathon races are scheduled at cooler times of the year or day, however, so that heat loss to the environment is adequate.
Typically, this postrace collapse is due simply to postural hypotension from decreased skeletal muscle massage of the venous return circulation to the heart on stopping.
- Elite athletes manage adequate hydration by ingesting about 200–800 mL/hour, and such collapse is rare.
- Athletes “back in the pack” are moving at a much slower pace, however, with heat accumulation unlikely and drinking much easier to manage. They are often urged to drink “as much as tolerable,” ostensibly to prevent dehydration from their hours out on the race course. Excessive drinking among these participants can lead to hyponatremia severe enough to cause fatalities.
A more reasonable approach is to urge these participants not to drink as much as possible but to drink ad libitum (according to the dictates of thirst) no more than 400–800 mL/hour.
Reference:
- Noakes, Tim MBChB, MD, DSc, FACSM. Fluid Replacement during Marathon Running. Clinical Journal of Sport Medicine 13(5):p 309-318, September 2003.
Study: Limits of Ultra: Towards an Interdisciplinary Understanding of Ultra-Endurance Running Performance edit
- Ultra-endurance running (UER) poses extreme mental and physical challenges that present many barriers to completion, let alone performance. Despite these challenges, participation in UER events continues to increase. With the relative paucity of research into UER training and racing compared with traditional endurance running distance (e.g., marathon), it follows that there are sizable improvements still to be made in UER if the limitations of the sport are sufficiently understood.
- The purpose of this review is to summarise our current understanding of the major limitations in UER.
- We begin with an evolutionary perspective that provides the critical background for understanding how our capacities, abilities and limitations have come to be.
- Although we show that humans display evolutionary adaptations that may bestow an advantage for covering large distances on a daily basis, these often far exceed the levels of our ancestors, which exposes relative limitations.
- From that framework, we explore the physiological and psychological systems required for running UER events.
- In each system, the factors that limit performance are highlighted and some guidance for practitioners and future research are shared.
- Examined systems include
- thermoregulation
- oxygen delivery and utilisation
- running economy and biomechanics
- fatigue
- the digestive system
- nutritional
- psychological strategies
- Examined systems include
- We show that minimising the cost of running, damage to lower limb tissue and muscle fatigability may become crucial in UER events.
- Maintaining a sustainable core body temperature is critical to performance, and an even pacing strategy, strategic heat acclimation and individually calculated hydration all contribute to sustained performance.
- Gastrointestinal issues affect almost every UER participant and can be due to a variety of factors.
- We present nutritional strategies for different event lengths and types, such as personalised and evidence-based approaches for varying types of carbohydrate, protein and fat intake in fluid or solid form, and how to avoid flavour fatigue. Psychology plays a vital role in UER performance, and we highlight the need to be able to cope with complex situations, and that specific long and short-term goal setting improves performance.
- Fatigue in UER is multi-factorial, both physical and mental, and the perceived effort or level of fatigue have a major impact on the ability to continue at a given pace.
- Understanding the complex interplay of these limitations will help prepare UER competitors for the different scenarios they are likely to face. Therefore, this review takes an interdisciplinary approach to synthesising and illuminating limitations in UER performance to assist practitioners and scientists in making informed decisions in practice and applicable research.
Reference:
- Berger NJA, Best R, Best AW, Lane AM, Millet GY, Barwood M, Marcora S, Wilson P, Bearden S. Limits of Ultra: Towards an Interdisciplinary Understanding of Ultra-Endurance Running Performance. Sports Med. 2023 Sep 26. doi: 10.1007/s40279-023-01936-8. Epub ahead of print. PMID: 37751076.
- https://link.springer.com/article/10.1007/s40279-023-01936-8
Study: Predictor Variables for A 100-km Race Time in Male Ultra-Marathoners edit
In 169 male 100-km ultra-marathoners, the variables of anthropometry, training, and prerace experience, in order to predict race time, were investigated.
In the bivariate analysis, age (r = .24), body mass (r = .20), Body Mass Index (r = .29), circumference of upper arm (r = .26), percent body fat (r = .45), mean weekly running hours (r = –.21), mean weekly running kilometers (r = –.43), mean speed in training (r = –.56), personal best time in a marathon (r = .65), the number of finished 100-km ultra-runs (r = .24), and the personal best time in a 100-km ultra-run (r = .72) were associated with race time.
Stepwise multiple regression showed that training speed (p < .0001), mean weekly running kilometers (p < .0001), and age (p < .0001) were the best correlations for a 100-km race time.
Performance may be predicted (n = 169, r2 = .43) by the following equation:
- 100-km race time (min) = 1085.60 - 36.26 x (training speed, km/hr.) - 1.43 x (training volume, km/wk.) + 2.50 x (age, yr.)
Overall, intensity of training might be more important for a successful outcome in a 100-km race than anthropometric attributes. Motivation to train intensely for such an ultra-endurance run should be explored as this might be the key for a successful finish.
Reference:
- Knechtle B, Knechtle P, Rosemann T, Lepers R. Predictor variables for a 100-km race time in male ultra-marathoners. Percept Mot Skills. 2010 Dec;111(3):681-93. doi: 10.2466/05.25.PMS.111.6.681-693. PMID: 21319608.
- https://journals.sagepub.com/doi/10.2466/05.25.PMS.111.6.681-693
Study: Sleep and Subjective Recovery in Amateur Trail Runners After the Ultra-Trail du Mont Blanc® (UTMB®)
Purpose
- The interaction between sleep and recovery is a fundamental issue for ultra-marathoners, especially after an ultra-trail, but literatures on this matter remains are scarce.
- The main objectives were
- to describe sleep parameters during the nights following an ultra-endurance event in amateur trail runners
- to evaluate the recovery kinetics
- to assess the relationship between sleep parameters and recovery
Methods
- Nineteen race finishers were tested daily, from 10 days before to 10 days after the Ultra-Trail du Mont-Blanc® (UTMB®).
- Hooper Index (HI) was used to assess recovery and sleep parameters (total sleep time, TST and wake after sleep onset, WASO) were monitored using a wrist-worn actigraph.
Results
- HI was higher than baseline until day 5 after the race (P < 0.05) and younger athletes had a lower HI than older ones during the recovery period (P < 0.001).
- TST was not modified by the race, but there was a WASO peak on the second night after.
- Positive correlations were found between WASO and muscle soreness (P < 0.001) and between TST and HI (P < 0.05).
Conclusions
- In conclusion, participants needed 6 days for recovery after UTMB® and younger runners seemed to recover faster than older ones.
- Post-race sleep quantity did not increase, but the second night was more fragmented, most likely due to muscle soreness.
- Correlations between sleep and recovery parameters highlighted the key role of sleep for recovery.
Reference:
Study: The Training Intensity Distribution of Marathon Runners Across Performance Levels
3 Running Zones:
- Below the threshold of able to talk without breathing hard
- VT1, or the first ventilatory threshold, is the point where lactate begins to accumulate in the blood, and a runner can no longer talk comfortably but can still string together a few words.
- For a runner, VT1 is usually around 70-75% of the Maximum Aerobic Speed (MAS) or Functional Power Threshold (FTP), while VT2 is between 85-90% of MAS or FTP.
- The first lactate threshold, also known as LT1 or the aerobic threshold is used to demarcate zone 1 and 2. LT1 is defined as the lowest intensity at which there is a sustained increase in blood lactate concentration above resting values
- HR Zones 1-2
- Above Z1 but below the threshold of struggling to talk without catching breath
- VT2, or the second ventilatory threshold, is a higher marker of intensity where lactate has quickly accumulated in the blood, and the runner needs to breathe heavily, making it difficult to speak.
- The second lactate threshold, also known as LT2 or maximal lactate steady state (MLSS) is used to demarcate zone 2 and 3. LT2 is defined as the intensity that causes a rapid increase in blood lactate indicating the upper limit of equilibrium between lactate production and clearance.
- HR Zones 3-4
- Above Z2
- HR Zone 5
Abstract:
Background:
- The training characteristics and training intensity distribution (TID) of elite athletes have been extensively studied, but a comprehensive analysis of the TID across runners from different performance levels is lacking.
Methods:
- Training sessions from the 16 weeks preceding 151,813 marathons completed by 119,452 runners were analysed.
- The TID was quantified using a three-zone approach (Z1, Z2 and Z3), where critical speed defined the boundary between Z2 and Z3, and the transition between Z1 and Z2 was assumed to occur at 82.3% of critical speed.
- Training characteristics and TID were reported based on marathon finish time.
Results:
- Training volume across all runners was 45.1 ± 26.4 km·week-1, but the fastest runners within the dataset (marathon time 120-150 min) accumulated > three times more volume than slower runners.
- The amount of training time completed in Z2 and Z3 running remained relatively stable across performance levels, but the proportion of Z1 was higher in progressively faster groups.
- The most common TID approach was pyramidal, adopted by > 80% of runners with the fastest marathon times. There were strong, negative correlations (p < 0.01, R2 ≥ 0.90) between marathon time and markers of training volume, and the proportion of training volume completed in Z1.
- However, the proportions of training completed in Z2 and Z3 were correlated (p < 0.01, R2 ≥ 0.85) with slower marathon times.
Conclusion:
- The fastest runners in this dataset featured large training volumes, achieved primarily by increasing training volume in Z1.
- Marathon runners adopted a pyramidal TID approach, and the prevalence of pyramidal TID increased in the fastest runners.
Reference:
- Muniz-Pumares D, Hunter B, Meyler S, Maunder E, Smyth B. The Training Intensity Distribution of Marathon Runners Across Performance Levels. Sports Med. 2024 Dec 1. doi: 10.1007/s40279-024-02137-7. Epub ahead of print. PMID: 39616560.
Study: Ultra-Marathon Nutrition
Recommendations for Training:
- Ultra-marathon runners should aim to meet the caloric demands of training by following an individualized and periodized strategy, comprising a varied, food-first approach;
- Athletes should plan and implement their nutrition strategy with sufficient time to permit adaptations that enhance fat oxidative capacity;
- The evidence overwhelmingly supports the inclusion of a moderate-to-high carbohydrate diet (i.e., ~ 60% of energy intake, 5–8 g·kg− 1·d− 1) to mitigate the negative effects of chronic, training-induced glycogen depletion;
- Limiting carbohydrate intake before selected low-intensity sessions, and/or moderating daily carbohydrate intake, may enhance mitochondrial function and fat oxidative capacity. Nevertheless, this approach may compromise performance during high-intensity efforts;
- Protein intakes of ~ 1.6 g·kg− 1·d− 1 are necessary to maintain lean mass and support recovery from training, but amounts up to 2.5 g.kg− 1·d− 1 may be warranted during demanding training when calorie requirements are greater
Recommendations for Racing:
- To attenuate caloric deficits, runners should aim to consume 150–400 Kcal/h (carbohydrate, 30–50 g·h− 1; protein, 5–10 g·h− 1) from a variety of calorie-dense foods. Consideration must be given to food palatability, individual tolerance, and the increased preference for savory foods in longer races;
- Fluid volumes of 450–750 mL/h (~ 150–250 mL every 20 min) are recommended during racing. To minimize the likelihood of hyponatraemia, electrolytes (mainly sodium) may be needed in concentrations greater than that provided by most commercial products (i.e., > 575 mg·L− 1 sodium). Fluid and electrolyte requirements will be elevated when running in hot and/or humid conditions;
- Evidence supports progressive gut-training and/or low-FODMAP diets (fermentable oligosaccharide, disaccharide, monosaccharide and polyol) to alleviate symptoms of gastrointestinal distress during racing;
- The evidence in support of ketogenic diets and/or ketone esters to improve ultra-marathon performance is lacking, with further research warranted;
- Evidence supports the strategic use of caffeine to sustain performance in the latter stages of racing, particularly when sleep deprivation may compromise athlete safety.
The values presented are based on data from empirical studies [28, 29], and corroborated by independent reports suggesting that the energy cost of running ranges from 200 to 300 kJ·km− 1 (47–71 Kcal·km− 1) [30, 31]. As an example, a 50 kg female with 15% bodyfat, engaging in continuous running for 1 h·d− 1 (at a pace of 11.5 min·mile− 1; 8.4 km·h− 1) will require an estimated total of ~ 2004 Kcal·d− 1 in order to maintain caloric balance. The same athlete undertaking 3 h training sessions at the same pace would require ~ 2726 Kcal·d− 1, whereas a 3 h session performed at a pace of 7 min·mile− 1 (13.8 km·h− 1) would necessitate a considerably higher energy intake (i.e., ~ 3423 Kcal·d− 1)
| PACE | FEMALE | FEMALE | FEMALE | FEMALE | MALE | MALE | MALE | MALE |
|---|---|---|---|---|---|---|---|---|
| 50 kg (15% BF) | 50 kg (15% BF) | 70 kg (24% BF) | 70 kg (24% BF) | 65 kg (10% BF) | 65 kg (10% BF) | 85 kg (20% BF) | 85 kg (20% BF) | |
| 1 h | 3 h | 1 h | 3 h | 1 h | 3 h | 1 h | 3 h | |
| 11.5 min/mile1 (8.4 km/h) | 2004 | 2726 | 2443 | 3455 | 2553 | 3492 | 2959 | 4187 |
| 9 min/mile (10.7 km/h) | 2103 | 3023 | 2581 | 3870 | 2681 | 3878 | 3127 | 4692 |
| 7 min/mile (13.8 km/h) | 2236 | 3423 | 2768 | 4430 | 2855 | 4398 | 3354 | 5372 |
Over the half-marathon distance (13.1 miles), mean sweat losses of ~1.4 L were observed in male runners and, when offset against fluid ingestion during exercise, resulted in net fluid losses of ~ 0.3 L [77]. Over longer training distances (marathon), high-level runners exhibited a body weight loss of 0.3 and 1.7%, in cool and warm conditions, respectively, even when consuming fluid at a rate of 1 L/h [78]. Furthermore, abstaining from fluid resulted in an average dehydration of 3.3 and 5.3%, respectively [78]
In order to reduce the risk of hyponatremia during long-duration exercise, runners should consume sodium in concentrations of 500–700 mg/L of fluid [118]. Slightly greater amounts of sodium (and other electrolytes) will be required in hot (e.g., > 25 °C / 77 °F) and/or humid (e.g., > 60%) conditions when sweat rates are elevated; in such conditions, runners should target ~ 300–600 mg/h of sodium (1000–2000 mg of NaCl)
Reference:
- Tiller NB, Roberts JD, Beasley L, Chapman S, Pinto JM, Smith L, Wiffin M, Russell M, Sparks SA, Duckworth L, O'Hara J, Sutton L, Antonio J, Willoughby DS, Tarpey MD, Smith-Ryan AE, Ormsbee MJ, Astorino TA, Kreider RB, McGinnis GR, Stout JR, Smith JW, Arent SM, Campbell BI, Bannock L. International Society of Sports Nutrition Position Stand: nutritional considerations for single-stage ultra-marathon training and racing. J Int Soc Sports Nutr. 2019 Nov 7;16(1):50. doi: 10.1186/s12970-019-0312-9. PMID: 31699159; PMCID: PMC6839090.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6839090/
Study: Widespread drastic reduction of brain myelin content upon prolonged endurance exercise edit
Recent evidence suggests that myelin lipids may act as glial energy reserves when glucose is lacking, a hypothesis yet to be solidly proven. Hereby, we examined the effects of running a marathon on the myelin content by MRI. Our findings show that marathon runners undergo widespread robust myelin decrease at completion of the effort. This reduction involves white and25 gray matter, and includes primary motor and sensory cortical areas and pathways, as well as the entire corpus callosum and internal capsule. Notably, myelin levels partially recover within two weeks after the marathon. These results reveal that myelin use and replenishment is an unprecedented form of metabolic plasticity aimed to maintain brain function during extreme conditions.
Our findings in marathon runners strongly suggest that widespread dramatic myelin loss, likely thinning, in exhausting conditions represents a new form of plasticity whereby20 brain function is preserved at the expense of myelin to optimize signal speed propagation.
Concluding paragraph Collectively, the findings reported here imply that the bulk of myelin is consumed upon strenuous conditions and steadily recovered later on, pointing to a novel concept of metabolic myelin25 plasticity. It remains to be clarified whether myelin constituents, mainly lipids, are used for fueling brain function in common life tasks including memory acquisition and retrieval, thought, sensory- motor processing, and hunger regulation, to name a few. The mechanisms driving metabolic myelin plasticity might be piloted by neural activity, and may also be modulated by neurotransmitter release at the axon-myelin unit during action potential propagation along with30 synaptic activity
Reference:
- Pedro Ramos-Cabrer, Alberto Cabrera-Zubizarreta, Daniel Padró, Mario Matute-González, Alfredo Rodríguez-Antigüedad, Carlos Matute. Widespread drastic reduction of brain myelin content upon prolonged endurance exercise. bioRxiv 2023.10.10.561303; doi: https://doi.org/10.1101/2023.10.10.561303
- https://www.biorxiv.org/content/10.1101/2023.10.10.561303v1.full.pdf
Study: Resistance Training Volume Enhances Muscle Hypertrophy but Not Strength in Trained Men
Purpose:
- The purpose of this study was to evaluate muscular adaptations between low-, moderate-, and high-volume resistance training protocols in resistance-trained men.
Methods:
- Thirty-four healthy resistance-trained men were randomly assigned to one of three experimental groups: a low-volume group performing one set per exercise per training session (n = 11), a moderate-volume group performing three sets per exercise per training session (n = 12), or a high-volume group performing five sets per exercise per training session (n = 11).
- Training for all routines consisted of three weekly sessions performed on nonconsecutive days for 8 wk.
- Muscular strength was evaluated with one repetition maximum (RM) testing for the squat and bench press. Upper-body muscle endurance was evaluated using 50% of subjects bench press 1RM performed to momentary failure.
- Muscle hypertrophy was evaluated using B-mode ultrasonography for the elbow flexors, elbow extensors, mid-thigh, and lateral thigh.
Results:
- Results showed significant preintervention to postintervention increases in strength and endurance in all groups, with no significant between-group differences. Alternatively, while all groups increased muscle size in most of the measured sites from preintervention to postintervention, significant increases favoring the higher-volume conditions were seen for the elbow flexors, mid-thigh, and lateral thigh.
Conclusions:
- Marked increases in strength and endurance can be attained by resistance-trained individuals with just three 13-min weekly sessions over an 8-wk period, and these gains are similar to that achieved with a substantially greater time commitment.
- Alternatively, muscle hypertrophy follows a dose-response relationship, with increasingly greater gains achieved with higher training volumes.
Reference:
- Schoenfeld BJ, Contreras B, Krieger J, Grgic J, Delcastillo K, Belliard R, Alto A. Resistance Training Volume Enhances Muscle Hypertrophy but Not Strength in Trained Men. Med Sci Sports Exerc. 2019 Jan;51(1):94-103. doi: 10.1249/MSS.0000000000001764. PMID: 30153194; PMCID: PMC6303131.
- https://pubmed.ncbi.nlm.nih.gov/30153194/
Study: Screen-based entertainment time, all-cause mortality, and cardiovascular events: population-based study with ongoing mortality and hospital events follow-up
Objectives:
- The aim of this study was to examine the independent relationships of television viewing or other screen-based entertainment ("screen time") with all-cause mortality and clinically confirmed cardiovascular disease (CVD) events.
- A secondary objective was to examine the extent to which metabolic (body mass index, high-density lipoprotein and total cholesterol) and inflammatory (C-reactive protein) markers mediate the relationship between screen time and CVD events.
Background:
- Although some evidence suggests that prolonged sitting is linked to CVD risk factor development regardless of physical activity participation, studies with hard outcomes are scarce.
Methods:
- A population sample of 4,512 (1,945 men) Scottish Health Survey 2003 respondents (≥35 years) were followed up to 2007 for all-cause mortality and CVD events (fatal and nonfatal combined). Main exposures were interviewer-assessed screen time (<2 h/day; 2 to <4 h/day; and ≥4 h/day) and moderate to vigorous intensity physical activity.
Results:
- Two hundred fifteen CVD events and 325 any-cause deaths occurred during 19,364 follow-up person-years.
- The covariable (age, sex, ethnicity, obesity, smoking, social class, long-standing illness, marital status, diabetes, hypertension)-adjusted hazard ratio (HR) for all-cause mortality was 1.52 (95% confidence interval [CI]: 1.06 to 2.16) and for CVD events was 2.30 (95% CI: 1.33 to 3.96) for participants engaging in ≥4 h/day of screen time relative to <2 h/day.
- Adjusting for physical activity attenuated these associations only slightly (all-cause mortality: HR: 1.48, 95% CI: 1.04 to 2.13; CVD events: HR: 2.25, 95% CI: 1.30 to 3.89).
- Exclusion of participants with CVD events in the first 2 years of follow-up and previous cancer registrations did not change these results appreciably.
- Approximately 25% of the association between screen time and CVD events was explained collectively by C-reactive protein, body mass index, and high-density lipoprotein cholesterol.
Conclusions:
- Recreational sitting, as reflected by television/screen viewing time, is related to raised mortality and CVD risk regardless of physical activity participation.
- Inflammatory and metabolic risk factors partly explain this relationship.
Reference:
- Stamatakis E, Hamer M, Dunstan DW. Screen-based entertainment time, all-cause mortality, and cardiovascular events: population-based study with ongoing mortality and hospital events follow-up. J Am Coll Cardiol. 2011 Jan 18;57(3):292-9. doi: 10.1016/j.jacc.2010.05.065. Erratum in: J Am Coll Cardiol. 2011 Apr 19;57(16):1717. PMID: 21232666.
Study: Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis
Background:
- The magnitude, consistency, and manner of association between sedentary time and outcomes independent of physical activity remain unclear.
Purpose:
- To quantify the association between sedentary time and hospitalizations, all-cause mortality, cardiovascular disease, diabetes, and cancer in adults independent of physical activity.
Data sources:
- English-language studies in MEDLINE, PubMed, EMBASE, CINAHL, Cochrane Library, Web of Knowledge, and Google Scholar databases were searched through August 2014 with hand-searching of in-text citations and no publication date limitations.
Study selection:
- Studies assessing sedentary behavior in adults, adjusted for physical activity and correlated to at least 1 outcome.
Data extraction:
- Two independent reviewers performed data abstraction and quality assessment, and a third reviewer resolved inconsistencies.
Data synthesis:
- Forty-seven articles met our eligibility criteria. Meta-analyses were performed on outcomes for cardiovascular disease and diabetes (14 studies), cancer (14 studies), and all-cause mortality (13 studies).
- Prospective cohort designs were used in all but 3 studies; sedentary times were quantified using self-report in all but 1 study.
- Significant hazard ratio (HR) associations were found with
- All-cause mortality (HR, 1.240 [95% CI, 1.090 to 1.410])
- Cardiovascular disease mortality (HR, 1.179 [CI, 1.106 to 1.257])
- Cardiovascular disease incidence (HR, 1.143 [CI, 1.002 to 1.729])
- Cancer mortality (HR, 1.173 [CI, 1.108 to 1.242])
- Cancer incidence (HR, 1.130 [CI, 1.053 to 1.213])
- Type 2 diabetes incidence (HR, 1.910 [CI, 1.642 to 2.222])
- Hazard ratios associated with sedentary time and outcomes were generally more pronounced at lower levels of physical activity than at higher levels.
Limitation:
- There was marked heterogeneity in research designs and the assessment of sedentary time and physical activity.
Conclusion:
- Prolonged sedentary time was independently associated with deleterious health outcomes regardless of physical activity.
Reference:
- Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, Alter DA. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015 Jan 20;162(2):123-32. doi: 10.7326/M14-1651. Erratum in: Ann Intern Med. 2015 Sep 1;163(5):400. doi: 10.7326/L15-5134. PMID: 25599350.
Study: Spending at least 120 minutes a week in nature is associated with good health and wellbeing
Spending time in natural environments can benefit health and well-being, but exposure-response relationships are under-researched.
We examined associations between recreational nature contact in the last seven days and self-reported health and well-being.
Methods:
- Participants (n = 19,806) were drawn from the Monitor of Engagement with the Natural Environment Survey (2014/15–2015/16); weighted to be nationally representative.
- Weekly contact was categorised using 60 min blocks.
- Analyses controlled for residential greenspace and other neighbourhood and individual factors.
Results:
- Compared to no nature contact last week, the likelihood of reporting good health or high well-being became significantly greater with contact ≥120 mins (e.g. 120–179 mins: ORs [95%CIs]:
- Health = 1.59 [1.31–1.92];
- Well-being = 1.23 [1.08–1.40]).
- Positive associations peaked between 200–300 mins per week with no further gain.
- The pattern was consistent across key groups including older adults and those with long-term health issues.
- It did not matter how 120 mins of contact a week was achieved (e.g. one long vs. several shorter visits/week).
Prospective longitudinal and intervention studies are a critical next step in developing possible weekly nature exposure guidelines comparable to those for physical activity.
Reference:
- White, M.P., Alcock, I., Grellier, J. et al. Spending at least 120 minutes a week in nature is associated with good health and wellbeing. Sci Rep 9, 7730 (2019). https://doi.org/10.1038/s41598-019-44097-3
- https://www.nature.com/articles/s41598-019-44097-3
Study: Stair walking is more energizing than low dose caffeine in sleep deprived young women
Highlights
- Chronically sleep deprived adults use low doses of caffeine to improve alertness.
- Energizing effect of brief stair walking was compared to 50 mg caffeine.
- Energizing effect of stairs was > 50 mg caffeine in sleep deprived women.
Introduction
- The acute energizing effect of exercise and caffeine has never been examined in a single study of adults with chronic sleep deprivation but evidence from a study of this type could help individuals choose between these two common alertness-enhancing options.
Aim
- The apriori primary aim of this experiment was to compare the influence of 10-min of low-to-moderate intensity stair walking to the consumption of capsules containing 50 mg caffeine or flour (placebo) on feelings of energy in physically active, college female caffeine users with chronic insufficient sleep. Effects on secondary outcomes related to feelings of energy also were assessed.
Material-method
- A repeated measures crossover experiment was conducted with 18 college women (18–23 years) who reported (i) daily caffeine consumption that was not extreme (40–400 mg), (ii) typical leisure time physical activity that was not extreme (at least 2 weekly mild 15-min or longer bouts and no > 5 strenuous 15-min or longer bouts), and (iii) sleeping < 45 h per week. Mood states (POMS-BF), focused on energy feelings (vigor), as well as working memory (N-back), sustained attention (CPT), simple reaction time (SRT), and motivation to complete the cognitive tasks were measured before and after a 10-min exercise condition (20 min seated rest followed by 10 min of low-to-moderate intensity stair walking) and compared to both a caffeine condition (50 mg caffeine capsule followed by 30 min of seated rest) and a similar flour (placebo) capsule condition. Condition (exercise, caffeine, placebo) × Time (Baseline, Post-1, Post-2, and for mood Post-3) ANCOVAs (controlling for Condition order) tested the hypothesized effects.
Results
- Condition × Time interactions showed that stair walking increased POMS-BF vigor at Post-1 compared to both placebo and caffeine. Other interactions were not significant.
Conclusion
- A brief bout of low-to-moderate intensity stair walking has transient energizing effects that exceed a low dose of caffeine for active young women with chronic insufficient sleep.
Reference:
- Randolph DD, O'Connor PJ. Stair walking is more energizing than low dose caffeine in sleep deprived young women. Physiol Behav. 2017 May 15;174:128-135. doi: 10.1016/j.physbeh.2017.03.013. Epub 2017 Mar 14. PMID: 28302573.
Study: Structured Exercise after Adjuvant Chemotherapy for Colon Cancer
Background
- Preclinical and observational studies suggest that exercise may improve cancer outcomes. However, definitive level 1 evidence is lacking.
Methods
- In this phase 3, randomized trial conducted at 55 centers, we assigned patients with resected colon cancer who had completed adjuvant chemotherapy to participate in a structured exercise program (exercise group) or to receive health-education materials alone (health-education group) over a 3-year period. The primary end point was disease-free survival.
Research Summary
- Structured Exercise after Adjuvant Chemotherapy for Colon Cancer
Results
- From 2009 through 2024, a total of 889 patients underwent randomization to the exercise group (445 patients) or the health-education group (444 patients).
- At a median follow-up of 7.9 years, disease-free survival was significantly longer in the exercise group than in the health-education group (hazard ratio for disease recurrence, new primary cancer, or death, 0.72; 95% confidence interval [CI], 0.55 to 0.94; P=0.02).
- The 5-year disease-free survival was 80.3% in the exercise group and 73.9% in the health-education group (difference, 6.4 percentage points; 95% CI, 0.6 to 12.2).
- Results support longer overall survival in the exercise group than in the health-education group (hazard ratio for death, 0.63; 95% CI, 0.43 to 0.94).
- The 8-year overall survival was 90.3% in the exercise group and 83.2% in the health-education group (difference, 7.1 percentage points; 95% CI, 1.8 to 12.3).
- Musculoskeletal adverse events occurred more often in the exercise group than in the health-education group (in 18.5% vs. 11.5% of patients).
Conclusions
- A 3-year structured exercise program initiated soon after adjuvant chemotherapy for colon cancer resulted in significantly longer disease-free survival and findings consistent with longer overall survival. (Funded by the Canadian Cancer Society and others; CHALLENGE ClinicalTrials.gov number, NCT00819208.)
Reference:
- Courneya KS, Vardy JL, O'Callaghan CJ, Gill S, Friedenreich CM, Wong RKS, Dhillon HM, Coyle V, Chua NS, Jonker DJ, Beale PJ, Haider K, Tang PA, Bonaventura T, Wong R, Lim HJ, Burge ME, Hubay S, Sanatani M, Campbell KL, Arthuso FZ, Turner J, Meyer RM, Brundage M, O'Brien P, Tu D, Booth CM; CHALLENGE Investigators. Structured Exercise after Adjuvant Chemotherapy for Colon Cancer. N Engl J Med. 2025 Jul 3;393(1):13-25. doi: 10.1056/NEJMoa2502760. Epub 2025 Jun 1. PMID: 40450658.
Study: The Acute Effects of Interrupting Prolonged Sitting Time in Adults with Standing and Light-Intensity Walking on Biomarkers of Cardiometabolic Health in Adults: A Systematic Review and Meta-analysis
Background
- Increasing evidence highlights that accumulating sitting time in prolonged bouts is detrimental to cardiometabolic health.
Objectives
- This systematic review aimed to compare the effects of fractionating prolonged sitting with frequent short bouts of standing and light-intensity walking on cardiometabolic health markers and conduct a meta-analysis for differences in systolic blood pressure (SBP), postprandial glucose and insulin.
Methods
- Experimental randomised crossover trials with at least three intervention arms that assessed interrupting sitting with frequent short bouts of standing and light-intensity walking over a single day compared to a prolonged sitting condition were retrieved. These studies measured at minimum one marker of cardiometabolic health in adults > 18 years. An electronic search was completed on the 2nd of August 2021, searching PubMed and Web of Science Core Collection, Scopus, Embase, Cochrane Library and APA PsycINFO. Risk of bias was assessed using a modified Downs and Black checklist. A meta-analysis was conducted using calculated Cohen’s d quantifying the magnitude of difference between experimental conditions.
Results
- Seven studies met the inclusion criteria for the systematic review. All seven studies were included within the meta-analysis for postprandial glucose, four studies were pooled for postprandial insulin and three for SBP. Biomarkers of cardiometabolic health were discussed qualitatively if fewer than three studies measured and reported the variable.
- A meta-analysis of seven acute, 1-day randomised crossover trials that sampled mixed-sex adults (aged > 18 years) who were predominately overweight or participants with obesity found that standing as an interruption to prolonged sitting significantly reduced postprandial glucose (∆ = − 0.31, 95% CI − 0.60, − 0.03; z = − 2.15, p < 0.04) but had no significant effect on insulin or SBP.
- Light-intensity walking was shown to significantly attenuate postprandial glucose (∆ = − 0.72, 95% CI − 1.03, − 0.41; z = − 4.57, p < 0.001) and insulin (∆ = − 0.83, 95% CI − 1.18, − 0.48; z = − 4.66, p < 0.001) compared to continued sitting.
- When comparing light-intensity walking breaks compared to standing breaks a significant reduction in glucose (∆ = − 0.30, 95% CI − 0.52, − 0.08; z = -2.64, p < 0.009) and insulin (∆ = − 0.54, 95% CI − 0.75, − 0.33; z = -4.98, p < 0.001) was observed. Both standing and light-intensity walking showed no effect on SBP.
Conclusions
- Frequent short interruptions of standing significantly attenuated postprandial glucose compared to prolonged sitting; however, light-intensity walking was found to represent a superior physical activity break. The feasibility and longitudinal implications of breaking sedentary behaviour with light-intensity walking should be investigated in a free-living setting.
Reference:
- Buffey AJ, Herring MP, Langley CK, Donnelly AE, Carson BP. The Acute Effects of Interrupting Prolonged Sitting Time in Adults with Standing and Light-Intensity Walking on Biomarkers of Cardiometabolic Health in Adults: A Systematic Review and Meta-analysis. Sports Med. 2022 Aug;52(8):1765-1787. doi: 10.1007/s40279-022-01649-4. Epub 2022 Feb 11. PMID: 35147898; PMCID: PMC9325803.
Study: The associations of "weekend warrior" and regularly active physical activity with abdominal and general adiposity in US adults
Objective
- This study examined the association between physical activity patterns and abdominal and general adiposity.
Methods
- Data were extracted among 20- to 59-year-old participants in the National Health and Nutrition Examination Survey (NHANES) from 2011 to 2018. Abdominal and general adiposity was assessed by dual-energy x-ray absorptiometry (DXA) and anthropometric measures. DXA-measured indicators were further normalized into z scores. Physical activity levels were collected by questionnaire and classified as inactive, "weekend warrior" (WW), and regularly active (RA). Survey linear regression models were used to assess associations between physical activity patterns and adiposity indicators.
Results
- Among 9629 participants, 772 (8.2%) reported the WW pattern and 3277 (36.9%) reported the RA pattern.
- Compared with inactive, both WW and RA had:
- lower DXA-measured abdominal adiposity (WW: β: −0.24, 95% CI: −0.38 to −0.10; RA: −0.18, 95% CI: −0.29 to −0.07)
- waist circumference (WW: β: −1.94, 95% CI: −3.16 to −0.73; RA: −1.31, 95% CI: −2.32 to −0.29)
- whole-body fat mass (WW: β: −0.16, 95% CI: −0.25 to −0.08; RA: −0.11, 95% CI: −0.18 to −0.04)
- BMI (WW: β: −0.78, 95% CI: −1.27 to −0.28; RA: −0.47, 95% CI: −0.89 to −0.04)
Conclusions
- The WW pattern was associated with similarly lower abdominal and general adiposity to the RA pattern versus the inactive pattern.
Reference:
- Lei L, Li J, Wang W, Yu Y, Pu B, Peng Y, Zhang L, Zhao Z. The associations of "weekend warrior" and regularly active physical activity with abdominal and general adiposity in US adults. Obesity (Silver Spring). 2024 Feb 20. doi: 10.1002/oby.23986. Epub ahead of print. PMID: 38374722.
- https://onlinelibrary.wiley.com/doi/10.1002/oby.23986?af=R
Study: The training—injury prevention paradox: should athletes be training smarter and harder?
Background
- There is dogma that higher training load causes higher injury rates. However, there is also evidence that training has a protective effect against injury.
- For example, team sport athletes who performed more than 18 weeks of training before sustaining their initial injuries were at reduced risk of sustaining a subsequent injury, while high chronic workloads have been shown to decrease the risk of injury.
- Second, across a wide range of sports, well-developed physical qualities are associated with a reduced risk of injury. Clearly, for athletes to develop the physical capacities required to provide a protective effect against injury, they must be prepared to train hard.
- Finally, there is also evidence that under-training may increase injury risk.
- Collectively, these results emphasise that reductions in workloads may not always be the best approach to protect against injury.
Main thesis
- This paper describes the ‘Training-Injury Prevention Paradox’ model; a phenomenon whereby athletes accustomed to high training loads have fewer injuries than athletes training at lower workloads. The Model is based on evidence that non-contact injuries are not caused by training per se, but more likely by an inappropriate training programme.
- Excessive and rapid increases in training loads are likely responsible for a large proportion of non-contact, soft-tissue injuries. If training load is an important determinant of injury, it must be accurately measured up to twice daily and over periods of weeks and months (a season). This paper outlines ways of monitoring training load (‘internal’ and ‘external’ loads) and suggests capturing both recent (‘acute’) training loads and more medium-term (‘chronic’) training loads to best capture the player's training burden. I describe the critical variable — acute:chronic workload ratio — as a best practice predictor of training-related injuries. This provides the foundation for interventions to reduce players risk, and thus, time-loss injuries.
Summary
- The appropriately graded prescription of high training loads should improve players’ fitness, which in turn may protect against injury, ultimately leading to (1) greater physical outputs and resilience in competition, and (2) a greater proportion of the squad available for selection each week.
Reference:
- Gabbett TJ The training—injury prevention paradox: should athletes be training smarter and harder? British Journal of Sports Medicine 2016;50:273-280.
Study: Timing of Moderate to Vigorous Physical Activity, Mortality, Cardiovascular Disease, and Microvascular Disease in Adults With Obesity
Objective
- To assess the association between timing of aerobic moderate to vigorous physical activity (MVPA) and risk of cardiovascular disease (CVD), microvascular disease (MVD), and all-cause mortality in adults with obesity and a subset with obesity and type 2 diabetes (T2D).
Research Design And Methods
- Participants included adults with obesity (BMI ≥30 kg/m2) and a subset of those with T2D from the UK Biobank accelerometry substudy. Aerobic MVPA was defined as bouts of MVPA lasting ≥3 continuous minutes. Participants were categorized into morning, afternoon, or evening MVPA based on when they undertook the majority of their aerobic MVPA. The reference group included participants with an average of less than one aerobic MVPA bout per day. Analyses were adjusted for established and potential confounders.
Results
- The core sample included 29,836 adults with obesity, with a mean age of 62.2 (SD 7.7) years. Over a mean follow-up period of 7.9 (SD 0.8) years, 1,425 deaths, 3,980 CVD events, and 2,162 MVD events occurred.
- Compared with activity in the reference group, evening MVPA was associated with the lowest risk of mortality (hazard ratio [HR] 0.39; 95% CI 0.27, 0.55), whereas afternoon (HR 0.60; 95% CI 0.51, 0.71) and morning MVPA (HR 0.67; 95% CI 0.56, 0.79) demonstrated significant but weaker associations.
- Similar patterns were observed for CVD and MVD incidence, with evening MVPA associated with the lowest risk of CVD (HR 0.64; 95% CI 0.54, 0.75) and MVD (HR 0.76; 95% CI 0.63, 0.92).
- Findings were similar in the T2D subset (n = 2,995).
Conclusions
- Aerobic MVPA bouts undertaken in the evening were associated with the lowest risk of mortality, CVD, and MVD.
- Timing of physical activity may play a role in the future of obesity and T2D management.
Reference:
- Sabag A, Ahmadi MN, Francois ME, Postnova S, Cistulli PA, Fontana L, Stamatakis E. Timing of Moderate to Vigorous Physical Activity, Mortality, Cardiovascular Disease, and Microvascular Disease in Adults With Obesity. Diabetes Care. 2024 May 1;47(5):890-897. doi: 10.2337/dc23-2448. PMID: 38592034; PMCID: PMC11043226.
- https://diabetesjournals.org/care/article/47/5/890/154403/Timing-of-Moderate-to-Vigorous-Physical-Activity
Study: Vigorous Intermittent Lifestyle Physical Activity and Cancer Incidence Among Nonexercising Adults
Key Points
- Question
- Does vigorous intermittent lifestyle physical activity (VILPA) in short bouts (≤1 and ≤2 minutes) have a dose-response association with incident cancer among nonexercising adults?
- Findings
- In this prospective cohort study of 22,398 self-reported nonexercising adults, a minimum dose of 3.4 to 3.6 minutes of VILPA per day was associated with a 17% to 18% reduction in total incident cancer risk compared with no VILPA.
- A median daily VILPA of 4.5 minutes was associated with a 31% to 32% reduction in physical activity–related cancer incidence.
- Meaning
- The findings of this large cohort study suggest that 3 to 4 minutes of VILPA per day may be associated with decreased cancer incidence risk; thus, VILPA may be a promising intervention for cancer prevention among individuals unable or unmotivated to exercise in leisure time.
Abstract
- Importance
- Vigorous physical activity (VPA) is a time-efficient way to achieve recommended physical activity (PA) for cancer prevention, although structured longer bouts of VPA (via traditional exercise) are unappealing or inaccessible to many individuals.
- Objectives
- To evaluate the dose-response association of device-measured daily vigorous intermittent lifestyle physical activity (VILPA) with incident cancer, and to estimate the minimal dose required for a risk reduction of 50% of the maximum reduction.
- Design, Setting, and Participants
- This was a prospective cohort analysis of 22,398 self-reported nonexercising adults from the UK Biobank accelerometry subsample. Participants were followed up through October 30, 2021 (mortality and hospitalizations), or June 30, 2021 (cancer registrations).
- Exposures
- Daily VILPA of up to 1 and up to 2 minutes, assessed by accelerometers worn on participants' dominant wrist.
- Main Outcomes and Measures
- Incidence of total cancer and PA-related cancer (a composite outcome of 13 cancer sites associated with low PA levels). Hazard ratios and 95% CIs were estimated using cubic splines adjusted for age, sex, education level, smoking status, alcohol consumption, sleep duration, fruit and vegetable consumption, parental cancer history, light- and moderate-intensity PA, and VPA from bouts of more than 1 or 2 minute(s), as appropriate.
- Results
- The study sample comprised 22,398 participants (mean [SD] age, 62.0 [7.6] years; 10,122 [45.2%] men and 12,276 [54.8%] women; 21,509 [96.0%] White individuals).
- During a mean (SD) follow-up of 6.7 (1.2) years (149,650 person-years), 2356 total incident cancer events occurred, 1084 owing to PA-related cancer. Almost all (92.3%) of VILPA was accrued in bouts of up to 1 minute.
- Daily VILPA duration was associated with outcomes in a near-linear manner, with steeper dose-response curves for PA-related cancer than total cancer incidence.
- Compared with no VILPA, the median daily VILPA duration of bouts up to 1 minute (4.5 minutes per day) was associated with an HR of 0.80 (95% CI, 0.69-0.92) for total cancer and 0.69 (95% CI, 0.55-0.86) for PA-related cancer.
- The minimal dose was 3.4 minutes per day for total (HR, 0.83; 95% CI, 0.73-0.93) and 3.7 minutes for PA-related (HR, 0.72; 95% CI, 0.59-0.88) cancer incidence. Findings were similar for VILPA bout of up to 2 minutes.
- Conclusions and Relevance
- The findings of this prospective cohort study indicate that small amounts of VILPA were associated with lower incident cancer risk.
- Daily VILPA may be a promising intervention for cancer prevention in populations not able or motivated to exercise in leisure time.
Reference:
- Stamatakis E, Ahmadi MN, Friedenreich CM, Blodgett JM, Koster A, Holtermann A, Atkin A, Rangul V, Sherar LB, Teixeira-Pinto A, Ekelund U, Lee IM, Hamer M. Vigorous Intermittent Lifestyle Physical Activity and Cancer Incidence Among Nonexercising Adults: The UK Biobank Accelerometry Study. JAMA Oncol. 2023 Jul 27:e231830. doi: 10.1001/jamaoncol.2023.1830. Epub ahead of print. PMID: 37498576; PMCID: PMC10375384.
- https://jamanetwork.com/journals/jamaoncology/fullarticle/2807734
Study: Walking as an intervention to reduce blood pressure in adults with hypertension: recommendations and implications for clinical practise
Hypertension affects more than 1 in 4 adults, equating to around 1.39 billion people worldwide. Hypertension is defined as an elevation in systolic blood pressure above 140mmHg. This can increase cardiovascular and stroke risk.
By lowering blood pressure, individuals can mitigate an increased risk of stroke and end-organ damage.
While medications have proven beneficial to lowering blood pressure, they do have the potential for side effects. Other non-pharmacological lifestyle and dietary changes exist. This article critically appraises a systematic review which assesses whether walking can reduce blood pressure.
In terms of clinical practise, the findings from this review identified that walking interventions of 20-40 mins, 3-5 times per week for around 15 weeks (in any environment; outdoors or indoors), significantly reduced blood pressure and heart rate (in adults 16 years and over).
The evidence suggests that under 40’s had the greatest effect of reduced blood pressure, but the results were relevant for all ages.
Furthermore, females appeared to have a greater reduction in blood pressure compared to males.
Reference:
- Mansoor M, Hamer O, Sandrasekar K, Argent C, Hill J. Walking as an intervention to reduce blood pressure in adults with hypertension: recommendations and implications for clinical practise. Br J Card Nurs. 2023 Mar 2;18(3):2022.0119. doi: 10.12968/bjca.2022.0119. Epub 2023 Mar 20. PMID: 38807750; PMCID: PMC7616014.
Study: Walk to a Better Night of Sleep: Testing the Relationship Between Physical Activity and Sleep
Objectives:
- Many do not sleep well, particularly middle-aged and older adults. Physical activity (PA) shows promise for improving sleep, however, populations with clinical sleep disturbances have been a research focus. It remains unclear whether low-impact daily PA, like walking, can affect sleep in healthy adults.
Design:
- The current study was embedded within a 4-week randomized controlled trial to increase PA.
Setting:
- Participants from the greater Boston area were recruited to participate in a 4-week walking intervention on a rolling basis, between October 2015 and August 2016.
Participants:
- 59 participants (72% female) were enrolled in the study, with an average age of 49.43(±8.40).
Intervention:
- The 4-week intervention was aimed at increasing participants’ daily steps as the primary outcome. The current, supplementary study examined relationships between monthly and daily PA and sleep.
Measurements:
- Steps and active minutes were measured daily using a Fitbit Zip. Self-reports of sleep quality and duration were assessed daily, along with before and after the intervention.
Results and Conclusions:
- Averaged across the month, daily active minutes were positively related to sleep quality, but not duration. Gender moderated this relationship; women who took more steps and were more active reported sleeping better than those less active. Within-persons, on days that participants were more active than average, they reported better sleep quality and duration in both genders.
- Results suggest that low-impact PA is positively related to sleep, more so in women than men. Findings also showed that PA plays a greater role in predicting sleep quality than duration.
Reference:
- Sullivan Bisson AN, Robinson SA, Lachman ME. Walk to a better night of sleep: testing the relationship between physical activity and sleep. Sleep Health. 2019 Oct;5(5):487-494. doi: 10.1016/j.sleh.2019.06.003. Epub 2019 Jul 26. PMID: 31358470; PMCID: PMC6801055.
Walking and energy use edit
The truth is that race walkers, when they complete 50km, don't do 20% more work than a marathon runner. Instead, walking 50km as fast as possible takes nearly double the work and energy than running a marathon, even though the distance is just 8km longer.
The key isn't the rate at which athletes consume energy. Surely, marathoners burn more fuel per unit time – that's why they finish much faster. But, at the same time, marathoners burn less fuel per unit distance traveled. This is measure by cost of transport.
Cost of transport expresses how much energy, measured in calories or joules, a person consumes per traveled kilometer per kilogram of body weight. In running, the cost of transport in relation to speed is roughly a straight line. This means that it doesn't matter how fast you run, you always spend about 1 kcal per traveled kilometer per kilogram of body weight.
Walking is a different case. When we walk, the cost of transport forms a U-shaped curve. The transition point, where humans switch from walking to running, occurs, on average, at around 7 km/h. At that point, running becomes more economical than walking. That's why when we walk very fast – to catch the bus, for example, we're likely to start running without thinking about it.
When we walk, the cost of transport forms a U-shaped curve. The transition point, where humans switch from walking to running, occurs, on average, at around 7 km/h. At that point, running becomes more economical than walking. That's why when we walk very fast – to catch the bus, for example, we're likely to start running without thinking about it.
The transition point, where humans switch from walking to running, occurs, on average, at around 7 km/h. At that point, running becomes more economical than walking.
Race walking is a peculiar sport because athletes are forced to walk beyond 7 km/h despite their natural urge to run. As a result, they consume 50% more energy per travelled distance as they would do if they ran.
That's why elIte race walkers competing during 50 km consume almost double the energy compared to marathoners. The marathon distance is already enough to drain most of the energy resources stored in one person's muscles and liver. Race walking takes this to extreme. After crossing the finish line, a race walker's muscles and mind are so depleted of energy and willpower that it becomes literally impossible for them to keep on walking.
Walking can and is a very effective exercise. Even if you happen to hit exactly the minima of the walking cost of transport curve, you'll be consuming nearly 80% of the energy per traveled distance as compared to running. If you push a little bit more, you'll consume more energy and get more out of your walking workouts.
This explanation also help us understand why walking can be a very effective exercise. First, even if you happen to hit exactly the minima of the walking cost of transport curve, you'll be consuming nearly 80% of the energy per traveled distance as compared to running. Secondly, walking causes less stress to your muscles and therefore, you can sustain a walking speed for a longer period of time and exercise for a longer time.
Once you know the science behind walking, it is easy to understand its benefits. Walking consumes lots of energy for a long time without the muscle strain of high-impact activities. To get more out of your walking, you only need to increase energy consumption by going beyond a comfortable speed and effort.
Here're three ways to achieve this effect:
- Try power walking – Walk faster than usual to use more energy.
- Walk uphill… and downhill – Positive slopes increase you energy consumption, and negative slops make your muscles do eccentric work that builds strength.
- Practice Nordic walking – The use of walking poles will eventually consume more energy.
Reference:
Walking increases life expectancy by 3.4-4.5 years - Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis
Compared with physically inactive individuals, those who walk briskly at or above 150 min/week can increase life expectancy by 3.4–4.5 years independent of body weight.
Background:
- Leisure time physical activity reduces the risk of premature mortality, but the years of life expectancy gained at different levels remains unclear.
- Our objective was to determine the years of life gained after age 40 associated with various levels of physical activity, both overall and according to body mass index (BMI) groups, in a large pooled analysis.
Methods and findings:
- We examined the association of leisure time physical activity with mortality during follow-up in pooled data from six prospective cohort studies in the National Cancer Institute Cohort Consortium, comprising 654,827 individuals, 21-90 y of age.
- Physical activity was categorized by metabolic equivalent hours per week (MET-h/wk). Life expectancies and years of life gained/lost were calculated using direct adjusted survival curves (for participants 40+ years of age), with 95% confidence intervals (CIs) derived by bootstrap. The study includes a median 10 y of follow-up and 82,465 deaths.
- A physical activity level of 0.1-3.74 MET-h/wk, equivalent to brisk walking for up to 75 min/wk, was associated with a gain of 1.8 (95% CI: 1.6-2.0) y in life expectancy relative to no leisure time activity (0 MET-h/wk).
- Higher levels of physical activity were associated with greater gains in life expectancy, with a gain of 4.5 (95% CI: 4.3-4.7) y at the highest level (22.5+ MET-h/wk, equivalent to brisk walking for 450+ min/wk).
- Substantial gains were also observed in each BMI group. In joint analyses, being active (7.5+ MET-h/wk) and normal weight (BMI 18.5-24.9) was associated with a gain of 7.2 (95% CI: 6.5-7.9) y of life compared to being inactive (0 MET-h/wk) and obese (BMI 35.0+).
- A limitation was that physical activity and BMI were ascertained by self report.
Conclusions:
- More leisure time physical activity was associated with longer life expectancy across a range of activity levels and BMI groups.
Reference:
- Moore SC, Patel AV, Matthews CE, Berrington de Gonzalez A, Park Y, Katki HA, Linet MS, Weiderpass E, Visvanathan K, Helzlsouer KJ, Thun M, Gapstur SM, Hartge P, Lee IM. Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis. PLoS Med. 2012;9(11):e1001335. doi: 10.1371/journal.pmed.1001335. Epub 2012 Nov 6. PMID: 23139642; PMCID: PMC3491006.
- https://pubmed.ncbi.nlm.nih.gov/23139642/
Water/Electrolyte Balance Table
Hypernatremia
- Hypernatremia Hydration: OK Electrolytes: HIGH Likelihood: rare, transitory if water available Weight is normal Thirst is high, and salty foods taste bad. Mouth is not very dry Causes: no access to water, or voluntary restriction of water intake, body electrolytes concentrated by loss of water What to do: Drink to satisfy thirst, so that excess electrolytes are removed by sweating and urination. Restrict salt intake until excess is urinated and sweated out.
- Hypernatremia with dehydration Hydration: LOW Electrolytes: HIGH Likelihood: moderate Weight is down a few pounds or more Thirst is high, and salty foods taste bad. Mouth and skin are dry Food acceptance is poor Absence of urination Causes: no access to water or voluntary restriction of water intake, body electrolytes concentrated by loss of water What to do: Get access to water and drink. Restrict electrolytes until weight is near normal.
- Hypernatremia with over-hydration Hydration: HIGH Electrolytes: HIGH Likelihood: very rare Weight is up a few pounds or more Thirst is high, and salty foods taste bad. Possible mental confusion Hands may be puffy Shortness of breath, rapid heart rate Food acceptance is poor Causes: over-consumption of salt, probably from a combination of sources What to do: Stop electrolyte intake, drink only to wet mouth until weight is normal.
Hyponatremia
- Hyponatremia Hydration: OK Electrolytes: LOW Likelihood: mild form is common Weight is normal Stomach is queasy, with poor food acceptance Wrists may be puffy Salty foods taste good Thirst is normal Mouth is moist – can spit May have cramping Causes: Insufficient electrolyte intake What to do: Increase electrolyte intake until stomach feels ok.
- Hyponatremia with dehydration Hydration: LOW Electrolytes: LOW Likelihood: very rare Weight is down a few pounds or more Thirst is high, and salty foods taste good Mouth is dry, can’t spit May have cramping Skin is dry and may tent if pinched May have dizziness on standing up Causes: insufficient drinking, no electrolyte intake What to do: Take electrolytes and drink sports drink or water
- Hyponatremia with over-hydration Dangerous! Hydration: HIGH Electrolytes: LOW Likelihood: moderate Weight is up a few pounds or more Wrists and hands are puffy. Nausea, stomach sloshing, possible vomiting. Thirst is low, and salty foods taste very good. Athlete may show mental confusion, odd behavior Mouth is moist – can spit Urination may be voluminous and crystal clear Causes: over-hydration, insufficient sodium intake What to do: Drink only to wet mouth until weight is normal, then correct any sodium deficit
Other
- Proper hydration and electrolyte balance Hydration: OK Electrolytes: OK Likelihood: common Weight is stable or slightly down Stomach is fine, food acceptance is normal Mouth is moist ( can spit ) and skin is normal Cramps: none Urination is normal Causes: proper water and electrolyte intake What to do: Continue with hydration and electrolyte practice unless conditions change
- Dehydration Hydration: LOW Electrolytes: OK Likelihood: common Weight is down a few pounds or more Thirst is high, and salty foods taste normal. Mouth is dry, food acceptance is poor Skin is dry and may tent if pinched May have dizziness on standing up May have cramping Mental performance may be affected Causes: insufficient fluid intake What to do: Drink sports drink with electrolytes, or water
- Over-hydrated Hydration: HIGH Electrolytes: OK Likelihood: moderate Weight is up a few pounds or more Wrists and hands are probably puffy Stomach is queasy Thirst is low, and salty foods taste normal. Mouth is moist – can spit. Causes: fluid intake in excess of needs What to do: Drink only to wet mouth until weight is near normal
Reference:
Study: Are There Deleterious Cardiac Effects of Acute and Chronic Endurance Exercise?
Lifelong Endurance Exercise Effects on Heart:
- Acute cardiovascular risks
- ↑ risk for sudden cardiac death
- ↑ risk for acute myocardial infarction
- ↓ ventricular function of the heart
- Evidence of acute myocardial injury
- ↑ CK and CK-MB concentrations
- ↑ cardiac troponin concentrations
- ↑ BNP and NT-proBNP concentrations
- Cardiac remodeling
- ↑ dimensions of right and left ventricle
- ↑ dimensions of right and left atria
- ↑ wall thickness
- Potential cardiac maladaptations
- =/↓ Carotid intima media thickening
- ↑ ↓ Coronary artery calcification
- ↑ prevalence of myocardial fibrosis
- ↑ risk for atrial fibrillation
- ↑ risk for bradycardia
- ↑ aortic diameter
- ↑ progression of ARVC
- Longevity
- ↑ life expectancy
- ↓ risk for cardiovascular mortality
Abstract:
Multiple epidemiological studies document that habitual physical activity reduces the risk of atherosclerotic cardiovascular disease (ASCVD), and most demonstrate progressively lower rates of ASCVD with progressively more physical activity. Few studies have included individuals performing high-intensity, lifelong endurance exercise, however, and recent reports suggest that prodigious amounts of exercise may increase markers for, and even the incidence of, cardiovascular disease.
This review examines the evidence that extremes of endurance exercise may increase cardiovascular disease risk by reviewing the causes and incidence of exercise-related cardiac events, and the acute effects of exercise on cardiovascular function, the effect of exercise on cardiac biomarkers, including “myocardial” creatine kinase, cardiac troponins, and cardiac natriuretic peptides. This review also examines the effect of exercise on coronary atherosclerosis and calcification, the frequency of atrial fibrillation in aging athletes, and the possibility that exercise may be deleterious in individuals genetically predisposed to such cardiac abnormalities as long QT syndrome, right ventricular cardiomyopathy, and hypertrophic cardiomyopathy. This review is to our knowledge unique because it addresses all known potentially adverse cardiovascular effects of endurance exercise.
The best evidence remains that physical activity and exercise training benefit the population, but it is possible that prolonged exercise and exercise training can adversely affect cardiac function in some individuals. This hypothesis warrants further examination.
Reference:
- Thijs M. H. Eijsvogels, Antonio B. Fernandez, and Paul D. Thompson. Are There Deleterious Cardiac Effects of Acute and Chronic Endurance Exercise? Physiological Reviews 2016 96:1, 99-125
Study: Association between physical activity and risk of incident arrhythmias in 402,406 individuals: Evidence from the UK Biobank cohort
Notes: An analysis of over 400,000 people found that those who said they did between 150-300 minutes of moderate-to-vigorous intensity physical activity per week had a 10-15% lower risk of developing atrial fibrillation compared to those who were inactive.
Aims
- Physical activity reduces cardiovascular disease burden and mortality, although its relationship with cardiac arrhythmias is less certain. The aim of this study was to assess the association between self-reported physical activity and atrial fibrillation (AF), ventricular arrhythmias and bradyarrhythmias, across the UK Biobank cohort.
Methods and results
- We included 402,406 individuals (52.5% female), aged 40–69 years, with over 2.8 million person-years of follow-up who underwent self-reported physical activity assessment computed in metabolic equivalent-minutes per week (MET-min/wk) at baseline, detailed physical assessment and medical history evaluation. Arrhythmia episodes were diagnosed through hospital admissions and death reports.
- Incident AF risk was lower amongst physically active participants, with a more pronounced reduction amongst female participants [hazard ratio (HR) for 1500 vs. 0 MET-min/wk: 0.85, 95% confidence interval (CI) 0.74–0.98] than males (HR for 1500 vs. 0 MET-min/wk: 0.90, 95% CI 0.82–1.0).
- Similarly, we observed a significantly lower risk of ventricular arrhythmias amongst physically active participants (HR for 1500 MET-min/wk 0.78, 95% CI 0.64–0.96) that remained relatively stable over a broad range of physical activity levels between 0 and 2500 MET-min/wk.
- A lower AF risk amongst female participants who engaged in moderate levels of vigorous physical activity was observed (up to 2500 MET-min/wk).
- Vigorous physical activity was also associated with reduced ventricular arrhythmia risk. Total or vigorous physical activity was not associated with bradyarrhythmias.
Conclusion
- The risk of AF and ventricular arrhythmias is lower amongst physically active individuals. These findings provide observational support that physical activity is associated with reduced risk of atrial and ventricular arrhythmias.
Reference:
- Adrian D Elliott, Dominik Linz, Ricardo Mishima, Kadhim Kadhim, Celine Gallagher, Melissa E Middeldorp, Christian V Verdicchio, Jeroen M L Hendriks, Dennis H Lau, Andre La Gerche, Prashanthan Sanders, Association between physical activity and risk of incident arrhythmias in 402 406 individuals: evidence from the UK Biobank cohort, European Heart Journal, Volume 41, Issue 15, 14 April 2020, Pages 1479–1486, https://doi.org/10.1093/eurheartj/ehz897
Studies: COVID-19 Related
Infection and Fatality Rates
Study: The infection fatality rate of COVID-19 inferred from seroprevalence data (For those <70 yo ->0.00-0.57%)
Methods:
- Population studies with sample size of at least 500 and published as peer-reviewed papers or preprints as of July 11, 2020 were retrieved from PubMed, preprint servers, and communications with experts.
- Studies on blood donors were included, but studies on healthcare workers were excluded.
- Infection fatality rate was estimated from each study dividing the number of COVID-19 deaths at a relevant time point by the number of estimated people infected in each relevant region.
- Secondarily, results from national studies were also examined from preliminary press releases and reports whenever a country had no other data presented in full papers of preprints.
Results:
- 36 studies (43 estimates) were identified with usable data to enter into calculations and another 7 preliminary national estimates were also considered for a total of 50 estimates.
- Seroprevalence estimates ranged from 0.222% to 47%.
- Infection fatality rates ranged from 0.00% to 1.63% and corrected values ranged from 0.00% to 1.31%.
- Across 32 different locations, the median infection fatality rate was 0.27% (corrected 0.24%). Most studies were done in pandemic epicenters with high death tolls.
- Median corrected IFR was 0.10% in locations with COVID-19 population mortality rate less than the global average (<73 deaths per million as of July 12, 2020), 0.27% in locations with 73-500 COVID-19 deaths per million, and 0.90% in locations exceeding 500 COVID-19 deaths per million.
- Among people <70 years old, infection fatality rates ranged from 0.00% to 0.57% with median of 0.05% across the different locations (corrected median of 0.04%).
Estimates of infection fatality rates inferred from seroprevalence studies tend to be much lower than original speculations made in the early days of the pandemic.
Reference:
- John P.A. Ioannidis. The infection fatality rate of COVID-19 inferred from seroprevalence data. doi: https://doi.org/10.1101/2020.05.13.20101253
Study: Age-stratified infection fatality rate of COVID-19 in the non-elderly informed from pre-vaccination national seroprevalence studies
Population age:
- 94% of the global population is younger than 70 years
- 86% is younger than 60 years
Methods:
- Systematic searches in SeroTracker and PubMed (protocol: https://osf.io/xvupr), we identified 40 eligible national seroprevalence studies covering 38 countries with pre-vaccination seroprevalence data.
- For 29 countries (24 high-income, 5 others), publicly available age-stratified COVID-19 death data and age-stratified seroprevalence information were available and were included in the primary analysis.
Results:
- The IFRs had a median of 0.035% (interquartile range (IQR) 0.013 - 0.056%) for the 0-59 years old population, and 0.095% (IQR 0.036 - 0.125%,) for the 0-69 years old.
- The median IFR was:
- 0.0003% at 0-19 years
- 0.003% at 20-29 years
- 0.011% at 30-39 years
- 0.035% at 40-49 years
- 0.129% at 50-59 years
- and 0.501% at 60-69 years
- Meta-regression analyses suggested global IFR of 0.03% for 0-59yo and 0.07% for 0-69yo
The current analysis suggests a much lower pre-vaccination IFR in non-elderly populations than previously suggested.
Large differences did exist between countries and may reflect differences in comorbidities and other factors.
These estimates provide a baseline from which to fathom further IFR declines with the widespread use of vaccination, prior infections, and evolution of new variants.
Reference:
- Angelo Maria Pezzullo, Cathrine Axfors, Despina G. Contopoulos-Ioannidis, Alexandre Apostolatos, John P.A. Ioannidis. Age-stratified infection fatality rate of COVID-19 in the non-elderly informed from pre-vaccination national seroprevalence studies. doi: https://doi.org/10.1101/2022.10.11.22280963
Study: Community transmission (Vaccinated vs Unvaccinated)
Primary outcomes for the epidemiological analysis were to assess the secondary attack rate (SAR) in household contacts stratified by contact vaccination status and the index cases' vaccination status. Primary outcomes for the viral load kinetics analysis were to detect differences in the peak viral load, viral growth rate, and viral decline rate between participants infected with pre-alpha versus alpha versus delta variants and between unvaccinated delta-infected participants and vaccinated delta-infected participants.
We analysed transmission risk by vaccination status for 231 contacts exposed to 162 epidemiologically linked delta variant-infected index cases. We compared viral load trajectories from fully vaccinated individuals with delta infection (n=29) with unvaccinated individuals with delta (n=16), alpha (B.1.1.7; n=39), and pre-alpha (n=49) infections.
The SAR in household contacts exposed to the delta variant was 25% (95% CI 18–33) for fully vaccinated individuals compared with 38% (24–53) in unvaccinated individuals.
NOTE: The Confidence intervals overlap
The SAR in household contacts exposed to fully vaccinated index cases was 25% (95% CI 15–35; 17 of 69), which is similar to the SAR in household contacts exposed to unvaccinated index cases (23% [15–31]; 23 of 100; table 2). The 53 PCR-positive contacts arose from household exposure to 39 PCR-positive index cases. Of these index cases who gave rise to secondary transmission, the proportion who were fully vaccinated (15 [38%] of 39) was similar to the proportion who were unvaccinated (16 [41%] of 39).
12 (39%) of 31 infections in fully vaccinated household contacts arose from fully vaccinated epidemiologically linked index cases, further confirmed by genomic and virological analysis in three index case–contact pairs.
Fully vaccinated individuals with breakthrough infections have peak viral load similar to unvaccinated cases and can efficiently transmit infection in household settings, including to fully vaccinated contacts.
Real World Evidence: No difference in Secondary Attack Rate
Ref:
- Singanayagam A, Hakki S, Dunning J, Madon KJ, Crone MA, Koycheva A, Derqui-Fernandez N, Barnett JL, Whitfield MG, Varro R, Charlett A, Kundu R, Fenn J, Cutajar J, Quinn V, Conibear E, Barclay W, Freemont PS, Taylor GP, Ahmad S, Zambon M, Ferguson NM, Lalvani A; ATACCC Study Investigators. Community transmission and viral load kinetics of the SARS-CoV-2 delta (B.1.617.2) variant in vaccinated and unvaccinated individuals in the UK: a prospective, longitudinal, cohort study. Lancet Infect Dis. 2021 Oct 29:S1473-3099(21)00648-4. doi: 10.1016/S1473-3099(21)00648-4. Epub ahead of print. Erratum in: Lancet Infect Dis. 2021 Dec;21(12):e363. PMID: 34756186; PMCID: PMC8554486.
Study: Ct values and infectivity of SARS-CoV-2 on surfaces
- Laboratory data showing for SARS-CoV-2 that Ct values of 29·3 (steel surface) or 29·5 (plastic surface) correlate with the detection of culturable virus, whereas Ct values of 32·5 (steel surface) or 32·7 (plastic surface) correlate with the detection of non-culturable virus.
- SARS-CoV-2 RNA can be found on inanimate surfaces up to 28 days after discharge of patients with COVID-19, which further limits the relevance of RNA detection on surfaces.
- A Ct (PCR cycle time) value higher than 33 obtained from a surface sample probably has no epidemiological relevance.
- In public settings, contamination with infectious virus is even less likely than in hospitals.
- Viral contamination can occur only in the unlikely event a SARS-CoV-2 carrier comes near to a surface.
- The potential viral source is not permanently present next to the surface, probably has no symptoms, and may wear a face mask, resulting in a low probability of viral spread. In workplaces it was found that only five (0·6%) of 841 tests among employees were positive for SARS-CoV-2 RNA over a period of 2 weeks, with Ct values between 33 and 36.
- Viral contamination can occur only in the unlikely event a SARS-CoV-2 carrier comes near to a surface.
- Among 5500 surface samples, only 44 (0.8%) were positive, with Ct values between 34 and 38, indicating that viral loads were indeed very low on surfaces in close and permanent proximity to viral shedders.
We propose to routinely clean public surfaces, and to consider surface disinfection only when there is evidence that a surface is contaminated with a sufficient amount of infectious virus and is likely to contribute to viral transmission that cannot be controlled by other measures, such as surface cleaning or handwashing.
Ref:
Lockdowns
Study: Lockdowns reduced COVID mortality by 0.2%
Lockdowns, school closures and limiting gatherings only reduced COVID mortality by 0.2% at 'enormous economic and social costs', study finds
Meta-analysis of 24 studies found Covid lockdown restrictions caused just 0.2% reduction in virus deaths Economists who carried out review said border closures had virtually zero effect on Covid mortality (-0.1%) However, researchers found closing nonessential shops was most effective intervention, causing 10.6% fall
Systematic review and meta-analysis to determine whether there is empirical evidence to support the belief that "lockdowns" reduce COVID-19 mortality.
- This study employed a systematic search and screening procedure in which 18,590 studies are identified that could potentially address the belief posed. After three levels of screening, 34 studies ultimately qualified. Of those 34 eligible studies, 24 qualified for inclusion in the meta-analysis.
- Separated into three groups:
- lockdown stringency index studies
- shelter-in-place-order (SIPO) studies
- specific NPI studies
- Separated into three groups:
Stringency index studies find that lockdowns in Europe and the United States only reduced COVID-19 mortality by 0.2% on average.
SIPOs were also ineffective, only reducing COVID-19 mortality by 2.9% on average.
Specific NPI studies also find no broad-based evidence of noticeable effects on COVID-19 mortality.
Reference:
- Jonas Herby, Lars Jonung, and Steve H. Hanke A LITERATURE REVIEW AND META-ANALYSIS OF THE EFFECTS OF LOCKDOWNS ON COVID-19 MORTALITY SAE./No.200/January 2022
Study: Shelter-in-place (SIP) policies likely did not work
Abstract:
As a way of slowing COVID-19 transmission, many countries and U.S. states implemented shelter-in-place (SIP) policies. However, the effects of SIP policies on public health are a-priori ambiguous. Using an event study approach and data from 43 countries and all U.S. states, we measure changes in excess deaths following the implementation of COVID-19 shelter-in-place (SIP) policies. We do not find that countries or U.S. states that implemented SIP policies earlier had lower excess deaths. We do not observe differences in excess deaths before and after the implementation of SIP policies, even when accounting for pre-SIP COVID-19 death rates
Overall, the results suggest that the implementation of SIP policies does not appear to have met the aim of reducing excess mortality or COVID-19 deaths.
Reference:
- Virat Agrawal, Jonathan H. Cantor, Neeraj Sood, and Christopher M. Whaley. The Impact of the COVID-19 Pandemic and Policy Responses on Excess Mortality. NBER Working Paper No. 28930. June 2021, Revised September 2022 JEL No. I1,I12,I18,I28
Study: The Covid-19 lesson from Sweden: Don't lock down edit
Covid-19 triggered a wave of lockdowns across the world, contributing to a severe downturn in economic activity. Governments responded by introducing expansionary fiscal and monetary measures.
We compare the health and economic outcomes in Sweden, commonly viewed as an outlier relying more on recommendations and voluntary adjustments than on strict lockdowns, with those of comparable European OECD countries.
Our results suggest that the Swedish policy of advice and trust in the population to reduce social interactions voluntarily was relatively successful. Sweden combined low excess death rates with relatively small economic costs.
In future pandemics, policymakers should rely on empirical evidence rather than panicking and adopting extreme measures. Even if policymakers appeared to act rapidly and decisively, the rushed implementation of strict lockdowns in 2020/21 probably did more harm than good.
Sweden and the other Nordic countries had among the lowest cumulative excess mortality rates of all European countries towards the end of the sample period.5 A temporarily higher mortality rate in Sweden during the spring of 2020 was fully compensated for by lower mortality thereafter. The initial excess mortality rate recorded in Sweden was mainly found in provinces that were enjoying a winter holiday during week nine of 2020. Because of this holiday, some Swedes visited the Alps, where they were exposed to the coronavirus. In other provinces, excess mortality was lower and largely followed the pattern in the other Nordic countries (Andersson, 2022).
Our evaluation, nearly four years after the outbreak of the pandemic in the spring of 2020, suggests that policymakers made two major mistakes. First, they introduced lockdowns that were too stringent and had negligible positive health effects despite the evidence available at the time pointing towards the limited benefits of such broad measures. Second, they responded to the downturn in economic activity with fiscal and monetary policies that were excessively expansionary.
For the future, we recommend that the response to a pandemic, or to any crisis, should focus on the long-term perspective as well. Long-term considerations should be built into short-term crisis management to limit the potential damage of measures taken in panic. We are not all dead in the long run – many have to live with the consequences of the pandemic crisis response. It is essential that crisis policies do not cause more harm than good.
The evaluation of the pandemic policies will continue. We are convinced that our policy conclusions will be reinforced, especially those relating to the harmful use of mandatory lockdowns. Perhaps these measures represent the greatest policy failure of modern times.
Reference:
- Andersson, F. N. G., & Jonung, L. (2024). The Covid-19 lesson from Sweden: Don't lock down. Economic Affairs, 44(1), 3–16. https://doi.org/10.1111/ecaf.12611
- https://onlinelibrary.wiley.com/doi/full/10.1111/ecaf.12611
Natural Immunity
Study: Natural Immunity is better than Vacinated Immunity against Delta Variant
A retrospective observational study comparing three groups:
- (1)SARS-CoV-2-naive individuals who received a two-dose regimen of the BioNTech/Pfizer mRNA BNT162b2 vaccine
- (2)previously infected individuals who have not been vaccinated
- (3)previously infected and single dose vaccinated individuals.
Evaluated four outcomes:
- SARS-CoV-2 infection
- symptomatic disease
- COVID-19-related hospitalization
- death
The follow-up period of June 1 to August 14, 2021, when the Delta variant was dominant in Israel.
Results:
- SARS-CoV-2-naïve vaccinees had a 13.06-fold (95% CI, 8.08 to 21.11) increased risk for breakthrough infection with the Delta variant compared to those previously infected, when the first event (infection or vaccination) occurred during January and February of 2021.
- The increased risk was significant (P<0.001) for symptomatic disease as well.
- When allowing the infection to occur at any time before vaccination (from March 2020 to February 2021), evidence of waning natural immunity was demonstrated, though SARS-CoV-2 naive vaccinees had a 5.96-fold (95% CI, 4.85 to 7.33) increased risk for breakthrough infection and a 7.13-fold (95% CI, 5.51 to 9.21) increased risk for symptomatic disease.
- SARS-CoV-2-naive vaccinees were also at a greater risk for COVID-19-related-hospitalizations compared to those that were previously infected.
This study demonstrated that natural immunity confers longer lasting and stronger protection against infection, symptomatic disease and hospitalization caused by the Delta variant of SARS-CoV-2, compared to the BNT162b2 two-dose vaccine-induced immunity. Individuals who were both previously infected with SARS-CoV-2 and given a single dose of the vaccine gained additional protection against the Delta variant.
Reference:
- Comparing SARS-CoV-2 natural immunity to vaccine-induced immunity: reinfections versus breakthrough infections Sivan Gazit, Roei Shlezinger, Galit Perez, Roni Lotan, Asaf Peretz, Amir Ben-Tov, Dani Cohen, Khitam Muhsen, Gabriel Chodick, Tal Patalon medRxiv 2021.08.24.21262415; doi: https://doi.org/10.1101/2021.08.24.21262415 Now published in Clinical Infectious Diseases doi: 10.1093/cid/ciac262
Study: Past SARS-CoV-2 infection protection against re-infection: a systematic review and meta-analysis
- Background
- Understanding the level and characteristics of protection from past SARS-CoV-2 infection against subsequent re-infection, symptomatic COVID-19 disease, and severe disease is essential for predicting future potential disease burden, for designing policies that restrict travel or access to venues where there is a high risk of transmission, and for informing choices about when to receive vaccine doses.
- We aimed to systematically synthesise studies to estimate protection from past infection by variant, and where data allow, by time since infection.
- Methods
- In this systematic review and meta-analysis, we identified, reviewed, and extracted from the scientific literature retrospective and prospective cohort studies and test-negative case-control studies published from inception up to Sept 31, 2022, that estimated the reduction in risk of COVID-19 among individuals with a past SARS-CoV-2 infection in comparison to those without a previous infection. We meta-analysed the effectiveness of past infection by outcome (infection, symptomatic disease, and severe disease), variant, and time since infection. We ran a Bayesian meta-regression to estimate the pooled estimates of protection. Risk-of-bias assessment was evaluated using the National Institutes of Health quality-assessment tools. The systematic review was PRISMA compliant and was registered with PROSPERO (number CRD42022303850).
- Findings
- We identified a total of 65 studies from 19 different countries.
- Our meta-analyses showed that protection from past infection and any symptomatic disease was high for ancestral, alpha, beta, and delta variants, but was substantially lower for the omicron BA.1 variant.
- Pooled effectiveness against re-infection by the omicron BA.1 variant was 45·3% (95% uncertainty interval [UI] 17·3–76·1) and 44·0% (26·5–65·0) against omicron BA.1 symptomatic disease.
- Mean pooled effectiveness was greater than 78% against severe disease (hospitalisation and death) for all variants, including omicron BA.1.
- Protection from re-infection from ancestral, alpha, and delta variants declined over time but remained at 78·6% (49·8–93·6) at 40 weeks.
- Protection against re-infection by the omicron BA.1 variant declined more rapidly and was estimated at 36·1% (24·4–51·3) at 40 weeks.
- On the other hand, protection against severe disease remained high for all variants, with 90·2% (69·7–97·5) for ancestral, alpha, and delta variants, and 88·9% (84·7–90·9) for omicron BA.1 at 40 weeks.
- Interpretation
- Protection from past infection against re-infection from pre-omicron variants was very high and remained high even after 40 weeks.
- Protection was substantially lower for the omicron BA.1 variant and declined more rapidly over time than protection against previous variants.
- Protection from severe disease was high for all variants. The immunity conferred by past infection should be weighed alongside protection from vaccination when assessing future disease burden from COVID-19, providing guidance on when individuals should be vaccinated, and designing policies that mandate vaccination for workers or restrict access, on the basis of immune status, to settings where the risk of transmission is high, such as travel and high-occupancy indoor settings.
Reference:
Study: Protective effectiveness of previous SARS-CoV-2 infection and hybrid immunity against the omicron variant and severe disease: a systematic review and meta-regression
Background:
- The global surge in the omicron (B.1.1.529) variant has resulted in many individuals with hybrid immunity (immunity developed through a combination of SARS-CoV-2 infection and vaccination).
- We aimed to systematically review the magnitude and duration of the protective effectiveness of previous SARS-CoV-2 infection and hybrid immunity against infection and severe disease caused by the omicron variant.
Methods:
- For this systematic review and meta-regression, we searched for cohort, cross-sectional, and case-control studies in MEDLINE, Embase, Web of Science, ClinicalTrials.gov, the Cochrane Central Register of Controlled Trials, the WHO COVID-19 database, and Europe PubMed Central from Jan 1, 2020, to June 1, 2022, using keywords related to SARS-CoV-2, reinfection, protective effectiveness, previous infection, presence of antibodies, and hybrid immunity.
- The main outcomes were the protective effectiveness against reinfection and against hospital admission or severe disease of hybrid immunity, hybrid immunity relative to previous infection alone, hybrid immunity relative to previous vaccination alone, and hybrid immunity relative to hybrid immunity with fewer vaccine doses.
- Risk of bias was assessed with the Risk of Bias In Non-Randomized Studies of Interventions Tool. We used log-odds random-effects meta-regression to estimate the magnitude of protection at 1-month intervals. This study was registered with PROSPERO (CRD42022318605).
Findings:
- 11 studies reporting the protective effectiveness of previous SARS-CoV-2 infection and 15 studies reporting the protective effectiveness of hybrid immunity were included.
- Previous infection
- For previous infection, there were 97 estimates (27 with a moderate risk of bias and 70 with a serious risk of bias). The effectiveness of previous infection against hospital admission or severe disease was 74.6% (95% CI 63.1-83.5) at 12 months.
- The effectiveness of previous infection against reinfection waned to 24.7% (95% CI 16.4-35.5) at 12 months.
- Hybrid immunity
- For hybrid immunity, there were 153 estimates (78 with a moderate risk of bias and 75 with a serious risk of bias).
- The effectiveness of hybrid immunity against hospital admission or severe disease was 97.4% (95% CI 91.4-99.2) at 12 months with primary series vaccination and 95.3% (81.9-98.9) at 6 months with the first booster vaccination after the most recent infection or vaccination.
- Against reinfection, the effectiveness of hybrid immunity following primary series vaccination waned to 41.8% (95% CI 31.5-52.8) at 12 months, while the effectiveness of hybrid immunity following first booster vaccination waned to 46.5% (36.0-57.3) at 6 months.
Interpretation:
- All estimates of protection waned within months against reinfection but remained high and sustained for hospital admission or severe disease.
- Individuals with hybrid immunity had the highest magnitude and durability of protection, and as a result might be able to extend the period before booster vaccinations are needed compared to individuals who have never been infected.
Reference:
- Bobrovitz N, Ware H, Ma X, Li Z, Hosseini R, Cao C, Selemon A, Whelan M, Premji Z, Issa H, Cheng B, Abu Raddad LJ, Buckeridge DL, Van Kerkhove MD, Piechotta V, Higdon MM, Wilder-Smith A, Bergeri I, Feikin DR, Arora RK, Patel MK, Subissi L. Protective effectiveness of previous SARS-CoV-2 infection and hybrid immunity against the omicron variant and severe disease: a systematic review and meta-regression. Lancet Infect Dis. 2023 Jan 18:S1473-3099(22)00801-5. doi: 10.1016/S1473-3099(22)00801-5. Epub ahead of print. PMID: 36681084.
- https://pubmed.ncbi.nlm.nih.gov/36681084/
Origin
Study: COVID-19 likely assembled in vitro
The genome of SARS-COV-2 contains a peculiar pattern of unique restriction endonuclease recognition sites allowing efficient dis- and re-assembly of the viral genome characteristic of synthetic viruses.
This study reports the likelihood of observing such a pattern in coronaviruses with no history of bioengineering.
They found:
- SARS-CoV-2 is an anomaly, more likely a product of synthetic genome assembly than natural evolution
- The restriction map of SARS-CoV-2 is:
- Consistent with many previously reported synthetic coronavirus genomes
- Meets all the criteria required for an efficient reverse genetic system
- Differs from closest relatives by a significantly higher rate of synonymous mutations in these synthetic-looking recognitions sites
- Has a synthetic fingerprint unlikely to have evolved from its close relatives
The study suggests a high likelihood that SARS-CoV-2 may have originated as an infectious clone assembled in vitro.
Reference:
- Valentin Bruttel, Alex Washburne, Antonius VanDongen Endonuclease fingerprint indicates a synthetic origin of SARS-CoV-2 bioRxiv 2022.10.18.512756; doi: https://doi.org/10.1101/2022.10.18.512756
- https://www.biorxiv.org/content/10.1101/2022.10.18.512756v1.full
Prevention
Study: Possible toxicity of chronic carbon dioxide exposure associated with face mask use, particularly in pregnant women, children and adolescents – A scoping review
Introduction:
- During the SARS-CoV-2-pandemic, face masks have become one of the most important ubiquitous factors affecting human breathing. It increases the resistance and dead space volume leading to a re-breathing of CO2. So far, this phenomenon and possible implications on early life has not been evaluated in depth.
Method:
- As part of a scoping review, literature was systematically reviewed regarding CO2 exposure and facemask use.
Results:
- Fresh air has around 0.04% CO2, while wearing masks more than 5 min bears a possible chronic exposure to carbon dioxide of 1.41% to 3.2% of the inhaled air. Although the buildup is usually within the short-term exposure limits, long-term exceedances and consequences must be considered due to experimental data.
- US Navy toxicity experts set the exposure limits for submarines carrying a female crew to 0.8% CO2 based on animal studies which indicated an increased risk for stillbirths.
- Additionally, mammals who were chronically exposed to 0.3% CO2 the experimental data demonstrate a teratogenicity with irreversible neuron damage in the offspring, reduced spatial learning caused by brainstem neuron apoptosis and reduced circulating levels of the insulin-like growth factor-1. With significant impact on three readout parameters (morphological, functional, marker) this chronic 0.3% CO2 exposure has to be defined as being toxic.
- Additional data exists on the exposure of chronic 0.3% CO2 in adolescent mammals causing neuron destruction, which includes
- less activity
- increased anxiety
- impaired learning and memory
- There is also data indicating testicular toxicity in adolescents at CO2 inhalation concentrations above 0.5%.
Discussion:
- There is a possible negative impact risk by imposing extended mask mandates especially for vulnerable subgroups.
- Circumstantial evidence exists that extended mask use may be related to current observations of stillbirths and to reduced verbal motor and overall cognitive performance in children born during the pandemic.
- A need exists to reconsider mask mandates.
Reference:
- Kisielinski K, Wagner S, Hirsch O, Klosterhalfen B, Prescher A. Possible toxicity of chronic carbon dioxide exposure associated with face mask use, particularly in pregnant women, children and adolescents - A scoping review. Heliyon. 2023;9(4):e14117. https://doi.org/10.1016/j.heliyon.2023.e14117
- https://www.cell.com/heliyon/pdf/S2405-8440(23)01324-5.pdf
Study: Physical interventions to interrupt or reduce the spread of respiratory viruses (Chochrane review of masks)
- Background
- Viral epidemics or pandemics of acute respiratory infections (ARIs) pose a global threat.
- This is an update of a Cochrane Review last published in 2020.
- We include results from studies from the current COVID‐19 pandemic.
- Objectives
- To assess the effectiveness of physical interventions to interrupt or reduce the spread of acute respiratory viruses.
- Main results
- We included 11 new RCTs and cluster‐RCTs (610,872 participants) in this update, bringing the total number of RCTs to 78.
- Six of the new trials were conducted during the COVID‐19 pandemic; two from Mexico, and one each from Denmark, Bangladesh, England, and Norway.
- We identified four ongoing studies, of which one is completed, but unreported, evaluating masks concurrent with the COVID‐19 pandemic.
- The risk of bias for the RCTs and cluster‐RCTs was mostly high or unclear.
- Medical/surgical masks compared to no masks
- We included 12 trials (10 cluster‐RCTs) comparing medical/surgical masks versus no masks to prevent the spread of viral respiratory illness (two trials with healthcare workers and 10 in the community).
- Wearing masks in the community probably makes little or no difference to the outcome of influenza‐like illness (ILI)/COVID‐19 like illness compared to not wearing masks (risk ratio (RR) 0.95, 95% confidence interval (CI) 0.84 to 1.09; 9 trials, 276,917 participants; moderate‐certainty evidence.
- Wearing masks in the community probably makes little or no difference to the outcome of laboratory‐confirmed influenza/SARS‐CoV‐2 compared to not wearing masks (RR 1.01, 95% CI 0.72 to 1.42; 6 trials, 13,919 participants; moderate‐certainty evidence).
- Harms were rarely measured and poorly reported (very low‐certainty evidence).
- N95/P2 respirators compared to medical/surgical masks
- We pooled trials comparing N95/P2 respirators with medical/surgical masks (four in healthcare settings and one in a household setting).
- We are very uncertain on the effects of N95/P2 respirators compared with medical/surgical masks on the outcome of clinical respiratory illness (RR 0.70, 95% CI 0.45 to 1.10; 3 trials, 7779 participants; very low‐certainty evidence).
- N95/P2 respirators compared with medical/surgical masks may be effective for ILI (RR 0.82, 95% CI 0.66 to 1.03; 5 trials, 8407 participants; low‐certainty evidence).
- Evidence is limited by imprecision and heterogeneity for these subjective outcomes.
- The use of a N95/P2 respirators compared to medical/surgical masks probably makes little or no difference for the objective and more precise outcome of laboratory‐confirmed influenza infection (RR 1.10, 95% CI 0.90 to 1.34; 5 trials, 8407 participants; moderate‐certainty evidence).
- Restricting pooling to healthcare workers made no difference to the overall findings.
- Harms were poorly measured and reported, but discomfort wearing medical/surgical masks or N95/P2 respirators was mentioned in several studies (very low‐certainty evidence).
- One previously reported ongoing RCT has now been published and observed that medical/surgical masks were non‐inferior to N95 respirators in a large study of 1009 healthcare workers in four countries providing direct care to COVID‐19 patients.
- Hand hygiene compared to control
- Nineteen trials compared hand hygiene interventions with controls with sufficient data to include in meta‐analyses.
- Settings included schools, childcare centres and homes.
- Comparing hand hygiene interventions with controls (i.e. no intervention), there was a 14% relative reduction in the number of people with ARIs in the hand hygiene group (RR 0.86, 95% CI 0.81 to 0.90; 9 trials, 52,105 participants; moderate‐certainty evidence), suggesting a probable benefit.
- In absolute terms this benefit would result in a reduction from 380 events per 1000 people to 327 per 1000 people (95% CI 308 to 342).
- When considering the more strictly defined outcomes of ILI and laboratory‐confirmed influenza, the estimates of effect for ILI (RR 0.94, 95% CI 0.81 to 1.09; 11 trials, 34,503 participants; low‐certainty evidence), and laboratory‐confirmed influenza (RR 0.91, 95% CI 0.63 to 1.30; 8 trials, 8332 participants; low‐certainty evidence), suggest the intervention made little or no difference.
- We pooled 19 trials (71, 210 participants) for the composite outcome of ARI or ILI or influenza, with each study only contributing once and the most comprehensive outcome reported. Pooled data showed that hand hygiene may be beneficial with an 11% relative reduction of respiratory illness (RR 0.89, 95% CI 0.83 to 0.94; low‐certainty evidence), but with high heterogeneity.
- In absolute terms this benefit would result in a reduction from 200 events per 1000 people to 178 per 1000 people (95% CI 166 to 188).
- Few trials measured and reported harms (very low‐certainty evidence).
- We found no RCTs on gowns and gloves, face shields, or screening at entry ports.
- Authors' conclusions
- The high risk of bias in the trials, variation in outcome measurement, and relatively low adherence with the interventions during the studies hampers drawing firm conclusions. There were additional RCTs during the pandemic related to physical interventions but a relative paucity given the importance of the question of masking and its relative effectiveness and the concomitant measures of mask adherence which would be highly relevant to the measurement of effectiveness, especially in the elderly and in young children.
- There is uncertainty about the effects of face masks. The low to moderate certainty of evidence means our confidence in the effect estimate is limited, and that the true effect may be different from the observed estimate of the effect. The pooled results of RCTs did not show a clear reduction in respiratory viral infection with the use of medical/surgical masks. There were no clear differences between the use of medical/surgical masks compared with N95/P2 respirators in healthcare workers when used in routine care to reduce respiratory viral infection. Hand hygiene is likely to modestly reduce the burden of respiratory illness, and although this effect was also present when ILI and laboratory‐confirmed influenza were analysed separately, it was not found to be a significant difference for the latter two outcomes. Harms associated with physical interventions were under‐investigated.
Reference:
- Jefferson T, Dooley L, Ferroni E, Al-Ansary LA, van Driel ML, Bawazeer GA, Jones MA, Hoffmann TC, Clark J, Beller EM, Glasziou PP, Conly JM. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database of Systematic Reviews 2023, Issue 1. Art. No.: CD006207. DOI: 10.1002/14651858.CD006207.pub6. Accessed 03 February 2023.
- https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006207.pub6/full
Study: FXR inhibition may protect from SARS-CoV-2 infection by reducing ACE2 (urodiol/actigall)
Prevention of SARS-CoV-2 infection through the modulation of viral host receptors, such as ACE2
Here, we identify the farnesoid X receptor (FXR) as a direct regulator of ACE2 transcription in multiple COVID19-affected tissues, including the gastrointestinal and respiratory systems.
We then use the over-the-counter compound z-guggulsterone (ZGG) and the off-patent drug ursodeoxycholic acid (UDCA) to reduce FXR signalling and downregulate ACE2 in human lung, cholangiocyte and intestinal organoids and in the corresponding tissues in mice and hamsters.
We demonstrate that UDCA-mediated ACE2 downregulation reduces susceptibility to SARS-CoV-2 infection in vitro, in vivo and in human lungs and livers perfused ex situ.
Furthermore, we illustrate that UDCA reduces ACE2 expression in the nasal epithelium in humans.
Finally, we identify a correlation between UDCA treatment and positive clinical outcomes following SARS-CoV-2 infection using retrospective registry data, and confirm these findings in an independent validation cohort of liver transplant recipients.
In conclusion, we identify a novel function of FXR in controlling ACE2 expression and provide evidence that modulation of this pathway could be beneficial for reducing SARS-CoV-2 infection, paving the road for future clinical trials.
Reference:
- Brevini, T., Maes, M., Webb, G.J. et al. FXR inhibition may protect from SARS-CoV-2 infection by reducing ACE2. Nature (2022). https://doi.org/10.1038/s41586-022-05594-0
Study: Japan supercomputer shows doubling masks offers little help preventing viral spread
Researchers used the Fugaku supercomputer to model the flow of virus particles from people wearing different types and combinations of masks, according to a study by research giant Riken and Kobe University.
- Using a single surgical-type mask, made of non-woven material, had 85% effectiveness in blocking particles when worn tightly around the nose and face.
- Adding a polyurethane mask on top boosted the effectiveness to just 89%.
- Wearing two non-woven masks isn't useful because air resistance builds up and causes leakage around the edges.
"The performance of double masking simply does not add up," wrote the researchers, led by Makoto Tsubokura.
In general, professional grade N95 masks were the best in protecting against infection, followed by:
- non-woven masks
- cloth masks
- and finally polyurethane types
Reference:
Study: Wastewater-based monitoring of SARS-CoV-2 at UK airports and its potential role in international public health surveillance (COVID travel restrictions on flying were a total failure)
It is well established that air travel plays a key role in the global spread of many enteric and respiratory diseases, including COVID-19. Even with travel restrictions (e.g. mask wearing, negative COVID-19 test prior to departure), SARS-CoV-2 may be transmitted by asymptomatic or pre-symptomatic individuals carrying the virus. Due to the limitation of current clinical surveillance approaches, complementary methods need to be developed to allow estimation of the frequency of SARS-CoV-2 entry across international borders.
Wastewater-based epidemiology (WBE) represents one such approach, allowing the unbiased sampling of SARS-CoV-2 carriage by passenger cohorts entering via airports.
Methods:
- In this study, we monitored sewage in samples from terminals (n = 150) and aircraft (n = 32) at three major international airports in the UK for 1–3 weeks in March 2022.
- As the raw samples were more turbid than typical municipal wastewater, we used beef extract treatment followed by polyethylene glycol (PEG) precipitation to concentrate viruses, followed by reverse transcription quantitative PCR (RT-qPCR) for the detection of SARS-CoV-2 and a faecal indicator virus, crAssphage.
Results:
- All samples taken from sewers at the arrival terminals of Heathrow and Bristol airports, and 85% of samples taken from sites at Edinburgh airport, were positive for SARS-CoV-2.
- This suggests a high COVID-19 prevalence among passengers and/or airport staff members.
- Samples derived from aircraft also showed 93% SARS-CoV-2 positivity.
- No difference in viral prevalence was found before and after COVID-19 travel restrictions were lifted.
Our results suggest that WBE is a useful tool for monitoring the global transfer rate of human pathogens and other disease-causing agents across international borders and should form part of wider international efforts to monitor and contain the spread of future disease outbreaks.
Reference:
- Farkas K, Williams R, Alex-Sanders N, Grimsley JMS, Pântea I, Wade MJ, et al. (2023) Wastewater-based monitoring of SARS-CoV-2 at UK airports and its potential role in international public health surveillance. PLOS Glob Public Health 3(1): e0001346. https://doi.org/10.1371/journal.pgph.0001346
- https://journals.plos.org/globalpublichealth/article?id=10.1371/journal.pgph.0001346
Study: N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel (RCT)
Key Points
- Question Is the use of N95 respirators or medical masks more effective in preventing influenza infection among outpatient health care personnel in close contact with patients with suspected respiratory illness?
- Findings In this pragmatic, cluster randomized clinical trial involving 2862 health care personnel, there was no significant difference in the incidence of laboratory-confirmed influenza among health care personnel with the use of N95 respirators (8.2%) vs medical masks (7.2%).
- Meaning As worn by health care personnel in this trial, use of N95 respirators, compared with medical masks, in the outpatient setting resulted in no significant difference in the rates of laboratory-confirmed influenza.
Abstract
Importance
- Clinical studies have been inconclusive about the effectiveness of N95 respirators and medical masks in preventing health care personnel (HCP) from acquiring workplace viral respiratory infections.
Objective
- To compare the effect of N95 respirators vs medical masks for prevention of influenza and other viral respiratory infections among HCP.
Design, Setting, and Participants
- A cluster randomized pragmatic effectiveness study conducted at 137 outpatient study sites at 7 US medical centers between September 2011 and May 2015, with final follow-up in June 2016.
- Each year for 4 years, during the 12-week period of peak viral respiratory illness, pairs of outpatient sites (clusters) within each center were matched and randomly assigned to the N95 respirator or medical mask groups.
Interventions
- Overall, 1993 participants in 189 clusters were randomly assigned to wear N95 respirators (2512 HCP-seasons of observation) and 2058 in 191 clusters were randomly assigned to wear medical masks (2668 HCP-seasons) when near patients with respiratory illness.
Main Outcomes and Measures
- The primary outcome was the incidence of laboratory-confirmed influenza.
- Secondary outcomes included incidence of acute respiratory illness, laboratory-detected respiratory infections, laboratory-confirmed respiratory illness, and influenzalike illness.
- Adherence to interventions was assessed.
Results
- Among 2862 randomized participants (mean [SD] age, 43 [11.5] years; 2369 [82.8%]) women), 2371 completed the study and accounted for 5180 HCP-seasons.
- There were 207 laboratory-confirmed influenza infection events (8.2% of HCP-seasons) in the N95 respirator group and 193 (7.2% of HCP-seasons) in the medical mask group (difference, 1.0%, [95% CI, −0.5% to 2.5%]; P = .18) (adjusted odds ratio [OR], 1.18 [95% CI, 0.95-1.45]).
- There were:
- 1556 acute respiratory illness events in the respirator group vs 1711 in the mask group (difference, −21.9 per 1000 HCP-seasons [95% CI, −48.2 to 4.4]; P = .10);
- 679 laboratory-detected respiratory infections in the respirator group vs 745 in the mask group (difference, −8.9 per 1000 HCP-seasons, [95% CI, −33.3 to 15.4]; P = .47);
- 371 laboratory-confirmed respiratory illness events in the respirator group vs 417 in the mask group (difference, −8.6 per 1000 HCP-seasons [95% CI, −28.2 to 10.9]; P = .39);
- 128 influenzalike illness events in the respirator group vs 166 in the mask group (difference, −11.3 per 1000 HCP-seasons [95% CI, −23.8 to 1.3]; P = .08).
- In the respirator group, 89.4% of participants reported "always" or "sometimes" wearing their assigned devices vs 90.2% in the mask group.
Conclusions and Relevance
- Among outpatient health care personnel, N95 respirators vs medical masks as worn by participants in this trial resulted in no significant difference in the incidence of laboratory-confirmed influenza.
Reference:
- Radonovich LJ, Simberkoff MS, Bessesen MT, et al. N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial. JAMA. 2019;322(9):824–833. https://doi.org/10.1001/jama.2019.11645
- https://jamanetwork.com/journals/jama/fullarticle/2749214
Study: Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers (RCT)
- Objective:
- To assess whether recommending surgical mask use outside the home reduces wearers' risk for SARS-CoV-2 infection in a setting where masks were uncommon and not among recommended public health measures.
- Design:
- Randomized controlled trial (DANMASK-19 [Danish Study to Assess Face Masks for the Protection Against COVID-19 Infection]). (ClinicalTrials.gov: NCT04337541)
- Participants:
- Adults spending more than 3 hours per day outside the home without occupational mask use.
- Intervention:
- Encouragement to follow social distancing measures for coronavirus disease 2019, plus either no mask recommendation or a recommendation to wear a mask when outside the home among other persons together with a supply of 50 surgical masks and instructions for proper use.
- Measurements:
- The primary outcome was SARS-CoV-2 infection in the mask wearer at 1 month by antibody testing, polymerase chain reaction (PCR), or hospital diagnosis. The secondary outcome was PCR positivity for other respiratory viruses.
- Results:
- A total of 3030 participants were randomly assigned to the recommendation to wear masks, and 2994 were assigned to control; 4862 completed the study.
- Infection with SARS-CoV-2 occurred in 42 participants recommended masks (1.8%) and 53 control participants (2.1%). The between-group difference was −0.3 percentage point (95% CI, −1.2 to 0.4 percentage point; P = 0.38) (odds ratio, 0.82 [CI, 0.54 to 1.23]; P = 0.33).
- Multiple imputation accounting for loss to follow-up yielded similar results. Although the difference observed was not statistically significant, the 95% CIs are compatible with a 46% reduction to a 23% increase in infection.
- Limitation:
- Inconclusive results, missing data, variable adherence, patient-reported findings on home tests, no blinding, and no assessment of whether masks could decrease disease transmission from mask wearers to others.
- Conclusion:
- The recommendation to wear surgical masks to supplement other public health measures did not reduce the SARS-CoV-2 infection rate among wearers by more than 50% in a community with modest infection rates, some degree of social distancing, and uncommon general mask use. The data were compatible with lesser degrees of self-protection.
Reference:
- Bundgaard H, Bundgaard JS, Raaschou-Pedersen DET, von Buchwald C, Todsen T, Norsk JB, Pries-Heje MM, Vissing CR, Nielsen PB, Winsløw UC, Fogh K, Hasselbalch R, Kristensen JH, Ringgaard A, Porsborg Andersen M, Goecke NB, Trebbien R, Skovgaard K, Benfield T, Ullum H, Torp-Pedersen C, Iversen K. Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers : A Randomized Controlled Trial. Ann Intern Med. 2021 Mar;174(3):335-343. doi: 10.7326/M20-6817. Epub 2020 Nov 18. PMID: 33205991; PMCID: PMC7707213.
- https://www.acpjournals.org/doi/10.7326/M20-6817
Study: Correlation Between Mask Compliance and COVID-19 Outcomes in Europe
Masking was the single most common non-pharmaceutical intervention in the course of the coronavirus disease 2019 (COVID-19) pandemic. Most countries have implemented recommendations or mandates regarding the use of masks in public spaces.
The aim of this short study was to analyse the correlation between mask usage against morbidity and mortality rates in the 2020-2021 winter in Europe.
Data from 35 European countries on morbidity, mortality, and mask usage during a six-month period were analysed and crossed.
Mask usage was more homogeneous in Eastern Europe than in Western European countries.
Spearman's correlation coefficients between mask usage and COVID-19 outcomes were either null or positive, depending on the subgroup of countries and type of outcome (cases or deaths).
- Positive correlations were stronger in Western than in Eastern European countries.
These findings indicate that countries with high levels of mask compliance did not perform better than those with low mask usage.
Reference:
- Spira B. Correlation Between Mask Compliance and COVID-19 Outcomes in Europe. Cureus. 2022 Apr 19;14(4):e24268. doi: 10.7759/cureus.24268. PMID: 35607577; PMCID: PMC9123350.
- https://www.cureus.com/articles/93826-correlation-between-mask-compliance-and-covid-19-outcomes-in-europe
Study: Modeling the filtration efficiency of a woven fabric: The role of multiple lengthscales
During the COVID-19 pandemic, many millions have worn masks made of woven fabric to reduce the risk of transmission of COVID-19. Masks are essentially air filters worn on the face that should filter out as many of the dangerous particles as possible. Here, the dangerous particles are the droplets containing the virus that are exhaled by an infected person.
Woven fabric is unlike the material used in standard air filters. Woven fabric consists of fibers twisted together into yarns that are then woven into fabric.
There are, therefore, two lengthscales: the diameters of (i) the fiber and (ii) the yarn. Standard air filters have only (i). To understand how woven fabrics filter, we have used confocal microscopy to take three-dimensional images of woven fabric. We then used the image to perform lattice Boltzmann simulations of the air flow through fabric.
With this flow field, we calculated the filtration efficiency for particles a micrometer and larger in diameter.
In agreement with experimental measurements by others, we found that for particles in this size range, the filtration efficiency is low.
For particles with a diameter of 1.5 μm, our estimated efficiency is in the range 2.5%–10%.
The low efficiency is due to most of the air flow being channeled through relatively large (tens of micrometers across) inter-yarn pores.
So, we conclude that due to the hierarchical structure of woven fabrics, they are expected to filter poorly.
Reference:
- Rios de Anda I, Wilkins JW, Robinson JF, Royall CP, Sear RP. Modeling the filtration efficiency of a woven fabric: The role of multiple lengthscales. Phys Fluids (1994). 2022 Mar;34(3):033301. doi: 10.1063/5.0074229. Epub 2022 Mar 1. PMID: 35342280; PMCID: PMC8939465.
- https://aip.scitation.org/doi/10.1063/5.0074229
Study: Revisiting Pediatric COVID-19 Cases in Counties With and Without School Mask Requirements—United States, July 1—October 20 2021
- Background:
- There has been considerable debate around mask requirements in schools in the United States and other countries during the Covid-19 pandemic. To date, there have been no randomized controlled trials of mask requirements in children.
- All analyses of the effectiveness of school mask mandates have relied on observational studies. The Centers for Disease Control in the U.S. have released multiple observational studies suggesting that school mask mandates significantly reduce case rates. However, there have also been numerous additional US and international observational studies finding no significant effect of school mask mandates on pediatric cases.
- Methods:
- Our study replicates a highly cited CDC study showing a negative association between school mask mandates and pediatric SARS-CoV-2 cases.
- We then extend the study using a larger sample of districts and a longer time interval, employing almost six times as much data as the original study.
- We examine the relationship between mask mandates and per-capita pediatric cases, using multiple regression to control for differences across school districts.
- Findings:
- Replicating the CDC study shows similar results; however, incorporating a larger sample and longer period showed no significant relationship between mask mandates and case rates.
- These results persisted when using regression methods to control for differences across districts.
- Interpretation:
- School districts that choose to mandate masks are likely to be systematically different from those that do not in multiple, often unobserved, ways.
- We failed to establish a relationship between school masking and pediatric cases using the same methods but a larger, more nationally diverse population over a longer interval.
- Our study demonstrates that observational studies of interventions with small to moderate effect sizes are prone to bias caused by selection and omitted variables.
- Randomized studies can more reliably inform public health policy.
Reference:
- Chandra, Ambarish and Høeg, Tracy Beth, Revisiting Pediatric COVID-19 Cases in Counties With and Without School Mask Requirements—United States, July 1—October 20 2021. Available at SSRN: https://ssrn.com/abstract=4118566 or http://dx.doi.org/10.2139/ssrn.4118566
- https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4118566
Study: Mask mandate and use efficacy in state-level COVID-19 containment
- Background
- Containment of the COVID-19 pandemic requires evidence-based strategies to reduce transmission. Because COVID-19 can spread via respired droplets, many states have mandated mask use in public settings. Randomized control trials have not clearly demonstrated mask efficacy against respiratory viruses, and observational studies conflict on whether mask use predicts lower infection rates. We hypothesized that statewide mask mandates and mask use are associated with lower COVID-19 case growth rates in the United States.
- Methods
- We calculated total COVID-19 case growth and mask use for the continental United States with data from the Centers for Disease Control and Prevention and Institute for Health Metrics and Evaluation. We estimated post-mask mandate case growth in non-mandate states using median issuance dates of neighboring states with mandates.
- Results
- Case growth was not significantly different between mandate and non-mandate states at low or high transmission rates, and surges were equivocal.
- Mask use predicted lower case growth at low, but not high transmission rates.
- Growth rates were comparable between states in the first and last mask use quintiles adjusted for normalized total cases early in the pandemic and unadjusted after peak Fall-Winter infections.
- Mask use did not predict Summer 2020 case growth for non-Northeast states or Fall-Winter 2020 growth for all continental states.
- Conclusions
- Mask mandates and use are not associated with slower state-level COVID-19 spread during COVID-19 growth surges. Containment requires future research and implementation of existing efficacious strategies.
References:
- Damian D. Guerra, Daniel J. Guerra. Mask mandate and use efficacy for COVID-19 containment in US States. medRxiv 2021.05.18.21257385; doi: https://doi.org/10.1101/2021.05.18.21257385
- https://www.medrxiv.org/content/10.1101/2021.05.18.21257385v2
Study: Associations of Physical Inactivity and COVID-19 Outcomes Among Subgroups (Physically active = less COVID symptoms)
- Introduction
- Physical activity before COVID-19 infection is associated with less severe outcomes. The study determined whether a dose‒response association was observed and whether the associations were consistent across demographic subgroups and chronic conditions.
- Methods
- A retrospective cohort study of Kaiser Permanente Southern California adult patients who had a positive COVID-19 diagnosis between January 1, 2020 and May 31, 2021 was created. The exposure was the median of at least 3 physical activity self-reports before diagnosis. Patients were categorized as follows: always inactive, all assessments at 10 minutes/week or less; mostly inactive, median of 0–60 minutes per week; some activity, median of 60–150 minutes per week; consistently active, median>150 minutes per week; and always active, all assessments>150 minutes per week. Outcomes were hospitalization, deterioration event, or death 90 days after a COVID-19 diagnosis. Data were analyzed in 2022.
- Results
- Of 194,191 adults with COVID-19 infection, 6.3% were hospitalized, 3.1% experienced a deterioration event, and 2.8% died within 90 days.
- Dose‒response effects were strong; for example, patients in the some activity category had higher odds of hospitalization (OR=1.43; 95% CI=1.26, 1.63), deterioration (OR=1.83; 95% CI=1.49, 2.25), and death (OR=1.92; 95% CI=1.48, 2.49) than those in the always active category.
- Results were generally consistent across sex, race and ethnicity, age, and BMI categories and for patients with cardiovascular disease or hypertension.
- Conclusions
- There were protective associations of physical activity for adverse COVID-19 outcomes across demographic and clinical characteristics.
- Public health leaders should add physical activity to pandemic control strategies.
Reference:
- Young DR, Sallis JF, Baecker A, Cohen DA, Nau CL, Smith GN, Sallis RE. Associations of Physical Inactivity and COVID-19 Outcomes Among Subgroups. Am J Prev Med. 2022 Dec 10:S0749-3797(22)00526-8. doi: 10.1016/j.amepre.2022.10.007. Epub ahead of print. PMID: 36528452; PMCID: PMC9750896.
- https://www.ajpmonline.org/article/S0749-3797(22)00526-8/fulltext
Study: Medical Masks Versus N95 Respirators for Preventing COVID-19 Among Health Care Workers (No difference)
- Objective:
- To determine whether medical masks are noninferior to N95 respirators to prevent COVID-19 in health care workers providing routine care.
- Design:
- Multicenter, randomized, noninferiority trial. (ClinicalTrials.gov: NCT04296643).
- Setting:
- 29 health care facilities in Canada, Israel, Pakistan, and Egypt from 4 May 2020 to 29 March 2022.
- Participants:
- 1009 health care workers who provided direct care to patients with suspected or confirmed COVID-19.
- Intervention:
- Use of medical masks versus fit-tested N95 respirators for 10 weeks, plus universal masking, which was the policy implemented at each site.
- Measurements:
- The primary outcome was confirmed COVID-19 on reverse transcriptase polymerase chain reaction (RT-PCR) test.
- Results:
- In the intention-to-treat analysis, RT-PCR–confirmed COVID-19 occurred in 52 of 497 (10.46%) participants in the medical mask group versus 47 of 507 (9.27%) in the N95 respirator group (hazard ratio [HR], 1.14 [95% CI, 0.77 to 1.69]).
- An unplanned subgroup analysis by country found that in the medical mask group versus the N95 respirator group RT-PCR–confirmed COVID-19 occurred in 8 of 131 (6.11%) versus 3 of 135 (2.22%) in Canada (HR, 2.83 [CI, 0.75 to 10.72]), 6 of 17 (35.29%) versus 4 of 17 (23.53%) in Israel (HR, 1.54 [CI, 0.43 to 5.49]), 3 of 92 (3.26%) versus 2 of 94 (2.13%) in Pakistan (HR, 1.50 [CI, 0.25 to 8.98]), and 35 of 257 (13.62%) versus 38 of 261 (14.56%) in Egypt (HR, 0.95 [CI, 0.60 to 1.50]).
- There were 47 (10.8%) adverse events related to the intervention reported in the medical mask group and 59 (13.6%) in the N95 respirator group.
- Limitation:
- Potential acquisition of SARS-CoV-2 through household and community exposure, heterogeneity between countries, uncertainty in the estimates of effect, differences in self-reported adherence, differences in baseline antibodies, and between-country differences in circulating variants and vaccination.
- Conclusion:
- Among health care workers who provided routine care to patients with COVID-19, the overall estimates rule out a doubling in hazard of RT-PCR–confirmed COVID-19 for medical masks when compared with HRs of RT-PCR–confirmed COVID-19 for N95 respirators. The subgroup results varied by country, and the overall estimates may not be applicable to individual countries because of treatment effect heterogeneity.
Reference:
- Loeb M, Bartholomew A, Hashmi M, et al. Medical Masks Versus N95 Respirators for Preventing COVID-19 Among Health Care Workers : A Randomized Trial [published online ahead of print, 2022 Nov 29]. Ann Intern Med. 2022;M22-1966. https://doi.org/10.7326/M22-1966
Study: Child mask mandates for COVID-19: a systematic review
Abstract
Background
- Mask mandates for children during the COVID-19 pandemic varied in different locations. A risk-benefit analysis of this intervention has not yet been performed. In this study, we performed a systematic review to assess research on the effectiveness of mask wearing in children.
Methods
- We performed database searches up to February 2023. The studies were screened by title and abstract, and included studies were further screened as full-text references. A risk-of-bias analysis was performed by two independent reviewers and adjudicated by a third reviewer.
Results
- We screened 597 studies and included 22 in the final analysis.
- There were no randomised controlled trials in children assessing the benefits of mask wearing to reduce SARS-CoV-2 infection or transmission.
- The six observational studies reporting an association between child masking and lower infection rate or antibody seropositivity had critical (n=5) or serious (n=1) risk of bias; all six were potentially confounded by important differences between masked and unmasked groups and two were shown to have non-significant results when reanalysed.
- Sixteen other observational studies found no association between mask wearing and infection or transmission.
Conclusions
- Real-world effectiveness of child mask mandates against SARS-CoV-2 transmission or infection has not been demonstrated with high-quality evidence.
- The current body of scientific data does not support masking children for protection against COVID-19.
WHAT IS ALREADY KNOWN ON THIS TOPIC
- Child mask mandates have been extensively used as a public health measure during the COVID-19 pandemic.
- Masking recommendations appear to be entirely based on mechanistic and observational data, and a systematic review assessing the evidence has not been performed.
WHAT THIS STUDY ADDS
- In this systematic review, 16 studies found no effect of mask wearing on infection or transmission, while six studies reporting a protective association had critical or serious risk of bias.
- Because benefits of masking for COVID-19 have not been identified, it should be recognised that mask recommendations for children are not supported by scientific evidence.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
- COVID-19-related policy recommendations should be informed by high-quality evidence and consider the possibility of harm, especially for children, who are vulnerable and an ethically protected group.
- Healthcare providers and adults working with children should be educated about the absence of high-quality data supporting masking to lower SARS-CoV-2 infection and transmission risks.
- Because absence of harm is not established, recommending child masking does not meet the accepted practice of promulgating only medical interventions where benefits clearly outweigh harms.
Reference:
- Sandlund J, Duriseti R, Ladhani SN, et al Child mask mandates for COVID-19: a systematic review Archives of Disease in Childhood Published Online First: 02 December 2023. doi: 10.1136/archdischild-2023-326215
- https://doi.org/10.1136/archdischild-2023-326215
- https://adc.bmj.com/content/early/2023/12/06/archdischild-2023-326215
Study: Coffee as a dietary strategy to prevent SARS-CoV-2 infection edit
Background
- To date, most countries lifted the restriction requirement and coexisted with SARS-CoV-2. Thus, dietary behavior for preventing SARS-CoV-2 infection becomes an interesting issue on a daily basis. Coffee consumption is connected with reduced COVID-19 risk and correlated to COVID-19 severity. However, the mechanisms of coffee for the reduction of COVID-19 risk are still unclear.
Results
- Here, we identified that coffee can inhibit multiple variants of the SARS-CoV-2 infection by restraining the binding of the SARS-CoV-2 spike protein to human angiotensin-converting enzyme 2 (ACE2), and reducing transmembrane serine protease 2 (TMPRSS2) and cathepsin L (CTSL) activity.
- Then, we used the method of "Here" (HRMS-exploring-recombination-examining) and found that isochlorogenic acid A, B, and C of coffee ingredients showed their potential to inhibit SARS-CoV-2 infection (inhibitory efficiency 43–54%).
- In addition, decaffeinated coffee still preserves inhibitory activity against SARS-CoV-2.
- Finally, in a human trial of 64 subjects, we identified that coffee consumption (approximately 1–2 cups/day) is sufficient to inhibit infection of multiple variants of SARS-CoV-2 entry, suggesting coffee could be a dietary strategy to prevent SARS-CoV2 infection.
Conclusions
- This study verified moderate coffee consumption, including decaffeination, can provide a new guideline for the prevention of SARS-CoV-2. Based on the results, we also suggest a coffee-drinking plan for people to prevent infection in the post-COVID-19 era.
Notes:
- Collected commercially available coffee beans produced from different places and measured their effects on the entry of SARS-CoV-2 by SARS-CoV-2 viral pseudo-particle (Vpp) infection assay assay in the 293T-ACE2 cell line (human embryonic kidney cells transfected with ACE2 expression vector for expressing ACE2), which are sensitive to test infection efficiency through spike and ACE2 interaction.
- We observed that ground coffee at 6 mg/ml (weight of coffee grinding powder/ water volume) has the effect of reducing the entry of SARS-CoV-2 into host cells with an inhibitory effect of about 60% to 81% and presented a dose-dependent manner
- Besides commercially available coffee beans, we further extended to verify whether commercially available instant coffee also had the potency to suppress the prospect of infection with SARS-CoV-2. The result showed that different brands of instant coffee significantly inhibit cell entry of SARS-CoV-2 at 1 mg/ml (coffee extract powder/ water volume), its inhibition efficacy (70–96%), and half maximal inhibitory concentration (IC50 = 0.237 mg/ml)
- After drinking coffee, the entry of the Omicron variant pseudovirus can be significantly inhibited within 6 h
- The data suggested that the optimal timeline for coffee to inhibit SARS-CoV-2 infection is within 6 h
Reference:
- Wu CS, Li YC, Peng SL, et al. Coffee as a dietary strategy to prevent SARS-CoV-2 infection. Cell Biosci. 2023;13(1):210. Published 2023 Nov 14. https://doi.org/10.1186/s13578-023-01154-9
- https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-023-01154-9
Risk Factors
Study: Risk factors for developing COVID-19
Risk factors for severe COVID-19 include:
- older age
- male sex
- obesity
- black or Asian ethnicity
- underlying medical conditions
A prospective, population-based cohort study (COVIDENCE UK) from 1 May 2020 to 5 February 2021.
Results:
- 446 incident cases of COVID-19 in 15 227 participants (2.9%)
- Increased odds of developing COVID-19 were independently associated with:
- Asian/Asian British versus white ethnicity (aOR 2.28, 95% CI 1.33 to 3.91)
- household overcrowding (aOR per additional 0.5 people/bedroom 1.26, 1.11 to 1.43)
- any versus no visits to/from other households in previous week (aOR 1.31, 1.06 to 1.62)
- number of visits to indoor public places (aOR per extra visit per week 1.05, 1.02 to 1.09)
- frontline occupation excluding health/social care versus no frontline occupation (aOR 1.49, 1.12 to 1.98)
- raised body mass index (BMI) (aOR 1.50 (1.19 to 1.89) for BMI 25.0–30.0 kg/m2 and 1.39 (1.06 to 1.84) for BMI >30.0 kg/m2 versus BMI <25.0 kg/m2)
- Atopic disease was independently associated with decreased odds (aOR 0.75, 0.59 to 0.97).
- No independent associations were seen for age, sex, other medical conditions, diet or micronutrient supplement use.
After rigorous adjustment for factors influencing exposure to SARS-CoV-2, Asian/Asian British ethnicity and raised BMI were associated with increased odds of developing COVID-19, while atopic disease was associated with decreased odds.
Reference:
- Holt H, Talaei M, Greenig M, et al Risk factors for developing COVID-19: a population-based longitudinal study (COVIDENCE UK) Thorax 2022;77:900-912
Study: Association between virus variants, vaccination, previous infections, and post-COVID-19 risk edit
Highlights
- Infection with Omicron is associated with a lower post-COVID-19 condition risk.
- Post-COVID-19 condition risk is lower among those who had previous infections.
- Post-COVID-19 condition risk did not differ by vaccination status.
- Symptom patterns were similar across variants.
Objectives
- The SARS-CoV-2 Omicron variant has spread rapidly and has been the dominant variant since 2022. The course of acute infection, in a vaccinated population, with Omicron is milder compared with earlier variants. However, little is known about how the occurrence of long-term symptoms after Omicron infection compared with other variants is modulated by previous infections and/or vaccinations.
Methods
- Participants of the DigiHero study provided information about their SARS-CoV-2 infections, vaccinations, and symptoms 12 or more weeks after infection (post-COVID-19 condition - PCC).
Results
- Participants infected with wildtype SARS-CoV-2 had the highest PCC risk (adjusted odds ratio [aOR] 6.44, 95% confidence interval (CI): 5.49; 7.56), followed by participants infected with Alpha and Delta compared with the reference group (individuals infected with Omicron having received three or more vaccinations).
- Among those infected with a specific variant, the number of preceding vaccinations was not associated with a risk reduction for PCC, whereas previous infection was strongly associated with a lower PCC risk (aOR 0.14, 95% CI 0.07; 0.25).
Conclusions
- While infection with Omicron is less likely to result in PCC compared with previous variants, lack of protection by vaccination suggests a substantial challenge for the healthcare system during the early endemic period.
- In the midterm, the protective effects of previous infections can reduce the burden of PCC.
Reference:
- Diexer S, Klee B, Gottschick C, Xu C, Broda A, Purschke O, Binder M, Frese T, Girndt M, Hoell JI, Moor I, Gekle M, Mikolajczyk R. Association between virus variants, vaccination, previous infections, and post-COVID-19 risk. Int J Infect Dis. 2023 Aug 25;136:14-21. doi: 10.1016/j.ijid.2023.08.019. Epub ahead of print. PMID: 37634619.
- https://www.ijidonline.com/article/S1201-9712(23)00702-6/fulltext
Sequelae
Study: Post-acute sequelae of SARS-CoV-2 associates with physical inactivity in a cohort of COVID-19 survivors
The aim of this study was to determine whether Post-acute Sequelae of SARS-CoV-2 Infection (PASC) are associated with physical inactivity in COVID-19 survivors.
Methods:
- This is a cohort study of COVID-19 survivors discharged from a tertiary hospital in Sao Paulo, Brazil.
- Patients admitted as inpatients due to laboratory-confirmed COVID-19 between March and August 2020 were consecutively invited for a follow-up in-person visit 6 to 11 months after hospitalization.
- Ten symptoms of PASC were assessed using standardized scales.
- Physical activity was assessed by questionnaire and participants were classified according to WHO Guidelines.
Results:
- 614 patients were analyzed (age: 56 ± 13 years; 53% male).
- Frequency of physical inactivity in patients exhibiting none, at least 1, 1–4, and 5 or more symptoms of PASC was 51%, 62%, 58%, and 71%, respectively.
- Adjusted models showed that patients with one or more persistent PASC symptoms have greater odds of being physically inactive than those without any persistent symptoms (OR: 1.57 [95% CI 1.04–2.39], P = 0.032).
- Dyspnea (OR: 2.22 [1.50–3.33], P < 0.001), fatigue (OR: 2.01 [1.40–2.90], P < 0.001), insomnia (OR: 1.69 [1.16–2.49], P = 0.007), post-traumatic stress (OR: 1.53 [1.05–2.23], P = 0.028), and severe muscle/joint pain (OR: 1.53 [95% CI 1.08–2.17], P = 0.011) were associated with greater odds of being physically inactive.
This study suggests that PASC is associated with physical inactivity, which itself may be considered as a persistent symptom among COVID-19 survivors. This may help in the early identification of patients who could benefit from additional interventions tailored to combat inactivity (even after treatment of PASC), with potential beneficial impacts on overall morbidity/mortality and health systems worldwide.
Reference:
- Gil, S., Gualano, B., de Araújo, A.L. et al. Post-acute sequelae of SARS-CoV-2 associates with physical inactivity in a cohort of COVID-19 survivors. Sci Rep 13, 215 (2023). https://doi.org/10.1038/s41598-022-26888-3
- https://www.nature.com/articles/s41598-022-26888-3#citeas
Study: Development of a Definition of Postacute Sequelae of SARS-CoV-2 Infection
Importance
- SARS-CoV-2 infection is associated with persistent, relapsing, or new symptoms or other health effects occurring after acute infection, termed postacute sequelae of SARS-CoV-2 infection (PASC), also known as long COVID. Characterizing PASC requires analysis of prospectively and uniformly collected data from diverse uninfected and infected individuals.
Objective
- To develop a definition of PASC using self-reported symptoms and describe PASC frequencies across cohorts, vaccination status, and number of infections.
Design, Setting, and Participants
- Prospective observational cohort study of adults with and without SARS-CoV-2 infection at 85 enrolling sites (hospitals, health centers, community organizations) located in 33 states plus Washington, DC, and Puerto Rico. Participants who were enrolled in the RECOVER adult cohort before April 10, 2023, completed a symptom survey 6 months or more after acute symptom onset or test date. Selection included population-based, volunteer, and convenience sampling.
Exposure
- SARS-CoV-2 infection.
Main Outcomes and Measures
- PASC and 44 participant-reported symptoms (with severity thresholds).
Results
- A total of 9764 participants (89% SARS-CoV-2 infected; 71% female; 16% Hispanic/Latino; 15% non-Hispanic Black; median age, 47 years [IQR, 35-60]) met selection criteria.
- Adjusted odds ratios were 1.5 or greater (infected vs uninfected participants) for 37 symptoms.
- Symptoms contributing to PASC score included:
- postexertional malaise
- fatigue
- brain fog
- dizziness
- gastrointestinal symptoms
- palpitations
- changes in sexual desire or capacity
- loss of or change in smell or taste
- thirst
- chronic cough
- chest pain
- abnormal movements
- Among 2231 participants first infected on or after December 1, 2021, and enrolled within 30 days of infection, 224 (10% [95% CI, 8.8%-11%]) were PASC positive at 6 months.
Conclusions and Relevance
- A definition of PASC was developed based on symptoms in a prospective cohort study.
- As a first step to providing a framework for other investigations, iterative refinement that further incorporates other clinical features is needed to support actionable definitions of PASC.
Reference:
- Thaweethai T, Jolley SE, Karlson EW, et al. Development of a Definition of Postacute Sequelae of SARS-CoV-2 Infection. JAMA. Published online May 25, 2023. https://doi.org/10.1001/jama.2023.8823
- https://jamanetwork.com/journals/jama/fullarticle/2805540?guestAccessKey=1fbcad3a-e2ab-492f-8dcc-0288c178fb94
Study: COVID-Specific Long-term Sequelae in Comparison to Common Viral Respiratory Infections: An Analysis of 17 487 Infected Adult Patients (The 7 Long Covid Symptoms)
The seven long COVID symptoms are:
- Rapid heartbeat
- Hair loss
- Chest pain
- Fatigue
- Joint pain
- Shortness of breath
- Obesity
Background
- We analyzed a large and diverse patient cohort to study health effects related to SARS-CoV-2 infection occurring >1 month postinfection.
Methods
- We analyzed 17,487 patients who received diagnoses for SARS-CoV-2 infection in a total of 122 health care facilities in the United States before April 14, 2022.
- Patients were propensity score–matched with patients diagnosed with the common cold, influenza, or viral pneumonia from March 1, 2020, to April 1, 2021.
- For each outcome, SARS-CoV-2 was compared with a generic viral respiratory infection (VRI) by predicting diagnoses in the period between 30 and 365 days postinfection.
- Both coronavirus disease 2019 (COVID-19) and VRI patients were propensity score–matched with patients with no record of COVID-19 or VRI, and the same methodology was applied.
- Diagnoses where COVID-19 infection was a significant positive predictor in both COVID-19 vs VRI and COVID-19 vs control comparisons were considered COVID-19-specific effects.
Results
- Compared with common VRIs, SARS-CoV-2 was associated with diagnoses of the following in the postinfectious period:
- palpitations
- hair loss
- fatigue
- chest pain
- dyspnea
- joint pain
- obesity
Conclusions
- We identify that some diagnoses commonly described as "long COVID" do not appear significantly more frequent post–COVID-19 infection compared with other common VRIs. We also identify sequelae that are specifically associated with a prior SARS-CoV-2 infection.
Reference:
- Baskett WI, Qureshi AI, Shyu D, Armer JM, Shyu CR. COVID-Specific Long-term Sequelae in Comparison to Common Viral Respiratory Infections: An Analysis of 17 487 Infected Adult Patients. Open Forum Infect Dis. 2022 Dec 21;10(1):ofac683. doi: 10.1093/ofid/ofac683. PMID: 36686632; PMCID: PMC9846186.
- https://academic.oup.com/ofid/article/10/1/ofac683/6953331?login=false
Study: Long COVID: major findings, mechanisms and recommendations
- Long COVID is an often debilitating illness that occurs in at least 10% of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections.
- More than 200 symptoms have been identified with impacts on multiple organ systems.
- At least 65 million individuals worldwide are estimated to have long COVID, with cases increasing daily.
Biomedical research has made substantial progress in identifying various pathophysiological changes and risk factors and in characterizing the illness; further, similarities with other viral-onset illnesses such as myalgic encephalomyelitis/chronic fatigue syndrome and postural orthostatic tachycardia syndrome have laid the groundwork for research in the field.
In this Review, we explore the current literature and highlight key findings, the overlap with other conditions, the variable onset of symptoms, long COVID in children and the impact of vaccinations. Although these key findings are critical to understanding long COVID, current diagnostic and treatment options are insufficient, and clinical trials must be prioritized that address leading hypotheses. Additionally, to strengthen long COVID research, future studies must account for biases and SARS-CoV-2 testing issues, build on viral-onset research, be inclusive of marginalized populations and meaningfully engage patients throughout the research process.
Reference:
- Davis, H.E., McCorkell, L., Vogel, J.M. et al. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol 21, 133–146 (2023). https://doi.org/10.1038/s41579-022-00846-2
- https://www.nature.com/articles/s41579-022-00846-2
Study: Machine learning links unresolving secondary pneumonia to mortality in patients with severe pneumonia, including COVID-19
BACKGROUND. Despite guidelines promoting the prevention and aggressive treatment of ventilator-associated pneumonia (VAP), the importance of VAP as a driver of outcomes in mechanically ventilated patients, including patients with severe COVID-19, remains unclear. We aimed to determine the contribution of unsuccessful treatment of VAP to mortality in patients with severe pneumonia.
METHODS. We performed a single-center prospective cohort study of 585 mechanically ventilated patients with severe pneumonia and respiratory failure, 190 of whom had COVID-19, who underwent at least one bronchoalveolar lavage. A panel of ICU physicians adjudicated pneumonia episodes and endpoints based on clinical and microbiologic data. Given the relatively long ICU length of stay among patients with COVID-19, we developed a machine learning approach called CarpeDiem, which groups similar ICU patient-days into clinical states based on electronic health record data.
RESULTS.
- CarpeDiem revealed that the long ICU length of stay among patients with COVID-19 is attributable to long stays in clinical states characterized primarily by respiratory failure.
- While VAP was not associated with mortality overall, mortality was higher in patients with one episode of unsuccessfully treated VAP compared with successfully treated VAP (76.4% versus 17.6%, P < 0.001).
- In all patients, including those with COVID-19, CarpeDiem demonstrated that unresolving VAP was associated with transitions to clinical states associated with higher mortality.
CONCLUSIONS.
- Unsuccessful treatment of VAP is associated with greater mortality.
- The relatively long length of stay among patients with COVID-19 is primarily due to prolonged respiratory failure, placing them at higher risk of VAP.
Reference:
- Gao CA, Markov NS, Stoeger T, et al. Machine learning links unresolving secondary pneumonia to mortality in patients with severe pneumonia, including COVID-19 [published online ahead of print, 2023 Apr 27]. J Clin Invest. 2023;e170682. https://doi.org/10.1172/JCI170682
- https://www.jci.org/articles/view/170682
Study: Orthostatic tachycardia after covid-19
What you need to know:
- Tachycardia on standing or minimal exertion may occur after covid-19 and may cause substantial functional impairment
- When assessing a patient with tachycardia, consider potential causes including autonomic dysfunction
- Measures to reduce tachycardia can greatly improve function and ability to return to activities and work
Long COVID: Signs and symptoms that persist for more than four weeks (and especially more than 12 weeks) following acute covid-19
Prevalence estimates vary depending on sample and setting, but indicate that about 25% of long covid patients may have dysautonomia and 2-14% will develop orthostatic tachycardia (postural orthostatic tachycardia syndrome) six to eight months after infection
Standardized tests:
- Active stand test
- NASA lean test
POTS:
- Upright or standing heart rate change sustained for 10 min in absence of hypotension
- Increase of >40 bpm in 12-19yo
- >30 bpm in >20yo
- OR >120 bpm at any age
Managment
- Identify and avoid triggers
- Compression hosiery
- Salt: 10g/day unless contraindicated
- Replace flulids: 2-3L/d
- Sleep optimisation
- Gradual return to exercise if tolerated
- Relaxation techniques such as yoga
- Small frequent meals, avoid refined carbohydrates
Medications (all off-label):
- alpha and beta blockers
- anticholinesterase inhibitors
- Ivabradine
- Peripheral vasoconstrictors
- Central adrenergic blockers
- Volume expanders
Reference:
- BMJ 2023;380:e073488
- https://www.bmj.com/content/380/bmj-2022-073488/infographic
Study: COVID does not increase incidence of neither pericarditis nor myocarditis
Retrospective cohort study of 196,992 adults after COVID-19 infection in Clalit Health Services members in Israel between March 2020 and January 2021.
Methods:
- Inpatient myocarditis and pericarditis diagnoses were retrieved from day 10 after positive PCR.
- Follow-up was censored on 28 February 2021, with minimum observation of 18 days.
- The control cohort of 590,976 adults with at least one negative PCR and no positive PCR were age- and sex-matched. Since the Israeli vaccination program was initiated on 20 December 2020, the time-period matching of the control cohort was calculated backward from 15 December 2020.
Results:
- Nine post-COVID-19 patients developed myocarditis (0.0046%), and eleven patients were diagnosed with pericarditis (0.0056%).
- In the control cohort, 27 patients had myocarditis (0.0046%) and 52 had pericarditis (0.0088%).
- Age (adjusted hazard ratio [aHR] 0.96, 95% confidence interval [CI]; 0.93 to 1.00) and male sex (aHR 4.42; 95% CI, 1.64 to 11.96) were associated with myocarditis.
- Male sex (aHR 1.93; 95% CI 1.09 to 3.41) and peripheral vascular disease (aHR 4.20; 95% CI 1.50 to 11.72) were associated with pericarditis.
Post COVID-19 infection was not associated with either myocarditis (aHR 1.08; 95% CI 0.45 to 2.56) or pericarditis (aHR 0.53; 95% CI 0.25 to 1.13).
We did not observe an increased incidence of neither pericarditis nor myocarditis in adult patients recovering from COVID-19 infection.
Reference:
- Tuvali O, Tshori S, Derazne E, Hannuna RR, Afek A, Haberman D, Sella G, George J. The Incidence of Myocarditis and Pericarditis in Post COVID-19 Unvaccinated Patients-A Large Population-Based Study. J Clin Med. 2022 Apr 15;11(8):2219. doi: 10.3390/jcm11082219. PMID: 35456309; PMCID: PMC9025013.
Study: SARS-CoV-2 infection triggers pro-atherogenic inflammatory responses in human coronary vessels edit
Patients with coronavirus disease 2019 (COVID-19) present increased risk for ischemic cardiovascular complications up to 1 year after infection. Although the systemic inflammatory response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection likely contributes to this increased cardiovascular risk, whether SARS-CoV-2 directly infects the coronary vasculature and attendant atherosclerotic plaques remains unknown.
Here we report that SARS-CoV-2 viral RNA is detectable and replicates in coronary lesions taken at autopsy from severe COVID-19 cases.
SARS-CoV-2 targeted plaque macrophages and exhibited a stronger tropism for arterial lesions than adjacent perivascular fat, correlating with macrophage infiltration levels.
SARS-CoV-2 entry was increased in cholesterol-loaded primary macrophages and dependent, in part, on neuropilin-1.
SARS-CoV-2 induced a robust inflammatory response in cultured macrophages and human atherosclerotic vascular explants with secretion of cytokines known to trigger cardiovascular events.
Our data establish that SARS-CoV-2 infects coronary vessels, inducing plaque inflammation that could trigger acute cardiovascular complications and increase the long-term cardiovascular risk.
Reference:
- Eberhardt N, Noval MG, Kaur R, Sajja S, Amadori L, Das D, Cilhoroz B, Stewart O, Fernandez DM, Shamailova R, Guillen AV, Jangra S, Schotsaert M, Gildea M, Newman JD, Faries P, Maldonado T, Rockman C, Rapkiewicz A, Stapleford KA, Narula N, Moore KJ, Giannarelli C. SARS-CoV-2 infection triggers pro-atherogenic inflammatory responses in human coronary vessels. bioRxiv [Preprint]. 2023 Aug 15:2023.08.14.553245. doi: 10.1101/2023.08.14.553245. PMID: 37645908; PMCID: PMC10461985.
- https://www.nature.com/articles/s44161-023-00336-5
Testing
Study: False Positive Results
False-Positive Results in Rapid Antigen Tests for SARS-CoV-2
There were 903,408 rapid antigen tests conducted for 537 workplaces, with 1322 positive results (0.15%), of which 1103 had PCR information. Approximately two-thirds of screens were trackable with a lot number. The number of false-positive results was 462 (0.05% of screens and 42% of positive test results with PCR information). Of these, 278 false-positive results (60%) occurred in 2 workplaces 675 km apart run by different companies between September 25 and October 8, 2021. All of the false-positive test results from these 2 workplaces were drawn from a single batch of Abbott's Panbio COVID-19 Ag Rapid Test Device.
Reference:
- Gans JS, Goldfarb A, Agrawal AK, Sennik S, Stein J, Rosella L. False-Positive Results in Rapid Antigen Tests for SARS-CoV-2. JAMA. 2022;327(5):485–486. https://doi.org/10.1001/jama.2021.24355
Study: Serologic Testing of US Blood Donations
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), was first identified in Wuhan, China, in December 2019, with subsequent worldwide spread. The first US cases were identified in January 2020. Methods
Methods:
- Residual archived samples from 7389 routine blood donations collected by the American Red Cross from 13 December 2019 to 17 January 2020 from donors resident in 9 states (California, Connecticut, Iowa, Massachusetts, Michigan, Oregon, Rhode Island, Washington, and Wisconsin) were tested at the Centers for Disease Control and Prevention for anti–SARS-CoV-2 antibodies.
- Specimens reactive by pan-immunoglobulin (pan-Ig) enzyme-linked immunosorbent assay (ELISA) against the full spike protein were tested by IgG and IgM ELISAs, microneutralization test, Ortho total Ig S1 ELISA, and receptor-binding domain/ACE2 blocking activity assay.
Results:
- Of the 7389 samples, 106 were reactive by pan-Ig.
- Of these 106 specimens, 90 were available for further testing.
- Eighty-four of 90 had neutralizing activity,
- 1 had S1 binding activity
- 1 had receptor-binding domain/ACE2 blocking activity >50%, suggesting the presence of anti–SARS-CoV-2–reactive antibodies.
- Donations with reactivity occurred in all 9 states.
These findings suggest that SARS-CoV-2 may have been introduced into the United States prior to 19 January 2020.
Reference:
- Sridhar V Basavaraju, Monica E Patton, Kacie Grimm, Mohammed Ata Ur Rasheed, Sandra Lester, Lisa Mills, Megan Stumpf, Brandi Freeman, Azaibi Tamin, Jennifer Harcourt, Jarad Schiffer, Vera Semenova, Han Li, Bailey Alston, Muyiwa Ategbole, Shanna Bolcen, Darbi Boulay, Peter Browning, Li Cronin, Ebenezer David, Rita Desai, Monica Epperson, Yamini Gorantla, Tao Jia, Panagiotis Maniatis, Kimberly Moss, Kristina Ortiz, So Hee Park, Palak Patel, Yunlong Qin, Evelene Steward-Clark, Heather Tatum, Andrew Vogan, Briana Zellner, Jan Drobeniuc, Matthew R P Sapiano, Fiona Havers, Carrie Reed, Susan Gerber, Natalie J Thornburg, Susan L Stramer, Serologic Testing of US Blood Donations to Identify Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)–Reactive Antibodies: December 2019–January 2020, Clinical Infectious Diseases, Volume 72, Issue 12, 15 June 2021, Pages e1004–e1009, https://doi.org/10.1093/cid/ciaa1785
Treatment
Study: Antidepressant drug prescription and incidence of COVID-19 in mental health outpatients: a retrospective cohort study
Background
- Currently, the main pharmaceutical intervention for COVID-19 is vaccination. While antidepressant (AD) drugs have shown some efficacy in treatment of symptomatic COVID-19, their preventative potential remains largely unexplored. Analysis of association between prescription of ADs and COVID-19 incidence in the population would be beneficial for assessing the utility of ADs in COVID-19 prevention.
Methods
- Retrospective study of association between AD prescription and COVID-19 diagnosis was performed in a cohort of community-dwelling adult mental health outpatients during the 1st wave of COVID-19 pandemic in the UK. Clinical record interactive search (CRIS) was performed for mentions of ADs within 3 months preceding admission to inpatient care of the South London and Maudsley (SLaM) NHS Foundation Trust. Incidence of positive COVID-19 tests upon admission and during inpatient treatment was the primary outcome measure.
Results
- AD mention was associated with approximately 40% lower incidence of positive COVID-19 test results when adjusted for socioeconomic parameters and physical health.
- This association was also observed for prescription of ADs of the selective serotonin reuptake inhibitor (SSRI) class.
Conclusions
- This preliminary study suggests that ADs, and SSRIs in particular, may be of benefit for preventing COVID-19 infection spread in the community.
- The key limitations of the study are its retrospective nature and the focus on a mental health patient cohort.
- A more definitive assessment of AD and SSRI preventative potential warrants prospective studies in the wider demographic.
Reference:
- Glebov OO, Mueller C, Stewart R, Aarsland D, Perera G. Antidepressant drug prescription and incidence of COVID-19 in mental health outpatients: a retrospective cohort study. BMC Med. 2023;21(1):209. Published 2023 Jun 21. https://doi.org/10.1186/s12916-023-02877-9
- https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-023-02877-9
Study: Discriminatory Attitudes Against the Unvaccinated During a Global Pandemic
During the COVID-19 pandemic sizeable groups of unvaccinated minorities persist even in countries with high vaccine access. Consequently, vaccination became a controversial subject of debate and even protest.
Here, we assess whether people express discriminatory attitudes in the form of negative affect, stereotypes and exclusionary attitudes in family and political settings across groups defined by COVID-19 vaccination status.
We quantify discriminatory attitudes between vaccinated and unvaccinated citizens in 21 countries, covering a diverse set of cultures across the world.
Across three conjoint experimental studies (N=15,233), we demonstrate that vaccinated people express discriminatory attitudes towards the unvaccinated, as high as the discriminatory attitudes suffered by common targets like immigrant and minority populations.
In contrast, there is an absence of evidence that unvaccinated individuals display discriminatory attitudes towards vaccinated people, except for the presence of negative affect in Germany and United States.
We find evidence in support of discriminatory attitudes against the unvaccinated in all countries except Hungary and Romania and find that discriminatory attitudes are more strongly expressed in cultures with stronger cooperative norms.
Prior research on the psychology of cooperation has shown that individuals react negatively against perceived free-riders including in the domain of vaccinations.
Consistent with this, the present findings suggest that contributors to the public good of epidemic control (i.e., the vaccinated) react with discriminatory attitudes against perceived free-riders (i.e., the unvaccinated). Elites and the vaccinated general public appealed to moral obligations to increase COVID-19 vaccine uptake but the present findings suggest that discriminatory attitudes including support for the removal of fundamental rights simultaneously emerged.
Refernce:
- Bor, A., Jørgensen, F. & Petersen, M.B. Discriminatory Attitudes Against the Unvaccinated During a Global Pandemic. Nature (2022). https://doi.org/10.1038/s41586-022-05607-y
- https://www.nature.com/articles/s41586-022-05607-y#citeas
Study: Alarming antibody evasion properties of rising SARS-CoV-2 BQ and XBB subvariants
NOTE:
- These variants, taken together, are currently causing 72% of new infections in the U.S., according to data from the Centers for Disease Control and Prevention.
- Vaccines not working against COVID in 2022
Article Summary:
The BQ and XBB subvariants of SARS-CoV-2 Omicron are now rapidly expanding, possibly due to altered antibody evasion properties deriving from their additional spike mutations.
Here, we report that neutralization of BQ.1, BQ.1.1, XBB, and XBB.1 by sera from vaccinees and infected persons was markedly impaired, including sera from individuals boosted with a WA1/BA.5 bivalent mRNA vaccine.
Titers against BQ and XBB subvariants were lower by 13-81-fold and 66-155-fold, respectively, far beyond what had been observed to date.
Monoclonal antibodies capable of neutralizing the original Omicron variant were largely inactive against these new subvariants, and the responsible individual spike mutations were identified.
These subvariants were found to have similar ACE2-binding affinities as their predecessors.
Together, our findings indicate that BQ and XBB subvariants present serious threats to current COVID-19 vaccines, render inactive all authorized antibodies, and may have gained dominance in the population because of their advantage in evading antibodies.
Reference:
- Wang, Q., Iketani, S., Li, Z., Liu, L., Guo, Y., Huang, Y., Bowen, A.D., Liu, M., Wang, M., Yu, J., Valdez, R., Lauring, A.S., Sheng, Z., Wang, H.H., Gordon, A., Liu, L., Ho, D.D., Alarming antibody evasion properties of rising SARS-CoV-2 BQ and XBB subvariants Cell (2023), doi: https://doi.org/10.1016/j.cell.2022.12.018.
- https://linkinghub.elsevier.com/retrieve/pii/S0092867422015318
- https://www.cell.com/cell/fulltext/S0092-8674(22)01531-8
Study: Effectiveness of the Coronavirus Disease 2019 (COVID-19) Bivalent Vaccine
Background
- The purpose of this study was to evaluate whether a bivalent COVID-19 vaccine protects against COVID-19.
Methods
- Employees of Cleveland Clinic in employment on the day the bivalent COVID-19 vaccine first became available to employees, were included. The cumulative incidence of COVID-19 was examined over the following weeks. Protection provided by vaccination (analyzed as a time-dependent covariate) was evaluated using Cox proportional hazards regression. The analysis was adjusted for the pandemic phase when the last prior COVID-19 episode occurred, and the number of prior vaccine doses received.
Results
- Among 51011 employees, 20689 (41%) had had a previous documented episode of COVID-19, and 42064 (83%) had received at least two doses of a COVID-19 vaccine.
- COVID-19 occurred in 2452 (5%) during the study.
- Risk of COVID-19 increased with time since the most recent prior COVID-19 episode and with the number of vaccine doses previously received.
- In multivariable analysis, the bivalent vaccinated state was independently associated with lower risk of COVID-19 (HR, .70; 95% C.I., .61-.80), leading to an estimated vaccine effectiveness (VE) of 30% (95% CI, 20-39%).
- Compared to last exposure to SARS-CoV-2 within 90 days, last exposure 6-9 months previously was associated with twice the risk of COVID-19, and last exposure 9-12 months previously with 3.5 times the risk.
Conclusions
- The bivalent COVID-19 vaccine given to working-aged adults afforded modest protection overall against COVID-19, while the virus strains dominant in the community were those represented in the vaccine.
Reference:
- Nabin K. Shrestha, Patrick C. Burke, Amy S. Nowacki, James F. Simon, Amanda Hagen, Steven M. Gordon. Effectiveness of the Coronavirus Disease 2019 (COVID-19) Bivalent Vaccine. medRxiv 2022.12.17.22283625; doi: https://doi.org/10.1101/2022.12.17.22283625 Now published in Open Forum Infectious Diseases doi: 10.1093/ofid/ofad209
- https://www.medrxiv.org/content/10.1101/2022.12.17.22283625v1
Study: Evaluation of Waning of SARS-CoV-2 Vaccine–Induced Immunity
Importance
- Estimates of the rate of waning of vaccine effectiveness (VE) against COVID-19 are key to assess population levels of protection and future needs for booster doses to face the resurgence of epidemic waves.
Objective
- To quantify the progressive waning of VE associated with the Delta and Omicron variants of SARS-CoV-2 by number of received doses.
Data Sources
- PubMed and Web of Science were searched from the databases' inception to October 19, 2022, as well as reference lists of eligible articles. Preprints were included.
Study Selection
- Selected studies for this systematic review and meta-analysis were original articles reporting estimates of VE over time against laboratory-confirmed SARS-CoV-2 infection and symptomatic disease.
Data Extraction and Synthesis
- Estimates of VE at different time points from vaccination were retrieved from original studies. A secondary data analysis was performed to project VE at any time from last dose administration, improving the comparability across different studies and between the 2 considered variants. Pooled estimates were obtained from random-effects meta-analysis.
Main Outcomes and Measures
- Outcomes were VE against laboratory-confirmed Omicron or Delta infection and symptomatic disease and half-life and waning rate associated with vaccine-induced protection.
Results
- A total of 799 original articles and 149 reviews published in peer-reviewed journals and 35 preprints were identified.
- Of these, 40 studies were included in the analysis.
- Pooled estimates of VE of a primary vaccination cycle against laboratory-confirmed Omicron infection and symptomatic disease were both lower than 20% at 6 months from last dose administration.
- Booster doses restored VE to levels comparable to those acquired soon after the administration of the primary cycle.
- However, 9 months after booster administration, VE against Omicron was lower than 30% against laboratory-confirmed infection and symptomatic disease.
- The half-life of VE against symptomatic infection was estimated to be 87 days (95% CI, 67-129 days) for Omicron compared with 316 days (95% CI, 240-470 days) for Delta.
- Similar waning rates of VE were found for different age segments of the population.
Conclusions and Relevance
- These findings suggest that the effectiveness of COVID-19 vaccines against laboratory-confirmed Omicron or Delta infection and symptomatic disease rapidly wanes over time after the primary vaccination cycle and booster dose. These results can inform the design of appropriate targets and timing for future vaccination programs.
Reference:
- Menegale F, Manica M, Zardini A, et al. Evaluation of Waning of SARS-CoV-2 Vaccine-Induced Immunity: A Systematic Review and Meta-analysis. JAMA Netw Open. 2023;6(5):e2310650. Published 2023 May 1. https://doi.org/10.1001/jamanetworkopen.2023.10650
- https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2804451
Study: Vaccines and Serious Adverse Effects Rate
Secondary analysis of serious adverse events reported in the placebo-controlled, phase III randomized clinical trials of Pfizer and Moderna mRNA COVID-19 vaccines in adults (NCT04368728 and NCT04470427), focusing analysis on Brighton Collaboration adverse events of special interest.
Results
- Pfizer and Moderna mRNA COVID-19 vaccines were associated with an excess risk of serious adverse events of special interest of 10.1 and 15.1 per 10,000 vaccinated over placebo baselines of 17.6 and 42.2 (95 % CI −0.4 to 20.6 and −3.6 to 33.8), respectively.
- Combined, the mRNA vaccines were associated with an excess risk of serious adverse events of special interest of 12.5 per 10,000 vaccinated (95 % CI 2.1 to 22.9); risk ratio 1.43 (95 % CI 1.07 to 1.92).
- The Pfizer trial exhibited a 36 % higher risk of serious adverse events in the vaccine group; risk difference 18.0 per 10,000 vaccinated (95 % CI 1.2 to 34.9); risk ratio 1.36 (95 % CI 1.02 to 1.83).
- The Moderna trial exhibited a 6 % higher risk of serious adverse events in the vaccine group: risk difference 7.1 per 10,000 (95 % CI –23.2 to 37.4); risk ratio 1.06 (95 % CI 0.84 to 1.33).
- Combined, there was a 16 % higher risk of serious adverse events in mRNA vaccine recipients: risk difference 13.2 (95 % CI −3.2 to 29.6); risk ratio 1.16 (95 % CI 0.97 to 1.39).
Reference:
- Joseph Fraiman, Juan Erviti, Mark Jones, Sander Greenland, Patrick Whelan, Robert M. Kaplan, Peter Doshi, Serious adverse events of special interest following mRNA COVID-19 vaccination in randomized trials in adults, Vaccine, Volume 40, Issue 40, 2022, Pages 5798-5805, ISSN 0264-410X, https://doi.org/10.1016/j.vaccine.2022.08.036.
Study: Sex-specific differences in myocardial injury incidence after COVID-19 mRNA-1273 Booster Vaccination
Aims
- To explore the incidence and potential mechanisms of oligosymptomatic myocardial injury following COVID-19 mRNA booster vaccination.
Methods and Results
- Hospital employees scheduled to undergo mRNA-1273 booster vaccination were assessed for mRNA-1273 vaccination-associated myocardial injury, defined as acute dynamic increase in high-sensitivity cardiac troponin T (hs-cTnT) concentration above the sex-specific upper-limit of normal on day 3 (48-96 h) after vaccination without evidence of an alternative cause.
- To explore possible mechanisms, antibodies against IL-1RA, the SARS-CoV2-Nucleoprotein(NP) and -Spike(S1) proteins and an array of 14 inflammatory cytokines were quantified.
- Among 777 participants, median age 37 years, 69.5% women:
- 40 participants (5.1% [95%CI, 3.7%–7.0%]) had elevated hs-cTnT concentration on day 3 and mRNA-1273 vaccine-associated myocardial injury was adjudicated in 22 participants (2.8% [95%CI, 1.7%–4.3%])
- Twenty cases occurred in women (3.7% [95%CI, 2.3%–5.7%]), two in men (0.8% [95%CI, 0.1%–3.0%])
- Hs-cTnT-elevations were mild and only temporary
- No patient had ECG-changes, and none developed major adverse cardiac events within 30 days (0% [95%CI, 0%–0.4%]).
- In the overall booster cohort, hs-cTnT concentrations (day 3; median 5 [IQR, 4–6] ng/L) were significantly higher compared to matched controls (n = 777, median 3 [IQR, 3–5] ng/L, p < 0.001). Cases had comparable systemic reactogenicity, concentrations of anti-IL-1RA, anti-NP, anti-S1, and markers quantifying systemic inflammation, but lower concentrations of IFN-λ1(IL-29) and GM-CSF versus persons without vaccine-associated myocardial injury.
Conclusion
- mRNA-1273 vaccine-associated myocardial injury was more common than previously thought, being mild and transient, and more frequent in women versus men.
- The possible protective role of IFN-λ1(IL-29) and GM-CSF warrant further studies.
Reference:
- Buergin N, Lopez-Ayala P, Hirsiger JR, Mueller P, Median D, Glarner N, Rumora K, Herrmann T, Koechlin L, Haaf P, Rentsch K, Battegay M, Banderet F, Berger CT, Mueller C. Sex-specific differences in myocardial injury incidence after COVID-19 mRNA-1273 Booster Vaccination. Eur J Heart Fail. 2023 Jul 20. doi: 10.1002/ejhf.2978. Epub ahead of print. PMID: 37470105.
- https://onlinelibrary.wiley.com/doi/abs/10.1002/ejhf.2978
Study: Aerobic exercises recommendations and specifications for patients with COVID-19: a systematic review
Objective:
- This review was conducted to systematically analyze the effects of aerobic exercise on immunological biomarkers to provide safe aerobic exercise recommendations and specifications for patients with COVID-19.
Materials and methods:
- A systematic search was conducted through MEDLINE (PubMed), Science Direct, Web of Science, Scopus, Cochrane Library, and SciELO databases. The search included the following keywords "immune system", "immune cell", or "immune function"; "aerobic training", "aerobic exercise", or "physical activity"; "human" or "adult"; and "cytokine", "killer cell", "T cell", "interleukin", "lymphocyte", "leukocyte" or "adhesion molecule".
Results:
- Eleven studies met the inclusion and exclusion criteria of this search.
- The most used exercise prescriptions included walking, cycling, or running. The duration of exercise ranged from 18 to 60 min with an intensity of 55% to 80% of VO2max or 60%-80% of maximum heart rate. The frequency range was 1 to 3 times/week.
- The mainly increased immunological biomarkers included leukocytes, lymphocytes, neutrophils, monocytes, eosinophils, IL-6, CD16-56, CD16, CD4, CD3, CD8, and CD19.
Conclusions:
- This review demonstrated that patients with COVID-19 should follow a regular program of aerobic exercise for 20-60 min.
- This program should be in the form of cycling or walking with an intensity of 55%-80% VO2max or 60%-80% of maximum heart rate. (Zone 2)
- This program should be repeated 2-3 sessions/week.
- These previous parameters could safely enhance immune functions without producing any exhaustion.
Refereence:
- Alawna M, Amro M, Mohamed AA. Aerobic exercises recommendations and specifications for patients with COVID-19: a systematic review. Eur Rev Med Pharmacol Sci. 2020 Dec;24(24):13049-13055. doi: 10.26355/eurrev20201224211. PMID: 33378057.
- https://pubmed.ncbi.nlm.nih.gov/33378057/
Study: Association between vitamin D supplementation and COVID-19 infection and mortality edit
In the population of US veterans, we show that Vitamin D2 and D3 fills were associated with:
- Reductions in COVID-19 infection of 28% and 20%, respectively [(D3 Hazard Ratio (HR) = 0.80, [95% CI 0.77, 0.83]), D2 HR = 0.72, [95% CI 0.65, 0.79]].
- Mortality within 30-days of COVID-19 infection was similarly 33% lower with Vitamin D3 and 25% lower with D2 (D3 HR = 0.67, [95% CI 0.59, 0.75]; D2 HR = 0.75, [95% CI 0.55, 1.04]).
- After controlling for vitamin D blood levels, veterans receiving higher dosages of Vitamin D obtained greater benefits from supplementation than veterans receiving lower dosages. Veterans with Vitamin D blood levels between 0 and 19 ng/ml exhibited the largest decrease in COVID-19 infection following supplementation.
- Black veterans received greater associated COVID-19 risk reductions with supplementation than White veterans.
As a safe, widely available, and affordable treatment, Vitamin D may help to reduce the severity of the COVID-19 pandemic.
Reference:
- Gibbons, J.B., Norton, E.C., McCullough, J.S. et al. Association between vitamin D supplementation and COVID-19 infection and mortality. Sci Rep 12, 19397 (2022). https://doi.org/10.1038/s41598-022-24053-4
Study: IgG4 Antibodies Induced by Repeated Vaccination May Generate Immune Tolerance to the SARS-CoV-2 Spike Protein
Less than a year after the global emergence of the coronavirus SARS-CoV-2, a novel vaccine platform based on mRNA technology was introduced to the market. Globally, around 13.38 billion COVID-19 vaccine doses of diverse platforms have been administered. To date, 72.3% of the total population has been injected at least once with a COVID-19 vaccine.
As the immunity provided by these vaccines rapidly wanes, their ability to prevent hospitalization and severe disease in individuals with comorbidities has recently been questioned, and increasing evidence has shown that, as with many other vaccines,
- they do not produce sterilizing immunity, allowing people to suffer frequent re-infections.
- Additionally, recent investigations have found abnormally high levels of IgG4 in people who were administered two or more injections of the mRNA vaccines.
HIV, Malaria, and Pertussis vaccines have also been reported to induce higher-than-normal IgG4 synthesis.
Overall, there are three critical factors determining the class switch to IgG4 antibodies:
- excessive antigen concentration
- repeated vaccination
- the type of vaccine used
It has been suggested that an increase in IgG4 levels could have a protecting role by preventing immune over-activation, similar to that occurring during successful allergen-specific immunotherapy by inhibiting IgE-induced effects.
However, emerging evidence suggests that the reported increase in IgG4 levels detected after repeated vaccination with the mRNA vaccines may not be a protective mechanism; rather, it constitutes an immune tolerance mechanism to the spike protein that could promote unopposed SARS-CoV2 infection and replication by suppressing natural antiviral responses.
Increased IgG4 synthesis due to repeated mRNA vaccination with high antigen concentrations may also, in susceptible individuals:
- Cause autoimmune diseases
- P romote cancer growth
- Autoimmune myocarditis
Reference:
- Uversky VN, Redwan EM, Makis W, Rubio-Casillas A. IgG4 Antibodies Induced by Repeated Vaccination May Generate Immune Tolerance to the SARS-CoV-2 Spike Protein. Vaccines. 2023; 11(5):991. https://doi.org/10.3390/vaccines11050991
- https://www.mdpi.com/2076-393X/11/5/991
Study: Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting
Background
- Preapproval trials showed that messenger RNA (mRNA)–based vaccines against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) had a good safety profile, yet these trials were subject to size and patient-mix limitations. An evaluation of the safety of the BNT162b2 mRNA vaccine with respect to a broad range of potential adverse events is needed.
Methods
- We used data from the largest health care organization in Israel to evaluate the safety of the BNT162b2 mRNA vaccine.
- For each potential adverse event, in a population of persons with no previous diagnosis of that event, we individually matched vaccinated persons to unvaccinated persons according to sociodemographic and clinical variables. Risk ratios and risk differences at 42 days after vaccination were derived with the use of the Kaplan–Meier estimator.
- To place these results in context, we performed a similar analysis involving SARS-CoV-2–infected persons matched to uninfected persons. The same adverse events were studied in the vaccination and SARS-CoV-2 infection analyses.
Results
- In the vaccination analysis, the vaccinated and control groups each included a mean of 884,828 persons.
- Vaccination was most strongly associated with an elevated risk of:
- myocarditis (risk ratio, 3.24; 95% confidence interval [CI], 1.55 to 12.44; risk difference, 2.7 events per 100,000 persons; 95% CI, 1.0 to 4.6)
- lymphadenopathy (risk ratio, 2.43; 95% CI, 2.05 to 2.78; risk difference, 78.4 events per 100,000 persons; 95% CI, 64.1 to 89.3),
- appendicitis (risk ratio, 1.40; 95% CI, 1.02 to 2.01; risk difference, 5.0 events per 100,000 persons; 95% CI, 0.3 to 9.9)
- herpes zoster infection (risk ratio, 1.43; 95% CI, 1.20 to 1.73; risk difference, 15.8 events per 100,000 persons; 95% CI, 8.2 to 24.2).
- SARS-CoV-2 infection was associated with a substantially increased risk of:
- myocarditis (risk ratio, 18.28; 95% CI, 3.95 to 25.12; risk difference, 11.0 events per 100,000 persons; 95% CI, 5.6 to 15.8)
- Additional serious adverse events, including:
- pericarditis
- arrhythmia
- deep-vein thrombosis
- pulmonary embolism
- myocardial infarction
- intracranial hemorrhage
- thrombocytopenia
Conclusions
- In this study in a nationwide mass vaccination setting, the BNT162b2 vaccine was not associated with an elevated risk of most of the adverse events examined.
- The vaccine was associated with an excess risk of myocarditis (1 to 5 events per 100,000 persons).
- The risk of this potentially serious adverse event and of many other serious adverse events was substantially increased after SARS-CoV-2 infection. (Funded by the Ivan and Francesca Berkowitz Family Living Laboratory Collaboration at Harvard Medical School and Clalit Research Institute.)
References:
- Barda N, Dagan N, Ben-Shlomo Y, et al. Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting. N Engl J Med. 2021;385(12):1078-1090. https://doi.org/10.1056/NEJMoa2110475
- https://www.nejm.org/doi/10.1056/NEJMoa2110475
- Critique
The entire vaccinated group must be compared with the entire unvaccinated group in investigations of serious symptoms and injuries that occurred after vaccination or after infection.
The comparison chosen was one where they looked at the risks of various serious symptoms and injuries after covid vaccination vs the risks of the corresponding ailments after infection in the unvaccinated – instead of looking at the corresponding risks for the entire unvaccinated group. This meant that the researchers obtained higher risk figures for the option "to abstain from the vaccine" than for the option "to take the vaccine." In addition, they'd chosen to look at the risks after confirmed infection instead of after estimated, which yielded an even smaller denominator in the division.
The authors consider the comparison between vaccinated and infected unvaccinated to be acceptable.
When I then looked at the results of the studies and used official statistics to make a correct comparison instead, I found they showed that the risk of serious symptoms and injuries after vaccination was many times higher than the risk of corresponding infection-related conditions in the unvaccinated state. In total, the risk of serious conditions after vaccination was about 13 times higher than if one abstained from the vaccine, according to this data.
The reason that the adequate comparison is between the risk of afflictions after vaccination and the risk of corresponding afflictions in the unvaccinated state is that the alternative to taking a vaccine isn't to contract the infection, but to be unvaccinated and thus perhaps contract the infection, perhaps not.
For the unvaccinated, the risk of ingesting viral RNA/DNA isn't 100 percent, as with vaccination, but very much lower; for covid, the risk has varied between about 0.5 and 15 percent, depending on where on the globe one was located and during what time period one was there.
From: https://brownstone.org/articles/comparing-risks-the-right-and-wrong-way/
Study: Exercise May Improve Fatigue Associated With Long COVID in Active Young Adults
Long COVID-19-related changes in physiology includes alterations in performing muscle work as fatigue. Data available do not allow us to define the usefulness of physical activity to attenuate long COVID-19 functional modifications.
The present observational study investigates the effects of physical activity on the perception of fatigue, maximum power output, sleep, and cognitive modifications in subjects affected by long COVID-19, distinguishing between active and sedentary subjects.
The data demonstrated the following:
- the perception of fatigue 1 year after the end of virus positivity was significantly reduced with respect to that observed after 6 months by more than 50% more in active subjects compared to sedentary ones
- 6 months after the end of virus positivity, the force developed by active subjects was reduced (RM factor: p < 0.001, η2p = 0.527, post hoc: p < 0.001), but the reduction was more pronounced in sedentary ones (mean difference = 38.499 W)
- poor sleep quality and mild cognitive impairment were assessed in both active and sedentary subjects.
In conclusion, the study suggests that the long COVID-19 fatigue was lower in active subjects respect to sedentary ones. A comparative analysis performed due to the overlap of functional alterations between long COVID-19 and ME/CFS showed that in a small percentage of the enrolled subjects (8%), the symptomatology reflected that of ME/CFS and was independent of the individual physical capacities.
Reference:
- Coscia F, Mancinelli R, Gigliotti PV, Checcaglini F, Fanò-Illic G. Physical Activity Effects on Muscle Fatigue in Sport in Active Adults with Long COVID-19: An Observational Study. Diagnostics. 2023; 13(7):1336. https://doi.org/10.3390/diagnostics13071336
- https://www.mdpi.com/2075-4418/13/7/1336
Study: Surveillance of COVID-19 vaccine safety among elderly persons aged 65 years and older (Temporal association with PE, AMI, DIC, and ITP)
- Background
- Monitoring safety outcomes following COVID-19 vaccination is critical for understanding vaccine safety especially when used in key populations such as elderly persons age 65 years and older who can benefit greatly from vaccination.
- Methods
- We evaluated 14 outcomes of interest following COVID-19 vaccination using the US Centers for Medicare & Medicaid Services (CMS) data covering 30,712,101 elderly persons.
- The CMS data from December 11, 2020 through Jan 15, 2022 included 17,411,342 COVID-19 vaccinees who received a total of 34,639,937 doses.
- We conducted weekly sequential testing and generated rate ratios (RR) of observed outcome rates compared to historical (or expected) rates prior to COVID-19 vaccination.
- Findings
- Four outcomes met the threshold for a statistical signal following BNT162b2 vaccination including:
- pulmonary embolism (PE; RR = 1.54)
- acute myocardial infarction (AMI; RR = 1.42)
- disseminated intravascular coagulation (DIC; RR = 1.91)
- immune thrombocytopenia (ITP; RR = 1.44).
- After further evaluation, only the RR for PE still met the statistical threshold for a signal; however, the RRs for AMI, DIC, and ITP no longer did. No statistical signals were identified following vaccination with either the mRNA-1273 or Ad26 COV2.S vaccines.
- Four outcomes met the threshold for a statistical signal following BNT162b2 vaccination including:
- Interpretation
- This early warning system is the first to identify temporal associations for PE, AMI, DIC, and ITP following BNT162b2 vaccination in the elderly.
- Because an early warning system does not prove that the vaccines cause these outcomes, more robust epidemiologic studies with adjustment for confounding, including age and nursing home residency, are underway to further evaluate these signals.
- FDA strongly believes the potential benefits of COVID-19 vaccination outweigh the potential risks of COVID-19 infection.
Reference:
- Wong HL, Tworkoski E, Ke Zhou C, Hu M, Thompson D, Lufkin B, Do R, Feinberg L, Chillarige Y, Dimova R, Lloyd PC, MaCurdy T, Forshee RA, Kelman JA, Shoaibi A, Anderson SA. Surveillance of COVID-19 vaccine safety among elderly persons aged 65 years and older. Vaccine. 2022 Dec 1:S0264-410X(22)01493-1. doi: 10.1016/j.vaccine.2022.11.069. Epub ahead of print. PMID: 36496287; PMCID: PMC9712075.
- https://www.sciencedirect.com/science/article/pii/S0264410X22014931
Study: Fenofibrate
Fenofibrate dramatically reduces symptoms of COVID-19.
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) pandemic has caused a significant number of fatalities and worldwide disruption. To identify drugs to repurpose to treat SARS-CoV-2 infections, we established a screen to measure the dimerization of angiotensin-converting enzyme 2 (ACE2), the primary receptor for the virus. This screen identified fenofibric acid, the active metabolite of fenofibrate. Fenofibric acid also destabilized the receptor-binding domain (RBD) of the viral spike protein and inhibited RBD binding to ACE2 in enzyme-linked immunosorbent assay (ELISA) and whole cell-binding assays. Fenofibrate and fenofibric acid were tested by two independent laboratories measuring infection of cultured Vero cells using two different SARS-CoV-2 isolates. In both settings at drug concentrations, which are clinically achievable, fenofibrate and fenofibric acid reduced viral infection by up to 70%. Together with its extensive history of clinical use and its relatively good safety profile, this study identifies fenofibrate as a potential therapeutic agent requiring an urgent clinical evaluation to treat SARS-CoV-2 infection.
Reference:
- Davies Scott P., Mycroft-West Courtney J., Pagani Isabel, Hill Harriet J., Chen Yen-Hsi, Karlsson Richard, Bagdonaite Ieva, Guimond Scott E., Stamataki Zania, De Lima Marcelo Andrade, Turnbull Jeremy E., Yang Zhang, Vicenzi Elisa, Skidmore Mark A., Khanim Farhat L., Richardson Alan. The Hyperlipidaemic Drug Fenofibrate Significantly Reduces Infection by SARS-CoV-2 in Cell Culture Models. Frontiers in Pharmacology, Vol 12, 2021 DOI: 10.3389/fphar.2021.660490
Study: Outcomes after early treatment with hydroxychloroquine and azithromycin: An analysis of a database of 30,423 COVID-19 patients
Background
- Many studies have evaluated the use of hydroxychloroquine in COVID-19. Most retrospective observational studies demonstrate a benefit of using HCQ on mortality, but not most randomized clinical trials.
Methods
- We analyzed raw data collected from a cohort of 30,423 patients with COVID-19 cared for at IHU Méditerranée Infection in Marseille France and extracted from the DRYAD open data platform. We performed univariate and multivariable logistic regressions with all-cause mortality within six weeks. Multivariable logistic regressions were adjusted for sex, age group (<50, 50–69, 70–89 and > 89 years), periods (or variants), and type of patient management.
Results
- Among 30,202 patients for whom information on treatment was available, 191/23,172 (0.82%) patients treated with HCQ-AZ died, compared to 344/7030 (4.89%) who did not receive treatment with HCQ-AZ.
- HCQ-AZ therapy was associated with a lower mortality than treatment without HCQ-AZ (odds ratio (OR) 0.16; 95% confidence interval (CI), 0.14–0.19).
- After adjustment for sex, age, period, and patient management, HCQ-AZ was associated with a significantly lower mortality rate (adjusted OR (aOR) 0.55, 95% CI 0.45–0.68).
- On a subsample of 21,664 patients with available variant information, results remained robust after adjustment on sex, age, patient management and variant (aOR 0.55; 95% CI 0.44–0.69).
- On a subsample of 16,063 patients, HCQ-AZ was still associated with a significantly lower mortality rate (aOR 0.47, 95%CI 0.29–0.75) after adjustment for sex, age, period, patient management, vaccination status and comorbidities.
Conclusion
- Analysis of this large online database showed that HCQ-AZ was consistently associated with the lowest mortality.
My calculations:
- Patient Expected Event Rate: 4.89 %
- Absolute Risk Reduction (95% CI)
- -0.041 (-0.046 to -0.036)
- Relative Risk Reduction (95% CI)
- -0.832 (0.141 to 0.200)
- Number Needed to Treat
- -24.4
- Odds Ratio
- 0.162
- Relative Risk
- 0.168
Reference:
- Philippe Brouqui, Matthieu Million, Philippe Parola, Peter A. Mccullough, Didier Raoult, Outcomes after early treatment with hydroxychloroquine and azithromycin: An analysis of a database of 30,423 COVID-19 patients, New Microbes and New Infections, Volume 55, 2023, 101188, ISSN 2052-2975, https://doi.org/10.1016/j.nmni.2023.101188.
- https://www.sciencedirect.com/science/article/pii/S2052297523001075?via%3Dihub
Study: The role of COVID-19 vaccines in preventing post-COVID-19 thromboembolic and cardiovascular complications edit
Objective:
- To study the association between COVID-19 vaccination and the risk of post-COVID-19 cardiac and thromboembolic complications.
Methods
- We conducted a staggered cohort study based on national vaccination campaigns using electronic health records from the UK, Spain and Estonia. Vaccine rollout was grouped into four stages with predefined enrolment periods. Each stage included all individuals eligible for vaccination, with no previous SARS-CoV-2 infection or COVID-19 vaccine at the start date. Vaccination status was used as a time-varying exposure. Outcomes included heart failure (HF), venous thromboembolism (VTE) and arterial thrombosis/thromboembolism (ATE) recorded in four time windows after SARS-CoV-2 infection: 0–30, 31–90, 91–180 and 181–365 days. Propensity score overlap weighting and empirical calibration were used to minimise observed and unobserved confounding, respectively.
- Fine-Gray models estimated subdistribution hazard ratios (sHR). Random effect meta-analyses were conducted across staggered cohorts and databases.
Results
- The study included 10.17 million vaccinated and 10.39 million unvaccinated people. Vaccination was associated with reduced risks of acute (30-day) and post-acute COVID-19 VTE, ATE and HF: for example, meta-analytic sHR of 0.22 (95% CI 0.17 to 0.29), 0.53 (0.44 to 0.63) and 0.45 (0.38 to 0.53), respectively, for 0–30 days after SARS-CoV-2 infection, while in the 91–180 days sHR were 0.53 (0.40 to 0.70), 0.72 (0.58 to 0.88) and 0.61 (0.51 to 0.73), respectively.
Conclusions
- COVID-19 vaccination reduced the risk of post-COVID-19 cardiac and thromboembolic outcomes. These effects were more pronounced for acute COVID-19 outcomes, consistent with known reductions in disease severity following breakthrough versus unvaccinated SARS-CoV-2 infection.
Reference:
- Mercadé-Besora N, Li X, Kolde R, Trinh NT, Sanchez-Santos MT, Man WY, Roel E, Reyes C, Delmestri A, Nordeng HME, Uusküla A, Duarte-Salles T, Prats C, Prieto-Alhambra D, Jödicke AM, Català M. The role of COVID-19 vaccines in preventing post-COVID-19 thromboembolic and cardiovascular complications. Heart. 2024 Mar 12:heartjnl-2023-323483. doi: 10.1136/heartjnl-2023-323483. Epub ahead of print. PMID: 38471729.
- https://heart.bmj.com/content/early/2024/01/24/heartjnl-2023-323483
Study: Analysis of the Association Between BNT162b2 mRNA COVID-19 Vaccination and Deaths Within 10 Days After Vaccination Using the Sex Ratio in Japan edit
Introduction:
- The association between coronavirus disease 2019 (COVID-19) vaccinations and deaths after vaccination has been investigated primarily through cohort and self-controlled case series studies. In the present study, the sex ratios of reported deaths were compared by period.
Methods:
- Descriptive analysis was conducted using data on deaths reported after vaccination with the BNT162b2 mRNA vaccine. The data used were published by the Ministry of Health, Labour and Welfare in Japan.
- The risk period was defined as within 10 days of vaccination, and the control period was defined as 11 to 180 days after vaccination.
- Sex ratios were calculated for all-cause deaths and each outcome by dividing the number of males by that of females and multiplying by 100.
- Fisher's exact test was performed to analyze the results. Graphs were created to show the number of days from vaccination to death and that of reported deaths.
Results:
- For all-cause deaths among individuals aged ≥65 years, the sex ratio during the risk period was 92, significantly lower than that during the control period (130) (p=0.0050).
- Conversely, for all-cause deaths among those aged ≤64 years, the sex ratio during the risk period was 204, significantly higher than that during the control period (111) (p=0.044).
- Reported deaths were concentrated during the risk period in both groups.
- Sex ratios by period for each outcome were also examined. However, the differences were not significant across any of the outcomes.
Conclusion:
- The results indicate that the BNT162b2 mRNA vaccination may influence the occurrence of death during the risk period.
- In a cohort study in Japan, there was no significant increase in all-cause mortality owing to vaccination.
- This does not contradict the results of the present study. The results of a cohort study provide support for vaccine safety.
- However, this does not indicate that vaccine-related deaths are nonexistent; it only indicates that their number is not large enough to make a significant difference.
- Japan has relief services for adverse health effects that provide financial support to patients. On this occasion, it is difficult to determine whether a postvaccination death is incidental or vaccine-related. A self-controlled risk interval design and a comparison of sex ratios by period may be useful in examining the association between vaccination and deaths after vaccination when a cohort study does not detect a significant difference due to a low mortality rate. The latter approach may be particularly useful for analyzing data with reporting bias. The author believes that this approach may not provide conclusive evidence, but it can offer valuable insights into assessing vaccine safety.
Reference:
- Suzumura Y (December 07, 2023) Analysis of the Association Between BNT162b2 mRNA COVID-19 Vaccination and Deaths Within 10 Days After Vaccination Using the Sex Ratio in Japan. Cureus 15(12): e50144. https://doi.org/10.7759/cureus.50144
- https://www.cureus.com/articles/199892-analysis-of-the-association-between-bnt162b2-mrna-covid-19-vaccination-and-deaths-within-10-days-after-vaccination-using-the-sex-ratio-in-japan#!/
Study: OpenSAFELY: Effectiveness of COVID-19 vaccination in children and adolescents
Background
- Children and adolescents in England were offered BNT162b2 as part of the national COVID-19 vaccine roll out from September 2021. We assessed the safety and effectiveness of first and second dose BNT162b2 COVID-19 vaccination in children and adolescents in England.
Methods
- With the approval of NHS England, we conducted an observational study in the OpenSAFELY-TPP database, including a) adolescents aged 12-15 years, and b) children aged 5-11 years and comparing individuals receiving i) first vaccination with unvaccinated controls and ii) second vaccination to single-vaccinated controls.
- We matched vaccinated individuals with controls on age, sex, region, and other important characteristics. Outcomes were positive SARS-CoV-2 test (adolescents only); COVID-19 Attendances and Emergency Admissions (A&E attendance); COVID-19 hospitalisation; COVID-19 critical care admission; COVID-19 death, with non-COVID-19 death and fractures as negative control outcomes and A&E attendance, unplanned hospitalisation, pericarditis, and myocarditis as safety outcomes.
Results
- Amongst 820,926 previously unvaccinated adolescents, the incidence rate ratio (IRR) for positive SARS-CoV-2 test comparing vaccination with no vaccination was 0.74 (95% CI 0.72-0.75), although the 20-week risks were similar.
- The IRRs were 0.60 (0.37-0.97) for COVID-19 A&E attendance
- 0.58 (0.38-0.89) for COVID-19 hospitalisation
- 0.99 (0.93-1.06) for fractures
- 0.89 (0.87-0.91) for A&E attendances
- 0.88 (0.81-0.95) for unplanned hospitalisation
- Amongst 441,858 adolescents who had received first vaccination IRRs comparing second dose with first dose only were 0.67 (0.65-0.69) for positive SARS-CoV-2 test
- 1.00 (0.20-4.96) for COVID-19 A&E attendance
- 0.60 (0.26-1.37) for COVID-19 hospitalisation
- 0.94 (0.84-1.05) for fractures
- 0.93 (0.89-0.98) for A&E attendance
- 0.99 (0.86-1.13) for unplanned hospitalisation
- Amongst 283,422 previously unvaccinated children and 132,462 children who had received a first vaccine dose, COVID-19-related outcomes were too rare to allow IRRs to be estimated precisely. A&E attendance and unplanned hospitalisation were slightly higher after first vaccination (IRRs versus no vaccination 1.05 (1.01-1.10) and 1.10 (0.95-1.26) respectively) but slightly lower after second vaccination (IRRs versus first dose 0.95 (0.86-1.05) and 0.78 (0.56-1.08) respectively).
- There were no COVID-19-related deaths in any group.
- Fewer than seven (exact number redacted) COVID-19-related critical care admissions occurred in the adolescent first dose vs unvaccinated cohort.
- Among both adolescents and children, myocarditis and pericarditis were documented only in the vaccinated groups, with rates of 27 and 10 cases/million after first and second doses respectively.
Conclusion
- BNT162b2 vaccination in adolescents reduced COVID-19 A&E attendance and hospitalisation, although these outcomes were rare.
- Protection against positive SARS-CoV-2 tests was transient.
Reference:
- Colm D Andrews, Edward P K Parker, Elsie Horne, Venexia Walker, Tom Palmer, Andrea L Schaffer, Amelia CA Green, Helen J Curtis, Alex J Walker, Lucy Bridges, Christopher Wood, Victoria Speed, Christopher Bates, Jonathan Cockburn, John Parry, Amir Mehrkar, Brian MacKenna, Sebastian CJ Bacon, Ben Goldacre, Miguel A Hernan, Jonathan AC Sterne, The OpenSAFELY Collaborative, William J Hulme. OpenSAFELY: Effectiveness of COVID-19 vaccination in children and adolescents. medRxiv 2024.05.20.24306810; doi: https://doi.org/10.1101/2024.05.20.24306810
- https://www.medrxiv.org/content/10.1101/2024.05.20.24306810v1
Study: An analysis of studies pertaining to masks in Morbidity and Mortality Weekly Report: Characteristics and quality of all studies from 1978 to 2023 edit
Importance
- Because the MMWR has substantial influence on United States public health policy and is not externally peer-reviewed, it is critical to understand the scientific process within the journal.
- Mask policies during COVID is one topic that has been highly influenced by data published in the MMWR.
Objective
- To describe and evaluate the nature and methodology of the reports and appropriateness of conclusions in MMWR pertaining to masks.
Design, Setting and Participants
- Retrospective cross-sectional study of MMWR publications pertaining to masks from 1978 to 2023.
Main outcome measures
- Study date, design, disease focus, setting, population and location. Whether the study was able to assess mask effectiveness, if results were statistically significant, if masks were concluded to be effective, if randomized evidence and/or conflicting data was mentioned or cited, if causal statements were made about effectiveness, and, if so, whether they were appropriate.
Results
- 77 studies, all published after 2019, met our inclusion criteria.
- 75/77 (97.4%) studies were from the United States alone. All geographic regions and age groups were represented.
- The most common study design was observational without a comparator group 22/77 (28.6%).
- The most common setting was the community (35/77;45.5%). 0/77 were randomized studies. 23/77 (29.9%) assessed mask effectiveness, with 11/77 (14.3%) being statistically significant, but 58/77 (75.3%) stated masks were effective. Of these, 41/58 (70.7%) used causal language.
- Only one mannequin study used causal language appropriately (1.3%). 72/77 (93.5%) pertained to SARS-CoV-2 alone. None cited randomized data. 1/77 (1.3%) cited conflicting evidence.
Conclusions and Relevance
- MMWR publications pertaining to masks drew positive conclusions about mask effectiveness over 75% of the time despite only 30% testing masks and <15% having statistically significant results.
- No studies were randomized, yet over half drew causal conclusions.
- The level of evidence generated was low and the conclusions drawn were most often unsupported by the data.
- Our findings raise concern about the reliability of the journal for informing health policy.
Reference:
- Tracy Beth Høeg, Alyson Haslam, Vinay Prasad. An analysis of studies pertaining to masks in Morbidity and Mortality Weekly Report: Characteristics and quality of all studies from 1978 to 2023. medRxiv 2023.07.07.23292338; doi: https://doi.org/10.1101/2023.07.07.23292338
- https://www.medrxiv.org/content/10.1101/2023.07.07.23292338v1
Study: A Critical Analysis of All-Cause Deaths during COVID-19 Vaccination in an Italian Province
Immortal time bias (ITB) is common in cohort studies and distorts the association estimates between the treated and untreated. We used data from an Italian study on COVID-19 vaccine effectiveness, with a large cohort, long follow-up, and adjustment for confounding factors, affected by ITB, with the aim to verify the real impact of the vaccination campaign by comparing the risk of all-cause death between the vaccinated population and the unvaccinated population.
We aligned all subjects on a single index date and considered the "all-cause deaths" outcome to compare the survival distributions of the unvaccinated group versus various vaccination statuses.
Results:
- The all-cause death hazard ratios in univariate analysis for vaccinated people with 1, 2, and 3/4 doses versus unvaccinated people were 0.88, 1.23, and 1.21, respectively.
- The multivariate values were 2.40, 1.98, and 0.99.
Possible explanations of this trend of the hazard ratios as vaccinations increase could be a harvesting effect; a calendar-time bias, accounting for seasonality and pandemic waves; a case- counting window bias; a healthy-vaccinee bias; or some combination of these factors.
With 2 and even with 3/4 doses, the calculated Restricted Mean Survival Time and Restricted Mean Time Lost have shown a small but significant downside for the vaccinated populations.
Reference:
- Alessandria M, Malatesta GM, Berrino F, Donzelli A. A Critical Analysis of All-Cause Deaths during COVID-19 Vaccination in an Italian Province. Microorganisms. 2024; 12(7):1343. https://doi.org/10.3390/microorganisms12071343
Study: Post Conditional Approval Active Surveillance Study Among Individuals in Europe Receiving the Pfizer-BioNTech Coronavirus Disease 2019 (COVID-19) Vaccine
BLUF:
| Condition | Hazard Ratio (95% CI) |
|---|---|
| Acute Cardiovascular Injury | 1.23 (1.18, 1.27) |
| Arrhythmia | 1.27 (1.21, 1.33) |
| Heart Failure | 1.02 (0.95, 1.09) |
| Stress Cardiomyopathy | 1.30 (0.53, 3.20) |
| Coronary Artery Disease | 1.40 (1.30, 1.50) |
| Myocarditis | 2.30 (0.94, 5.66) |
| Cerebral Venous Sinus Thrombosis (CVST) | 0.43 (0.14, 1.27) |
| Secondary Amenorrhoea | 1.24 (1.17, 1.30) |
| Bell'S Palsy | 0.99 (0.75, 1.29) |
| Glomerulonephritis | 0.88 (0.67, 1.16) |
Notes:
- A Hazard Ratio of 1.23 means that the condition is 23% more likely in the vaccinated cohort, and "CI" mean confidence interval, i.e., we can be 95% confident that the 'true' number lies between the following two numbers. So those data are extremely worrying. This is the manufacturer bearing out the numerous anecdotal reports of increasing heart issues since 2020 as well as various independent research reports.
- None of the above can be attributed to Covid itself: the exposure to Covid will be broadly the same in both the vaccinated and unvaccinated cohorts, which comprise millions of individual patients.
—
Pfizer's report C4591021 'Interim Report 5' dated March 12th 2024
- Rationale and background: The Pfizer-BioNTech COVID-19 vaccine, tozinameran (Comirnaty®), a novel mRNA-based vaccine, has been authorised for use in several countries including the United States and European Union, for the prevention of COVID-19. Efficient and timely monitoring of the safety of the vaccine is needed. The overall goal of the study is to determine whether an increased risk of prespecified adverse events of special interest (AESIs) exists following the administration of at least one dose of the Pfizer- BioNTech COVID-19 vaccine. This non-interventional study is designated as a Post- Authorization Safety Study (PASS) and is a commitment to the EMA and a Postmarketing Requirement to the Food and Drug Administration (FDA).
- Research question and objectives: To determine if there is an increased risk of prespecified AESI following the administration of at least one dose of the Pfizer-BioNTech COVID-19 vaccine.
- Study design: This post-authorisation active surveillance study of AESIs following administration of the Pfizer-BioNTech COVID-19 vaccine used a retrospective cohort design comparing the risk in vaccinated and unvaccinated individuals matched by the date of vaccination with data from multiple databases. Additional control for confounding was conducted using propensity score (PS) adjustment. In the final report, comparison with historical controls and a self-controlled risk interval (SCRI) design will also be used.
- Setting: Data were available from six electronic healthcare data sources in Europe for the objectives of the fifth interim report: Pedianet, IT; PHARMO Institute for Drug Outcomes Research (PHARMO), NL; University of Oslo - Norwegian Health Registries (NHR), NO; EpiChron Research Group on Chronic Diseases at the Aragon Health Sciences Institute (EpiChron), ES; Sistema d'Informació per el Desenvolupament de la Investigació en Atenció Primària (SIDIAP), ES and CPRD (Clinical Practice Research Datalink) Aurum (UK). As per protocol the study originally included two additional electronic healthcare data sources who could not contribute data for the fifth interim report. These were ARS Toscana (Agenzia Regionale di Sanita' della Toscana), a research institute in the Tuscany region of Italy, IT), and Health Search Database (HSD), IT.
- Participating data sources: The source population was all individuals registered in the electronic healthcare data sources listed below. The study period included the following calendar time for:
- Pedianet (family paediatrician diagnoses) between 31 May 2021 and 31 December 2022
- PHARMO (general practitioner diagnoses and inpatient diagnoses) between 6 January 2021 and 30 June 2023 (and 6 January 2021 and 31 December 2022 for inpatient data)
- NHR (general practice and outpatient specialist diagnoses) between 1 January 2021 and 31 December 2022
- EpiChron (general practice and inpatient diagnoses) between 27 December 2020 and 31 July 2023
- SIDIAP (general practice and inpatient diagnoses) between 1 January 2021 and 30 June 2023
- CPRD Aurum (general practice and inpatient diagnoses) between 8 December 2020 and 21 March 2022)
- Variables and data sources: Exposure was based on recorded prescription, dispensing, or administration of the Pfizer-BioNTech COVID-19 vaccine. Outcomes were identified in the data sources with algorithms based on codes for diagnoses and free text. The selected adverse events of special interest (AESIs) were based initially on the ACCESS project but the list has been extended with new AESIs and the code lists have been reviewed and tagged as narrow and possible codes on the descendant code level.
Results: Data for 17,677,132 individuals who had received ≥1 dose of Pfizer-BioNTech COVID-19 vaccine and satisfied the inclusion criteria were included in the non-matched vaccinated cohort from Italy (Pedianet: 0.08%), the Netherlands (PHARMO: 8.65%), Norway (NHR: 27.44%), Spain (EpiChron: 5.83%; and SIDIAP: 24.50%) and the UK (CPRD Aurum: 32.50%). This is an increase of 9,537,893 individuals compared with interim report 4, mainly due to the inclusion of data from CPRD Aurum.
A total of 10,665,306 (84.6%) individuals received a second dose, 4,642,445 (36.8%) received a third dose, 1,021,555 (8.1%) received a fourth dose and 7,801 (0.1%) a fifth dose of the Pfizer-BioNTech COVID-19 vaccine. Among these individuals 12,400,847 (98.32%) were matched with an unvaccinated individual.
A total of 26,980 pregnant women who had received at least one dose of the Pfizer- BioNTech COVID-19 vaccine were included of whom 9,234 (34.23%) received the dose during their first trimester of pregnancy and 9,763 (36.19%) in their second trimester. Pregnancy data were not available from PHARMO or CPRD for this report, but they are expected to be available for the final report. To assess baseline exchangeability of the comparator cohorts, the incidences of COVID-19 in the first 12 days after vaccination in the vaccinated and unvaccinated cohorts were compared. These incidences were similar, demonstrating that matching had achieved comparable cohorts. Despite the satisfactory matching process, the analyses in the matched cohorts were performed with additional control for confounding to evaluate the effect of the propensity score (PS) adjustment.
This interim report 5 provides a description of the characteristics and incidence rates of 37 AESIs in more than 12.4 million vaccinated individuals and more than 12.4 million unvaccinated controls. The incidence rates in the vaccinated and unvaccinated cohorts were similar for most of the AESIs.
The following 11 AESIs were discussed further in interim report 5 either at the request of EMA or because they were newly included for analysis as AESIs.
- For acute cardiovascular injury the adjusted HRs were 1.38 (95% CI: 0.73, 2.61) in Pedianet, 1.01 (95% CI: 0.99, 1.04) in NHR, 1.38 (95% CI: 1.31, 1.45) in PHARMO, 1.10 (95% CI: 1.03, 1.18) in EpiChron, 0.99 (95% CI: 0.96, 1.03) in SIDIAP, and 1.23 (95% CI: 1.18, 1.27) in CPRD Aurum.
- For arrhythmia the adjusted HRs were 1.75 (95% CI: 0.88, 3.49) in Pedianet, 1.03 (95% CI: 1, 1.05) in NHR, 1.36 (95% CI: 1.29, 1.44) in PHARMO, 1.12 (95% CI: 1.04, 1.21) in EpiChron, 0.99 (95% CI: 0.96, 1.03) in SIDIAP, and 1.27 (95% CI: 1.21, 1.33) in CPRD Aurum.
- For heart failure, the adjusted HRs were 0.77 (95% CI: 0.73, 0.82) in NHR, 1.29 (95% CI: 1.13, 1.47) in PHARMO, 0.90 (95% CI: 0.80, 1.01) in EpiChron, 0.89 (95% CI: 0.82, 0.96) in SIDIAP, and 1.02 (95% CI: 0.95, 1.09) in CPRD Aurum.
- For stress cardiomyopathy, the adjusted HRs were 0.69 (95% CI: 0.18, 2.67) in NHR, 1.49 (95% CI: 0.33, 6.69) in PHARMO, 0.85 (95% CI: 0.21, 3.47) in EpiChron, 1.51 (95% CI: 0.75, 3.04) in SIDIAP, 1.30 (95% CI: 0.53, 3.20) in CPRD Aurum.
- For coronary artery disease, the adjusted HRs were 0.99 (95% CI: 0.94, 1.04) in NHR, 1.49 (95% CI: 1.31, 1.69) in PHARMO, 0.97 (95% CI: 0.80, 1.17) in EpiChron, 1.00 (95% CI: 0.91, 1.10) in SIDIAP, 1.40 (95% CI: 1.30, 1.50) in CPRD Aurum.
- For myocarditis within 21 days, the adjusted HRs were 0.94 (95% CI: 0.46, 1.94) in NHR, 1.23 (95% CI: 0.13, 11.84) in PHARMO, 3.64 (95% CI: 0.41, 32.53) in EpiChron, 1.05 (95% CI: 0.35, 3.16) in SIDIAP, and 2.30 (95% CI: 0.94, 5.66) in CPRD Aurum.
- For cerebral venous sinus thrombosis (CVST), the adjusted HRs were 10.63 (95% CI: 0.23, 1.74) in NHR, 0.90 (95% CI: 0.06, 14.09) in EpiChron, 0.68 (95% CI: 0.11, 4.20) in SIDIAP, 0.43 (95% CI: 0.14, 1.27) in CPRD Aurum.
- For secondary amenorrhoea, the adjusted HRs were 0.91 (95% CI: 0.69, 1.21) in NHR, 1.71 (95% CI: 1.34, 2.18) in EpiChron, 0.99 (95% CI: 0.91, 1.07) in SIDIAP, and 1.24 (95% CI: 1.17, 1.30) in CPRD Aurum.
- For hypermenorrhoea, the adjusted HRs were 0.62 (95% CI: 0.08, 4.66) in Pedianet, 1.40 (95% CI: 1.23, 1.60) in EpiChron, and 1.02 (95% CI: 0.95, 1.09) in SIDIAP.
- For Bell's Palsy, the adjusted HRs were 1.15 (95% CI: 0.88, 1.50) in NHR, 0.65 (95% CI: 0.28, 1.51) in PHARMO, 0.84 95% CI: (95% CI: 0.34, 2.09) in EpiChron, 0.96 (95% CI: 0.75, 1.24) in SIDIAP, and 0.99 (95% CI: 0.75, 1.29) in CPRD Aurum.
- Glomerulonephritis was analysed for the first time in this fifth interim report. No events were identified in Pedianet, NHR or PHARMO. The adjusted HRs were 0.59 (0.22, 1.55) in EpiChron, 1.29 (0.88, 1.87) in SIDIAP and 0.88 (0.67, 1.16) in CPRD Aurum.
Discussion: The incidence rates for the majority of the 37 AESIs were generally very low in the risk intervals studied and were comparable with background incidence rates from previous studies (e.g., ACCESS) in unvaccinated cohorts. Among the 11 AESIs that were highlighted for further discussion, the divergence in the cumulative incidences observed for several of the cardiovascular events with long risk windows (e.g., 365 days) resulted in small increases in risk in some of the data sources. These increases could be explained by a number of factors. Some of these events may have presented with mild symptoms that did not require immediate medical attention, and vaccinated individuals may have sought medical attention more frequently than those who were unvaccinated (healthy vaccinee effect). Another plausible explanation is differences in the composition of the unvaccinated cohort as follow-up progresses. Unvaccinated individuals were censored in the unvaccinated cohort if they were vaccinated and were then followed up in the vaccinated cohort from that time point. Hence, the individuals who remained in the unvaccinated cohort were those who were never vaccinated and who were possibly less likely seek medical attention at all, if it was not urgently needed. These differences may have been minimal earlier in follow-up but may have become more pronounced as follow-up progressed.
Results for CVST, Bell's Palsy and glomerulonephritis all showed no evidence of an increased risk in the vaccinated cohort based on adjusted HRs. Adjusted HRs for secondary amenorrhoea were slightly elevated in EpiChron and CPRD Aurum. For hypermenorhoea, only the adjusted HR for EpiCrhon was slightly elevated. These events, along with the cardiovascular events described above, will continue to be monitored and further refined for inclusion in the final study report.
Reference:
Study: Postacute sequelae of SARS-CoV-2 in the population: Risk factors and vaccines
The contribution of pre-existing conditions to severe versus mild postacute sequelae (PASC) of SARS-CoV-2 in the population is lacking. Here, we evaluated reproductive and other PASC side-by-side in unvaccinated and vaccinated individuals after 1st SARS-CoV-2 infection.
In an online global survey of 7,541 individuals from 95 countries, high grade fever (> 102˚F)/ hospitalization after a first SARS-CoV-2 infection were more likely to be reported by vaccinated males than unvaccinated males (13.64% vs. 8.34%; p = 0.0483; HR = 1.63 [95% CI: 1.008, 2.65]). Women reported experiencing more frequent PASC than men. More women than men reported vaccine-associated adverse events (AEs) after the 1st dose (60.85% vs 48.79%, p < 0.01).
Vaccine-associated hospitalization was reported by 6.24% SARS-CoV-2 naïve respondents versus 1.06% of unvaccinated after 1st SARS-CoV-2 infection.
Pre-existing thyroid disease, osteoporosis, and autoimmune disorders were more prevalent in women, whereas more men reported back problems, elevated cholesterol, and hypertension; several pre-existing conditions posed ≥ 2.0 relative risk of developing severe vs mild COVID-19.
Individuals aged < 55 years had an absolute risk of 6.01%, whereas individuals ≥ 55 years had an absolute risk of 11.69% of getting severe vs mild COVID-19 disease.
Vaccinated women reported significantly greater menstrual cycle-associated reproductive PASC compared to unvaccinated women.
Vaccinated men reported hormonal changes and sexual dysfunction as reproductive PASC compared to unvaccinated men.
A detailed and thorough follow-up is needed to better understand if pre-existing health conditions and/or vaccine-associated AEs exacerbated COVID-19 sequelae.
Notes: The risk ratio (RR) for hospitalization in vaccinated COVID-naïve individuals vs. unvaccinated post-infection individuals is:
- RR = 5.89
- 95% Confidence Interval: [4.80, 7.22]
This means individuals were nearly 6 times more likely to be hospitalized after COVID vaccination than unvaccinated individuals were to be hospitalized after a COVID infection.
Reference:
- Aditi Bhargava, Sabra Inslicht. Postacute sequelae of SARS-CoV-2 in the population: Risk factors and vaccines, 17 March 2025, PREPRINT (Version 1) available at Research Square https://doi.org/10.21203/rs.3.rs-6175467/v1
Study: Rates of successful conceptions according to COVID-19 vaccination status: Data from the Czech Republic
Background
- Adverse effects of COVID-19 vaccination on human menstrual cycle characteristics have been observed, but limited data are available on the relationship between COVID-19 vaccination status and birth rates.
Objectives
- Therefore, we used nationwide data from the Czech Republic to examine rates of successful conceptions (SCs), that is, conceptions leading to live births 9 months later, for women who were either vaccinated or unvaccinated against COVID-19 before SC.
Methods
- Summary monthly COVID-19 vaccination and birth data for women in the Czech Republic aged 18–39 years were retrieved for the period from January 2021 to December 2023. The numbers of SCs per month per 1000 women were calculated for preconception-vaccinated or unvaccinated women, respectively, as well as the number of SCs per month per 1000 women for all women aged 18–39 years.
Results
- During the study period, there were approximately 1,300,000 women aged 18–39 years in the Czech Republic, and the proportion of COVID-19-vaccinated women increased from January 2021 until reaching a steady state of around 70% by the end of 2021.
- At least from June 2021, SCs per 1000 women were considerably lower for women who were vaccinated, compared to those that were unvaccinated, before SC.
- Furthermore, SC rates for the vaccinated group were much lower than expected based on their proportion of the total population.
Conclusions
- In the Czech Republic, SC rates were substantially lower for women vaccinated against COVID-19 before SC than for those who were not vaccinated. These hypothesis-generating and preliminary results call for further studies of the potential influence of COVID-19 vaccination on human fecundability and fertility.
Reference:
- Manniche V, Fürst T, Schmeling M, Gilthorpe JD, Hansen PR. Rates of successful conceptions according to COVID-19 vaccination status: Data from the Czech Republic. International Journal of Risk & Safety in Medicine. 2025;0(0). https://doi.org/10.1177/09246479251353384
Study: The impact of SARS-CoV-2 infection on vaccinated versus unvaccinated pregnant women: a retrospective cohort study
Background/objectives:
- Pregnant women were included in the COVID-19 vaccination strategy adopted in Spain in May 2021. We evaluated the obstetric and neonatal symptoms and complications presented by these first pregnant women infected with SARS-CoV-2, vaccinated and unvaccinated.
Methods:
- A retrospective observational cohort study of 156 pregnant women with a positive diagnosis of SARS-CoV-2 (infection rate of 4.2%, 156/3719 births), treated at two public hospitals in the Valencian Community (Spain) over two years (2020-2022). Of those pregnant women infected, 28.8% (45) had received at least one dose of the COVID-19 vaccine before infection. The data were obtained from the digital medical record, the Nominal Vaccination Registry (RNV), and symptom data from the Epidemiological Surveillance Application (AVE) of the CV, supervised by the epidemiology units. We analyzed the symptoms of the disease and the main obstetric and neonatal variables depending on whether or not they were vaccinated with mRNA vaccines.
Results:
- Most pregnant women were diagnosed in the third trimester of pregnancy (p = 0.003) and reported symptoms associated with the infection (73%), but vaccinated women reported all the symptoms described to a lesser extent, with headache (R1.38, 95%IC 1.15 to 1.66) and vomiting (R 1.38, 95%IC 1.15 to 1.66) statistically significant.
- All cases of pneumonia occurred in unvaccinated pregnant women who required ventilatory assistance and referral to the Intensive Care Unit.
- Pregnant women vaccinated against SARS-CoV-2 infection had lower rates of gestational pathology, milder symptoms, and fewer postpartum complications than unvaccinated women, although the small sample size did not allow for a significant difference to be seen.
- Neonatal outcomes were similar in both groups.
Conclusions:
- COVID-19 vaccination in pregnant women with at least one dose is associated with reduced symptoms, less headache and vomiting, and fewer maternal complications, including pneumonia, which did not occur in the vaccinated cohort.
- Furthermore, the Apgar score at one and five minutes is higher than 7 in children of immunized mothers. Public health strategies should promote access to vaccines during pregnancy as an urgent priority, to minimize the risk of complications from COVID-19.
Reference:
- Rodríguez-Blanco N, Sánchez-Más J, Herrero EG, Moreno PC, Gonzalez-Román MM, Duro-Torrijos JL. The impact of SARS-CoV-2 infection on vaccinated versus unvaccinated pregnant women: a retrospective cohort study. BMC Pregnancy Childbirth. 2025 Apr 30;25(1):519. doi: 10.1186/s12884-025-07630-z. PMID: 40307731; PMCID: PMC12042551.
Study: Impact of mRNA and Inactivated COVID-19 Vaccines on Ovarian Reserve
Objectives: This study aimed to elucidate the effects of messenger RNA (mRNA) and inactivated coronavirus disease 2019 (COVID-19) vaccines on ovarian histology and reserve in rats.
Methods: Thirty female Wistar albino rats, aged 16–24 weeks, were randomly divided into three groups (n = 10): control, mRNA vaccine, and inactivated vaccine groups. Each vaccine group received two doses (on day 0 and day 28) at human-equivalent doses. Four weeks post-second vaccination, ovarian tissues were harvested for analysis.
Results:
- Immunohistochemical analysis was performed to evaluate the expression of transforming growth factor beta-1 (TGF-β1), vascular endothelial growth factor (VEGF), caspase-3, and anti-Müllerian hormone (AMH) in ovarian follicles.
- Both vaccines induced significant increases in TGF-β1, VEGF, and caspase-3 expression, with more pronounced effects in the mRNA vaccine group. Conversely, AMH expression in the granulosa cells of primary, secondary, and antral follicles showed marked reductions (p < 0.001).
- The counts of primordial, primary, and secondary follicles decreased significantly in the inactivated vaccine group relative to controls and further in the mRNA vaccine group compared to the inactivated group (p < 0.001).
- Additionally, the mRNA vaccine group exhibited a decrease in antral and preovulatory follicles and an increase in atretic follicles compared to the other groups (p < 0.05).
- The serum AMH level was diminished with the mRNA vaccination in comparison with the control and inactivated groups.
Conclusions:
- Our findings suggest that both mRNA and inactivated COVID-19 vaccines may detrimentally impact ovarian reserve in rats, primarily through accelerated follicular loss and alterations in apoptotic pathways during folliculogenesis. Given these observations in a rat model, further investigations into the vaccines’ effects on human ovarian reserve are needed.
Reference:
- Karaman E, Yavuz A, Karakas E, Balcioglu E, Karaca B, Doganay HN, Sacinti KG, Yildiz O. Impact of mRNA and Inactivated COVID-19 Vaccines on Ovarian Reserve. Vaccines. 2025; 13(4):345. https://doi.org/10.3390/vaccines13040345
Studies: Weight Management
Patient Messaging: Bariatric Surgery
There are a few types of bariatric surgery options that I would recommend considering:
- Gastric Sleeve: Removes a significant portion of the stomach, leaving a narrow, tube-like shape, restricting food intake.
- Gastric Bypass: Reroutes the small intestine to connect to a small stomach pouch, reducing food intake and altering nutrient absorption.
- Duodenal Switch: A two-part procedure that restricts intake and decreases nutrient absorption, typically reserved for specific patients.
Here are a few links to resources I trust for more information:
Reference: Weight Watcher's to Calorie Conversion edit
Guestimate: 45-50 cal/point (~50 cal = 1 pt)
- Round down if high in protein/fiber
- Round up if its high in fat/simple carbs
Study: Alternate Day Fasting Combined With Endurance Exercise for the Treatment of Fatty Liver Disease
Background: Approximately 65% of individuals with obesity have non-alcoholic fatty liver disease (NAFLD). The primary treatment for NAFLD is regulating weight per diet and exercise. Alternate day fasting (ADF) has been shown to improve body composition and cardiometabolic risk factors in animals. This is the first human trial to compare the effects of ADF plus endurance exercise, ADF alone, endurance exercise alone versus a no intervention control, on body weight and metabolic disease risk factors in participants with obesity and NAFLD.
Methods: Subjects with obesity and NAFLD (n = 48) were randomized to 1 of 4 groups for 12 weeks: 1) ADF (600 kcal "fast day", alternated with an ad libitum intake "feast day"), 2) exercise (endurance exercise 5 times/week for 60 min/d), 3) combination (ADF + exercise), or 4) control (usual diet).
Results: Body weight was reduced (P < 0.05) in the ADF group (-5.3 ± 1.0 %) and combination group (-4.9 ± 0.6 %), but not the exercise group (-1.9 ± 0.6 %), versus controls (-0.3 ± 1.2 %). ALT was reduced (P < 0.05) in the combination group (-29 ± 9%), but not in the ADF group (-9 ± 8%), exercise group (1 ± 3%), versus controls (17 ? 10%). No significant changes were observed for liver fat, body composition, AST, lipid markers, or glucoregulatory factors. Subjects in the ADF and combination groups were adherent with the fast day energy goal (600 kcal) at week 12 (ADF: 548 kcal; combination: 657 kcal). Subjects in the exercise and combination groups were adherent with attending the 5 workout sessions per week (exercise: 79% attendance; combination: 83% attendance).
Conclusions: These preliminary findings suggest that combination of ADF plus exercise and ADF alone may be effective non-pharmacological therapies to reduce body weight and ALT. However, neither combination intervention nor ADF alone have had any effect on liver fat, metabolic risk factors, or glucoregulatory factors such as insulin.
Reference:
- Poster presentation: ObesityWeek 2022
Study: A population-based study of appetite-suppressant drugs and the risk of cardiac-valve regurgitation
Background: Recent case reports suggest that a combination of the appetite suppressants fenfluramine and phentermine is associated with an increased risk of cardiac-valve regurgitation. There are also reports of valvular disorders in persons taking fenfluramine or dexfenfluramine alone, particularly for more than three months.
Methods: We conducted a population-based follow-up study and a nested case-control analysis of 6532 subjects who received dexfenfluramine, 2371 who received fenfluramine, and 862 who received phentermine to assess the risk of a subsequent clinical diagnosis of a valvular disorder of uncertain origin. For comparison, we identified a group of 9281 obese subjects who had not taken appetite suppressants who were matched to the treated subjects for age, sex, and weight. All subjects were free of diagnosed cardiovascular disease at the start of follow-up. The average duration of follow-up for all subjects was about four years.
Results:
- There were 11 cases of newly diagnosed idiopathic valvular disorders, 5 after the use of dexfenfluramine and 6 after the use of fenfluramine.
- There were six cases of aortic regurgitation, two cases of mitral regurgitation, and three cases of combined aortic and mitral regurgitation.
- There were no cases of idiopathic cardiac-valve abnormalities among the subjects who had not taken appetite suppressants or among those who took only phentermine.
- The five-year cumulative incidence of idiopathic cardiac-valve disorders was 0 per 10,000 subjects among those who had not taken appetite suppressants (95 percent confidence interval, 0 to 15.4) and among those who took phentermine alone (95 percent confidence interval, 0 to 76.6), 7.1 per 10,000 subjects among those who took either fenfluramine or dexfenfluramine for less than four months (95 percent confidence interval, 3.6 to 17.8; P=0.02 for the comparison with subjects who had not taken appetite suppressants), and 35.0 per 10,000 subjects among those who received either of these medications for four or more months (95 percent confidence interval, 16.4 to 76.2; P<0.001).
Conclusions: The use of fenfluramine or dexfenfluramine, particularly for four months or longer, is associated with an increased risk of newly diagnosed cardiac-valve disorders, particularly aortic regurgitation.
Reference:
- Jick H, Vasilakis C, Weinrauch LA, Meier CR, Jick SS, Derby LE. A population-based study of appetite-suppressant drugs and the risk of cardiac-valve regurgitation. N Engl J Med. 1998 Sep 10;339(11):719-24. doi: 10.1056/NEJM199809103391102. PMID: 9731087.
Study: A randomized double-blind placebo-controlled study of the long-term efficacy and safety of diethylpropion in the treatment of obese subjects
Objective:
To evaluate the efficacy of diethylpropion on a long-term basis, with emphasis in cardiovascular and psychiatric safety aspects.
Design:
Randomized, double-blind, placebo-controlled trial
Measurements:
Following a 2-week screening period, 69 obese healthy adults received a hypocaloric diet and were randomized to diethylpropion 50 mg BID (n=37) or placebo (n=32) for 6 months. After this period, all participants received diethylpropion in an open-label extension for an additional 6 months. The primary outcome was percentage change in body weight. Electrocardiogram (ECG), echocardiography and clinical chemistry were performed at baseline and every 6 months. Psychiatric evaluation and application of Hamilton rating scales for depression and anxiety were also performed by experienced psychiatrists at baseline and every 3 months.
Results:
- After 6 months, the diethylpropion group lost an average of 9.8% (s.d. 6.9%) of initial body weight vs 3.2% (3.7%) in the placebo group (P<0.0001).
- From baseline to month 12, the mean weight loss produced by diethylpropion was 10.6% (8.3%).
- Participants in the placebo group who were switched to diethylpropion after 6 months lost an average of 7.0% (7.7%) of initial body weight. The difference between groups at month 12 was not significant (P=0.07).
- No differences in blood pressure, pulse rate, ECG and psychiatric evaluation were observed. Dry mouth and insomnia were the most frequent adverse events.
Conclusion:
- Diethylpropion plus diet produced sustained and clinically significant weight loss over 1 year. It seems to be safe in relation to cardiovascular and psychiatric aspects in a well-selected population.
Reference:
- Cercato C, Roizenblatt VA, Leança CC, Segal A, Lopes Filho AP, Mancini MC, Halpern A. A randomized double-blind placebo-controlled study of the long-term efficacy and safety of diethylpropion in the treatment of obese subjects. Int J Obes (Lond). 2009 Aug;33(8):857-65. doi: 10.1038/ijo.2009.124. Epub 2009 Jun 30. PMID: 19564877.
- https://www.nature.com/articles/ijo2009124
Study: Association between insulin sensitivity and lean mass loss during weight loss
Objective
- The study objective was to assess the relationship between insulin sensitivity and changes in total lean mass (LM) and appendicular LM (ALM) during weight loss.
Methods
- Individuals were randomly assigned to either a standard or a moderately reduced carbohydrate diet for 16 weeks. Body composition was assessed using dual-energy x-ray absorptiometry and insulin sensitivity index (SI) using an intravenous glucose tolerance test. Multiple linear regression was used to determine whether baseline SI was predictive of changes in total LM and ALM.
Results
- Participants (n = 57; baseline BMI 32.1 ± 3.8 kg/m2) lost an average of 6.8 ± 3.2 kg of body weight (p < 0.001), with 1.5 ± 2.6 kg coming from LM (p < 0.05) and 0.5 ± 0.73 kg from ALM (p < 0.05).
- Multiple regression analysis demonstrated that SI was inversely associated with changes in total LM (kilograms; β = 0.481, p < 0.001), after adjusting for baseline LM, fat mass, acute insulin response to glucose, and weight loss.
- Similar results were seen when assessing ALM loss (β = 0.359, p < 0.05).
Conclusions
- Identifying individuals with low insulin sensitivity prior to weight loss interventions may allow for a personalized approach aiming at minimizing LM loss.
Reference:
- Bartholomew CL, Martins C, Gower B. Association between insulin sensitivity and lean mass loss during weight loss. Obesity (Silver Spring). 2024 Jun;32(6):1156-1162. doi: 10.1002/oby.24022. PMID: 38803306.
- https://onlinelibrary.wiley.com/doi/10.1002/oby.24022?af=R
Study: Brain responses to nutrients are severely impaired and not reversed by weight loss in humans with obesity: a randomized crossover study
Post-ingestive nutrient signals to the brain regulate eating behaviour in rodents, and impaired responses to these signals have been associated with pathological feeding behaviour and obesity. To study this in humans, we performed a single-blinded, randomized, controlled, crossover study in 30 humans with a healthy body weight (females N = 12, males N = 18) and 30 humans with obesity (females N = 18, males N = 12).
We assessed the effect of intragastric glucose, lipid and water (noncaloric isovolumetric control) infusions on the primary endpoints cerebral neuronal activity and striatal dopamine release, as well as on the secondary endpoints plasma hormones and glucose, hunger scores and caloric intake.
To study whether impaired responses in participants with obesity would be partially reversible with diet-induced weight loss, imaging was repeated after 10% diet-induced weight loss.
We show that:
- intragastric glucose and lipid infusions induce orosensory-independent and preference-independent, nutrient-specific cerebral neuronal activity and striatal dopamine release in lean participants.
- In contrast, participants with obesity have severely impaired brain responses to post-ingestive nutrients.
- Importantly, the impaired neuronal responses are not restored after diet-induced weight loss.
Impaired neuronal responses to nutritional signals may contribute to overeating and obesity, and ongoing resistance to post-ingestive nutrient signals after significant weight loss may in part explain the high rate of weight regain after successful weight loss.
Reference:
- van Galen KA, Schrantee A, Ter Horst KW, et al. Brain responses to nutrients are severely impaired and not reversed by weight loss in humans with obesity: a randomized crossover study [published online ahead of print, 2023 Jun 12]. Nat Metab. 2023;10.1038/s42255-023-00816-9. https://doi.org/10.1038/s42255-023-00816-9
- https://www.nature.com/articles/s42255-023-00816-9
Study: Calorie Restriction with or without Time-Restricted Eating in Weight Loss
Background:
- The long-term efficacy and safety of time-restricted eating for weight loss are not clear.
Methods:
- We randomly assigned 139 patients with obesity to time-restricted eating (eating only between 8:00 a.m. and 4:00 p.m.) with calorie restriction or daily calorie restriction alone. For 12 months, all the participants were instructed to follow a calorie-restricted diet that consisted of 1500 to 1800 kcal per day for men and 1200 to 1500 kcal per day for women.
- The primary outcome was the difference between the two groups in the change from baseline in body weight
- Secondary outcomes included changes in waist circumference, body-mass index (BMI), amount of body fat, and measures of metabolic risk factors
- Results:
- Of the total 139 participants who underwent randomization, 118 (84.9%) completed the 12-month follow-up visit.
- The mean weight loss from baseline at 12 months was -8.0 kg (95% confidence interval [CI], -9.6 to -6.4) in the time-restriction group and -6.3 kg (95% CI, -7.8 to -4.7) in the daily-calorie-restriction group.
- Changes in weight were not significantly different in the two groups at the 12-month assessment (net difference, -1.8 kg; 95% CI, -4.0 to 0.4; P = 0.11).
- Results of analyses of waist circumferences, BMI, body fat, body lean mass, blood pressure, and metabolic risk factors were consistent with the results of the primary outcome. In addition, there were no substantial differences between the groups in the numbers of adverse events.
Conclusions:
- Among patients with obesity, a regimen of time-restricted eating was not more beneficial with regard to reduction in body weight, body fat, or metabolic risk factors than daily calorie restriction. (Funded by the National Key Research and Development Project [No. 2018YFA0800404] and others; ClinicalTrials.gov number, NCT03745612.).
Reference:
- Liu D, Huang Y, Huang C, et al. Calorie Restriction with or without Time-Restricted Eating in Weight Loss. N Engl J Med. 2022;386(16):1495-1504. https://doi.org/10.1056/NEJMoa2114833
- https://www.nejm.org/doi/10.1056/NEJMoa2114833
Study: Changes in diet and lifestyle and long-term weight gain in women and men
Background:
- Specific dietary and other lifestyle behaviors may affect the success of the straightforward-sounding strategy "eat less and exercise more" for preventing long-term weight gain.
Methods:
- We performed prospective investigations involving three separate cohorts that included 120,877 U.S. women and men who were free of chronic diseases and not obese at baseline, with follow-up periods from 1986 to 2006, 1991 to 2003, and 1986 to 2006. The relationships between changes in lifestyle factors and weight change were evaluated at 4-year intervals, with multivariable adjustments made for age, baseline body-mass index for each period, and all lifestyle factors simultaneously. Cohort-specific and sex-specific results were similar and were pooled with the use of an inverse-variance-weighted meta-analysis.
Results:
- Within each 4-year period, participants gained an average of 3.35 lb (5th to 95th percentile, -4.1 to 12.4).
- On the basis of increased daily servings of individual dietary components,
- 4-year weight change was most strongly associated with the intake of
- potato chips (1.69 lb)
- potatoes (1.28 lb)
- sugar-sweetened beverages (1.00 lb)
- unprocessed red meats (0.95 lb)
- processed meats (0.93 lb)
- was inversely associated with the intake of
- vegetables (-0.22 lb)
- whole grains (-0.37 lb)
- fruits (-0.49 lb)
- nuts (-0.57 lb)
- yogurt (-0.82 lb)
- (P≤0.005 for each comparison)
- 4-year weight change was most strongly associated with the intake of
- Aggregate dietary changes were associated with substantial differences in weight change (3.93 lb across quintiles of dietary change).
- Other lifestyle factors were also independently associated with weight change (P<0.001), including physical activity (-1.76 lb across quintiles); alcohol use (0.41 lb per drink per day), smoking (new quitters, 5.17 lb; former smokers, 0.14 lb), sleep (more weight gain with <6 or >8 hours of sleep), and television watching (0.31 lb per hour per day).
Conclusions:
- Specific dietary and lifestyle factors are independently associated with long-term weight gain, with a substantial aggregate effect and implications for strategies to prevent obesity. (Funded by the National Institutes of Health and others.).
Reference:
- Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011 Jun 23;364(25):2392-404. doi: 10.1056/NEJMoa1014296. PMID: 21696306; PMCID: PMC3151731.
Study: Consumption of Soft Drinks and Overweight and Obesity Among Adolescents in 107 Countries and Regions
Key Points
- Question
- What is the association between soft drink consumption and prevalence of overweight and obesity in adolescents?
- Findings
- In this cross-sectional study using data of 405,528 school-going adolescents (children enrolled in school) from 107 countries and regions, the prevalence of daily soft drink consumption was associated with the prevalence of overweight and obesity.
- Meaning
- These findings suggest that reducing soft drink consumption is important for lowering overweight and obesity in adolescents, and action should be used to reduce the consumption of soft drinks.
Abstract
- Importance
- Soft drink consumption is associated with weight gain in children and adolescents, but little is known about the association between soft drink consumption and prevalence of the overweight and obesity in adolescents.
- Objective
- To investigate the association of soft drink consumption with overweight and obesity in adolescents enrolled in school (hereafter, school-going adolescents) using country-level and individual-level data.
- Design, Setting, and Participants
- This cross-sectional study used data from 3 cross-sectional studies including 107 countries and regions that participated in the Global School-Based Student Health Survey (2009-2017), the European Health Behavior in School-Aged Children study (2017-2018), and the US Youth Risk Behavior Survey (2019).
- Exposure
- Daily soft drink consumption (consuming soft drinks 1 or more times per day or not).
- Main Outcome and Measure
- Overweight and obesity defined by the World Health Organization Growth Reference Data.
- Results
- Among the 107 countries and regions, 65 were low- and middle-income, and 42 were high-income countries and regions, with a total of 405,528 school-going adolescents (mean [SD] age, 14.2 [1.7] years; 196,147 [48.4%] males).
- The prevalence of overweight and obesity among adolescent students varied from 3.3% (95% CI, 2.6 to 4.1) in Cambodia to 64.0% (95% CI, 57.0 to 71.6) in Niue, and the prevalence of adolescent students consuming soft drinks 1 or more times per day varied from 3.3% (95% CI, 2.9 to 3.7) in Iceland to 79.6% (95% CI, 74.0 to 85.3) in Niue.
- There was a positive correlation between the prevalence of daily soft drink consumption and the prevalence of overweight and obesity (R, 0.44; P < .001).
- The pooled analysis using individual-level data also showed a statistically significant association between daily soft drink consumption and overweight and obesity (daily soft drink consumption vs nondaily soft drink consumption), with an odds ratio of 1.14 (95% CI, 1.08 to 1.21) among school-going adolescents.
- Conclusions and Relevance
- In this study of 107 countries and regions, the prevalence of daily consumption of soft drinks was associated with the prevalence of overweight and obesity among adolescent students.
- Our results, in conjunction with other evidence, suggest that reducing soft drink consumption should be a priority in combating adolescent overweight and obesity.
Reference:
- Hu H, Song J, MacGregor GA, He FJ. Consumption of Soft Drinks and Overweight and Obesity Among Adolescents in 107 Countries and Regions. JAMA Netw Open. 2023 Jul 3;6(7):e2325158. doi: 10.1001/jamanetworkopen.2023.25158. PMID: 37486630; PMCID: PMC10366702.
- https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2807548
Study: Continued Treatment With Tirzepatide for Maintenance of Weight Reduction in Adults With Obesity
Key Points
- Question
- Does once-weekly subcutaneous tirzepatide with diet and physical activity affect maintenance of body weight reduction in individuals with obesity or overweight?
- Findings
- After 36 weeks of open-label maximum tolerated dose of tirzepatide (10 or 15 mg), adults (n = 670) with obesity or overweight (without diabetes) experienced a mean weight reduction of 20.9%. From randomization (at week 36), those switched to placebo experienced a 14% weight regain and those continuing tirzepatide experienced an additional 5.5% weight reduction during the 52-week double-blind period.
- Meaning
- In participants with obesity/overweight, withdrawing tirzepatide led to substantial regain of lost weight, whereas continued treatment maintained and augmented initial weight reduction.
Abstract
- Importance
- The effect of continued treatment with tirzepatide on maintaining initial weight reduction is unknown.
- Objective
- To assess the effect of tirzepatide, with diet and physical activity, on the maintenance of weight reduction.
- Design, Setting, and Participants
- This phase 3, randomized withdrawal clinical trial conducted at 70 sites in 4 countries with a 36-week, open-label tirzepatide lead-in period followed by a 52-week, double-blind, placebo-controlled period included adults with a body mass index greater than or equal to 30 or greater than or equal to 27 and a weight-related complication, excluding diabetes.
- Interventions
- Participants (n = 783) enrolled in an open-label lead-in period received once-weekly subcutaneous maximum tolerated dose (10 or 15 mg) of tirzepatide for 36 weeks.
- At week 36, a total of 670 participants were randomized (1:1) to continue receiving tirzepatide (n = 335) or switch to placebo (n = 335) for 52 weeks.
- Main Outcomes and Measures
- The primary end point was the mean percent change in weight from week 36 (randomization) to week 88. Key secondary end points included the proportion of participants at week 88 who maintained at least 80% of the weight loss during the lead-in period.
- Results
- Participants (n = 670; mean age, 48 years; 473
[0%]women; mean weight, 107.3 kg) who completed the 36-week lead-in period experienced a mean weight reduction of 20.9%. - The mean percent weight change from week 36 to week 88 was −5.5% with tirzepatide vs 14.0% with placebo (difference, −19.4% [95% CI, −21.2% to −17.7%]; P < .001).
- Overall, 300 participants (89.5%) receiving tirzepatide at 88 weeks maintained at least 80% of the weight loss during the lead-in period compared with 16.6% receiving placebo (P < .001).
- The overall mean weight reduction from week 0 to 88 was 25.3% for tirzepatide and 9.9% for placebo. The most common adverse events were mostly mild to moderate gastrointestinal events, which occurred more commonly with tirzepatide vs placebo.
- Participants (n = 670; mean age, 48 years; 473
- Conclusions and Relevance
- In participants with obesity or overweight, withdrawing tirzepatide led to substantial regain of lost weight, whereas continued treatment maintained and augmented initial weight reduction.
Reference:
- Aronne LJ, Sattar N, Horn DB, et al. Continued Treatment With Tirzepatide for Maintenance of Weight Reduction in Adults With Obesity: The SURMOUNT-4 Randomized Clinical Trial. JAMA. 2024;331(1):38–48. https://doi.org/10.1001/jama.2023.24945
- https://jamanetwork.com/journals/jama/article-abstract/2812936
Study: Dietary Macronutrient Composition and Protein Concentration for Weight Loss Maintenance
Study Importance
- What is already known?
- What represents an optimal macronutrient composition for long-term weight loss maintenance (WLM) remains an open question.
- Studies have suggested that protein intake is tightly controlled in humans, which drives excess food and energy intake when dietary protein is diluted by other energy-yielding macronutrients, termed “protein leverage.”
- However, the role of dietary macronutrient composition and protein leverage in long-term WLM remained unclear.
- What does this study add?
- In the prospective analysis of 1518 adults with initial weight loss (≥5%), nutritional geometry revealed that a lower percentage of energy from protein, diluted by high fat and/or carbohydrate, was associated with higher total food and energy intake and greater 12-month increases in body weight, waist-height ratio, and hip-height ratio.
- Additionally, high consumption of discretionary foods was associated with increased energy intake by lowering the percentage of energy from protein in the diet.
- How might these results change the direction of research or the focus of clinical practice?
- Avoiding dietary protein dilution, particularly through low consumption of discretionary foods, may decrease food and energy intake and benefit long-term WLM.
Objective:
- To examine the association between dietary macronutrient composition and 12-month weight loss maintenance (WLM) in adults who achieved initial weight loss (≥5%).
Methods:
- This prospective cohort analysis used 12-month follow-up data from the Navigating to a Healthy Weight trial. Macronutrient composition (%) was assessed using a 4-day, 24-h dietary recall. Food sources were categorized as discretionary foods, lean meat, vegetables, fruit, grains, and dairy. Primary outcomes included 12-month changes in body weight, fat mass index (FMI), waist-to-height ratio (WHtR), and hip-to-height ratio (HHtR). A nutritional geometry approach was used to examine individual and interactive associations of macronutrient intake, visualizing as response surfaces.
Results:
- Among 1518 participants (69.8% women; mean age 45±12years), mean macronutrient composition was 20.6% protein, 33.8% fat, and 43.1% carbohydrate.
- Protein energy percentage was inversely associated with energy intake (β: −0.33; 95% CI: −0.39, −0.27).
- Response surfaces revealed that lower proportional energy from protein, diluted by high fat and/or carbohydrate, was associated with higher total energy intake and greater 12-month increases in body weight, WHtR, and HHtR, but not FMI.
- Consumption of discretionary food, not other food sources, increased energy intake by reducing proportional energy from protein.
Conclusions:
- Maintaining dietary proportional energy from protein, particularly by limiting discretionary food consumption, was associated with reduced energy intake and improved WLM.
Reference:
- H. Zhang, A. Vasileiou, D. Searle, et al., “ Dietary Macronutrient Composition and Protein Concentration for Weight Loss Maintenance,” Obesity (2025): 1–10, https://doi.org/10.1002/oby.24370.
Study: Diets for weight management in adults with type 2 diabetes: an umbrella review of published meta-analyses and systematic review of trials of diets for diabetes remission
- Abstract
- Weight reduction is fundamental for type 2 diabetes management and remission, but uncertainty exists over which diet type is best to achieve and maintain weight loss.
- We evaluated dietary approaches for weight loss, and remission, in people with type 2 diabetes to inform practice and clinical guidelines.
- Methods
- First, we conducted a systematic review of published meta-analyses of RCTs of weight-loss diets.
- Second, we conducted a systematic review of any intervention studies reporting type 2 diabetes remission with weight-loss diets
- Results
- We identified 19 meta-analyses of weight-loss diets, involving 2–23 primary trials (n = 100–1587), published 2013–2021.
- Twelve were 'critically low' or 'low' AMSTAR 2 quality, with seven 'high' quality.
- Greatest weight loss was reported with very low energy diets, 1.7–2.1 MJ/day (400–500 kcal) for 8–12 weeks (high-quality meta-analysis, GRADE low), achieving 6.6 kg (95% CI −9.5, −3.7) greater weight loss than low-energy diets (4.2–6.3 MJ/day [1000–1500 kcal]).
- Formula meal replacements (high quality, GRADE moderate) achieved 2.4 kg (95% CI −3.3, −1.4) greater weight loss over 12–52 weeks.
- Low-carbohydrate diets were no better for weight loss than higher-carbohydrate/low-fat diets (high quality, GRADE high).
- High-protein, Mediterranean, high-monounsaturated-fatty-acid, vegetarian and low-glycaemic-index diets all achieved minimal (0.3–2 kg) or no difference from control diets (low to critically low quality, GRADE very low/moderate).
- For type 2 diabetes remission, of 373 records, 16 met inclusion criteria. Remissions at 1 year were reported for a median 54% of participants in RCTs including initial low-energy total diet replacement (low-risk-of-bias study, GRADE high), and 11% and 15% for meal replacements and Mediterranean diets, respectively (some concerns for risk of bias in studies, GRADE moderate/low). For ketogenic/very low-carbohydrate and very low-energy food-based diets, the evidence for remission (20% and 22%, respectively) has serious and critical risk of bias, and GRADE certainty is very low.
- Conclusions/interpretation
- Published meta-analyses of hypocaloric diets for weight management in people with type 2 diabetes do not support any particular macronutrient profile or style over others.
- Very low energy diets and formula meal replacement appear the most effective approaches, generally providing less energy than self-administered food-based diets.
- Programmes including a hypocaloric formula 'total diet replacement' induction phase were most effective for type 2 diabetes remission.
- Most of the evidence is restricted to 1 year or less.
References:
- Churuangsuk, C., Hall, J., Reynolds, A. et al. Diets for weight management in adults with type 2 diabetes: an umbrella review of published meta-analyses and systematic review of trials of diets for diabetes remission. Diabetologia 65, 14–36 (2022). https://doi.org/10.1007/s00125-021-05577-2
- https://link.springer.com/article/10.1007/s00125-021-05577-2
Study: Does time-restricted eating add benefits to calorie restriction? A systematic review edit
Objective
- A growing body of evidence has supported the health benefits of extended daily fasting, known as time-restricted eating (TRE); however, whether the addition of TRE enhances the known benefits of calorie restriction (CR) remains unclear.
Methods
- PubMed, Scopus, the Cochrane Library, and Google Scholar were searched through April 2023. This systematic review includes randomized controlled trials (RCTs) that compared CR + TRE with CR alone in energy-matched conditions of at least 8 weeks in duration that assessed changes in body weight and cardiometabolic disease risk factors in adults with overweight and/or obesity.
Results
- Seven studies were identified (n = 579). Two studies reported greater weight loss and reductions in diastolic blood pressure with CR + TRE compared with CR alone after 8 to 14 weeks, whereas one study reported greater improvements in triglycerides and glucose tolerance with CR + TRE (3 d/wk) compared with CR alone following 26 weeks. One study reported significant increases in Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) levels with CR + TRE versus CR alone after 8 weeks. There were no statistically significant differences in any other outcome variable between the two interventions.
Conclusions
- The addition of TRE to CR regimens resulted in greater weight loss and improvements in cardiometabolic risk factors in some studies; however, the majority of studies did not find additional benefits.
Reference:
- Ezzati A, McLaren C, Bohlman C, Tamargo JA, Lin Y, Anton SD. Does time-restricted eating add benefits to calorie restriction? A systematic review. Obesity (Silver Spring). 2024 Feb 21. doi: 10.1002/oby.23984. Epub ahead of print. PMID: 38383703.
- https://onlinelibrary.wiley.com/doi/10.1002/oby.23984?af=R
Study: Effectiveness of Intermittent Fasting and Time-Restricted Feeding Compared to Continuous Energy Restriction for Weight Loss
The current obesity epidemic is staggering in terms of its magnitude and public health impact. Current guidelines recommend continuous energy restriction (CER) along with a comprehensive lifestyle intervention as the cornerstone of obesity treatment, yet this approach produces modest weight loss on average. Recently, there has been increased interest in identifying alternative dietary weight loss strategies that involve restricting energy intake to certain periods of the day or prolonging the fasting interval between meals (i.e., intermittent energy restriction, IER).
These strategies include intermittent fasting (IMF; >60% energy restriction on 2-3 days per week, or on alternate days) and time-restricted feeding (TRF; limiting the daily period of food intake to 8-10 h or less on most days of the week).
Here, we summarize the current evidence for IER regimens as treatments for overweight and obesity. Specifically, we review randomized trials of ≥8 weeks in duration performed in adults with overweight or obesity (BMI ≥ 25 kg/m2) in which an IER paradigm (IMF or TRF) was compared to CER, with the primary outcome being weight loss.
Overall, the available evidence suggests that IER paradigms produce equivalent weight loss when compared to CER, with 9 out of 11 studies reviewed showing no differences between groups in weight or body fat loss.
Reference:
- Rynders CA, Thomas EA, Zaman A, Pan Z, Catenacci VA, Melanson EL. Effectiveness of Intermittent Fasting and Time-Restricted Feeding Compared to Continuous Energy Restriction for Weight Loss. Nutrients. 2019;11(10):2442. Published 2019 Oct 14. https://doi.org/10.3390/nu11102442
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6836017/
Study: Efficacy and safety of tirzepatide, GLP-1 receptor agonists, and other weight loss drugs in overweight and obesity: a network meta-analysis
Objective
- This network meta-analysis evaluates the efficacy and safety of tirzepatide compared to glucagon-like peptide-1 receptor agonists (GLP-1 RA) and other weight loss drugs in the treatment of overweight and obesity.
Methods
- MEDLINE, Embase, and Cochrane CENTRAL were searched for randomized controlled trials on tirzepatide, GLP-1 RA, and weight loss drugs approved by the US Food and Drug Administration. A network meta-analysis was performed, drawing direct and indirect comparisons between treatment groups. Network diagrams and surface under the cumulative ranking curve analysis were performed for primary (≥5%, ≥10%, ≥15%, absolute weight loss) and secondary outcomes and adverse effects.
Results
- Thirty-one randomized controlled trials, involving more than 35,000 patients, were included in this study.
- Tirzepatide 15 mg ranked in the top three across
- Weight-related parameters
- Glycemic profile (glycated hemoglobin)
- Lipid parameters (total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglycerides)
- Blood pressure
- Tirzepatide 15 mg had the highest efficacy compared with placebo for achieving ≥15% weight loss (risk ratio 10.24, 95% CI: 6.42–16.34).
- As compared to placebo, tirzepatide and GLP-1 RA across all doses had significant increases in gastrointestinal adverse effects.
- Tirzepatide 15 mg ranked in the top three across
Conclusions
- The superiority of tirzepatide and GLP-1 RA in inducing weight loss and their ability to target multiple metabolic parameters render them promising candidates in the treatment of patients with overweight and obesity.
Reference:
- Pan XH, Tan B, Chin YH, Lee ECZ, Kong G, Chong B, Kueh M, Khoo CM, Mehta A, Majety P, Grandhi GR, Dimitriadis GK, Foo R, Chew NWS, Le Roux CW, Mamas MA, Chan MY. Efficacy and safety of tirzepatide, GLP-1 receptor agonists, and other weight loss drugs in overweight and obesity: a network meta-analysis. Obesity (Silver Spring). 2024 Feb 27. doi: 10.1002/oby.24002. Epub ahead of print. PMID: 38413012.
Study: Energy expenditure and obesity across the economic spectrum
Significance
- Economic development is associated with increased prevalence of obesity and related health problems, but the relative importance of increased caloric intake and reduced energy expenditure remains unresolved. We show that daily energy expenditures are greater in developed populations, and activity energy expenditures are not reduced in more industrialized populations, challenging the hypothesis that decreased physical activity contributes to rises in obesity with economic development.
- Instead, our results suggest that dietary intake plays a far greater role than reduced expenditure in the elevated prevalence of obesity associated with economic development.
Abstract
- Global economic development has been associated with an increased prevalence of obesity and related health problems. Increased caloric intake and reduced energy expenditure are both cited as development-related contributors to the obesity crisis, but their relative importance remains unresolved.
- Here, we examine energy expenditure and two measures of obesity (body fat percentage and body mass index, BMI) for 4,213 adults from 34 populations across six continents and a wide range of lifestyles and economies, including hunter-gatherer, pastoralist, farming, and industrialized populations.
- Economic development was positively associated with greater body mass, BMI, and body fat, but also with greater total, basal, and activity energy expenditure.
- Body size–adjusted total and basal energy expenditures both decreased approximately 6 to 11% with increasing economic development, but were highly variable among populations and did not correspond closely with lifestyle.
- Body size–adjusted total energy expenditure was negatively, but weakly, associated with measures of obesity, accounting for roughly one-tenth of the elevated body fat percentage and BMI associated with economic development.
- In contrast, estimated energy intake was greater in economically developed populations, and in populations with available data (n = 25), the percentage of ultraprocessed food in the diet was associated with body fat percentage, suggesting that dietary intake plays a far greater role than reduced energy expenditure in obesity related to economic development.
Reference:
- A. McGrosky, A. Luke, L. Arab, K. Bedu-Addo, A.G. Bonomi, P. Bovet, S. Brage, M.S. Buchowski, N. Butte, S.G. Camps, R. Casper, D.K. Cummings, S. Krupa Das, S. Deb, L.R. Dugas, U. Ekelund, T. Forrester, B.W. Fudge, M. Gillingham, A.H. Goris, M. Gurven, C. Hambly, A. Joosen, P.T. Katzmarzyk, K.P. Kempen, W.E. Kraus, W. Kriengsinyos, R. Kuriyan, R.F. Kushner, E.V. Lambert, C.L. Larsson, W.R. Leonard, N. Lessan, M. Löf, C.K. Martin, A.C. Medin, M.L. Neuhouser, K.H. Pietilainen, G. Plasqui, R.L. Prentice, S.B. Racette, D.A. Raichlen, E. Ravussin, L. Redman, R.M. Reynolds, E.B. Rimm, S. Roberts, A.Y. Rosinger, M.H. Samuels, S. Sinha, J.J. Snodgrass, E. Stice, R. Uauy, S.S. Urlacher, J.A. Verbunt, B. Wolfe, B. Wood, X. Zhang, A.J. Murphy-Alford, C.J. Loechl, J. Rood, H. Sagayama, D.A. Schoeller, K.R. Westerterp, W.W. Wong, Y. Yamada, J.R. Speakman, H. Pontzer, & The IAEA DLW Database Consortium, Energy expenditure and obesity across the economic spectrum, Proc. Natl. Acad. Sci. U.S.A. 122 (29) e2420902122, https://doi.org/10.1073/pnas.2420902122 (2025).
Study: Healthy weight loss maintenance with exercise, GLP-1 receptor agonist, or both combined followed by one year without treatment: a post-treatment analysis of a randomised placebo-controlled trial edit
Background
- New obesity medications result in large weight losses. However, long-term adherence in a real-world setting is challenging, and termination of obesity medication results in weight regain towards pre-treatment body weight. Therefore, we investigated whether weight loss and improved body composition are sustained better at 1 year after termination of active treatment with glucagon-like peptide-1 (GLP-1) receptor agonist, supervised exercise program, or both combined for 1 year.
Methods
- We conducted a post-treatment study in extension of a randomised, controlled trial in Copenhagen. Adults with obesity (aged 18–65 years and initial body mass index 32–43 kg/m2) completed an eight-week low-calorie diet-induced weight loss of 13.1 kg (week −8 to 0) and were randomly allocated (1:1:1:1) to one-year weight loss maintenance (week 0–52) with either supervised exercise, the GLP-1 receptor agonist once-daily subcutaneous liraglutide 3.0 mg, the combination of exercise and liraglutide, or placebo.
- 166 Participants completed the weight loss maintenance phase. All randomised participants were invited to participate in the post-treatment study with outcome assessments one year after treatment termination, at week 104.
- The primary outcome of the post-treatment assessment was change in body weight from after the initial weight loss (at randomisation, week 0) to one year after treatment termination (week 104) in the intention-to-treat population.
- The secondary outcome was change in body-fat percentage (week 0–104). The study is registered with EudraCT, 2015-005585-32, and with ClinicalTrials.gov, NCT04122716.
Findings
- Between Dec 17, 2018, and Dec 17, 2020, 109 participants attended the post-treatment study. From randomisation to one year after termination of combined exercise and liraglutide treatment (week 0–104), participants had reduced body weight (−5.1 kg [95% CI −10.0; −0.2]; P = 0.040) and body-fat percentage (−2.3%-points [−4.3 to −0.3]; P = 0.026) compared with after termination of liraglutide alone.
- More participants who had previously received combination treatment maintained a weight loss of at least 10% of initial body weight one year after treatment termination (week −8 to 104) compared with participants who had previously received placebo (odds ratio [OR] 7.2 [2.4; 21.3]) and liraglutide (OR 4.2 [1.6; 10.8]).
- More participants who had previously received supervised exercise maintained a weight loss of at least 10% compared with placebo (OR 3.7 [1.2; 11.1]).
- During the year after termination of treatment (week 52–104), weight regain was 6.0 kg [2.1; 10.0] larger after termination of liraglutide compared with after termination of supervised exercise and 2.5 kg [−1.5 to 6.5] compared with after termination of combination treatment.
Interpretation
- The addition of supervised exercise to obesity pharmacotherapy seems to improve healthy weight maintenance after treatment termination compared with treatment termination of obesity pharmacotherapy alone.
- Body weight and body composition were maintained one year after termination of supervised exercise, in contrast to weight regain after termination of treatment with obesity pharmacotherapy alone.
Reference:
- Simon Birk Kjær Jensen, Martin Bæk Blond, Rasmus Michael Sandsdal, Lisa Møller Olsen, Christian Rimer Juhl, Julie Rehné Lundgren, Charlotte Janus, Bente Merete Stallknecht, Jens Juul Holst, Sten Madsbad, Signe Sørensen Torekov, Healthy weight loss maintenance with exercise, GLP-1 receptor agonist, or both combined followed by one year without treatment: a post-treatment analysis of a randomised placebo-controlled trial, eClinicalMedicine, Volume 69, 2024, 102475, ISSN 2589-5370, https://doi.org/10.1016/j.eclinm.2024.102475.
- https://www.sciencedirect.com/science/article/pii/S2589537024000543
Study: Host-diet-gut microbiome interactions influence human energy balance: a randomized clinical trial
- P: Equal numbers of males and females 18–45 years of age with a BMI ≤ 30 kg/m2 who were weight stable, otherwise healthy, and had not used antibiotics for the 3 months prior to screening
- I: Randomized crossover study with a control Western Diet (WD) compared to a Microbiome Enhancer Diet (MBD)
- the MBD was higher in fiber and resistant starch, which are known substrates for microbial fermentation
- also provided larger food particles (whole nuts vs. nut butter, for example) because fine grinding of foods makes nutrients more bioavailable to the human host and thus, less available to the gut microbes
- minimizing processed foods on the MBD, in contrast to the known excess of processed foods in the WD
- C: Each participant served as their own control (crossover study)
- Outcomes:
- Diet modulated host metabolizable energy
- MBD increased mean daily fecal energy losses, compared to the WD, over the six calorimetry days of the domiciled controlled-feeding period (73.0 ± 6.1 gCOD/day on MBD vs. 32.1 ± 2.5 gCOD/day on WD; P = 2.96 ×10−7; Fig. 1a).
- When fecal energy loss was adjusted to total energy intake to calculate host metabolizable energy (primary endpoint), we found that it was lower with the MBD (89.5 ± 0.73% on the MBD vs. 95.4 ± 0.21% on the WD (Fig. 1b; P = 2.73 ×10−7), which equates to an additional 116 ± 56 kcals daily channeled to feces on the MBD vs. the WD (Fig. 1c; P = 4.95 ×10−7).
- Diet modulated the gut microbiome
- WD led to conditions in which the gut microbes were "starved" because a higher proportion of metabolizable energy had been digested and absorbed by the host in the upper gastrointestinal tract.
- Microbial contribution to human energy balance
- host metabolizable energy was lower due to higher fecal energy loss on the MBD.
- Diet modulated host metabolizable energy
- T: 6 days
- S: Whole-room indirect calorimetry
Abstract
- The gut microbiome is emerging as a key modulator of human energy balance. Prior studies in humans lacked the environmental and dietary controls and precision required to quantitatively evaluate the contributions of the gut microbiome.
- Using a Microbiome Enhancer Diet (MBD) designed to deliver more dietary substrates to the colon and therefore modulate the gut microbiome, we quantified microbial and host contributions to human energy balance in a controlled feeding study with a randomized crossover design in young, healthy, weight stable males and females (NCT02939703).
- In a metabolic ward where the environment was strictly controlled, we measured energy intake, energy expenditure, and energy output (fecal and urinary).
- The primary endpoint was the within-participant difference in host metabolizable energy between experimental conditions [Control, Western Diet (WD) vs. MBD].
- The secondary endpoints were enteroendocrine hormones, hunger/satiety, and food intake. Here we show that, compared to the WD, the MBD leads to an additional 116 ± 56 kcals (P < 0.0001) lost in feces daily and thus, lower metabolizable energy for the host (89.5 ± 0.73%; range 84.2-96.1% on the MBD vs. 95.4 ± 0.21%; range 94.1-97.0% on the WD; P < 0.0001) without changes in energy expenditure, hunger/satiety or food intake (P > 0.05).
- Microbial 16S rRNA gene copy number (a surrogate of biomass) increases (P < 0.0001), beta-diversity changes (whole genome shotgun sequencing; P = 0.02), and fermentation products increase (P < 0.01) on an MBD as compared to a WD along with significant changes in the host enteroendocrine system (P < 0.0001).
- The substantial interindividual variability in metabolizable energy on the MBD is explained in part by fecal SCFAs and biomass. Our results reveal the complex host-diet-microbiome interplay that modulates energy balance.
Reference:
- Corbin, K.D., Carnero, E.A., Dirks, B. et al. Host-diet-gut microbiome interactions influence human energy balance: a randomized clinical trial. Nat Commun 14, 3161 (2023). https://doi.org/10.1038/s41467-023-38778-x
- https://www.nature.com/articles/s41467-023-38778-x
Study: Impact of weight loss achieved through a multidisciplinary intervention on appetite in patients with severe obesity edit
The impact of lifestyle-induced weight loss (WL) on appetite in patients with obesity remains controversial.
This study aimed to assess the short- and long-term impact of WL achieved by diet and exercise on appetite in patients with obesity.
Thirty-five (22 females) adults with severe obesity (body mass index: 42.5 ± 5.0 kg/m2) underwent a 2-yr WL program focusing on diet and exercise. Body weight (BW), cardiovascular fitness (V̇o2max), appetite feelings, and plasma concentrations of insulin, active ghrelin (AG), glucagon-like peptide 1 (GLP-1), peptide YY (PYY), and cholecystokinin (CCK), in the fasting and postprandial states, were measured at baseline (B), week 4 (W4), and 1 and 2 yr (and average values for all fasting and postprandial time points computed).
Results:
- BW was significantly reduced and V̇o2max (ml·kg−1·min−1) increased at all time points compared with B (3.5, 8.1, and 8.4% WL and 7, 11, and 8% increase at W4 and 1 and 2 yr, respectively).
- Basal hunger and average hunger and desire to eat were significantly increased at 1 and 2 yr.
- Basal fullness was significantly increased at W4, and average ratings were reduced at 1 yr.
- Average AG and PYY were significantly increased, and insulin was reduced, at all time points compared with B.
- Average GLP-1 was reduced at W4, and CCK was increased at 2 yr.
After lifestyle-induced WL, patients with severe obesity will, therefore, have to deal with increased hunger in the long term.
In conclusion:
- sustained WL at 2 yr achieved with diet and exercise is associated with increased hunger feelings and ghrelin concentration but also increased postprandial concentrations of satiety hormones.
Reference:
- Coutinho SR, Rehfeld JF, Holst JJ, Kulseng B, Martins C. Impact of weight loss achieved through a multidisciplinary intervention on appetite in patients with severe obesity. Am J Physiol Endocrinol Metab. 2018 Jul 1;315(1):E91-E98. doi: 10.1152/ajpendo.00322.2017. Epub 2018 Jan 23. PMID: 29360396.
- https://journals.physiology.org/doi/full/10.1152/ajpendo.00322.2017
Study: Incident type 2 diabetes attributable to suboptimal diet in 184 countries
Abstract points
- The global burden of diet-attributable type 2 diabetes (T2D) is not well established.
- This risk assessment model estimated T2D incidence among adults attributable to direct and body weight-mediated effects of 11 dietary factors in 184 countries in 1990 and 2018.
- In 2018, suboptimal intake of these dietary factors was estimated to be attributable to 14.1 million (95% uncertainty interval (UI), 13.8–14.4 million) incident T2D cases, representing 70.3% (68.8–71.8%) of new cases globally.
- Largest T2D burdens were attributable to
- Insufficient whole-grain intake (26.1% (25.0–27.1%))
- Excess refined rice and wheat intake (24.6% (22.3–27.2%))
- Excess processed meat intake (20.3% (18.3–23.5%))
- Across regions
- highest proportional burdens were in central and eastern Europe and central Asia (85.6% (83.4–87.7%)) and Latin America and the Caribbean (81.8% (80.1–83.4%))
- lowest proportional burdens were in South Asia (55.4% (52.1–60.7%))
- Proportions of diet-attributable T2D were generally larger in men than in women and were inversely correlated with age.
- Diet-attributable T2D was generally larger among urban versus rural residents and higher versus lower educated individuals, except in high-income countries, central and eastern Europe and central Asia, where burdens were larger in rural residents and in lower educated individuals.
- Compared with 1990, global diet-attributable T2D increased by 2.6 absolute percentage points (8.6 million more cases) in 2018, with variation in these trends by world region and dietary factor.
- These findings inform nutritional priorities and clinical and public health planning to improve dietary quality and reduce T2D globally.
| Global Consumption, g/d (mean, 95% UI) | Global Consumption, g/d (mean, 95% UI) | Diet- T2D Relative Risk (95% CI) | Diet- T2D Relative Risk (95% CI) | Diet- BMI Effect Estimate (95% CI), kg/m2 | Diet- BMI Effect Estimate (95% CI), kg/m2 | |||
|---|---|---|---|---|---|---|---|---|
| 1990 | 2018 | Optimal Consumption Mean (g/d) | Unit of RR and effect estimate | Age 50 y | Age 70 y | Baseline BMI <25 | Baseline BMI >25 | |
| Fruit | 81.9 (78.8 - 85.2) | 87.9 (84.9 - 90.8) | 300 | per 100 g/d | - | - | -0.06 (-0.08, -0.02) | -0.06 (-0.10, -0.02) |
| Potatoes | 45.5 (42.5 - 49.2) | 47.8 (42.7 - 55.2) | 0 | per 100 g/d | 1.06 (1.02 - 1.09) | 1.04 (1.02 - 1.06) | 0.08 (0.03, 0.12) | 0.14 (0.08, 0.21) |
| Nuts and seeds | 3.1 (2.8 - 3.5) | 8.6 (7.7 - 9.7) | 20.3 | per 28.35 g/d | -0.1 (-0.15, -0.04) | -0.14 (-0.25, -0.03) | ||
| Refined rice and wheat | 304.8 (264.1 – 363.3) | 302.9 (265.1 - 354.8) | 0 | Per 1 serving/d | 1.31 (1.18 - 1.44) | 1.21 (1.12 - 1.29) | 0.05 (0.01, 0.09) | 0.07 (0.03, 0.11) |
| Whole grains | 44.9 (40.6 - 49.1) | 50.1 (44.2 - 55.2) | 90 | 30g/d | -0.1 (-0.15, -0.04) | >= 40g: 0.84 (0.77-0.92) | -0.05 (-0.07, -0.03) | 0.08 (-0.10, -0.06) |
| 41-90g: 0.91(0.87-0.95) | 41-90g: 0.93 (0.90-0.96) | |||||||
| Processed meats | 15.5 (13.5 - 18.4) | 16.8 (14.7 - 19.9) | 0 | 21.4 g/d | 1.19 (1.17 - 1.22) | 1.13 (1.11 - 1.15) | 0.06 (0.03, 0.08) | 0.07 (0.05, 0.09) |
| Unprocessed red meat | 43.6 (41.8 - 45.4) | 56.5 (53.3 - 59.9) | 14.3 | 42.9 g/d | 1.18 (1.17 - 1.19) | 1.12 (1.11 - 1.13) | 0.06 (0.03, 0.08) | 0.10 (0.06, 0.14) |
| Yogurt | 23.4 (20.0 - 28.5) | 21.2 (18.3 - 25.1) | 87.1 | 244 g/d | 0.70 (0.56 - 0.85) | 0.78 (0.67 - 0.90) | -0.09 (-0.12, -0.06) | -0.20 (-0.29, -0.11) |
| Sugar-sweetened beverages | 82.9 (79.1 - 87.1) | 95.6 (89.1 – 103.0) | 0 | 244 g/d | 1.20 (1.14 - 1.26) | 1.14 (1.10 - 1.18) | 0.09 (0.04, 0.13) | .23 (0.14, 0.31) |
| Fruit juice | 17.7 (16.4 - 19.2) | 15.1 (14.0 - 16.4) | 0 | 248 g/d | - | - | 0.04 (0.01, 0.07) | 0.11 (0.03, 0.18) |
References:
- O'Hearn, M., Lara-Castor, L., Cudhea, F. et al. Incident type 2 diabetes attributable to suboptimal diet in 184 countries. Nat Med 29, 982–995 (2023). https://doi.org/10.1038/s41591-023-02278-8
- https://www.nature.com/articles/s41591-023-02278-8
Study: Increased Physical Activity Associated with Less Weight Regain Six Years After "The Biggest Loser" Competition
Objective
- The aim of this study was to explore how physical activity (PA) and energy intake (EI) changes were related to weight loss and regain following "The Biggest Loser" competition.
Methods
- At baseline, week 6 and week 30 of the competition, and 6 years after the competition, body composition was measured via dual-energy x-ray absorptiometry, resting energy expenditure was measured by using indirect calorimetry, and EI and PA were measured by using doubly labeled water.
Results
- Six years after the competition, median weight loss in 14 of "The Biggest Loser" participants was 13%, with those maintaining a greater weight loss (mean ± SE) of 24.9% ± 3.8% having increased PA by 160% ± 23%, compared with a PA increase of 34% ± 25% (P = 0.0033) in the weight regainers who were 1.1% ± 4.0% heavier than the precompetition baseline.
- EI changes were similar between weight loss maintainers and regainers (−8.7% ± 5.6% vs. −7.4% ± 2.7%, respectively; P = 0.83).
- Weight regain was inversely associated with absolute changes in PA (r = −0.82; P = 0.0003) but not with changes in EI (r = −0.15; P = 0.61).
- EI and PA changes explained 93% of the individual weight loss variability at 6 years.
Conclusions
- Consistent with previous reports, large and persistent increases in PA may be required for long-term maintenance of lost weight.
Reference:
- Kerns JC, Guo J, Fothergill E, Howard L, Knuth ND, Brychta R, Chen KY, Skarulis MC, Walter PJ, Hall KD. Increased Physical Activity Associated with Less Weight Regain Six Years After "The Biggest Loser" Competition. Obesity (Silver Spring). 2017 Nov;25(11):1838-1843. doi: 10.1002/oby.21986. PMID: 29086499; PMCID: PMC5757520.
- https://onlinelibrary.wiley.com/doi/10.1002/oby.21986
Study: Less frequent dosing of GLP-1 receptor agonists as a viable weight maintenance strategy
Objective
- Incretin mimetics are revolutionizing obesity treatment, but high prices and supply shortages limit patient access. Some clinicians have suggested less frequent dosing as an off-ramping strategy to maintain weight loss, but this approach lacks published evidence regarding its weight loss efficacy. We aim to provide such clinical evidence and to rationalize these results with mathematical modeling.
Methods
- We present a real-world case series of two patients who took their incretin mimetic less frequently than recommended. We complement this case report with a pharmacokinetic-pharmacodynamic model of virtual patients that simulates long-term weight change with semaglutide and tirzepatide administered at various frequencies.
Results
- Both real-world and virtual patients maintained significant weight loss under reduced dosing frequencies. Our results indicate that reducing frequency does not commensurately reduce efficacy. The majority of weight loss persists even when patients wait 2, 3, or perhaps even 4 weeks between doses.
Conclusions
- Our findings support the hypothesis that less frequent administration of incretin mimetics can be a viable and cost-saving long-term weight maintenance strategy in conjunction with sustained lifestyle modification. Further research is warranted to validate the effectiveness of this off-label approach, define optimal dosing regimens to meet individual patient needs, and evaluate the cost–benefit implications.
Reference:
- Wu CC, Cengiz A, Lawley SD. Less frequent dosing of GLP-1 receptor agonists as a viable weight maintenance strategy. Obesity (Silver Spring). 2025; 1-5. https://doi.org/10.1002/oby.24302
Study: Lifestyle Strategies after Intentional Weight Loss: Results from the MAINTAIN-pc Randomized Trial
Introduction/Purpose
- Weight maintenance after intentional weight loss is challenging and often unsuccessful.
- Physical activity and self-monitoring are strategies associated with successful weight loss maintenance.
- However, less is known about the type and number of lifestyle strategies used after intentional weight loss. The purpose of this study was to determine the types and amounts of strategies associated with successful long-term weight loss maintenance.
Methods
- Data from the 24-month Maintaining Activity and Nutrition Through Technology-Assisted Innovation in Primary Care (MAINTAIN-pc) trial were analyzed. MAINTAIN-pc recruited adults (n = 194; 53.4 ± 12.2 yr of age; body mass index, 30.4 ± 5.9 kg·m−2; 74% female) with recent intentional weight loss of ≥5%, randomized to tracking tools plus coaching (i.e., coaching group) or tracking tools without coaching (i.e., tracking-only group).
- At baseline and at 6, 12, and 24 months, participants reported lifestyle strategies used in the past 6 months, including self-monitoring, group support, behavioral skills, and professional support. General linear models evaluated changes in the number of strategies over time between groups and the consistency of strategies used over the 24-month intervention.
Results
- At baseline, 100% used behavioral skills, 73% used group support, 69% used self-monitoring, and 68% used professional support in the past 6 months; at 24 months, these rates were 98%, 60%, 75%, and 61%, respectively.
- Although the number of participants utilizing individual strategies did not change significantly over time, the overall number of strategies participants reported decreased.
- More strategies were used at baseline and 6 months compared with 12- and 24-month follow-ups.
- The coaching group used more strategies at months 6 and 12 than the tracking-only group.
- Consistent use of professional support strategies over the 24-month study period was associated with less weight regain.
Conclusion
- Weight loss maintenance interventions that incorporate continued follow-up and support from healthcare professionals are likely to prevent weight regain after intentional weight loss.
Reference:
- Halliday TM, McFadden M, Cedillo M, Barone Gibbs B, Hess R, Bryce C, Fischer GS, Huber K, McTigue KM, Conroy MB. Lifestyle strategies after intentional weight loss: results from the MAINTAIN-pc randomized trial. Transl J Am Coll Sports Med. 2023 Spring;8(2):e000220. doi: 10.1249/tjx.0000000000000220. Epub 2023 Feb 10. PMID: 37458000; PMCID: PMC10348773.
- https://journals.lww.com/acsm-tj/Fulltext/2023/04130/Lifestyle_Strategies_after_Intentional_Weight.3.aspx
Study: Liraglutide versus semaglutide for weight reduction—A cost needed to treat analysis
Objective:
- Higher doses of the glucagon-like peptide-1 agonists liraglutide and, more recently, semaglutide have demonstrated a significant reduction in body weight. However, their comparative value for money for this indication is unclear.
Methods:
- The cost needed to treat to achieve a 1% reduction in body weight using semaglutide or liraglutide was calculated. The body weight reductions were extracted from the published STEP 1 trial and the SCALE trial results, respectively. A scenario analysis was performed to mitigate the primary differences between the two studies' populations. Drug costs were based on US GoodRx prices as of October 2022.
Results:
- Liraglutide in STEP 1 resulted in a weight loss of 5.4% (95% CI: 5%-5.8%).
- Semaglutide in SCALE resulted in a weight loss of 12.4% (95% CI: 11.5%-13.4%).
- The total cost of therapy with liraglutide during the trial was estimated at $17,585 compared with $22,878 with semaglutide.
- Accordingly, the cost needed to treat per 1% of body weight reduction with liraglutide is estimated at $3256 (95% CI: $3032-$3517) compared with $1845 (95% CI: $1707-$1989) with semaglutide.
Conclusions:
- Semaglutide provides significantly better value for money than liraglutide for weight reduction.
Reference:
- Azuri J, Hammerman A, Aboalhasan E, Sluckis B, Arbel R. Liraglutide versus semaglutide for weight reduction-a cost needed to treat analysis. Obesity (Silver Spring). 2023;31(6):1510-1513. https://doi.org/10.1002/oby.23752
- https://onlinelibrary.wiley.com/doi/10.1002/oby.23752
Study: Low-calorie diet-induced weight loss is associated with altered brain connectivity and food desire in obesity
Objective
- The main objective of this study is to better understand the effects of diet-induced weight loss on brain connectivity in response to changes in glucose levels in individuals with obesity.
Methods
- A total of 25 individuals with obesity, among whom 9 had a diagnosis of type 2 diabetes, underwent functional magnetic resonance imaging (fMRI) scans before and after an 8-week low-calorie diet. We used a two-step hypereuglycemia clamp approach to mimic the changes in glucose levels observed in the postprandial period in combination with task-mediated fMRI intrinsic connectivity distribution (ICD) analysis.
Results
- After the diet, participants lost an average of 3.3% body weight.
- Diet-induced weight loss led to
- a decrease in leptin levels
- an increase in hunger and food intake
- greater brain connectivity in the parahippocampus, right hippocampus, and temporal cortex (limbic–temporal network)
- Group differences (with vs. without type 2 diabetes) were noted in several brain networks.
- Connectivity in the limbic–temporal and frontal–parietal brain clusters inversely correlated with hunger.
Conclusions
- A short-term low-calorie diet led to a multifaceted body response in patients with obesity, with an increase in connectivity in the limbic–temporal network (emotion and memory) and hormone and eating behavior changes that may be important for recovering the weight lost.
Reference:
- Hoang H, Lacadie C, Hwang J, et al. Low-calorie diet-induced weight loss is associated with altered brain connectivity and food desire in obesity. Obesity (Silver Spring). 2024; 1-11. https://doi.org/10.1002/oby.24046
- https://onlinelibrary.wiley.com/doi/10.1002/oby.24046?af=R
Study: Modeling potential cost-effectiveness of tirzepatide versus lifestyle modification for patients with overweight and obesity
What is already known?
- Obesity is a chronic, progressive disease that is increasingly prevalent in the United States. People with obesity are subject to increased risk of various complications, including cardiovascular events and type 2 diabetes.
- Lifestyle modification (LSM; i.e., diet and exercise) is the current mainstay of treatment for obesity, but even with intensive lifestyle interventions, most individuals are not able to maintain weight loss. Therefore, alternative treatments for obesity are needed.
What does this study add?
- Our model, which employs an individual-level simulation approach with results driven by the full published outcomes from the SURMOUNT-1 trial (including cardiometabolic factor change), suggests that tirzepatide may be a cost-effective alternative to LSM based on typical US willingness-to-pay thresholds ranging from $100,000 to $150,000 per quality-adjusted life year.
How might these results change the direction of research or the focus of clinical practice?
- Tirzepatide is a first-in-class glucose dependent insulinotropic polypeptide and glucagon-like peptide-1 receptor agonist approved by the Food and Drug Administration for treatment of type 2 diabetes and obesity. In the SURMOUNT-1 trial, the mean change in body weight at week 72 with tirzepatide 15 mg was −22.5%, compared with −2.4% with placebo.
- To understand the potential implications of tirzepatide in clinical practice, estimates of its long-term economic and clinical impacts are needed.
Objective
- Our objective was to model the potential cost-effectiveness of tirzepatide as an alternative to lifestyle modification (LSM) for the management of obesity and overweight.
Methods
- An individual-level discrete event simulation was implemented in Microsoft Excel linking short-term outcomes from the SURMOUNT-1 trial to key obesity-related complications to estimate costs and health benefits of tirzepatide (5-mg, 10-mg, or 15-mg doses) and LSM over a lifetime time horizon.
- Treatment-related changes in cardiometabolic factors were modeled using data from SURMOUNT-1; the relationship between patient status and risk of obesity complications was obtained from published literature.
- Modeled complications included cardiovascular events, onset of type 2 diabetes, cancer, osteoarthritis, and sleep apnea.
- The model simulated 1000 adult patients with overweight or obesity over their lifetimes, applying a 3% annual discount rate to cost and health outcomes.
- Only direct medical costs were considered.
Results
- Tirzepatide 5, 10, and 15 mg provided 0.54, 0.55, and 0.61 additional quality-adjusted life years (QALYs) and additional costs of $79,288, $70,453, and $75,839 versus LSM, yielding incremental cost-effectiveness ratios of $146,331, $127,644, and $125,053 per QALY gained, respectively.
Conclusions
- The model predicted that all doses of tirzepatide represent cost-effective alternatives to LSM for management of overweight and obesity at a willingness-to-pay threshold of $150,000 per QALY.
Reference:
- Hoog MM, Kan H, Deger KA, et al. Modeling potential cost-effectiveness of tirzepatide versus lifestyle modification for patients with overweight and obesity. Obesity. 2025; 1-12. https://doi.org/10.1002/oby.24310
Study: Nut consumption, gut microbiota, and body fat distribution: results of a large, community-based population study
Objective
- We aimed to investigate the relationships among nut consumption, gut microbiota, and body fat distribution.
Methods
- We studied 2255 Chinese adults in the Lanxi Cohort living in urban areas in Lanxi City, China.
- Fat distribution was assessed by dual-energy x-ray absorptiometry, and nut consumption was assessed using food frequency questionnaires. 16S ribosomal RNA (rRNA) sequencing was performed on stool samples from 1724 participants. Linear regression and Spearman correlation were used in all analyses. A validation study was performed using 1274 participants in the Lanxi Cohort living in rural areas.
Results
- Nut consumption was beneficially associated with regional fat accumulation.
- Gut microbial analysis suggested that a high intake of nuts was associated with greater microbial α diversity.
- Six genera were found to be associated with nut consumption, and the abundance of genera Anaerobutyricum, Anaerotaenia, and Fusobacterium was significantly associated with fat distribution.
- Favorable relationships between α diversity and fat distribution were also observed.
- Similar relationships between gut microbiota and fat distribution were obtained in the validation analysis.
Conclusions
- We have shown that nut consumption is beneficially associated with body fat distribution and gut microbiota diversity and taxonomy. Furthermore, the microbial features related to high nut intake are associated with a favorable pattern of fat distribution.
Reference:
- Shi Y, Kan J, Wang W, Cao Y, Wu Y, Chen X, Zheng W, Yang F, Du J, He W, Zhu S. Nut consumption, gut microbiota, and body fat distribution: results of a large, community-based population study. Obesity (Silver Spring). 2024 Jul 23. doi: 10.1002/oby.24099. Epub ahead of print. PMID: 39041418.
- https://onlinelibrary.wiley.com/doi/10.1002/oby.24099?af=R
Study: Persistent metabolic adaptation 6 years after "The Biggest Loser" competition
Objective
- To measure long-term changes in resting metabolic rate (RMR) and body composition in participants of "The Biggest Loser" competition.
Methods
- Body composition was measured by dual energy X-ray absorptiometry, and RMR was determined by indirect calorimetry at baseline, at the end of the 30-week competition and 6 years later. Metabolic adaptation was defined as the residual RMR after adjusting for changes in body composition and age.
Results
- Of the 16 "Biggest Loser" competitors originally investigated, 14 participated in this follow-up study.
- Weight loss at the end of the competition was (mean ± SD) 58.3 ± 24.9 kg (P < 0.0001), and RMR decreased by 610 ± 483 kcal/day (P = 0.0004).
- After 6 years, 41.0 ± 31.3 kg of the lost weight was regained (P = 0.0002), while RMR was 704 ± 427 kcal/day below baseline (P < 0.0001) and metabolic adaptation was −499 ± 207 kcal/day (P < 0.0001).
- Weight regain was not significantly correlated with metabolic adaptation at the competition's end (r = −0.1, P = 0.75), but those subjects maintaining greater weight loss at 6 years also experienced greater concurrent metabolic slowing (r = 0.59, P = 0.025).
Conclusions
- Metabolic adaptation persists over time and is likely a proportional, but incomplete, response to contemporaneous efforts to reduce body weight.
Reference:
- Fothergill E, Guo J, Howard L, Kerns JC, Knuth ND, Brychta R, Chen KY, Skarulis MC, Walter M, Walter PJ, Hall KD. Persistent metabolic adaptation 6 years after "The Biggest Loser" competition. Obesity (Silver Spring). 2016 Aug;24(8):1612-9. doi: 10.1002/oby.21538. Epub 2016 May 2. PMID: 27136388; PMCID: PMC4989512.
- https://onlinelibrary.wiley.com/doi/10.1002/oby.21538
Study: Pharmacotherapy for adults with overweight and obesity: a systematic review and network meta-analysis of randomised controlled trials
Background:
- Pharmacotherapy provides an option for adults with overweight and obesity to reduce their bodyweight if lifestyle modifications fail. We summarised the latest evidence for the benefits and harms of weight-lowering drugs.
Methods:
- This systematic review and network meta-analysis included searches of PubMed, Embase, and Cochrane Library (CENTRAL) from inception to March 23, 2021, for randomised controlled trials of weight-lowering drugs in adults with overweight and obesity. We performed frequentist random-effect network meta-analyses to summarise the evidence and applied the Grading of Recommendations Assessment, Development, and Evaluation frameworks to rate the certainty of evidence, calculate the absolute effects, categorise interventions, and present the findings. The study was registered with PROSPERO, CRD 42021245678.
Findings:
- 14,605 citations were identified by our search, of which 132 eligible trials enrolled 48 209 participants.
- All drugs lowered bodyweight compared with lifestyle modification alone; all subsequent numbers refer to comparisons with lifestyle modification.
- High to moderate certainty evidence established phentermine-topiramate as the most effective in lowering weight (odds ratio [OR] of ≥5% weight reduction 8.02, 95% CI 5.24 to 12.27; mean difference [MD] of percentage bodyweight change -7.98, 95% CI -9.27 to -6.69) followed by GLP-1 receptor agonists (OR 6.33, 95% CI 5.00 to 8.00; MD -5.79, 95% CI -6.34 to -5.25).
- Naltrexone-bupropion (OR 2.69, 95% CI 2.10 to 3.44), phentermine-topiramate (2.40, 1.68 to 3.44), GLP-1 receptor agonists (2.22, 1.74 to 2.84), and orlistat (1.71, 1.42 to 2.05) were associated with increased adverse events leading to drug discontinuation.
- In a post-hoc analysis, semaglutide, a GLP-1 receptor agonist, showed substantially larger benefits than other drugs with a similar risk of adverse events as other drugs for both likelihood of weight loss of 5% or more (OR 9.82, 95% CI 7.09 to 13.61) and percentage bodyweight change (MD -11.40, 95% CI -12.51 to -10.29).
Interpretation:
- In adults with overweight and obesity, phentermine-topiramate and GLP-1 receptor agonists proved the best drugs in reducing weight; of the GLP-1 agonists, semaglutide might be the most effective.
Reference:
- Shi Q, Wang Y, Hao Q, Vandvik PO, Guyatt G, Li J, Chen Z, Xu S, Shen Y, Ge L, Sun F, Li L, Yu J, Nong K, Zou X, Zhu S, Wang C, Zhang S, Qiao Z, Jian Z, Li Y, Zhang X, Chen K, Qu F, Wu Y, He Y, Tian H, Li S. Pharmacotherapy for adults with overweight and obesity: a systematic review and network meta-analysis of randomised controlled trials. Lancet. 2024 Apr 6;403(10434):e21-e31. doi: 10.1016/S0140-6736(24)00351-9. PMID: 38582569.
Study: Polycystic ovary syndrome is associated with weight-loss attempts and perception of overweight independent of BMI: a population-based cohort study
Objective
- Up to 70% of women with polycystic ovary syndrome (PCOS) have pre-obesity or obesity.
- The aim of this study was to investigate whether women with PCOS have more weight-loss attempts than women without PCOS, regardless of BMI.
- Moreover, women's weight perceptions in relation to previous weight-loss attempts were evaluated.
Methods
- A population-based birth cohort study included women with (n = 278) and without PCOS (control individuals, n = 1560) who were examined at ages 31 and 46 years with questionnaires and clinical examinations.
Results
- Women with PCOS had more weight-loss attempts compared with control individuals at age 31 (47% vs. 34%, p < 0.001) and 46 years (63% vs. 47%, p < 0.001).
- At age 46 years, PCOS was associated with multiple weight-loss attempts in the adjusted model (odds ratio: 1.43 [95% CI: 1.00-2.03], p = 0.05).
- The perception of having overweight was more prevalent in those with PCOS, even among participants with normal weight, at age 31 (PCOS 47% vs. control 34%, p = 0.014) and 46 years (PCOS 60% vs. control 39%, p = 0.001).
Conclusions
- Women with PCOS were more likely to have experienced multiple weight-loss attempts and a perception of having overweight compared with control individuals, regardless of obesity status.
Study Importance
- What is already known?
- Commonly, all women with polycystic ovary syndrome (PCOS), regardless of BMI, receive information about the risk of weight gain; however, support for weight management is limited.
- Women with PCOS are more likely to be using both healthy and detrimental weight-management practices compared with women without PCOS. Also, body-image distress and a perceived susceptibility to weight issues are common in women with PCOS.
- Prevalence of weight-loss attempts during a life course has not been investigated, to our knowledge, in women with PCOS.
- What does this study add?
- Multiple weight-loss attempts were more common in women with PCOS compared with women without PCOS at ages 31 and 46 years. Perception of having overweight was a strong predictor of weight-loss attempts.
- Women with PCOS perceived themselves as having overweight significantly more often than women without PCOS, even when their BMI was in the normal range.
- At age 46 years, PCOS was an independent predictor of multiple weight-loss attempts and a perception of having overweight.
- How might these results change the direction of research or the focus of clinical practice?
- The results challenge clinicians to evaluate how they discuss weight-related matters with women with PCOS, especially when they are at a normal weight.
- Emphasis should be placed on supporting women with PCOS to reduce inefficient weight-loss attempts and stress.
- A weight-neutral approach to lifestyle interventions should be a key area of future research.
Reference:
- Pesonen E, Nurkkala M, Niemelä M, et al. Polycystic ovary syndrome is associated with weight-loss attempts and perception of overweight independent of BMI: a population-based cohort study. Obesity (Silver Spring). 2023;31(4):1108-1120. https://doi.org/10.1002/oby.23681
- https://onlinelibrary.wiley.com/doi/10.1002/oby.23681
Study: Reducing Social Media Use Improves Appearance and Weight Esteem in Youth With Emotional Distress
Background
- Adolescence and young adulthood are vulnerable periods in which mental health challenges often emerge.
- Cross-sectional research has shown that high social media use (SMU) is associated with poor body image in youth, a known predictor of eating disorders; however, high-quality experimental evidence is scarce, limiting the ability to make causal inferences. The present study experimentally examined the effects of reducing smartphone SMU on appearances and weight esteem in youth with emotional distress.
Methods
- A randomized controlled trial was conducted where 220 participants (17–25 years; 76% female, 23% male, and 1% other) were assigned to either an intervention (SMU limited to 1 hr/day) or control (unrestricted access to SMU) group.
- SMU was monitored via screen time trackers and submitted daily during 1-week baseline and 3-week intervention periods.
- Baseline and post-intervention measurements were taken to assess changes in appearance and weight esteem.
Results
- Compared to the controls, the intervention group yielded significant increases in both appearance ( p , .022) and weight esteem ( p , .026).
- The intervention group significantly increased in appearance esteem (from M = 2.95 to 3.15, p , .001, dz = 0.33) and weight esteem (from M = 3.16 to 3.32, p , .001, dz = 0.27), whereas the control group did not significantly change (appearance: M = 2.72 to 2.76, p = .992, d z = 0.13; weight: M = 3.01 to 3.02, p = .654, d z = 0.06) from baseline to post-intervention.
- No effects of gender were detected.
Conclusion
- Findings suggest that reducing SMU on smartphones may be a feasible and effective method of improving body image in a vulnerable population of youth.
Reference:
Study: RE: Pulmonary Hypertension Associated with Use of Phentermine?
Dear Sir,
Recently Bang, et al.1 reported a case of a 29 year-old obese woman who was hospitalized with pulmonary arterial hypertension (PAH) and a history of having taken phentermine hydrochloride 37.5 milligrams daily for 35 days. Since common etiologies of PAH were excluded by the patient's history, examination procedures, and hospital course, the authors suggest this is the first case of phentermine-induced PAH. We suggest instead this is a case of idiopathic pulmonary arterial hypertension (IPAH) rather than PAH secondary to therapeutic phentermine.
The authors suggest, based on one case report, that phentermine mono-therapy produces the same increase in incidence of PAH previously seen in patients treated with fenfluramine mono-therapy and in patients treated with a combination of fenfluramine and phentermine. However, a survey of 95 European cases of PAH by Abenhaim, et al.2 found that of the 30 patients that had a history of taking anorexic agents, 24 had taken a fenfluramine, but none had taken phentermine. Moreover, Rich, et al.,3 in a North American prospective study in which 579 patients with pulmonary hypertension were studied, found that the odds ratios for an association of pulmonary hypertension and fenfluramine to be 7.5, an odds ratio for a similar association for phentermine of 0.6, and concluded that fenfluramines, but not phentermine are risk factors for PAH. Since fenfluramines were taken off-market in 1997 there have been no subsequent reports linking PAH or IPAH to anorectic medicines. Hence the literature does not support the contention of Bang, et al. that phentermine mono-therapy has caused an increased incidence of secondary PAH similar to that caused by fenfluramine.
Physicians in other countries may not be aware that phentermine has long been the most widely used anti-obesity medicine in the United States. A recent survey of United States obesity treatment specialists found that for 97%, phentermine was their first choice among the available anti-obesity drugs.4 The majority of physicians surveyed reported they prescribed phentermine long-term in any patient provided the medicine was effective and produced no intolerable side effects. The longest duration of phentermine therapy reported in the literature has been forty years with no serious adverse effects.5 The survey confirmed that most specialists have employed doses higher than the maximum dose of 37.5 milligrams daily recommended by the U.S. Food and Drug Administration (FDA)-approved label. There are other reports of the safe use of higher doses.4,6-9 Thus, in spite of continued widespread use of phentermine for longer durations and higher doses than recommended by the FDA-approved label, there is no report of an increased incidence of pulmonary hypertension due to phentermine in the U.S. The incidence of IPAH is approximately one case per million per year in the general population. Since phentermine is so widely used, it is reasonable to expect an occasional patient diagnosed with IPAH will coincidently have taken phentermine.
PAH and IPAH are characterized by an increase in pulmonary vascular resistance due to progressive obliteration of pulmonary arterioles, which in turn are induced by pulmonary arteriole smooth muscle cell proliferation and arteriolar vasoconstriction with accompanying inflammation and thrombosis. One hypothesis to explain fenfluramine-induced PAH is that fenfluramine releases 5-hydroxytryptophan (5-HT) via the 5-HT transporter (SERT), and that the increased concentration of plasma 5-HT provokes pulmonary vasoconstriction and pulmonary arterial smooth muscle cell proliferation.10 However, recent data raises questions about this hypothesis.11 5-HT is also thought to play a central role in the pathogenesis of IPAH. Bang, et al. imply that phentermine is active as a serotonin transporter producing increases in 5-HT levels, and therefore has the potential to cause PAH. However, Rothman, et al.12 have shown previously that phentermine has considerably less potent SERT substrate activity, and is considerably less effective in elevating plasma 5-HT compared to fenfluramine, and compared to the commonly abused stimulants methamphetamine and 3,4-methylenedioxymethamphetamine. In another study Rothman, et al. found that phentermine produced minimal increases in 5HT, insufficient to provoke pulmonary arteriolar smooth muscle proliferation.13 These studies suggest that it is unlikely phentermine could induce PAH by the mechanism proposed by Bang, et al.
In summary we suggest that phentermine, after 52 years of widespread use has proven to be both effective and safe. Historically, an association between phentermine mono-therapy and PAH has been suggested but confirming evidence has not appeared. Currently, while we have few effective pharmacologic agents to include in obesity treatment, patients and physicians are fortunate to have phentermine available. Bang, et al. are correct in noting the absence of 870long-term, dose ranging, clinical trials with phentermine; we concur that such trials are needed and should be conducted. Meanwhile, while we await trials, phentermine treatment should not be withheld from the obese because of fear of theoretical but unproven adverse effects.
Reference:
- Hendricks EJ, Rothman RB. RE: Pulmonary hypertension associated with use of phentermine? Yonsei Med J. 2011 Sep;52(5):869-70. doi: 10.3349/ymj.2011.52.5.869. PMID: 21786457; PMCID: PMC3159930.
Study: Semaglutide 2.4 mg/wk for weight loss in patients with severe obesity and with or without a history of bariatric surgery
Objective
- This retrospective cohort study aimed to assess the effectiveness of semaglutide 2.4 mg in patients with severe obesity (BMI ≥ 40 kg/m2) who had previously undergone bariatric surgery (BS) but failed to achieve satisfactory weight loss or experienced weight regain compared with patients without a history of BS with similar BMI.
Methods
- The authors analyzed data from 129 patients with a BMI ≥ 40 kg/m2, including 39 with (BS+) and 90 without (BS−) a history of BS.
- The patients received semaglutide treatment for 24 weeks starting at 0.25 mg/wk and gradually increasing to reach a final dose of 2.4 mg/wk.
- The treatment outcomes were assessed based on the
- percentage of weight loss
- changes in BMI
- waist circumference.
Results
- Semaglutide treatment resulted in significant 9.1% weight loss in the BS+ group, with no significant difference in weight loss between the BS+ and BS− groups.
Conclusions
- This study is the first, to the authors' knowledge, to compare the effectiveness of semaglutide treatment in patients with versus those without a history of BS, providing valuable evidence of its efficacy. By focusing on individuals with severe obesity (BMI > 40 kg/m2 and associated comorbidities), it fills a gap in the current literature and highlights the potential of semaglutide 2.4 mg as a treatment option for this specific population.
Reference:
- Bonnet JB, Tournayre S, Anitcheou J, Faivre M, Boegner C, Jalek A, Jullien D, Attalin V, Myzia J, Marty L, Kemba Y, Nocca D, Sultan A, Avignon A. Semaglutide 2.4 mg/wk for weight loss in patients with severe obesity and with or without a history of bariatric surgery. Obesity (Silver Spring). 2023 Nov 5. doi: 10.1002/oby.23922. Epub ahead of print. PMID: 37927153.
- https://onlinelibrary.wiley.com/doi/10.1002/oby.23922?af=R
Study: Sugar-sweetened beverage consumption and weight gain in children and adults: a systematic review and meta-analysis of prospective cohort studies and randomized controlled trials
- Background Sugar-sweetened beverages (SSBs) have been implicated in fueling the obesity epidemic.
- Objectives This study aimed to update a synthesis of the evidence on SSBs and weight gain in children and adults.
- Methods MEDLINE, Embase, and Cochrane databases were searched through September 8, 2022, for prospective cohort studies and randomized controlled trials (RCTs) that evaluated intake of SSBs in relation to BMI and body weight in children and adults, respectively. Eligible interventions were compared against a noncaloric control. Study-level estimates were pooled using random-effects meta-analysis and presented as β-coefficients with 95% CIs for cohorts and weighted mean differences (MDs) with 95% CIs for RCTs.
- Results
We identified 85 articles including 48 in children (40 cohorts, n = 91,713; 8 RCTs, n = 2783) and 37 in adults (21 cohorts, n = 448,661; 16 RCTs, n = 1343).
- Among cohort studies, each serving/day increase in SSB intake was associated with a 0.07-kg/m2 (95% CI: 0.04 kg/m2, 0.10 kg/m2) higher BMI in children and a 0.42-kg (95% CI: 0.26 kg, 0.58 kg) higher body weight in adults.
- RCTs in children indicated less BMI gain with SSB reduction interventions compared with control (MD: −0.21 kg/m2; 95% CI: −0.40 kg/m2, −0.01 kg/m2).
- In adults, randomization to addition of SSBs to the diet led to greater body weight gain (MD: 0.83 kg; 95% CI: 0.47 kg, 1.19 kg), and subtraction of SSBs led to weight loss (MD: −0.49 kg; 95% CI: −0.66 kg, −0.32 kg) compared with the control groups.
- A positive linear dose–response association between SSB consumption and weight gain was found in all outcomes assessed.
- Conclusions Our updated systematic review and meta-analysis expands on prior evidence to confirm that SSB consumption promotes higher BMI and body weight in both children and adults, underscoring the importance of dietary guidance and public policy strategies to limit intake. This meta-analysis was registered at the International Prospective Register of Systematic Reviews as CRD42020209915.
Reference:
- Nguyen M, Jarvis SE, Tinajero MG, Yu J, Chiavaroli L, Mejia SB, Khan TA, Tobias DK, Willett WC, Hu FB, Hanley AJ, Birken CS, Sievenpiper JL, Malik VS. Sugar-sweetened beverage consumption and weight gain in children and adults: a systematic review and meta-analysis of prospective cohort studies and randomized controlled trials. Am J Clin Nutr. 2023 Jan;117(1):160-174. doi: 10.1016/j.ajcnut.2022.11.008. Epub 2022 Dec 20. PMID: 36789935.
- https://www.sciencedirect.com/science/article/pii/S0002916522105290
Study: The association between weight loss medications and cardiovascular complications
- How might these results change the direction of research or the focus of clinical practice?
- AOM utilization among people with obesity, a modifiable risk factor, could potentially alleviate the high prevalence of CVD.
- AOM use in patients with obesity was associated with less incidence of heart failure and atrial fibrillation compared to patients with obesity without AOMs.
Objective
- Obesity and its cardiovascular complications are major causes of morbidity and mortality. Little is known in real-world settings about the effect of newly approved antiobesity medications (AOMs) on cardiovascular complications among patients with obesity.
Methods
- This retrospective cohort study examined the association between newly approved AOM use and cardiovascular events among Medicare patients with obesity using data from 2020 to 2022.
- Patient age, gender, comorbidity scores, socioeconomic status, and baseline cardiovascular comorbidities were compared descriptively. Subgroup analysis compared variables by medication type. Relative risk and absolute risk of cardiovascular disease (CVD) events were estimated using Cox and Aalen regression models.
Results
- The analysis included 5926 patients treated with semaglutide and tirzepatide, including Ozempic (5404 patients), Wegovy (375 patients), or Mounjaro (147 patients).
- Hypertension, type 2 diabetes, and hyperlipidemia were the most common comorbidities.
- For patients with AOMs, less incidence of the following was found versus patients without AOMs.
- Heart failure (4.89% vs. 6.13%, p < 0.0001)
- Atrial fibrillation (3.83% vs. 5.17%, p < 0.0001)
- Arrhythmia (3.59% vs. 4.14%, p < 0.0153)
- Peripheral vascular disease (3.44% vs. 2.94%, p < 0.0395)
- Patients receiving AOMs showed an 8% risk reduction in any CVD.
- Protective effect on CVD was apparent over the first 375 days.
Conclusions
- Results suggest that utilization of AOMs effectively alleviates the high prevalence of CVD.
Reference:
- Baser O, Samayoa G, Rodchenko K, Isenman L, Baser E, Yapar N. The association between weight loss medications and cardiovascular complications. Obesity (Silver Spring). 2024 May 6. doi: 10.1002/oby.24037. Epub ahead of print. PMID: 38706431.
- https://onlinelibrary.wiley.com/doi/10.1002/oby.24037?af=R
Study: The spread of obesity in a large social network over 32 years
Background:
- The prevalence of obesity has increased substantially over the past 30 years. We performed a quantitative analysis of the nature and extent of the person-to-person spread of obesity as a possible factor contributing to the obesity epidemic.
Methods:
- We evaluated a densely interconnected social network of 12,067 people assessed repeatedly from 1971 to 2003 as part of the Framingham Heart Study. The body-mass index was available for all subjects. We used longitudinal statistical models to examine whether weight gain in one person was associated with weight gain in his or her friends, siblings, spouse, and neighbors.
Results:
- Discernible clusters of obese persons (body-mass index [the weight in kilograms divided by the square of the height in meters], > or =30) were present in the network at all time points, and the clusters extended to three degrees of separation. These clusters did not appear to be solely attributable to the selective formation of social ties among obese persons.
- A person's chances of becoming obese increased by 57% (95% confidence interval [CI], 6 to 123) if he or she had a friend who became obese in a given interval.
- Among pairs of adult siblings, if one sibling became obese, the chance that the other would become obese increased by 40% (95% CI, 21 to 60).
- If one spouse became obese, the likelihood that the other spouse would become obese increased by 37% (95% CI, 7 to 73).
- These effects were not seen among neighbors in the immediate geographic location.
- Persons of the same sex had relatively greater influence on each other than those of the opposite sex.
- The spread of smoking cessation did not account for the spread of obesity in the network.
Conclusions:
- Network phenomena appear to be relevant to the biologic and behavioral trait of obesity, and obesity appears to spread through social ties.
- These findings have implications for clinical and public health interventions.
Reference:
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007 Jul 26;357(4):370-9. doi: 10.1056/NEJMsa066082. Epub 2007 Jul 25. PMID: 17652652.
Study: Three- and six-month efficacy and safety of phentermine in a Mexican obese population
Objective: Mexico has the second largest prevalence of obesity among adults worldwide, a condition especially affecting the low-income population. There is a pressing need to improve therapeutic options for weight loss. Phentermine is an old and low-cost agent given as an adjuvant therapy for obesity for a 12-week period, at an initial dose of 15 mg or 30 mg. However, there are no precise guidelines on the suitability of both the starting dose and the continuation of treatment for 6 months.
The aim of this study was to evaluate the 3- and 6-month efficacy and safety of phentermine in obese Mexican patients to elucidate the aforementioned.
Materials and methods: In this prospective, multi-center, open-label study, 932 obese adults received 15 mg or 30 mg phentermine once daily for 6 months.
Results:
- 30 mg phentermine was more effective than 15 mg phentermine in improving anthropometric variables in the 3-month follow-up, but not after completing the 6-month treatment period.
- Nearly 40% of 3-month non-responders reached a body weight reduction of at least 5% at 6 months.
- Conversely, ~ 65% and 25% of 3-month responders maintained or improved, respectively, their body weight reduction with long-term phentermine.
- Potential tolerance as weight regain was ~ 10% from 3 to 6 months.
- None of the doses increased cardiovascular risk, although mild-to-moderate adverse events were more frequent with 30 mg phentermine.
Conclusion: 30 mg phentermine was more effective than 15 mg phentermine after 3 months, but not at 6 months of treatment. An important number of subjects could benefit following the therapy from 3 to 6 months.
Reference:
- Márquez-Cruz M, Kammar-García A, Huerta-Cruz JC, Carrasco-Portugal MDC, Barranco-Garduño LM, Rodríguez-Silverio J, Rocha González HI, Reyes-García JG. Three- and six-month efficacy and safety of phentermine in a Mexican obese population. Int J Clin Pharmacol Ther. 2021 Aug;59(8):539-548. doi: 10.5414/CP203943. PMID: 34236303; PMCID: PMC8295716.
Study: Time-Restricted Eating Without Calorie Counting for Weight Loss in a Racially Diverse Population
Background:
- Time-restricted eating (TRE), without calorie counting, has become a popular weight loss strategy, yet long-term randomized trials evaluating its efficacy are limited.
Objective:
- To determine whether TRE is more effective for weight control and cardiometabolic risk reduction compared with calorie restriction (CR) or control.
Design:
- 12-month randomized controlled trial. (ClinicalTrials.gov: NCT04692532)
Setting:
- University of Illinois Chicago from January 2021 to September 2022.
Participants:
- 90 adults with obesity.
Intervention:
- 8-hour TRE (eating between noon and 8:00 p.m. only, without calorie counting), CR (25% energy restriction daily), or control (eating over a period of 10 or more hours per day). Participants were not blinded.
Measurements:
- Change in body weight, metabolic markers, and energy intake by month 12.
Results:
- Seventy-seven persons completed the study.
- Mean age was 40 years (SD, 11), 33% were Black, and 46% were Hispanic.
- Mean reduction in energy intake was −425 kcal/d (SD, 531) for TRE and −405 kcal/d (SD, 712) for CR.
- Compared with the control group, weight loss by month 12 was −4.61 kg (95% CI, −7.37 to −1.85 kg; P ≤ 0.01) (−4.87% [CI, −7.61% to −2.13%]) for the TRE group and −5.42 kg (CI, −9.13 to −1.71 kg; P ≤ 0.01) (−5.30% [CI, −9.06% to −1.54%]) for the CR group, with no statistically significant difference between TRE and CR (0.81 kg [CI, −3.07 to 4.69 kg; P = 0.68]) (0.43% [CI, −3.48% to 4.34%]).
Limitation:
- Not blinded, not powered to detect relatively large differences in weight loss, and lack of adjustment for multiple comparisons.
Conclusion:
- Time-restricted eating is more effective in producing weight loss when compared with control but not more effective than CR in a racially diverse population.
Reference:
- Lin S, Cienfuegos S, Ezpeleta M, et al. Time-Restricted Eating Without Calorie Counting for Weight Loss in a Racially Diverse Population : A Randomized Controlled Trial [published online ahead of print, 2023 Jun 27]. Ann Intern Med. 2023;10.7326/M23-0052. https://doi.org/10.7326/M23-0052
- https://www.acpjournals.org/doi/10.7326/M23-0052
Study: Tirzepatide Once Weekly for the Treatment of Obesity
BACKGROUND Obesity is a chronic disease that results in substantial global morbidity and mortality. The efficacy and safety of tirzepatide, a novel glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 receptor agonist, in people with obesity are not known.
METHODS In this phase 3 double-blind, randomized, controlled trial, we assigned 2539 adults with a body-mass index (BMI; the weight in kilograms divided by the square of the height in meters) of 30 or more, or 27 or more and at least one weight-related complication, excluding diabetes, in a 1:1:1:1 ratio to receive once-weekly, subcutaneous tirzepatide (5 mg, 10 mg, or 15 mg) or placebo for 72 weeks, including a 20-week dose-escalation period. Coprimary end points were the percentage change in weight from baseline and a weight reduction of 5% or more. The treatment-regimen estimand assessed effects regardless of treatment discontinuation in the intention-to-treat population.
RESULTS At baseline, the mean body weight was 104.8 kg, the mean BMI was 38.0, and 94.5% of participants had a BMI of 30 or higher. The mean percentage change in weight at week 72 was −15.0% (95% confidence interval [CI], −15.9 to −14.2) with 5-mg weekly doses of tirzepatide, −19.5% (95% CI, −20.4 to −18.5) with 10-mg doses, and −20.9% (95% CI, −21.8 to −19.9) with 15-mg doses and −3.1% (95% CI, −4.3 to −1.9) with placebo (P<0.001 for all comparisons with placebo). The percentage of participants who had weight reduction of 5% or more was 85% (95% CI, 82 to 89), 89% (95% CI, 86 to 92), and 91% (95% CI, 88 to 94) with 5 mg, 10 mg, and 15 mg of tirzepatide, respectively, and 35% (95% CI, 30 to 39) with placebo; 50% (95% CI, 46 to 54) and 57% (95% CI, 53 to 61) of participants in the 10-mg and 15-mg groups had a reduction in body weight of 20% or more, as compared with 3% (95% CI, 1 to 5) in the placebo group (P<0.001 for all comparisons with placebo). Improvements in all prespecified cardiometabolic measures were observed with tirzepatide. The most common adverse events with tirzepatide were gastrointestinal, and most were mild to moderate in severity, occurring primarily during dose escalation. Adverse events caused treatment discontinuation in 4.3%, 7.1%, 6.2%, and 2.6% of participants receiving 5-mg, 10-mg, and 15-mg tirzepatide doses and placebo, respectively.
CONCLUSIONS In this 72-week trial in participants with obesity, 5 mg, 10 mg, or 15 mg of tirzepatide once weekly provided substantial and sustained reductions in body weight.
Reference:
Study: Triple–Hormone-Receptor Agonist Retatrutide for Obesity — A Phase 2 Trial
Background
- Retatrutide (LY3437943) is an agonist of the glucose-dependent insulinotropic polypeptide, glucagon-like peptide 1, and glucagon receptors.
- Its dose–response relationships with respect to side effects, safety, and efficacy for the treatment of obesity are not known.
Methods
- We conducted a phase 2, double-blind, randomized, placebo-controlled trial involving adults who had a body-mass index (BMI, the weight in kilograms divided by the square of the height in meters) of 30 or higher or who had a BMI of 27 to less than 30 plus at least one weight-related condition. Participants were randomly assigned in a 2:1:1:1:1:2:2 ratio to receive subcutaneous retatrutide (1 mg, 4 mg [initial dose, 2 mg], 4 mg [initial dose, 4 mg], 8 mg [initial dose, 2 mg], 8 mg [initial dose, 4 mg], or 12 mg [initial dose, 2 mg]) or placebo once weekly for 48 weeks. The primary end point was the percentage change in body weight from baseline to 24 weeks. Secondary end points included the percentage change in body weight from baseline to 48 weeks and a weight reduction of 5% or more, 10% or more, or 15% or more. Safety was also assessed.
Results
- We enrolled 338 adults, 51.8% of whom were men.
- The least-squares mean percentage change in body weight at 24 weeks in the retatrutide groups was
- −7.2% in the 1-mg group
- −12.9% in the combined 4-mg group
- −17.3% in the combined 8-mg group
- −17.5% in the 12-mg group
- as compared with −1.6% in the placebo group
- At 48 weeks, the least-squares mean percentage change in the retatrutide groups was
- −8.7% in the 1-mg group
- −17.1% in the combined 4-mg group
- −22.8% in the combined 8-mg group
- −24.2% in the 12-mg group
- as compared with −2.1% in the placebo group.
- At 48 weeks, a weight reduction of 5% or more, 10% or more, and 15% or more had occurred in 92%, 75%, and 60%, respectively, of the participants who received 4 mg of retatrutide; 100%, 91%, and 75% of those who received 8 mg; 100%, 93%, and 83% of those who received 12 mg; and 27%, 9%, and 2% of those who received placebo.
- The most common adverse events in the retatrutide groups were gastrointestinal; these events were dose-related, were mostly mild to moderate in severity, and were partially mitigated with a lower starting dose (2 mg vs. 4 mg).
- Dose-dependent increases in heart rate peaked at 24 weeks and declined thereafter.
Conclusions
- In adults with obesity, retatrutide treatment for 48 weeks resulted in substantial reductions in body weight. (Funded by Eli Lilly; ClinicalTrials.gov number, NCT04881760.)
Reference:
- Jastreboff AM, Kaplan LM, Frías JP, Wu Q, Du Y, Gurbuz S, Coskun T, Haupt A, Milicevic Z, Hartman ML; Retatrutide Phase 2 Obesity Trial Investigators. Triple-Hormone-Receptor Agonist Retatrutide for Obesity - A Phase 2 Trial. N Engl J Med. 2023 Aug 10;389(6):514-526. doi: 10.1056/NEJMoa2301972. Epub 2023 Jun 26. PMID: 37366315.
Study: Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension edit
Aim
- To explore changes in body weight and cardiometabolic risk factors after treatment withdrawal in the STEP 1 trial extension.
Materials and Methods
- STEP 1 (NCT03548935) randomized 1961 adults with a body mass index ≥ 30 kg/m2 (or ≥ 27 kg/m2 with ≥ 1 weight‐related co‐morbidity) without diabetes to 68 weeks of once‐weekly subcutaneous semaglutide 2.4 mg (including 16 weeks of dose escalation) or placebo, as an adjunct to lifestyle intervention. At week 68, treatments (including lifestyle intervention) were discontinued. An off‐treatment extension assessed for a further year a representative subset of participants who had completed 68 weeks of treatment. This subset comprised all eligible participants from any site in Canada, Germany and the UK, and sites in the United States and Japan with the highest main phase recruitment. All analyses in the extension were exploratory.
Results
- Extension analyses included 327 participants.
- From week 0 to week 68, mean weight loss was 17.3% (SD: 9.3%) with semaglutide and 2.0% (SD: 6.1%) with placebo.
- Following treatment withdrawal, semaglutide and placebo participants regained 11.6 (SD: 7.7) and 1.9 (SD: 4.8) percentage points of lost weight, respectively, by week 120, resulting in net losses of 5.6% (SD: 8.9%) and 0.1% (SD: 5.8%), respectively, from week 0 to week 120.
- Cardiometabolic improvements seen from week 0 to week 68 with semaglutide reverted towards baseline at week 120 for most variables.
Conclusions
- One year after withdrawal of once‐weekly subcutaneous semaglutide 2.4 mg and lifestyle intervention, participants regained two‐thirds of their prior weight loss, with similar changes in cardiometabolic variables.
- Findings confirm the chronicity of obesity and suggest ongoing treatment is required to maintain improvements in weight and health.
Reference:
- Wilding JPH, Batterham RL, Davies M, Van Gaal LF, Kandler K, Konakli K, Lingvay I, McGowan BM, Oral TK, Rosenstock J, Wadden TA, Wharton S, Yokote K, Kushner RF; STEP 1 Study Group. Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension. Diabetes Obes Metab. 2022 Aug;24(8):1553-1564. doi: 10.1111/dom.14725. Epub 2022 May 19. PMID: 35441470; PMCID: PMC9542252.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9542252/
Weight and Psychiatric Medications edit
| Antidepressant | Quantitative Weight Change in kg. >12 weeks unless indicated | Author | Study Level | Quality of Study | Quality of Evidence for the Drug | Funding Source | Articles used for ranking |
|---|---|---|---|---|---|---|---|
| Weight gain | |||||||
| Paroxetine | 2.73 CI 0.78 to 4.68* | Serretti [55] | I | B | 1 | U | [55], [66]–[68] |
| Mirtazapine | 2.59 CI –0.23 to 5.41* | Serretti [55] | I | B | 1 | U | [55], [66]–[69] |
| Doxepin | 2.73 | Feighner [70] | III | B | 2 | U | Not ranked, placement based on quantitative data |
| Amitriptyline | 2.24 CI 1.82 to 2.66 | Serretti [55] | I | B | 1 | U | [55], [60], [69] |
| Citalopram | 1.69 CI –0.97 to 4.34 | Serretti [55] | I | B | 1 | U | [55] |
| Nortriptyline | 1.24 CI –0.51 to 2.99 | Serretti [55] | I | B | 1 | U | [55], [60] |
| Clomipramine | 1.0 CI –0.44 to 2.43≤12 weeks | Serretti [55] | I | B | 3 | U | [55] |
| Desipramine | 0.82 CI –0.77 to 2.42≤12 weeks | Serretti [55] | I | B | 3 | U | [55] [64] |
| Imipramine | -0.04 CI –1.36 to 1.28* | Serretti [55] | I | B | 1 | U | [55] [64] Ranking based on expert panel recommendation |
| Duloxetine | 0.71 CI –0.23 to 1.65 | Serretti [55] | I | B | 1 | U | [55] |
| Escitalopram | 0.65 CI –0.16 to 1.45 | Serretti [55] | I | B | 1 | U | [55] |
| Trimipramine | Qualitative data only | Harris [71] | VI | 3 | U | Not ranked | |
| Minimal effect on weight | |||||||
| Venlafaxine | -0.5 CI –0.74 to -0.27≤12 weeks * | Serretti [55] | I | B | 3 | U | [55] |
| Fluvoxamine | -0.02 CI -0.49 to 0.45≤12 weeks | Serretti [55] | I | B | 3 | U | [55] |
| Fluvoxamine CR | Qualitative data only | Davidson [72] | III | B | 1 | D | Not ranked |
| Qualitative data only | Westenberg [73] | III | B | 1 | D | Not ranked | |
| Sertraline | -0.12 CI –1.65 to 1.42 | Serretti [55] | I | B | 1 | U | [55], [67] |
| Trazodone | -0.2 CI -0.94 to 0.54≤12 weeks | Serretti [55] | I | B | 3 | U | [55] |
| Moclobemide | -0.21 CI -0.30 to -0.13≤12 weeks | Serretti [55] | I | B | 3 | U | [55] |
| Fluoxetine | -0.31 CI -1.04 to 0.43 | Serretti [55] | I | B | 1 | U | [55], [66], [67] |
| Desvenlafaxine | -0.8 kg, Minimal effect on weight in both short-term and long term use (12 weeks) | Perry [74] | II | B | 2 | U | Not ranked |
| Weight Loss | |||||||
| Bupropion | -1.87 CI -2.37 to -1.37 | Serretti [55] | I | B | 1 | U | [55] |
*Controversy in the ranking table.
| Antipsychotic | Quantitative Weight Gain | Author | Study Level | Quality of Study | Quality of Evidence for the Drug | Funding Source | Comments |
|---|---|---|---|---|---|---|---|
| Weight gain | |||||||
| Levopromazine | Qualitative data only | Sivaraman [113] | II | A | 2 | I | Similar weight gain as Chlorpromazine, 30 weeks |
| Trifluoperazine | Qualitative data only | Marques [114] | I | A | 1 | I | No difference in wt gain vs Pimozide, 6 studies only 2>12 weeks |
| Loxapine | 18.6% | Chakrabarti [115] | II | A | 1 | I | At 12 weeks vs 0% in placebo |
| Depot flupenthixol decanoate | 62% gained 1.5 to >11 kg | Johnson [116] | IV | C | 3 | U | 6 months: 16% lost 1.5 to 4.9 kg; 22% no change; Similar to fluphenazine decanoate |
| Zuclopenthixol | Qualitative data only | Kumar [117] | I | A | 3 | I | Two studies 10 and 12 weeks: short duration and low N. No difference in weight gain compared to sulpride |
| Paliperidone extended release | 1.5 kg | Chwieduk [118] | I | C | 2 | U | 3–6 wk trials with 52 wk extensions. Olanzapine 3.8 kg |
| Paliperidone injectable | 0.7 kg or 12% (mild) | Citrome [119] | I | B | 2 | U | Open label prior to randomization. |
| 6% | Double blind phase: placebo 3% since randomization. | ||||||
| 13% | I | B | 2 | Open-label extension period (relative to starting the extension phase). Lowest incidence among patients who received double-blind paliperidone – presumably had already gained the weight they were going to. | |||
| Perospirone | Mean Weight Gain: 2.2 kg | Okugawa [120] | III | C | 3 | D | Greater mean weight gain vs risperidone, 1.7 kg |
| Iloperidone | 4.8 kg | Marino [121] | I | C | 2 | U | 52 week duration: Haloperidol 3.0 kg. Weight gain may be dose related. Majority of weight gain occurs in first 6 weeks of treatment. |
| 3.8 kg | Hale [122] | I | C | 2 | U | Haloperidol 2.3 kg; 1 study of 52 weeks | |
| Flunarizine | mean wt gain 1.2 kg or 8% | Bisol [123] | III | A | 1 | I | 12 weeks: Haloperidol -0.8 kg or 7.4% |
| Asenapine | 23% | Citrome [124] | I | B | 2 | D | vs olanzapine, 57.1% in patients with initial BMI <23 |
| 9.3% | I | B | 2 | vs olanzapine, 21.9% in patients with initial BMI >27. Weight gain is not dose related. |
Change in weight caused by mood stabilizers (Ranked most to least weight gain).
| Mood Stabilizer | Author | Study Level | Quality of Study | Quality of Evidence for the Drug | Funding Source | Quantitative Weight Change | Comments |
|---|---|---|---|---|---|---|---|
| Weight Gain and Ranked [77]–[78] | |||||||
| Valproate | Leslie [80] | I | B | 2 | D | 2.5 kg to 1.2 kg | At 12 weeks and 47 weeks respectively. |
| Valproate Extended Release | Smith [125] | I | B | 3 | D | 19/103 | 9 studies (2–6 weeks x 5; 1–12 weeks x 4). Compared to delayed release caused less weight gain 29/103. (not ranked) |
| Lithium | Bowden [79] | III | A | 1 | D | 1.1 kg in lean patients | A randomized, double-blind, placebo-controlled study at 52 weeks. 6.1 kg in obese patients. |
| Weight Neutral | |||||||
| Carbamazepine Extended Release | Ketter [126] | IV | B | 2 | D | Qualitative data only | 26 weeks. Based on one study. |
| Carbamazepine | Melvin [77] | II | B | 3 | I | Qualitative data only | Study duration not provided. |
| Oxcarbazine | Reinstein [127] | III | C | 2 | D | Qualitative data only | 10 weeks |
| Lamotrigine | Bowden [79] | III | A | 1 | D | - 0.5 kg in lean patients | A randomized, double-blind, placebo-controlled study at 52 weeks. -4.2 kg in obese patients. |
| Weight Loss | |||||||
| Topiramate | Stoffers [128] | I | A | 3 | I | Qualitative data only | 3 studies all <12 weeks demonstrate weight loss vs placebo. Many studies have used topiramate for weight loss however, few were done in psychiatric illness. |
| Anxiolytics | Author | Study Level | Quality of Study | Quality of Evidence for the Drug | Funding Source | Quantitative Weight Change | Comments |
|---|---|---|---|---|---|---|---|
| Benzodiazepines – Weight Neutral | |||||||
| Nitrazepam | Oswald [129] | III | B | 2 | U | Qualitative data only | 5 months |
| Chlordiazepoxide | Bjertnaes [130] | VI | NA | 3 | U | Qualitative data only | 6 weeks |
| Lorazepam | Smits [131] | IV | A | 2 | U | Qualitative data only | Cross sectional |
| Diazepam | Smits [131] | IV | A | 2 | U | Qualitative data only | Cross sectional |
| Oxazepam | Smits[131] | IV | A | 2 | U | Qualitative data only | Cross sectional |
| Serotonin 1A Agonists – Weight Neutral | |||||||
| Buspirone | Yuanguang [132] | VI | NA | NA | U | Qualitative data only | 4 weeks |
Reference:
- Dent R, Blackmore A, Peterson J, Habib R, Kay GP, Gervais A, Taylor V, Wells G. Changes in body weight and psychotropic drugs: a systematic synthesis of the literature. PLoS One. 2012;7(6):e36889. doi: 10.1371/journal.pone.0036889. Epub 2012 Jun 15. PMID: 22719834; PMCID: PMC3376099.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3376099/
Study: People With Lowest Physical Functioning Scores Showed Greatest Improvement After Tirzepatide Treatment
Objective
- This post hoc analysis of SURMOUNT trials assessed the association of baseline physical function (PF) with obesity-related complications (ORCs), efficacy measures, and PF. The mechanism of tirzepatide-led improvements in PF was evaluated.
Methods
- Outcomes were assessed among participants (SURMOUNT-1=2539; SURMOUNT-3=579; SURMOUNT-4=670) grouped by baseline quartiles (Q) of SF-36v2 PF scores within study (higher scores=better PF). Least-squares mean changes from baseline in efficacy measures and PF were estimated using ANCOVA. Pearson's correlation between weight reduction and improvement in PF was calculated.
Results
- In SURMOUNT-1, participants with lower baseline PF had more ORCs. Tirzepatide-treated participants showed similar reductions in weight (kg; −20.1% to −22.8%), waist circumference (−17.2 to −20.2cm), and BMI (−7.2 to −9.0kg/m2) across quartiles.
- Participants with lower baseline PF reported greater improvements in PF with tirzepatide (Q1=12.5; Q4=−0.8).
- Results were similar in SURMOUNT-3 and SURMOUNT-4. A weak to mild correlation was noted between weight reduction and improved PF; the strength of correlation decreased from Q1 to Q4.
Conclusions
- Lower baseline PF was associated with a higher prevalence of ORCs.
- Patients taking tirzepatide experienced substantial weight loss, regardless of their baseline PF.
- Tirzepatide may improve PF through both weight loss-dependent and -independent mechanisms, especially in those with lower baseline PF.
Reference:
Study: Obesity as a Risk Factor for Autoimmune Diseases: A Systematic Review and Meta-Analysis
Objective
- Obesity is characterized by a proinflammatory condition contributing to poor outcomes, but its association with autoimmunity is inconclusive. To fill this gap in knowledge, we searched PubMed and Embase for studies analyzing the association between obesity and the prevalence and/or incidence of autoimmune diseases.
Methods
- Adjusted odds ratios (OR) or hazard ratios (HR) with 95% CI relating to the prevalence or incidence of autoimmune diseases in people with BMI >30, compared to BMI <25, were pooled using generic inverse variance and fixed effect models. Of 1,311 records, 26 (8 cross-sectional and 18 longitudinal) studies were included in the meta-analysis.
Results
- Obesity, compared with normal weight, was associated with increased prevalence of rheumatoid arthritis and psoriasis (OR=1.11 [1.06, 1.16], p<0.00001; OR=1.35 [1.14, 1.59], p=0.0004, respectively) and increased risk of developing rheumatoid arthritis (HR=1.30 [1.15, 1.49], p<0.0001), psoriasis (HR=1.18 [1.16, 1.20], p<0.00001), multiple sclerosis (HR=1.49 [1.25, 1.77], p<0.00001), and Crohn's/ulcerative colitis (HR=1.35 [1.11, 1.65], p<0.003).
- Obesity was also significantly associated with incidence of any autoimmune disease (HR=1.41 [1.24, 1.62], p<0.00001).
Conclusions
- Although definitive conclusions are still precluded for the single diseases, overall evidence supports obesity as a risk factor for autoimmunity.
Reference:
- I. Spatocco, G. Mele, G. De Rosa, et al., “ Obesity as a Risk Factor for Autoimmune Diseases: A Systematic Review and Meta-Analysis,” Obesity (2025): 1–15, https://doi.org/10.1002/oby.70044.
Wegovy Studies
STEP 1 Study
- Design
- 1961 adults with obesity or overweight with 1 comorbidity
- No DM patients
- Randomized 2:1
- In conjunction with reduced calorie diet and incrased physical activity
- Baseline:
- Mean body weight: 232.4 lbs
- Mean BMI: 37.9
- Weight loss
- Wegovy -14.9%
- Placebo -2.4%
- Clinically meaningful weight loss at 68 wks
- Wegovy 83.5%
- Placebo 31.1%
- 10% Weight loss at 68 wks
- Wegovy 66.1%
- Placebo 12%
- 15% Weight loss at 68 wks
- Wegovy 47.9%
- Placebo 4.8%
- 20% Weight loss at 68 wks (~46 lbs)
- Wegovy 30.2%
- Placebo 1.7%
Study: Addition of Phentermine-Topiramate to a Digitally Enhanced Lifestyle Intervention: A Double-Blind Randomized Clinical Trial
Objective
- This study compared the effects of phentermine-topiramate-ER (mid-dose 7.5/46 mg) versus placebo on weight loss and cardiovascular disease (CVD) risk outcomes when used as an adjunct to a digitally enhanced lifestyle intervention (DELI).
Methods
- We conducted a 12-month, randomized, double-blind, placebo-controlled trial at a single tertiary academic center in the United States (June 2020–June 2022). Eighty participants with obesity (BMI ≥ 30 kg/m2) were enrolled in the DELI program, consisting of in-person and telehealth modalities, dietary and physical activity goals, and use of a smartphone application integrated with digital devices (Apple Watch and Bluetooth-enabled weight scale and blood pressure monitor). Participants were randomized 1:1 to receive either phentermine-topiramate-ER (n = 42) or placebo (n = 38) in addition to the DELI.
Results
- At 3 months, the phentermine-topiramate group lost a mean of 10.82 kg versus 4.04 kg in the placebo group (mean difference −6.78 kg; p = 0.002).
- At 12 months, weight loss was 15.32 kg versus 5.85 kg, respectively (mean difference −9.48 kg; p < 0.001).
- Participants receiving phentermine-topiramate-ER experienced a 3.35% reduction in the estimated atherosclerotic CVD risk compared to baseline (p = 0.004).
Conclusions
- Phentermine-topiramate-ER, when combined with a DELI, produced significant and sustained weight loss and reduced CVD risk in adults with obesity.
Reference:
- Campos, A., Ghusn, W., Cifuentes, L., Sacoto, D., Fansa, S., Anazco, D., Ricardo-Silgado, M.L., Hashem, A., Schaefer, M., Harmsen, W.S., Gunn, H.J., Peterson, C., Larsen, D., Varghese, S.T., Hurtado, M.D. and Acosta, A. (2026), Addition of Phentermine-Topiramate to a Digitally Enhanced Lifestyle Intervention: A Double-Blind Randomized Clinical Trial. Obesity (Silver Spring). https://doi.org/10.1002/oby.70108
Study: Weight regain after cessation of medication for weight management: systematic review and meta-analysis
Notes:
- What is already known on this topic
- The development of highly effective weight management medications (WMMs) has transformed the treatment of obesity
- Real world observations estimate that around 50% of people with obesity discontinue WMMs within 12 months
- A previous systematic review quantified and compared the rate of weight regain with behavioural weight management programmes (BWMPs)
- What this study adds
- People on average regain weight at a rate of 0.4 kg/month after cessation of WMMs, leading to a projected return to baseline weight after 1.7 years
- Although weight loss resulted in improvements in HbA1c, fasting glucose, total cholesterol, triglycerides, systolic and diastolic blood pressure, all markers returned to baseline within 1.4 years of treatment cessation
- The rate of weight regain after the cessation of WMMs was faster than after the cessation of BWMPs, independent of the amount of weight lost during treatment
Abstract
Objectives
- To quantify and compare the rate of weight regain after cessation of weight management medications (WMMs) in adults with overweight or obesity.
Design
- Systematic review and meta-analysis.
Study
- selection Trial registries and databases (Medline, Embase, PsycINFO, CINAHL, Cochrane, Web of Science, and trial registries) were searched from inception until February 2025 for randomised controlled trials (RCTs), non-randomised trials, and observational studies that included WMM (≥8 weeks) with follow-up for ≥4 weeks after cessation of treatment in adults with overweight or obesity. Comparators were any non-drug weight loss intervention or placebo.
Data extraction and synthesis
- The review followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines. Two independent reviewers screened titles, extracted data, and assessed the risk of bias using the Cochrane Risk of Bias 2 tool for RCTs and the ROBINS-I tool for non-randomised trials. Data were analysed using mixed effect, meta-regression, and time-to-event models. Weight regain after cessation of WMM was compared with that reported after cessation of behavioural weight management programmes (BWMPs).
Main outcome measures
- The primary outcome was rate of weight regain from end of treatment, with associated changes in cardiometabolic markers as a secondary outcome.
Results
- Of the 9288 titles screened, 37 studies (63 intervention arms, 9341 participants) were included. Average treatment duration was 39 (range 11-176) weeks, with average follow-up of 32 (4-104) weeks. The average monthly rate of weight regain was 0.4 kg (95% confidence interval (CI) 0.3 to 0.5) (mixed model 0.3 kg (0.2 to 0.4) monthly v control in RCTs).
- All cardiometabolic markers were projected to return to baseline within 1.4 years after the cessation of WMM.
- Weight regain was faster after WMM than after BWMP (by 0.3 kg (0.22 to 0.34) monthly), independent of initial weight loss. Estimates and precision were robust in sensitivity analyses.
Conclusions
- This review found that cessation of WMM is followed by rapid weight regain and reversal of beneficial effects on cardiometabolic markers. Regain after WMM was faster than after BWMP. These findings suggest caution in short term use of these drugs without a more comprehensive approach to weight management.
Reference:
- West S, Scragg J, Aveyard P, Oke JL, Willis L, Haffner SJP, Knight H, Wang D, Morrow S, Heath L, Jebb SA, Koutoukidis DA. Weight regain after cessation of medication for weight management: systematic review and meta-analysis. BMJ. 2026 Jan 7;392:e085304. doi: 10.1136/bmj-2025-085304. PMID: 41500720.
Study: Energy expenditure and obesity across the economic spectrum
Notes:
- Humans burn roughly the same number of calories per day regardless of activity level.
- Exercise improves health, but it doesn’t provide the calorie “bonus” people expect. What and how much you eat is what moves the needle on weight.
Significance Economic development is associated with increased prevalence of obesity and related health problems, but the relative importance of increased caloric intake and reduced energy expenditure remains unresolved.
We show that daily energy expenditures are greater in developed populations, and activity energy expenditures are not reduced in more industrialized populations, challenging the hypothesis that decreased physical activity contributes to rises in obesity with economic development.
Instead, our results suggest that dietary intake plays a far greater role than reduced expenditure in the elevated prevalence of obesity associated with economic development.
Abstract
- Global economic development has been associated with an increased prevalence of obesity and related health problems. Increased caloric intake and reduced energy expenditure are both cited as development-related contributors to the obesity crisis, but their relative importance remains unresolved.
- Here, we examine energy expenditure and two measures of obesity (body fat percentage and body mass index, BMI) for 4,213 adults from 34 populations across six continents and a wide range of lifestyles and economies, including hunter-gatherer, pastoralist, farming, and industrialized populations.
Results:
- Economic development was positively associated with greater body mass, BMI, and body fat, but also with greater total, basal, and activity energy expenditure.
- Body size–adjusted total and basal energy expenditures both decreased approximately 6 to 11% with increasing economic development, but were highly variable among populations and did not correspond closely with lifestyle.
- Body size–adjusted total energy expenditure was negatively, but weakly, associated with measures of obesity, accounting for roughly one-tenth of the elevated body fat percentage and BMI associated with economic development.
Conclusions
- In contrast, estimated energy intake was greater in economically developed populations, and in populations with available data (n = 25), the percentage of ultraprocessed food in the diet was associated with body fat percentage, suggesting that dietary intake plays a far greater role than reduced energy expenditure in obesity related to economic development.
Reference:
- A. McGrosky,A. Luke,L. Arab,K. Bedu-Addo,A.G. Bonomi,P. Bovet,S. Brage,M.S. Buchowski,N. Butte,S.G. Camps,R. Casper,D.K. Cummings,S. Krupa Das,S. Deb,L.R. Dugas,U. Ekelund,T. Forrester,B.W. Fudge,M. Gillingham,[…] & The IAEA DLW Database Consortium, Energy expenditure and obesity across the economic spectrum, Proc. Natl. Acad. Sci. U.S.A. 122 (29) e2420902122, https://doi.org/10.1073/pnas.2420902122 (2025).
Trauma/Emergency
Anaphylaxis
Common Triggers for Anaphylaxis
- Medications (21% to 58.8%):
- Antibiotics (most commonly beta-lactams 4%)
- Nonsteroidal anti-inflammatory drugs (7% to 12%)
- Chemotherapy agents (2%)
- Allopurinol
- ACE inhibitors
- ASA
- Biologic modifiers (e.g., interferon)
- Opioids
- Foods (32% to 37%):
- Eggs (1% to 4%)
- Fish/shellfish (10% to 15%)
- Milk (2% to 10%, highest in infants)
- Peanuts (2% to 13%)
- Tree nuts (7% to 12%)
- Insect venom (15.2% to 25%):
- Hymenoptera stinging insects (e.g., bees, wasps, fire ants)
- Idiopathic anaphylaxis (11% to 19.5%)
- Occupational allergens:
- Food allergens, medications, bee stings, tick bites, natural rubber latex (2.6% to 6.2%), and chemicals (e.g., dyes, bleaches, insecticides, fungicides, iodine, chlorhexidine)
- Physical factors (rare):
- Cold, heat, exercise (2%), sunlight
- Radiocontrast media (1% to 5%)
Differential Diagnosis of Anaphylaxis
- Flush syndrome
- Autonomic epilepsy
- Carcinoid
- Medullary carcinoma of the thyroid
- Perimenopausal hot flashes
- Red man syndrome (i.e., adverse reaction to vancomycin)
- Hypotension
- Cardiogenic shock
- Hypovolemic shock
- Septic shock
- Vasovagal reaction
- Miscellaneous
- Anxiety, panic attacks
- Hereditary angioedema
- Leukemia with excess histamine production
- Systemic mastocytosis
- Postprandial collapse
- Airway foreign body
- Monosodium glutamate ingestion
- Scombroid fish poisoning
- Sulfite ingestion
- Respiratory distress with wheezing or stridor
- Aspiration of a foreign body
- Asthma and chronic obstructive pulmonary disease exacerbation
- Vocal cord dysfunction syndrome
References:
- AFP Sep 2020 Vol 102 No 6
Management
Outpatient Setting
- First line: EPInephrine auto injector
- Adjunctive:
- Bronchodilator
- Histamine H1 antagonist (diphenhydramine 1-2mg/Kg/dose)
- Histamine H2 blocker (cimetidine 1-2mg/Kg/dose)
- Corticosteroids (prednisone 1mg/Kg)
- Vasopressors for refractory hypotension
- Glucagon for refractory hypoglycemia
- Atropine for bradicardia
- Supplemental O2
- IV Fluids
- Place patient in recumbent position
Hospital setting
- First line: Epi auto injector
- Adjunctive:
- Bronchodilator
- Histamine H1 antagonist (diphenhydramine)
- Supplemental O2
- IV Fluids
- Place patient in recumbent position
Discharge
- Epi pen
- H1 antagonist every 6hrs for 2-3 days
- H2 blocker twice a day for 2-3 days
- Corticosteroid: prednisone daily for 2-3 days
References:
- AFP Vol 6 No 1 Jul 2012
Basics
ABCDEs
- A - Airway
- B - Breathing
- C - Circulation
- D - Disability/GCS
- E - Exposure/Environment
AMPLE History:
- A - Allergies
- M - Meds
- P - PMH
- L - Last Meal
- E - Events
GCS
Glascow Coma Score:
- Eyes: 4
- Verbal: 5
- Motor: 6
Low GCS Differential Diagnosis:
- AEIOUTIPS:
- A - Allergies
- E - Epilepsy
- I - Infection
- O - Overdose
- U - Underdose
- T - Trauma
- I - Insulin
- P - Psych
- S - Stroke
Trauma Labs
- CBC
- Type/Cross
- ABG
Trauma Radiology
- CXR,
- Pelvis,
- C-spine (lat)
Rapid Sequence intubation (RSI)
- Sedation:
- Etomidate 0.3mg/kg or 30mg or
- Midazolam 2-5mg IV
- Paralysis
- Succinylcholine 1-2mg/kg (usually 100mg)
Stroke
- AMS
- Droop
- Arm drift
- Any 1/3 is 72% sensitivity
Human Trafficking
Red Flags
- Inconsistent or scripted history
- Discrepancy between story and observations
- Appears much younger than stated age
- Doesn't know current city and can't give address
- Minor trading sex for something of value (food, shelter, drugs, money)
- Unusually high number of sexual partners
- Seasonally or situationally inapporpriate clothing
- Carrying large amounts of cash (or none at all)
Ref: FMX 2016
Intervention
- Provide the patient with NHTRC hotline number and encourage call.
- 888-3737-888
- Life threatening danger:
- Follow institutional policies Partner with patient when possible
- Provide resources for services, reporting
- Safety assessment as part of discharge process
- Disclosure and exam findings must be documented accurately
Ref: FMX 2016
Resources
- National Human Trafficking Resource Center
- 888-3737-888
- Text "befree"
- nhtrc@polarisproject.org
- National Center for Missing and Exploited Children
- 800-THE-LOST
- ICE victim assistance program
- 866-872-4973
- Polaris Project
- HEAL Trafficking
- Physicians Against the Trafficking of Humans (PATH)
Ref: FMX 2016
Hypothermia and Frostbite
Swiss Staging System for Hypothermia
| Stage | Symptoms | Suspected core temperature |
|---|---|---|
| I | Conscious and shivering | 89.6 to 95°F (32 to 35°C) |
| II | Altered mental status, not shivering | 82.4 to 89.6°F (28 to 32°C) |
| III | Unconscious, not shivering, vital signs present | 75.2 to 82.4°F (24 to 28°C) |
| IV | No vital signs | < 75.2°F (< 24°C) |
Traditional Frostbite Grading System
- First degree (superficial)
- Edema, pallor, and erythema; slightly raised plaque; no blisters; absent to minimal tissue loss
- Second degree (superficial)
- Clear blisters with edema and erythema; absent to minimal tissue loss; blisters develop 6 to 24 hours after rewarming1
- Third degree (deep)
- Hemorrhagic blisters suggest subcutaneous or dermal involvement; black eschar develops over weeks; tissue loss
- Fourth degree (deep)
- Muscle and/or bone involvement; mummification and gangrene; full-thickness tissue loss; absence of blisters in deep frostbite is a poor prognostic factor1
Frostbite Grading System Immediately After Rewarming
| Grade | Presentation | Prognosis and management |
|---|---|---|
| I | Absence of cyanosis and blisters | 99mTc scintigraphy not necessary Amputation unlikely |
| II | Cyanosis restricted to distal phalanx, clear blisters at 48 hours | 99mTc scintigraphy at 48 hours: decreased uptake Risk of tissue loss; hypoxemia and injury at higher elevation (4,000 m [13,000 ft]) increase risk; consider treating as grade III or IV in these scenarios |
| III | Cyanosis on proximal phalanx, hemorrhagic blisters at 48 hours | 99mTc scintigraphy at 48 hours: absence of radiotracer High risk of amputation |
| IV | Cyanosis on carpal/tarsal, hemorrhagic blisters at 48 hours | 99mTc scintigraphy at 48 hours: absence of radiotracer 100% risk of amputation |
Management:
- Only rewarm if no risk of refreezing
- Rapid rewarming via water bath immersion and IV low-molecular weight dextran leads to improved outcomes
- PO ibuprofen should be started as soon as available and continued until surgery or recovery
- Tissue plasminogen activator improves outcomes for deep frostbite extending to proximal interphalangeal joints if given within 24 hours
References:
- AFP Vol 100 No 11 Dec 2019
- AFP Vol 101 No 7 Apr 2020
Inflight Emergencies
Recommended response:
- Introduce yourself and state medical qualifications
- Ask passenger for permission to treat, if feasible
- Request access to the medical kit or automated external defibrillator, as needed
- Use a language interpreter, if necessary, but be aware of patient privacy.
- Take a patient history, perform a focused physical examination, and obtain vital signs.
- Administer treatments within the scope of their qualifications, with the patient remaining seated, when possible
- Recommend diversion of the flight if the patient's medical condition is critical
- Communicate and coordinate with ground-based medical resources
- Continue to provide care until the emergency medical condition is stabilized or care is transferred to other qualified medical personnel.
- Document the patient encounter
References:
- NEJM 373;10 Sep 2015
Intimate Partner Violence
National Resources
- Futures Without Violence
- National Coalition Against Domestic Violence
- http://www.ncadv.org
- Online tool for safety plan
- National Domestic Violence Hotline
- 1-800-799-SAFE
- http://www.ndvh.org
- Help with safety planning and crisis interventions
Assessment of immediate safety for domestic violence victims.
- Are you in immediate danger?
- Is your partner at the health facility now?
- Do you want to or have to go home with your partner?
- Do you have somewhere safe to go?
- Have there been threats or direct abuse of the children if applicable?
- Are you afraid your life might be in danger?
- Has the violence gotten worse or is it getting scarier? Is it happening more often?
- Has your partner used weapons, alcohol or drugs?
- Has your partner ever held you or your children against your will?
- Does your partner ever watch you closely, follow you or stalk you?
- Has your partner ever threatened to kill you, him or herself or your children?
References:
- AFP Vol 94 No 8 Oct 2016
Principles of Rapid Tranquilization
- Limit diagnostic tests to:
- Finger stick glucose
- Pulse ox
- Consider sustance abuse and adverse effects of previous treatments, especially benzos and barbituates
- Treat any immediate identifiale causes
- Initiate rapid tranquilization with one of the following in order of preference:
- Haloperidol 2.5-10mg IM or IV
- Chlorpromazine 25-50mg PO or IM
- Olanzapine 2.5-10mg IM
- Ziprasidone 10-20mg IM
References:
- AFP Vol 77 No 3 Feb 2008
Routine steps for possible fractures
- Perform and document neurovascular exam by testing and immediately addressing any deficiency:
- capillary refill
- pulses
- sensation
- Carefully inspect the skin for:
- Wounds that may indicate open fracture
- Tenting of skin over displaced fracture
- Devitalized skin that may necrose
- Common fracture findings (e.g. swelling , ecchymosis)
- Less common findings (eg. deformity, fracture blisters)
- Palpate for point tenderness
- Evaluate nearby joints/structures
- Be alert for signs/symptoms of compartment syndrome including disproportionate pain
References:
- AFP Vol 76 No 6 Sep 2007
Sexual assault
Testing After Sexual Assault
- Urine pregnancy
- All survivors
- On presentation Repeat if missed menses
- Nucleic acid amplification testing for gonorrhea and chlamydia from all sites of penetration or attempted penetration
- All survivors
- On presentation Repeat in one to two weeks if not treated or symptomatic
- Nucleic acid amplification testing for Trichomonas vaginalis
- All survivors
- On presentation Repeat in one to two weeks if not treated or symptomatic
- Wet mount for bacterial vaginosis
- Symptomatic survivors
- On presentation Repeat if symptomatic
- Serum HIV
- All survivors
- On presentation Consider repeat at six weeks, three months, and six months if assailant status unknown
- Serum hepatitis B antigen
- All survivors
- On presentation Repeat at six months
- Serum rapid plasma reagin for syphilis
- All survivors
- On presentation Consider repeat at four to six weeks and three months if assailant status unknown
- Serum hepatitis C
- All survivors
- On presentation Consider repeat at three and six months if assailant status unknown
- Urine drug screen (include chloral hydrate, gamma hydroxybutyrate, ketamine [Ketalar], and benzodiazepines)
- When concern for drug-facilitated sexual assault such as partial or complete amnesia
- On presentation if within 72 hours of assault
Victims Services Center
- Refer patients for up to 120 hours after a sexual assault for a forensic exam.
- They provide free prophylactic medications, support and counseling.
- They have RNs for the exams, and they are certified to do the forensic testing for prosecution.
Contact info
- VSC hot line: (407) 497-6701
- https://www.victimservicecenter.org/
References:
- AFP Feb 2021 Vol 103 No 3
Urology
Acute simple cystitis in women (Simple UTI)
The preferred agents for empiric therapy of acute simple cystitis are (favorable balance between efficacy and adverse effects - including the risk of selecting for resistant organisms):
- First Line
- nitrofurantoin monohydrate/macrocrystals
- Dosed at 100 mg orally twice daily for five days.
- trimethoprim-sulfamethoxazole
- Dosed as one double-strength tablet (160/800 mg) orally twice daily for three days.
- fosfomycin
- Dosed as 3 grams of powder mixed in water as a single oral dose.
- if available, pivmecillinam
- Dosed as 400 mg orally twice daily for five to seven days.
- nitrofurantoin monohydrate/macrocrystals
- Alternative antimicrobial options
- oral beta-lactams (other than pivmecillinam) are appropriate options (5-7 days)
- amoxicillin-clavulanate (500 mg twice daily)
- cefpodoxime (100 mg twice daily)
- cefdinir (300 mg twice daily)
- cefadroxil (500 mg twice daily)
- If beta-lactams cannot be used, a fluoroquinolone is reasonable (3 days)
- ciprofloxacin (250 mg twice daily or 500 mg extended release daily)
- levofloxacin (250 mg daily)
- oral beta-lactams (other than pivmecillinam) are appropriate options (5-7 days)
If an Enterococcus or Group B Streptococcus grows as the only isolate on culture and is determined to be the cause of cystitis, amoxicillin is usually the preferred agent, as long as the isolate is susceptible.
References:
- UpToDate.com
Bladder Cancer
See also: Hematuria
Signs and Symptoms:
- Hematuria (gross or microscopic)
- Irritative symptoms
- Dysuria
- Frequency
- Nocturia
- Urge incontinence
- Urgency
- Obstructive symptoms
- Decreased force of stream
- Feeling of incomplete voiding
- Intermittent stream
- Straining
- Signs and symptoms of metastases
- Abdominal, bone, flank, or pelvic pain
- Anorexia
- Cachexia
- Lower extremity edema
- Renal failure
- Respiratory symptoms
- Suprapubic palpable mass
Survival by stage
| Tumor stage | 5yr survival rate |
|---|---|
| All | 76% |
| In situ | 96% |
| Localized | 70% |
| Regional | 35% |
| Distant | 5% |
| Unknown | 46% |
Reference:
- AFP Vol 96 No 8 Oct 2017
BPH
Medication plan:
- First Line:
- tamsulosin 0.4 mg 30 min before same meal daily
- PDE-5 inhibitors (with and without ED)
- Second Line:
- dutasteride 0.5 mg daily
- Anticholinergis
Reference:
- AFP Vol 107 No 6 Jun 2023
Prostate screening (PSA)
| Effect | Number |
|---|---|
| Invited | 1000 |
| Number with 1 positive PSA | 240 |
| >1 transrectal prostate biopsy | 220 |
| Hospitalized for biopsy complication | 2 |
| Diagnosed with prostate ca | 100 |
| Initial radical prostatectoy or radiation therapy | 65 |
| Initial active surveillance | 30 |
| Initial active surveillance then active therapy | 15 |
| With sexual dysfunction who received initial or deferred treatment | 50 |
| With urinary incontinence who received initial or deferred treatment | 15 |
| Men who avoided metastatic prostate ca | 3 |
| Men who died of causes other than prostate ca | 200 |
| Men who died of prostate ca despite screening, diagnosis, and treatment | 5 |
| Men who avoided dying of prostate ca | 1.3 |
| Benefit/Harm | Men Screened | Men Treated |
|---|---|---|
| Avoiding death | 0.1% | 1.6% |
| Avoiding met ca | 0.3% | 3.8% |
| Developing Urinary incontinence | 1.5% | 18.8% |
| Developing Sexual dysfunction | 5% | 62.5% |
There is still no evidence of mortality benefit from prostate cancer screening asymptomatic men in the PLCO Cancer screening trial (after almost 20 years)
References:
- JAMA Vol 319 No 18 May 2018
- AFP Vol 97 No 9 May 2018
- AFP Vol 98, No 8 Oct 2018
Common Causes of Abnormal Urine Coloration
| Color | Pathologic causes | Food and drug causes |
|---|---|---|
| Cloudy | Phosphaturia, pyuria, chyluria, lipiduria, hyperoxaluria | Diet high in purine-rich foods (hyperuricosuria) |
| Brown | Bile pigments, myoglobin | Fava beans |
| Levodopa (Larodopa), metronidazole (Flagyl), nitrofurantoin (Furadantin), some antimalarial agents | ||
| Brownish-black | Bile pigments, melanin, methemoglobin | Cascara, levodopa, methyldopa (Aldomet), senna |
| Green or blue | Pseudomonal UTI, biliverdin | Amitriptyline (Elavil), indigo carmine, IV cimetidine (Tagamet), IV promethazine (Phenergan), methylene blue, triamterene (Dyrenium) |
| Orange | Bile pigments Phenothiazines, phenazopyridine (Pyridium) | |
| Red | Hematuria, hemoglobinuria, myoglobinuria, porphyria | Beets, blackberries, rhubarb |
| Phenolphthalein, rifampin (Rifadin) | ||
| Yellow | Concentrated urine | Carrots |
| Cascara |
Reference:
- Am Fam Physician. 2005;71(6):1153-1162
Urine Color
Color:
- Brown
- Hemolysis
- Metastatic melanoma
- Porphyria
- Black
- Alcaptonuria
- Metastatic melanoma
- Porphyria
- White
- Chyluria
- Filiariasis
- Hypercalciuria
- Hyperoxaluria
- Lipiduria
- Lymphatic fistula
- Phosphaturia
- Proteinuria
- Pyuria due to UTI
- Schistosomiasis
- Urinary tuberculosis
- Blue or Green
- Biliverdin
- Blue diaper syndrome (familial benign hypercalcemia)
- Hartnup disease
- Porphyria
- Psuedomonas UTI
- Purple
- Purple urine bag syndrome
References:
- AFP Vol 94 No 7 Oct 2016
Erectile Dysfunction
Workup:
- H&P
- Labs: Fasting BG, Lipids, TSH, Total Testosterone
- Optional Laboratory Testing:
- CBC
- Free Testosterone
- Luteinizing hormone
- Prolactin levels
- Sex hormone-binding globulin test
- Urinalysis
- Optional Laboratory Testing:
- If medical etiology, maximize treatment:
- CAD
- DM
- Hormonal disorders (hypogonadism, hypothyroidism)
- HLD
- HTN
- Metabolic syndrome
- Neurologic conditions (Alzheimers, MS, etc)
- Obesity
- Vascular disease
- If no medical etiology:
- Screen for psychological causes
- Anxiety
- Depression
- Guilt
- H/o sexual abuse, marital or relationship problems
- Stress
- Refer for behavioral therapy
- Remove negative psychosocial factor(s)
- Screen for psychological causes
Treatment
- First line:
- Lifestyle
- Increase exercise
- Smoking cessation
- Pharmacotherapy
- PDE-5 inhibitors
- Testosterone supplementation if clinical hypogonadism
- Lifestyle
- Second line:
- Intraurethral or intracavernosal alprostadil
- Vacuum pump devices
- Consider referral to urologist for implantable device
Risk Factors:
- Advancing Age
- Cardiovascular disease
- Smoking
- DM
- History of pelvic irradiation or surgery
- Hormonal disorders
- HLD
- HTN
- Illicit drug use
- Medications
- Obesity
- Psychological conditions
- Sedentary lifestyle
- Venous leakage
Medications and Substances that can Cause ED
- Analgesics
- Opiates
- Anticholinergics
- TCAs
- Antidepressants
- Lithium
- MOA I
- SSRI
- TCA
- Antihistamines
- diphenhydramine, hydroxyzine, meclizine, promethazine
- Antihypertensivees
- Alpha blocers, BB, clonidine
- Anti-parkinson agents
- bromocriptine, levodopa
- Cardiovascular agents
- digoxin, gemfibrozil
- Diuretcs
- spironolactone, thiazides
- Hormones
- 5-alpha reductase inhibitors, corticosteroids, estrogens, progesterone
- Alcohol, nicotine, illicits
- amphetamines, barbituates, cocaine, heroin, marijuana
- Immunomodulators
- interferon-alfa
- Tranquilizers
- benzodiazepines, phenothiazines
References:
- AFP Feb 2010 Vol 81, No 3
Hematuria
See also: Bladder Cancer
Asymptomatic microscopic hematuria
Definition:
- >= 3 RBCs per HPF on properly collected urinalysis
- In absence of benign cause:
- Infection
- Menstruation
- Vigorous exercise
- medical renal disease
- Virla illness
- Trauma
- Recent urologic procedure
- Workup recommended regardless of anticoagulation status
Workup:
- Low risk
- Shared decisionmaking between:
- Repeat urinalysis in 6 mo
- Renal ultrasound
- Shared decisionmaking between:
- Intermediate risk
- Cystoscopy and renal ultrasound
- High risk
- Cystoscopy and axial upper tract imaging
- CT urogram (preferred) but MRI urogram or renal ultrasound and retrograde pyelograms if contraindication to both CT and MRI
- Cystoscopy and axial upper tract imaging
- If neg workup - repeat urinalysis in 12 mo
- If neg, discontinue further evaluation
- If pos, initiate shared decision making regarding need to pursue additional evaluation
Microscopic Hematuria Risk Stratification System
| Low risk (Meets all criteria) | Intermediate risk (Meets any 1 criteria) | High risk (Meets any 1 criteria) |
|---|---|---|
| Women (<50yo); Men (<40 yo) | Women (50-59yo); Men (40-59yo) | Women or Men >60 yo |
| Never smoker or <10 pack yr | 10-30 pack yr smoking history | >30 pack year smoking history |
| 3-10 RBCs/HPF in single UA | 11-25 RPBs/HPF on single UA | >25 RBCs/HPF on single UA |
| No risk factors | Low risk pt with no prior evaluation and 3-10 RBC/HPF on repeat UA | History of gross hematuria |
| Additional risk factors |
Risk factors:
- Irritative lower urinary tract symptoms
- Prior pelvic radiation therapy
- Prior cyclophasphamide/ifosfamide chemotherapy
- Family history of urothelial cancer or Lynch syndrome
- Occupational exposures to benzene chemicals or aromatic amines (rubber, petrochemicals, dyes)
- Chronic indwelling foreign body in the urinary tract
Dipstick positive for blood:
- Microscopic urinalysis:
- <3 RBC
- Repeat UA 3 times at 6wk intervals
- Negative - No additional work-up
- Repeat UA 3 times at 6wk intervals
- >3 RBC or positive on a repeat UA
- Assess for UTI and other benign causes (vigorous exercise, menstruation, recent procedure)
- Repeat UA 6 weeks after treatment or discontinuation of contributing factor
- Negative - No additional work-up
- Positive - Renal function testing to assess for medical renal disease (dysmorphic RBC, cellular casts, proteinuria)
- Positive - Nephrology referral
- Negative - Assess for risk factors for malignancy, contraindications to radiation, renal insufficiency
- High risk for malignancy and/or Good renal function, no allergy or contraindication to radiation
- CT and Urology referral
- Cystoscopy
- Negative - annual UA for 2 years
- Positive - Treat
- Cystoscopy
- CT and Urology referral
- Low risk for malignancy or renal insufficiency, radiation sensitivity, allergy
- Less optimal imaging like MRI, Non-contrast CT, and Urology referral
- High risk for malignancy and/or Good renal function, no allergy or contraindication to radiation
- <3 RBC
References:
- AFP Vol 96 No 8 Oct 2017
- JAMA Nov 2020 Vol 324, No 19
Gross hematuria
Definition
- Visible blood in urine
- Color ranges from dark brown/orange to bright red
- May contain clots
- Rule out benign causes
- Workup recommended regardless of anticoagulation status
Workup
- Cystoscopy for bladder evaluation
- Axial upper tract imaging:
- CT urogram (preferred) but MRI urogram or renal ultrasound and retrograde pyelograms if contraindication to both CT and MRI
References:
- JAMA Nov 2020 Vol 324, No 19
Incontinence edit
Referral Indications
- Symptoms or physical exam concerning for neurologic disease
- Lifelong history of incontinence
- Recurrent symptomatic UTI
- Pelvic organ prolapse beyond the hymen
- Elevated postvoid residual (>1/3 total volume or 100mL in Adults)
- Long-term catheterization
- Difficulty passing a urethral catheter
- Diagnostic uncertainty or poor improvement with treatment
- Dominant symptom of pain
- Sterile hematuria
Management
- Urge: The 3 main categories of drugs used to treat urge incontinence include anticholinergic drugs, antispasmodics, and TCAs.
- Stress: Sympathomimetic drugs, estrogen, and TCAs increase bladder outlet resistance to improve symptoms of stress urinary incontinence.
- Pharmacologic therapy for stress incontinence and an overactive bladder may be most effective when combined with a pelvic exercise regimen
Medications
- Anticholinergic Agents
- First-line medicinal therapy in women with urge incontinence
- Inhibit the binding of acetylcholine to the cholinergic receptor, thereby suppressing involuntary bladder contraction of any etiology
- dicyclomine blocks the action of acetylcholine at parasympathetic sites in secretory glands and smooth muscle.
- Darifenacin is an extended-release product eliciting competitive muscarinic receptor antagonistic activity. It reduces bladder smooth muscle contractions.
- Solifenacin elicits competitive muscarinic receptor antagonist activity, which results in anticholinergic effects and inhibition of bladder smooth muscle contraction
- Tolterodine is a competitive muscarinic receptor antagonist for overactive bladder. However, it differs from other anticholinergic types in that it has selectivity for urinary bladder over salivary glands.
- Alpha-Adrenergic Agonists
- midodrine, desglymidodrine, is an alpha1-agonist that may increase bladder outlet resistance
- Antispasmodic Drugs
- oxybutynin have both an anticholinergic and a direct smooth muscle relaxant effect on the urinary bladder. In addition, oxybutynin provides a local anesthetic effect on the irritable bladder.
- Flavoxate is used for symptomatic relief of dysuria, urgency, nocturia, and incontinence, as may occur in cystitis, prostatitis, urethritis, and urethrocystitis/urethrotrigonitis
- TCAs
- Imipramine 75 mg qhs
- A typical TCA, imipramine facilitates urine storage by decreasing bladder contractility and increasing outlet resistance. It has an alpha-adrenergic effect on the bladder neck and an antispasmodic effect on the detrusor muscle. Imipramine also has a local anesthetic effect on bladder mucosa.
- amitriptyline
- A TCA with sedative properties, amitriptyline increases the circulating levels of norepinephrine and serotonin by blocking their reuptake at nerve endings. It ineffective for use in urge incontinence but is extremely effective in decreasing symptoms of urinary frequency in women with pelvic floor muscle dysfunction. Amitriptyline restores serotonin levels and helps break the cycle of pelvic floor muscle spasms. It is well tolerated and effective in the majority of women with urinary frequency.
- Imipramine 75 mg qhs
- Beta3 Agonists
- Mirabegron (Myrbetriq) or Vibegron (Gemtesa)
- Indicated for overactive bladder (OAB) with symptoms of urge urinary incontinence, urgency, and urinary frequency
- Mirabegron (Myrbetriq) or Vibegron (Gemtesa)
- Estrogens
- Conjugated estrogens increase the tone of urethral muscle by up-regulating the alpha-adrenergic receptors in the surrounding area, and they enhance alpha-adrenergic contractile response to strengthen the pelvic muscles
- Conjugated estrogen may be used as an adjunctive pharmacologic agent for postmenopausal women with stress or mixed incontinence.
- Oral or vaginal form of estrogen may be used.
- The usual oral dose is 0.3-1.25 mg taken daily in a cyclic regimen.
- Alpha-Adrenergic Blockers
- Used to decrease bladder overactivity
- Patients who have decentralized or autonomous bladders as the result of myelodysplasia, spinal cord injury, or radical pelvic surgery.
- Phenoxybenzamine
- decreases bladder contractions through long-lasting, noncompetitive, alpha-adrenergic blockade of postganglionic synapses at smooth muscle and exocrine glands.
- Prazosin decreases internal sphincter tone and can improve the flow of urine, improving emptying of bladder. Although doses greater than 20 mg/d usually do not increase efficacy
References:
- JAMA Vol 318 No 16 Oct 2017
- https://emedicine.medscape.com/article/452289-medication#1
Urinary Incontinence in Women
Pelvic floor muscle training:
- Video instruction: https://youtu.be/kQKR5uLkeUM
- Participant perceived cure after 8-12 weeks: NNT: 3.7; ARR = 26.7%
- Participant perceived cure after 6-8 weeks: NNT: 2.5; ARR = 39.9%
- Leakage episodes in 24hrs (after 8-12 weeks):
- Expect 1.06 to 2.5 episodes per 24 hrs
- Mean reduction of 1 episode per 24 hrs (0.64 to 1.37)
Reference:
- AFP Vol 101 No 7 Apr 2020
Infertility (Male)
See also: Infertility
Modifiable Risk Factors:
- Alcohol use
- Exposure to toxic chemicals
- Illicit drug use
- Obesity
- Smoking
- Varicocele
Evaluation:
- Semen Analysis
Reference:
- AFP Vol 107 No 6 Jun 2023
Interstitial Cystitis and Bladder Pain Syndrome
- Initial assessment
- Myofascial tenderness on pelvic floor muscle exam
- Refer to pelvic floor physical therapy
- Infection or other pelvic pathology for symptoms
- Treat identified disease (like UTI, nephrolithiasis)
- Labs:
- Urinalysis
- Urine culture
- Myofascial tenderness on pelvic floor muscle exam
- Conservative management
- Symptom diary
- Titrate level of hydration, bladder volume, frequency of voids to improve symptoms
- Food diary
- Diet modification
- Stress reduction
- Avoid bladder irritants (acidic foods, coffee/tea, carbonation, alcohol)
- Symptom diary
- Multidisciplinary and/or referral
- Musculoskeletal or neurologic pelvic pain: Physical medicine and rehab
- Endometriosis, vulvodynia, menorrhagia: Gynecology
- Hematuria, voiding symptoms: Urology
- Pelvic organ prolapse, incontinence: Urogynecology
- Psychiatric comorbiditis, history of abuse: psychology psychiatry
- Irritable bowel syndrome: gastroenterology
Things you can do to help with your symptoms:
- Symptom diary
- Titrate level of hydration, bladder volume, frequency of voids to improve symptoms
- Food diary
- Diet modification
- Stress reduction
- Avoid bladder irritants (acidic foods, coffee/tea, carbonation, alcohol)
References:
- JAMA Vol 322 No 24 Dec 2019
Bladder retraining edit
- SCHEDULE BATHROOM VISITS Once you've determined how frequently you use the bathroom, you add 15 minutes to that time. Let's say you go to the bathroom ever hour. During retraining, you will aim to go every hour and fifteen minutes. Even if you don't have to go, you still want to make the trip to the bathroom. This trains the brain and body. After a set number of days, gradually increase the amount of time between bathroom breaks.
- DELAY URINATION Easier said than done. But when you feel the need to go, try holding off for at least 5 minutes. Then 10. And so on until you can make it 3-4 hours between urination. The key will be to stay on schedule, which keeps the training on track.
PERFORM KEGEL EXERCISES By strengthening the muscles that are directly and indirectly involved with urination, you will be able to better control when you have to go. For a full guide on how to do kegel exercises, click here. And men, Kegels are for you, too – click here for a guide specifically to help you do them as well.
Sometimes, it's the simplest of things that can make a massive difference. To improve your success with bladder retraining, you can also try these tips:
- Limit beverages that increase urination, including caffeinated drinks like sodas, coffee, and tea (click here to see more about diet and exercise tips for bladder control)
- Drink less fluid before bedtime
- Go to the bathroom before you go to bed at night, and as soon as you get up in the morning
Kegels:
- To do a Kegel:
- Squeeze the muscles you normally use to stop the flow of urine.
- Hold the contraction for five seconds, and then relax for five seconds.
- Gradually increase to 10-second contractions with 10 seconds of rest in between.
- Work up to doing three sets of 10 contractions each day.
- Women who can't find the right muscles to squeeze during a Kegel can either insert a finger into the vagina to feel the muscles contract or ask a doctor about trying biofeedback.
Reference:
Bladder Irritants edit
The seven MOST IRRITATING are listed first:
- All alcoholic beverages
- Cigarettes/Tobacco
- Cola drinks
- Tea
- Artificial Sweeteners
- Chocolate
- Coffee
Other possible irritants include:
- Fruits (and their juices): cranberries, grapes, oranges, lemons, peaches, pineapple, plums, apples, and cantaloupe
- Vegetables: onions, tomatoes, chilies, peppers
- Milk/Dairy: aged cheese, sour cream, yogurt
- Grains: rye & sourdough breads
- Seasonings: spices & spicy food, especially peppers, acidic foods and beverages, walnuts & peanuts, vinegar
List of Common Bladder Irritants (*Most people are not sensitive to ALL of these products; your goal is to find the foods that make YOUR symptoms worse):
- Alcoholic beverages
- Apples and apple juice
- Cantaloupe
- Carbonated beverages
- Chili and spicy foods
- Chocolate
- Citrus fruit
- Coffee (including decaffeinated)
- Cranberries and cranberry juice
- Grapes
- Guava
- Milk Products: milk, cheese, cottage cheese, yogurt, ice cream
- Peaches
- Pineapple
- Plums
- Strawberries
- Sugar especially artificial sweeteners, saccharin, aspartame, corn sweeteners, honey, fructose, sucrose, lactose
- Tea
- Tomatoes and tomato juice
- Vitamin B complex
- Vinegar
Certain foods and drinks have been associated with worsening symptoms of urinary frequency, urgency, urge incontinence, or bladder pain. If you suffer from any of these conditions, you may wish to try eliminating one or more of these foods from your diet and see if your symptoms improve. If bladder symptoms are related to dietary factors, strict adherence to a diet that eliminates the food should bring marked relief in 10 days.
Once you are feeling better, you can begin to add foods back into your diet, one at a time.
If symptoms return, you will be able to identify the irritant.
As you add foods back to your diet it is very important that you drink significant amounts of water.
Substitutions:
- Low-acid fruit substitutions include apricots, papaya, pears and watermelon.
- Coffee drinkers can drink Kava or other lowacid instant drinks.
- Tea drinkers can substitute non-citrus herbal and sun brewed teas.
- Calcium carbonate co-buffered with calcium ascorbate can be substituted for Vitamin C.
- Prelief is a dietary supplement that works as an acid blocker for the bladder.
Reference:
- https://www.ichelp.org/understanding-ic/diet/foods-to-avoid/
- https://www.ichelp.org/wp-content/uploads/2022/07/AUA-IC-Guideline-2022.pdf
- https://www.hopkinsmedicine.org/johns_hopkins_bayview/_docs/medical_services/gynecology_obstetrics/bladder_irritants.pdf
- https://www.brighamandwomens.org/assets/BWH/obgyn/pdfs/bladder-irritants.pdf
Male Hormones 2025
Basic Men's Hormone:
- Testosterone (Free, Bioavailable, and Total)
- Sex Hormone-Binding Globulin (SHBG)
- Albumin
Expanded panel includes:
- Estradiol
- Prolactin
Symptoms of low testosterone in men can include:
- Decrease in sex drive
- Difficulty getting or maintaining an erection
- Decrease in muscle mass
- Bone weakness
- Breast tissue development
- Hair loss
- Difficulty sleeping
- Difficulty with memory and concentration
- Decrease in testicle size
- Decrease in semen production that can lead to fertility problems
Symptoms of high testosterone in men can include:
- Elevated blood pressure
- Heart or liver problems
- Headaches
- Aggressive behavior
- Excessive body hair growth
- Acne
- Prostate enlargement
- Decrease in sperm production
- Insomnia
Reference:
Men's Health
- General Stats
- 12.2% of men >18yo are in fair or poor health
- 14.7% <65yo who do not have health insurance
- 18.9% of men >18yo smoke cigarettes
- 32.6% of men >20yo have HTN
- 34.5% of men >20yo are obese
- Single biggest reason men go to the doctor - women in their lives
- Random recent study results
- Long term testosterone in not linked with aggressive prostate cancer.
- Frequent ejaculation is linked to decreased prostate cancer risk.
- Men who ejaculate more frequently in adulthood (21x/mo vs 4-7x/mo) are 19% less likely to develop prostate ca
- Observed in all age groups
- Daily sugary drinks raise men's heart failure risk by 23%
References:
- Consultant Jun 2016
- Gallup
- Eur Urol. https://doi.org/10.1016/j.eurouro.2016.03.027
Nephrolithiasis
| Stone location | Common symptoms |
|---|---|
| Kidney | Vague flank pain, hematuria |
| Proximal ureter | Renal colic, flank pain, upper abdominal pain |
| Middle section of ureter | Renal colic, anterior abdominal pain, flank pain |
| Distal ureter | Renal colic, dysuria, urinary frequency, anterior abdominal pain, flank pain |
Complications of Urolithiasis
- Renal failure
- Ureteral stricture
- Infection, sepsis
- Urine extravasation
- Perinephric abscess
- Xanthogranulomatous pyelonephritis
| Stone location and size | Probability of passage (%) |
|---|---|
| Proximal ureter | |
| >5 mm | 0 |
| 5 mm | 57 |
| <5 mm | 53 |
| Middle section of ureter | |
| >5 mm | 0 |
| 5 mm | 20 |
| <5 mm | 38 |
| Distal ureter | |
| >5 mm | 25 |
| 5 mm | 45 |
| <5 mm | 74 |
Management:
- tamsulosin 0.4 mg capsule daily
- Increase fluids
- Pain management
Clinical recommendations:
- Nonsteroidal anti-inflammatory drugs are the first choice for pain relief in patients with kidney stones. SOR: A
- Alpha blockers are the first choice for medical expulsive therapy in patients with kidney stones. SOR: A
- Increasing fluid intake does not relieve pain or accelerate passage of kidney stones. SOR: B
- Patients at low risk of stone recurrence should not routinely undergo extensive metabolic evaluation. SOR: C
- Patients should increase daily fluid intake to 2.5 to 3 L per day to prevent recurrence of kidney stones. SOR: A
- Thiazide diuretics, potassium citrate, or allopurinol should be prescribed after recurrence of calcium stones, even in the absence of metabolic abnormalities. SOR: A
Reference:
- Am Fam Physician. 2001;63(7):1329-1339
- Am Fam Physician. 2019;99(8):490-496
- Increased fluid intake to achieve urine output of >2L is recommended for prevention
- If increased fluid does not prevent nephrolithiasis, treatment with thiazide, citrate, or allopurinol is recommended
Reference:
- AFP Vol 92, No 4 Aug 2015
Do not prescribe tamsulosin or nifedipine for stone expulsion in patients with ureteral stones <10mm (SOR A)
Reference:
- JFP Vol 65 No 2 Feb 2016
Nocturia
Associated with:
- Increased risk of falls and fractures
- Cognitive impairment
- Depressed mood
4 categories:
- Increased nighttime urine production
- Decreased storage ability
- Incomplete bladder emptying
- Primary sleep disorder
Initial workup:
- Assess urinary symptoms
- Fluid intake
- Comorbidities
Testing:
- Urinalysis for all patients.
- BP
- Bladder diary for 2-3 days (Freq/Vol)
- 24hr Urine (eval for nocturnal polyuria)
Lifestyle modifications
- Limitation of fluid intake, especially in the evening
- Addressing timing of diuretic intake
- Sleep hygiene
Pharmacotherapy should target the etiology of nocturia such as:
- Nocturnal polyuria
- Overactive bladder
- Benign prostatic hyperplasia
- Genitourinary syndrome of menopause
Patients with refractory symptoms should be referred for further treatment.
Reference:
- Am Fam Physician. 2025;111(6):515-523B
Prostate Specific Antigen (PSA)
See also:
PSA testing should be performed only after a comprehensive discussion of the risks and benefits of prostate cancer screenings.
- A single baseline PSA level is suggested for all men aged 40 to 45.
- Annual testing is reasonable in higher-risk men starting at 45.
- A change of >0.75 ng/mL per year or >25% is considered suspicious.
- At least 2 separate elevated PSA tests are required to confirm the increase.
- Routine screening should be discontinued in men with a life expectancy of 10 years or less based on comorbidities or by the age of 75.
- Men who fall outside of guidelines but are fully informed and are requesting testing should have a PSA level performed.
- PSA screening is not recommended for men who do not benefit from testing or refuse treatment if cancer is detected.
- High-risk individuals include those men with the following:
- African descent
- Lynch syndrome
- Family history of prostate cancer, especially if a first-degree relative was diagnosed before 65
- Family history of multiple malignancies
- PSA density of 0.15 or higher
- Positive germline testing for BRCA1 and BRCA2
Magnetic resonance imaging (MRI) can also be used to detect prostate cancer.
- MRI can also miss about 25% of clinically significant malignancies.
- The increasing use of MRI scans and risk stratification bioassays can eliminate 25% to 30% or more of low-yield biopsies by better identifying patients unlikely to have clinically significant (Gleason grade 4) disease.
The 95th percentile PSA value is commonly used for the age-adjusted normal reference ranges in men:
- 40-49: ≤2.5 ng/mL
- 50-59: ≤3.5 ng/mL
- 60-69: ≤4.5 ng/mL
- 70-79: ≤6.5 ng/mL
When the total PSA is between 4 and 10 ng/mL, free % PSA can be used
- The higher the free % PSA, the lower the risk of cancer.
- The actual cancer risk varies according to age.
- If the free % PSA is <10%, the cancer risk is 50%.
- If the free % PSA is >25%, the cancer risk is <10%.
Prostate-Specific Antigen Velocity:
- A slow increase in PSA level is expected over time, but a more rapid rise could indicate malignancy.
- Generally, a yearly increase in PSA of no more than 0.75 ng/mL higher per year and no more than 25% is considered acceptable.
- More significant increases are considered suspicious.
- Calculating the PSA velocity requires 3 separate PSA determinations over at least 18 months.
Prostate-Specific Antigen Doubling Time:
- Aggressive, rapidly growing prostate cancers are more dangerous than slow-growing malignancies, which can be estimated using the PSA doubling time in patients with known prostate cancer.
- A PSA doubling time of 2 years or longer is generally considered reasonably acceptable.
- As the PSA doubling time becomes shorter, the 5-year prostate cancer mortality rate increases.
- A PSA doubling time longer than 12 months is associated with a 5-year prostate cancer-specific death rate of 10% compared to those with a doubling time of 1 year or less who have a 50% mortality.
- If the PSA doubling time is less than 3 months, the prostate cancer mortality rate is 20 times greater.
- A higher Gleason score tends to lower the survival rate as well.
Reference:
- David MK, Leslie SW. Prostate-Specific Antigen. [Updated 2024 Sep 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557495/
Semen
Semen analysis from Quest: https://www.questhealth.com/product/yo-male-fertility-at-home-test-kit-3-pack-K0003M.html
| Parameter | Normal |
| pH | 7.2-7.8 |
| Volume | 1.5 ml |
| Total Count | 39 million |
| Concentration | >=15 Million sperm/mL (less = oligozoospermia) |
| Motility | >=40% Forward progression (less=ashenozoospermia) |
| Morphology | >=4% Normal forms (less=teratospermia) |
| WBC Count | <1 Million/mcL |
References:
- JAMA Jul 2021 Vol 326 No 1
Study: Efficacy of Clomiphene Citrate Versus Enclomiphene Citrate for Male Infertility Treatment: A Retrospective Study
Introduction
- Infertility and hypogonadism in males can greatly affect their reproductive health and overall well-being. Since exogenous testosterone administration for hypogonadism management may disrupt the normal hormonal cascade necessary for spermatogenesis, clomiphene citrate (CC) and enclomiphene citrate (EC) are medications often used to manage hypogonadism and male infertility.
- This study aims to directly compare the effects of CC and EC on serum testosterone levels and semen parameters in men to determine which medication may have an advantage in managing these conditions.
Materials and methods
- We retrospectively analyzed ≥18-year-old men presenting with primary infertility, abnormal semen parameters, or hypogonadism who received CC or EC monotherapy for at least three months between January 2021 and December 2022.
- We compared baseline and follow-up hormone levels, semen parameters, and demographics. Variables were compared using paired and unpaired t-tests. Significance was assessed at p<0.05.
Results
- A total of 46 men received EC and 32 men received CC.
- The median age was 42 (IQR: 34-47.75) years in men who received EC and 41 (IQR: 36-44) years in men who received CC (p=0.450).
- The two treatment groups exhibited a significant increase in serum total testosterone, while only EC had a statistically significant increase in FSH and LH.
- Semen volume and concentration did not significantly change with either treatment. Sperm motility increased in both groups, but total motile sperm count (TMSC) only significantly increased in men who received EC.
Conclusions
- Our study found that EC and CC are effective treatments in increasing total testosterone without negatively affecting spermatogenesis.
- EC demonstrated to be more effective in raising gonadotropin levels and TMSC.
Reference:
- Thomas J, Suarez Arbelaez MC, Narasimman M, Weber AR, Blachman-Braun R, White JT, Ledesma B, Ghomeshi A, Jara-Palacios MA, Ramasamy R. Efficacy of Clomiphene Citrate Versus Enclomiphene Citrate for Male Infertility Treatment: A Retrospective Study. Cureus. 2023 Jul 6;15(7):e41476. doi: 10.7759/cureus.41476. PMID: 37546076; PMCID: PMC10404117.
Uncomplicated cystitis
See also:
Treatment:
- fosfomycin 3g single dose
- nitrofurantoin 100 mg bid 5d
- TMP-SMX bid 3d
- Second line
- Fluroquinolones
- Amoxicillin
Urinary Tract Infections
| Symptom | Prob UTI | Liklihood | ||
|---|---|---|---|---|
| Pos | Neg | Pos | Neg | |
| Pos Nitrites | 85% | 36% | 5.5 | 0.56 |
| Self diagnosis | 80% | 9.1% | 4.0 | 0.1 |
| Pos Hematuria | 63% | 47% | 1.7 | 0.89 |
| Urgency & Dysuria | 60% | 31% | 1.5 | 0.44 |
| Pos Leukocytes | 58% | 29% | 1.4 | 0.40 |
| Dysuria | 56% | 40% | 1.3 | 0.67 |
| Urgency | 55% | 43% | 1.2 | 0.75 |
| Frequency | 52% | 41% | 1.1 | 0.71 |
Recommendations:
- Adequate fluid intake 1.5L/d and cranberry products are effective in preventing UTI (LOE B)
- Menthenamine hippurate is effective in preventing recurrent UTI (LOE B)
- Diagnose an uncomplicated UTI in women who believe they have a UTI and report typical acute lower urinary symptoms without vaginal discharge (LOE C)
For Uncomplicated Acute Cystitis and Recurrent UTI's:
- 1st Line:
- Trimethoprim/sulfamethoxazole
- 160/800 mg bid for 3d
- 93% effectiveness; 24.2% resistance
- Nitrofurantoin
- 100 mg bid for 5d
- 93% effectiveness; 1.6% resistance
- Fosfomycin
- 3-g packet one time
- 91% effectiveness; 0.6% resistance
- Trimethoprim/sulfamethoxazole
- 2nd Line (Flouroquinolones):
- Ciprofloxacin
- 250mg bid for 3d
- 90% effectiveness; 17% resistance
- Levofloxacin
- 250-500mg daily for 3d
- 90% effectiveness; 6% resistance
- Ciprofloxacin
- Alternatives:
- Amoxicillin/clavulanate
- 500/125mg bid for 3d
- 89% effectiveness
- Cefaclor
- 250mg tid for 5d
- 89% effectiveness
- Cefdinir
- 300mg bid for 5d
- 89% effectiveness
- Cefpodoxime
- 100mg bid for 3d
- 89% effectiveness
- Cephalexin
- 500mg bid for 7d
- 89% effectiveness
- Amoxicillin/clavulanate
Reference:
- AFP Vol 93 No 7 Apr 2016
- AFP Feb 2024 Vol 109 No 2
Prophylaxis for recurrent UTI
Common agents used:
- Nitrofurantoin 50-100mg daily (continuous)
- Nitrofurantoin 100mg (postcoital)
- Trimethoprim/sulfamethoxazole 40/200mg daily or 40/200mg 3/wk (continuous)
- Trimethoprim/sulfamethoxazole 40/200mg or 80/200mg (postcoital)
Occassionally used:
- Cephalexin 125-250mg daily (continuous)
- Cephalexin 250mg daily (postcoital)
References:
- AFP Vol 93 No 7 Apr 2016
Weight Management/ABCD
Adiposity Based Chronic Disease (ABCD)
ObesityDefinition: Excess adiposity that may impair health.- Framework components:
- Anthropometric - uses BMI as a screening tool that requires further confirmation Fill out: central adiposity by examination and waist circumference
- Clinical - identifies the presence and severity of obesity complications
The Obesity ABCD Algorithm
- Identify appropriate patients
- Assess risk with history, physical, labs
- Assess and screen for depression, sleep, eating, and mood disorders
- Treat comorbidities and other health risks
- Lifestyle modification
- Nutrition - Reduce energy intake
- Physical Activity - Increase activity
- Cognitive behavior therapy
- Pharmacotherapy +/- bariatric surgery
Reference:
- AFP Dec 2023 Vol 108 No 6
5 A's of discussing Obesity/ABCD
- Ask if you can discuss weight and the health impact of ABCD
- Assess health status and complications
- Advise on treatment options based on severity of ABCD
- Agree on treatment plan and goals for weight loss
- Assist in the ongoing process of weight management and reassessment of goals and treatment options
Reference:
- AFP Dec 2023 Vol 108 No 6
Weight Loss Success Strategies
- Emphasize more weight loss in the first 3 months
- Advise patients to consume fewer calories and eat more nonglycemic fruits and vegetables
- Lower glycemic vegetables: most vegetables except: corn, potatoes, and peas
- Strongest benefit with berries, apples, pears, tofu or soy, califlower, and cruciferous and green leafy vegetables
- Encourage patients to eat at home and to avoid processed foods
- Eating at a restaurant associated with excess of ~200 kcal/meal
- Emphasize the importance of eating breakfast and increasing protein intake (1.2g/Kg)
- Breakfast daily
- Lower fat diet
- Fewer calories (1500 kcal/d)
- Underscore importance of self monitoring
- Encourage patients to spend more time exercising
- Focus on moving 1 hr/d or 200-300 min/wk
- Resistance not shown to be helpful for weight loss but might be helpful for weight maintenance
- Work with patients to ensure sound sleep hygeine
- 7-8 hrs/night - like 10p-6a
- Address sleep apnea
- Start a trial of medical therapy
- Address mental health challenges
- Bupropion can be first line
- Encourage patients to modify old habits and adopt new ones
References:
- JFP Jan/Feb 2020 Vol 69, No 1
National Weight Control Registry
The researchers behind the study found that people who have had success losing weight have a few things in common:
- They weigh themselves at least once a week.
- They restrict their calorie intake, stay away from high-fat foods, and watch their portion sizes.
- They also exercise regularly.
"Pretend you didn't exercise at all," she said. "You will most likely compensate anyway, so think of exercising just for health improvement but not for weight loss."
- (1) - Identify appropriate patients who need to lose weight
Obesity classification and disease risk relative to normal weight and waist circumference
NIH
| Class | BMI | Stage | <40" M | >40" M |
|---|---|---|---|---|
| <35" F | >35" F | |||
| Underweight | <18.5 | - | - | - |
| Normal | 18.5-24.9 | - | - | - |
| Overweight | 25-29.9 | - | Incr | High |
| Obesity | 30-34.9 | I | High | Very High |
| 35-39.9 | II | Very High | Very High | |
| >40 | III | Ext High | Ext High |
Ref:
- National Heart, Lung, and Blood Institute Classification of overweight and obesity by BMI, waist circumference, and associated disease risks. 2013
Edmonton Obesity Staging
| Stage | Obesity Related RF | Example | Patient Health Risks |
|---|---|---|---|
| 0 | None | None | |
| 1 | Subclinical | Pre-DM, Pre-HTN | Mild |
| 2 | Established | HTN, DM OSA, GERD | |
| PCOS, Anxiety | Moderate | ||
| 3 | Establised End-Organ | MI, HF, DM complication | Significant |
| Damage | Arthritis | ||
| 4 | Severe Disabilities | End-stage disabilities | Severe |
Abdominal Obesity - Waist
| Ethnic background | Size |
|---|---|
| USA | Male >40in (102cm) |
| Female >35in (88cm) | |
| Europids (Caucasians) | Male >37in (94cm) |
| Female >31in (80cm) | |
| S Asians, Chinese, Japanese | Male >35in (90cm) |
| Female >31in ( 80cm) |
Ref:
- Sharma Int J Obes 2009
- OMA Review Course 2016
Lifestyle History
- Nutrition:
- Fruits and veggies
- Eating out
- Beverages
- Snacks
- 24hr food recall
- Pleased with food eaten?
- Cooking skills
- Time and money constraints
- Physical Activity:
- Exercise vs physical activity
- Minutes/Intensity/Frequency
- Daily Screen Time: Work and Recreation
- Sleep:
- Number of hours of sleep
- Easily fall asleep?
- Rested in the morning?
- Stress
- Social Connections
- Screen time
Ref:
- FMX 2016
Predictors of successful weight loss
- High level of physical activity (90% exercise for 1hr a day)
- Continued calorie restriction (Avg 1380kcal/day)
- 78% eat breakfast
- More likely to eat 5x/day
- Self monitoring - weighing or counting calories
Ref:
- National weight control registry
Unexplained weight loss
Involuntary weight loss producing a significant health risk:
- ≥ 5% weight loss in 30 days
- ≥ 7.5% weight loss in 90 days
- 10% weight loss in 180 days
- (2) - Physical Assessment
Risk assessment:
- BMI
- Waist circumference
- Co-morbidities
Body Composition
Definitions:
- Total Body Fat Percentage (%BF): The percent of the body that is composed of fat. This will change based on the amount of fat there is as well as the amount of lean mass there is.
- Fat Mass Index (FMI): The total amount of fat you have (in kilograms) relative to your height (in meters2). It is a measure of how much total fat you have, relative to your size and independent of lean mass.
- Visceral Adipose Tissue (VAT): VAT is a hormonally active component of total body fat. The measurement reflects the amount of internal abdominal fat around the organs. This is different than subcutaneous fat, which lies beneath the skin. Increased VAT has a high correlation to cardiovascular and metabolic disease risk. Current research shows and elevated risk at around 100-160 cm2 and
- Android to Gynoid Ratio: The "apple" to "pear" shape ratio. It describes where the fat is stored. Android (apple shape) refers to having most of the fat around the stomach and mid-section. Gynoid (pear shape) refers to having the fat stored around the hips. A bigger number means more android and a smaller number means more gynoid. From a health risk standpoint, ideal values are believed to be less than 0.8 for women and 1.0 for men.
- Fat Free Mass Index (FFMI): The amount of mass that is not fat, relative to your height. This includes muscle, bone, organs and connective tissue. It can be used to gauge relative muscle mass in lean individuals.
- Skeletal Muscle Mass (SMM): An estimate of the total amount of skeletal muscle you have. Because muscle has approximately the same density as other organs (liver, skin, etc…) and other types of muscle (heart, smooth muscle, etc…) we are not able to directly the amount of skeletal muscle you have. This is true of any commercially available body composition measurement (bioelectrical impedance, underwater weighing). However, several scientific studies have been performed that demonstrate good accuracy between our estimated SMM and that measured by MRI or CT scanning.
- Skeletal Muscle Mass Percentage (%SMM): The percent of the body that is composed of skeletal muscle. Like %BF, this number is relative to your total mass.
- Appendicular Lean Mass to Height Ratio (ALM/Height2): The amount of lean mass in the arms and legs relative to height. A low ALM/Ht2 is a risk factor for sarcopenia (low muscle mass), primarily in lean individuals. Cut points in research are generally around 5.5 for women and 7.0 for men.
- Appendicular Lean Mass to BMI Ratio (ALM/BMI): The amount of lean mass in the arms and legs relative to Body Mass Index. This can also be used as a risk factor for sarcopenia and is more relevant than ALM/ht2 in overweight individuals. Cut points in research are generally around 0.51 for women and 0.79 for men.
- Resting Metabolic Rate (RMR): The number of calories the body needs to maintain its current mass under resting conditions. The value provided by the DXA scan is estimated from the amounts of different tissues, and tissue specific metabolic rates. It can be thought of as the "ideal" RMR, given an individual's body size and composition.
- Bone Density: Shows how dense the bones are and can be used to assess the risk of osteopenia and osteoporosis. The z-score compares your bone density to what is normal for people similar in age and body size. The t-score compares your bone density to that of a 30-year-old. Anything higher than -1.0 is representative of normal bone density. Between -1.0 and -2.5 is a risk for osteopenia. Anything under -2.5 is a risk for osteoporosis.
Reference:
Body fat
Tools:
- Bioelectrical Impedance
- Air plethysmography
Abdominal obesity:
- Waist circumference >40in (102cm) in men
- Waist circumference >35in (88cm) in women
- Women:
- >31% Obesity
- 25-31% Acceptable
- 21-24% Fitness
- 14-20% Athletic
- < 13% Essential fat levels
- Men:
- >24% Obesity
- 18-24% Acceptable
- 14-17% Fitness
- 6-13% Athletic
- < 2-5% Essential fat levels
- Waist to Hip Ratio - Measure at the superior border of the iliac crest.
- Women:
- >0.8
- Men:
- >1:1
- Women:
TO DETERMINE LEAN/FAT MASS
- Fat mass: Weight x body fat percentage
- Lean mass: Weight - (weight x body fat percentage)
Body composition
- Use Indirect calorimetry
- Resting energy rate
- Measures O2 consumption, CO2 production
- Respiratory exchange ratio (RER = VCO2/VO2)
Consider as Alternatives for BMI edit
What should we use instead?
Rather than seeing BMI as the primary diagnostic test for determining a person's health, it should be used in conjunction with other measures and considerations.
Since researchers know belly fat around our vital organs carries the most health risk, waist circumference, waist-to-hip ratio or waist-to-height ratio offer more accurate measurements of health.
Waist circumference: is an effective measure of fat distribution, particularly for athletes who carry less fat and more muscle. It's most useful as a predictor of health when combined with the BMI. Waist circumference should be less than 94cm for men and 80cm for women for optimal health, as measured from halfway between the bottom of your ribs and your hip bones.
Waist-to-hip ratio: calculates the proportion of your body fat and how much is stored on your waist, hips, and buttocks. It's the waist measurement divided by hip measurement and according to the World Health Organisation it should be 0.85 or less for women, and 0.9 or less in men to reduce health risks. It's especially beneficial in predicting health outcomes in older people, as the ageing process alters the body proportions on which BMI is founded. This is because fat mass increases and muscle mass decreases with age.
Waist-to-height ratio: is height divided by waist circumference, and it's recommended a person's waist circumference be kept at less than half their height. Some studies have found this measure is most strongly correlated with health predictions.
Body composition and body fat percentage can also be calculated through skinfold measurement tests, by assessing specific locations on the body (such as the abdomen, triceps or quadriceps) with skin callipers.
Additional ways to gauge your heart health include asking your doctor to monitor your cholesterol and blood pressure. These more formal tests can be combined with a review of lifestyle, diet, physical activity, and family medical history.
How to measure your waist
- Find the top of your hip bone and the bottom of your ribs.
- Breathe out normally.
- Place the tape measure midway between these points, in line with your belly button, and wrap it around your waist loose enough to fit one finger inside the tape.
- Check your measurement.
Results:
- Men: Over 94cm (about 37 inches)*
- Women: Over 80cm (about 31.5 inches)*
Other ways:
- Dual Energy X-ray Absorptiometry (DEXA)
- X-ray beams pass through different body tissues at different rates. So DEXA uses two low-level X-ray beams to develop estimates of fat-free mass, fat mass, and bone mineral density. (1) DEXA is typically only used for this purpose in research settings.
- Strengths
- Accurate
- Limitations
- Equipment is expensive and cannot be moved
- Cannot accurately distinguish between different types of fat (fat under the skin, also known as "subcutaneous" fat vs. fat around the internal organs, or "visceral" fat)
- Cannot be used with pregnant women, since it requires exposure to a small dose of radiation
- Most current systems cannot accommodate individuals with a BMI of 35 or higher
- Computerized Tomography (CT) and Magnetic Resonance Imaging (MRI)
- These two imaging techniques are now considered to be the most accurate methods for measuring tissue, organ, and whole-body fat mass as well as lean muscle mass and bone mass. (1) CT and MRI scans are typically only used for this purpose in research settings.
- Strengths
- Accurate
- Allows for measurement of specific body fat compartments, such as abdominal fat and subcutaneous fat
- Limitations
- Equipment is extremely expensive and cannot be moved
- CT scans cannot be used with pregnant women or children, due to the high amounts of ionizing radiation used
- Some MRI and CT scanners may not be able to accommodate individuals with a BMI of 35 or higher
Reference:
- Waist-to-height ratio as an indicator of 'early health risk': simpler and more predictive than using a 'matrix' based on BMI and waist circumference
- Keep the size of your waist to less than half of your height, updated NICE draft guideline recommends
- Waist Circumference and Waist–Hip Ratio (WHO)
- Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity
- Central fatness and risk of all cause mortality: systematic review and dose-response meta-analysis of 72 prospective cohort studies
Focused Physical Exam
- Vitals: Use appropriate cuff size
- General appearance: clothing, self care, hygiene
- Habitus: distribution (central, gynoid)
- HEENT: periorbital edema, tongue, mucosa, parotid, Mallampoti score, dentition, neck size, thyroid, buffalo hump fat pad, retracted jaw, facial hair including eye brows, hirsutism
- Heart: Rhythm (PACs, AF), murmur
- Lungs: Asthma, hypoventilation
- Chest: Gynecomastia, irritation under breasts
- Abdomen: scars, striae, pannus, liver size, hernia
- MSK: atrophy, ROM, limitations, amputations
- Neuro: reflexes, balance
- Extremities: edema, dry cracking, ulcers, varicosities
- Gait: funtion, stability
- Skin: hirsutism, acne, Cushingoid, acrochordons, acanthosis nigricans, infection, psoriasis, rash, self mutilation, bruising
- Mental: motivation, mood, energy, insight, comprehension
Labs
Medical Weight Loss:
- Glucose, A1c
- BUN, Cr, Electrolytes
- Transaminases
- Lipid profile
- Hs C-Reactive protein
- Uric acid
- CBC
- TSH
- Urine/microalbumin
- Pregnancy
- Vitamin D
- Testosterone (Men)
Surgical Weight Loss:
- Medical labs
- H. pylori
- Fe, Ferritin
- B12, Folate, B 1
- 25(OH) Vit D
- Ion calcium, PTH
- 24 hr urine Ca
- Cu, zinc, selenium prn
Ref:
- Mechanic Endocr Pract 2013
Malnutrition Key Signs/Symptoms
- B1 (thiamine): wet beriberi (CVD), dry Wernicke-Korsakoff syndrome (ataxia, neuropathy, mental confustion)
- B2 (riboflavin): anemia, mout/lip/skin disorders
- B3 (niacin): Pellagra: demenia, diarrhea, dermatitis, death
- B6 (pyridoxine): coordination, mental changes, oral lesions
- B9 (folic acid): macrocytic anemia, glossitis, spinal bifida
- B12 (cyanocobalamin): macrocytic anemia, dementia, balance, peripheral neuropathy
- Vitamin C: Scurvy: gum bleeding and disease, poor wound healing
- Calcium: osteoporosis, osteomalacia, dentitian
- Iron: Microcytic anemia
- Zinc: poor wound healing, immunity
- Copper: microcytic anemia, Wilson's disease
- Selenium: fatigue (physical and mental)
- Iodine: Thyromegally, cretinism
- Chromium: insulin resistance
- Magnesium: hypertension, cramps, constipation
- Potassium: cramps, palpitations
- Vitamin K: bruising/bleeding, warfarin management
- Vitamin A: skin disorders, night vision, night blindness
- Vitamin D: rickets, bone/teeth/muscle issues, growth issues, falls, immunity, CVD
- Kwashiorkor: protein deficientcy (thun ext/round belly)
- Marasmus: calorie deficit wasting, deep wrinkled skin, loss of buccal fat, hair flag sign' (alternating bands of pale and dark hair)
Ref:
- OMA Review Course 2016
Metabolic Syndrome
| Risk Factor | Def |
|---|---|
| Waist circumference (M) | >102 cm |
| Waist circumference (F) | >88 cm |
| Trig | >150 mg/dL |
| HDL (M) | <40 mg/dL |
| HDL (F) | <50 mg/dL |
| Blood Pressure | >130/85 mm Hg |
| Fasting Glucose | >100 mg/dL |
Diagnosis requires >2
Presence of any three of these five criteria is diagnostic:
- Blood pressure
- ≥ 130 mm Hg systolic or ≥ 85 mm Hg diastolic, or antihypertensive pharmacotherapy needed in a patient with a history of hypertension
- Fasting glucose level
- ≥ 100 mg per dL (5.55 mmol per L) or pharmacotherapy needed for elevated glucose level
- HDL cholesterol level
- < 50 mg per dL (1.29 mmol per L) in women or < 40 mg per dL (1.04 mmol per L) in men, or pharmacotherapy needed for reduced HDL cholesterol level
- Triglyceride level
- ≥ 150 mg per dL (1.69 mmol per L) or pharmacotherapy needed for elevated triglyceride level
- Waist circumference
- ≥ 35 in (89 cm) in women or ≥ 40 in (102 cm) in men
Reference:
- Consultant Mar 2016
- The Lancet 2005 Apr 2005;364(9468);1415-1428
- AFP Nov 2020 Vol 102 No 10
Other tests
As needed and appropriate:
- Cardiac stress +/- echo
- Sedentary, cardiac risk esp if HF and valve assessment, FH, Ex, Surg
- Sleep study
- Cardiac angiography
- Psychosocial screening
- Secondary obesity workup
- Abdominal US
- NAFLD, cholelithiasis, nephrolithiasis, PCOS ovaries / uterine thickness
- Cancer screening
- Pulmonary function tests
- (3) - Screening
- Eating Disorder Scales:
- Binge eating scale (BES)
- Binge eating questionnaire (BEQ)
- Eating inventory (EI)
- Weight and lifestyle inventory (WALI)
- Personality and Psychopathology
- Basic personality invetory (BPI)
- Personality assessment inventory (PAI)
- Beck depression inventory-II (BDI-II)
- Health related Quality of Life
- Quality of life questionnaire (QLQ)
- Quality of life inventory (QOLI)
- Impact of weight on quality of life (IWQOL-Lite)
- Drug and Alcohol
- Alcohol use disorder test (AUDIT-C)
- Drug abuse screening test (DAST)
- (4) - Treat Comorbidities
Obesity related conditions and consequences (Can also divide into conditions secondary to fat mass (1) vs pathologic dysfunction/adiposopathy (2)):
- Pulmonary
- Sleep apnea (1)
- Abnormal function (1)
- Hypoventilation syndrome (1)
- Nonalcoholic fatty liver (1) - (See Gastroenterology entry)
- Steatosis
- Steatohepatitis
- Cirrhosis
- Gall bladder disease (2)
- Gynecologic abnormalitis
- Abnormal menses (1)
- Infertility (2)
- Polycystic ovarian syndrome (2)
- Osteoarthritis (1)
- Skin
- Psoriasis(2)
- Cellulitis (1)
- Gout (2)
- Idiopathic intracranial hypertension (2)
- Stroke (2)
- Cataracts (2)
- Heart disease (2)
- Type 2 DM (2)
- Cancers (endometrial, breast, colon, esophagus, uterus, cervix, pancrease, kidney, prostate) (2)
- Phlebitis (1)
- Higher rates of depression and anxiety (2)
- More likely to face discrimination at work and elsewhere (1)
Medical and psychosocial consequences of obesity
- Type 2 DM:
- Adults with BMI >35 have a 40x risk compared to normal BMI
- Asthma:
- Obese girls are 5-7x more likely to develop asthma after 11yo compared to normal BMI
- COPD:
- Every 5.3 increase in BMI increases odds by 1.6
- HTN:
- In women, every 1kg of weight gain after 18yo increases risk by 5%
- HLD:
- BMI>30 is associated with almost 6x the odds of low HDL level and 2x the odds of high total cholesterol level
- Heart disease:
- Every 2.3kg weight gain after 16yo increases risk of CAD by 20% in men and 37% in women
- Gallstones:
- Adults with BMI>25 have 1.9x the risk of developing gallstones
- Fatty liver disease:
- Approximately 75% of obese individuals have steatosis of liver and 20% have steatohepatitis
- Colorectal cancer:
- Obesity increases risk by 60% in men and 30% in women
- Esophageal and gastric cancers:
- Obese individuals have 2.7x the risk
- Breast cancer:
- Obesity increases risk by 40% in postmenopausal women
- Endometrial cancer:
- Obesity incresaes the risk 2.2x to 3.6x
- Renal cancer:
- Obesity increases the risk 1.7x in men and 2.2x in women
- Osteoarthritis:
- Obesity increases the risk 5x
- Pain:
- Obese children have 4x the odds of experiencing musculoskeletal pain as normal weight
- Depression:
- Obese adults have 1.21x the odds of a lifetime history of depression as normal weight
- Bipolar disease:
- Obese adults have 1.47x the odds of a lifetime history compared to normal weight
- Panic disorder, agoraphobia:
- Obese adults have 1.27x the odds of a lifetime history compared to normal weight
FP Essentials #349
Obesity and Atrial Fibrilation
- For every increase in BMI by 1 => 4% increase in risk for AF
- Affected by:
- increased plasma volume
- LA/LV dysfunction
- oxidative stress
- hypoxemia
- increased afterload
Obesity and Cancer
- For every BMI increase of 5 -> Linear association with cancers of:
- Uterus
- Gallbladder
- Kidney
- Cervix
- Thyroid
- Leukemia
- BMI positively associated with:
- Liver
- Colon
- Ovarian
- Post-menopausal breast cancers
- Underweight associated with increase in:
- oral cavity
- Esophagus and Stomach
- Decreased risk of post-menopausal breast and prostate ca
Obesity and Gall bladder disease
- Recycling of weight increases RR for cholecystectomy
- Increased incidence with rapid weight loss
- Increased gallstones due to incresaed cholesterol turnover to relative body fat
- Cholesterol is linearly related to body fat - 20mg of additional cholesterol is synthesized for each Kg of excess body adipose tissue -> then excreted in bile
Obesity and Heart Disease
- Increased risk of heart failure
- Alterations in myocardium structure, arterial wall remodeling
- LV dysfunction from increased cardiac output
- Increased intra-myocardial fatty acid deposition
- For every increase of BMI by 1 unit, there is an increase risk of heart failure of 5% in men and 7% in women
NEJM Aug 2002 1;34(5):305-13
Obesity and Hypertension
- Renal structure changes -> tubular reabsorption enhancing Sodium Retention
- Increased arterial pressure
- Increased sympathetic nervous syste activity
- Increased vasoconstriction
- Increase in Norepinephrine, angiotensin II levels
- Increased damage to nephrons
Central obesity:
- Increases leptin levels
- Increases Sympathetic nervous system
- Increases Renin-angiotensin-aldosterone system stimulation
- Increases Angiotensinogen from visceral adipocytes
- Increases Aldosterone production from excess angiotensin stimulation
- Increases Salt sensitivity from renal sodium reabsorption with renal blood flow redistribution
Obesity and Non-alcoholic Fatty Liver Disease (NAFLD)
- 15-30% of general population - up to 70% of those with DM 2
- 57-74% prevalence in those with BMI >30
- 90% prevalence in those with BMI >40 - most also have hepatic steatosis
In weight loss, especially rapid, will see a transient increase in transaminases (ALT)
Obesity and Psychosocial impact
- Lifetime prevalence increases 1.5-2x for Major Depression in those with BMI >30
- Prevalence of obesity increases from 25% in those without MDD to 57.8% in those with mod-severe MDD
Obesity and Sleep
- Sleep 8 hours -> Decreased BMI
- Sleep 5 hours -> 14.9% Increase in Ghrelin and 15.5% Decrease in Leptin = 3.6% increase in BMI
Obesity and Sleep Apnea
- Occurs in >30% of those with BMI >30
- Occurs in 50-98% of those with BMI >40
Obesity and Stroke
- For every increase in BMI by 1 => 6% increase in risk for hemorrhagic stroke and 4% for ischemic stroke
Obesity Paradox - Things made worse with weight loss
- 5x increase in successful suicide rate following gastric bypass surgery (undiagnosed depression??)
- Sarcopenia
- Those who lose weight who had HF -> Decreased mortality
- (5) - Lifestyle modification
Rensberry's Simple Changes for Weight Loss
Simple Changes for Weight Loss:
- Track your calorie intake:
- Eat more vegetables (but not potatoes)
- Stop eating after 7 pm
- Don't drink calories
- Avoid foods with added sugars or excess sugar
- Try a simple meal replacement (For 1 or 2 meals)
- Sleep 7 to 9 hours a night
- Do 2 to 5 minutes of breathing exercises daily
- Start a daily walking habit (30+ min)
Behavioral Factors regarding weight loss maintenance
Factors associated with successful weight loss maintenance
- Establish a social support network
- Limit or avoid disinhibited eating
- Avoid binge eating
- Avoid eating in response to negative emotions and stress
- Be accountable for one's decisions
- Foster a strong sense of autonomy, internal motivation, and self-efficacy toward weight loss maintenance
Risk factors associated with weight regain
- Disinhibited eating
- Binge eating
- Periods of excessive hunger
- Eating in response to negative emotions and stress
- Passive reactions to problems
- Less assumption of responsibility in life
Reference:
- AFP Vol 82 No 6 Sep 2010
Eating Disorders
- Anorexia
- Thin but concerns of feeling fat
- Pain/anxiety with foods
- Electrolyte abnormalities
- High achiever, perfectionist
- Binge Eating Disorder
- Obesity, failed weight loss
- Rapid eating, large amount, embarrassed, disgust, distress
- Obesity related medical conditions
- Bulimia
- Bathroom after meals
- Salivary hypertrophy, dental/finger/hand erosion
- Depression/anxiety
- Weight swings, diet shopping
- Electrolyte abnormalities
- Esophageal abnormalities
iPhone/Android Apps for Weight Management
Malnutrition Signs/Symptoms
- B1 (thiamine): wet beriberi (CVD), dry WErnicke-Korsakoff syndrome (Ataxia, neuropathy, mental confusion)
- B2 (riboflavin): anemia, mouth/lip/skin disorders
- B3 (niacin): Pellagra: Demetia, Diarrhea, Dermatitis, Death
- B6 (pyridoxine): coordination, mental changes, oral lesions
- B9 (folic acid): macrocytic anemia, glossitis, spinal bifida
- B12 (cyanocobalamin): macrocytic anemia, dementia, balance, peripheral neropathy
- Vitamin C: Scurvy - gum bleeding, poor wound healing
- Calcium: osteoporosis, osteomalacia, dentitian
- Iron: Microcytic anemia
- Zinc: poor wound healing, immunity
- Copper: microcytic anemia, Wilson's disease
- Selenium: fatigue (physical/mental)
- Iodine: thyromegally, cretinism
- Chromium: Insulin resistance
- Magnesium: Hypertension, cramps, constipation
- Potassium: Cramps, palpitations
- Vitamin K: Bruising, bleeding
- Vitamin A: Skin disorders, night vision, night blindness
- Vitain D: Rickets, bone/teeth/muscle issues, growth issues, falls, immunity, CVD
- Kwashiorkor: Protein deficiency
- Marasmus: Calorie deficit wasting, deep wrinkled skin, loss of buccal fat, hair "flag sign"
Reference:
- Kullie J Am Board Fam Med 2009
Physical Activity
- Exercise leads to a weight loss of 0.5-7.6 kg compared with a 0.1kg weight loss to 0.7kg weight gain with no treatment.
- Being sedentary is almost the same as being a smoker in terms of health risks
- Each daily 2hr increment of television watching is associated with 23% incresae in risk for developing obesity.
Regular physical activity decreases risk of:
- Dementia
- DM 2
- Cardiovascular disease
- Some cancers
Recommendations:
- 150 min - General Health Benefits
- 150-300 min - Prevention of Weight Gain
- 300-420 min - Prevention of Weight Regain
Give Physical Activity Prescription in form of SMART Goals:
- S - Specific
- M - Measurable
- A - Achievable
- R - Realistic
- T - Time-bound
SMART Goal Physical Activity Example:
- Bike 30min three times a week at the park near my house with my neighbor after dinner
All Physical Activity prescriptions need FITTE:
- F - Frequency (5/wk)
- I - Intensity (3.8mph)
- T - Time (30 min)
- T - Type (walk)
- E - Enjoyment (with a partner)
Walking energy efficiency:
- A 68 kg (150 lb) person walking at 4 km/h (2.5 mph) requires approximately 210 kilocalories (880 kJ) of food energy per hour
- Which is equivalent to 4.55 km/MJ.
- 1 US gallon (3.8 L) of gasoline contains about 114,000 British thermal units(120 MJ) of energy
- Walking thus is approximately equivalent to 360 miles per US gallon (0.65 L/100 km).
Total Energy Expenditure (TEE): 24hr energy needs
- A 10% weight loss lowers TEE by 20-25%
- It will take 300-400kcal/day to maintain the same body weight as somebody who hasn't lost 10% of their weight
- Persists for 6mo - 7yrs
EE = REE + TEM + EEPA
- EE - Energy Expenditure
- REE - Resting Energy Expenditure
- 60-75%
- TEM - Thermic Effects of Meals
- 10%
- EEPA - Energy Expenditure from Physical Activity
- 15-30%
- This is the variable we can affect
NEAT = EEPA - EE from Exercise
- NEAT - Non-exercise Activity Therogenesis
- Factors that affect NEAT:
- Biological - weight, gender, body composition
- Environmental - occupation, transportation, sitting
References:
- AFP Vol 75 No 9 May 2007
- FMX 2016
- OMA Review Course 2016
- Shiels Health Reports 2008
- USDHHS. PA Guidelines for Americans. 2008.
- (6a) - Pharmacotherapy
Weight Gaining Medications
| Category | Drug | Rel wt gain | Alternatives |
|---|---|---|---|
| Antidepressant | |||
| Mirtazapine | <1.5kg | Bupropion or fluoxetine | |
| Citalopram | vortioxetine | ||
| Sertraline | |||
| Escitalopram | |||
| Duloxetine | |||
| Venlafaxine | |||
| Paroxetine | |||
| Amitriptyline | <4kg | Nortiptyline (still weight gaining) | |
| Antidiabetic | |||
| Meglitinide | <1.5kg | Detemir (qd is better than bid); | |
| Metformin (weight loss); | |||
| Acarbose; Miglitol; GLP-1 agonists (weight loss); | |||
| DPP-IV inhibitor | |||
| Insulin | >4kg | ||
| Sulfonylureas | >4kg | ||
| Thiazolidinedione | <4kg | ||
| Antipsychotic | |||
| Clozapine | >4kg | Ziprasidone, Aripiprazole, haloperidol | |
| Olanzapine | >4kg | ||
| Risperidone | <4kg | ||
| Antiepileptic | |||
| Carbamazepine | <1.5kg | Zonisamide; Topiramate (weight loss); | |
| Gabapentin | <4kg | Lamotrigine; Levetiracetam | |
| Valproic acid | >4kg | ||
| Cardiovascular | |||
| Amlodipine | ACE Inhibitors; ARB | ||
| B-blockers | <4kg | ||
| Nifedipine | |||
| Hormone | |||
| Medroxyprogesterone | >4kg | Progestins, testosterone | |
| Corticosteroids | >4kg | ||
| Estrogens |
References:
- CME Bulletin Vol 16 No 2 Apr 2016
- JFP 2010;59(7)
- AFP Vol 94 No 5 Sep 2016
Weight Loss Medications
Use in:
- Persons with BMI >27 with 1 co-morbidity (OSA, HTN, HLD, DM)
- Persons with BMI >30
Long-term use:
- Orlistat (Xenical)
- Modestly effective
- MOA: Reduces absorption of fats from food (30%) by inactivating gastric and pancreatic lipases
- Should be taken with each meal
- Adverse Effects: gassiness, cramps, oily stools
- Average wt loss: 2.5-3.4Kg
- 30d Cost: $512 (120mg); $44 (60mg)
Lorcaserin (Belviq)REMOVED FROM MARKET!!!- Modestly effective and well tolerated
- MOA: Acts on serotonin receptors (2C receptor agonist) in brain to decrease appetite, increases feeling of fullness
- Adverse Effects: Headaches, dizziness, fatigue, dry mouth, constipation, and URI
- Do not use if murmur present, on SSRIs, or migraines
- Average weight loss: 2.9-3.6Kg
- 30d Cost: $199
- Good candidates: Patients who report inadequate meal satiety
- Poor candidates: Patients on other serotonin modulating medications, known cardiac valvular disease
- Phentermine/topiramate (Qsymia)
- Most effective drug available for weight loss
- MOA: Adrenergic agonist/neurostabilizer - Decreases appetite, increases feeling of fullness
- Adverse Effects: Increased heart rate, birth defects, paraesthesias, insomnia, dizziness, constipation, dry mouth
- Need to be enrolled in a risk evaluation and mitigation strategy program to prescribe (REMS)
- Average wt loss: 4.1-10.7Kg
- 30d Cost: $170
- Good candidates: Younger patients who need assistance with appetite suppression
- Poor candidates: Patients with uncontrolled HTN, unstable coronary disease, hyperthyroidism, glaucoma, anxiety, insomnia, sensitive to stimulants, history of drug abuse, history of nephrolithiasis
- Buproprion/naltrexone (Contrave)
- Effective but common nausea
- MOA: Opioid receptor antagonist/dopamine and norepinephrine reuptake inhibitor
- Decrease apetite and regulate dopamine reward system in brane controlling food cravings and overeating behaviors
- Adverse Effects: Nausea, Constipation, Headache, Vomiting, dizziness, insomnia, dry mouth
- Caution with HTN as initially (first 3mo) can increase BP
- Contraindicated with HTN, Sz
- Pt friendly packaging
- Average weight loss: 3.7-5.2Kg
- 30d Cost: $199
- Good candidates: Patients who describe cravings for food and/or addictive behaviors related to food, patients who are trying to quit smoking, reduce EtOH intake, and/or concomitant depression
- Poor candidates: Patients with uncontrolled HTN, seizures, abrupt discontinuation of EtOH, benzodiazepins, barbituates or antiepileptic medications
- Liraglutide 3mg (Saxenda) / Semaglutide (Wegovy) / Tirzepatide (Zepbound)
- Injection (GLP-1 agonist)
- MOA - GLP1-receptor agonist - Decreases caloric intake through delayed gastric emptying and appetite regulation
- Adverse Effects: Nausea, Diarrhea, Vomiting, Constipation, Dyspepsia, Abdominal pain
- Use in persons with DM
- Average weight loss: 5.8-5.9Kg
- 30d Cost: $1068
- Good candidates: Patients who report inadequate meal satiety and/or have DM II, prediabetwes, or impaired clucose tolerance; patients requireing concomitant psychiatric medications
- Poor candidates: Patients with aversion to needles, history of pancreatitis, personal or FH of medullary thyroid carcinoma, or Multiple endocrine neoplasia syndrome type 2
- Setmelanotide (Imcivree)
- Approved 2020
- Activates melanocortin-4 receptors in the brain, specifically in the paraventricular nucleus of the hypothalamus and lateral hypothalamic area
- Subcutanous injection 2-3 mg once daily
- 10% body weight loss
- For those with genetically dertermined deficiency of proopiomelanocortin, proprotein subtilisin/kexin type 1 or leptin receptor or a clinical diagnosis of Bardet-Biedl syndrome
- Short-term use: Contraindicated in patients with CAD, HTN, Hyperthyroidism, and h/o drug abuse
- phentermine
- MOA: Adrenergic agonist
- Adverse effects: Dry mouth, insomnia, dizziness, irritability
- Weight loss: 2% - 6% body weight
- Good candidates: Younger patients who need assistance with appetite suppression
- Poor candidates: Patients with uncontrolled HTN, unstable coronary disease, hyperthyroidism, glaucoma, anxiety, insomnia, sensitive to stimulants, history of drug abuse
- benzphentamine
- diethylpropion
- phendimetrazine
- phentermine
- Other Notes
- Orlistat, lorcaserin, naltrexone-bupropion, phentermine-topiramate, and liraglutide were associated with 5% weight loss at 52wks compared to placebo
- Phentermine-topiramate and liraglutide were associated with highest odds of achieving 5% weight loss
- Rank for weight loss (most->least):
- Phentermine-topiramate
- Liraglutide
- Naltrexone-bupropion
- Lorcaserin
- Orlistat
- Placebo
- Rank for discontinuation due to Adverse Effects (least->most):
- Placebo
- Lorcaserin
- Orlistat
- Phentermine-topiramate
- Naltrexone-bupropion
- Liraglutide
Nutrition management of gastrointestinal adverse effects
- Nausea
- Eat regularly with smaller portions than usual
- Eat Slowly
- Stop At First Signs Of Fullness
- Limit High Fat Or Spicy Foods
- Stay Hydrated - Drink Fluid Intake Of 64 Ounces
- Limit Consumption Of Sweetened Beverages
- Constipation
- Maintain High Fiber Diet Of Vegetables, Fruits, And Whole Grains
- Stay Hydrated - Drink Fluid Intake Of 64 Ounces
- Increase Physical Activity - Reduce Sedentary Behavior
- Think About Adding Daily Magnesium
- Consider A Stool Softener Or Polyethylene Glycol
- Diarrhea
- Avoid Sugar Alcohols
- Limit Intake Of Coffee, Dairy, Alcohol, And Carbonated Beverages
- Increase Dietary Fiber
- Stay Hydrated - Drink Fluid Intake Of 64 Ounces
References:
- JAMA Vol 315 No 11 Mar 2016
- JAMA Vol 315 No 22 Jun 2016
- JFP Vol 66 No 10 Oct 2017
- JFP Supplement Oct 2025
Study: Risk of Gastrointestinal Adverse Events Associated With Glucagon-Like Peptide-1 Receptor Agonists for Weight Loss
Background
- Glucagon-like peptide 1 (GLP-1) agonists are medications approved for treatment of diabetes that recently have also been used off label for weight loss.1 Studies have found increased risks of gastrointestinal adverse events (biliary disease,2 pancreatitis,3 bowel obstruction,4 and gastroparesis5) in patients with diabetes.2-5 Because such patients have higher baseline risk for gastrointestinal adverse events, risk in patients taking these drugs for other indications may differ. Randomized trials examining efficacy of GLP-1 agonists for weight loss were not designed to capture these events2 due to small sample sizes and short follow-up. We examined gastrointestinal adverse events associated with GLP-1 agonists used for weight loss in a clinical setting.
Methods
- We used a random sample of 16 million patients (2006-2020) from the PharMetrics Plus database (IQVIA), a large health claims database that captures 93% of all outpatient prescriptions and physician diagnoses in the US through the International Classification of Diseases, Ninth Revision (ICD-9) or ICD-10.
- In our cohort study, we included new users of semaglutide or liraglutide, 2 main GLP-1 agonists, and the active comparator bupropion-naltrexone, a weight loss agent unrelated to GLP-1 agonists. Because semaglutide was marketed for weight loss after the study period (2021), we ensured all GLP-1 agonist and bupropion-naltrexone users had an obesity code in the 90 days prior or up to 30 days after cohort entry, excluding those with a diabetes or antidiabetic drug code.
- Patients were observed from first prescription of a study drug to first mutually exclusive incidence (defined as first ICD-9 or ICD-10 code) of biliary disease (including cholecystitis, cholelithiasis, and choledocholithiasis), pancreatitis (including gallstone pancreatitis), bowel obstruction, or gastroparesis (defined as use of a code or a promotility agent).
- They were followed up to the end of the study period (June 2020) or censored during a switch.
- Hazard ratios (HRs) from a Cox model were adjusted for age, sex, alcohol use, smoking, hyperlipidemia, abdominal surgery in the previous 30 days, and geographic location, which were identified as common cause variables or risk factors.6
- Two sensitivity analyses were undertaken, one excluding hyperlipidemia (because more semaglutide users had hyperlipidemia) and another including patients without diabetes regardless of having an obesity code.
- Due to absence of data on body mass index (BMI), the E-value was used to examine how strong unmeasured confounding would need to be to negate observed results, with E-value HRs of at least 2 indicating BMI is unlikely to change study results. Statistical significance was defined as 2-sided 95% CI that did not cross 1. Analyses were performed using SAS version 9.4. Ethics approval was obtained by the University of British Columbia's clinical research ethics board with a waiver of informed consent.
Results
- Our cohort included 4144 liraglutide, 613 semaglutide, and 654 bupropion-naltrexone users. Incidence rates for the 4 outcomes were elevated among GLP-1 agonists compared with bupropion-naltrexone users (Table 1).
- For example, incidence of biliary disease (per 1000 person-years) was 11.7 for semaglutide, 18.6 for liraglutide, and 12.6 for bupropion-naltrexone and 4.6, 7.9, and 1.0, respectively, for pancreatitis.
- Use of GLP-1 agonists compared with bupropion-naltrexone was associated with increased risk of pancreatitis (adjusted HR, 9.09 [95% CI, 1.25-66.00]), bowel obstruction (HR, 4.22 [95% CI, 1.02-17.40]), and gastroparesis (HR, 3.67 [95% CI, 1.15-11.90) but not biliary disease (HR, 1.50 [95% CI, 0.89-2.53]).
- Exclusion of hyperlipidemia from the analysis did not change the results (Table 2).
- Inclusion of GLP-1 agonists regardless of history of obesity reduced HRs and narrowed CIs but did not change the significance of the results (Table 2). E-value HRs did not suggest potential confounding by BMI.
Discussion
- This study found that use of GLP-1 agonists for weight loss compared with use of bupropion-naltrexone was associated with increased risk of pancreatitis, gastroparesis, and bowel obstruction but not biliary disease.
- Given the wide use of these drugs, these adverse events, although rare, must be considered by patients who are contemplating using the drugs for weight loss because the risk-benefit calculus for this group might differ from that of those who use them for diabetes.
- Limitations include that although all GLP-1 agonist users had a record for obesity without diabetes, whether GLP-1 agonists were all used for weight loss is uncertain.
Reference:
- Sodhi M, Rezaeianzadeh R, Kezouh A, Etminan M. Risk of Gastrointestinal Adverse Events Associated With Glucagon-Like Peptide-1 Receptor Agonists for Weight Loss. JAMA. 2023 Oct 5:e2319574. doi: 10.1001/jama.2023.19574. Epub ahead of print. PMID: 37796527; PMCID: PMC10557026.
- https://jamanetwork.com/journals/jama/fullarticle/2810542?guestAccessKey=31a6dd82-d1ee-46d6-b95e-e4ef621c2ddf&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=100523
Patient Messaging: Weight Habits Along With Medications
I also recommend:
- Daily calorie tracking (1700 1500 cal/day)
You can use one of these free apps to do it easily:
- Nitritionix
- MyNetDiary
- Cronometer
- Sleep 7 to 9 hours a night
- Do 2 to 5 minutes of breathing exercises daily
- Start a daily walking habit (20-30 min)
- (6b) - Bariatric surgery
Results with bariatric surgery and sleeve gastrectomy:
- More patients achieve A1c <6%
- Greater reductions in body weight and triglyceride levels
- Greater increases in HDL
- Require less diabetes medications
| Procedure | Percent of excess weight lost | Indications | Complications | Mechanism |
|---|---|---|---|---|
| Adjustable gastric banding | 44% | BMI >40 | Band erosion or slippage | Restrictive |
| BMI >35 with comorbidities | Need for revision/removal | Silicone band placed around gastric | ||
| BMI >30 with DM II or met syndrome | Reservoir leakage | fundus - inflates/deflates to adjust | ||
| Roux-en-Y gastric bypass | 67% | BMI >40 | Anastomotic leak | Restrictive and malabsorptive |
| BMI >35 with comorbidities | Delayed gastric emptying | <50mL pouch anastomosed to Roux-limb | ||
| Dumping syndrome | 30-50cm distal to bypass a | |||
| Gastric dilation, hernia | portion of small bowel | |||
| Nutritional deficiencies | ||||
| Obstruction | ||||
| Stable line failure | ||||
| Stoma narrowing | ||||
| Sleeve gastrectomy | 56% | BMI >40 | Gastric leakage, vomiting | Restrictive, hormonal |
| BMI >35 with comorbidities | Size of stomach is reduced to 25% | |||
| with pylorus intact |
References:
- AFP Vol 94 No 5 Sep 2016
Select appropriate patients for bariatric treatment
Selection Criteria:
- Able to adhere to postop care
- BMI >40
- BMI >35 and at least 1 severe obesity-related comorbidities
- BMI >30 with DM or metabolic syndrome (weaker evidence)
Exclusion Criteria:
- Cardiopulmonary disease increasing surgical risk
- Current drug/alcohol abuse
- Lack of comprehension of risks, benefits, expected outcomes, alternatives, and required lifestyle changes
- Reversible endocrne or other disorders causing obesity
- Uncontrolled severe psychiatric illness
Benefits:
- Weight loss of 60-70% in short term; up to 50% at 10 years
- Mortality risk <0.5%
- Surgery reduces all-cause mortality by 30-50% at 7-15 years
- DM remission in 60-80% 1-2 years after R&Y (retained by 30% at 15 years)
- 23% patients undergoing baritric surgery report a curretn mood disorder - most common is depression (JAMA Vol 315 No 2 Jan 2016)
References:
- AFP Vol 93 No 1 Jan 2016
Preop Evaluation
Recommended:
- Age and risk appropriate cancer screening
- Complete H&P
- Labs (A1c, CBC, CMP, Folic acid, B12, 25-OH Vit D, TSH)
- Nutritional eval - Should fail 6 months of attempt to lose weight without surgery first
- Pregnancy counseling (NOT recommended for 12-18mo post-op)
- Psychosocial and behavioral evaluations
- Tobacco cessation counseling for wound healing
Additional to consider:
- Cardiopulmonary eval (Sleep study, EKG, echo, etc)
- Gastrointestinal eval (H pylori, gallbladder, upper endoscopy, etc)
AFP Vol 93 No 1 Jan 2016
Post-op Follow-up
General Principles
- Adjust postop medications as needed
- Avoid NSAIDs
- Avoid pregnancy for 12-18 mo
- DEXA at 2 years
- Labs (CBC, CMP, Folic acid, B12, 24-hr urinary calcium excretion, 25-OH Vit D)
- Monitor adherence to dietary, behavioral, and physical activity recommendations
Yearly Laboratory Studies After Roux-en-Y Gastric Bypass
- CBC
- Complete Metabolic Panel
- A1c
- Folate / Iron
- Vitamin B-12
- Phosphate
- Magnesium
- Lipid Panel
- TSH
- PTH
- For R&Y:
- Zinc
- Vitamin D
- Vitamin B-1
Post-op Supplementation:
- >60g protein / day
- Calcium citrate - 1200-1500mg/d
- Vit D3 - 3000 IU/d - titrate to >30ng/mL
- Folic acid 400mg in MVI
- Elemental Fe - 45-65mg/d plus multivitamin
- B12 - >350mcg/d or 1000mg/mo IM or 3000mg/6mo IM or 500mg/wk intranasal
- MVI - 2/day
Nutritional deficiencies after bariatric surgery
- Protein
- Prevalence: 3%-18%
- Symptoms: Edema, weakness, decreased muscle mass
- Measurement: Serum albumin (<3.5 mg/dL)
- Frequency of screening: q6mo for 2 years then annually
- Supplement for prevention: 60-120g/d protein OR 1.1 g/Kg ideal body weight
- Supplement for deficiency treatment: Oral lactose-free supplementation rich in branched chain amino acids (2nd line: Enteral or parenteral nutrition)
- Calcium
- Prevalence: 10%
- Symptoms: Low bone density, osteoporosis, parestheseia, muscle spasms, tetany
- Measurement: Ionized calcium (<4.48 mg/dL)
- Frequency of screening: Ca and PTH q6mo for 2 years then annually
- Supplement for prevention: 1200-2000 mg/d Ca citrate or dietary
- Supplement for deficiency treatment:
- Intensity Ca and Vid D supplementation
- IV bisphosphonates for osteoporosis
- Vitamin B1 (Thiamine)
- Prevalence: 49%
- Symptoms: Dry beriberi, wet beriberi, Werrnicke's encephalopathy
- Measurement: Serrum thiamine (<10mcg/L)
- Frequency of screening: Optional starting at 3mo; every 6mo for 2 years then annually
- Supplement for prevention: 6mg/d oral
- Supplement for deficiency treatment:
- Subclinical: 100mg/d oral
- Clinical: 100-200 mg IV/IM
- With psychoses and Wernicke's encephalopathy: 200-300 mg/d IV for 3d followed by 250mg/d IV until clinical improvement
- Vitamin B12 (Cobalamin)
- Prevalence: 4%-62%
- Symptoms: Macrocytic anemia, fatigue, glossitis, paresthesia, sensory deficits, ataxia, dementia
- Measurement: B12 (<200 pg/mL); homocysteine increases sensitivity when symptomatic (<10 mcmol/L)
- Frequency of screening: q6mo for 2 years then annually
- Supplement for prevention:
- 250-600mcg/d oral OR
- 1000 mcg/month IM OR
- 3000 mcg IM q6mo
- Supplement for deficiency treatment:
- Asymptomatic: 1000-2000 mcg/d oral OR 1000mcg/wk IM
- Clinical symptoms: 1000mcg/d IM/SC for 5-7d then 1000mcg/wk IM/SC x4-5wks, then monthly
- Folic acid
- Prevalence: 9%-38%
- Symptoms:Macrocytic anemia, fatigue, neural tube defets
- Measurement: folate (<4 nmol/L)
- Frequency of screening: q6mo for 2 years then annually
- Supplement for prevention: 400-1000mcg/d oral
- Supplement for deficiency treatment: 1000 mcg/d oral
- Vitamin A
- Prevalence: 8%-12.5% for RYGB; 61%-69% for BPD-DS
- Symptoms: Rare - dry hair, decreased immunity, xerophthalmia
- Measurement: Vit A (<38 mcg/dL)
- Frequency of screening: Optional annual
- Supplement for prevention: 5000-10,000 IU/d oral
- Supplement for deficiency treatment: 50,000 IU/d oral - if corneal lesions 50,000 to 100,000 IM for 2 weeks (Not over 10,000 if pregnant)
- Vitamin D
- Prevalence: 25%-80%
- Symptoms: Osteomalacia, fractures, depression, myalgia, bone pain
- Measurement: 25-OH Vit D (<20 ng/mL)
- Frequency of screening: q6mo for 2 years then annually
- Supplement for prevention:
- 2000 IU/d for malabsorptive procedures
- 1000 IU/d for LSG
- 3000 IU/d for pediatric patients
- Supplement for deficiency treatment: 1500-9100 IU/d
- Iron
- Prevalence: 17% LSG, 30%-45% post-malabsorptive
- Symptoms: Microcytic anemia, fatigue, dyspnea on exertion, angular stomatitis, glossitis
- Measurement: Serum iron saturation <15%, Total iron <40 mcg/dL
- Frequency of screening: q6mo for 2 years then annually
- Supplement for prevention: 45-65 mg/d elemental iron; 50-100mg/d for pregnancy
- Supplement for deficiency treatment: Calculate iron deficit; IV iron 1000mg, then weekly 500mg IV infusion to calculated dose
- Zinc
- Prevalence: 12% LSG; 21%-33% RYGB; 74%-91% BPD-DS
- Symptoms: Poor wound healing, skin lesions, dermatitis, diminished taste, hair loss, altered immune function, glossitis
- Measurement: Plasma zinc (<11 mcmol/L)
- Frequency of screening: Optional q6mo for 1 year then annual
- Supplement for prevention: No standard recommendation
- Supplement for deficiency treatment: 220 mg/d zinc sulfate OR 50 mg/d zinc gluconate OR 30 mg/d zinc histidine
- Copper
- Prevalence: 2% RYGB; 10%-24% BPD-DS
- Symptoms: Anemia, pancytopenia, fatigue, dyspnea on exertion, spastic gait, sensory ataxia, peripheral neuropathy, paresthesias
- Measurement: Serum copper (<11 mcmol/L)
- Frequency of screening: None recommended but monitor if on zinc
- Supplement for prevention: 2mg/d oral
- Supplement for deficiency treatment: 2-4.4 oral copper OR 2mg IV/d copper for 5-6d
Recommended patients for Body contouring surgery:
- Weight stability for more than 1 year after Bariatric surgery
- Age >16yo
- Excess skin causing significant funtional impairment
- Non-smoking status
- Good social support
References:
- AFP Vol 93 No 1 Jan 2016
- JFP Vol 66 No 6 Jun 2017
- JAMA Sep 2020 Vol 324, No 9
- Others
Bariatric Surgery Evidence edit
Bariatric Surgery Associated with Decreased All-Cause Mortality and Lower Rates of Other Obesity-Related Events
Based on population registry data, bariatric surgery is associated with lower all-cause mortality and a lower risk of developing many subsequent obesity-related conditions. Because the investigators excluded randomized trials, the patients' health habits and other unmeasured factors might account for the findings. (Level of Evidence = 2a–)
The authors searched PubMed, EMBASE, and the Web of Science for national or regional administrative database studies that evaluated mortality or incident obesity-related diseases for patients who have undergone any form of bariatric surgery. They defined obesity-related illnesses as type 2 diabetes mellitus, hypertension, obstructive sleep apnea, ischemic heart disease, cardiac failure, dyslipidemia, and venous thromboembolism. The authors excluded randomized trials but included studies that had a control group and a minimum of 18 months of follow-up. Two authors independently evaluated studies for inclusion. The authors did not describe searching for unpublished studies. They included 18 studies with 1,539,904 patients, in which 269,818 patients received some form of bariatric surgery: gastric bypass (n = 137,578, 51%), sleeve gastrectomy (n = 58,916, 22%), adjustable gastric band (n = 52,973, 20%), vertical banded gastroplasty (n = 6,397, 2%), biliopancreatic diversion (n = 1,002, 0.4%), or an alternative procedure or unspecified operation (n = 12,952, 5%). The median follow-up period was 59 months. The authors reported that the quality of the studies was high.
Eleven studies found a decreased association between surgery and all-cause mortality (odds ratio [OR] = 0.62; 95% CI, 0.55 to 0.69) with heterogeneity but no evidence for publication bias. Six studies found a decreased association between surgery and the subsequent development of type 2 diabetes (OR = 0.39; 95% CI, 0.18 to 0.83), but with statistical heterogeneity and no evidence for publication bias. Five studies found a lower risk of incident hypertension after surgery (OR = 0.36; 95% CI, 0.32 to 0.40) with no evidence for heterogeneity or publication bias. One study reported incident sleep apnea, which occurred in 1.1% of patients undergoing surgery compared with 2% of control patients. Five studies reported that incident ischemic heart disease was lower after surgery (OR = 0.46; 95% CI, 0.29 to 0.73), but with statistical heterogeneity and no evidence for publication bias. Two studies found no association between surgery and incident heart failure. One study reported venous thromboembolism, which occurred in 1.7% of patients undergoing surgery compared with 4.4% of control patients (hazard ratio = 0.60; 95% CI, 0.43 to 0.84). Because this analysis excluded randomized trials, it is possible that the magnitude of the lower risks of bad outcomes associated with bariatric surgery is inflated.
Study design: Meta-analysis (other)
Funding source: Government
Setting: Various (meta-analysis)
Reference: Wiggins T, Guidozzi N, Welbourn R, et al. Association of bariatric surgery with all-cause mortality and incidence of obesity-related disease at a population level: a systematic review and meta-analysis. PLoS Med. 2020;17(7):e1003206.
References:
- AFP Feb 2021 Vol 103 No 4
- (7) - Maintenance of Weight Loss and Prevention of Weight Regain
From the National Weight Control Registry:
- The researchers behind the study found that people who have had success losing weight have a few things in common:
- They weigh themselves at least once a week.
- Regular self weighing
- They restrict their calorie intake, stay away from high-fat foods, and watch their portion sizes.
- Calorie restriction
- They also exercise regularly.
- Regular exercise
- "Pretend you didn't exercise at all, you will most likely compensate anyway, so think of exercising just for health improvement but not for weight loss."
- They weigh themselves at least once a week.
Healthy Lifestyle Mnemonic 5-2-1-0
- 5
- 5 servings of fruits and vegetables per day
- 5% weight loss if body mass index ≥ 30 kg per m2; consider body mass index ≥ 27 kg per m2 in Asian or Asian American patients
- 2
- 2 hours or less of nonwork screen time per day
- 2 drinks or less of alcohol per day for men
- 1
- 1 hour of activity per day
- 1 drink or less of alcohol per day for women
- 0
- 0 sweetened drinks
- No smoking
References:
- National Weight Control Registry
- AFP Nov 2020 Vol 102, No 9
National Weight Control Registry
NWCR Stats:
- 80% of persons in the registry are women and 20% are men.
- The "average" woman is 45 years of age and currently weighs 145 lbs, while the "average" man is 49 years of age and currently weighs 190 lbs.
- Registry members have lost an average of 66 lbs and kept it off for 5.5 years.
- These averages, however, hide a lot of diversity:
- Weight losses have ranged from 30 to 300 lbs.
- Duration of successful weight loss has ranged from 1 year to 66 years!
- Some have lost the weight rapidly, while others have lost weight very slowly–over as many as 14 years.
- We have also started to learn about how the weight loss was accomplished: 45% of registry participants lost the weight on their own and the other 55% lost weight with the help of some type of program.
- 98% of Registry participants report that they modified their food intake in some way to lose weight.
- 94% increased their physical activity, with the most frequently reported form of activity being walking.
- There is variety in how NWCR members keep the weight off. Most report continuing to maintain a low calorie, low fat diet and doing high levels of activity.
- 78% eat breakfast every day.
- 75% weigh themselves at least once a week.
- 62% watch less than 10 hours of TV per week.
- 90% exercise, on average, about 1 hour per day.
References:
Research Findings
- Prospective Evaluation of Internalized Weight Bias and Weight Change Among Successful Weight-Loss Maintainers
Objective: Internalized weight bias (IWB) has been associated with weight regain after intentional weight loss, but reliance on cross-sectional data limits the understanding of this relationship. This study prospectively evaluated IWB as a predictor of weight change in a longitudinal observational study of successful weight-loss maintainers.
Methods: National Weight Control Registry participants (maintained 13.6-kg weight loss for ≥ 1 y) were asked to complete an online questionnaire including current weight and Weight Bias Internalization Scale-Modified (WBIS-M) at baseline and 12 months.
Results: At baseline, 1,250 of 1,643 eligible individuals completed the baseline assessment (71% female; 94% white; mean age ± SD: 52 y ± 13.1; BMI: 27 ± 5.5). The average WBIS-M score was 3.0 (± 1.3). Study completers (n = 862) reported 2.2% (± 7.8%) weight gain. Higher baseline IWB predicted weight gain among men (n = 254; t = -2.28; P = 0.02) but not women (n = 608; t = 1.22; P = 0.22). A one-point reduction in WBIS-M score at follow-up was associated with a 3.0% weight loss.
Conclusions: Among weight-loss maintainers, IWB may be a risk factor for weight gain among men. Weight loss at follow-up was associated with reduced IWB in both men and women. Reliance on female-only samples may limit our understanding of IWB and its implications for weight control.
Olson KL, Lillis J, Graham Thomas J, Wing RR. Prospective Evaluation of Internalized Weight Bias and Weight Change Among Successful Weight-Loss Maintainers. Obesity (Silver Spring). 2018 Dec;26(12):1888-1892. doi: 10.1002/oby.22283. Epub 2018 Nov 13. PMID: 30421843; PMCID: PMC6249105.
- Sustaining Regular Exercise During Weight Loss Maintenance: The Role of Consistent Exercise Timing
Background: Exercising at a consistent versus variable time of day cross-sectionally relates to greater moderate to vigorous physical activity (MVPA) among weight loss maintainers. This study evaluated the relationships between exercise timing and both MVPA levels and habit strength, as well as stability in exercise timing, over 1 year among maintainers in the National Weight Control Registry.
Methods: Participants (n = 709) completed questionnaires assessing exercise timing, MVPA, and exercise automaticity (a measure of habit) at baseline and 1-year follow-up. At each assessment, participants were labeled temporally consistent exercisers if >50% of their exercise sessions per week occurred in one time window: early morning, late morning, afternoon, or evening. Participants exercising consistently during the same window at both assessments were labeled as having stable patterns.
Results: Temporally consistent exercise at baseline, regardless of its specific time, related to greater MVPA over time (Ps< .05). Approximately half of temporally consistent exercisers at baseline exhibited stable patterns. Early morning exercise and greater exercise automaticity at baseline predicted stable patterns (Ps< .005). Temporally consistent exercise, especially during the early morning, related to greater automaticity across time (Ps< .01).
Conclusions: Consistent exercise timing may help maintainers accrue more MVPA. Consistent early morning exercise was most strongly related to exercise automaticity and routine stability.
Schumacher LM, Thomas JG, Wing RR, Raynor HA, Rhodes RE, Bond DS. Sustaining Regular Exercise During Weight Loss Maintenance: The Role of Consistent Exercise Timing. J Phys Act Health. 2021 Aug 14;18(10):1253-1260. doi: 10.1123/jpah.2021-0135. PMID: 34391207; PMCID: PMC8764567.
- Relationship of Consistency in Timing of Exercise Performance and Exercise Levels Among Successful Weight Loss Maintainers
Objective: This study aimed to evaluate whether consistency in time of day that moderate- to vigorous-intensity physical activity (MVPA) is performed relates to MVPA levels among successful weight loss maintainers in the National Weight Control Registry.
Methods: Participants (n = 375) reporting MVPA on ≥ 2 d/wk completed measures of temporal consistency in physical activity (PA) (> 50% of MVPA sessions per week occurring during the same time window: early/late morning, afternoon, or evening), PA levels, PA automaticity, and consistency in cues underlying PA habit formation (e.g., location).
Results: Most (68.0%) participants reported temporally consistent MVPA. These individuals reported higher MVPA frequency (4.8 ± 1.6 vs. 4.4 ± 1.5 d/wk; P = 0.007) and duration (median [IQR]: 350.0 [200.0-510.0] vs. 285.0 [140.0-460.0] min/wk; P = 0.03), and they were more likely to achieve the national MVPA guideline (≥ 150 min/wk) than temporally inconsistent exercisers (86.3% vs. 74.2%, P = 0.004). Among temporally consistent exercisers, 47.8% were early-morning exercisers; MVPA levels did not differ by time of day of routine MVPA performance (P > 0.05). Greater automaticity and consistency in several cues were related to greater MVPA among all participants.
Conclusions: Most participants reported consistent timing of MVPA. Temporal consistency was associated with greater MVPA, regardless of the specific time of day of routine MVPA performance. Consistency in exercise timing and other cues might help explain characteristic high PA levels among successful maintainers.
Schumacher LM, Thomas JG, Raynor HA, Rhodes RE, O'Leary KC, Wing RR, Bond DS. Relationship of Consistency in Timing of Exercise Performance and Exercise Levels Among Successful Weight Loss Maintainers. Obesity (Silver Spring). 2019 Aug;27(8):1285-1291. doi: 10.1002/oby.22535. Epub 2019 Jul 3. PMID: 31267674.
- Conscientiousness in weight loss maintainers and regainers
Objective: The role of personality in weight loss maintenance (WLM) is poorly understood. Although the personality trait of conscientiousness has been associated with health-promoting behaviors in general, no study has specifically evaluated the importance of conscientiousness for WLM. This study compared conscientiousness (both in aggregate and on the facet level) and control over healthy lifestyle behaviors (e.g., food quantity and temptations, consistent meal and sleep timing, exercise adherence, and psychosocial health and stress coping) in successful weight loss maintainers and regainers.
Method: The sample included 869 National Weight Control Registry participants who reported maintaining ≥ 30-lb weight loss for ≥ 1 year (maintainers) and 484 participants from Amazon's MTurk crowdsourcing marketplace who reported trying but failing to maintain weight loss for 1 year (regainers). Both groups self-reported the Cherynshenko Conscientiousness Scale, the Healthy Lifestyle & Personal Control Questionnaire, body mass index, and demographics in an online survey.
Results: Maintainers reported higher levels of total conscientiousness (p = .005), order, virtue, responsibility, and industriousness (ps ≤ .05), but not self-control, compared with regainers after controlling for basic demographic differences. Unexpectedly, regainers scored significantly higher on the facet of traditionalism (p < .001). Maintainers also reported greater degree of control over food quantity and temptations, consistent meal and sleep timing, and exercise adherence (ps < .001), but not psychosocial health and stress coping, compared to with regainers.
Conclusions: Successful weight loss maintainers reported small-to-moderately higher levels of conscientiousness compared with regainers. Evaluating whether conscientiousness can be incorporated into WLM treatment is warranted. (PsycInfo Database Record (c) 2020 APA, all rights reserved).
Gold JM, Carr LJ, Thomas JG, Burrus J, O'Leary KC, Wing R, Bond DS. Conscientiousness in weight loss maintainers and regainers. Health Psychol. 2020 May;39(5):421-429. doi: 10.1037/hea0000846. Epub 2020 Jan 30. PMID: 31999176.
- Self-control as measured by delay discounting is greater among successful weight losers than controls
Long-term weight loss maintenance is likely to require strong self-control in order to sustain changes in behavior patterns. We, therefore, tested the hypothesis that those who have successfully maintained weight loss may have superior self-control compared to control participants. Self-control was assessed using a delay discounting task through a webbased assessment of members of the National Weight Control Registry (NWCR: N = 757; non-obese = 605; obese = 152) and control participants (Control N = 443; nonobese = 236; obese = 207) from Amazon's Mechanical Turk. Both NWCR members that were currently obese (t = 5.42, p < 0.001) and nonobese (t = 5.28, p < 0.001) discounted the future less than control participants with comparable weight statuses. These results are indicative of higher levels of self-control behaviors in individuals that have lost and successfully maintained weight loss. Thus, successful weight losers may exhibit stronger self-control, as measured through discounting of future rewards, However, further research is needed to determine whether strong selfcontrol enables individuals to succeed at weight loss maintenance or develops as a consequence.
Bickel WK, Moody LN, Koffarnus M, Thomas JG, Wing R. Self-control as measured by delay discounting is greater among successful weight losers than controls. J Behav Med. 2018 Dec;41(6):891-896. doi: 10.1007/s10865-018-9936-5. Epub 2018 May 15. PMID: 29766471; PMCID: PMC6237669.
- A descriptive study of individuals successful at long-term maintenance of substantial weight loss
Despite extensive histories of overweight, the 629 women and 155 men in the registry lost an average of 30 kg and maintained a required minimum weight loss of 13.6 kg for 5 y. A little over one-half of the sample lost weight through formal programs; the remainder lost weight on their own. Both groups reported having used both diet and exercise to lose weight and nearly 77% of the sample reported that a triggering event had preceded their successful weight loss. Mean (+/-SD) current consumption reported by registry members was 5778 +/- 2200 kJ/d, with 24 +/- 9% of energy from fat, Members also appear to be highly active: they reported expending approximately 11830 kJ/wk through physical activity. Surprisingly, 42% of the sample reported that maintaining their weight loss was less difficult than losing weight. Nearly all registry members indicated that weight loss led to improvements in their level of energy, physical mobility, general mood, self-confidence, and physical health.
Klem ML, Wing RR, McGuire MT, Seagle HM & Hill JO (1997). A descriptive study of individuals successful at long-term maintenance of substantial weight loss.American Journal of Clinical Nutrition, 66, 239-246.
- Persons successful at long-term weight loss and maintenance continue to consume a low-energy, low-fat diet
Successful maintainers of weight loss reported continued consumption of a low-energy and low-fat diet.
Women in the registry reported eating an average of 1,306 kcal/day (24.3% of energy from fat); men reported consuming 1,685 kcal (23.5% of energy from fat).
Shick SM, Wing RR, Klem ML, McGuire MT, Hill JO & Seagle HM (1998). Persons successful at long-term weight loss and maintenance continue to consume a low calorie, low fat diet. Journal of the American Dietetic Association, 98, 408-413.
- Long-term maintenance of weight loss: do people who lose weight through various weight loss methods use different behaviors to maintain their weight?
Despite using different methods to lose weight, individuals who lost weight on their own, through an organized program, or with a liquid formula, use similar behavioral strategies to maintain their weight loss.
All three groups are maintaining their weight losses similarly by eating a low calorie diet (5792.3 kJ/d and 25% of daily calories from fat) and engaging in high levels of physical activity (11847.3 kJ/week).
McGuire MT, Wing RR, Klem ML, Seagle HM & Hill JO (1998). Long-term maintenance of weight loss: Do people who lose weight through various weight loss methods use different behaviors to maintain their weight? International Journal of Obesity, 22, 572-577.
- Psychological symptoms in individuals successful at long-term maintenance of weight loss
Maintainers' levels of distress and depression were lower than those of psychiatric samples and resembled those of community-based samples. Binge-eating and purging rates were comparable to rates of community samples. Maintainers' levels of restraint and disinhibition were markedly different from those of eating-disordered samples, resembling levels found in patients recently treated for obesity. There was no evidence that long-term suppression of body weight is associated with psychological distress.
Klem ML, Wing RR, McGuire MT, Seagle HM & Hill JO. (1998). Psychological symptoms in individuals successful at long-term maintenance of weight loss. Health Psychology, 17, 336-345.
- The behavioral characteristics of individuals who lose weight unintentionally
Unintentional weight losers had higher levels of smoking and drinking, were less physically active, and were less concerned about their diet and fat intake. Unintentional weight losers did not report having higher levels of disease such as high blood pressure or diabetes. However, unintentional weight losers who reported having such diseases were more likely to report that their weight loss had no effect or had worsened their disorder.
Discussion: Compared to intentional weight losers, those who lost their weight unintentionally reported engaging in more negative health behaviors that are related to disease morbidity and mortality. These data suggest that unintentional weight loss may be part of a cluster of behaviors that have a negative health impact.
McGuire MT, Wing RR, Klem ML, Hill JO (1999). The Behavioral characterstics of individuals who lose weight unintentionally. Obesity Research, 7, 485-490.
- Resting energy expenditure in reduced-obese subjects in the National Weight Control Registry
Background: Weight loss in obese subjects is associated with a reduction in resting metabolic rate (RMR). Whether the reduction can be explained solely by a reduction in lean body mass remains controversial.
Objective: Our objective was to determine whether the reduction in RMR after weight loss was proportional to the decrease in lean mass alone or was greater than could be explained by body composition.
Design: We measured the RMR, fasting respiratory quotient (RQ), and body composition in 40 reduced-obese subjects [ie, 7 men and 33 women who had lost > or = 13.6 kg (30 lb) and maintained the loss for > or = 1 y] enrolled in the National Weight Control Registry and 46 weight-matched control subjects (9 men, 37 women).
Results: A stepwise multiple regression found lean mass, fat mass, age, and sex to be the best predictors of RMR in both groups. After adjusting RMR for these variables, we found no significant difference in RMR (5926 +/- 106 and 6015 +/- 104 kJ/d) between the 2 groups (P = 0.35). When we adjusted fasting RQ for percentage body fat and age, the reduced-obese group had a slightly higher (0.807 +/- 0.006) RQ than the control group (0.791 +/- 0.005, P = 0.05). This may have been due to the consumption of a diet lower in fat or to a reduced capacity for fat oxidation in the reduced-obese group.
Conclusion: These results show that in at least some reduced-obese individuals there does not seem to be a permanent obligatory reduction in RMR beyond the expected reduction for a reduced lean mass.
Wyatt HR, Grunwald GK, Seagle HM, Klem ML, McGuire MT, Wing RR & Hill JO. (1999). Resting energy expenditure in reduced-obese subjects in the National Weight Control Registry. American Journal of Clinical Nutrition, 69, 1189-1193.
- What predicts weight regain in a group of successful weight losers?
This study identified predictors of weight gain versus continued maintenance among individuals already successful at long-term weight loss. Weight, behavior, and psychological information was collected on entry into the study and 1 year later. Thirty-five percent gained weight over the year of follow-up, and 59% maintained their weight losses. Risk factors for weight regain included more recent weight losses (less than 2 years vs. 2 years or more), larger weight losses (greater than 30% of maximum weight vs. less than 30%), and higher levels of depression, dietary disinhibition, and binge eating levels at entry into the registry. Over the year of follow-up, gainers reported greater decreases in energy expenditure and greater increases in percentage of calories from fat. Gainers also reported greater decreases in restraint and increases in hunger, dietary disinhibition, and binge eating. This study suggests that several years of successful weight maintenance increase the probability of future weight maintenance and that weight regain is due at least in part to failure to maintain behavior changes.
McGuire MT, Wing RR, Klem ML, Lang W & Hill JO. (1999). What predicts weight regain among a group of successful weight losers? Journal of Consulting & Clinical Psychology, 67, 177-185.
- Behavioral strategies of individuals who have maintained long-term weight losses
Objective: The purpose of the present study was to compare the behaviors of individuals who have achieved long-term weight loss maintenance with those of regainers and weight-stable controls.
Research methods and procedures: Subjects for the present study were participants in a random-digit dial telephone survey that used a representative sample of the U.S. adult population. Eating, exercise, self-weighing, and dietary restraint characteristics were compared among weight-loss maintainers: individuals who had intentionally lost > or =10% of their weight and maintained it for > or = 1 year (n = 69), weight-loss regainers: individuals who intentionally lost > or = 10% of their weight but had not maintained it (n = 56), and weight-stable controls: individuals who had never lost > or = 10% of their maximum weight and had maintained their current weight (+/-10 pounds) within the past 5 years (n = 113).
Results: Weight-loss maintainers had lost an average of 37 pounds and maintained it for over 7 years. These individuals reported that they currently used more behavioral strategies to control dietary fat intake, have higher levels of physical activity (especially strenuous activity), and greater frequency of self-weighing than either the weight-loss regainers or weight-stable controls. Maintainers and regainers did not differ in reported levels of dietary restraint, but both had higher levels of restraint than the weight-stable controls.
Discussion: These results suggest that weight-loss maintainers use more behavioral strategies to control their weight than either regainers or weight-stable controls. It would thus appear that long-term weight maintenance requires ongoing adherence to a low-fat diet and an exercise regimen in addition to continued attention to body weight.
McGuire MT, Wing RR, Klem ML, Hill JO. (1999). Behavioral strategies of indivduals who have maintained long-term weight losses. Obesity Research, 7, 334-341.
- The prevalence of weight loss maintenance among American adults
Background: Previous studies suggest that few individuals achieve long-term weight loss maintenance. Because most of these studies were based on clinical samples and focused on only one episode of weight loss, these results may not reflect the actual prevalence of weight loss maintenance in the general population.
Design: A random digit dial telephone survey was conducted to determine the point prevalence of weight loss maintenance in a nationally representative sample of adults in the United States. Weight loss maintainers were defined as individuals who, at the time of the survey, had maintained a weight loss of > or =10% from their maximum weight for at least 1 y. The prevalence of weight loss maintenance was first determined for the total group (n = 500), and then for the subgroup of individuals who were overweight (body mass index BMI > or =27 kg/m2 at their maximum (n = 228).
Results: Weight loss was quite common in this sample: 54% of the total sample and 62% of those who were ever overweight reported that they had lost > or =10% of their maximum weight at least once in their lifetime, with approximately one-half to two-thirds of these cases being intentional weight loss. Among those who had achieved an intentional weight loss of > or =10%, 47-49% had maintained this weight loss for at least 1 y at the time of the survey; 25-27% had maintained it for 5 y or more. Fourteen percent of all subjects surveyed and 21% of those with a history of obesity were currently 10% below their highest weight, had reduced intentionally, and had maintained this 10% weight loss for at least 1 y.
Conclusions: A large proportion of the American population has lost > or =10% of their maximum weight and has maintained this weight loss for at least 1 y. These findings are in sharp contrast to the belief that few people succeed in long-term weight loss maintenance.
McGuire MT, Wing RR, Hill JO. (1999). The prevalence of weight loss maintenance among American adults. International Journal of Obesity, 23, 1314-1319.
- A case-control study of successful maintenance of a substantial weight loss: individuals who lost weight through surgery versus those who lost weight through non-surgical means
Objective: To determine if method of weight loss (surgery; non-surgery) is associated with current levels of psychosocial functioning or current weight maintenance behaviors in individuals who have lost large amounts of weight.
Design: Subjects were 67 cases and 67 controls selected from the National Weight Control Registry, a longitudinal study of individuals successful at long-term maintenance of weight loss. Cases had initially lost weight through bariatric surgery while controls had lost weight through non-surgical means. The current psychosocial functioning and weight maintenance behaviors of cases and controls were assessed and compared.
Results: Cases and controls were matched on gender, current weight and total weight loss. Surgical cases reported significantly higher fat intake and lower physical activity levels. There were no differences in cases' and controls' reports of the impact of weight loss on other areas of their lives, neither were there differences on measures of depression or binge-eating.
Conclusions: Reported improvement in psychosocial functioning did not depend upon how weight was initially lost, but cases and controls appear to be using very different behaviors to maintain their weight losses.
Klem ML, Wing RR, Chang CH, Lang W, McGuire MT, Sugerman HJ, Hutchison SL, Makovich AL & Hill JO. (2000). A case-control study of successful maintenance of a substantial weight loss: Individuals who lost weight through surgery versus those who lost weight through non-surgical means. International Journal of Obesity, 24, 573-579.
- Does weight loss maintenance become easier over time?
Objective: Studies of health-related behaviors, including weight loss, have shown that risk of relapse decreases over time, although reasons for this relationship are unclear. The purpose of this cross-sectional study was to determine if subjects who have maintained weight losses for varying periods of time report different strategies for weight loss maintenance or differences in the effort and pleasure associated with weight maintenance behaviors.
Research methods and procedures: Subjects were 758 women and 173 men who had maintained losses of at least 30 lb (mean = 60 lb) for 2 years or longer (mean = 6.8 +/- 7.0 years). Self-administered questionnaires assessed subjects' use of weight maintenance strategies in the past year and their perceptions of the effort, attention, and pleasure associated with weight maintenance.
Results: Subjects who had maintained weight losses longer used fewer weight maintenance strategies and reported that less effort was required to diet and maintain weight and that less attention was required to maintain weight. The pleasure derived from exercise, low-fat eating, and maintaining weight was unrelated to duration of weight loss maintenance.
Discussion: As duration increases, a shift in the balance between the effort and pleasure of weight maintenance may occur. This shift may increase the likelihood of continued maintenance.
Klem ML, Wing, RR, Lang W, McGuire MT & Hill JO. (2000). Does weight loss maintenance become easier over time? Obesity Research, 8, 438-444.
- Successful weight loss maintenance
Obesity is now recognized as a serious chronic disease, but there is pessimism about how successful treatment can be. A general perception is that almost no one succeeds in long-term maintenance of weight loss. To define long-term weight loss success, we need an accepted definition. We propose defining successful long-term weight loss maintenance as intentionally losing at least 10% of initial body weight and keeping it off for at least 1 year. According to this definition, the picture is much more optimistic, with perhaps greater than 20% of overweight/obese persons able to achieve success. We found that in the National Weight Control Registry, successful long-term weight loss maintainers (average weight loss of 30 kg for an average of 5.5 years) share common behavioral strategies, including eating a diet low in fat, frequent self-monitoring of body weight and food intake, and high levels of regular physical activity. Weight loss maintenance may get easier over time. Once these successful maintainers have maintained a weight loss for 2-5 years, the chances of longer-term success greatly increase.
Wing RR & Hill JO. (2001). Successful weight loss maintenance. Annual Review of Nutrition, 21, 323-341.
- Long-term weight loss and breakfast in subjects in the National Weight Control Registry
Objective: To examine breakfast consumption in subjects maintaining a weight loss in the National Weight Control Registry (NWCR).
Research methods and procedures: A cross-sectional study in which 2959 subjects in the NWCR completed demographic and weight history questionnaires as well as questions about their current breakfast consumption. All subjects had maintained a weight loss of at least 13.6 kg (30 lb) for at least 1 year; on average these subjects had lost 32 kg and kept it off for 6 years.
Results: A large proportion of NWCR subjects (2313 or 78%) reported regularly eating breakfast every day of the week. Only 114 subjects (4%) reported never eating breakfast. There was no difference in reported energy intake between breakfast eaters and non-eaters, but breakfast eaters reported slightly more physical activity than non-breakfast eaters (p = 0.05).
Discussion: Eating breakfast is a characteristic common to successful weight loss maintainers and may be a factor in their success.
Wyatt HR, Grunwald OK, Mosca CL, Klem ML, Wing RR, Hill JO. (2002). Long-term weight loss and breakfast in subjects in the National Weight Control Registry. Obesity Research, 10, 78-82.
- Promoting long-term weight control: does dieting consistency matter?
Objective: The present study examined whether long-term weight loss maintenance is enhanced by maintaining the same diet regimen across the week and year or by dieting more strictly on weekdays and nonholiday periods than at other times.
Method: National Weight Control Registry participants (N=1429) indicated on an eight-point scale whether they dieted more strictly on weekends than weekdays, adhered to the same diet regimen throughout the week, or dieted more strictly on weekdays. Participants responded to a similar question about holiday and vacation eating. Participants were then followed prospectively to determine whether scores on these questions were related to self-reported weight regain over the subsequent 12 months.
Results: There was a linear relationship between scores on the dieting consistency questions and weight change over the 1-y period (P's <0.01), with smaller weight gains in those who reported more consistency. Participants who reported a consistent diet across the week were 1.5 times more likely to maintain their weight within 5 pounds over the subsequent year (OR=1.58, 95% CI: 1.2-2.2) than participants who dieted more strictly on weekdays. A similar relationship emerged between dieting consistency across the year and subsequent weight regain.
Conclusion: Dieting consistency appears to be a behavioral strategy that predicts subsequent long-term weight loss maintenance.
Gorin AA, Phelan S, Wing RR, Hill JO. (2004). Promoting long-term weight control: does dieting consistency matter? International Journal of Obesity and Related Metabolic Disorders, 28, 278-81.
- Amount of food group variety consumed in the diet and long-term weight loss maintenance
Objective: Decreases in variety of foods consumed within high-fat-dense food groups and increases in variety of foods consumed within low-fat-dense food groups are associated with lower energy intake and greater weight loss during obesity treatment and may assist with weight loss maintenance. This study examined food group variety in 2237 weight loss maintainers in the National Weight Control Registry, who had lost 32.2 +/- 18.0 kg (70.9 +/- 39.5 lbs) and maintained a weight loss of at least 13.6 kg (30 lbs) for 6.1 +/- 7.7 years.
Research methods and procedures: At entry into the registry, registry members completed a food frequency questionnaire from which amount of variety consumed from different food groups was assessed. To provide a context for interpreting the level of variety occurring in the diet of registry participants, food group variety was compared between registry participants and 96 individuals who had recently participated in a behavioral weight loss program and had lost at least 7% of initial body weight.
Results: Registry members reported consuming a diet with very low variety in all food groups, especially in those food groups higher in fat density. Registry participants consumed significantly (p < 0.001) less variety within all food groups, except fruit and combination foods, than recent weight losers after 6 months of weight loss treatment.
Discussion: These results suggest that successful weight loss maintainers consume a diet with limited variety in all food groups. Restricting variety within all food groups may help with consuming a low-energy diet and maintaining long-term weight loss.
Raynor H, Wing RR, Phelan S. (2005). Amount of food group variety consumed in the diet and long-term weight loss maintenance. Obesity Research, 13, 883-890.
- Medical triggers are associated with better short- and long-term weight loss outcomes
Background: Medical events are often reported as triggers for weight loss, but it is unknown whether medical triggers result in better short- and long-term weight control.
Methods: The relationship between medical triggers and weight loss was examined in the National Weight Control Registry (NWCR), a database of individuals who have lost > or =30 lbs and kept it off for > or =1 year. Recall of weight loss triggers may become difficult over time, thus participants were limited to those reporting weight loss <5 years ago. Three groups were examined: (1) participants with medical triggers (N = 207), (2) participants with nonmedical triggers (N = 539), and (3) participants with no trigger (N = 171).
Results: Participants with medical triggers were older than those with nonmedical triggers or no trigger (50.5 +/- 11.7, 44.9 +/- 11.8, 46.7 +/- 13.3 years; P = 0.0001), had a higher initial BMI at entry into the NWCR (26.1 +/- 5.0, 25.0 +/- 4.3, 24.8 +/- 4.4 kg/m2; P = 0.004), and were more likely to be male (37.1%, 18%, 17.2%; P = 0.0001). Participants with medical triggers reported greater initial weight loss than those with nonmedical triggers or no trigger (36.5 +/- 25.0, 31.8 +/- 16.6, 31.8 +/- 17.1 kg; P = 0.01). Participants with medical triggers also gained less weight over 2 years of follow-up than those with nonmedical triggers or no trigger (P = 0.003).
Conclusions: Medical triggers may produce a teachable moment for weight control, resulting in better initial weight loss and long-term maintenance.
Gorin AA, Phelan S, Hill JO, Wing RR. (2004). Medical triggers are associated with better short- and long-term weight loss outcomes. Preventive Medicine, 39, 612-16.
- Recovery from relapse among successful weight maintainers
Background: Little is known about the natural history of weight change among persons who are successful at losing weight.
Objective: This study evaluated the occurrence of weight regain and recovery among 2400 persons in the National Weight Control Registry (NWCR) who had lost an average (+/- SD) of 32.1 +/- 17.8 kg and had kept it off for 6.5 +/- 8.1 y.
Design: Participants were evaluated prospectively over 2 y.
Results: The mean reported weight change from entry into the NWCR to 2 y later was 3.8 +/- 7.6 kg. At year 2, 96.4% of the sample remained > or =10% below their maximum lifetime weight. However, small regains were common, and few persons were able to re-lose weight after any weight regain. Of the participants who gained any weight between baseline and year 1 (n = 1483; 65.7%), only 11.0% returned to their baseline weight or below at year 2. Of the participants who relapsed, which was defined as a weight regain of > or =5% at year 1 (n = 575, or 25.5% of the sample), only 4.7% returned to their baseline weight or below at year 2, and only 12.9% re-lost at least half of their year 1 gain by year 2. Logistic regression showed that recovery was related to gaining less at year 1 and to smaller increases in depressive symptoms between baseline and year 1.
Conclusion: Although successful weight losers continued to maintain a large percentage of their weight losses over 2 y, recovery from even minor weight regain was uncommon.
Phelan S, Wing RR, Hill JO, Dibello J. (2003). Recovery from relapse among successful weight maintainers. American Journal of Clinical Nutrition, 78, 1079-1084.
- Lessons from Patients Who Have Successfully Maintained Weight Loss
Lessons of Weight Control
- There is an important difference between weight loss and weight maintenance
- People who have successfully maintained weight loss share similarities in how they keep weight off
- Many people wishing to lose weight experience an important "trigger" event in their lives that becomes self-motivating
- Maintenance of weight loss becomes easier over time
- Weight loss is reported to improve the overall quality of a person's life
- Maintaining weight loss does not increase eating disorders
- Successful weight-loss maintenance is achievable
Successful Behaviors of NWCR Participants for Weight-Loss Maintenance
- Eat a moderately low-fat diet
- Watch total calories
- Eat breakfast
- Self-monitor
- Engage in high levels of physical activity
Wyatt HR, Phelan S, Wing RR, Hill JO. (2005). Lessons from patients who have successfully maintained weight loss. Obesity Managament, 1, 56-61.
- The National Weight Control Registry: is it useful in helping deal with our obesity epidemic?
The National Weight Control Registry (NWCR) consists of over 4800 individuals who have been successful in long-term weight loss maintenance. The purpose of establishing the NWCR was to identify the common characteristics of those who succeed in long-term weight loss maintenance. We found very little similarity in how these individuals lost weight but some common behaviors in how they are keeping their weight off. To maintain their weight loss NWCR participants report eating a relatively low-fat diet, eating breakfast almost every day, weighing themselves regularly, and engaging in high levels (about 1 hour/day) of physical activity. Because this is not a random sample of those who attempt weight loss, the results have limited generalizability to the entire population of overweight and obese individuals. The value of this project lies in identifying potential strategies that may help others be more successful in keeping weight off.
Hill JO, Wyatt HR, Phelan S, Wing RR. (2005). The National Weight Control Registry: is it useful in helping deal with our obesity epidemic? Journal of Nutrition Education and Behavior, 37, 206-210.
- Long-term weight loss maintenance
There is a general perception that almost no one succeeds in long-term maintenance of weight loss. However, research has shown that approximately 20% of overweight individuals are successful at long-term weight loss when defined as losing at least 10% of initial body weight and maintaining the loss for at least 1 y. The National Weight Control Registry provides information about the strategies used by successful weight loss maintainers to achieve and maintain long-term weight loss. National Weight Control Registry members have lost an average of 33 kg and maintained the loss for more than 5 y. To maintain their weight loss, members report engaging in high levels of physical activity ( approximately 1 h/d), eating a low-calorie, low-fat diet, eating breakfast regularly, self-monitoring weight, and maintaining a consistent eating pattern across weekdays and weekends. Moreover, weight loss maintenance may get easier over time; after individuals have successfully maintained their weight loss for 2-5 y, the chance of longer-term success greatly increases. Continued adherence to diet and exercise strategies, low levels of depression and disinhibition, and medical triggers for weight loss are also associated with long-term success. National Weight Control Registry members provide evidence that long-term weight loss maintenance is possible and help identify the specific approaches associated with long-term success
Wing RR & Phelan S. (2005). Long-term weight loss maintenance. American Journal of Clinical Nutrition, 82, 222S-225S.
- Are the eating and exercise habits of successful weight losers changing?
Objective: The purpose of this study was to examine whether the diet and exercise behaviors of successful weight losers entering the National Weight Control Registry (NWCR) have changed between 1995 and 2003.
Research method and procedures: Participants (N = 2708) were members of the NWCR who enrolled in intermittent years since 1995. Participants had lost an average of 33.1 kg and maintained a 13.6-kg loss for 5.8 years before enrollment. Evaluations of diet and physical activity were conducted at entry into the NWCR and prospectively over 1 year.
Results: From 1995 to 2003, the daily percentage of calories from fat increased from 23.8% to 29.4%, saturated fat intake increased from 12.3 to 154.0 g/d, and calories from carbohydrate decreased from 56.0% to 49.3% (p < 0.0001). The proportion consuming <90 grams of carbohydrate (considered a low-carbohydrate diet) increased from 5.9% to 17.1% (p = 0.0001). Physical activity was elevated in 1995 (mean = 3316 kcal/wk) but comparable in all other years (mean = 2620 kcal/wk). Stepwise regression collapsing across cohorts indicated that weight regain over 1 year was related to higher levels of caloric intake, fast food consumption, and fat intake and lower levels of physical activity (p < 0.03).
Discussion: The macronutrient composition of the diet of NWCR members has shifted over the past decade. Still, only a minority consumes a low-carbohydrate diet. Despite changes in the diet over time, the variables associated with long-term maintenance of weight loss were the same: continued consumption of a low-calorie diet with moderate fat intake, limited fast food, and high levels of physical activity.
Phelan S, Wyatt H, Hill JO, Wing RR. (2006). Are the Eating and Exercise Habits of Successful Weight Losers Changing? Obesity Research, 14, 710-716.
- Television viewing and long-term weight maintenance: results from the National Weight Control Registry
Objective: To examine the role of television (TV) viewing in long-term maintenance of weight loss.
Research methods and procedures: All subjects (N = 1422) were enrolled in the National Weight Control Registry (NWCR), a national sample of adults who have maintained a minimum weight loss of 13.6 kg for at least 1 year. Participants self-reported the average number of hours of weekly TV viewing at entry into the NWCR and at a 1-year follow-up. Cross-sectional and prospective analyses were performed to determine the frequency of TV viewing and the extent to which TV viewing was independently associated with weight regain over the 1-year of follow-up.
Results: A relatively high proportion (62.3%) of participants reported watching 10 or fewer hours of TV per week on entry in the NWCR. More than one third of the sample (36.1%) reported watching <5 h/wk, whereas only 12.4% watched > or =21 h/wk, which contrasts markedly from the national average of 28 hours of TV viewing per week reported by American adults. Both baseline TV viewing (p < or = 0.02) and increases in TV viewing (p < or = 0.001) over the follow-up were significant predictors of 1-year weight regain, independent of physical activity and dietary behaviors.
Discussion: Individuals who are successful at maintaining weight loss over the long term are likely to spend a relatively minimal amount of time watching TV
Raynor D, Phelan S, Hill JO, Wing RR. (2006). Television Viewing and Long-Term Weight Maintenance: Results from the National Weight Control Registry. Obesity Research, 14, 1816-1824.
- Empirical evaluation of physical activity recommendations for weight control in women
Purpose: Recent recommendations advise 30-60 min of physical activity per day to prevent weight gain and 60-90 min to prevent weight regain. No studies have used objective measures of physical activity to verify these public health recommendations. The purpose of this study was to use objective measures to quantify the amount and intensity of physical activity in a weight-loss-maintainer group and an always-normal-weight group, and, thus,empirically evaluate the recommendations for prevention of weight gain versus regain.
Methods: The weight-loss-maintainer group (N = 135) lost >or= 30.6 kg, maintained >or= 10% weight loss for 14.2 yr, and had a BMI of 22.0 kg.m(-2). The always-normal-weight group (N = 102) had a BMI of 21.1 kg.m(-2) and no history of overweight. Accelerometry was used to assess the amount and intensity of physical activity.
Results: The weight-loss-maintainer group spent significantly more minutes per day than the always-normal-weight group in physical activity (58.6 vs 52.1; P = 0.0001), largely because of more time spent in higher-intensity activities (24.4 vs 16.9; P = 0.02). The majority of individuals in the always-normal-weight group engaged in 30-60 min.d(-1) of physical activity, whereas a greater proportion of individuals in the weight-loss-maintainer group engaged in > 60 min (P = 0.002).
Conclusions: Findings support current recommendations that more activity may be needed to prevent weight regain than to prevent weight gain. Including some higher-intensity activity may also be advisable for weight-loss maintenance.
Phelan S, Roberts M, Lang W, Wing RR. (2007). Empirical Evaluation of Physical Activity Recommendations for Weight Control in Women. Medicine & Science in Sports & Exercise, 39, 1832-1836.
- Three-year weight change in successful weight losers who lost weight on a low-carbohydrate diet
Objective: The purpose of this study was to evaluate long-term weight loss and eating and exercise behaviors of successful weight losers who lost weight using a low-carbohydrate diet.
Research methods and procedures: This study examined 3-year changes in weight, diet, and physical activity in 891 subjects (96 low-carbohydrate dieters and 795 others) who enrolled in the National Weight Control Registry between 1998 and 2001 and reported >or=30-lb weight loss and >or=1 year weight loss maintenance.
Results: Only 10.8% of participants reported losing weight after a low-carbohydrate diet. At entry into the study, low-carbohydrate diet users reported consuming more kcal/d (mean +/- SD, 1,895 +/- 452 vs. 1,398 +/- 574); fewer calories in weekly physical activity (1,595 +/- 2,499 vs. 2,542 +/- 2,301); more calories from fat (64.0 +/- 7.9% vs. 30.9 +/- 13.1%), saturated fat (23.8 +/- 4.1 vs. 10.5 +/- 5.2), monounsaturated fat (24.4 +/- 3.7 vs. 11.0 +/- 5.1), and polyunsaturated fat (8.6 +/- 2.7 vs. 5.5 +/- 2.9); and less dietary restraint (10.8 +/- 2.9 vs. 14.9 +/- 3.9) compared with other Registry members. These differences persisted over time. No differences in 3-year weight regain were observed between low-carbohydrate dieters and other Registry members in intent-to-treat analyses (7.0 +/- 7.1 vs. 5.7 +/- 8.7 kg).
Discussion: It is possible to achieve and maintain long-term weight loss using a low-carbohydrate diet. The long-term health effects of weight loss associated with a high-fat diet and low activity level merits further investigation.
Phelan S, Wyatt H, DiBello J, Fava JL, Hill JO, Wing RR. (2007). Three-Year Weight Change in Successful Weight Losers Who Lost Weight in a Low-Carbohydrate Diet. Obesity; 15, 2470-2477.
- Internal disinhibition predicts weight regain following weight loss and weight loss maintenance
Objective: The disinhibition scale of the Eating Inventory predicts weight loss outcome; however, it may include multiple factors. The purpose of this study was to examine the factor structure of the disinhibition scale and determine how its factors independently relate to long-term weight loss outcomes.
Research methods and procedures: Exploratory factor analysis of the disinhibition scale was conducted on 286 participants in a behavioral weight loss trial (TRIM), and confirmatory factor analysis was conducted on 3,345 members of the National Weight Control Registry (NWCR), a registry of successful weight loss maintainers. Multivariate regressions were used to examine the relationships between the disinhibition scale factors and weight over time in both samples.
Results: Using baseline data from TRIM, two factors were extracted from the disinhibition scale: 1) an "internal" factor that described eating in response to internal cues, such as feelings and thoughts; and 2) an "external" factor that described eating in response to external cues, such as social events. This factor structure was confirmed using confirmatory factor analysis in the NWCR. In TRIM, internal disinhibition significantly predicted weight loss at 6 months (p = 0.03) and marginally significantly predicted weight loss at 18 months (p = 0.06), with higher levels of internal disinhibition at baseline predicting less weight loss; external disinhibition did not predict weight loss at any time-point. In NWCR, internal disinhibition significantly predicted one-year weight change (p = 0.001), while external disinhibition did not.
Discussion: These results suggest that it is the disinhibition of eating in response to internal cues that is associated with poorer long-term weight loss outcomes.
Niemeier HM, Phelan S, Fava JL, Wing RR. (2007). Internal Disinhibition Predicts Weight Regain Following Weight Loss and Weight Loss Maintenance. Obesity, 15, 2485-2494.
- Consistent self-monitoring of weight: a key component of successful weight loss maintenance
Objective: The objectives were to investigate the characteristics associated with frequent self-weighing and the relationship between self-weighing and weight loss maintenance.
Research methods and procedures: Participants (n = 3003) were members of the National Weight Control Registry (NWCR) who had lost >or=30 lbs, kept it off for >or=1 year, and had been administered the self-weighing frequency assessment used for this study at baseline (i.e., entry to the NWCR). Of these, 82% also completed the one-year follow-up assessment.
Results: At baseline, 36.2% of participants reported weighing themselves at least once per day, and more frequent weighing was associated with lower BMI and higher scores on disinhibition and cognitive restraint, although both scores remained within normal ranges. Weight gain at 1-year follow-up was significantly greater for participants whose self-weighing frequency decreased between baseline and one year (4.0 +/- 6.3 kg) compared with those whose frequency increased (1.1 +/- 6.5 kg) or remained the same (1.8 +/- 5.3 kg). Participants who decreased their frequency of self-weighing were more likely to report increases in their percentage of caloric intake from fat and in disinhibition, and decreases in cognitive restraint. However, change in self-weighing frequency was independently associated with weight change.
Discussion: Consistent self-weighing may help individuals maintain their successful weight loss by allowing them to catch weight gains before they escalate and make behavior changes to prevent additional weight gain. While change in self-weighing frequency is a marker for changes in other parameters of weight control, decreasing self-weighing frequency is also independently associated with greater weight gain.
Butryn ML, Phelan S, Hill JO, Wing RR. (2007). Consistent Self-monitoring of Weight: A Key Component of Successful Weight Loss Maintenance. Obesity, 15, 3091-3096.
- Physical activity patterns in the National Weight Control Registry
Objective: The National Weight Control Registry (NWCR) was established in 1993 to examine the characteristics of those who are successful at weight loss: individuals maintaining a 13.6-kg weight loss for >1 year. The size of the registry has increased substantially since the early descriptions of this group a decade ago. The purpose of this study was to describe in detail the weekly physical activity habits of NWCR members, to examine the relationship between amount of activity and demographic characteristics, and to determine if changes in activity parameters have occurred over time.
Methods and procedures: Participants were 887 men and 2,796 women who enrolled in the NWCR between 1993 and 2004. Physical activity was evaluated at registry entry using the Paffenbarger Physical Activity Questionnaire.
Results: NWCR entrants report an average of 2,621 +/- 2,252 kcal/week in physical activity. There is considerable variability in the amount of activity reported: 25.3% report <1,000 kcal/week and 34.9% report >3,000 kcal/week. Activity level on registry entry is related to the magnitude but not the duration of weight loss. The amount of activity reported by men has decreased over time while no significant change was observed in women. Changes in the types of activities most frequently reported were also observed.
Discussion: Overall, NWCR participants are an extremely physically active group. However, the amount of activity reported is highly variable, making it difficult to develop a single recommendation for the optimum amount of physical activity for weight loss maintenance. A better understanding of individual-specific determinants of how much activity is required for weight loss maintenance ought to be a high research priority.
Catenacci VA, Ogden LG, Stuht J, Phelan S, Wing RR, Hill JO, Wyatt HR. (2008). Physical Activity Patterns in the National Weight Control Registry. Obesity; 16, 153-161.
- Holiday weight management by successful weight losers and normal weight individuals
This study compared weight control strategies during the winter holidays among successful weight losers (SWL) in the National Weight Control Registry and normal weight individuals (NW) with no history of obesity. SWL (n = 178) had lost a mean of 34.9 kg and had kept > or = 13.6 kg off for a mean of 5.9 years. NW (n = 101) had a body mass index of 18.5-24.9 kg/m(2). More SWL than NW reported plans to be extremely strict in maintaining their usual dietary routine (27.3% vs. 0%) and exercise routine (59.1% vs. 14.3%) over the holidays. Main effects for group indicated that SWL maintained greater exercise, greater attention to weight and eating, greater stimulus control, and greater dietary restraint, both before and during the holidays. A Group x Time interaction indicated that, over the holidays, attention to weight and eating declined significantly more in SW than in NW. More SWL (38.9%) than NW (16.7%) gained > or = 1 kg over the holidays, and this effect persisted 1 month later (28.3% and 10.7%, respectively). SWL worked harder than NW did to manage their weight, but they appeared more vulnerable to weight gain during the holidays.
Phelan S, Wing RR, Raynor HA, Dibello J, Nedeau K, Peng W. (2008). Holiday Weight Management by Successful Weight Losers and Normal Weight Individuals. Journal of Consulting and Clinical Psychology; 76, 442-448.
- Weight-loss maintenance in successful weight losers: surgical vs non-surgical methods
Objective: As large weight losses are rarely achieved through any method except bariatric surgery, there have been no studies comparing individuals who initially lost large amounts of weight through bariatric surgery or non-surgical means. The National Weight Control Registry (NWCR) provides a resource for making such unique comparisons. This study compared the amount of weight regain, behaviors and psychological characteristics in NWCR participants who were equally successful in losing and maintaining large amounts of weight through either bariatric surgery or non-surgical methods.
Design: Surgical participants (n=105) were matched with two non-surgical participants (n=210) on gender, entry weight, maximum weight loss and weight-maintenance duration, and compared prospectively over 1 year.
Results: Participants in the surgical and non-surgical groups reported having lost approximately 56 kg and keeping > or =13.6 kg off for 5.5+/-7.1 years. Both groups gained small but significant amounts of weight from registry entry to 1 year (P=0.034), but did not significantly differ in magnitude of weight regain (1.8+/-7.5 and 1.7+/-7.0 kg for surgical and non-surgical groups, respectively; P=0.369). Surgical participants reported less physical activity, more fast food and fat consumption, less dietary restraint, and higher depression and stress at entry and 1 year. Higher levels of disinhibition at entry and increased disinhibition over 1 year were related to weight regain in both groups.
Conclusions: Despite marked behavioral differences between the groups, significant differences in weight regain were not observed. The findings suggest that weight-loss maintenance comparable with that after bariatric surgery can be accomplished through non-surgical methods with more intensive behavioral efforts. Increased susceptibility to cues that trigger overeating may increase risk of weight regain regardless of initial weight-loss method.
Bond DS, Phelan S, Leahey TM, Hill JO, Wing RR. (2009). Weight-loss maintenance in successful weight losers: surgical vs non-surgical methods. International Journal of Obesity, 33, 173-180.
- Physical activity patterns using accelerometry in the National Weight Control Registry
The National Weight Control Registry (NWCR) was established in 1993 to examine characteristics of successful weight-loss maintainers. This group consistently self-reports high levels of physical activity. The aims of this study were to obtain objective assessments of physical activity in NWCR subjects and compare this to physical activity in both normal-weight and overweight controls. Individuals from the NWCR (n = 26) were compared to a never obese normal-weight control group matched to the NWCR group's current BMI (n = 30), and an overweight control group matched to the NWCR group's self-reported pre-weight-loss BMI (n = 34). Objective assessment of physical activity was obtained for a 1-week period using a triaxial accelerometer. Bouts of moderate-to-vigorous physical activity (MVPA) ≥10 min in duration, as well as nonbout MVPA (bouts of MVPA 1-9 min in duration) were summed and characterized. NWCR subjects spent significantly (P = 0.004) more time per day in sustained bouts of MVPA than overweight controls (41.5 ± 35.1 min/day vs. 19.2 ± 18.6 min/day) and marginally (P = 0.080) more than normal controls (25.8 ± 23.4). There were no significant differences between the three groups in the amount of nonbout MVPA. These results provide further evidence that physical activity is important for long-term maintenance of weight loss and suggest that sustained volitional activity (i.e., ≥10 min in duration) may play an important role. Interventions targeting increases in structured exercise may be needed to improve long-term weight-loss maintenance.
Catenacci VA, Grunwald GK, Ingebrigtsen JP, Jakicic JM, McDermott MD Phelan S, Wing RR, Hill JO, Wyatt HR. (2011).Physical Activity Patterns Using Accelerometry in the National Weight Control Registry. Obesity, 19, 6, 1163-1170.
- Cluster analysis of the national weight control registry to identify distinct subgroups maintaining successful weight loss
The National Weight Control Registry (NWCR) is the largest ongoing study of individuals successful at maintaining weight loss; the registry enrolls individuals maintaining a weight loss of at least 13.6 kg (30 lb) for a minimum of 1 year. The current report uses multivariate latent class cluster analysis to identify unique clusters of individuals within the NWCR that have distinct experiences, strategies, and attitudes with respect to weight loss and weight loss maintenance. The cluster analysis considers weight and health history, weight control behaviors and strategies, effort and satisfaction with maintaining weight, and psychological and demographic characteristics. The analysis includes 2,228 participants enrolled between 1998 and 2002. Cluster 1 (50.5%) represents a weight-stable, healthy, exercise conscious group who are very satisfied with their current weight. Cluster 2 (26.9%) has continuously struggled with weight since childhood; they rely on the greatest number of resources and strategies to lose and maintain weight, and report higher levels of stress and depression. Cluster 3 (12.7%) represents a group successful at weight reduction on the first attempt; they were least likely to be overweight as children, are maintaining the longest duration of weight loss, and report the least difficulty maintaining weight. Cluster 4 (9.9%) represents a group less likely to use exercise to control weight; they tend to be older, eat fewer meals, and report more health problems. Further exploration of the unique characteristics of these clusters could be useful for tailoring future weight loss and weight maintenance programs to the specific characteristics of an individual.
Ogden LG, Stroebele N, Wyatt HR, Catenacci VA, Peters JC, Stuht J, Wing RR, Hill JO. (2012). Cluster analysis of the National Weight Control Registry to identify distinct subgroups maintaining successful weight loss. Obesity, 20, 10, 2039-2047.
- Differences in motivations and weight loss behaviors in young adults and older adults in the National Weight Control Registry
Objective: The goal of this study was to compare young adults (YA) and older adults (OA) in the National Weight Control Registry on motivations for weight loss and weight-loss behaviors.
Design and methods: Participants (n = 2,964, 82% female, 94% White, BMI = 24.8 ± 4.4) were divided into two age groups (18-35 vs. 36-50) and compared on motivations, strategies for weight loss, diet, physical activity (PA), and the three-factor eating questionnaire.
Results: YA were 28.6% of the sample (n = 848). YA and OA achieved similar weight losses (P = 0.38), but duration of maintenance was less in YA (43 vs. 58 months, P < 0.001). YA were more likely to cite appearance and social motivations for weight loss, were less motivated by health, and were less likely to report a medical trigger for weight loss (P's < 0.001). YA were more likely to use exercise classes and to lose weight on their own, and less likely to use a commercial program (P's < 0.001). YA reported engaging in more high-intensity PA (P = 0.001). There were no group differences in total calories consumed (P = 0.47), or percent calories from fat (P = 0.97), alcohol (P = 0.52), or sugar-sweetened beverages (P = 0.26).
Conclusions: YA successful weight losers (SWL) are motivated more by appearance and social influences than OA, and physical activity appears to play an important role in their weight-loss efforts. The differences reported by YA and OA SWL should be considered when developing weight-loss programs for YA.
LaRose JG, Leahey TM, Hill JO, Wing RR. (2013). Differences in motivations and weight loss behaviors in young adults and older adults in the National Weight Control Registry. Obesity, 21, 3, 449-453.
- Weight-loss maintenance for 10 years in the National Weight Control Registry
Background: The challenge of weight-loss maintenance is well known, but few studies have followed successful weight losers over an extended period or evaluated the effect of behavior change on weight trajectories.
Purpose: To study the weight-loss trajectories of successful weight losers in the National Weight Control Registry (NWCR) over a 10-year period, and to evaluate the effect of behavior change on weight-loss trajectories.
Methods: A 10-year observational study of self-reported weight loss and behavior change in 2886 participants (78% female; mean age 48 years) in the NWCR who at entry had lost at least 30 lbs (13.6 kg) and kept it off for at least one year. Data were collected in 1993-2010; analysis was conducted in 2012.
Main outcome measures: Weight loss (kilograms; percent weight loss from maximum weight).
Results: Mean weight loss was 31.3 kg (95% CI=30.8, 31.9) at baseline, 23.8 kg (95% CI=23.2, 24.4) at 5 years and 23.1±0.4 kg (95% CI=22.3, 23.9) at 10 years. More than 87% of participants were estimated to be still maintaining at least a 10% weight loss at Years 5 and 10. Larger initial weight losses and longer duration of maintenance were associated with better long-term outcomes. Decreases in leisure-time physical activity, dietary restraint, and frequency of self-weighing and increases in percentage of energy intake from fat and disinhibition were associated with greater weight regain.
Conclusions: The majority of weight lost by NWCR members is maintained over 10 years. Long-term weight-loss maintenance is possible and requires sustained behavior change.
Thomas JG, Bond DS, Phelan S, Hill JO, Wing RR. (2014). Weight-loss maintenance for 10 years in the National Weight Control Registry. American Journal of Preventive Medicine, 46, 1, 17-23.
- Dietary habits and weight maintenance success in high versus low exercisers in the National Weight Control Registry
Background: The National Weight Control Registry (NWCR) was established to examine characteristics of successful weight loss maintainers. This study compares the diet and behavioral characteristics and weight regain trajectories of NWCR members with differing physical activity (PA) levels at baseline.
Methods: Participants (n = 3591) were divided into 4 levels of self-reported PA at registry entry (< 1000, 1000 to < 2250, 2250 to < 3500, and ≥ 3500 kcals/week). We compared self-reported energy intake (EI), macronutrient composition, eating behaviors (dietary restraint, hunger, and disinhibition), weight loss maintenance strategies, and 3 year weight regain between these 4 activity groups.
Results: Those with the highest PA at registry entry had lost the most weight, and reported lower fat intake, more dietary restraint, and greater reliance on several specific dietary strategies to maintain weight loss. Those in the lowest PA category maintained weight loss despite low levels of PA and without greater reliance on dietary strategies. There were no differences in odds of weight regain at year 3 between PA groups.
Conclusions: These findings suggest that there is not a "one size fits all strategy" for successful weight loss maintenance and that weight loss maintenance may require the use of more strategies by some individuals than others.
Catenacci VA, Odgen L, Phelan S, Thomas JG, Hill JO, Wing RR, Wyatt H. (2014). Dietary habits and weight maintenance success in high versus low exercisers in the National Weight Control Registry. Journal of Physical Activity and Health, 11, 8, 1540-1548.
- Low/no calorie sweetened beverage consumption in the National Weight Control Registry
Objective: The aim of this cross-sectional study was to evaluate prevalence of and strategies behind low/no calorie sweetened beverage (LNCSB) consumption in successful weight loss maintainers.
Methods: An online survey was administered to 434 members of the National Weight Control Registry (NWCR, individuals who have lost ≥13.6 kg and maintained weight loss for > 1 year).
Results: While few participants (10%) consume sugar-sweetened beverages on a regular basis, 53% regularly consume LNCSB. The top five reasons for choosing LNCSB were for taste (54%), to satisfy thirst (40%), part of routine (27%), to reduce calories (22%) and to go with meals (21%). The majority who consume LNCSB (78%) felt they helped control total calorie intake. Many participants considered changing patterns of beverage consumption to be very important in weight loss (42%) and maintenance (40%). Increasing water was by far the most common strategy, followed by reducing regular calorie beverages.
Conclusions: Regular consumption of LNCSB is common in successful weight loss maintainers for various reasons including helping individuals to limit total energy intake. Changing beverage consumption patterns was felt to be very important for weight loss and maintenance by a substantial percentage of successful weight loss maintainers in the NWCR.
Catenacci VA, Pan Z, Thomas JG, Ogden LG, Roberts SA, Wyatt HR, Wing RR, Hill JO. (2014). Low/no calorie sweetened beverage consumption in the National Weight Control Registry. Obesity, 22, 10, 2244-2251.
- Successful weight loss maintenance associated with morning chronotype and better sleep quality
It is not known whether individuals successful at long term weight loss maintenance differ in chronotype (i.e., being a "morning" or "evening" person) or sleep habits compared to those who are overweight and obese. We compared Morningness-Eveningness Questionnaire (MEQ) and Pittsburgh Sleep Quality Index scores of 690 National Weight Control Registry (NWCR) members (73 % female, 93 % white, age = 51.7 ± 12.5, BMI = 26.4 ± 5.1) to 75 enrollees in two behavioral weight loss interventions (INT; 77 % female, 88 % white, age = 55.7 ± 10.4, BMI = 36.2 ± 4.7). Controlling for age, MEQ scores were higher in NWCR than INT, p = .004, such that more NWCR than INT were morning-types and fewer were evening types, p = .014. Further, NWCR participants reported better sleep quality, longer sleep duration, and shorter latency to sleep onset compared to INT, ps < .05, and fewer NWCR participants reported <6 or <7 h of sleep, ps < .01. Future studies should examine if these factors change as a result of weight loss or are predictors of weight outcome.
Ross KM, Thomas JG, Wing RR. (2015). Successful weight loss maintenance associated with morning chronotype and better sleep quality. Journal of Behavioral Medicine.
- Strategies to manage weight during the holiday season among US adults: A descriptive study from the National Weight Control Registry
Background: Holidays are challenging for weight control and are consistently associated with weight gain. Managing holiday weight gain may be especially difficult for individuals with higher body weight or a history of overweight/obesity. The current study evaluated how individuals with a history of successful weight loss plan for the holiday season and how the use of weight control strategies was associated with weight change.
Methods: A subgroup of participants in the National Weight Control Registry (NWCR) were asked to complete a survey before (November) and after the holidays (January). At pre-holiday, participants reported height, weight, and weight goals for the holiday season (lose, maintain, minimize gains, or gain), and selected the top three weight control strategies they planned to use (from a list of 18). Post-holiday, participants reported weight and how often (frequently, infrequently, or not at all) they used each of the 18 strategies throughout the holidays.
Results: Individuals who completed both surveys were included in the analysis (n = 683; 69% female, 93% white, 54.6 years [SD: 13.2], 26.9 kg/m2 [SD: 5.5]). Pre-holiday, 64% of participants were currently trying to lose weight. Only 35% of the sample wanted to continue losing weight during the holiday season. The most common strategies individuals planned to use during the holiday season were evidence based (maintaining exercise, monitoring portions, tracking foods, and self-weighing). Participants gained 0.66 kg (SD: 1.85) from pre- to post-holiday and reported using an average of 12/18 strategies. A greater number of strategies were associated with less weight gain (F[1, 670] = 4.28, p = 0.04). Daily self-weighing (p = 0.03) and prioritizing food choices (p = 0.02) were individually associated with less weight gain.
Discussion: Participants in the NWCR entered the holiday season with a variety of goals for their weight and used many different strategies to control their weight. Having a wider range of strategies may be helpful to navigate the challenges to weight control during the holidays.
Olson K, Coffino JA, Thomas JG, Wing RR. Strategies to manage weight during the holiday season among US adults: A descriptive study from the National Weight Control Registry. Obes Sci Pract. 2020 Dec 15;7(2):232-238. doi: 10.1002/osp4.470. PMID: 33841893; PMCID: PMC8019277.
**
Basics of all practice guidelines:
- Identify patients who need to lose weight
- Match treatment benefits with risk profiles
- Diet for weight loss
- Lifestyle and intervention counseling
- Select appropriate patients for bariatric treatment
Other notes:
- Initial weight loss is predictor for later weight loss and weight loss maintenance
- Weight loss plateau typically at 6 months
- To continue weight loss, need to further reduce calorie intake and/or increase calorie expenditure
- Weight cycling does not result in alterations in body composition, resting energy expenditure, or alteration of fat mobilization
- Resting and non-resting metabolic rates decrease as individuals lose weight
- Lean body mass decreases leading to compensatory changes in energy expenditure, muscle efficiency during physical activity, and decrease in leptin levels combats starvation (and the weight loss)
- Body weight change is primary dependent on calorie deficit not macronutrient composition
- Initial clinical goal:
- Structured and planned eating schedule
- Use food journal for 3-7 days
- Look for food choices/patterns
Coding for Weight Loss
| Intake/New | Coding |
|---|---|
| Initial Evaluation | 99202-99205 |
| Screening for Obesity | 99420 |
| EKG | 93000 |
| Behavioral counseling | 99401 ~15min |
| 99402 ~30min | |
| Dietary counseling 15min | 97802 |
| Follow-up | Coding |
|---|---|
| Manage disease process | 99212-9214 |
| Behavioral counseling | 99401 or 99402 |
| Group therapy ~30min | 99411 |
| Dietary counseling 15min | 97803 |
| Dietary group 30min | 97804 |
References:
- FMX 2016
Epidemiology and physiology
General Statistics:
- 34.9% of US Adults are obese (2011-2012)
- Midwest > South > North East > West
- 1 out of 5 US adolescents are obese
- 1 out of 6 US Elementary age children are obese
- 1 out of 12 pre school age children are obese
- If friend becomes obese - your chance increases 57-171%
- If spouse becomes obese - risk increases 37%
- US Children prevalence on obesity was 17% in 2011-2014 and 5.8% extreme obesity
- US prevalence in 2013-2014 of obesity was 35% for men and 40.4% for women. For class 3 obesity - 5.5% (M)and 9.9% (W)
- By income:
- 29.7% among highest-income women vs 45.2% among lowest-income women
- Consistent across racial groups except:
- Non-Hispanic black women (no difference in prevalence)
- Non-Hispanic black men (prevalence higher in the highest income group than lowest)
References:
- Christakis NEJM 2007
- JAMA 2016;315(21)
- JAMA 2018;319(6)
Adipose cells
Secrete adipokines and free fatty acids (FFA)
- Produces increased low level systemic inflammation
- Induces insulin resistance in muscle
- Increases plasma triglycerides -> atherosclerosis
Effects of Clinically Meaningful Weight Loss
Effects of 5-10% decrease in weight:
- Reduction in T2DM
- Improvement in BP
- 10mmHg decrease in SBP
- Reduction in CVD
- Improved lipid profile
- 1.7 mg/dL increase in HDL
- 3.9 mg/dL decrease in LDL
- 6.6 mg/dL decrease in Trig
- Improvement of OSA up to 50% with 10% weight loss
Weight loss:
- WEIGHT LOSS OF 4 KG by diet reduces systolic and diastolic blood pressure (BP) by 4.5 and 3.2 mm Hg, respectively
- SOR: A, systematic review with consistent findings
- Weight loss of 1 to 1.2 kg by exercise may produce small reductions in systolic or diastolic BP
- SOR: B, mixed quality of studies
- Available evidence is inadequate to examine the combined effects of diet and exercise.
Walking:
- On average, participants walked for 38.3 minutes, 4.4 days per week, for 34.9 weeks at a relative intensity of 70.1% of predicted maximum heart rate (in 6 studies) or 56.3% oxygen consumption intensity (VO2) (in 14 studies).
- Walking significantly reduced body weight (WMD, –0.95 kg; P<.001) and BMI (WMD, –0.28 kg/m2; P = .015), leading to a significant reduction in diastolic BP (WMD, –1.54 mm Hg; P = .026) but not systolic BP (WMD, –1.06 mm Hg; P = .316).
- Pedometer use for 3 to 104 weeks increased physical activity (for RCTs, a 2491-steps-per-day increase; 95% CI, 1098-3885 steps per day; for observational studies, a 2183-steps-per-day increase; 95% CI, 1571-2796 steps per day) and decreased BMI by 0.38 kg/m2 (95% CI, 0.05-0.72 kg/m2).
- For an 80-kg, 170-cm tall person with a BMI of 27.7 kg/m2, reducing BMI by 0.4 units translates to a 1.2-kg weight loss. This weight loss reduced systolic BP by 3.8 mm Hg (95% CI, 1.7-5.9 mm Hg), but not diastolic BP (–0.3 mm Hg; 95% CI, 0.02 to –0.46). Using a 10,000-steps-per-day goal (P = .001) and a step diary (P<.001) further increased walking.
References:
- J Fam Pract. 2013 May;62(5):258-259.
- OMA Review Course 2016
Etiology
Physiological:
- Genetic
- Pregnancy
- Menopause
- Weight gaining medications
- Smoking cessation
- Endocrine
- PCOS
- hypothyroidism
- Cushings
Behavioral:
- Dietary
- Unhealthy eating patterns
- Grazing
- Nibbling
- Mindless eating
- Large volume consumption
- BED
- Bulemia
Physical Activity:
- Decrease leisure time
- Increase sedentary time
- Insufficient mod-vig intensity exercise
- Development of physical limitations to exercise
Food states
Fasting 8-12h/d (post-absorptive state)
- Main energy source: Lipid oxidation
- Muscle:
- ~40% of body weight in males (30% in females)
- Overabundance of intra-myocellular lipid associated with impaired glucose uptake and oxidation
- Adipose:
- ~20% in males (30% in females)
- Small role in glucose disposal
- Liver:
- Increase in glucose production
Fed (post-prandial state)
- Starts with calorie injestion
Exercise
- Higher intensity exercise
- Carbohydrate (CHO) predominant fuel source for 1-2 hours then lipid oxidation once glycogen is depleted
- Brief intense in less fit -> CHO dependent
- Rapid switch to lipid metabolism in trained athletes
- Low fat diets -> reduced fat oxidation
- Low CHO diets -> increased fat oxidation
Genetics
- FTO Gene - Fat mass and obesity associated gene - Chromosome 16 q12.2
- NOT simple Mendelian - 97 BMI associated genetic loci
- The only chromosome without obesity loci = Y Chromosome
Most commons:
- Most common Syndromal cause of Obesity = Prader Willi Syndrome (1/25,000) - hypotonia, short stature, hyperphagia
- Most common Obesity Syndrome = MC4R Syndrome (1/2000)
Genetics of Obesity Workup:
- Suspect genetic - Is there Developmental delay or Dysmorphic features
- Yes -> Karyotype/FISH
- Pos -> Prader Willi or Fragile X
- Neg -> Polydactyly or renal abnormalities or retinal dystrophy
- Yes -> Bardet-Biedl Syndrome (BBS)
- No -> Albright hereditary osteodystrophy or Wilson Turner Syndrome or BDNF/TrKB Def
- No -> Photophobia and nystagmus
- Yes -> Alstroms syndrome
- No -> Dysmorphic skeletal abnormalities
- Yes -> Ulnar mammary syndrome or Simpso Golabo-Behmel type 2
- No -> Undetectable serum leptin levels
- Yes -> Cong leptin def
- No -> high serum insulin levels
- Yes -> MC4R Deficiency
Genetic Obesity Syndromes:
- Prader Willi Syndrome
- Gene: Paternal deletion of q11-13 region
- Increased ghrelin
- Hypotonia at birth, difficult feeding followed with hyperphagia, hypogonadism, MR
- Almond shaped eyes, thin upper lips, thin faces
- Treat with
- Calorie control and behavioral management
- Growth hormone therapy and replacement of sex hormones at puberty
- Bardet-Biedl Syndrome
- Gene: BBS1-16
- Polydactyly, retinal dystrophy, hypogonadism, renal abnormalities, developmental delay
- Fragile X
- Macro-orchidism, MR, prominent jaw, large ears
- MC4R Deficiency
- Gene: MC4R
- Accelerated growth, increased final height, severe hyperinsulinemia (Single gene defect)
- POMC Deficiency
- Gene: POMC
- Hypopigmentation, isolated ACTH deciency with adrenal crisis, hyperphagia and early-onset obesity
- Alstrom Syndrome
- Gene: ALMS1
- Photophobia, nystagmus, visual impairment, deafness, severe insulin resistance
- Very rare
- Cohen Syndrome
- Gene: Chrom 8q22 mutation
- Microagnatha, shortened area between the nose and upper lip, high raised palate, MR, central obesity
- LEP Deficiency
- Gene: LEP
- Hypogonadism, freq infections, undetectable serum leptin
- LEPR Deficiency
- Gene: LEPR
- Hypogonadism
- PCSK1/3 Deficiency
- Gene: PCSK1
- Postprandial hypoglycemia, hypogonadism, elevated plasma proinsulin and 32-33 split proinsulin
- BDNF Deficiency
- Gene: BDNF
- Developmental delay, hyperactivity, impaired memory, impaired pain sensation
- TrkB Deficiency
- Gene: NTRK2
- Developmental delay, hyperactivity, impaired memory, impaired pain sensation
- SIM1 Deficiency
- Gene: SIM1
- Spectrum of developmental delay
- AHO
- Gene: GNAS1
- Short stature, skeletal defects, hormone resistance
Ref:
- J Clin Invest Jun 2011 121(6)2080-2086
Hormones
Socioeconomics
- Higher the income -> lower the rates of obesity EXCEPT non-hispanic african american ad Mexican-American men
- Most women with obesity are not low income but lower income has higher prevalence of obesity
- Higher educated women have lower rates of obesity
- Between 1988 and 2008 obesity increased in all income and education levels
Mortality Stats
- Overweight associated with significantly lower all-cause mortality
- Class I obesity – no higher mortality risk than normal body weight
- Class II and III – significantly higher all-cause mortality
| BMI | Chance of reaching 70yo |
|---|---|
| 22.5-25 | 80% |
| 35-40 | 60% |
| >40 | 50% |
References:
- Flegal et al. 2013, JAMA, Systematic Review/Meta-Analysis
- Lancet 2009
Medicine Quotes
- "Those who think they have not time for bodily exercise will sooner or later have to find time for illness." - Edward Stanley - Earl of Derby 1873
- "A healthy diet, regular exercise, and smoking avoidance can eliminate 80% of heart disease and 70% of some cancers." - Drink and Be Healthy 2005
Pediatric Obesity
Stats:
- 1/3 children with obesity have fatty liver disease
- Children with severe obesity have 40% higher risk of GERD
- Children with obesity are 8x more likely to have gallstones
Risk Factors:
- Biggest risk factor is parental obesity
- 1 parent = 3x risk
- 2 parents = 10x risk
- Intrauterine risk factors
- Excessive maternal weight gain
- High pre-pregnancy weight
- Gestational DM
- Small for gestational age
- Maternal smoking
- Cesarean sections
- Formula > Breast
- 15-30% decrease in rates if any breastfeeding occured
- Each month of breastfeeding gives a 4% reduction in risk
- Breast fed infants are more likely to self regulate intake volume
- Use WHO charts for breastfed infants - they gain faster in first 3mo then slower
- Early (<6mo) introduction of complementary foods
- Sleep duration <9hrs
- Early menarche is associated with higher risk
- Risk of obesity persisting into adulthod is higher in adolescents than younger children
Diagnosis in Children: (Barow SE. Pediatrics. 2007.)
- BMI <5% - Underweight
- Recommended labs: None
- BMI 5-84% - Healthy weight
- Recommended labs: None
- BMI 85-94% - Overweight
- Recommended labs: Fasting lipids if NO rsk factors
- Recommended labs: Fasting lipids and glucose, ALT/AST with risk factors
- BMI 95-99% - Obese
- Recommended labs: Fasting lipids and glucose, ALT/AST
- BMI 120% of 95% - Severely obese
Assessment for children with obesity
- History
- Birth weight, breast fed, early intro of food
- Past weight gain/loss
- Earlier onset of rebound adiposity
- Developmental delay
- Nutrition, physical activity
- Parental history
- Obesity, DM II, HTN, HLD, CAD, OSA
- PMH
- Weght positive medications
- Co-morbidities
- Labs
- See above
- Consider: CBC, CMP, CPK, A1c, 25 Vit D, Uric Acid, TSH, UA
Modifiable risk factors
Pre-natal modifiable risk factors:
- High maternal pre-pregnancy BMI
- Fetal nutrition
- Maternal smoking
- Gestational Diabetes
Post-natal modifiable risk factors:
- Infant growth
- Infant nutrition
- Sleep duration
Both pre and post natal modifiable risk factors:
- Smoking exposure
- Greater maternal weight increase during pregnancy
- Breast feeding duratino (longer is better)
- Infant sleep
Recommendations to parents to avoid Childhood Obesity
- Limit consumption of sugar-sweetened beverages
- Encourage fruits/vegetables
- Limit screen time to 1-2 hrs daily
- Remove screens from bedroom
- Eat breakfast daily
- Limit eating out
- Eat meals together
- Limit portions to appropriate serving sizes
References:
- AFP Vol 78 No 1 Jul 2008
Pregnancy and Weight
Pregnancy
- Weight loss before pregnancy is the most effective way to reduce maternal and fetal risks.
Weight Gain in Pregnancy
| Category | Weight |
|---|---|
| Normal | 25-35 lbs |
| Overweight | 15-25 lbs |
| Obese | 11-20 lbs |
Adjusted Predicted Absolute Risk (%) of adverse Fetal and Maternal Outcomes according to Maternal BMI
| BMI | Macrosomia | Shoulder | Stillbirth | In-hospital | Preeclampsia | Gest DM | Preterm | C-section |
|---|---|---|---|---|---|---|---|---|
| Dystocia | Newborn mortality | birth | ||||||
| 25 | 1.9 | 3.8 | 0.3 | 0.4 | 8.0 | 6.9 | 1.8 | 35.8 |
| 30 | 2.7 | 4.0 | 0.4 | 0.5 | 13.1 | 11.0 | 2.3 | 42.6 |
| 35 | 3.5 | 4.1 | 0.4 | 0.6 | 17.2 | 13.9 | 2.8 | 48.2 |
| 40 | 4.3 | 4.2 | 0.5 | 0.6 | 21.4 | 16.9 | 3.4 | 53.5 |
Interventions to reduce obesity and related complications in pregnancy (Relative Risk):
- Dietary interventions decrease risk of:
- Preeclampsia - RR 0.67
- Gestational diabetes mellitus - 0.39
- Gestational hypertension - 0.30
- Preterm delivery - 0.68
- Exercise decreases risk of cesarean - 0.66
- Exercise during pregnancy decreases risk of gest diabetes - 0.69
- Exercise in the year before pregnancy decreases risk of gest diabetes - 0.34
- Exercise increases likelihood of noninstrumented delivery - 1.12
- Low glycemic load diet, exercise, or both lead to lower rates of gestational weight gain - 0.80
References:
- AFP Vol 97 No 9 May 2018
Resources
Nutritional guidance:
- Good and cheap cookbook $4/day: http://www.leannebrown.com/good-and-cheap.pdf
- Good and Cheap Cookbook: https://goodandcheap.website/
Websites:
- Americans in Motion from AFP
- How many calories burned per activity:
CME Sites:
- http://www.obesityed.com
- http://search.medscape.com/search/?q=obesity%20cme&plr=edu&age=-1YEAR&credits=.75&page=1
Other web resources
- AHA Guidelines: http://circ.ahajournals.org/content/129/25_suppl_2/S102
- Coding Obesity visits: https://www.medicaid.gov/medicaid-chip-program-information/by-topics/quality-of-care/reducing-obesity.html
- Educational tools: http://www.vindicocme.com/educationaltools
- Weight-loss and Nutrition Myths: https://www.niddk.nih.gov/health-information/health-topics/weight-control/myths/Pages/weight-loss-and-nutrition-myths.aspx
Patient Messaging
List:
- Aesthetics
- Allergy/Immunology
- Cardiology
- Endocrinology
- ENT
- Gastroenterology
- General
- Geriatrics
- Infectious Diseases
- Upper Respiratory Infections
- Musculoskeletal
- Neurology
- Nutrition
- OB/GYN
- Ophthalmology
- Pediatrics
- Psychology
- Pulmonary
- Rheumatology
- Weight Management
Beginner Run/Walk Program edit
Week Schedule (3-4 nonconsecutive days of run/walking):
- Day 1: 30 min run/walk
- Day 2: 30 min run/walk
- Day 3: 30 min run/walk
- +/- Day 4: 3-6 miles
| Sun | Mon | Tue | Wed | Thurs | Fri | Sat |
|---|---|---|---|---|---|---|
| Rest | 30 min | Rest | 30 min | Rest | 30 min | 3 mi |
Example Schedule:
- Sun: Rest
- Mon: 30 min
- Tue: Rest
- Wed: 30 min
- Thurs: Rest
- Fri: 30 min
- Sat: 3 miles
Run/Walk Minutes:
- Start with 3 min run/1 min walk (3:1)
- Alternatively, start with 1:1
- Run effort: 6-7 out of 10 (can carry a conversation, but not full sentences)
- Walk effort: 2-3 out of 10 (fast walk)
Example Exercise Routines edit
Hello,
You asked for an idea for a simple exercise routine. I am offering 3 here:
- Kettlebell program - I think this is safe, fun, simple, with minimal equipment
- Dumbell routine - This is also simple, can be done with just a couple dumbells, and is full body
- Walking routine - An idea for using walking as an exercise if you want
—
Kettlebell Routine:
Here's a simple kettlebell routine that you can try at home. You'll need one or two kettlebells for this routine.
- Kettlebell Swing: Stand with feet hip-width apart, hold a kettlebell in front of you with both hands at arm's length. Bend at your hips and knees, and then swing the kettlebell back between your legs. Quickly reverse the direction and drive your hips forward, swinging the kettlebell up to shoulder height. Swing the kettlebell back between your legs and repeat. Do 10-15 reps.
- Goblet Squat: Hold a kettlebell by the horns (the handle and head of the kettlebell) in front of your chest with your feet hip-width apart. Push your hips back, bend your knees, and lower your body as far as you can into a squat. Pause, then slowly push yourself back to the starting position. Do 10-15 reps.
- Kettlebell Clean: Stand with feet hip-width apart, hold a kettlebell in front of you with one hand at arm's length. Bend at your hips and knees, and then swing the kettlebell back between your legs. Quickly reverse the direction and drive your hips forward, pulling the kettlebell up to shoulder height. Rotate your wrist so that your palm faces forward. Bend your knees and then push your hips back to lower the kettlebell back between your legs. Do 10-15 reps on each side.
- Kettlebell Overhead Press: Hold a kettlebell in front of your shoulder with your elbow bent and your fist pointing toward the ceiling. Press the kettlebell straight above your shoulder, then lower it back to the starting position. Do 10-15 reps on each side.
Remember to start slow and gradually increase the weight and intensity as you get stronger. Always prioritize form over speed or weight to avoid injury.
Recommended kettlebell weights to start with:
- Women: 6-8 Kg or 13-18 lbs
- Men: 12-16 Kg or 26-35 lbs
—
Dumbell Routine:
Here's a simple routine you can try:
- Dumbbell Squats: 3 sets of 10-12 reps
- Dumbbell Bench Press: 3 sets of 10-12 reps
- Dumbbell Shoulder Press: 3 sets of 10-12 reps
- Dumbbell Bicep Curls: 3 sets of 10-12 reps
- Dumbbell Tricep Extensions: 3 sets of 10-12 reps
Remember to start with a weight that is comfortable for you and gradually increase the weight as you get stronger. It's also important to warm up before starting your workout and cool down afterwards.
—
Walking For Exercise
Here is a simple walking routine you can try:
- Start by walking at a comfortable pace for 5-10 minutes to warm up.
- Increase your pace to a brisk walk for 20-30 minutes. This should be a pace where you can still hold a conversation, but it's challenging.
- After your brisk walk, slow down to a comfortable pace for 5-10 minutes to cool down.
- Aim to do this routine 3-5 times per week.
To make your walking routine more challenging, you can try adding hills or stairs, or increasing your pace. You can also add intervals, where you alternate between a brisk walk and a faster pace for short periods of time.
Remember to wear comfortable shoes and dress appropriately for the weather.
Org
CBD Autism
The evidence supporting the use of cannabidiol (CBD) in children with autism spectrum disorder (ASD) is limited and primarily consists of open-label studies, small observational cohorts, and a few randomized controlled trials (RCTs), with mixed results.
Several open-label and observational studies report improvements in behavioral symptoms, social responsiveness, and communication, with some families noting enhanced quality of life and reductions in comorbid symptoms such as irritability, aggression, and sleep disturbances.
Adverse effects are generally mild to moderate, including somnolence, decreased appetite, and irritability, but can occasionally lead to treatment discontinuation.
However, contradictory evidence comes from the only published double-blind, placebo-controlled RCTs, which have not demonstrated a clear benefit of CBD over placebo for core ASD symptoms. For example, a recent crossover RCT in autistic boys with severe behavioral problems found no significant difference between CBD and placebo on primary outcome measures, with a strong placebo effect observed. Improvements seen in open-label settings may be confounded by expectancy and reporting bias, and the heterogeneity in study design, dosing, and outcome measures further limits interpretability.
No major professional society in the United States has endorsed CBD as a standard treatment for ASD, and high-quality, large-scale RCTs are still needed to establish efficacy and safety.
At present, CBD should not be considered a first-line or routine therapy for ASD in children, and its use should be limited to research settings or highly selected, refractory cases with careful monitoring.
Reference:
- Trauner D, Umlauf A, Grelotti DJ, et al. Cannabidiol (CBD) Treatment for Severe Problem Behaviors in Autistic Boys: A Randomized Clinical Trial. Journal of Autism and Developmental Disorders. 2025;:10.1007/s10803-025-06884-y. https://doi.org/10.1007/s10803-025-06884-y.
- Parrella NF, Hill AT, Enticott PG, et al. A Systematic Review of Cannabidiol Trials in Neurodevelopmental Disorders. Pharmacology, Biochemistry, and Behavior. 2023;230:173607. https://doi.org/10.1016/j.pbb.2023.173607.
Anxiety Stuff and Messaging edit
Anxiety Messaging
What you need to know about anxiety:
- Anxiety is normal. Everyone experiences anxiety at some point in time. For example, it is normal to feel anxious when on a rollercoaster or before a job interview.
- Anxiety is adaptive. It helps us to prepare for real danger (such as a bear jumping out of the woods) or performing at our best (for example, it motivates us to get ready for an important meeting or presentation). When we experience anxiety, it triggers our "fight-flight-freeze" response and gets our body ready to defend itself (for instance, our heart beats faster to pump blood to our muscles so we have the energy to run away or fight off danger). Without it, we would not survive.
- Anxiety can become a problem when our body reacts when there is no real danger. It can be helpful to think of anxiety as a smoke alarm. A smoke alarm can help protect us when there is an actual fire, but sometimes the alarm goes off when there isn't a real fire (e.g. burning toast in the toaster). Like a smoke alarm, anxiety is helpful when it alerts us to real danger. But when it goes off when there is no real danger, then we may want to fix it. We don't want to take the batteries out of the alarm in case there is a real fire, but we do want to fix the alarm so that it doesn't go off every time we make toast.
Learn to relax
- Calm breathing
- Muscle relaxation.
Calm Breathing:
- This is a strategy that you can use to calm down quickly. We tend to breathe faster when we are anxious, which can make us feel dizzy and lightheaded, and even more anxious. Calm breathing involves taking slow and gentle breaths. Breathe in through the nose, pause, and then breathe out through the mouth, pausing for several seconds before taking another breath.
- Try 4-10 breaths of: Breathing in over 3-4 seconds, holding for 3-4 seconds, breathing out for 3-4 seconds, and holding 3-4 seconds
Progressive Muscle Relaxation:
- Another helpful strategy is learning to relax your body by tensing various muscles and then relaxing them. This strategy can help lower overall tension and stress levels. It also helps you to be more aware of when you are feeling stressed.
- Progressive Muscle Relaxation teaches you how to relax your muscles through a two step process. First, you systematically tense particular muscle groups in your body, such as your neck and shoulders. Next, you release the tension and notice how your muscles feel when you relax them. This exercise will help you to lower your overall tension and stress levels, and help you relax when you are feeling anxious. It can also help reduce physical problems such as stomach aches and headaches, as well as improve your sleep.
- YouTube Videos:
General Anxiety Strategies:
- Learn to breathe Breathing exercises are one of the best and quickest ways to help regulate your body and emotion when you feel anxious. There are many breathing techniques but one of the best is called abdominal or diaphragmatic breathing. The technique is simple and you can do this just about anywhere. In just a few minutes you can get instant relief from anxiety. Take a deep breath in through your nose and pull the air into your lungs from the lower part of your abdomen (the diaphragm). You can tell whether you are pulling the air in properly because your abdomen (not your chest) will rise. When you've taken in as much air as you can, hold it for a count of 7 and then slowly exhale through the mouth. Repeat this process two or three times for maximum relaxation.
- Focus on what you can control A lot of the anxiety revolves around people and circumstances that you can't control. For example, your health insurance company is raising your premium well beyond what you can afford to pay. You can get yourself worked up about corporate greed and the injustice of raising premiums on average citizens or you can spend that energy working toward a solution to find a more affordable policy. In other words, focus your energy on what you can control. Granted, this is not always easy to do, but once you begin to focus on the variables that you can change through your actions, you no longer feel so helpless or overwhelmed.
- Identify and challenge distorted thoughts If you are prone to feel a lot of anxiety, chances are that you have faulty thoughts or beliefs that are fueling your anxiety. For example, you may see danger in a lot of everyday situations that other people see as benign. Or, you might immediately assume that when a given situation doesn't turn out as expected that it will become a worst-case scenario. These ways of thinking are distortions and act as lenses through which you typically see the world. The way out of these distortions is to train your mind to be objective and consider the other possibilities that might be present. For example, instead of defaulting to negative about all the things that went wrong in that job interview, focus on what went well and what you might do differently the next time you are in a similar situation.
- Practice mindfulness Mindfulness is simply the act of living in the present moment. Many people who are full of anxiety tend to focus a lot of their mental energy on the future. They spend an inordinate amount of their time and energy trying to make the future as predictable as possible. This type of living is driven by fear of the unknown. But, mindfulness refocuses that energy and tries to live fully in the present. It takes practice to live in the present moment when you are used to leaning out into the future, but the present is a far more peaceful place to live.
- Caring for self It might not seem obvious, but self-care plays a large role in your ability to manage anxiety. When you are getting an adequate amount of sleep, eating healthy meals, being active on a daily basis and avoiding dependence on substances like alcohol and nicotine, you are building up your body and mind's resilience to stress so that you can handle most of the challenges that come your way.
Resources:
CBT edit
The Cognitive Model:
- Situation: Something happens
- Thought: The situation is interpreted
- Emotion: A feeling occurs as a result of the thought
- Behavior: An action in response to the Emotion
Situation: You are required to give a presentation in front of a large group.
| Thought | Emotion | Behavior | |
|---|---|---|---|
| Person 1 | I'll practice and do great! | confident, anticipatory | Practices and completes the presentation without problem |
| Person 2 | I bet I make a fool of myself in front of everyone. | anxious, worried, scared | Puts off practicing, attempts to get out of doing the presentation. |
Education about the Yerkes-Dodson law can help a client to understand why they have anxiety, how it is hurting them, and how a certain amount of anxiety can be beneficial. The Yerkes-Dodson law states that too little or too much anxiety are both harmful, and that a person reaches optimal performance on a task with a moderate level of anxiety.
Situation: You are required to give a presentation in front of a large group.
| No Anxiety | Moderate Anxiety | High Anxiety |
|---|---|---|
| A presentation you say? Eh, whatever. I'll wing it. | I know I can do this, but I need to be prepared. I'll plan and practice before I have to speak. | This is too much. I'm going to look like a fool. How can I get out of this? I feel sick just thinking about it. |
Challenging Negative Thoughts Ask the client to practice identifying their thoughts by practicing in session, and then completing a thought log for homework. A thought log requires a client to describe situations that they experience, record the thought they had during that situation, and then the resulting consequence (both a behavior and emotion). Without practice identifying how thoughts and emotions are linked, the most important thoughts will pass by unnoticed and unchallenged. In this case, the client should focus on thoughts that contribute to anxiety.
After having a thought that contributes to anxiety, the client will want to ask themselves: "Do I have evidence to support this thought, or am I making assumptions? Do I have good reason to be anxious?".
Situation: You are required to give a presentation in front of a large group.
| Thought | Challenge | Consequence |
|---|---|---|
| I'm going to mess up and make a fool of myself. | This is scary for me, but I've never seriously messed up a presentation before. Even if I do, what's the worst that could happen? Everyone will forget in a day or two. | You're nervous, but not to such a debilitating level. You follow through with the presentation. Now the next time will be easier! |
One technique to help ease this process is for clients to ask themselves a series of questions to assess their thoughts. Here are some examples:
- "Is there evidence for my thought, or am I making assumptions?"
- "What's the worst that could happen? Is that outcome likely?"
- "What's the best that could happen?"
- "What's most likely to happen?"
- "Will this matter a week from now, a year from now, or five years from now?"
After successfully challenging an old belief, your client will need to replace it with a new belief. I want to emphasize that the new belief does not need to be full of sunshine, rainbows, and happiness. Sometimes, the best replacement thought is just less negative. Some situations really are scary, and denying that won't do any good. The idea is to think neutrally rather than negatively, and to put fears into perspective. Someone suffering from extreme anxiety usually perceives a situation as more dangerous than it really is.
Exposure Therapy / Systematic Desensitization
The first step of systematic desensitization is to create a fear hierarchy. Identify the anxiety you would like to address with your client, and then create a list of steps leading up to it with rankings of how anxiety-producing you think the situation would be. Here's an example:
Fear Hierarchy for a Spider Phobia
| Situation | Fear Ranking (1-10) |
|---|---|
| Listen to a story about finding a spider | 2 |
| Rest a picture of a spider on my arm | 4 |
| Sit in a room with a nearby spider in a cage | 6 |
| Let the spider out of the cage, but keep it at a distance | 8 |
| Let a spider walk across my arm | 11 |
Now, before following through and exposing a client to these stimuli, they must learn relaxation techniques to learn during the process. These can include deep breathing, progressive muscle relaxation, or meditation. They're described in detail in the next session of this guide.
Finally, the client will follow through with the fear hierarchy (with the clinician's assistance). The goal is for the client to be exposed to stimuli that are only moderately anxiety-producing while using relaxation skills to manage their response. Eventually, the client can move on to the more challenging situations that they identified in the fear hierarchy.
Instructions: Deep Breathing
- Sit comfortably in your chair. Place your hand on your stomach so you are able to feel your diaphragm move as you breathe.
- Take a deep breath through your nose. Breathe in slowly. Time the breath to last 5 seconds.
- Hold the breath for 5 seconds. You can do less time if it's difficult or uncomfortable.
- Release the air slowly (again, time 5 seconds). Do this by puckering your lips and pretending that you are blowing through a straw (it can be helpful to actually use a straw for practice).
- Repeat this process for about 5 minutes, preferably 3 times a day. The more you practice, the more effective deep breathing will be when you need it.
| Event | Thought | Consequence (emotion and behavior) | Alternate response |
|---|---|---|---|
Videos:
Progressive Muscle Relaxation
Progressive Muscle Relaxation:
- Another helpful strategy is learning to relax your body by tensing various muscles and then relaxing them. This strategy can help lower overall tension and stress levels. It also helps you to be more aware of when you are feeling stressed.
- Progressive Muscle Relaxation teaches you how to relax your muscles through a two step process. First, you systematically tense particular muscle groups in your body, such as your neck and shoulders. Next, you release the tension and notice how your muscles feel when you relax them. This exercise will help you to lower your overall tension and stress levels, and help you relax when you are feeling anxious. It can also help reduce physical problems such as stomach aches and headaches, as well as improve your sleep.
- Adult PMR
- Children PMR
| Muscle group | Action |
|---|---|
| Hands | Clench/make a fist. |
| Wrists and forearms | Extend and bend your hands back at the wrist. |
| Biceps and upper arms | Make a fist and bend your arms at the elbows, flexing your biceps. |
| Shoulders | Shrug them (raise them toward your ears). |
| Forehead | Wrinkle into a deep frown. |
| Around the eyes and bridge of the nose | Close your eyes as tightly as possible while remaining comfortable (preferably remove contact lenses before you start.) |
| Cheeks and jaws | Smile as widely as you can. |
| Around the mouth | Press your lips together tightly. |
| Check your face for tension. | |
| Back of the neck | Press the back of your head against your support (chair headrest or the floor.) |
| Front of the neck | Touch your chin to your chest, but avoid creating tension in your neck and head. |
| Chest | Take a deep breath and hold it for 5 to 10 seconds. |
| Back | Arch your back up and away from the floor or chair. |
| Stomach | Suck into a tight knot. (Check your chest and stomach for tension.) |
| Hips and buttocks | Press your buttocks together tightly. |
| Thighs | Clench them hard. |
| Lower legs | Point your toes toward your face. Then point your toes away and curl them downward at the same time. |
Face your fears (Graded Exposure)
Graded exposure: https://youtu.be/HHfUdOM8QIQ
If you have been avoiding certain situations, places, or objects out of fear, it will be important for you to start exposing yourself to those things so that you can get over your fears in the long run. However, it is usually easier to start with something that is not too scary and then work up to the things that cause a great deal of anxiety.
- Start by making a list of feared situations, places, or objects, such as saying "hi" to a coworker, entering a crowded grocery store, riding the bus, or anything else that you are avoiding.
- Once you have made a list, try and arrange them from the least scary to the most scary.
- Starting with the situations that cause the least anxiety, repeatedly enter that situation and remain there until you notice your anxiety start to come down.
- Once you can enter that situation or face that fear (on numerous occasions) without experiencing much anxiety, you can move on to the next thing on the list.
When completing exposures, sometimes it can feel a lot scarier than you anticipated! If this is the case, adjust the difficulty of these by changing mediating variables. These are things that you can change during exposures to make them easier or harder, such as:
- How long you interact with the trigger
- How far away you stand from the trigger
- How much reassurance you allow yourself to have after the exposure (eg. asking your friend once vs 3 times or using half a pump of soap when washing your hand vs two pumps of soap)
- How long you wait until you complete your compulsion in more extreme situations where not using one may be really challenging (eg. waiting 10 minutes before you use a compulsion if the idea of not using it is too overwhelming)
Challenge your thoughts
Learn to challenge your thoughts:
When we are anxious, we tend to see the world as very threatening and dangerous. However, this way of thinking can be overly negative and unrealistic. If we remember to evaluate our thoughts more realistically and reframe them, we can reduce our anxiety in the process. We can create more realistic and balanced thoughts by doing the following:
- Learn to identify when your thoughts have any "thinking traps" in them (eg. "Mind Reading" when you are convinced what someone thinks about you or "Fortune Telling" when we assume with certainty that we know what will happen during a feared outcome).
- Test your anxious thoughts by completing belief experiments. Our brain likes to assume we know with confidence what will happen in situations that we have fear over, but often those anxious beliefs are not as accurate as we think they are. Eg. "If I pet a dog it will bite me" or "If I raise my hand to answer a question in class I'll get it wrong."
This takes time to shift anxious thinking, so be patient and consistently practice these skills.
Calming imagery
Calming imagery:
- Visualization is the idea of building an image in your mind of a calm, safe place (e.g., beach, forest, familiar place). This soothes the anxiety response and distracts from anxious thinking (Hart, 2008; Welford, 2010).
Time Management Strategies
| Strategies | Structure | Protection | Adaptation |
| Time wasters | x | x | |
| Perfectionism | x | x | x |
| Procrastination | x | x | |
| Say no | x | x | |
| Determine priorities | x | x | x |
| Deep work | x | x | |
| 80/20 | x | x | x |
- Identify and Eliminate Time Wasters
- Type of time waster: Distractions or electronic interruptions
- Checking the news, emails, social media, and messaging channels
- Block out specific time for administrative tasks, including checking emails.
- Checking the news, emails, social media, and messaging channels
- Type of time waster: Disorganized/messy
- Using a scattered, disorganized filing system and not planning tasks and time appropriately
- Adopt an organized online and offline filing structure.
- Spend 30 minutes at the end of the day planning the next day's tasks.
- Using a scattered, disorganized filing system and not planning tasks and time appropriately
- Type of time waster: Physical interruptions
- Colleagues or family members walking in when you are concentrating on a task
- Close the door when you're working and communicate that this time is meant to be uninterrupted.
- Schedule focused time.
- Colleagues or family members walking in when you are concentrating on a task
- Type of time waster: Meetings
- Unclear/undefined agenda and starting meetings late
- All meetings need a clear agenda communicated beforehand.
- Start meetings on time.
- Make meetings shorter.
- Unclear/undefined agenda and starting meetings late
- Type of time waster: Dead time
- Commuting or waiting
- Plan smaller, less-intense tasks for dead-time periods
- Commuting or waiting
- Type of time waster: Repeating the same task
- Writing multiple reports with the same structure and budgeting from scratch each month
- Where possible, automate. Use templates.
- Do not complete the same task more than once.
- Writing multiple reports with the same structure and budgeting from scratch each month
- Type of time waster: Procrastinating
- Spending time completing other tasks rather than focusing on the task at hand
- Just start working on the task, even if only for five minutes.
- Avoid ruminating in anxiety or perfectionism.
- Spending time completing other tasks rather than focusing on the task at hand
- Type of time waster: Distractions or electronic interruptions
- Steer Away From Perfectionism
- Perfectionists rely on binary thinking models (right–wrong) and have a low tolerance for mistakes (Shafran et al., 2016). Help your client recognize that a project will never be perfect, adopt a kinder inner voice, and schedule time for feedback.
- Break tasks into smaller, attainable goals with clear expectations when setting goals. For example, the first goal is to produce a draft version containing mistakes but with the correct structure. For the second goal, the client can focus on refining the piece and attending to typos.
- "Perfect" work is unattainable, and "perfect" is typically poorly defined. Instead, identify the core aspects of the project that will have the most impact and achieve the same outcome as a perfect one. Focus on these aspects rather than the less important ones.
- Eliminate Procrastination
- Say No to Extra Work
- Practice declining the opportunity in a neutral way where the implications of the extra work on available time are made explicit
- Determine Priorities
- Eisenhower Matrix
- To classify tasks, start with the due date and work backward from high urgency to low urgency. Urgency refers to the immediacy of the task deadline. Under a heading of urgency, tasks that are due soon are urgent, and tasks with later deadlines are not urgent.
- Then, add an additional classification to each task: importance. Evaluate the importance of each task by looking at its impact and contribution to long-term goals. Tasks that contribute to essential goals have high importance, whereas those that don't contribute are not important.
- Then act:
- Do – Priority 1
- In the top-left quadrant are tasks high on both dimensions. These are the most pressing tasks that require your immediate attention. They should be completed first.
- Schedule – Priority 2
- Tasks that are important but not urgent (top-right quadrant) do not have concrete deadlines yet. These tasks should be broken down into smaller tasks or scheduled for later.
- Delegate – Priority 3
- Tasks that are urgent but not important (bottom-left quadrant) do not require your personal attention. Instead, these tasks can be delegated to someone else.
- Delete – Priority 4
- Tasks in the opposite bottom-right quadrant are the least important and not urgent. They can be discarded or kept for when there is a lull in workload.
- Do – Priority 1
- Eisenhower Matrix
- Focus on Deep Work
- Allocate a significant portion of time to uninterrupted focus (i.e., no time wasters and no interruptions).
- Allocate this time for the morning when you're feeling refreshed and motivated. Do not check emails or other communications beforehand to avoid being distracted.
- Like exercise, plan for sufficient rest and sleep. It is only possible to work constantly at the same pace with rest. So assign the more manageable, less cognitively demanding tasks to other work periods and take time to recover.
- Follow the 80/20 Way
- 80/20
- 20% of the time will yield 80% of the work. Imagine your client has a presentation due. Putting together a rough but comprehensive draft (80%) will take little time (20%).
- However, the remaining 20% of the work will take approximately 80% of the time. Even though the bulk of the work is done, the remaining work needed to refine the presentation (20%) takes considerable time (80%). If your client had planned their project so that they only had 20% of the time left for this work, they would not meet their deadline.
- 20% of the work is essential, whereas 80% is not. Knowing how to prioritize the critical 20% over the less consequential 80% is vital to managing our time and workload.
- When planning a schedule, do the following (Vaccaro, 2000):
- Split the available time unequally to account for the 80/20 split. Leave ample time for refinement, corrections, and feedback.
- Go through tasks and classify them as belonging to the 20% or 80% category. The 20% tasks are essential, yield significant results, and directly impact other goals. The 80% tasks are urgent but optional, take longer than expected, and are draining.
- Classify subtasks as 20% or 80% when working on a bigger project. Always prioritize the essential tasks (20%) over the nonessential tasks (80%).
- 80/20
Reference:
Do Stretches
Simple stretches
- What they are:
- Releasing tension with movements you can do almost anywhere
- How to do them:
- Gently press the tip of your tongue to the roof of mouth, and your jaw will often fall open and relax on its own. Tilt your head forward and roll it around slowly on your neck clockwise, then counterclockwise. Raise your eyebrows up and down a few times to loosen your facial muscles. Shrug your shoulders as if saying, "I don't know," then leave them up high for a few seconds before letting them fall.
- Why they work:
- "People carry so much tension in their jaw, neck and shoulders and don't even realize it," notes Wygant. "But as psychologist Dr. Therese Rando once said, 'If you can relax your body, you can relax your mind.'"
Mindful Breathing
Khazan (2019, p. 41) suggests that mindful breathing is a practical and straightforward way to make "helpful breathing changes" by allowing you to "breathe just the way you do without a struggle."
Try the following, letting go of expectations (Khazan, 2019):
- Find a comfortable place to sit upright, away from noise.
- Begin by closing your eyes and noticing physical sensations (your body's contact with the seat and your feet on the floor).
- Gently focus on the sensation of inhalation (the air coming in your nose, and your chest and stomach rising).
- Without judgment or expectation, transition gently between inhalation and exhalation.
- Focus on the sensation of exhalation (the air coming out of your nose, and chest and your stomach falling).
- Notice and acknowledge thoughts, emotions, and sensations accompanying each breath without engaging, letting them pass with kindness and compassion.
- If your mind wanders, gently return your focus to each breath – just as it is.
- Repeat for as long as you wish.
Reference:
- https://positivepsychology.com/breathing-exercises-for-stress-relief/
- Khazan, I. Z. (2019). Biofeedback and mindfulness in everyday life: Practical solutions for improving your health and performance. W. W. Norton & Company.
- Nestor, J. (2020). Breath: The new science of a lost art. Penguin Books.
Name that emotion
Use your words
- What it is:
- Describing strong feelings verbally
- How to do it:
- Ask yourself questions that force the analytical parts of your brain to engage. "What emotion am I feeling right now? Is it anger? Fear? Rage? Why am I feeling this way? Is it because of something that's already happened or something that I'm only afraid might happen?"
- Why it works:
- "Post-traumatic stress disorder studies show that some people take longer than usual to perceive a threat has diminished," notes Wygant. "But when they're asked to label or describe their emotions, it engages the prefrontal cortex in their brain and helps calm them down. Then, they can recognize, 'Oh, that's just a stick, not a snake.'"
Relaxation Strategies
Breathing
- Box breathing is also known as square breathing. It has been shown to reduce stress and boost focus and concentration (Sharma et al., 2014). This exercise involves breathing in through the nose for a count of four, holding the breath for a count of four, breathing out slowly for a count of four, and then holding for another count of four, essentially making a "square" or "box" with the breath.
- 4-7-8 breathing is especially helpful for falling asleep (Arizona Center for Integrative Medicine, 2010). Focusing on the breath and counting can distract the mind from worry and ruminating thoughts. This technique involves breathing in through the nose for a count of four, holding the breath for a count of seven, and exhaling through the lips for a count of eight.
- Pursed-lip breathing is a great technique to relieve stress and anxiety, but it is also helpful for people with asthma or COPD (Srivastava & Singhal, 2005). It helps get the diaphragm working and increases the amount of oxygen entering the body. To do this exercise, simply breathe in slowly through the nose and breathe out through the mouth with pursed lips (as if sucking through a straw). Make the breath out approximately twice as long as the breath in.
Exercises (for panic)
- Progressive muscle relaxation (PMR) PMR is a technique that involves actively contracting muscles to create tension and then progressively releasing them throughout the body. The technique was developed by Edmund Jacobson in the 1920s using the principles of neural top-down and bottom-up processing, and it provides relatively quick relief from tension and anxiety (Keptner, Fitzgibbon, & O'Sullivan, 2020).
- Try the 5–4–3–2–1 exercise This exercise involves looking at five objects, listening for four sounds, touching three objects, identifying two smells, and naming one thing you can taste. It brings you into the present moment and can help distract the mind from panic.
- Inhale lavender Research has demonstrated that inhaling the smell of lavender essential oils significantly reduced anxiety in a short period of time (Donelli, Antonelli, Bellinazi, Gensini, & Firenzuoli, 2019). Lavender was the preferred anxiety-reducing scent in this research, but other essential oils can provide similar calming effects based on preference. Simply open the bottle of oil and slowly inhale the scent through the nose and breath out through the mouth.
Reference:
- https://positivepsychology.com/breathing-exercises/
- Arizona Center for Integrative Medicine. (2010, February). 4-7-8 Breath relaxation exercise. Retrieved from https://www.cordem.org/globalassets/files/academic-assembly/2017-aa/handouts/day-three/biofeedback-exercises-for-stress-2%E2%80%94fernances-j.pdf
- Sharma, V., Rajajeyakumar, M., Velkumary, S., Subramanian, S., Bhavanani, A., Madanmohan, A., & Thangavel, D. (2014). Effect of fast and slow pranayama practice on cognitive functions in healthy volunteers. Journal of Clinical Diagnostic Resources, 8, 10–30.
- Khazan, I. Z. (2019). Biofeedback and mindfulness in everyday life: Practical solutions for improving your health and performance. W. W. Norton & Company.
- Nestor, J. (2020). Breath: The new science of a lost art. Penguin Books.
- Srivastava, S., & Singhal, A. (2005). Influence of alternate nostril breathing on cardiorespiratory & autonomic function in healthy young adults. Indian Journal of Physiological Pharmacology, 49(6), 475–483.
- Keptner, K., Fitzgibbon, C., & O'Sullivan, J. (2020). Effectiveness of anxiety reduction interventions on test anxiety: A comparison of four techniques incorporating sensory modulation. British Journal of Occupational Therapy, 70(6), 1–9.
- Donelli, D., Antonelli, M., Bellinazi, C., Gensini, F. & Firenzuoli, F. (2019). Effects of lavender on anxiety: A systematic review and meta analysis. Phytomedicine, 65, 95–112.
Challenge your Negative Thoughts edit
WHAT IS THE EVIDENCE?
- Am I confusing a thought with a fact?
- The fact that you believe something to be true does not necessarily mean that it is. Would your thought be accepted as correct by other people? Would it stand up in court, or be dismissed as circumstantial? What objective evidence do you have to back it up and to contradict it?
- Automatic thought
- When I met Peter in the street today, he didn't smile at me. I must have done something to offend him.
- Possible answer
- It's true that he didn't smile at me but I have no reason to believe he's offended with me. It probably had nothing at all to do with me – maybe he just had something on his mind.
- Am I jumping to conclusions?
- This is the result of basing what you think on poor evidence. For instance, depressed people often believe that others are thinking critically about them. But none of us are mind-readers. How do you know what someone else is thinking? You may be right, but don't jump to conclusions – stick to what you know, and if you don't know, see if you can find out.
- Automatic thought
- My husband didn't eat that chocolate cake I baked for him. He thinks I'm a terrible cook.
- Possible answer
- All I know for sure is that he didn't eat it. I don't actually know whether he thinks I'm a terrible cook or not. Maybe he just wasn't hungry – I can ask him.
WHAT ALTERNATIVES ARE THERE?
- Am I assuming my view of things is the only one possible?
- Automatic thought
- That was a terrible mistake; I'll never learn to do this properly.
- Possible answer
- If I wasn't depressed, I'd probably shrug my shoulders and do what I could to set the situation right and learn from my errors. Tom made just the same mistake last week, and he made a joke of it.
- Automatic thought
WHAT IS THE EFFECT OF THINKING THE WAY I DO?
- What do you want? What are your goals? Do you want to be happy and get the most out of life? Is the way you are thinking now helping you to achieve this? Or is it standing in the way of what you want?
- Automatic thought
- I've wasted my life – so many lost opportunities.
- Possible answer
- Brooding about the past only makes me depressed. The question is what am I going to make of my future?
- Automatic thought
- What are the advantages and disadvantages of thinking this way?
- Many distorted thought patterns do have some pay off – that is what keeps them going. But do the disadvantages outweigh the advantages? If so, you can think of a new way of looking at things which will give you the advantages, but avoid the disadvantages of the old way.
- Automatic thought
- I must make a good impression at this party.
- Advantage: I'll go out of my way to talk to people. If they like me, I'll feel marvellous.
- Disadvantage: If somebody doesn't like me, I'll feel terrible and think badly of myself.
- Possible answer
- Telling myself I must make a good impression just puts pressure on me, and will make it difficult to relax and enjoy myself. It is impossible for everyone to like me all of the time. It's very nice when they do, but if they don't, it's not the end of the world.
- Am I asking questions that have no answers?
- Questions like "How can I undo the past?" "Why aren't I different?", "What is the meaning of life?", "Why does this always happen to me?", "Why is life so unfair?" Brooding over questions like these is a guaranteed way to depress yourself. If you can turn them into answerable questions, so much the better. If not, don't waste time on them.
- Automatic thought
- When will I do better again?
- Possible answer
- There's no answer to that. Going over and over it just makes me worried and upset. I'd do better to work out what I can do to help myself get over this depression as quickly as possible.
WHAT THINKING ERRORS AM I MAKING?
- Am I thinking in all-or-nothing terms?
- Nearly everything is relative. People, for instance, are not usually all good or all bad. They are a mixture of the two. Are you applying this kind of black-and-white thinking to yourself?
- Automatic thought
- I did that really badly. I might as well not bother.
- Possible answer
- The fact is you didn't do it as well as you wanted to. That doesn't mean it was no good at all. You can't expect to do everything 100% right. If you do, you'll never be satisfied.
- Am I using ultimatum words in my thinking?
- Watch out for words like always/never, everyone/none, everything/nothing. The chances are that the situation is actually less clear-cut than that. Mostly it's a case of sometimes, some people and some things.
- Automatic thought
- Everything always goes badly for me.
- Possible answer
- That's an exaggeration. Some things go badly for me, just like they do for anyone else, but some things go well.
- Am I condemning myself as a total person on the basis of a single event?
- Depressed people often take difficulties to mean that they have no value at all as a person. Are you making this kind of blanket judgement?
- Automatic thought
- I was so irritable with the children this morning. I'm a terrible mother and a wicked person.
- Possible answer
- The fact that on a particular day, at a particular time, in particular circumstances, I was irritable does not mean I'm a terrible mother or a wicked person. I can't reasonably expect never to be irritated and making myself depressed by writing myself off completely is not going to help me to be nicer to the children when they get in from school.
- Am I concentrating on my weakness and forgetting my strengths?
- When people become depressed, they often overlook problems they handled successfully in the past, and resources which would help them to overcome current difficulties. Once they change their thinking they are often amazed at their ability to deal with problems. How have you coped with similar difficulties in the past?
- Automatic thought
- I can't stand being alone now that Jane has gone.
- Possible answer
- I was alone before I met her. I made an effort to get out and meet people, and spent time doing things I enjoyed. In fact, I was quite happy – and probably can be again. I'll phone Bob for a start.
- Am I blaming myself for something which is not really my fault?
- Depressed people, for instance, blame themselves for being depressed. They put it down to lack of willpower, or weakness, and criticise themselves for not "pulling themselves together". In fact, scientists have been studying depression for many years, and they are still not certain what causes it. Depression is a difficult problem to solve, and blaming yourself for it will only make you more depressed.
- Automatic thought
- I must be really stupid to have these distorted thoughts.
- Possible answer
- Stupidity is one possible reason. When I look at myself as a whole, there's not much evidence that I'm stupid. I have these thoughts because I'm depressed. When I'm feeling better, I think quite differently.
- Am I taking something personally which has little or nothing to do with me?
- When things go wrong, depressed people often believe that in some way this is directed at them personally, or caused by them. In fact, it may have nothing to do with them.
- Automatic thought
- Mary doesn't like me at all. She would never have shouted at me like that if she did.
- Possible answer
- I'm not the only person Mary shouts at. She's always on the edge when things aren't going well for her, and she shouts at whoever is around. I've seen her. She'll get over it and probably apologize.
- Am I expecting myself to be perfect?
- It is simply not possible to get everything right all the time. Depressed people often set up unrealistically high standards for themselves. They then condemn themselves for making mistakes, or acting in ways they would rather not have done. Accepting that you can't be perfect does not mean you have to give up trying to do things well. It means that you can learn from your difficulties and mistakes, instead of being upset and paralyzed by them.
- Automatic thought
- This is not good enough. I should have completed everything I planned to do.
- Possible answer
- I can't always expect to carry out everything I plan. I'm not God; I'm fallible, like any other human being. It would have been nice if I had finished, but the fact that I haven't is not a disaster. Focus on what you have done, not on what you have failed to do. That way you will be encouraged to try again.
- Am I using a double standard?
- You may be expecting more of yourself than you would of another person. How would you react to someone else in your situation? Would you be so hard on them? You can afford to be as kind to yourself as you would to someone else. It won't lead to collapse.
- Automatic thought
- I'm pathetic. I shouldn't be so upset by things.
- Possible answer
- If someone else was upset by this situation, I'd be sympathetic towards them, and try to help them try to find a solution to the problem. I certainly wouldn't call them pathetic – I'd be able to see that it wouldn't help. I can do the same for myself. It will give me the courage to carry on.
- Am I paying attention only to the black side of things?
- Are you, for instance, focusing on everything that has gone wrong during the day, and forgetting or discounting things you have enjoyed or achieved?
- Automatic thought
- That was really a terrible day.
- Possible answer
- Hang on a moment. You were late for a meeting, and you had a disagreement with your son, but on the whole your work went well, and you enjoyed the cinema this evening. All in all, it wasn't a bad day. Only remembering the bad things is part of depression – watch out for it.
- Am I overestimating the chances of disaster?
- Depressed people often believe that if things go at all wrong, disaster is sure to follow. If the day starts badly, it can only get worse. How likely is it that what you expect will really happen? Is there really nothing you can do to change the course of events?
- Automatic thought
- I didn't get all my work done today again. I'll get the sack.
- Possible answer
- When was the last time they sacked someone from this firm for not having time to finish the job? It's perfectly normal not to finish, when we all have to work under so much pressure. If my boss comments, I can explain the situation to him.
- Am I exaggerating the importance of events?
- What difference does a particular event really make to your life? What will you make of it in a week, a year, 10 years? Will anyone else remember what you now see as a terrible thing today? If you do, will you feel the same way about it? Probably not.
- Automatic thought
- I made a real fool of myself at that party. I'll never be able to face them again.
- Possible answer
- Don't make a mountain out of a molehill. Most people didn't even notice. I don't suppose anyone who did thought anything of it. We'll probably laugh at it in the future – it certainly makes a good story.
- Am I fretting about the way things ought to be, instead of accepting and dealing with them as they are?
- Are you allowing events in the world at large to feed your depression? Telling yourself life is unjust, and people are brutes? It is sad that there is so much suffering in the world, and you may decide to do what you can to change things, but getting depressed about it does nothing to help.
- Automatic thought
- That presentation about old people in the projects was awful. Life is terribly cruel. Things should be different.
- Possible answer
- Things are as they are, and to want them different is counter to reality – like wishing the zebra had no stripes. Getting depressed about it is not going to help the situation. Why not see if I can visit someone at the long-term care facility?
- Am I assuming I can do nothing to change my situation?
- Pessimism about the chances of changing things is central to depression. It makes you give up before you even start. You can't know that there is no solution to your problems until you try. Is the way you are thinking helping you to find answers, or is it making you turn down possible solutions without even giving them a go?
- Automatic thought
- It's no good. I'll never sort this out.
- Possible answer
- If you tell yourself that, you certainly won't. Sit down and work out what you could do. Even if some of your solutions haven't worked before, that does not mean they won't now. What was it that stopped them from working?
- Pessimism about the chances of changing things is central to depression. It makes you give up before you even start. You can't know that there is no solution to your problems until you try. Is the way you are thinking helping you to find answers, or is it making you turn down possible solutions without even giving them a go?
- Am I predicting the future instead of experimenting with it?
- The fact that you have acted in a certain way in the past does not mean to say that you have to do so in the future. If you predict the future, instead of trying something different, you are cutting yourself off from the chance of change. Change may be difficult, but it is not impossible.
- Automatic thought
- I'll never manage to stand up for myself. I never have.
- Possible answer
- The fact that I never have does not mean I never can. Doing so will make me feel uncomfortable, but if I stick with it, it will become more natural. Also other people will respect me more.
- Socratic Method to Question Thoughts
Fill these out with "why" and "why not":
- Thought to be questioned:
- What is the evidence for and against this thought?
- Am I basing this thought on facts or on feelings?
- Is this thought black and white or more complicated (nuanced)?
- Could I be misinterpreting the evidence? Am I making assumptions?
- Might other people have different interpretations of the same situation? What are they?
- Am I looking at all the evidence or just what supports my thought?
- Could my thought be an exaggeration of what is true?
- Am I having this thought out of habit, or do the facts support it?
- Did someone pass this thought/belief to me? If so, are they a reliable source?
- Is my thought a likely scenario, or is it the worst case scenario?
Reference:
Decatastrophizing edit
Decatastrophizing Ask very simple questions: "What if?" or "What's the worst that could happen?"
For Example:
- Client: I always worry that my date won't like how I look, or I'll make a fool of myself. This leads to me getting so nervous that I do make a fool of myself.
- Therapist: So, what if those things come true? What if your date doesn't like how you look, or you make a fool of yourself?
- Client: Well, we probably won't have a second date…
- Therapist: What if you don't have a second date? What happens then?
- Client: I guess nothing. I just won't see them again.
This sequence of questioning helps to reduce the irrational level of anxiety associated with cognitive distortions. It highlights the fact that even the worst-case scenario is manageable.
Note: Decatastrophizing is sometimes called the "what if" technique because of the style of questioning.
Cognitive Distortions
There are 15 main cognitive distortions that can plague even the most balanced thinkers.
- Filtering Filtering refers to the way a person can ignore all of the positive and good things in life to focus solely on the negative. It's the trap of dwelling on a single negative aspect of a situation, even when surrounded by an abundance of good things.
- Polarized thinking / Black-and-white thinking This cognitive distortion is all-or-nothing thinking, with no room for complexity or nuance—everything's either black or white, never shades of gray. If you don't perform perfectly in some area, then you may see yourself as a total failure instead of simply recognizing that you may be unskilled in one area.
- Overgeneralization Overgeneralization is taking a single incident or point in time and using it as the sole piece of evidence for a broad conclusion. For example, someone who overgeneralizes could bomb an important job interview and instead of brushing it off as one bad experience and trying again, they conclude that they are terrible at interviewing and will never get a job offer.
- Jumping to conclusions Similar to overgeneralization, this distortion involves faulty reasoning in how one makes conclusions. Unlike overgeneralizing one incident, jumping to conclusions refers to the tendency to be sure of something without any evidence at all. For example, we might be convinced that someone dislikes us without having any real evidence, or we might believe that our fears will come true before we have a chance to really find out.
- Catastrophizing / Magnifying or Minimizing This distortion involves expecting that the worst will happen or has happened, based on an incident that is nowhere near as catastrophic as it is made out to be. For example, you may make a small mistake at work and be convinced that it will ruin the project you are working on, that your boss will be furious, and that you'll lose your job. Alternatively, one might minimize the importance of positive things, such as an accomplishment at work or a desirable personal characteristic.
- Personalization This is a distortion where an individual believes that everything they do has an impact on external events or other people, no matter how irrational that may be. A person with this distortion will feel that he or she has an exaggerated role in the bad things that happen around them. For instance, a person may believe that arriving a few minutes late to a meeting led to it being derailed and that everything would have been fine if they were on time.
- Control fallacies This distortion involves feeling like everything that happens to you is either a result of purely external forces or entirely due to your own actions. Sometimes what happens to us is due to forces we can't control, and sometimes what it's due to our own actions, but the distortion is assuming that it is always one or the other. We might assume that difficult coworkers are to blame for our own less-than-stellar work, or alternatively assume that every mistake another person makes is because of something we did.
- Fallacy of fairness We are often concerned about fairness, but this concern can be taken to extremes. As we all know, life is not always fair. The person who goes through life looking for fairness in all their experiences will end up resentful and unhappy. Sometimes things will go our way, and sometimes they will not, regardless of how fair it may seem.
- Blaming When things don't go our way, there are many ways we can explain or assign responsibility for the outcome. One method of assigning responsibility is blaming others for what goes wrong. Sometimes we may blame others for making us feel or act a certain way, but this is a cognitive distortion. Only you are responsible for the way you feel or act.
- "Shoulds" "Shoulds" refer to the implicit or explicit rules we have about how we and others should behave. When others break our rules, we are upset. When we break our own rules, we feel guilty. For example, we may have an unofficial rule that customer service representatives should always be accommodating to the customer. When we interact with a customer service representative that is not immediately accommodating, we might get angry. If we have an implicit rule that we are irresponsible if we spend money on unnecessary things, we may feel exceedingly guilty when we spend even a small amount of money on something we don't need.
- Emotional reasoning This distortion involves thinking that if we feel a certain way, it must be true. For example, if we feel unattractive or uninteresting in the current moment, we think we are unattractive or uninteresting. This cognitive distortion boils down to: "I feel it, therefore it must be true." Clearly, our emotions are not always indicative of the objective truth, but it can be difficult to look past how we feel.
- Fallacy of change The fallacy of change lies in expecting other people to change as it suits us. This ties into the feeling that our happiness depends on other people, and their unwillingness or inability to change, even if we demand it, keeps us from being happy. This is a damaging way to think because no one is responsible for our own happiness except ourselves.
- Global labeling / mislabeling This cognitive distortion is an extreme form of generalizing, in which we generalize one or two instances or qualities into a global judgment. For example, if we fail at a specific task, we may conclude that we are a total failure in not only that area but all areas. Alternatively, when a stranger says something a bit rude, we may conclude that he or she is an unfriendly person in general. Mislabeling is specific to using exaggerated and emotionally loaded language, such as saying a woman has abandoned her children when she leaves her children with a babysitter to enjoy a night out.
- Always being right While we all enjoy being right, this distortion makes us think we must be right, that being wrong is unacceptable. We may believe that being right is more important than the feelings of others, being able to admit when we've made a mistake or being fair and objective.
- Heaven's Reward Fallacy This distortion involves expecting that any sacrifice or self-denial will pay off. We may consider this karma, and expect that karma will always immediately reward us for our good deeds. This results in feelings of bitterness when we do not receive our reward (Grohol, 2016).
Reference:
9 Essential CBT Techniques and Tools
- Journaling This technique is a way to gather about one's moods and thoughts. A CBT journal can include the time of the mood or thought, the source of it, the extent or intensity, and how we reacted, among other factors. This technique can help us to identify our thought patterns and emotional tendencies, describe them, and change, adapt, or cope with them (Utley & Garza, 2011). Follow the link to find out more about using a thought diary for journaling.
- Unraveling cognitive distortions This is a primary goal of CBT and can be practiced with or without the help of a therapist. In order to unravel cognitive distortions, you must first become aware of the distortions from which you commonly suffer (Hamamci, 2002). Part of this involves identifying and challenging harmful automatic thoughts, which frequently fall into one of the 15 categories listed earlier.
- Cognitive restructuring Once you identify the distortions you hold, you can begin to explore how those distortions took root and why you came to believe them. When you discover a belief that is destructive or harmful, you can begin to challenge it (Larsson, Hooper, Osborne, Bennett, & McHugh, 2015). For example, if you believe that you must have a high-paying job to be a respectable person, but you're then laid off from your high-paying job, you will begin to feel bad about yourself. Instead of accepting this faulty belief that leads you to think negative thoughts about yourself, with cognitive restructuring you could take an opportunity to think about what really makes a person "respectable," a belief you may not have explicitly considered before.
- Exposure and response prevention This technique is specifically effective for those who suffer from obsessive-compulsive disorder (OCD; Abramowitz, 1996). You can practice this technique by exposing yourself to whatever it is that normally elicits a compulsive behavior, but doing your best to refrain from the behavior. You can combine journaling with this technique, or use journaling to understand how this technique makes you feel.
- Interoceptive exposure Interoceptive Exposure is intended to treat panic and anxiety. It involves exposure to feared bodily sensations in order to elicit the response (Arntz, 2002). Doing so activates any unhelpful beliefs associated with the sensations, maintains the sensations without distraction or avoidance, and allows new learning about the sensations to take place. It is intended to help the sufferer see that symptoms of panic are not dangerous, although they may be uncomfortable.
- Nightmare exposure and rescripting Nightmare exposure and rescripting are intended specifically for those suffering from nightmares. This technique is similar to interoceptive exposure, in that the nightmare is elicited, which brings up the relevant emotion (Pruiksma, Cranston, Rhudy, Micol, & Davis, 2018). Once the emotion has arisen, the client and therapist work together to identify the desired emotion and develop a new image to accompany the desired emotion.
- Play the script until the end This technique is especially useful for those suffering from fear and anxiety. In this technique, the individual who is vulnerable to crippling fear or anxiety conducts a sort of thought experiment in which they imagine the outcome of the worst-case scenario. Letting this scenario play out can help the individual to recognize that even if everything he or she fears comes to pass, the outcome will still be manageable (Chankapa, 2018).
- Progressive muscle relaxation This is a familiar technique to those who practice mindfulness. Similar to the body scan, progressive muscle relaxation instructs you to relax one muscle group at a time until your whole body is in a state of relaxation (McCallie, Blum, & Hood, 2006). You can use audio guidance, a YouTube video, or simply your own mind to practice this technique, and it can be especially helpful for calming nerves and soothing a busy and unfocused mind.
- Relaxed breathing This is another technique that will be familiar to practitioners of mindfulness. There are many ways to relax and bring regularity to your breath, including guided and unguided imagery, audio recordings, YouTube videos, and scripts. Bringing regularity and calm to your breath will allow you to approach your problems from a place of balance, facilitating more effective and rational decisions (Megan, 2016).
Reference:
Diabetes Care Standards (2024) edit
All need editing
Reference:
Reference:
1. Improving Care and Promoting Health in Populations: Standards of Care in Diabetes—2024
Diabetes and Population Health
- 1.1 Ensure treatment decisions are timely, rely on evidence-based guidelines, capture key elements within the social determinants of health, and are made collaboratively with people with diabetes and care partners based on individual preferences, prognoses, comorbidities, and informed financial considerations. B
- 1.2 Align approaches to diabetes management with the Chronic Care Model. This model emphasizes person-centered team care, integrated long-term treatment approaches to diabetes and comorbidities, and ongoing collaborative communication and goal setting between all team members. A
- 1.3 Care systems should facilitate in-person and virtual team-based care, include those knowledgeable and experienced in diabetes management as part of the team, and utilize patient registries, decision support tools, and community involvement to meet needs of individuals with diabetes. B
- 1.4 Assess diabetes health care maintenance (Table 4.1) using reliable and relevant data metrics to improve processes of care and health outcomes, with attention to care costs, individual preferences and goals for care, and treatment burden. B
Tailoring Treatment for Social Context
- 1.5 Assess food insecurity, housing insecurity/homelessness, financial barriers, and social capital/social community support to inform treatment decisions, with referral to appropriate local community resources. A
- 1.6 Provide people with diabetes with additional self-management support from lay health coaches, navigators, or community health workers when available. A
- 1.7 Consider the involvement of community health workers to support the management of diabetes and cardiovascular risk factors, especially in underserved communities and health care systems. B
Reference:
- American Diabetes Association Professional Practice Committee; 1. Improving Care and Promoting Health in Populations: Standards of Care in Diabetes—2024. Diabetes Care 1 January 2024; 47 (Supplement1): S11–S19. https://doi.org/10.2337/dc24-S001
- https://diabetesjournals.org/care/article/47/Supplement_1/S11/153937/1-Improving-Care-and-Promoting-Health-in
2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2024
Diagnostic Tests for Diabetes Recommendations
- 2.1a Diagnose diabetes based on A1C or plasma glucose criteria, either the fasting plasma glucose (FPG) value, 2-h plasma glucose (2-h PG) value during a 75-g oral glucose tolerance test (OGTT), or random glucose value accompanied by classic hyperglycemic symptoms/crises criteria (Table 2.1 ). A
- 2.1b In the absence of unequivocal hyperglycemia (e.g., hyperglycemic crises), diagnosis requires confirmatory testing (Table 2.1 ). A
- Criteria for the diagnosis of diabetes in nonpregnant individuals
- A1C ≥6.5% (≥48 mmol/mol). The test should be performed in a laboratory using a method that is NGSP certified and standardized to the DCCT assay.
- OR FPG ≥126 mg/dL (≥7.0 mmol/L). Fasting is defined as no caloric intake for at least 8 h.*
- OR 2-h PG ≥200 mg/dL (≥11.1 mmol/L) during OGTT. The test should be performed as described by the WHO, using a glucose load containing the equivalent of 75 g anhydrous glucose dissolved in water.*
- OR In an individual with classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose ≥200 mg/dL (≥11.1 mmol/L). Random is any time of the day without regard to time since previous meal.
- Criteria defining prediabetes in nonpregnant individuals
- A1C 5.7–6.4% (39–47 mmol/mol)
- OR FPG 100 mg/dL (5.6 mmol/L) to 125 mg/dL (6.9 mmol/L) (IFG)
- OR 2-h PG during 75-g OGTT 140 mg/dL (7.8 mmol/L) to 199 mg/dL (11.0 mmol/L) (IGT)
Use of A1C for Screening and Diagnosis of Diabetes
- 2.2a The A1C test should be performed using a method that is certified by the National Glycohemoglobin Standardization Program (NGSP) as traceable to the Diabetes Control and Complications Trial (DCCT) reference assay. B
- 2.2b Point-of-care A1C testing for diabetes screening and diagnosis should be restricted to U.S. Food and Drug Administration–approved devices at Clinical Laboratory Improvement Amendments (CLIA)–certified laboratories that perform testing of moderate complexity or higher by trained personnel. B
- 2.3 Marked discordance between A1C and repeat blood glucose values should raise the possibility of a problem or interference with either test. B
- 2.4 In conditions associated with an altered relationship between A1C and glycemia, such as some hemoglobin variants, pregnancy (second and third trimesters and the postpartum period), glucose-6-phosphate dehydrogenase deficiency, HIV, hemodialysis, recent blood loss or transfusion, or erythropoietin therapy, plasma glucose criteria should be used to diagnose diabetes. B
Classification
- 2.5 Classify people with hyperglycemia into appropriate diagnostic categories to aid in personalized management. E
- Diabetes is classified conventionally into several clinical categories, although these are being reconsidered based on genetic, metabolomic, and other characteristics and pathophysiology (2):
- Type 1 diabetes (due to autoimmune β-cell destruction, usually leading to absolute insulin deficiency, including latent autoimmune diabetes in adults)
- Type 2 diabetes (due to a non-autoimmune progressive loss of adequate β-cell insulin secretion, frequently on the background of insulin resistance and metabolic syndrome)
- Specific types of diabetes due to other causes, e.g., monogenic diabetes syndromes (such as neonatal diabetes and maturity-onset diabetes of the young), diseases of the exocrine pancreas (such as cystic fibrosis and pancreatitis), and drug- or chemical-induced diabetes (such as with glucocorticoid use, in the treatment of people with HIV, or after organ transplantation)
- Gestational diabetes mellitus (diabetes diagnosed in the second or third trimester of pregnancy that was not clearly overt diabetes prior to gestation or other types of diabetes occurring throughout pregnancy, such as type 1 diabetes).
- Diabetes is classified conventionally into several clinical categories, although these are being reconsidered based on genetic, metabolomic, and other characteristics and pathophysiology (2):
One useful clinical tool for distinguishing diabetes type is the AABBCC approach: Age (e.g., for individuals <35 years old, consider type 1 diabetes); Autoimmunity (e.g., personal or family history of autoimmune disease or polyglandular autoimmune syndromes); Body habitus (e.g., BMI <25 kg/m2); Background (e.g., family history of type 1 diabetes); Control (e.g., level of glucose control on noninsulin therapies); and Comorbidities (e.g., treatment with immune checkpoint inhibitors for cancer can cause acute autoimmune type 1 diabetes)
Type 1 Diabetes
- 2.6 Screening for presymptomatic type 1 diabetes may be done by detection of autoantibodies to insulin, glutamic acid decarboxylase (GAD), islet antigen 2 (IA-2), or zinc transporter 8 (ZnT8). B
- 2.7 Having multiple confirmed islet autoantibodies is a risk factor for clinical diabetes. Testing for dysglycemia may be used to further forecast near-term risk. When multiple islet autoantibodies are identified, referral to a specialized center for further evaluation and/or consideration of a clinical trial or approved therapy to potentially delay development of clinical diabetes should be considered. B
- 2.8 Standardized islet autoantibody tests are recommended for classification of diabetes in adults who have phenotypic risk factors that overlap with those for type 1 diabetes (e.g., younger age at diagnosis, unintentional weight loss, ketoacidosis, or short time to insulin treatment). E
Prediabetes and Type 2 Diabetes
- 2.9 Screening for prediabetes and type 2 diabetes with an assessment of risk factors or validated risk calculator should be done in asymptomatic adults. B
- 2.10a Testing for prediabetes or type 2 diabetes in asymptomatic people should be considered in adults of any age with overweight or obesity who have one or more risk factors (Table 2.4 ). B
- 2.10b For all other people, screening should begin at age 35 years. B
- 2.11 If tests are normal, repeat screening recommended at a minimum of 3-year intervals is reasonable, sooner with symptoms or change in risk (e.g., weight gain). C
- 2.12 To screen for prediabetes and type 2 diabetes, FPG, 2-h PG during 75-g OGTT, and A1C are each appropriate (Table 2.1 and Table 2.2 ). B
- 2.13 When using OGTT as a screen for prediabetes or diabetes, adequate carbohydrate intake (at least 150 g/day) should be assured for 3 days prior to testing. A
- 2.14 Risk-based screening for prediabetes or type 2 diabetes should be considered after the onset of puberty or after 10 years of age, whichever occurs earlier, in children and adolescents with overweight (BMI ≥85th percentile) or obesity (BMI ≥95th percentile) and who have one or more risk factors for diabetes. (See Table 2.5 for evidence grading of risk factors.) B
- 2.15a Consider screening people for prediabetes or diabetes if on certain medications, such as glucocorticoids, statins, thiazide diuretics, some HIV medications, and second-generation antipsychotic medications, as these agents are known to increase the risk of these conditions. E
- 2.15b In people who are prescribed second-generation antipsychotic medications, screen for prediabetes and diabetes at baseline and repeat 12–16 weeks after medication initiation or sooner, if clinically indicated, and annually. B
- 2.16 People with HIV should be screened for diabetes and prediabetes with an FPG test before starting antiretroviral therapy, at the time of switching antiretroviral therapy, and 3–6 months after starting or switching antiretroviral therapy. If initial screening results are normal, FPG should be checked annually. E
Criteria for screening for diabetes or prediabetes in asymptomatic adults
- Testing should be considered in adults with overweight or obesity (BMI ≥25 kg/m2 or ≥23 kg/m2 in Asian American individuals) who have one or more of the following risk factors:
- First-degree relative with diabetes
- High-risk race and ethnicity (e.g., African American, Latino, Native American, Asian American, Pacific Islander)
- History of cardiovascular disease
- Hypertension (≥130/80 mmHg or on therapy for hypertension)
- HDL cholesterol level <35 mg/dL (<0.9 mmol/L) and/or a triglyceride level >250 mg/dL (>2.8 mmol/L)
- Individuals with polycystic ovary syndrome
- Physical inactivity
- Other clinical conditions associated with insulin resistance (e.g., severe obesity, acanthosis nigricans)
- People with prediabetes (A1C ≥5.7% [≥39 mmol/mol], IGT, or IFG) should be tested yearly.
- People who were diagnosed with GDM should have lifelong testing at least every 3 years.
- For all other people, testing should begin at age 35 years.
- If results are normal, testing should be repeated at a minimum of 3-year intervals, with consideration of more frequent testing depending on initial results and risk status.
- People with HIV, exposure to high-risk medicines, history of pancreatitis
Risk-based screening for type 2 diabetes or prediabetes in asymptomatic children and adolescents in a clinical setting Screening should be considered in youth* who have overweight (≥85th percentile) or obesity (≥95th percentile) A and who have one or more additional risk factors based on the strength of their association with diabetes:
- Maternal history of diabetes or GDM during the child's gestation A
- Family history of type 2 diabetes in first- or second-degree relative A
- Race and ethnicity (e.g., Native American, African American, Latino, Asian American, Pacific Islander) A
- Signs of insulin resistance or conditions associated with insulin resistance (acanthosis nigricans, hypertension, dyslipidemia, polycystic ovary syndrome, or small-for-gestational-age birth weight) B
Pancreatic Diabetes or Diabetes in the Context of Disease of the Exocrine Pancreas Recommendation
- 2.17 Screen people for diabetes within 3–6 months following an episode of acute pancreatitis and annually thereafter. Screening for diabetes is recommended annually for people with chronic pancreatitis. E
Cystic Fibrosis–Related Diabetes
- 2.18 Annual screening for cystic fibrosis–related diabetes (CFRD) with an OGTT should begin by age 10 years in all people with cystic fibrosis not previously diagnosed with CFRD. B
- 2.19 A1C is not recommended as a screening test for CFRD due to low sensitivity. However, a value of ≥6.5% (≥48 mmol/mol) is consistent with a diagnosis of CFRD. B
- 2.20 Beginning 5 years after the diagnosis of CFRD, annual monitoring for complications of diabetes is recommended. E
Posttransplantation Diabetes Mellitus
- 2.21 After organ transplantation, screening for hyperglycemia should be done. A formal diagnosis of posttransplantation diabetes mellitus (PTDM) is best made once the individual is stable on an immunosuppressive plan and in the absence of an acute infection. B
- 2.22 The OGTT is the preferred test to make a diagnosis of PTDM. B
- 2.23 Immunosuppressive plans shown to provide the best outcomes for individuals and graft survival should be used, irrespective of PTDM risk. E
Monogenic Diabetes Syndromes
- 2.24a Regardless of current age, all people diagnosed with diabetes in the first 6 months of life should have immediate genetic testing for neonatal diabetes. A
- 2.24b Children and young adults who do not have typical characteristics of type 1 or type 2 diabetes and who often have a family history of diabetes in successive generations (suggestive of an autosomal dominant pattern of inheritance) should have genetic testing for maturity-onset diabetes of the young (MODY). A
- 2.24c In both instances, consultation with a center specializing in diabetes genetics is recommended to understand the significance of genetic mutations and how best to approach further evaluation, treatment, and genetic counseling. E
Gestational Diabetes Mellitus
- 2.25 In individuals who are planning pregnancy, screen those with risk factors (Table 2.4 ) B and consider testing all individuals of childbearing potential for undiagnosed prediabetes or diabetes. E
- 2.26a Before 15 weeks of gestation, test individuals with risk factors (Table 2.4 ) B and consider testing all individuals E for undiagnosed diabetes at the first prenatal visit using standard diagnostic criteria if not screened preconception.
- 2.26b Before 15 weeks of gestation, screen for abnormal glucose metabolism to identify individuals who are at higher risk of adverse pregnancy and neonatal outcomes, are more likely to need insulin, and are at high risk of a later gestational diabetes mellitus (GDM) diagnosis. B Early treatment for individuals with abnormal glucose metabolism may provide some benefit. E
- 2.26c Screen for early abnormal glucose metabolism with dysglycemia using FPG of 110–125 mg/dL (6.1–6.9 mmol/L) or A1C 5.9–6.4% (41–47 mmol/mol). B
- 2.27 Screen for GDM at 24–28 weeks of gestation in pregnant individuals not previously found to have diabetes or high-risk abnormal glucose metabolism detected earlier in the current pregnancy. A
- 2.28 Screen individuals with GDM for prediabetes or diabetes at 4–12 weeks postpartum, using the 75-g OGTT and clinically appropriate nonpregnancy diagnostic criteria. A
- 2.29 Individuals with a history of GDM should have lifelong screening for the development of prediabetes or diabetes at least every 3 years. B
- GDM diagnosis (Table 2.7 ) can be accomplished with either of two strategies:
- The "one-step" 75-g OGTT derived from the IADPSG criteria, or
- The older "two-step" approach with a 50-g (nonfasting) screen followed by a 100-g OGTT for those who screen positive based on the work of Carpenter-Coustan's interpretation of the older O'Sullivan and Mahan (207) criteria.
Reference:
- American Diabetes Association Professional Practice Committee; 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2024. Diabetes Care 1 January 2024; 47 (Supplement1): S20–S42. https://doi.org/10.2337/dc24-S002
- https://diabetesjournals.org/care/article/47/Supplement_1/S20/153954/2-Diagnosis-and-Classification-of-Diabetes
3.
ADHD Stuff to Edit
ADHD Tips (New) edit
- General
- Cleaning
- Memory
- Time Blindness
- Distractions
- Getting Things Done
- Emotional Dysregulation
- Sleep
- Relationships
- Work
- School
- Executive Function
- Nutrition/Medication
- General
- Pack things the day before so you don't forget
- Don't drink alcohol. Causes brain fog and it can negatively interact with medications. Alcohol can even cause ADHD-like symptoms in non-ADHD people
- Do Cardio before you need to do stuff that requires sitting. It helps you focus.
- Use text-to-speech generators to help you read webpages/books
- Keep things at eye level (Especially notes/todo lists)
- Be stupidly early to places just in case you forget something
- Stretch once in awhile.
- Take a deep breath.
- Take a cold shower in the morning or turn it cold just for 30-60 seconds at the end of your shower. Wakes you up, gets your blood flowing and gets you out of the shower.
- Get a therapist if you can.
- Buy a whiteboard to sketch out things when your mind starts going into overdrive.
- Enjoy the journey more than the destination, don't be in a hurry to finish something you are doing, but always at least do something small everyday. Life is not a race, rather, it is an accumulation of smaller improvements to oneself.
- People are in such a rush these days… You can't expect to become a superhuman overnight. Focus on sustainability first and enjoy the journey.
- Cleaning
- Have a designated spot for every single item (Put it in the same place every time)
- Have a "misc" basket in each room. If you're truly unable to put something away, put it in the basket. Have a designated period of time, once a week, when your sole priority is to put everything away, all at once.
- Whenever you lose something that you "put away," start keeping it in the first place you looked for it.
- In order to not get overwhelmed when cleaning, remember there are only 5 things you need to tackle:
- Trash
- Laundry
- Dishes
- Putting things back that have a place
- Put things in a pile that don't have a place
- If you're moving from one room to another, take the item with you that needs to go to the other room. It's already on your way and it's one less thing cluttering your room.
- If you can afford it: Get a cleaning person; It takes them 3 hours to do what you can do in 3 weeks. While they are there, use them as an accountability buddy and sort out your misc tasks like paying bills.
- Embrace chaos. Let your brain get distracted when you're cleaning. Cleaning dishes and spot trash? It's fine, go clean that and then get back to the dishes
- Have a dedicated playlist for cleaning. High tempo songs help keep you moving.
- Do chores before you go to bed. No matter what your routine is, you have to go to bed at some point. You can "habit-chain" cleaning into going to bed.
- Listen to podcasts/audiobooks when doing chores. My excitement to listen to a new episode of my favorite podcast motivates me to do boring stuff like dishes or laundry.
- Memory
- Park in the same place/area every time when you go to a common place. You won't forget where you park that way.
- Keep a spare house key in your car and one outside your house.
- Keep important items in visible and convenient locations. e.g: Take pills when you eat? Keep your bottle beside your table where you eat.
- Get a Tile. Bluetooth GPS trackers that are a game changer for ADHD people that lose keys/wallets.
- Tape your most often made recipes to the inside of your kitchen cabinet doors.
- Three point check when you close the front door: Phone, wallet, keys
- Use voice assistants. "Remind me to do X tomorrow at Y time"
- Use the mind palace memory exercise to help solve retention issues.
- Keep forgetting your lunch? Put your keys or phone on it. That way you can't leave without your lunch - This can be helpful with other related things
- If you need to remember to bring something with you the next day, place it right in front of the exit door so you HAVE to touch it before you leave the house. If it's something in the fridge, put a sticky note on the exit door's handle.
- Buy multiple items that you use often. Setup multiple chargers at work/home (so you have a spare if you lose one). e.g. buy 10 different lip balms so you can always find it when you need it.
- Have convenient, labeled spaces for things. It's hard to forget your phone when you ALWAYS put it beside your charger.
- Have rules for placement of the important things in your life. (it's too hard to do it for everything)
- Create a second brain for yourself - in whatever way is most appealing to you.
- Count your steps as you walk into a new room. It'll help you remember why you entered that room. It gives you something to focus on but it's not too much that you'll get distracted.
- Use a bowl to throw your keys, badges, and wallet into when you get home. That way you can't leave without ALL the stuff you need.
- ALWAYS have a bag with the essentials. On mine a have my keys, charger, papers and even tooth brush. If I'm going out, I do not waste time searching for everything. Just search for a bag.
- Make a calendar entry for every scheduled thing religiously unless it's routine like a 9-5 job. Make the calendar entry immediately while making the appointment. Do this for parties, birthdays, dates, finals, med refills, trash night, etc.
- Use Spaced Repetition to study for your exams, remember things about people in your life, and literally everything you can possibly make a flashcard for.
- Time Blindness
- Set your phone clock 10-15 mins fast on purpose
- Put appointments in your calendar 10-20 minutes earlier than the actual appointment
- A schedule is only as good as the alarms and info you put in
- Set timers for activites you hyperfocus on. BUT set the timer for X minutes less than the task takes. (Give yourself time to wrap up whatever you're working on) Additional Protip: Use this on a watch rather than your phone to avoid getting distracted. A basic watch/smart watch will save your life.
- Download an app on your phone that chimes and buzzes every half an hour during your awake time. Keeps you aware of how much time has passed.
- Track your time. Every morning, write out a todo list by hand and track the time taken for each task. (Write down the time whenever you take a break or switch tasks) - I personally use Toggl to track my time
- Get an electric toothbrush with a timer. ADHD people have time blindness and it'll make sure you brush for at least two minutes.
- Distractions
- Disable all your notifications on your phone except for essential apps (Texting, Voicemail, Calendar)
- Use website blockers for distracting websites
- Cold Turkey
- Freedom and News Feed removers for social media + Youtube
- If you can't stop yourself from answering that text/email/IM right away but don't actually have time to deal with it, tell the person you'll respond when you get a minute.
- Your brain focuses better after some exercise. Cardio works best.
- Use a noise-cancelling headset and listen to music/white noise/brown noise. Enables hyperfocus and blocks out distractions
- If the headset isn't in your budget: Brown noise + earphones will get you 80% of the way there.
- Limit Distractions: For instance, you could:
- Try noise-canceling headphones.
- Be wise with your choice of music while working. Lyric-less music tends to be the least distracting for many people.
- Download apps that block social media apps for a set time.
- Keep your workspace tidy.
- Write down distracting thoughts as they come, then forget about them until you've completed your tasks.
- Getting Things Done
- If you have an Android: Put a widget from your todo list app on your home screen so it's the first thing you see
- Break tasks down into as many smaller tasks as you need for it to feel manageable.
- Learn to plan around transitions. It's easier to start things if you chain them with another task that is ending.
- Use the pomodoro technique for everything. It's great having a break to look forward to.
- Remember that something is better than nothing. If you only get 26% of a task done then it's further than if you never started. It's better to do little bits of every task rather than procrastinating.
- Attach numbers to events. e.g: Going to bed (3) - Brush, Floss, Mouthwash.
- Lie to yourself. I'll tell myself that I'm just going to unload one dish from the dishwasher. Once I've started, I'll at least unload a few, and maybe clean the whole kitchen.
- Decide what you're going to do each day beforehand, preferably while your meds are at their workingest. Make sure it's only 1 thing.
- Understand that FUTURE YOU IS STILL YOU. If you think you'll do something later, understand that future you is still you. Future you isn't more likely to muster up the desire to do the work. f you don't have the motivation to do it in the next 24 hours then future you probably won't either.
- When you need to transition between tasks, pretend that you are talking to a friend who is having issues with something. Give yourself a nudge and remind yourself it's time to switch tasks/get started. (Detach yourself from the task)
- When you take breaks, make sure your break isn't too interesting. That way you won't get absorbed in your break. Just clean during your break or something like that.
- Gamify things and set a limited amount of time to accomplish something. e.g: Brew your coffee and get as many chores done as you can before the coffee is finished brewing.
- Write TODO lists as a brain dump. And then order them in importance or the order you want to do them in. That way you don't pause while writing down tasks.
- Don't be afraid to stimulate yourself if you need it. Listen to a podcast or music to get yourself to do something.
- Reward yourself when you get things done. Positive Reinforcement is good and you'll feel like getting more things done.
- Change your environment and work from a place where there are fewer distractions. e.g: Cafe/library. You'll get more stuff done
- Set a time to do work, and a time to relax; that way you don't feel guilty about relaxing during the time you set aside for yourself.
- Change your alarm sounds/timer sounds frequently, but use alarms and timers as much as possible.
- Treat timers and alarms like non-negotiable laws. When the timer goes off, doesn't matter what you were doing seconds ago, it's time to go. Half showered, wet hair, one eye done, whatever it is, you're out the door.
- Body doubling - if you need to do some work that requires focus without much fun, have someone in the room with you. They could be working too, or not. Just having them there makes everything just a little more interesting and a little more accountable.
- I feel like a lot of people are missing some sort of accountability system in their lives. I don't do body doubling but I use Beeminder to keep me accountable.
- Emotional Dysregulation
- Brain dump in a notebook by your bed every night.
- Don't feel bad about sucking at school/work. You'll get better as you learn more strategies for coping with ADHD. Things get better
- Use writing/journaling as cognitive therapy to defuse emotional history
- Remind yourself that the world won't end if a few things fall behind.
- Write a reverse todo-list. Write down the things you have accomplished for the day. That way you won't feel overwhelmed and it'll make you feel better.
- You're allowed to let things go. Forget irrelevant things and forgive yourself. Ignore the awkward thing you did last week. Life will move on.
- Forgive yourself for your limits.
- Meditation. Active breaks for people that struggle to take breaks. Use a meditation app when you're starting. Like Headspace
- Start working on letting go of shame. It depresses your motivation and only makes things worse. You wouldn't shame someone in a wheelchair for not getting things done, your difficulty is in your brain instead of your legs but it's no less real.
- Cognitive Behavioural Therapy + meditation
- You're allowed to let things go. Forget irrelevant things and forgive yourself. Ignore the awkward thing you did last week. Life will move on.
- Stop hating yourself. Don't look at the future. Don't look at the past. Look at the present. I used to always hate myself for being so unproductive. I realised how pointless that was and I started to focus on improving myself in the present.
- Sleep
- Put your phone on the other side of the room and make your alarm super loud. Gets you out off bed and will make you turn it off so you don't wake other people up.
- If you're having trouble getting out of bed then set a timer on your phone for 5 minutes and chuck it across the room. It'll force you to get up and turn it off.
- Buy 2 bright lamps and 2 timers. Set them up to turn on automatically 5-15min before you want your alarm to go off in the morning. The lights help your body know its daytime
- Change your thermostat so the temperature goes down an hour before bedtime and gets warmer 30 minutes before you wake up. The cooler temperatures get your body to sleep and the warmer temperatures help you wake up
- Use a reminder app for starting your bedtime routine, not just your bedtime. (And have a bedtime routine)
- Try setup meetings/commitments early in the morning. They'll force you to get out of bed
- Set two alarms when you get up in the morning. One to get out of bed and one for your medication. e.g: 5:30 AM wake up and take medication and then fall back to bed. By your 6AM alarm you'll have waken up and your meds will have kicked in
- What a great lifehack. I've been doing this the past few days (except I don't wake up at 6AM) - it works pretty well. Also I throw my phone on the other side of the room so it forces me to get out of bed.
- Relationships
- It's okay to be in a room with people and just let people breathe. You don't need to fill the silence.
- When having a conversation or learning something, repeat every word the person says in your head. It'll help you not drift off as much. It also makes it so you'll interrupt people less.
- Try to avoid the word 'but' when faced with a conflict. Instead try be constructive towards arguments/discussions with the word 'and'.
- For maintaining eye contact: Imagine a red dot on someone's nose for intense focus. Bridge of the nose for paying attention.
- Haven't tried this one but I used to have trouble with eye contact a few years ago so this stood out to me. I'm pretty good with eye contact now, but I'll be trying it over the next few weeks anyway.
- Work
- If you hate your job. Make a job switch. It'll help you make positive changes in your life.
- Find a job that works WITH your system. If you can't wake up and be functional in the morning then stop trying. Find a job that doesn't need you to wake up in the morning. Stop beating yourself up over things your brains isn't designed for
- Be self-employed and start a business. "No matter where I worked or what I did, I was constantly watching the clock, hating every single second of it. On Saturday I worked 27 straight hours to finish a job on time and it was still less painful than working an 8 hour shift as an employee. Those 27 hours disappeared and left me feeling gratified because I made someone's house beautiful and I got to see how happy I made her the first time she saw her new home."
- When promising a timescale to a client, double or triple the amount of time that you initially think it will take. That way worst case scenario, you will finish it on deadline and meet expectations or best case, finish before and exceed expectations.
- The moment you know you aren't going to make a deadline, let the client know and again give them an overestimate of time for new deadline. People are always understanding and appreciative for this quick communication.
- Reply to emails and messages when you read them. 99% of the time, days and weeks will go by if you tell yourself that you'll reply later on…
- Be honest about your limitations and own your shit. Most people have no idea how much adhd affects so many things and therefore can't understand our inability to do basic things at times. Especially if you come across as smart and creative, they can misplace our struggles for laziness and lack of care. If you fuck up own it, explain why and apologise. It doesn't have to be long winded but it is important to state how you aim to rectify the situation and again.
- Stop comparing your output and motivation to others and embrace a slower, more considered, creative one. You are not other people. You are you. Trying to jam your freeform, 12 sided shape into the round hole is painful and won't work. You don't need a hole, you need self acceptance.
- Learn to say no to taking on things that you know may cause you stress and excess pressure just because it's money. It is not worth it, just put the boundaries that will save your mental health in the first place and you won't have to deal with the fallout later. The more you do it, the easier it becomes.
- God yes… ADHD people have a dangerous habit of overcommitting to stuff. Personally I think I just forget that I'm already working on X, Y and Z. Sustainability is important - don't overcommit.
- School
- Use Active Recall + Spaced Repetition to study for all your exams. I've seen countless people go from C's to straight A's after adopting them
- If you're finding it difficult to start assignments early then ONLY read + annotate the assignment brief early and go take a break after that. Your subconscious should process the information and it'll be easier to start later on.
- It's better to turn in an assignment that is 75% done. It'll drag your grades down less than if you never turned it in
- Print out lectures and powerpoints in advance (ask the teacher for them). That way you won't need to listen and write at the same time. You can annotate the printed versions instead.
- Visit your school's inclusivity and disability team. They will hopefully have policies for helping people with ADHD
- This is something I never took advantage of while at University, but I probably should have. A few assignment extensions when my meds stopped working would have saved me from countless all nighters…
- Executive Function
- Setup a morning routine + a reset routine. A reset routine is something you do when you're feeling super unfocused. Mine consists of meditation, exercise, journaling, playing music and making some tea.
- If it takes less than ten minutes to do the task, just do it immediately.
- Have a uniform for work, social and casual scenarios. Don't mix your work clothes with your casual clothes.
- If you start to feel frustrated for no reason, eat something and keep yourself hydrated. (Self-care flowchart)
- it's better to half-ass most things than it is to not do them at all.
- Set alarms using music rather than the default alarm sounds. It'll help you get going. (And music releases norepinephrine in your brain!)
- Make yourself kits for common repeated household tasks. e.g: Cleaning Kit, Package mailing kit… Reduces the friction needed to get started on a task
- Refine your routine and rituals to reduce the overall time it takes to get them ready. Reduce the friction needed to start your morning routine. e.g: Prepare a filled pot of coffee the night before.
- Set just a few non-negotiable standards and laws for yourself. Pick those that improve your life the most. e.g: No phone in bed at night or in the morning. Not even a quick email check. And read your goals every morning.
- When you're trying to get started on a task: Write down the steps you've already done and the steps you plan to do next. Helps a lot with spaghetti thoughts
- Drink a big glass of water when you know you are going to have to start doing a thing in a bit. When you inevitably have to go pee, start after you wash your hands. You are already up and your brain already had to switch gears. Use it as momentum.
- On tough days. Use the 1-thing theory. Just try and accomplish just one-thing for that day. e.g. Clean the kitchen.
- A bit less life-hacky compared to the others but I've found that getting started is a lot easier when you only have a single priority.
- Nutrition/Medication
- If you are Vitamin D deficient then take Vitamin D supplements (see a doctor first). It'll help your mood and energy levels.
- Eat lots of protein and stay hydrated.
- Figure out if you're deficient in anything and try fix those things. This includes getting a food allergy test, figuring out deficiencies and eating a healthy diet.
- Use a 7-day pill organiser with AM/PM slots and put your medication and supplements there.
- I know a lot of people have issues with remembering if they took their medication. This is an easy, simple and cheap fix.
Reference:
More ADHD Tips
- Improve productivity
- A wall calendar: A dry erase wall calendar is a great way to keep on top of things. You can write appointments and deadlines in bright colors and cross off each day that goes by– this helps a ton with time blindness.
- Use color: People with ADHD are often visually oriented. Use colors to help things stick in your memory, such as highlighting important dates, color-coding files, putting to-dos on bright paper, and adding stickers or color to virtually anything that needs your attention. You can also use color-coding on Google calendar to make things stand out.
- Break down tasks: Have a goal or deadline? Create mini-deadlines along the way. This can help boost confidence and keep you from feeling overwhelmed,
- Try the Pomodoro Technique: Set a timer for 20 minutes and begin working on your task. After 20 minutes, take a 5-minute break and repeat again. Give yourself a check mark for every cycle completed.
- Reframing: Combat unhelpful thought patterns by reframing tasks in a positive or more realistic way. For instance, if you are delaying beginning a project and your initial thought is, "there's so much work it'll take forever," try checking yourself with a less negative and more realistic thought like, "if I begin this today, I'll feel better, and there will be less work tomorrow."
- 24-Hour Hot Spot: Have a designated area somewhere like your desk where you can place your "need to-dos." Place anything there that needs your attention within 24 hours so that it doesn't get lost.
- Pocket Notes: Writing on your hand is risky; try writing important things on notes and putting them in your pocket. Make sure it's your dominant side pocket, so you're more likely to reach in there and find your reminder.
- Get Smart(phone): Utilize your notepad, reminder alerts, and calendars to help you meet deadlines. Don't be shy about setting several obnoxious reminders leading up to your deadline.
- Sleep better with ADHD
- Set a Wind-down Alarm: Most smartphones allow you to program your bedtime and will alert you an hour before you intend to be sleeping. Use this alert to power down electronics, dim the lights and begin your bedtime routine.
- Happy Lamp: Many people with ADHD have physiological differences in their circadian rhythms that make it hard to get consistent sleep. Using a happy lamp or getting 20 minutes of early morning light exposure is a great way to help boost your circadian rhythm.
- Melatonin: Many people with ADHD have lower levels of melatonin. Try a supplement (0.3mg is the ideal dose) or have melatonin-inducing snacks like tart cherry juice.
- No Late Lattes: It takes your body up to 12 hours to fully metabolize caffeine. Skip caffeinated beverages within 5-7 hours before bed for better sleep.
- Quiet your mind: Racing mind keeping you awake? Using techniques like progressive muscle relaxation can help quiet your mind and ease you into sleep.
- Get Noisy: Noise machines, especially pink noise (think ocean waves and raindrops), can boost sleep and improve sleep stability.
- Keep it Cool: Turn the temperature in your room down to 65-68 °F (18-20 °C), the ideal temperature range for sleep and melatonin production.
- Wake up at the same time every morning: Your body's sleep system thrives on consistency. Keeping a regular wake time is the most realistic way to maintain a consistent schedule and regulate your sleep hormones.
- Sleep Mask: Using an eye mask or blackout curtains can completely transform your sleep because darkness is key to keeping melatonin flowing.
- Only use the bed for sleep: Doing non-sleep activities in your bed can create unhelpful associations like bed + work, bed+ horror films, or bed+ existential dread. Only use your bed for sleep (and intimacy); sleep therapists call this stimulus control.
- Get chores done
- Start small: Give yourself the luxury of tiny tasks that bring you closer to your big tasks. Need to clean the kitchen? Start with one section of the countertop. Some progress is better than none. Always start one room at a time and narrow it down to one section of that room if needed.
- Grocery apps: Apps like Out of Milk help you track grocery lists using a simple scanning system. You can even sync your list with other people in the household.
- Home routine calendar: Keep things simple by building out a chore list that you can follow each week. Use a wall calendar and lots of colors to remind yourself which chores you should be doing on which days.
- Let your plants live: Keep house plants alive with apps like Happy plant that help you track your watering schedule.
- 20-minute rule: Before you allow yourself to indulge in some "downtime" (aka Netflix binge), earn the privilege with the 20-minute rule. Simply set a timer for 20-minutes and use that time to tackle a task. You can do the same task every time, such as cleaning up the clothes in your room. Try making a game out of it if you have a spouse or kids!
- Make it fun: Chores can feel daunting, but they aren't actually that bad. Set the tone by adding fun tunes, putting on a cute "cleaning outfit," and set your focus on one single task at a time.
- Invite people over: Nothing motivates you to tidy up quite like a guest. Make an attempt to have people over for dinner or drinks regularly and use it as motivation to tidy up.
- Ask for Help: if you feel overwhelmed, ask for help. Reaching out to a loved one can make it feel less overwhelming, and sometimes all you need is a little encouragement to get started. Plus, maybe they have time to lend a hand.
- Make it fitness: Put on your pedometer and vow to use chores as your workout for the day.
- Hunt for old food: Pick a day of the week where you empty old food from the fridge (feeling seen now, aren't you?).
- Control & reduce ADHD impulsivity
- The 24-hour rule: Whenever you go to make an impulsive decision or impulsively sign-up for something, give yourself a mandatory cooling-off period. Aim for at least 24-hours before diving in. If it's actually something you "need," the desire will still be there.
- Where will this live? When shopping and feeling compelled to buy, ask yourself, "where will this live?" Stopping to visualize its place in your life can lead to a humbling moment of clarity.
- Repeat before speaking: Impulsive reactions are hard to control. When listening, make an effort to paraphrase what was said before going ahead with your response. It will not only clarify any potential misconceptions but will also give you a second to mull over your response.
- Analyze yourself: Practice labeling your impulsivity by writing out the situation, how you felt before you acted, and what you need to do next time to stop the impulsive behavior. Approach it like a logical scientist trying to solve a puzzle.
- Elastic Band: Put an elastic band around your wrist, and whenever you feel the urge to act impulsively, snap the band. It's a technique that brings your senses back to the present moment and can help break unhelpful patterns.
- Note it: Before speaking up in meetings or discussions give yourself a moment to write it out. You can use a notepad or your phone to quickly note what you want to say and bring it up later if it's still important.
- Meditate: Daily meditation practice helps improve your ability to pause before acting. You can start with as little as 2-3 minutes a day and aim to work up to 10-20 minutes.
- Exercise: Daily activity is an excellent way to get rid of feelings of angst and restlessness that feed impulsive behaviors. Aim for 20 minutes a day and do something you enjoy. Even a daily walk is enough for major benefits.
- Practice pausing: Make an effort to carefully listen to every word when someone is talking and then take a three second pause before speaking. You can start out with someone you trust then try it out in the wild.
- Apologize: Interrupting happens. If you cut someone off acknowledge it, apologize, and give them a chance to finish their thought. Explain why you did it if you feel like it.
- Overcome procrastination
- Lock Box: Phones are one of the biggest distractions, especially for people with ADHD. Use a timed lock box to put away your phone when you have important tasks to do! Tik Tok will still be there when you're done.
- Look around you: Creating a clear space that is void of distractions is pretty important for productivity. Do your best to have a clear space or use baskets to hide distractions while you're working.
- Just do the thing: Whenever possible, do things immediately. When life gets busy or distractions come along the ADHD mind has a hard time regrouping. No matter how annoying it may feel, take a deep breath, put on your disciplined pants, and just do the thing.
- Get stimulated: ADHD minds often feel understimulated which can lead to dropping boring tasks for more exciting ones. Add in a fidget spinner, soothing music, slime, exercise, a podcast or anything that helps you get going. It's perfectly ok to pair activities as long as it helps you move closer to your goal.
- Try L-Theanine with caffeine: Supplementing L-theanine with Caffeine can help boost the "focus" effects of caffeine while lulling anxiety. Studies show this combo helps improve sustained attention and cognitive performance in people with ADHD.
- Positive Self-talk: Meet your negative inner voice with an encouraging one. Try phrases like "I tried my best and that's enough", "nothing is perfect, it's ok to be human", or "I am strong, capable, and I can get through anything."
- Hug your inner child: Many people with ADHD grow up feeling misunderstood, so, positive reassurance from your adult self to your inner child can go a long way. Imagine your inner child and give them an little encouraging hug. Try cheering them on and letting them know that you'll do your best to guide them through life with acceptance and understanding.
- Clarify your goals: Clarify your final goal and then break down the "mini" goals you need to meet along the way to get there. Focus on the very first mini-goal, set a deadline, and work on that alone. If you still feel overwhelmed, break your mini-goals down further. The point is to just get moving ahead.
- Better manage your mood
- Schedule downtime: Set aside some time every week (or even a slot every day) to just do whatever the heck you want. You can blast music, zone out on your phone, indulge in a hobby– whatever brings you joy. Scheduling in this "do whatever I want" time brings structure to much-needed downtime, so you don't end up wasting hours then feeling guilty.
- Accept the highs and lows: Learning to accept the emotions that you experience without judgement can bring a ton of relief. When you feel extremely sad, frustrated or anxious, try not to fight it or seek a reason. Sit with the feeling, allow the thoughts to come and go without judgement, and remind yourself that everything passes in time. Emotions aren't the end of the world; they'll just make you uncomfortable for a little while.
- Journal it: Writing out your thoughts and feelings every day, or when upset, can help you work through what you're experiencing and find calm.
- Breathwork: Feeling frazzled, overwhelmed, and anxious is a common concern with ADHD. When you feel these sensations, try to focus on your breath and take a few deep breaths in through your nose and slow breaths out through your mouth. It activates your parasympathetic nervous system, which calms down your body's stress response.
- Take a time-out: When you feel angry, frustrated, overstimulated or ready to lash out – take a time-out. You can choose a walk, sitting quietly, headphones and soothing music, or anything that brings you calm. Feel empowered to remove yourself from situations in order to take care of your mental health.
- Learn to be kind: Your brain is wired in a way that makes planning, attention, biting your tongue and execution of daily tasks challenging. Instead of being mean to yourself when things go wrong, try to develop an open dialogue. You can try phrases like "ok, ADHD, you win this round."
- Find like-minded people: Being surrounded by people who understand you is important. If your current circle is open, try sharing articles about ADHD or telling them what it's like. You can also find support groups online, ADHD forums or Instagram accounts that help you feel seen and understood.
- Get a therapist: Therapy can be a huge help for learning emotional regulation skills and self-acceptance. Think of therapy as personal training for your brain– sometimes, you need a little guidance to whip things into shape. There are many online options available now which makes therapy more convenient and affordable than ever.
- Self-care
- Identify triggers: Knowing what triggers you is important. Identify sounds, situations, and even people who cause you to feel overwhelmed and frustrated and plan for it. It may be as simple as carrying earplugs or headphones.
- Schedule a meal: Skipping meals and binging is a hard habit to break. Do your best to get in a protein-rich meal or shake early in the day, no matter what. It will help regulate your appetite and make sure your body has what it needs to make things like dopamine.
- Hygiene: Staying on top of hygiene routines can sometimes be hard, yet other times you're pulling off 25-step skincare routines. Try simplifying when you're struggling, use dry shampoo, seek an accountability buddy, and be kind to yourself about the ups and downs.
- Stains happen: ADHD is a life of stains. Become a stain-removing guru using tips from this site and save your favorite clothes.
- Add yoga: Even just 10-15 minutes a day of yoga can make a huge difference for your wellbeing, frustration tolerance, and stress levels.
- Add a mantra: Sometimes, you're going to have a hard day. Try repeating a mantra like "Now is not forever. Be here now."
- Practice Gratitude: Add a reminder on your phone for the same time every day to practice gratitude. Stop what you are doing when it goes off, and think of one thing you are truly grateful for in that moment. Do your best to sit with it for just 60 seconds.
- Indulge when down: Give yourself permission to put on a face mask, have a hearty snack, and watch your favorite show at the end of a hard day. Sometimes you just need to treat yourself to a dream date…with yourself. Take the time you need, and don't feel like you're being selfish.
- Build boundaries: It's hard to say no. Avoid burning yourself out by giving yourself permission to not participate or to bow out if you've agreed to something without thinking it through.
- Take off your cape: Being a superhero is fun, but you can lose yourself along the way. You don't have to take care of everyone, and you don't have to be perfect. Try to stay realistic in how much you can balance and repeat the phrase "I am human."
- Love yourself: Write a positive affirmation on a sticky note and place it on a mirror you see every day. Make sure it's placed where you'll always read it. Start with something like "I am enough" and switch it up regularly to create subtle inner self-hype and love. You deserve it.
Reference:
More ADHD Tips
- Tips for getting organized and controlling clutter
- The hallmark traits of ADHD are inattention and distractibility—making organization perhaps the biggest challenge adults with the disorder face. If you have ADHD, the prospect of getting organized, whether it be at work or home, may leave you feeling overwhelmed.
- However, you can learn to break tasks down into smaller steps and follow a systematic approach to organization. By implementing various structures and routines, and taking advantage of tools such as daily planners and reminders, you can set yourself up to maintain organization and control clutter.
- Develop structure and neat habits—and keep them up
To organize a room, home, or office, start by categorizing your objects, deciding which are necessary and which can be stored or discarded. To organize yourself, get in the habit of taking notes and writing lists. Maintain your newly organized structure with regular, daily routines.
- Create space. Ask yourself what you need on a daily basis, and find storage bins or closets for things you don't. Designate specific areas for things like keys, bills, and other items that can be easily misplaced. Throw away things you don't need.
- Use a calendar app or day planner. Effective use of a day planner or a calendar on your smartphone or computer can help you remember appointments and deadlines. With electronic calendars, you can also set up automatic reminders so scheduled events don't slip your mind.
- Use lists. Make use of lists and notes to keep track of regularly scheduled tasks, projects, deadlines, and appointments. If you decide to use a daily planner, keep all lists and notes inside it. You also have many options for use on your smartphone or computer. Search for "to do" apps or task managers.
- Deal with it now. You can avoid forgetfulness, clutter, and procrastination by filing papers, cleaning up messes, or returning phone calls immediately, not sometime in the future. If a task can be done in two minutes or less, do it on the spot, rather than putting it off for later.
- Tame your paper trail
If you have ADHD, paperwork might make up a major part of your disorganization. But you can put a stop to the endless piles of mail and papers strewn across your kitchen, desk, or office. All it takes is some time to set up a paperwork system that works for you.
- Deal with mail on a daily basis. Set aside a few minutes each day to deal with the mail, preferably as soon as you bring it inside. It helps to have a designated spot where you can sort the mail and either trash it, file it, or act on it.
- Go paperless. Minimize the amount of paper you have to deal with. Request electronic statements and bills instead of paper copies. In the U.S., you can reduce junk mail by opting out of the Direct Marketing Association's (DMA) Mail Preference Service.
- Set up a filing system. Use dividers or separate file folders for different types of documents (such as medical records, receipts, and income statements). Label and color-code your files so that you can find what you need quickly.
- Tips for managing your time and staying on schedule
Trouble with time management is a common effect of ADHD. You may frequently lose track of time, miss deadlines, procrastinate, underestimate how much time you need for tasks, or find yourself doing things in the wrong order. Many adults with ADHD spend so much time on one task—known as "hyperfocusing"—that nothing else gets done. These difficulties can leave you feeling frustrated and inept, and make others impatient. But, there are solutions to help you better manage your time.
- Time management tips
- Adults with attention deficit disorder often have a different perception of how time passes. To align your sense of time with everyone else, use the oldest trick in the book: a clock.
- Become a clock-watcher. Use a wristwatch or highly visible wall or desk clock to help you keep track of time. When you start a task, make a note of the time by saying it out loud or writing it down.
- Use timers. Allot yourself limited amounts of time for each task and use a timer or alarm to alert you when your time is up. For longer tasks, consider setting an alarm to go off at regular intervals to keep you productive and aware of how much time is going by.
- Give yourself more time than you think you need. Adults with ADHD are notoriously bad at estimating how long it will take to do something. For every thirty minutes of time you think it will take you to get someplace or complete a task, give yourself a cushion by adding ten minutes.
- Plan to be early and set up reminders. Write down appointments for fifteen minutes earlier than they really are. Set up reminders to ensure you leave on time and make sure you have everything you need ahead of time so you're not frantically looking for your keys or phone when it's time to go.
- Prioritization tips
Because adults with ADHD often struggle with impulse control and jump from one subject to another, completing tasks can be difficult and large projects can seem overwhelming. To overcome this:
- Decide what to tackle first. Ask yourself what the most important task is that you need to accomplish, and then order your other priorities after that one.
- Take things one at a time. Break down large projects or jobs into smaller, manageable steps.
- Stay on task. Avoid getting sidetracked by sticking to your schedule, using a timer to enforce it if necessary.
- Learn to say no Impulsiveness can lead adults with ADHD to agree to too many projects at work or make too many social engagements. But a jam-packed schedule can leave you feeling overwhelmed, overtired, and affect the quality of your work. Saying no to certain commitments may improve your ability to accomplish tasks, keep social dates, and live a healthier lifestyle. Check your schedule first before agreeing to something new.
- Time management tips
- Tips for managing money and bills
Money management requires budgeting, planning, and organization, so for many adults with ADHD, it can pose a true challenge. Many common systems of money management don't tend to work for adults with ADHD because they require too much time, paper, and attention to detail. But if you create your own system that is both simple and consistent, you can get on top of your finances and put a stop to overspending, overdue bills, and penalties for missed deadlines.
- Control your budget
- An honest assessment of your financial situation is the first step to getting budgeting under control. Start by keeping track of every expense, no matter how small, for a month. This will allow you to effectively analyze where your money is going. You may be surprised at how much you're spending on unnecessary items and impulse purchases. You can then use this snapshot of your spending habits to create a monthly budget based on your income and needs.
- Figure out how you can avoid straying from your budget. For example, if you're spending too much at restaurants, you can make an eating-in plan and factor in time for grocery shopping and meal preparation.
- Set up a simple money management and bill paying system
Establish an easy, organized system that helps you save documents, receipts, and stay on top of bills. For an adult with ADHD, the opportunity to manage banking on the computer can be the gift that keeps on giving. Organizing money online means less paperwork, no messy handwriting, and no misplaced slips.
- Switch to online banking. Signing up for online banking can turn the hit-or-miss process of balancing your budget into a thing of the past. Your online account will list all deposits and payments, tracking your balance automatically, to the penny, every day. You can also set up automatic payments for your regular monthly bills and log on as needed to pay irregular and occasional ones. The best part: no misplaced envelopes or late fees.
- Set up bill pay reminders. If you prefer not to set up automatic payments, you can still make the process of bill paying easier with electronic reminders. You may be able to set up text or email reminders through online banking or you can schedule them in your calendar app.
- Take advantage of technology. Free services can help you keep track of your finances and accounts. They typically take some time to set up, but once you've linked your accounts they automatically update. Such tools can make your financial life easier.
- Put a stop to impulse shopping
Impulsivity from ADHD and shopping can be a very dangerous combination. It can put you in debt and make you feel guilty and ashamed. You can prevent impulsive buys with a few strategic tactics.
- Shop with cash only—leave your checkbook and credit cards at home.
- Cut up all but one credit card. When you shop, make a list of what you need and stick to it.
- Use a calculator to keep a running total when shopping (hint: there's one on your mobile phone).
- Stay away from places where you're likely to spend too much money, throw away catalogs as they arrive, and block emails from retailers.
- Control your budget
- Tips for staying focused and productive at work
- ADHD can create special challenges at work. The things you may find toughest—organization, completion of tasks, sitting still, listening quietly—are the very things you're often asked to do all day long.
- Juggling ADHD and a challenging job is no easy task, but by tailoring your workplace environment you can take advantage of your strong points while minimizing the negative impact of your ADHD symptoms.
- Get organized at work
Organize your office, cubicle, or desk, one manageable step at a time. Then use the following strategies to stay tidy and organized:
- Set aside daily time for organization. Mess is always distracting so set aside 5 to 10 minutes a day to clear your desk and organize your paperwork. Experiment with storing things inside your desk or in bins so that they don't clutter your workspace as unnecessary distractions.
- Use colors and lists. Color-coding can be very useful to people with ADHD. Manage forgetfulness by writing everything down.
- Prioritize. More important tasks should be placed first on your to-do list so you remember to do them before lower priority tasks. Set deadlines for everything, even if they are self-imposed.
- End distractions
When you have attention issues, where you work and what is around you can significantly affect how much you are able to get done. Let your workmates know you need to concentrate, and try the following techniques to minimize distractions:
- Where you work matters. If you don't have your own office, you may be able to take your work to an empty office or conference room. If you are in a lecture hall or conference, try sitting close to the speaker and away from people who chat during the meeting.
- Minimize external commotion. Face your desk towards a wall and keep your workplace free of clutter. To discourage interruptions, you could even hang a "Do Not Disturb" sign. If possible, let voicemail pick up your phone calls and return them later, turn off email and social media during certain times of the day, or even log off the Internet completely. If noise distracts you, consider noise-canceling headphones or a sound machine
- Save big ideas for later. All those great concepts or random thoughts that keep popping into your head and distracting you? Jot them down on paper or on your smartphone for later consideration. Some people with ADHD like to schedule time at the end of the day to go through all the notes they've made.
- Stretch your attention span
As an adult with ADHD, you are capable of focusing—it's just that you may have a hard time keeping that focus, especially when the activity isn't one that you find particularly engaging. Boring meetings or lectures are hard on anyone, but for adults with ADHD, they may pose a special challenge. Similarly, following multiple directions can also be difficult for those with ADHD. Use these tips to improve your focus and ability to follow instructions:
- Get it in writing. If you're attending a meeting, lecture, workshop, or another gathering that requires close attention, ask for an advance copy of the relevant materials—such as a meeting agenda or lecture outline. At the meeting, use the written notes to guide your active listening and note taking. Writing as you listen will help you stay focused on the speaker's words.
- Echo directions. After someone gives verbal instructions, say them aloud to make sure you got it right.
- Move around. To prevent restlessness and fidgeting, go ahead and move around—at the appropriate times in the right places. As long as you are not disturbing others, try squeezing a stress ball during a meeting, for example. Or taking a walk or even jumping up and down during a meeting break can help you pay attention later on.
- Tips for managing stress and boosting mood
Due to the impulsivity and disorganization that often accompany ADHD, you may struggle with erratic sleep, an unhealthy diet, or the effects of too little exercise—all issues that can lead to extra stress, bad moods, and feeling out of control. The best way to stop this cycle is to take charge of your lifestyle habits and create healthy new routines.
Eating well, getting plenty of sleep, and exercising regularly can help you stay calm, minimize mood swings, and fight any symptoms of anxiety and depression. Healthier habits can also reduce ADHD symptoms like inattention, hyperactivity, and distractibility, while regular routines can help your life feel more manageable.
- Exercise and spend time outdoors
Working out is perhaps the most positive and efficient way to reduce hyperactivity and inattention from ADHD. Exercise can relieve stress, boost your mood, and calm your mind, helping work off the excess energy and aggression that can get in the way of relationships and feeling stable.
- Exercise on a daily basis. Choose something vigorous and fun that you can stick with, like a team sport or working out with a friend.
- Increase stress relief by exercising outdoors—people with ADHD often benefit from sunshine and green surroundings.
- Try relaxing forms of exercise, such as mindful walking, yoga, or tai chi. In addition to relieving stress, they can teach you to better control your attention and impulses.
- Get plenty of sleep
Sleep deprivation can increase symptoms of adult ADHD, reducing your ability to cope with stress and maintain focus during the day. Simple changes to daytime habits go a long way toward ensuring solid nightly sleep.
- Avoid caffeine late in the day.
- Exercise vigorously and regularly, but not within an hour of bedtime.
- Create a predictable and quiet "bedtime" routine, including taking a hot shower or bath just before bed.
- Stick to a regular sleep-wake schedule, even on weekends.
- Eat healthfully
While unhealthy eating habits don't cause ADHD, a poor diet can exacerbate symptoms. By making simple changes in what and how you eat, you may experience big reductions in distractibility, hyperactivity, and stress levels.
- Eat small meals throughout day.
- Avoid sugar and junk food as much as possible.
- Make sure you include healthy protein at every meal.
- Aim for several servings of fiber-rich whole grains each day.
- Practice mindfulness As well as reducing stress, regular mindfulness meditation can help you to better resist distractions, lower impulsivity, improve your focus, and provide more control over your emotions. Since hyperactivity symptoms can make meditation a challenge for some adults with ADHD, starting slowly can help. Meditate for short periods and gradually increase your meditation time as you become more comfortable with the process—and are better able to maintain focus. The key is to then draw on these mindfulness techniques during your daily life to keep you on track. Experiment with free or inexpensive smartphone apps or online guided meditations.
- Exercise and spend time outdoors
Working out is perhaps the most positive and efficient way to reduce hyperactivity and inattention from ADHD. Exercise can relieve stress, boost your mood, and calm your mind, helping work off the excess energy and aggression that can get in the way of relationships and feeling stable.
Hotlines and support
- Talk with an ADHD Information Specialist at 1-866-200-8098, Monday-Friday, 1-5 pm ET, or search the Professional Directory for ADHD clinics and other resources. (CHADD)
Reference:
ADHD Study Tips edit
- Establish a study routine. Creating a routine–such as studying for an hour after dinner, or for a half hour each morning–will encourage consistency. When getting started, create a study schedule and set reminders on your phone to help build the habit.
- Create a dedicated study area. Choose an area that is free of distractions where you can set up your study materials and leave them between sessions. When it's time to study, you won't spend time searching for something you need. Just sit down, and you're ready to go.
- Focus on the quality of studying, not the quantity. It's more effective to space out many short study sessions, rather than having one marathon session. Try studying in half-hour to hour-long blocks, with breaks in between. This way, you can stay alert and focused the whole time.
- Make studying a priority. When it's time to study, take it as seriously as you would take a job. Don't skip study sessions, start on time, and give the task 100% of your attention.
- Set specific study goals. Goals give direction to a study session and provide a sense of accomplishment when completed. Create goals that can realistically be completed in a single study session, such as: Learn the terms in chapter 1, pass the chapter 2 practice quiz, take notes on chapter 4, or review class notes for 30 minutes.
- Don't stop at reading–write down what you learn. By typing or hand-writing information, you will engage in active learning, which can improve retention and understanding. Try making flashcards, writing chapter summaries, or creating an outline of the material. As a bonus, you can refer back to what you've written to quickly review the material.
- Quiz yourself to make information "stick". Look for practice tests or discussion questions after each chapter you read. Another way to "quiz" yourself is to teach something you've studied to a friend, a pet, or even an inanimate object, without looking at the material.
- A change of scenery can improve information retention. If you're feeling unfocused, unmotivated, or just plain bored, try studying somewhere new. Libraries, parks and coffee shops are great alternatives for breaking out of your routine.
- Take care of your mind and body. Healthy sleep habits, exercise, and a balanced diet will boost memory and brain function. Studying is most effective when it's balanced with good habits.
Notes: Find Your Motivation - INCUP
Use INCUP to find your motivation:
- I - Interest
- Engaging in activities that are interesting or enjoyable provides the brain with a surge of dopamine. And more dopamine means more motivation.
- N - Novelty
- New experiences are naturally more alluring
- C - Challenge
- In order for people with ADHD to want to do something, they need stimulation and engagement. And you can make a task stimulating and engaging by making it challenging.
- U - Urgency
- You don't necessarily need external deadlines or pressure to spur you into action. Instead, you can hack your ADHD brain by artificially creating that same sense of urgency.
- P - Passion
- There are two primary types of motivation: extrinsic and intrinsic. Extrinsic motivation is tied to an external reward or benefit, while intrinsic motivation is driven by your own desires. In other words, you're not doing a task because you need to, but because you want to.
- To increase intrinsic motivation, there are three factors to consider:
- Autonomy: Having a choice allows us to feel free and independent.
- Competence: Being good at something offers a sense of accomplishment.
- Relatedness: Doing things that make us feel connected with other people provides a sense of purpose.
- Research studies have found that people with ADHD tend to score higher on extrinsic motivation and lower on intrinsic motivation. Basically, if a task isn't intrinsically motivating, ADHDers may need more frequent and immediate external rewards
Reference:
Core CBT Techniques
The basics forming the foundation of CBT (techniques can be used in tandem or individually):
Behavioural experiments Behavioural experiments are the cornerstone of CBT. These experiments are designed to test thinking and identify thought patterns that influence behaviour.
By intentionally 'trying out' specific ways of thinking and observing the outcome behaviours, clients gain a deeper awareness of the patterns of thinking that may be holding them back from reaching their goals.1
- Thought records Thought records are also designed to test the validity of our thoughts. Actually recording our thoughts provides a way for us to evaluate the evidence for or against a particular way of thinking – essentially, is it true or not true based on the situation? Thought records help the client to establish a more balanced way of thinking based on logic – what is as opposed to what they feel.1,2
- Behaviour activation (aka scheduling pleasant activities) This strategy is at once so simple yet so powerful. Pleasurable activities are among the first to go when people are faced with adversity. Intentionally taking part in activities that are enjoyable helps to reduce negative thinking and promotes more positive emotions and feelings of wellbeing. This technique is particularly helpful for clients with depression.3
Exposure Exposure is a powerful technique used to help clients face their fears or phobias in a controlled way. Basically, you're asking the client to be exposed to the very thing they fear. It will, of course, be scary for them.
When used properly, exposure has been proven to be effective in the reduction of fears and phobias. Exposure techniques are best utilized as part of a therapeutic intervention with a therapist who is well trained in their use.
There are many exposure techniques, and even more ways to implement them.4 Here are some of the more common and well known techniques.
Situation exposure hierarchies In this technique, the therapist helps the client make a list of feared objects or situations. The client then rates, on a scale of 0 to 10, how distressed they would be by each item. For example, a person who fears dogs might say "Not seeing a dog in the yard" is 0. "A dog licking my hand" might be their 10.
Starting with the least distressing, the therapist helps the client work through each situation in the list. This is a way of gradually increasing exposure and diminishing the distress of exposure.
- Flooding Flooding also uses exposure hierarchies, but generally begins with the more difficult or distressing scenarios or objects. Caution should be used when choosing this technique, as it can elicit strong responses. This technique is best utilized as part of a therapeutic intervention.
- Systematic desensitization This technique involves combining exposure with relaxation exercises. The client is taught strategies to remain relaxed in situations that would normally elicit fear. Gradually, they start to associate their feared object or situation with relaxation rather than powerful negative feelings.
- Journaling Journaling is a great way to gather information about thoughts and feelings. The journal can be used as a place to identify, describe, and evaluate moods, thoughts, scenarios, and responses. Having a place to 'unpack' and explore can lead to tremendous insight.
Cognitive restructuring – unravelling cognitive distortions Cognitive distortions are patterns of faulty thinking that convince us something is true when it is not. There are several types of cognitive distortions. To unravel them, the client must learn which are present for them and how to challenge those ways of thinking.
There are any number of worksheets on the Internet that can be used to help a client identify and challenge their distortions in thinking. This can also be accomplished through the therapist-client dialogue. The goal, of course, is to help the client learn to do this on their own.1
Here are five 'thought challenges' from the NHS Fife Department of Psychology's Negative Thinking CBT Tools. You can use these to get your client to take a closer look at their negative thought patterns.
- What are the chances…? The things you worry about may be very unlikely to happen. Would you be willing to put money on it happening?
- What is the worst thing…? The things you worry about might happen, but you're making way too much of them. Consider whether it would really be that bad if the worst did happen, and realize that it might not be worth all that anxiety.
- Am I right to think that…? You might be missing important information that would help you with decisions. As you gather more information, your worry and stress may abate.
- The five year rule ('the history game') This challenge has been applied to lots of situations within and outside of CBT to put events that have happened or will happen into perspective. Ask yourself, "Five years from now, will it really matter?"
- What is this worth? Consider just how important this thing you're worrying about is. Life is too short to be spent worrying about things that just don't deserve that kind of time investment.
- Functional assessment (ABCs) A functional assessment tool allows the client to record the ABCs (antecedents, behaviours, consequences) of a situation. This data allows the therapist and client to begin to identify patterns of behaviour.3 There are plenty of these forms on the Internet, but it's also super easy to design your own.
Reframing It's easy to fall into familiar patterns of negative thinking. One way to counteract negative thinking is through reframing. Reframing is the act of replacing negative thoughts with positive ones as soon as the negative thought occurs.
Reframing disrupts the negative cycle of perpetuation and resets the focus on something positive.1 This technique can be used both in sessions and as part of homework, using a thought record or similar tool.
- Homework Homework is an essential part of the CBT process. Homework assignments help clients learn new skills and integrate the concepts learned in sessions into daily life, improving treatment compliance and contributing to symptom reduction.1,3
Relaxation and mindfulness Three of my favourite relaxation and mindfulness practices are progressive muscle relaxation (PMR), meditation, and deep breathing. Each is a bit different in its implementation and intent.
- PMR involves the systematic tensing and releasing of each muscle group, combined with deep breathing and mental imagery.
- Mindfulness meditation involves clearing the mind and focusing on the sensations and thoughts in the moment, observing them and allowing them to pass.
- Deep breathing is an action that is physiologically incompatible with anxiety.
Relaxation and mindfulness techniques give the client a new and different way to respond to distressing situations. This change of response can break the cycle of perpetuation. Relaxation also helps the client to quiet their mind so that they can think more rationally and logically. YouTube videos, audio recordings, apps, and even relaxing music can all be good resources here.
- The SOLVED technique
This technique is used to teach the client problem-solving skills.3 While there are many variations on this technique (and lots of other names for it), structured problem solving is a critical skill for clients to learn. The acronym SOLVED gives the client a tangible, memorable tool for working through the problem-solving steps.
- S – Select a problem that the client wants to solve.
- O – Open your mind to all solutions – brainstorm all the options with your client.
- L – List the potential pros and cons of each potential solution.
- V – Verify the best solution – decide which choices are practical or desirable.
- E – Enact the plan.
- D – Decide if the plan worked.
- Role play Role play has a significant place in CBT. It can be used to help clients discover automatic thoughts, practise new responses, or modify core beliefs. Role play is also a useful tool for learning new social skills such as assertiveness.1
The 'pie' technique Based on the simple pie chart, the 'pie' technique lets clients see their goals and ideas in graph form. The 'pie' technique can help with things like setting goals and determining responsibility for outcomes.1
Simply have the client place each idea or goal into a pie chart, divided according to importance as they see fit. This process can be done as part of a homework assignment or as part of the ongoing therapist-client dialogue. Beck (2011) has several illustrations and examples of the use of this technique.1
Credit list technique This is a simple technique that can yield powerful results. Clients coming to therapy often lack confidence in their ability to change and may not immediately recognize the positive steps they are taking. The credit list is simply a daily list that the client makes of positive things he or she deserves credit for.
Not only does this technique help the client to recognize their progress, it also strengthens their ability to identify underlying positive beliefs and qualities when doing their core beliefs work in therapy.1
- Letting the story play out This technique is a sort of thought experiment. The therapist asks the client to imagine the outcome of their worst-case scenario, then encourages them to let the scene play out to its conclusion. Allowing the worrisome event to play out allows the client to see that even if their worst fear should come to pass, things can and do pass and get better.2
Reference:
Basic Principles of Cognitive Behavior Therapy edit
Read: - https://psychcentral.com/pro/the-basic-principles-of-cognitive-behavior-therapy The Basic Principles of Cognitive Behavior Therapy by Judith Beck, psychcentral.com December 13, 2011 Although therapy must be tailored to the individual, there are, nevertheless, certain principles that underlie cognitive behavior therapy for all patients. I will use a depressed patient, "Sally," to illustrate these central tenets and to demonstrate how to use cognitive theory to understand patients difficulties and how to use this understanding to plan treatment and conduct therapy sessions.
Sally was an 18-year-old single female when she sought treatment with me during her second semester of college. She had been feeling quite depressed and anxious for the previous 4 months and was having difficulty with her daily activities. She met criteria for a major depressive episode of moderate severity according to DSM-IV-TR (the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision; American Psychiatric Association, 2000). The basic principles of cognitive behavior therapy are as follows:
Principle No. 1: Cognitive behavior therapy is based on an ever-evolving formulation of patients problems and an individual conceptualization of each patient in cognitive terms. I consider Sallys difficulties in three timeframes. From the beginning, I identify her current thinking that contributesto her feelings of sadness (Im a failure, I cantdo anything right,Ill never be happy), and her problematic behaviors (isolating herself,spending a great deal of unproductive time in her room, avoiding askingfor help). These problematic behaviors both flow from and in turnreinforce Sallys dysfunctional thinking.
Second, I identify precipitatingfactors that influenced Sallys perceptions at the onset of her depression(e.g., being away from home for the first time and struggling in her studies contributed to her belief that she was incompetent).
Third, I hypothesize about key developmental events and her enduring patterns of interpreting these events that may have predisposed her to depression (e.g., Sally has had a lifelong tendency to attribute personal strengths and achievement to luck, but views her weaknesses as a reflection of her true self).
I base my conceptualization of Sally on the cognitive formulation of depression and on the data Sally provides at the evaluation session. I continue to refine this conceptualization at each session as I obtain more data. At strategic points, I share the conceptualization with Sally to ensure that it rings true to her. Moreover, throughout therapy I help Sally view her experience through the cognitive model. She learns, for example, to identify the thoughts associated with her distressing affect and to evaluate and formulate more adaptive responses to her thinking. Doing so improves how she feels and often leads to her behaving in a more functional way.
Principle No. 2: Cognitive behavior therapy requires a sound therapeutic alliance.Sally, like many patients with uncomplicated depression andanxiety disorders, has little difficulty trusting and working with me. Istrive to demonstrate all the basic ingredients necessary in a counselingsituation: warmth, empathy, caring, genuine regard, and competence.I show my regard for Sally by making empathic statements, listeningclosely and carefully, and accurately summarizing her thoughts andfeelings. I point out her small and larger successes and maintain a realisticallyoptimistic and upbeat outlook. I also ask Sally for feedback atthe end of each session to ensure that she feels understood and positiveabout the session.
Principle No. 3: Cognitive behavior therapy emphasizes collaboration and active participation.I encourage Sally to view therapy as teamwork;together we decide what to work on each session, how often we shouldmeet, and what Sally can do between sessions for therapy homework. Atfirst, I am more active in suggesting a direction for therapy sessions andin summarizing what wevediscussed during a session. As Sally becomesless depressed and more socialized into treatment, I encourage her tobecome increasingly active in the therapy session: deciding which problemsto talk about, identifying the distortions in her thinking, summarizingimportant points, and devising homework assignments.
Principle No. 4: Cognitive behavior therapy is goal oriented and problem focused. I ask Sally in our first session to enumerate her problems andset specific goals so both she and I have a shared understanding of whatshe is working toward. For example, Sally mentions in the evaluationsession that she feels isolated. With my guidance, Sally states a goal inbehavioral terms: to initiate new friendships and spend more time withcurrent friends. Later, when discussing how to improve her day-to-dayroutine, I help her evaluate and respond to thoughts that interfere withher goal, such as: My friends wontwant to hang out with me. Im too tired togo out with them. First, I help Sally evaluate the validity of her thoughtsthrough an examination of the evidence. Then Sally is willing to testthe thoughts more directly through behavioral experiments in which she initiates plans with friends. Once she recognizesand corrects the distortion in her thinking, Sally is able to benefit fromstraightforward problem solving to decrease her isolation.
Principle No. 5: Cognitive behavior therapy initially emphasizes the present.The treatment of most patients involves a strong focus on current problems and on specific situations that are distressing to them. Sally begins to feel better once she is able to respond to her negative thinking and take steps to improve her life. Therapy starts with an examination of here-and-now problems, regardless of diagnosis. Attention shifts to the past in two circumstances: One, when patients express a strong preference to do so, and a failure to do so could endanger the therapeutic alliance. Two, when patients get stuck in their dysfunctional thinking, and an understanding of the childhood roots of their beliefs can potentially help them modify their rigid ideas. (Well, no wonder you still believe youre incompetent. Can you see how almost any childwho had the same experiences as youwould grow up believing she was incompetent, and yet it might not be true, or certainly not completely true?)
For example, I briefly turn to the past midway through treatment to help Sally identify a set of beliefs she learned as a child: If I achieve highly, it means Im worthwhile, and If I dont achieve highly, it meansIm a failure. I help her evaluate the validity of these beliefs both in the past and present. Doing so leads Sally, in part, to develop more functional and more reasonable beliefs. If Sally had had a personality disorder, I would have spent proportionally more time discussing her developmental history and childhood origin of beliefs and coping behaviors.
Principle No. 6: Cognitive behavior therapy is educative, aims to teach the patient to be her own therapist, and emphasizes relapse prevention.Inour first session I educate Sally about the nature and course of her disorder,about the process of cognitive behavior therapy, and about thecognitive model (i.e., how her thoughts influence her emotions andbehavior). I not only help Sally set goals, identify and evaluate thoughtsand beliefs, and plan behavioral change, but I also teach her how todo so. At each session I ensure that Sally takes home therapy notesimportant ideas she has learnedso she can benefit from her newunderstanding in the ensuing weeks and after treatment ends.
Principle No. 7: Cognitive behavior therapy aims to be time limited.Many straightforward patients with depression and anxiety disorders are treated for six to 14 sessions. Therapists goals are to provide symptom relief, facilitate a remission of the disorder, help patients resolve their most pressing problems, and teach them skills to avoid relapse. Sally initially has weekly therapy sessions. (Had her depression been more severe or had she been suicidal, I may have arranged more frequent sessions.) After 2 months, we collaboratively decide to experiment with biweekly sessions, then with monthly sessions. Even after termination, we plan periodic booster sessions every 3 months for a year. Not all patients make enough progress in just a few months, however. Some patients require 1 or 2 years of therapy (or possibly longer) to modify very rigid dysfunctional beliefs and patterns of behavior that contribute to their chronic distress. Other patients with severe mental illness may need periodic treatment for a very long time to maintain stabilization.
Principle No. 8: Cognitive behavior therapy sessions are structured.No matter what the diagnosis or stage of treatment, following a certain structure in each session maximizes efficiency and effectiveness. This structure includes an introductory part (doing a mood check, briefly reviewing the week, collaboratively setting an agenda for the session), a middle part (reviewing homework, discussing problems on the agenda, setting new homework, summarizing), and a final part (eliciting feedback). Following this format makes the process of therapy more understandable to patients and increases the likelihood that they will be able to do self-therapy after termination.
Principle No. 9: Cognitive behavior therapy teaches patients to identify, evaluate, and respond to their dysfunctional thoughts and beliefs. Patientscan have many dozens or even hundreds of automatic thoughts a daythat affect their mood, behavior, or physiology (the last is especiallypertinent to anxiety). Therapists help patients identify key cognitionsand adopt more realistic, adaptive perspectives, which leadspatients to feel better emotionally, behave more functionally, ordecrease their physiological arousal. They do so through the processof guided discovery, using questioning (often labeled or mislabeled asSocratic questioning) to evaluate their thinking (rather than persuasion,debate, or lecturing). Therapists also create experiences, calledbehavioral experiments, for patients to directly test their thinking (e.g.,If I even look at a picture of a spider, Ill get so anxious I wontbe ableto think). In these ways, therapists engage in collaborative empiricism.Therapists do not generally know in advance to what degree a patientsautomatic thought is valid or invalid, but together they test the patientsthinking to develop more helpful and accurate responses.
When Sally was quite depressed, she had many automatic thoughts throughout the day, some of which she spontaneously reported and others that I elicited (by asking her what was going through her mind when she felt upset or acted in a dysfunctional manner). We often uncovered important automatic thoughts as we were discussing one of Sallys specific problems, and together we investigated their validity and utility. I asked her to summarize her new viewpoints, and we recorded them in writing so that she could read these adaptive responses throughout the week to prepare her for these or similar automatic thoughts. I did not encourage her to uncritically adopt a more positive viewpoint, challenge the validity of her automatic thoughts, or try to convince her that her thinking was unrealistically pessimistic. Instead we engaged in a collaborative exploration of the evidence.
Principle No. 10: Cognitive behavior therapy uses a variety of techniques to change thinking, mood, and behavior.Although cognitive strategies such as Socratic questioning and guided discovery are central to cognitive behavior therapy, behavioral and problem-solving techniques are essential, as are techniques from other orientations that are implemented within a cognitive framework. For example, I used Gestalt-inspired techniques to help Sally understand how experiences with her family contributed to the development of her belief that she was incompetent. I use psychodynamically inspired techniques with some Axis II patients who apply their distorted ideas about people to the therapeutic relationship. The types of techniques you select will be influenced by your conceptualization of the patient, the problem you are discussing, and your objectives for the session.
These basic principles apply to all patients. Therapy does, however, vary considerably according to individual patients, the nature of their difficulties, and their stage of life, as well as their developmental and intellectual level, gender, and cultural background. Treatment also varies depending on patients goals, their ability to form a strong therapeutic bond, their motivation to change, their previous experience with therapy, and their preferences for treatment, among other factors. The emphasis in treatment also depends on the patients particular disorder(s). Cognitive behavior therapy for panic disorder involves testing the patients catastrophic misinterpretations (usually life- or sanity-threatening erroneous predictions) of bodily or mental sensations[1]. Anorexia requires a modification of beliefs about personal worth and control[2]. Substance abuse treatment focuses on negative beliefs about the self and facilitating or permission-granting beliefs about substance use[3].
Excerpted from Cognitive Behavior Therapy, Second Edition: Basics and Beyond by Judith S. Beck. Copyright 2011 The Guilford Press. http://www.guilford.com
[1] Clark, 1989 [2] Garner & Bemis, 1985
[3] Beck, Wright, Newman, & Liese, 1993
Reference:
CBT Techniques: 25 Cognitive Behavioral Therapy Worksheets edit
CBT Techniques: 25 Cognitive Behavioral Therapy Worksheets by Courtney E. Ackerman, MA., positivepsychology.com March 20, 2017 09:02 AM
Read here: https://positivepsychology.com/cbt-cognitive-behavioral-therapy-techniques-worksheets
Even if you're relatively unfamiliar with psychology, chances are you've heard of cognitive-behavioral therapy, commonly known as CBT. It's an extremely common type of talk therapy practiced around the world.
If you've ever interacted with a mental health therapist, a counselor, or a psychiatry clinician in a professional setting, it's likely you've participated in CBT.
If you've ever heard friends or loved ones talk about how a mental health professional helped them identify unhelpful thoughts and patterns and behavior and alter them to more effectively work towards their goals, you've heard about the impacts of CBT.
CBT is one of the most frequently used tools in the psychologist's toolbox. Though it's based on simple principles, it can have wildly positive outcomes when put into practice.
In this article, we'll explore what CBT is, how it works, and how you can apply its principles to improve your own life or the lives of your clients.
Before you read on, we thought you might like to download our 3 Positive CBT Exercises for free. These science-based exercises will provide you with a comprehensive insight into Positive CBT and will give you the tools to apply it in your therapy or coaching.
What is CBT? "This simple idea is that our unique patterns of thinking, feeling, and behaving are significant factors in our experiences, both good and bad. Since these patterns have such a significant impact on our experiences, it follows that altering these patterns can change our experiences" (Martin, 2016).
Cognitive-behavioral therapy aims to change our thought patterns, our conscious and unconscious beliefs, our attitudes, and, ultimately, our behavior, in order to help us face difficulties and achieve our goals.
Psychiatrist Aaron Beck was the first to practice cognitive behavioral therapy. Like most mental health professionals at the time, Beck was a psychoanalysis practitioner.
While practicing psychoanalysis, Beck noticed the prevalence of internal dialogue in his clients and realized how strong the link between thoughts and feelings can be. He altered the therapy he practiced in order to help his clients identify, understand, and deal with the automatic, emotion-filled thoughts that regularly arose in his clients.
Beck found that a combination of cognitive therapy and behavioral techniques produced the best results for his clients. In describing and honing this new therapy, Beck laid the foundations of the most popular and influential form of therapy of the last 50 years.
This form of therapy is not designed for lifelong participation and aims to help clients meet their goals in the near future. Most CBT treatment regimens last from five to ten months, with clients participating in one 50- to 60-minute session per week.
CBT is a hands-on approach that requires both the therapist and the client to be invested in the process and willing to actively participate. The therapist and client work together as a team to identify the problems the client is facing, come up with strategies for addressing them, and creating positive solutions (Martin, 2016).
- Cognitive Distortions
Many of the most popular and effective cognitive-behavioral therapy techniques are applied to what psychologists call "cognitive distortions," inaccurate thoughts that reinforce negative thought patterns or emotions (Grohol, 2016).
There are 15 main cognitive distortions that can plague even the most balanced thinkers.
- Filtering Filtering refers to the way a person can ignore all of the positive and good things in life to focus solely on the negative. It's the trap of dwelling on a single negative aspect of a situation, even when surrounded by an abundance of good things.
Polarized thinking / Black-and-white thinking This cognitive distortion is all-or-nothing thinking, with no room for complexity or nuance—everything's either black or white, never shades of gray.
If you don't perform perfectly in some area, then you may see yourself as a total failure instead of simply recognizing that you may be unskilled in one area.
Overgeneralization Overgeneralization is taking a single incident or point in time and using it as the sole piece of evidence for a broad conclusion.
For example, someone who overgeneralizes could bomb an important job interview and instead of brushing it off as one bad experience and trying again, they conclude that they are terrible at interviewing and will never get a job offer.
Jumping to conclusions Similar to overgeneralization, this distortion involves faulty reasoning in how one makes conclusions. Unlike overgeneralizing one incident, jumping to conclusions refers to the tendency to be sure of something without any evidence at all.
For example, we might be convinced that someone dislikes us without having any real evidence, or we might believe that our fears will come true before we have a chance to really find out.
Catastrophizing / Magnifying or Minimizing This distortion involves expecting that the worst will happen or has happened, based on an incident that is nowhere near as catastrophic as it is made out to be. For example, you may make a small mistake at work and be convinced that it will ruin the project you are working on, that your boss will be furious, and that you'll lose your job.
Alternatively, one might minimize the importance of positive things, such as an accomplishment at work or a desirable personal characteristic.
Personalization This is a distortion where an individual believes that everything they do has an impact on external events or other people, no matter how irrational that may be. A person with this distortion will feel that he or she has an exaggerated role in the bad things that happen around them.
For instance, a person may believe that arriving a few minutes late to a meeting led to it being derailed and that everything would have been fine if they were on time.
Control fallacies This distortion involves feeling like everything that happens to you is either a result of purely external forces or entirely due to your own actions. Sometimes what happens to us is due to forces we can't control, and sometimes what it's due to our own actions, but the distortion is assuming that it is always one or the other.
We might assume that difficult coworkers are to blame for our own less-than-stellar work, or alternatively assume that every mistake another person makes is because of something we did.
Fallacy of fairness We are often concerned about fairness, but this concern can be taken to extremes. As we all know, life is not always fair. The person who goes through life looking for fairness in all their experiences will end up resentful and unhappy.
Sometimes things will go our way, and sometimes they will not, regardless of how fair it may seem.
Blaming When things don't go our way, there are many ways we can explain or assign responsibility for the outcome. One method of assigning responsibility is blaming others for what goes wrong.
Sometimes we may blame others for making us feel or act a certain way, but this is a cognitive distortion. Only you are responsible for the way you feel or act.
"Shoulds" "Shoulds" refer to the implicit or explicit rules we have about how we and others should behave. When others break our rules, we are upset. When we break our own rules, we feel guilty. For example, we may have an unofficial rule that customer service representatives should always be accommodating to the customer.
When we interact with a customer service representative that is not immediately accommodating, we might get angry. If we have an implicit rule that we are irresponsible if we spend money on unnecessary things, we may feel exceedingly guilty when we spend even a small amount of money on something we don't need.
Emotional reasoning This distortion involves thinking that if we feel a certain way, it must be true. For example, if we feel unattractive or uninteresting in the current moment, we think we are unattractive or uninteresting. This cognitive distortion boils down to:
"I feel it, therefore it must be true."
Clearly, our emotions are not always indicative of the objective truth, but it can be difficult to look past how we feel.
Fallacy of change The fallacy of change lies in expecting other people to change as it suits us. This ties into the feeling that our happiness depends on other people, and their unwillingness or inability to change, even if we demand it, keeps us from being happy.
This is a damaging way to think because no one is responsible for our own happiness except ourselves.
Global labeling / mislabeling This cognitive distortion is an extreme form of generalizing, in which we generalize one or two instances or qualities into a global judgment. For example, if we fail at a specific task, we may conclude that we are a total failure in not only that area but all areas.
Alternatively, when a stranger says something a bit rude, we may conclude that he or she is an unfriendly person in general. Mislabeling is specific to using exaggerated and emotionally loaded language, such as saying a woman has abandoned her children when she leaves her children with a babysitter to enjoy a night out.
Always being right While we all enjoy being right, this distortion makes us think we must be right, that being wrong is unacceptable.
We may believe that being right is more important than the feelings of others, being able to admit when we've made a mistake or being fair and objective.
- Heaven's Reward Fallacy This distortion involves expecting that any sacrifice or self-denial will pay off. We may consider this karma, and expect that karma will always immediately reward us for our good deeds. This results in feelings of bitterness when we do not receive our reward (Grohol, 2016).
Many tools and techniques found in cognitive behavioral therapy are intended to address or reverse these cognitive distortions.
- 9 Essential CBT Techniques and Tools
There are many tools and techniques used in cognitive behavioral therapy, many of which can be used in both a therapy context and in everyday life. The nine techniques and tools listed below are some of the most common and effective CBT practices.
Journaling This technique is a way to gather about one's moods and thoughts. A CBT journal can include the time of the mood or thought, the source of it, the extent or intensity, and how we reacted, among other factors.
This technique can help us to identify our thought patterns and emotional tendencies, describe them, and change, adapt, or cope with them (Utley & Garza, 2011).
Follow the link to find out more about using a thought diary for journaling.
Unraveling cognitive distortions This is a primary goal of CBT and can be practiced with or without the help of a therapist. In order to unravel cognitive distortions, you must first become aware of the distortions from which you commonly suffer (Hamamci, 2002).
Part of this involves identifying and challenging harmful automatic thoughts, which frequently fall into one of the 15 categories listed earlier.
Cognitive restructuring Once you identify the distortions you hold, you can begin to explore how those distortions took root and why you came to believe them. When you discover a belief that is destructive or harmful, you can begin to challenge it (Larsson, Hooper, Osborne, Bennett, & McHugh, 2015).
For example, if you believe that you must have a high-paying job to be a respectable person, but you're then laid off from your high-paying job, you will begin to feel bad about yourself.
Instead of accepting this faulty belief that leads you to think negative thoughts about yourself, with cognitive restructuring you could take an opportunity to think about what really makes a person "respectable," a belief you may not have explicitly considered before.
Exposure and response prevention This technique is specifically effective for those who suffer from obsessive-compulsive disorder (OCD; Abramowitz, 1996). You can practice this technique by exposing yourself to whatever it is that normally elicits a compulsive behavior, but doing your best to refrain from the behavior.
You can combine journaling with this technique, or use journaling to understand how this technique makes you feel.
Interoceptive exposure Interoceptive Exposure is intended to treat panic and anxiety. It involves exposure to feared bodily sensations in order to elicit the response (Arntz, 2002). Doing so activates any unhelpful beliefs associated with the sensations, maintains the sensations without distraction or avoidance, and allows new learning about the sensations to take place.
It is intended to help the sufferer see that symptoms of panic are not dangerous, although they may be uncomfortable.
Nightmare exposure and rescripting Nightmare exposure and rescripting are intended specifically for those suffering from nightmares. This technique is similar to interoceptive exposure, in that the nightmare is elicited, which brings up the relevant emotion (Pruiksma, Cranston, Rhudy, Micol, & Davis, 2018).
Once the emotion has arisen, the client and therapist work together to identify the desired emotion and develop a new image to accompany the desired emotion.
Play the script until the end This technique is especially useful for those suffering from fear and anxiety. In this technique, the individual who is vulnerable to crippling fear or anxiety conducts a sort of thought experiment in which they imagine the outcome of the worst-case scenario.
Letting this scenario play out can help the individual to recognize that even if everything he or she fears comes to pass, the outcome will still be manageable (Chankapa, 2018).
Progressive muscle relaxation This is a familiar technique to those who practice mindfulness. Similar to the body scan, progressive muscle relaxation instructs you to relax one muscle group at a time until your whole body is in a state of relaxation (McCallie, Blum, & Hood, 2006).
You can use audio guidance, a YouTube video, or simply your own mind to practice this technique, and it can be especially helpful for calming nerves and soothing a busy and unfocused mind.
Relaxed breathing This is another technique that will be familiar to practitioners of mindfulness. There are many ways to relax and bring regularity to your breath, including guided and unguided imagery, audio recordings, YouTube videos, and scripts. Bringing regularity and calm to your breath will allow you to approach your problems from a place of balance, facilitating more effective and rational decisions (Megan, 2016).
These techniques can help those suffering from a range of mental illnesses and afflictions, including anxiety, depression, OCD, and panic disorder, and they can be practiced with or without the guidance of a therapist. To try some of these techniques without the help of a therapist, see the next section for worksheets and handouts to assist with your practice.
- Cognitive-Behavioral Therapy Worksheets (PDFs) To Print and Use
If you're a therapist looking for ways to guide your client through treatment or a hands-on person who loves to learn by doing, there are many cognitive-behavioral therapy worksheets that can help.
Coping styles worksheet This PDF Coping Styles Formulation Worksheet instructs you or your client to first list any current perceived problems or difficulties – "The Problem". You or your client will work backward to list risk factors above (i.e., why you are more likely to experience these problems than someone else) and triggers or events (i.e., the stimulus or source of these problems).
Once you have defined the problems and understand why you are struggling with them, you then list coping strategies. These are not solutions to your problems, but ways to deal with the effects of those problems that can have a temporary impact. Next, you list the effectiveness of the coping strategies, such as how they make you feel in the short- and long-term, and the advantages and disadvantages of each strategy.
Finally, you move on to listing alternative actions. If your coping strategies are not totally effective against the problems and difficulties that are happening, you are instructed to list other strategies that may work better.
This worksheet gets you (or your client) thinking about what you are doing now and whether it is the best way forward.
ABC functional analysis One popular technique in CBT is ABC functional analysis. Functional analysis helps you (or the client) learn about yourself, specifically, what leads to specific behaviors and what consequences result from those behaviors.
In the middle of the worksheet is a box labeled "Behaviors." In this box, you write down any potentially problematic behaviors you want to analyze.
On the left side of the worksheet is a box labeled "Antecedents," in which you or the client write down the factors that preceded a particular behavior. These are factors that led up to the behavior under consideration, either directly or indirectly.
On the right side is the final box, labeled "Consequences." This is where you write down what happened as a result of the behavior under consideration. "Consequences" may sound inherently negative, but that's not necessarily the case; some positive consequences can arise from many types of behaviors, even if the same behavior also leads to negative consequences.
This ABC Functional Analysis Worksheet can help you or your client to find out whether particular behaviors are adaptive and helpful in striving toward your goals, or destructive and self-defeating.
Case formulation worksheet In CBT, there are 4 "P's" in Case Formulation:
- Predisposing factors;
- Precipitating factors;
- Perpetuating factors; and
- Protective factors
They help us understand what might be leading a perceived problem to arise, and what might prevent them from being tackled effectively.
In this worksheet, a therapist will work with their client through 4 steps.
First, they identify predisposing factors, which are those external or internal and can add to the likelihood of someone developing a perceived problem ("The Problem"). Examples might include genetics, life events, or their temperament.
Together, they collaborate to identify precipitating factors, which provide insight into precise events or triggers that lead to "The Problem" presenting itself. Then they consider perpetuating factors, to discover what reinforcers may be maintaining the current problem.
Last, they identify protective factors, to understand the client's strengths, social supports, and adaptive behavioral patterns.
Download this Case Formulation Worksheet as a PDF here.
Extended case formulation worksheet This worksheet builds on the last. It helps you or your client address the "Four P Factors" described just above—predisposing, precipitating, perpetuating, and protective factors. This formulation process can help you or your client connect the dots between core beliefs, thought patterns, and present behavior.
This worksheet presents six boxes on the left of the page (Part A), which should be completed before moving on to the right-hand side of the worksheet (Part B).
The first box is labeled "The Problem," and corresponds with the perceived difficulty that your client is experiencing. In this box, you are instructed to write down the events or stimuli that are linked to a certain behavior. The next box is labeled "Early Experiences" and corresponds to the predisposing factor. This is where you list the experiences that you had early in life that may have contributed to the behavior. The third box is "Core Beliefs," which is also related to the predisposing factor. This is where you write down some relevant core beliefs you have regarding this behavior. These are beliefs that may not be explicit, but that you believe deep down, such as "I'm bad" or "I'm not good enough." The fourth box is "Conditional assumptions/rules/attitudes," which is where you list the rules that you adhere to, whether consciously or subconsciously. These implicit or explicit rules can perpetuate the behavior, even if it is not helpful or adaptive. Rules are if-then statements that provide a judgment based on a set of circumstances. For instance, you may have the rule "If I do not do something perfectly, I'm a complete failure." The fifth box is labeled "Maladaptive Coping Strategies" This is where you write down how well these rules are working for you (or not). Are they helping you to be the best you can be? Are they helping you to effectively strive towards your goals? Finally, the last box us titled "Positives." This is where you list the factors that can help you deal with the problematic behavior or thought, and perhaps help you break the perpetuating cycle. These can be things that help you cope once the thought or behavior arises or things that can disrupt the pattern once it is in motion. On the right, there is a flow chart that you can fill out based on how these behaviors and feelings are perpetuated. You are instructed to think of a situation that produces a negative automatic thought and record the emotion and behavior that this thought provokes, as well as the bodily sensations that can result. Filling out this flow chart can help you see what drives your behavior or thought and what results from it.
Download our PDF Extended Case Formulation Worksheet.
Dysfunctional thought record This worksheet is especially helpful for people who struggle with negative thoughts and need to figure out when and why those thoughts are most likely to pop up. Learning more about what provokes certain automatic thoughts makes them easier to address and reverse.
The worksheet is divided into seven columns:
On the far left, there is space to write down the date and time a dysfunctional thought arose. The second column is where the situation is listed. The user is instructed to describe the event that led up to the dysfunctional thought in detail. The third column is for the automatic thought. This is where the dysfunctional automatic thought is recorded, along with a rating of belief in the thought on a scale from 0% to 100%. The next column is where the emotion or emotions elicited by this thought are listed, also with a rating of intensity on a scale from 0% to 100%. Use this fifth column to note the dysfunctional thought that will be addressed. Example maladaptive thoughts include distortions such as over-inflating the negative while dismissing the positive of a situation, or overgeneralizing. The second-to-last column is for the user to write down alternative thoughts that are more positive and functional to replace the negative one. Finally, the last column is for the user to write down the outcome of this exercise. Were you able to confront the dysfunctional thought? Did you write down a convincing alternative thought? Did your belief in the thought and/or the intensity of your emotion(s) decrease? Download this Dysfunctional Thought Record as a PDF.
Fact-checking One of my favorite CBT tools is this Fact Checking Thoughts Worksheet because it can be extremely helpful in recognizing that your thoughts are not necessarily true.
At the top of this worksheet is an important lesson:
Thoughts are not facts.
Of course, it can be hard to accept this, especially when we are in the throes of a dysfunctional thought or intense emotion. Filling out this worksheet can help you come to this realization.
The worksheet includes 16 statements that the user must decide are either fact or opinion. These statements include:
I'm a bad person. I failed the test. I'm selfish. I didn't lend my friend money when they asked. This is not a trick—there is a right answer for each of these statements. (In case you're wondering, the correct answers for the statements above are as follows: opinion, fact, opinion, fact.)
This simple exercise can help the user to see that while we have lots of emotionally charged thoughts, they are not all objective truths. Recognizing the difference between fact and opinion can assist us in challenging the dysfunctional or harmful opinions we have about ourselves and others.
Cognitive restructuring This worksheet employs the use of Socratic questioning, a technique that can help the user to challenge irrational or illogical thoughts.
The first page of the worksheet has a thought bubble for "What I'm Thinking". You or your client can use this space to write down a specific thought, usually, one you suspect is destructive or irrational.
Next, you write down the facts supporting and contradicting this thought as a reality. What facts about this thought being accurate? What facts call it into question? Once you have identified the evidence, you can use the last box to make a judgment on this thought, specifically whether it is based on evidence or simply your opinion.
The next page is a mind map of Socratic Questions which can be used to further challenge the thought. You may wish to re-write "What I'm Thinking" in the center so it is easier to challenge the thought against these questions.
One question asks whether this thought is truly a black-and-white situation, or whether reality leaves room for shades of gray. This is where you think about (and write down) whether you are using all-or-nothing thinking, for example, or making things unreasonably simple when they are complex. Another asks whether you could be misinterpreting the evidence or making any unverified assumptions. As with all the other bubbles, writing it down will make this exercise more effective. A third bubble instructs you to think about whether other people might have different interpretations of the same situation, and what those interpretations might be. Next, ask yourself whether you are looking at all the relevant evidence or just the evidence that backs up the belief you already hold. Try to be as objective as possible. It also helps to ask yourself whether your thought may an over-inflation of a truth. Some negative thoughts are based in truth but extend past their logical boundaries. You're also instructed to consider whether you are entertaining this negative thought out of habit or because the facts truly support it. Then, think about how this thought came to you. Was it passed on from someone else? If so, is that person a reliable source of truth? Finally, you complete the worksheet by identifying how likely the scenario your thought brings up actually is, and whether it is the worst-case scenario. These Socratic questions encourage a deep dive into the thoughts that plague you and offer opportunities to analyze and evaluate those thoughts. If you are having thoughts that do not come from a place of truth, this Cognitive Restructuring Worksheet can be an excellent tool for identifying and defusing them.
- Some More CBT Interventions and Exercises
Haven't had enough CBT tools and techniques yet? Read on for additional useful and effective exercises.
Behavioral experiments These are related to thought experiments, in that you engage in a "what if" consideration. Behavioral experiments differ from thought experiments in that you actually test out these "what ifs" outside of your thoughts (Boyes, 2012).
In order to test a thought, you can experiment with the outcomes that different thoughts produce. For example, you can test the thoughts:
"If I criticize myself, I will be motivated to work harder" versus "If I am kind to myself, I will be motivated to work harder."
First, you would try criticizing yourself when you need the motivation to work harder and record the results. Then you would try being kind to yourself and recording the results. Next, you would compare the results to see which thought was closer to the truth.
These Behavioral Experiments to Test Beliefs can help you learn how to achieve your therapeutic goals and how to be your best self.
Thought records Thought records are useful in testing the validity of your thoughts (Boyes, 2012). They involve gathering and evaluating evidence for and against a particular thought, allowing for an evidence-based conclusion on whether the thought is valid or not.
For example, you may have the belief "My friend thinks I'm a bad friend." You would think of all the evidence for this belief, such as "She didn't answer the phone the last time I called," or "She canceled our plans at the last minute," and evidence against this belief, like "She called me back after not answering the phone," and "She invited me to her barbecue next week. If she thought I was a bad friend, she probably wouldn't have invited me."
Once you have evidence for and against, the goal is to come up with more balanced thoughts, such as, "My friend is busy and has other friends, so she can't always answer the phone when I call. If I am understanding of this, I will truly be a good friend."
Thought records apply the use of logic to ward off unreasonable negative thoughts and replace them with more balanced, rational thoughts (Boyes, 2012).
Here's a helpful Thought Record Worksheet to download.
Pleasant activity scheduling This technique can be especially helpful for dealing with depression (Boyes, 2012). It involves scheduling activities in the near future that you can look forward to.
For example, you may write down one activity per day that you will engage in over the next week. This can be as simple as watching a movie you are excited to see or calling a friend to chat. It can be anything that is pleasant for you, as long as it is not unhealthy (i.e., eating a whole cake in one sitting or smoking).
You can also try scheduling an activity for each day that provides you with a sense of mastery or accomplishment (Boyes, 2012). It's great to do something pleasant, but doing something small that can make you feel accomplished may have more long-lasting and far-reaching effects.
This simple technique can introduce more positivity into your life, and our Pleasant Activity Scheduling Worksheet is designed to help.
Imagery-based exposure This exercise involves thinking about a recent memory that produced strong negative emotions and analyzing the situation.
For example, if you recently had a fight with your significant other and they said something hurtful, you can bring that situation to mind and try to remember it in detail. Next, you would try to label the emotions and thoughts you experienced during the situation and identify the urges you felt (e.g., to run away, to yell at your significant other, or to cry).
Visualizing this negative situation, especially for a prolonged period of time, can help you to take away its ability to trigger you and reduce avoidance coping (Boyes, 2012). When you expose yourself to all of the feelings and urges you felt in the situation and survive experiencing the memory, it takes some of its power away.
This Imagery Based Exposure Worksheet is a useful resource for this exercise.
Graded exposure worksheet This technique may sound complicated, but it's relatively simple.
Making a situation exposure hierarchy involves means listing situations that you would normally avoid (Boyes, 2012). For example, someone with severe social anxiety may typically avoid making a phone call or asking someone on a date.
Next, you rate each item on how distressed you think you would be, on a scale from 0 to 10, if you engaged in it. For the person suffering from severe social anxiety, asking someone on a date may be rated a 10 on the scale, while making a phone call might be rated closer to a 3 or 4.
Once you have rated the situations, you rank them according to their distress rating. This will help you recognize the biggest difficulties you face, which can help you decide which items to address and in what order. It's often advised to start with the least distressing items and work your way up to the most distressing items.
Download our Graded Exposure Worksheet here.
A CBT Manual and Workbook for Your Own Practice and for Your Client If you're interested in giving CBT a try with your clients, there are many books and manuals that can help get you started. Some of these books are for the therapist only, and some are to be navigated as a team or with guidance from the therapist.
There are many manuals out there for helping therapists apply cognitive behavioral therapy in their work, but these are some of the most popular:
A Therapist's Guide to Brief Cognitive Behavioral Therapy by Jeffrey A. Cully and Andra L. Teten (PDF here); Individual Therapy Manual for Cognitive-Behavioral Treatment of Depression by Ricardo F. Munoz and Jeanne Miranda (PDF here); Provider's Guidebook: "Activities and Your Mood" by Community Partners in Care (PDF here); Treatment Manual for Cognitive Behavioral Therapy for Depression by Jeannette Rosselló, Guillermo Bernal, and the Institute for Psychological Research (PDF here). Here are some of the most popular workbooks and manuals for clients to use alone or with a therapist:
The CBT Toolbox: A Workbook for Clients and Clinicians by Jeff Riggenbach (Amazon); Client's Guidebook: "Activities and Your Mood" by Community Partners in Care (PDF here); The Cognitive Behavioral Workbook for Anxiety: A Step-by-Step Program by William J. Knaus and Jon Carlson (Amazon); The Cognitive Behavioral Workbook for Depression: A Step-by-Step Program by William J. Knaus and Albert Ellis (Amazon); Cognitive-Behavioral Therapy Skills Workbook by Barry Gregory (Amazon); A Course in CBT Techniques: A Free Online CBT Workbook by Albert Bonfil and Suraji Wagage (online here). There are many other manuals and workbooks available that can help get you started with CBT, but the tools above are a good start. Peruse our article: 30 Best CBT Books to Master Cognitive Behavioral Therapy for an excellent list of these books.
5 Final Cognitive Behavioral Activities
- Before we go, there are a few more CBT activities and exercises that may be helpful for you or your clients that we'd like to cover.
Mindfulness meditation Mindfulness can have a wide range of positive impacts, including helping with depression, anxiety, addiction, and many other mental illnesses or difficulties.
The practice can help those suffering from harmful automatic thoughts to disengage from rumination and obsession by helping them stay firmly grounded in the present (Jain et al., 2007).
Mindfulness meditations, in particular, can function as helpful tools for your clients in between therapy sessions, such as to help ground them in the present moment during times of stress.
If you are a therapist who uses mindfulness-based approaches, consider finding or pre-recording some short mindfulness meditation exercises for your clients.
You might then share these with your clients as part of a toolkit they can draw on at their convenience, such as using the blended care platform Quenza (pictured here), which allows clients to access meditations or other psychoeducational activities on-the-go via their portable devices.
Successive approximation This is a fancy name for a simple idea that you have likely already heard of: breaking up large tasks into small steps.
It can be overwhelming to be faced with a huge goal, like opening a business or remodeling a house. This is true in mental health treatment as well, since the goal to overcome depression or anxiety and achieve mental wellness can seem like a monumental task.
By breaking the large goal into small, easy-to-accomplish steps, we can map out the path to success and make the journey seem a little less overwhelming (e.g., Emmelkamp & Ultee, 1974).
Writing self-statements to counteract negative thoughts This technique can be difficult for someone who's new to CBT treatment or suffering from severe symptoms, but it can also be extremely effective (Anderson, 2014).
When you (or your client) are being plagued by negative thoughts, it can be hard to confront them, especially if your belief in these thoughts is strong. To counteract these negative thoughts, it can be helpful to write down a positive, opposite thought.
For example, if the thought "I am worthless" keeps popping into your head, try writing down a statement like "I am a person with worth," or "I am a person with potential." In the beginning, it can be difficult to accept these replacement thoughts, but the more you bring out these positive thoughts to counteract the negative ones, the stronger the association will be.
Visualize the best parts of your day When you are feeling depressed or negative, it is difficult to recognize that there are positive aspects of life. This simple technique of bringing to mind the good parts of your day can be a small step in the direction of recognizing the positive (Anderson, 2014).
All you need to do is write down the things in your life that you are thankful for or the most positive events that happen in a given day. The simple act of writing down these good things can forge new associations in your brain that make it easier to see the positive, even when you are experiencing negative emotions.
Reframe your negative thoughts It can be easy to succumb to negative thoughts as a default setting. If you find yourself immediately thinking a negative thought when you see something new, such as entering an unfamiliar room and thinking "I hate the color of that wall," give reframing a try (Anderson, 2014).
Reframing involves countering the negative thought(s) by noticing things you feel positive about as quickly as possible. For instance, in the example where you immediately think of how much you hate the color of that wall, you would push yourself to notice five things in the room that you feel positively about (e.g., the carpet looks comfortable, the lampshade is pretty, the windows let in a lot of sunshine).
You can set your phone to remind you throughout the day to stop what you are doing and think of the positive things around you. This can help you to push your thoughts back into the realm of the positive instead of the negative.
- A Take-Home Message
In this post, we offered many techniques, tools, and resources that can be effective in the battle against depression, anxiety, OCD, and a host of other problems or difficulties.
However, as is the case with many treatments, they depend on you (or your client) putting in a lot of effort. We encourage you to give these techniques a real try and allow yourself the luxury of thinking that they could actually work.
When we approach a potential solution with the assumption that it will not work, that assumption often becomes a self-fulfilling prophecy. When we approach a potential solution with an open mind and the belief that it just might work, it has a much better chance of succeeding.
So if you are struggling with negative automatic thoughts, please consider these tips and techniques and give them a shot. Likewise, if your client is struggling, encourage them to make the effort, because the payoff can be better than they can imagine.
If you are struggling with severe symptoms of depression or suicidal thoughts, please call the following number in your respective country:
USA: National Suicide Prevention Hotline at 988; UK: Samaritans hotline at 116 123; The Netherlands: Netherlands Suicide Hotline at 09000767; France: Suicide écoute at 01 45 39 40 00; Germany: Telefonseelsorge at 0800 111 0 111 for Protestants, 0800 111 0 222 for Catholics, and 0800 111 0 333 for children and youth. For a list of other suicide prevention websites, phone numbers, and resources, see this website.
Please know that there are people out there who care and that there are treatments that can help.
Please let us know about your experiences with CBT in the comments section. If you've tried it, how did it work for you? Are there any other helpful exercises or techniques that we did not touch on in this piece? We'd love to know your thoughts.
We hope you enjoyed this article. For more information, don't forget to download our 3 Positive CBT Exercises for free.
Reference:
CBT Tools edit
CBT (Cognitive Behavioral Therapy) tools like STOPP and 3-2-1 Grounding are practical techniques designed to help individuals manage overwhelming emotions, reduce anxiety, or interrupt unhelpful thought patterns. They’re rooted in CBT principles, which focus on changing negative thoughts and behaviors to improve emotional well-being. Here’s a breakdown of each: ### STOPP STOPP is an acronym that stands for a structured, step-by-step process to pause and regain control when you’re caught in a spiral of negative thinking or emotional distress. It’s commonly used to manage automatic reactions and encourage more rational responses. The steps are: - **S – Stop**: Pause what you’re doing or thinking. Don’t react immediately. - **T – Take a Breath**: Slow down with a few deep breaths to calm your mind and body. - **O – Observe**: Notice what’s happening. What are you thinking? Feeling? What’s triggering this? - **P – Pull Back**: Get some perspective. Ask yourself: Is this thought a fact or an opinion? What would I tell a friend in this situation? - **P – Practice What Works**: Decide on a constructive next step. What’s the best thing to do right now for yourself or the situation? It’s like hitting the brakes on a runaway train of thoughts—giving you space to respond rather than react. Therapists often teach this to help people with anxiety, anger, or impulsive behaviors. ### 3-2-1 Grounding The 3-2-1 Grounding technique is a sensory-based exercise to bring you back to the present moment, often used for anxiety, panic attacks, or dissociation. It anchors you by focusing on your immediate surroundings through your senses. Here’s how it works: - **3 – Name 3 things you can see**: Look around and identify three specific things (e.g., a blue mug, a tree outside, your shoe). - **2 – Name 2 things you can hear**: Tune in to sounds (e.g., a car passing, your own breathing). - **1 – Name 1 thing you can feel**: Focus on a physical sensation (e.g., the chair beneath you, the texture of your clothes). You can repeat or adjust it as needed. The idea is to shift your attention away from racing thoughts or flashbacks and into the here-and-now, using your senses as an anchor. Both tools are simple, portable, and don’t require anything but your attention. STOPP is more cognitive—tackling thought patterns—while 3-2-1 is sensory, pulling you out of your head and into your environment. They’re often taught together in CBT to give people a toolkit for emotional regulation. Want more examples of how to use them in real situations? In addition to STOPP and 3-2-1 Grounding, CBT offers a variety of other simple, practical tools to help manage emotions, challenge negative thoughts, and build resilience. These are designed to be easy to use in everyday life, often without needing a therapist present. Here are some popular ones: ### 1. Thought Record (or ABC Model) - **What it is**: A way to break down and analyze thoughts to see how they affect your feelings and actions. - **How it works**: - **A – Activating Event**: What happened? (e.g., "I got a critical email from my boss.") - **B – Belief**: What did you think about it? (e.g., "I’m terrible at my job.") - **C – Consequence**: How did you feel or act? (e.g., "I felt anxious and avoided work.") - Then, challenge the belief: Is there evidence for this? What’s an alternative thought? (e.g., "One email doesn’t define my skills.") - **Why it’s useful**: Helps you spot distorted thinking (like catastrophizing) and replace it with balanced perspectives. ### 2. 5-4-3-2-1 Grounding (Expanded Version) - **What it is**: A more detailed version of 3-2-1 Grounding, engaging all five senses. - **How it works**: - 5 things you see - 4 things you can touch - 3 things you hear - 2 things you smell - 1 thing you taste (or imagine tasting) - **Why it’s useful**: Great for intense anxiety or dissociation, as it fully immerses you in the present. ### 3. Worry Postponement - **What it is**: A technique to delay worrying instead of getting stuck in it. - **How it works**: When a worry pops up, tell yourself, “I’ll think about this later.” Set a specific “worry time” (e.g., 15 minutes at 6 PM). Until then, redirect your focus to something else. - **Why it’s useful**: Breaks the cycle of endless rumination and often, by “worry time,” the issue feels less urgent. ### 4. Behavioral Activation - **What it is**: A simple action-oriented tool to combat low mood or procrastination. - **How it works**: Pick a small, manageable task (e.g., washing dishes, taking a walk) and do it, even if you don’t feel like it. Notice how it affects your mood afterward. - **Why it’s useful**: Gets you moving when depression or inertia sets in, proving action can shift feelings. ### 5. Positive Data Log - **What it is**: A way to counter negative self-beliefs by collecting evidence of your strengths. - **How it works**: Keep a daily note of anything positive about yourself (e.g., “I helped a friend,” “I finished a task”). Review it regularly. - **Why it’s useful**: Builds self-esteem and challenges beliefs like “I’m worthless” with real examples. ### 6. Square Breathing (or Box Breathing) - **What it is**: A breathing exercise to calm the nervous system. - **How it works**: - Inhale for 4 seconds - Hold for 4 seconds - Exhale for 4 seconds - Hold for 4 seconds - Repeat a few times. - **Why it’s useful**: Quick way to reduce stress or panic by regulating your breath. ### 7. The 3 Cs (Catch, Check, Change) - **What it is**: A shorthand for reframing negative thoughts. - **How it works**: - **Catch**: Notice the negative thought (e.g., “I’ll fail this test”). - **Check**: Question it—Is it 100% true? What’s the evidence? - **Change**: Replace it with a more balanced thought (e.g., “I might struggle, but I’ve prepared as best I can”). - **Why it’s useful**: Fast and memorable for on-the-spot thought management. These tools are all about empowerment—giving you quick ways to step in when your mind starts running wild. They’re flexible too; you can mix and match depending on what you’re dealing with. Want me to dive deeper into any of these or show how they’d work in a specific scenario?
DM with Hemoglobinopathies
Hemoglobinopathies (like Sickle Cell) falsely lower hemoglobin A1c as a result of hemolysis and abnormal glycation.
Fructosamine reflects total glycated serum proteins and is a measurement of average blood glucose over the past 2–3 weeks. It may be used instead of hemoglobin A1c for assessing glucose control in patients with diabetes and hemoglobinopathies.
A 2-hour glucose tolerance test or hemoglobin electrophoresis would not provide useful information.
Urine ketone studies would not be useful either.
Continuous glucose monitoring would be another option in this scenario to monitor glucose levels and provide a "time in range," which has been shown to correlate with hemoglobin A1c levels.
Male Infertility
A semen analysis is the first step in the evaluation of male infertility.
In males with oligozoospermia (sperm count <10 million/mL), the American Urological Association recommends an endocrine evaluation with FSH and early morning total testosterone levels.
- Antisperm antibody testing is rarely recommended and should only be considered in consultation with a fertility specialist.
- Scrotal ultrasonography is not recommended in individuals with a normal physical examination.
- Testicular biopsy is rarely performed to help differentiate between obstructive and nonobstructive azoospermia.
AF
The 2023 guidelines from the American College of Cardiology and the American Heart Association recommend anticoagulation for patients with an estimated annual risk for thromboembolic disease of ≥2%.
The CHA2DS2-VASc instrument is a validated tool to aid in assessing this risk; patients witih scores >1 are considered high risk.
- Direct-acting oral anticoagulants (DOACs) are recommended over warfarin in patients without a history of moderate to severe rheumatic heart disease and in patients who do not have a mechanical heart valve.
- DOACs have been found in randomized, controlled trials to be superior or noninferior to warfarin for preventing strokes and systemic embolic events, with a lower risk for serious bleeding.
- However, warfarin is still recommended over a DOAC for valvular atrial fibrillation that occurs in the presence of moderate to severe mitral stenosis or a mechanical heart valve.
Notes:
- For patients with atrial fibrillation and end-stage chronic kidney disease (CKD), both apixaban (a direct factor Xa inhibitor) and warfarin are options.
- However, there is no clinical trial data on safety and efficacy in patients with advanced CKD, and some experts avoid the use of apixaban in patients with a creatinine clearance <25 mL/min/1.73 m2 since safety and efficacy cannot be assured.
Asymptomatic Hypertension
Severe asymptomatic hypertension, sometimes called hypertensive urgency.
It is defined as a confirmed blood pressure >180/110–120 mm Hg without symptoms or signs of end-organ damage.
Patients without symptoms in the setting of severe hypertension rarely have end-organ damage and do not require emergent blood pressure–lowering therapy.
The most common cause of severe hypertension in patients with known hypertension is nonadherence to the use of antihypertensive medications.
When a significantly elevated blood pressure is measured, it should be repeated after 20–30 minutes of quiet rest.
- Blood pressures should be taken in both arms and a thigh to confirm elevation.
- One-third of patients with an initially elevated blood pressure will have significantly lower pressure after rest.
Little evidence exists to guide clinicians, but a common approach to assessing for end-organ damage includes obtaining a basic metabolic panel, CBC, urinalysis, EKG, and troponin level.
Patients with physical or laboratory evidence of end-organ damage should be admitted to the ICU for intravenous treatment of blood pressure.
Without symptoms or end-organ damage there is no need to transport patients to the emergency department, as asymptomatic hypertension can be managed with oral medication in the outpatient environment.
Chronic Urticaria
Second-generation H1 antihistamines are generally first-line treatment for chronic urticaria, though fewer than 50% of patients experience a satisfactory result with this treatment alone.
- Dose escalation of these medications can be helpful, with some guidelines recommending up to 4 times the FDA-approved dosing.
- Second-generation antihistamines are preferred over first-generation antihistamines due to the lower likelihood of side effects such as drowsiness.
Other options:
- For those who fail to achieve the desired result with monotherapy using an H1 antihistamine, the addition of an H2 antihistamine such as famotidine is often beneficial.
- The tricyclic antidepressant doxepin has strong H1 and H2 antihistamine effects and has been used as an off-label treatment option in some studies.
- A short course of oral corticosteroids, cyclosporine, or narrowband UV light treatment can be used in the management of recalcitrant chronic urticaria, but these are considered second- or third-line options.
As compared to acute urticaria in which a cause can often be identified, in chronic urticaria there is usually no identifiable cause.
Osteoporosis
Patients are at risk for developing glucocorticoid-induced osteoporosis if they are on long-term glucocorticoid therapy.
The American College of Rheumatology recommends pharmacologic osteoporosis treatment for patients who are taking >2.5 mg of prednisone for a duration of 3 months or longer and are assessed to be at medium, high, or very high risk for osteoporotic fracture.
In adults ≥40 years of age, only those with a FRAX estimated 10-year risk of major osteoporotic fracture (MOF) of <10%, hip fracture <1%, and bone mineral density >–1.0 are considered to be in a low-risk category.
Treatment is also recommended for patients receiving glucocorticoids who have a bone mineral density T-score ≤–2.5 at either the spine or the femoral neck and are either male and ≥50 years of age, or female and postmenopausal.
Therapy is also recommended in patients ≥40 years of age who do not meet these criteria but have a 10-year risk for major osteoporotic fracture of at least 20% or a risk for hip fracture of at least 3% according to the FRAX tool.
Oral bisphosphonates are recommended agents for preventing glucocorticoid-induced osteoporotic fractures in moderate-risk patients taking long-term glucocorticoids.
Intravenous bisphosphonates can be used if patients are unable to use the oral forms.
Supplementation of calcium (800–1000 mg) and vitamin D (400–800 IU) is also recommended.
High-dose vitamin D is not routinely indicated.
Denosumab, raloxifene, teriparatide, and romosozumab are additional options in high-risk or very high–risk patients and for those who are not candidates for bisphosphonate therapy.
Minimal Exercise Necessary edit
A new study plots the progression of thousands of people following an ultra-minimalist training plan. The results are impressive—at least initially.
There's good news and bad news in a remarkable new multi-year study of nearly 15,000 people who followed an ultra-minimalist strength training plan involving just one short workout a week. The good news is that the training really works, despite taking less than 20 minutes a week all in street clothes. The bad news is that it eventually stops working, or at least gets less effective—a phenomenon that the researchers argue may be universal rather than specific to the training plan, and that has important implications for how we think about long-term training goals.
https://osf.io/preprints/sportrxiv/eq485
The training plan involves one workout a week, typically including six exercises on Nautilus One machines: chest press, pulldown, leg press, abdominal flexion, back extension, and either hip adduction or abduction. For each exercise, you do one set with a weight chosen so that you'll reach momentary failure after four to six reps. The reps are performed slowly, taking ten seconds up and ten seconds down, without locking the limbs or resting at the top or bottom of the motion. Rest between exercises is typically about 20 seconds. The loads are adjusted from session to session to keep you failing after four to six reps. There's no music and no mirrors.
After a year, the typical subject has gotten about 30 percent stronger. After seven years, you're up by about 50 percent. You keep gaining, but the margins get smaller. The patterns are similar for the other exercises, though the numbers differ a bit. Leg press, for example, ends up about 70 percent higher than baseline.
There are various ways you can slice and dice the data, most obviously by considering the effects of age and sex. The subjects had an average age of 47 but spanned a wide spectrum, with a standard deviation of 12 years; 60 percent of them were female. None of it seemed to make a difference. Younger subjects tended to be stronger initially, as did males, but the rate of progress and the plateau after a year were consistent across groups.
From a public health perspective, the takeaway here seems clear: a "minimal effective dose" approach to resistance training really works. Once you reach adulthood, you typically start losing about one percent of your strength per year, with a steeper decline in your 60s and beyond. So even the plateau phase of this data, in which the subjects are making modest strength gains, represents a significant bending of the age curve. If you follow a program like this—or any program that produces similar slow-but-steady progress—you're winning. You don't need to feel guilty that you're not racking up big training volumes, following sophisticated periodization plans, promoting muscle confusion, or whatever else is currently in vogue.
One possibility is that all programs eventually produce diminishing returns, and the solution is to add a new or different stimulus. It's certainly likely that if you plateau in one program then switch to another, you'll see rapid initial progress in the new routine's specific movements and challenges. But it's less clear whether that progress is task-specific, or whether you're actually resuming rapid gains in generalizable strength.
As for whether this minimalist approach is really enough to optimize strength gains, the question reminds me of the epidemiological data suggesting that you can get "most" of the benefits of running by doing as little as five minutes a day. That doesn't square with the experience of competitive runners, who don't get "mostly" race fit on five minutes a day. The key is to remember that the minimum dose for health and the optimal dose for performance are two separate questions. The new data from Fit20 offers some fascinating insights on the former question, but shouldn't be confused with the latter.
https://www.eurekalert.org/pub_releases/2014-07/acoc-rrr072414.php
Overcome Social Anxiety edit
Challenge your negative thoughts Social anxiety develops negative thoughts. The first step to help yourself is to challenge your mentality. These negative thoughts contribute to their fears and anxiety and some of them are:
"I know I'll end up looking like a fool." "My voice will start shaking and I'll humiliate myself." "People will think I'm stupid" "I won't have anything to say. I'll seem boring." For example, when you are worried about an upcoming social gathering, identify the underlying negative thought. It could be "I won't have anything to say. I'll seem boring."
Next, analyze and challenge this negative thought. Be objective enough and ask questions like "Do I know for sure that they will get bored with me?"
Through this logical evaluation of your negative thought, replace them with encouraging and positive ways of looking at social situations that trigger your anxiety. When you understand the reasons for your anxieties, it will help lessen their negative impact on your life.
- Stop unhelpful thinking
Unhelpful thoughts are those that bring you down and fuel your anxiety. To help your anxiety level go down, stop the following unhelpful thinking:
- Mind reading – This is when you find yourself assuming that you know what other people are thinking. Stop thinking that people see you in the same negative way that you see yourself.
- Fortune telling – This refers to the times when you are predicting the future and assuming the worst will happen. How do you know that things will really go horribly? When you are fortune telling, you make yourself more anxious before you're even in the situation.
- Catastrophizing – This is when you blow things out of proportion. For example, if people notice that you're nervous, you immediately conclude that they think it will be "awful", "terrible", or "disastrous."
- Personalizing – This is when you assume that people are focusing on you in a negative way or that what's going on with other people has to do with you.
Focus on other things but yourself When we are in a social situation that makes you anxious, we tend to get caught up in our anxious thoughts and feelings. You are convincing yourself that all the people are looking at you and judging you.
Normally, our focus is on our bodily sensations, hoping that by paying extra close attention to them, we are controlling them. But nothing can be farther from the truth.
This excessive self-focus only makes us more aware of how nervous we're feeling, thus triggering even more anxiety! And when we focus on our racing heartbeat and cold hands, we are preventing ourselves from fully concentrating on the conversations around us.
Here are some things you can do instead:
- Focus your attention on other people – Take time to appreciate what other people are wearing or how the ambiance feels like. Avoid thinking about what other people are thinking of you! Instead, do your best to engage them and make a genuine connection.
- Remember that anxiety isn't as visible as you think. – Most of the time, people don't notice that you are anxious. They won't know how your heartbeat is racing unless you tell them. And even if they know that you're nervous, that doesn't mean they'll think badly of you. It is more likely that they are also nervous just like you.
- Really listen to what is being said – Avoid listening to your own negative thoughts. Listen to what other people are talking about.
- Focus on the present moment – Rather than worrying about what you're going to say, focus on the present moment. Tell yourself everything will be okay.
- Release the pressure to be perfect. – No one is perfect, and that includes you. Instead of putting pressure on yourself to be perfect, focus on being genuine and attentive because these are qualities that other people will appreciate.
- Breathe and let go – Take a deep breath and let go. Enjoy the moment and avoid beating yourself up if things don't go as planned.
Learn to control your breathing When you become anxious, you begin to breathe quickly. In turn, it throws off the balance of oxygen and carbon dioxide in your body.
Hyperventilation leads to more physical symptoms of anxiety, such as dizziness, a feeling of suffocation, increased heart rate, and muscle tension. But if you learn how to control your breathing, it can help bring your physical symptoms of anxiety back under control.
Practice the following breathing exercise to stay calm:
- Sit comfortably – Relax and with your back straight and your shoulders relaxed, put one hand on your chest and the other on your stomach.
- Inhale slowly – Inhale deeply and slowly through your nose for 4 seconds.
- Hold your breath for 2 seconds.
- Exhale slowly – Exhale slowly through your mouth for 6 seconds, pushing out as much air as you can.
- Continue to breathe – Repeat the inhale and exhale exercise. Focus on keeping a slow and steady breathing pattern of 4-in, 2-hold, and 6-out.
Face your fears Avoidance will only keep your social anxiety disorder going.
When you avoid what you fear, it will help you feel better in the short term. But, it prevents you from becoming more comfortable in social situations and learning how to cope in the long term.
Not only that, the longer you avoid a feared social situation, the more frightening it becomes. Also, avoidance prevents you from doing things you'd like to do – it is restricting you.
Face your fears gradually – take one small step at a time to avoid being overwhelmed. Start with a situation that you can handle like talking to one office mate. When you have successfully done it, your confidence will be boosted. Then, gradually work your way up to more challenging situations.
Here are steps that can help you work your way up the "anxiety ladder":
- Don't try to face your biggest fear right away. – One small step will do. In fact, it's never a good idea to move too fast, take on too much, or force things. This may result in more anxiety for you.
- Be patient – Success is not achieved in a day and so is overcoming social anxiety. It takes time and practice. Be patient with yourself and give yourself some credit.
- Be calm – Use skills to remain calm like focusing on your breathing and challenging your negative thoughts. When you master them, you will find it easier to overcome your anxiety.
Reference:
Study: Objective assessment of health or pre-chronic disease state based on a health test index derived from routinely measured clinical laboratory parameters
BLUF:
- The basic concept underlying the analysis was the evaluation of the impact of different trait-based health indices of somatic health as indictors of health status, which can be used to simplify a complex problem. Dynamic changes in adverse health status-related experimental indicators within specific ranges can be observed systematically, and biological markers of health status can be selected. In this manner, we aimed to establish a quantitative or semi-quantitative system to objectively assess the general health levels of an individual using laboratory indices.
- Most laboratory indicators reflect the risk of a disease rather than the presence of a disease; therefore, although laboratory indices are mainly used for the diagnosis of disease, they are considered indicators of health or pre-chronic disease state
- In theory, an HTI score >1 is considered a marker of disease. In the healthy population in our study, the mean of the actual observed HTI was 0.70, and the standard deviation was 0.07; therefore, it was considered a one-tailed test distribution; if the HTI was >0.8 (0.7 + 1.64*0.07), it was considered to indicate ill health or pre-chronic disease state, and medical investigations were recommended. Put simply, a lower HTI corresponded to a better health status.
- The evaluation indicators of organ function included albumin (Alb, 37 ~ 53 g/L) and creatinine (CRE, 60 ~ 130 μmol/L for males; 40 ~ 110 μmol/L for females); the evaluation indicators of blood lipids included triglycerides (TG, 0.22 ~ 2.29 mmol/L), cholesterol (Chol, 2.80 ~ 5.20 mmol/L), high-density lipoprotein (HDL, 0.80 ~ 3.26 mmol/L) and low-density lipoprotein levels (LDL, <3.12 mmol/L); and the evaluation indicators of stress included the neutrophil count (Neut; 2.0 ~ 7.0× 109/L) and glucose level (GLU: 3.60 ~ 6.10 mmol/L)
| Indicators | Cut-off values | Ratio of cut-offs | Indicators | Cut-off values | Ratio of cut-offs |
|---|---|---|---|---|---|
| Alb | 37 | 37/MV | TG | 2.29 | MV/2.29 |
| CRE | Male: 130; Female: 110 | Male: MV/130; Female: MV/110 | Chol | 5.20 | MV/5.20 |
| Neut | 7.0 | MV/7.0 | HDL | 0.80 | 0.80/MV |
| Glucose | 6.1 | MV/6.1 | LDL | 3.12 | MV/3.12 |
MV = Measured Value
- For example, if the upper limit value of Neut was 7.0, and the measured value of Neut was 3.5, the ratio of the cut-off value was 0.5 (3.5/7.0) for Neut. In theory, an HTI score >1 was considered a marker of disease.
- Organ Function Index: The means of the cut-off ratios of ALB and CRE were defined as the organ function index
- Blood Lipid Index: the means of the cut-off ratios of TG, Chol, HDL and LDL were defined as the blood lipid index
- Stress Index: the means of the cut-off ratios of Neut and GLU were defined as the stress index.
- Health Test Index: Finally, the mean of the above three indexes was defined as the health test index (HTI).
Objective
- To develop a quantitative system to enable the objective assessment of health or pre-chronic disease state.
Methods
- On the basis of measured values and reference ranges, we obtained the organ function index (mean of the cut-off ratios of albumin and creatinine), blood lipid index (mean of the cut-off ratios of triglycerides, cholesterol, high-density lipoproteins and low-density lipoproteins), stress index (mean of the cut-off ratios of neutrophils and glucose), and the health test index (mean of the above three indexes, HTI). Elderly populations, individuals with nonalcoholic fatty liver disease and administrators were included in the groups of observed subjects to verify the organ function index, blood lipid index and stress index.
Results
- The scores of the three indexes were all statistically higher in the observed group than in the control group (p < 0.05). The mean HTI score was 0.7 ± 0.07 and was normally distributed in the control population. The rates of hypertension, obesity, fatty liver disease and health (undetectable organic diseases) increased with increasing HTI scores in a random population.
Conclusions
- The HTI is easily derived from routinely measured clinical laboratory parameters. It can reflect the health status of an individual and may be a useful tool for the quantitative differentiation of health status.
Reference:
- Wenping S, Ying L, Song L, Yuzhong L, Hui L. Objective assessment of health or pre-chronic disease state based on a health test index derived from routinely measured clinical laboratory parameters. J Transl Med. 2015 Apr 22;13:127. doi: 10.1186/s12967-015-0487-z. PMID: 25896310; PMCID: PMC4423109.
To Capture edit 2025
Well-designed RCTs have not proven that mood disorder or food insecurity screening improve mood disorders or food insecurity. Colonoscopy and mammogram screenings are unlikely to improve all-cause mortality.
Capture:
- Universal Depression Screening Leads to Unnecessary Harm
- Screening for Food Insecurity: US Preventive Services Task Force Recommendation Statement | Guidelines | JAMA | JAMA Network
- Staying True to Trial Analyses – The Tale of Two Screening Trials
- Mammography - everything you need to know - by Vinay Prasad
Capture: Weight Hormones
- Cholecystokinin
Cholecystokinin (CCK) is a lot like GLP-1.
- Made in the gut and helps SATIATION.
- It's important for energy production, protein synthesis, digestion, and other bodily functions.
- It also increases the release of the fullness hormone leptin.
People with obesity may have a reduced sensitivity to CCK's effects, which may lead to chronic overeating. In turn, this may further reduce CCK sensitivity, creating a negative feedback loop.
Here are some tips for maintaining healthy levels of CCK:
- Eat plenty of protein. Some research suggests a high protein diet may help increase CCK levels, and therefore fullness.
- Exercise. While research is limited, some evidence supports regular exercise for increasing CCK levels.
- Cortisol
Created within the adrenal glands, cortisol is known as the stress hormone.
- Essential for survival
- Whenever your body or mind perceives it's under stress, cortisol is released into the bloodstream.
- Elevated cortisol is linked to overeating and increased central obesity
- Balanced cortisol levels:
- Consider what relaxes you. Is it meditation? A walk in the park? A bubble bath? Engaging in a creative project? Find what relieves stress for you, and integrate it into your daily routine.
- Exercise regularly, and give yoga a try if it's not already part of your workout regimen. The synchronized breathwork that accompanies a nice, flowing vinyasa routine calms the nervous system and reduces cortisol — all while giving your body and mind a thorough workout.
- Listen to your favorite music. A 2011 study published in the journal Frontiers in Psychology found that patients who listened to instrumental music during surgery had lower cortisol levels than a control group.
- Get enough sleep at night. Have you ever noticed how easily stressed and anxious you become on days when you're sleep deprived? This happens because during a night of deep, restorative sleep, your body is working to balance all hormones, including cortisol. A study published in the peer-reviewed journal Aviation, Space, and Environmental Medicine explored how sleep deprivation impacted helicopter pilots on a 7-day emergency medical duty. Findings suggested it was sleep deprivation — not the act of emergency medical care — that elevated adrenaline and cortisol levels.
Chronic high levels may lead to:
- heart disease
- diabetes
- low energy levels
- high blood pressure
- sleep disturbances
- weight gain
Certain lifestyle factors contribute to high cortisol levels:
- poor sleep habits
- chronic stress
- a high intake of high glycemic foods
Tips for lowering cortisol levels:
- Optimize sleep. Chronic sleep issues, including insomnia, sleep apnea, and irregular sleep habits (like those of shift workersTrusted Source), may contribute to high cortisol levels. Focus on developing a regular bedtime and sleep schedule.
- Exercise regularly. Cortisol levels temporarily increase after high intensity exercise, but regular exercise generally helps decrease levels by improving overall health and lowering stress levels.
- Practice mindfulness. ResearchTrusted Source suggests that regularly practicing mindfulness lowers cortisol levels, though more research is needed. Try adding meditation to your daily routine.
- Maintain a moderate body weight. Because obesity may increase cortisol levels and high cortisol levels can cause weight gain, maintaining a moderate weight may help keep levels in check.
- Eat a balanced diet. Research has shown that diets high in added sugars, refined grains, and saturated fat may lead to higher cortisol levels. Additionally, following the Mediterranean dietTrusted Source may help lower cortisol levels.
- Estrogen
- Produced in the Ovaries
- Estrogen promotes the storage of fat for healthy reproductive years lead to weight gain.
- Overweight women typically have high amounts of estrogen, as do women in the first half of pregnancy.
- In perimenopause and menopause, characterized by less hormonal weight and notable decrease in estrogen.
- Ways to manage Estrogen:
- Commit to a regular exercise routine. Many studies, including this 2012 one, published in the Journal of Clinical Oncology, explain how exercise lowers estrogen levels in obese women.
- Eat your fiber. Fibrous foods help decrease elevated estrogen levels.
- Eat veggies in the cruciferous family. These include broccoli, cauliflower, Brussels sprouts, cabbage, kale, and bok choy.
- Consider hormone replacement therapy
Tips to maintain healthy estrogen levels
- Try to manage your weight. Weight loss or maintenance may reduce the risk of heart disease due to low estrogen levels in women ages 55–75.
- Exercise regularly. Low estrogen levels may leave you feeling less capable of working out. Nonetheless, during periods of low estrogen output, such as menopause, regular exercise is still important to aid weight management.
- Follow a balanced diet. Diets high in red meat, processed foods, sweets, and refined grains have been shown to increase estrogen levels, which may raise your risk of chronic disease. As such, you may wish to limit your intake of these foods.
- Ghrelin
- The hunger hormone.
- When the stomach becomes empty, it naturally releases ghrelin into your bloodstream.
- Ghrelin levels are lowest just after you've finished a meal. They're at their highest when the stomach is empty and you're ready for your next meal.
- In most healthy weight individuals, ghrelin levels decrease in a way that satiates them and signals their brains to stop eating.
- But in obese individuals, ghrelin levels don't decrease enough after eating, which fails to send the brain the signal it needs to stop eating and feel satisfied.
- How are a couple of ways to balance them:
- Eat adequate amounts of protein. Protein helps you feel full and should be consumed with every meal. Studies show how eating protein promotes healthy ghrelin levels.
- Avoid sugar as much as possible. As you can see by now, consuming too much sugar disrupts hormonal balance, making weight loss seem an impossible feat. Be sure to read labels. If an item contains high-fructose corn syrup, don't buy it. A 2013 study published in Nutritional Diabetes shows how high-fructose corn syrup is one of the primary culprits of imbalance when it comes to hormones and weight gain.
—
Ghrelin is essentially the opposite of leptin. It's the hunger hormone that sends a message to your hypothalamus indicating that your stomach is empty and needs food. Its main function is to increase appetite.
Normally, ghrelin levels are highest before eating and lowest after a meal.
Curiously, research indicates that people with obesity have low ghrelin levels but are more sensitive to its effects. This sensitivity may lead to overeating .
Tips to manage ghrelin levels One reason weight loss can be difficult is that restricting calories often leads to increased ghrelin levels, leaving you hungry. Additionally, metabolism tends to slow down and leptin levels decrease.
As such, here are some tips for lowering ghrelin to help reduce appetite:
Maintain a moderate body weight. Obesity may increase your sensitivity to ghrelin, ultimately increasing your appetite. Try to get good quality sleep. Poor sleep may lead to increases in ghrelin, overeating, and weight gain. Eat regularly. Because ghrelin levels are highest before a meal, listen to your body and eat when you're hungry. Summary People with obesity may become more sensitive to the effects of the hunger hormone ghrelin. Research suggests that maintaining a moderate body weight and prioritizing sleep help with managing this hormone.
- Glucagon-like Peptide-1
- GLP-1 is a hormone produced in the intestines when nutrients are digested. This gut hormone supports the balance of blood sugar and helps you feel satiated. Maintain healthy GLP-1 levels by eating enough protein, probiotics, leafy green veggies, and anti-inflammatory foods.
—
Glucagon-like peptide-1 (GLP-1) is a hormone produced in your gut when nutrients enter your intestines. It plays a major role in keeping blood sugar levels stable and making you feel full.
Research suggests that people with obesity may have problems with GLP-1 signaling.
As such, GLP-1 is added to medications — particularly for people with diabetes — to reduce body weight and waist circumference.
Tips for keeping GLP-1 levels in check Here are some tips to help maintain healthy levels of GLP-1:
Eat plenty of protein. High protein foods such as whey protein and yogurt have been shown to increase GLP-1 levels. Consider taking probiotics. Preliminary research suggests that probiotics may increase GLP-1 levels, though more human research is needed. Additionally, it's best to chat with a healthcare professional before starting any new supplements. Summary GLP-1 is a fullness hormone, but people with obesity may not be as sensitive to its effects. To maintain healthy GLP-1 levels, try to eat a well-rounded diet with plenty of protein.
- Insulin
Insulin is one of the most important hormones when it comes to weight loss and weight gain. Made by the pancreas, insulin is responsible for storing blood sugar, or utilizing it, depending upon your body's needs of the moment. After you eat a large meal, a substantial amount of insulin releases itself into the bloodstream. It also enters the bloodstream as needed throughout the day, ensuring that high blood pressure and high blood sugar levels remain stable.
Another key function of this essential hormone is fat storage. Insulin decides how much fat to store, and how much fat tissue has to convert for energy expenditure. Chronically high levels of insulin can lead to a condition known as insulin resistance, which is linked to an uptick in blood sugar as well as continued elevated insulin levels.
Preventing this insulin imbalance is crucial to healthy lifestyle, as it leads to weight gain, and eventually type 2 diabetes. When insulin levels remain high over an extended period of time, obesity, cardiovascular disease and metabolic syndrome are often the unfortunate outcome of chronic disease.
What you can do: Stop overeating the foods that cause insulin resistance How do we ensure our insulin levels remain balanced? First, we need to stop eating too much. It's a known fact that overeating leads to insulin resistance cause weight gain, especially when we eat too much food that's no good for our bodies and minds. When we eat too much sugar, too much fast food, and too many processed carbohydrates, insulin goes haywire. These elevated insulin levels lead to weight gain and low-grade inflammation. A 2010 study published in the journal Diabetes found that even eating too much of these foods in the short term leads to insulin resistance and weight gain.
You may also want to restrict carbohydrates in your diet. According to a study published in the journal Nutrition and Metabolism, a low-carb diet prevents metabolic syndrome and the insulin resistance that causes it. Other findings show drinking green tea, consuming omega-3 fatty acids from fatty fish, and eating adequate amounts of protein all help balance insulin levels.
—
Insulin, the main storage hormone in your body, is produced by your pancreas. In healthy individuals, insulin promotes the storage of glucose — a simple sugar you get from food — in the muscle, liver, and fat cells for later use.
Your body secretes insulin in small amounts throughout the day and in larger amounts after meals. This hormone then transfers glucose from food into your cells for either energy or storage, depending on your body's current needs.
Insulin resistance is a fairly common condition that causes your cells to stop responding to insulin. This condition results in high blood sugar because the insulin cannot move glucose into your cells.
Your pancreas then produces even more insulin in an attempt to boost glucose absorption.
Insulin resistance has been linked to obesity, which in turn can play a role in other conditions, such as type 2 diabetes and heart disease.
Insulin sensitivity can be thought of as the opposite of insulin resistance. It means your cells are sensitive to insulin. Thus, it's a good idea to focus on lifestyle habits that help improve insulin sensitivity, such as the following.
Tips to improve insulin sensitivity Exercise regularly. Research supports exercise, at both high and moderate intensities, as a means of improving insulin sensitivity and decreasing insulin resistance. Improve your sleep habits. Not getting enough sleep, or not getting quality sleep, is linked to obesity and insulin resistance. Get more omega-3 fatty acids. Research indicates that omega-3 supplements may improve insulin sensitivity in people with metabolic conditions such as diabetes. If you aren't a fan of supplements, try eating more fish, nuts, seeds, and plant oils. Change your diet. The Mediterranean diet — which includes many veggies, as well as healthy fats from nuts and extra-virgin olive oil — may help reduce insulin resistance. Decreasing your intake of saturated and trans fats may also help. Maintain a moderate weight. In people with overweight, healthy weight loss and weight management may improve insulin sensitivity. Focus on low glycemic carbs. Rather than try to eliminate carbs from your diet, aim to make most of them low glycemic and high fiber. Examples include whole grains, fruits, vegetables, and legumes. Summary Insulin resistance is linked to chronic conditions such as type 2 diabetes and heart disease. To promote insulin sensitivity, focus on regular exercise, a healthy diet, and better sleep habits.
- Leptin
Leptin is a fullness hormone that works by telling your hypothalamus — the portion of your brain that regulates appetite — that you're full.
However, people with obesity may experience leptin resistance. This means the message to stop eating doesn't reach your brain, eventually causing you to overeat.
In turn, your body may produce even more leptin until your levels become elevated.
The direct cause of leptin resistance is unclear, but it may be due to inflammation, gene mutations, and/or excessive leptin production, which can occur with obesity.
Tips to improve leptin levels Although no known treatment exists for leptin resistance, a few lifestyle changes may help lower leptin levels:
Maintain a healthy weight. Because leptin resistance is associated with obesity, it's important to maintain a healthy weight. Additionally, research suggests that a decrease in body fat may help reduce leptin levels. Improve your sleep quality. Leptin levels may be related to sleep quality in people with obesity. Although this association may not exist in people without obesity, there are numerous other reasons to get better sleep. Exercise regularly. Research links regular, consistent exercise to a decrease in leptin levels. Summary In people with obesity, resistance to the hormone leptin, which helps you feel full, may lead to overeating. Research suggests that exercising regularly, sleeping well, and maintaining a healthy body weight help lower leptin levels.
—
Think of leptin as the appetite suppressant hormone. Made within fat cells, leptin is what is belly fat and makes you feel satiated. It "talks" to your brain, telling it when you feel hungry or full.
When your leptin levels regulate appetite are balanced, you don't overeat because you feel full after eating a well-rounded meal, and that fullness lasts for hours. Leptin is like insulin in that it hates the wrong foods. Ever notice how sweets and processed foods leave you feeling empty and wanting for more even after a short period of time? Eating trans fats and processed foods over the long term eventually leads to leptin resistance.
- Leptin Resistance
When your body becomes resistant to leptin, leptin levels become too high for normal weight. In fact, overweight individuals who get their leptin levels tested typically find their leptin levels to be as high as four times the normal level. What's more, it's really difficult to balance leptin levels with normal body weight, once they've become resistant.
With leptin resistance, communication between the brain and leptin is impaired, so that your brain doesn't understand that it's full, and tells your body to keep eating. It's as if your brain thinks you're starving when in reality, you're just leptin resistant.
To reverse leptin resistance or prevent it from happening to you in the first place, let's talk food, drink, and supplements. Everything in your body impacted by what you put into it, and leptin's no different. Sugar, in particular, can cause leptin levels in your body to skyrocket, so you'll want to eat less sugar.
Other ways to prevent or reduce leptin resistance include:
- Consuming an anti-inflammatory diet
- Supplementing with anti-inflammatory fish oil
- Committing to a regular exercise routine
- Getting truly restorative sleep on a regular basis
- Leptin Resistance
- Neuropeptide Y
- This hunger-stimulating hormone is made in the brain and nervous system. It influences appetite, especially for carbs. During times of stress and fasting, NPY levels increase dramatically. To maintain healthy NPY levels, make sure you're eating plenty of protein and soluble fiber. If you have a fasting routine, don't overdo it. Intermittent fasting is fine, but if you fast for longer periods, you could disrupt the delicate balance of NPY levels and sabotage your otherwise healthy lifestyle and weight loss and-loss goals in the process.
—
Neuropeptide Y (NPY) is a hormone produced by cells in your brain and nervous system that stimulates appetite and decreases energy expenditure in response to fasting or stress.
Because it may stimulate food intake, NPY is associated with obesity and weight gain.
It's activated in fat tissue and may increase fat storage and lead to abdominal obesity and metabolic syndrome, a condition that can increase the risk of chronic diseases.
Research has shown that NPY's mechanisms that lead to obesity may also cause an inflammatory response, further worsening health conditions.
Tips for maintaining low NPY levels Here are some tips for maintaining healthy levels of NPY:
Exercise. Some studies suggest that regular exercise may help decrease NPY levels, though research is mixed. Eat a nutritious diet. Although more research is needed, high fat, high sugar diets may increase NPY levels — so you may want to consider lowering your intake of foods high in sugar and fat. Summary NPY is an appetite-stimulating hormone that may lead to obesity. To maintain healthy levels, it may be helpful to exercise regularly and eat well.
- Peptide YY
- Yet another hormone found in the gut that has to do with appetite control, PYY needs to be balance hormones remain at relatively high levels in order to prevent overeating gain weight from. Make sure you focus on a low-carb diet, with plenty of protein and fiber. This type of balanced diet and healthy eating habits ensures the healthy balance of PYY to help prevent weight gain.
—
Peptide YY (PYY) is another gut hormone that decreases appetite.
PYY levels may be lower in people with obesity, and this may lead to a greater appetite and overeating. Sufficient levels are believed to play a major role in reducing food intake and decreasing the risk of obesity.
Tips for raising PYY levels
- Follow a well-rounded diet. Eating plenty of protein may promote healthy PYY levels and fullness. Additionally, the paleo diet — which includes ample protein, fruits, and veggies — may raise PYY levels, but more research is needed.
- Exercise. While research on exercise and PYY levels is mixed, staying active is generally beneficial for health.
Summary People with obesity may have low levels of the fullness hormone PYY. Eating a high protein diet and staying active may help raise levels.
- Capture: Weight Hormones
Lifestyle Medicine
- https://pubmed.ncbi.nlm.nih.gov/31105044/
- https://pubmed.ncbi.nlm.nih.gov/11396693/
- https://pubmed.ncbi.nlm.nih.gov/28338764/
- https://pubmed.ncbi.nlm.nih.gov/28399126/
- https://pubmed.ncbi.nlm.nih.gov/28338764/
- https://pubmed.ncbi.nlm.nih.gov/10837285/
- https://pubmed.ncbi.nlm.nih.gov/24493081/
- https://pubmed.ncbi.nlm.nih.gov/32011623/
- https://pubmed.ncbi.nlm.nih.gov/24476641/
- https://pubmed.ncbi.nlm.nih.gov/30660336/
Menopause
Labs
[ ]Parathyroid (for hypercalcinemia)[ ]Prolactin (for galactorrhea/pituitary eval)
Mg:
Links to keep
Things to Capture
- https://www.news.straighthealthcare.com/phentermine.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7801751/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4011567/
- https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/751590
- https://www.va.gov/WHOLEHEALTHLIBRARY/tools/glycemic-index.asp
- https://www.botoxmedical.com/Common/Assets/Reconstitution%20Guide.pdf
- https://hcp.botoxcosmetic.com/~/media/Unique%20Sites/BotoxCosmeticHCP/Files/PDFs/BHCP-0231_Injection_Dosing.pdf
- https://onlinelibrary.wiley.com/doi/full/10.1111/joim.12496
- https://www.regenxhealth.com/post/how-to-manage-estrogen-levels-in-men-on-testosterone-replacement-therapy-trt
- https://www.aafp.org/pubs/afp/issues/2020/0501/p530.html
- https://www.aafp.org/pubs/afp/issues/2023/0400/systemic-lupus-erythematosus.html
Supplements
- https://informationisbeautiful.net/visualizations/snake-oil-scientific-evidence-for-nutritional-supplements-vizsweet/
- https://ods.od.nih.gov/factsheets/list-all/
- https://examine.com/interventions/#m
- https://ods.od.nih.gov/Research/Evidence-Based_Review_Program.aspx
- https://www.nccih.nih.gov/
- Vitamin B12 - PMC
Study: Role of Inactivity in Chronic Diseases: Evolutionary Insight and Pathophysiological Mechanisms
This review proposes that physical inactivity could be considered a behavior selected by evolution for resting, and also selected to be reinforcing in life-threatening situations in which exercise would be dangerous.
Underlying the notion are human twin studies and animal selective breeding studies, both of which provide indirect evidence for the existence of genes for physical inactivity.
Approximately 86% of the 325 million in the United States (U.S.) population achieve less than the U.S. Government and World Health Organization guidelines for daily physical activity for health.
Although underappreciated, physical inactivity is an actual contributing cause to at least 35 unhealthy conditions, including the majority of the 10 leading causes of death in the U.S. First, we introduce nine physical inactivity-related themes. Next, characteristics and models of physical inactivity are presented.
Following next are individual examples of phenotypes, organ systems, and diseases that are impacted by physical inactivity, including behavior, central nervous system, cardiorespiratory fitness, metabolism, adipose tissue, skeletal muscle, bone, immunity, digestion, and cancer.
Importantly, physical inactivity, itself, often plays an independent role as a direct cause of speeding the losses of cardiovascular and strength fitness, shortening of healthspan, and lowering of the age for the onset of the first chronic disease, which in turn decreases quality of life, increases health care costs, and accelerates mortality risk.
| Age Range | Frequency & Duration | Type of Physical Activity |
|---|---|---|
| 5–17 yr | <60 min/day | Including both moderate- or vigorous-intensity aerobic, including some muscle strengthening |
| >18 yr | <150 min/wk | <150 min/wk of either moderate- or vigorous-intensity aerobic, or <75 min/week of mixed moderate and high-intensity aerobic, preferably spread throughout the week; plus 2 days/wk of resistance training involving moderate to high intensities for all major muscle groups |
- Cardiovascular diseases Individuals performing no physical activity had 45% more cardiovascular diseases than those performing 41 MET·hr/wk (where 1 MET is the value of resting oxygen consumption).
- T2D Low activity groups had a 35 and 26% greater risk of T2D than in high activity groups in meta-analyses when total activity was determined in 14 cohort studies and leisure time activity was reported in a different 55 cohort studies, respectively (10).
- Breast cancer A 25% average increase in breast risk was present in the low physical activity groups compared with the high activity groups in the 51 studies that showed an increased risk. Case-control studies had a stronger effect (an average 30% increase) than cohort studies (a 20% increase) (310).
- Colon cancer The risk of proximal and distal colon cancers were increased by 27 and 26%, respectively, among the least active individuals in 21 meta-analyzed studies, as compared with the most physically active people (63).
- Dementia Beyboun et al. (37) noted that decreased physical activity was a strong predictor of incident Alzheimer’s disease based on an average of 27 studies that found an estimated population attributable risk percentage in dementia by physical activity to be 31.9%.
- Depression Meta-analysis of 25 studies (453) showed a large significant improvement of depression by exercise and that >1,000 studies with negative results would be required to reject the positive effects of exercise on depression, including larger effects for interventions in major depressive disorders. The effect size of exercise on depression is at a moderate level of 0.56 (533). Furthermore, it has been shown that exercise improves depressive symptoms to a comparable extent as pharmacotherapy and psychotherapy (48).
Reference:
- Booth FW, Roberts CK, Thyfault JP, Ruegsegger GN, Toedebusch RG. Role of Inactivity in Chronic Diseases: Evolutionary Insight and Pathophysiological Mechanisms. Physiol Rev. 2017 Oct 1;97(4):1351-1402. doi: 10.1152/physrev.00019.2016. PMID: 28814614; PMCID: PMC6347102.
Study: Optimism is associated with exceptional longevity in 2 epidemiologic cohorts of men and women
Significance
- Optimism is a psychological attribute characterized as the general expectation that good things will happen, or the belief that the future will be favorable because one can control important outcomes. Previous studies reported that more optimistic individuals are less likely to suffer from chronic diseases and die prematurely.
- Our results further suggest that optimism is specifically related to 11 to 15% longer life span, on average, and to greater odds of achieving “exceptional longevity,” that is, living to the age of 85 or beyond.
- These relations were independent of socioeconomic status, health conditions, depression, social integration, and health behaviors (e.g., smoking, diet, and alcohol use).
- Overall, findings suggest optimism may be an important psychosocial resource for extending life span in older adults.
Abstract
- Most research on exceptional longevity has investigated biomedical factors associated with survival, but recent work suggests nonbiological factors are also important. Thus, we tested whether higher optimism was associated with longer life span and greater likelihood of exceptional longevity.
- Data are from 2 cohorts, women from the Nurses’ Health Study (NHS) and men from the Veterans Affairs Normative Aging Study (NAS), with follow-up of 10 y (2004 to 2014) and 30 y (1986 to 2016), respectively. Optimism was assessed using the Life Orientation Test–Revised in NHS and the Revised Optimism–Pessimism Scale from the Minnesota Multiphasic Personality Inventory-2 in NAS.
- Exceptional longevity was defined as survival to age 85 or older.
- Primary analyses used accelerated failure time models to assess differences in life span associated with optimism; models adjusted for demographic confounders and health conditions, and subsequently considered the role of health behaviors. Further analyses used logistic regression to evaluate the likelihood of exceptional longevity.
- In both sexes, we found a dose-dependent association of higher optimism levels at baseline with increased longevity (P trend < 0.01).
- For example, adjusting for demographics and health conditions, women in the highest versus lowest optimism quartile had 14.9% (95% confidence interval, 11.9 to 18.0) longer life span.
- Findings were similar in men.
- Participants with highest versus lowest optimism levels had 1.5 (women) and 1.7 (men) greater odds of surviving to age 85; these relationships were maintained after adjusting for health behaviors.
- Given work indicating optimism is modifiable, these findings suggest optimism may provide a valuable target to test for strategies to promote longevity.
Reference:
- L.O. Lee, P. James, E.S. Zevon, E.S. Kim, C. Trudel-Fitzgerald, A. Spiro, F. Grodstein, & L.D. Kubzansky, Optimism is associated with exceptional longevity in 2 epidemiologic cohorts of men and women, Proc. Natl. Acad. Sci. U.S.A. 116 (37) 18357-18362, https://doi.org/10.1073/pnas.1900712116 (2019).
homocysteine
From what I have read, supplementation with B vitamins is the primary approach to reduce homocysteine concentrations in individuals with elevated levels or vascular dysfunction.
- Folic acid supplementation (0.5 - 5 mg/d), reportedly can reduce homocysteine by approximately 25%.
- An alternative is the active form of folate, L-methylfolate
- Lifestyle factors that may help include limiting coffee intake to less than 4 cups/d and moderating alcohol consumption
Follow up: HRT testosterone edit 2025
Clomid Alternatives for Men
Clomiphene citrate (Clomid) is commonly used off-label as an alternative to testosterone replacement therapy (TRT) for men with hypogonadism, stimulating the body's natural testosterone production by blocking estrogen receptors in the hypothalamus and pituitary gland, which increases luteinizing hormone (LH) and follicle-stimulating hormone (FSH) secretion However, for men who do not respond to Clomid or seek a more targeted treatment, alternatives include enclomiphene citrate, human chorionic gonadotropin (hCG), aromatase inhibitors, and testosterone replacement therapy (TRT)
- Enclomiphene citrate: This is the purified active isomer of Clomid (enclomiphene) without the inactive isomer (zuclomiphene), which may result in fewer side effects like mood swings and visual disturbances. It is specifically designed for testosterone optimization in men and is considered a safer, more targeted alternative to Clomid
- Human chorionic gonadotropin (hCG): Used to stimulate the testes to produce testosterone naturally and can help maintain fertility, often used in combination with other treatments
- Aromatase inhibitors (e.g., anastrozole): These medications inhibit the conversion of testosterone to estrogen, potentially increasing testosterone levels and are being researched for use in men with low testosterone
- Testosterone replacement therapy (TRT): This is a first-line treatment for men with low testosterone, involving direct supplementation via injections, patches, or gels, and is often considered when other alternatives are ineffective
- Combination therapies: Research suggests that combining clomiphene with anastrozole or hCG may enhance treatment effectiveness for hypogonadism symptoms
Look up: https://www.urologytimes.com/view/alternatives-t-therapy-lessons-male-infertility
Helping healthy people? edit 2025
| Endpoint | Efficacy | NNV* |
|---|---|---|
| Community-acquired pneumonia (CAP) caused by vaccine-type strains (VTS) | 45.6% (21.8 - 62.5) | 1031 |
| Nonbacteremic/noninvasive CAP caused by VTS. | 45.0% (14.2 - 65.3) | 1563 |
| Invasive pneumococcal disease caused by VTS | 75.0% (41.4 - 90.8) | 2040 |
| CAP | 5.1% (5.4 -14.2) | Not significant |
Consider seeing a healthy 60-year-old man in December of 2025 who comes in for a check-up. Besides measuring his blood pressure, the value of which I will not argue, I am encouraged to do the following:
- Offer the COVID, Flu, RSV, shingles, and Prevnar vaccines
- Discuss colon cancer and prostate cancer screening
- Order some blood work: hemoglobin A1C, lipid panel, and, if he hasn’t been tested, hepatitis C and HIV.
- If I had time, and looked into the United States Preventive Services Task Force grade A and B recommendations, I would screen for depression, suicide risk, fall risk, and alcohol or drug use. I would also counsel regarding a healthy diet and physical activity.2
Healthy people coming to a doctor are generally, well, healthy. The likelihood of suffering any of the endpoints in column two is small. Also, our treatments aren’t perfect. Even things that are gospel in medicine — aspirin at the time of a STEMI or a statin in someone with CVD — have NNTs to prevent death of 42 and 83, respectively. The result is that we need to screen a lot of people to find someone at risk and then treat a lot of people to benefit someone.
| Intervention | Endpoint | NNV/NNT/NNS* |
|---|---|---|
| COVID Vaccine (1) | Composite of COVID- associated ER visits; COVID- associated hospitalization; COVID-associated death | 549 (assume no change in overall mortality) |
| Colon cancer screening with colonoscopy (2) | Prevention of colon cancer | 455 (no change in overall mortality) |
| Prostate Cancer screening with PSA (3) | Death from prostate cancer | 628 (at 16 years) 456 (at 23 years) |
| Lipid-lowering therapy in people without CAD (4) | Non-fatal MI | 247 (no change in overall mortality) |
| Depression screening | lower prevalence of depression/clinically important depressive symptomatology at 6-12 months | Thave no idea (5) |
If the prevalence of a disease in an asymptomatic population is 1/1000 and your NNT is 100, your number needed to screen (NNS) is 100,000.
Not all of our problems come from us being blinded by beneficence and medicine’s success. There is also, of course, profit. The benefit of adult pneumococcal vaccination is, at best, small. For some, vaccination might be the right decision, for others, not. What encourages the recommendation that every adult over fifty receive the shot? A whole lot of money. Given the prohibition on generic vaccines, a company able to get a vaccine recommended for every adult over a certain age inherits a bottomless trust fund.
Reference:
Study: Why more social interactions lead to more polarization in societies
Over the past two decades, the number of close social connections increased substantially, at least by a factor of two. At the same time, societal opinions have become increasingly polarized in many Western countries. To explore whether these trends could be connected, we employ a simple computational model of society, where people—within their social networks—continuously compare and update their opinions. Here, we show that the model that is known to realistically capture both homophily and social balance exhibits a phase transition phenomenon where, above a critical social connectivity, an explosive transition toward strong polarization must occur. The model allows us to understand the empirical inflation of polarization during the last decades as a function of the observed increased values of social connectivity. In the presence of a small fraction of synchronized influencers, the transition becomes continuous; however, polarization then appears at lower connectivities. We discuss the implications of the presence of a phase transition in social polarization.
From Discussion:
- What can be done is to shift the critical connectivity (the onset of the transition) in two ways.
- One is by changing ϐ. Lower ϐ values shift the critical connectivity upward. A ϐ of 2 means a critical polarization onset of a degree well above 5, which is above current connectivities. When ϐ is interpreted as an individual’s sensitivity to social stress, a reduction effectively means more “tolerance” toward opposing opinions.
- The way out of social polarization is either by reducing social contacts (which seems unrealistic) or by increasing tolerance in the society which might well be achieved by educational means.
- The other option for shifting the polarization transition is to reduce the disproportionate influence of a small radical minority. This could be achieved through stronger regulatory requirements for content moderation (61) and by disrupting know pathways for radicalization (62). As we have seen, this can increase the critical connectivity threshold and mitigate the onset of polarization. Similarly, building cross-cutting friendships (63)–possibly modeled as a few enforced “bridge” friendships between opposed clusters, or small, targeted network rewiring (64) could lead to a reduction in polarization.
- One is by changing ϐ. Lower ϐ values shift the critical connectivity upward. A ϐ of 2 means a critical polarization onset of a degree well above 5, which is above current connectivities. When ϐ is interpreted as an individual’s sensitivity to social stress, a reduction effectively means more “tolerance” toward opposing opinions.
Reference:
- S. Thurner,M. Hofer, & J. Korbel, Why more social interactions lead to more polarization in societies, Proc. Natl. Acad. Sci. U.S.A. 122 (44) e2517530122, https://doi.org/10.1073/pnas.2517530122 (2025).
Counselors edit 2025
NATHALIA DIBENARDO LMHC
ADVANCED PSYCHIATRIC GROUP PA
736 N MAGNOLIA AVE
ORLANDO, FL 32803
LANGUAGES SPOKEN:
ENGLISH
HOURS OF OPERATION:
MONDAY 8:00:00 AM - 5:00:00 PM
TUESDAY 8:00:00 AM - 5:00:00 PM
WEDNESDAY 8:00:00 AM - 5:00:00 PM
FRIDAY 8:00:00 AM - 2:00:00 PM
THURSDAY 8:00:00 AM - 5:00:00 PM
Map/Directions
SPECIALTY: COUNSELOR MENTAL HEALTH
Phone: 407.423.7149
WEB SITE: www.apghealth.com
MICHELLE CUMMINS LMHC
21 W COLUMBIA ST SUITE 201
ORLANDO, FL 32806
Map/Directions
SPECIALTY: COUNSELOR MENTAL HEALTH
Phone: 407.262.2220
ALEXIS GOOLKASIAN LMHC
ORLANDO HEALTH MEDICAL GROUP BEHAVIORAL HEALTH
21 W COLUMBIA ST SUITE 201
ORLANDO, FL 32806
LANGUAGES SPOKEN:
ENGLISH
HOURS OF OPERATION:
MONDAY 8:00:00 AM - 5:00:00 PM
TUESDAY 8:00:00 AM - 5:00:00 PM
WEDNESDAY 8:00:00 AM - 5:00:00 PM
FRIDAY 8:00:00 AM - 2:00:00 PM
THURSDAY 8:00:00 AM - 5:00:00 PM
Map/Directions
SPECIALTY: COUNSELOR MENTAL HEALTH
Phone: 407.262.2220
ALEXANDRIA M TURNBOW MA
MINDFUL PERCEPTIONS LLC
315 N WYMORE RD
WINTER PARK, FL 32789
LANGUAGES SPOKEN:
ENGLISH
HOURS OF OPERATION:
MONDAY 9:00:00 AM - 7:00:00 PM
TUESDAY 9:00:00 AM - 7:00:00 PM
WEDNESDAY 9:00:00 AM - 7:00:00 PM
THURSDAY 9:00:00 AM - 7:00:00 PM
FRIDAY 9:00:00 AM - 5:00:00 PM
SATURDAY 0:00:00 AM - 5:00:00 PM
Map/Directions
SPECIALTY: COUNSELOR MENTAL HEALTH
Phone: 407.490.3082
WEB SITE: www.mindful-perceptions.com
MARISOL COLLAZO LMHC
ME TIME THERAPY
7200 LAKE ELLENOR DR SUITE 252
ORLANDO, FL 32809
LANGUAGES SPOKEN:
ENGLISH
SPANISH
Map/Directions
SPECIALTY: COUNSELOR MENTAL HEALTH
Phone: 407.744.8599
E-Mail: therapymetime@gmail.com
WEB SITE: https://metimeth.com/
SCOTT JONES LMHC
NEW DIRECTIONS COUNSELING
931 W MORSE BLVD SUITE 100
WINTER PARK, FL 32789
LANGUAGES SPOKEN:
ENGLISH
Map/Directions
SPECIALTY: COUNSELOR MENTAL HEALTH
Phone: 561.918.2287
WEB SITE: www.newdirectionscounselingfl.com
Pompe Disease edit
Pompe disease is a rare, progressive, and often fatal muscular disease. The underlying pathology is a deficiency of the enzyme acid alpha-glucosidase (GAA) that hydrolyzes lysosomal glycogen. Pompe disease is a single disease which manifests as a clinical spectrum that varies with respect to age at onset, rate of disease progression, and extent of organ involvement. The advent of enzyme replacement therapy for this condition will necessitate early diagnosis. This guideline for the management of Pompe disease was developed as an educational resource for health care providers to facilitate the prompt and accurate diagnosis and treatment of patients. An international group of experts in various aspects of Pompe disease met to review the evidence base from the scientific literature and their expert opinions. Consensus was developed in each area of diagnosis, treatment and management in the development of this guideline. This management guideline specifically addresses evaluation and diagnosis across multiple organ systems (cardiology, pulmonary, gastrointestinal/nutrition, musculoskeletal, neurological) involved in both infantile and late-onset Pompe disease. Conditions to consider in a differential diagnosis stemming from presenting features and diagnostic algorithms are provided. Aspects of functional assessment, rehabilitation, nutritional management, emerging therapeutics, care coordination, nursing, genetic counseling, prenatal diagnosis and screening also are addressed. A guideline that will facilitate the appropriate diagnosis, treatment and management of patients with Pompe disease was developed. It will raise awareness of this condition and the presentation of patients across the disease spectrum in order to expedite their diagnosis so they can take advantage of emerging therapeutics such as enzyme replacement therapy (ERT).
Reference:
- Kishnani PS, Steiner RD, Bali D, Berger K, Byrne BJ, Case LE, Crowley JF, Downs S, Howell RR, Kravitz RM, Mackey J, Marsden D, Martins AM, Millington DS, Nicolino M, O'Grady G, Patterson MC, Rapoport DM, Slonim A, Spencer CT, Tifft CJ, Watson MS. Pompe disease diagnosis and management guideline. Genet Med. 2006 May;8(5):267-88. doi: 10.1097/01.gim.0000218152.87434.f3. Erratum in: Genet Med. 2006 Jun;8(6):382. ACMG Work Group on Management of Pompe Disease [removed]; Case, Laura [corrected to Case, Laura E]. PMID: 16702877; PMCID: PMC3110959.
Management
Cardiology
- The common cardiac issues occurring in Pompe disease include cardiomyopathy, heart failure and arrhythmia.
- Cardiology Recommendations:
- Chest x-ray at regular intervals (see pulmonary recommendations).
- Obtain an initial echocardiogram to evaluate the extent of cardiomyopathy, of regular intervals.
- Medical management may be useful based on stage of cardiomyopathy.
- Avoid drastic changes in fluid status, either through dehydration or fluid overload.
- Obtain a twenty-four hour ambulatory ECG at baseline and regular intervals as patients are at risk for life-threatening arrhythmias.
- Monitor for arrhythmias, including in patients on ERT.
Pulmonary
- As Pompe disease progresses, the muscles weaken leading to low lung volumes, an impaired cough, blood gas abnormalities, and sleep-disordered breathing.
- Pulmonary Recommendations:
- Clinical assessment of respiratory status, both asleep and awake, should be performed at each medical visit.
- When feasible, assessment of pulmonary function and gas exchange should be performed at diagnosis, annually, and at every visit or with changes in patients’ clinical condition.
- Chest radiographs should be obtained upon diagnosis and when clinically indicated.
- Polysomnography should be performed upon diagnosis and when clinically indicated in infantile and late onset Pompe disease.
- Maximizing clearance of airway secretions should routinely be performed.
- Assessment of respiratory function during sleep needs to be made whenever the patient complains of daytime sleepiness, unexplained fatigue or has observed apneas during sleep, or when vital capacity falls below 40–50% predicted.
- Supplemental oxygen and/or noninvasive positive pressure ventilation should be prescribed based on underlying ventilatory abnormalities such as hypoxemia, obstructive sleep apnea, and hypoventilation. Treatment modality should be based on a firm diagnosis of the type of respiratory events seen during sleep.
- All pulmonary infections should be aggressively managed.
Gastrointestinal/Nutrition
- Patients with Pompe disease have feeding and swallowing difficulties and often fail to thrive.
- Gastrointestinal/Nutrition Recommendations:
- Obtain videofluoroscopic swallowing assessment and evaluation for GE reflux to guide management of feeding (oral/gavage feeding) at baseline and as clinically indicated.
- Provide oral stimulation and non-nutritive sucking for infants who are nonoral feeders.
- Monitor growth parameters carefully.
- Provide adequate nutrition (high protein consisting of 20–25% protein) with attention to vitamins and minerals.
- Encourage appropriate exercise in consultation with a physical therapist with experience in Pompe disease.
Musculoskeletal/Functional/Rehabilitation
- Musculoskeletal involvement in Pompe disease is characterized by progressive weakness that leads to decreased motor function, altered postural tendencies and positioning, and the use of compensatory patterns of movement. Secondary musculoskeletal impairments such as contracture, deformity, and osteoporosis can occur and further compromise function.
- Musculoskeletal/Functional/Rehabilitation Recommendations:
- Monitor cardiorespiratory status and response to position and activity with pulse oximetry during evaluation and treatment initially and with changes in status or activity.
- Screen for osteopenia/osteoporosis with DEXA and follow-up as needed.
- Assess musculoskeletal impairments, functional deficits, levels of disability, and societal participation at regular intervals and as needed, including radiographs as needed for monitoring of scoliosis, hip stability, and long bone integrity.
- Enhance Muscle Function:
- increase biomechanical advantage for movement:
- provide practice, movement, and gentle strengthening within limits of physiological stability.
- provide rests as needed to avoid overexertion.
- Follow Guidelines For Strengthening From Other Progressive Muscle Diseases:
- submaximal, functional, and aerobic exercise recommended.
- avoid excessive resistive and eccentric exercise.
- avoid overwork weakness.
- avoid disuse atrophy.
- allow compensatory movements necessary for function, but prevent negative results (contracture and deformity).
- Prevent/Minimize/Correct 2° Musculoskeletal Impairment (Contracture/Deformity):
- stretching/positioning.
- orthotic intervention and splinting.
- seating systems/standers.
- Optimize function with adaptation and assistive technology as needed.
- Educate the patient and family about the natural history and recommendations for intervention.
Neurological
- Neurology Recommendations:
- Motor and functional assessments are recommended to establish a baseline with repeat testing at 3–6 month intervals for children under age five years, and annually in older children and adults, except where additional testing is clinically indicated by change in function or failure to make expected progress.
- Perform needle electromyography (EMG) in initial evaluation to determine presence of denervation as evidence of anterior horn cell involvement.
- Perform nerve conduction studies at initial evaluation.
- Perform hearing tests including behavioral assessment otoacoustic emissions, tympanometry and auditory evoked potentials (ABR/BAER) using air and bone conducted stimuli to establish baseline and repeat age and condition appropriate hearing testing, annually, as clinically indicated and following medical/surgical intervention.
General Medical Care Recommendations:
- There should be strict hand washing and aggressive management of infections.
- Routine immunizations, including pneumococcal vaccination, should be used.
- There should be influenza vaccination for patients and other household contacts and use of palivizumab when indicated.
- There should be careful use of over-the-counter medications and concomitant medications.
Surgery/Anesthesia Recommendations:
- Anesthetic procedure only when absolutely necessary
- Consolidation of procedures requiring anesthesia, to reduce risk of repeated anesthetic exposures
- Judicious use of anesthetics, with precautions followed due to underlying cardiomyopathy
- Procedures at centers with experience anesthetizing patients with Pompe disease or consulting with experts
- Avoidance of intubation, if possible
Reference:
- Kishnani PS, Steiner RD, Bali D, Berger K, Byrne BJ, Case LE, Crowley JF, Downs S, Howell RR, Kravitz RM, Mackey J, Marsden D, Martins AM, Millington DS, Nicolino M, O'Grady G, Patterson MC, Rapoport DM, Slonim A, Spencer CT, Tifft CJ, Watson MS. Pompe disease diagnosis and management guideline. Genet Med. 2006 May;8(5):267-88. doi: 10.1097/01.gim.0000218152.87434.f3. Erratum in: Genet Med. 2006 Jun;8(6):382. ACMG Work Group on Management of Pompe Disease [removed]; Case, Laura [corrected to Case, Laura E]. PMID: 16702877; PMCID: PMC3110959.
Study: Open-label placebos—a systematic review and meta-analysis of experimental studies with non-clinical samples edit
Notes:
- The effect size of open placebo, on stuff ranging from pain to depression, is around 0.43.
Abstract:
The use of open-label placebos (OLPs) has shown to be effective in clinical trials. We conducted a systematic review and meta-analysis to examine whether OLPs are effective in experimental studies with non-clinical populations.
We searched five databases on April 15, 2021. We conducted separate analyses for self-reported and objective outcomes and examined whether the level of suggestiveness of the instructions influenced the efficacy of OLPs. Of the 3573 identified records, 20 studies comprising 1201 participants were included, of which 17 studies were eligible for meta-analysis.
The studies investigated the effect of OLPs on well-being, pain, stress, arousal, wound healing, sadness, itchiness, test anxiety, and physiological recovery.
- We found a significant effect of OLPs for self-reported outcomes (k=13; standardized mean difference (SMD)=0.43; 95% CI=0.28, 0.58; I2=7.2%), but not for objective outcomes (k=8; SMD=−0.02; 95% CI=−0.25, 0.21; I2=43.6%).
- The level of suggestiveness of the instructions influenced the efficacy of OLPs for objective outcomes (p=0.02), but not for self-reported outcomes.
The risk of bias was moderate for most studies, and the overall quality of the evidence was rated low to very low.
In conclusion, OLPs appear to be effective when examined in experimental studies. However, further research is needed to better understand the mechanisms underlying OLPs.
Reference:
- Spille L, Fendel JC, Seuling PD, Göritz AS, Schmidt S. Open-label placebos-a systematic review and meta-analysis of experimental studies with non-clinical samples. Sci Rep. 2023 Mar 4;13(1):3640. doi: 10.1038/s41598-023-30362-z. PMID: 36871028; PMCID: PMC9985604.
Study: Listening to Prozac but hearing placebo: A meta-analysis of antidepressant medication edit
Abstract
Mean effect sizes for changes in depression were calculated for 2,318 patients who had been randomly assigned to either antidepressant medication or placebo in 19 double-blind clinical trials. As a proportion of the drug response, the placebo response was constant across different types of medication (75%), and the correlation between placebo effect and drug effect was 0.90. These data indicate that virtually all of the variation in drug effect size was due to the placebo characteristics of the studies. The effect size for active medications that are not regarded to be antidepressants was as large as that for those classified as antidepressants, and in both cases, the inactive placebos produced improvement that was 75% of the effect of the active drug. These data raise the possibility that the apparent drug effect (25% of the drug response) is actually an active placebo effect. Examination of pre-post effect sizes among depressed individuals assigned to no-treatment or wait-list control groups suggest that approximately one quarter of the drug response is due to the administration of an active medication, one half is a placebo effect, and the remaining quarter is due to other nonspecific factors.
Key takeaways
- Approximately 75% of the antidepressant drug response is attributed to placebo effects.
- The correlation between drug and placebo responses is exceptionally high at r = 0.90.
- Active medications not classified as antidepressants show similar effect sizes to traditional antidepressants.
- Only 25% of the drug response may be due to actual pharmacological effects of the medication.
- The study reviews data from 19 trials involving 2,318 patients to analyze antidepressant efficacy.
Reference:
- Kirsch, I., & Sapirstein, G. (1998). Listening to Prozac but hearing placebo: A meta-analysis of antidepressant medication. Prevention & Treatment, 1(2), Article 2a. https://doi.org/10.1037/1522-3736.1.1.12a
Study: Efficacy of antidepressants: a re-analysis and re-interpretation of the Kirsch data edit
Recently there has been much debate on the true usefulness of antidepressant therapy especially after the publication of a meta-analysis by Kirsch et al. (PLoS Medicine 2008, 5, e45). The aim of the current paper was to recalculate and re-interpret the data of that study.
Effect-size and mean-score changes were calculated for each agent separately as well as pooled effect sizes and mean changes on the basis of the data reported by Kirsch et al.
- The weighted mean improvement was (depending on the method of calculation) 10.04 or 10.16 points on the Hamilton Depression Rating Scale (HAMD) in the drug groups, instead of 9.60, and thus the correct drug–placebo difference is 2.18 or 2.68 instead of 1.80.
- Kirsch et al. failed to report that that the change in HAMD score was 3.15 or 3.47 points for venlafaxine and 3.12 or 3.22 for paroxetine, which are above the NICE threshold.
- Still the figures for fluoxetine and nefazodone are low.
Thus it seems that the Kirsch et al.’s meta-analysis suffered from important flaws in the calculations; reporting of the results was selective and conclusions unjustified and overemphasized.
Overall the results suggest that although a large percentage of the placebo response is due to expectancy this is not true for the active drug and effects are not additive. The drug effect is always present and is unrelated to depression severity, while this is not true for placebo.
Reference:
- Fountoulakis KN, Möller HJ. Efficacy of antidepressants: a re-analysis and re-interpretation of the Kirsch data. Int J Neuropsychopharmacol. 2011 Apr;14(3):405-12. doi: 10.1017/S1461145710000957. Epub 2010 Aug 27. PMID: 20800012.
Study: The effect of vitamin D supplementation on depression: a systematic review and dose–response meta-analysis of randomized controlled trials edit
Notes:
- The upper range of uncertainty is lowest at 5000 IU (International Units) of Vitamin D a day, with an estimated effect size of 1.82, with a 95% uncertainty range, from 0.98 to 2.66.
The impact of vitamin D supplementation on depressive symptoms remains uncertain. This study aimed to investigate the dose-dependent effects of vitamin D supplementation on depressive and anxiety symptoms in adults.
We systematically searched PubMed, Scopus, and Web of Science up to December 2022 to identify randomized controlled trials evaluating the effects of vitamin D3 supplementation on depression and anxiety symptoms in adults.
Using a random-effects model, we calculated the standardized mean difference (SMD) for each 1000 IU/day vitamin D3 supplementation. The GRADE tool assessed the certainty of evidence. Our analysis included 31 trials with 24189 participants.
- Each 1000 IU/day vitamin D3 supplementation slightly reduced depressive symptoms in individuals with and without depression (SMD: −0.32, 95% CI −0.43 to −0.22; GEADE = moderate).
- The effect was more pronounced in those with depressive symptoms (SMD: −0.57, 95% CI −0.69 to −0.44; n = 15).
- The greatest reduction occurred at 8000 IU/day (SMD: −2.04, 95% CI −3.77 to −0.31).
- Trials with follow-up ⩽8 weeks (SMD: −0.45, 95% CI −0.70 to −0.20; n = 8) and 8 to ⩽24 weeks (SMD: −0.47, 95% CI −0.70 to −0.24; n = 15) showed stronger effects compared to those lasting 24 to ⩽52 weeks (SMD: −0.13, 95% CI −0.28 to 0.02; n = 5) or longer than 52 weeks (SMD: 0.14, 95% CI −0.16 to 0.44; n = 3) (p group difference <0.001).
- Vitamin D3 supplementation had no significant effects on anxiety symptoms.
In summary, this study suggests that vitamin D3 supplementation may effectively reduce depressive symptoms in short term. Further high-quality trials are warranted for a conclusive assessment of its impact on anxiety.
Reference:
- Ghaemi S, Zeraattalab-Motlagh S, Jayedi A, Shab-Bidar S. The effect of vitamin D supplementation on depression: a systematic review and dose-response meta-analysis of randomized controlled trials. Psychol Med. 2024 Nov 18;54(15):1-10. doi: 10.1017/S0033291724001697. Epub ahead of print. PMID: 39552387; PMCID: PMC11650176.
Study: Risk of suicide, suicide attempt, and suicidal ideation among people with vitamin D deficiency: a systematic review and metaanalysis edit
Background
- Evidence shows that vitamin D affects brain function. Transcription of over 1000 genes is known to be controlled by vitamin D, potentially contributing to the neurotrophic and neuroprotective effects that can influence suicidal behavior. Several investigations with contradicting findings have identified an association between suicidal behaviors (SBs) or depressive symptoms and low vitamin D levels. This meta-analysis aimed to analyze the pooled association between vitamin D deficiency and the risk of suicide, suicide attempt (SA), and suicidal ideation (SI).
Methods
- A systematic search was performed through PubMed, Web of science (ISI), Scopus, Embase, and grey literature up to 10 October 2024. Meta-analysis included observational studies that assessed the association between SBs and vitamin D blood serum level and/or vitamin D deficiency. After screening and quality assessment, meta-analysis and sensitivity analysis using random effects model were carried out to estimate the pooled odds ratios (ORs) for the risk of suicide, SA, and SI. We also calculated pooled standard mean difference (SMD) of vitamin D levels between control subjects and patients with SBs.
Results
- A total of 14,095 records were identified. Finally, 13 studies participating 515,406 subjects were included in the meta-analysis after eligibility assessment.
- Vitamin D deficiency non-significantly increased the risk of suicide, SA, and SI (OR=1.7; 95% CI: 0.93 – 3.12), (OR=1.65; 95% CI: 0.98 – 2.80), and (OR=1.15; 95% CI: 0.94 – 1.41), respectively.
- However, levels of vitamin D in patients with SBs were significantly lower than in controls without any SBs (SMD=-0.69; 95% CI: -0.89 – -0.49).
Conclusion
- The results of this meta-analysis indicated that vitamin D levels are lower among patients with SBs. These findings can inform suicide prevention programs, particularly for target groups experiencing significant vitamin D deficiency.
Reference:
- Yu J, Mohammad SN, Khachatryan LG, Mohammed JS, Menon SV, Kaur M, Sapaev I, Jabir MS, Husseen B, Azizi H. Risk of suicide, suicide attempt, and suicidal ideation among people with vitamin D deficiency: a systematic review and meta-analysis. BMC Psychiatry. 2025 Feb 26;25(1):177. doi: 10.1186/s12888-025-06613-w. PMID: 40000977; PMCID: PMC11863558.
Effect sizes on Depression edit
See effect calculator: Effect size converter
The effect sizes on depression:
- The best antidepressant: +0.417
- like your mental health grade going from F to F+, or C to C+
- 1500mg of ≥60%-EPA Omega-3: +0.558
- like your mental health grade going from F to D–, or C to B–
- 4000 IU of Vitamin D: +0.98
- like your mental health grade going from F to D, or C to B
- Any mainstream "bona-fide" psychotherapy (CBT, Psychodynamic, Humanist, Solutions-Focused): +0.35, source: Kamenov et al 2016
- like going from C to C+
- Aerobic/Cardio Exercise: +0.79, source Ioannis et al 2018
- like going from C to B– (dose: "45 minutes, at moderate intensity, three times/week" ⇒ ~20 min/day)
- Good Sleep: +1.10(???), a lot of interpretation & calculations
- like going from C to B (dose: going from moderate insomnia to healthy sleep)
- Bright Light Therapy: +0.487, source Menegaz de Almeida et al 2025 (the above paper reports Odds Ratio of 2.42, which converts to Cohen's d effect size of +0.487)
- like going from C to C+
- (dose: 10,000 lux, 30 min a day)
- Mindfulness Meditation: +0.42, source Breedvelt et al 2019
- like going from C to C+ (dose: 7 weeks, "153 min each week" ⇒ ~20 min/day)
Reference:
Study: Cholesterol-lowering effects of oats induced by microbially produced phenolic metabolites in metabolic syndrome: a randomized controlled trial edit
Oats have various positive effects on human health, but the underlying mechanisms are not fully understood.
To identify oat-microbiome-host interactions contributing to metabolic improvements, we conducted two randomized controlled dietary interventions in parallel-design in individuals with metabolic syndrome, comparing a short-term, high-dose and a six-week, moderate oat intake with respective controls (DRKS00022169).
Both oat diets lead to an increase in plasma ferulic acid (0.64 [0.26, 1.02], P=0.002; 0.55 [0.21, 0.89], P=0.003), while the high-dose oat-diet also increased dihydroferulic acid (1.23 [0.44, 2.01], P=0.003).
Here we show that microbial phenolic metabolites are driving factors for the cholesterol-lowering effect of oats, which might be of relevance since short-term, high-dose oat-diet is a suitable approach to alleviate obesity-related lipid disorders.
Reference:
- Two days of oatmeal reduce cholesterol level — University of Bonn
- Klümpen L, Mantri A, Philipps M, Seel W, Schlautmann L, Yaghmour MH, Wiemann V, Stoffel-Wagner B, Coenen M, Weinhold L, Hasenauer J, Fließwasser T, Burgdorf S, Thiele C, Stehle P, Simon MC. Cholesterol-lowering effects of oats induced by microbially produced phenolic metabolites in metabolic syndrome: a randomized controlled trial. Nat Commun. 2026 Jan 14;17(1):598. doi: 10.1038/s41467-026-68303-9. PMID: 41535271; PMCID: PMC12808737.
Study: Safety and Efficacy of Glucagon-Like Peptide-1 Receptor Agonists Use in Elderly People With Obesity—A Meta-Analysis
Objective
- This meta-analysis evaluates the safety and efficacy of glucagon-like peptide-1 receptor agonists (GLP-1 RA) for the treatment of older adults with obesity compared to younger individuals.
Methods
- A systematic review was conducted following PRISMA guidelines (PROSPERO CRD420251074381). PubMed, Embase, and Scopus were searched until May 17, 2025, for randomized controlled trials and observational studies assessing GLP-1 RA in adults ≥65years with obesity with or without type 2 diabetes. Random effects meta-analyses calculated the log odds ratios (LOR) for dichotomous outcomes and the mean differences (MD) for continuous outcomes, with equivalence testing via two one-sided tests (TOST) and meta-regression for baseline adjustments.
Results
- Five studies involving 1229 participants were included. No significant difference in serious adverse events was found between older and younger adults (pooled LOR: 0.06, p=0.9).
- Older adults had a trend toward lower frequency of nausea (LOR: −0.44, p=0.06) but higher incidence of constipation (LOR: 0.72, p=0.02) and hypoglycemia (LOR: 0.97, p<0.001).
- Efficacy in metabolic and weight control was comparable.
- Additionally, one study suggested that liraglutide could reduce fat mass without worsening sarcopenia.
Conclusions
- GLP-1 RA therapy seems to be safe and effective in older adults with obesity, achieving similar effects on weight loss and glycemic control as in younger individuals.
Reference:
- I. Rego de Figueiredo, F. S. Simas, A. Ghiletchi, J. Oliveira Torres, and J. Silva-Nunes, “ Safety and Efficacy of Glucagon-Like Peptide-1 Receptor Agonists Use in Elderly People With Obesity—A Meta-Analysis,” Obesity (2026): 1–11, https://doi.org/10.1002/oby.70098.
Study: Heritability of intrinsic human life span is about 50% when confounding factors are addressed edit
How heritable is human life span? If genetic heritability is high, longevity genes can reveal aging mechanisms and inform medicine and public health. However, current estimates of heritability are low—twin studies show heritability of only 20 to 25%, and recent large pedigree studies suggest it is as low as 6%. Here we show that these estimates are confounded by extrinsic mortality—deaths caused by extrinsic factors such as accidents or infections. We use mathematical modeling and analyses of twin cohorts raised together and apart to correct for this factor, revealing that heritability of human life span due to intrinsic mortality is above 50%. Such high heritability is similar to that of most other complex human traits and to life-span heritability in other species.
Reference:
- Ben Shenhar et al. ,Heritability of intrinsic human life span is about 50% when confounding factors are addressed.Science391,504-510(2026).doi:10.1126/science.adz1187
Study: Effect of exercise on depression and anxiety symptoms: systematic umbrella review with meta-meta-analysis edit
Objective
- To synthesise meta-analytic outcomes from randomised controlled trials examining exercise effects on depression and anxiety across all population groups, including children and adults with both clinically diagnosed and subclinical symptoms, excluding those with pre-existing chronic physiological conditions.
Design
- Meta-meta-analysis (Preferred Reporting Items for Overviews of Reviews (PRIOR) framework).
Data sources
- Five electronic databases were searched for eligible meta-analyses published from inception to 31 July 2025.
Eligibility criteria for selecting studies
- Meta-analyses of randomised controlled trials examining exercise interventions for the management of depression and anxiety symptoms were included. To avoid contamination effects, meta-analyses exclusively focused on populations in which chronic physiological conditions were excluded. Study selection was undertaken in duplicate by two independent reviewers.
Results
- 63 studies (81 meta-analyses, 1079 component studies and 79 551 participants) were included. Exercise reduced depression (standardised mean difference (SMD)=−0.61, 95% CI −0.69 to −0.54) and anxiety (SMD=−0.47, 95% CI −0.59 to −0.36) symptoms, with aerobic exercise demonstrating the most substantial impact on both depression and anxiety symptoms.
- The greatest benefits by population group for depression were seen in emerging adults aged 18–30 and postnatal women.
- Greater reductions in depression were associated with exercise in group and supervised settings.
- Exercise of shorter duration and at lower intensity was most strongly associated with anxiety reduction.
Conclusion and relevance
- The findings of the study support that exercise based interventions, in all formats and parameters, can help mitigate depression and anxiety symptoms across all population categories. These results can help health professionals provide targeted, cost effective, evidence based support that aligns with individual profiles and preferences.
Reference:
- Munro NR, Teague S, Somoray K, et alEffect of exercise on depression and anxiety symptoms: systematic umbrella review with meta-meta-analysisBritish Journal of Sports Medicine Published Online First: 10 February 2026. doi: 10.1136/bjsports-2025-110301
Evidence Based Ways To Increase Testosterone Using Lifestyle Changes
Evidence Based Ways To Increase Testosterone Using Lifestyle Changes
- Exercise and Resistance Training
- Engaging in regular resistance training can significantly boost testosterone levels, especially when performed at moderate to high intensity. These workouts trigger short-term testosterone spikes and support long-term hormonal balance by improving body composition and reducing insulin resistance.
- Even lifting weights twice a week for 30-40 minutes can make a meaningful difference.
- Prioritize Sleep Quality
- Testosterone production primarily occurs during sleep. Chronic sleep deprivation is strongly linked to lower testosterone levels.
- The goal is to aim for 7-9 hours of restful, high-quality sleep per night.
- Maintain a Healthy Weight
- Excess body fat is associated with decreased testosterone.
- Weight loss for those with extra weight (5-10% of body weight) can lead to measurable increases in testosterone.
- Eat a Balanced, Nutrient-Rich Diet
- Focus on whole, unprocessed foods rich in healthy fats (e.g., olive oil, avocados, nuts), high-quality protein (e.g., eggs, fish, lean meats), and complex carbohydrates.
- Avoid low-fat diets, which have been shown to reduce testosterone.
- Include foods high in zinc, vitamin D, and magnesium, as deficiencies in these nutrients are linked to lower testosterone.
- Manage Stress and Cortisol
- Chronic stress elevates cortisol, which suppresses testosterone.
- Practice stress-reduction techniques such as mindfulness, meditation, or spending time in nature to maintain hormonal balance. You can also do deep breathing exercises like Box breathing or 4-7-8 breathing.
- Avoid Hormone-Disrupting Chemicals and Alcohol
- Avoid excessive alcohol consumption.
- Alcohol can drop testosterone levels within just five days and disrupt endocrine function.